Noninvasive Measurement of Time-Varying Arterial Wall Elastance Using a Single-Frequency Vibration Approach
Abstract
1. Introduction
2. Materials and Methods
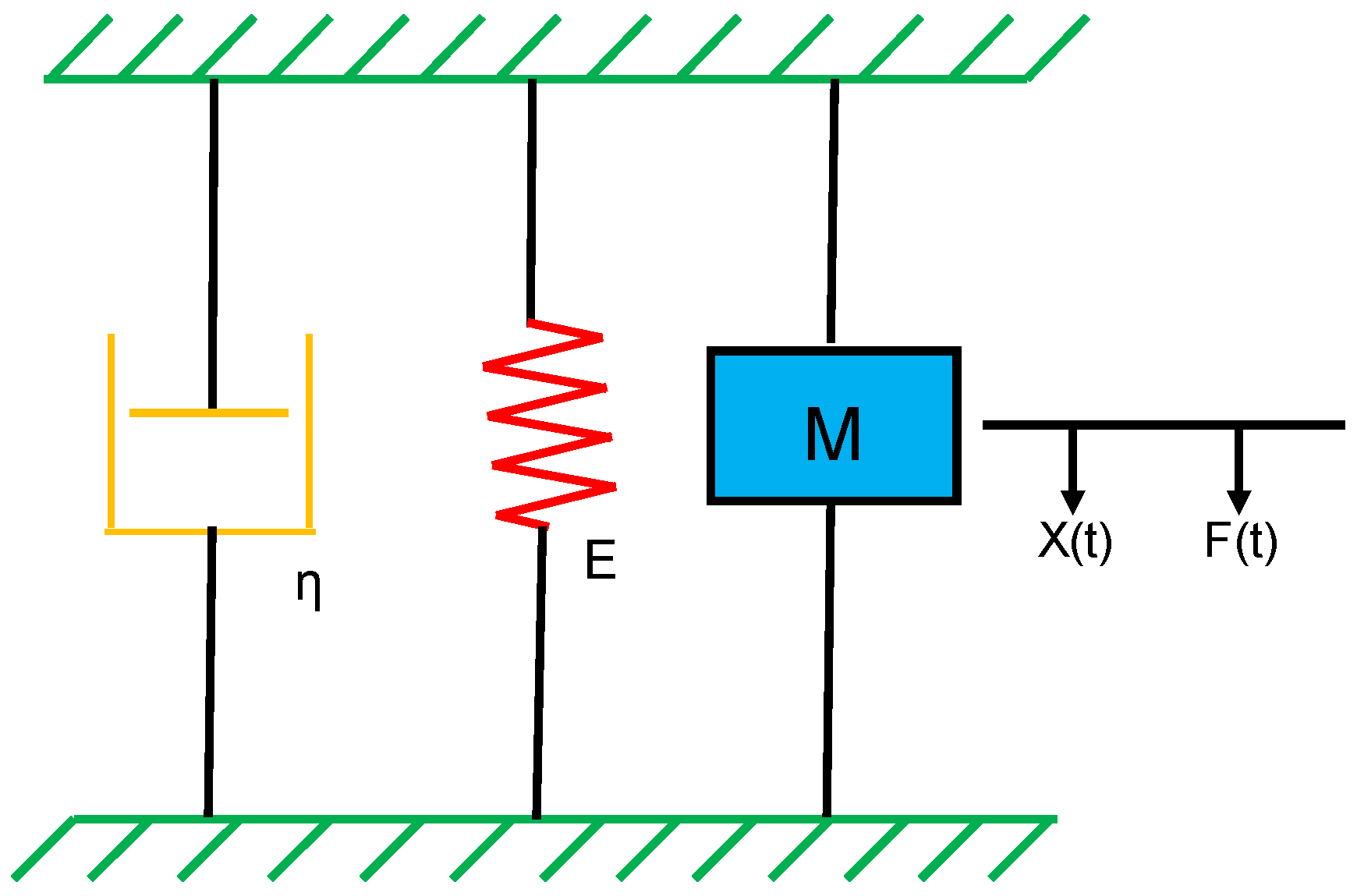
2.1. Vascular Wall Model
2.2. Multiple-Frequency Estimation of Wall Elastance
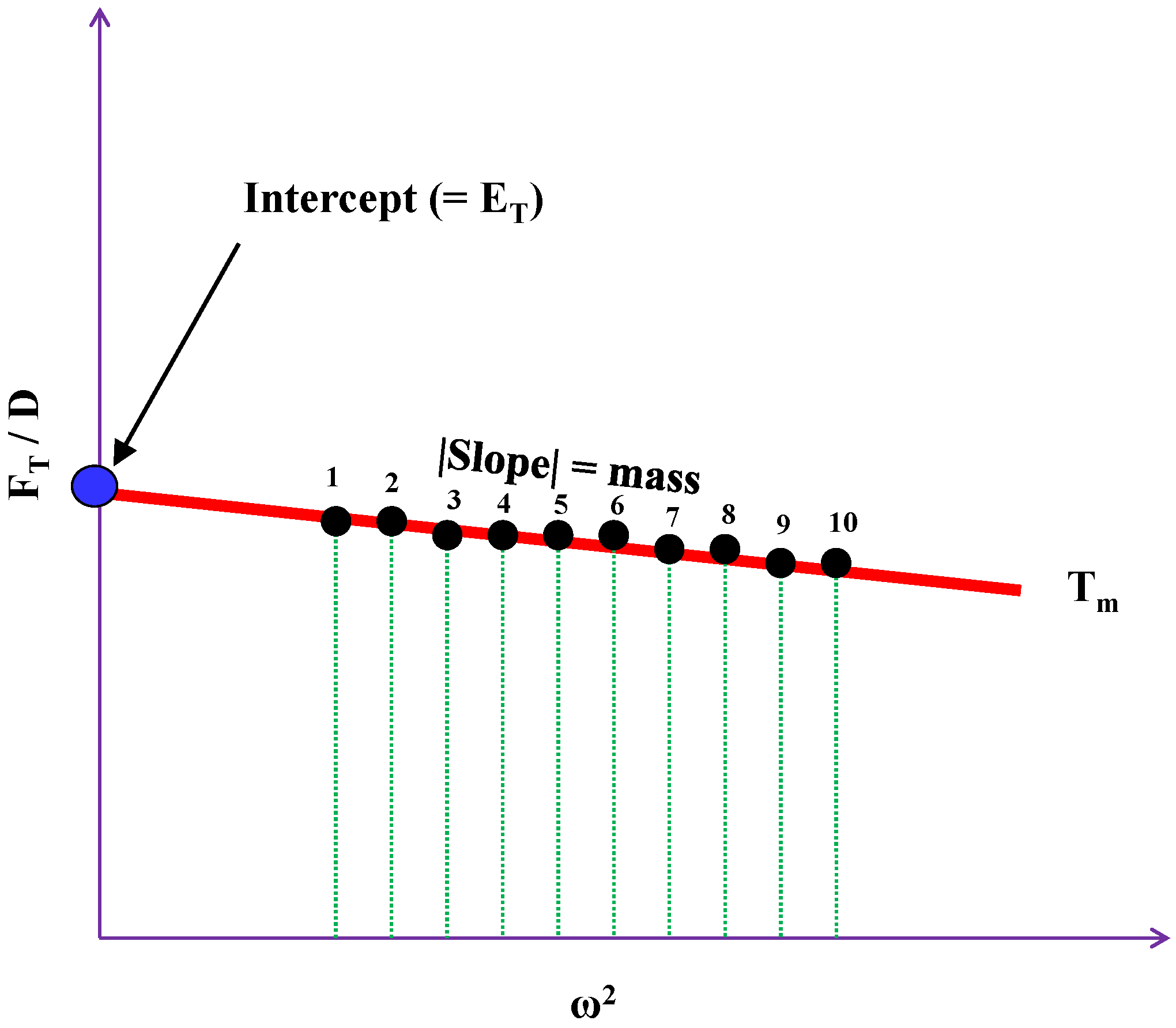
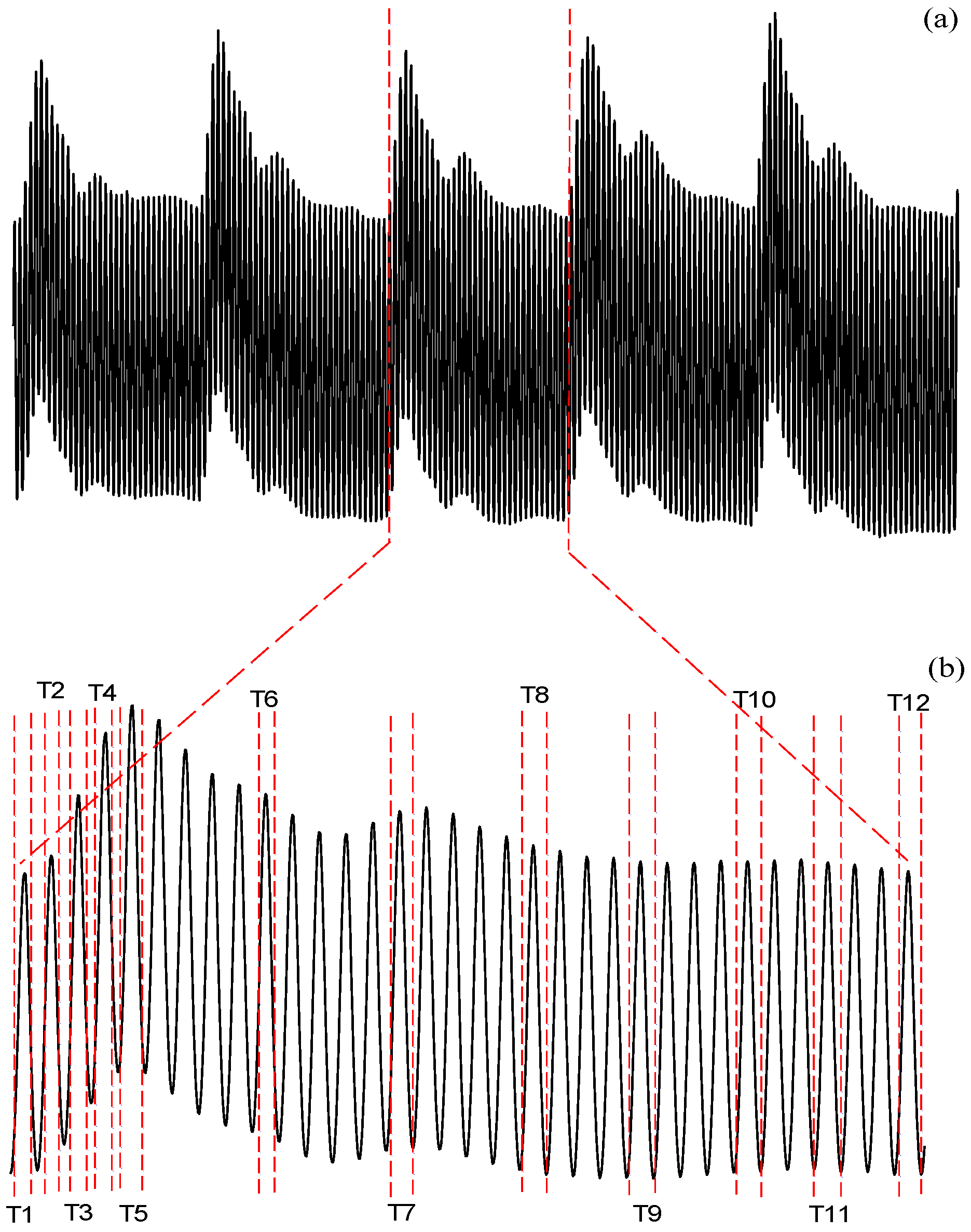
2.3. Single-Frequency Estimation of Wall Elastance
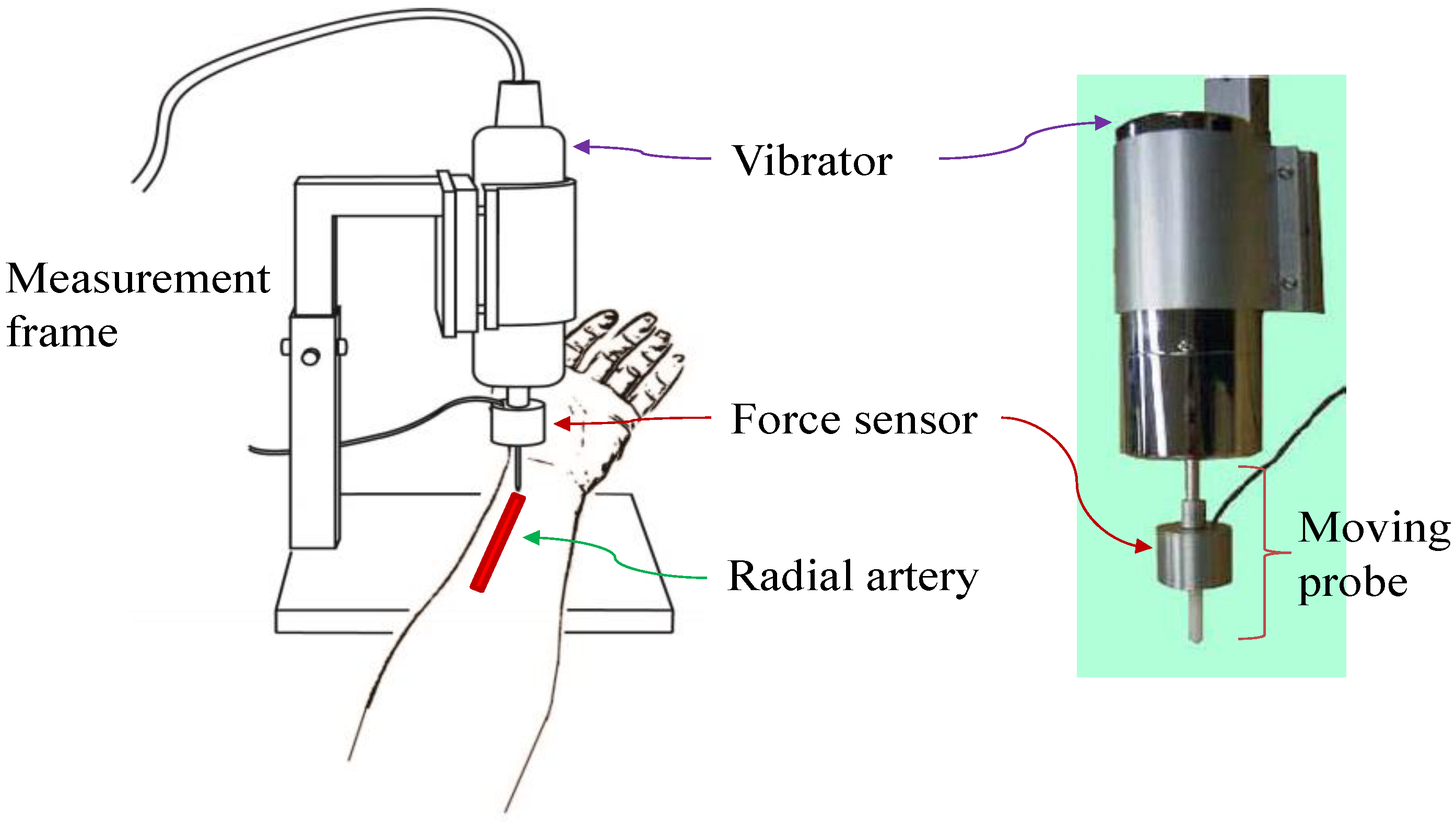
3. Measurement System
4. Experimental Protocol
5. Statistical Analysis
6. Results
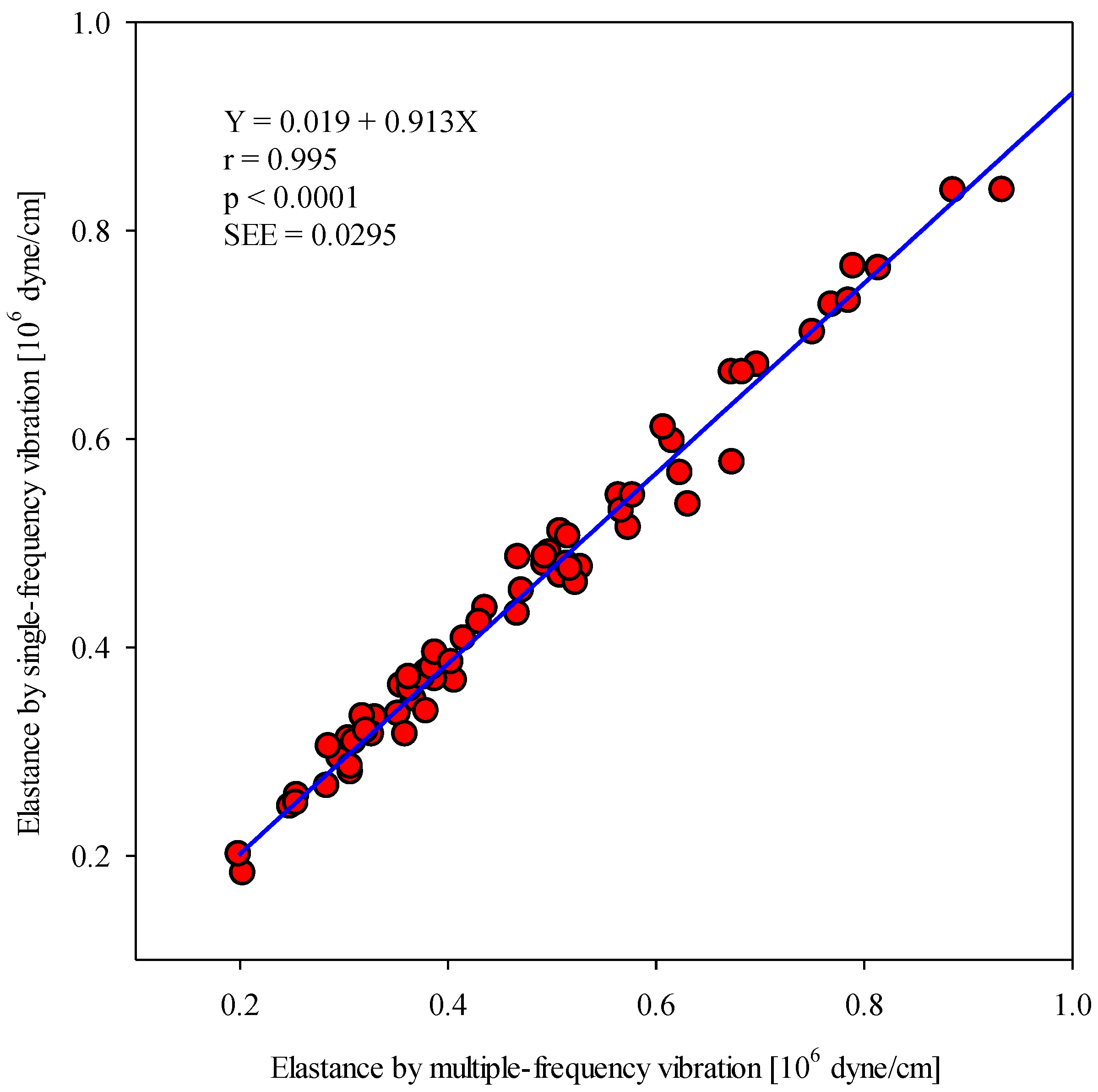
6.1. Comaprison of Maximum Wall Elastances Using Multiple- and Single-Frequency Approaches
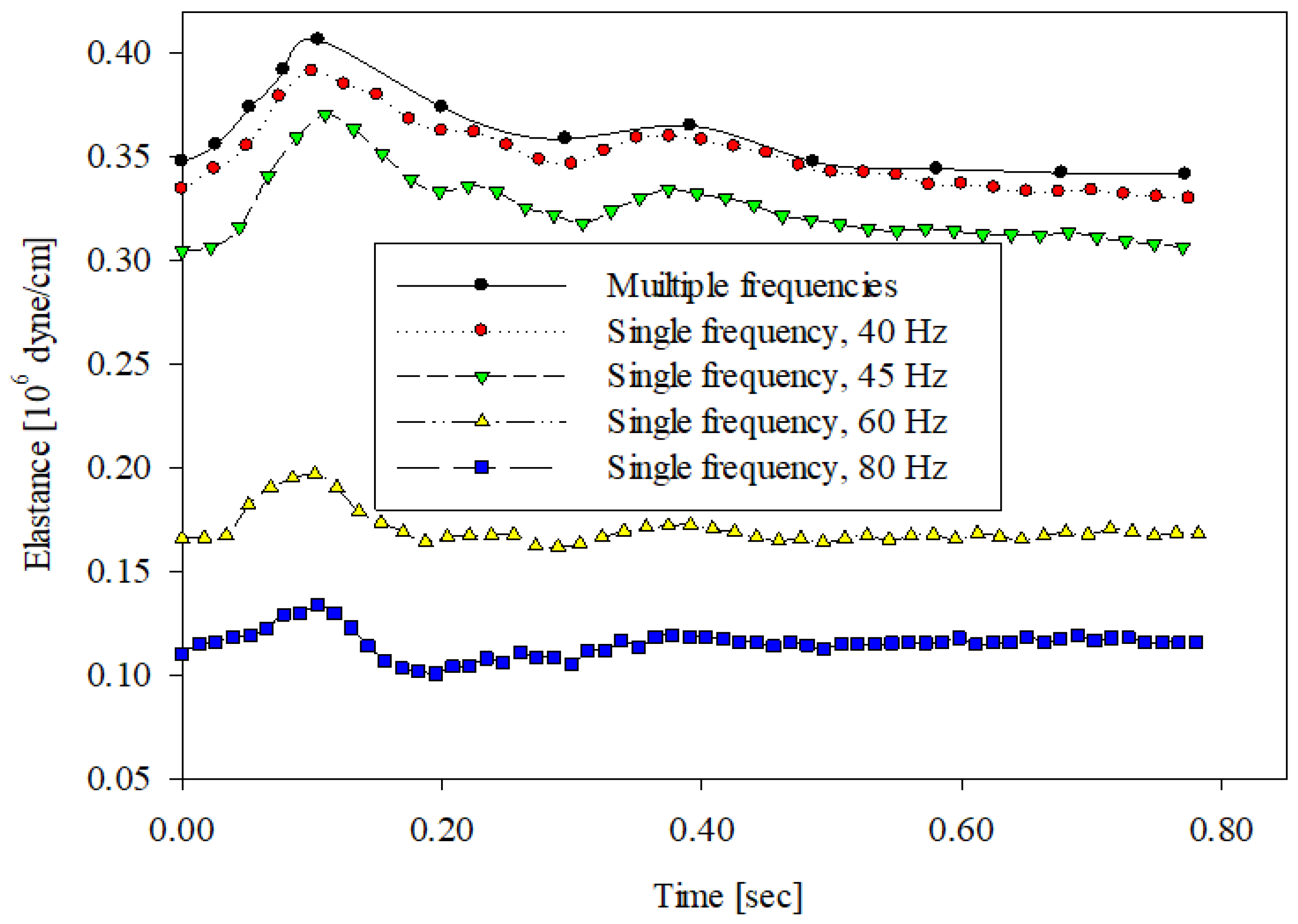
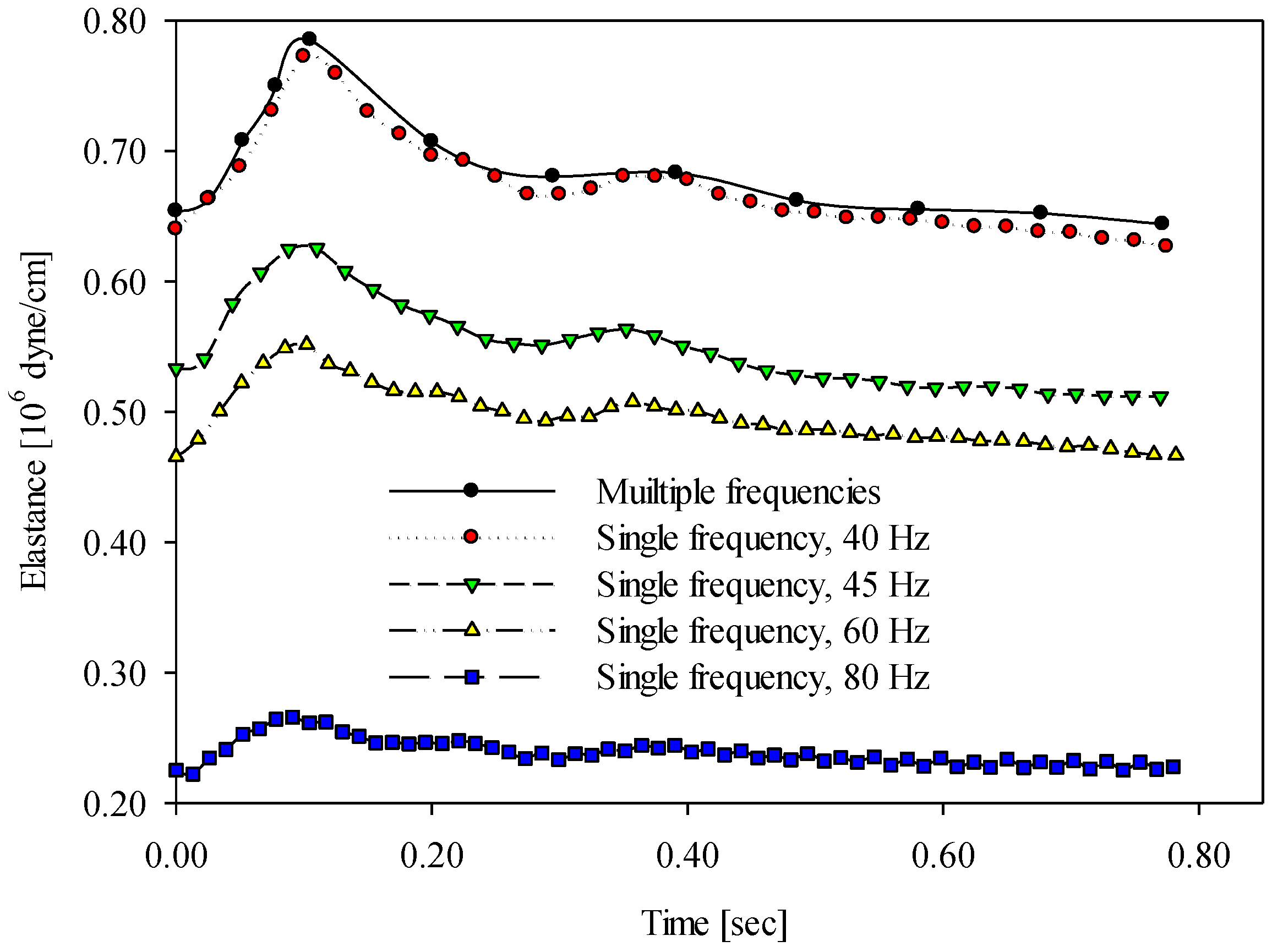
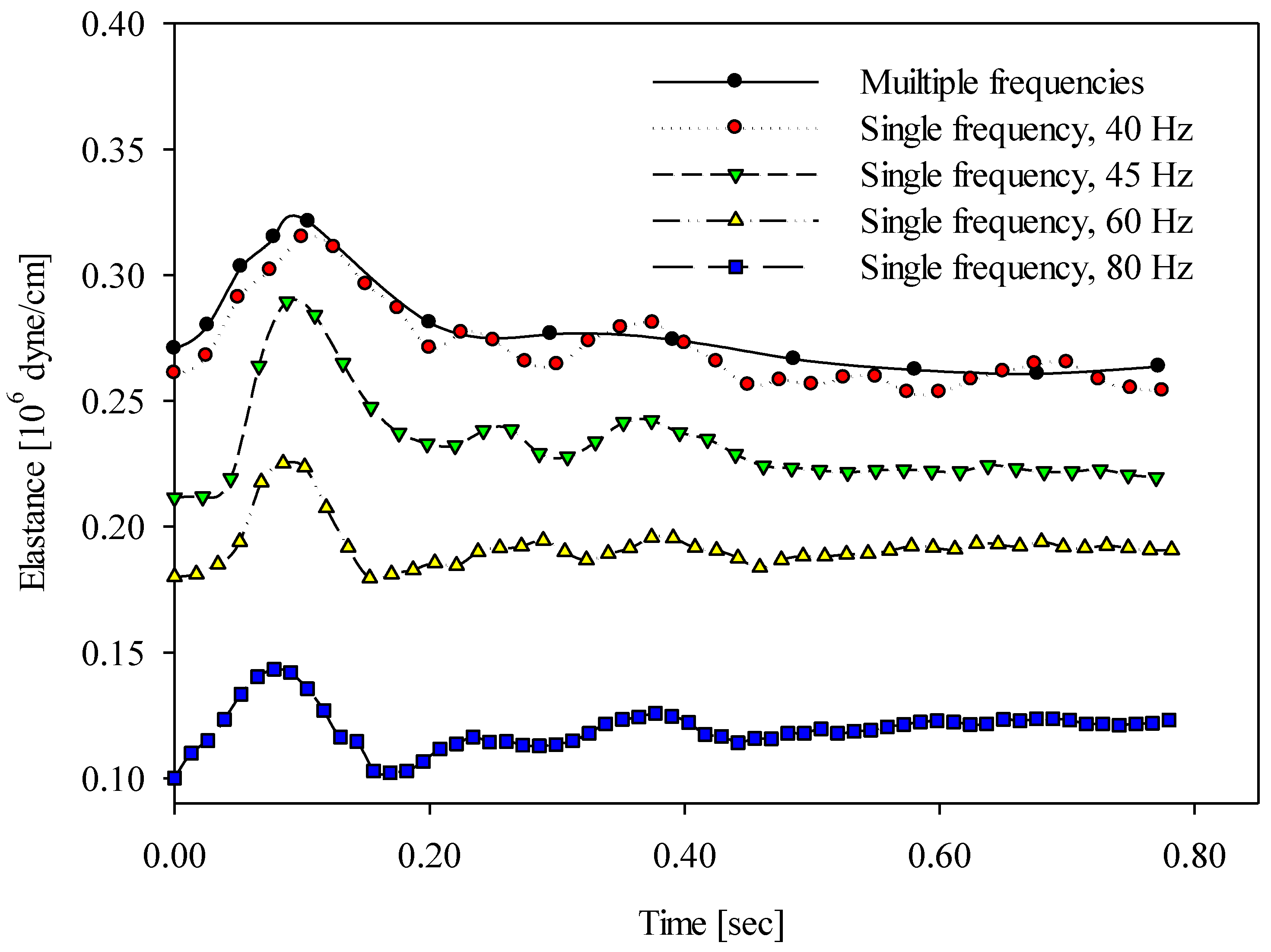
6.2. Comparison of Time-Varying Wall Elastances Using Multiple- and Single-Frequency Approaches
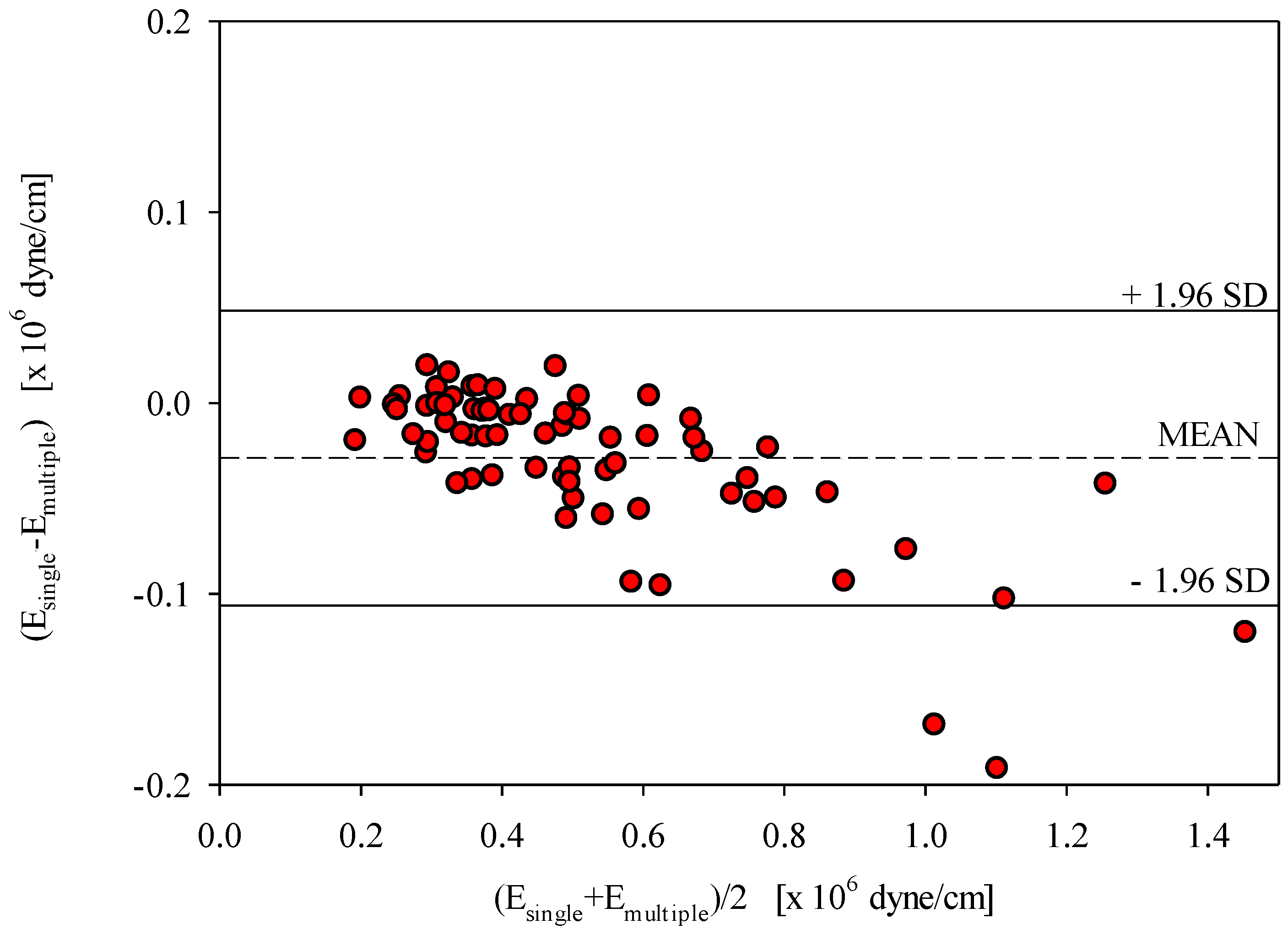
6.3. Bland–Altman Plot
7. Discussion
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Glasser, S.P.; Arnett, D.K.; McVeigh, G.E.; Finkelstein, S.M.; Bank, A.J.; Morgan, D.J.; Cohn, J.N. Vascular compliance and cardiovascular disease: A risk factor or a marker? Am. J. Hypertens. 1997, 10, 1175–1189. [Google Scholar] [CrossRef]
- Hallock, P.; Benson, I.C. Studies on the elastic properties of human isolated aorta. J. Clin. Investig. 1937, 16, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Kinlay, S.; Creager, M.A.; Fukumoto, M.; Hikita, H.; Fang, J.C.; Selwyn, A.P.; Ganz, P. Endothelium-derived nitric oxide regulates arterial elasticity in human arteries in vivo. Hypertension 2001, 38, 1049–1053. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, I.B.; Qasem, A.; McEniery, C.M.; Webb, D.J.; Avolio, A.P.; Cockcroft, J.R. Nitric oxide regulates local arterial distensibility in vivo. Circulation 2002, 105, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, Y.; Takumi, T.; Mathew, V.; Chung, W.Y.; Barsness, G.W.; Rihal, C.S.; Gulati, R.; McCue, E.T.; Holmes, D.R.; Eeckhout, E.; et al. Plaque characteristics and arterial remodeling in coronary and peripheral arterial systems. Atherosclerosis 2012, 223, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Choi, K.H.; Koo, B.K.; Park, J.; Kim, J.; Hwang, D.; Rhee, T.M.; Kim, H.Y.; Jung, H.W.; Kim, K.J.; et al. Prognostic implications of plaque characteristics and stenosis severity in patients with coronary artery disease. J. Am. Coll. Cardiol. 2019, 73, 2413–2424. [Google Scholar] [CrossRef] [PubMed]
- Avolio, A.P.; Kuznetsova, T.; Heyndrickx, G.R.; Kerkhof, P.L.M.; Li, J.K. Arterial flow, pulse pressure and pulse wave velocity in men and women at various ages. Adv. Exp. Med. Biol. 2018, 1065, 153–168. [Google Scholar] [PubMed]
- Chirinos, J.A.; Segers, P.; Hughes, T.; Townsend, R. Large-artery stiffness in health and disease: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2019, 74, 1237–1263. [Google Scholar] [CrossRef]
- Bhuiyan, A.R.; Li, S.; Li, H.; Chen, W.; Srinivasan, S.R.; Berenson, G.S. Distribution and correlates of arterial compliance measures in asymptomatic young adults: The Bogalusa Heart Study. Am. J. Hypertens. 2005, 18, 684–691. [Google Scholar] [CrossRef][Green Version]
