Wearable Physiological Monitoring System Based on Electrocardiography and Electromyography for Upper Limb Rehabilitation Training
Abstract
1. Introduction
2. Materials and Methods
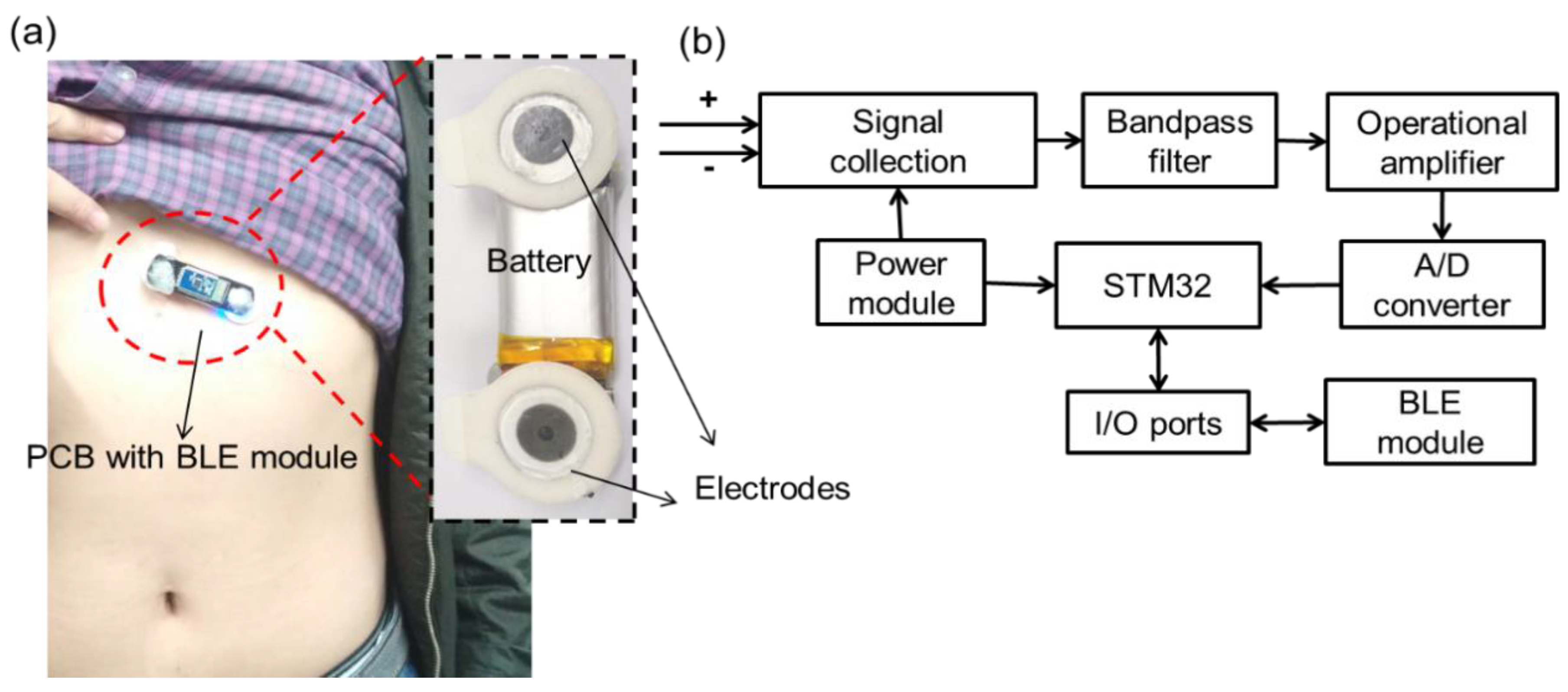
2.1. ECG System Design and Fabrication
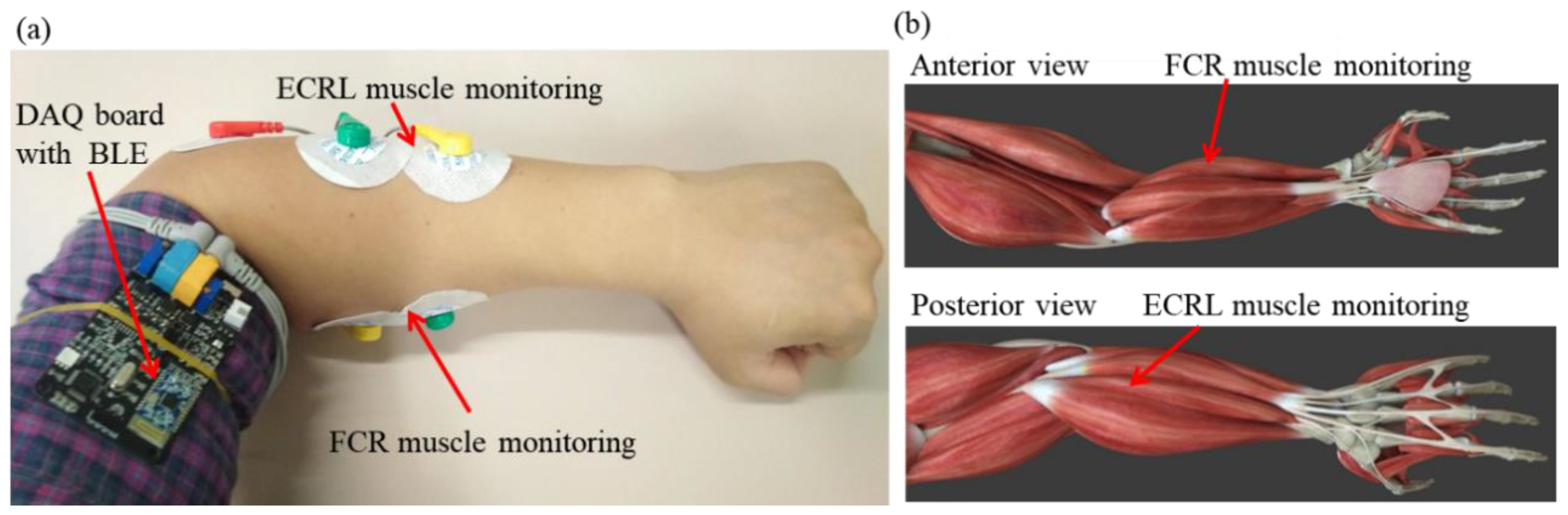
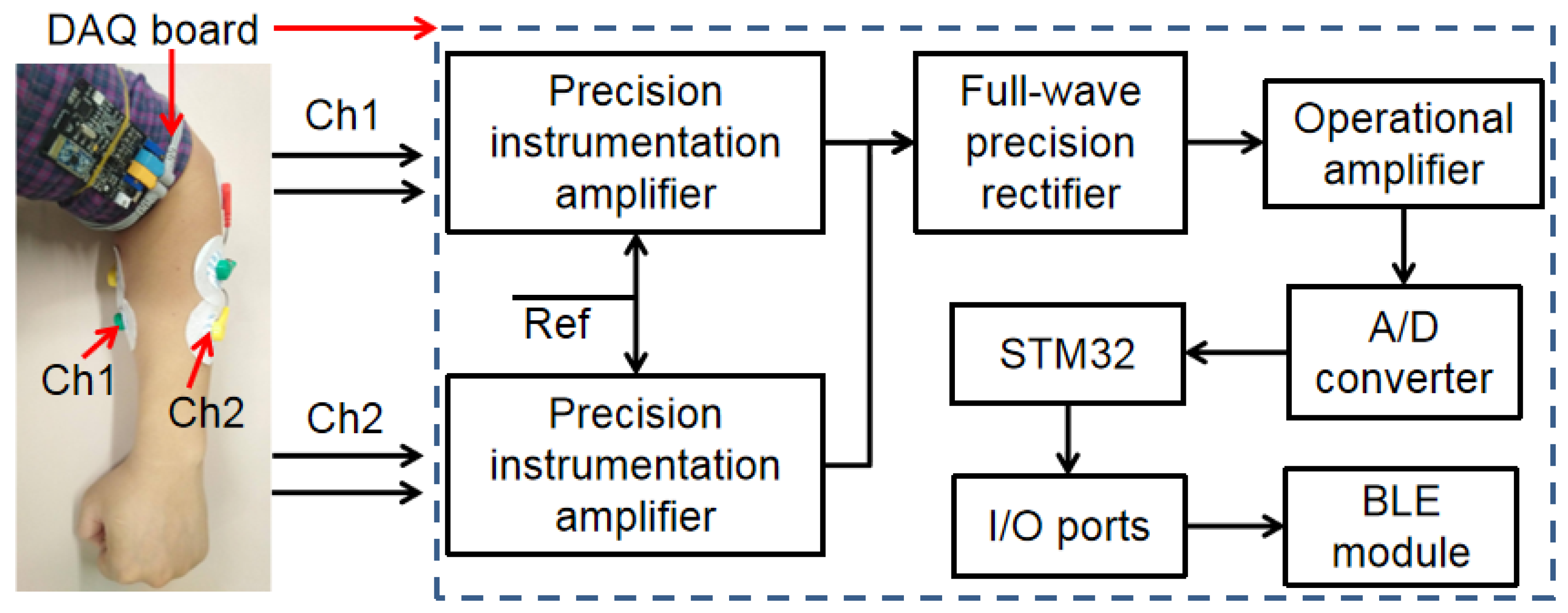
