Wearable Multi-Frequency and Multi-Segment Bioelectrical Impedance Spectroscopy for Unobtrusively Tracking Body Fluid Shifts during Physical Activity in Real-Field Applications: A Preliminary Study
Abstract
:1. Introduction
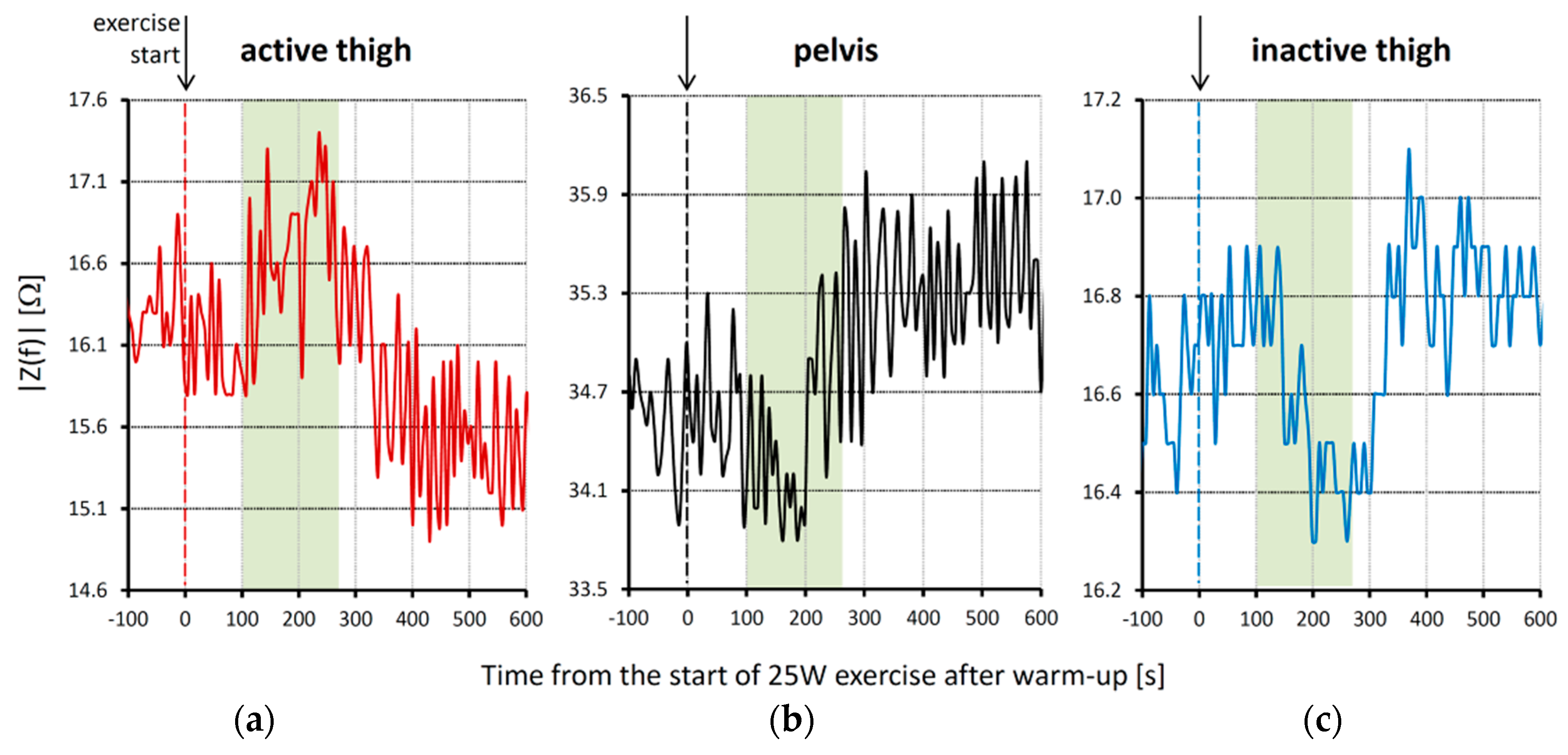
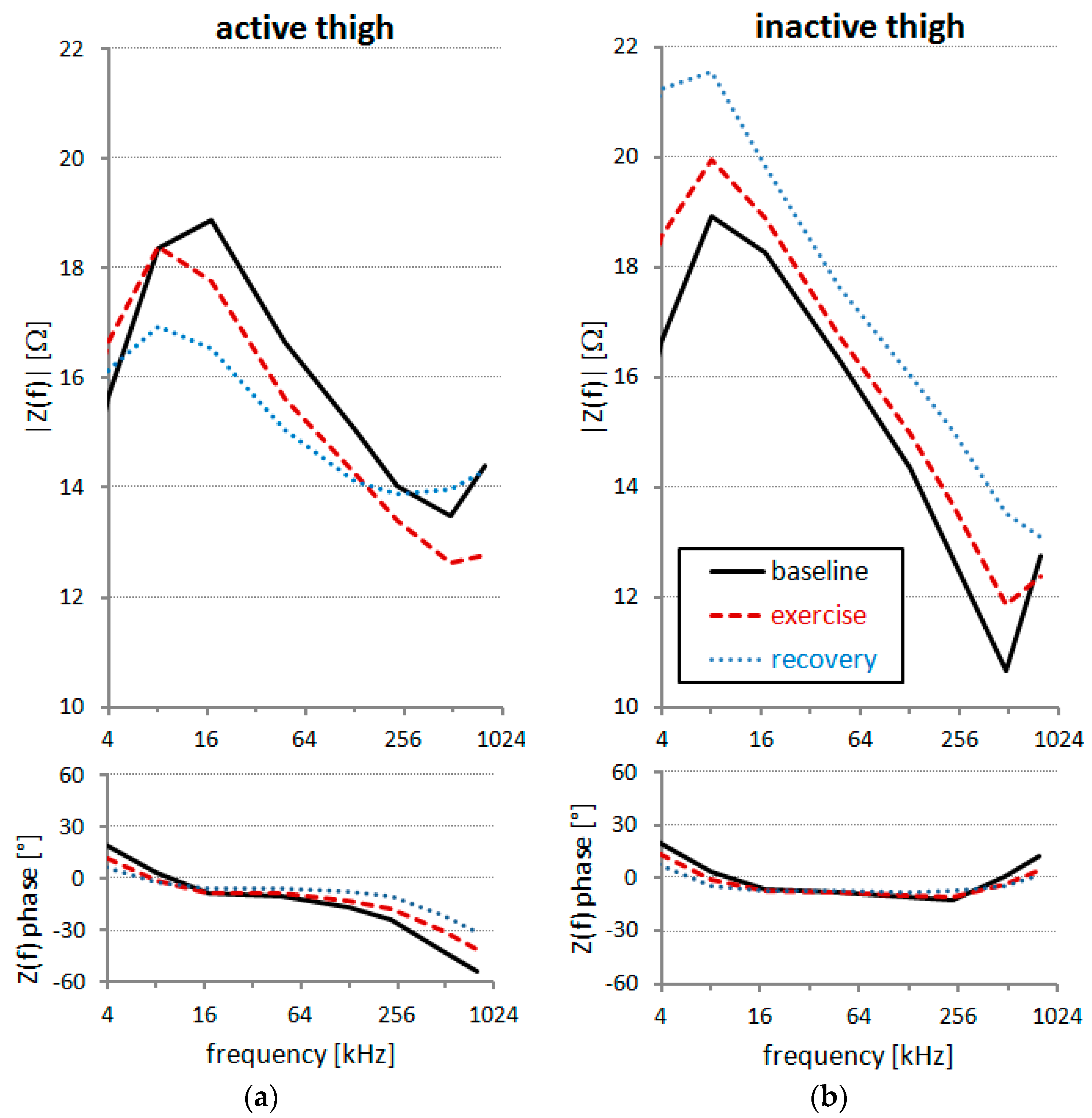
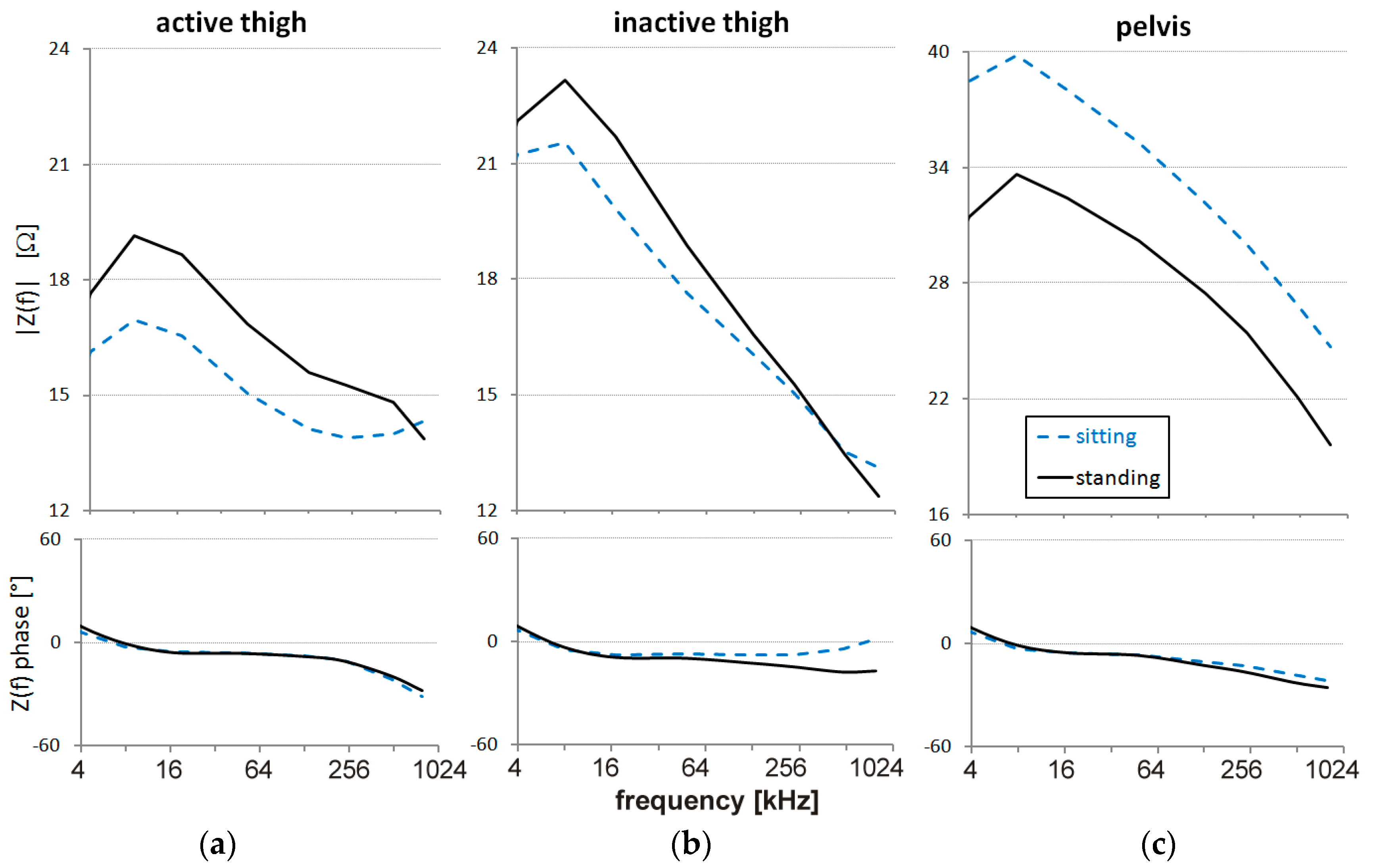
2. Materials and Methods
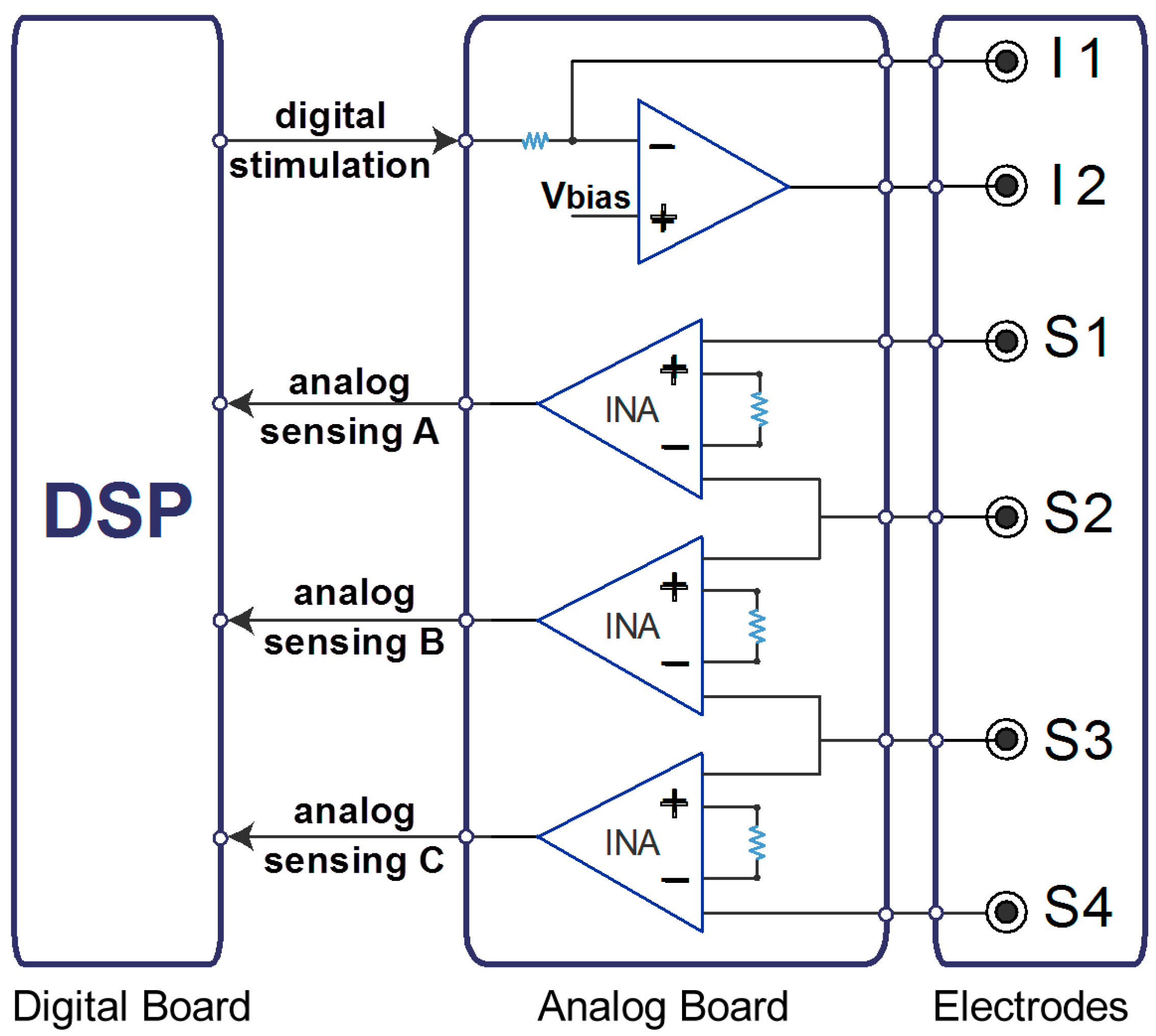
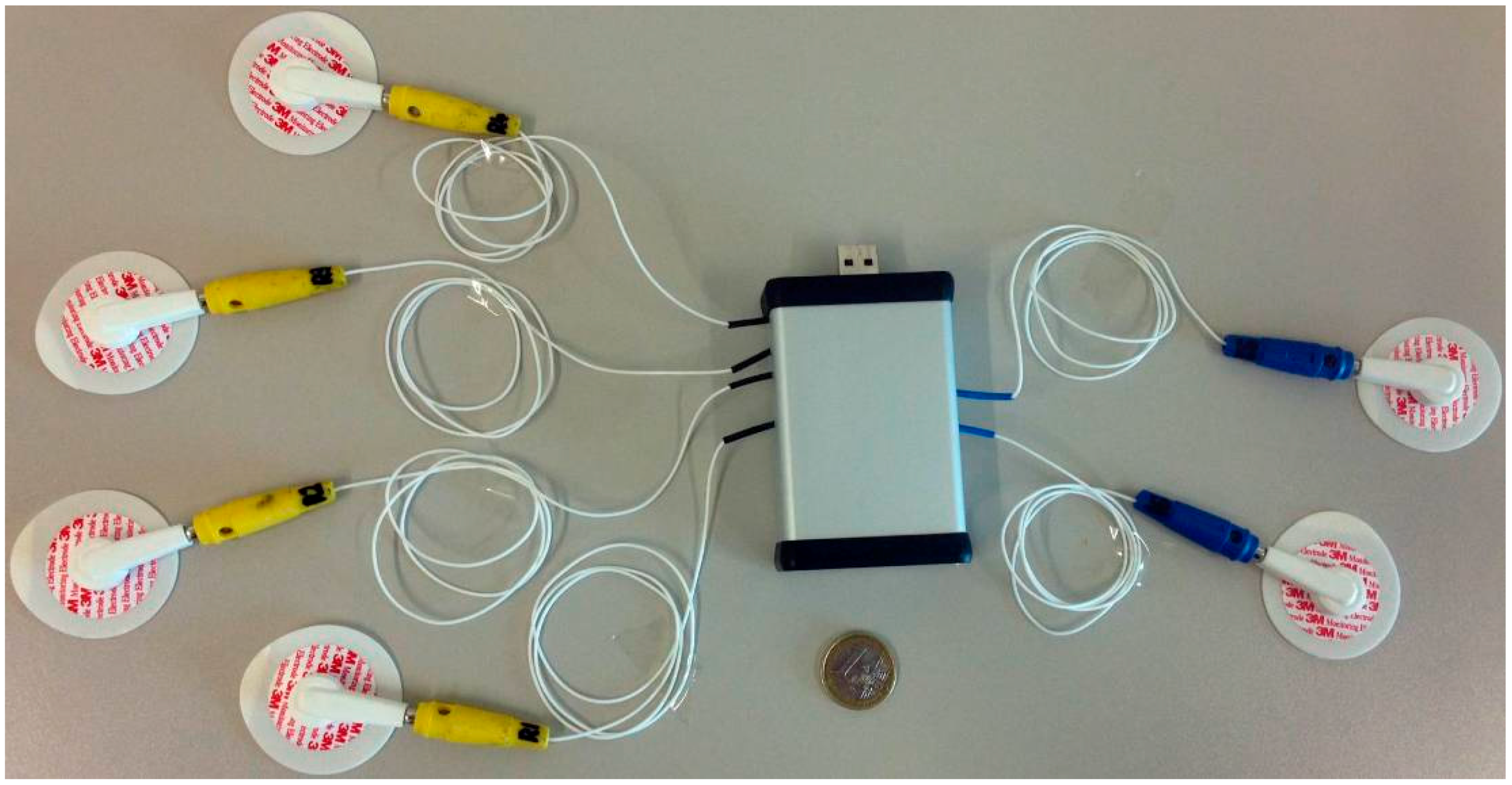
2.1. Description of the BIS Device
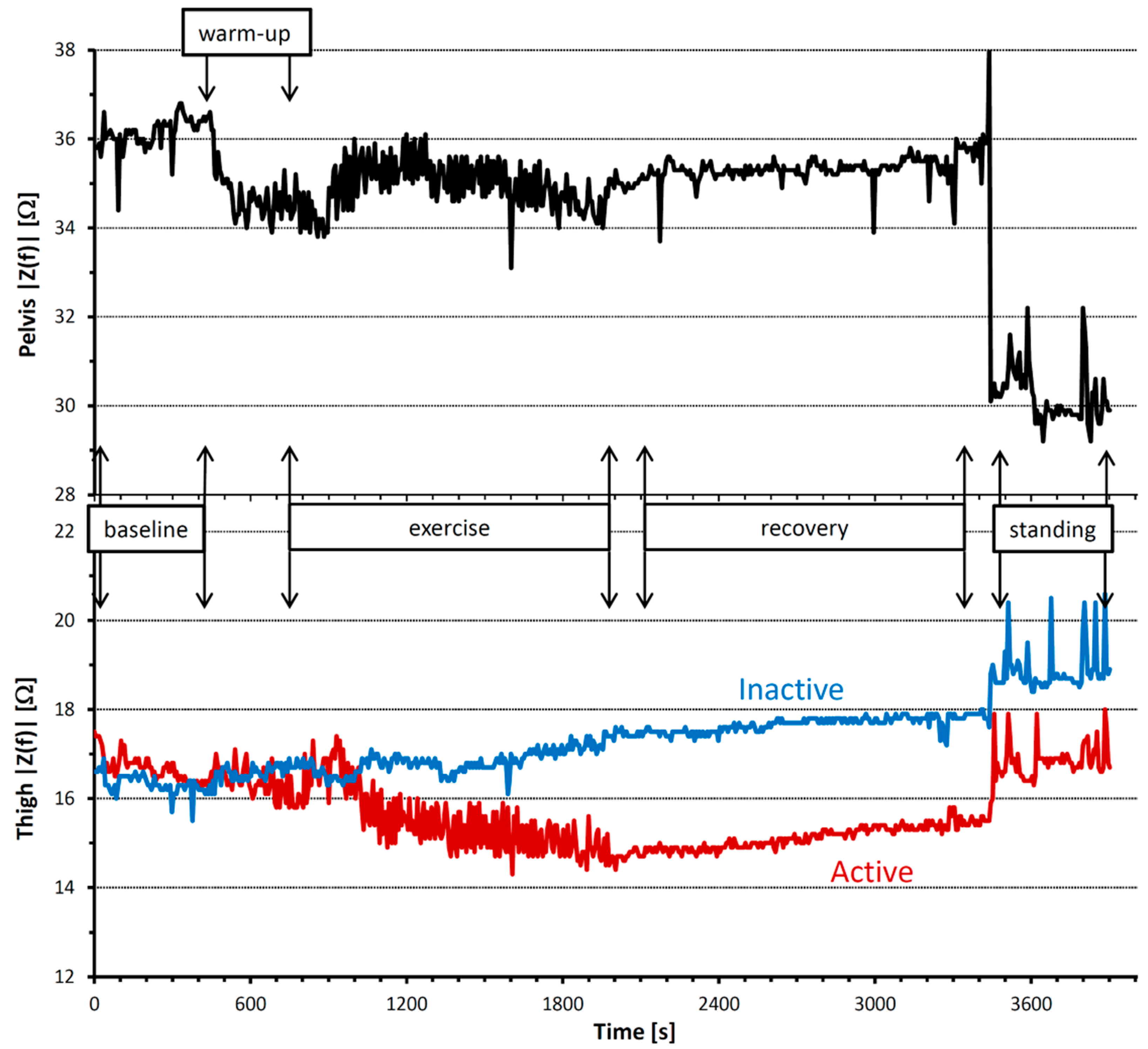
2.2. Experimental Application
3. Results and Discussion
4. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
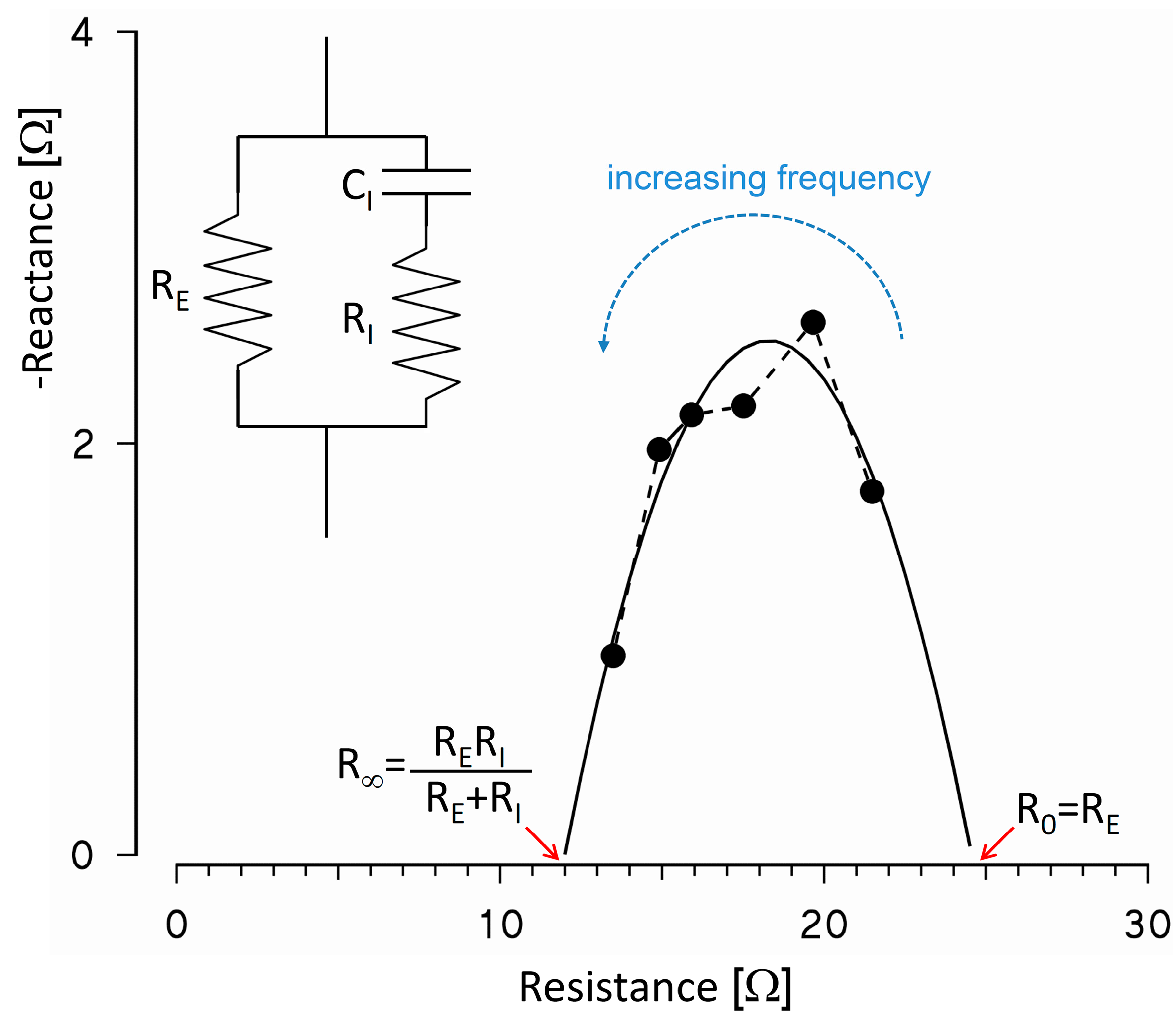
Appendix A: From BIS Measures to the Determination of Body Fluids Volumes
References
- Stahn, A.; Terblanche, E.; Gunga, H.C. Use of bioelectrical impedance: General principles and overview. In Handbook of Anthropometry: Physical Measures of Human Form in Health and Disease; Preedy, V.R., Ed.; Springer Science+Business Media: New York, NY, USA, 2012; pp. 49–90. [Google Scholar]
- Sverre, G.; Ørjan, G.M. Bioimpedance and Bioelectricity Basics, 2nd ed.; Elsevier Academic Press: Oxford, UK, 2008. [Google Scholar]
