Recent Advances in Electrochemical and Optical Biosensors Designed for Detection of Interleukin 6
Abstract
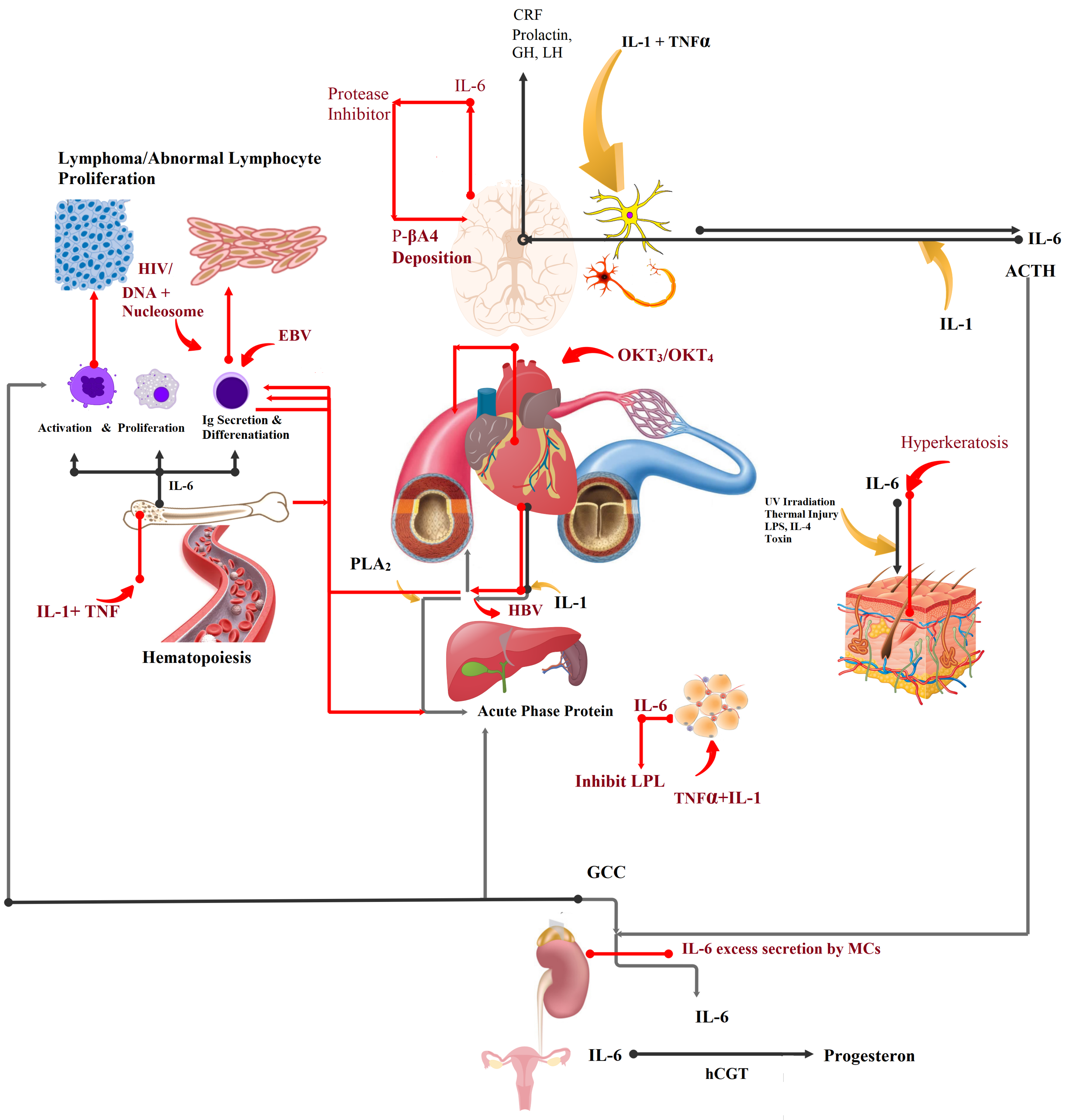
1. Introduction
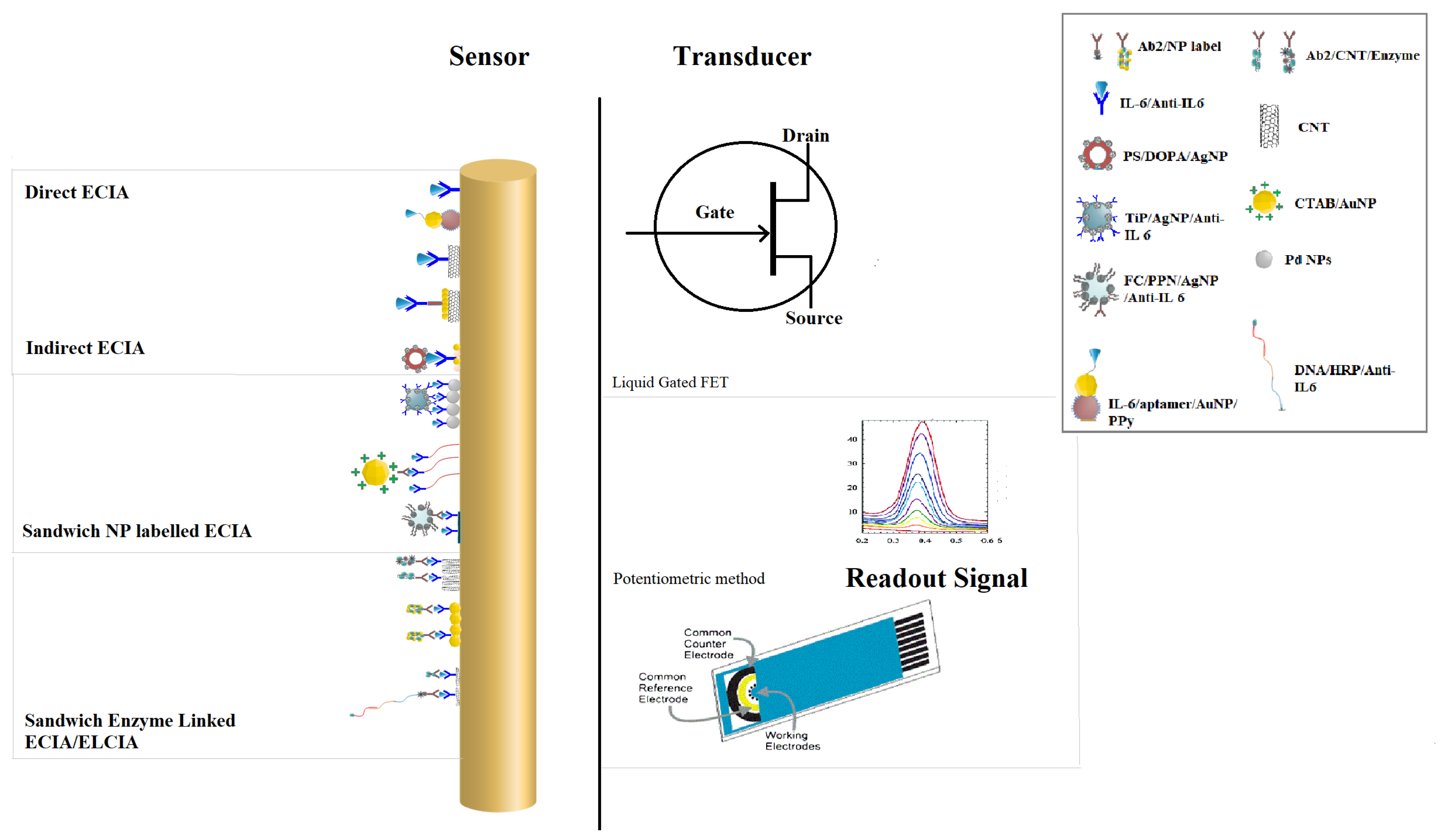
2. Electrochemical Biosensors
2.1. Detection Mechanism
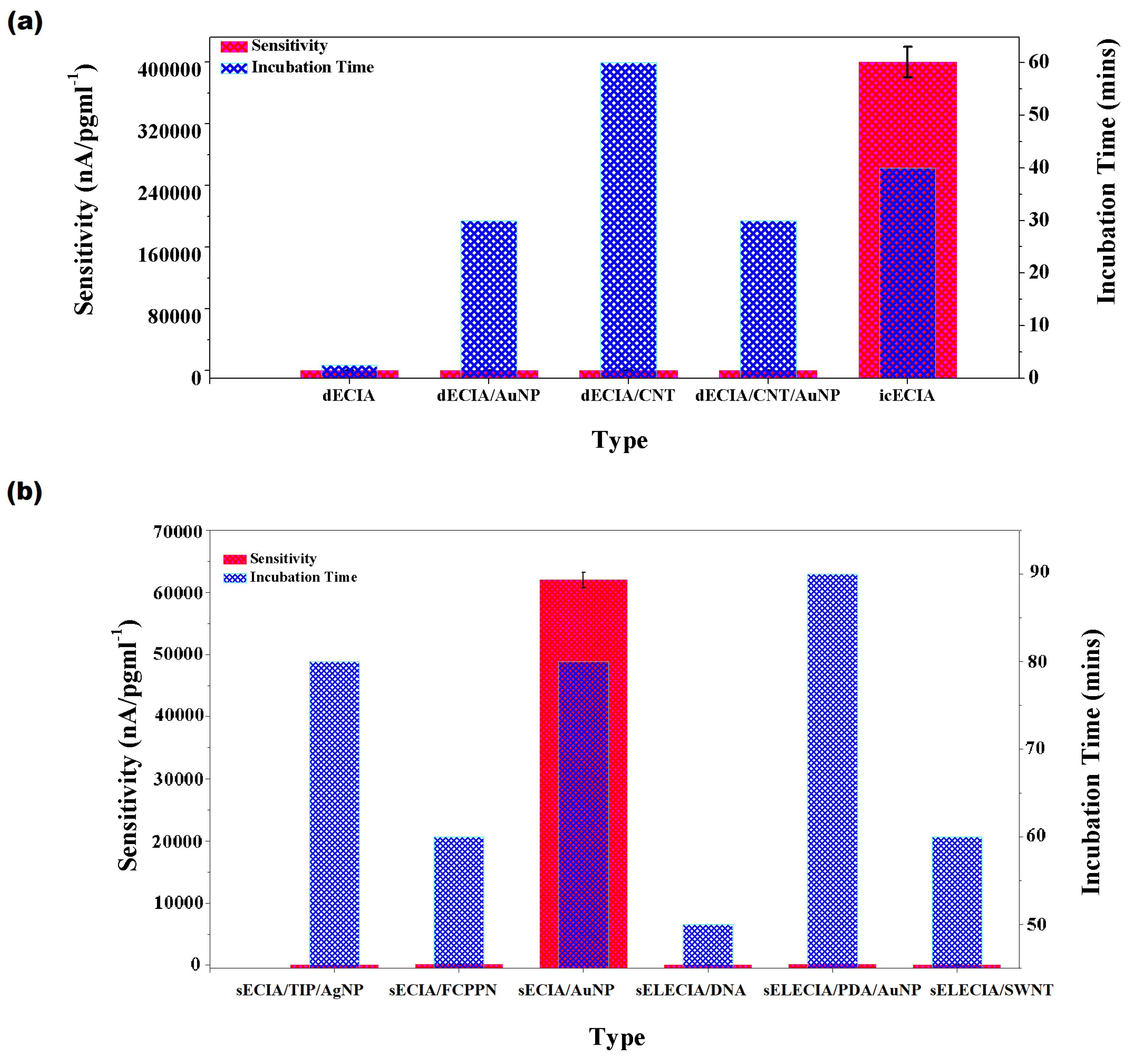
2.1.1. Direct Electrochemical Immunoassay (dECIA)
2.1.2. Indirect Competitive Electrochemical Immunoassay (icECIA)
2.1.3. Sandwich Nanoparticles Labeled Electrochemical Immunoassay (sECIA-NP)
2.1.4. Sandwich Enzyme Linked Electrochemical Immunoassay (sELECIA)
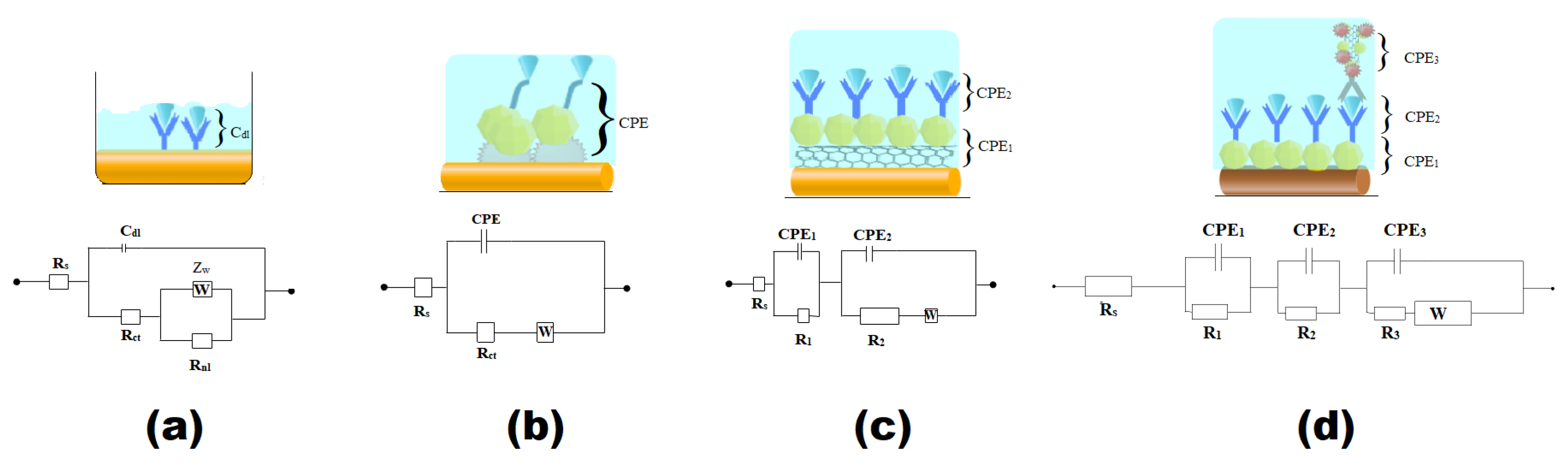
2.2. Electrode Interface
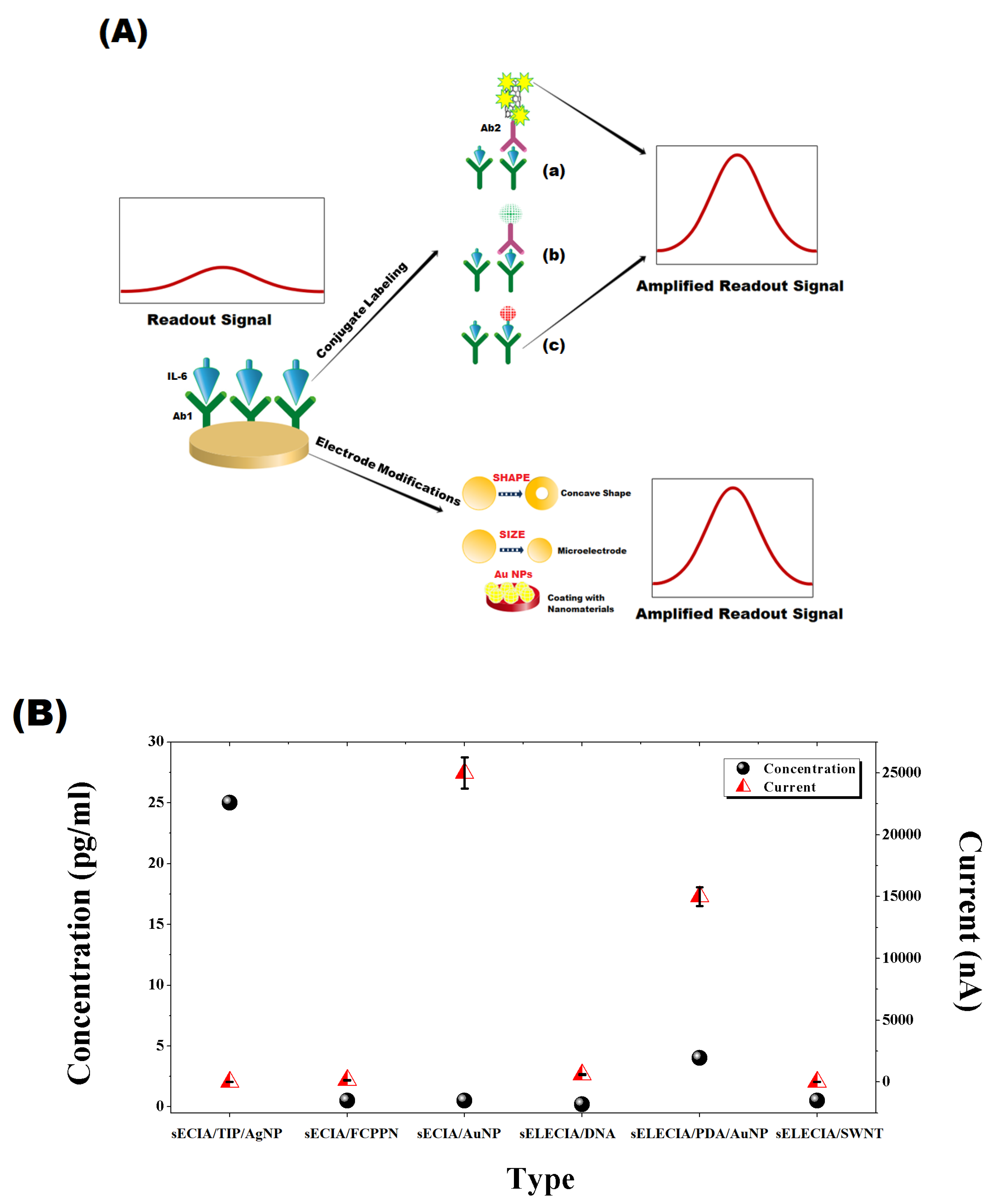
2.3. Signal Amplification
2.4. Sensitivity and Selectivity
2.5. Dynamic Range
2.6. Stability
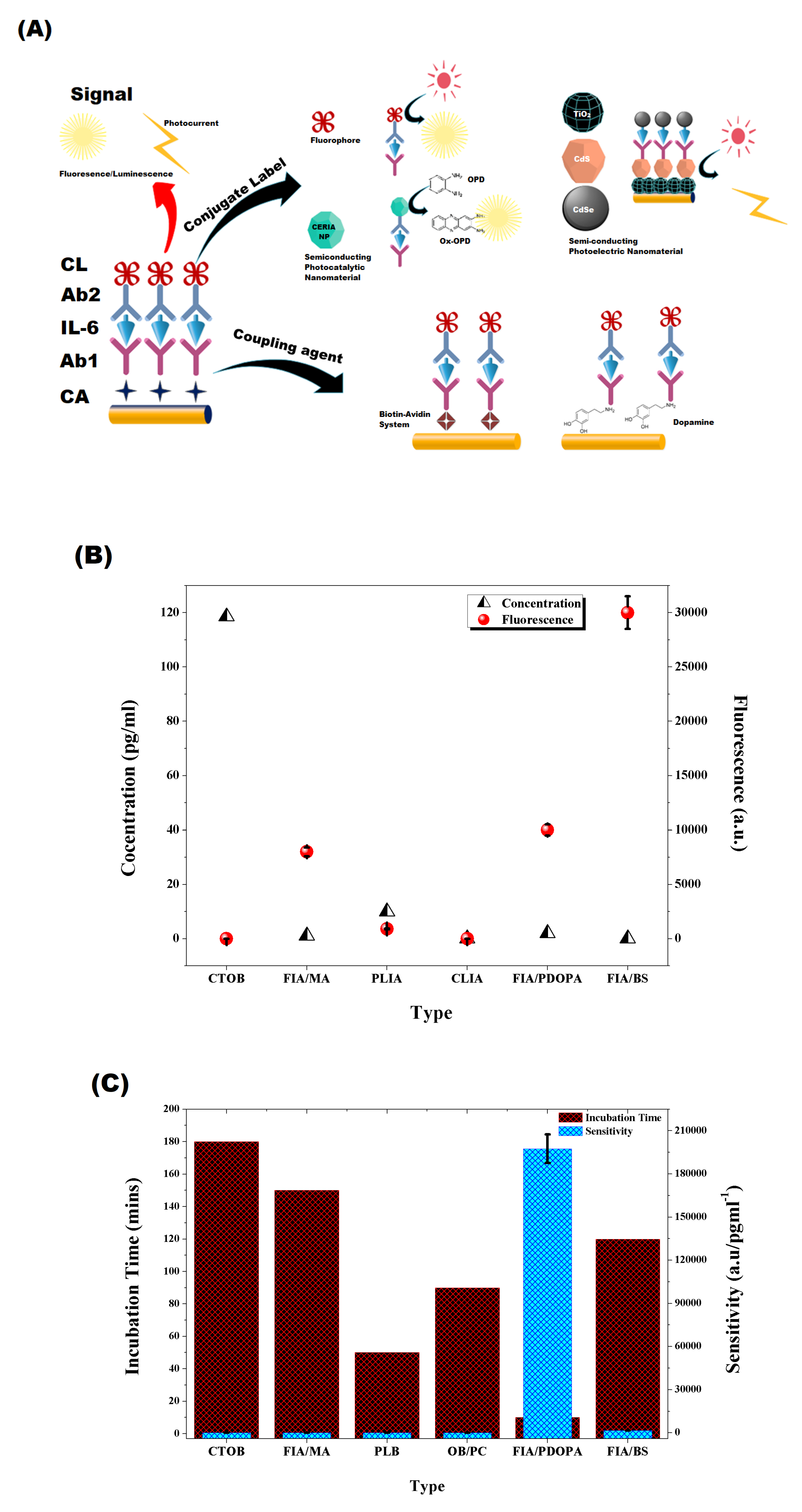
3. Optical Biosensor
3.1. Sensor Structure
3.2. Signal Amplification Strategies in Optical Biosensor
3.2.1. Coupling Agent
3.2.2. Conjugate Labeling
3.2.3. Detecting Signal
4. Conclusions
Funding
Conflicts of Interest
Abbreviations
| IL-6 | Interleukin 6 |
| IL-6R | Interleukin 6 Receptor |
| TNF | Tumor Necrosis Factor |
| ACTH | Adrenocorticotrophic Hormone |
| CRF | Corticotrophin Releasing Factor |
| GCC | Glucocorticoid Hormone |
| CRP | c-reactive Protein |
| AD | Alzheimer’s Disease |
| LPL | Lipoprotein Lipase |
| dECIA | Direct Electrochemical Immunoassay |
| icECIA | Indirect Competitive Electrochemical Immunoassay |
| sECIA-NP | Sandwich Nanoparticles Labeled Electrochemical Immunoassay |
| sELECIA | Sandwich Enzyme Linked Electrochemical Immunoassay |
| FIA | Fluorescent Immunoassay |
| CLIA | Chemiluminescent Immunoassay |
| PECIA | Photo-Electrochemical Immunoassay |
| PLIA | Photoluminescence Immunoassay |
| PPy | Polypyrrole |
| CNT | Carbon Nanotubes |
| CTOB | Combination Tapered Optic Fiber Biosensor |
References
- Kishimoto, T.; Tanaka, T. Interleukin 6. In Encyclopedia of Inflammatory Diseases; Springer: New York, NY, USA, 2015; pp. 1–8. [Google Scholar]
- Sehgal, P. Interleukin-6: A regulator of plasma protein gene expression in hepatic and non-hepatic tissues. Mol. Biol. Med. 1990, 7, 117–130. [Google Scholar] [PubMed]
- Akira, S.; Hirano, T.; Taga, T.; Kishimoto, T. Biology of multifunctional cytokines: IL-6 and related molecules (IL 1 & TNF). FASEB J. 1990, 4, 2860–2867. [Google Scholar]
- Hirano, T.; Akira, S.; Taga, T.; Kishimoto, T. Biological and clinical aspects of interleukin 6. Immunol. Today 1990, 11, 443–449. [Google Scholar] [CrossRef]
- Van Snick, J. Interleukin-6: An overview. Annu. Rev. Immunol. 1990, 8, 253–278. [Google Scholar] [CrossRef] [PubMed]
- Akira, S.; Taga, T.; Kishimoto, T. Interleukin-6 in biology and medicine. In Advances in Immunology; Elsevier: Amsterdam, The Netherlands, 1993; Volume 54, pp. 1–78. [Google Scholar]
- May, L.T.; Santhanam, U.; Tatter, S.B.; Bhardwaj, N.; Ghrayeb, J.; Sehgal, P.B. Phosphorylation of secreted forms of human β2-interferon/hepatocyte stimulating factor/interleukin-6. Biochem. Biophys. Res. Commun. 1988, 152, 1144–1150. [Google Scholar] [CrossRef]
