The Impact of Weather and Seasons on Falls and Physical Activity among Older Adults with Glaucoma: A Longitudinal Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Falls and Follow-Up Data Collection
2.3. Physical Activity Data Collection
2.4. Weather and Seasons
2.5. Visual Field Data Collection
2.6. Covariates
2.7. Statistical Analysis
3. Results
3.1. Study Cohort
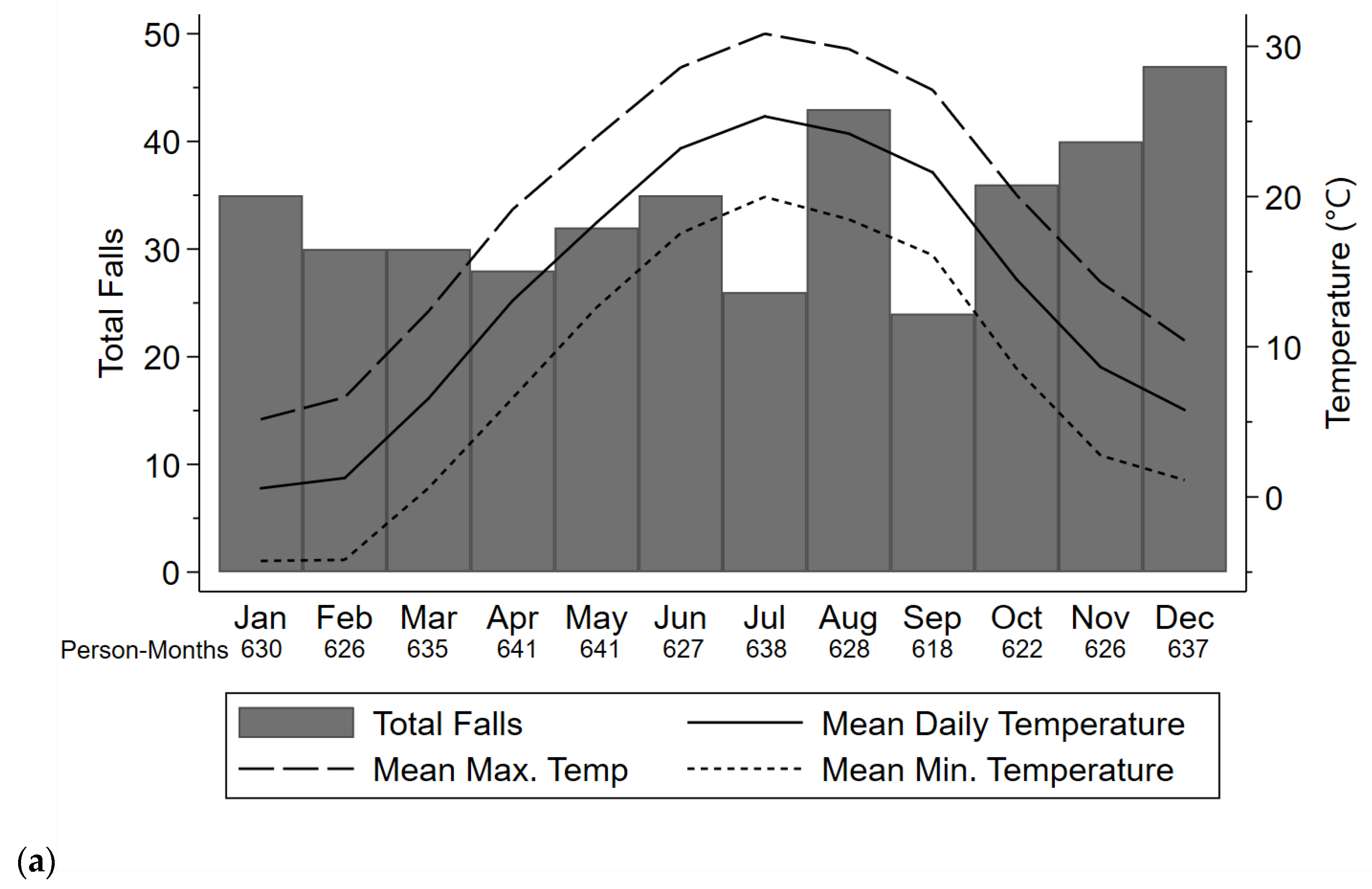
3.2. Falls
3.3. Injurious Falls
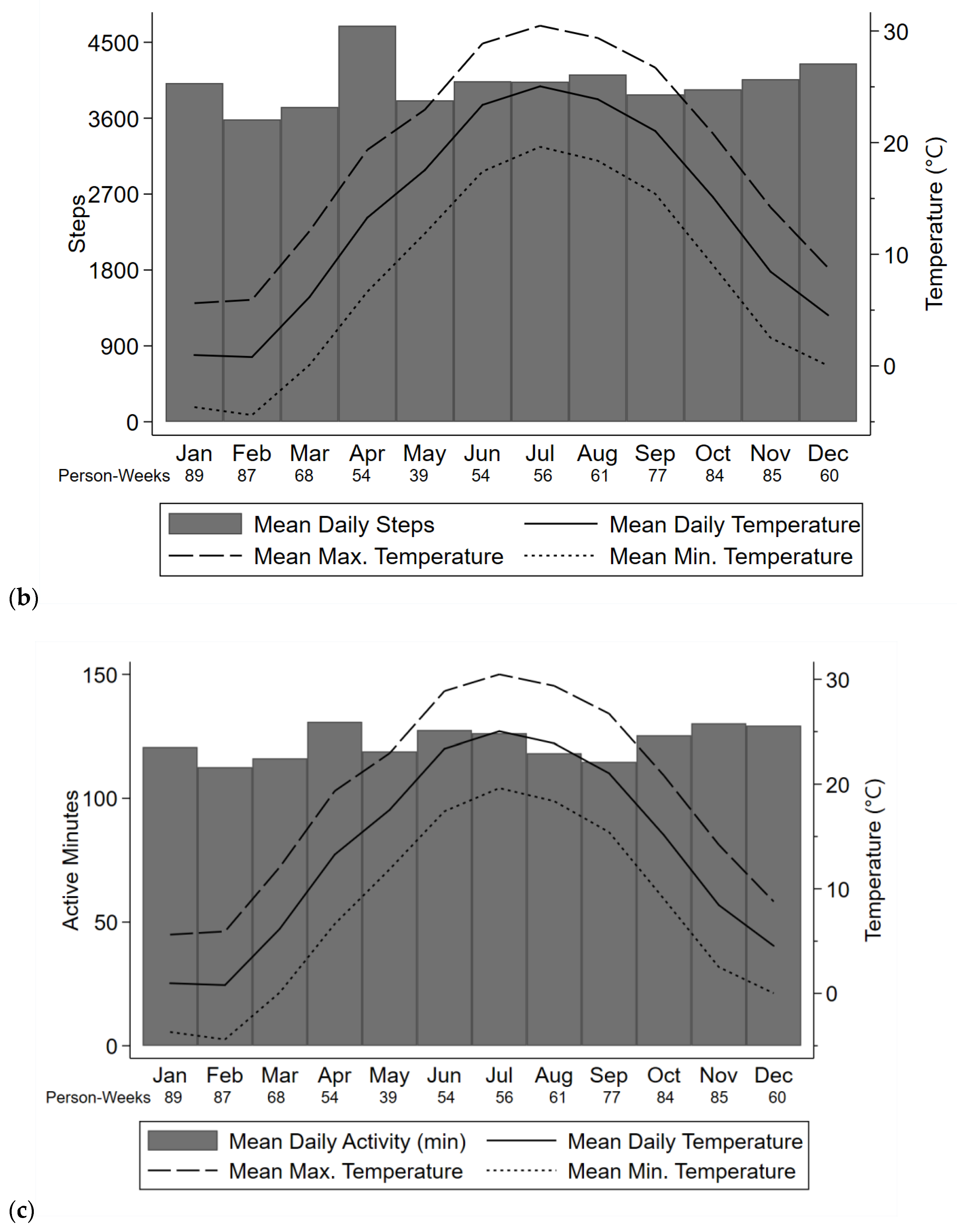
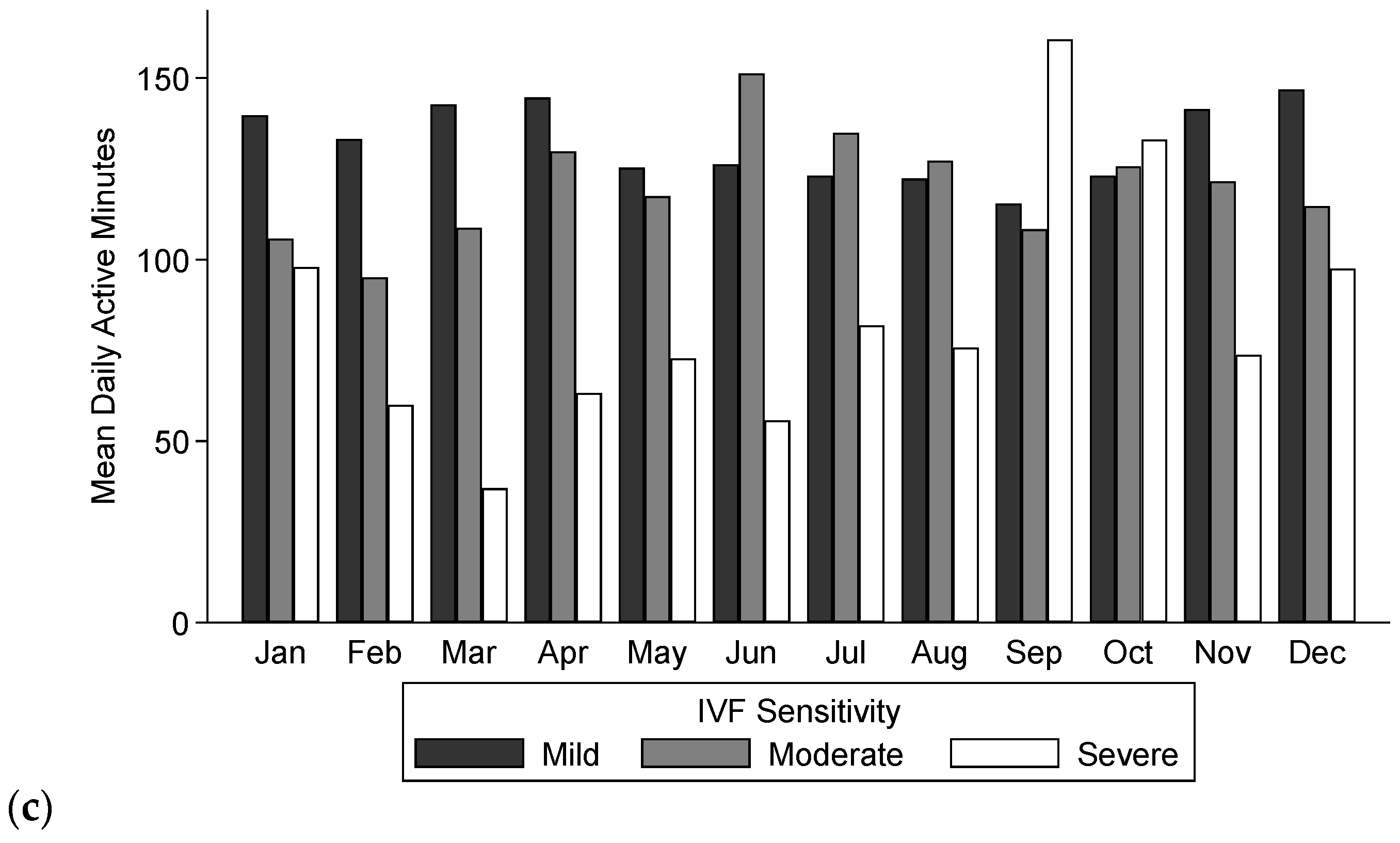
3.4. Daily Steps and Active Minutes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- 10 Leading Causes of Injury Deaths by Age Group Highlighting Unintentional Injury Deaths, United States-2018. Available online: https://www.cdc.gov/injury/images/lc-charts/leading_causes_of_death_by_age_group_unintentional_2018_1100w850h.jpg (accessed on 30 July 2020).
