Influence of BMI on Gait Characteristics of Young Adults: 3D Evaluation Using Inertial Sensors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Acquisition System
2.3. Test Protocol and System Calibration
- (1).
- Anatomical measurements of pelvis breadth, thigh height, shank height, and sphyrion height.
- (2).
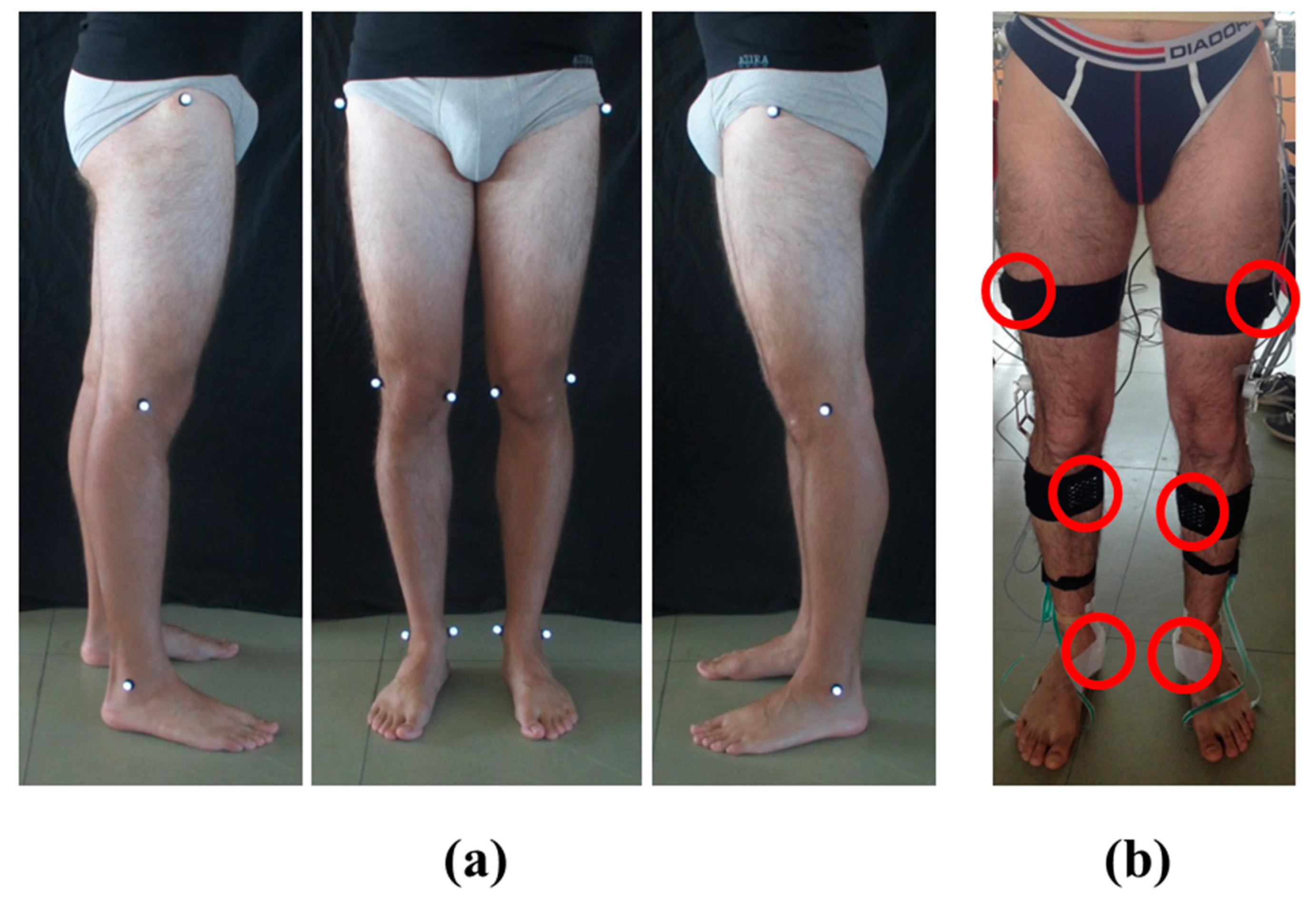
- Placement of reflective markers, bilaterally, on the anatomical representative points: greater trochanter, lateral epicondyle of the femur, medial epicondyle of the femur, lateral malleolus and medial malleolus. Three photos were shot from the front, left, and right sides of the subject (Figure 1a). The markers were removed.
