It May Be Possible to Prevent both Early and Late Relapses in Breast Cancer; Perhaps This Is an Opportunity for Sensors or Biosensors to Help
Conflicts of Interest
References
- Retsky, M.; Demicheli, R.; Hrushesky, W.; James, T.; Rogers, R.; Baum, M.; Vaidya, J.S.; Erhabor, O.; Forget, P. Breast cancer and the black swan. Ecancermedicalscience 2020, 14. [Google Scholar] [CrossRef]
- Is this One Dollar Pill a Breast Cancer Breakthrough? Available online: https://www.mossreports.com/breast-cancer-pill-ketorolac/ (accessed on 10 December 2020).
- Forget, P.; Vandenhende, J.; Berliere, M.; Machiels, J.-P.; Nussbaum, B.; Legrand, C.; De Kock, M. Do Intraoperative Analgesics Influence Breast Cancer Recurrence After Mastectomy? A Retrospective Analysis. Anesthesia Analg. 2010, 110, 1630–1635. [Google Scholar] [CrossRef]
- Desmedt, C.; Demicheli, R.; Fornili, M.; Bachir, I.; Duca, M.; Viglietti, G.; Berlière, M.; Piccart, M.; Sotiriou, C.; Sosnowski, M.; et al. Potential Benefit of Intra-operative Administration of Ketorolac on Breast Cancer Recurrence According to the Patient’s Body Mass Index. J. Natl. Cancer Inst. 2018, 110, 1115–1122. [Google Scholar] [CrossRef] [PubMed]
- Krall, J.A.; Reinhardt, F.; Mercury, O.A.; Pattabiraman, D.R.; Brooks, M.W.; Dougan, M.; Lambert, A.W.; Bierie, B.; Ploegh, H.L.; Dougan, S.K.; et al. The systemic response to surgery triggers the outgrowth of distant immune-controlled tumors in mouse models of dormancy. Sci. Transl. Med. 2018, 10, 3464. [Google Scholar] [CrossRef] [PubMed]
- Panigrahy, D.; Gartung, A.; Yang, J.; Yang, H.; Gilligan, M.M.; Sulciner, M.L.; Bhasin, S.S.; Bielenberg, D.R.; Chang, J.; Schmidt, B.A.; et al. Preoperative stimulation of resolution and inflammation blockade eradicates micrometastases. J. Clin. Investig. 2019, 129, 2964–2979. [Google Scholar] [CrossRef] [PubMed]
- Schack, A.; Fransgaard, T.; Klein, M.F.; Gögenur, I. Perioperative Use of Nonsteroidal Anti-inflammatory Drugs Decreases the Risk of Recurrence of Cancer After Colorectal Resection: A Cohort Study Based on Prospective Data. Ann. Surg. Oncol. 2019, 26, 3826–3837. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Kenney, S.R.; Cook, L.; Adams, S.F.; Rutledge, T.; Romero, E.; Oprea, T.; Sklar, L.A.; Bedrick, E.; Wiggins, C.L.; et al. A Novel Pharmacologic Activity of Ketorolac for Therapeutic Benefit in Ovarian Cancer Patients. Clin. Cancer Res. 2015, 21, 5064–5072. [Google Scholar] [CrossRef] [PubMed]
