Smart Homes for Elderly Healthcare—Recent Advances and Research Challenges
Abstract
1. Motivation
2. Introduction
3. Remote Health Monitoring
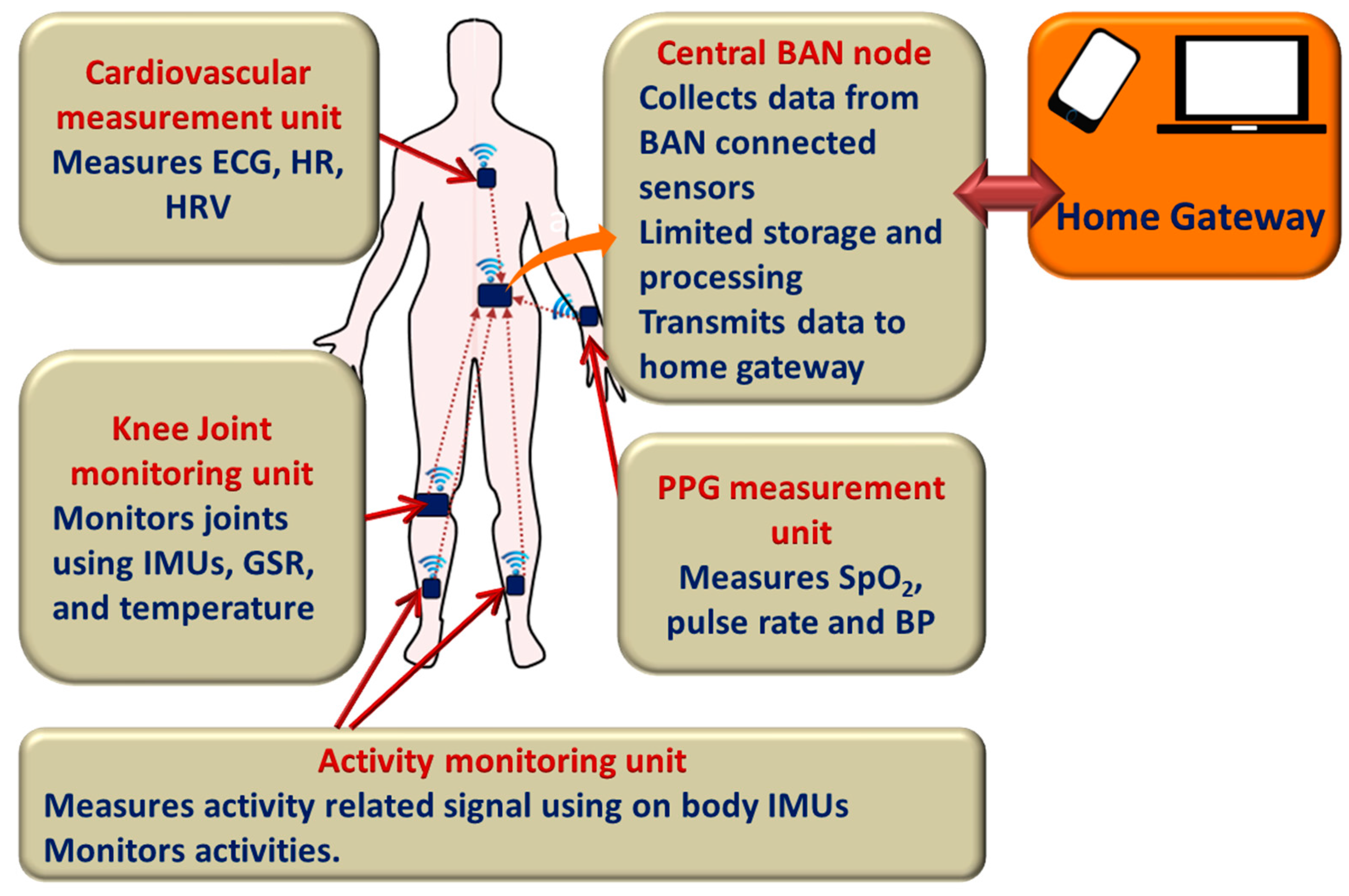
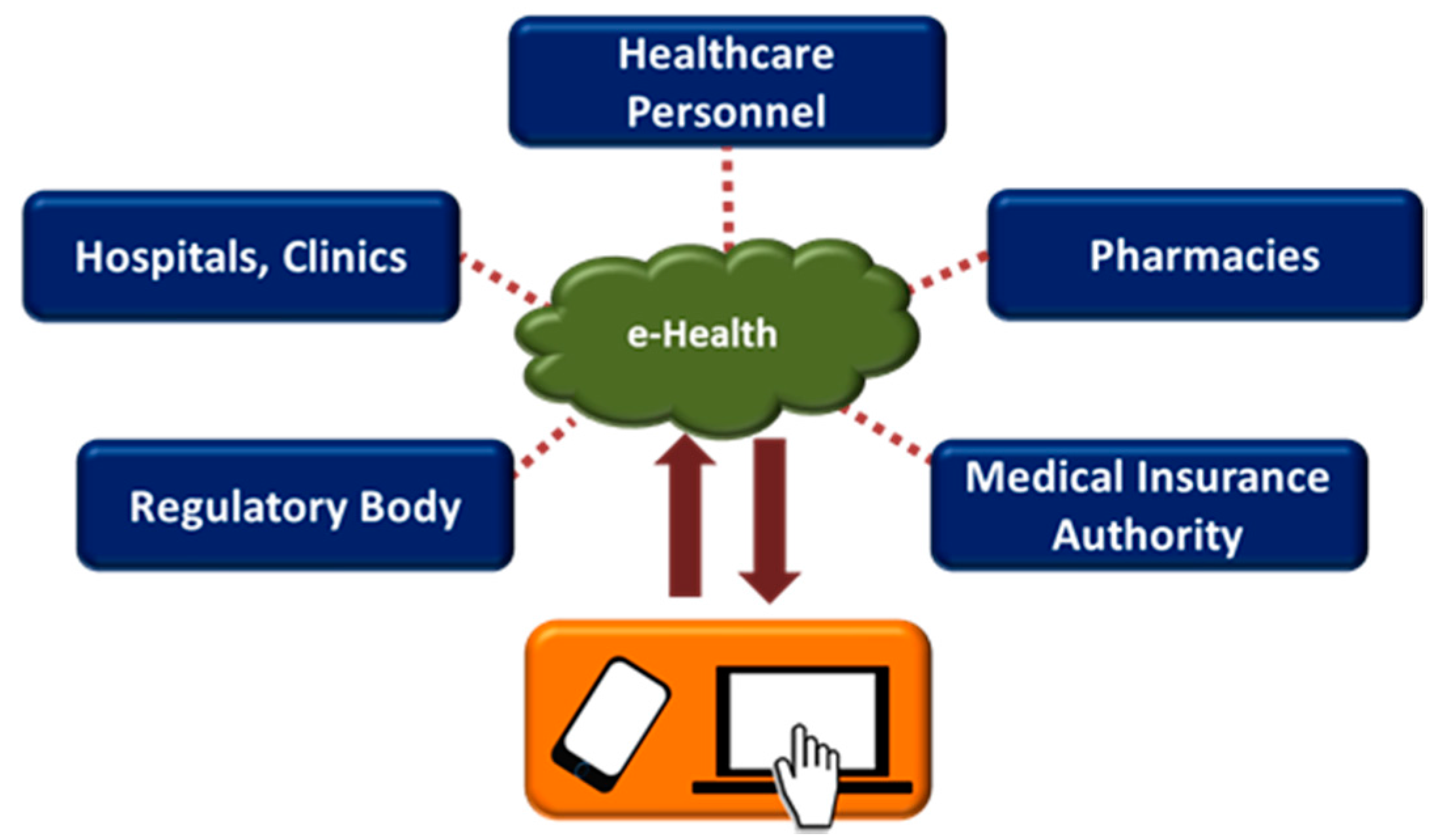
3.1. E-Health and M-Health
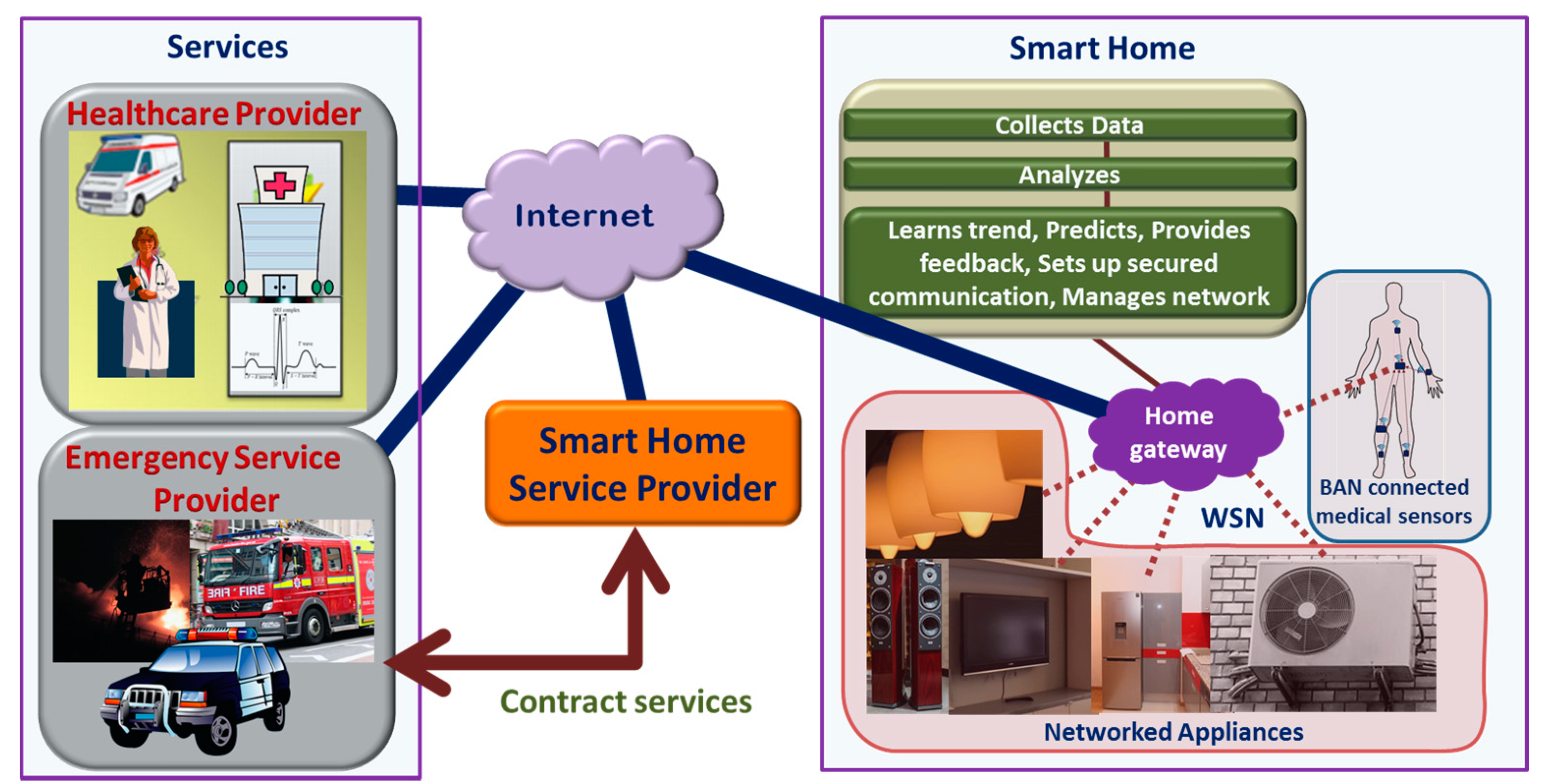
3.2. Home-Based Remote Health Monitoring
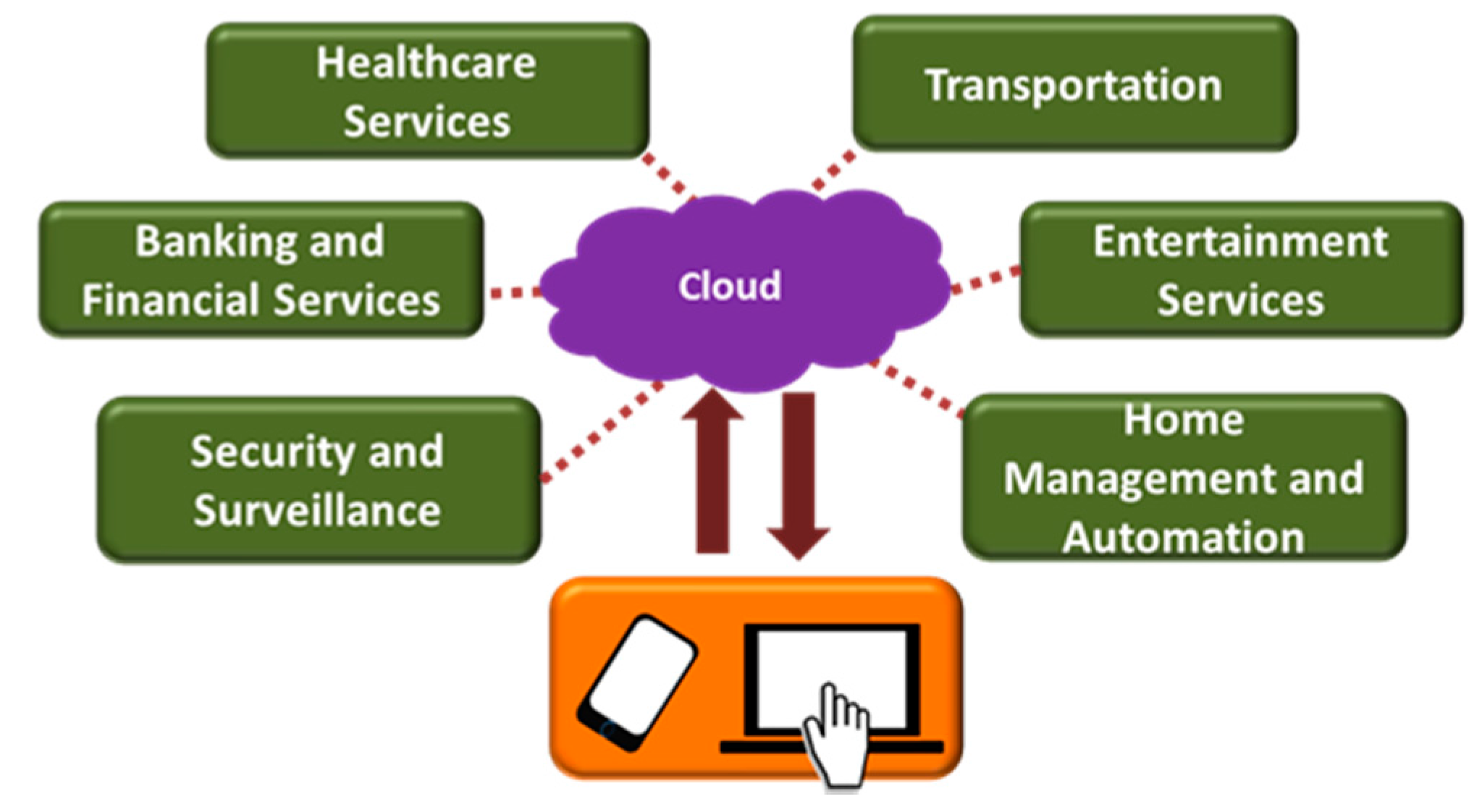
4. Internet-of-Things and Connected Homes
4.1. Layered Architechture of Smart Home
4.1.1. Sensors and Actuators
4.1.2. Communication Network
4.1.3. Computing and Decision Making Platform
4.1.4. Services
4.2. Interoperability and Standardization
5. Smart Monitoring Systems for Elderly and People with Disability
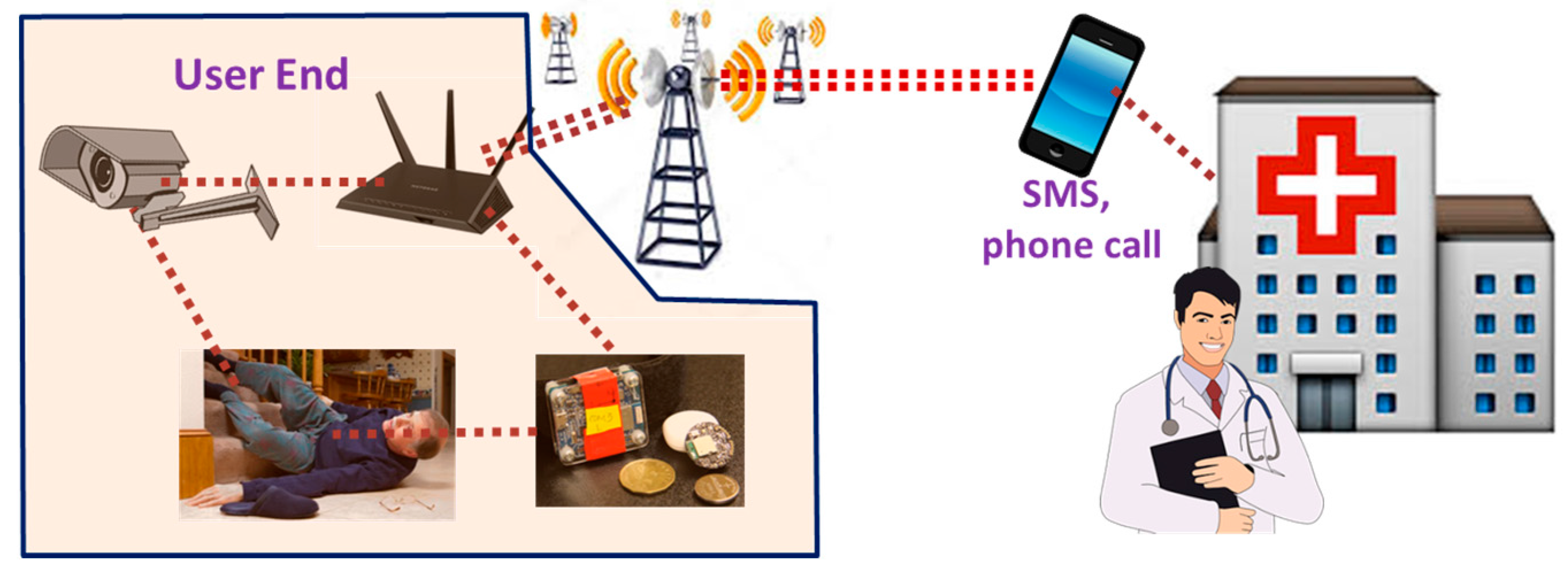
5.1. Automated Emergency Call Systems
5.2. Automated Activity and Fall Detection Systems
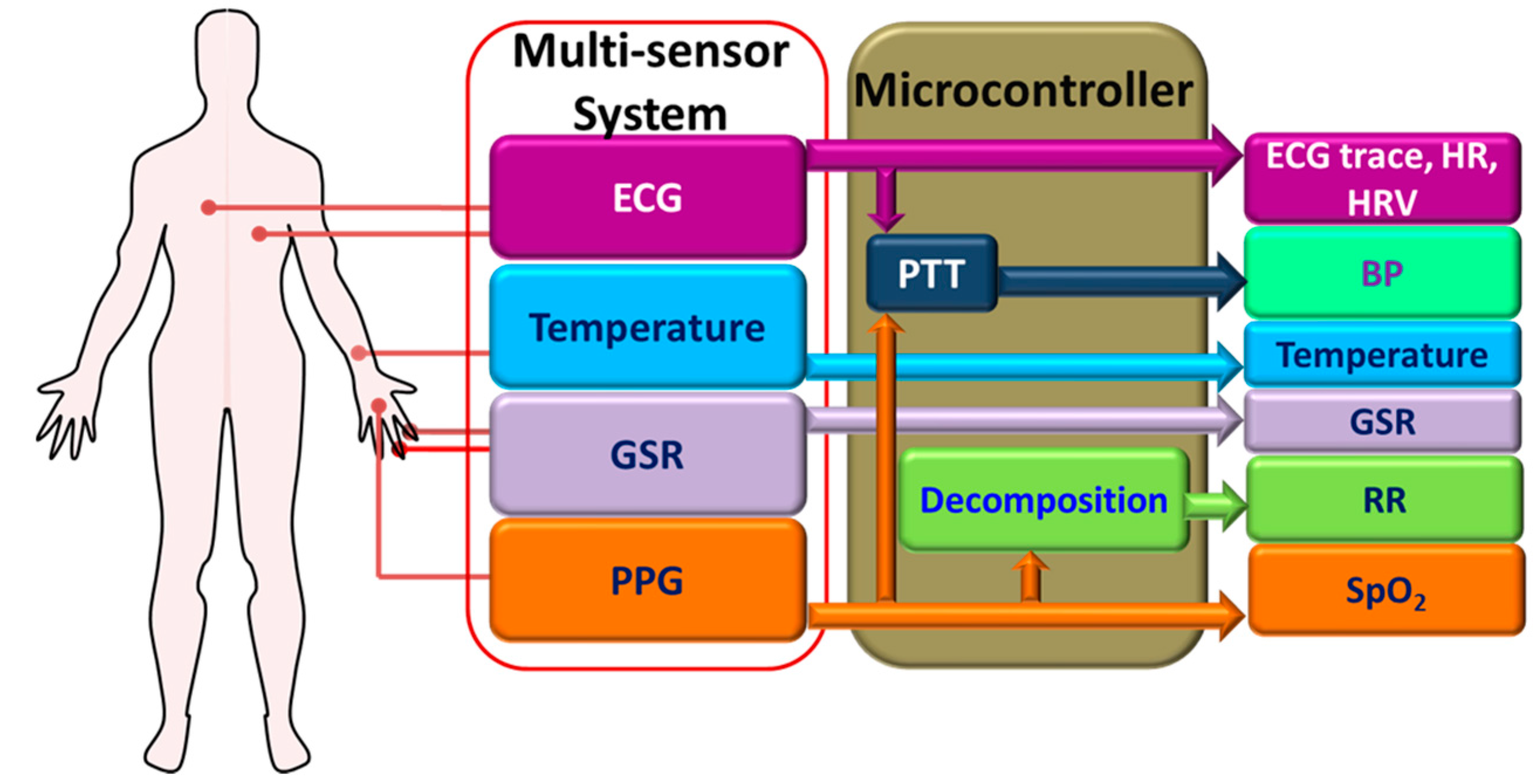
5.3. Vital Signs Monitoring Systems
5.4. Reminding Systems
5.5. Automated Health Assessment
6. Smart Homes for Elderly Healthcare: Prototypes and Commercial Solutions
6.1. Smart Home Solutions in the Literature
6.2. Commercial Solutions for Remote Elderly Care
7. Research Challenges for Smart Homes
8. Future Perspectives and Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Thomas, V.S.; Darvesh, S.; MacKnight, C.; Rockwood, K. Estimating the prevalence of dementia in elderly people: A comparison of the Canadian Study of Health and Aging and National Population Health Survey approaches. Int. Psychogeriatr. 2001, 13, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Kalache, A.; Gatti, A. Active ageing: A policy framework. Adv. Gerontol. Uspekhi Gerontol. Akad. Nauk. Gerontol. Obs. 2002, 11, 7–18. [Google Scholar]
- World Health Organization (WHO). Are you ready? What You Need to Know about Ageing. Available online: http://www.who.int/world-health-day/2012/toolkit/background/en/ (accessed on 11 May 2017).
- Kulik, C.T.; Ryan, S.; Harper, S.; George, G. Aging Populations and Management. Acad. Manag. J. 2014, 57, 929–935. [Google Scholar] [CrossRef]
- World Health Organization. Disability and Health. Available online: http://www.who.int/mediacentre/factsheets/fs352/en/ (accessed on 11 May 2017).
