A Scheduling Mechanism Based on Optimization Using IoT-Tasks Orchestration for Efficient Patient Health Monitoring
Abstract
:1. Introduction
- Development of a scheduling mechanism based on optimization and time-constraint-aware scheduling techniques using a real-time IoT-based task orchestration architecture to efficiently monitor vital signs data of remote patients;
- Development of an optimization module based on objective function to minimize information lost during context switching of sensing devices and minimize the sensor’s failure rate to improve recovery and reliability of the proposed smart PHMS;
- Development of a PSO-enabled Time-constraint aware scheduling mechanism using a real-time IoT-based task orchestration architecture to schedule healthcare tasks efficiently;
- Development of real-time IoT-based task orchestration architecture to handle the deployment of critical and emergent healthcare tasks effectively and dynamically;
- Utilization of different evaluation metrics are to evaluate the effectiveness of the proposed smart PHMS, such as RTT, latency, throughput, response time, and task drop and starvation rates.
2. Related Work
3. Materials and Methods
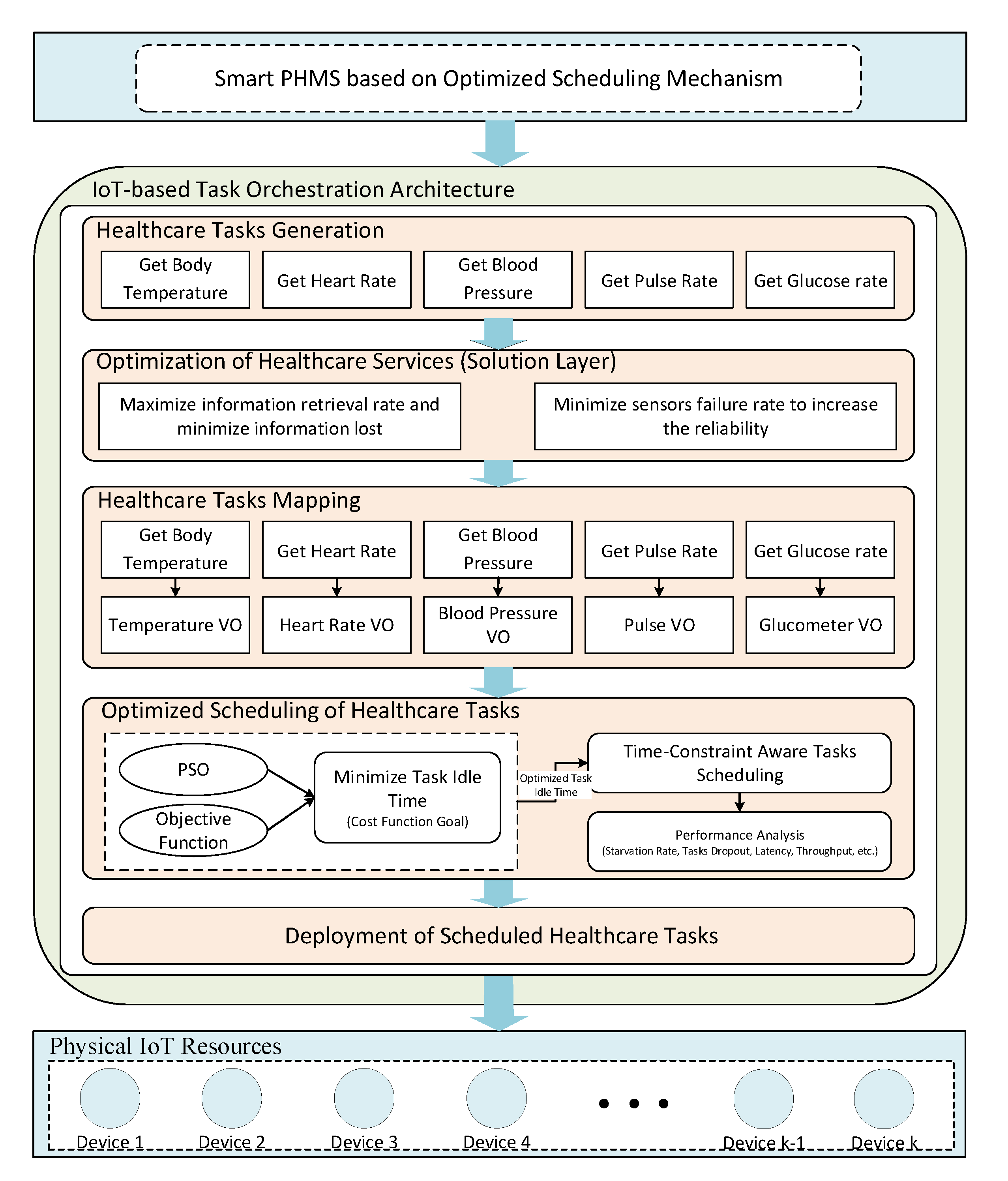
3.1. Design of Proposed Smart PHMS
3.2. Mathematical Formulations for Smart PHMS
3.3. Task Orchestration Architecture for Smart PHMS
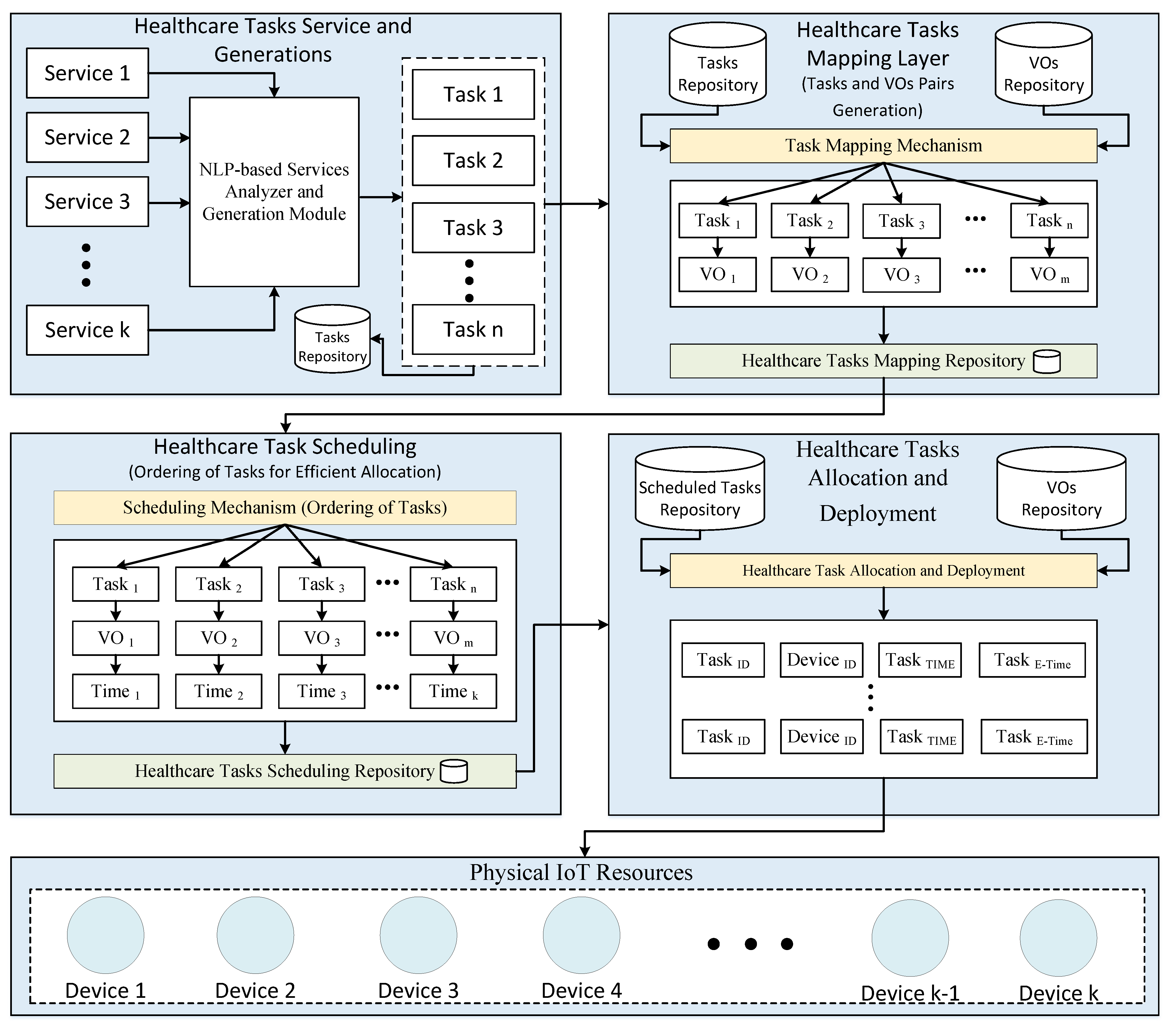
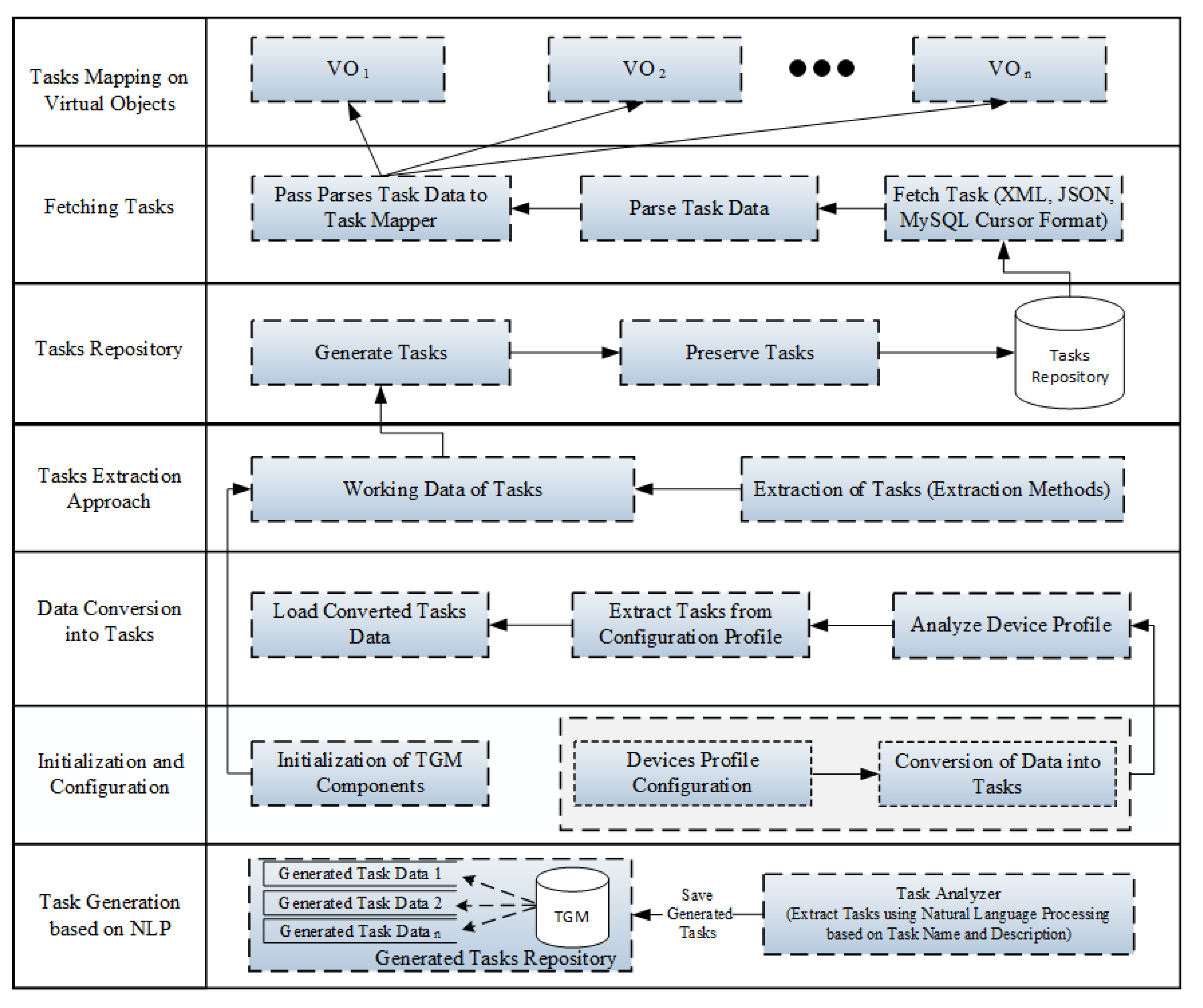
3.3.1. Service Analysis and Decomposition of Health Tasks
3.3.2. Virtualization of IoT Resources
3.3.3. Task/Virtual Object Pair Generation and Mapping
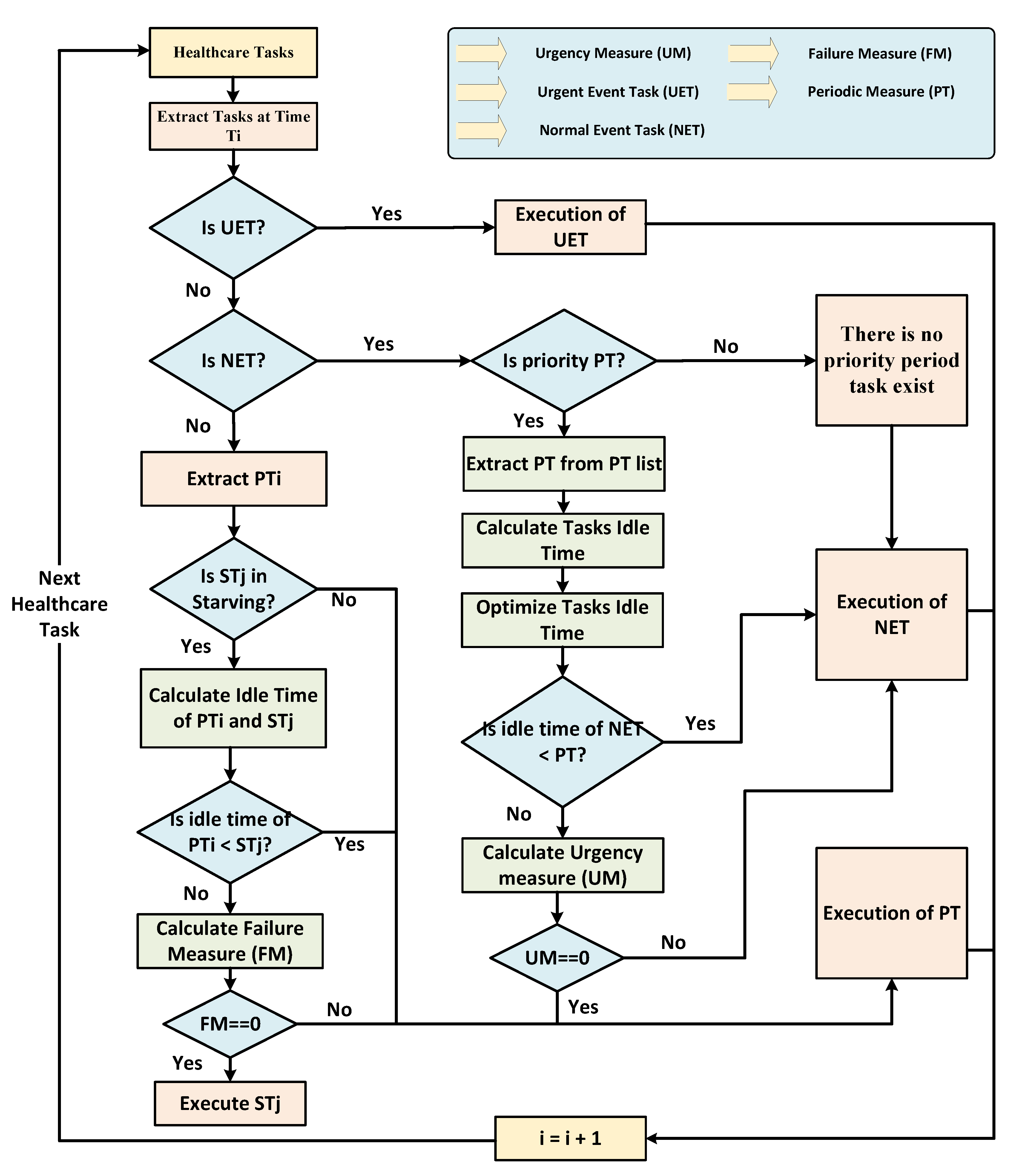
3.3.4. Healthcare Task Scheduling for Efficient Resource Utilization
- must be greater than 0 and less than , For instance, .
