Testing the Performance of an Innovative Markerless Technique for Quantitative and Qualitative Gait Analysis
Abstract
1. Introduction
2. Materials and Methods
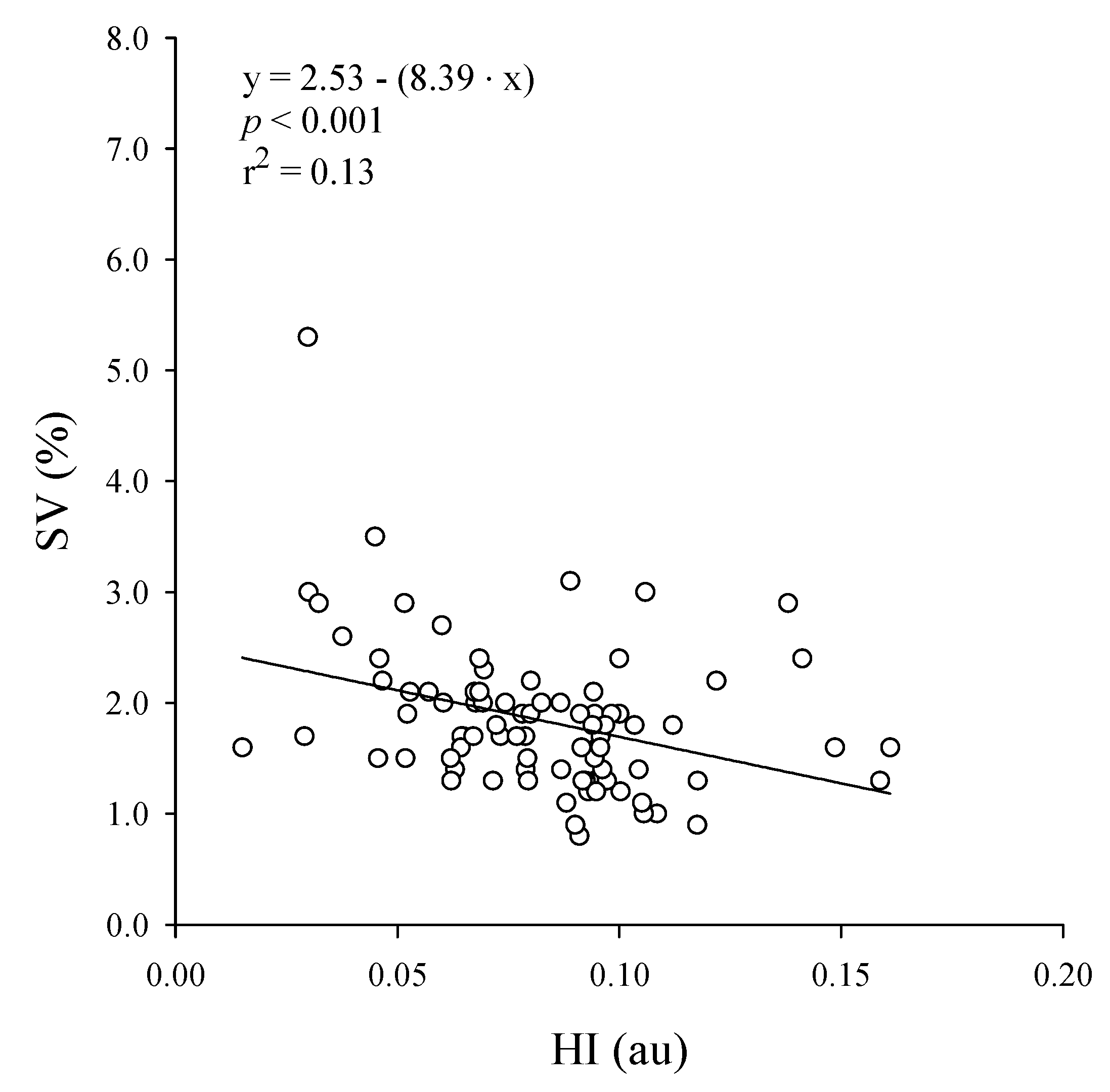
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- WHO. International Classification of Functioning, Disability and Health; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Bugané, F.; Benedetti, M.G.; Casadio, G.; Attala, S.; Biagi, F.; Manca, M.; Leardini, A. Estimation of spatial-temporal gait parameters in level walking based on a single accelerometer: Validation on normal subjects by standard gait analysis. Comput. Methods Programs Biomed. 2012, 108, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Wren, T.A.L.; Gorton, G.E.; Õunpuu, S.; Tucker, C.A. Efficacy of clinical gait analysis: A systematic review. Gait Posture 2011, 34, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Dicharry, J. Kinematics and kinetics of gait: From lab to clinic. Clin. Sports Med. 2010, 29, 347–364. [Google Scholar] [CrossRef] [PubMed]
- Esser, P.; Dawes, H.; Collett, J.; Feltham, M.G.; Howells, K. Assessment of spatio-temporal gait parameters using inertial measurement units in neurological populations. Gait Posture 2011, 34, 558–560. [Google Scholar] [CrossRef]
- Chow, J.W.; Yablon, S.A.; Horn, T.S.; Stokic, D.S. Temporospatial characteristics of gait in patients with lower limb muscle hypertonia after traumatic brain injury. Brain Inj. 2010, 24, 1575–1584. [Google Scholar] [CrossRef]
- Maffiuletti, N.A.; Impellizzeri, F.M.; Widler, K.; Bizzini, M.; Kain, M.S.; Munzinger, U.; Leunig, M. Spatiotemporal parameters of gait after total hip replacement: Anterior versus posterior approach. Orthop. Clin. N. Am. 2009, 40, 407–415. [Google Scholar] [CrossRef]
- Erdem, M.M.; Koc, G.; Kismet, K.; Yasti, C.; Topuz, S. Evaluation of spatio-temporal gait parameters and gait symmetry in diabetic polyneuropathic patients with burn injury: A pilot study. Burn 2020, 46, 897–905. [Google Scholar] [CrossRef]
- Gomez, G.; Khanna, M.; Gupta, A.; Nalini, A.; Thennarasu, K.; Nashi, S.; Polavarapu, K.; Vengalil, S. GNE myopathy—A cross-sectional study on spatio-temporal gait characteristics. Neuromuscul. Disord. 2019, 29, 961–967. [Google Scholar] [CrossRef]
- Iosa, M.; Fusco, A.; Marchetti, F.; Morone, G.; Caltagirone, C.; Paolucci, S.; Peppe, A. The golden ratio of gait harmony: Repetitive proportions of repetitive gait phases. BioMed Res. Int. 2013, 2013, 1–7. [Google Scholar] [CrossRef]
- Iosa, M.; Morone, G.; Fusco, A.; Marchetti, F.; Caltagirone, C.; Paolucci, S.; Peppe, A. Loss of fractal gait harmony in Parkinson’s Disease. Clin. Neurophysiol. 2016, 127, 1540–1546. [Google Scholar] [CrossRef]