2.2. EMG System Design and Fabrication
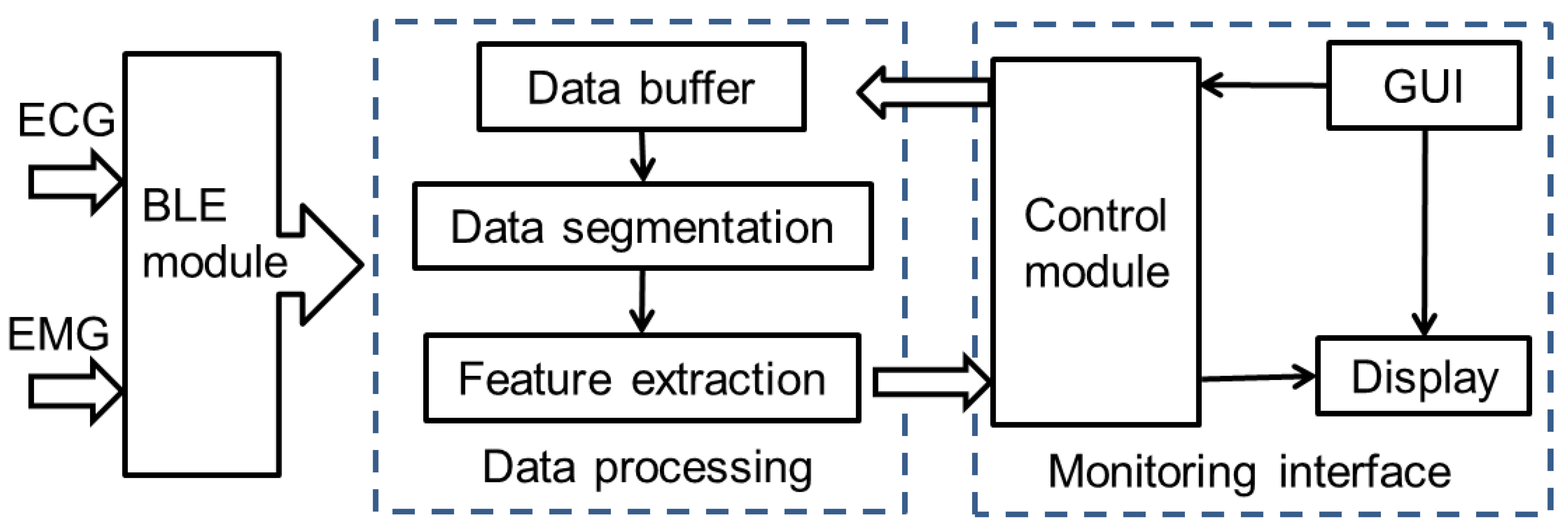
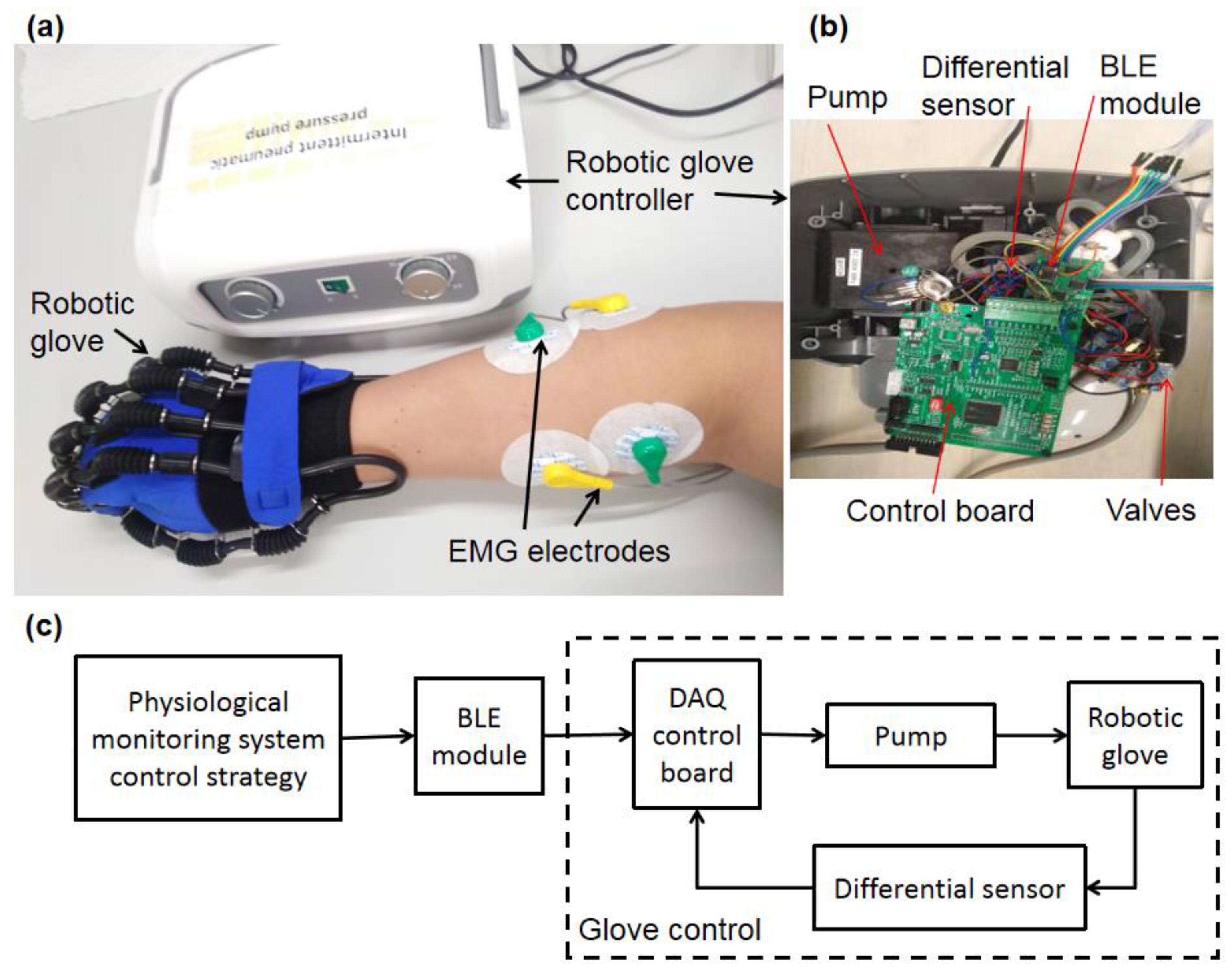
2.3. Physiological Monitoring System for Rehabilitation Training
3. Results and Discussion
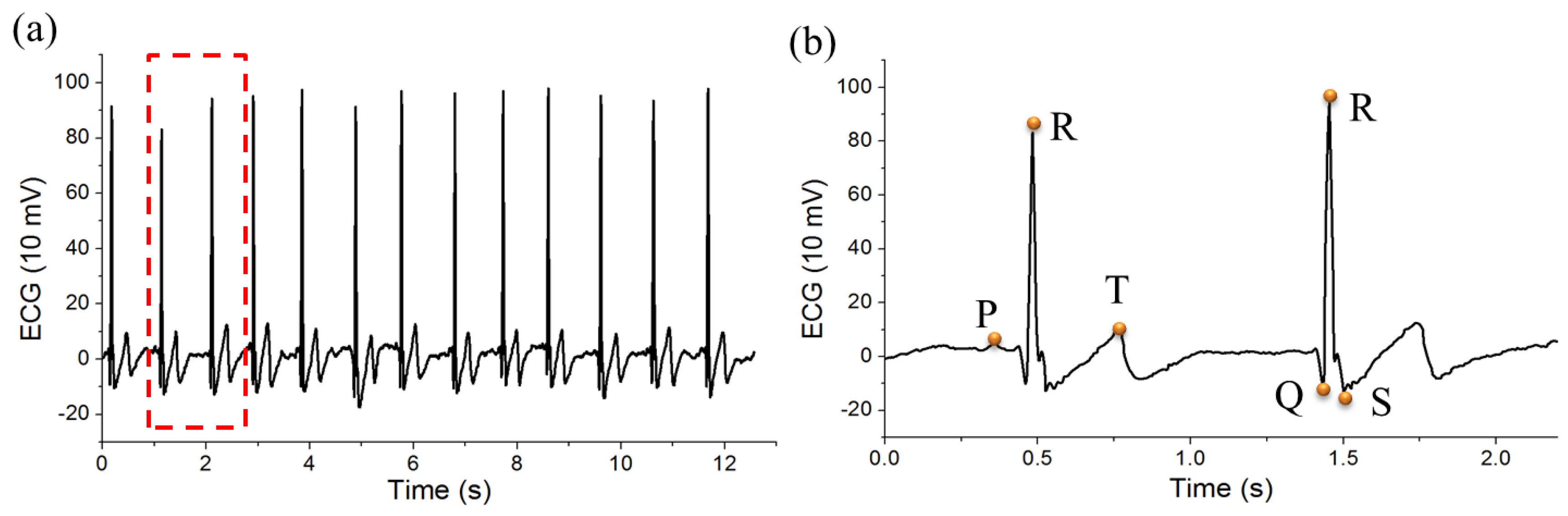
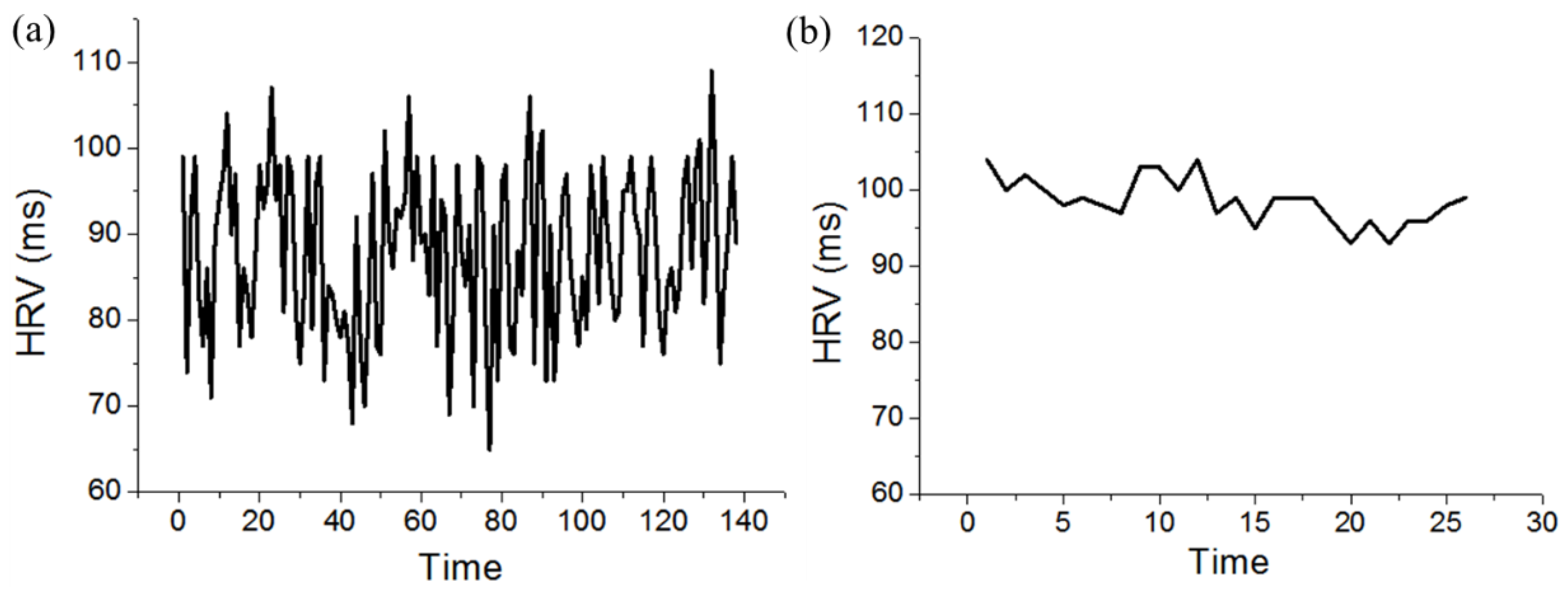
3.1. ECG Signal Processing