- Sahebkar, A.; Pein, I.; Tedeschi-Reiner, E.; Derosa, G.; Maffioli, P.; Reiner, Z. Effects of statin therapy on augmentation index as a measure of arterial stiffness: A systematic review and meta-analysis. Int. J. Cardiol. 2016, 212, 160–168. [Google Scholar] [CrossRef]
- Pan, F.S.; Xu, M.; Yu, L.; Luo, J.; Li, M.Y.; Liang, J.Y.; Zheng, Y.L.; Xie, X.Y. Relationship between carotid intima-media thickness and carotid artery stiffness assessed by ultrafast ultrasound imaging in patients with type 2 diabetes. Eur. J. Radiol. 2019, 111, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Ryden, A.; Lanne, T.; Wollmer, P. Increased arterial stiffness in women, but not in men, with IDDM. Diabetologia 1995, 38, 1082–1089. [Google Scholar] [CrossRef] [PubMed]
- Komine, H.; Asai, Y.; Yokoi, T.; Yoshizawa, M. Non-invasive assessment of arterial stiffness using oscillometric blood pressure measurement. Biomed. Eng. OnLine 2012, 11, 6. [Google Scholar] [CrossRef] [PubMed]
- Simon, G.; Danneman, K.J. Dilation and reduced distensibility of rat carotid artery with aging. Clin. Exp. Hypertens. 2005, 27, 459–466. [Google Scholar] [CrossRef]
- Wei, C. An innovative method to measure the peripheral arterial elasticity: Spring constant modeling based on the arterial pressure wave with radial vibration. Ann. Biomed. Eng. 2011, 39, 2695–2705. [Google Scholar] [CrossRef]
- Tomiyama, Y.; Yoshinaga, K.; Fujii, S.; Ochi, N.; Inoue, M.; Nishida, M.; Aziki, K.; Horie, T.; Katoh, C.; Tamaki, N. Accurate quantitative measurements of brachial artery cross-sectional vascular area and vascular volume elastic modulus using automated oscillometric measurements: Comparison with brachial artery ultrasound. Hypertens. Res. 2015, 38, 478–484. [Google Scholar] [CrossRef]