- Centers for Disease Control and Prevention. Chronic Disease Overview. Available online: http://www.cdc.gov/chronicdisease/overview/ (accessed on 11 May 2017).
- Centers for Disease Control and Prevention. Deaths and Mortality. Available online: https://www.cdc.gov/nchs/fastats/deaths.htm (accessed on 11 May 2017).
- Ontario. Budget in Brief: Strengthening Health Care. Available online: https://www.ontario.ca/page/2017-budget-brief-strengthening-health-care (accessed on 23 May 2017).
- Venkat, R. Global Outlook of the Healthcare Industry; Frost & Sullivan: San Antonio, TX, USA, 2015. [Google Scholar]
- Population Ageing Projections. Available online: http://www.helpage.org/global-agewatch/population-ageing-data/population-ageing-projections/ (accessed on 4 June 2017).
- Gelineau, K. Canada Ranks Fifth in Well-Being of Elderly: Study. The Globe and Mail. Available online: https://www.theglobeandmail.com/life/health-and-fitness/health/canada-ranks-fifth-in-well-being-of-elders-study/article14621721/ (accessed on 4 June 2017).
- Canadian Institute for Health Information. National Health Expenditure Trends, 1975 to 2014. Available online: https://www.cihi.ca/en/nhex_2014_report_en.pdf (accessed on 4 June 2017).
- The Economist. Working-Age Shift. Available online: http://www.economist.com/news/finance-and-economics/21570752-growth-will-suffer-workers-dwindle-working-age-shift (accessed on 4 June 2017).
- Anderson, G.; Knickman, J.R. Changing the Chronic Care System to Meet Peoples Needs. Health Aff. 2001, 20, 146–160. [Google Scholar] [CrossRef]
- Advantages & Disadvantages of Nursing Homes. AmeriGlide Stair Lifts and Vertical Platform Lifts. Available online: http://www.ameriglide.com/advantages-disadvantages-nursing-homes.htm (accessed on 11 May 2017).
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable Sensors for Remote Health Monitoring. Sensors 2017, 17, 45. [Google Scholar] [CrossRef] [PubMed]
- Deen, M.J. Information and communications technologies for elderly ubiquitous healthcare in a smart home. Pers. Ubiquitous Comput. 2015, 19, 573–599. [Google Scholar] [CrossRef]
- Agoulmine, N.; Deen, M.J.; Lee, J.-S.; Meyyappan, M. U-Health Smart Home. IEEE Nanotechnol. Mag. 2011, 5, 6–11. [Google Scholar] [CrossRef]