- National Estimates of the 10 Leading Causes of Nonfatal Injuries Treated in Hospital Emergency Departments, United States-2017. Available online: https://www.cdc.gov/injury/images/lc-charts/leading_causes_of_nonfatal_injury_2017_1100w850h.jpg (accessed on 30 July 2020).
- Bergen, G.; Stevens, M.R.; Burns, E.R. Falls and Fall Injuries Among Adults Aged ≥65 Years—United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 993–998. [Google Scholar] [CrossRef]
- Hartholt, K.A.; van Beeck, E.F.; Polinder, S.; van der Velde, N.; van Lieshout, E.M.M.; Panneman, M.J.M.; van der Cammen, T.J.M.; Patka, P. Societal Consequences of Falls in the Older Population: Injuries, Healthcare Costs, and Long-Term Reduced Quality of Life. J. Trauma Inj. Infect. Crit. Care 2011, 71, 748–753. [Google Scholar] [CrossRef] [PubMed]
- Zijlstra, G.A.R.; van Haastregt, J.C.M.; van Eijk JThM, I.E.; van Rossum, E.; Stalenhoef, P.A.; Kempen, G.I.J.M. Prevalence and Correlates of Fear of Falling, and Associated Avoidance of Activity in the General Population of Community-Living Older People. Age Ageing 2007, 36, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Florence, C.S.; Bergen, G.; Atherly, A.; Burns, E.; Stevens, J.; Drake, C. Medical Costs of Fatal and Nonfatal Falls in Older Adults: Medical Costs of Falls. J. Am. Geriatr. Soc. 2018, 66, 693–698. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention How Much Physical Activity Do Older Adults Need? Available online: https://www.cdc.gov/physicalactivity/basics/older_adults/index.htm (accessed on 1 January 2021).
- E, J.-Y.; Mihailovic, A.; Schrack, J.A.; Li, T.; Friedman, D.S.; West, S.K.; Gitlin, L.N.; Ramulu, P.Y. Characterizing Longitudinal Changes in Physical Activity and Fear of Falling after Falls in Glaucoma. J. Am. Geriatr. Soc. 2021. [Google Scholar] [CrossRef]
- Sun, F.; Norman, I.J.; While, A.E. Physical Activity in Older People: A Systematic Review. BMC Public Health 2013, 13, 449. [Google Scholar] [CrossRef]
- Yokota, M.; Fujita, T.; Nakahara, S.; Sakamoto, T. Clarifying Differences in Injury Patterns between Ground-Level Falls and Falls from Heights among the Elderly in Japan. Public Health 2020, 181, 114–118. [Google Scholar] [CrossRef]
- Qian, X.X.; Chau, P.H.; Kwan, C.W.; Lou, V.W.; Leung, A.Y.M.; Ho, M.; Fong, D.Y.T.; Chi, I. Seasonal Pattern of Single Falls and Recurrent Falls amongst Community-Dwelling Older Adults First Applying for Long-Term Care Services in Hong Kong. Age Ageing 2020, 49, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Launonen, A.P.; Lepola, V.; Saranko, A.; Flinkkilä, T.; Laitinen, M.; Mattila, V.M. Epidemiology of Proximal Humerus Fractures. Arch Osteoporos 2015, 10, 2. [Google Scholar] [CrossRef]
- Arnold, C.M.; Bello-Haas, V.P.M.D.; Farthing, J.P.; Crockett, K.L.; Haver, C.R.A.; Johnston, G.; Basran, J. Falls and Wrist Fracture: Relationship to Women’s Functional Status after Age 50. Can. J. Aging Rev. Can. Vieil. 2016, 35, 361–371. [Google Scholar] [CrossRef]