- of healthcare task must be greater than 0 .
| Algorithm 1 Calculation of Failure Measure for Scheduling of Periodic Tasks. |
| function CALCULATEFAILUREMEASURE() |
| for do |
| end for |
| if then Return 1 |
| else |
| Return 0 |
| end if |
| end function |
| Algorithm 2 An Optimized Time-Constraint Aware Scheduling Mechanism | |
| function HEALTHCARETASKSSCHEDULING (, ) | |
| ▹ Input: Array of the given tasks and and is the time step at which tasks arrived in the queue for the execution. | |
| ▹ Urgency measure | |
| ▹ Failure measure | |
| if then | ▹ Urgent Event Task (UET) |
| Execute the UET | |
| else if then | ▹ Normal Event Task (NET) |
| if then | ▹ Periodic Task(PT) |
| Extract at time slot i from | |
| Calculate and using Equation (12) | |
| if then | |
| Execute the NET with nearest deadline | |
| else | |
| Calculate using Equation (14) | |
| if then | |
| Execute the with nearest deadline | |
| else | |
| Execute the NET with nearest deadline | |
| end if | |
| end if | |
| else | |
| Execute the NET with nearest deadline | |
| end if | |
| else if then | |
| if then | ▹ represents starved task |
| Extract at time interval i from | |
| Calculate and using Equation (12) | |
| if then | |
| Execute the High Priority PT | |
| else | |
| Calculate using Algorithm 1 | |
| if then | |
| Execute Low Priority Starving Task | |
| else | |
| Execute the High Priority PT | |
| end if | |
| end if | |
| else | |
| Execute the High Priority PT | |
| end if | |
| else | |
| Invalid Task Type | |
| end if | |
| end function | |
3.3.5. Allocation and Deployment Process of Scheduled Healthcare Tasks
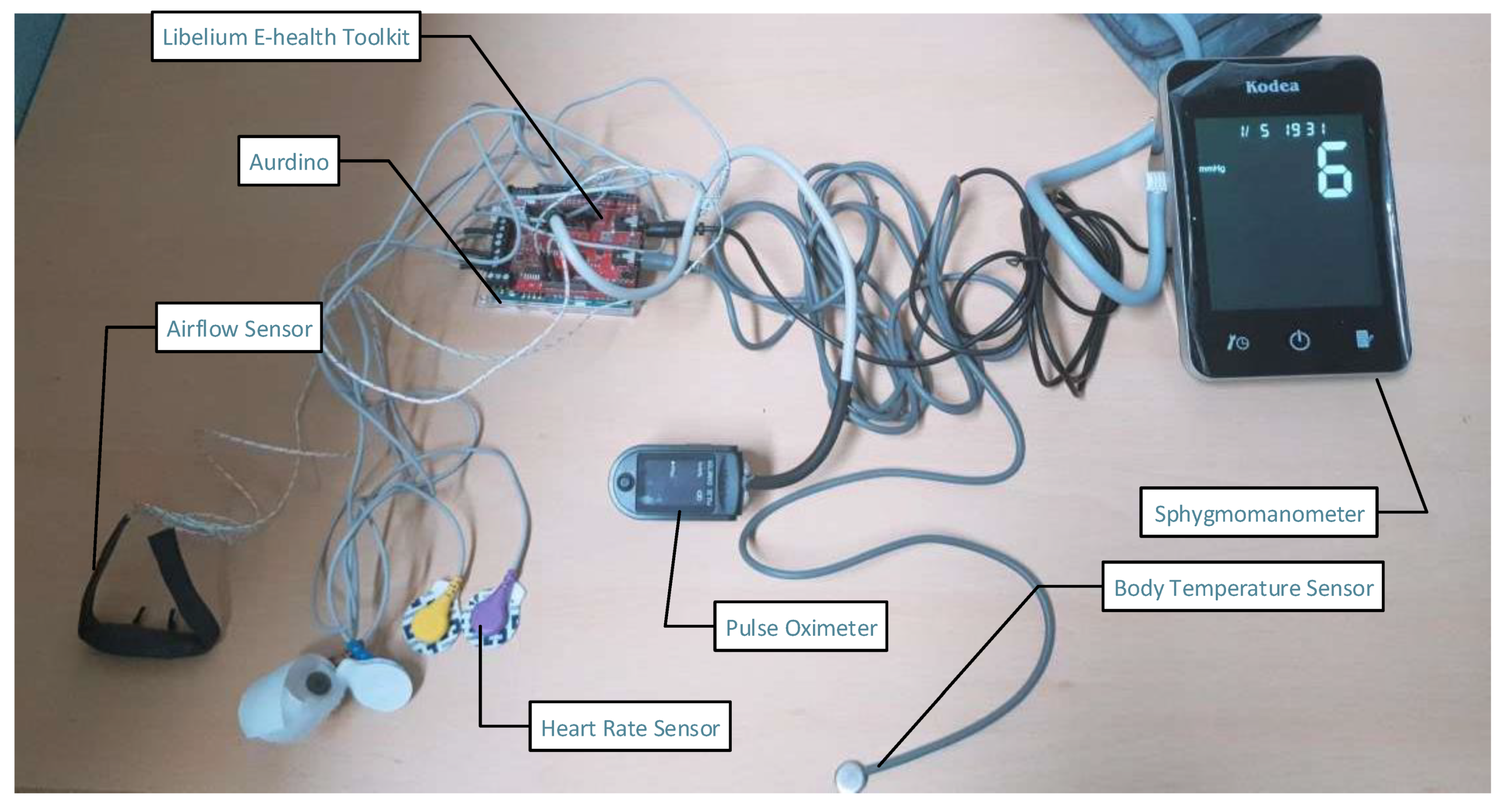
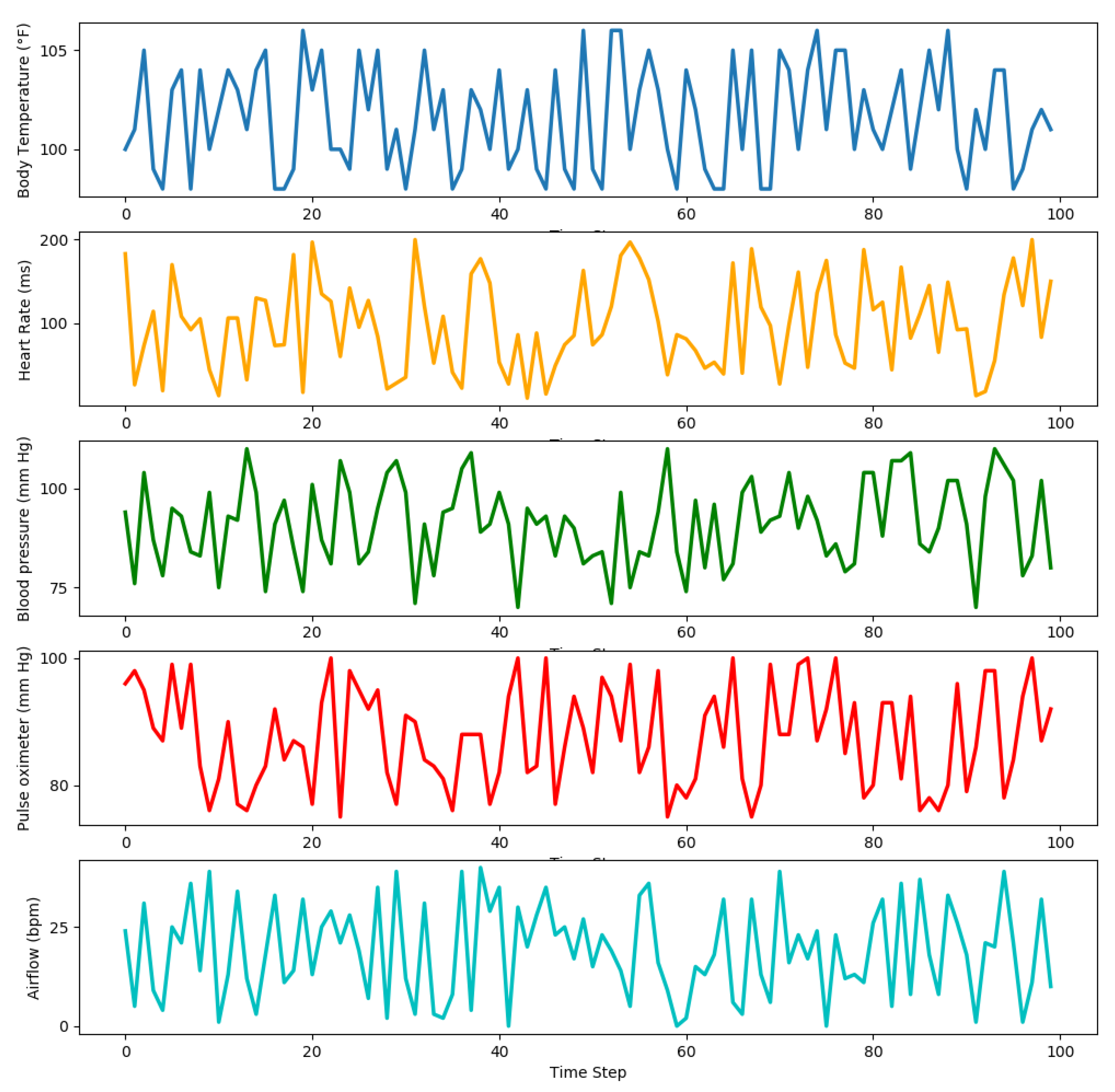
4. Experimental Environment of Proposed Smart PHMS
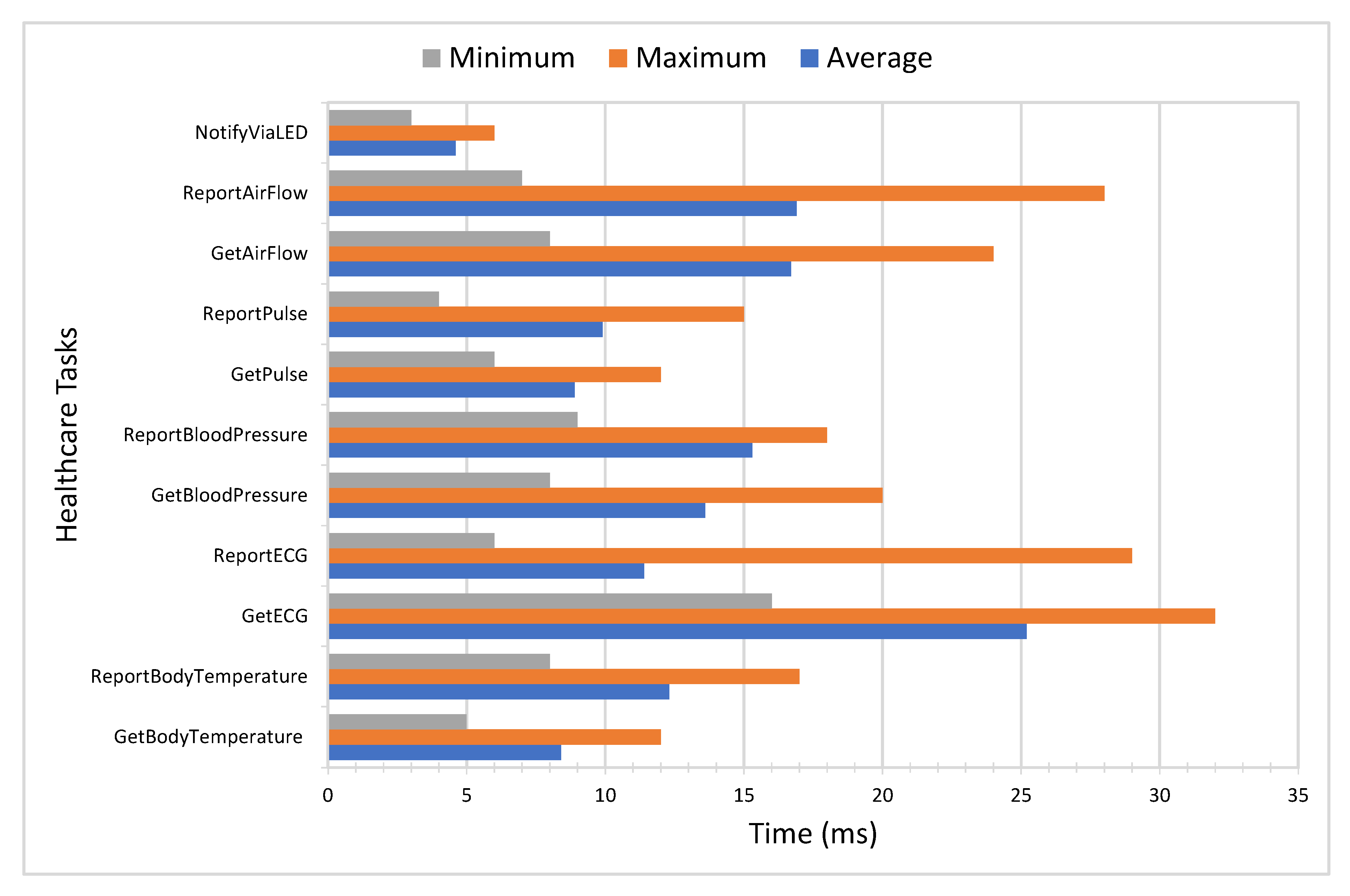
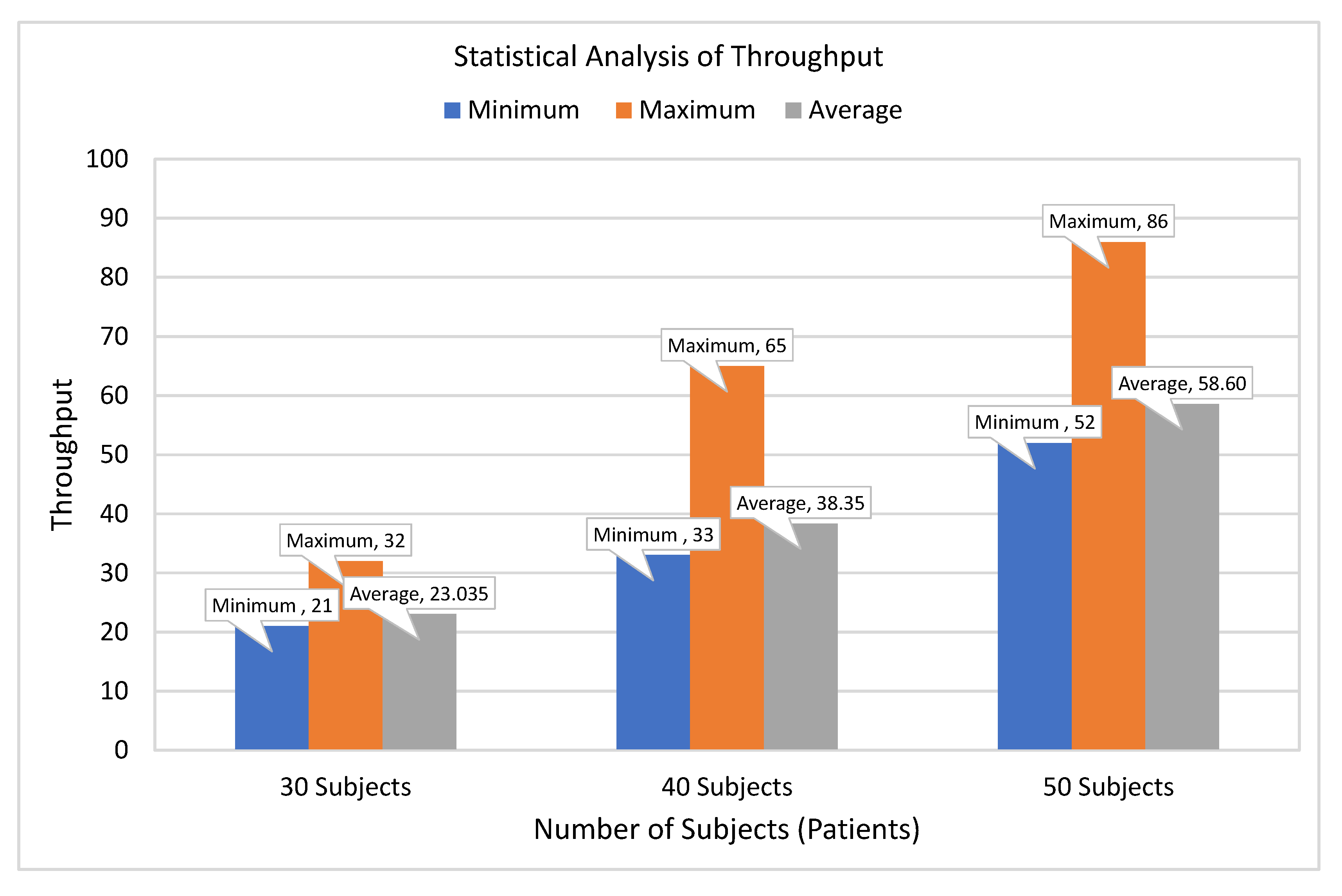
5. Performance and Comparative Analysis
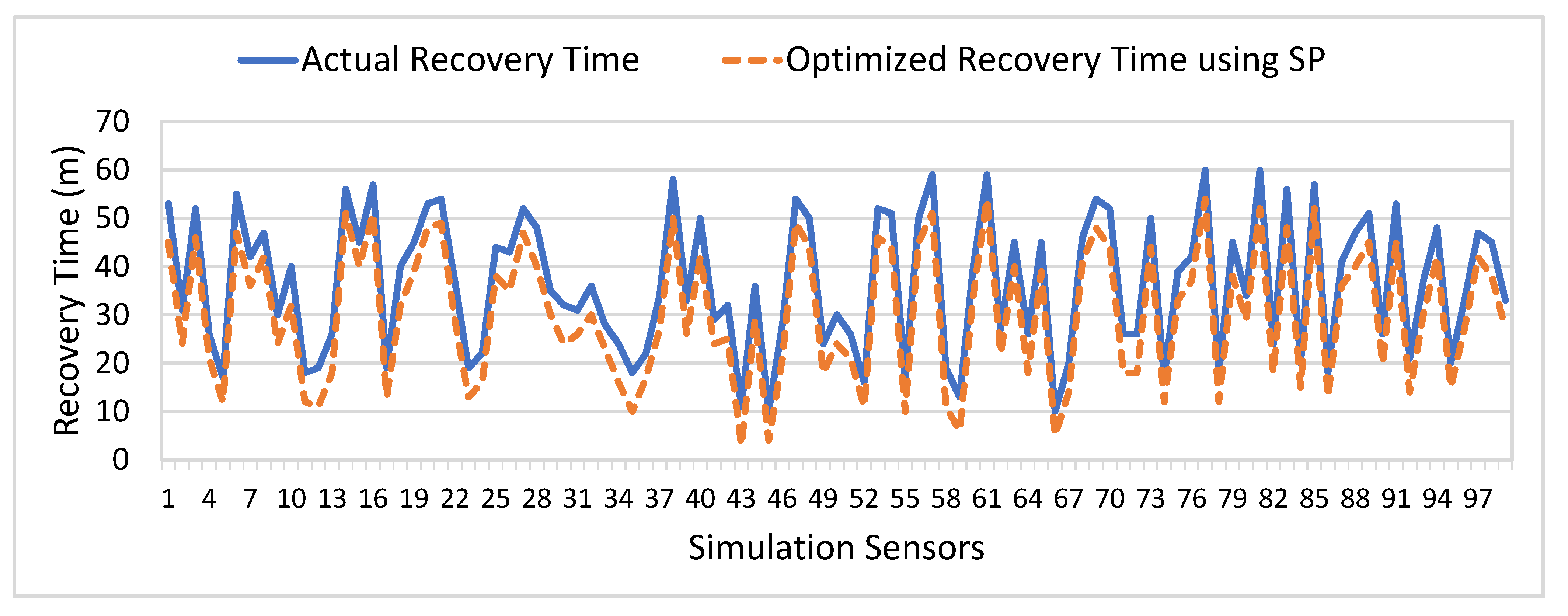
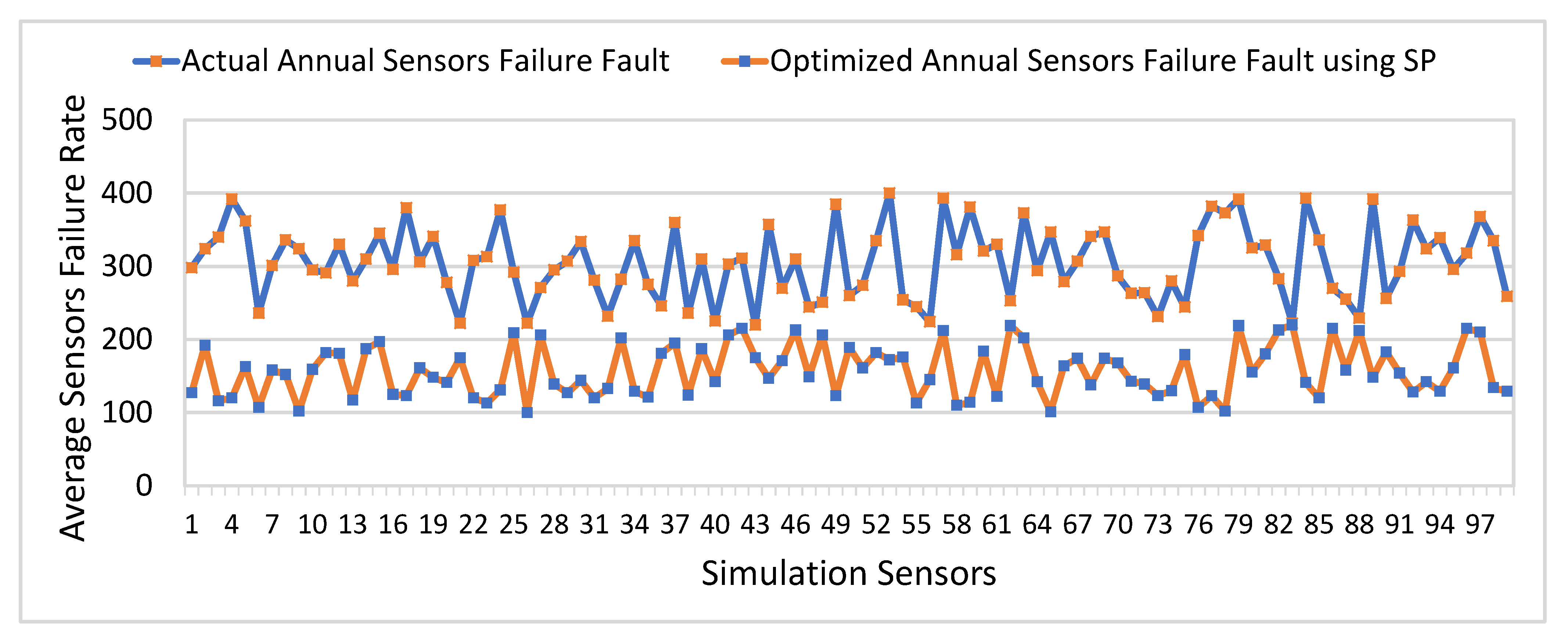
5.1. Performance Analysis
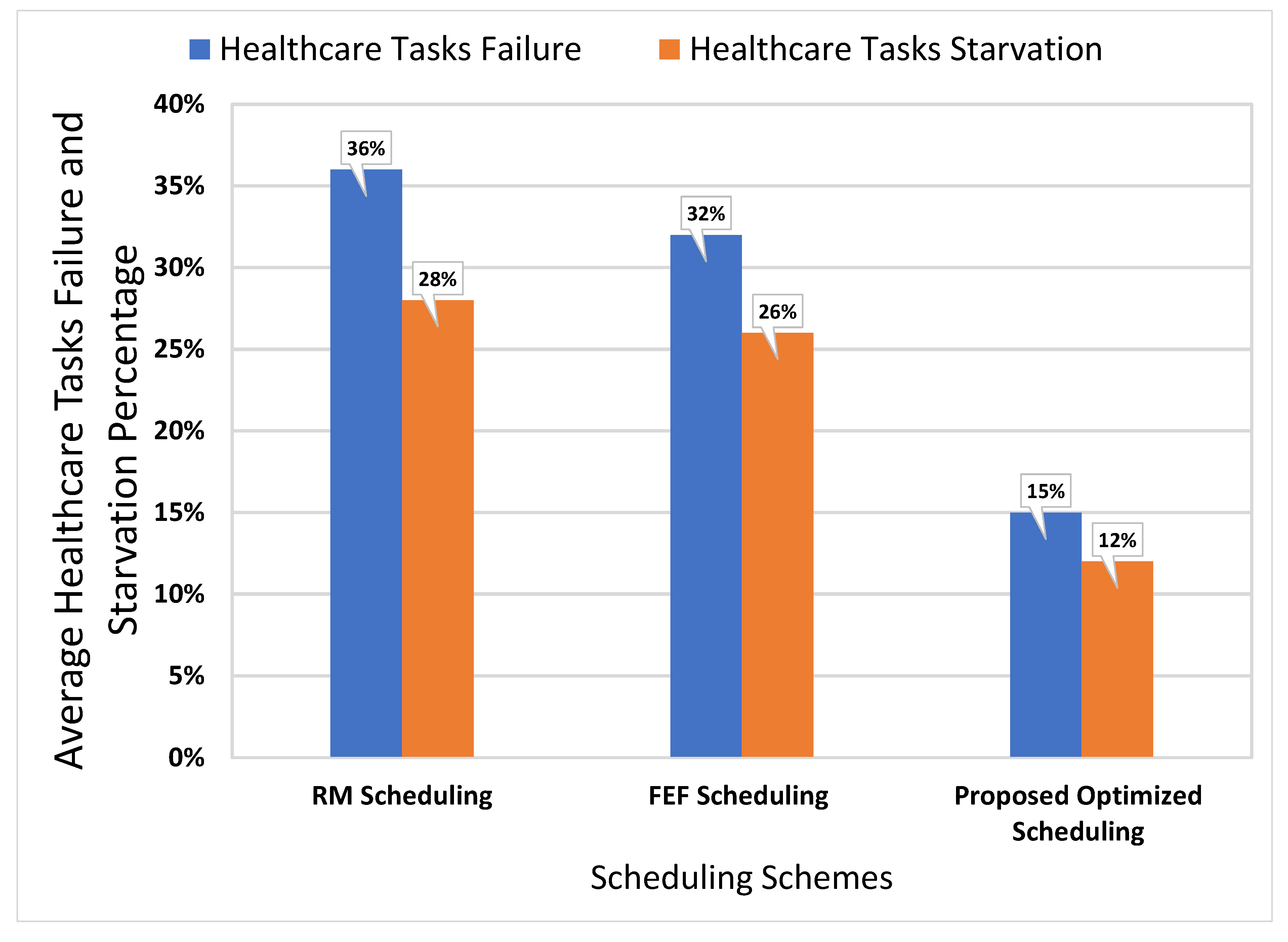
5.2. Comparative Analysis
6. Conclusions and Future Work
Author Contributions
Funding
Conflicts of Interest
References
- Imran; Ghaffar, Z.; Alshahrani, A.; Fayaz, M.; Alghamdi, A.M.; Gwak, J. A Topical Review on Machine Learning, Software Defined Networking, Internet of Things Applications: Research Limitations and Challenges. Electronics 2021, 10, 880. [Google Scholar] [CrossRef]
- Sicari, S.; Rizzardi, A.; Grieco, L.A.; Coen-Porisini, A. Security, privacy and trust in Internet of Things: The road ahead. Comput. Netw. 2015, 76, 146–164. [Google Scholar] [CrossRef]
- Zanella, A.; Bui, N.; Castellani, A.; Vangelista, L.; Zorzi, M. Internet of things for smart cities. IEEE Internet Things J. 2014, 1, 22–32. [Google Scholar] [CrossRef]
- Zheng, J.; Simplot-Ryl, D.; Bisdikian, C.; Mouftah, H.T. The internet of things [Guest Editorial]. IEEE Commun. Mag. 2011, 49, 30–31. [Google Scholar] [CrossRef]