- Hirano, T.; Yasukawa, K.; Harada, H.; Taga, T.; Watanabe, Y.; Matsuda, T.; Kashiwamura, S.I.; Nakajima, K.; Koyama, K.; Iwamatsu, A.; et al. Complementary DNA for a novel human interleukin (BSF-2) that induces B lymphocytes to produce immunoglobulin. Nature 1986, 324, 73–76. [Google Scholar] [CrossRef]
- Van Snick, J.; Cayphas, S.; Szikora, J.P.; Renauld, J.C.; Van Roost, E.; Boon, T.; Sirnpson, R.J. cDNA cloning of murine interleukin-HP1: Homology with human interleukin 6. Eur. J. Immunol. 1988, 18, 193–197. [Google Scholar] [CrossRef]
- Northemann, W.; Braciak, T.; Hattori, M.; Lee, F.; Fey, G.H. Structure of the rat interleukin 6 gene and its expression in macrophage-derived cells. J. Biol. Chem. 1989, 264, 16072–16082. [Google Scholar]
- Bazan, J.F. Haemopoietic receptors and helical cytokines. Immunol. Today 1990, 11, 350–354. [Google Scholar] [CrossRef]
- Yamasaki, K.; Taga, T.; Hirata, Y.; Yawata, H.; Kawanishi, Y.; Seed, B.; Taniguchi, T.; Hirano, T.; Kishimoto, T. Cloning and expression of the human interleukin-6 (BSF-2/IFN beta 2) receptor. Science 1988, 241, 825–828. [Google Scholar] [CrossRef]
- Sugita, T.; Totsuka, T.; Saito, M.; Yamasaki, K.; Taga, T.; Hirano, T.; Kishimoto, T. Functional murine interleukin 6 receptor with the intracisternal A particle gene product at its cytoplasmic domain. Its possible role in plasmacytomagenesis. J. Exp. Med. 1990, 171, 2001–2009. [Google Scholar] [CrossRef] [PubMed]
- Taga, T.; Narazaki, M.; Yasukawa, K.; Saito, T.; Miki, D.; Hamaguchi, M.; Davis, S.; Shoyab, M.; Yancopoulos, G.D.; Kishimoto, T. Functional inhibition of hematopoietic and neurotrophic cytokines by blocking the interleukin 6 signal transducer gp130. Proc. Natl. Acad. Sci. USA 1992, 89, 10998–11001. [Google Scholar] [CrossRef] [PubMed]
- Yawata, H.; Yasukawa, K.; Natsuka, S.; Murakami, M.; Yamasaki, K.; Hibi, M.; Taga, T.; Kishimoto, T. Structure-function analysis of human IL-6 receptor: Dissociation of amino acid residues required for IL-6-binding and for IL-6 signal transduction through gp130. EMBO J. 1993, 12, 1705–1712. [Google Scholar] [CrossRef] [PubMed]
- Taga, T.; Hibi, M.; Hirata, Y.; Yamasaki, K.; Yasukawa, K.; Matsuda, T.; Hirano, T.; Kishimoto, T. Interleukin-6 triggers the association of its receptor with a possible signal transducer, gp130. Cell 1989, 58, 573–581. [Google Scholar] [CrossRef]
- Hibi, M.; Murakami, M.; Saito, M.; Hirano, T.; Taga, T.; Kishimoto, T. Molecular cloning and expression of an IL-6 signal transducer, gp130. Cell 1990, 63, 1149–1157. [Google Scholar] [CrossRef]
- Murakami, M.; Narazaki, M.; Hibi, M.; Yawata, H.; Yasukawa, K.; Hamaguchi, M.; Taga, T.; Kishimoto, T. Critical cytoplasmic region of the interleukin 6 signal transducer gp130 is conserved in the cytokine receptor family. Proc. Natl. Acad. Sci. USA 1991, 88, 11349–11353. [Google Scholar] [CrossRef]
