1. Introduction
Body temperature is an indicator of human physiological activity and health, especially in pediatrics, surgery and general emergency departments [
1].
Most of the early methods of measuring body temperature used contact mercury thermometers. Advances in electrical technology mean that contact-type electronic thermometers have become widely used. The measurement sites are the sublingual mouth, the rectum, the axillary and the base of the urethra. Some medical reports show that contact thermometers accurately measure body temperature [
2,
3]. To screen for an illness, the body temperature of many individuals must be measured, so noncontact type infrared thermometers (IRT) are used to measure the tympanic (ear) and forehead temperature. These IRTs are fast, convenient and safe to use. Medical IRTs for ear temperature and forehead temperature are used in medicine.
When the temperature of a natural object is higher than the absolute temperature, the surface emits thermal radiation. The infrared thermometer (IRT) detects this radiant energy that is released by the object via sensing elements and converts it into an electrical signal. After signal processing, the measured temperature is displayed on the IRT. This principle is used to develop an IRT to measure body temperature [
4,
5,
6,
7].
In 2003, severe acute respiratory syndrome, which is commonly known as SARS, was prevalent in Asia and caused panic in many countries. IRT is a rapid detection method and the most commonly used IRTs measure the temperature of the tympanic and the forehead. The tympanic is close to the core temperature of the body and gives the most accurate representation of the body temperature [
4,
6,
7,
8,
9,
10]. The screening of passengers for signs of Ebola infection was observed with a noncontact thermometer at five airports in USA in 2014 [
11].
IRTs are used to measure the tympanic or forehead temperatures. The probe cover must be changed, and the probe must be adjusted to fit the shape of the ear canal, so measuring the tympanic temperature is a troublesome process. A forehead IRT is convenient and noninvasive, so any risk of mutual infection is prevented, and as such, public places, such as airports, schools, hospital, and transportation vehicles, used this type of device to screen the public in the SARS era [
12,
13,
14]. This method is also currently used to prevent the spread of the coronavirus (COVID-19). However, noncontact IRTs are not proven in terms of accuracy, so it is necessary to determine whether an IRT gives as reliable information as other thermometers. The performance of forehead thermometers has been questioned [
15]. Hsiao et al. [
16] suggested taking temperature measurements twice for people before entering the hospital to reduce the risk of COVID-19 spread.
The surface emissivity of an object has the most significant effect on the temperature that is measured by an IRT. The emissivity of the tympanic membrane is assumed to be 1.0, but the emissivity of human skin is between 0.976 and 0.984 [
17,
18,
19,
20].
There are two types of infrared techniques available for the surface temperature detection. One is the point estimation to detect the tympanic temperature or the forehead temperature, and the device is called tympanic IRT or forehead IRT. The other is the IR thermography or thermal imaging. The thermal detector is used to detect the receive radiation from the targets. The sensing elements of thermal detectors are the pyroelectric detector and the thermopile for infrared thermometers and the bolometer focal plane arrays (Bolometer FDA) for IR thermography.
Recently, research on the application of infrared thermography on human body temperature measurement has been carried out. Sharma and Yadav [
21] proposed a noncontact temperature algorithm for face detection in a video sequence and validated its performance against standard temperature device. Rodriguez-Lozand et al. [
22] proposed a novel method to segment the forehead region of the human beings and to calculate the mean temperature of these area. With this simple and accurate method, the thermal face images in different features are presented. Chaglla et al. [
23] introduced an ear-based device to measure the ear temperature continuously. The novel design involved coating graphene platelets on the lens of an infrared thermopile sensor, and the performance of this device was validated by comparing it with others commercial ear thermometers. Tay et al. [
24] evaluated three types of infrared thermal detection systems for fever screening in tropical conditions and found that the devices with video monitoring had very high specificity and the handheld thermograph could not be used for fever screening.
Many factors affect the temperature measurement of the human body [
25,
26]. Erickson and Kirklin [
27] performed invasive measurements using pulmonary artery temperature as an indicator to compare tympanic, bladder, oral and axillary temperature. The difference between the pulmonary artery temperature and the ear temperature was 0.07 °C ± 0.41 °C, for the bladder temperature, the value was 0.03 °C ± 0.23 °C, for the oral temperature, the value was 0.05 °C ± 0.26 °C and for the axillary temperature, the value was −0.68 °C ± 0.57 °C. These results show that the bladder temperature and the mouth temperature are closest to the pulmonary artery temperature, followed by the tympanic temperature, and the value for the axillary temperature was low.
Patel et al. [
28] compared the correlation between esophageal temperature, tympanic temperature and forehead surface temperature. The difference between the temperature of the esophagus and the frontal temperature was −1.64 ° C to 2.32 °C, for the ear temperature, the difference was −1.02 °C to 0.74 °C and for the tympanic temperature and forehead temperature, the difference was −1.48 °C to 2.52 °C. The correlation coefficients for the forehead temperature, the esophageal temperature, and ear temperature are small.