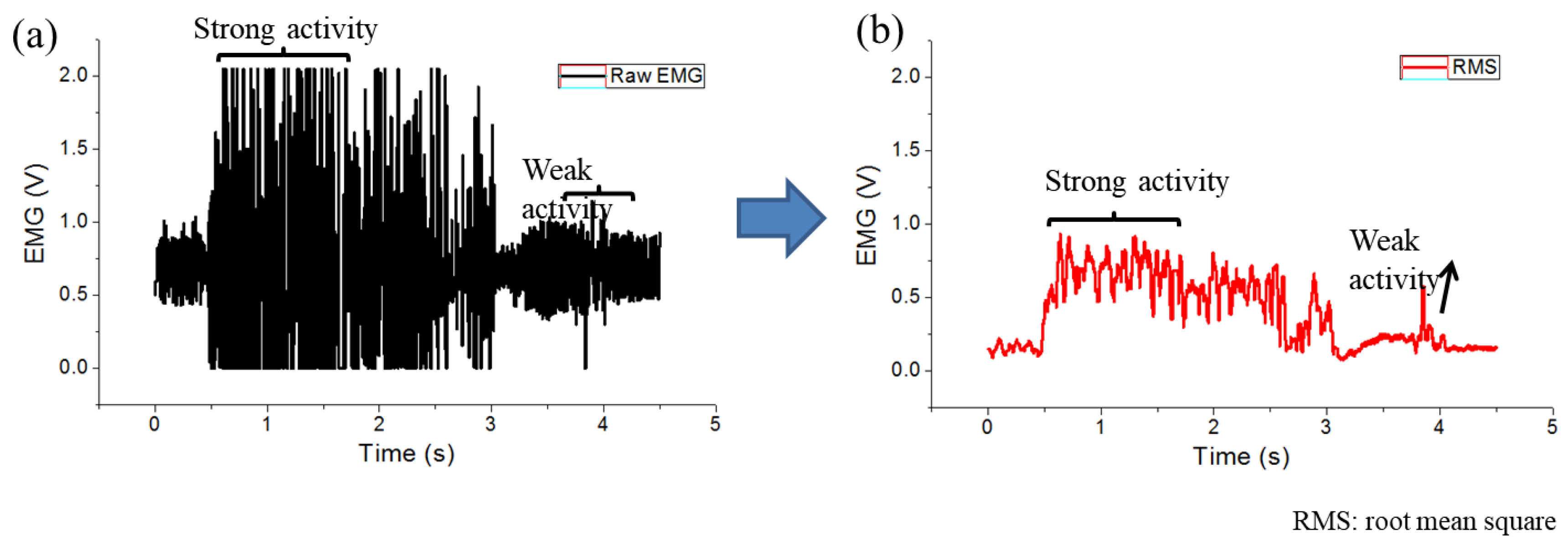
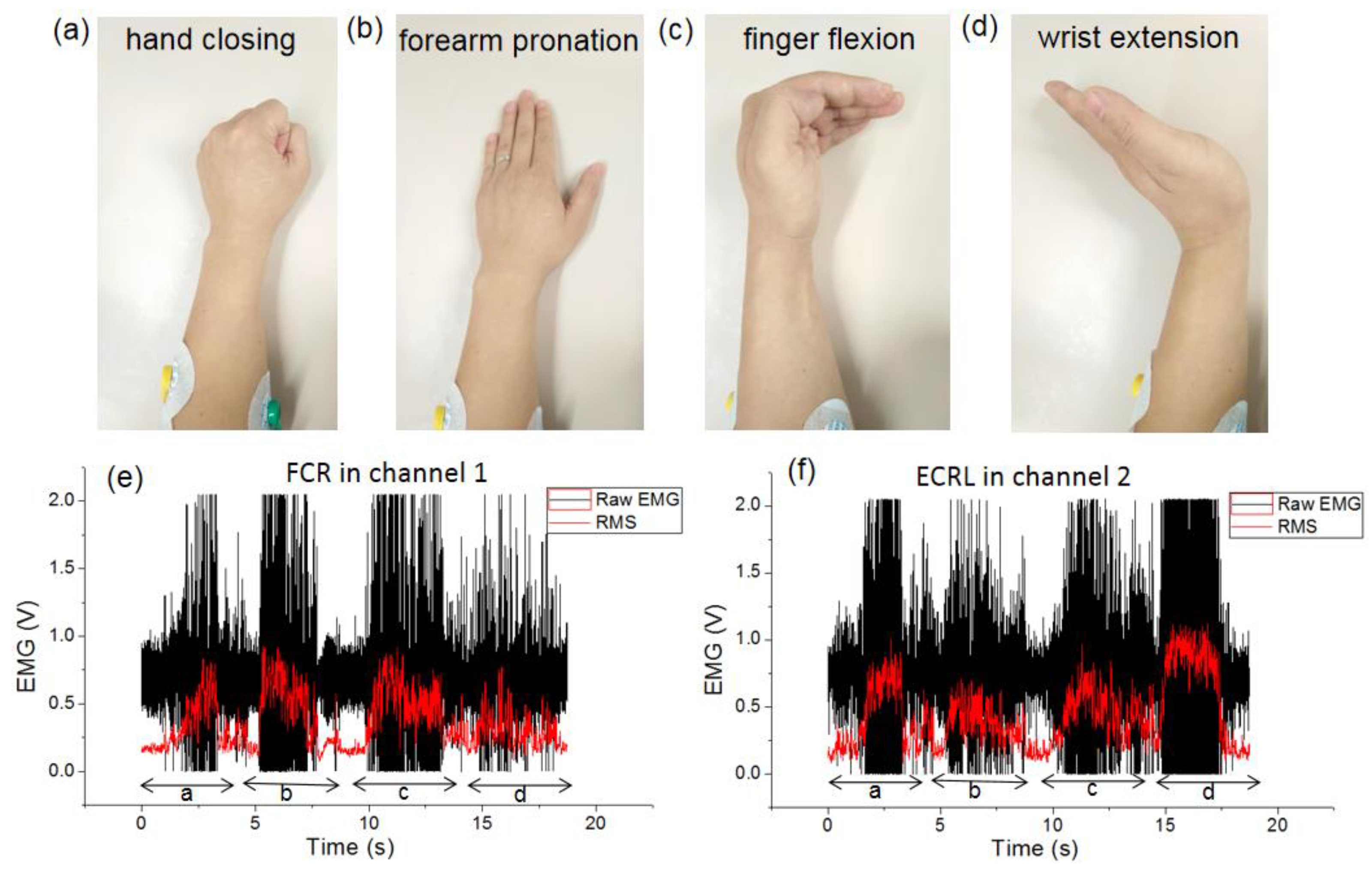
3.2. EMG Signal Processing
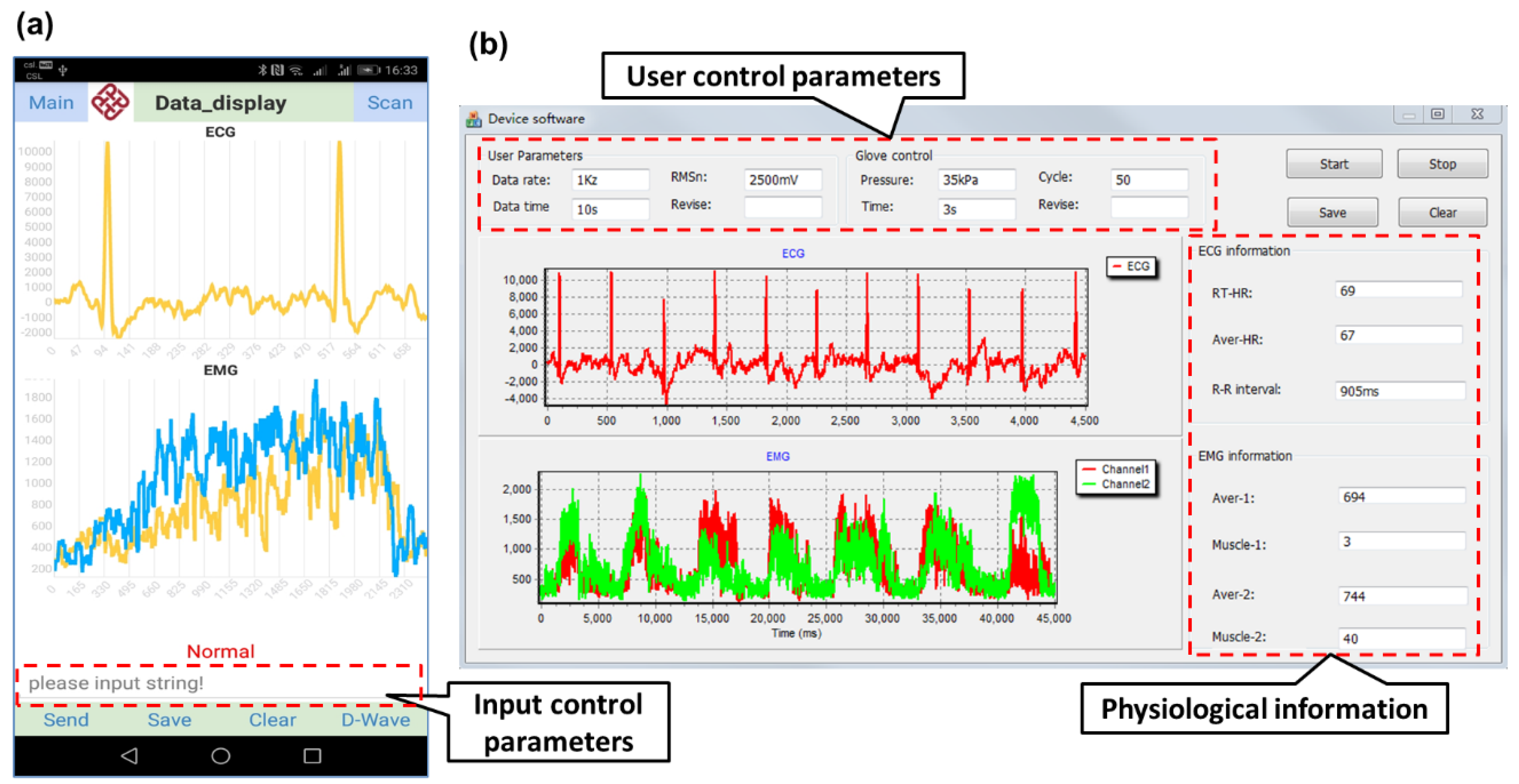
3.3. Physiological Monitoring System Interface
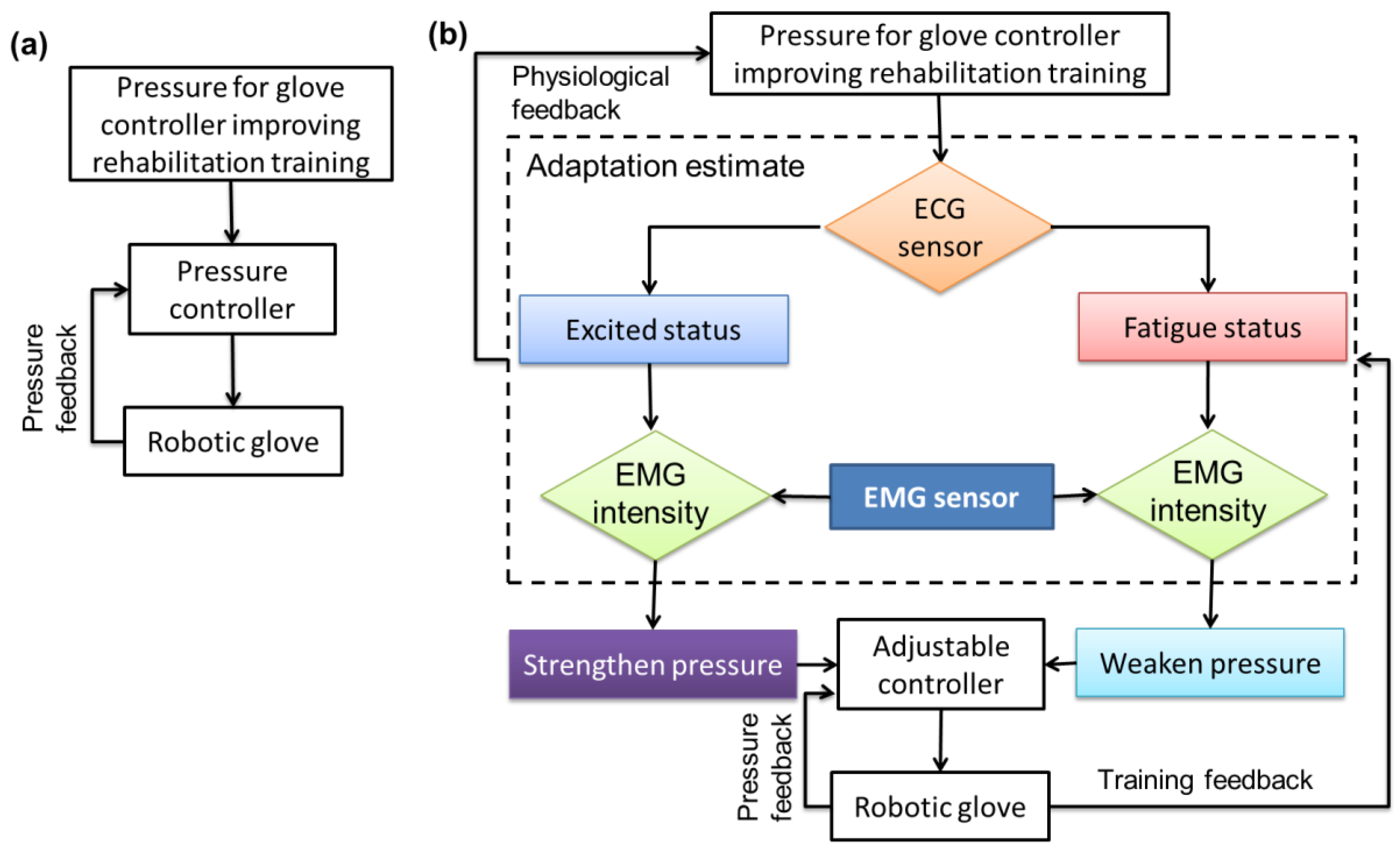
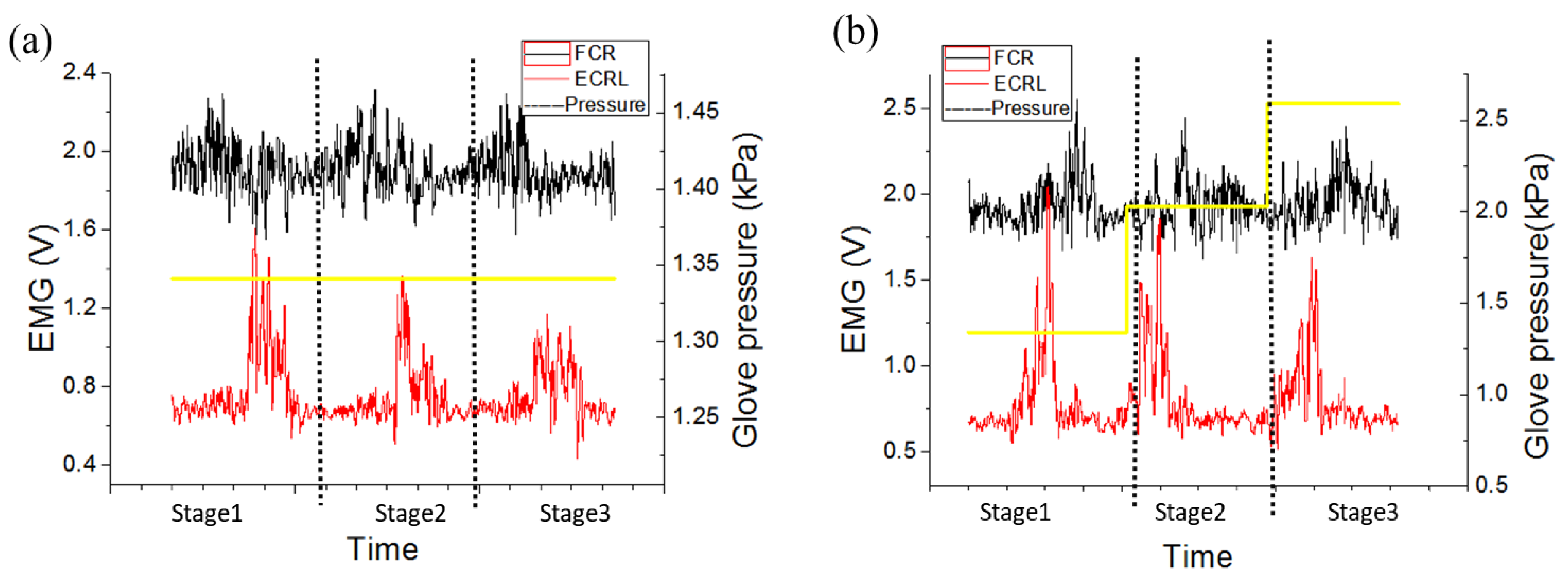
3.4. Upper Limb Rehabilitation Application
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Soh, P.J.; Vandenbosch, G.A.E.; Mercuri, M.; Schreurs, D.M.M.P. Wearable Wireless Health Monitoring: Current Developments, Challenges, and Future Trends. IEEE Microw. Mag. 2015, 16, 55–70. [Google Scholar] [CrossRef]
- Guk, K.; Han, G.; Lim, J.; Jeong, K.; Kang, T.; Lim, E.-K.; Jung, J. Evolution of Wearable Devices with Real-Time Disease Monitoring for Personalized Healthcare. Nanomaterials 2019, 9, 813. [Google Scholar] [CrossRef] [PubMed]
- Wearable Technology Applications in Healthcare: A Literature Review. Available online: https://www.himss.org/resources/wearable-technology-applications-healthcare-literature-review (accessed on 25 November 2019).