- Jaffrin, M.Y.; Morel, H. Body fluid volumes measurements by impedance: A review of bioimpedance spectroscopy (BIS) and bioimpedance analysis (BIA) methods. Med. Eng. Phys. 2008, 30, 1257–1269. [Google Scholar] [CrossRef] [PubMed]
- Stahn, A.; Terblanche, E.; Strobel, G. Monitoring exercised-induced fluid losses by segmental bioelectrical impedance analysis. In Kinanthropometry IX, Proceedings of the 9th International Conference of the International Society for the Advancement of Kinanthropometry; Marfell-Jones, M., Stewart, A., Olds, T., Eds.; Routledge: Abingdon, UK, 2008; pp. 65–95. [Google Scholar]
- Fenech, M.; Jaffrin, M.Y. Extracellular and intracellular volume variations during postural change measured by segmental and wrist-ankle bioimpedance spectroscopy. IEEE Trans. Biomed. Eng. 2004, 51, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Raaijmakers, E.; Faes, T.J.; Meijer, J.M.; Kunst, P.W.; Bakker, J.; Goovaerts, H.G.; Heethaar, R.M. Estimation of non-cardiogenic pulmonary oedema using dual-frequency electrical impedance. Med. Biol. Eng. Comput. 1998, 36, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Ward, L.C. Bioelectrical impedance analysis: Proven utility in lymphedema risk assessment and therapeutic monitoring. Lymphat. Res. Biol. 2006, 4, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Organ, L.W.; Bradham, G.B.; Gore, D.T.; Lozier, S.L. Segmental bioelectrical impedance analysis: Theory and application of a new technique. J. Appl. Physiol. 1994, 77, 98–112. [Google Scholar] [PubMed]