- Iosa, M.; Morone, G.; Bini, F.; Fusco, A.; Paolucci, S.; Marinozzi, F. The connection between anthropometry and gait harmony unveiled through the lens of the golden ratio. Neurosci. Lett. 2016, 612, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Menz, H.B.; Lord, S.R.; Fitzpatrick, R.C. Acceleration patterns of the head and pelvis when walking are associated with risk of falling in community-dwelling older people. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2003, 58, M446–M452. [Google Scholar] [CrossRef] [PubMed]
- Howcroft, J.; Kofman, J.; Lemaire, E.D.; McIlroy, W.E. Analysis of dual-task elderly gait in fallers and non-fallers using wearable sensors. J. Biomech. 2016, 49, 992–1001. [Google Scholar] [CrossRef] [PubMed]
- Williams, G.; Vicinanza, D. Coordination in gait: Demonstration of a spectral approach. J. Sports Sci. 2017, 36, 1768–1775. [Google Scholar] [CrossRef] [PubMed]
- Bellanca, J.; Lowry, K.; VanSwearingen, J.; Brach, J.; Redfern, M. Harmonic ratios: A quantification of step to step symmetry. J. Biomech. 2013, 46, 828–831. [Google Scholar] [CrossRef]
- Serrao, M.M.; Chini, G.; Iosa, M.; Casali, C.C.; Morone, G.; Conte, C.; Bini, F.; Marinozzi, F.; Coppola, G.; Pierelli, F.; et al. Harmony as a convergence attractor that minimizes the energy expenditure and variability in physiological gait and the loss of harmony in cerebellar ataxia. Clin. Biomech. 2017, 48, 15–23. [Google Scholar] [CrossRef]
- Morelli, D.; Marro, T.; Paolucci, S.; Fusco, A.; Iosa, M. Ability and stability of running and walking in children with cerebral palsy. Neuropediatrics 2013, 44, 147–154. [Google Scholar] [CrossRef]
- Iosa, M.; Paradisi, F.; Brunelli, S.; Delussu, A.S.; Pellegrini, R.; Zenardi, D.; Paolucci, S.; Traballesi, M. Assessment of gait stability, harmony, and symmetry in subjects with lower-limb amputation evaluated by trunk accelerations. J. Rehabil. Res. Dev. 2014, 51, 623–634. [Google Scholar] [CrossRef]
- Pasciuto, I.; Bergamini, E.; Iosa, M.; Vannozzi, G.; Cappozzo, A. Overcoming the limitations of the Harmonic Ratio for the reliable assessment of gait symmetry. J. Biomech. 2017, 53, 84–89. [Google Scholar] [CrossRef]
- Radzak, K.N.; Putnam, A.M.; Tamura, K.; Hetzler, R.K.; Stickley, C.D. Asymmetry between lower limbs during rested and fatigued state running gait in healthy individuals. Gait Posture 2017, 51, 268–274. [Google Scholar] [CrossRef]