- (3).
- Fixing of inertial sensors on subject’s pelvis and both lower limbs using elastic Velcro® bands and medical tape. The sensor on the pelvis was located posteriorly in the middle point between iliac crests. The six sensors on the lower limbs were positioned on the lateral side of the thighs, on the anterior side of the tibia, and below the medial malleolus, bilaterally [6,28,29] (Figure 1b).
- (4).
- Acquisition of H-Gait signals for three seconds, with the subject in sitting posture, and for another three seconds in upright standing posture.
2.4. Data Analysis
2.5. Statistical Analysis
3. Results
3.1. Spatio-Temporal Parameters
3.2. Joint Kinematics
4. Discussion
4.1. Spatio-Temporal Parameters
4.2. Joint Kinematics
4.3. Limitation
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| Aa | Area of ankle trajectory |
| Ak | Area of knee trajectory |
| BMI | Body Mass Index |
| HC | Heel contact |
| NW | Normal weight |
| OW | Overweight/obese |
| ROM | Range of motion |
| TO | Toe off |
| θa | Ankle opening angle between the left and right major axes |
| θk | Knee opening angle between the left and right major axes |
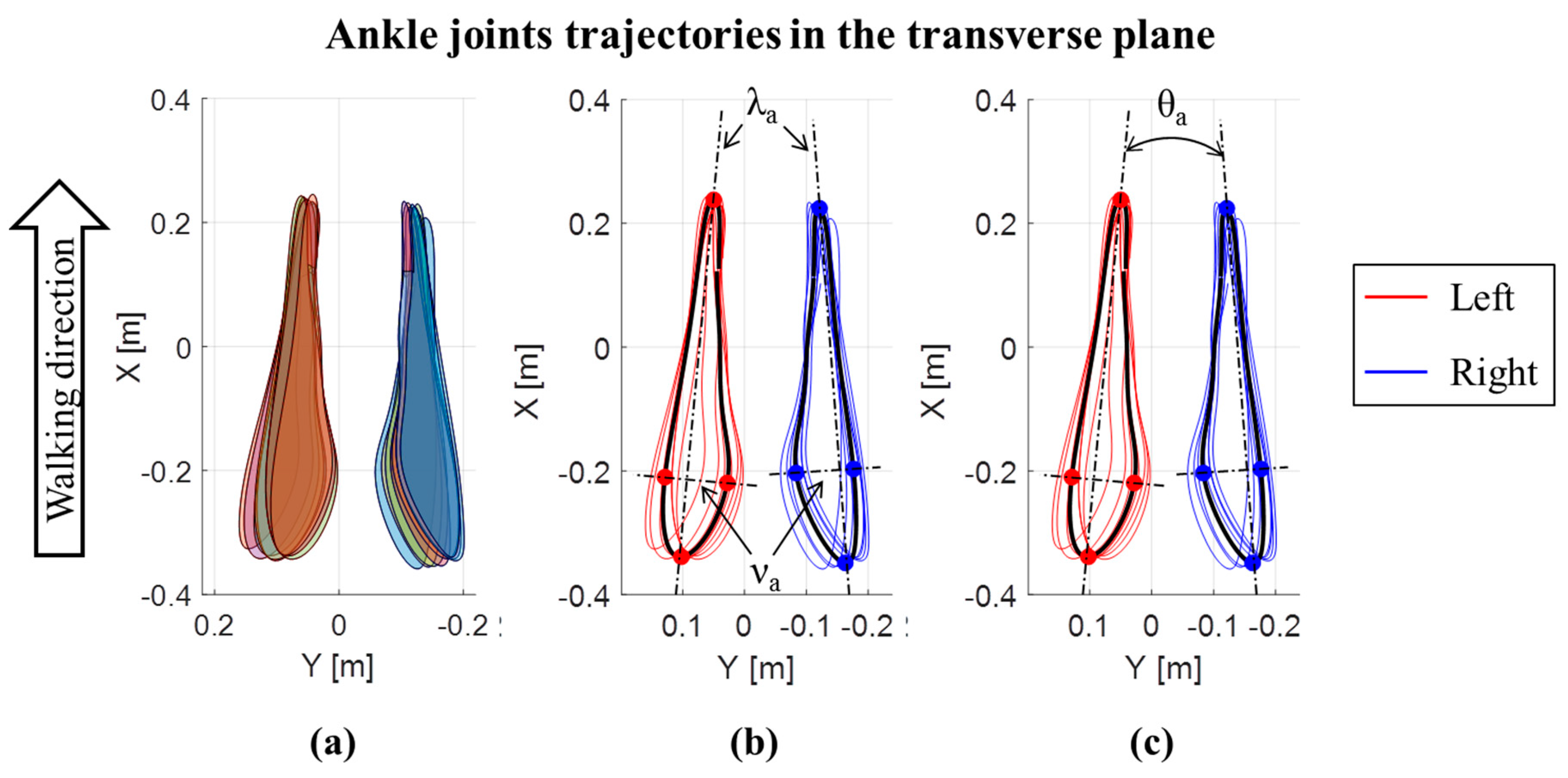
| λa | Major diameters of the average ankle trajectories |
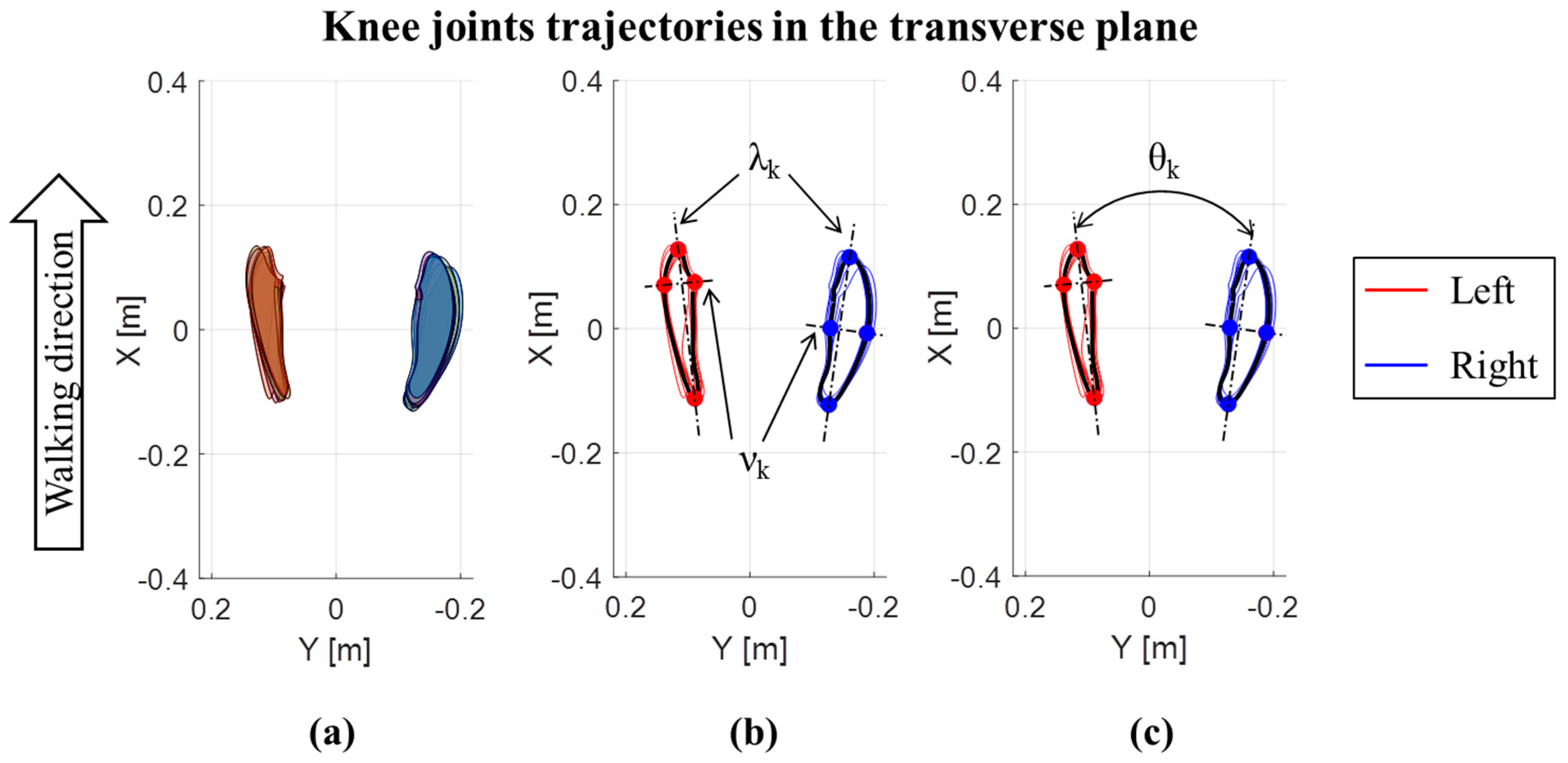
| λk | Major diameters of the average knee trajectories |
| νa | Minor diameters of the average ankle trajectories |
| νk | Minor diameters of the average knee trajectories |
References
- World Health Organization (WHO). Global Strategy on Diet, Physical Activity and Health. Available online: https://www.who.int/dietphysicalactivity/childhood_what/en/ (accessed on 3 June 2019).