- Van Hoof, J.; Demiris, G.; Wouters, E.J.M. Handbook of Smart Homes, Health Care and Well-Being; Springer: Basel, Switzerland, 2017. [Google Scholar]
- Pantelopoulos, A.; Bourbakis, N. A Survey on Wearable Sensor-Based Systems for Health Monitoring and Prognosis. IEEE Trans. Syst. Man Cybern. Part C (Appl. Rev.) 2010, 40, 1–12. [Google Scholar] [CrossRef]
- Atzori, L.; Iera, A.; Morabito, G. The internet of things: A survey. Comput. Netw. 2010, 54, 2787–2805. [Google Scholar] [CrossRef]
- International Telecommunication Union (ITU). ITU Internet Reports 2005: The Internet of Things. Available online: https://www.itu.int/pub/S-POL-IR.IT-2005/e (accessed on 11 May 2017).
- Bassi, A.; Horn, G. Internet of Things in 2020: A Roadmap for the Future. Eur. Commun. Inf. Soc. Media 2008, 22, 97–114. [Google Scholar]
- Shah, S.H.; Iqbal, A.; Shah, S.S.A. Remote health monitoring through an integration of wireless sensor networks, mobile phones amp; Cloud Computing technologies. In Proceedings of the 2013 IEEE Global Humanitarian Technology Conference (GHTC), San Jose, CA, USA, 20–23 October 2013; pp. 401–405. [Google Scholar]
- Chen, C.; Pomalaza-Raez, C. Design and Evaluation of a Wireless Body Sensor System for Smart Home Health Monitoring. In Proceedings of the GLOBECOM 2009 IEEE Global Telecommunications Conference, Honolulu, HI, USA, 30 November–4 December 2009; pp. 1–6. [Google Scholar]
- Park, Y.-J.; Cho, H.-S. Transmission of ECG data with the patch-type ECG sensor system using Bluetooth Low Energy. In Proceedings of the 2013 International Conference on ICT Convergence (ICTC), Jeju Island, Korea, 14–16 October 2013; pp. 289–294. [Google Scholar]
- Rotariu, C.; Pasarica, A.; Costin, H.; Adochiei, F.; Ciobotariu, R. Telemedicine system for remote blood pressure and heart rate monitoring. In Proceedings of the 2011 E-Health and Bioengineering Conference (EHB), Iasi, Romania, 24–26 November 2011; pp. 1–4. [Google Scholar]
- Statista. Total Market Value of the Global Smart Homes Market in 2014 and 2020 (in Billion U.S. Dollars). Available online: http://www.statista.com/statistics/420755/global-smart-homes-market-value/ (accessed on 11 May 2017).