- Hudson, L.G.; Cook, L.S.; Grimes, M.M.; Muller, C.Y.; Adams, S.F.; Wandinger-Ness, A. Dual Actions of Ketorolac in Metastatic Ovarian Cancer. Cancers 2019, 11, 1049. [Google Scholar] [CrossRef] [PubMed]
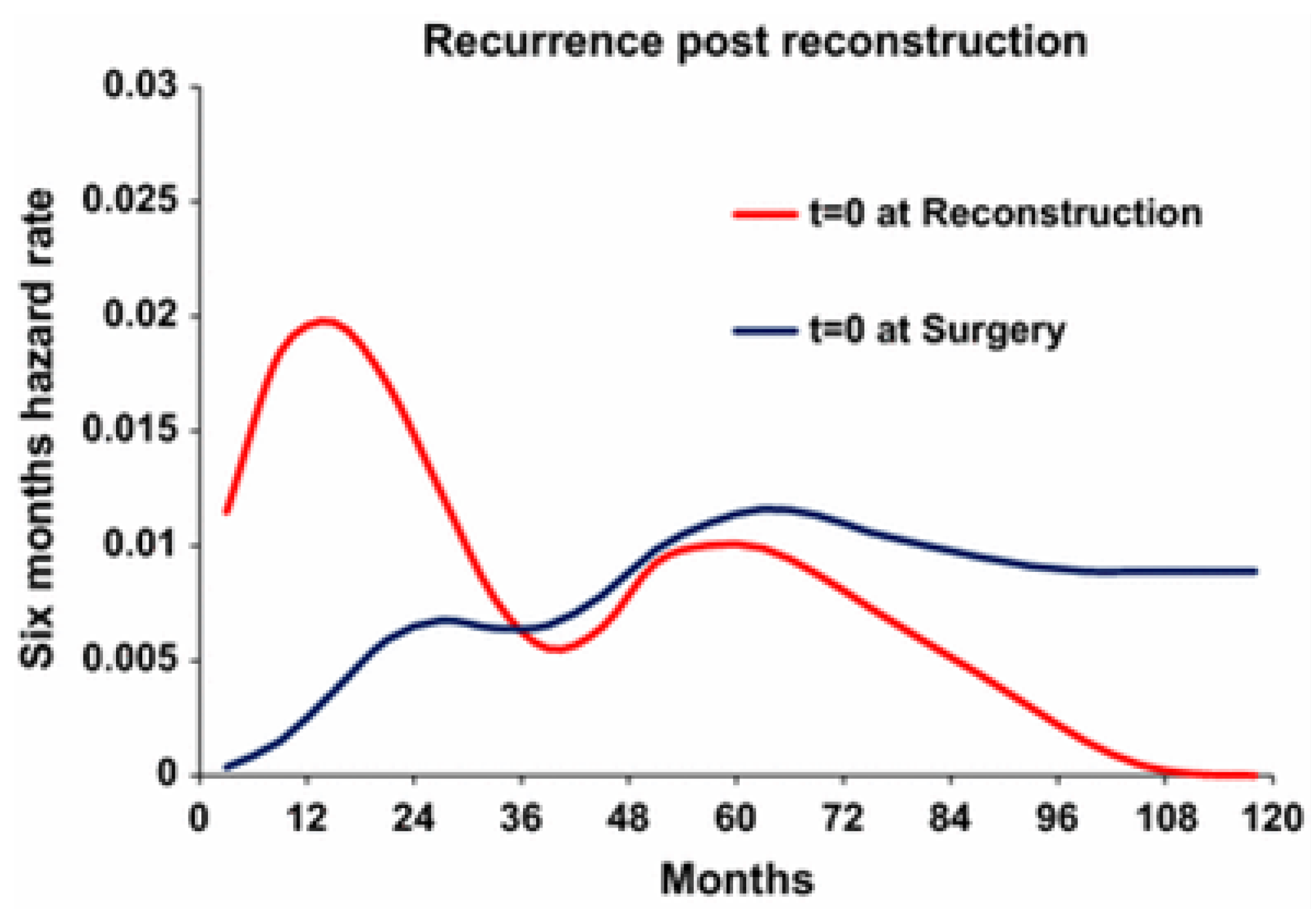
- Dillekås, H.; Demicheli, R.; Ardoino, I.; Jensen, S.A.H.; Biganzoli, E.; Straume, O. The recurrence pattern following delayed breast reconstruction after mastectomy for breast cancer suggests a systemic effect of surgery on occult dormant micrometastases. Breast Cancer Res. Treat. 2016, 158, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Casas, R.; Sacanella, E.; Urpí-Sardà, M.; Chiva-Blanch, G.; Ros, E.; Martínez-González, M.-A.; Covas, M.-I.; Salas-Salvadó, J.; Fiol, M.; Arós, F.; et al. The Effects of the Mediterranean Diet on Biomarkers of Vascular Wall Inflammation and Plaque Vulnerability in Subjects with High Risk for Cardiovascular Disease. A Randomized Trial. PLoS ONE 2014, 9, e100084. [Google Scholar] [CrossRef] [PubMed]
- Kita, H.; Shiraishi, Y.; Watanabe, K.; Suda, K.; Ohtsuka, K.; Koshiishi, Y.; Goya, T. Does Postoperative Serum Interleukin-6 Influence Early Recurrence after Curative Pulmonary Resection of Lung Cancer? Ann. Thorac. Cardiovasc. Surg. 2011, 17, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Omidvari, S.; Hamedi, S.H.; Mohammadianpanah, M.; Nasrolahi, H.; Mosalaei, A.; Talei, A.; Ahmadloo, N.; Ansari, M. Very Late Relapse in Breast Cancer Survivors: A Report of 6 Cases. Iran. J. Cancer Prev. 2013, 6, 113–117. [Google Scholar] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Retsky, M. It May Be Possible to Prevent both Early and Late Relapses in Breast Cancer; Perhaps This Is an Opportunity for Sensors or Biosensors to Help. Sensors 2020, 20, 7261. https://doi.org/10.3390/s20247261
Retsky M. It May Be Possible to Prevent both Early and Late Relapses in Breast Cancer; Perhaps This Is an Opportunity for Sensors or Biosensors to Help. Sensors. 2020; 20(24):7261. https://doi.org/10.3390/s20247261
Chicago/Turabian StyleRetsky, Michael. 2020. "It May Be Possible to Prevent both Early and Late Relapses in Breast Cancer; Perhaps This Is an Opportunity for Sensors or Biosensors to Help" Sensors 20, no. 24: 7261. https://doi.org/10.3390/s20247261
APA StyleRetsky, M. (2020). It May Be Possible to Prevent both Early and Late Relapses in Breast Cancer; Perhaps This Is an Opportunity for Sensors or Biosensors to Help. Sensors, 20(24), 7261. https://doi.org/10.3390/s20247261