- Browning, R.C.; Kram, R. Effects of obesity on the biomechanics of walking at different speeds. Med. Sci. Sports Exerc. 2007, 39, 1632–1641. [Google Scholar] [CrossRef] [PubMed]
- Lerner, Z.F.; Board, W.J.; Browning, R.C. Effects of obesity on lower extremity muscle function during walking at two speeds. Gait Posture 2014, 39, 978–984. [Google Scholar] [CrossRef] [PubMed]
- Runhaar, J.; Koes, B.W.; Clockaerts, S.; Bierma-Zeinstra, S.M.A. A systematic review on changed biomechanics of lower extremities in obese individuals: A possible role in development of osteoarthritis. Obes. Rev. 2011, 12, 1071–1082. [Google Scholar] [CrossRef] [PubMed]
- Aspden, R.M. Obesity punches above its weight in osteoarthritis. Nat. Rev. Rheumatol. 2011, 7, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Tadano, S.; Takeda, R.; Sasaki, K.; Fujisawa, T.; Tohyama, H. Gait characterization for osteoarthritis patients using wearable gait sensors (H-Gait systems). J. Biomech. 2016, 49, 684–690. [Google Scholar] [CrossRef] [PubMed]
- Winter, D.A. Biomechanics and Motor Control. of Human Gait: Normal, Elderly, and Pathological, 4th ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2009; ISBN 9780470549148. [Google Scholar]
- Agostini, V.; Lo Fermo, F.; Massazza, G.; Knaflitz, M. Does texting while walking really affect gait in young adults? J. Neuroeng. Rehabil. 2015, 12, 86. [Google Scholar] [CrossRef]
- Strazza, A.; Mengarelli, A.; Fioretti, S.; Burattini, L.; Agostini, V.; Knaflitz, M.; Di Nardo, F. Surface-EMG analysis for the quantification of thigh muscle dynamic co-contractions during normal gait. Gait Posture 2017, 51, 228–233. [Google Scholar] [CrossRef]
- Winter, D.A.; Patla, A.E.; Frank, J.S.; Walt, S.E. Biomechanical walking pattern changes in the fit and healthy elderly. Phys. Ther. 1990, 70, 340–347. [Google Scholar] [CrossRef]
- Gastaldi, L.; Lisco, G.; Pastorelli, S.; Dimanico, U. Effects of botulinum neurotoxin on spatio-temporal gait parameters of patients with chronic stroke: A prospective open-label study. Eur. J. Phys. Rehabil. Med. 2015, 51, 609–618. [Google Scholar]
- Agostini, V.; Knaflitz, M.; Nascimberi, A.; Gaffuri, A. Gait measurements in hemiplegic children: An automatic analysis of foot-floor contact sequences and electromyographic patterns. In Proceedings of the IEEE MeMeA 2014-IEEE International Symposium on Medical Measurements and Applications, Lisboa, Portugal, 11–12 June 2014. [Google Scholar]
- Agostini, V.; Lanotte, M.; Carlone, M.; Campagnoli, M.; Azzolin, I.; Scarafia, R.; Massazza, G.; Knaflitz, M. Instrumented gait analysis for an objective pre-/postassessment of tap test in normal pressure hydrocephalus. Arch. Phys. Med. Rehabil. 2015, 96, 1235–1241. [Google Scholar] [CrossRef]