Measuring the temperature of the forehand using an IRT is convenient, but some studies show that the measurements are not accurate. There are three types of forehead thermometer: a thermistor probe, a liquid crystal strip and an IR thermometer. The thermistor probe and the liquid crystal strip are contact-type thermometers. The thermistor probe is a deep body thermometer because it is inserted into the tissue of the forehead.
Studies show that a contact-type deep skin forehead thermometer is suited to clinical use [
29,
30,
31,
32,
33]. This device was very accurate. Duran et al. [
8] compared the performance of a contact-type forehead thermometer with that of an axillary glass–mercury thermometer and found that both thermometers give similar readings. Zeiner et al. [
34] compared the body temperature that was measured using a deep forehead thermometer and a bladder thermometer and found no significant difference between the two readings. Liquid crystal thermometers have been used to measure forehead temperature [
35,
36,
37,
38,
39]. These studies show that liquid crystal devices are not as accurate as forehead thermistor thermometers and do not give as accurate a reading for core temperature as a rectal or tympanic measurement.
Patel et al. [
27] compared esophageal, tympanic and forehead temperature for adults. The mean difference between the esophageal and the forehead temperature was 0.3 °C and the mean difference between the tympanic and the forehead temperature was 0.5 °C. The forehead temperature was measured using a contact-type, liquid crystalline thermometry strip. The authors noted that the forehead temperature was not an accurate representation of the standard core temperature. Asadian et al. [
40] measured the oral, axillary, tympanic and forehead temperature. The central nasopharyngeal measurement was used as a standard value. The results show that the forehead and tympanic readings were the least and most accurate, respectively. The forehead temperature was measured using a contact-type strip thermometer. Berksoy et al. [
41] used a noncontact IRT to measure forehand temperature and compared the reading with those for tympanic and rectal temperature. The results show that measurements of the tympanic temperature are more practical than axillary thermometry.
Duncan et al. [
42] showed that the difference between the oral temperature and the temperature that was recorded using an IRT was 0.89 °C ± 0.58 °C. The authors commented that the thermometers were not interchangeable. Kocoglu et al. [
10] compared the accuracy of a tympanic IRT reading with the readings for axillary and rectal temperature that were measured using a glass thermometer. The highest temperature was the rectal temperature and the lowest temperature was the axillary temperature. The difference between the mean values for tympanic and rectal temperature was <0.2 °C.
Yeoh et al. [
43] studied the tympanic membrane vicinity as the measurement site of core body temperature and found the mean temperature of rectum, esophagus, left ear and right ears were 37.2 °C, 36.8 °C, 36.2 °C and 36.1 °C, respectively. Oguz et al. [
44] measured the tympanic and axillary body temperature of 1364 children and found the mean axillary and tympanic temperatures were 36.04 °C and 36.91 °C, respectively. The axillary and tympanic temperature that are considered as fever are >37.0 °C and >37.8 °C, respectively. Cutuli et al. [
45] reported the inconsistent opinions of the unit protocol for measuring body temperature and suggested the requirement of detailed studies of the noninvasive temperature measurement methods.
Mogensen et al. [
46] used the rectal temperature as a standard value. The study measured the tympanic temperature using an IRT and the forehead temperature using a contact-type temporal thermometer. The results show that the tympanic measurement was adequate for screening purposes but the forehead temperature was not. Kistemaker et al. [
47] tested two types of contact forehead thermometers and compared the readings with those for a rectal thermistor. The results showed that a contact-type forehead thermometer registered a higher temperature than a rectal thermistor. Dante et al. [
48] compared the performance for contact-type forehead, tympanic and axillary thermometers. The mean value for tympanic temperature was higher than that for the forehead and axillary thermometers, and these devices were not interchangeable. Ng et al. [
13] used a noncontact, handheld IRT to measure the forehead skin temperature. The reference temperature was measured using an electronic thermometer. The surface temperature was underestimated by 2 °C, so a temperature of 35.6 °C was the index temperature for fever if the forehead temperature was measured using a noncontact, handheld IRT. Ng et al. [
14] studied the relationship between the facial skin temperature that was detected by an IRT, and the actual temperature was detected using a direct thermometer. They recommend that the measured temperature of 35.5 °C signified a fever.
Measuring body temperature is an effective technique for screening SARS and other flus. The coronavirus (COVID-19) has spread globally and temperature measurement is used to rapidly screen people. Handheld forehead IRTs are easy to use, rapid, noncontact and inexpensive, so they are widely used. This IRTs was reported to measure wrist temperature and forehead temperature. However, these devices have unproven reliability [
15].
