Design and Development of a Low Cost, Non-Contact Infrared Thermometer with Range Compensation
Abstract
1. Introduction
2. Materials and Methods
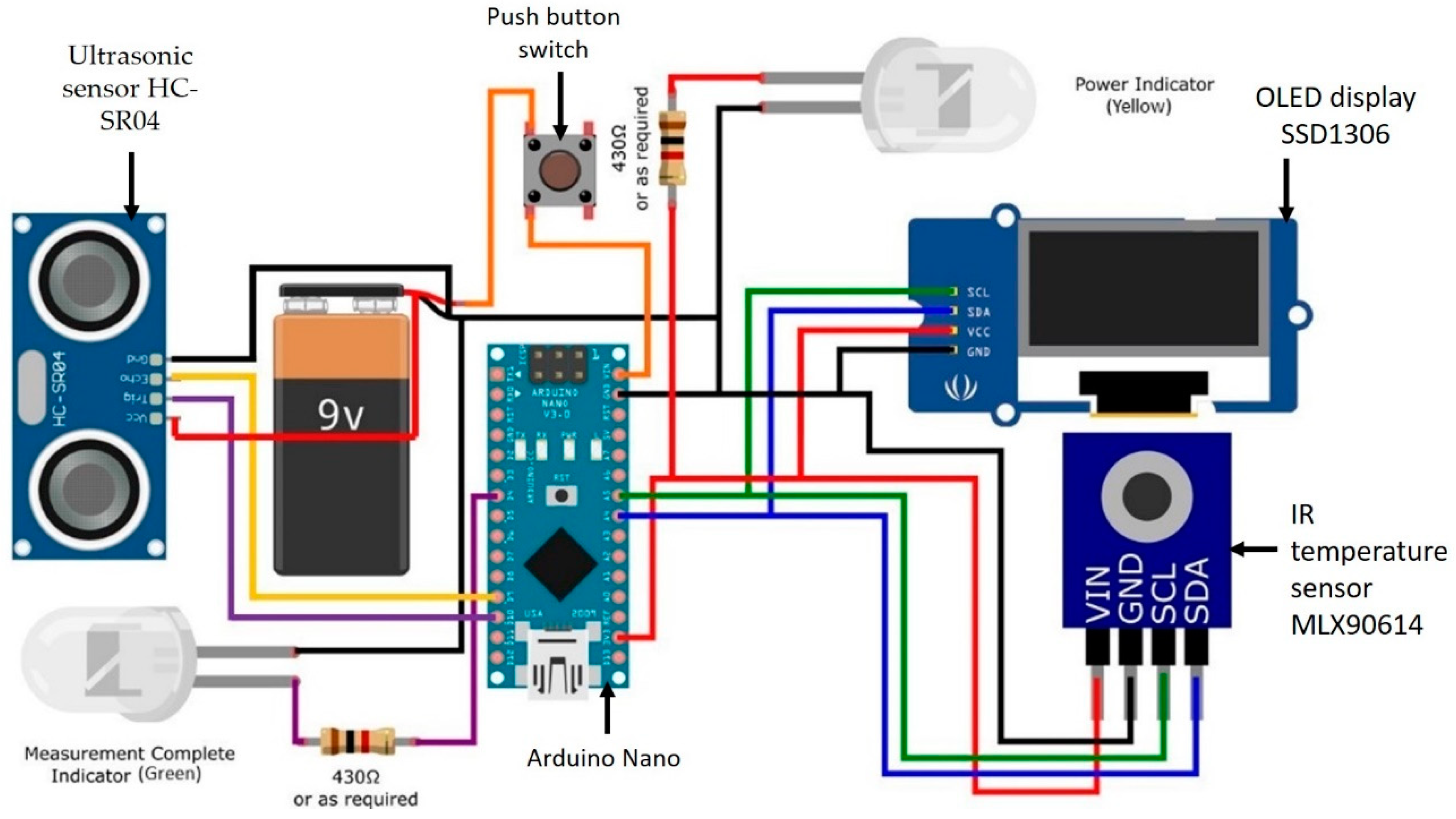
2.1. Components and Specifications
2.2. Assembly of Infrared Thermometer
2.2.1. Physical Assembly
2.2.2. Circuitry Design and Implementation
2.3. Programming Arrangement
2.4. Sensor Calculations
2.4.1. Infrared Sensor
2.4.2. Ultrasound Sensor
2.4.3. Experimental Setup
2.4.4. Statistical Analysis
3. Results
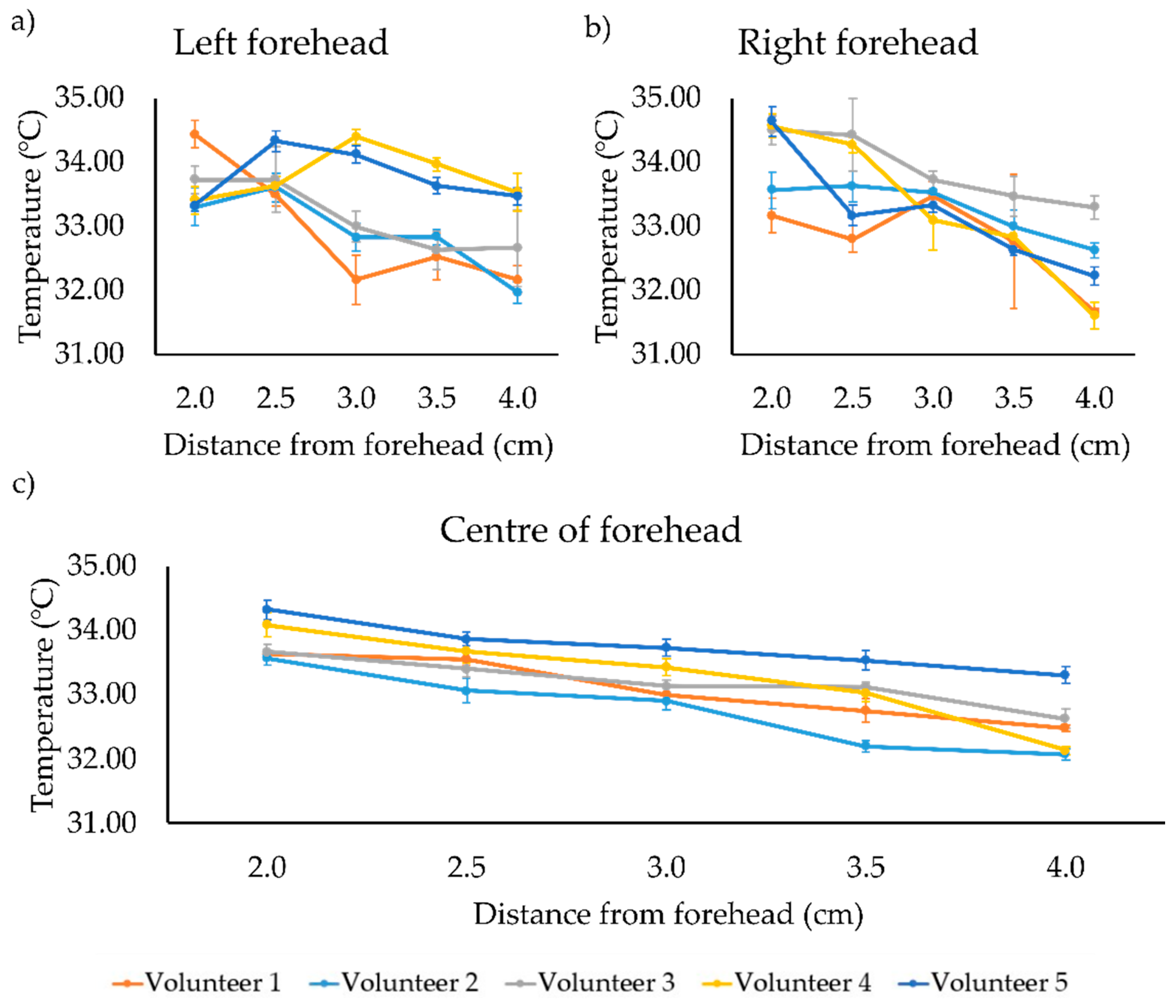
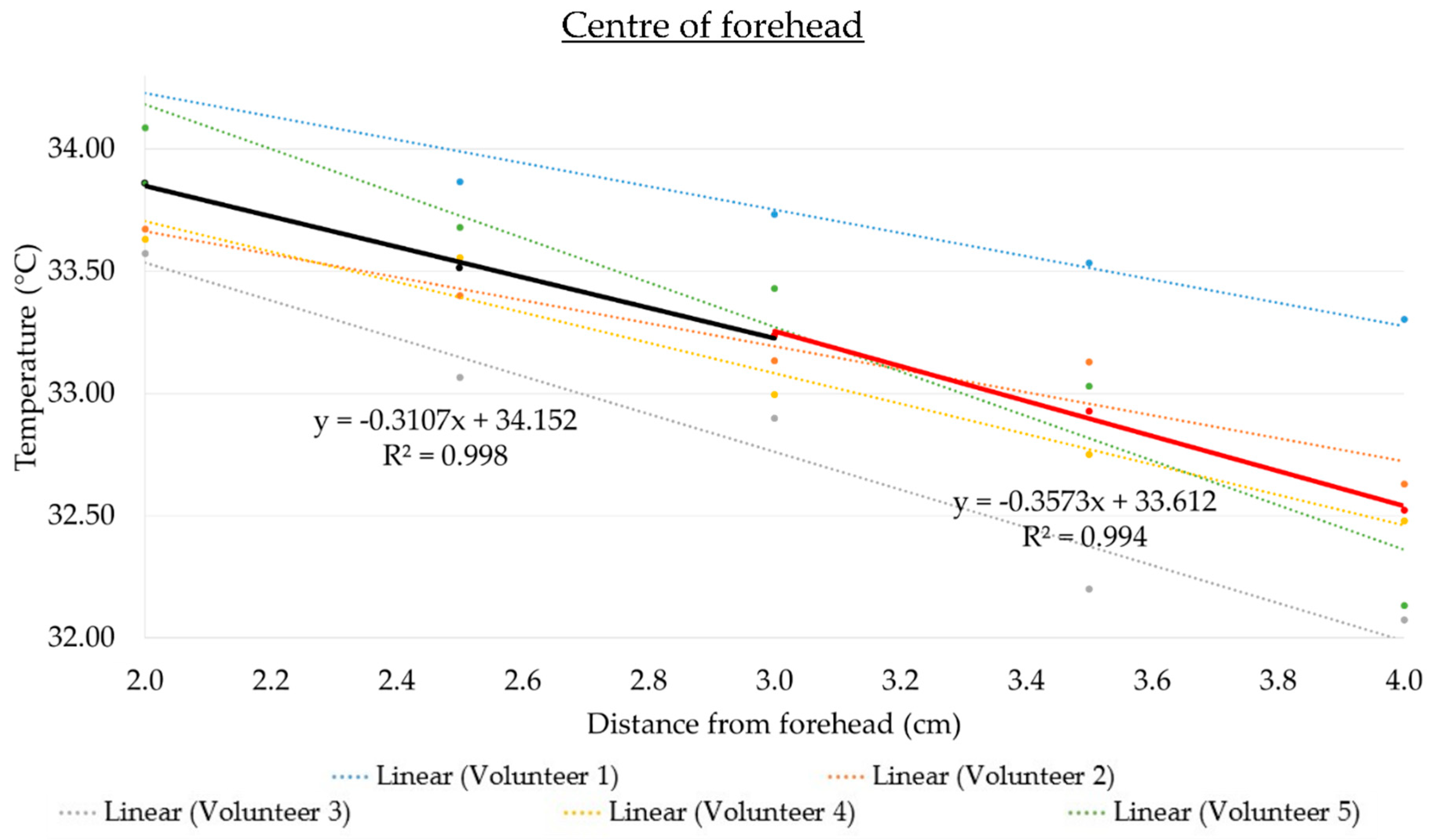
3.1. Performance of IR Thermomter on the Forehead
3.2. Performance of IR Thermomter on the Wet Forehead
3.3. Compensation Adjustments and Testing of IR Thermometer
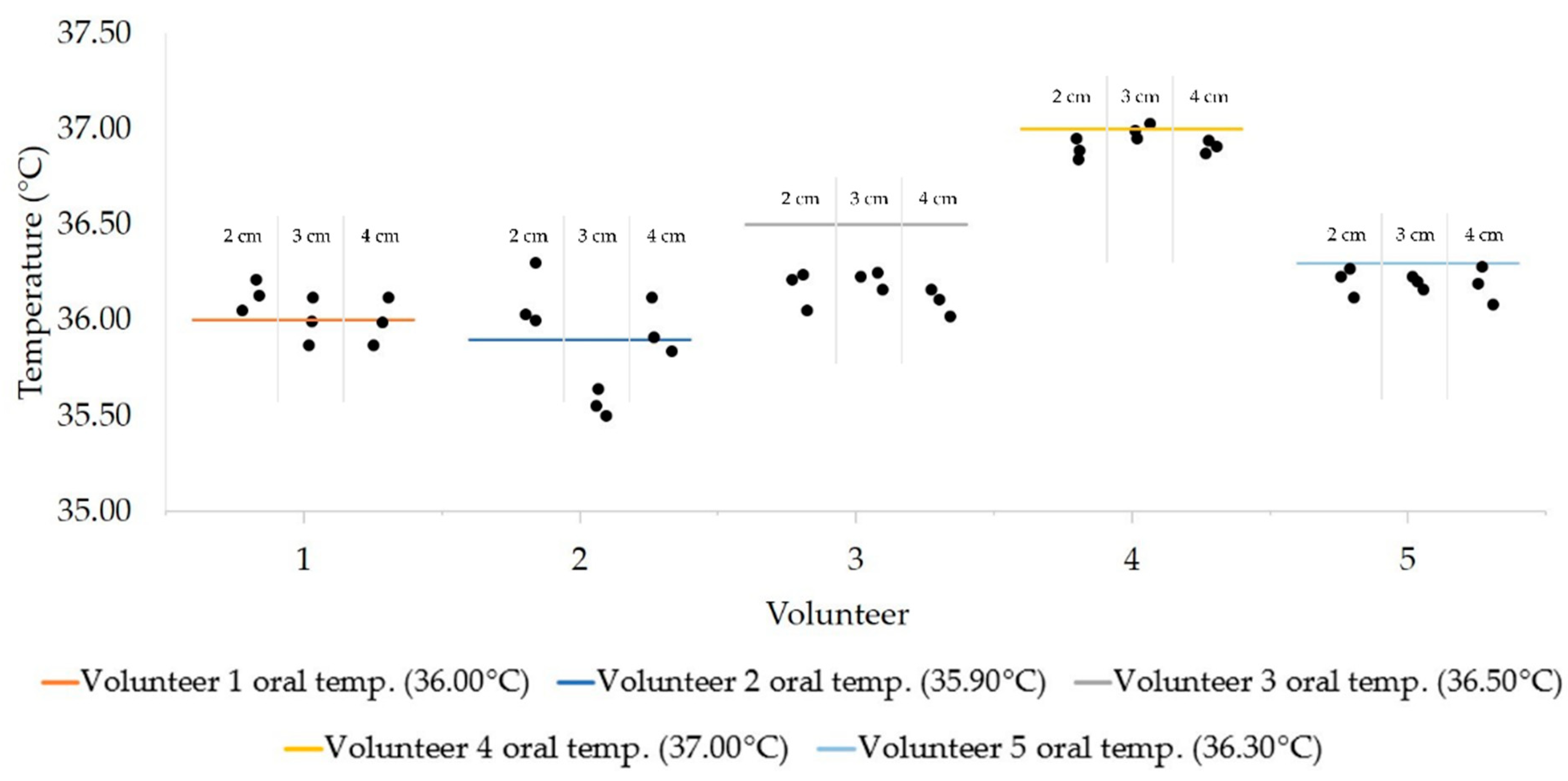
3.4. Test Performance of the Optimized IR Temperature System
4. Discussion
4.1. Assembly of the Arduino-Based Thermometer
4.2. Differences in Temperature between the Center and Lateral Areas of the Forehead
4.3. Wetness of Forehead
4.4. Performance of Calibrated IR Thermometer
