The Role of Bedroom Privacy in Social Interaction among Elderly Residents in Nursing Homes: An Exploratory Case Study of Hong Kong
Abstract
1. Introduction
1.1. Privacy in Hong Kong Nursing Homes
1.2. Measuring Social Interaction
1.3. Theoretical Framework
1.4. Monitoring of Social Behaviour
1.5. Impact of Physical Environment on Social Interaction
1.6. Analysis of Social Interaction
- What are the mobility patterns among the elderly participants and to what extent are the different levels of privacy reflected by these patterns?
- What are the social behavioural patterns among the elderly participants and to what extent are they associated with the different privacy levels in shared bedrooms?
2. Materials and Methods
2.1. Location Data
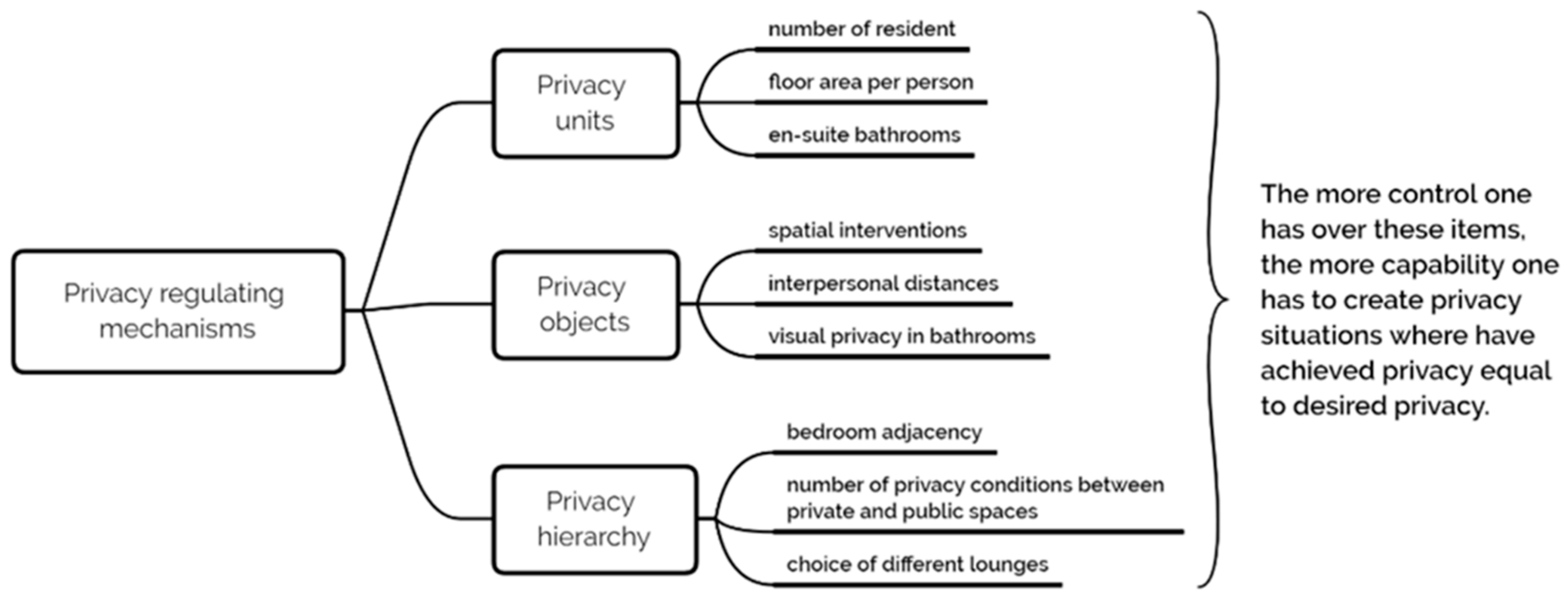
2.2. Assessing Privacy and Topology in Shared Rooms
2.3. Tracking Social Interaction and Behaviour
3. Results
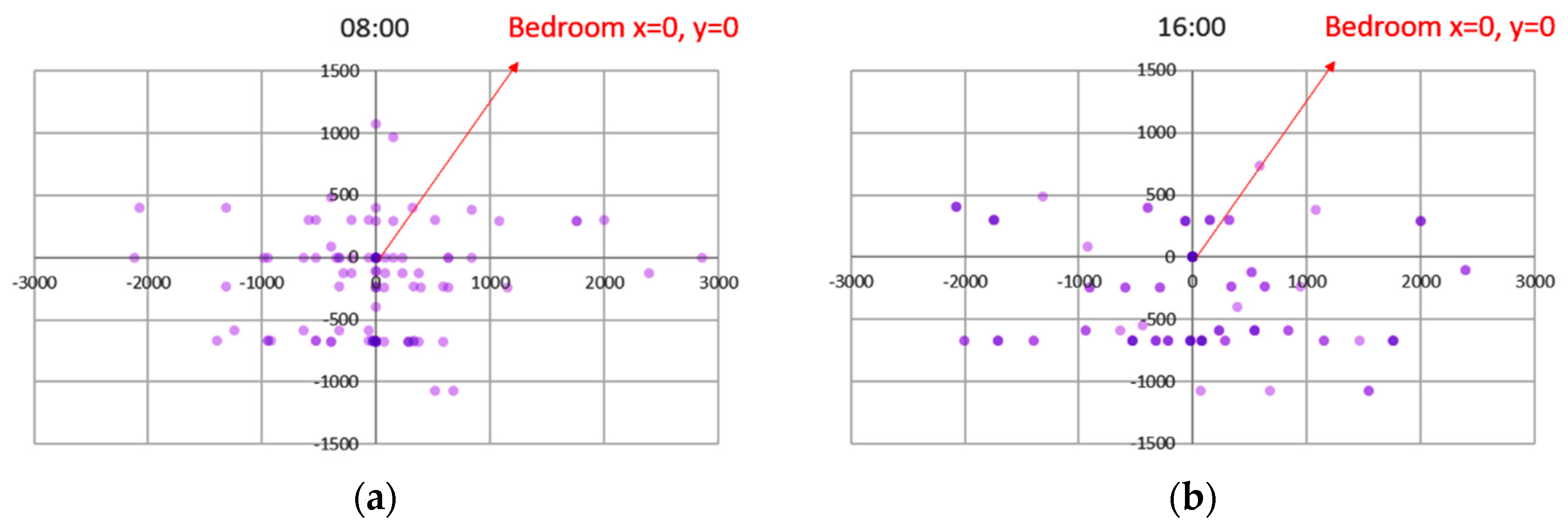