- Stahn, A.; Terblanche, E.; Strobel, G. Modeling upper and lower limb muscle volume by bioelectrical impedance analysis. J. Appl. Physiol. 2007, 103, 1428–1435. [Google Scholar] [CrossRef] [PubMed]
- Elleby, B.; Knudsen, L.F.; Brown, B.H.; Crofts, C.E.; Woods, M.J.; Trowbridge, E.A. Electrical impedance assessment of muscle changes following exercise. Clin. Phys. Physiol. Meas. 1990, 11, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Rutkove, S.B. Electrical impedance myography: Background, current state, and future directions. Muscle Nerve 2009, 40, 936–946. [Google Scholar] [CrossRef] [PubMed]
- Stahn, A.; Terblanche, E.; Grunert, S.; Strobel, G. Estimation of maximal oxygen uptake by bioelectrical impedance analysis. Eur. J. Appl. Physiol. 2006, 96, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Stahn, A.; Strobel, G.; Terblanche, E. VO(2max) prediction from multi-frequency bioelectrical impedance analysis. Physiol. Meas. 2008, 29, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Medrano, G.; Beckmann, L.; Zimmermann, N.; Grundmann, T.; Gries, T.; Leonhardt, S. Bioimpedance Spectroscopy with Textile Electrodes for a Continuous Monitoring Application. In 4th International Workshop on Wearable and Implantable Body Sensor Networks (BSN 2007), 13th ed.; Leonhardt, S., Falck, T., Mahonen, P., Eds.; Springer: Berlin, Germany, 2007; pp. 23–28. [Google Scholar]