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fulbrook, P. Core temperature measurement: A comparison of rectal, axillary and pulmonary artery blood temperature. Intensive Crit. Care Nurs. 1993, 9, 217–225. [Google Scholar] [CrossRef]
- Mogensen, C.B.; Wittenhoff, L.; Fruerhøj, G.; Hansen, S. Forehead or ear temperature measurement cannot replace rectal measurements, except for screening purposes. BMC Pediatrics 2018, 18, 15. [Google Scholar] [CrossRef]
- Quast, S.; Kimberger, O. The Significance of Core Temperature—Pathophysiology and Measurement Methods; Dräger Medical GmbH: Stuttgart, Germany, 2014. [Google Scholar]
- Poh, J.-J.; Wu, W.-L.; Goh, N.W.-J.; Tan, S.M.-X.; Gan, S.K.-E. Spectrophotometer on-the-go: The development of a 2-in-1 UV–Vis portable Arduino-based spectrophotometer. Sens. Actuators A Phys. 2021, 325, 112698. [Google Scholar] [CrossRef]
- Ng, K.M.; Wong, C.-F.; Liang, A.C.; Liew, Y.-H.; Liang, A.C.; Yeo, J.Y.; Lua, W.-H.; Qian, X.-J.; Gan, S.K.-E. Republication—APD SpectBT: Arduino-based mobile vis-Spectrophotometer. Sci. Phone Apps Mob. Devices 2019, 5. [Google Scholar] [CrossRef]