- Lieberman, A.P.; Pitha, P.M.; Shin, H.S.; Shin, M.L. Production of tumor necrosis factor and other cytokines by astrocytes stimulated with lipopolysaccharide or a neurotropic virus. Proc. Natl. Acad. Sci. USA 1989, 86, 6348–6352. [Google Scholar] [CrossRef]
- Satoh, T.; Nakamura, S.; Taga, T.; Matsuda, T.; Hirano, T.; Kishimoto, T.; Kaziro, Y. Induction of neuronal differentiation in PC12 cells by B-cell stimulatory factor 2/interleukin 6. Mol. Cell. Biol. 1988, 8, 3546–3549. [Google Scholar] [CrossRef]
- Spangelo, B.L.; Judd, A.M.; Isakson, P.C.; Macleod, R.M. Interleukin-6 stimulates anterior pituitary hormone release in vitro. Endocrinology 1989, 125, 575–577. [Google Scholar] [CrossRef]
- Lyson, K. The stimulatory effect of interleukin-6 on corticotrophin-releasing factor and thyrotropin-releasing hormone secretion in vitro. Prog. Neuroendocrinol. Immunol. 1991, 4, 161–165. [Google Scholar]
- Navarra, P.; Tsagarakis, S.; Faria, M.S.; Rees, L.H.; Besser, G.M.; Grossman, A.B. Interleukins-1 and -6 stimulate the release of corticotropin-releasing hormone-41 from rat hypothalamus in vitro via the eicosanoid cyclooxygenase pathway. Endocrinology 1991, 128, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Naitoh, Y.; Fukata, J.; Tominaga, T.; Nakai, Y.; Tamai, S.; Mori, K.; Imura, H. Interleukin-6 stimulates the secretion of adrenocorticotropic hormone in conscious, freely-moving rats. Biochem. Biophys. Res. Commun. 1988, 155, 1459–1463. [Google Scholar] [CrossRef]
- De Simoni, M.G.; Sironi, M.; De Luigi, A.; Manfridi, A.; Mantovani, A.; Ghezzi, P. Intracerebroventricular injection of interleukin 1 induces high circulating levels of interleukin 6. J. Exp. Med. 1990, 171, 1773–1778. [Google Scholar] [CrossRef] [PubMed]
- LeMay, L.; Vander, A.J.; Kluger, M.J. Role of interleukin 6 in fever in rats. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 1990, 258, R798–R803. [Google Scholar] [CrossRef] [PubMed]
- Leu, S.J.C.; Singh, V.K. Stimulation of interleukin-6 production by corticotropin-releasing factor. Cell. Immunol. 1992, 143, 220–227. [Google Scholar] [CrossRef]
- Salas, M.; Evans, S.; Levell, M.; Whicher, J. Interleukin-6 and ACTH act synergistically to stimulate the release of corticosterone from adrenal gland cells. Clin. Exp. Immunol. 1990, 79, 470–473. [Google Scholar] [CrossRef]
- Schooltink, H.; Schmitz-Van de Leur, H.; Heinrich, P.C.; Rose-John, S. Up-regulation of the interleukin-6-signal transducing protein (gp130) by interleukin-6 and dexamethasone in HepG2 cells. FEBS Lett. 1992, 297, 263–265. [Google Scholar] [CrossRef]
- Snyers, L.; De Wit, L.; Content, J. Glucocorticoid up-regulation of high-affinity interleukin 6 receptors on human epithelial cells. Proc. Natl. Acad. Sci. USA 1990, 87, 2838–2842. [Google Scholar] [CrossRef]
- Kushner, I. The phenomenon of the acute phase response. Ann. N. Y. Acad. Sci. 1982, 389, 39–48. [Google Scholar] [CrossRef]
- Koj, A. The Acute-Phase Response to Injury and Infection. 1985. Available online: https://ci.nii.ac.jp/naid/10008639154/ (accessed on 22 July 2019).
