Scanning Laser Rangefinders for the Unobtrusive Monitoring of Gait Parameters in Unsupervised Settings
Abstract
1. Introduction
2. Materials and Methods
2.1. Unobtrusive Gait Monitoring (UGMO)
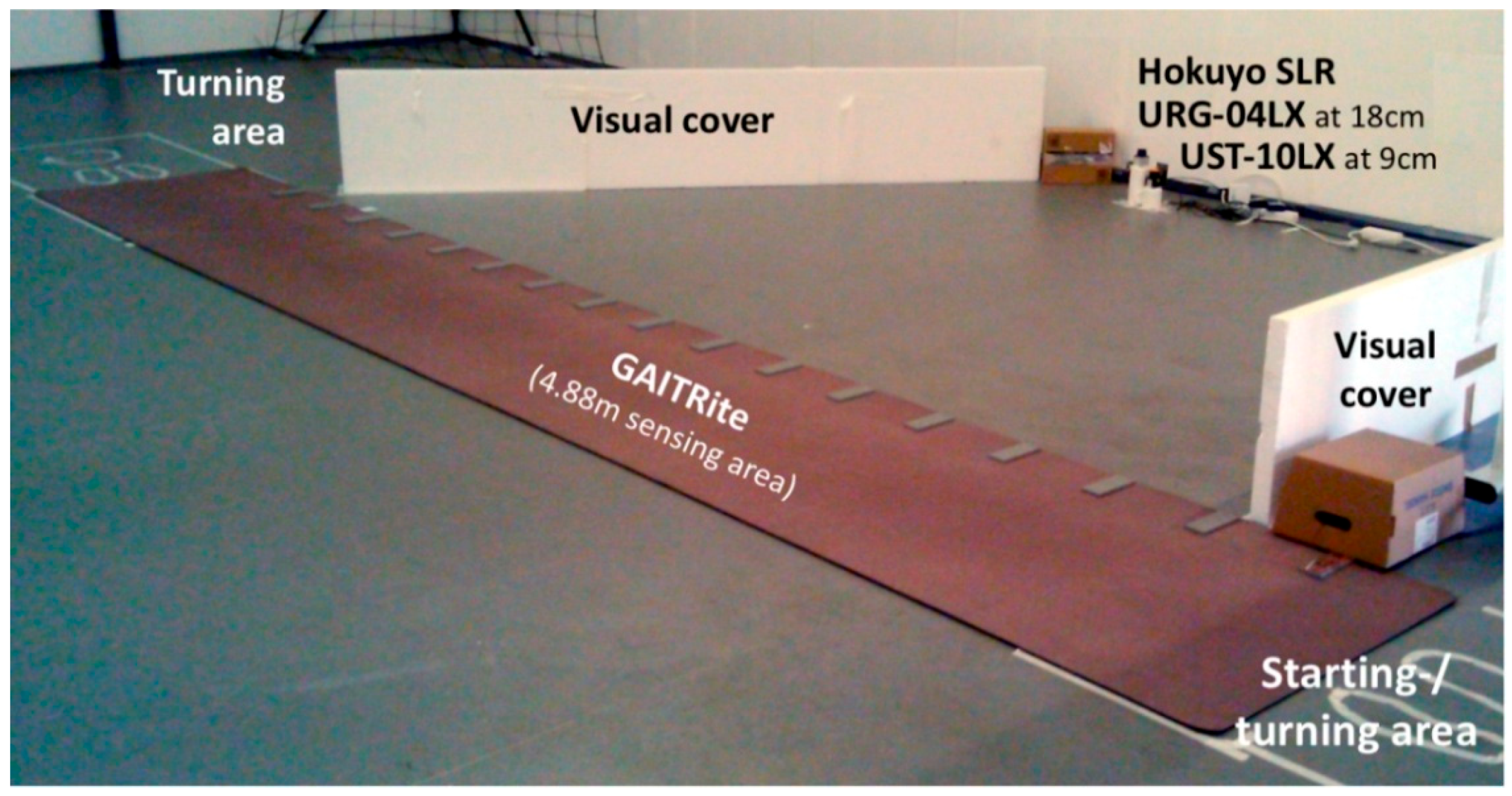
2.1.1. UGMO Hardware
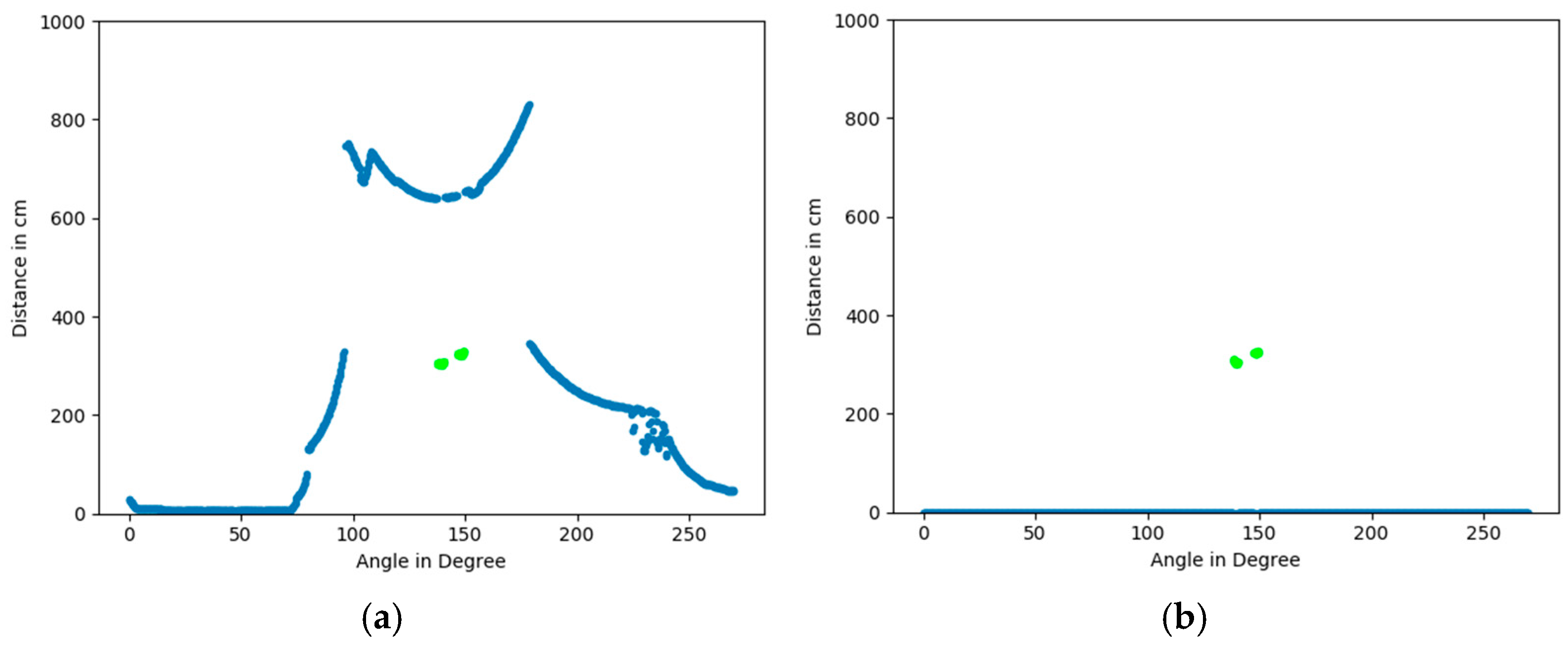