- Wang, J.J.; Liu, S.H.; Su, H.M.; Chang, S.; Tseng, W.K. A vibration-based approach to quantifying the dynamic elastance of the superficial arterial wall. Biomed. Eng. Online 2016, 15, 40. [Google Scholar] [CrossRef]
- Cerik, I.B.; Meric, M.; Gulel, O.; Ozturk, C.H.; Coksevim, M.; Soylu, K.; Deveci, A.; Sahin, M. Echocardiographic assessment of pulmonary arterial stiffness in human immunodeficiency virus-infected patients. Echocardiography 2019, 36, 1123–1131. [Google Scholar] [CrossRef]
- Wowern, E.; Östling, G.; Nilsson, P.M.; Olofsson, P. Digital photoplethysmography for assessment of arterial stiffness: Repeatability and comparison with applanation tonometry. PLoS ONE 2015, 10, e0135659. [Google Scholar] [CrossRef]
- Collette, M.; Lalande, A.; Willoteaux, S.; Leftheriotis, G.; Humeau, A. Measurement of the local aortic stiffness by a noninvasive bioelectrical impedance technique. Med. Biol. Eng. Comput. 2011, 49, 431–439. [Google Scholar] [CrossRef]
- Wang, J.J.; Liu, S.H.; Chern, C.I.; Hsieh, J.H. Development of an arterial applanation tonometer for detecting arterial blood pressure and volume. Biomed. Eng. Appl. Basis Commun. 2004, 16, 322–330. [Google Scholar] [CrossRef]
- Liu, S.H.; Wang, J.J.; Huang, K.S. A new oscillometry-based method for estimating the brachial arterial compliance under loaded conditions. IEEE Trans. Biomed. Eng. 2008, 55, 2463–2470. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.L.; Zheng, Y.Y.; Ma, Z.C.; Sun, Y.N. Radial pulse transit time is an index of arterial stiffness. Hypertens. Res. 2011, 34, 884–887. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, J.; Ito, S. Central diastolic pressure decay mediates the relationship between aortic stiffness and myocardial viability: Potential implications for aortosclerosis-induced myocardial ischemia. J. Hypertens. 2017, 35, 2034–2043. [Google Scholar] [CrossRef] [PubMed]
- Milnor, W.R. Chapter 4: Properties of the Vascular Wall. In Hemodynamics, 2nd ed.; Williams and Wilkins: Baltimore, MD, USA, 1989; pp. 58–101. [Google Scholar]
- Wei, C. Developing an effective arterial stiffness monitoring system using the spring constant method and photoplethysmography. IEEE Trans. Biomed. Eng. 2013, 60, 151–154. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Kock, K.S.; Silva, J.B.F.; Marques, J.L.B. Comparison of the ankle-brachial index with parameters of stiffness and peripheral arterial resistance assessed by photoplethysmography in elderly patients. J. Vasc. Bras. 2019, 15, e20180084. [Google Scholar] [CrossRef] [PubMed]
- Collette, M.; Leftheriotis, G.; Humeau, A. Modeling and interpretation of the bioelectrical impedance signal for the determination of the local arterial stiffness. Med. Phys. 2009, 36, 4340–4348. [Google Scholar] [CrossRef][Green Version]
- Brunt, V.E.; Howard, M.J.; Francisco, M.A.; Ely, B.R.; Minson, C.T. Passive heat therapy improves endothelial function, arterial stiffness and blood pressure in sedentary humans. J. Physiol. 2016, 15, 5329–5342. [Google Scholar] [CrossRef]