- Gauldie, J.; Richards, C.; Harnish, D.; Lansdorp, P.; Baumann, H. Interferon β2/B-cell stimulatory factor type 2 shares identity with monocyte-derived hepatocyte-stimulating factor and regulates the major acute phase protein response in liver cells. Proc. Natl. Acad. Sci. USA 1987, 84, 7251–7255. [Google Scholar] [CrossRef]
- Hack, C.E.; De Groot, E.R.; Felt-Bersma, R.; Nuijens, J.H.; Van Schijndel, R.S.; Eerenberg-Belmer, A.; Thijs, L.G.; Aarden, L.A. Increased plasma levels of interleukin-6 in sepsis. Blood 1989, 74, 1704–1710. [Google Scholar] [CrossRef] [PubMed]
- Waage, A.; Brandtzaeg, P.; Halstensen, A.; Kierulf, P.; Espevik, T. The complex pattern of cytokines in serum from patients with meningococcal septic shock. Association between interleukin 6, interleukin 1, and fatal outcome. J. Exp. Med. 1989, 169, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Bauer, J.; Herrmann, F. Interleukin-6 in clinical medicine. Ann. Hematol. 1991, 62, 203–210. [Google Scholar] [CrossRef]
- Crowl, R.M.; Stoller, T.; Conroy, R.; Stoner, C. Induction of phospholipase A2 gene expression in human hepatoma cells by mediators of the acute phase response. J. Biol. Chem. 1991, 266, 2647–2651. [Google Scholar] [PubMed]
- Ganter, U.; Strauss, S.; Jonas, U.; Weidemann, A.; Beyreuther, K.; Volk, B.; Berger, M.; Bauer, J. Alpha 2-macroglobulin synthesis in interleukin-6-stimulated human neuronal SH-SY5Y neuroblastoma cells Potential significance for the processing of Alzheimer β-amyloid precursor protein. FEBS Lett. 1991, 282, 127–131. [Google Scholar] [CrossRef]
- Griffin, W.; Stanley, L.; Ling, C.; White, L.; MacLeod, V.; Perrot, L.; White, C.r.; Araoz, C. Brain interleukin 1 and S-100 immunoreactivity are elevated in Down syndrome and Alzheimer disease. Proc. Natl. Acad. Sci. USA 1989, 86, 7611–7615. [Google Scholar] [CrossRef] [PubMed]
- Vandenabeele, P.; Fiers, W. Is amyloidogenesis during Alzheimer’s disease due to an IL-1-/IL-6-mediated ‘acute phase response’ in the brain? Immunol. Today 1991, 12, 217–219. [Google Scholar] [CrossRef]
- Cojocaru, I.M.; Cojocaru, M.; Miu, G.; Sapira, V. Study of interleukin-6 production in Alzheimer’s disease. Rom. J. Intern. Med. 2011, 49, 55–58. [Google Scholar]
- Chavanet, P.; Bonnotte, B.; Guiguet, M.; Zeller, V.; Solary, E.; Maurice, L.; Casasnovas, O.; Caillot, D.; Waldner, A.; Kisterman, J.; et al. High concentrations of intrathecal interleukin-6 in human bacterial and nonbacterial meningitis. J. Infect. Dis. 1992, 166, 428–431. [Google Scholar] [CrossRef]
- Miyao, Y.; Yasue, H.; Ogawa, H.; Misumi, I.; Masuda, T.; Sakamoto, T.; Morita, E. Elevated plasma interleukin-6 levels in patients with acute myocardial infarction. Am. Heart J. 1993, 126, 1299–1304. [Google Scholar] [CrossRef]
- Jourdan, M.; Bataille, R.; Seguin, J.; Zhang, X.G.; Chaptal, P.A.; Klein, B. Constitutive production of interleukin-6 and immunologic features in cardiac myxomas. Arthritis Rheum. Off. J. Am. Coll. Rheumatol. 1990, 33, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Nachbaur, D.; Herold, M.; Maneschg, A.; Huber, H. Serum levels of interleukin-6 in multiple myeloma and other hematological disorders: Correlation with disease activity and other prognostic parameters. Ann. Hematol. 1991, 62, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Ndede, I.; Mining, S.K.; Patel, K.; Wanjala, F.M.; Chumba, D.; Tenge, C. Cytokines associated with Burkitt’s lymphoma in western Kenya. BMC Res. Notes 2017, 10, 519. [Google Scholar] [CrossRef] [PubMed]
- Tosato, G.; Jones, K.; Breinig, M.K.; Mcwilliams, H.P.; McKnight, J. Interleukin-6 production in posttransplant lymphoproliferative disease. J. Clin. Investig. 1993, 91, 2806–2814. [Google Scholar] [CrossRef]
- Iwase, S.; Murakami, T.; Saito, Y.; Nakagawa, K. Steep elevation of blood interleukin-6 (IL-6) associated only with late stages of cachexia in cancer patients. Eur. Cytokine Netw. 2004, 15, 312–316. [Google Scholar]
- Linker-Israeli, M.; Deans, R.; Wallace, D.; Prehn, J.; Ozeri-Chen, T.; Klinenberg, J. Elevated levels of endogenous IL-6 in systemic lupus erythematosus. A putative role in pathogenesis. J. Immunol. 1991, 147, 117–123. [Google Scholar]
- Grossman, R.M.; Krueger, J.; Yourish, D.; Granelli-Piperno, A.; Murphy, D.P.; May, L.T.; Kupper, T.S.; Sehgal, P.B.; Gottlieb, A.B. Interleukin 6 is expressed in high levels in psoriatic skin and stimulates proliferation of cultured human keratinocytes. Proc. Natl. Acad. Sci. USA 1989, 86, 6367–6371. [Google Scholar] [CrossRef]
- Wong, V.W.S.; Yu, J.; Cheng, A.S.L.; Wong, G.L.H.; Chan, H.Y.; Chu, E.S.H.; Ng, E.K.O.; Chan, F.K.L.; Sung, J.J.Y.; Chan, H.L.Y. High serum interleukin-6 level predicts future hepatocellular carcinoma development in patients with chronic hepatitis B. Int. J. Cancer 2009, 124, 2766–2770. [Google Scholar] [CrossRef]
- Ikebuchi, K.; Wong, G.G.; Clark, S.C.; Ihle, J.N.; Hirai, Y.; Ogawa, M. Interleukin 6 enhancement of interleukin 3-dependent proliferation of multipotential hemopoietic progenitors. Proc. Natl. Acad. Sci. USA 1987, 84, 9035–9039. [Google Scholar] [CrossRef]
- Okano, A.; Suzuki, C.; Takatsuki, F.; Akiyama, Y.; Koike, K.; Ozawa, K.; Hirano, T.; Kishimoto, T.; Nakahata, T.; Asano, S. In vitro expansion of the murine pluripotent hemopoietic stem cell population in response to interleukin 3 and interleukin 6. Application to bone marrow transplantation. Transplantation 1989, 48, 495–498. [Google Scholar] [CrossRef]
- Rennick, D.; Jackson, J.; Yang, G.; Wideman, J.; Lee, F.; Hudak, S. Interleukin-6 interacts with interleukin-4 and other hematopoietic growth factors to selectively enhance the growth of megakaryocytic, erythroid, myeloid, and multipotential progenitor cells. Blood 1989, 73, 1828–1835. [Google Scholar] [CrossRef] [PubMed]
- Ishibashi, T.; Kimura, H.; Uchida, T.; Kariyone, S.; Friese, P.; Burstein, S.A. Human interleukin 6 is a direct promoter of maturation of megakaryocytes in vitro. Proc. Natl. Acad. Sci. USA 1989, 86, 5953–5957. [Google Scholar] [CrossRef] [PubMed]
- Hill, R.; Warren, M.; Levin, J. Stimulation of thrombopoiesis in mice by human recombinant interleukin 6. J. Clin. Investig. 1990, 85, 1242–1247. [Google Scholar] [CrossRef] [PubMed]
- Navarro, S.; Debili, N.; Le Couedic, J.P.; Klein, B.; Breton-Gorius, J.; Doly, J.; Vainchenker, W. Interleukin-6 and its receptor are expressed by human megakaryocytes: In vitro effects on proliferation and endoreplication. Blood 1991, 77, 461–471. [Google Scholar] [CrossRef] [PubMed]
- Shabo, Y.; Lotem, J.; Sachs, L. Autoregulation of interleukin 6 and granulocyte-macrophage colony-stimulating factor in the differentiation of myeloid leukemic cells. Mol. Cell. Biol. 1989, 9, 4109–4112. [Google Scholar] [CrossRef] [PubMed]
- Van Damme, J.; Opdenakker, G.; Simpson, R.; Rubira, M.; Cayphas, S.; Vink, A.; Billiau, A.; Van Snick, J. Identification of the human 26-kDa protein, interferon beta 2 (IFN-beta 2), as a B cell hybridoma/plasmacytoma growth factor induced by interleukin 1 and tumor necrosis factor. J. Exp. Med. 1987, 165, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Kawano, M.; Hirano, T.; Matsuda, T.; Taga, T.; Horii, Y.; Iwato, K.; Asaoku, H.; Tang, B.; Tanabe, O.; Tanaka, H.; et al. Autocrine generation and requirement of BSF-2/IL-6 for human multiple myelomas. Nature 1988, 332, 83–85. [Google Scholar] [CrossRef]
- Nordan, R.; Pumphrey, J.; Rudikoff, S. Purification and NH2-terminal sequence of a plasmacytoma growth factor derived from the murine macrophage cell line P388D1. J. Immunol. 1987, 139, 813–817. [Google Scholar]
- Aarden, L.A.; De Groot, E.R.; Schaap, O.L.; Lansdorp, P.M. Production of hybridoma growth factor by human monocytes. Eur. J. Immunol. 1987, 17, 1411–1416. [Google Scholar] [CrossRef]