- Seoane, F.; Ferreira, J.; Sanchez, J.J.; Bragos, R. An analog front-end enables electrical impedance spectroscopy system on-chip for biomedical applications. Physiol. Meas. 2008, 29, S267–S278. [Google Scholar] [CrossRef] [PubMed]
- Villa, F.; Magnani, A.; Merati, G.; Castiglioni, P. Feasibility of long-term monitoring of multifrequency and multisegment body impedance by portable devices. IEEE Trans. Biomed. Eng. 2014, 61, 1877–1886. [Google Scholar] [CrossRef] [PubMed]
- Villa, F.; Magnani, A.; Castiglioni, P. Portable Body Impedance System for Long-Term Monitoring of Body Hydration. In Proceedings of the 2012 8th Conference on Ph.D. Research in Microelectronics and Electronics (PRIME), Aachen, Germany, 12–15 June 2012; pp. 229–232.
- Gabriel, C.; Gabriel, S.; Corthout, E. The dielectric properties of biological tissues: I. Literature survey. Phys. Med. Biol. 1996, 41, 2231–2249. [Google Scholar] [CrossRef] [PubMed]
- Schwan, H.P.; Kay, C.F. The conductivity of living tissues. Ann. N. Y. Acad. Sci. 1957, 65, 1007–1013. [Google Scholar] [CrossRef] [PubMed]