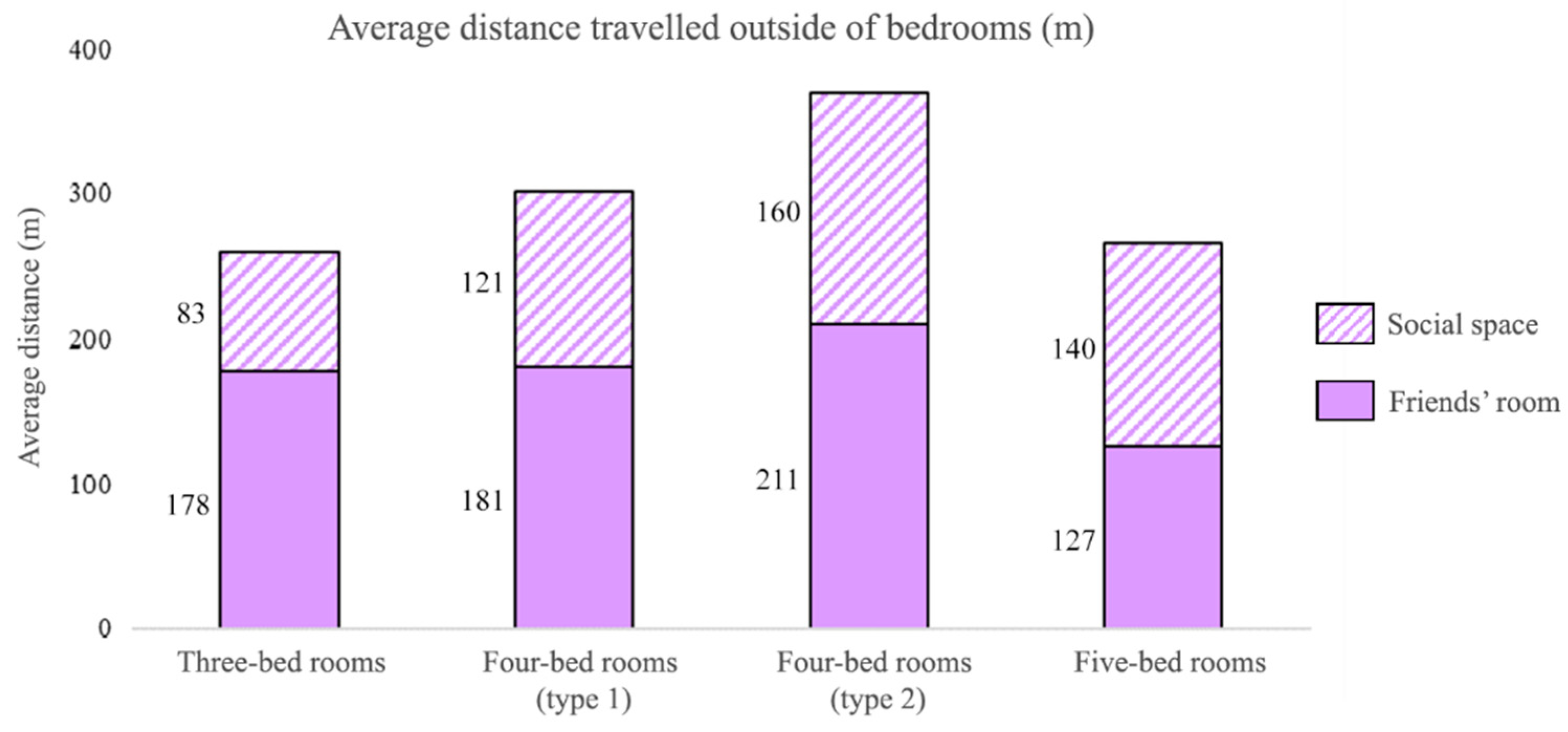
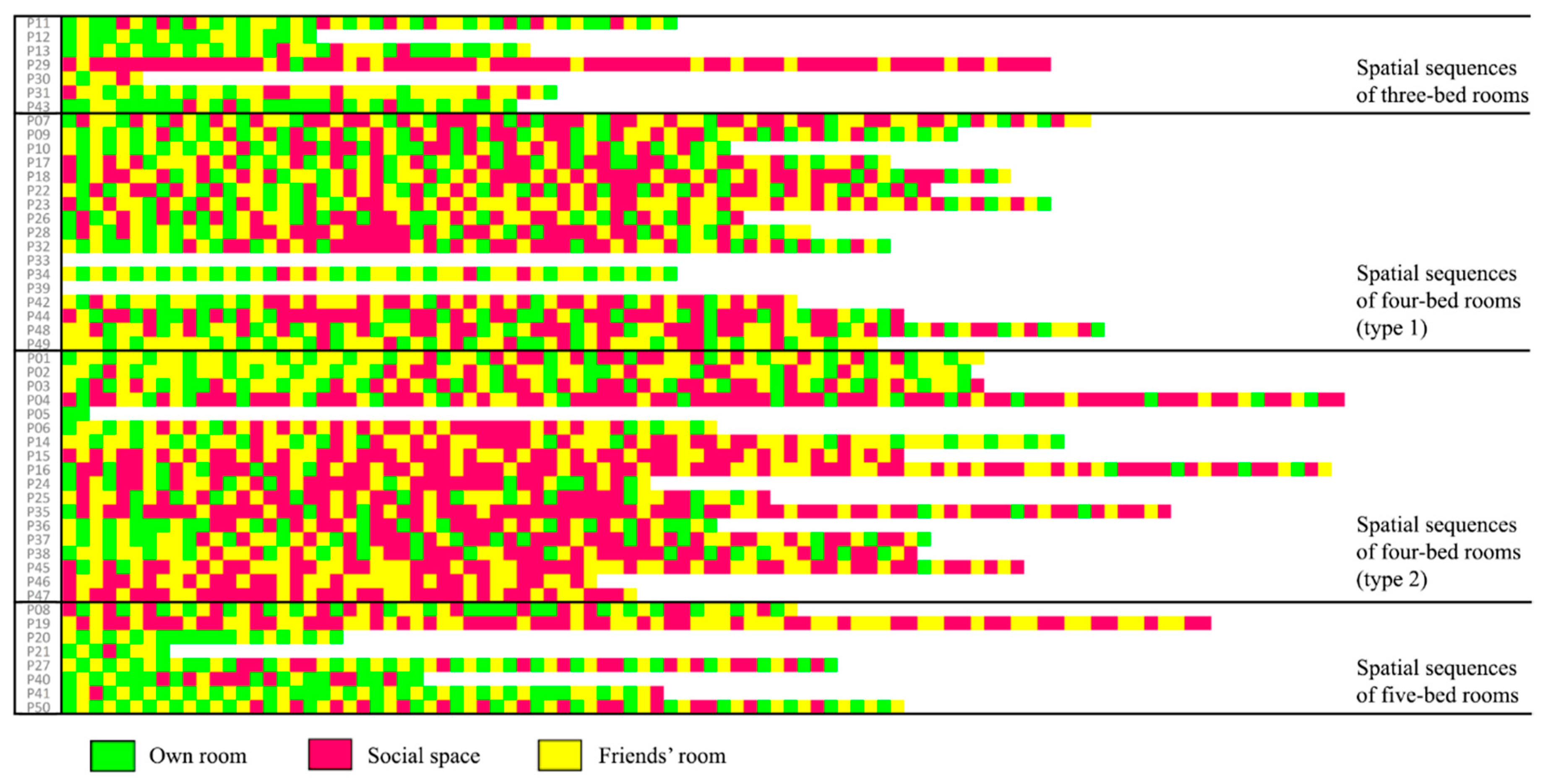
3.1. Mobility Patterns
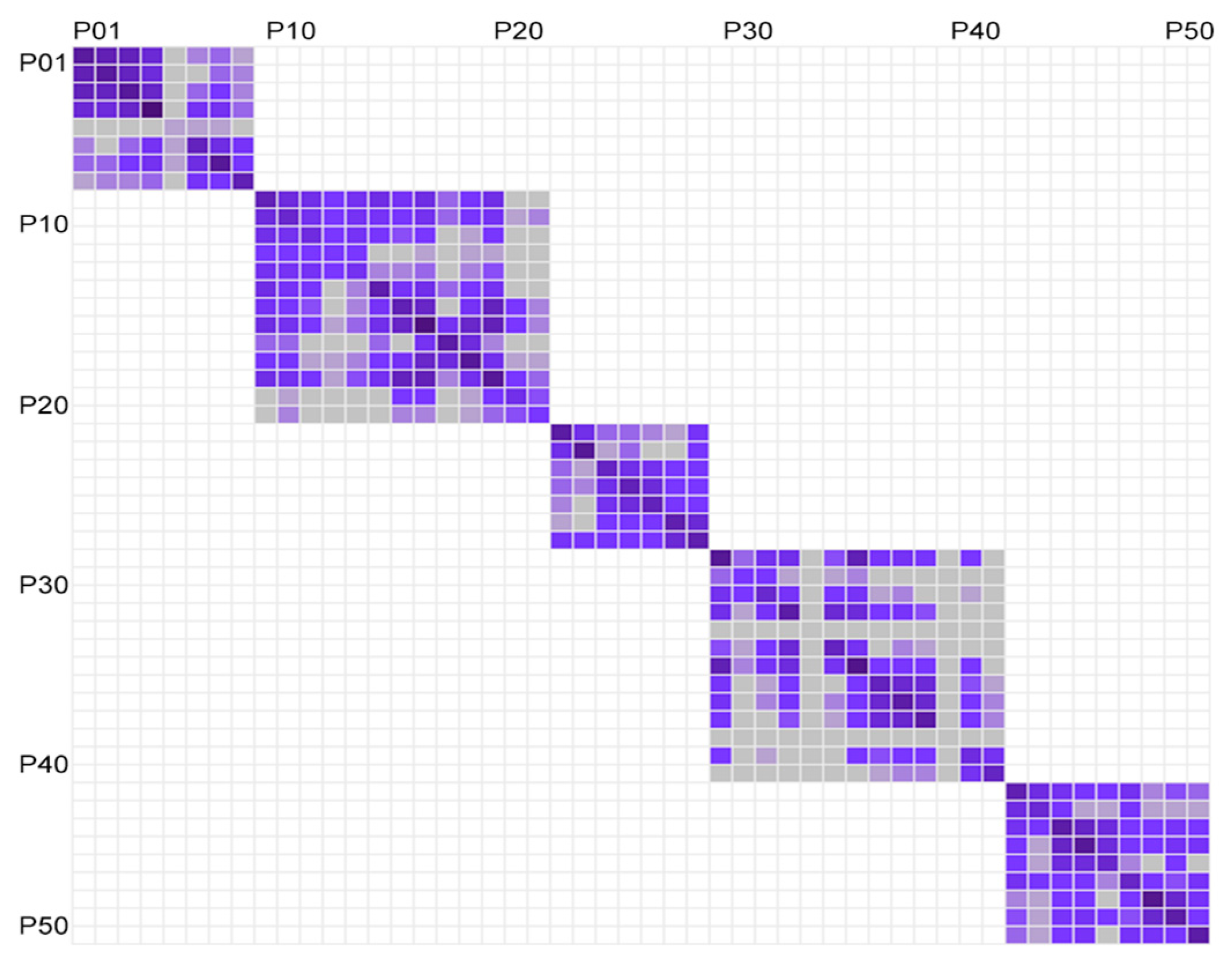
3.2. Social Behavioural Patterns
4. Discussion
4.1. Theoretical Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Brod, M.; Stewart, A.L.; Sands, L.; Walton, P. Conceptualization and Measurement of Quality of Life in Dementia: The Dementia Quality of Life Instrument (DQoL). Gerontologist 1999, 39, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Kitwood, T.; Bredin, K. Towards a Theory of Dementia Care: Personhood and Well-Being. Ageing Soc. 1992, 12, 269–287. [Google Scholar] [CrossRef]
- Campo, M.; Chaudhury, H. Informal Social Interaction among Residents with Dementia in Special Care Units: Exploring the Role of the Physical and Social Environments. Dementia 2012, 11, 401–423. [Google Scholar] [CrossRef]