- Jernberg-Wiklund, H.; Pettersson, M.; Carlsson, M.; Nilsson, K. Increase in interleukin 6 (IL-6) and IL-6 receptor expression in a human multiple myeloma cell line U–266, during long-term in vitro culture and the development of a possible autocrine IL-6 loop. Leukemia 1992, 6, 310–318. [Google Scholar]
- Tosato, G.; Tanner, J.; Jones, K.; Revel, M.; Pike, S. Identification of interleukin-6 as an autocrine growth factor for Epstein-Barr virus-immortalized B cells. J. Virol. 1990, 64, 3033–3041. [Google Scholar] [CrossRef] [PubMed]
- Yokoi, T.; Miyawaki, T.; Yachie, A.; Kato, K.; Kasahara, Y.; Taniguchi, N. Epstein-Barr virus-immortalized B cells produce IL-6 as an autocrine growth factor. Immunology 1990, 70, 100–105. [Google Scholar] [PubMed]
- Yee, C.; Biondi, A.; Wang, X.; Iscove, N.N.; de Sousa, J.; Aarden, L.A.; Wong, G.G.; Clark, S.C.; Messner, H.A.; Minden, M.D. A possible autocrine role for interleukin-6 in two lymphoma cell lines. Blood 1989, 74, 798–804. [Google Scholar] [CrossRef] [PubMed]
- Swinnen, L.J.; Costanzo-Nordin, M.R.; Fisher, S.G.; O’Sullivan, E.J.; Johnson, M.R.; Heroux, A.L.; Dizikes, G.J.; Pifarre, R.; Fisher, R.I. Increased incidence of lymphoproliferative disorder after immunosuppression with the monoclonal antibody OKT3 in cardiac-transplant recipients. N. Engl. J. Med. 1990, 323, 1723–1728. [Google Scholar] [CrossRef] [PubMed]
- Abramowicz, D.; Schandené, L.; Goldman, M.; Crusiaux, A.; Vereerstraeten, P.; De, L.P.; Wybran, J.; Kinnaert, P.; Dupont, E.; Toussaint, C. Release of tumor necrosis factor, Interleukin-2, and gamma-interferon in serum after injection of OKT3 monoclonal antibody in kidney transplant recipients. Transplantation 1989, 47, 606–608. [Google Scholar] [CrossRef]
- Chatenoud, L.; Ferran, C.; Reuter, A.; Legendre, C.; Gevaert, Y.; Kreis, H.; Franchimont, P.; Bach, J. Systemic reaction to the anti-T-cell monoclonal antibody OKT3 in relation to serum levels of tumor necrosis factor and interferon-gamma [corrected]. N. Engl. J. Med. 1989, 320, 1420–1421. [Google Scholar]
- Hirohata, S.; Miyamoto, T. Elevated levels of interleukin-6 in cerebrospinal fluid from patients with systemic lupus erythematosus and central nervous system invol vement. Arthritis Rheum. 1990, 33, 644–649. [Google Scholar] [CrossRef]
- Kitani, A.; Hara, M.; Hirose, T.; Norioka, K.; Harigai, M.; Hirose, W.; Suzuki, K.; Kawakami, M.; Kawagoe, M.; Nakamura, H. Heterogeneity of B cell responsiveness to interleukin 4, interleukin 6 and low molecular weight B cell growth factor in discrete stages of B cell activation in patients with systemic lupus erythematosus. Clin. Exp. Immunol. 1989, 77, 31–36. [Google Scholar]
- Rumore, P.M.; Steinman, C.R. Endogenous circulating DNA in systemic lupus erythematosus. Occurrence as multimeric complexes bound to histone. J. Clin. Investig. 1990, 86, 69–74. [Google Scholar] [CrossRef]
- Hefeneider, S.H.; Cornell, K.A.; Brown, L.E.; Bakke, A.C.; McCoy, S.L.; Bennett, R.M. Nucleosomes and DNA bind to specific cell-surface molecules on murine cells and induce cytokine production. Clin. Immunol. Immunopathol. 1992, 63, 245–251. [Google Scholar] [CrossRef]
- Bataille, R.; Chappard, D.; Klein, B. The critical role of interleukin-6, interleukin-1B and macrophage colony-stimulating factor in the pathogenesis of bone lesions in multiple myeloma. Int. J. Clin. Lab. Res. 1992, 21, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Calderon, T.M.; Sherman, J.; Wilkerson, H.; Hatcher, V.B.; Berman, J.W. Interleukin 6 modulates c-sis gene expression in cultured human endothelial cells. Cell. Immunol. 1992, 143, 118–126. [Google Scholar] [CrossRef]
- Nabata, T.; Morimoto, S.; Koh, E.; Shiraishi, T.; Ogihara, T. Interleukin-6 stimulates c-myc expression and proliferation of cultured vascular smooth muscle cells. Biochem. Int. 1990, 20, 445–453. [Google Scholar] [PubMed]
- Finkel, M.S.; Oddis, C.V.; Jacob, T.D.; Watkins, S.C.; Hattler, B.G.; Simmons, R.L. Negative inotropic effects of cytokines on the heart mediated by nitric oxide. Science 1992, 257, 387–389. [Google Scholar] [CrossRef] [PubMed]
- Entman, M.L.; Michael, L.; Rossen, R.D.; Dreyer, W.; Anderson, D.C.; Taylor, A.; Smith, C.W. Inflammation in the course of early myocardial ischemia. FASEB J. 1991, 5, 2529–2537. [Google Scholar] [CrossRef]
- Ikeda, U.; Ohkawa, F.; Seino, Y.; Yamamoto, K.; Hidaka, Y.; Kasahara, T.; Kawai, T.; Shimada, K. Serum interleukin 6 levels become elevated in acute myocardial infarction. J. Mol. Cell. Cardiol. 1992, 24, 579–584. [Google Scholar] [CrossRef]
- Fleming, I.; Gray, G.A.; Julou-Schaeffer, G.; Parratt, J.R.; Stoclet, J.C. Incubation with endotoxin activates the L-arginine pathway in vascular tissue. Biochem. Biophys. Res. Commun. 1990, 171, 562–568. [Google Scholar] [CrossRef]
- Westenberger, U.; Thanner, S.; Ruf, H.H.; Gersonde, K.; Sutter, G.; Trentz, O. Formation of free radicals and nitric oxide derivative of hemoglobin in rats during shock syndrome. Free Radic. Res. Commun. 1990, 11, 167–178. [Google Scholar] [CrossRef]
- Hirano, T.; Taga, T.; Yasukawa, K.; Nakajima, K.; Nakano, N.; Takatsuki, F.; Shimizu, M.; Murashima, A.; Tsunasawa, S.; Sakiyama, F. Human B-cell differentiation factor defined by an anti-peptide antibody and its possible role in autoantibody production. Proc. Natl. Acad. Sci. USA 1987, 84, 228–231. [Google Scholar] [CrossRef]
- Löwik, C.; Van der Pluijm, G.; Bloys, H.; Hoekman, K.; Bijvoet, O.; Aarden, L.; Papapoulos, S. Parathyroid hormone (PTH) and (PTH)-like protein (PLP) stimulate interleukin-6 production by osteogenic cells: A possible role of interleukin-6 in osteoclastogenesis. Biochem. Biophys. Res. Commun. 1989, 162, 1546–1552. [Google Scholar] [CrossRef]
- Ishimi, Y.; Miyaura, C.; Jin, C.H.; Akatsu, T.; Abe, E.; Nakamura, Y.; Yamaguchi, A.; Yoshiki, S.; Matsuda, T.; Hirano, T. IL-6 is produced by osteoblasts and induces bone resorption. J. Immunol. 1990, 145, 3297–3303. [Google Scholar] [PubMed]
- Feyen, J.H.; di Padova, F.E.; Trechsel, U.; Elford, P. Interleukin-6 is produced by bone and modulated by parathyroid hormone. J. Bone Miner. Res. 1989, 4, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Girasole, G.; Jilka, R.L.; Passeri, G.; Boswell, S.; Boder, G.; Williams, D.C.; Manolagas, S.C. 17 β-estradiol inhibits interleukin-6 production by bone marrow-derived stromal cells and osteoblasts in vitro: A potential mechanism for the antiosteoporotic effect of estrogens. J. Clin. Investig. 1992, 89, 883–891. [Google Scholar] [CrossRef] [PubMed]
- Jilka, R.L.; Hangoc, G.; Girasole, G.; Passeri, G.; Williams, D.C.; Abrams, J.S.; Boyce, B.; Broxmeyer, H.; Manolagas, S.C. Increased osteoclast development after estrogen loss: Mediation by interleukin-6. Science 1992, 257, 88–91. [Google Scholar] [CrossRef]
- Hirano, T.; Matsuda, T.; Turner, M.; Miyasaka, N.; Buchan, G.; Tang, B.; Sato, K.; Shimi, M.; Maid, R.; Feldmann, M.; et al. Excessive production of interleukin 6/B cell stimulatory factor-2 in rheumatoid arthritis. Eur. J. Immunol. 1988, 18, 1797–1802. [Google Scholar] [CrossRef]
- Houssiau, F.A.; Devogelaer, J.P.; Van Damme, J.; De Deuxchaisnes, C.N.; Van Snick, J. Interleukin-6 in synovial fluid and serum of patients with rheumatoid arthritis and other inflammatory arthritides. Arthritis Rheum. 1988, 31, 784–788. [Google Scholar] [CrossRef]
- Bhardwaj, N.; Santhanam, U.; Lau, L.; Tatter, S.; Ghrayeb, J.; Rivelis, M.; Steinman, R.; Sehgal, P.; May, L. IL-6/IFNβ-2 in synovial effusions of patients with rheumatoid arthritis and other arthritides. Identification of several isoforms and studies of cellular sources. J. Immunol. 1989, 143, 2153–2159. [Google Scholar]