- Yeung, P.-Y.; Chau, P.-H.; Woo, J.; Yim, V.W.-T.; Rainer, T.H. Higher Incidence of Falls in Winter among Older People in Hong Kong. J. Clin. Gerontol. Geriatr. 2011, 2, 13–16. [Google Scholar] [CrossRef]
- Bulajic-Kopjar, M. Seasonal Variations in Incidence of Fractures among Elderly People. Inj. Prev. 2000, 6, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, S.E.L.; Bell, K.; Ward, N.; Cooke, C.; Inder, W.J. Seasonality of Hip Fracture and Vitamin D Deficiency Persists in a Sub-tropical Climate. Intern. Med. J. 2019, 49, 1029–1032. [Google Scholar] [CrossRef]
- Stevens, J.A.; Thomas, K.E.; Sogolow, E.D. Seasonal Patterns of Fatal and Nonfatal Falls among Older Adults in the U.S. Accid. Anal. Prev. 2007, 39, 1239–1244. [Google Scholar] [CrossRef]
- Witham, M.D.; Donnan, P.T.; Vadiveloo, T.; Sniehotta, F.F.; Crombie, I.K.; Feng, Z.; McMurdo, M.E.T. Association of Day Length and Weather Conditions with Physical Activity Levels in Older Community Dwelling People. PLoS ONE 2014, 9, e85331. [Google Scholar] [CrossRef]
- Sumukadas, D.; Witham, M.; Struthers, A.; McMurdo, M. Day Length and Weather Conditions Profoundly Affect Physical Activity Levels in Older Functionally Impaired People. J. Epidemiol. Community Health 2009, 63, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Klenk, J.; Büchele, G.; Rapp, K.; Franke, S.; Peter, R.; ActiFE Study Group. Walking on Sunshine: Effect of Weather Conditions on Physical Activity in Older People. J. Epidemiol. Community Health 2012, 66, 474–476. [Google Scholar] [CrossRef]
- Jones, G.R.; Brandon, C.; Gill, D.P. Physical Activity Levels of Community-Dwelling Older Adults Are Influenced by Winter Weather Variables. Arch. Gerontol. Geriatr. 2017, 71, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Togo, F.; Watanabe, E.; Park, H.; Shephard, R.J.; Aoyagi, Y. Meteorology and the Physical Activity of the Elderly: The Nakanojo Study. Int. J. Biometeorol. 2005, 50, 83–89. [Google Scholar] [CrossRef]
- Hasegawa, J.; Suzuki, H.; Yamauchi, T. Impact of Season on the Association between Muscle Strength/Volume and Physical Activity among Community-Dwelling Elderly People Living in Snowy-Cold Regions. J. Physiol. Anthropol. 2018, 37, 25. [Google Scholar] [CrossRef]
- Reed-Jones, R.J.; Solis, G.R.; Lawson, K.A.; Loya, A.M.; Cude-Islas, D.; Berger, C.S. Vision and Falls: A Multidisciplinary Review of the Contributions of Visual Impairment to Falls among Older Adults. Maturitas 2013, 75, 22–28. [Google Scholar] [CrossRef]