- Gan, S.K.-E.; Yeo, J.Y. Editorial: The promises of Microcontroller kits and Smartphone apps for Psychological research. Sci. Phone Apps Mob. Devices 2020, 6. [Google Scholar] [CrossRef]
- Yaffe-Bellany, D. Thermometer Guns’ on Coronavirus Front Lines are “Notoriously not Accurate”; The New York Times: New York, NY, USA, 2020. [Google Scholar]
- Bitar, D.; Goubar, A.; Desenclos, J.C. International travels and fever screening during epidemics: A literature review on the effectiveness and potential use of non-contact infrared thermometers. Eurosurveillance 2009, 14, 19115. [Google Scholar] [CrossRef]
- Hsiao, S.H.; Chen, T.C.; Chien, H.C.; Yang, C.J.; Chen, Y.H. Measurement of body temperature to prevent pandemic COVID-19 in hospitals in Taiwan: Repeated measurement is necessary. J. Hosp. Infect. 2020, 105, 360–361. [Google Scholar] [CrossRef] [PubMed]
- Hudoklin, D.; Drnovšek, J. The New LMK Primary Standard for Dew-Point Sensor Calibration: Evaluation of the High-Range Saturator Efficiency. Int. J. Thermophys. 2008, 29, 1652–1659. [Google Scholar] [CrossRef]