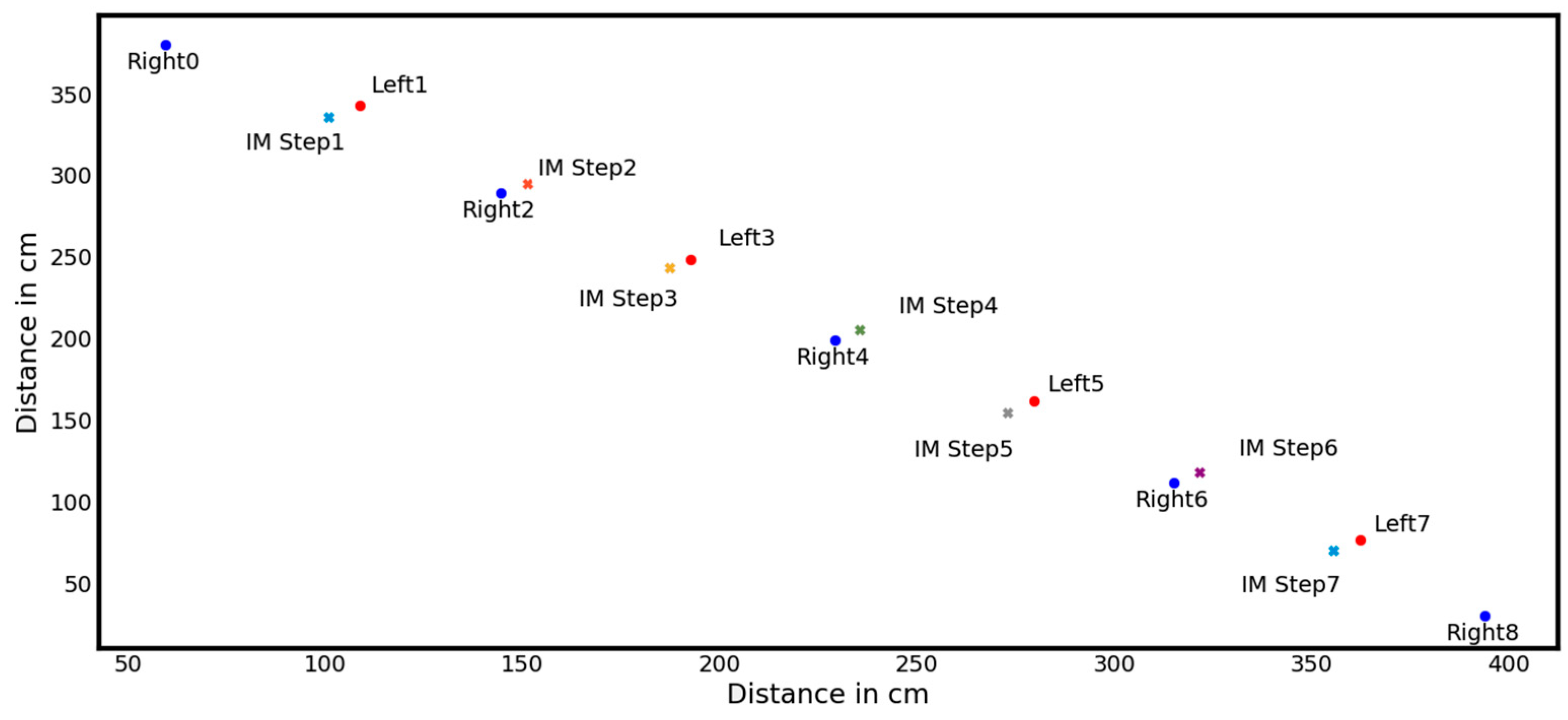
2.1.2. Signal-Processing
- Per walk: subject ID, timestamp, distance, cadence, speed (speed and GAITRite’s parameter of velocity are used synonymously);
- Per step: first contact time, last contact time, left/right stride length (cm), left/right stance phases (s), left/right swing phases.