- Greenough, J. The US Smart Home Market Has Been Struggling—Here’s How and Why the Market Will Take off. Business Insider. Available online: http://www.businessinsider.com/the-us-smart-home-market-report-adoption-forecasts-top-products-and-the-cost-and-fragmentation-problems-that-could-hinder-growth-2015-9 (accessed on 26 May 2017).
- Meola, A. How IoT & Smart Home Automation Will Change the Way We Live. Business Insider. Available online: http://www.businessinsider.com/internet-of-things-smart-home-automation-2016-8 (accessed on 11 May 2017).
- Ullah, S.; Higgins, H.; Braem, B.; Latre, B.; Blondia, C.; Moerman, I.; Saleem, S.; Rahman, Z.; Kwak, K.S. A comprehensive survey of wireless body area networks. J. Med. Syst. 2012, 36, 1065–1094. [Google Scholar] [CrossRef] [PubMed]
- Latré, B.; Braem, B.; Moerman, I.; Blondia, C.; Demeester, P. A survey on wireless body area networks. Wirel. Netw. 2010, 17, 1–18. [Google Scholar] [CrossRef]
- Movassaghi, S.; Abolhasan, M.; Lipman, J.; Smith, D.; Jamalipour, A. Wireless Body Area Networks: A Survey. IEEE Commun. Surv. Tutor. 2014, 16, 1658–1686. [Google Scholar] [CrossRef]
- Hadjem, M.; Salem, O.; Abdesselam, F.N.; Mehaoua, A. Early detection of Myocardial Infarction using WBAN. In Proceedings of the 2013 IEEE 15th International Conference on e-Health Networking, Applications and Services (Healthcom 2013), Lisbon, Portugal, 9–12 October 2013; pp. 135–139. [Google Scholar]
- Lipprandt, M.; Eichelberg, M.; Thronicke, W.; Kruger, J.; Druke, I.; Willemsen, D.; Busch, C.; Fiehe, C.; Zeeb, E.; Hein, A. OSAMI-D: An open service platform for healthcare monitoring applications. In Proceedings of the 2009 2nd Conference on Human System Interactions, Catania, Italy, 21–23 May 2009. [Google Scholar]
- Shivakumar, N.S.; Sasikala, M. Design of vital sign monitor based on wireless sensor networks and telemedicine technology. In Proceedings of the 2014 International Conference on Green Computing Communication and Electrical Engineering (ICGCCEE), Coimbatore, India, 6–8 March 2014; pp. 1–5. [Google Scholar]
- World Health Organization. Cardiovascular Diseases (CVDs). Available online: http://www.who.int/cardiovascular_diseases/en/ (accessed on 11 July 2017).
- Mathers, C.D.; Loncar, D. Projections of Global Mortality and Burden of Disease from 2002 to 2030. PLoS Med. 2006, 3, 11. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Asthma. Available online: http://www.who.int/mediacentre/factsheets/fs307/en/ (accessed on 11 May 2017).
- Centers for Disease Control and Prevention. Chronic Disease Prevention and Health Promotion. Available online: https://www.cdc.gov/chronicdisease/ (accessed on 11 May 2017).
- Takei, K.; Honda, W.; Harada, S.; Arie, T.; Akita, S. Toward flexible and wearable human-interactive health-monitoring devices. Adv. Healthc. Mater. 2015, 4, 487–500. [Google Scholar] [CrossRef] [PubMed]
- Varshney, U. Pervasive Healthcare Computing: EMR/EHR, Wireless and Health Monitoring; Springer Science & Business Media: Berlin, Germany, 2009. [Google Scholar]
- Poissant, L.; Pereira, J.; Tamblyn, R.; Kawasumi, Y. The impact of electronic health records on time efficiency of physicians and nurses: A systematic review. J. Am. Med. Inform. Assoc. 2005, 12, 505–516. [Google Scholar] [CrossRef] [PubMed]
- Menachemi, N.; Taleah, C.H. Benefits and drawbacks of electronic health record systems. Risk Manag. Healthc. Policy 2011, 4, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Lorenzi, N.M.; Kouroubali, A.; Detmer, D.E.; Bloomrosen, M. How to successfully select and implement electronic health records (EHR) in small ambulatory practice settings. BMC Med. Inform. Decis. Mak. 2009, 9, 15. [Google Scholar] [CrossRef] [PubMed]
- Kyriacou, E.; Pattichis, M.S.; Pattichis, C.S.; Panayides, A.; Pitsillides, A. m-Health e-Emergency Systems: Current Status and Future Directions [Wireless corner]. Antennas Propag. Mag. IEEE 2007, 49, 216–231. [Google Scholar]
- Patel, M.; Wang, J. Applications, challenges, and prospective in emerging body area networking technologies. Wirel. Commun. IEEE 2010, 17, 80–88. [Google Scholar] [CrossRef]
- Benavides, G.M.; Duque, J.D.L. EnViBo: Embedded network for vital sign and Biomedical Signal Monitoring. In Proceedings of the 2014 IEEE Colombian Conference on Communications and Computing (COLCOM), Bogota, Colombia, 4–6 June 2014; pp. 1–6. [Google Scholar]
- Kuryloski, P.; Giani, A.; Giannantonio, R.; Gilani, K.; Gravina, R.; Seppa, V.-P.; Seto, E.; Shia, V.; Wang, C.; Yan, P.; et al. DexterNet: An open platform for heterogeneous body sensor networks and its applications. In Proceedings of the 2009 Sixth International Workshop on Wearable and Implantable Body Sensor Networks (BSN 2009), Berkeley, CA, USA, 3–5 June 2009; pp. 92–97. [Google Scholar]
- Kim, H.H.; Ha, K.N.; Lee, S.; Lee, K.C. Resident Location-Recognition Algorithm Using a Bayesian Classifier in the PIR Sensor-Based Indoor Location-Aware System. IEEE Trans. Syst. Man Cybern. Part C (Appl. Rev.) 2009, 39, 240–245. [Google Scholar]
- Lu, C.-H.; Fu, L.-C. Robust Location-Aware Activity Recognition Using Wireless Sensor Network in an Attentive Home. IEEE Trans. Autom. Sci. Eng. 2009, 6, 598–609. [Google Scholar]
- Lin, M.-H.; Yuan, W.-L.; Huang, T.-C.; Zhang, H.-F.; Mai, J.-T.; Wang, J.-F. Clinical effectiveness of telemedicine for chronic heart failure: A systematic review and meta-analysis. J. Investig. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Abo-Zahhad, M.; Ahmed, S.M.; Elnahas, O. A Wireless Emergency Telemedicine System for Patients Monitoring and Diagnosis. Int. J. Telemed. Appl. 2014, 2014, 4. [Google Scholar] [CrossRef] [PubMed]
- En. Healthcare. Available online: http://www.polycom.com/collaboration-solutions/solutions-by-industry/healthcare.html (accessed on 11 May 2017).
- Vidyo. Telemedicine & Telehealth Video Conferencing Solutions. Available online: https://www.vidyo.com/video-conferencing-solutions/healthcare (accessed on 12 May 2017).
- The Simple, Free & Secure Telemedicine Solution™. Telemedicine Solution—Simple, Free, and Secure|Doxy Me. Available online: https://doxy.me/ (accessed on 11 May 2017).
- VSee. HIPAA Video Chat Telemedicine Platform. Available online: https://vsee.com/ (accessed on 11 May 2017).
- Madakam, S.; Ramaswamy, R.; Tripathi, S. Internet of Things (IoT): A Literature Review. J. Comput. Commun. 2015, 3, 164–173. [Google Scholar] [CrossRef]
- Aggarwal, R.; Das, M.L. RFID security in the context of ‘internet of things’. In Proceedings of the First International Conference on Security of Internet of Things—SecurIT ’12, Kollam, India, 17–19 August 2012; pp. 51–56. [Google Scholar]
- National Intelligence Council. Available online: https://fas.org/irp/nic/ (accessed on 11 May 2017).
- Miorandi, D.; Sicari, S.; de Pellegrini, F.; Chlamtac, I. Internet of things: Vision, applications and research challenges. Ad Hoc Netw. 2012, 10, 1497–1516. [Google Scholar] [CrossRef]
- Weiser, M. The Computer for the 21st Century. Sci. Am. 1991, 265, 94–104. [Google Scholar] [CrossRef]
- Noury, N.; Virone, G.; Barralon, P.; Ye, J.; Rialle, V.; Demongeot, J. New trends in health smart homes. In Proceedings of the 5th International Workshop on Enterprise Networking and Computing in Healthcare Industry, Santa Monica, CA, USA, 7 June 2003; pp. 118–127. [Google Scholar]
- Zhou, C.; Huang, W.; Zhao, X. Study on architecture of smart home management system and key devices. In Proceedings of the 2013 3rd International Conference on Computer Science and Network Technology (ICCSNT), Dalian, China, 12–13 October 2013; pp. 1255–1258. [Google Scholar]
- Li, B.; Yu, J. Research and Application on the Smart Home Based on Component Technologies and Internet of Things. Procedia Eng. 2011, 15, 2087–2092. [Google Scholar] [CrossRef]
- Zanella, A.; Bui, N.; Castellani, A.; Vangelista, L.; Zorzi, M. Internet of things for smart cities. IEEE Internet Things J. 2014, 1, 22–32. [Google Scholar] [CrossRef]
- Park, S.; Kautz, H. Hierarchical recognition of activities of daily living using multi-scale, multi-perspective vision and RFID. In Proceedings of the 4th International Conference on Intelligent Environments (IE 08), Seattle, WA, USA, 21–22 July 2008; pp. 1–4. [Google Scholar]
- Hussain, S.; Schaffner, S.; Moseychuck, D. Applications of Wireless Sensor Networks and RFID in a Smart Home Environment. In Proceedings of the 2009 Seventh Annual Communication Networks and Services Research Conference, Moncton, NB, Canada, 11–13 May 2009; pp. 153–157. [Google Scholar]
- Ha, K.; Lee, K.; Lee, S. Development of PIR sensor based indoor location detection system for smart home. In Proceedings of the 2006 SICE-ICASE International Joint Conference, Busan, Korea, 18–21 October 2006; pp. 2162–2167. [Google Scholar]
- EnOcean GmbH|Kolpingring 18a|D-82041 Oberhaching. EnOcean. Smart Home Applications for Home Automation Using Energy Harvesting Wireless Sensor Technology|EnOcean—Applications. Available online: https://www.enocean.com/en/internet-of-things-applications/smart-home-and-home-automation/ (accessed on 11 May 2017).