- Patel, N.; Smith, C.E.; Pinchak, A.C.; Hagen, J.F. Comparison of esophageal, tympanic, and forehead skin temperatures in adult patients. J. Clin. Anesth. 1996, 8, 462–468. [Google Scholar] [CrossRef]
- Teran, C.G.; Torrez-Llanos, J.; Teran-Miranda, T.E.; Balderrama, C.; Shah, N.S.; Villarroel, P. Clinical accuracy of a non-contact infrared skin thermometer in paediatric practice. Child. Care Health Dev. 2012, 38, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Pušnik, I.; Miklavec, A. Dilemmas in Measurement of Human Body Temperature. Instrum. Sci. Technol. 2009, 37, 516–530. [Google Scholar] [CrossRef]
- Wang, K.; Gill, P.; Wolstenholme, J.; Price, C.P.; Heneghan, C.; Thompson, M.; Plüddemann, A. Non-contact infrared thermometers for measuring temperature in children: Primary care diagnostic technology update. Br. J. Gen. Pract. 2014, 64, e681–e683. [Google Scholar] [CrossRef]
- Dean, W. Effect of Sweating. JAMA 1981, 246, 623. [Google Scholar] [CrossRef]
- Ng, D.K.-K.; Chan, C.-H.; Chan, E.Y.-T.; Kwok, K.-L.; Chow, P.-Y.; Lau, W.-F.; Ho, J.C.-S. A brief report on the normal range of forehead temperature as determined by noncontact, handheld, infrared thermometer. Am. J. Infect. Control. 2005, 33, 227–229. [Google Scholar] [CrossRef] [PubMed]
- Ariyaratnam, S.; Rood, J.P. Measurement of facial skin temperature. J. Dent. 1990, 18, 250–253. [Google Scholar] [CrossRef]
- Chen, K.S.; Lin, Y.C.; Yang, H.O. Non-Contact Temperature-Measuring Device and the Method Thereof; Google Patents: Mountain Veiw, CA, USA, 2010. [Google Scholar]
- ElecFreaks. Ultrasonic Ranging Module HC—SR04. Available online: https://cdn.sparkfun.com/datasheets/Sensors/Proximity/HCSR04.pdf (accessed on 23 October 2020).
- Melexis. Datasheet for MLX90614. Available online: https://components101.com/sites/default/files/component_datasheet/MLX90614-Datasheet.pdf (accessed on 30 October 2020).
- Systech, S. Advance Information 128 × 64 Dot Matrix OLED/PLED Segment/Common Driver with Controller. Available online: https://cdn-shop.adafruit.com/datasheets/SSD1306.pdf (accessed on 30 October 2020).