Many studies compare temperature measurements for different parts of the human body using different thermometers. Most of the forehead thermometers are contact-type. The measurements of body temperature depend on the type of thermometer, the sensing elements and the manufacturers’ claimed performance for each thermometer.
This study uses two commercial tympanic IRTs and an industrial IRT to measure the tympanic, forehead and wrist temperatures, and the measurement data is analyzed using statistical techniques. The results for the measurement of body temperature are used to define the threshold for fever screening using a forehead IRT.
4. Discussion
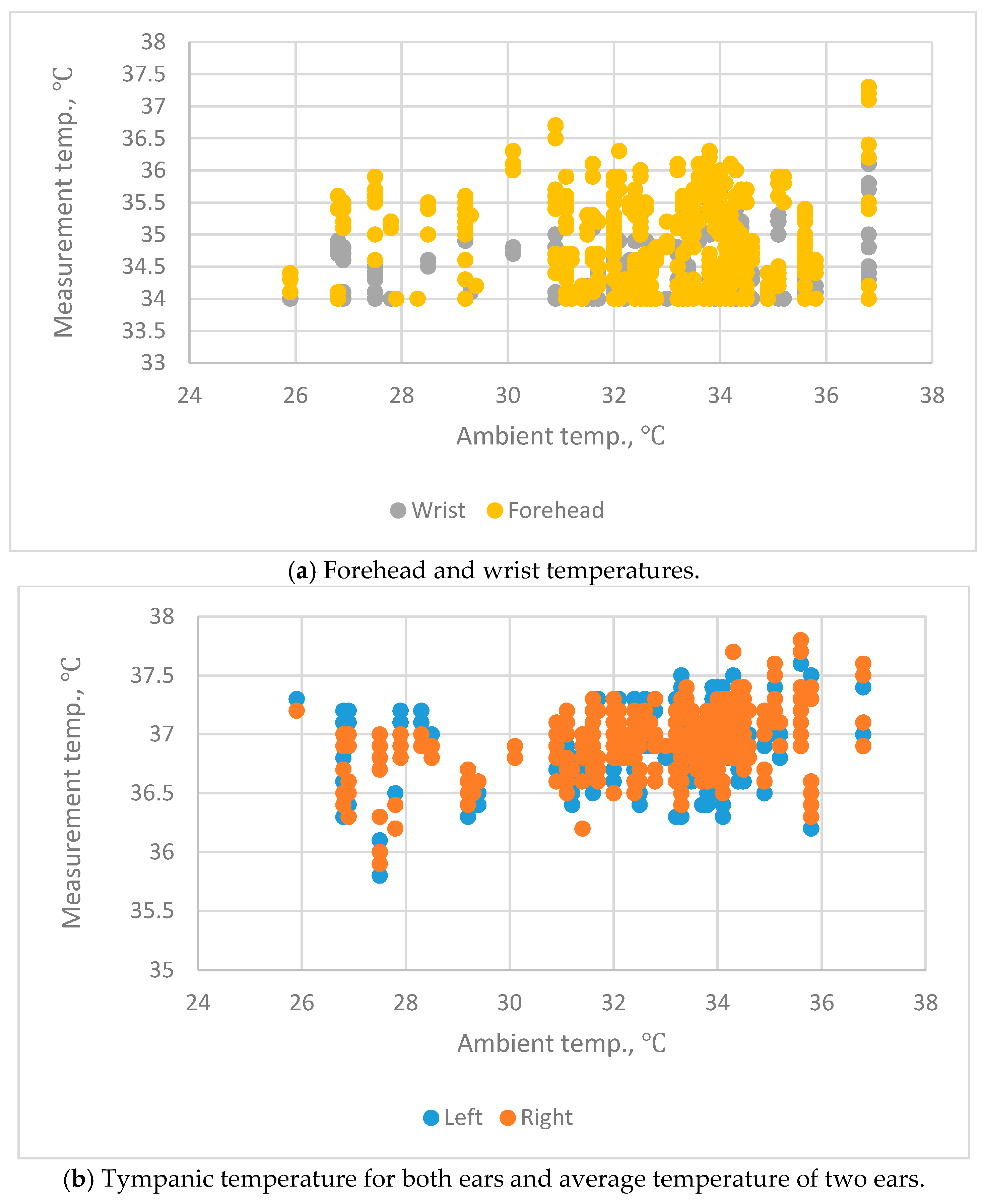
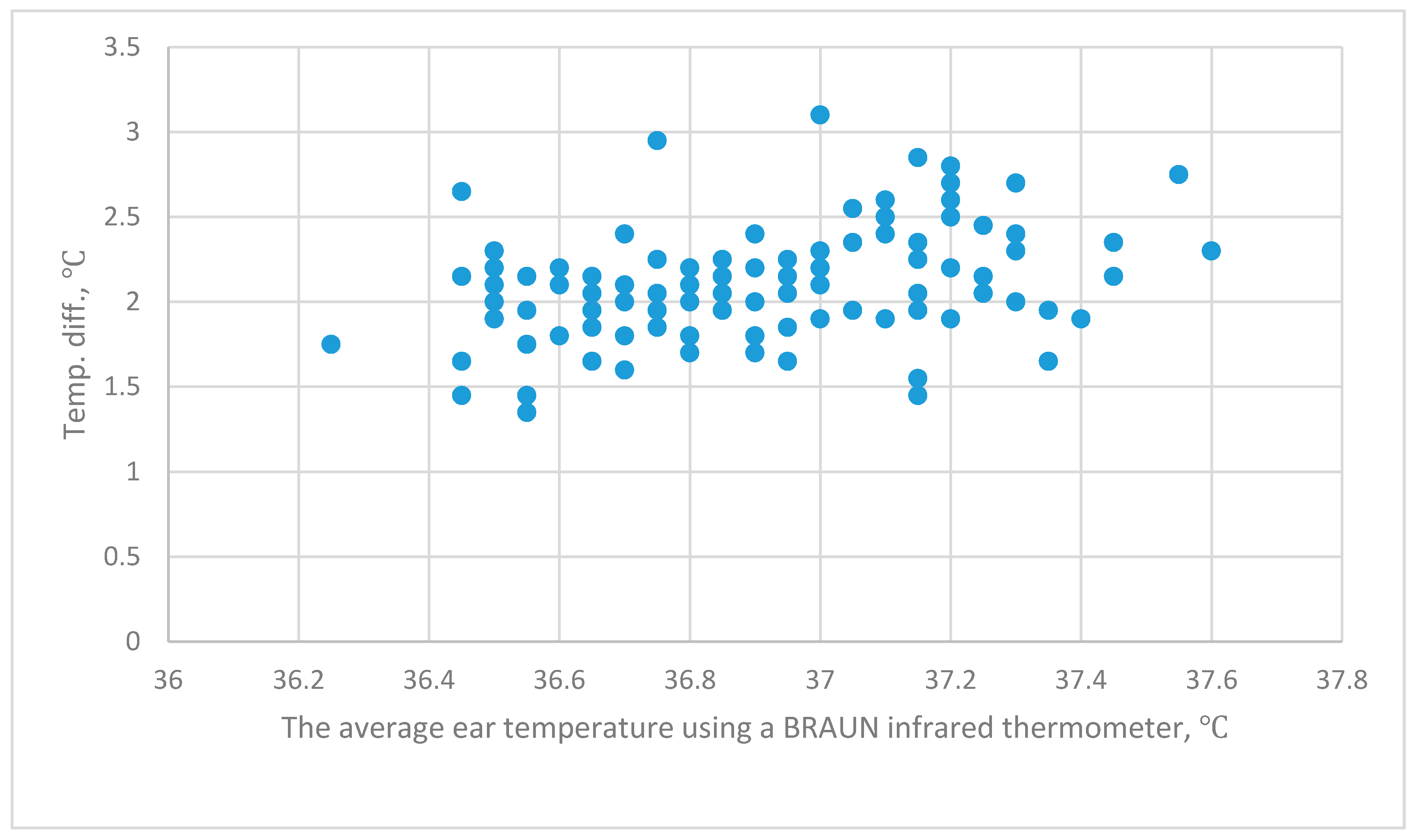
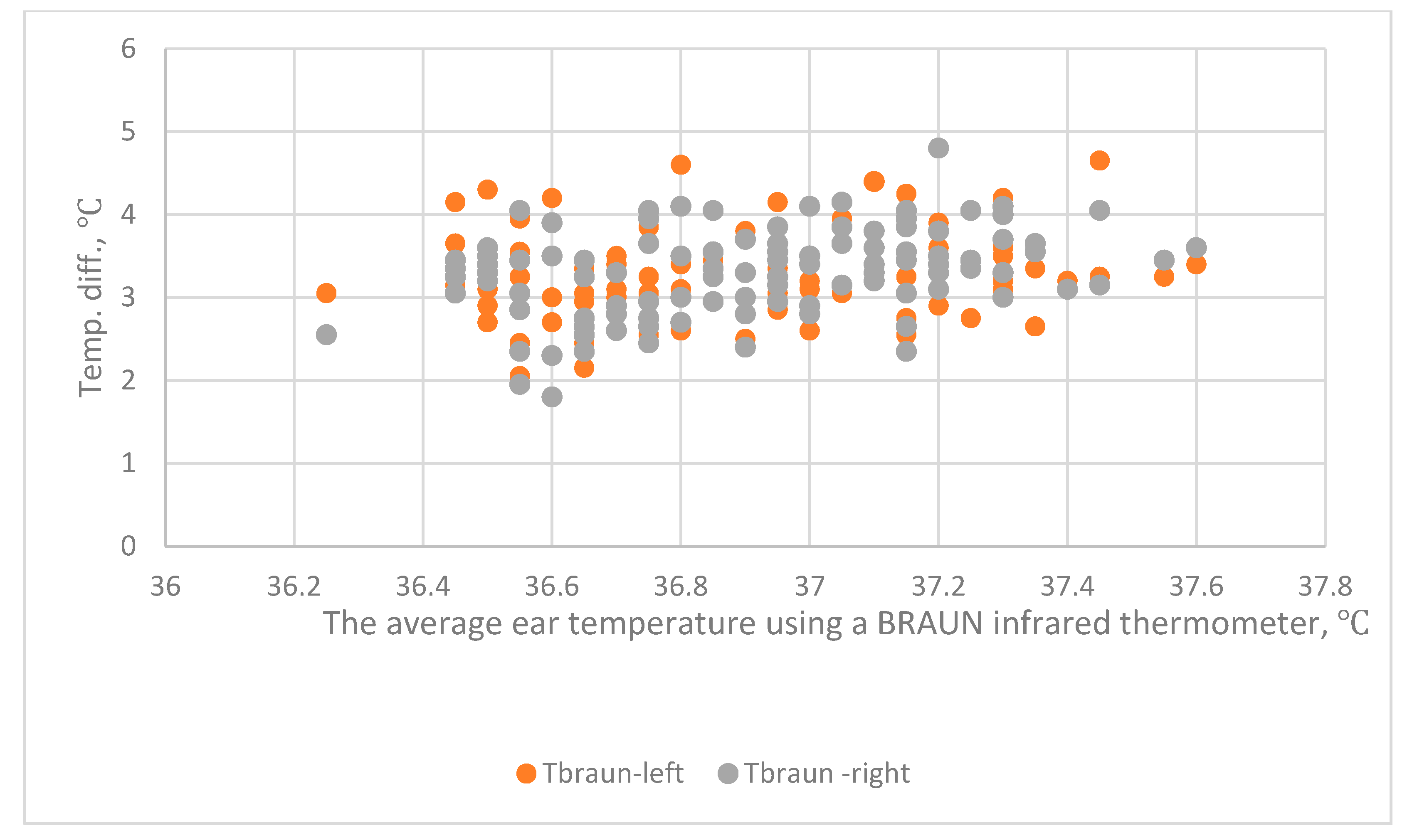
These results show the diversity of the body temperature. There is a high correlation between the tympanic temperature in the left and right ears. However, a paired t-test shows different results for the two experiments. In the first experiment, there is no significant difference between the temperature