- Grimnes, S.; Martinsen, Ø.G. Alpha-dispersion in human tissue. J. Phys. Conf. Ser. 2010, 224, 012073. [Google Scholar] [CrossRef]
- De Lorenzo, A.; Andreoli, A.; Matthie, J.; Withers, P. Predicting body cell mass with bioimpedance by using theoretical methods: A technological review. J. Appl. Physiol. 1997, 82, 1542–1558. [Google Scholar] [PubMed]
- Andersen, P.; Saltin, B. Maximal perfusion of skeletal muscle in man. J. Physiol. 1985, 366, 233–249. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Yamamoto, Y.; Yamamoto, T.; Tsuji, H. Fundamental characteristics of human limb electrical impedance for biodynamic analysis. Med. Biol. Eng. Comput. 1992, 30, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Boushel, R. Muscle metaboreflex control of the circulation during exercise. Acta Physiol. (Oxf.) 2010, 199, 367–383. [Google Scholar] [CrossRef] [PubMed]
- Yoshizawa, M.; Shimizu-Okuyama, S.; Kagaya, A. Transient increase in femoral arterial blood flow to the contralateral non-exercising limb during one-legged exercise. Eur. J. Appl. Physiol. 2008, 103, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Caton, J.R.; Mole, P.A.; Adams, W.C.; Heustis, D.S. Body composition analysis by bioelectrical impedance: Effect of skin temperature. Med. Sci. Sports Exerc. 1988, 20, 489–491. [Google Scholar] [CrossRef] [PubMed]