- Raj, A. Make a Non-Contact Infrared Thermometer with MLX90614 IR Temperature Sensor. Available online: https://circuitdigest.com/microcontroller-projects/ir-thermometer-using-arduino-and-ir-temperature-sensor (accessed on 22 May 2021).
- Arduino. Arduino Nano Datasheet. Available online: http://www.farnell.com/datasheets/1682238.pdf (accessed on 23 October 2020).
- Chen, H.-Y.; Chen, A.; Chen, C. Investigation of the Impact of Infrared Sensors on Core Body Temperature Monitoring by Comparing Measurement Sites. Sensors 2020, 20, 2885. [Google Scholar] [CrossRef]
- Sirinturk, S.; Govsa, F.; Pinar, Y.; Ozer, M.A. Study of frontal hairline patterns for natural design and restoration. Surg. Radiol. Anat. 2017, 39, 679–684. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; Version 3.6.2; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Micro: Bit Educational Foundation. BBC Micro:bit v2. Available online: https://tech.microbit.org/hardware/ (accessed on 23 October 2020).
- Broadcom Corporation. BCM2835 ARM Peripherals. Available online: https://www.raspberrypi.org/documentation/hardware/raspberrypi/bcm2835/BCM2835-ARM-Peripherals.pdf (accessed on 23 October 2020).