- Capitman, J.; Leutz, W.; Bishop, C.; Casler, R. Long-Term Care Quality: Historical Overview and Current Initiatives; Schneider Institute for Health Policy, Heller School for Social Policy and Management, Brandeis University: Waltham, MA, USA, 2005; 47p. [Google Scholar]
- Sloane, P.; Zimmerman, S. Improvement and Innovation in Long-Term Care: A Research Agenda—Report and Recommendations from a National Consensus Conference; Cecil, G., Ed.; Sheps Center for Health Services Research, University of North Carolina at Chapel Hill: Chapel Hill, NC, USA, 2005. [Google Scholar]
- Chaudhury, H.; Mahmood, A.; Valente, M. Advantages and Disadvantages of Single-Versus Multiple-Occupancy Rooms in Acute Care Environments: A Review and Analysis of the Literature. Environ. Behav. 2005, 37, 760–786. [Google Scholar] [CrossRef]
- Calkins, M.; Cassella, C. Exploring the Cost and Value of Private versus Shared Bedrooms in Nursing Homes. Gerontologist 2007, 47, 169–183. [Google Scholar] [CrossRef] [PubMed]
- Kahn, D.L. Living in a Nursing Home: Experiences of Suffering and Meaning in Old Age. Ph.D. Thesis, University of Washington, Seattle, WA, USA, 1991. [Google Scholar]
- Townend, P. The Last Refuge a Survey of Residential Institutions and Homes for the Aged in England and Wales; Routledge: London, UK, 1962. [Google Scholar] [CrossRef]
- Lawton, M.P.; Bader, J. Wish for Privacy by Young and Old. J. Gerontol. 1970, 25, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Willcocks, D.; Peace, S.; Kellaher, L. Private Lives in Public Places; Routledge: Abingdon, UK, 1987. [Google Scholar] [CrossRef]
- Kane, R.; Kane, R.A. What Older People Want from Long-Term Care, and How They Can Get It. Health Aff. 2001, 20, 114–127. [Google Scholar] [CrossRef] [PubMed]
- Census and Statistics Department. Hong Kong Population Projections for 2017 to 2066. Available online: https://www.censtatd.gov.hk/media_workers_corner/pc_rm/hkpp2017_2066/index.jsp (accessed on 21 July 2020).