- Scremin, G.; Kenney, W.L. Aging and the skin blood flow response to the unloading of baroreceptors during heat and cold stress. J. Appl. Physiol. 2004, 96, 1019–1025. [Google Scholar] [CrossRef]
- Wilson, T.E.; Gao, Z.; Hess, K.L.; Monahan, K.D. Effect of aging on cardiac function during cold stress in humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 298, R1627–R1633. [Google Scholar] [CrossRef]
- Ganio, M.S.; Brothers, R.M.; Shibata, S.; Hastings, J.L.; Crandall, C.G. Effect of passive heat stress on arterial stiffness. Exp. Physiol. 2011, 96, 919–926. [Google Scholar] [CrossRef] [PubMed]
- Roca, F.; Bellien, J.; Iacob, M.; Joannides, R. Endothelium-dependent adaptation of arterial wall viscosity during blood flow increase is impaired in essential hypertension. Atherosclerosis 2019, 285, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Roca, F.; Iacob, M.; Remy-Jouet, I.; Bellien, J.; Joannides, R. Evidence for a role of vascular endothelium in the control of arterial wall viscosity in humans. Hypertension 2018, 71, 143–150. [Google Scholar] [CrossRef]
- Chen, X.; Sala-Mercado, J.A.; Hammond, R.L.; Ichinose, M.; Soltani, S.; Mukkamala, R.; O’Leary, D.S. Dynamic control of maximal ventricular elastance via the baroreflex and force-frequency relation in awake dogs before and after pacing-induced heart failure. Am. J. Physiol. Heart Circ. Physiol. 2010, 299, H62–H69. [Google Scholar] [CrossRef] [PubMed]
| Subject | Room Temperature (N = 28) | Cold Stress (N = 23) | Hot Stress (N = 21) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Emultiple | Esingle | Difference | Emultiple | Esingle | Difference | Emultiple | Esingle | Difference | |
