Measurement of the Chair Rise Performance of Older People Based on Force Plates and IMUs
Abstract
:1. Introduction
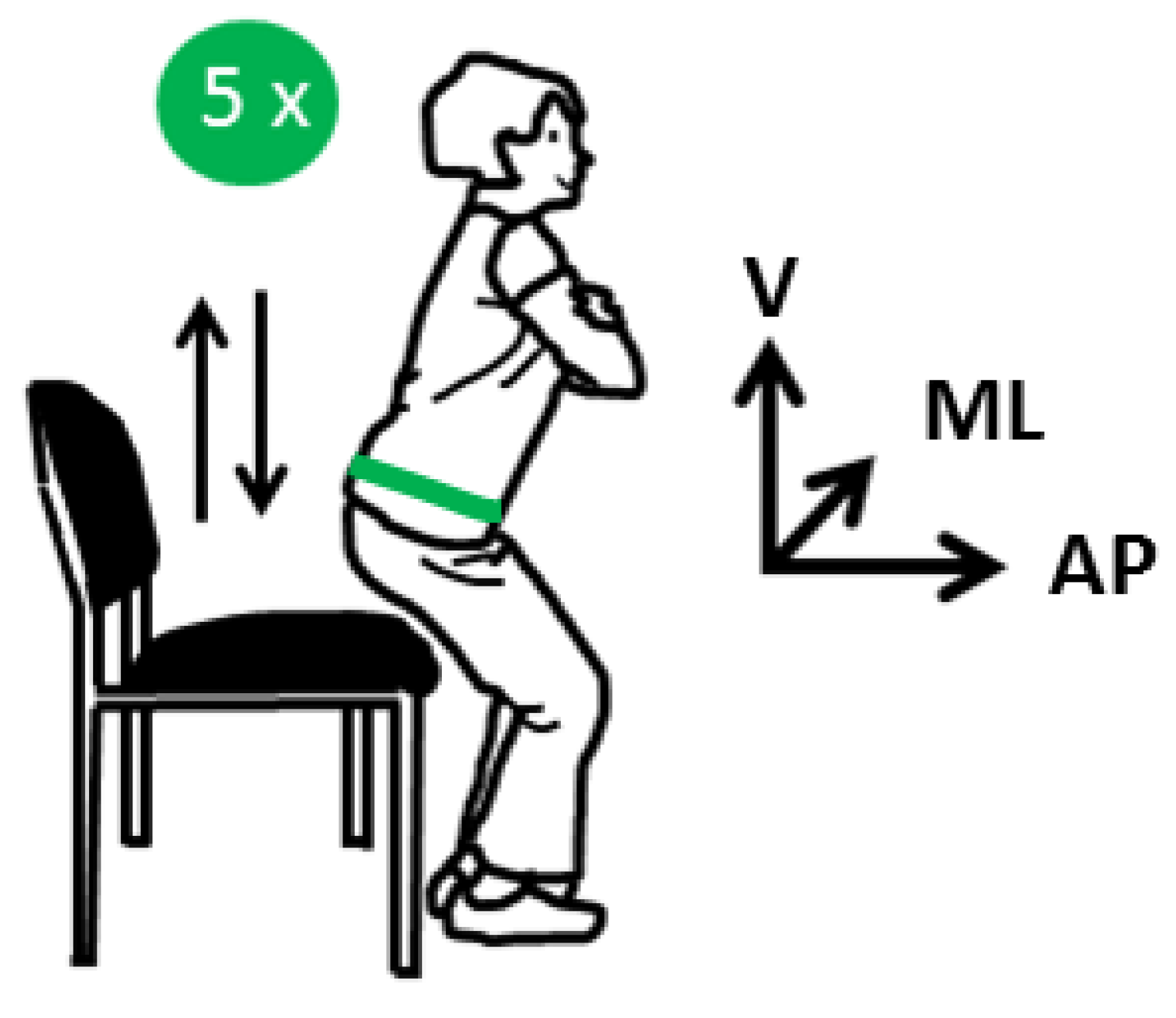
2. Materials and Methods
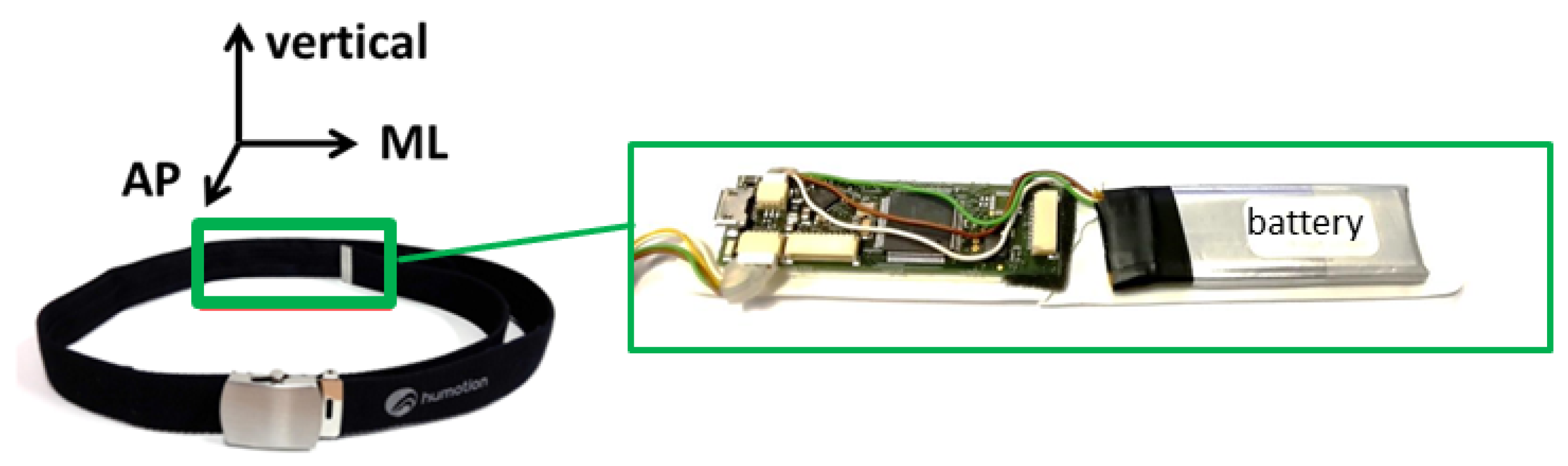
2.1. Measurement Systems
2.1.1. Sensor Belt
2.1.2. Force Plate
2.1.3. Microsoft Kinect
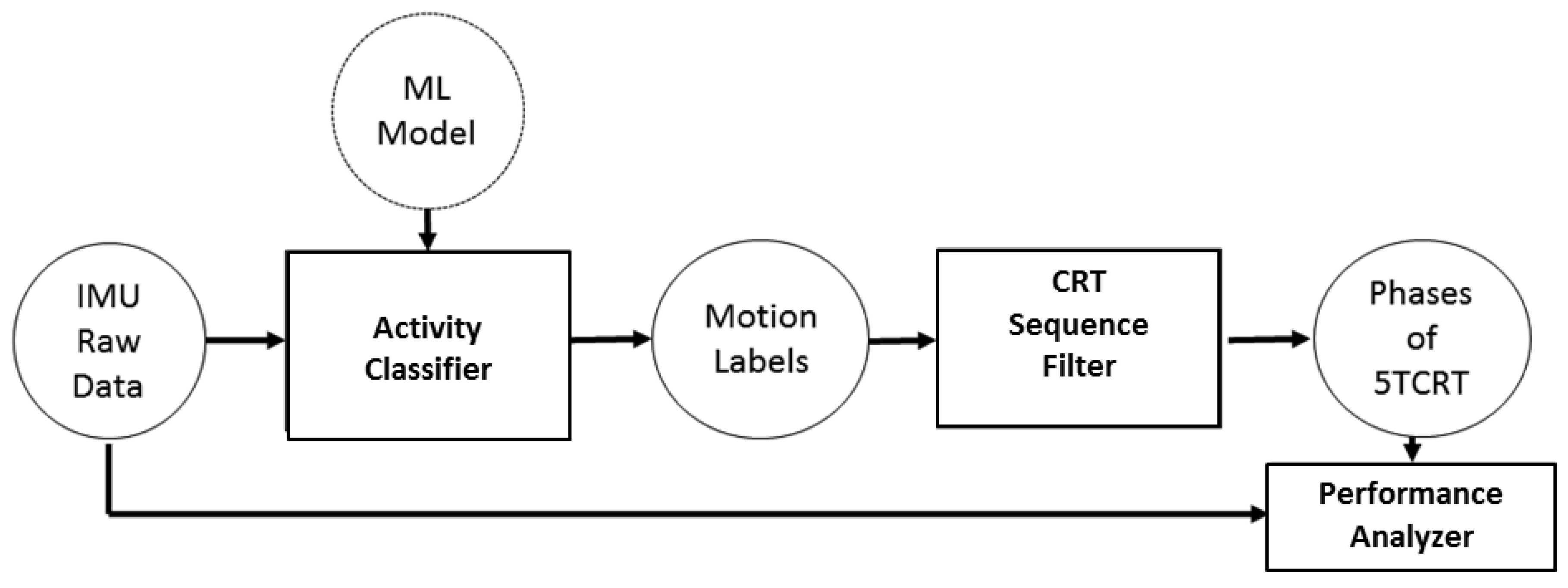
2.2. Machine Learning Classification-Model for Activity
- Root Mean Square (RMS),
- Mean,
- Signal Energy (SE),
- Auto Correlation (AC),
- Correlation (C),
- Signal Magnitude Area (SMA),
- Standard Deviation (SD),
- Pitch.
2.3. Statistical Data Analysis
3. Results
3.1. Study Population
3.2. Sensitivity and Specificity of Applied Machine Learning Classifiers
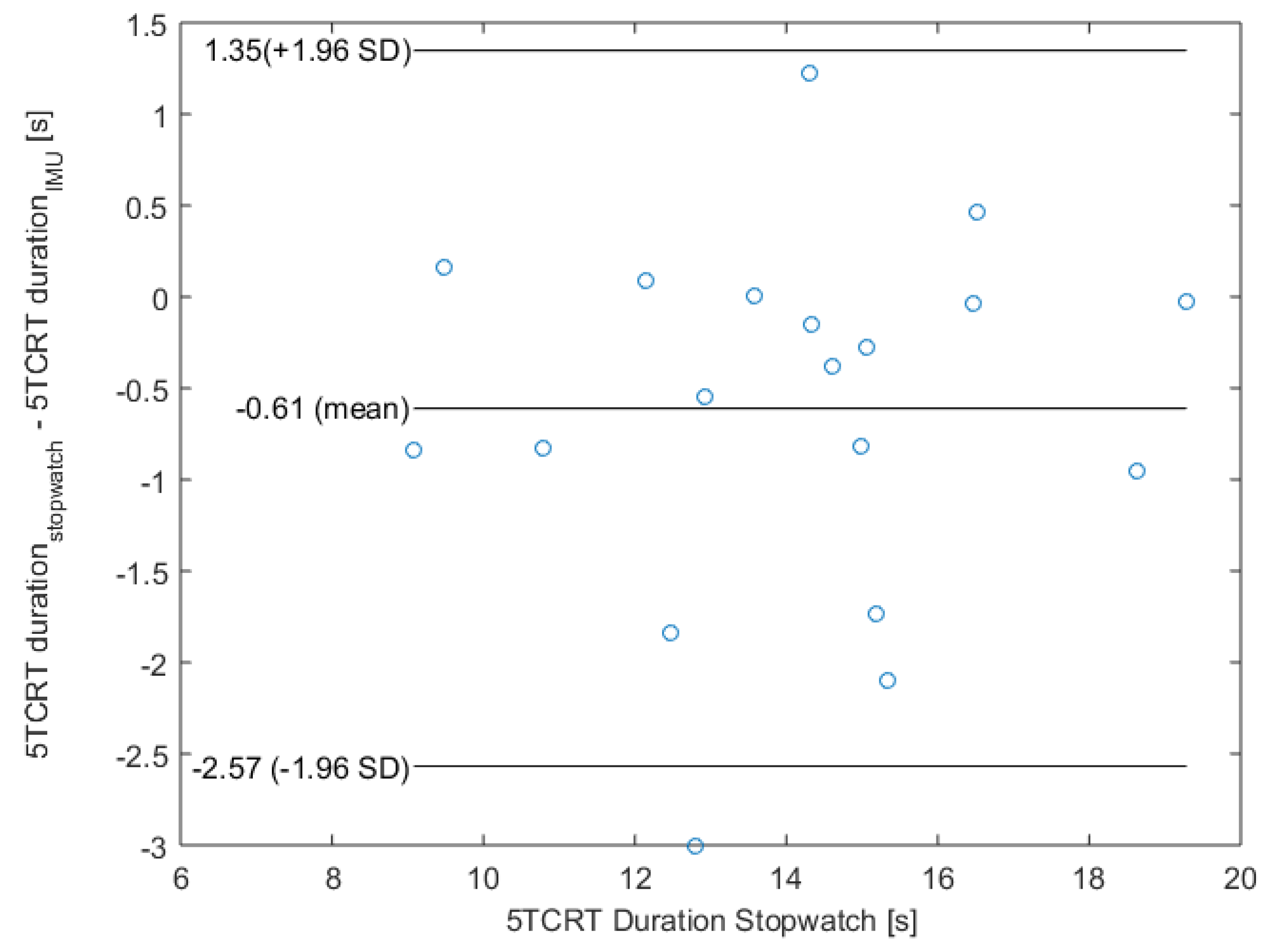
3.3. Evaluation of Overall 5CRT Duration Accuracy
3.4. Evaluation of Distinct Transitions
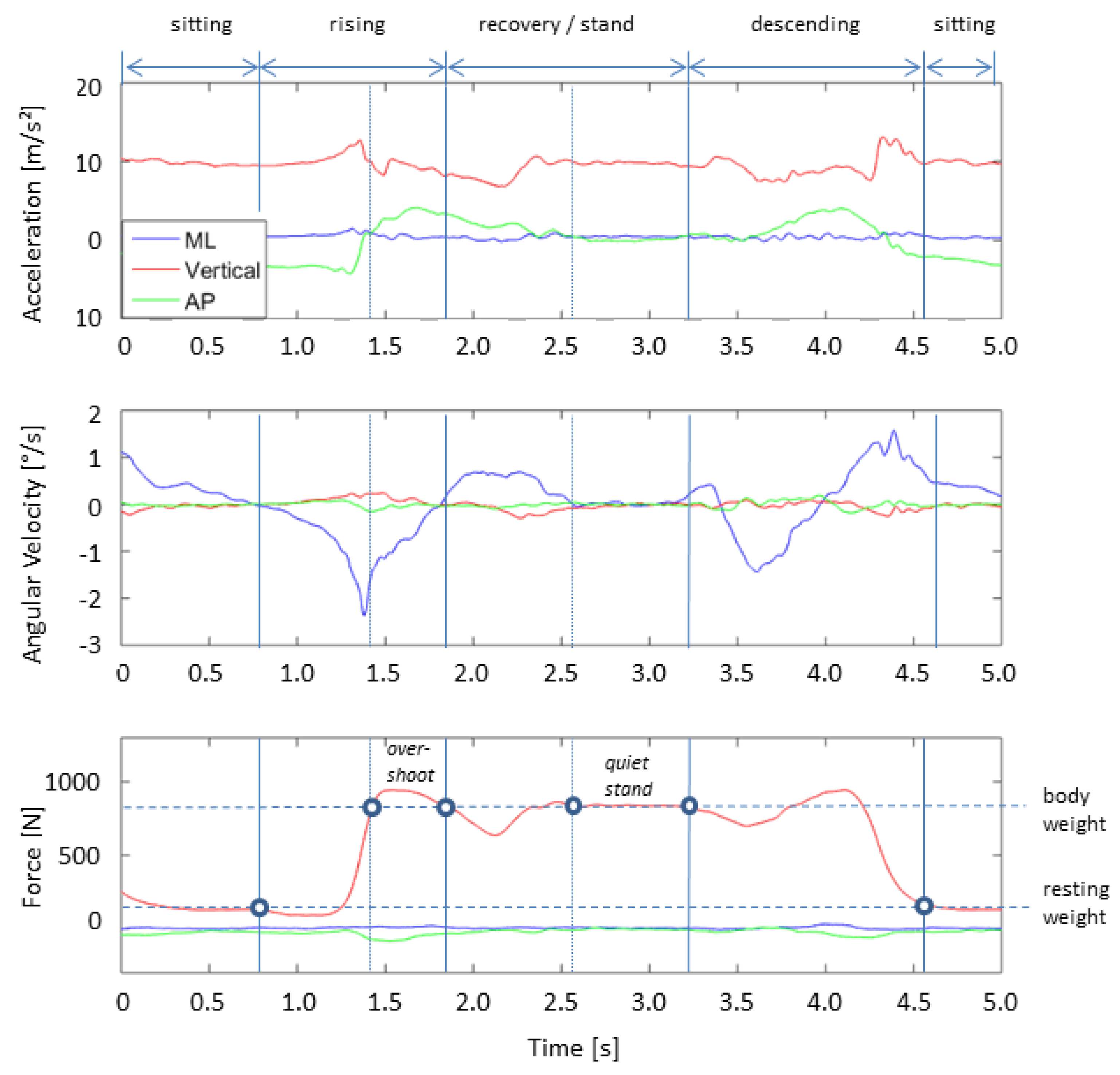
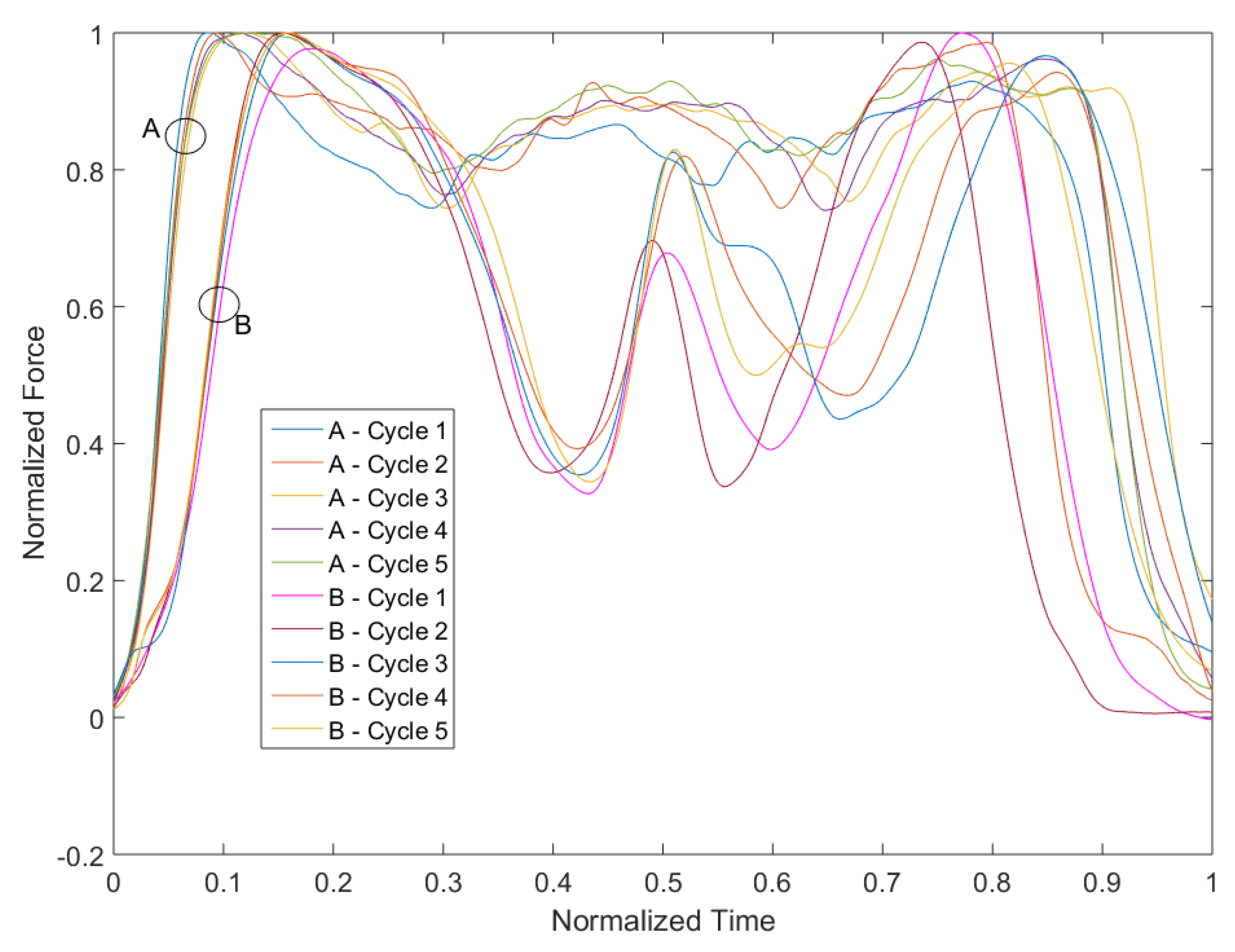
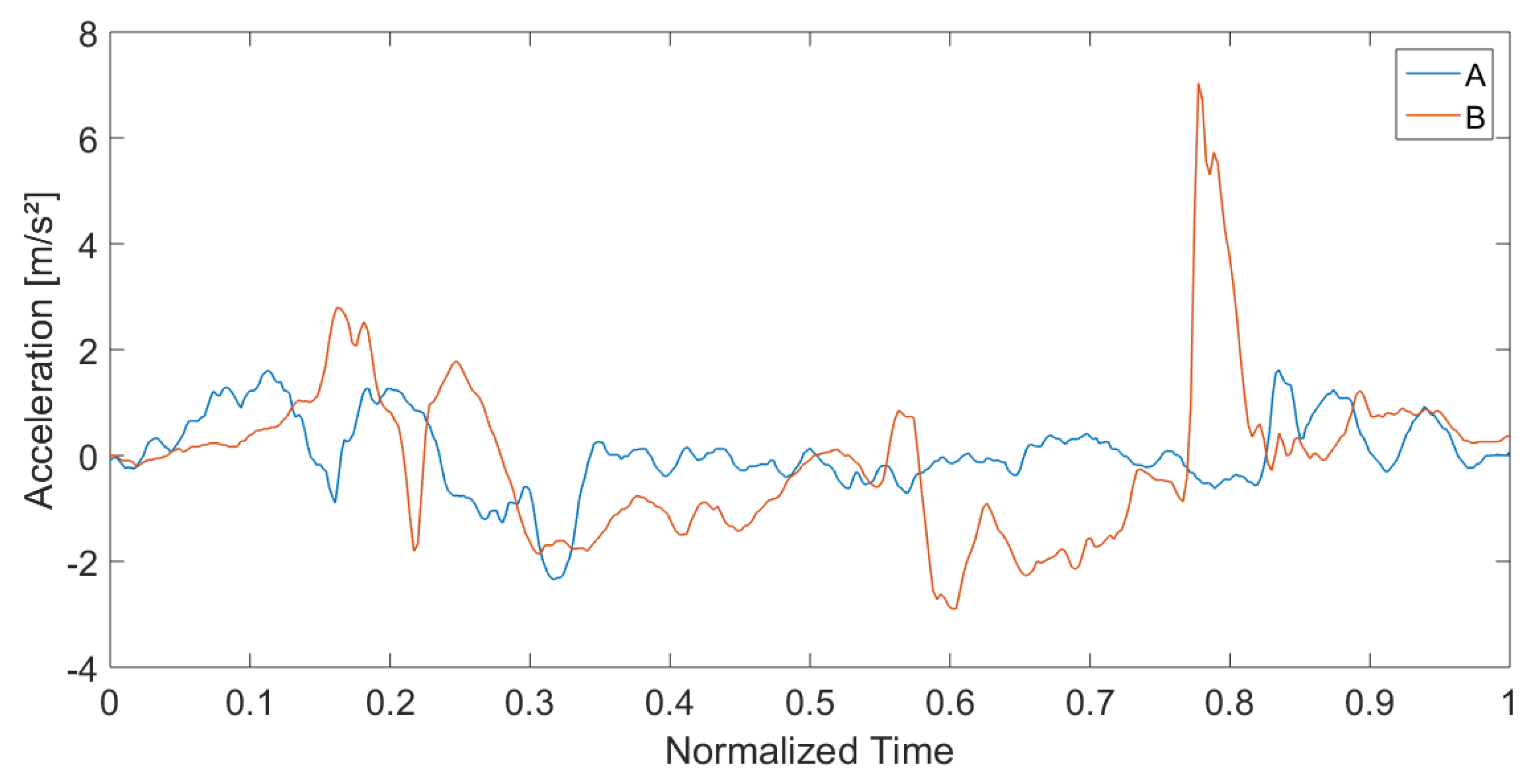
3.5. Signal-Pattern and Qualitative Progress of the Movements
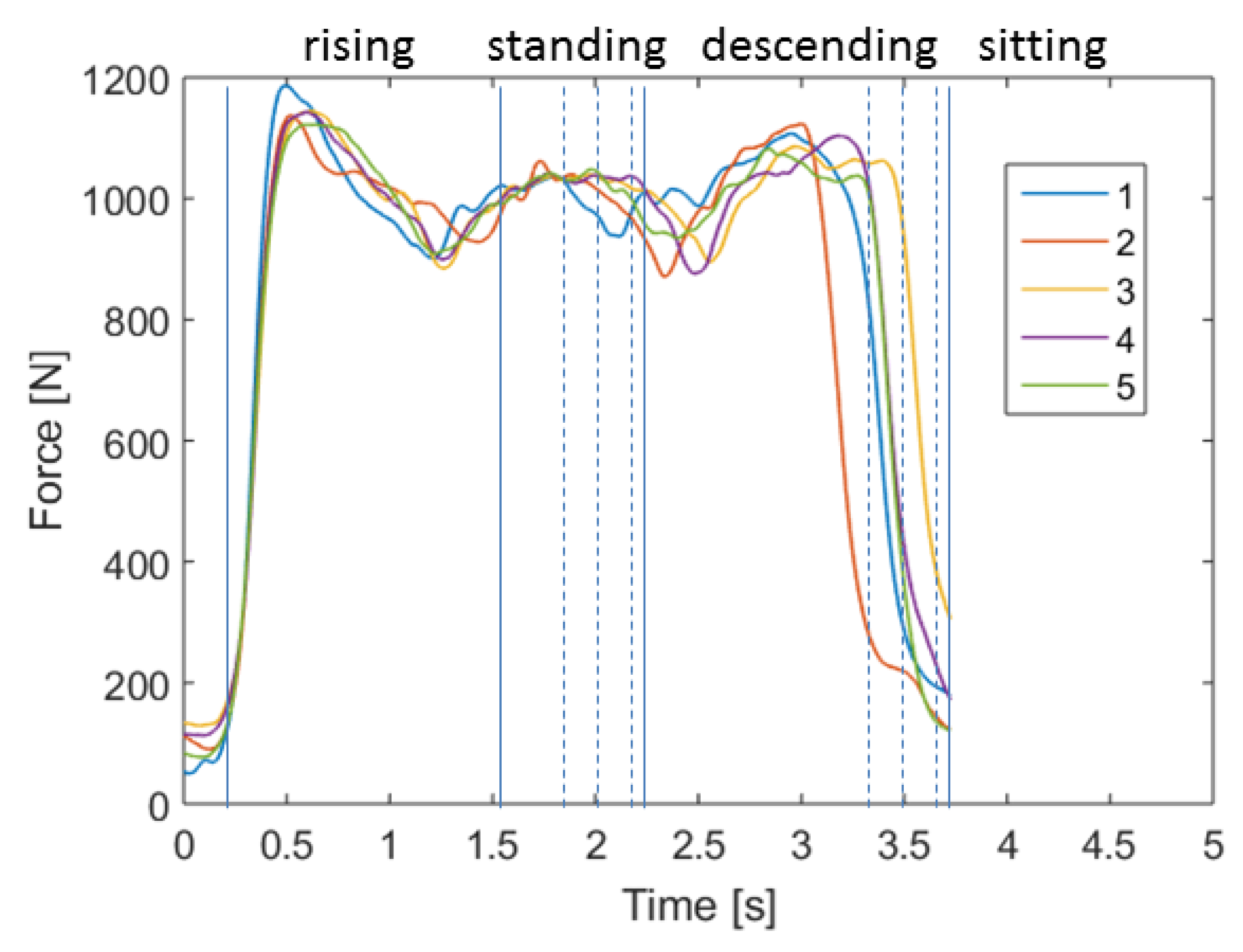
3.6. Investigation of Movement Patterns
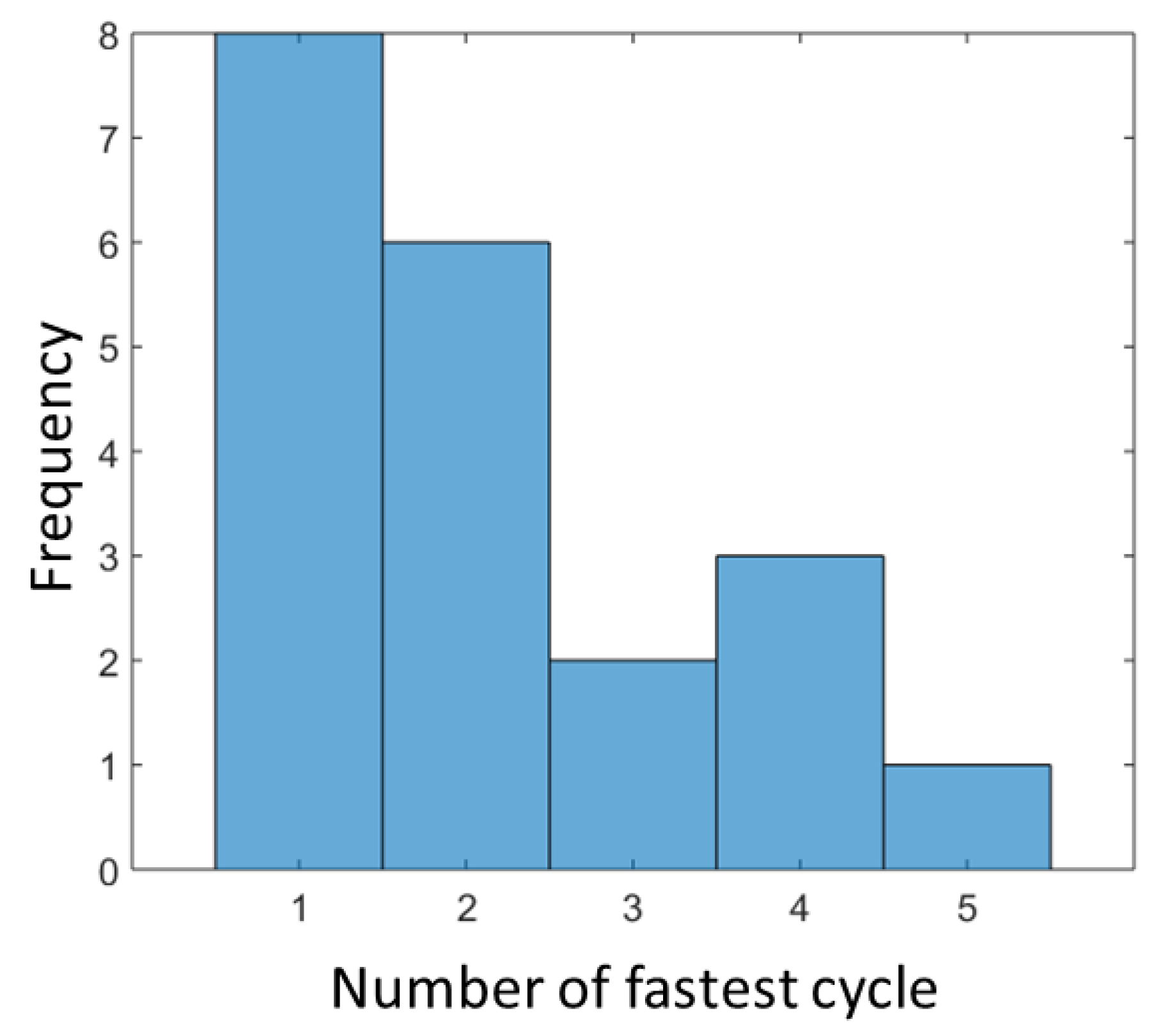
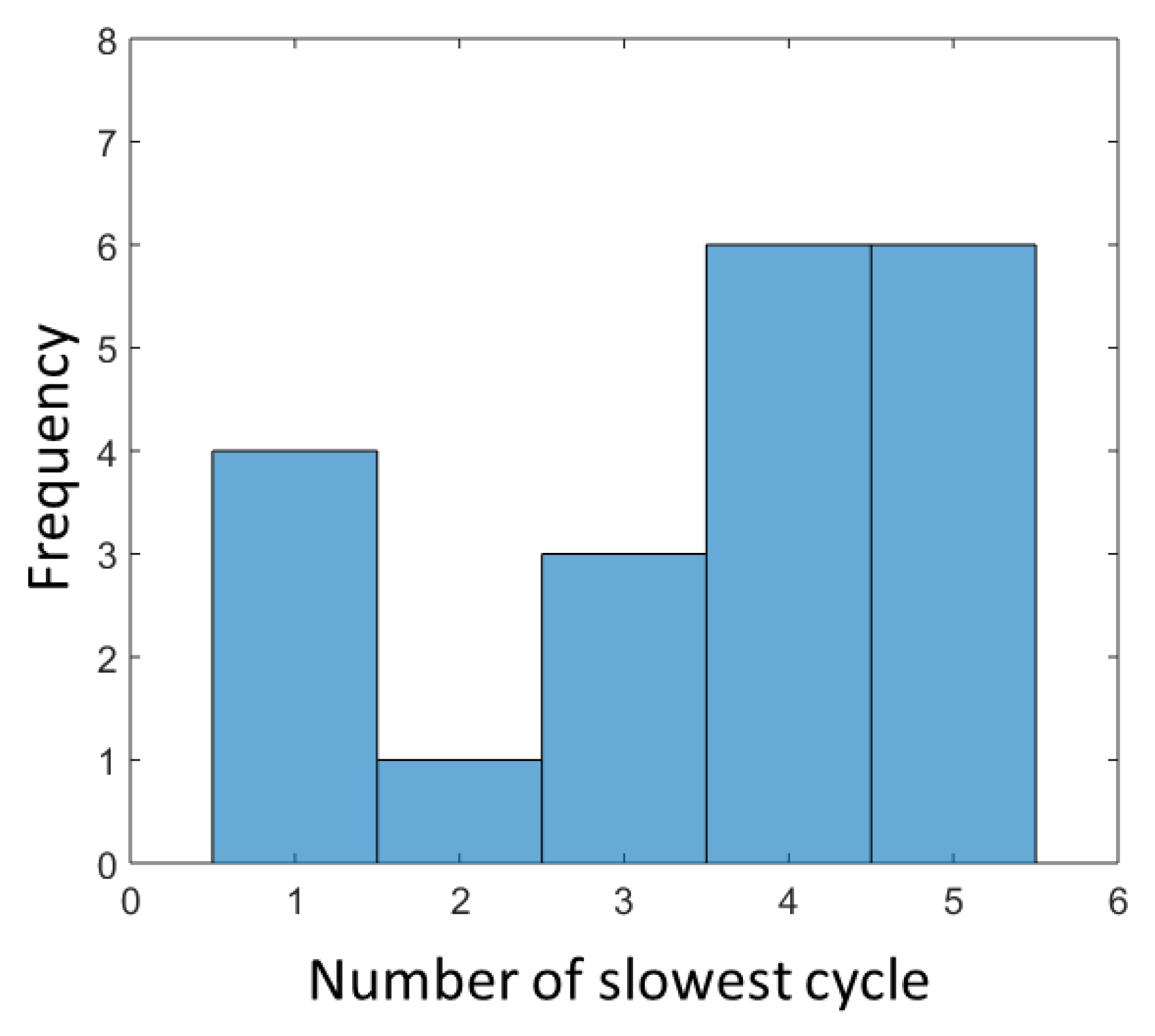
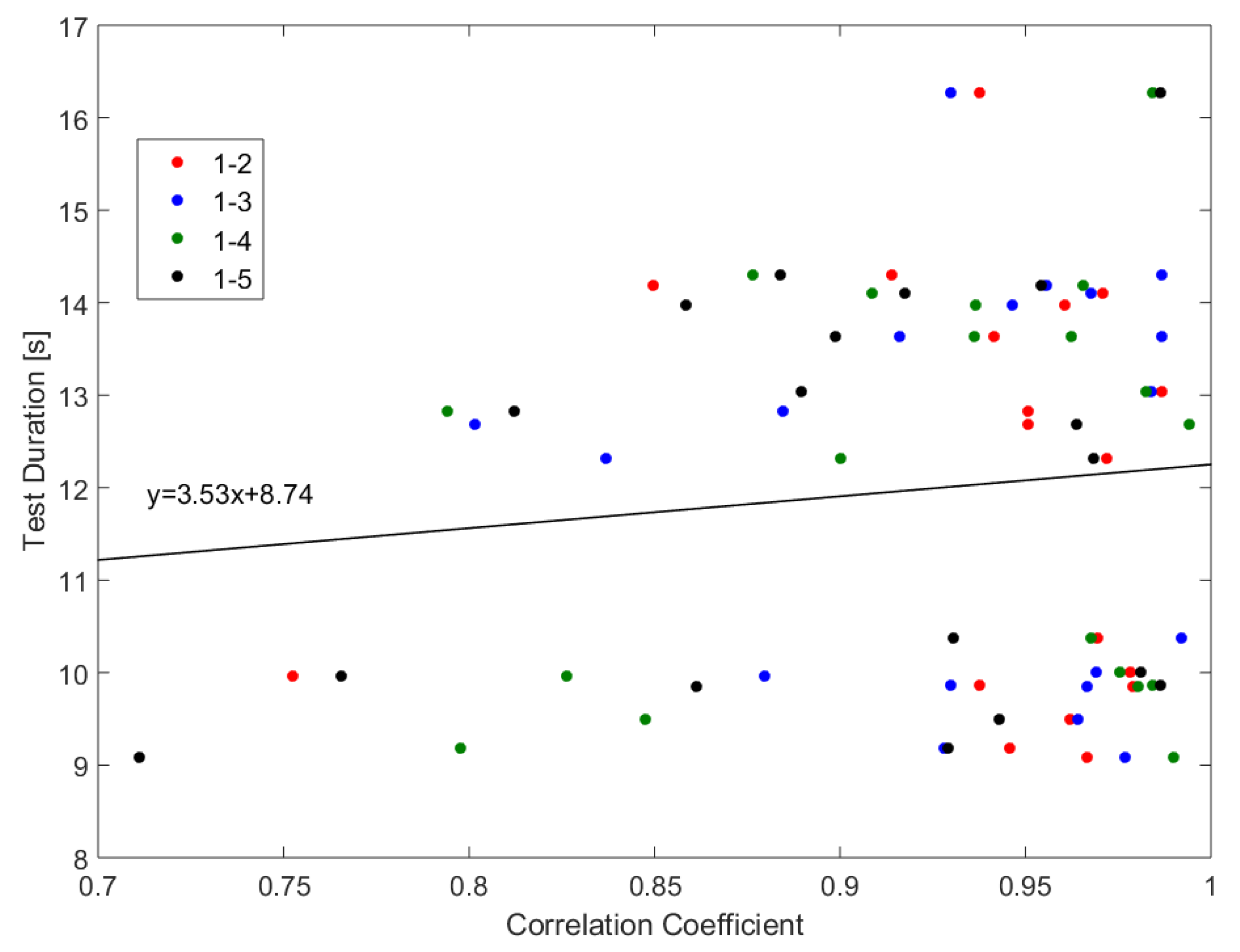
3.6.1. Intrapersonal-Variability: Cycles of the Same Participant
3.6.2. Interpersonal-Variability: Cycles of Different Participants
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Grady, P.A. Advancing the health of our aging population: A lead role for nursing science. Nurs. Outlook 2011, 59, 207. [Google Scholar] [CrossRef] [PubMed]
- Beaton, K.; Grimmer, K. Tools that assess functional decline: Systematic literature review update. Clin. Interv. Aging 2013, 8, 485. [Google Scholar] [CrossRef] [PubMed]