- Axisa, F.; Schmitt, P.M.; Gehin, C.; Delhomme, G.; McAdams, E.; Dittmar, A. Flexible technologies and smart clothing for citizen medicine, home healthcare, and disease prevention. IEEE Trans. Inf. Technol. Biomed. 2005, 9, 325–336. [Google Scholar] [CrossRef]
- Lymberis, A. Smart wearable systems for personalised health management: Current R&D and future challenges. In Proceedings of the 25th Annual International Conference of the IEEE, Engineering in Medicine and Biology Society, Cancun, Mexico, 17–21 September 2003; Volume 4, pp. 3716–3719. [Google Scholar]
- Alam, M.R.; Reaz, M.B.I.; Ali, M.A.M. A Review of Smart Homes—Past, Present, and Future. IEEE Trans. Syst. Man Cybern. Part C (Appl. Rev.) 2012, 42, 1190–1203. [Google Scholar] [CrossRef]
- Abbasi-Kesbi, R.; Memarzadeh-Tehran, H.; Deen, M.J. Technique to estimate human reaction time based on visual perception. Healthc. Technol. Lett. 2017, 4, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Chen, Z.; Yang, L.T.; Zhang, Q.; Deen, M.J. Deep Convolutional Computation Model for Feature Learning on Big Data in Internet of Things. IEEE Trans. Ind. Inform. 2017. [Google Scholar] [CrossRef]
- Wang, X.; Yang, L.T.; Feng, J.; Chen, X.; Deen, M.J. A Tensor-Based Big Service Framework for Enhanced Living Environments. IEEE Cloud Comput. 2016, 3, 36–43. [Google Scholar] [CrossRef]
- Zhang, Q.; Yang, L.T.; Chen, Z.; Li, P.; Deen, M.J. Privacy-preserving Double-projection Deep Computation Model with Crowdsourcing on Cloud for Big Data Feature Learning. IEEE Internet Things J. 2017. [Google Scholar] [CrossRef]
- Ramos, C.; Augusto, J.C.; Shapiro, D. Ambient Intelligence—The Next Step for Artificial Intelligence. IEEE Intell. Syst. 2008, 23, 15–18. [Google Scholar] [CrossRef]
- Xu, K.; Wang, X.; Wei, W.; Song, H.; Mao, B. Toward software defined smart home. IEEE Commun. Mag. 2016, 54, 116–122. [Google Scholar] [CrossRef]
- Das, S.; Cook, D.; Battacharya, A.; Heierman, E.; Lin, T.-Y. The role of prediction algorithms in the MavHome smart home architecture. IEEE Wirel. Commun. 2002, 9, 77–84. [Google Scholar] [CrossRef]
- Amiribesheli, M.; Benmansour, A.; Bouchachia, A. A review of smart homes in healthcare. J. Ambient Intell. Humaniz. Comput. 2015, 6, 495–517. [Google Scholar] [CrossRef]
- Rashidi, P.; Cook, D. Keeping the Resident in the Loop: Adapting the Smart Home to the User. IEEE Trans. Syst. Man Cybern. Part A Syst. Hum. 2009, 39, 949–959. [Google Scholar] [CrossRef]
- Rantz, M.J.; Porter, R.T.; Cheshier, D.; Otto, D.; Servey, C.H.; Johnson, R.A.; Aud, M.; Skubic, M.; Tyrer, H.; He, Z.; et al. TigerPlace, A State-Academic-Private Project to Revolutionize Traditional Long-Term Care. J. Hous. Elder. 2008, 22, 66–85. [Google Scholar] [CrossRef] [PubMed]
- Wilbik, A.; Keller, J.M.; Alexander, G.L. Linguistic summarization of sensor data for eldercare. In Proceedings of the 2011 IEEE International Conference on Systems, Man, and Cybernetics, Anchorage, AK, USA, 9–12 October 2011. [Google Scholar]
- Amato, G.; Bacciu, D.; Broxvall, M.; Chessa, S.; Coleman, S.; Rocco, M.D.; Dragone, M.; Gallicchio, C.; Gennaro, C.; Lozano, H.; et al. Robotic Ubiquitous Cognitive Ecology for Smart Homes. J. Intell. Robot. Syst. 2015, 80, 57–81. [Google Scholar] [CrossRef]
- Huijnen, C.; Badii, A.; Heuvel, H.V.D.; Caleb-Solly, P.; Thiemert, D. Maybe It Becomes a Buddy, But Do Not Call It a Robot”—Seamless Cooperation between Companion Robotics and Smart Homes. In Lecture Notes in Computer Science Ambient Intelligence; Springer: Cham, Switzerland, 2011; pp. 324–329. [Google Scholar]
- Microsoft Research. HomeOS: Enabling Smarter Homes for Everyone. Available online: https://www.microsoft.com/en-us/research/project/homeos-enabling-smarter-homes-for-everyone/ (accessed on 11 May 2017).
- Mumtaz, S.; Alsohaily, A.; Pang, Z.; Rayes, A.; Tsang, K.F.; Rodriguez, J. Massive Internet of Things for Industrial Applications: Addressing Wireless IIoT Connectivity Challenges and Ecosystem Fragmentation. IEEE Ind. Electron. Mag. 2017, 11, 28–33. [Google Scholar] [CrossRef]
- JaeSeung, S.; Kunz, A.; Al Marzouqi, N.; Legare, C.; Costa, J. Standards News. IEEE Commun. Mag. 2016, 54, 14–16. [Google Scholar]
- Meddeb, A. Internet of things standards: Who stands out from the crowd? IEEE Commun. Mag. 2016, 54, 40–47. [Google Scholar] [CrossRef]
- Next Generation Mobile Networks (NGMN). 5G Prospects—Key Capabilities to Unlock Digital Opportunities, V. 1.1. Available online: https://www.ngmn.org/uploads/media/160701_NGMN_BPG_Capabilities_Whitepaper_v1_1.pdf (accessed on 11 May 2017).
- ABB-Free@Home®. ABB-Free@Home—Home and Building Automation. Available online: http://new.abb.com/low-voltage/products/building-automation/product-range/abb-freeathome (accessed on 25 August 2017).
- Connected Home. What Is Thread? Available online: https://threadgroup.org/What-is-Thread/Connected-Home (accessed on 25 August 2017).
- ASEA Brown Boveri (ABB). A New Age of Industrial Production: The Internet of Things, Services and People. Available online: http://new.abb.com/docs/default-source/technology/a-new-age-of-industrial-production---iotsp.pdf (accessed on 25 August 2017).
- Hughes, K. European Telecommunications Standards Institute (ETSI). CoAP 4 Plugtests. Available online: http://www.etsi.org/news-events/events/741-plugtests-2014-coap4 (accessed on 25 August 2017).
- Sfez, A.C.A. European Telecommunications Standards Institute (ETSI). 6LoWPAN Plugtests. Available online: http://www.etsi.org/news-events/events/663-2013-6lowpan-plugtest (accessed on 25 August 2017).
- Internet Engineering Task Force (IETF) Tools. Neighbor Discovery Optimization for IPv6 over Low-Power Wireless Personal Area Networks (6LoWPANs). Available online: https://tools.ietf.org/html/rfc6775 (accessed on 25 August 2017).
- Mineraud, J.; Mazhelis, O.; Su, X.; Tarkoma, S. A gap analysis of Internet-of-Things platforms. Comput. Commun. 2016, 89–90, 5–16. [Google Scholar] [CrossRef]
- Atzori, L.; Iera, A.; Morabito, G. From “smart objects” to “social objects”: The next evolutionary step of the internet of things. IEEE Commun. Mag. 2014, 52, 97–105. [Google Scholar] [CrossRef]
- Wolf, M. Here’s Why Elder Care May be the Next Billion Dollar Technology Opportunity. Forbes. Available online: http://www.forbes.com/sites/michaelwolf/2014/04/24/heres-why-elder-care-may-be-the-next-billion-dollar-technology-opportunity/#43d7d7f67226 (accessed on 11 May 2017).