- Rantalainen, T.; Hart, N.H.; Nimphius, S.; Wundersitz, D.W. Associations between step duration variability and inertial measurement unit derived gait characteristics. J. Appl. Biomech. 2016, 32, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Petraglia, F.; Scarcella, L.; Pedrazzi, G.; Brancato, L.; Puers, R.; Costantino, C. Inertial sensors versus standard systems in gait analysis: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2019, 55, 265–280. [Google Scholar] [CrossRef]
- Colyer, S.L.; Evans, M.; Cosker, D.P.; Salo, A.I.T. A review of the evolution of vision-based motion analysis and the integration of advanced computer vision methods towards developing a markerless system. Sports Med.-Open 2018, 4, 1–15. [Google Scholar] [CrossRef] [PubMed]
- García-Pinillos, F.; Latorre-Román, P. Ángel; Ramírez-Campillo, R.; Roche-Seruendo, L.E. Agreement between spatiotemporal parameters from a photoelectric system with different filter settings and high-speed video analysis during running on a treadmill at comfortable velocity. J. Biomech. 2019, 93, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Lowry, K.A.; Smiley-Oyen, A.L.; Carrel, A.J.; Kerr, J.P. Walking stability using harmonic ratios in Parkinson’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 2009, 24, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Muro-De-La-Herran, A.; Garcia-Zapirain, B.; Mendez-Zorrilla, A. Gait analysis methods: An overview of wearable and non-wearable systems, highlighting clinical applications. Sensors 2014, 14, 3362–3394. [Google Scholar] [CrossRef]
- Verlekar, T.T.; Soares, L.D.; Correia, P.L. Automatic classification of gait impairments using a markerless 2d video-based system. Sensors 2018, 18, 2743. [Google Scholar] [CrossRef]
- Auvinet, E.; Multon, F.; Meunier, J. New lower-limb gait asymmetry indices based on a depth camera. Sensors 2015, 15, 4605–4623. [Google Scholar] [CrossRef]
- Zhang, A.; Yang, S.; Zhang, X.; Zhang, J.; Zhang, W. Abnormal Gait Detection in Surveillance Videos with FFT-Based Analysis on Walking Rhythm. In International Conference on Image and Graphics; Springer: Cham, Switzerland, 2017; pp. 108–117. [Google Scholar]
- Wall, J.C.; Charteris, J. A kinematic study of long-term habituation to treadmill walking. Ergonomics 1981, 24, 531–542. [Google Scholar] [CrossRef]
- Meyer, C.; Killeen, T.; Easthope, C.S.; Curt, A.; Bolliger, M.; Linnebank, M.; Zörner, B.; Filli, L. Familiarization with treadmill walking: How much is enough? Sci. Rep. 2019, 9, 1–10. [Google Scholar] [CrossRef]