- Chiu, P. Hong Kong’s Cramped Care Homes Could Get Bigger—But No Time Soon. Available online: https://www.scmp.com/news/hong-kong/society/article/2189379/change-could-be-way-hong-kongs-cramped-care-homes-no-time (accessed on 21 July 2020).
- Available online: http://www.hkag.org/rpl/PDF/ECS%20SCS%201st%20version%202014_12_chi_ALL.pdf (accessed on 23 July 2020). [Chinese Version Only].
- Tse, M.M.Y. Nursing Home Placement: Perspectives of Community-Dwelling Older Persons. J. Clin. Nurs. 2007, 16, 911–917. [Google Scholar] [CrossRef]
- Yeung, J.W.K.; Ching, K.Y.L.; Chung, A. Correlates and Prevalence of Depression in Chinese Residents of Nursing Homes in Hong Kong and Implications for Services and Intervention Policies. Annu. Soc. Work 2010, 17, 445–460. [Google Scholar]
- Lee, D.T.F. Perceptions of Hong Kong Chinese Elders on Adjustment to Residential Care. J. Interprof. Care 2001, 15, 235–244. [Google Scholar] [CrossRef]
- Kane, R.A.; Baker, M.O.; Salmon, J.; Veazie, W. Consumer Perspectives on Private versus Shared Accommodations in Assisted Living Settings; American Association of Retired Persons: Washington, DC, USA, 1998; 65p. [Google Scholar]
- Ulrich, R.; Quan, X.; Zimring, C.; Joseph, A.; Choudbary, R. The Role of the Physical Environment in the Hospital of the 21st Century: A Once-in-a-Lifetime Opportunity; The Center for Health Design: Concord, CA, USA, 2004; 69p. [Google Scholar]
- Low, L.P.L.; Lee, D.T.F.; Chan, A.W.Y. An Exploratory Study of Chinese Older People’s Perceptions of Privacy in Residential Care Homes. J. Adv. Nurs. 2007, 57, 605–613. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.T.; Yu, D.S.; Kwong, A.N. Quality of Life of Older People in Residential Care Home: A Literature Review. J. Nurs. Healthc. Chronic Illn. 2009, 1, 116–125. [Google Scholar] [CrossRef]
- Terakawa, Y. The Relationship between Environment and Behavior at the Institutional Setting for the Elderly. In Proceedings of the 35th Annual Conference of the Environmental Design Research Association, Albuquerque, NM, USA, 2–6 June 2004. [Google Scholar]
- Whyte, W.F. Street Corner Society: The Social Structure of an Italian Slum; University of Chicago Press: Chicago, IL, USA, 2012. [Google Scholar]
- Bradburn, N.M.; Sudman, S.; Blair, E.; Stocking, C. Question Threat and Response Bias. Public Opin. Q. 1978, 42, 221–234. [Google Scholar] [CrossRef]
- Fernández-Llatas, C.; Benedi, J.-M.; García-Gómez, J.M.; Traver, V. Process Mining for Individualized Behavior Modeling Using Wireless Tracking in Nursing Homes. Sensors 2013, 13, 15434–15451. [Google Scholar] [CrossRef] [PubMed]
- Altman, I. The Environment and Social Behavior: Privacy, Personal Space, Territory, and Crowding; Brooks/Cole Publishing Company: Monterey, CA, USA, 1975. [Google Scholar]
- Westin, A.F. Privacy and Freedom; Atheneum: New York, NY, USA, 1967. [Google Scholar]
- Proshansky, H.M.; Ittelson, W.H.; Rivlin, L.G. Environmental Psychology: Man and His Physical Setting; Holt, Rinehart & Winston: Oxford, UK, 1970; 690p. [Google Scholar]
- Bates, A.P. Privacy—A Useful Concept? Soc. Forces 1964, 42, 429–434. [Google Scholar] [CrossRef]
- Jourard, S.M. Some Psychological Aspects of Privacy. Law Contemp. Probl. 1966, 31, 307–318. [Google Scholar] [CrossRef]
- Lewis, O. The Children of Sanchez: Autobiography of a Mexican Family; Knopf Doubleday Publishing Group: New York, NY, USA, 2011; ISBN 978-0-307-74454-8. [Google Scholar]
- Hall, E.T. The Hidden Dimension; Doubleday: Garden City, NY, USA, 1966; Volume 609. [Google Scholar]
- Sommer, R. Personal Space. In The Behavioral Basis of Design; Prentice-Hall, Inc.: Upper Saddle River, NJ, USA, 1969. [Google Scholar]
- Gehl, J. “Soft Edges” in Residential Streets. Scand. Hous. Plan. Res. 1986, 3, 89–102. [Google Scholar] [CrossRef]
- Alidoust, S.; Bosman, C.; Holden, G. Socially Healthy Ageing: The Importance of Third Places, Soft Edges and Walkable Neighbourhoods. In State of Australian Cities Conference 2015: Refereed Proceedings; Urban Research Program at Griffith University on behalf of the Australian Cities Research Network: Gold Coast, Australia, 2015; ISBN 978-1-925455-03-8. [Google Scholar]
- Koncelik. Designing the Open Nursing Home; Dowden, Hutchinson & Ross: Stroudsburg, PA, USA, 1976; Volume 27.