- Hellmers, S.; Steen, E.E.; Dasenbrock, L.; Heinks, A.; Bauer, J.M.; Fudickar, S.; Hein, A. Towards a minimized unsupervised technical assessment of physical performance in domestic environments. In Proceedings of the 11th EAI International Conference on Pervasive Computing Technologies for Healthcare, Barcelona, Spain, 23–26 May 2017; ACM: New York, NY, USA, 2017; pp. 207–216. [Google Scholar] [CrossRef]
- Bean, J.F.; Leveille, S.G.; Kiely, D.K.; Bandinelli, S.; Guralnik, J.M.; Ferrucci, L. A comparison of leg power and leg strength within the InCHIANTI study: which influences mobility more? J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2003, 58, M728–M733. [Google Scholar] [CrossRef]
- Hardy, R.; Cooper, R.; Shah, I.; Harridge, S.; Guralnik, J.; Kuh, D. Is chair rise performance a useful measure of leg power? Aging Clin. Exp. Res. 2010, 22, 412. [Google Scholar] [CrossRef] [PubMed]
- Takai, Y.; Ohta, M.; Akagi, R.; Kanehisa, H.; Kawakami, Y.; Fukunaga, T. Sit-to-stand test to evaluate knee extensor muscle size and strength in the elderly: A novel approach. J. Physiol. Anthropol. 2009, 28, 123–128. [Google Scholar] [CrossRef]
- Kanehisa, H.; Fukunaga, T. Age-related change in sit-to-stand power in Japanese women aged 50 years or older. J. Physiol. Anthropol. 2014, 33, 26. [Google Scholar] [CrossRef]
- Ganea, R.; Paraschiv-lonescu, A.; Aminian, K. Detection and classification of postural transitions in real-world conditions. IEEE Trans. Neural Syst. Rehabil. Eng. 2012, 20, 688–696. [Google Scholar] [CrossRef]
- Regterschot, G.R.H.; Folkersma, M.; Zhang, W.; Baldus, H.; Stevens, M.; Zijlstra, W. Sensitivity of sensor-based sit-to-stand peak power to the effects of training leg strength, leg power and balance in older adults. Gait Posture 2014, 39, 303–307. [Google Scholar] [CrossRef] [Green Version]