- Abdelmoneem, R.M.; Benslimane, A.; Shaaban, E. Mobility-Aware Task Scheduling in Cloud-Fog IoT-Based Healthcare Architectures. Comput. Netw. 2020, 107348. [Google Scholar] [CrossRef]
- Catarinucci, L.; De Donno, D.; Mainetti, L.; Palano, L.; Patrono, L.; Stefanizzi, M.L.; Tarricone, L. An IoT-aware architecture for smart healthcare systems. IEEE Internet Things J. 2015, 2, 515–526. [Google Scholar] [CrossRef]
- Chernbumroong, S.; Cang, S.; Atkins, A.; Yu, H. Elderly activities recognition and classification for applications in assisted living. Expert Syst. Appl. 2013, 40, 1662–1674. [Google Scholar] [CrossRef]
- Jamil, F.; Ahmad, S.; Iqbal, N.; Kim, D.H. Towards a Remote Monitoring of Patient Vital Signs Based on IoT-Based Blockchain Integrity Management Platforms in Smart Hospitals. Sensors 2020, 20, 2195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, P.M.; Gandhi, U.D. A novel three-tier Internet of Things architecture with machine learning algorithm for early detection of heart diseases. Comput. Electr. Eng. 2018, 65, 222–235. [Google Scholar] [CrossRef]
- Farahani, B.; Firouzi, F.; Chakrabarty, K. Healthcare iot. In Intelligent Internet of Things; Springer: Berlin/Heidelberg, Germany, 2020; pp. 515–545. [Google Scholar]
- Imran; Iqbal, N.; Ahmad, S.; Kim, D.H. Health Monitoring System for Elderly Patients Using Intelligent Task Mapping Mechanism in Closed Loop Healthcare Environment. Symmetry 2021, 13, 357. [Google Scholar] [CrossRef]
- Majumder, S.; Aghayi, E.; Noferesti, M.; Memarzadeh-Tehran, H.; Mondal, T.; Pang, Z.; Deen, M.J. Smart homes for elderly healthcare—Recent advances and research challenges. Sensors 2017, 17, 2496. [Google Scholar] [CrossRef] [Green Version]
- Swaroop, K.N.; Chandu, K.; Gorrepotu, R.; Deb, S. A health monitoring system for vital signs using IoT. Internet Things 2019, 5, 116–129. [Google Scholar] [CrossRef]
- Wu, F.; Wu, T.; Yuce, M.R. An internet-of-things (IoT) network system for connected safety and health monitoring applications. Sensors 2019, 19, 21. [Google Scholar] [CrossRef] [Green Version]
- Misbahuddin, S.; Zubairi, J.A.; Alahdal, A.R.; Malik, M.A. IoT-Based Ambulatory Vital Signs Data Transfer System. J. Comput. Netw. Commun. 2018, 2018. [Google Scholar] [CrossRef]
- Maksimović, M.; Vujović, V. Internet of Things based e-health systems: Ideas, expectations and concerns. In Handbook of Large-Scale Distributed Computing in Smart Healthcare; Springer: Berlin/Heidelberg, Germany, 2017; pp. 241–280. [Google Scholar]
- Abdelmoneem, R.M.; Shaaban, E.; Benslimane, A. A Survey on Multi-Sensor Fusion Techniques in IoT for Healthcare. In Proceedings of the 2018 13th International Conference on Computer Engineering and Systems (ICCES), Cairo, Egypt, 18–19 December 2018; pp. 157–162. [Google Scholar]
- Suh, M.k.; Chen, C.A.; Woodbridge, J.; Tu, M.K.; Kim, J.I.; Nahapetian, A.; Evangelista, L.S.; Sarrafzadeh, M. A remote patient monitoring system for congestive heart failure. J. Med Syst. 2011, 35, 1165–1179. [Google Scholar] [CrossRef] [Green Version]
