A Study of Thermistor Performance within a Textile Structure
Abstract
:1. Introduction
2. Materials and Methods
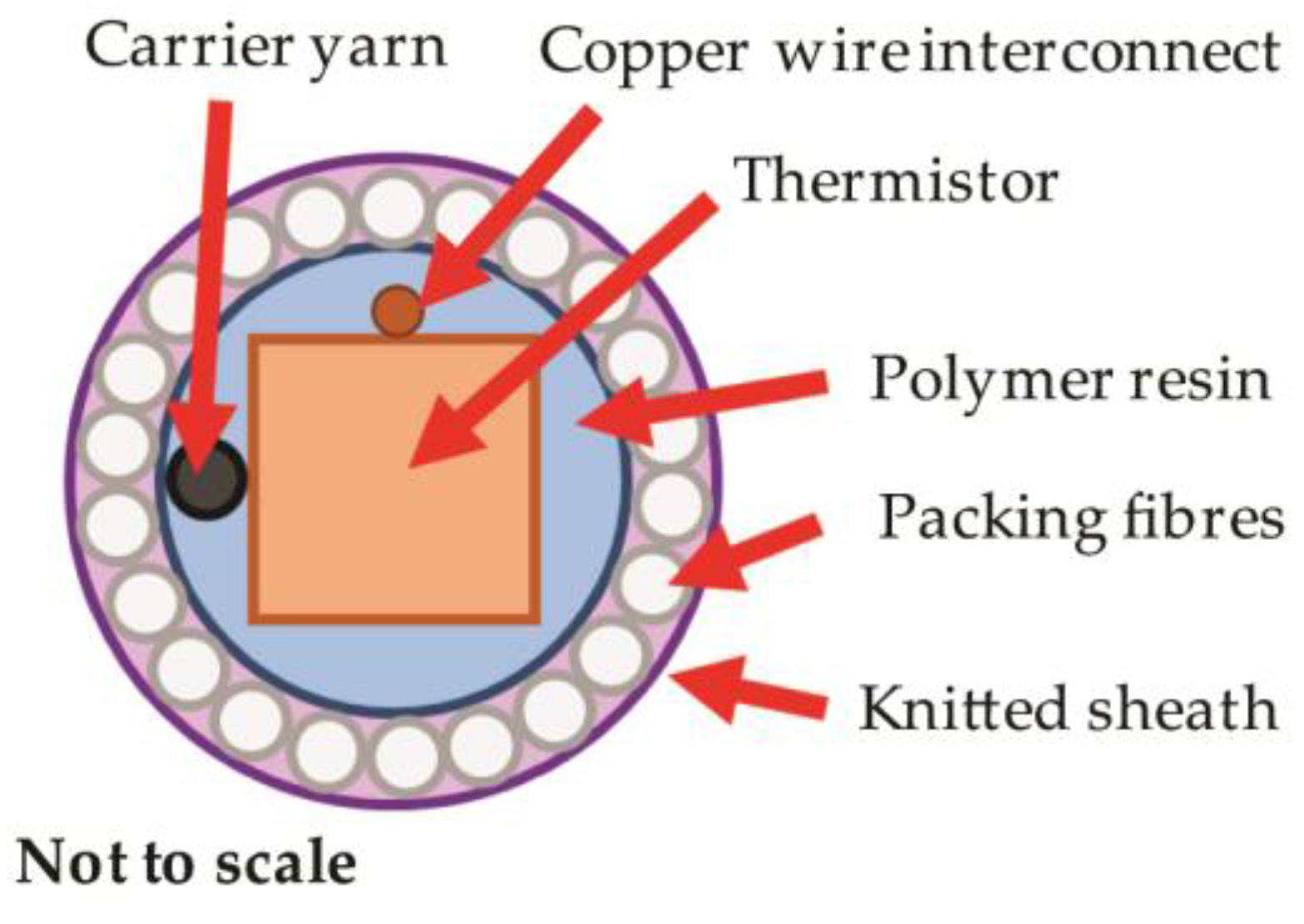
2.1. Electronic Temperature-Sensing Yarn Construction
2.2. Supporting Hardware for Temperature Measurements
2.3. Response of Electronic Temperature-Sensing Yarns
2.3.1. Step Response Time Theory
2.3.2. Response Time Experiments
2.4. Calibration of Sensor Yarn
2.5. Prototype Temperature-Sensing Sock
3. Results and Discussion
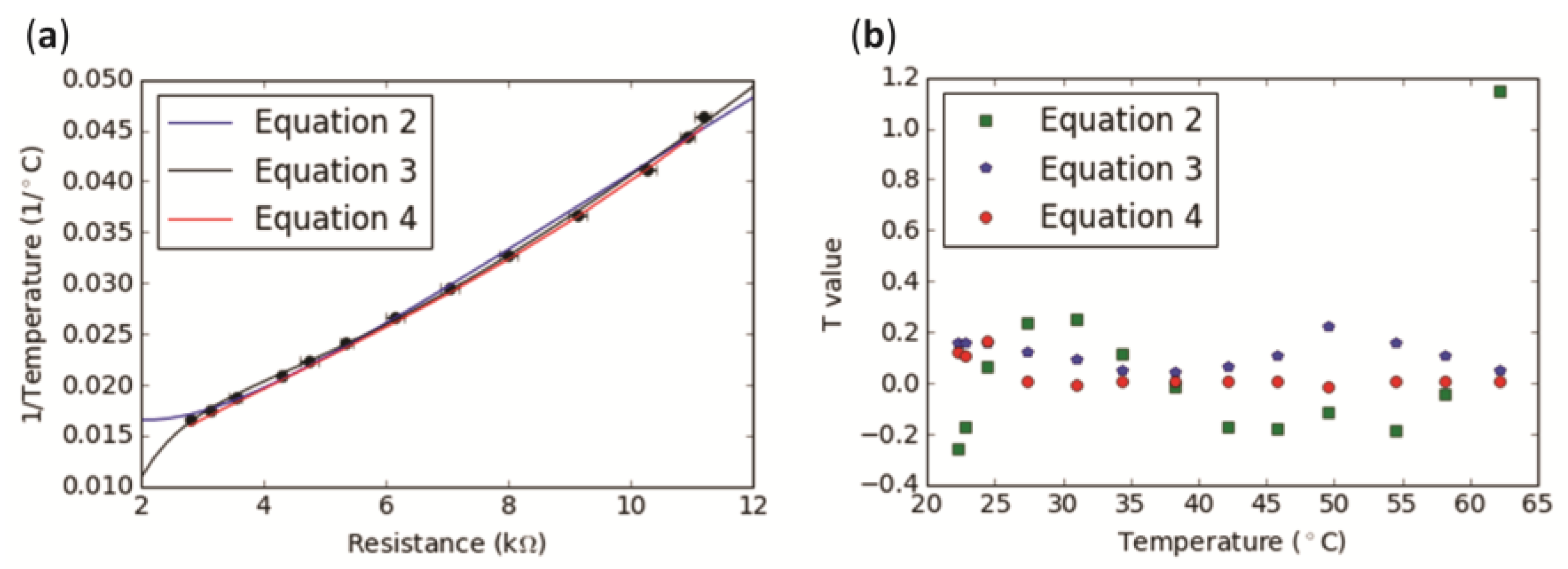
3.1. Electronic Temperature-Sensing Yarn Calibration
3.2. Response Time of Encapsulated Thermistor and Stability of Readings