- Vesnovsky, O.; Li, Y.; Topoleski, L.D.T.; Zhu, L. Modeling of Differences Between Body Core and Forehead Temperatures Measured by Infrared Thermometers. In Proceedings of the 2017 Design of Medical Devices Conference, Minneapolis, MN, USA, 10–13 April 2017. [Google Scholar]
- Kistemaker, J.A.; Den Hartog, E.A.; Daanen, H.A. Reliability of an infrared forehead skin thermometer for core temperature measurements. J. Med. Eng. Technol. 2006, 30, 252–261. [Google Scholar] [CrossRef]
- Priego Quesada, J.I.; Martínez Guillamón, N.; Cibrián Ortiz de Anda, R.M.; Psikuta, A.; Annaheim, S.; Rossi, R.M.; Corberán Salvador, J.M.; Pérez-Soriano, P.; Salvador Palmer, R. Effect of perspiration on skin temperature measurements by infrared thermography and contact thermometry during aerobic cycling. Infrared Phys. Technol. 2015, 72, 68–76. [Google Scholar] [CrossRef]
- Liu, C.C.; Chang, R.E.; Chang, W.C. Limitations of forehead infrared body temperature detection for fever screening for severe acute respiratory syndrome. Infect. Control. Hosp. Epidemiol. 2004, 25, 1109–1111. [Google Scholar] [CrossRef]
- Jensen, B.N.; Jensen, F.S.; Madsen, S.N.; Løssl, K. Accuracy of digital tympanic, oral, axillary, and rectal thermometers compared with standard rectal mercury thermometers. Eur. J. Surg. 2000, 166, 848–851. [Google Scholar] [CrossRef] [PubMed]
- Cui, S.; Sun, B.; Sun, X. A method for improving temperature measurement accuracy on an infrared thermometer for the ambient temperature field. Rev. Sci. Instrum. 2020, 91, 054903. [Google Scholar] [CrossRef] [PubMed]
- Liedberg, H. Calibration of Infrared Radiation Thermometers; ResearchGate Technical Notes. 2013. Available online: https://www.researchgate.net/publication/281492916_Calibration_of_infrared_radiation_thermometers (accessed on 30 May 2021). [CrossRef]
- MacRae, B.A.; Annaheim, S.; Spengler, C.M.; Rossi, R.M. Skin Temperature Measurement Using Contact Thermometry: A Systematic Review of Setup Variables and Their Effects on Measured Values. Front. Physiol. 2018, 9. [Google Scholar] [CrossRef]
- Türe, E.; Yazar, A. How Should We Measure Body Temperature in the Pediatric Emergency Department? Which One Is the Most Accurate? J. Pediatric Infect. Dis. 2019, 14. [Google Scholar] [CrossRef]
- White, D.R.; Rourke, P.M.C. Standard platinum resistance thermometer interpolations in a revised temperature scale. Metrologia 2020, 57, 035003. [Google Scholar] [CrossRef]
- Quattrocchi, A.; Freni, F.; Montanini, R. Self-heat generation of embedded piezoceramic patches used for fabrication of smart materials. Sens. Actuators A Phys. 2018, 280, 513–520. [Google Scholar] [CrossRef]


| Volunteer | Temperature Difference between the Center of the Forehead and Left Forehead (°C) | Temperature Difference between the Center of the Forehead and Right Forehead (°C) |