- Gudivaka, R.; Schoeller, D.; Kushner, R.F. Effect of skin temperature on multifrequency bioelectrical impedance analysis. J. Appl. Physiol. 1996, 81, 838–845. [Google Scholar] [PubMed]
- Cornish, B.H.; Thomas, B.J.; Ward, L.C. Effect of temperature and sweating on bioimpedance measurements. Appl. Radiat. Isot. 1998, 49, 475–476. [Google Scholar] [CrossRef]
- Liang, M.T.; Norris, S. Effects of skin blood flow and temperature on bioelectric impedance after exercise. Med. Sci. Sports Exerc. 1993, 25, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Buono, M.J.; Burke, S.; Endemann, S.; Graham, H.; Gressard, C.; Griswold, L.; Michalewicz, B. The effect of ambient air temperature on whole-body bioelectrical impedance. Physiol. Meas. 2004, 25, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Kanai, H.; Haeno, M.; Sakamoto, K. Electrical measurement of fluid distribution in legs and arms. In Medical Progress through Technology; Martinus Nijhoff Publishers: Boston, MA, USA, 1987; pp. 159–170. [Google Scholar]
- Van Loan, M.D.; Withers, P.O.; Matthie, J.R.; Mayclin, P.L. Use of Bioimpedance Spectroscopy to Determine Extracellular Fluid, Intracellular Fluid, Total Body Water, and Fat-Free Mass. In Human Body Composition: In Vivo Methods, Models and Assessment; Ellis, K.J., Eastman, J.D., Eds.; Plenum: New York, NY, USA, 1993; pp. 67–70. [Google Scholar]