2.2. Study Design
2.3. Methodology
3. Results
3.1. Descriptive Statistics
3.2. Influence of Scanning Laser Rangefinder (SLR) Frequencies and Resolution onto Step Detection Sensitivity
3.3. Sensitivity of Gait Parameters
- 75 walks (73 GAITRite and 2 SLR; 59 of them occurring in the fast pace group) had a distance of less than 3 m and thus were removed automatically (even though shorter distances can be expected to achieve reliable results either, we defined it as a min requirement to achieve comparability among the 4.88 m active GAITRite and the SLR).
- For 60 walks (0.8%; among them 48 of them occurred in the fast pace group) no gait parameters could be calculated due to an error in the SLR data representation.
- 9 walks (6 SLR and 3 GAITRite; all in the fast pace group) included stride-length of more than 2 m and thus were removed automatically
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Florence, C.S.; Bergen, G.; Atherly, A.; Burns, E.; Stevens, J.; Drake, C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J. Am. Geriatr. Soc. 2018, 66, 693–698. [Google Scholar] [CrossRef] [PubMed]
- Jager, T.E.; Weiss, H.B.; Coben, J.H.; Pepe, P.E. Traumatic brain injuries evaluated in U.S. emergency departments, 1992–1994. Acad. Emerg. Med. 2000, 7, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Jefferis, B.J.; Iliffe, S.; Kendrick, D.; Kerse, N.; Trost, S.; Lennon, L.T.; Ash, S.; Sartini, C.; Morris, R.W.; Wannamethee, S.G.; et al. How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC Geriatr. 2014, 14, 114. [Google Scholar] [CrossRef] [PubMed]
- Scheffer, A.C.; Schuurmans, M.J.; van Dijk, N.; van der Hooft, T.; de Rooij, S.E. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing 2008, 37, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Schepens, S.; Sen, A.; Painter, J.A.; Murphy, S.L. Relationship Between Fall-Related Efficacy and Activity Engagement in Community-Dwelling Older Adults: A Meta-Analytic Review. Am. J. Occup. Ther. 2012, 66, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Zijlstra, G.A.R.; Van Haastregt, J.C.M.; Van Rossum, E.; Van Eijk, J.T.M.; Yardley, L.; Kempen, G.I.J.M. Interventions to Reduce Fear of Falling in Community-Living Older People: A Systematic Review. J. Am. Geriatr. Soc. 2007, 55, 603–615. [Google Scholar] [CrossRef] [PubMed]
- Al-Aama, T. Falls in the elderly: Spectrum and prevention. Can. Fam. Physician 2011, 57, 771–776. [Google Scholar] [PubMed]
- Grobe, S.; Kakar, R.S.; Smith, M.L.; Mehta, R.; Baghurst, T.; Boolani, A. Impact of cognitive fatigue on gait and sway among older adults: A literature review. Prev. Med. Rep. 2017, 6, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Mielke, M.M.; Roberts, R.O.; Savica, R.; Cha, R.; Drubach, D.I.; Christianson, T.; Pankratz, V.S.; Geda, Y.E.; Machulda, M.M.; Ivnik, R.J.; et al. Assessing the Temporal Relationship Between Cognition and Gait: Slow Gait Predicts Cognitive Decline in the Mayo Clinic Study of Aging. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013, 68, 929–937. [Google Scholar] [CrossRef] [PubMed]
- Savica, R.; Wennberg, A.M.V.; Hagen, C.; Edwards, K.; Roberts, R.O.; Hollman, J.H.; Knopman, D.S.; Boeve, B.F.; Machulda, M.M.; Petersen, R.C.; et al. Comparison of Gait Parameters for Predicting Cognitive Decline: The Mayo Clinic Study of Aging. J. Alzheimers Dis. 2016, 55, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Association. 2012 Alzheimer’s disease facts and figures. Alzheimers Dement. 2012, 8, 131–168. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.P.; Drought, A.B.; Kory, R.C. Walking Patterns of Normal Men. J. Bone Joint Surg. Am. 1964, 46, 335–360. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.P.; Kory, R.C.; Sepic, S.B. Walking patterns of normal women. Arch. Phys. Med. Rehabil. 1970, 51, 637–650. [Google Scholar] [PubMed]
- Finley, F.R.; Cody, K.A.; Finizie, R. V Locomotion patterns in elderly women. Arch. Phys. Med. Rehabil. 1969, 50, 140–146. [Google Scholar] [PubMed]
- Ostrosky, K.M.; VanSwearingen, J.M.; Burdett, R.G.; Gee, Z. A comparison of gait characteristics in young and old subjects. Phys. Ther. 1994, 74, 637–644. [Google Scholar] [CrossRef] [PubMed]
- Kressig, R.W.; Gregor, R.J.; Oliver, A.; Waddell, D.; Smith, W.; O’Grady, M.; Curns, A.T.; Kutner, M.; Wolf, S.L. Temporal and spatial features of gait in older adults transitioning to frailty. Gait Posture 2004, 20, 30–35. [Google Scholar] [CrossRef]
- Wang, F.; Stone, E.; Skubic, M.; Keller, J.M.; Abbott, C.; Rantz, M. Toward a passive low-cost in-home gait assessment system for older adults. IEEE J. Biomed. Heal. Inform. 2013, 17, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Hellmers, S.; Steen, E.-E.; Dasenbrock, L.; Heinks, A.; Bauer, J.M.; Fudickar, S.; Hein, A. Towards a minimized unsupervised technical assessment of physical performance in domestic environments. In Proceedings of the 11th EAI International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth ’17), Barcelona, Spain, 23–26 May 2017; ACM Press: New York, NY, USA, 2017; pp. 207–216. [Google Scholar]