- Hermann, E.; Fleischer, B.; Mayet, W.; Poralla, T. Correlation of synovial fluid interleukin 6 (IL-6) activities with IgG concentrations in patients with inflammatory joint disease and osteoarthritis. Clin. Exp. Rheumatol. 1989, 7, 411–414. [Google Scholar]
- Firestein, G.; Alvaro-Gracia, J.; Maki, R.; Alvaro-Garcia, J. Quantitative analysis of cytokine gene expression in rheumatoid arthritis. J. Immunol. 1990, 144, 3347–3353. [Google Scholar]
- Neurath, A.R.; Strick, N.; Sproul, P. Search for hepatitis B virus cell receptors reveals binding sites for interleukin 6 on the virus envelope protein. J. Exp. Med. 1992, 175, 461–469. [Google Scholar] [CrossRef]
- Horii, Y.; Muraguchi, A.; Iwano, M.; Matsuda, T.; Hirayama, T.; Yamada, H.; Fujii, Y.; Dohi, K.; Ishikawa, H.; Ohmoto, Y. Involvement of IL-6 in mesangial proliferative glomerulonephritis. J. Immunol. 1989, 143, 3949–3955. [Google Scholar] [PubMed]
- Ruef, C.; Budde, K.; Lacy, J.; Northemann, W.; Baumann, M.; Sterzel, R.B.; Coleman, D.L. Interleukin 6 is an autocrine growth factor for mesangial cells. Kidney Int. 1990, 38, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Neuner, P.; Urbanski, A.; Trautinger, F.; Möller, A.; Kirnbauer, R.; Kapp, A.; Schöpf, E.; Schwarz, T.; Luger, T.A. Increased IL-6 production by monocytes and keratinocytes in patients with psoriasis. J. Investig. Dermatol. 1991, 97, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Tracey, K.; Wei, H.; Manogue, K.R.; Fong, Y.; Hesse, D.G.; Nguyen, H.T.; Kuo, G.C.; Beutler, B.; Cotran, R.; Cerami, A. Cachectin/tumor necrosis factor induces cachexia, anemia, and inflammation. J. Exp. Med. 1988, 167, 1211–1227. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, A.S.; Nordan, R.P.; McIntosh, J.; Calvo, J.C.; Scow, R.O.; Jablons, D. Interleukin 6 reduces lipoprotein lipase activity in adipose tissue of mice in vivo and in 3T3-L1 adipocytes: A possible role for interleukin 6 in cancer cachexia. Cancer Res. 1992, 52, 4113–4116. [Google Scholar] [PubMed]
- Feingold, K.R.; Grunfeld, C. Role of cytokines in inducing hyperlipidemia. Diabetes 1992, 41, 97–101. [Google Scholar] [CrossRef]
- Russell, C.; Ward, A.C.; Vezza, V.; Hoskisson, P.; Alcorn, D.; Steenson, D.P.; Corrigan, D.K. Development of a needle shaped microelectrode for electrochemical detection of the sepsis biomarker interleukin-6 (IL-6) in real time. Biosens. Bioelectron. 2019, 126, 806–814. [Google Scholar] [CrossRef]
- Tertiş, M.; Ciui, B.; Suciu, M.; Săndulescu, R.; Cristea, C. Label-free electrochemical aptasensor based on gold and polypyrrole nanoparticles for interleukin 6 detection. Electrochim. Acta 2017, 258, 1208–1218. [Google Scholar] [CrossRef]
- Chen, H.; Choo, T.K.; Huang, J.; Wang, Y.; Liu, Y.; Platt, M.; Palaniappan, A.; Liedberg, B.; Tok, A.I.Y. Label-free electronic detection of interleukin-6 using horizontally aligned carbon nanotubes. Mater. Des. 2016, 90, 852–857. [Google Scholar] [CrossRef]
- Yang, T.; Wang, S.; Jin, H.; Bao, W.; Huang, S.; Wang, J. An electrochemical impedance sensor for the label-free ultrasensitive detection of interleukin-6 antigen. Sens. Actuators B Chem. 2013, 178, 310–315. [Google Scholar] [CrossRef]
- Lou, Y.; He, T.; Jiang, F.; Shi, J.J.; Zhu, J.J. A competitive electrochemical immunosensor for the detection of human interleukin-6 based on the electrically heated carbon electrode and silver nanoparticles functionalized labels. Talanta 2014, 122, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.; Feng, L.N.; Ren, Z.J.; Jiang, L.P.; Zhu, J.J. Synthesis of Silver Nanoparticle–Hollow Titanium Phosphate Sphere Hybrid as a Label for Ultrasensitive Electrochemical Detection of Human Interleukin-6. Small 2011, 7, 2921–2928. [Google Scholar] [CrossRef] [PubMed]
- Deng, C.; Qu, F.; Sun, H.; Yang, M. Sensitive electrochemical immunosensor based on enlarged and surface charged gold nanoparticles mediated electron transfer. Sens. Actuators B Chem. 2011, 160, 471–474. [Google Scholar] [CrossRef]
- Li, T.; Yang, M. Electrochemical sensor utilizing ferrocene loaded porous polyelectrolyte nanoparticles as label for the detection of protein biomarker IL-6. Sens. Actuators B Chem. 2011, 158, 361–365. [Google Scholar] [CrossRef]
- Malhotra, R.; Patel, V.; Vaqué, J.P.; Gutkind, J.S.; Rusling, J.F. Ultrasensitive electrochemical immunosensor for oral cancer biomarker IL-6 using carbon nanotube forest electrodes and multilabel amplification. Anal. Chem. 2010, 82, 3118–3123. [Google Scholar] [CrossRef]
- Wang, G.; Huang, H.; Zhang, G.; Zhang, X.; Fang, B.; Wang, L. Dual amplification strategy for the fabrication of highly sensitive interleukin-6 amperometric immunosensor based on poly-dopamine. Langmuir 2010, 27, 1224–1231. [Google Scholar] [CrossRef]
- Wang, G.; Huang, H.; Wang, B.; Zhang, X.; Wang, L. A supersandwich multienzyme–DNA label based electrochemical immunosensor. Chem. Commun. 2011, 48, 720–722. [Google Scholar] [CrossRef]
- Khosravi, F.; Loeian, S.; Panchapakesan, B. Ultrasensitive label-free sensing of IL-6 based on PASE functionalized carbon nanotube micro-arrays with RNA-aptamers as molecular recognition elements. Biosensors 2017, 7, 17. [Google Scholar] [CrossRef]
- Shoorideh, K.; Chui, C.O. On the origin of enhanced sensitivity in nanoscale FET-based biosensors. Proc. Natl. Acad. Sci. USA 2014, 111, 5111–5116. [Google Scholar] [CrossRef]
- Schasfoort, R.B.; Bergveld, P.; Kooyman, R.; Greve, J. Possibilities and limitations of direct detection of protein charges by means of an immunological field-effect transistor. Anal. Chim. Acta 1990, 238, 323–329. [Google Scholar] [CrossRef]
- Huang, W.; Diallo, A.K.; Dailey, J.L.; Besar, K.; Katz, H.E. Electrochemical processes and mechanistic aspects of field-effect sensors for biomolecules. J. Mater. Chem. C 2015, 3, 6445–6470. [Google Scholar] [CrossRef]
- Israelachvili, J.N. Intermolecular and Surface Forces; Academic Press: Cambridge, MA, USA, 2011. [Google Scholar]
- Sørensen, M.H.; Mortensen, N.A.; Brandbyge, M. Screening model for nanowire surface-charge sensors in liquid. Appl. Phys. Lett. 2007, 91, 102105. [Google Scholar] [CrossRef]
- Wang, H.; Pilon, L. Accurate simulations of electric double layer capacitance of ultramicroelectrodes. J. Phys. Chem. C 2011, 115, 16711–16719. [Google Scholar] [CrossRef]
- Dickinson, E.J.; Compton, R.G. Diffuse double layer at nanoelectrodes. J. Phys. Chem. C 2009, 113, 17585–17589. [Google Scholar] [CrossRef]
- Zhang, A.; Lieber, C.M. Nano-bioelectronics. Chem. Rev. 2015, 116, 215–257. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Majumdar, H.S.; Kaisti, M.; Prabhu, A.; Ivaska, A.; Österbacka, R.; Rahman, A.; Levon, K. Surface functionalization of ion-sensitive floating-gate field-effect transistors with organic electronics. IEEE Trans. Electron Devices 2015, 62, 1291–1298. [Google Scholar] [CrossRef]
- Maddalena, F.; Spijkman, M.; Brondijk, J.; Fonteijn, P.; Brouwer, F.; Hummelen, J.; De Leeuw, D.; Blom, P.; De Boer, B. Device characteristics of polymer dual-gate field-effect transistors. Org. Electron. 2008, 9, 839–846. [Google Scholar] [CrossRef]
- Gao, N.; Zhou, W.; Jiang, X.; Hong, G.; Fu, T.M.; Lieber, C.M. General strategy for biodetection in high ionic strength solutions using transistor-based nanoelectronic sensors. Nano Lett. 2015, 15, 2143–2148. [Google Scholar] [CrossRef]
- Kaisti, M. Detection principles of biological and chemical FET sensors. Biosens. Bioelectron. 2017, 98, 437–448. [Google Scholar] [CrossRef]
- Sosna, M.; Denuault, G.; Pascal, R.W.; Prien, R.D.; Mowlem, M. Development of a reliable microelectrode dissolved oxygen sensor. Sens. Actuators B Chem. 2007, 123, 344–351. [Google Scholar] [CrossRef]
- Blair, E.O.; Corrigan, D.K.; Terry, J.G.; Mount, A.R.; Walton, A.J. Development and optimization of durable microelectrodes for quantitative electroanalysis in molten salt. J. Microelectromech. Syst. 2015, 24, 1346–1354. [Google Scholar] [CrossRef]