- Jara, A.J.; Zamora-Izquierdo, M.A.; Skarmeta, A.F. Interconnection framework for mHealth and remote monitoring based on the internet of things. IEEE J. Sel. Areas Commun. 2013, 31, 47–65. [Google Scholar] [CrossRef]
- Banaee, H.; Ahmed, M.U.; Loutfi, A. Data mining for wearable sensors in health monitoring systems: A review of recent trends and challenges. Sensors 2013, 13, 17472–17500. [Google Scholar] [CrossRef] [Green Version]
- Bansal, A.; Kumar, S.; Bajpai, A.; Tiwari, V.N.; Nayak, M.; Venkatesan, S.; Narayanan, R. Remote health monitoring system for detecting cardiac disorders. IET Syst. Biol. 2015, 9, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Klingeberg, T.; Schilling, M. Mobile wearable device for long term monitoring of vital signs. Comput. Methods Programs Biomed. 2012, 106, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, N.; Han, L.; Iqbal, K.; Ahmad, R.; Abid, M.A.; Iqbal, N. SARM: Salah activities recognition model based on smartphone. Electronics 2019, 8, 881. [Google Scholar] [CrossRef] [Green Version]
- Kakria, P.; Tripathi, N.; Kitipawang, P. A real-time health monitoring system for remote cardiac patients using smartphone and wearable sensors. Int. J. Telemed. Appl. 2015, 2015. [Google Scholar] [CrossRef] [Green Version]
- Hagargund, A.G.; Srivastav, A.; Nayak, C.K.; Singh, M.K. Smart and Automatic Health Monitoring of Patient Using Wireless Sensor Network. In Proceedings of the 2018 9th International Conference on Computing, Communication and Networking Technologies (ICCCNT), Bengaluru, India, 10–12 July 2018; pp. 1–7. [Google Scholar]
- Mahmood, D.; Fadhil, A.; Rafaa, M.M. IoT based on Health Caring Systems Survey. Int. J. Comput. Digit. Syst. 2020, 10, 1–10. [Google Scholar]
- Noury, N.; Rumeau, P.; Bourke, A.; ÓLaighin, G.; Lundy, J. A proposal for the classification and evaluation of fall detectors. Irbm 2008, 29, 340–349. [Google Scholar] [CrossRef]
- Giorgi, G.; Galli, A.; Narduzzi, C. Smartphone-based IOT systems for personal health monitoring. IEEE Instrum. Meas. Mag. 2020, 23, 41–47. [Google Scholar] [CrossRef]
- Pandya, B.; Pourabdollah, A.; Lotfi, A. Fuzzy logic web services for real-time fall detection using wearable accelerometer and gyroscope sensors. In Proceedings of the 13th ACM International Conference on PErvasive Technologies Related to Assistive Environments, Corfu Greece, 30 Julne–3 July 2020; pp. 1–7. [Google Scholar]
- Bet, P.; Castro, P.C.; Ponti, M.A. Fall detection and fall risk assessment in older person using wearable sensors: A systematic review. Int. J. Med. Inform. 2019, 130, 103946. [Google Scholar] [CrossRef] [PubMed]
- Mdhaffar, A.; Chaari, T.; Larbi, K.; Jmaiel, M.; Freisleben, B. IoT-based health monitoring via LoRaWAN. In Proceedings of the IEEE EUROCON 2017-17th International Conference on Smart Technologies, Ohrid, North Macedonia, 6–8 July 2017; pp. 519–524. [Google Scholar]
- Selvaraj, S.; Sundaravaradhan, S. Challenges and opportunities in IoT healthcare systems: A systematic review. SN Appl. Sci. 2020, 2, 139. [Google Scholar] [CrossRef] [Green Version]