3.2.1. Step Response Time
3.2.2. Step Response Time for Electronic Temperature-Sensing Yarns with a Fibre Sheath
3.2.3. Stability and Accuracy of Temperature Readings
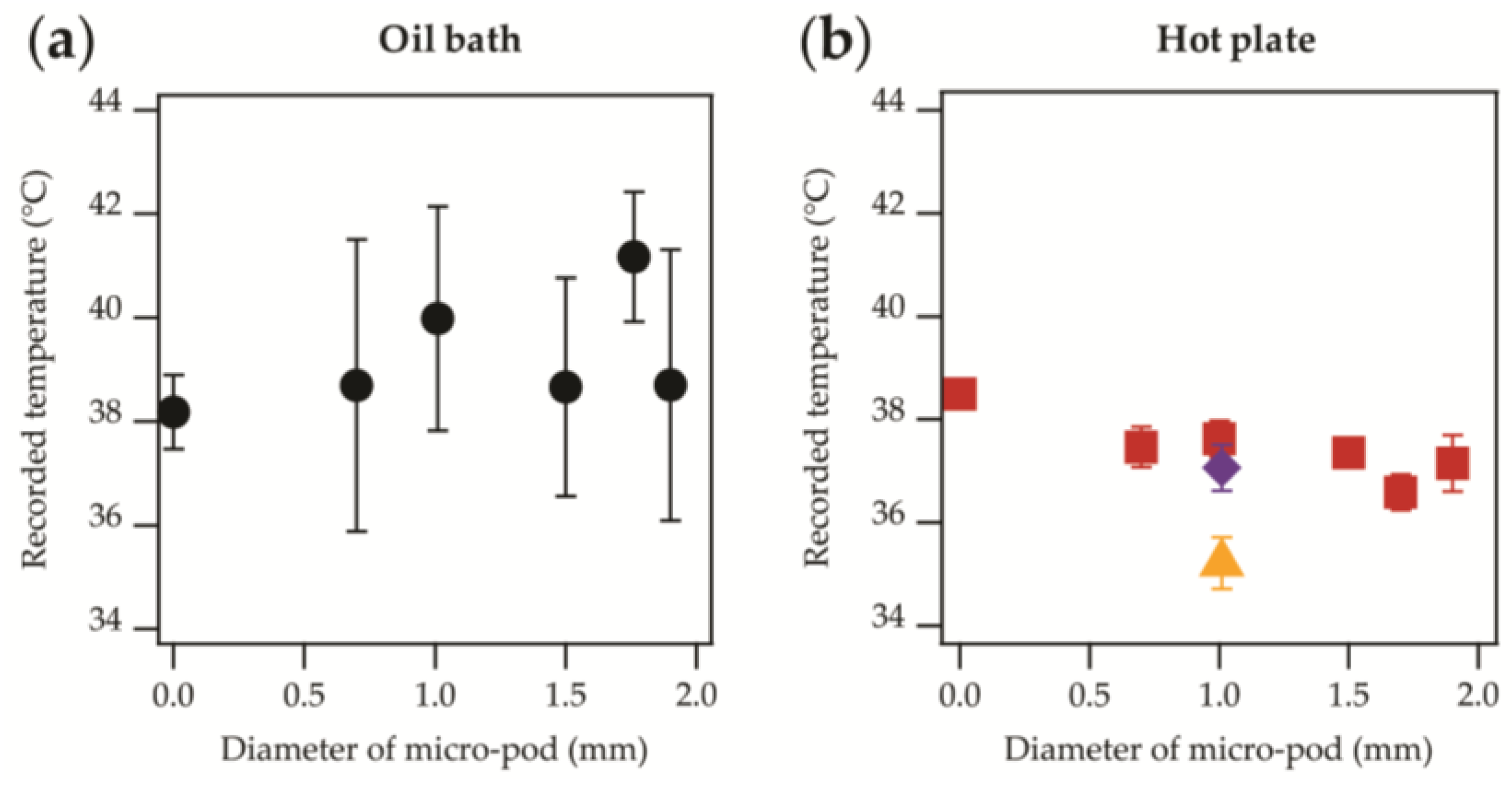
 ) is in agreement with the other data. It is possible that the yarn with the additional fibrous sheath gave higher recorded temperatures than when only one sheath was used (i.e., normal temperature-sensing yarn;
) is in agreement with the other data. It is possible that the yarn with the additional fibrous sheath gave higher recorded temperatures than when only one sheath was used (i.e., normal temperature-sensing yarn;  ) due to warm air becoming trapped within the loops of the knitted structure, and small air-gaps between the sheath and temperature-sensing yarn. As discussed earlier, this may create a microclimate around the temperature-sensing yarn, minimizing heat losses to the environment. It is important to highlight that within a textile the temperature-sensing yarn would be surrounded by an additional fibrous layer, making the temperature-sensing yarn within an additional fibre sheath a more representative model of the yarns in their final intended use.