- Agostini, V.; Ganio, D.; Facchin, K.; Cane, L.; Moreira Carneiro, S.; Knaflitz, M. Gait parameters and muscle activation patterns at 3, 6 and 12 months after total hip arthroplasty. J. Arthroplast. 2014, 29, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Agostini, V.; De Luca, R.; Mansin, L.C.; Knaflitz, M. Reduction of gait abnormalities in type 2 diabetic patients due to physical activity: A quantitative evaluation based on statistical gait analysis. J. Mech. Med. Biol. 2012, 12, 1240025. [Google Scholar] [CrossRef]
- Leardini, A.; Chiari, A.; Della Croce, U.; Cappozzo, A. Human movement analysis using stereophotogrammetry Part 3. Soft tissue artifact assessment and compensation. Gait Posture 2005, 21, 212–225. [Google Scholar] [CrossRef] [PubMed]
- Aminian, K.; Najafi, B. Capturing human motion using body-fixed sensors: Outdoor measurement and clinical applications. Comput. Animat. Virtual Worlds 2004, 15, 79–94. [Google Scholar] [CrossRef]
- Carcreff, L.; Gerber, C.N.; Paraschiv-Ionescu, A.; De Coulon, G.; Newman, C.J.; Armand, S.; Aminian, K. What is the best configuration of wearable sensors to measure spatiotemporal gait parameters in children with cerebral palsy? Sensors 2018, 18, 394. [Google Scholar] [CrossRef] [PubMed]
- Sabatini, A.M.; Martelloni, C.; Scapellato, S.; Cavallo, F. Assessment of walking features from foot inertial sensing. IEEE Trans. Biomed. Eng. 2005, 52, 486–494. [Google Scholar] [CrossRef] [PubMed]
- Seel, T.; Raisch, J.; Schauer, T. IMU-based joint angle measurement for gait analysis. Sensors 2014, 14, 6891–6909. [Google Scholar] [CrossRef] [PubMed]
- Moufawad El Achkar, C.; Lenoble-Hoskovec, C.; Paraschiv-Ionescu, A.; Major, K.; Büla, C.; Aminian, K. Physical behavior in older persons during daily life: Insights from instrumented shoes. Sensors 2016, 16, 1225. [Google Scholar] [CrossRef]
- Schlachetzki, J.C.M.; Barth, J.; Marxreiter, F.; Gossler, J.; Kohl, Z.; Reinfelder, S.; Gassner, H.; Aminian, K.; Eskofier, B.M.; Winkler, J.; et al. Wearable sensors objectively measure gait parameters in Parkinson’s disease. PLoS ONE 2017, 12, e0183989. [Google Scholar] [CrossRef]
- Zijlstra, W.; Hof, A.L. Assessment of spatio-temporal gait parameters from trunk accelerations during human walking. Gait Posture 2003, 18, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Trojaniello, D.; Cereatti, A.; Pelosin, E.; Avanzino, L.; Mirelman, A.; Hausdorff, J.M.; Della Croce, U. Estimation of step-by-step spatio-temporal parameters of normal and impaired gait using shank-mounted magneto-inertial sensors: Application to elderly, hemiparetic, parkinsonian and choreic gait. J. Neuroeng. Rehabil. 2014, 11, 152. [Google Scholar] [CrossRef] [PubMed]