- Liu, L.; Stroulia, E.; Nikolaidis, I.; Miguel-Cruz, A.; Rios Rincon, A. Smart homes and home health monitoring technologies for older adults: A systematic review. Int. J. Med. Inform. 2016, 91, 44–59. [Google Scholar] [CrossRef] [PubMed]
- Perry, J.; Burnfield, J.M.; Cabico, L.M. Gait Analysis: Normal and Pathological Function; SLACK Inc.: Thorofare, NJ, USA, 2010; ISBN 9781556427664. [Google Scholar]
- Wick, J.Y.; Zanni, G.R. Tiptoeing Around Gait Disorders: Multiple Presentations, Many Causes. Consult. Pharm. 2010, 25, 724–737. [Google Scholar] [CrossRef] [PubMed]
- Maki, B.E. Gait changes in older adults: Predictors of falls or indicators of fear. J. Am. Geriatr. Soc. 1997, 45, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Menz, H.B.; Latt, M.D.; Tiedemann, A.; Mun San Kwan, M.; Lord, S.R. Reliability of the GAITRite walkway system for the quantification of temporo-spatial parameters of gait in young and older people. Gait Posture 2004, 20, 20–25. [Google Scholar] [CrossRef]
- Merriaux, P.; Dupuis, Y.; Boutteau, R.; Vasseur, P.; Savatier, X. A Study of Vicon System Positioning Performance. Sensors 2017, 17, 1591. [Google Scholar] [CrossRef] [PubMed]
- Hellmers, S.; Fudickar, S.; Büse, C.; Dasenbrock, L.; Heinks, A.; Bauer, J.M.; Hein, A. Technology Supported Geriatric Assessment. In Ambient Assisted Living; Springer: Cham, Switzerland, 2017; pp. 85–100. [Google Scholar]
- Byun, S.; Han, J.W.; Kim, T.H.; Kim, K.W. Test-Retest Reliability and Concurrent Validity of a Single Tri-Axial Accelerometer-Based Gait Analysis in Older Adults with Normal Cognition. PLoS ONE 2016, 11, e0158956. [Google Scholar] [CrossRef] [PubMed]
- Dehzangi, O.; Taherisadr, M.; ChangalVala, R. IMU-Based Gait Recognition Using Convolutional Neural Networks and Multi-Sensor Fusion. Sensors 2017, 17, 2735. [Google Scholar] [CrossRef] [PubMed]
- Yorozu, A.; Takahashi, M. Development of gait measurement robot using laser range sensor for evaluating long-distance walking ability in the elderly. In Proceedings of the 2015 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Hamburg, Germany, 28 September–2 October 2015; pp. 4888–4893. [Google Scholar]
- Chalvatzaki, G.; Papageorgiou, X.S.; Tzafestas, C.S.; Maragos, P. Comparative experimental validation of human gait tracking algorithms for an intelligent robotic rollator. In Proceedings of the 2017 IEEE International Conference on Robotics and Automation (ICRA), Singapore, 29 May–3 June 2017; pp. 6026–6031. [Google Scholar]
- Papageorgiou, X.S.; Chalvatzaki, G.; Lianos, K.-N.; Werner, C.; Hauer, K.; Tzafestas, C.S.; Maragos, P. Experimental validation of human pathological gait analysis for an assisted living intelligent robotic walker. In Proceedings of the 2016 6th IEEE International Conference on Biomedical Robotics and Biomechatronics (BioRob), Singapore, 26–29 June 2016; pp. 1086–1091. [Google Scholar]
- Frenken, T.; Lohmann, O.; Frenken, M.; Steen, E.-E.; Hein, A. Performing gait analysis within the timed up & go assessment test: Comparison of aTUG to a marker-based tracking system. Inform. Health Soc. Care 2014, 39, 232–248. [Google Scholar] [CrossRef] [PubMed]
- Fudickar, S.; Kiselev, J.; Frenken, T.; Wegel, S.; Dimitrowska, S.; Steinhagen-Thiessen, E.; Hein, A. Validation of the ambient TUG chair with light barriers and force sensors in a clinical trial. Assist. Technol. 2018, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Pallejà, T.; Teixidó, M.; Tresanchez, M.; Palacín, J. Measuring Gait Using a Ground Laser Range Sensor. Sensors 2009, 9, 9133–9146. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.J.; Rauh, W.; Warnecke, H.-J. Least-squares orthogonal distances fitting of circle, sphere, ellipse, hyperbola, and parabola. Pattern Recognit. 2001, 34, 2283–2303. [Google Scholar] [CrossRef]
- Tanabe, S.; Ii, T.; Koyama, S.; Saitoh, E.; Itoh, N.; Ohtsuka, K.; Katoh, Y.; Shimizu, A.; Tomita, Y. Spatiotemporal treadmill gait measurements using a laser range scanner: Feasibility study of the healthy young adults. Physiol. Meas. 2017, 38, N81–N92. [Google Scholar] [CrossRef] [PubMed]
- Yorozu, A.; Moriguchi, T.; Takahashi, M. Improved Leg Tracking Considering Gait Phase and Spline-Based Interpolation during Turning Motion in Walk Tests. Sensors 2015, 15, 22451–22472. [Google Scholar] [CrossRef] [PubMed]
- Catmull, E.; Rom, R. A Class of Local Interpolating Splines. Comput. Aided Geom. Des. 1974, 317–326. [Google Scholar] [CrossRef]
- Dubois, A.; Charpillet, F. Measuring frailty and detecting falls for elderly home care using depth camera. J. Ambient Intell. Smart Environ. 2017, 9, 469–481. [Google Scholar] [CrossRef]
- Dubois, A.; Charpillet, F. Human activities recognition with RGB-Depth camera using HMM. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan, 3–7 July 2013; pp. 4666–4669. [Google Scholar]
- Rui, L.; Chen, S.; Ho, K.C.; Rantz, M.; Skubic, M. Estimation of human walking speed by Doppler radar for elderly care. J. Ambient Intell. Smart Environ. 2017, 9, 181–191. [Google Scholar] [CrossRef]
- Hokuyo Automatic Co. Ltd. Scanning Laser Range Finder URG-04LX-UG01 Specifications. Available online: https://www.robotshop.com/media/files/pdf/hokuyo-urg-04lx-ug01-specifications.pdf (accessed on 26 September 2018).