| 1 | 203 | 183 | 9.8 | 471 | 454 | 3.5 | 379 | 339 | 10.7 |
| 2 | 415 | 408 | 1.6 | 430 | 424 | 1.4 | 631 | 537 | 14.9 |
| 3 | 574 | 515 | 10.3 | 1012 | 935 | 7.6 | 305 | 312 | 2.6 |
| 4 | 673 | 664 | 1.3 | 683 | 664 | 2.7 | 379 | 376 | 0.8 |
| 5 | 307 | 280 | 8.6 | 623 | 567 | 9.0 | 508 | 469 | 7.7 |
| 6 | 367 | 350 | 4.7 | 751 | 703 | 6.4 | 310 | 309 | 0.2 |
| 7 | 564 | 546 | 3.3 | 578 | 546 | 5.6 | 321 | 320 | 0.4 |
| 8 | 330 | 333 | 0.8 | 385 | 381 | 1.1 | 364 | 360 | 1.0 |
| 9 | 406 | 368 | 9.4 | 785 | 733 | 6.7 | - | - | - |
| 10 | 296 | 294 | 0.6 | 362 | 371 | 2.5 | - | - | - |
| 11 | 255 | 258 | 1.3 | 616 | 598 | 2.9 | - | - | - |
| 12 | 248 | 247 | 0.5 | 284 | 267 | 5.9 | - | - | - |
| 13 | 327 | 316 | 3.2 | 1198 | 1007 | 16.0 | 364 | 360 | 1.0 |
| 14 | 492 | 480 | 2.5 | 514 | 480 | 6.7 | - | - | - |
| 15 | 790 | 766 | 3.0 | 607 | 611 | 0.6 | - | - | - |
| 16 | 355 | 363 | 2.4 | 523 | 462 | 11.6 | 199 | 201 | 1.3 |
| 17 | 318 | 334 | 4.9 | 388 | 395 | 1.8 | 352 | 336 | 4.5 |
| 18 | 886 | 839 | 5.3 | - | - | - | 527 | 477 | 9.6 |
| 19 | 1164 | 1061 | 8.8 | - | - | - | 814 | 764 | 6.1 |
| 20 | 306 | 285 | 6.8 | 403 | 386 | 4.3 | 359 | 316 | 11.8 |
| 21 | 436 | 437 | 0.4 | 517 | 475 | 8.1 | 933 | 839 | 10.0 |
| 22 | 567 | 531 | 6.3 | - | - | - | 467 | 432 | 7.4 |
| 23 | 769 | 729 | 5.2 | 1098 | 929 | 15.4 | 497 | 491 | 1.3 |
| 24 | 1514 | 1394 | 8.0 | 1778 | 1750 | 1.6 | 387 | 370 | 4.6 |
| 25 | 697 | 671 | 3.7 | - | - | - | 376 | 371 | 1.2 |
| 26 | 508 | 511 | 0.7 | 515 | 507 | 1.7 | 254 | 250 | 1.4 |