) due to warm air becoming trapped within the loops of the knitted structure, and small air-gaps between the sheath and temperature-sensing yarn. As discussed earlier, this may create a microclimate around the temperature-sensing yarn, minimizing heat losses to the environment. It is important to highlight that within a textile the temperature-sensing yarn would be surrounded by an additional fibrous layer, making the temperature-sensing yarn within an additional fibre sheath a more representative model of the yarns in their final intended use.3.3. Prototype Temperature-Sensing Sock
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Sessler, D.I. Temperature monitoring and perioperative thermoregulation. J. Am. Soc. Anesthesiol. 2008, 109, 318–338. [Google Scholar] [CrossRef] [PubMed]
- Guadagni, D.N.; Kreith, F.; Smyth, C.J.; Bartholomew, B.A. Contact probe for skin temperature measurements. J. Phys. E Sci. Instrum. 1972, 5, 869. [Google Scholar] [CrossRef]
- Stoll, A.M. Techniques and uses of skin temperature measurements. Ann. N. Y. Acad. Sci. 1964, 121, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Webb, R.C.; Bonifas, A.P.; Behnaz, A.; Zhang, Y.; Yu, K.J.; Cheng, H.; Shi, M.; Bian, Z.; Liu, Z.; Kim, Y.S.; et al. Ultrathin conformal devices for precise and continuous thermal characterization of human skin. Nat. Mater. 2013, 12, 938. [Google Scholar] [CrossRef] [PubMed]
- Burnham, R.S.; McKinley, R.S.; Vincent, D.D. Three types of skin-surface thermometers: A comparison of reliability, validity, and responsiveness. Am. J. Phys. Med. Rehabilit. 2006, 85, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Tanda, G. The use of infrared thermography to detect the skin temperature response to physical activity. J. Phys. Conf. Ser. 2015, 655, 012062. [Google Scholar] [CrossRef]
- Hardy, J.D. The radiation of heat from the human body: III. The human skin as a black-body radiator. J. Clin. Investig. 1934, 13, 615. [Google Scholar] [CrossRef] [PubMed]
- Lugoda, P.; Dias, T.; Morris, R. Electronic Temperature Sensing Yarn. J. Multidiscip. Eng. Sci. Stud. 2015, 1, 100–103. [Google Scholar]
- Dias, T.K.; Rathnayake, A. Electronically Functional Yarns. Patent WO2016/038342 A1, 17 March 2016. [Google Scholar]
- Lavery, L.A.; Higgins, K.R.; Lanctot, D.R.; Constantinides, G.P.; Zamorano, R.G.; Armstrong, D.G.; Athanasiou, K.A.; Agrawal, C.M. Home monitoring of foot skin temperatures to prevent ulceration. Diabetes Care 2004, 27, 2642–2647. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Holtz-Neiderer, K.; Wendel, C.; Mohler, M.J.; Kimbrielb, H.R.; Lavery, L.A. Skin Temperature Monitoring Reduces the Risk for Diabetic Foot Ulceration in High-Risk Patients. Am. J. Med. 2007, 120, 1042–1046. [Google Scholar] [CrossRef] [PubMed]
- Lavery, L.A.; Higgins, K.R.; Lanctot, D.R.; Constantinides, G.P.; Zamorano, R.G.; Athanasiou, K.A.; Armstrong, D.G.; Agrawal, C.M. Preventing diabetic foot ulcer recurrence in high-risk patients: Use of temperature monitoring as a self-assessment tool. Diabetes Care 2007, 30, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Nakagami, G.; Sanada, H.; Iizaka, S.; Kadono, T.; Higashino, T.; Koyanagi, H.; Haga, N. Predicting delayed pressure ulcer healing using thermography: A prospective cohort study. J. Wound Care 2010, 19, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Peregrina-Barreto, H.; Morales-Hernandez, L.A.; Rangel-Magdaleno, J.J.; Avina-Cervantes, J.G.; Ramirez-Cortes, J.M.; Morales-Caporal, R. Quantitative Estimation of Temperature Variations in Plantar Angiosomes: A Study Case for Diabetic Foot. Comput. Math. Methods Med. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Chaves, M.E.A.; Silva, F.S.; Soares, V.P.C.; Ferreira, R.A.M.; Gomes, F.S.L.; Andrade, R.M.; Pinotti, M. Evaluation of healing of pressure ulcers through thermography: A preliminary study. Res. Biomed. Eng. 2015, 31, 3–9. [Google Scholar] [CrossRef]