- Meng, H.; O’Connor, D.P.; Lee, B.C.; Layne, C.S.; Gorniak, S.L. Alterations in over-ground walking patterns in obese and overweight adults. Gait Posture 2017, 53, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Tadano, S.; Takeda, R.; Miyagawa, H. Three dimensional gait analysis using wearable acceleration and gyro sensors based on quaternion calculations. Sensors 2013, 13, 9321–9343. [Google Scholar] [CrossRef] [PubMed]
- Takeda, R.; Lisco, G.; Fujisawa, T.; Gastaldi, L.; Tohyama, H.; Tadano, S. Drift Removal for Improving the Accuracy of Gait Parameters Using Wearable Sensor Systems. Sensors 2014, 14, 23230–23247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agostini, V.; Gastaldi, L.; Rosso, V.; Knaflitz, M.; Tadano, S. A wearable magneto-inertial system for gait analysis (H-gait): Validation on normalweight and overweight/obese young healthy adults. Sensors 2017, 17, 2406. [Google Scholar] [CrossRef] [PubMed]
- Gastaldi, L.; Rosso, V.; Gabola, V.; Agostini, V.; Frutos, M.M.L.; Knaflitz, M.; Takeda, R.; Tadano, S. Technical challenges using magneto-inertial sensors for gait analysis. In Proceedings of the 2016 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Benevento, Italy, 15–18 May 2016; pp. 274–279. [Google Scholar]
- Takeda, R.; Tadano, S.; Natorigawa, A.; Todoh, M.; Yoshinari, S. Gait posture estimation using wearable acceleration and gyro sensors. J. Biomech. 2009, 42, 2486–2494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosso, V.; Gastaldi, L.; Agostini, V.; Takeda, R.; Tadano, S. Gait measurements in the transverse plane using a wearable system: An experimental study of test-retest reliability. In Proceedings of the I2MTC 2017 IEEE International Instrumentation and Measurement Technology Conference, Turin, Italy, 22–25 May 2017. [Google Scholar]
- Spyropoulos, P.; Pisciotta, J.C.; Pavlou, K.N.; Cairns, M.A.; Simon, S.R. Biomechanical gait analysis in obese men. Arch. Phys. Med. Rehabil. 1991, 72, 1065–1070. [Google Scholar]
- DeVita, P.; Hortobágyi, T. Obesity is not associated with increased knee joint torque and power during level walking. J. Biomech. 2003, 36, 1355–1362. [Google Scholar] [CrossRef]
- Wearing, S.C.; Hennig, E.M.; Byrne, N.M.; Steele, J.R.; Hills, A.P. The biomechanics of restricted movement in adult obesity. Obes. Rev. 2006, 7, 13–24. [Google Scholar] [CrossRef]
- Lai, P.P.K.; Leung, A.K.L.; Li, A.N.M.; Zhang, M. Three-dimensional gait analysis of obese adults. Clin. Biomech. 2008, 23, S2–S6. [Google Scholar] [CrossRef]