- Nelson, G.G. Household Models for Nursing Home Environments. Available online: http://www.artifactsofculturechange.org/Data/Documents/NelsonHousehold-ResidentialPaper.pdf (accessed on 29 May 2020).
- Brown, C.; Efstratiou, C.; Leontiadis, I.; Quercia, D.; Mascolo, C.; Scott, J.; Key, P. The Architecture of Innovation: Tracking Face-to-Face Interactions with Ubicomp Technologies. In Proceedings of the 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing; Association for Computing Machinery: New York, NY, USA, 2014. [Google Scholar] [CrossRef]
- Génois, M.; Vestergaard, C.L.; Fournet, J.; Panisson, A.; Bonmarin, I.; Barrat, A. Data on Face-to-Face Contacts in an Office Building Suggest a Low-Cost Vaccination Strategy Based on Community Linkers. Netw. Sci. 2015, 3, 326–347. [Google Scholar] [CrossRef]
- Sloane, P.; Mitchell, C.; Weisman, G.D.; Zimmerman, S.; Foley, K.M.L.; Lynn, M.; Calkins, M.P.; Lawton, M.P.; Terei, J.; Grant, L.; et al. Therapeutic Environment Screening Survey for Nursing Homes (TESS-NH). J. Gerontol. B Psychol. Sci. Soc. Sci. 2002, 57, S69–S78. [Google Scholar] [CrossRef]
- Parker, C.; Barnes, S.; Mckee, K.; Morgan, K.; Torrington, J.; Tregenza, P. Quality of Life and Building Design in Residential and Nursing Homes for Older People. Ageing Soc. 2004, 24, 941–962. [Google Scholar] [CrossRef]
- Fleming, R. An Environmental Audit Tool Suitable for Use in Homelike Facilities for People with Dementia. Australas. J. Ageing 2011, 30, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Lotfi, A.; Langensiepen, C.; Mahmoud, S.M.; Akhlaghinia, M.J. Smart Homes for the Elderly Dementia Sufferers: Identification and Prediction of Abnormal Behaviour. J. Ambient Intell. Humaniz. Comput. 2012, 3, 205–218. [Google Scholar] [CrossRef]
- Sweeney, D.; Quinlan, L.R.; Browne, P.; Richardson, M.; Meskell, P.; ÓLaighin, G. A Technological Review of Wearable Cueing Devices Addressing Freezing of Gait in Parkinson’s Disease. Sensors 2019, 19, 1277. [Google Scholar] [CrossRef] [PubMed]
- Bijnens, W.; Aarts, J.; Stevens, A.; Ummels, D.; Meijer, K. Optimization and Validation of an Adjustable Activity Classification Algorithm for Assessment of Physical Behavior in Elderly. Sensors 2019, 19, 5344. [Google Scholar] [CrossRef]
- Mainetti, L.; Patrono, L.; Rametta, P. Capturing Behavioral Changes of Elderly People through Unobtruisive Sensing Technologies. In Proceedings of the 2016 24th International Conference on Software, Telecommunications and Computer Networks (SoftCOM), Split, Croatia, 22–24 September 2016; pp. 1–3. [Google Scholar] [CrossRef]
- Charlon, Y.; Fourty, N.; Campo, E. A Telemetry System Embedded in Clothes for Indoor Localization and Elderly Health Monitoring. Sensors 2013, 13, 11728–11749. [Google Scholar] [CrossRef] [PubMed]
- Pigini, L.; Bovi, G.; Panzarino, C.; Gower, V.; Ferratini, M.; Andreoni, G.; Sassi, R.; Rivolta, M.W.; Ferrarin, M. Pilot Test of a New Personal Health System Integrating Environmental and Wearable Sensors for Telemonitoring and Care of Elderly People at Home (SMARTA Project). Gerontology 2017, 63, 281–286. [Google Scholar] [CrossRef]
- Prociow, P.A.; Crowe, J.A. Towards Personalised Ambient Monitoring of Mental Health via Mobile Technologies. Technol. Health Care 2010, 18, 275–284. [Google Scholar] [CrossRef]
- Montanari, A.; Nawaz, S.; Mascolo, C.; Sailer, K. A Study of Bluetooth Low Energy Performance for Human Proximity Detection in the Workplace. In Proceedings of the 2017 IEEE International Conference on Pervasive Computing and Communications (PerCom), Kona, HI, USA, 13–17 March 2017. [Google Scholar] [CrossRef]
- Day, K.; Calkins, M.P. Design and Dementia. In Handbook of Environmental Psychology; Bechtel, R.B., Churchman, A., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2003. [Google Scholar]
- Morgan, D.G.; Stewart, N.J. Multiple Occupancy versus Private Rooms on Dementia Care Units. Environ. Behav. 1998, 30, 487–503. [Google Scholar] [CrossRef]
- Lawton, M.P.; Fulcomer, M.; Kleban, M.H. Architecture for the Mentally Impaired Elderly. Environ. Behav. 1984, 16, 730–757. [Google Scholar] [CrossRef]