- Mufti, A.; Coutts, P.; Sibbald, R.G. Validation of commercially available infrared thermometers for measuring skin surface temperature associated with deep and surrounding wound infection. Adv. Skin Wound Care 2015, 28, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Okuwa, M.; Shigeta, Y.; Dai, M.; Iuchi, T.; Rahman, S.; Usman, A.; Kasim, S.; Sugama, J.; Nakatani, T.; et al. Microclimate and development of pressure ulcers and superficial skin changes. Int. Wound J. 2015, 12, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Husain, M.D.; Kennon, R.; Dias, T. Design and fabrication of Temperature Sensing Fabric. J. Ind. Text. 2013, 44, 398–417. [Google Scholar] [CrossRef]
- Sibinski, M.; Jakubowska, M.; Sloma, M. Flexible temperature sensors on fibers. Sensors 2010, 10, 7934–7946. [Google Scholar] [CrossRef] [PubMed]
- Moser, Y.; Gijs, M.A.M. Miniaturized Flexible Temperature Sensor. J. Microelectromech. Syst. 2007, 16, 1349–1354. [Google Scholar] [CrossRef]
- Krzysztof, G.; Jacek, G.; Jacek, L. Temperature Measurements in a Textronic Fireman Suit and Visualisation of the Results. Fibres Text. East. Eur. 2009, 17, 97–101. [Google Scholar]
- Cherenack, K.; Zysset, C.; Kinkeldei, T.; Münzenrieder, N.; Tröster, G. Woven electronic fibers with sensing and display functions for smart textiles. Adv. Mater. 2010, 22, 5178–5182. [Google Scholar] [CrossRef] [PubMed]
- Joint Committee for Guides in Metrology. International Vocabulary of Metrology–Basic and General Concepts and Associated Terms (VIM), 3rd ed.; International Organization for Standardization: Geneva, Switzerland, 2012. [Google Scholar]
- Egan, G.F.; Johnson, J.; Farrell, M.; MacAllen, R.; Zamarripa, F.; McKinley, M.J.; Lancaster, J.; Denton, D.; Fox, P.T. Cortical, thalamic, and hypothalamic responses to cooling and warming the skin in awake humans: A positron-emission tomography study. Proc. Natl. Acad. Sci. USA 2005, 102, 5262–5267. [Google Scholar] [CrossRef] [PubMed]
- Gockenbach, M.; Schmidtke, K. Newton’s law of heating and the heat equation. Involv. J. Math. 2009, 2, 419–437. [Google Scholar] [CrossRef]
- Jones, E.; Oliphant, T.; Peterson, P. SciPy: Open Source Scientific Tools for Python. 2001. Available online: http://www.scipy.org/ (accessed on 4 May 2017).
- Hunter, J.D. Matplotlib: A 2D graphics environment. Comput. Sci. Eng. 2007, 9, 90–95. [Google Scholar] [CrossRef]
- Kimball, B.R.; DeCristofano, B.; Caldarella, G. Thermistor Calibration Procedure for Simulated Skin Sensors; Technical Report Natick/TR93/024 1993; U.S. Army Natick Research, Development and Engineering Center Natick: Natick, MA, USA, 1993.
- White, D.R.; Hill, K.; del Campo, D.; Garcia Izquierdo, C. Guide on Secondary Thermometry: Thermistor Thermometry; Bureau International des Poids et Mesures: Paris, France, 2014. [Google Scholar]
- Ohizumi-Mfg.jp. Technical Note: Ohizumi Mfg. Co., Ltd. 2017. Available online: http://www.ohizumi-mfg.jp/english/product/technote1.html (accessed on 14 June 2017).