- Arcelus, A.; Jones, M.H.; Goubran, R.; Knoefel, F. Integration of Smart Home Technologies in a Health Monitoring System for the Elderly. In Proceedings of the 21st International Conference on Advanced Information Networking and Applications Workshops (AINAW’07), Niagara Falls, ON, Canada, 21–23 May 2007; Volume 2, pp. 820–825. [Google Scholar]
- Avgerinakis, K.; Briassouli, A.; Kompatsiaris, I. Recognition of activities of daily living for smart home environments. In Proceedings of the 2013 9th International Conference on Intelligent Environments (IE), Athens, Greece, 16–17 July 2013; pp. 173–180. [Google Scholar]
- Edwards, W.K.; Grinter, R.E. At home with ubiquitous computing: Seven challenges. In Proceedings of the UbiComp: International Conference on Ubiquitous Computing, Atlanta GA, USA, 30 September–2 October 2001; pp. 256–272. [Google Scholar]
- Rashidi, P.; Mihailidis, A. A survey on ambient-assisted living tools for older adults. IEEE J. Biomed. Heal. Inform. 2013, 17, 579–590. [Google Scholar] [CrossRef]
- Bottazzi, D.; Corradi, A.; Montanari, R. Context-aware middleware solutions for anytime and anywhere emergency assistance to elderly people. IEEE Commun. Mag. 2006, 44, 82–90. [Google Scholar] [CrossRef]
- Choudhury, B.; Choudhury, T.S.; Pramanik, A.; Arif, W.; Mehedi, J. Design and implementation of an SMS based home security system. In Proceedings of the 2015 IEEE International Conference on Electrical, Computer and Communication Technologies (ICECCT), Coimbatore, India, 5–7 March 2015; pp. 1–7. [Google Scholar]
- Freitas, D.J.; Marcondes, T.B.; Nakamura, L.H.V.; Ueyama, J.; Gomes, P.H.; Meneguette, R.I. Combining cell phones and WSNs for preventing accidents in smart-homes with disabled people. In Proceedings of the 2015 7th International Conference on New Technologies, Mobility and Security (NTMS), Paris, France, 27–29 July 2015; pp. 1–5. [Google Scholar]
- Raad, M.W.; Yang, L.T. A ubiquitous smart home for elderly. In Proceedings of the 2008 4th IET International Conference on Advances in Medical, Signal and Information Processing (MEDSIP 2008), Santa Margherita Ligure, Italy, 14–16 July 2008; pp. 1–4. [Google Scholar]
- Zhou, Z.; Dai, W.; Eggert, J.; Giger, J.; Keller, J.; Rantz, M.; He, Z. A real-time system for in-home activity monitoring of elders. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 6115–6118. [Google Scholar]
- Ni, B.; Wang, G.; Moulin, P. RGBD-HuDaAct: A Color-Depth Video Database for Human Daily Activity Recognition. In Consumer Depth Cameras for Computer Vision; Springer: London, UK, 2013; pp. 193–208. [Google Scholar]
- Perego, P.; Tarabini, M.; Bocciolone, M.; Andreoni, G. SMARTA: Smart Ambiente and Wearable Home Monitoring for Elderly. In Internet of Things, IoT Infrastructures; Springer: Cham, Switzerland, 2016; pp. 502–507. [Google Scholar]
- Le, X.H.B.; di Mascolo, M.; Gouin, A.; Noury, N. Health Smart Home—Towards an assistant tool for automatic assessment of the dependence of elders. In Proceedings of the 29th Annual International Conference of the IEEE the Engineering in Medicine and Biology Society (EMBS 2007), Lyon, France, 23–26 August 2007; pp. 3806–3809. [Google Scholar]
- Rashidi, P.; Cook, D.J. COM: A Method for Mining and Monitoring Human Activity Patterns in Home-Based Health Monitoring Systems. ACM Trans. Intell. Syst. Technol. 2013, 4, 1–20. [Google Scholar] [CrossRef]
- Yu, M.; Rhuma, A.; Naqvi, S.M.; Wang, L.; Chambers, J. A Posture Recognition-Based Fall Detection System for Monitoring an Elderly Person in a Smart Home Environment. IEEE Trans. Inf. Technol. Biomed. 2012, 16, 1274–1286. [Google Scholar]
- Popescu, M.; Li, Y.; Skubic, M.; Rantz, M. An acoustic fall detector system that uses sound height information to reduce the false alarm rate. In Proceedings of the 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBS 2008), Vancouver, BC, Canada, 21–24 August 2008; pp. 4628–4631. [Google Scholar]
- Wang, J.; Zhang, Z.; Li, B.; Lee, S.; Sherratt, R. An enhanced fall detection system for elderly person monitoring using consumer home networks. IEEE Trans. Consum. Electron. 2014, 60, 23–29. [Google Scholar] [CrossRef]
- Abbate, S.; Avvenuti, M.; Bonatesta, F.; Cola, G.; Corsini, P.; Vecchio, A. A smartphone-based fall detection system. Pervasive Mob. Comput. 2012, 8, 883–899. [Google Scholar] [CrossRef]
- Zhang, Q.; Ren, L.; Shi, W. HONEY: A multimodality fall detection and telecare system. Telemed. e-Health 2013, 19, 415–429. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Jang, D.-G.; Park, J.; Youm, S.-K. Wearable Sensing of In-Ear Pressure for Heart Rate Monitoring with a Piezoelectric Sensor. Sensors 2015, 15, 23402–23417. [Google Scholar] [CrossRef] [PubMed]
- Shu, Y.; Li, C.; Wang, Z.; Mi, W.; Li, Y.; Ren, T.-L. A Pressure sensing system for heart rate monitoring with polymer-based pressure sensors and an anti-interference post processing circuit. Sensors 2015, 15, 3224–3235. [Google Scholar] [CrossRef] [PubMed]
- Boano, C.A.; Lasagni, M.; Romer, K. Non-invasive measurement of core body temperature in Marathon Runners. In Proceedings of the 2013 IEEE International Conference on Body Sensor Networks, Cambridge, MA, USA, 6–9 May 2013; pp. 1–6. [Google Scholar]
- Milici, S.; Amendola, S.; Bianco, A.; Marrocco, G. Epidermal RFID passive sensor for body temperature Measurements. In Proceedings of the 2014 IEEE RFID Technology and Applications Conference (RFID-TA), Tampere, Finland, 8–9 September 2014; pp. 140–144. [Google Scholar]
- Gaddam, A.; Kaur, K.; Gupta, G.S.; Mukhopadhyay, S.C. Determination of sleep quality of inhabitant in a smart home using an intelligent bed sensing system. In Proceedings of the 2010 IEEE Instrumentation and Measurement Technology Conference (I2MTC), Austin, TX, USA, 3–6 May 2010; pp. 1613–1617. [Google Scholar]
- Gaddam, A.; Mukhopadhyay, S.C.; Gupta, G.S. Necessity of a bed-sensor in a smart digital home to care for elder-people. In Proceedings of the 2008 IEEE Sensors, Lecce, Italy, 26–29 October 2008; pp. 1340–1343. [Google Scholar]
- Barsocchi, P.; Bianchini, M.; Crivello, A.; Rosa, D.L.; Palumbo, F.; Scarselli, F. An unobtrusive sleep monitoring system for the human sleep behaviour understanding. In Proceedings of the 2016 7th IEEE International Conference on Cognitive Infocommunications (CogInfoCom), Wroclaw, Poland, 16–18 October 2016. [Google Scholar]
- Nam, Y.; Kim, Y.; Lee, J. Sleep Monitoring Based on a Tri-Axial Accelerometer and a Pressure Sensor. Sensors 2016, 16, 750. [Google Scholar] [CrossRef] [PubMed]
- Waltisberg, D.; Arnrich, B.; Tröster, G. Sleep Quality Monitoring with the Smart Bed in Pervasive Health; Springer: Berlin, Germany, 2014; pp. 211–227. [Google Scholar]
- Hong, Y.; Kim, S.-G.; Kim, B.-H.; Ha, S.-J.; Lee, H.-J.; Yun, G.-H.; Yook, J.-G. Noncontact Proximity Vital Sign Sensor Based on PLL for Sensitivity Enhancement. IEEE Trans. Biomed. Circuits Syst. 2014, 8, 584–593. [Google Scholar] [CrossRef] [PubMed]
- Adib, F.; Mao, H.; Kabelac, Z.; Katabi, D.; Miller, R.C. Smart Homes that Monitor Breathing and Heart Rate. In Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems—CHI’15, Seoul, Korea, 18–23 April 2015. [Google Scholar]
- Small, S.A.; Stern, Y.; Tang, M.; Mayeux, R. Selective decline in memory function among healthy elderly. Neurology 1999, 52, 1392. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.W.; Kim, M.C.; Park, S.H.; Jin, Y.K.; Choi, W.S. Gate reminder: A design case of a smart reminder. In Proceedings of the 5th Conference on Designing Interactive Systems: Processes, Practices, Methods, and Techniques, Cambridge, MA, USA, 1–4 August 2004; pp. 81–90. [Google Scholar]
- Zao, J.K.; Wang, M.-Y.; Tsai, P.; Liu, J.W.S. Smartphone based medicine in-take scheduler, reminder and monitor. In Proceedings of the 2010 12th IEEE International Conference on e-Health Networking Applications and Services (Healthcom), Lyon, France, 1–3 July 2010; pp. 162–168. [Google Scholar]
- Fahim, M.; Fatima, I.; Lee, S.; Lee, Y.-K. Daily life activity tracking application for smart homes using android smartphone. In Proceedings of the 2012 14th International Conference on Advanced Communication Technology (ICACT), PyeongChang, Korea, 19–22 February 2012; pp. 241–245. [Google Scholar]
- Moshnyaga, V.; Koyanagi, M.; Hirayama, F.; Takahama, A.; Hashimoto, K. A medication adherence monitoring system for people with dementia. In Proceedings of the 2016 IEEE International Conference on Systems, Man, and Cybernetics (SMC), Budapest, Hungary, 9–12 October 2016. [Google Scholar]