- Crews, J.E.; Chou, C.-F.; Stevens, J.A.; Saaddine, J.B. Falls Among Persons Aged ≥65 Years With and Without Severe Vision Impairment—United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Freeman, E.E.; Mun~oz, B.; Rubin, G.; West, S.K. Visual Field Loss Increases the Risk of Falls in Older Adults: The Salisbury Eye Evaluation. Investig. Opthalmol. Vis. Sci. 2007, 48, 4445. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.R.; Crowston, J.G.; Loprinzi, P.D.; Ramulu, P.Y. Physical Activity, Visual Impairment, and Eye Disease. Eye 2018, 32, 1296–1303. [Google Scholar] [CrossRef] [PubMed]
- Willis, J.R. Visual Impairment, Uncorrected Refractive Error, and Accelerometer-Defined Physical Activity in the United States. Arch. Ophthalmol. 2012, 130, 329. [Google Scholar] [CrossRef] [PubMed]
- van Landingham, S.W.; Willis, J.R.; Vitale, S.; Ramulu, P.Y. Visual Field Loss and Accelerometer-Measured Physical Activity in the United States. Ophthalmology 2012, 119, 2486–2492. [Google Scholar] [CrossRef] [PubMed]
- Ramulu, P.Y.; Maul, E.; Hochberg, C.; Chan, E.S.; Ferrucci, L.; Friedman, D.S. Real-World Assessment of Physical Activity in Glaucoma Using an Accelerometer. Ophthalmology 2012, 119, 1159–1166. [Google Scholar] [CrossRef]
- Lee, M.J.; Wang, J.; Friedman, D.S.; Boland, M.V.; De Moraes, C.G.; Ramulu, P.Y. Greater Physical Activity Is Associated with Slower Visual Field Loss in Glaucoma. Ophthalmology 2019, 126, 958–964. [Google Scholar] [CrossRef]
- E, J.-Y.; Schrack, J.A.; Mihailovic, A.; Wanigatunga, A.A.; West, S.K.; Friedman, D.S.; Gitlin, L.N.; Li, T.; Ramulu, P.Y. Patterns of Daily Physical Activity across the Spectrum of Visual Field Damage in Glaucoma Patients. Ophthalmology 2021, 128, 70–77. [Google Scholar] [CrossRef]
- Average Weather in Baltimore. Available online: https://weatherspark.com/y/21918/Average-Weather-in-Baltimore-Maryland-United-States-Year-Round#:~:text=The%20hot%20season%20lasts%20for,temperature%20below%2052%C2%B0F (accessed on 16 January 2021).
- Ramulu, P.Y.; Mihailovic, A.; West, S.K.; Gitlin, L.N.; Friedman, D.S. Predictors of Falls per Step and Falls per Year At and Away From Home in Glaucoma. Am. J. Ophthalmol. 2019, 200, 169–178. [Google Scholar] [CrossRef]
- Mihailovic, A.; Swenor, B.K.; Friedman, D.S.; West, S.K.; Gitlin, L.N.; Ramulu, P.Y. Gait Implications of Visual Field Damage from Glaucoma. Transl. Vis. Sci. Technol. 2017, 6, 23. [Google Scholar] [CrossRef] [PubMed]
- Ramulu, P.Y.; Mihailovic, A.; West, S.K.; Friedman, D.S.; Gitlin, L.N. What Is a Falls Risk Factor? Factors Associated with Falls per Time or per Step in Individuals with Glaucoma. J. Am. Geriatr. Soc. 2019, 67, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Sotimehin, A.E.; Yonge, A.V.; Mihailovic, A.; West, S.K.; Friedman, D.S.; Gitlin, L.N.; Ramulu, P.Y. Locations, Circumstances, and Outcomes of Falls in Patients With Glaucoma. Am. J. Ophthalmol. 2018, 192, 131–141. [Google Scholar] [CrossRef]
- Climate Data Online. Available online: https://www.ncdc.noaa.gov/cdo-web/datasets/GHCND/stations/GHCND:USW00093721/detail (accessed on 9 May 2020).