- Djelouat, H.; Amira, A.; Bensaali, F.; Boukhennoufa, I. Secure compressive sensing for ECG monitoring. Comput. Secur. 2020, 88, 101649. [Google Scholar] [CrossRef]
- Saidi, H.; Labraoui, N.; Ari, A.A.A.; Bouida, D. Remote health monitoring system of elderly based on Fog to Cloud (F2C) computing. In Proceedings of the 2020 International Conference on Intelligent Systems and Computer Vision (ISCV), Fez, Morocco, 2–4 April 2020; pp. 1–7. [Google Scholar]
- Yang, Z.; Zhou, Q.; Lei, L.; Zheng, K.; Xiang, W. An IoT-cloud based wearable ECG monitoring system for smart healthcare. J. Med Syst. 2016, 40, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Al Mamun, K.A.; Alhussein, M.; Sailunaz, K.; Islam, M.S. Cloud based framework for Parkinson’s disease diagnosis and monitoring system for remote healthcare applications. Future Gener. Comput. Syst. 2017, 66, 36–47. [Google Scholar] [CrossRef]
- Hussein, A.F.; Burbano-Fernandez, M.; Ramírez-González, G.; Abdulhay, E.; De Albuquerque, V.H.C. An automated remote cloud-based heart rate variability monitoring system. IEEE Access 2018, 6, 77055–77064. [Google Scholar] [CrossRef]
- Fortino, G.; Parisi, D.; Pirrone, V.; Di Fatta, G. BodyCloud: A SaaS approach for community body sensor networks. Future Gener. Comput. Syst. 2014, 35, 62–79. [Google Scholar] [CrossRef] [Green Version]
- Gia, T.N.; Jiang, M.; Rahmani, A.M.; Westerlund, T.; Liljeberg, P.; Tenhunen, H. Fog Computing in Healthcare internet of Things: A Case Study on ecg Feature Extraction. In Proceedings of the 2015 IEEE International Conference on Computer and Information Technology; Ubiquitous Computing and Communications; Dependable, Autonomic and Secure Computing; Pervasive Intelligence and Computing, Liverpool, UK, 26–28 October 2015; pp. 356–363. [Google Scholar]
- Negash, B.; Gia, T.N.; Anzanpour, A.; Azimi, I.; Jiang, M.; Westerlund, T.; Rahmani, A.M.; Liljeberg, P.; Tenhunen, H. Leveraging fog computing for healthcare IoT. In Fog Computing in the Internet of Things; Springer: Berlin, Germany, 2018; pp. 145–169. [Google Scholar]
- Rahmani, A.M.; Gia, T.N.; Negash, B.; Anzanpour, A.; Azimi, I.; Jiang, M.; Liljeberg, P. Exploiting smart e-Health gateways at the edge of healthcare Internet-of-Things: A fog computing approach. Future Gener. Comput. Syst. 2018, 78, 641–658. [Google Scholar] [CrossRef]
- Mutlag, A.A.; Abd Ghani, M.K.; Arunkumar, N.a.; Mohammed, M.A.; Mohd, O. Enabling technologies for fog computing in healthcare IoT systems. Future Gener. Comput. Syst. 2019, 90, 62–78. [Google Scholar] [CrossRef]
- Verma, P.; Sood, S.K. Fog assisted-IoT enabled patient health monitoring in smart homes. IEEE Internet Things J. 2018, 5, 1789–1796. [Google Scholar] [CrossRef]
- Dubey, H.; Yang, J.; Constant, N.; Amiri, A.M.; Yang, Q.; Makodiya, K. Fog data: Enhancing telehealth big data through fog computing. In Proceedings of the ASE Bigdata & Socialinformatics, New York, NY, USA, 7 October 2015; pp. 1–6. [Google Scholar]