- Coutinho, E.S.F.; Bloch, K.V.; Coeli, C.M. One-year mortality among elderly people after hospitalization due to fall-related fractures: Comparison with a control group of matched elderly. Cad. Saúde Públ. 2012, 28, 801–805. [Google Scholar] [CrossRef]
- Snijders, A.H.; Warrenburg, B.P.V.D.; Giladi, N.; Bloem, B.R. Neurological gait disorders in elderly people: Clinical approach and classification. Lancet Neurol. 2007, 6, 63–74. [Google Scholar] [CrossRef]
- Bo, J.; Thu, T.H.; Baek, E.; Sakong, S.H.; Xiao, J.; Mondal, T.; Deen, M.J. Walking-Age Analyzer for Healthcare Applications. IEEE J. Biomed. Health Inform. 2014, 18, 1034–1042. [Google Scholar]
- Mandal, P.; Tank, K.; Monday, T.; Chen, C.-H.; Deen, M.J. Predictive Walking-Age Health Analyzer. IEEE J. Biomed. Health Inform. 2017. [Google Scholar] [CrossRef] [PubMed]
- Dawadi, P.N.; Cook, D.J.; Schmitter-Edgecombe, M. Automated Cognitive Health Assessment Using Smart Home Monitoring of Complex Tasks. IEEE Trans. Syst. Man Cybern. Syst. 2013, 43, 1302–1313. [Google Scholar] [CrossRef] [PubMed]
- Rabbi, M.; Ali, S.; Choudhury, T.; Berke, E. Passive and In-Situ assessment of mental and physical well-being using mobile sensors. In Proceedings of the 13th International Conference on Ubiquitous Computing—UbiComp 11, Beijing, China, 17–21 September 2011. [Google Scholar]
- Stefanov, D.H.; Bien, Z.; Bang, W.-C. The smart house for older persons and persons with physical disabilities: Structure, technology arrangements, and perspectives. Neural Syst. Rehabil. Eng. IEEE Trans. 2004, 12, 228–250. [Google Scholar] [CrossRef] [PubMed]
- Eckl, R.; MacWilliams, A. Smart home challenges and approaches to solve them: A practical industrial perspective. In Intelligent Interactive Assistance and Mobile Multimedia Computing; Springer: Berlin, Germany, 2009; pp. 119–130. [Google Scholar]
- Pang, Z.; Zheng, L.; Tian, J.; Kao-Walter, S.; Dubrova, E.; Chen, Q. Design of a terminal solution for integration of in-home health care devices and services towards the Internet-of-Things. Enterp. Inf. Syst. 2013, 9, 86–116. [Google Scholar] [CrossRef]
- Mozer, M.C. The neural network house: An environment hat adapts to its inhabitants. Proc. AAAI Spring Symp. Intell. Environ. 1998, 58, 110–114. [Google Scholar]
- Cook, D.J.; Youngblood, M.; I, E.O.H.I.I.; Gopalratnam, K.; Rao, S.; Litvin, A.; Khawaja, F. MavHome: An agent-based smart home. In Proceedings of the First IEEE International Conference on Pervasive Computing and Communications (PerCom 2003), Fort Worth, TX, USA, 26 March 2003; p. 521. [Google Scholar]
- Helal, S.; Mann, W.; El-Zabadani, H.; King, J.; Kaddoura, Y.; Jansen, E. The Gator Tech Smart House: A programmable pervasive space. Computer 2005, 38, 50–60. [Google Scholar] [CrossRef]
- Ricquebourg, V.; Menga, D.; Durand, D.; Marhic, B.; Delahoche, L.; Loge, C. The Smart Home Concept : Our immediate future. In Proceedings of the 2006 1st IEEE International Conference on E-Learning in Industrial Electronics, Hammamet, Tunisia, 18–20 December 2006; pp. 23–28. [Google Scholar]
- Hartkopf, V.; Loftness, V.; Mahdavi, A.; Lee, S.; Shankavaram, J. An integrated approach to design and engineering of intelligent buildings—The Intelligent Workplace at Carnegie Mellon University. Autom. Constr. 1997, 6, 401–415. [Google Scholar] [CrossRef]
- Kientz, J.A.; Patel, S.N.; Jones, B.; Price, E.; Mynatt, E.D.; Abowd, G.D. The Georgia Tech aware home. In Proceeding of the Twenty-Sixth Annual CHI Conference Extended Abstracts on Human Factors in Computing Systems—CHI 08, Florence, Italy, 5–10 April 2008. [Google Scholar]
- University Creates Medical “Smart Home” to Study Future Health Technology. Available online: https://www.urmc.rochester.edu/news/story/-103/university-creates-medical-smart-home-to-study-future-health-technology.aspx (accessed on 25 August 2017).
- Brooks, R.A. The Intelligent Room project. In Proceedings of the Second International Conference on Cognitive Technology Humanizing the Information Age, Aizu-Wakamatsu City, Japan, 25–28 August 1987. [Google Scholar]
- Soliman, M.; Abiodun, T.; Hamouda, T.; Zhou, J.; Lung, C.-H. Smart Home: Integrating Internet of Things with Web Services and Cloud Computing. In Proceedings of the 2013 IEEE 5th International Conference on Cloud Computing Technology and Science, Bristol, UK, 2–5 December 2013. [Google Scholar]
- Wang, X.; Yang, L.T.; Xie, X.; Jin, J.; Deen, M.J. Tensor-Based Big Data Framework for Enhanced Living Environments in Cyber-Physical-Social Systems. IEEE Commun. Mag. 2017, 55, 36–43. [Google Scholar]
- Yang, L.; Ge, Y.; Li, W.; Rao, W.; Shen, W. A home mobile healthcare system for wheelchair users. In Proceedings of the 2014 IEEE 18th International Conference on Computer Supported Cooperative Work in Design (CSCWD), Hsinchu, Taiwan, 21–23 May 2014. [Google Scholar]
- Jacobs, P.G.; Kaye, J.A. Ubiquitous Real-World Sensing and Audiology-Based Health Informatics. J. Am. Acad. Audiol. 2015, 26, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Ransing, R.S.; Rajput, M. Smart home for elderly care, based on Wireless Sensor Network. In Proceedings of the 2015 International Conference on Nascent Technologies in the Engineering Field (ICNTE), Navi Mumbai, India, 9–10 January 2015; pp. 1–5. [Google Scholar]
- Woznowski, P.; Burrows, A.; Diethe, T.; Fafoutis, X.; Hall, J.; Hannuna, S.; Camplani, M.; Twomey, N.; Kozlowski, M.; Tan, B.; et al. SPHERE: A Sensor Platform for Healthcare in a Residential Environment. In Designing, Developing, and Facilitating Smart Cities; Springer: Berlin, Germany, 2016; pp. 315–333. [Google Scholar]
- Pigini, L.; Bovi, G.; Panzarino, C.; Gower, V.; Ferratini, M.; Andreoni, G.; Sassi, R.; Rivolta, M.W.; Ferrarin, M. Pilot Test of a New Personal Health System Integrating Environmental and Wearable Sensors for Telemonitoring and Care of Elderly People at Home (SMARTA Project). Gerontology 2017, 63, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Health Apps, Cell Phones for Seniors, Medical Alert|GreatCall. Available online: https://www.greatcall.com/ (accessed on 11 May 2017).
- Medical Alert Systems from MobileHelp: Updated Review. Available online: https://www.theseniorlist.com/2017/02/mobilehelp-updated-review/ (accessed on 4 May 2017).
- Home. GrandCare. Available online: https://www.grandcare.com/ or https://grandcare.com/ (accessed on 4 May 2017).
- Jacobson, J. IoT Loose Ends: Alarm.com, Icontrol, Comcast, Vivint, Qolsys, FTC and the Smart-Home Landscape. Recently Filed Really Simple Syndication (RSS). Available online: https://www.cepro.com/article/iot_alarm.com_icontrol_comcast_vivint_qolsys_ftc_zendo_smart_home (accessed on 4 October 2017).
- A Smarter Solution for Independent Living. Available online: http://www.alarm.com/blog/wellness-solution (accessed on 4 October 2017).
- Caresmart. Remote SMART Monitoring. Available online: http://caresmart.ca/remote-smart-monitoring/ (accessed on 9 June 2017).
- Care Link Advantage. Care Link Advantage—Medical Care Systems for Independent Living. Available online: https://carelinkadvantage.ca/carelink_advantage.php (accessed on 9 June 2017).
- Independa, Inc. INDEPENDA—Care from Anywhere. Available online: http://www.independa.com/ (accessed on 11 May 2017).
- Rogers: Wireless, Internet, TV, Home Monitoring, and Home Phone. Available online: http://www.rogers.com/web/content/smart-home-monitoring-solutions-new?ipn=1 (accessed on 12 June 2017).
- Remote Monitoring. Available online: https://business.bell.ca/shop/enterprise/remote-monitoring-solutions (accessed on 12 June 2017 ).
- AT&T Smart Solutions—Smart Apps and Services from AT&T. Available online: https://www.att.com/att/smartsolutions/ (accessed on 12 June 2017).
- BT Home Products. Wi-Fi Extenders, Home Monitors and Home Phones|BT. Available online: https://www.productsandservices.bt.com/products/home-products/?s_intcid=userguideshelp_banner_productpages#home-monitoring (accessed on 12 June 2017).
- Philips. Healthcare|Patient Monitorings. Philips. Available online: http://www.philips.ca/healthcare/solutions/patient-monitoring (accessed on 12 June 2017).
- Health Care. BuildingSpace|ABB. Available online: http://new.abb.com/buildings/buildingspace/health-care (accessed on 12 June 2017).
- Diving Medical Services. Diving Medical Services|Iqarus. Available online: http://www.iqarus.com/our-solutions/offshore-and-onshore-services/diving-medical-services/ (accessed on 12 June 2017).
- Samsung Electronics America. Business Home. Available online: http://www.samsung.com/us/business/by-industry/healthcare-solutions/in-home (accessed on 11 May 2017).