- Hokuyo Scanning Laser Range Finder UST-10LX Specifications. Available online: https://www.generationrobots.com/media/Hokuyo UST-10LX/UST-10LX_Specification.pdf#page=1&zoom=auto,-107,848 (accessed on 26 September 2018).
- Fleiss, J. The Design and Analysis of Clinical Experiments; John Wiley & Sons: New York, NY, USA, 1986. [Google Scholar] [CrossRef]
- Springer, S.; Seligmann, G.Y. Validity of the Kinect for Gait Assessment: A Focused Review. Sensors 2016, 16, 194. [Google Scholar] [CrossRef] [PubMed]




| Gait Parameter | Description | Algorithm | Separately per Foot |
|---|---|---|---|
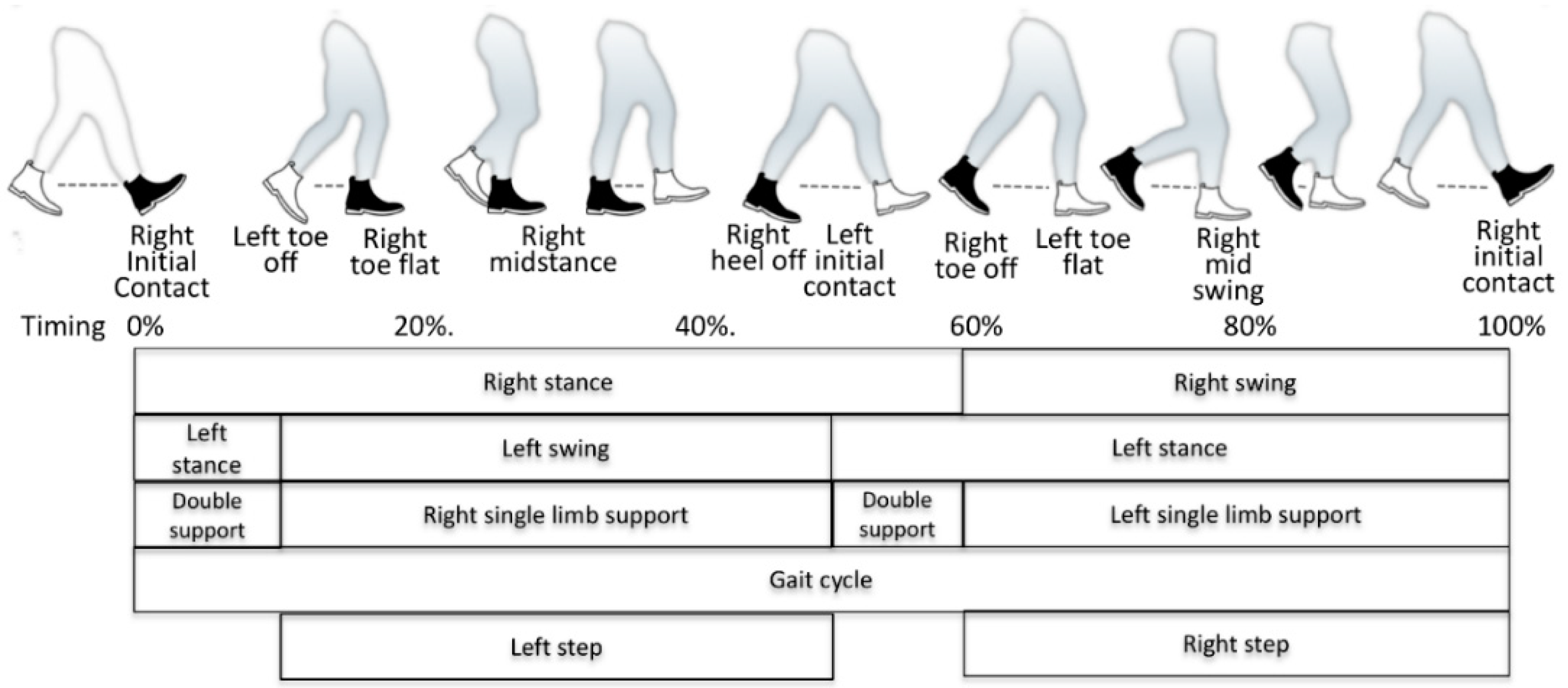
| Step length [m] | Distance between the heel of one foot to the heel of the next one along walking direction (see left and right step in Figure 1) | Distance passed from toe off to initial contact. | x |
| Cadence [1/min] | Step frequency | Number of steps/time [min] | |
| Walking velocity [m/min] | Gait speed | Distance [m]/time [min] = stride_length [m] × cadence [1/min]/2 | |
| Stance time [s] | Time each foot has contact with the ground per step (see left and right stance in Figure 1.) | Last_contact_time – first_contact_time | x |
| Swing time [s] | Time each foot has no contact with the ground per step (see left and right swing in Figure 1) | Step[i + 1]. first_contact_time – step[i]. last_contact_time | x |
| Stride length [m] | Distance from one foot hitting the ground to its next ground contact (see full gait cycle shown in Figure 1 as example for right stride). | Step_lengthLeft + step_lengthRight | x |
| Parameter | Men Normal [20] | Women Normal [20] | Normal (Gender Independent) [21] | Transition to Frailty+ [16] | Fearful Fallers + [22] |
|---|---|---|---|---|---|
| Velocity [m/min] | 86 (80–91) | 77 (73–81) | 82 | 58.2 ± 13.8 (29%) | 39.6 ± 11.4 (51%) |
| Cadence [1/min] | 111 | 117 | 113 | 105.7 ± 12.7 (6%) | 95.4 ± 11.2 (15%) |