- Kane, R.A.; Lum, T.Y.; Cutler, L.J.; Degenholtz, H.B.; Yu, T.C. Resident Outcomes in Small-House Nursing Homes: A Longitudinal Evaluation of the Initial Green House Program. J. Am. Geriatr. Soc. 2007, 55, 832–839. [Google Scholar] [CrossRef]
- Zeisel, J.; Silverstein, N.M.; Hyde, J.; Levkoff, S.; Lawton, M.P.; Holmes, W. Environmental Correlates to Behavioral Health Outcomes in Alzheimer’s Special Care Units. Gerontologist 2003, 43, 697–711. [Google Scholar] [CrossRef] [PubMed]
- Hanson, J.; Zako, R. Configuration and Design in Caring Environments: Syntax and Quality of Life in a Sample of Residential Care Homes for Older People. In Proceedings of the 5th International Space Syntax Symposium; van Nes, A., Ed.; TU Delft: Delft, The Netherlands, 2005; Volume 2, pp. 117–128. [Google Scholar]
- Marquardt, G.; Schmieg, P. Dementia-Friendly Architecture: Environments that Facilitate Wayfinding in Nursing Homes. Am. J. Alzheimer’s Dis. Other Dement. 2009, 24, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Hubbard, G.; Cook, A.; Tester, S.; Downs, M. Beyond Words: Older People with Dementia Using and Interpreting Nonverbal Behaviour. J. Aging Stud. 2002, 16, 155–167. [Google Scholar] [CrossRef]
- Kelley, M.F. Social Interaction among People with Dementia. J. Gerontol. Nurs. 1997, 23, 16–20. [Google Scholar] [CrossRef]
- The Hong Kong Social Welfare Department. Residential Care Services for the Elderly. Available online: https://www.swd.gov.hk/en/index/site_pubsvc/page_elderly/sub_residentia/id_enhancedbo (accessed on 29 May 2020).
- Mollenkopf, H.; Marcellini, F.; Ruoppila, I.; Flaschenträger, P.; Gagliardi, C.; Spazzafumo, L. Outdoor Mobility and Social Relationships of Elderly People. Arch. Gerontol. Geriatr. 1997, 24, 295–310. [Google Scholar] [CrossRef]
- Haitsma, K.V.; Curyto, K.; Calkins, M.; Saperstein, A. The Environmental Design Lexicon for Dementia Care, Final Report of Grant IIRG-00-2058, Funded by the Alzheimer’s Association; Polisher Research Institute: North Wales, PA, USA, 2004. [Google Scholar]
- Elmståhl, S.; Annerstedt, L.; Ahlund, O. How Should a Group Living Unit for Demented Elderly Be Designed to Decrease Psychiatric Symptoms? Alzheimer Dis. Assoc. Disord. 1997, 11, 47–52. [Google Scholar] [CrossRef]
- Sloane, P.; Mitchell, C.; Preisser, J.; Phillips, C.; Commander, C.; Burker, E. Environmental Correlates of Resident Agitation in Alzheimer’s Disease Special Care Units. J. Am. Geriatr. Soc. 1998, 46, 862–869. [Google Scholar] [CrossRef]
- Chaudhury, H.; Cooke, H.A.; Cowie, H.; Razaghi, L. The Influence of the Physical Environment on Residents with Dementia in Long-Term Care Settings: A Review of the Empirical Literature. Gerontologist 2018, 58, e325–e337. [Google Scholar] [CrossRef]
- Capriglione, D.; Casinelli, D.; Ferrigno, L. Use of Frequency Diversity to Improve the Performance of RSSI-Based Distance Measurements. In Proceedings of the 2015 IEEE International Workshop on Measurements Networking (M&N), Coimbra, Portugal, 12–13 October 2015; pp. 1–6. [Google Scholar] [CrossRef]






| Room Typology | Floor Area (sqm) per Resident | Distance between Beds (m) | Bedroom Adjacent to | Objects Used by Residents to Achieve Privacy in Bedrooms |
|---|---|---|---|---|
| #1 Three-bed room | 3.99 | 1 | A pocket area along the corridor | No curtains were on the bedroom door. No objects were used between beds. Beds were not visible from the corridor or social area. |
| #2 Four-bed room (type 1) | 4.38 | 1.2 | Double-loaded corridor | Half curtains were on the bedroom door. Personal objects (towels, clothing) were hung between beds. Beds were visible from the corridor but not social area. |
| #3 Four-bed room (type 2) | 4.38 | 1.2 | Social space | Half curtains were on the bedroom door. Personal objects (towels, clothing) were hung between beds. Beds were visible from the social area as well as corridor. |
| #4 Five-bed room | 3.79 | 1 | Double-loaded corridor | Half curtains were on the bedroom door. No objects were used between beds. Beds were not visible from the corridor or social area. |
| Dimensions | Definition | Geometrical Indicators |
|---|---|---|
| Privacy units | Assess how many people share a bedroom (TESS-NH; SCEAM). | 3 people = 3 |
| 4 people = 2 | ||
| 5+ people = 1 | ||
| Assess how much floor area each resident has in shared bedrooms ([61]; SCEAM). | Above 12 sqm = 3 | |