- Greene, B.R.; Doheny, E.P.; Kenny, R.A.; Caulfield, B. Classification of frailty and falls history using a combination of sensor-based mobility assessments. Physiol. Meas. 2014, 35, 2053. [Google Scholar] [CrossRef]
- Millor, N.; Lecumberri, P.; Gómez, M.; Martínez-Ramírez, A.; Izquierdo, M. An evaluation of the 30-s chair stand test in older adults: Frailty detection based on kinematic parameters from a single inertial unit. J. Neuroeng. Rehabil. 2013, 10, 86. [Google Scholar] [CrossRef]
- Schwenk, M.; Gogulla, S.; Englert, S.; Czempik, A.; Hauer, K. Test–retest reliability and minimal detectable change of repeated sit-to-stand analysis using one body fixed sensor in geriatric patients. Physiol. Meas. 2012, 33, 1931–1946. [Google Scholar] [CrossRef] [PubMed]
- Kanai, A.; Kiyama, S.; Goto, H.; Tomita, H.; Tanaka, A.; Kunimi, M.; Okada, T.; Nakai, T. Use of the sit-to-stand task to evaluate motor function of older adults using telemetry. BMC Geriatr. 2016, 16, 121. [Google Scholar] [CrossRef] [PubMed]
- Chorin, F.; Cornu, C.; Beaune, B.; Frère, J.; Rahmani, A. Sit to stand in elderly fallers vs non-fallers: new insights from force platform and electromyography data. Aging Clin. Exp. Res. 2016, 28, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Lindemann, U.; Muche, R.; Stuber, M.; Zijlstra, W.; Hauer, K.; Becker, C. Coordination of strength exertion during the chair-rise movement in very old people. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2007, 62, 636–640. [Google Scholar] [CrossRef]