- Nardin, R.A.; Fogerson, P.M.; Nie, R.; Rutkove, S.B. Foot temperature in healthy individuals: Effects of ambient temperature and age. J. Am. Podiatr. Med. Assoc. 2010, 100, 258–264. [Google Scholar] [CrossRef] [PubMed]
 = 0.70 mm,
= 0.70 mm,  = 1.00 mm,
= 1.00 mm,  = 1.90 mm. Markers appear as lines in the figure due to the density of data.
= 1.90 mm. Markers appear as lines in the figure due to the density of data.
 = 0.70 mm,
= 0.70 mm,  = 1.00 mm,
= 1.00 mm,  = 1.90 mm. Markers appear as lines in the figure due to the density of data.
= 1.90 mm. Markers appear as lines in the figure due to the density of data.
 ) or the samples were attached directly to a hotplate (
) or the samples were attached directly to a hotplate (  ). (a) Heating time constant; (b) Cooling time constant. In both cases the effect of the micro-pod on the time constants were negligible within the experimental error.
). (a) Heating time constant; (b) Cooling time constant. In both cases the effect of the micro-pod on the time constants were negligible within the experimental error.
 ) or the samples were attached directly to a hotplate (
) or the samples were attached directly to a hotplate (  ). (a) Heating time constant; (b) Cooling time constant. In both cases the effect of the micro-pod on the time constants were negligible within the experimental error.