in the right and left ears, as measured using a BRAUN IRT (p < 0.05). In the second experiment, there is a significant difference in the temperature in the right and left ears for the two types of IRT (p < 0.002). The subjects for the two experiments were different. The first experiment involved 659 subjects and the second experiment involved 114. The size of the sample and a different age distribution affects the standard deviation, which affects the calculation of t values.
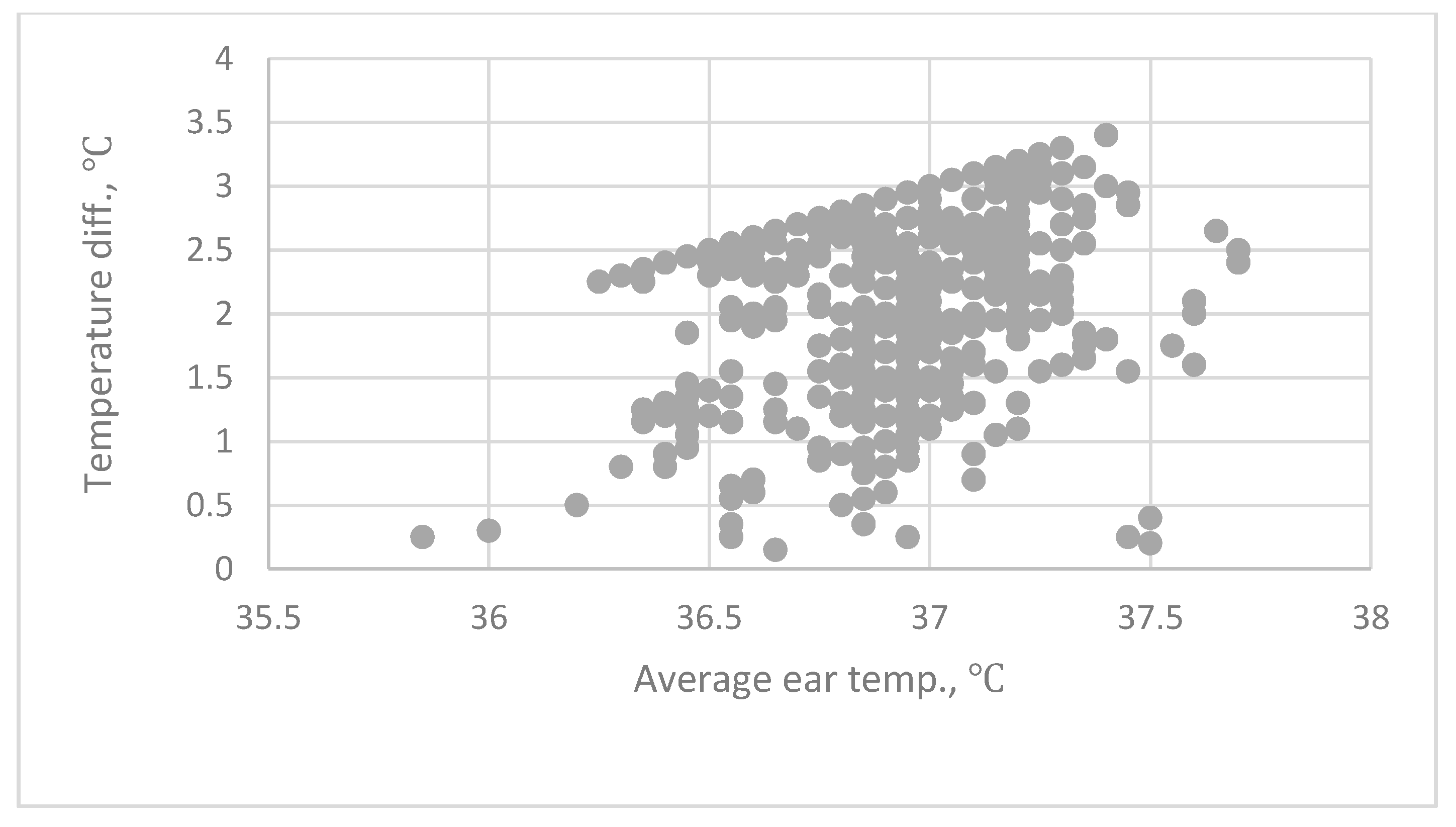
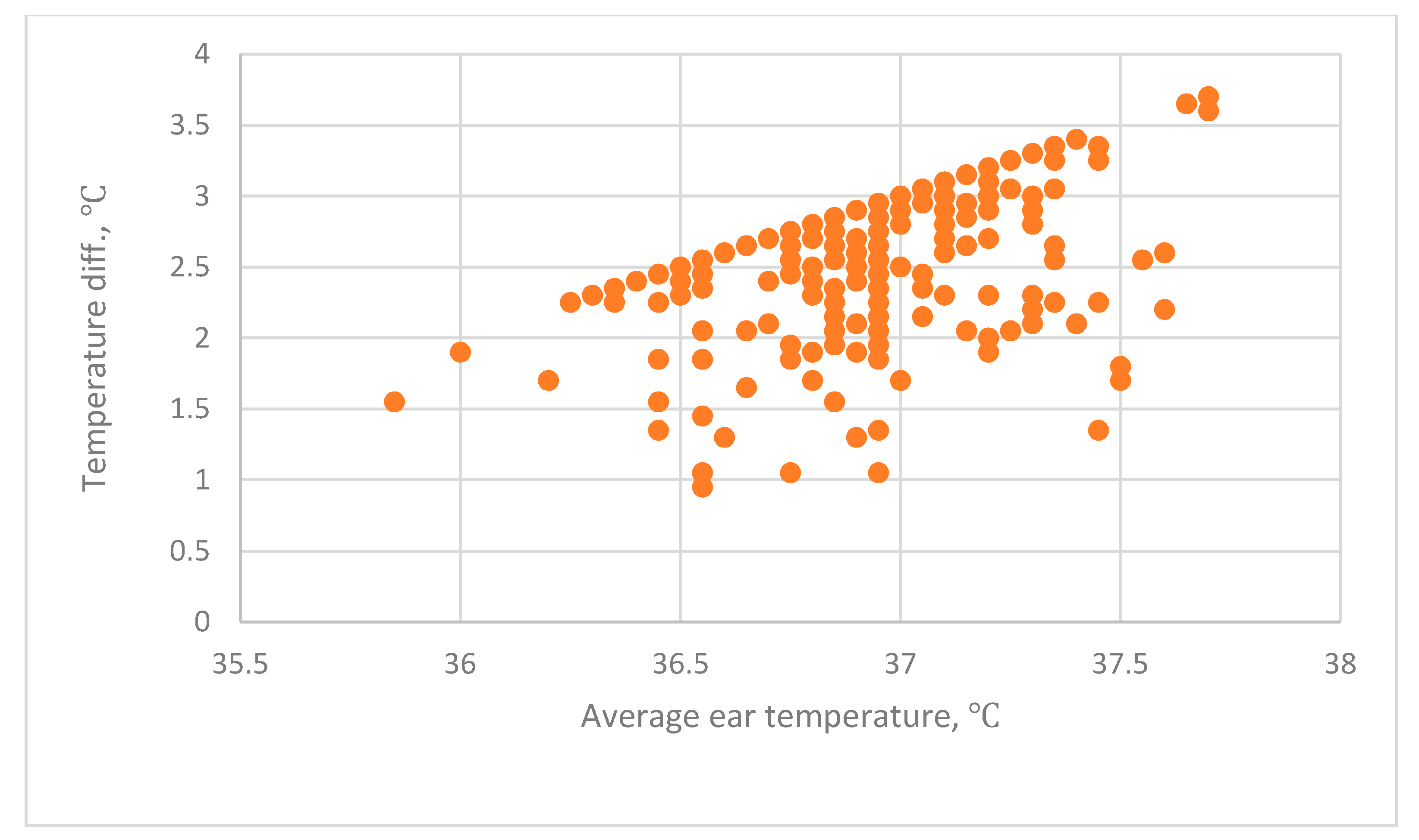
In the first experiment, the difference between the mean tympanic temperature and the forehead temperature is 2.20 °C ± 0.711 °C. This experiment used a tympanic IRT to detect the forehead temperature. The emissivity of this device cannot be adjusted. In the second experiment, the difference between the mean tympanic temperature and the forehead temperature is 2.1 °C ± 0.301 °C. This experiment used an industrial IRT to measure the forehead temperature. The emissivity of this industrial device was adjusted