- Zijlstra, A.; Chiari, L.; Mancini, M.; Lindemann, U.; Zijlstra, W. Sit-stand and stand-sit transitions in older adults and patients with Parkinson’s disease: event detection based on motion sensors versus force plates. J. Neuroeng. Rehabil. 2012, 9, 75. [Google Scholar] [CrossRef] [PubMed]
- Ganea, R.; Paraschiv-Ionescu, A.; Büla, C.; Rochat, S.; Aminian, K. Multi-parametric evaluation of sit-to-stand and stand-to-sit transitions in elderly people. Med. Eng. Phys. 2011, 33, 1086–1093. [Google Scholar] [CrossRef] [PubMed]
- Kerr, K.; White, J.; Barr, D.; Mollan, R. Analysis of the sit-stand-sit movement cycle in normal subjects. Clin. Biomech. 1997, 12, 236–245. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Ferrucci, L.; Pieper, C.F.; Leveille, S.G.; Markides, K.S.; Ostir, G.V.; Studenski, S.; Berkman, L.F.; Wallace, R.B. Lower Extremity Function and Subsequent Disability: Consistency Across Studies, Predictive Models, and Value of Gait Speed Alone Compared with the Short Physical Performance Battery. J. Gerontol. Ser. 2000, 55, M221–M231. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Fudickar, S.; Kiselev, J.; Frenken, T.; Wegel, S.; Dimitrowska, S.; Steinhagen-Thiessen, E.; Hein, A. Validation of the ambient TUG chair with light barriers and force sensors in a clinical trial. Assist. Technol. 2018, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Troosters, T.; Gosselink, R.; Decramer, M. Six minute walking distance in healthy elderly subjects. Eur. Respir. J. 1999, 14, 270–274. [Google Scholar] [CrossRef] [Green Version]