). (a) Heating time constant; (b) Cooling time constant. In both cases the effect of the micro-pod on the time constants were negligible within the experimental error.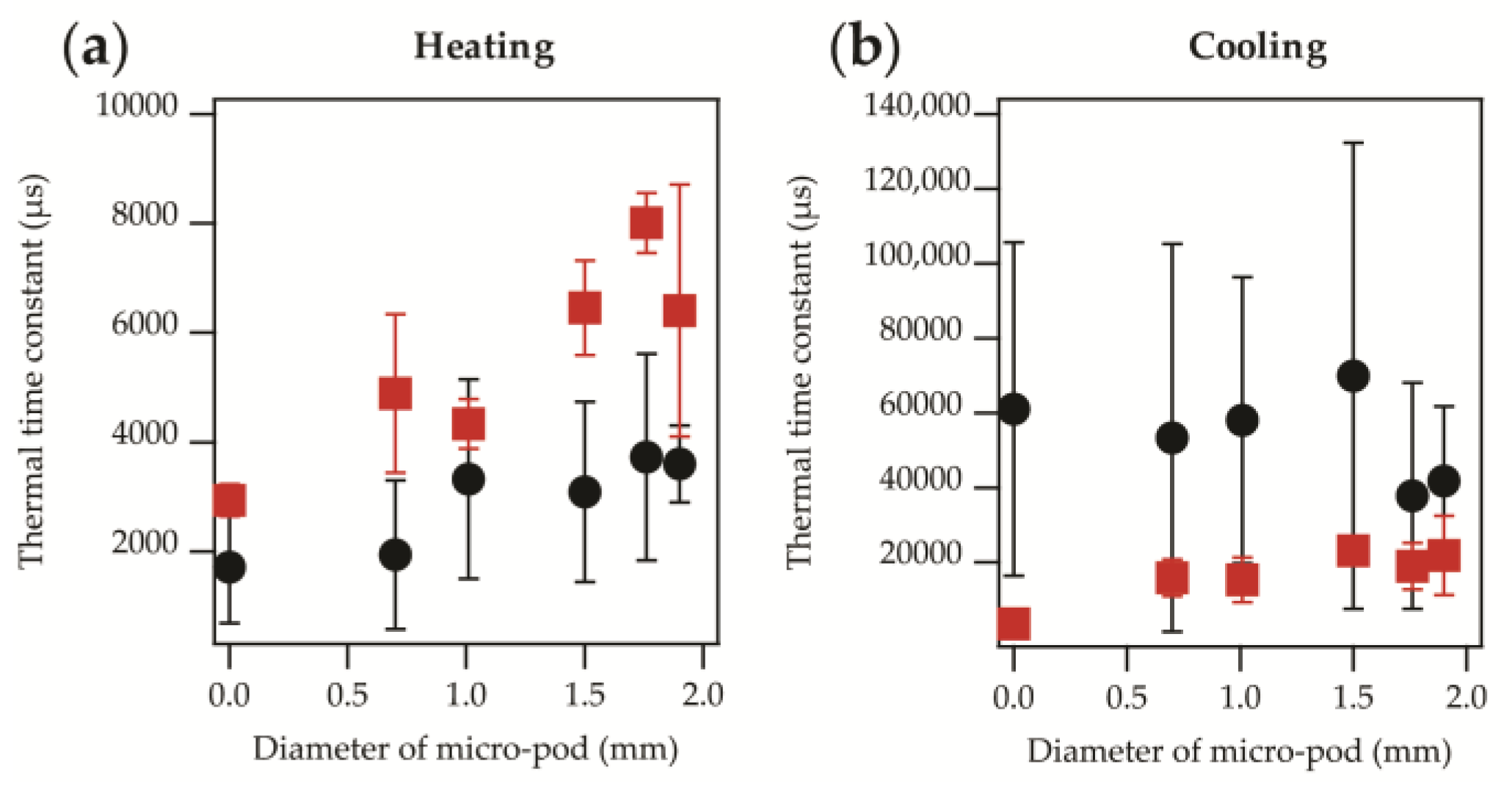
 ; previously shown in Figure 4a). (a) Heating thermal time constant. A direct linear relationship (r2 = 0.776) is observed as shown in Equation (5); (b) Cooling thermal time constant. The linear relationship (r2 = 0.629) observed is shown in Equation (6).
; previously shown in Figure 4a). (a) Heating thermal time constant. A direct linear relationship (r2 = 0.776) is observed as shown in Equation (5); (b) Cooling thermal time constant. The linear relationship (r2 = 0.629) observed is shown in Equation (6).
 ; previously shown in Figure 4a). (a) Heating thermal time constant. A direct linear relationship (r2 = 0.776) is observed as shown in Equation (5); (b) Cooling thermal time constant. The linear relationship (r2 = 0.629) observed is shown in Equation (6).
; previously shown in Figure 4a). (a) Heating thermal time constant. A direct linear relationship (r2 = 0.776) is observed as shown in Equation (5); (b) Cooling thermal time constant. The linear relationship (r2 = 0.629) observed is shown in Equation (6).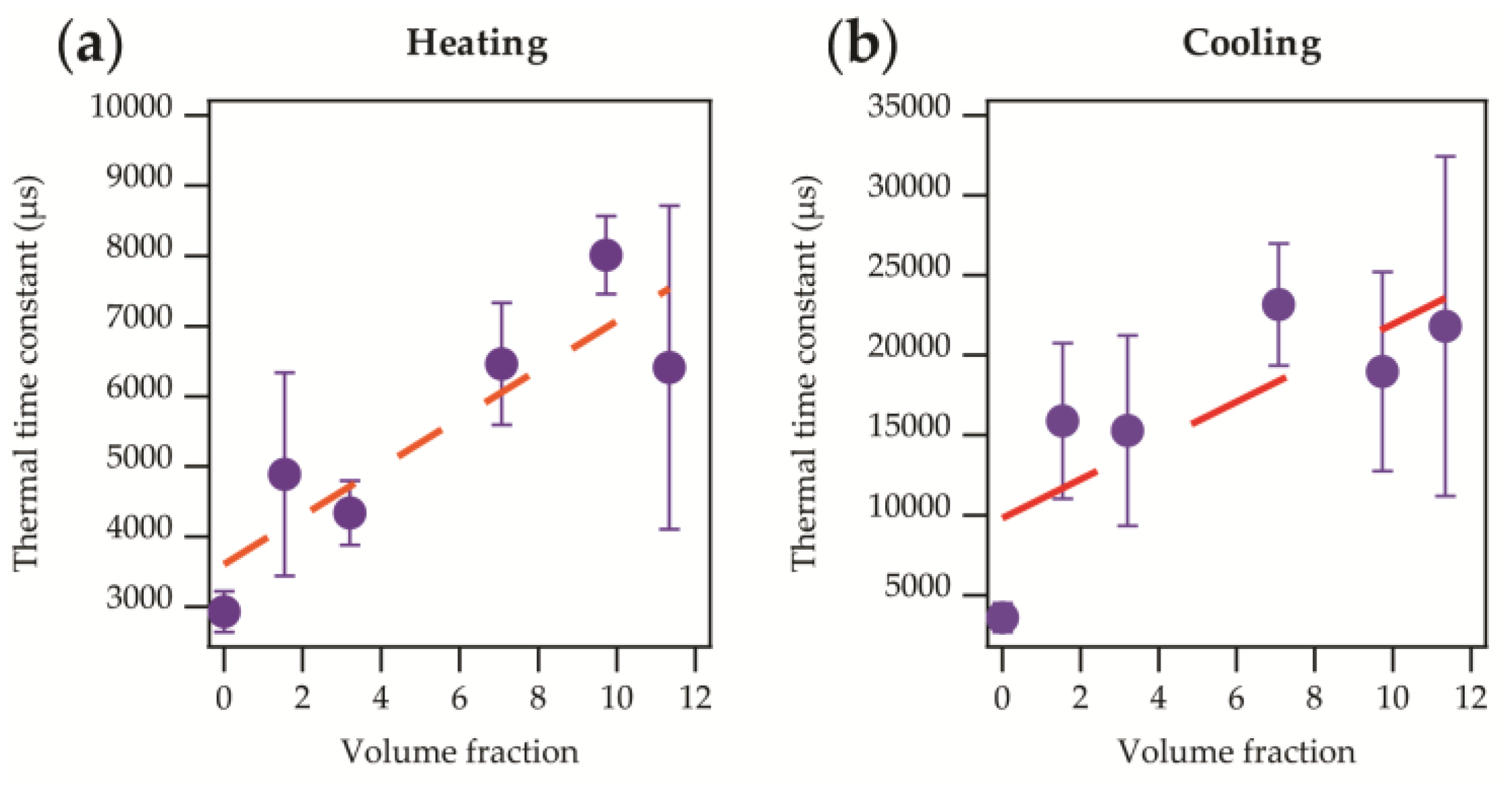
 ); (b) The samples were attached directly to a hotplate (
); (b) The samples were attached directly to a hotplate (  ). Data from samples that have included covering fibres; temperature-sensing yarn (