- Pham, M.; Mengistu, Y.; Do, H.M.; Sheng, W. Cloud-Based Smart Home Environment (CoSHE) for home healthcare. In Proceedings of the 2016 IEEE International Conference on Automation Science and Engineering (CASE), Fort Worth, TX, USA, 21–25 August 2016. [Google Scholar]
- Coradeschi, S.; Cesta, A.; Cortellessa, G.; Coraci, L.; Galindo, C.; Gonzalez, J.; Karlsson, L.; Forsberg, A.; Frennert, S.; Furfari, F.; et al. GiraffPlus: A System for Monitoring Activities and Physiological Parameters and Promoting Social Interaction for Elderly. In Advances in Intelligent Systems and Computing Human-Computer Systems Interaction: Backgrounds and Applications 3; Springer: Berlin, Germany, 2014; pp. 261–271. [Google Scholar]
- Cazorla, M.; Garcıa-Rodrıguez, J.; Plaza, J.M.C.; Varea, I.G.; Matellán, V.; Rico, F.M.; Martınez-Gómez, J.; Lera, F.J.R.; Mejias, C.S.; Sahuquillo, M.E.M. SIRMAVED: Development of a comprehensive monitoring and interactive robotic system for people with acquired brain damage and dependent people. In Proceedings of the Actas de la XVI Conferencia CAEPIA, Albacete, Spain, 9–12 November 2015. [Google Scholar]
- Suryadevara, N.; Mukhopadhyay, S.; Wang, R.; Rayudu, R. Forecasting the behavior of an elderly using wireless sensors data in a smart home. Eng. Appl. Artif. Intell. 2013, 26, 2641–2652. [Google Scholar] [CrossRef]
- Cook, D.J.; Crandall, A.S.; Thomas, B.L.; Krishnan, N.C. CASAS: A Smart Home in a Box. Computer 2013, 46, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Tsukiyama, T. In-home Health Monitoring System for Solitary Elderly. Procedia Comput. Sci. 2015, 63, 229–235. [Google Scholar] [CrossRef]
- Medjahed, H.; Istrate, D.; Boudy, J.; Baldinger, J.-L.; Dorizzi, B. A pervasive multi-sensor data fusion for smart home healthcare monitoring. In Proceedings of the 2011 IEEE International Conference on Fuzzy Systems (FUZZ-IEEE 2011), Taipei, Taiwan, 27–30 June 2011. [Google Scholar]



| WBAN Applications | Wearable WBAN |
|
| Implantable WBAN |
| |
| Remote Health Monitoring |
| Wireless Tech. | Frequency | Range | Data Rate | Power (mW) | Maximum Nodes | Network Topologies | Security |
|---|---|---|---|---|---|---|---|
| RFID | 13.56 MHz 860–960 MHz | 0–3 m | 640 kbps | 200 | 1 at a time | peer-to-peer (P2P) passive | N/A |
| Bluetooth | 2.4–2.5 GHz | 1–100 m | 1–3 Mbps | 2.5–100 | 1 M + 7 S | P2P, star | 56–128 bit key |
| BLE | 2.4–2.5 GHz | 1–100 m | 1 Mbps | 10 | 1 M + 7 S | P2P, star | 128-bit AES |
| HomePlug GP | 1.8–30 MHz | ~100 m | 4–10 Mbps | 500 | - | P2P, star, tree and mesh | 128-bit AES |
| EnOcean | 902, 928, 868 MHz | 30–300 m | 125 kbps | ~0.05 with energy harvesting | - | P2P, star, tree and mesh | 128-bit AES |
| ZigBee | 2.4–2.5 GHz | 10–100 m | 250 kbps | 50 | 65,533 | P2P, star, tree and mesh | 128-bit AES |
| WiFi | 2.4–2.5 GHz | 150–200 m | 54 Mbps | 1000 | 255 | P2P, star | WEP,WPA, WPA2 |
| DASH7 | 315–915 MHz | 200 m–2 km | 167 kbps | <1 | - | P2P, star, tree and mesh | 128-bit AES |
| Insteon | RF: 869.85, 915, 921 MHz powerline: 131.65 KHz | 40–50 m | 38 kbps (RF) 2–13 kbps (powerline) | - | 64,000 nodes per network | P2P, star, tree and mesh | 256-bit AES |
| Sigfox | 868/902 MHz | 10–50 km | 10–1000 bps | 0.01–100 | - | P2P, star | No default encryption |
| NFC | 13.56 MHz | 5 cm | 424 kbps | 15 | 1 at a time | P2P | AES |
| Wireless HART™ | 2.4 GHz | 50–100 m | 10 | - | P2P, star, tree and mesh | 128-bit AES | |
| 6LoWPAN | 2.4 GHz | 25–50 m | 250 kbps | 2.23 | - | P2P, star, tree and mesh | 128-bit AES |
| ANT | 2.4–2.5 GHz | 30 m | 20–60 kbps | 0.01–1 | 65,533 in one channel | P2P, star, tree and mesh | 64-bit key |
| Z-Wave | 860–960 MHz | 100 m | 9.6–100 kbps | 100 | 232 | mesh | 128-bit AES |
| Ref. | Proposition | Country (Year) | Resident activity Monitoring | Home Environment Monitoring | Resident Health Monitoring | Home Appliance Monitoring | Wireless Connectivity | Summary | Alert/Reminder Service |
|---|---|---|---|---|---|---|---|---|---|
| [116] | Fall detection system for smart home | China and Korea (2014) |
| Temperature and humidity sensors | Pulse pressure sensor: HR | ZigBee with multiple access points | Proposed but not implemented | ||
| [133] | Daily activity tracking for smart home | Korea (2012) | RFID Tags and self-developed biosensor and logging system | RFID | Developed applications in android platform for tracking ADL of the elderly | Smartphone based application for the elderly and the caregivers, family | |||
| [153] | Smart home based on cloud computing | Canada (2013) |
| Temperature, humidity, ambient light | Light and fans | ZigBee, RFID | Arduino-based application communicates with the user, sensors, and actuators as well as interacts with the cloud-based computing service | ||
| [154] | Mobile healthcare system for wheelchair users | China and Canada (2014) |
| Temperature, humidity, smoke sensor |
| Lights and air conditions | ZigBee and Bluetooth | User can interact with the home environment remotely and locally via smart phones | Connected to a third-party service to notify emergency situation using SMS and telephone |
| [155] | Cloud-based platform for assessing elderly health and wellbeing | USA (2004 to date) |
| Air quality and room temperature | Weight, heart rate, and body mass index | Bluetooth, WiFi, Zigbee | Developed a cloud-based cognitive and physical health assessment platform using mostly commercial ambient and passive sensing technologies. | ||
| [156] | Smart home for elderly care | India (2015) |
| ZigBee | Developed an Arduino based software |
| |||
| [157] | Sensor platform for healthcare services in a home environment | Bristol, UK (2016) |
| Temperature, humidity, luminosity, noise level, air quality, occupancy | Electricity metering, cold and hot water consumption | BLE , IEEE 80 2.15.4, WiFi |
| Remote system generates the alerts | |
| [158] | Home tele-monitoring of vital parameters and detection of anomalies in daily activities | Milano, Italy (2017) |
| ECG , BP and SpO2 weight, ear temperature, glycaemia | Water tap, refrigerator, and dishwasher | Bluetooth LE | Developed a clinical governance system to interact between patient and clinicians | Clinical governance system generates and displays alerts both to the patient and the clinicians | |
| [175] | Cloud-based home healthcare | USA and China (2016) |
| ECG, SpO2 | ZigBee | Cloud based service for storage, processing and interaction with healthcare personnel | |||
| [176] | Activity and physiological parameter monitoring and social interaction | Sweden, Italy, Spain (2014) |
|
|
| Not mentioned | A telepresence robot with camera, lens, microphone and LCD screen to facilitate video communication with caregivers | Context recognition for event detection, trend analysis and alert generation | |
| [177] | Monitoring and interactive robotic system | Spain (2015) |
|
| Alarms are programmed for fall, intrusion and abnormal pattern detection | ||||
| [178] | Behavior and wellness prediction | New Zealand (2013) |
| Microwave, water kettle, toaster, room heater, TV | ZigBee | Software for data acquisition, activity recognition, behavior recognition and wellness determination are developed in C# | |||
| [179] | Easy-to-install and lightweight smart home kit | USA (2013) | Infrared motion/light sensor, relays, Door sensor and temperature sensor | ZigBee | Developed a activity visualizer software to display and keep record of the ADL | ||||
| [180] | In-home Health Monitoring System | Japan (2015) | IR motion sensor, water flow sensor for monitoring urination, kitchen work, and washing | RFID | Monitors and assesses occupant’s health status by monitoring urination, kitchen work, washing activities and movements in the house | Generates and e-mail report on the occupants’ health condition | |||
| [181] | Health monitoring using data fusion techniques | France (2011) |
| Temperature sensors | Wearable device: HR | ZigBee |
| ||
| Data fusion based on fuzzy logic: detect several distress situations | |||||||||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Majumder, S.; Aghayi, E.; Noferesti, M.; Memarzadeh-Tehran, H.; Mondal, T.; Pang, Z.; Deen, M.J. Smart Homes for Elderly Healthcare—Recent Advances and Research Challenges. Sensors 2017, 17, 2496. https://doi.org/10.3390/s17112496
Majumder S, Aghayi E, Noferesti M, Memarzadeh-Tehran H, Mondal T, Pang Z, Deen MJ. Smart Homes for Elderly Healthcare—Recent Advances and Research Challenges. Sensors. 2017; 17(11):2496. https://doi.org/10.3390/s17112496
Chicago/Turabian StyleMajumder, Sumit, Emad. Aghayi, Moein Noferesti, Hamidreza Memarzadeh-Tehran, Tapas Mondal, Zhibo Pang, and M. Jamal Deen. 2017. "Smart Homes for Elderly Healthcare—Recent Advances and Research Challenges" Sensors 17, no. 11: 2496. https://doi.org/10.3390/s17112496
APA StyleMajumder, S., Aghayi, E., Noferesti, M., Memarzadeh-Tehran, H., Mondal, T., Pang, Z., & Deen, M. J. (2017). Smart Homes for Elderly Healthcare—Recent Advances and Research Challenges. Sensors, 17(11), 2496. https://doi.org/10.3390/s17112496