- De Morton, N.A.; Lane, K. Validity and reliability of the de Morton Mobility Index in the subacute hospital setting in a geriatric evaluation and management population. J. Rehabil. Med. 2010, 42, 956–961. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hellmers, S.; Kromke, T.; Dasenbrock, L.; Heinks, A.; Bauer, J.M.; Hein, A.; Fudickar, S. Stair Climb Power Measurements via Inertial Measurement Units—Towards an Unsupervised Assessment of Strength in Domestic Environments. In HEALTHINF, Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies, Funchal, Portugal, 19–21 January 2018; INSTICC, SciTePress: Setúbal, Portugal, 2018; Volume 5, pp. 39–47. [Google Scholar] [CrossRef]
- Bean, J.F.; Kiely, D.K.; LaRose, S.; Alian, J.; Frontera, W.R. Is stair climb power a clinically relevant measure of leg power impairments in at-risk older adults? Arch. Phys. Med. Rehabil. 2007, 88, 604–609. [Google Scholar] [CrossRef]
- Runge, M.; Rittweger, J.; Russo, C.R.; Schiessl, H.; Felsenberg, D. Is muscle power output a key factor in the age-related decline in physical performance? A comparison of muscle cross section, chair-rising test and jumping power. Clin. Physiol. Funct. Imaging 2004, 24, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Hellmers, S.; Fudickar, S.; Büse, C.; Dasenbrock, L.; Heinks, A.; Bauer, J.M.; Hein, A. Technology Supported Geriatric Assessment. In Ambient Assisted Living: 9. AAL-Kongress, Frankfurt/M, Germany, April 20–21, 2016; Wichert, R., Mand, B., Eds.; Springer: Cham, Switzerland, 2017; pp. 85–100. [Google Scholar]
- Hellmers, S.; Izadpanah, B.; Dasenbrock, L.; Diekmann, R.; Bauer, J.; Hein, A.; Fudickar, S. Towards an Automated Unsupervised Mobility Assessment for Older People Based on Inertial TUG Measurements. Sensors 2018, 18, 3310. [Google Scholar] [CrossRef] [PubMed]
- Figo, D.; Diniz, P.C.; Ferreira, D.R.; Cardoso, J.M. Preprocessing techniques for context recognition from accelerometer data. Pers. Ubiquitous Comput. 2010, 14, 645–662. [Google Scholar] [CrossRef] [Green Version]