- Helbostad, J.; Vereijken, B.; Becker, C.; Todd, C.; Taraldsen, K.; Pijnappels, M.; Aminian, K.; Mellone, S. Mobile health applications to promote active and healthy ageing. Sensors 2017, 17, 622. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-W.; Yun, K.-S. ECG Monitoring Garment Using Conductive Carbon Paste for Reduced Motion Artifacts. Polymers 2017, 9, 439. [Google Scholar]
- Kim, J.; Campbell, A.S.; de Avila, B.E.; Wang, J. Wearable biosensors for healthcare monitoring. Nat. Biotechnol. 2019, 37, 389–406. [Google Scholar] [CrossRef]
- Reilly, R.B.; Lee, T.C. Electrograms (ECG, EEG, EMG, EOG). Technol. Health Care 2010, 18, 443–458. [Google Scholar] [CrossRef]
- Li, J.; Igbe, T.; Liu, Y.; Nie, Z.; Qin, W.; Wang, L.; Hao, Y. An Approach for Noninvasive Blood Glucose Monitoring Based on Bioimpedance Difference Considering Blood Volume Pulsation. IEEE Access 2018, 6, 51119–51129. [Google Scholar] [CrossRef]
- Jung, H.C.; Moon, J.H.; Baek, D.H.; Lee, J.H.; Choi, Y.Y.; Hong, J.S.; Lee, S.H. CNT/PDMS composite flexible dry electrodes for long-term ECG monitoring. IEEE Trans. Biomed. Eng. 2012, 59, 1472–1479. [Google Scholar] [CrossRef]
- Sun, F.; Yi, C.; Li, W.; Li, Y. A wearable H-shirt for exercise ECG monitoring and individual lactate threshold computing. Comput. Ind. 2017, 92, 1–11. [Google Scholar] [CrossRef]
- Li, W.; Zhang, H.; Wan, J.; Li, Y. A wearable exercise heart rate detection device based on single-arm ECG. In Proceedings of the International Conference on Biological Information and Biomedical Engineering (BIBE 2018), Shanghai, China, 6–8 June 2018; pp. 1–4. [Google Scholar]
- Lapkova, D.; Kralik, L.; Adámek, M. EMG analysis for basic self-defense techniques. In Computer Science On-Line Conference; Springer: Cham, Switzerland, 2016; pp. 353–362. [Google Scholar]
- Ali, A.A. EMG signals detection technique in voluntary muscle movement. In Proceedings of the 2012 6th International Conference on New Trends in Information Science, Service Science and Data Mining (ISSDM2012), Taipei, Taiwan, 23–25 October 2012; pp. 738–742. [Google Scholar]
- Zulkifli, A.; Ummu, J.K.; Aishah, A.F.Q.A.; Najeb, J.M. Development of wearable electromyogram (EMG) device for upper extremity in aerobic exercise. IOP Conf. Ser. Mater. Sci. Eng. 2019, 469, 012085. [Google Scholar] [CrossRef]
- Benatti, S.; Casamassima, F.; Milosevic, B.; Farella, E.; Schonle, P.; Fateh, S.; Burger, T.; Huang, Q.; Benini, L. A Versatile Embedded Platform for EMG Acquisition and Gesture Recognition. IEEE Trans. Biomed. Circuits Syst. 2015, 9, 620–630. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, A.; Nayak, S.K.; Pande, K.; Ray, S.S.; Pal, K.; Champaty, B.; Anis, A.; Tibarewala, D. Acquisition and classification of EMG using a dual-channel EMG biopotential amplifier for controlling assistive devices. In Proceedings of the 2016 IEEE Annual India Conference (INDICON), Bangalore, India, 16–18 December 2016; pp. 1–5. [Google Scholar]
- Al-Jumaily, A.; Olivares, R.A. Electromyogram (EMG) driven system based virtual reality for prosthetic and rehabilitation devices. In Proceedings of the 11th International Conference on Information Integration and Web-based Applications & Services, Kuala Lumpur, Malaysia, 14–16 December 2009; pp. 582–586. [Google Scholar]
- Nazmi, N.; Rahman, M.A.A.; Mazlan, S.A.; Zamzuri, H.; Mizukawa, M. Electromyography (EMG) based signal analysis for physiological device application in lower limb rehabilitation. In Proceedings of the 2015 2nd International Conference on Biomedical Engineering (ICoBE), Penang, Malaysia, 30–31 March 2015; pp. 1–6. [Google Scholar]
- Dobkin, B.H.; Dorsch, A. New evidence for therapies in stroke rehabilitation. Curr. Atheroscler. Rep. 2013, 15, 331. [Google Scholar] [CrossRef] [PubMed]
- Salbach, N.M.; Guilcher, S.J.; Jaglal, S.B.; Davis, D.A. Factors influencing information seeking by physical therapists providing stroke management. Phys. Ther. 2009, 89, 1039–1050. [Google Scholar] [CrossRef] [PubMed]
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Deruyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L. Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Martin, E.; Cazorla, M. Rehabilitation Technology: Assistance from Hospital to Home. Comput. Intell. Neurosci. 2019, 2019. [Google Scholar] [CrossRef]
- Takahashi, C.D.; Der-Yeghiaian, L.; Le, V.; Motiwala, R.R.; Cramer, S.C. Robot-based hand motor therapy after stroke. Brain 2008, 131, 425–437. [Google Scholar] [CrossRef]
- Lambercy, O.; Dovat, L.; Yun, H.; Wee, S.K.; Kuah, C.W.; Chua, K.S.; Gassert, R.; Milner, T.E.; Teo, C.L.; Burdet, E. Effects of a robot-assisted training of grasp and pronation/supination in chronic stroke: A pilot study. J. Neuroeng. Rehabil. 2011, 8, 63. [Google Scholar] [CrossRef]
- Hu, X.; Tong, K.; Wei, X.; Rong, W.; Susanto, E.; Ho, S. The effects of post-stroke upper-limb training with an electromyography (EMG)-driven hand robot. J. Electromyogr. Kinesiol. 2013, 23, 1065–1074. [Google Scholar] [CrossRef]
- Volpe, B.T.; Lynch, D.; Rykman-Berland, A.; Ferraro, M.; Galgano, M.; Hogan, N.; Krebs, H.I. Intensive sensorimotor arm training mediated by therapist or robot improves hemiparesis in patients with chronic stroke. Neurorehabilit. Neural Repair 2008, 22, 305–310. [Google Scholar] [CrossRef]
- Volpe, B.T.; Ferraro, M.; Lynch, D.; Christos, P.; Krol, J.; Trudell, C.; Krebs, H.I.; Hogan, N. Robotics and other devices in the treatment of patients recovering from stroke. Curr. Atheroscler. Rep. 2004, 6, 314–319. [Google Scholar] [CrossRef]
- Thakor, N.V.; Webster, J.G. Ground-free ECG recording with two electrodes. IEEE Trans. Biomed. Eng. 1980, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Javaid, A.Q.; Ashouri, H.; Dorier, A.; Etemadi, M.; Heller, J.A.; Roy, S.; Inan, O.T. Quantifying and reducing motion artifacts in wearable seismocardiogram measurements during walking to assess left ventricular health. IEEE Trans. Biomed. Eng. 2016, 64, 1277–1286. [Google Scholar] [CrossRef] [PubMed]