- Corrigan, D.; Vezza, V.; Schulze, H.; Bachmann, T.; Mount, A.; Walton, A.; Terry, J. A microelectrode array with reproducible performance shows loss of consistency following functionalization with a self-assembled 6-mercapto-1-hexanol layer. Sensors 2018, 18, 1891. [Google Scholar] [CrossRef] [PubMed]
- Li, P.Q.; Piper, A.; Schmueser, I.; Mount, A.R.; Corrigan, D.K. Impedimetric measurement of DNA–DNA hybridisation using microelectrodes with different radii for detection of methicillin resistant Staphylococcus aureus (MRS/A). Analyst 2017, 142, 1946–1952. [Google Scholar] [CrossRef] [PubMed]
- Lisdat, F.; Schäfer, D. The use of electrochemical impedance spectroscopy for biosensing. Anal. Bioanal. Chem. 2008, 391, 1555–1567. [Google Scholar] [CrossRef]
- Ciani, I.; Schulze, H.; Corrigan, D.K.; Henihan, G.; Giraud, G.; Terry, J.G.; Walton, A.J.; Pethig, R.; Ghazal, P.; Crain, J.; et al. Development of immunosensors for direct detection of three wound infection biomarkers at point of care using electrochemical impedance spectroscopy. Biosens. Bioelectron. 2012, 31, 413–418. [Google Scholar] [CrossRef]
- Eissa, S.; Zourob, M. A graphene-based electrochemical competitive immunosensor for the sensitive detection of okadaic acid in shellfish. Nanoscale 2012, 4, 7593–7599. [Google Scholar] [CrossRef]
- Moschou, D.; Greathead, L.; Pantelidis, P.; Kelleher, P.; Morgan, H.; Prodromakis, T. Amperometric IFN-γ immunosensors with commercially fabricated PCB sensing electrodes. Biosens. Bioelectron. 2016, 86, 805–810. [Google Scholar] [CrossRef]
- Ianeselli, L.; Grenci, G.; Callegari, C.; Tormen, M.; Casalis, L. Development of stable and reproducible biosensors based on electrochemical impedance spectroscopy: Three-electrode versus two-electrode setup. Biosens. Bioelectron. 2014, 55, 1–6. [Google Scholar] [CrossRef]
- Molazemhosseini, A.; Magagnin, L.; Vena, P.; Liu, C.C. Single-use disposable electrochemical label-free immunosensor for detection of glycated hemoglobin (HbA1c) using differential pulse voltammetry (DPV). Sensors 2016, 16, 1024. [Google Scholar] [CrossRef]
- Yi, Q.; Liu, Q.; Gao, F.; Chen, Q.; Wang, G. Application of an electrochemical immunosensor with a MWCNT/PDAA modified electrode for detection of serum trypsin. Sensors 2014, 14, 10203–10212. [Google Scholar] [CrossRef]
- Kemmler, M.; Sauer, U.; Schleicher, E.; Preininger, C.; Brandenburg, A. Biochip point-of-care device for sepsis diagnostics. Sens. Actuators B Chem. 2014, 192, 205–215. [Google Scholar] [CrossRef]
- Wang, G.L.; Yu, P.P.; Xu, J.J.; Chen, H.Y. A label-free photoelectrochemical immunosensor based on water-soluble CdS quantum dots. J. Phys. Chem. C 2009, 113, 11142–11148. [Google Scholar] [CrossRef]
- Peng, J.; Guan, J.; Yao, H.; Jin, X. Magnetic colorimetric immunoassay for human interleukin-6 based on the oxidase activity of ceria spheres. Anal. Biochem. 2016, 492, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Fan, G.C.; Ren, X.L.; Zhu, C.; Zhang, J.R.; Zhu, J.J. A new signal amplification strategy of photoelectrochemical immunoassay for highly sensitive interleukin-6 detection based on TiO2/CdS/CdSe dual co-sensitized structure. Biosens. Bioelectron. 2014, 59, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Liu, G.; Goldys, E.M. Robust immunosensing system based on biotin-streptavidin coupling for spatially localized femtogram/ mL−1 level detection of interleukin-6. Biosens. Bioelectron. 2018, 102, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Toma, M.; Tawa, K. Polydopamine thin films as protein linker layer for sensitive detection of interleukin-6 by surface plasmon enhanced fluorescence spectroscopy. ACS Appl. Mater. Interfaces 2016, 8, 22032–22038. [Google Scholar] [CrossRef] [PubMed]
- Xiong, W.W.; Yang, G.H.; Wu, X.C.; Zhu, J.J. Aqueous synthesis of color-tunable CuInS2/ZnS nanocrystals for the detection of human interleukin 6. ACS Appl. Mater. Interfaces 2013, 5, 8210–8216. [Google Scholar] [CrossRef]
- Kapoor, R.; Wang, C.W. Highly specific detection of interleukin-6 (IL-6) protein using combination tapered fiber-optic biosensor dip-probe. Biosens. Bioelectron. 2009, 24, 2696–2701. [Google Scholar] [CrossRef]
- Buchegger, P.; Sauer, U.; Toth-Székély, H.; Preininger, C. Miniaturized protein microarray with internal calibration as point-of-care device for diagnosis of neonatal sepsis. Sensors 2012, 12, 1494–1508. [Google Scholar] [CrossRef] [PubMed]
- Liang, K.Z.; Qi, J.S.; Mu, W.J.; Chen, Z.G. Biomolecules/gold nanowires-doped sol–gel film for label-free electrochemical immunoassay of testosterone. J. Biochem. Biophys. Methods 2008, 70, 1156–1162. [Google Scholar] [CrossRef]
- Wood, J.B.; Szyndler, M.W.; Halpern, A.R.; Cho, K.; Corn, R.M. Fabrication of DNA microarrays on polydopamine-modified gold thin films for SPR imaging measurements. Langmuir 2013, 29, 10868–10873. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Wang, L.; Su, R.; Liu, B.; Huang, R.; Qi, W.; He, Z. A polydopamine-modified optical fiber SPR biosensor using electroless-plated gold films for immunoassays. Biosens. Bioelectron. 2015, 74, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Lynge, M.E.; van der Westen, R.; Postma, A.; Städler, B. Polydopamine: A nature-inspired polymer coating for biomedical science. Nanoscale 2011, 3, 4916–4928. [Google Scholar] [CrossRef] [PubMed]
- Loget, G.; Wood, J.B.; Cho, K.; Halpern, A.R.; Corn, R.M. Electrodeposition of polydopamine thin films for DNA patterning and microarrays. Anal. Chem. 2013, 85, 9991–9995. [Google Scholar] [CrossRef] [PubMed]
- Green, N.M. Avidin. In Advances in Protein Chemistry; Elsevier: Amsterdam, The Netherlands, 1975; Volume 29, pp. 85–133. [Google Scholar]
- Holmberg, A.; Blomstergren, A.; Nord, O.; Lukacs, M.; Lundeberg, J.; Uhlén, M. The biotin-streptavidin interaction can be reversibly broken using water at elevated temperatures. Electrophoresis 2005, 26, 501–510. [Google Scholar] [CrossRef] [PubMed]
- Schetters, H. Avidin and streptavidin in clinical diagnostics. Biomol. Eng. 1999, 16, 73–78. [Google Scholar] [CrossRef]
- Diamandis, E.P.; Christopoulos, T.K. The biotin-(strept) avidin system: Principles and applications in biotechnology. Clin. Chem. 1991, 37, 625–636. [Google Scholar] [CrossRef] [PubMed]
- Dundas, C.M.; Demonte, D.; Park, S. Streptavidin–biotin technology: Improvements and innovations in chemical and biological applications. Appl. Microbiol. Biotechnol. 2013, 97, 9343–9353. [Google Scholar] [CrossRef]
- Guzman, J.; Carrettin, S.; Corma, A. Spectroscopic evidence for the supply of reactive oxygen during CO oxidation catalyzed by gold supported on nanocrystalline CeO2. J. Am. Chem. Soc. 2005, 127, 3286–3287. [Google Scholar] [CrossRef]
- Asati, A.; Santra, S.; Kaittanis, C.; Nath, S.; Perez, J.M. Oxidase-like activity of polymer-coated cerium oxide nanoparticles. Angew. Chem. Int. Ed. 2009, 48, 2308–2312. [Google Scholar] [CrossRef]
- Karakoti, A.; Singh, S.; Dowding, J.M.; Seal, S.; Self, W.T. Redox-active radical scavenging nanomaterials. Chem. Soc. Rev. 2010, 39, 4422–4432. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, V.K.; Shcherbakov, A.; Usatenko, A. Structure-sensitive properties and biomedical applications of nanodispersed cerium dioxide. Russ. Chem. Rev. 2009, 78, 855. [Google Scholar] [CrossRef]
- Celardo, I.; Pedersen, J.Z.; Traversa, E.; Ghibelli, L. Pharmacological potential of cerium oxide nanoparticles. Nanoscale 2011, 3, 1411–1420. [Google Scholar] [CrossRef] [PubMed]