- Mukaka, M.M. A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar]
- Frykberg, G.E.; Häger, C.K. Movement analysis of sit-to-stand–research informing clinical practice. Phys. Ther. Rev. 2015, 20, 156–167. [Google Scholar] [CrossRef]
- Gross, M.; Stevenson, P.; Charette, S.; Pyka, G.; Marcus, R. Effect of muscle strength and movement speed on the biomechanics of rising from a chair in healthy elderly and young women. Gait Posture 1998, 8, 175–185. [Google Scholar] [CrossRef] [Green Version]
- Schenkman, M.; Berger, R.A.; Riley, P.O.; Mann, R.W.; Hodge, W.A. Whole-body movements during rising to standing from sitting. Phys. Ther. 1990, 70, 638–648. [Google Scholar] [CrossRef] [PubMed]
- Allen, F.R.; Ambikairajah, E.; Lovell, N.H.; Celler, B.G. Classification of a known sequence of motions and postures from accelerometry data using adapted Gaussian mixture models. Physiol. Meas. 2006, 27, 935. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Dallas, T. Feature selection and activity recognition system using a single triaxial accelerometer. IEEE Trans. Biomed. Eng. 2014, 61, 1780–1786. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, A.; Chavis, M.; Watkins, J.; Wilson, T. The five-times-sit-to-stand test: Validity, reliability and detectable change in older females. Aging Clin. Exp. Res. 2012, 24, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Blackwood, J. Reliability, Validity and Minimal Detectable Change in the Timed Up and Go and Five Times Sit to Stand Tests in Older Adults with Early Cognitive Loss. J. Physiother. Rehabil. 2017, 1, 1–5. [Google Scholar]