| 7.6–12 sqm = 2 | ||
| under 7.6 sqm = 1 | ||
| Assess if there are en-suite washing and WC facilities in the bedroom (SCEAM). | Yes = 3 | |
| Yes, but only washing area or only WC = 2 | ||
| None = 1 | ||
| Privacy objects | Assess how privacy is achieved in shared rooms (TESS-NH; SCEAM). | Solid partitions = 3 |
| Privacy curtains = 2 | ||
| None = 1 | ||
| Assess the distance between beds in shared rooms [33]. | 120+ cm = 3 | |
| 45 < x < 120 cm = 2 | ||
| 0 < x < 45 cm = 1 | ||
| Assess if there is visual privacy within bathrooms from helpers (SCEAM). | Alcove = 3 | |
| Screen = 2 | ||
| None = 1 | ||
| Privacy hierarchy | Assess which space is the bedroom adjacent to ([37,38]; EAT; SCEAM). | Semi-private space = 3 |
| Public social space = 2 | ||
| Semi-public corridor = 1 | ||
| Assess the number of transitional spaces (semi-private and semi-public) between the bedroom and social area ([37,38]; EAT). | 2 transitional spaces = 3 | |
| 1 transitional space = 2 | ||
| No transitional space = 1 | ||
| Assess if residents have the choice of more than one lounge (SCEAM). | Yes = 3 | |
| Yes, but it has more than four corners = 2 | ||
| No = 1 |
| Room Type | Three-Bed | Four-Bed (Type 1) | Four-Bed (Type 2) | Five-Bed |
|---|---|---|---|---|
| Number of Residents | 1 | 14 | 14 | 4 |
| Percentage (%) | 14 | 82 | 78 | 50 |
| Mobility Variables | r for Network Size | r for Privacy |
|---|---|---|
| Duration own rooms | 0.17 (0.236) | −0.01 (0.960) |
| Duration social spaces | 0.46 (0.001) | −0.13 (0.350) |
| Duration friends’ rooms | 0.36 (0.010) | −0.16 (0.269) |
| Frequency own rooms | 0.156 (0.279) | −0.054 (0.707) |
| Frequency social spaces | 0.486 (0.000) | −0.155 (0.282) |
| Frequency friends’ rooms | 0.425 (0.002) | −0.219 (0.126) |
| Number of social spaces | 0.541 (<0.0001) | −0.262 (0.066) |
| Number of friends’ rooms | 0.429 (0.002) | −0.109 (0.450) |
| Distances travelled to friends’ rooms | 0.562 (<0.0001) | −0.184 (0.201) |
| Distances travelled to social spaces | 0.364 (0.009) | 0.015 (0.919) |
| Values in bold are different from 0 with a significance level alpha = 0.05 | ||
| Friends’ Room (%) | Social Space (%) | Own Room (%) | |
|---|---|---|---|
| Three-bed rooms | 33 | 49 | 18 |
| Four-bed rooms (type 1) | 39 | 38 | 23 |
| Four-bed rooms (type 2) | 32 | 43 | 25 |
| Five-bed rooms | 35 | 42 | 24 |
| Mean | 35 | 43 | 22 |
| Room Type | Informal Interaction (%) | Formal Interaction (%) | Social Withdrawal (%) | Social Isolation (%) |
|---|---|---|---|---|
| Friends’ Room > 35% and Social Space < 43% and Own Room < 22% OR Friends’ Room > 35% and Social Space < 43% and Own Room > 22% | Friends’ Room > 35% and Social Space > 43% and Own Room < 22% OR Friends’ Room < 35% and Social Space > 43% and Own Room < 22% | Friends’ Room < 35% and Social Space > 43% and Own Room > 22% OR Friends’ Room > 35% and Social Space > 43% and Own Room > 22% | Friends’ Room < 35% and Social Space < 43% and Own Room > 22% OR Friends’ Room < 35% and Social Space < 43% and Own Room < 22% | |
| Three-bed | 29 | 43 | 14 | - |
| Four-bed (type 1) | 35 | 24 | 18 | 24 |
| Four-bed (type 2) | 22 | 33 | 17 | 28 |
| Five-bed | 38 | 38 | 13 | 13 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, A.C.H.; Lau, N.; Ho, J.C.F. The Role of Bedroom Privacy in Social Interaction among Elderly Residents in Nursing Homes: An Exploratory Case Study of Hong Kong. Sensors 2020, 20, 4101. https://doi.org/10.3390/s20154101
Yang ACH, Lau N, Ho JCF. The Role of Bedroom Privacy in Social Interaction among Elderly Residents in Nursing Homes: An Exploratory Case Study of Hong Kong. Sensors. 2020; 20(15):4101. https://doi.org/10.3390/s20154101
Chicago/Turabian StyleYang, Aria C. H., Newman Lau, and Jeffrey C. F. Ho. 2020. "The Role of Bedroom Privacy in Social Interaction among Elderly Residents in Nursing Homes: An Exploratory Case Study of Hong Kong" Sensors 20, no. 15: 4101. https://doi.org/10.3390/s20154101
APA StyleYang, A. C. H., Lau, N., & Ho, J. C. F. (2020). The Role of Bedroom Privacy in Social Interaction among Elderly Residents in Nursing Homes: An Exploratory Case Study of Hong Kong. Sensors, 20(15), 4101. https://doi.org/10.3390/s20154101