- Sung, M.; Jeong, K.; Cho, G. Suggestion for optimal location of textile-based ECG electrodes on an elastic shirts considering clothing pressure of the shirt. In Proceedings of the 2008 12th IEEE International Symposium on Wearable Computers, Pittsburgh, PA, USA, 28 September–1 October 2008; pp. 121–122. [Google Scholar]
- Retamosa, J.D.T.; Araujo, A.; Wawrzyniak, Z.M. Low power wearable device for elderly people monitoring. In Proceedings of the Photonics Applications in Astronomy, Communications, Industry, and High-Energy Physics Experiments 2018, Wilga, Poland, 3–10 June 2018. [Google Scholar]
- Liu, J.; Zhou, Y. Design of a novel portable ECG monitor for heart health. In Proceedings of the 2013 Sixth International Symposium on Computational Intelligence and Design, Hangzhou, China, 28–29 October 2013; pp. 257–260. [Google Scholar]
- Tosi, J.; Taffoni, F.; Santacatterina, M.; Sannino, R.; Formica, D. Performance evaluation of Bluetooth low energy: A systematic review. Sensors 2017, 17, 2898. [Google Scholar] [CrossRef] [PubMed]
- Song, W.; Yu, H.; Liang, C.; Wang, Q.; Shi, Y. Body monitoring system design based on android smartphone. In Proceedings of the 2012 World Congress on Information and Communication Technologies, Trivandrum, India, 30 October–2 November 2012; pp. 1147–1151. [Google Scholar]
- Ai, Z.; Zheng, L.; Qi, H.; Cui, W. Low-Power Wireless Wearable ECG Monitoring System Based on BMD101. In Proceedings of the 2018 37th Chinese Control Conference (CCC), Wuhan, China, 25–27 July 2018; pp. 7374–7379. [Google Scholar]
- Wang, J.-S.; Zhang, Y.; Zhang, P.; Sun, S.-F. Research on denoising algorithm for ECG signals. In Proceedings of the 29th Chinese Control Conference, Beijing, China, 29–31 July 2010; pp. 2936–2940. [Google Scholar]
- Imtiaz, U.; Bartolomeo, L.; Lin, Z.; Sessa, S.; Ishii, H.; Saito, K.; Zecca, M.; Takanishi, A. Design of a wireless miniature low cost EMG sensor using gold plated dry electrodes for biomechanics research. In Proceedings of the 2013 IEEE International Conference on Mechatronics and Automation, Takamatsu, Japan, 4–7 August 2013; pp. 957–962. [Google Scholar]
- Perotto, A.O. Anatomical Guide for the Electromyographer: The Limbs and Trunk, 5th ed.; Charles C Thomas Publisher: Springfield, IL, USA, 2011. [Google Scholar]
- Choi, C.; Kim, J. A real-time EMG-based assistive computer interface for the upper limb disabled. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 459–462. [Google Scholar]
- Weiss, L.D.; Weiss, J.M.; Silver, J.K. Easy EMG E-Book: A Guide to Performing Nerve Conduction Studies and Electromyography, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Webster, J.G. Reducing motion artifacts and interference in biopotential recording. IEEE Trans. Biomed. Eng. 1984, 823–826. [Google Scholar] [CrossRef] [PubMed]
- Searle, A.; Kirkup, L. A direct comparison of wet, dry and insulating bioelectric recording electrodes. Physiol. Meas. 2000, 21, 271. [Google Scholar] [CrossRef]
- A designer’s Guide to Instrumentation Amplifiers. Available online: https://d1.amobbs.com/bbs_upload782111/files_3/armok0169547.pdf (accessed on 28 August 2020).
- Important Factors in Surface EMG Measurement. Available online: https://pdfs.semanticscholar.org/33f2/f59c47d28387533208284d1991e12fed18bd.pdf (accessed on 28 August 2020).
- Rainoldi, A.; Melchiorri, G.; Caruso, I. A method for positioning electrodes during surface EMG recordings in lower limb muscles. J. Neurosci. Methods 2004, 134, 37–43. [Google Scholar] [CrossRef]
- Kugelstadt, T. Getting the most out of your instrumentation amplifier design. SAT 2005, 1, 2. [Google Scholar]
- Saad, I.; Bais, N.H.; Bolong, N. Electromyogram (emg) signal processing analysis for clinical rehabilitation application. In Proceedings of the 2015 3rd International Conference on Artificial Intelligence, Modelling and Simulation (AIMS), Kota Kinabalu, Malaysia, 2–4 December 2015; pp. 105–110. [Google Scholar]
- Reaz, M.B.I.; Hussain, M.S.; Mohd-Yasin, F. Techniques of EMG signal analysis: Detection, processing, classification and applications. Biol. Proced. Online 2006, 8, 11–35. [Google Scholar] [CrossRef]
- Polygerinos, P.; Galloway, K.C.; Savage, E.; Herman, M.; O’Donnell, K.; Walsh, C.J. Soft robotic glove for hand rehabilitation and task specific training. In Proceedings of the 2015 IEEE international conference on robotics and automation (ICRA), Seattle, WA, USA, 26–30 May 2015; pp. 2913–2919. [Google Scholar]
- Chu, C.Y.; Patterson, R.M. Soft robotic devices for hand rehabilitation and assistance: A narrative review. J. Neuroeng. Rehabil. 2018, 15, 9. [Google Scholar] [CrossRef]
- Wang, L.; Li, H.; Wang, Z.; Meng, F. Study on upper limb rehabilitation system based on surface EMG. Biomed. Mater. Eng. 2015, 26, S795–S801. [Google Scholar] [CrossRef]
- Qin, J.; Li, C.; Chen, Z.; Jia, J. 3 DOF upper limb rehabilitation robot-assisted training system. In Proceedings of the 2014 International Conference on Mechatronics, Electronic, Industrial and Control Engineering (MEIC-14), Shenyang, China, 15–17 November 2014. [Google Scholar]
- Deepu, C.J.; Zhang, X.; Wong, D.; Lian, Y. An ECG-on-chip with joint QRS detection & data compression for wearable sensors. In Proceedings of the 2016 IEEE International Symposium on Circuits and Systems (ISCAS), Montreal, QC, Canada, 22–25 May 2016; p. 2908. [Google Scholar]
- Strasser, F.; Muma, M.; Zoubir, A.M. Motion artifact removal in ECG signals using multi-resolution thresholding. In Proceedings of the 2012 Proceedings of the 20th European Signal Processing Conference (EUSIPCO), Bucharest, Romania, 27–31 August 2012; pp. 899–903. [Google Scholar]