| Stride length [m] | 1.46 | 1.28 | 1.41 | 1.11 ± 0.18 (21%) | 0.83 ± 0.16 (41%) |
| Sensor System | Resulting Sensitivity | Study Design | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Year | Sensor | Algorithm | Orient/Height | Detection Rate of Steps/Walks (in %) | Gait Velocity/Speed Error (cm/s) | Stride Length Error (cm) | Swing Time Error (s) | Reference System | Subjects (m/f); Age |
| 2015 [28] | 04-LX-UG01, UTM-30LX | KF, GNN | F 27 cm | Leg tracking (97.1%) Foot contact (99.3%) | n.d. | 3.5 cm | n.d. | Vicon | 7 (4/3); 70.9 years ± 3.5 |
| 2017 [29] | 04LX-F01 | KF/PF | F 40 cm | KF: 18.4% (10.5–30.1%) PF: 0.6% (0–2.3%) | KF: 7.9 (4.5–11.3) cm/s PF: 6.4 cm/s (4.2–9.9) RMSE | n.d. | n.d. | Vicon | 4; 65 + years |
| 2016 [30] | 04LX-F01 | HMM, KM, KF | F 40 cm walker | n.d. | n.d. | HMM: 8.9% ± 5.2% RB: 10.1% ± 6.8% | HMM: 10.9% ± 6.2% RB: 16.9% ± 5.7% | GAITRite | 5; 65 + years |
| 2014 [31,32] | SLR, 4 force sensors | BGS, DIET [13] | F/B 35 cm | n.d. | n.d. | 3 cm | 0.08 s | SIMI Motion | 7 (5/2); 23–31 years |
| 2009 [33] | UTM-30LX | LMS fitting [34] | F 10 cm | n.d. | n.d. | 1.1 SD 0.8 cm | n.d. | n.d. | 6 (3/3); n.d. |
| 2017 [35] | UTM-30LX | n.d. | F 25 cm | n.d. | n.d. | 25.9 cm (3.37%) ± 23.8 cm (3.53%) | 0.091 s (22.9%) ± 0.051 s (12.1%) | KC | 34 (21/13); 22–30 years |
| 2015 [36] | UTM-30LX | KF, Catmull–Rom spline [37] | F/B | 96.4% (tracking success rate) | n.d. | 3–5 cm RMSE | n.d. | Vicon | 7 (6/1); 23.0 ± 1.9 years |
| 2017 [38] | Kinect | BGS [39] LSM, EDF, HMM | F | n.d. | 0.3; SD 0.12 cm/s | 0.6; SD 8.31 cm | n.d. | GAITRite | 11 (7/4); 22–53 years |
| 2017 [40] | DR, Precision Line RCR-50 | Zero-crossing in time domain IQR filter | F 15 cm | n.d. | 1.08 RMSE | n.d. | n.d. | Vicon, Kinect | 8; seniors |
| SLR Scanner-Type | Hokuyo URG-04LX (SLR-04) [41] | Hokuyo UST-10LX (SLR-10) [42] |
|---|---|---|
| Scanning rate | 10 Hz | 40 Hz |
| Measuring area | 2–560 cm | 6–1000 cm |
| 240° | 270° | |