- Lee, M.M.; Song, C.H.; Lee, K.J.; Jung, S.W.; Shin, D.C.; Shin, S.H. Concurrent validity and test-retest reliability of the OPTOGait photoelectric cell system for the assessment of spatio-temporal parameters of the gait of young adults. J. Phys. Ther. Sci. 2014, 26, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Jacksteit, R.; Mau-Moeller, A.; Völker, A.; Bader, R.; Mittelmeier, W.; Skripitz, R.; Stöckel, T. The mental representation of the human gait in hip osteoarthrosis and total hip arthroplasty patients: A clinical cross-sectional study. Clin. Rehabil. 2018, 33, 335–344. [Google Scholar] [CrossRef] [PubMed]
- Alguacil, J.M.; Paez-Moguer, J.; Jiménez-Cebrián, A.M.; Muñoz, B. Álvarez; Gijon-Nogueron, G.; Asencio, J.M. The influence of childhood obesity on spatio-temporal gait parameters. Gait Posture 2019, 71, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Urbanek, J.K.; Zipunnikov, V.; Harris, T.; Fadel, W.; Glynn, N.W.; Koster, A.; Caserotti, P.; Crainiceanu, C.M.; Harezlak, J. Prediction of sustained harmonic walking in the free-living environment using raw accelerometry data. Physiol. Meas. 2018, 39, 02NT02. [Google Scholar] [CrossRef] [PubMed]
- Bisi, M.C.; Riva, F.; Stagni, R. Measures of gait stability: Performance on adults and toddlers at the beginning of independent walking. J. Neuroeng. Rehabil. 2014, 11, 131. [Google Scholar] [CrossRef]
- Bezryadin, S.; Bourov, P.; Ilinih, D. Brightness calculation in digital image processing. Int. Symp. Technol. Digit. Photo Fulfillment 2007, 2007, 10–15. [Google Scholar] [CrossRef]
- MadehKhaksar, F.; Klenk, J.; Sczuka, K.; Gordt, K.; Melzer, I.; Schwenk, M. The effects of unexpected mechanical perturbations during treadmill walking on spatiotemporal gait parameters, and the dynamic stability measures by which to quantify postural response. PLoS ONE 2018, 13, e0195902. [Google Scholar] [CrossRef]
- Yamasaki, M.; Sasaki, T.; Torii, M. Sex difference in the pattern of lower limb movement during treadmill walking. Graefe’s Arch. Clin. Exp. Ophthalmol. 1991, 62, 99–103. [Google Scholar] [CrossRef]
- Stoquart, G.; Detrembleur, C.; Lejeune, T.M. Effect of speed on kinematic, kinetic, electromyographic and energetic reference values during treadmill walking. Neurophysiol. Clin. Neurophysiol. 2008, 38, 105–116. [Google Scholar] [CrossRef]
- Donath, L.; Faude, O.; Lichtenstein, E.; Nüesch, C.; Mündermann, A. Validity and reliability of a portable gait analysis system for measuring spatiotemporal gait characteristics: Comparison to an instrumented treadmill. J. Neuroeng. Rehabil. 2016, 13, 1–9. [Google Scholar] [CrossRef]
- Clark, R.A.; Bower, K.J.; Mentiplay, B.F.; Paterson, K.; Pua, Y.-H. Concurrent validity of the Microsoft Kinect for assessment of spatiotemporal gait variables. J. Biomech. 2013, 46, 2722–2725. [Google Scholar] [CrossRef] [PubMed]