- Asati, A.; Kaittanis, C.; Santra, S.; Perez, J.M. pH-tunable oxidase-like activity of cerium oxide nanoparticles achieving sensitive fluorigenic detection of cancer biomarkers at neutral pH. Anal. Chem. 2011, 83, 2547–2553. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.; Xiao, J.; Chen, B.; Li, Y. Catalytically stable and active CeO2 mesoporous spheres. Inorg. Chem. 2010, 49, 8188–8190. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Xu, B.; Fu, T.; Cai, M.; Li, F.; Zhang, Y.; Wang, Q. Near-infrared photoluminescent Ag2S quantum dots from a single source precursor. J. Am. Chem. Soc. 2010, 132, 1470–1471. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.P.; Cui, R.; Zhang, Z.L.; Xie, Z.X.; Pang, D.W. Ultrasmall near-infrared Ag2Se quantum dots with tunable fluorescence for in vivo imaging. J. Am. Chem. Soc. 2011, 134, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.S.; Liu, W.; Misra, P.; Tanaka, E.; Zimmer, J.P.; Ipe, B.I.; Bawendi, M.G.; Frangioni, J.V. Renal clearance of quantum dots. Nat. Biotechnol. 2007, 25, 1165. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.A.; Mandal, G.; Darragh, M.; Heyes, C.D. Cadmium-free quantum dots as time-gated bioimaging probes in highly-autofluorescent human breast cancer cells. Chem. Commun. 2013, 49, 624–626. [Google Scholar]
- Xie, R.; Rutherford, M.; Peng, X. Formation of high-quality I- III- VI semiconductor nanocrystals by tuning relative reactivity of cationic precursors. J. Am. Chem. Soc. 2009, 131, 5691–5697. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Kim, S.W. CuInS2/ZnS core/shell quantum dots by cation exchange and their blue-shifted photoluminescence. J. Mater. Chem. 2011, 21, 3745–3750. [Google Scholar] [CrossRef]
- Park, N.; van de Lagemaat, J.; Frank, A.J. Comparison of dye-sensitized rutile-and anatase-based TiO2 solar cells. J. Phys. Chem. B 2000, 104, 8989–8994. [Google Scholar] [CrossRef]
- Kuang, D.; Ito, S.; Wenger, B.; Klein, C.; Moser, J.E.; Humphry-Baker, R.; Zakeeruddin, S.M.; Grätzel, M. High molar extinction coefficient heteroleptic ruthenium complexes for thin film dye-sensitized solar cells. J. Am. Chem. Soc. 2006, 128, 4146–4154. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.L.; Lo, Y.S. Highly efficient quantum-dot-sensitized solar cell based on co-sensitization of CdS/CdSe. Adv. Funct. Mater. 2009, 19, 604–609. [Google Scholar] [CrossRef]
- Bauch, M.; Toma, K.; Toma, M.; Zhang, Q.; Dostalek, J. Plasmon-enhanced fluorescence biosensors: A review. Plasmonics 2014, 9, 781–799. [Google Scholar] [CrossRef] [PubMed]
- Cao, S.H.; Cai, W.P.; Liu, Q.; Li, Y.Q. Surface plasmon–coupled emission: What can directional fluorescence bring to the analytical sciences? Annu. Rev. Anal. Chem. 2012, 5, 317–336. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Brunsen, A.; Jonas, U.; Dostalek, J.; Knoll, W. Prostate specific antigen biosensor based on long range surface plasmon-enhanced fluorescence spectroscopy and dextran hydrogel binding matrix. Anal. Chem. 2009, 81, 9625–9632. [Google Scholar] [CrossRef]
- Liebermann, T.; Knoll, W. Surface-plasmon field-enhanced fluorescence spectroscopy. Colloids Surf. A Physicochem. Eng. Asp. 2000, 171, 115–130. [Google Scholar] [CrossRef]
- Rissin, D.M.; Kan, C.W.; Campbell, T.G.; Howes, S.C.; Fournier, D.R.; Song, L.; Piech, T.; Patel, P.P.; Chang, L.; Rivnak, A.J.; et al. Single-molecule enzyme-linked immunosorbent assay detects serum proteins at subfemtomolar concentrations. Nat. Biotechnol. 2010, 28, 595–599. [Google Scholar] [CrossRef]
- Song, L.; Hanlon, D.W.; Chang, L.; Provuncher, G.K.; Kan, C.W.; Campbell, T.G.; Fournier, D.R.; Ferrell, E.P.; Rivnak, A.J.; Pink, B.A.; et al. Single molecule measurements of tumor necrosis factor α and interleukin-6 in the plasma of patients with Crohn’s disease. J. Immunol. Methods 2011, 372, 177–186. [Google Scholar] [CrossRef]
- Kapoor, R.; Kaur, N.; Nishanth, E.T.; Halvorsen, S.W.; Bergey, E.J.; Prasad, P.N. Detection of trophic factor activated signaling molecules in cells by a compact fiber-optic sensor. Biosens. Bioelectron. 2004, 20, 345–349. [Google Scholar] [CrossRef] [PubMed]
| Disease | Interleukin 6 Level (pg/mL) | Reference |
|---|---|---|
| Alzheimer’s Disease | 85–567 | [41] |
| Meningitis | 450–32,000 | [42] |
| Myocardial Infarction | 28.5–46.5 | [43] |
| Cardiac Myxoma | greater than 56 | [44] |
| Multiple Myeloma | 5–33 | [45] |
| Burkitt Lymphoma | 100.3 | [46] |
| Post-Transplant Lymphoproliferative Disease/PTLD | 143–11,020 | [47] |
| Cachexia | 100 | [48] |
| Rheumatoid Arthritis | 17 | [49] |
| Psoriasis | 30,000 | [50] |
| Hepatitis B Virus Infection/Hepatocyte Carcinoma | 7–18.9 | [51] |
| Sepsis | 5000–100,000 | [36] |
| Detection Method | Technique | Receptor | Analyte & Conjugate | Signal Type | LOD † | Dynamic Range † | Ref |
|---|---|---|---|---|---|---|---|
| Direct ECIA | CV, EIS, DPV | Anti-IL-6/Gold ME | IL-6 | R and Current | 20 | 20–100 | [100] |
| Direct EC aptasensor assay | CV, EIS | PPyNS/AuNP/IL-6-Aptamer | IL-6 | R | 0.33 | 1–15,000,000 | [101] |
| Direct EC aptasensor | FET | CNT/PASE/IL-6-Aptamer | IL-6 | Drain Current | 1 | 1–100 | [111] |
| Direct ECIA | LGFET | CNTFET/Anti IL-6 | IL-6 | Drain Current | 1.37 | 1–100 | [102] |
| Indirect competitive ECIA | EIS, LSV | ERGO/AuPdNP/Anti IL-6 | PS/PDA/AgNP/IL-6 | R and Current | 0.059 | 0.1–100,000 | [104] |
| Direct ECIA | EIS | CNT/AuNP/Anti IL-6 | IL-6 | R t | 0.00001 | 0.00001–0.1 | [103] |
| Sandwich ECIA/NP | CV, DPV | SPION/Ab | TiP/AgNP/ Ab/IL-6 | Current | 0.1 | 0.00001–10,000 | [105] |
| Sandwich ECIA/NP | CV, SWV | GC/GO/Ab | FC/PPN/ Ab/IL-6 | Current | 1 | 2–20,000 | [107] |
| Sandwich ECIA/NP | CV,(SWV) | 11-MUA/Ab | CTAB(AuNP)/ Ab/IL-6 | Current | 2 | 5–50,000 | [106] |
| Sandwich ELECIA | Amperometry | GCE/MWCNT/Ab | S1-Avidin/Biotin-Ab S2-HRP-S3(TargetDNA) | Current | 0.05 | 0.2–20 | [110] |
| Sandwich ELECIA | EIS, Amperometry | ITO/PDA/AuNPs/Ab | CNT/PDA/AuNP/ Ab-HRP-IL-6 | Current | 1 | 4–800 | [109] |
| Sandwich ELECIA | Rotating Disc Amperometry | SWNTForest/Ab | Ab-Biotin/(m)HRP-Streptavidin/(h) Ab-MWNT-HRP | Current/Absorbance | 0.5 | 0.5–30 | [108] |
| Detection Method | Technique | Receptor | Conjugate | Signal Type | LOD † | Dynamic Range † | Ref |
|---|---|---|---|---|---|---|---|
| FIA ⋄ | Fluorescent Imaging | OpticFiber/Streptavidin-Biotin/Ab | Ab/FMNPs | Fluorescence | 0.1 | 0.4–400 | [139] |
| FIA ⋄ | SPFS | Glass/AuNP/PDOPA/Ab | Ab/AlexaFluor647 | Fluorescence | 2 | 2–2372 | [140] |
| FIA ⋄ | FIA | Ab/IL-6 | Dy647/Streptavidin/MNP/Biotin-Ab2 | Fluorescence | 20 | 1.1–1000 | [143] |
| CLIA ▽ | UV-Vis Spectroscopy | Ab1/Fe3O4MNP | Ab2/CeO2NP | Absorbance | 0.04 | 0.1–10,000 | [137] |
| Indirect Competitive PECIA ‡ | EIS, Amperometry | Ab1/CS/CdS//TiO2/ITO | IL-6/CdSe | R & I | 0.38 | 1–100,000 | [138] |
| PLIA ☆ | Photoluminescence | PDA/PDMS/AuNP/Ab | Ab2/CuInS2/ZnSNCs | Fluorescence | 0.02 | 20–20,000 | [141] |
| CTOB ∓ | FIA | CTOB/APTS/Sulfo-SMCC/Ab | Alex488/Ab/ and IL-6 | Fluorescence | 120 | 118–11,859 | [176] |
| SiMoA ♣ | Digital ELISA | Micro Magnetic Bead/Ab/IL-6 | Biotin-Ab/SG δ | Fluorescence | 0.006 | 0.006–250 | [175]. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, M.A.; Mujahid, M. Recent Advances in Electrochemical and Optical Biosensors Designed for Detection of Interleukin 6. Sensors 2020, 20, 646. https://doi.org/10.3390/s20030646
Khan MA, Mujahid M. Recent Advances in Electrochemical and Optical Biosensors Designed for Detection of Interleukin 6. Sensors. 2020; 20(3):646. https://doi.org/10.3390/s20030646
Chicago/Turabian StyleKhan, Munezza Ata, and Mohammad Mujahid. 2020. "Recent Advances in Electrochemical and Optical Biosensors Designed for Detection of Interleukin 6" Sensors 20, no. 3: 646. https://doi.org/10.3390/s20030646
APA StyleKhan, M. A., & Mujahid, M. (2020). Recent Advances in Electrochemical and Optical Biosensors Designed for Detection of Interleukin 6. Sensors, 20(3), 646. https://doi.org/10.3390/s20030646