| Measuring Accuracy | ±10 mm (0.20–1 m), ±3% (1–5.6 m) | ±40 mm |
| Angular resolution | approx. 0.36° | approx. 0.25° |
| I/O | Universal series bus (USB) | Local-area network (LAN) |
| Power Supply | 5V DC, 500 mA (800 mA during start up) | 12VDC/24VDC, 150 mA (450 mA during start up) |
| Synchronisation Overlap (s) between SLR and GAITRite | Number of Steps (% of Overall 56351 Considered Steps) | |
|---|---|---|
| URG04LX | UST-10LX | |
| 4 | 43162 (75.6%) | 55083 (97.7%) |
| 3.5 | 43253 (76.8%) | 55167 (97.9%) |
| 3 | 43260 (76.8%) | 55181 (97.9%) |
| 2.5 | 43092 (76.5%) | 55188 (97.9%) |
| 2 | 42035 (74.6%) | 55153 (97.9%) |
| 1.5 | 37240 (66.1%) | 54516 (96.7%) |
| 1 | 25221 (44.8%) | 46879 (83.2%) |
| 0.5 | 11473 (20.4%) | 23961 (42.5%) |
| Average | SD | Min | Max | |
|---|---|---|---|---|
| Age (years) | 59.6 | 22.8 | 21 | 82 |
| Height (cm) | 173.3 | 10.2 | 151 | 196 |
| Weight (kg) | 76.1 | 12.8 | 53 | 103 |
| Left leg-length (cm) | 80.8 | 5.59 | 67 | 94 |
| Right leg-length (cm) | 80.79 | 5.65 | 67 | 94 |
| Parameter | Walking Speed | Min | 1. IQR | Median | 3. IQR | 99% | Max | CC |
|---|---|---|---|---|---|---|---|---|
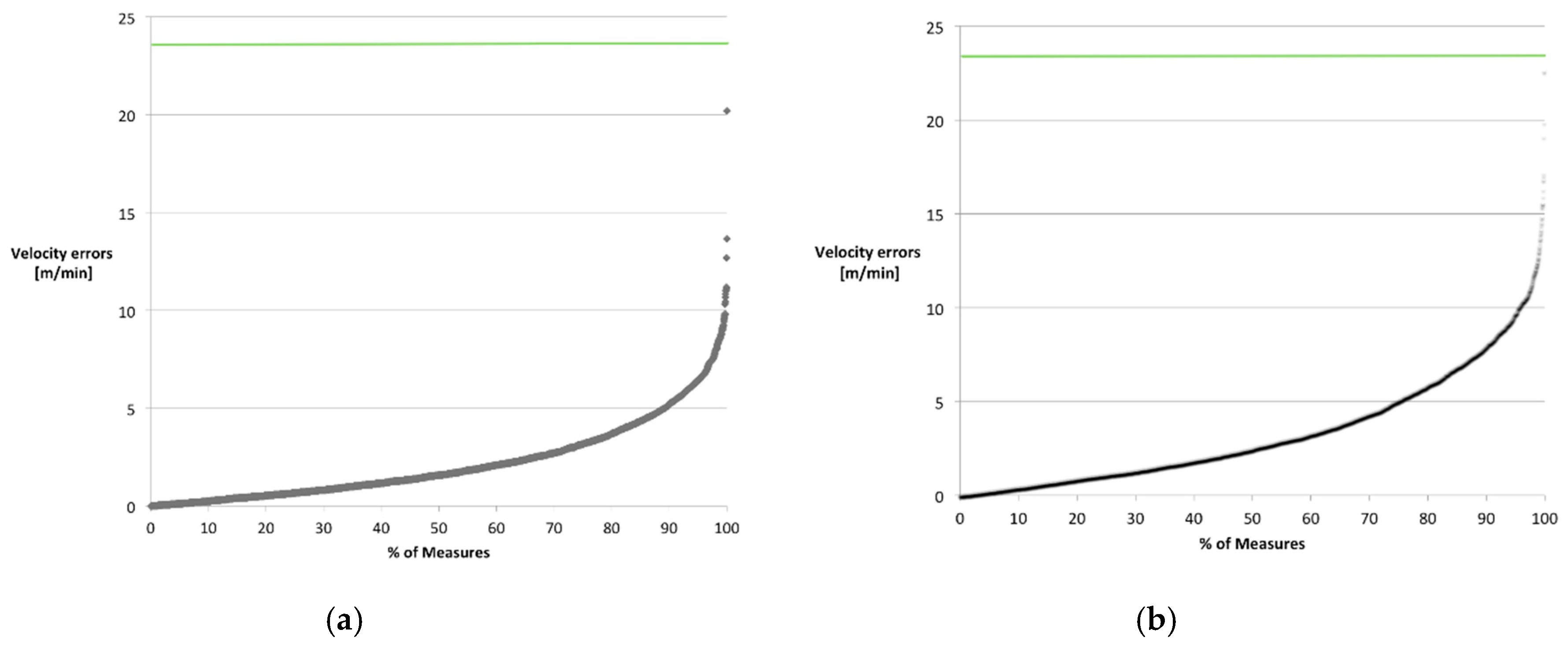
| Velocity [m/min] | normal | 0 | 0.68 | 1.58 | 3.17 | 8.8 | 20.19 | 0.95 |
| fast | 0 | 1.08 | 2.46 | 5.03 | 12.96 | 45.81 | 0.93 | |
| Left Stride Length Mean (cm) | normal | −68.66 | −5.43 | −2.49 | −1.50 | 1.85 | 18.03 | 0.91 |
| fast | −53.59 | −3.92 | −2.33 | −1.41 | 2.22 | 16.45 | 0.95 | |
| Right Stride Length Mean (cm) | normal | −56.46 | −5.56 | −3.30 | −2.15 | 1.24 | 17.76 | 0.93 |
| fast | −42.75 | −5.17 | −3.44 | −2.22 | 0.93 | 7.51 | 0.96 | |
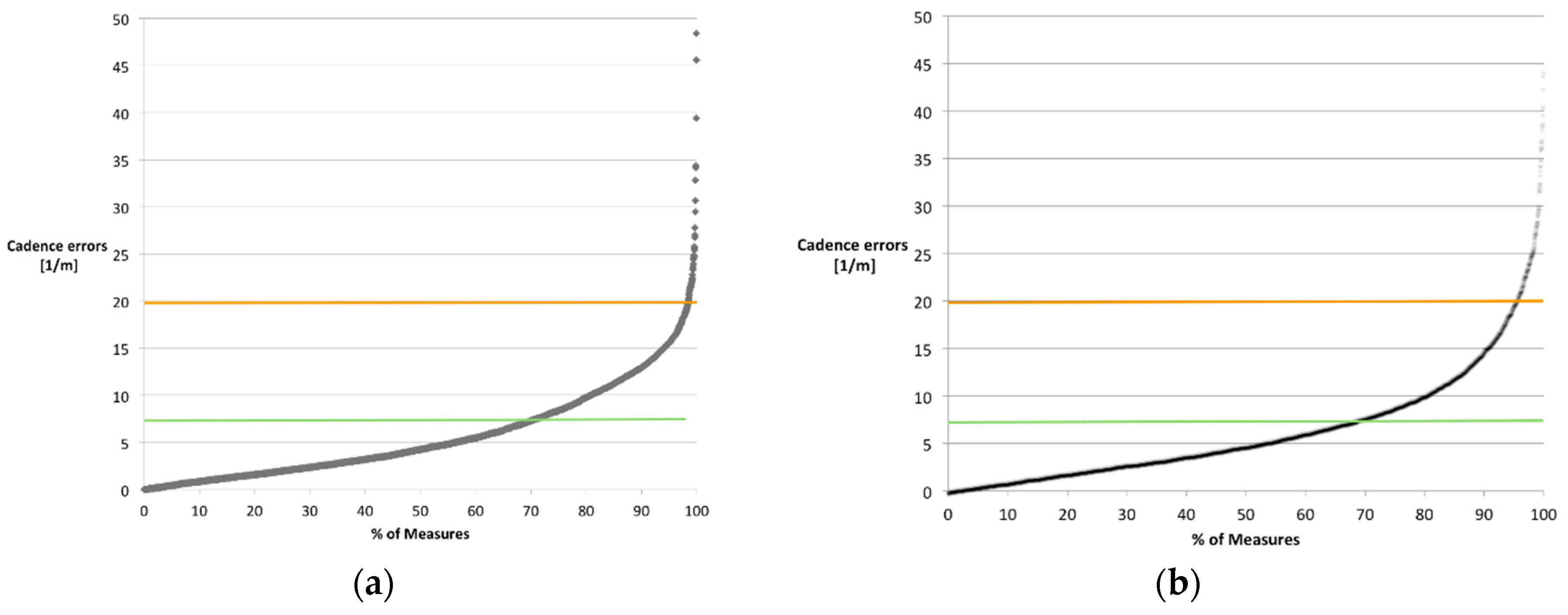
| Cadence [1/min] | normal | −19.6 | 0.1 | 3.2 | 8.4 | 28.66 | 111.4 | 0.71 |
| fast | −23.4 | −1.8 | 2.6 | 6.8 | 28.94 | 66.3 | 0.79 | |
| Left Stance Time Mean (s) | normal | −0.56 | 0 | 0.03 | 0.05 | 0.12 | 0.23 | 0.75 |