). Data from samples that have included covering fibres; temperature-sensing yarn (  ), temperature-sensing yarn with an additional fibrous sheath (
), temperature-sensing yarn with an additional fibrous sheath (  ).
).
 ); (b) The samples were attached directly to a hotplate (
); (b) The samples were attached directly to a hotplate (  ). Data from samples that have included covering fibres; temperature-sensing yarn (
). Data from samples that have included covering fibres; temperature-sensing yarn (  ), temperature-sensing yarn with an additional fibrous sheath (
), temperature-sensing yarn with an additional fibrous sheath (  ).
).

© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hughes-Riley, T.; Lugoda, P.; Dias, T.; Trabi, C.L.; Morris, R.H. A Study of Thermistor Performance within a Textile Structure. Sensors 2017, 17, 1804. https://doi.org/10.3390/s17081804
Hughes-Riley T, Lugoda P, Dias T, Trabi CL, Morris RH. A Study of Thermistor Performance within a Textile Structure. Sensors. 2017; 17(8):1804. https://doi.org/10.3390/s17081804
Chicago/Turabian StyleHughes-Riley, Theodore, Pasindu Lugoda, Tilak Dias, Christophe L. Trabi, and Robert H. Morris. 2017. "A Study of Thermistor Performance within a Textile Structure" Sensors 17, no. 8: 1804. https://doi.org/10.3390/s17081804
APA StyleHughes-Riley, T., Lugoda, P., Dias, T., Trabi, C. L., & Morris, R. H. (2017). A Study of Thermistor Performance within a Textile Structure. Sensors, 17(8), 1804. https://doi.org/10.3390/s17081804