- Nixon, M.; Carter, J. Advances in automatic gait recognition. In Proceedings of the Sixth IEEE International Conference on Automatic Face and Gesture Recognition, Seoul, Korea, 19 May 2004; pp. 11–16. [Google Scholar]
- Pogorelc, B.; Bosnić, Z.; Gams, M. Automatic recognition of gait-related health problems in the elderly using machine learning. Multimed. Tools Appl. 2011, 58, 333–354. [Google Scholar] [CrossRef]
- Stone, E.E.; Skubic, M. Unobtrusive, continuous, in-home gait measurement using the Microsoft Kinect. IEEE Trans. Biomed. Eng. 2013, 60, 2925–2932. [Google Scholar] [CrossRef] [PubMed]
- Danion, F.; Varraine, E.; Bonnard, M.; Pailhous, J. Stride variability in human gait: The effect of stride frequency and stride length. Gait Posture 2003, 18, 69–77. [Google Scholar] [CrossRef]
- Herssens, N.; Verbecque, E.; Hallemans, A.; Vereeck, L.; Van Rompaey, V.; Saeys, W. Do spatiotemporal parameters and gait variability differ across the lifespan of healthy adults? A systematic review. Gait Posture 2018, 64, 181–190. [Google Scholar] [CrossRef]



| Patients | Males n = 66 | Females n = 20 | Total n = 86 |
|---|---|---|---|
| Speed (km/h) | 1.1 (0.1) | 1.01 (0.1) | 1.1 (0.1) |
| Stride length (cm) | 126.8 (12.5) | 114.9 (11.1) | 123.8 (13.3) |
| Normalized stride length | 0.72 (0.06) | 0.69 (0.07) | 0.71 (0.07) |
| Stride frequency (Hz) | 0.89 (0.08) | 0.89 (0.08) | 0.89 (0.08) |
| Step frequency or Cadence (Hz) | 1.79 (0.16) | 1.79 (0.18) | 1.79 (0.16) |
| Stride variability | 1.78 (0.57) | 2.04 (0.90) | 1.84 (0.66) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simoni, L.; Scarton, A.; Gerli, F.; Macchi, C.; Gori, F.; Pasquini, G.; Pogliaghi, S. Testing the Performance of an Innovative Markerless Technique for Quantitative and Qualitative Gait Analysis. Sensors 2020, 20, 6654. https://doi.org/10.3390/s20226654
Simoni L, Scarton A, Gerli F, Macchi C, Gori F, Pasquini G, Pogliaghi S. Testing the Performance of an Innovative Markerless Technique for Quantitative and Qualitative Gait Analysis. Sensors. 2020; 20(22):6654. https://doi.org/10.3390/s20226654
Chicago/Turabian StyleSimoni, Laura, Alessandra Scarton, Filippo Gerli, Claudio Macchi, Federico Gori, Guido Pasquini, and Silvia Pogliaghi. 2020. "Testing the Performance of an Innovative Markerless Technique for Quantitative and Qualitative Gait Analysis" Sensors 20, no. 22: 6654. https://doi.org/10.3390/s20226654
APA StyleSimoni, L., Scarton, A., Gerli, F., Macchi, C., Gori, F., Pasquini, G., & Pogliaghi, S. (2020). Testing the Performance of an Innovative Markerless Technique for Quantitative and Qualitative Gait Analysis. Sensors, 20(22), 6654. https://doi.org/10.3390/s20226654