| fast | −0.47 | −0.02 | 0 | 0.03 | 0.09 | 0.54 | 0.81 | |
| Right Stance Time Mean (s) | normal | −0.53 | −0.10 | −0.05 | 0 | 0.09 | 0.14 | 0.66 |
| fast | −0.43 | −0.11 | −0.058 | −0.01 | 0.07 | 0.12 | 0.61 | |
| Left Swing Time Mean (s) | normal | −0.28 | −0.04 | −0.02 | 0 | 0.14 | 0.41 | 0.49 |
| fast | −0.17 | −0.01 | 0.01 | 0.02 | 0.19 | 0.45 | 0.56 | |
| Right Swing Time Mean (s) | normal | −0.18 | −0.04 | −0.02 | 0 | 0.15 | 0.41 | 0.51 |
| fast | −0.23 | −0.01 | 0.01 | 0.02 | 0.13 | 0.40 | 0.65 | |
| Walks’ Distance [m] | normal | 0 | 0.43 | 0.63 | 1.03 | 1,64 | 1.95 | n.a. |
| fast | 0 | 0.39 | 0.63 | 1.04 | 1.58 | 2.08 | n.a. |
| Common Age- and Disease-Related Variations | Error of SLR as 99 Percentile (Normal/Fast Walking Pace) | ||
|---|---|---|---|
| Parameter | Min [16] | Max [22] | |
| Velocity Diff [m/min] | 23.8 | 42.4 | 8.8/12.96 |
| Stride Length [cm] | 30 | 58 | 1.85/2.22 |
| Cadence Diff [1/min] | 7.3 | 19.6 | 28.66/28.94 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fudickar, S.; Stolle, C.; Volkening, N.; Hein, A. Scanning Laser Rangefinders for the Unobtrusive Monitoring of Gait Parameters in Unsupervised Settings. Sensors 2018, 18, 3424. https://doi.org/10.3390/s18103424
Fudickar S, Stolle C, Volkening N, Hein A. Scanning Laser Rangefinders for the Unobtrusive Monitoring of Gait Parameters in Unsupervised Settings. Sensors. 2018; 18(10):3424. https://doi.org/10.3390/s18103424
Chicago/Turabian StyleFudickar, Sebastian, Christian Stolle, Nils Volkening, and Andreas Hein. 2018. "Scanning Laser Rangefinders for the Unobtrusive Monitoring of Gait Parameters in Unsupervised Settings" Sensors 18, no. 10: 3424. https://doi.org/10.3390/s18103424
APA StyleFudickar, S., Stolle, C., Volkening, N., & Hein, A. (2018). Scanning Laser Rangefinders for the Unobtrusive Monitoring of Gait Parameters in Unsupervised Settings. Sensors, 18(10), 3424. https://doi.org/10.3390/s18103424