- Ellis, K.J.; Wong, W.W. Human hydrometry: Comparison of multifrequency bioelectrical impedance with 2H2O and bromine dilution. J. Appl. Physiol. 1998, 85, 1056–1062. [Google Scholar] [PubMed]
- Zhu, F.; Leonard, E.F.; Levin, N.W. Body composition modeling in the calf using an equivalent circuit model of multi-frequency bioimpedance analysis. Physiol. Meas. 2005, 26, S133–S143. [Google Scholar] [CrossRef] [PubMed]
- Van Kreel, B.K.; Cox-Reyven, N.; Soeters, P. Determination of total body water by multifrequency bio-electric impedance: Development of several models. Med. Biol. Eng. Comput. 1998, 36, 337–345. [Google Scholar] [CrossRef] [PubMed]


| Time | Condition | Thigh Temperature (°C) | |
|---|---|---|---|
| Active | Inactive | ||
| 400 s | Baseline | 32.5 | 32.5 |
| 750 s | warm-up (10W) | 32.5 | 31.5 |
| 1250 s | exercise (25W) | 31.0 | 29.0 |
| 1500 s | exercise (25W) | 32.0 | 29.0 |
| 1800 s | exercise (25W) | 32.5 | 29.5 |
| 1950 s | exercise (50W) | 33.0 | 30.5 |
| 2550 s | Recovery | 33.0 | 31.0 |
| 3900 s | Standing | 33.0 | 30.5 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Villa, F.; Magnani, A.; Maggioni, M.A.; Stahn, A.; Rampichini, S.; Merati, G.; Castiglioni, P. Wearable Multi-Frequency and Multi-Segment Bioelectrical Impedance Spectroscopy for Unobtrusively Tracking Body Fluid Shifts during Physical Activity in Real-Field Applications: A Preliminary Study. Sensors 2016, 16, 673. https://doi.org/10.3390/s16050673