- Browning, R.C.; Baker, E.A.; Herron, J.A.; Kram, R. Effects of obesity and sex on the energetic cost and preferred speed of walking. J. Appl. Physiol. 2006, 100, 390–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Browning, R.C.; Kram, R. Energetic cost and preferred speed of walking in obese vs. normal weight women. Obes. Res. 2005, 13, 891–899. [Google Scholar] [CrossRef] [PubMed]
- Westlake, C.G.; Milner, C.E.; Zhang, S.; Fitzhugh, E.C. Do thigh circumference and mass changes alter knee biomechanics during walking? Gait Posture 2013, 37, 359–362. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.H.; Park, J.M.; Kwon, O.Y. Gender differences in three dimensional gait analysis data from 98 healthy Korean adults. Clin. Biomech. 2004, 191, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Freedman Silvernail, J.; Milner, C.E.; Thompson, D.; Zhang, S.; Zhao, X. The influence of body mass index and velocity on knee biomechanics during walking. Gait Posture 2013, 37, 575–579. [Google Scholar] [CrossRef] [PubMed]
- Messier, S.P.; Davies, A.B.; Moore, D.T.; Davis, S.E.; Pack, R.J.; Kazmar, S.C. Severe obesity: Effects on foot mechanics during walking. Foot Ankle Int. 1994, 15, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Sharma, L.; Lou, C.; Cahue, S.; Dunlop, D.D. The mechanism of the effect of obesity in knee osteoarthritis: The mediating role of malalignment. Arthritis Rheum. 2000, 43, 568–575. [Google Scholar] [CrossRef]
- Laughton, C.A.; Slavin, M.; Katdare, K.; Nolan, L.; Bean, J.F.; Kerrigan, D.C.; Phillips, E.; Lipsitz, L.A.; Collins, J.J. Aging, muscle activity, and balance control: Physiologic changes associated with balance impairment. Gait Posture 2003, 18, 101–108. [Google Scholar] [CrossRef]
- Molina-Garcia, P.; Migueles, J.H.; Cadenas-Sanchez, C.; Esteban-Cornejo, I.; Mora-Gonzalez, J.; Rodriguez-Ayllon, M.; Plaza-Florido, A.; Vanrenterghem, J.; Ortega, F.B. A systematic review on biomechanical characteristics of walking in children and adolescents with overweight/obesity: Possible implications for the development of musculoskeletal disorders. Obes. Rev. 2019, 20, 1033–1044. [Google Scholar] [CrossRef]
- Robert-Lachaine, X.; Mecheri, H.; Larue, C.; Plamondon, A. Validation of inertial measurement units with an optoelectronic system for whole-body motion analysis. Med. Biol. Eng. Comput. 2017, 55, 609–619. [Google Scholar] [CrossRef]
| Parameter | NW | OW | p Value |
|---|---|---|---|
| Age (years) | 26 ± 1.5 | 26 ± 2.2 | 0.92 |
| Height (cm) | 180.0 ± 8.8 | 175.3 ± 7.6 | 0.16 |
| Weight (kg) | 74.3 ± 8.2 | 95.5 ± 12.4 | <0.001* |
| BMI (kg/m2) | 22.7 ± 1.2 | 31.1 ± 3.3 | <0.001* |
| Parameter | NW | OW | p Value |