- Roldán-Jiménez, C.; Bennett, P.; Cuesta-Vargas, A.I. Muscular activity and fatigue in lower-limb and trunk muscles during different sit-to-stand tests. PLoS ONE 2015, 10, e0141675. [Google Scholar] [CrossRef]
- Cuesta-Vargas, A.I.; González-Sánchez, M. Differences in muscle activation patterns during sit to stand task among subjects with and without intellectual disability. Biomed. Res. Int. 2013, 2013, 173148. [Google Scholar] [CrossRef]
- Kale, N.; Lee, J.; Lotfian, R.; Jafari, R. Impact of sensor misplacement on dynamic time warping based human activity recognition using wearable computers. In Proceedings of the Conference on Wireless Health, San Diego, CA, USA, 23–25 October 2012; ACM: New York, NY, USA, 2012; p. 7. [Google Scholar] [CrossRef]








| Score | Test Duration |
|---|---|
| 4 points | ≤11.19 s |
| 3 points | 11.20–13.69 s |
| 2 points | 13.70–16.69 s |
| 1 point | 16.70–60 s |
| 0 points | >60 s or are unable to complete 5 rises |
| Min | Max | Mean | SD | |
|---|---|---|---|---|
| age [years] | 72 | 89 | 78.2 | 4.6 |
| weight [kg] | 55.85 | 101.20 | 78.83 | 12.41 |
| height [cm] | 145.8 | 188.2 | 165.19 | 11.32 |
| 5CRT [s] | 9.08 | 16.27 | 12.04 | 2.26 |
| Classifier | Method | Window Size (s) | Step Width (s) | Filter | Feature-Set |
|---|---|---|---|---|---|
| State | Boosted Decision Trees | 1.405 | 0.072 | Low pass ( = 6.1 Hz) | AC, C, Mean (Acc), RMS, SD, SE (Acc + Gyro) |
| Static | Multilayer Perceptrons (5 HL, 7 HN) | 2.511 | 0.427 | - | Mean, SMA (Acc), Pitch, AC, C (Acc + Gyro) |
| Transition | Multilayer Perceptrons (4 HL, 40 HN) | 1.135 | 0.073 | Low pass ( = 4.5 Hz) | RMS (Acc), Mean, SE (Gyro), AC, C, SMA, SD (Acc+Gyro), Pitch |
| Duration of | TUG | Walk Test | SCPT |
|---|---|---|---|
| 1. sit-to-stand | 0.02 * | 0.09 | 0.75 |