Villa F, Magnani A, Maggioni MA, Stahn A, Rampichini S, Merati G, Castiglioni P. Wearable Multi-Frequency and Multi-Segment Bioelectrical Impedance Spectroscopy for Unobtrusively Tracking Body Fluid Shifts during Physical Activity in Real-Field Applications: A Preliminary Study. Sensors. 2016; 16(5):673. https://doi.org/10.3390/s16050673
Chicago/Turabian StyleVilla, Federica, Alessandro Magnani, Martina A. Maggioni, Alexander Stahn, Susanna Rampichini, Giampiero Merati, and Paolo Castiglioni. 2016. "Wearable Multi-Frequency and Multi-Segment Bioelectrical Impedance Spectroscopy for Unobtrusively Tracking Body Fluid Shifts during Physical Activity in Real-Field Applications: A Preliminary Study" Sensors 16, no. 5: 673. https://doi.org/10.3390/s16050673
APA StyleVilla, F., Magnani, A., Maggioni, M. A., Stahn, A., Rampichini, S., Merati, G., & Castiglioni, P. (2016). Wearable Multi-Frequency and Multi-Segment Bioelectrical Impedance Spectroscopy for Unobtrusively Tracking Body Fluid Shifts during Physical Activity in Real-Field Applications: A Preliminary Study. Sensors, 16(5), 673. https://doi.org/10.3390/s16050673