to 0.98. Both experiments produce similar results. The forehead temperature is 2.1 °C or 2.2 °C lower than the tympanic temperature. In the second experiment, the wrist temperature that is measured using a THI-301 IRT is 3.3 °C lower than the tympanic temperature. These measurements for wrist temperature do not represent the actual body temperature, so measurements of the wrist temperature cannot be used to establish a threshold for screening for fever.
Measurements of forehead temperature are convenient, fast and involve a low risk of infection, so they are used to screen for fever to identify possible victims of the novel coronavirus (COVID-19). However, there is no international standard for the threshold of forehead temperature that indicates fever. The Department of Health of Hong Kong [
54] recommended a threshold level for fever of >38 °C for ear temperature and >36 °C for forehead temperature. The difference between the two critical temperatures is 2 °C. The results of this study are close to these figures.
Liu et al. [
12] determined the accuracy of alternative IR techniques for fever screening during the 2003 SARS epidemic. Two types of IRTs were used to measure tympanic and forehead temperature. The results for 276 subjects showed a tympanic temperature of 36.44 °C ± 0.37 °C and a forehead temperature of 35.63 °C ± 0.36 °C. Ng et al. [
13] measured forehead temperature for 1000 healthy subjects using three handheld IRTs. The temperature was measured as 33.3 °C ± 1.18 °C using IR thermometers, but the results of the three IR thermometers were inconsistent. Their study noted that a forehead temperature of more than 35.5 °C suggests fever. Ng et al. [
14] determined that the forehead and tympanic temperature for 567 patients, measured using an IRT, differs by 2.34 °C. However, the study does not report the specifications of the sensors or the calibration technique. Williams et al. [
55] measured tympanic and forehead temperature using different IRTs. The tympanic was measured as 36.7 °C ± 0.5 °C and the forehead temperature as 34.0 °C ± 0.7 °C, and they concluded that measurements of forehead temperature are not as representative of the actual body temperature as tympanic temperature. In our study, the tympanic and forehead temperatures measured by BRAUN IRT were 36.9 °C ± 0.286 °C and 34.714 °C ± 0.392 °C, respectively. The results of our study were similar to those of Ng et al. [
14].
There is inconsistency in the results of studies. Ganio et al. [
56] and Edling et al. [
57] reported that a forehead IRT has good repeatability but cannot be applied as a clinical device because there is a fixed offset. Langham et al. [
39] reported a 2 °C difference in forehead temperature, as measured using an IRT, and the reference value was the bladder temperature. Chiappini et al. [
58] and Teran et al. [
59] determined that the use of an IRT to measure forehead temperature gives accurate results, so these are suited to clinical use. However, the fixed offset could be explained as the physiological phenomenon explained by the different temperature distribution between the inner and surface forehead skin. The precision of forehead IRT could be evaluated with the CV values in our study.