- Hodapp, E.; Parrish, R.K.; Anderson, D.R. Clinical Decisions in Glaucoma; Mosby: St. Louis, MO, USA, 1993; ISBN 978-0-8016-6799-2. [Google Scholar]
- Saari, P.; Heikkinen, E.; Sakari-Rantala, R.; Rantanen, T. Fall-Related Injuries among Initially 75- and 80-Year Old People during a 10-Year Follow-Up. Arch. Gerontol. Geriatr. 2007, 45, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Vikman, I.; Nordlund, A.; Näslund, A.; Nyberg, L. Incidence and Seasonality of Falls amongst Old People Receiving Home Help Services in a Municipality in Northern Sweden. Int. J. Circumpolar Health 2011, 70, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Spalt, E.W.; Curl, C.L.; Allen, R.W.; Cohen, M.; Adar, S.D.; Stukovsky, K.H.; Avol, E.; Castro-Diehl, C.; Nunn, C.; Mancera-Cuevas, K.; et al. Time-Location Patterns of a Diverse Population of Older Adults: The Multi-Ethnic Study of Atherosclerosis and Air Pollution (MESA Air). J. Expo. Sci. Environ. Epidemiol. 2016, 26, 349–355. [Google Scholar] [CrossRef]
- Chippendale, T.; Raveis, V. Knowledge, Behavioral Practices, and Experiences of Outdoor Fallers: Implications for Prevention Programs. Arch. Gerontol. Geriatr. 2017, 72, 19–24. [Google Scholar] [CrossRef]
- Ganz, D.A.; Higashi, T.; Rubenstein, L.Z. Monitoring Falls in Cohort Studies of Community-Dwelling Older People: Effect of the Recall Interval: Monitoring Falls in Community-Dwelling Older People. J. Am. Geriatr. Soc. 2005, 53, 2190–2194. [Google Scholar] [CrossRef]


| Characteristics | Values (n = 244) |
|---|---|
| Age (years), mean (SD) | 70.6 (7.6) |
| Male, n (%) | 125 (51.2) |
| African-American race, n (%) | 70 (28.7) |
| Living alone, n (%) | 49 (20.1) |
| Employed, n (%) | 87 (35.7) |
| Education *, n (%) | |
| Less than high school | 8 (3.3) |
| High school | 29 (11.9) |
| Some college | 33 (13.5) |
| Bachelor’s degree | 59 (24.2) |
| Higher than Bachelor’s degree | 114 (46.7) |
| Health | |
| Comorbid illnesses >1, n (%) | 159 (65) |
| Polypharmacy, n (%) | 81 (33) |
| Body mass index (kg/m2), mean (SD) | 27.2 (5.1) |
| Grip strength (kg), mean (SD) | 31.6 (10.3) |
| Lower body strength (kg), mean (SD) | 17.7 (6.0) |
| Vision, median (IQR) | |
| IVF sensitivity (dB) | 28 (26.0, 29.7) |
| Mean deviation better eye | −2.5 (−5.4, −0.7) |
| Mean deviation worse eye | −5.7 (−12.9, −2.8) |
| Better eye visual acuity-logMAR | 0.1 (0, 0.2) |
| Binocular log CS | 1.7 (1.6, 1.8) |
| Likelihood of Falling | Likelihood a Fall Is Injurious vs. Non-Injurious | Likelihood of Fall Occurring Outdoors vs. Indoors | Likelihood of Injurious Fall Occurring Outdoors vs. Indoors | |||||
|---|---|---|---|---|---|---|---|---|
| Weather Variable | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p |
| Temperature | ||||||||
| Average daily temperature per 10 °C increment | 0.92 (0.84, 1.02) | 0.12 | 1.24 (1.01, 1.53) | 0.04 | 1.03 (0.84, 1.26) | 0.76 | 1.46 (1.03, 2.07) | 0.03 |