| 27 | 1277 | 1235 | 3.3 | - | - | - | 673 | 577 | 14.2 |
| 28 | 467 | 486 | 4.1 | 493 | 487 | 1.2 | 285 | 305 | 6.8 |
| Mean ± STD | 554 ± 324 | 532 ± 301 | 4.3 ± 3.1 | 653 ± 339 ** | 641 ± 325 ** | 5.4 ± 4.4 | 444 ± 185 * | 417 ± 158 * | 5.4 ± 4.8 |
| Condition | Linear Regression | Correlation Coefficient, r | SEE | p-Value |
|---|---|---|---|---|
| Room temperature (25 °C) (N = 28) | Esingle = 0.021 + 0.922Emultiple | 0.998 | 0.0198 | <0.0001 |
| Cold stress (4 °C) (N = 23) | Esingle = 0.017 + 0.915Emultiple | 0.991 | 0.0423 | <0.0001 |
| Hot stress (42 °C) (N = 21) | Esingle = 0.041 + 0.846Emultiple | 0.993 | 0.0198 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, J.-J.; Liu, S.-H.; Tseng, W.-K.; Chen, W. Noninvasive Measurement of Time-Varying Arterial Wall Elastance Using a Single-Frequency Vibration Approach. Sensors 2020, 20, 6463. https://doi.org/10.3390/s20226463
Wang J-J, Liu S-H, Tseng W-K, Chen W. Noninvasive Measurement of Time-Varying Arterial Wall Elastance Using a Single-Frequency Vibration Approach. Sensors. 2020; 20(22):6463. https://doi.org/10.3390/s20226463
Chicago/Turabian StyleWang, Jia-Jung, Shing-Hong Liu, Wei-Kung Tseng, and Wenxi Chen. 2020. "Noninvasive Measurement of Time-Varying Arterial Wall Elastance Using a Single-Frequency Vibration Approach" Sensors 20, no. 22: 6463. https://doi.org/10.3390/s20226463
APA StyleWang, J.-J., Liu, S.-H., Tseng, W.-K., & Chen, W. (2020). Noninvasive Measurement of Time-Varying Arterial Wall Elastance Using a Single-Frequency Vibration Approach. Sensors, 20(22), 6463. https://doi.org/10.3390/s20226463