The mean difference between a tympanic IRT and a contact-type deep skin forehead thermometer was less than 1 °C [
27,
28,
34]. If an IRT is used to measure the forehead temperature, the surface temperature of the skin is measured, not the muscle temperature near the superficial temporal artery [
47]. Core body temperature is the standard temperature of the body. It is defined as the temperature of the blood perfusing the thermoregulatory receptor in the hypothalamus [
4]. The tympanic membrane has the same vascular supply that perfuse the hypothalamus, so it is the best site to measure the core body temperature [
60].
The superficial temporal is a side drench of the carotid artery and feeds beneath the vascular bed of the head’s skin [
47]. If a contact type thermometer is used to measure the forehead temperature, the sensing element, which is a thermistor, must touch the skin of the forehead. The sensors must be inserted into the muscle. The effect of the environment, such as wind speed, is neglected, so the measurement of forehead temperature using a contact-type thermometer is close to the tympanic temperature [
33,
34]. However, the fixed difference between the measurement values of tympanic and forehead IRTs needs to be considered.
A tympanic IRT is painless in use, does not involve contact with the membrane and gives a rapid result. However, the cover must be frequently replaced and the probe position must be adjusted to reduce distress to subjects. The measurement of forehead temperature using an IRT is more convenient than that of tympanic IRT.
The performance of an IRT is affected by the calibration method and environmental factors, such as solar radiation and wind speed over the skin [
61,
62]. Standard calibration practices [
6,
7,
62,
63] and proper operational procedures ensure the accuracy of the measurement of the forehead temperature.
The critical tympanic temperature that is used to screen for fever is 38 °C [
1,
54]. The Hong Kong government’s threshold level for fever is 38 °C for tympanic temperature and 36 °C for forehead temperature. Ng et al. [
13,
14] recommended a temperature of 35.5 °C to screen for fever. Previous studies show that the mean difference between forehead and tympanic temperature is 1.9 °C [
64]; 2.7 °C [
55]; and 2.0 °C [
39]. This study determines that the mean difference between tympanic temperature and forehead temperature is 2.2 °C.
The uncertainty of three IRTs was calculated by Chen et al. [
55]. At 36 °C, the combined uncertainty for the BRAUN is 0.15 °C, for the OMERO is 0.23 °C and for the THI-301 is 0.29 °C. This study determines that the tympanic temperature that is measured by the BRAUN IRT for the two experiments is 36.9 °C ± 0.286 °C and 36.937 °C ± 0.301 °C. The forehead temperature that is measured by the BRAUN is 34.714 °C ± 0.392 °C and by the THI-301 IRT is 34.80 °C ± 0.343 °C. The difference temperature between tympanic and forehead temperature for the two experiments is 2.20 °C ± 0.411 °C and 2.107 °C ± 0.311 °C. The difference between tympanic temperature and forehead temperature ranges from 2.1 °C to 2.2 °C for the two experiments.
The threshold for fever level for tympanic temperature is 38 °C. The measurement uncertainty for an IRT means that the threshold for fever for forehead temperature that is measured using an IRT could be 36 °C. Therefore, forehead temperature does not give as accurate a representation of actual body temperature as the tympanic temperature, and as such, forehead IRTs are suitable for quick screening but are not as accurate as a traditional body temperature thermometer.
The combined uncertainty of two IRTs at 36 °C for the BRAUN and the THI-301 was 0.42 °C and 0.45 °C, respectively. For the BRAUN IRT, the mean forehead temperature was 34.714 °C. The 95th and 99th percentiles were 35.40 °C and 35.69 °C, respectively. For the THI-301 IRT, the mean forehead temperature was 34.802 °C. The 95th and 99th percentiles were 35.54 °C and 35.85 °C, respectively.
If the 35.5 °C is selected as the threshold value for fever screening, the percentiles are 96.94% and 93.96% for BRAUN IRT and THI IRT, respectively. That is, there could be a false-positive region of 3.06% or 6.04%, respectively, and this will cause trouble in the fever screening of the masses. If the 36.0 °C is selected as the threshold value for fever screening, the percentiles are 96.89% and 99.61% for BRAUN IRT and THI IRT, respectively and the region of false are small.
Considering the measurement uncertainty of IRTs and the requirement of practical operation (ease of use, speed and convenience), the standard operating procedure (SOP) is proposed to screen for fever using measurements of forehead temperature.
Tympanic and forehead IRTs should be used.
Both IRTs must be calibrated using a black box method to ensure accuracy [
6,
7,
47,
63].
The threshold level for fever is 36.0 °C for a forehead temperature measurement using an IRT.
If the forehead temperature of a subject is measured to be higher than 36.0 °C, the tympanic temperature must be measured.
If the tympanic temperature is >38 °C. The subject is considered to have a fever condition and clinical treatment is advised.