| Average daily temperature > 10 °C vs. ≤10 °C | 0.84 (0.69, 1.02) | 0.09 | 1.42 (0.92, 2.18) | 0.11 | 1.02 (0.67, 1.54) | 0.94 | 1.91 (0.98, 3.69) | 0.06 |
| Precipitation | ||||||||
| Daily precipitation (mm) | 1.05 (0.82, 1.35) | 0.70 | 1.28 (0.68, 2.41) | 0.44 | 0.56 (0.29, 1.09) | 0.09 | 0.48 (0.17, 1.38) | 0.18 |
| Presence of precipitation vs. no precipitation | 1.12 (0.92, 1.37) | 0.27 | 0.96 (0.62, 1.47) | 0.84 | 0.74 (0.48, 1.13) | 0.16 | 1.24 (0.64, 2.40) | 0.52 |
| Season | ||||||||
| Spring vs. Winter | 0.87 (0.65, 1.15) | 0.33 | 0.61 (0.33, 1.13) | 0.12 | 0.57 (0.31, 1.04) | 0.07 | 1.53 (0.56, 4.16) | 0.41 |
| Summer vs. Winter | 0.98 (0.74, 1.29) | 0.90 | 1.55 (0.86, 2.77) | 0.14 | 1.15 (0.64, 2.06) | 0.65 | 2.69 (1.12, 6.50) | 0.03 |
| Autumn vs. Winter | 1.15 (0.88, 1.51) | 0.31 | 1.11 (0.62, 1.98) | 0.73 | 0.79 (0.44, 1.41) | 0.43 | 1.11 (0.46, 2.66) | 0.82 |
| Average Daily Steps | Average Daily Active Minutes | |||
|---|---|---|---|---|
| Weather Variable | RR (95% CI) | p | RR (95% CI) | p |
| Temperature | ||||
| Average daily temperature per 10 °C increment | 1.01 (0.94, 1.09) | 0.77 | 1.01 (0.94, 1.09) | 0.77 |
| Average daily temperature > 10 °C vs. ≤10 °C | 1.00 (0.87, 1.16) | 0.95 | 1.01 (0.88, 1.17) | 0.88 |
| Precipitation | ||||
| Average daily precipitation (mm) | 1.11 (0.72, 1.71) | 0.63 | 0.93 (0.59, 1.44) | 0.73 |
| Presence of precipitation vs. no precipitation | 0.97 (0.80, 1.18) | 0.77 | 0.94 (0.77, 1.15) | 0.57 |
| Season | ||||
| Spring vs. Winter | 1.10 (0.90, 1.34) | 0.35 | 1.07 (0.87, 1.31) | 0.54 |
| Summer vs. Winter | 1.03 (0.85, 1.26) | 0.74 | 1.04 (0.85, 1.28) | 0.69 |
| Autumn vs. Winter | 1.07 (0.90, 1.28) | 0.44 | 1.07 (0.90, 1.29) | 0.44 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vongsachang, H.; Mihailovic, A.; E, J.-Y.; Friedman, D.S.; West, S.K.; Gitlin, L.N.; Ramulu, P.Y. The Impact of Weather and Seasons on Falls and Physical Activity among Older Adults with Glaucoma: A Longitudinal Prospective Cohort Study. Sensors 2021, 21, 3415. https://doi.org/10.3390/s21103415
Vongsachang H, Mihailovic A, E J-Y, Friedman DS, West SK, Gitlin LN, Ramulu PY. The Impact of Weather and Seasons on Falls and Physical Activity among Older Adults with Glaucoma: A Longitudinal Prospective Cohort Study. Sensors. 2021; 21(10):3415. https://doi.org/10.3390/s21103415
Chicago/Turabian StyleVongsachang, Hursuong, Aleksandra Mihailovic, Jian-Yu E, David S. Friedman, Sheila K. West, Laura N. Gitlin, and Pradeep Y. Ramulu. 2021. "The Impact of Weather and Seasons on Falls and Physical Activity among Older Adults with Glaucoma: A Longitudinal Prospective Cohort Study" Sensors 21, no. 10: 3415. https://doi.org/10.3390/s21103415
APA StyleVongsachang, H., Mihailovic, A., E, J.-Y., Friedman, D. S., West, S. K., Gitlin, L. N., & Ramulu, P. Y. (2021). The Impact of Weather and Seasons on Falls and Physical Activity among Older Adults with Glaucoma: A Longitudinal Prospective Cohort Study. Sensors, 21(10), 3415. https://doi.org/10.3390/s21103415