- Craciunescu, R.; Mihovska, A.; Mihaylov, M.; Kyriazakos, S.; Prasad, R.; Halunga, S. Implementation of Fog computing for reliable E-health applications. In Proceedings of the 2015 49th Asilomar Conference on Signals, Systems and Computers, Grove, CA, USA, 8–11 November; pp. 459–463.
- Alsaffar, A.A.; Pham, H.P.; Hong, C.S.; Huh, E.N.; Aazam, M. An architecture of iot service delegation and resource allocation based on collaboration between fog and cloud computing. Mob. Inf. Syst. 2016, 2016. [Google Scholar] [CrossRef] [Green Version]
- Arabnejad, H.; Barbosa, J.G. List scheduling algorithm for heterogeneous systems by an optimistic cost table. IEEE Trans. Parallel Distrib. Syst. 2013, 25, 682–694. [Google Scholar] [CrossRef]
- Jiang, H.J.; Huang, K.C.; Chang, H.Y.; Gu, D.S.; Shih, P.J. Scheduling concurrent workflows in HPC cloud through exploiting schedule gaps. In International Conference on Algorithms and Architectures for Parallel Processing; Springer: Berlin, Germany, 2011; pp. 282–293. [Google Scholar]
- Agarwal, S.; Yadav, S.; Yadav, A.K. An efficient architecture and algorithm for resource provisioning in fog computing. Int. J. Inf. Eng. Electron. Bus. 2016, 8, 48. [Google Scholar] [CrossRef]
- Pham, X.Q.; Man, N.D.; Tri, N.D.T.; Thai, N.Q.; Huh, E.N. A cost-and performance-effective approach for task scheduling based on collaboration between cloud and fog computing. Int. J. Distrib. Sens. Netw. 2017, 13, 1550147717742073. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Qi, D.; Zhou, N.; Wu, Y. A task scheduling algorithm based on classification mining in fog computing environment. Wirel. Commun. Mob. Comput. 2018, 2018. [Google Scholar] [CrossRef] [Green Version]
- Artalejo, J.R.; Lopez-Herrero, M. Quasi-stationary and ratio of expectations distributions: A comparative study. J. Theor. Biol. 2010, 266, 264–274. [Google Scholar] [CrossRef] [Green Version]
- Sahab, M.G.; Toropov, V.V.; Gandomi, A.H. A review on traditional and modern structural optimization: Problems and techniques. Metaheuristic Appl. Struct. Infrastruct. 2013, 25–47. [Google Scholar]
- Rath, M.; Darwish, A.; Pati, B.; Pattanayak, B.K.; Panigrahi, C.R. Swarm intelligence as a solution for technological problems associated with Internet of Things. In Swarm Intelligence for Resource Management in Internet of Things; Elsevier: Amsterdam, The Netherlands, 2020; pp. 21–45. [Google Scholar]
- Ahmad, S.; Mehmood, F.; Kim, D.H. A DIY approach for the design of mission-planning architecture using autonomous task–object mapping and the deployment model in mission-critical IoT systems. Sustainability 2019, 11, 3647. [Google Scholar] [CrossRef] [Green Version]
- Ahmad, S.; Hang, L.; Kim, D.H. Design and implementation of cloud-centric configuration repository for DIY IoT applications. Sensors 2018, 18, 474. [Google Scholar] [CrossRef] [Green Version]
- Vital Signs Data. Available online: https://healthjade.net/vital-signs/ (accessed on 5 November 2020).