|---|---|---|---|
| Walking speed (m/s) | 1.1 ± 0.1 | 1.0 ± 0.2 | 0.50 |
| Step length (cm) | 62.4 ± 5.1 | 56.5 ± 4.2 | 0.07 |
| Step width (cm) | 18.3 ± 9.0 | 18.7 ± 4.1 | 0.94 |
| Stride length (cm) | 123.5 ± 10.0 | 113.0 ± 8.3 | 0.10 |
| Cycle time (s) | 1.2 ± 0.2 | 1.1 ± 0.1 | 0.11 |
| Stance time (% gait cycle) | 55 ± 2 | 57 ± 2 | 0.14 |
| Cadence (stride/min) | 51.6 ± 4.9 | 53.8 ± 2.9 | 0.16 |
| Parameter | NW | OW | p Value | |
|---|---|---|---|---|
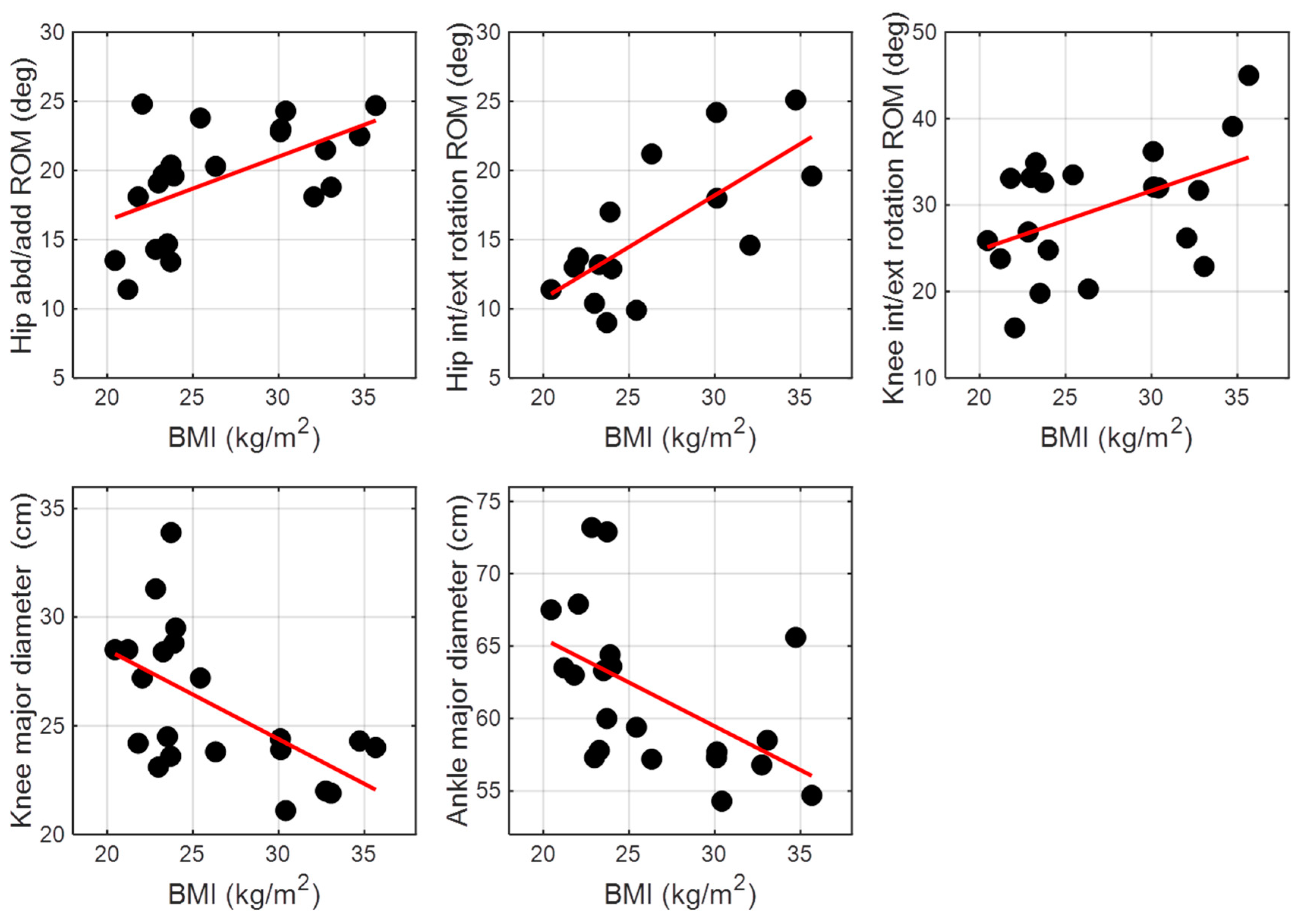
| Hip | Flexion/extension ROM (deg) | 34.7 ± 3.3 | 32.7 ± 3.4 | 0.16 |
| Abduction/adduction ROM (deg) | 17.2 ± 4.0 | 22.0 ± 2.3 | 0.01* | |
| Internal/external rotation ROM (deg) | 12.6 ± 2.4 | 18.9 ± 5.4 | 0.02* | |
| Knee | Flexion/extension ROM (deg) | 60.2 ± 6.7 | 60.7 ± 8.1 | 0.87 |
| Abduction/adduction ROM (deg) | 15.2 ± 3.9 | 15.3 ± 4.4 | 0.86 | |
| Internal/external rotation ROM (deg) | 27.1 ± 6.4 | 32.3 ± 9.9 | 0.24 | |
| Trajectory area, Ak (cm2) | 142.2 ± 44.4 | 133.8 ± 45.1 | 0.59 | |
| Major diameter, λk (cm) | 26.6 ± 3.6 | 23.9 ± 2.8 | 0.01* | |
| Minor diameter, νk (cm) | 6.8 ± 1.9 | 7.8 ± 2.2 | 0.43 | |
| Opening angle, θk (deg) | 5.3 ± 13.2 | 20.2 ± 9.8 | 0.02* | |
| Ankle | Flexion/extension ROM (deg) | 17.9 ± 3.6 | 18.1 ± 5.2 | 0.64 |
| Abduction/adduction ROM (deg) | 12.6 ± 2.6 | 15.2 ± 3.4 | 0.12 | |
| Internal/external rotation ROM (deg) | 19.4 ± 5.4 | 19.4 ± 2.0 | 0.76 | |
| Trajectory area, Aa (cm2) | 402.2 ± 112.3 | 361.7 ± 80.3 | 0.34 | |
| Major diameter, λa (cm) | 63.8 ± 5.2 | 57.0 ± 2.2 | 0.01* | |
| Minor diameter, νa (cm) | 9.2 ± 2.7 | 10.1 ± 1.4 | 0.32 | |
| Opening angle, θa (deg) | −10.1 ± 8.7 | −5.4 ± 12.9 | 0.56 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosso, V.; Agostini, V.; Takeda, R.; Tadano, S.; Gastaldi, L. Influence of BMI on Gait Characteristics of Young Adults: 3D Evaluation Using Inertial Sensors. Sensors 2019, 19, 4221. https://doi.org/10.3390/s19194221
Rosso V, Agostini V, Takeda R, Tadano S, Gastaldi L. Influence of BMI on Gait Characteristics of Young Adults: 3D Evaluation Using Inertial Sensors. Sensors. 2019; 19(19):4221. https://doi.org/10.3390/s19194221
Chicago/Turabian StyleRosso, Valeria, Valentina Agostini, Ryo Takeda, Shigeru Tadano, and Laura Gastaldi. 2019. "Influence of BMI on Gait Characteristics of Young Adults: 3D Evaluation Using Inertial Sensors" Sensors 19, no. 19: 4221. https://doi.org/10.3390/s19194221
APA StyleRosso, V., Agostini, V., Takeda, R., Tadano, S., & Gastaldi, L. (2019). Influence of BMI on Gait Characteristics of Young Adults: 3D Evaluation Using Inertial Sensors. Sensors, 19(19), 4221. https://doi.org/10.3390/s19194221