- Liu, S.-H. Motion artifact reduction in electrocardiogram using adaptive filter. J. Med. Biol. Eng. 2011, 31, 67–72. [Google Scholar] [CrossRef]
- Chatterjee, S.; Changawala, N. Fragmented QRS complex: A novel marker of cardiovascular disease. Clin. Cardiol. 2010, 33, 68–71. [Google Scholar] [CrossRef] [PubMed]
- Kashani, A.; Barold, S.S. Significance of QRS complex duration in patients with heart failure. J. Am. Coll. Cardiol. 2005, 46, 2183–2192. [Google Scholar] [CrossRef] [PubMed]
- Bornas, X.; Llabrés, J.; Noguera, M.; López, A.M.; Barceló, F.; Tortella-Feliu, M.; Fullana, M.À. Self-implication and heart rate variability during simulated exposure to flight-related stimuli. Anxiety Stress Coping 2004, 17, 331–339. [Google Scholar] [CrossRef]
- Choi, U.S.; Kim, K.-J.; Lee, S.-S.; Kim, K.-S.; Kim, J. A Simple Fatigue Condition Detection Method by Using Heart Rate Variability Analysis; Springer: Singapore, 2016; pp. 203–208. [Google Scholar]
- Kurian, D.; Joseph, J.; Radhakrishnan, K.; Balakrishnan, A.A. Drowsiness Detection Using Photoplethysmography Signal. In Proceedings of the 2014 Fourth International Conference on Advances in Computing and Communications, Kochi, India, 27–29 August 2014. [Google Scholar] [CrossRef]
- Lin, Y.-H.; Lin, C.-F.; You, H.-Z. A driver’s physiological monitoring system based on a wearable PPG sensor and a smartphone. In International Conference on Security-Enriched Urban Computing and Smart Grid; Springer: Berlin/Heidelberg, Germany, 2011; pp. 326–335. [Google Scholar]
- Asl, B.M.; Setarehdan, S.K.; Mohebbi, M. Support vector machine-based arrhythmia classification using reduced features of heart rate variability signal. Artif. Intell. Med. 2008, 44, 51–64. [Google Scholar] [CrossRef]
- Kampouraki, A.; Manis, G.; Nikou, C. Heartbeat time series classification with support vector machines. IEEE Trans. Inf. Technol. Biomed. 2008, 13, 512–518. [Google Scholar] [CrossRef]
- Raut, R.; Gurjar, A. Bio-medical (EMG) Signal Analysis and Feature Extraction Using Wavelet Transform. Int. J. Eng. Res. Appl. 2015, 5, 17–19. [Google Scholar]
- Mahaphonchaikul, K.; Sueaseenak, D.; Pintavirooj, C.; Sangworasil, M.; Tungjitkusolmun, S. EMG signal feature extraction based on wavelet transform. In Proceedings of the The 2010 ECTI International Confernce on Electrical Engineering/Electronics, Computer, Telecommunications and Information Technology (ECTI-CON2010), Chiang Mai, Thailand, 19–21 May 2010; pp. 327–331. [Google Scholar]
- Zhao, S.; Liu, R.; Fei, C.; Guan, D. Dynamic Interface Pressure Monitoring System for the Morphological Pressure Mapping of Intermittent Pneumatic Compression Therapy. Sensors 2019, 19, 2881. [Google Scholar] [CrossRef]
- Octavia, J.R.; Coninx, K. Adaptive personalized training games for individual and collaborative rehabilitation of people with multiple sclerosis. BioMed Res. Int. 2014, 2014. [Google Scholar] [CrossRef]
- Wen, Y.; Liu, M.; Si, J.; Huang, H.H. Adaptive control of powered transfemoral prostheses based on adaptive dynamic programming. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 5071–5074. [Google Scholar]
- Weinberg, B.; Nikitczuk, J.; Patel, S.; Patritti, B.; Mavroidis, C.; Bonato, P.; Canavan, P. Design, control and human testing of an active knee rehabilitation orthotic device. In Proceedings of the 2007 IEEE International Conference on Robotics and Automation, Roma, Italy, 10–14 April 2007; pp. 4126–4133. [Google Scholar]
- Dong, S.; Lu, K.-Q.; Sun, J.Q.; Rudolph, K. Adaptive force regulation of muscle strengthening rehabilitation device with magnetorheological fluids. IEEE Trans. Neural Syst. Rehabil. Eng. 2006, 14, 55–63. [Google Scholar] [CrossRef]
- Nur, N.M.; Dawal, S.Z.M.; Dahari, M.; Sanusi, J. Muscle activity, time to fatigue, and maximum task duration at different levels of production standard time. J. Phys. Ther. Sci. 2015, 27, 2323–2326. [Google Scholar] [CrossRef] [PubMed]
- Fu, R.; Wang, H. Detection of driving fatigue by using noncontact EMG and ECG signals measurement system. Int. J. Neural. Syst. 2014, 24, 1450006. [Google Scholar] [CrossRef] [PubMed]
- Turner, D.L.; Murguialday, A.R.; Birbaumer, N.; Hoffmann, U.; Luft, A. Neurophysiology of robot-mediated training and therapy: A perspective for future use in clinical populations. Front. Neurol. 2013, 4, 184. [Google Scholar] [CrossRef] [PubMed]
| Time Interval | Excited Status | Fatigue Status | ||||
|---|---|---|---|---|---|---|
| ECRL (RMS) | FCR (RMS) | ECG (HRV) | ECRL (RMS) | FCR (RMS) | ECG (HRV) | |
| 1st min | 2.0 ± 0.4 V | 1.6 ± 0.4 V | 101 ms | 1.8 ± 0.3 V | 1.5 ± 0.3 V | 96 ms |
| 30th min | 1.8 ± 0.3 V | 1.5 ± 0.4 V | 80 ms | 1.5 ± 0.2 V | 1.4 ± 0.2 V | 99 ms |
| 60th min | 1.6 ± 0.4 V | 1.5 ± 0.3 V | 113 ms | 1.3 ± 0.3 V | 1.5 ± 0.2 V | 98 ms |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, S.; Liu, J.; Gong, Z.; Lei, Y.; OuYang, X.; Chan, C.C.; Ruan, S. Wearable Physiological Monitoring System Based on Electrocardiography and Electromyography for Upper Limb Rehabilitation Training. Sensors 2020, 20, 4861. https://doi.org/10.3390/s20174861
Zhao S, Liu J, Gong Z, Lei Y, OuYang X, Chan CC, Ruan S. Wearable Physiological Monitoring System Based on Electrocardiography and Electromyography for Upper Limb Rehabilitation Training. Sensors. 2020; 20(17):4861. https://doi.org/10.3390/s20174861
Chicago/Turabian StyleZhao, Shumi, Jianxun Liu, Zidan Gong, Yisong Lei, Xia OuYang, Chi Chiu Chan, and Shuangchen Ruan. 2020. "Wearable Physiological Monitoring System Based on Electrocardiography and Electromyography for Upper Limb Rehabilitation Training" Sensors 20, no. 17: 4861. https://doi.org/10.3390/s20174861
APA StyleZhao, S., Liu, J., Gong, Z., Lei, Y., OuYang, X., Chan, C. C., & Ruan, S. (2020). Wearable Physiological Monitoring System Based on Electrocardiography and Electromyography for Upper Limb Rehabilitation Training. Sensors, 20(17), 4861. https://doi.org/10.3390/s20174861