- Imran; Ahmad, S.; Kim, D. Design and Implementation of Thermal Comfort System based on Tasks Allocation Mechanism in Smart Homes. Sustainability 2019, 11, 5849. [Google Scholar] [CrossRef] [Green Version]
- Imran; Ahmad, S.; Kim, D.H. A Task Orchestration Approach for Efficient Mountain Fire Detection Based on Microservice and Predictive Analysis in IoT Environment. J. Intell. Fuzzy Syst. 2021, 40, 5681–5696. [Google Scholar] [CrossRef]
- Imran; Iqbal, N.; Ahmad, S.; Kim, D.H. Towards mountain fire safety using fire spread predictive analytics and mountain fire containment in iot environment. Sustainability 2021, 13, 2461. [Google Scholar] [CrossRef]
- Qamar, S.; Abdelrehman, A.M.; Elshafie, H.E.; Mohiuddin, K. Sensor Based IoT Industrial Healthcare. Int. J. Sci. Eng. Sci. 2018, 2, 29–34. [Google Scholar]
- Brezulianu, A.; Geman, O.; Zbancioc, M.D.; Hagan, M.; Aghion, C.; Hemanth, D.J.; Son, L.H. IoT based heart activity monitoring using inductive sensors. Sensors 2019, 19, 3284. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Application | Platform | Objective | Pros | Cons |
|---|---|---|---|---|
| Remote health monitoring [22] | IoT | The proposed system was developed to monitor critical events related to cardiac diseases. | Provides real-time alerts, low computation cost to process remote patients data. | No-fault tolerance, static deployment process of healthcare tasks, high cost. |
| Vital signs monitoring [23] | IoT | This study aimed to record vital signs data of patients, such as ECG, blood pressure, etc. | Correct or reject distorted signals of vital signs based on the data fusion approach. | High energy consumption and static platform for handling emergent conditions |
| Health monitoring system [24] | IoT | Advanced paradigms of IoT-based system for monitoring critical symptoms related to cardiac disease. | Emergencies alerts, GUI, reduce energy consumption due to Bluetooth. | Delay in emergencies alerts, and low reliability. |
| F2C model [34] | Cloud-Computing | The main objective is to monitor the health conditions of remote patients based on the fog-to-cloud paradigm. | It uses the F2C model to provide storage and security of healthcare data. It sends emergencies alert using a smartphone. | No-fault tolerance, static scheduling of tasks related to heart rate monitoring. |
| ECG monitoring system [35] | Cloud-Computing | The authors developed a Cloud-based reliable architecture for ECG monitoring of remote patients in smart health. | High bandwidth rates for healthcare data transmission, and web-based GUI for versatile services. | No scheduling mechanism for handling emergent condition of remote patients. |
| Heart rate monitoring system [37] | Cloud-Computing | Attempted to monitor heart rate on a continuous basis to facilitate cardiac patients. | Ease of use, GUI, and healthcare data security. | Scalability issues. |
| BodyCloud [38] | Cloud-Computing | The proposed BodyCloud is a SaaS approach for real-time monitoring cardiac patient’s data. | Scalable approach for healthcare data storage and analysis. | Lack of emergency alerts and global security. |
| Case study [39] | Fog-Computing | The authors presented a case study to analyze ECG signals to play a vital role in the diagnosis of cardiac diseases. | Real-time monitoring of ECG signals, and bandwidth efficiency. | Lack of emergency alarms and scalability issues. |
| Smart e-Health [40] | Fog-Computing | Introduction of Fog-layer in IoT-based healthcare platforms for health monitoring in the home and in the hospital. | Reducing latency and improve consistency. | Inefficient consumption of energy, lack of scheduling for handling emergent conditions. |
| Smart e-Health gateway [41] | Fog-Computing | This study aimed to integrate fog-computing into existing IoT-based healthcare systems for efficient data processing and mining. | Real-time vital signs data processing, and provide mobility support for home and hospital patients. | Interoperability issue for a variety of nodes, lack of dealing with emergent healthcare tasks. |
| Patient health monitoring [43] | Fog-Computing | The authors proposed patient’s health monitoring system based on fog computing to process and store data at the smart edge gateway. | Real-time health monitoring, data mining, and notification services. | High computational cost at edge node, scalability issue, and static allocation of healthcare tasks. |
| Notation | Description |
|---|---|
| There are N number of sensors (measurements). | |
| It indicates collected sensing data for sensor at time t. | |
| It indicates total number of available sensors. | |
| It indicates total number of additional sensors. | |
| It is total amount of information retrieve from sensing devices. | |
| It is total amount of lost information from sensing devices at time t. | |
| It represents ratio of available sensing devices and additional (backup) sensing devices. | |
| It represents ratio of retrieve information and lost information. | |
| It is defined as information loss recovery index. | |
| It represents the lower threshold function. | |
| It represents the upper threshold function. | |
| It is an average value of the maximum value of a sensor measurement signal. | |
| It is an average value of the minimum value of a sensor measurement signal. | |
| It denotes a quasi-natural ratio. | |
| It represents safety factor to minimize sensors failure frequency to increase the reliability of the proposed smart PHMS. | |
| It represents safety index based on and . |
| Parameter | Description |
|---|---|
| Message ID | It is a unique identifier of a message. |
| Micro-Service ID | It indicates micro-service to which the given task belongs. |
| Input Task ID | It represents an identifier of the given input task. |
| Virtual Object ID | It represents an identifier of the given virtual object. |
| Timestamp | It represents timestamp at which the task mapping process occurred. |
| Notation | Description |
|---|---|
| There are N number of sensing devices. | |
| There are K number of healthcare tasks for each sensing device. | |
| It is identifier that represents healthcare task. | |
| It represents start time of the arrived healthcare task. | |
| It indicates finish time of healthcare task. | |
| It represents execution time of healthcare task. | |
| It is an idle amount of task completion time. |
| System Component | Description |
|---|---|
| Operating System | Microsoft Windows 10 |
| CPU | Intel ®Core ™ i3-2130 CPU at 3.40 GHz |
| Primary Memory | PyCharm Professional 2020 |
| Framework | Flask Framework |
| Libraries | Drools, JSPlumb |
| Core Programming Language | Python, JavaScript and jQuery |
| Front End Framework | Bootstrap |
| Backend Persistence | MySQL |
| Healthcare Toolkit | Libelium e-Health Sensor Shield V2.0 |
| Hardware | Arduino |
| Server | CoAP Server |
| Sensing Devices | Normal Range | Abnormal Range | Objective |
|---|---|---|---|
| Body Temperature Sensor [57] | 97.8 °F to 99 °F (36.5 °C to 37.2 °C) | Temperature higher than 100.4 °F (38 °C) | It is used to determine body temperature. |
| Heart Rate Sensor (ECG) [57] | ECG is used to measure the electrical activity of the heart. | ||
| Sphygmomanometer [57] | Systolic: (mm Hg) Diastolic: (mm Hg) | Systolic: 90–119 (mm Hg) Diastolic: 60–79 (mm Hg) | It is used to monitor the blood pressure rate. It is used to measure both systolic and diastolic pressures. |
| Pulse Oximeter (SpO2) [57] | (70–100 bpm) | It is used to measure the quantity of oxygen in the blood. | |
| Airflow Sensor [57] | or | Airflow sensor is used to measure the respiration rate. |
| E-Health System | Self-Management Support | Type of Application | Real Simulation | Tasks Scheduling | Optimization Functionality | Objective |
|---|---|---|---|---|---|---|
| IoT-SHS [6] | No | Mobile/Web | Yes | No | No | Monitor both patinet health and environmental conditions |
| H-IoT [8] | Yes | Web-based | No | Yes | No | Vital signs management |
| PHMS [22] | Partial | Mobile | Yes | No | No | Vital signs management |
| HMS [24] | No | Mobile | Yes | No | No | Real time monitoring of patient heart condition |
| WSN [25] | Yes | Web-based | Yes | No | No | Vital signs management |
| VSM [43] | No | Middleware | No | No | No | Vital signs management and classification of event occurrence |
| FDS [45] | Yes | Mobile/Web | Yes | No | No | Fall detection system |
| HAMS [62] | No | Unknown | Yes | No | No | To monitor patient heart pulse and respiration data |
| HI-IoT [61] | No | Unknown | No | No | No | Monitor patient vital signs data |
| Proposed smart PHMS | Yes | Mobile/Web | Yes | Dynamic | Yes | Optimal healthcare tasks management, vital signs monitoring, optimization of tasks starvation rate and minimization of tasks failure rate. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iqbal, N.; Imran; Ahmad, S.; Ahmad, R.; Kim, D.-H. A Scheduling Mechanism Based on Optimization Using IoT-Tasks Orchestration for Efficient Patient Health Monitoring. Sensors 2021, 21, 5430. https://doi.org/10.3390/s21165430
Iqbal N, Imran, Ahmad S, Ahmad R, Kim D-H. A Scheduling Mechanism Based on Optimization Using IoT-Tasks Orchestration for Efficient Patient Health Monitoring. Sensors. 2021; 21(16):5430. https://doi.org/10.3390/s21165430
Chicago/Turabian StyleIqbal, Naeem, Imran, Shabir Ahmad, Rashid Ahmad, and Do-Hyeun Kim. 2021. "A Scheduling Mechanism Based on Optimization Using IoT-Tasks Orchestration for Efficient Patient Health Monitoring" Sensors 21, no. 16: 5430. https://doi.org/10.3390/s21165430
APA StyleIqbal, N., Imran, Ahmad, S., Ahmad, R., & Kim, D.-H. (2021). A Scheduling Mechanism Based on Optimization Using IoT-Tasks Orchestration for Efficient Patient Health Monitoring. Sensors, 21(16), 5430. https://doi.org/10.3390/s21165430