| 1. stand-to-sit | 0.39 | 0.26 | 0.23 |
| last sit-to-stand | 0.22 | 0.46 | 0.88 |
| last stand-to-sit | 0.17 | 0.11 | 0.32 |
| average sit-to-stand | 0.02 * | 0.09 | 0.89 |
| average stand-to-sit | 0.22 | 0.32 | 0.64 |
| five time chair rise test | 0.59 | 0.67 | 0.71 |
| Cycle | 1–2 | 1–3 | 1–4 | 1–5 |
|---|---|---|---|---|
| min | 0.75 | 0.8 | 0.79 | 0.71 |
| max | 0.98 | 0.99 | 0.99 | 0.99 |
| mean | 0.95 | 0.94 | 0.93 | 0.92 |
| median | 0.96 | 0.96 | 0.96 | 0.96 |
| SD | 0.06 | 0.05 | 0.07 | 0.08 |
| range | 0.23 | 0.19 | 0.20 | 0.28 |
| Min | Max | Mean | Median | SD | Range |
|---|---|---|---|---|---|
| 0.65 | 1 | 0.88 | 0.88 | 0.09 | 0.34 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hellmers, S.; Fudickar, S.; Lau, S.; Elgert, L.; Diekmann, R.; Bauer, J.M.; Hein, A. Measurement of the Chair Rise Performance of Older People Based on Force Plates and IMUs. Sensors 2019, 19, 1370. https://doi.org/10.3390/s19061370
Hellmers S, Fudickar S, Lau S, Elgert L, Diekmann R, Bauer JM, Hein A. Measurement of the Chair Rise Performance of Older People Based on Force Plates and IMUs. Sensors. 2019; 19(6):1370. https://doi.org/10.3390/s19061370
Chicago/Turabian StyleHellmers, Sandra, Sebastian Fudickar, Sandra Lau, Lena Elgert, Rebecca Diekmann, Jürgen M. Bauer, and Andreas Hein. 2019. "Measurement of the Chair Rise Performance of Older People Based on Force Plates and IMUs" Sensors 19, no. 6: 1370. https://doi.org/10.3390/s19061370
APA StyleHellmers, S., Fudickar, S., Lau, S., Elgert, L., Diekmann, R., Bauer, J. M., & Hein, A. (2019). Measurement of the Chair Rise Performance of Older People Based on Force Plates and IMUs. Sensors, 19(6), 1370. https://doi.org/10.3390/s19061370