|---|---|---|
| 1 | 0.13 | 0.31 |
| 2 | −0.16 | −0.51 |
| 3 | 0.04 | −0.69 |
| 4 | −0.51 | 0.00 |
| 5 | −0.03 | 0.55 |
| Distance (cm) | Volunteer | Difference between the Dry and Wet (Dry-Wet) Forehead (°C) | ||
|---|---|---|---|---|
| Center | Left | Right | ||
| 2.0 | 1 | 1.34 ± 0.01 | −2.85 ± 0.02 | 1.57 ± 0.01 |
| 2 | 1.85 ± 0.08 | 0.80 ± 0.07 | 2.35 ± 0.25 | |
| 3 | 2.49 ± 0.03 | 2.01 ± 0.06 | 0.34 ± 0.05 | |
| 4 | 1.89 ± 0.04 | 1.41 ± 0.02 | 0.96 ± 0.19 | |
| 5 | 1.03 ± 0.06 | 1.55 ± 0.07 | −0.18 ± 0.22 | |
| 2.5 | 1 | 1.69 ± 0.05 | 2.20 ± 0.01 | 2.81 ± 0.27 |
| 2 | 1.58 ± 0.01 | 0.28 ± 0.01 | 0.26 ± 0.07 | |
| 3 | 2.07 ± 0.02 | 1.55 ± 0.01 | −0.35 ± 0.18 | |
| 4 | 2.33 ± 0.05 | 1.34 ± 0.08 | 2.55 ± 0.17 | |
| 5 | 0.51 ± 0.89 | 0.72 ± 0.01 | −0.24 ± 0.22 | |
| 3.0 | 1 | 1.37 ± 0.06 | 1.86 ± 0.05 | 2.00 ± 0.01 |
| 2 | 2.60 ± 0.12 | −0.04 ± 0.00 | 1.47 ± 0.04 | |
| 3 | 2.36 ± 0.16 | 0.98 ± 0.01 | 1.26 ± 0.05 | |
| 4 | 1.79 ± 0.03 | 1.47 ± 0.04 | 0.90 ± 0.03 | |
| 5 | 1.66 ± 0.06 | 1.73 ± 0.02 | 1.32 ± 0.55 | |
| 3.5 | 1 | 1.87 ± 0.02 | 2.83 ± 0.08 | 2.75 ± 0.01 |
| 2 | 1.54 ± 0.00 | 0.00 ± 0.02 | 1.31 ± 0.02 | |
| 3 | 0.77 ± 0.09 | 0.82 ± 0.23 | 1.01 ± 0.22 | |
| 4 | 1.73 ± 0.00 | 2.13 ± 0.19 | 1.80 ± 0.23 | |
| 5 | 2.07 ± 0.00 | 0.76 ± 0.01 | 0.76 ± 0.01 | |
| 4.0 | 1 | 1.16 ± 0.06 | 2.83 ± 0.02 | 3.06 ± 0.00 |
| 2 | 0.80 ± 0.06 | 0.09 ± 0.01 | 1.49 ± 0.03 | |
| 3 | 1.09 ± 0.05 | −0.29 ± 0.17 | 0.36 ± 0.07 | |
| 4 | 1.69 ± 0.02 | 1.10 ± 0.03 | 1.10 ± 0.18 | |
| 5 | 1.93 ± 0.11 | 1.49 ± 0.01 | 0.94 ± 0.03 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goh, N.W.-J.; Poh, J.-J.; Yeo, J.Y.; Aw, B.J.-J.; Lai, S.C.; Cheng, J.J.W.; Tan, C.Y.L.; Gan, S.K.-E. Design and Development of a Low Cost, Non-Contact Infrared Thermometer with Range Compensation. Sensors 2021, 21, 3817. https://doi.org/10.3390/s21113817
Goh NW-J, Poh J-J, Yeo JY, Aw BJ-J, Lai SC, Cheng JJW, Tan CYL, Gan SK-E. Design and Development of a Low Cost, Non-Contact Infrared Thermometer with Range Compensation. Sensors. 2021; 21(11):3817. https://doi.org/10.3390/s21113817
Chicago/Turabian StyleGoh, Nicholas Wei-Jie, Jun-Jie Poh, Joshua Yi Yeo, Benjamin Jun-Jie Aw, Szu Cheng Lai, Jayce Jian Wei Cheng, Christina Yuan Ling Tan, and Samuel Ken-En Gan. 2021. "Design and Development of a Low Cost, Non-Contact Infrared Thermometer with Range Compensation" Sensors 21, no. 11: 3817. https://doi.org/10.3390/s21113817
APA StyleGoh, N. W.-J., Poh, J.-J., Yeo, J. Y., Aw, B. J.-J., Lai, S. C., Cheng, J. J. W., Tan, C. Y. L., & Gan, S. K.-E. (2021). Design and Development of a Low Cost, Non-Contact Infrared Thermometer with Range Compensation. Sensors, 21(11), 3817. https://doi.org/10.3390/s21113817






