Plantar Pressure Detection with Fiber Bragg Gratings Sensing System
Abstract
:1. Introduction
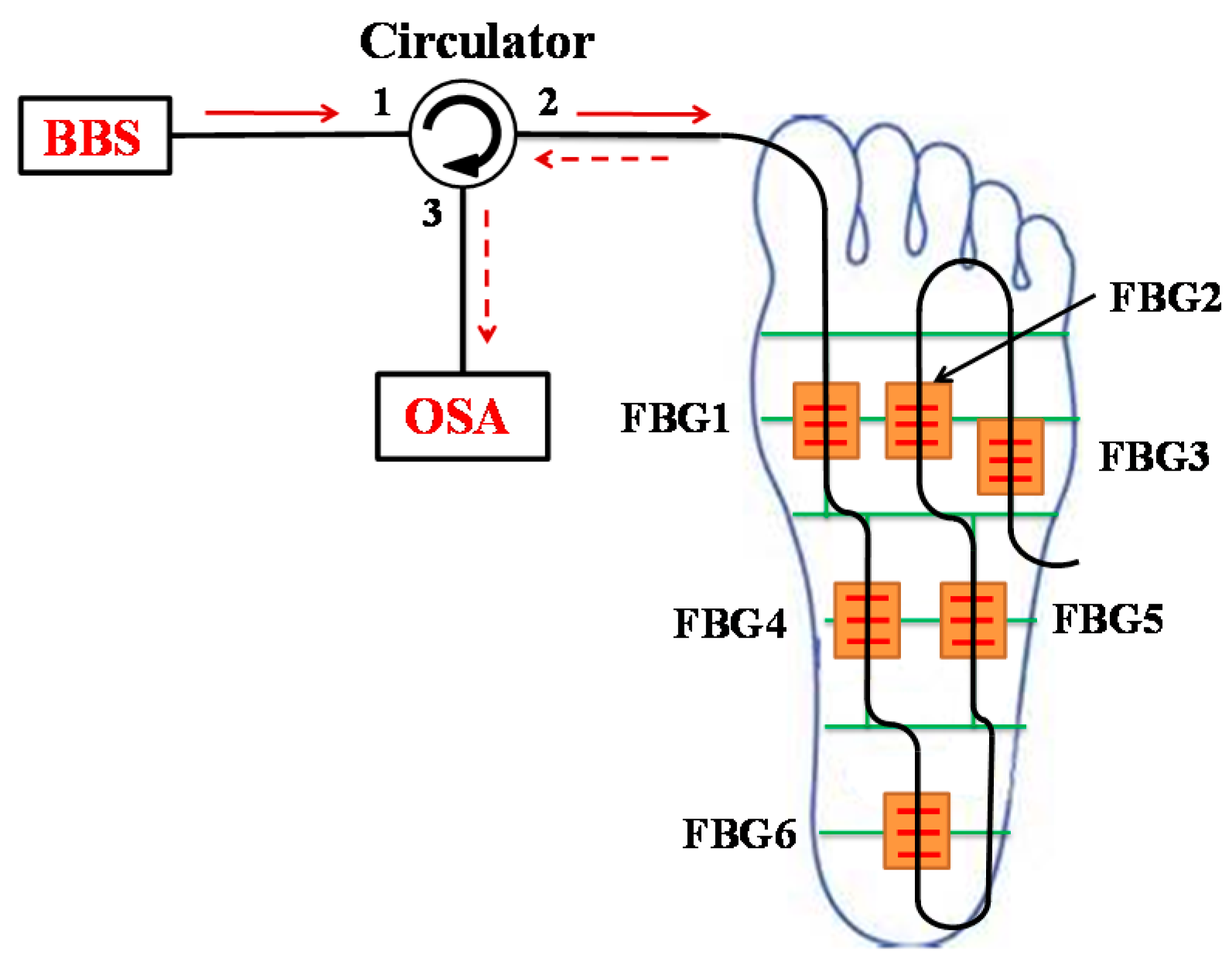
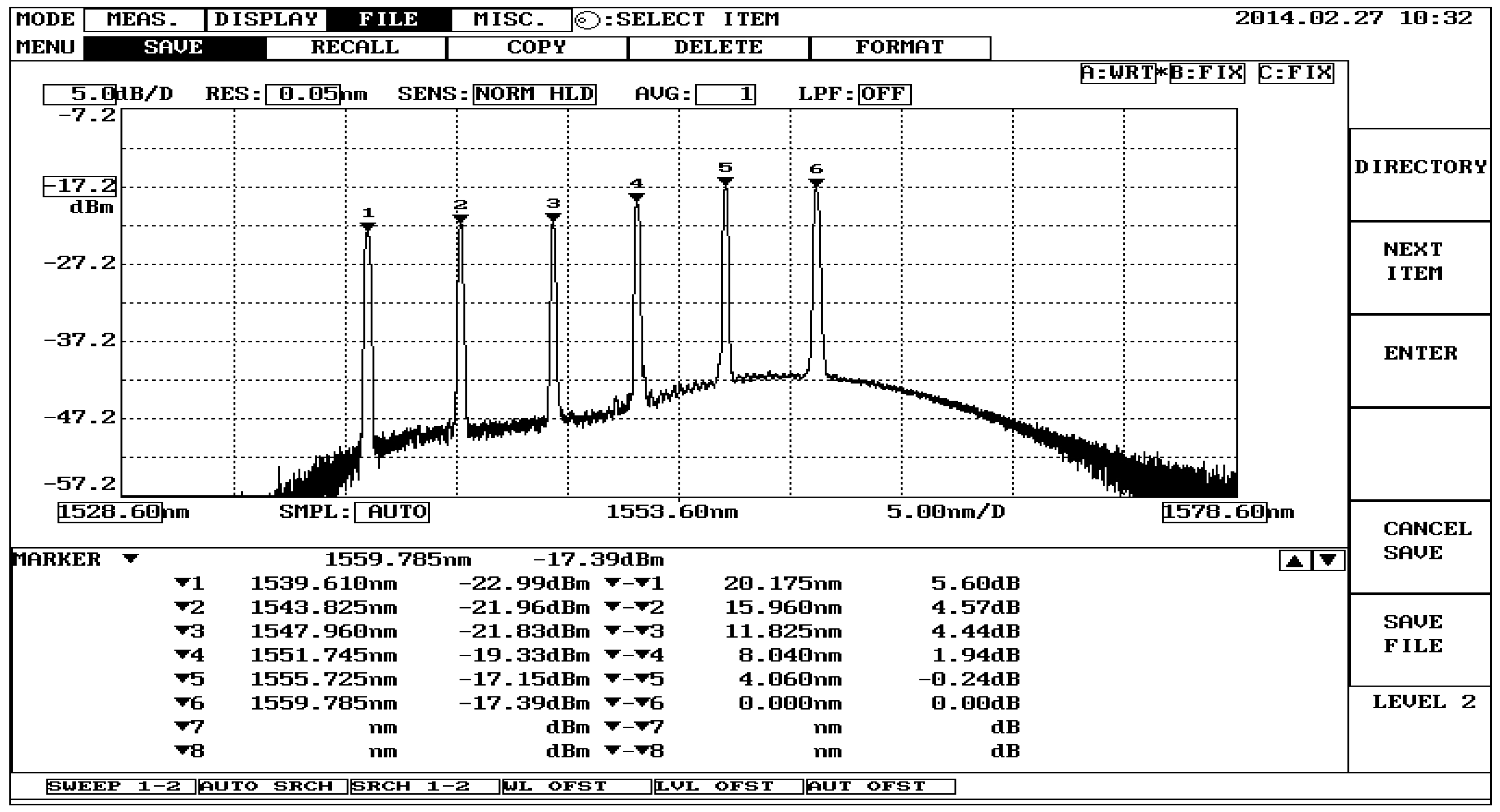
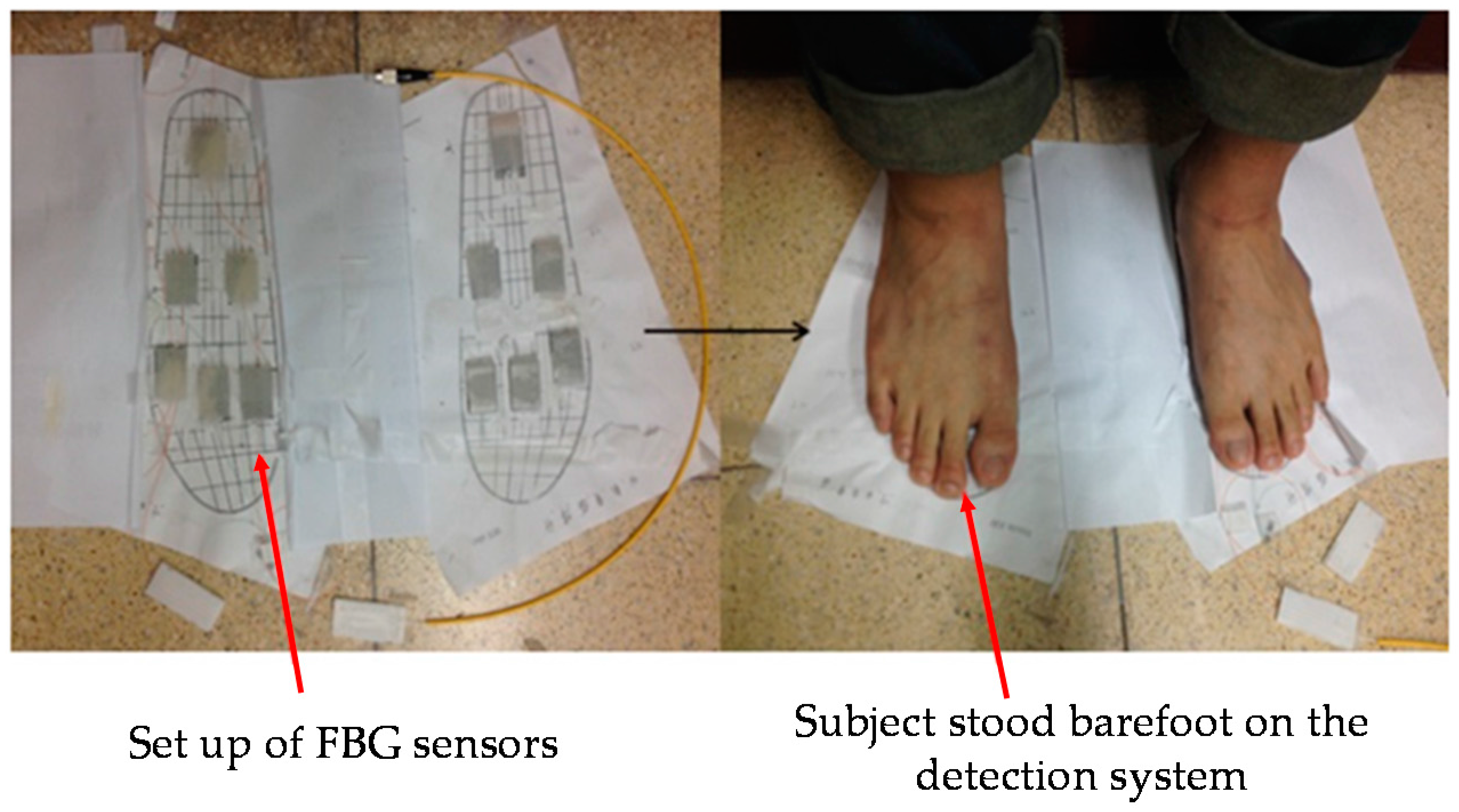
2. General Description and Fiber-Optic Sensor Configuration
3. Methods and Results
3.1. Subjects
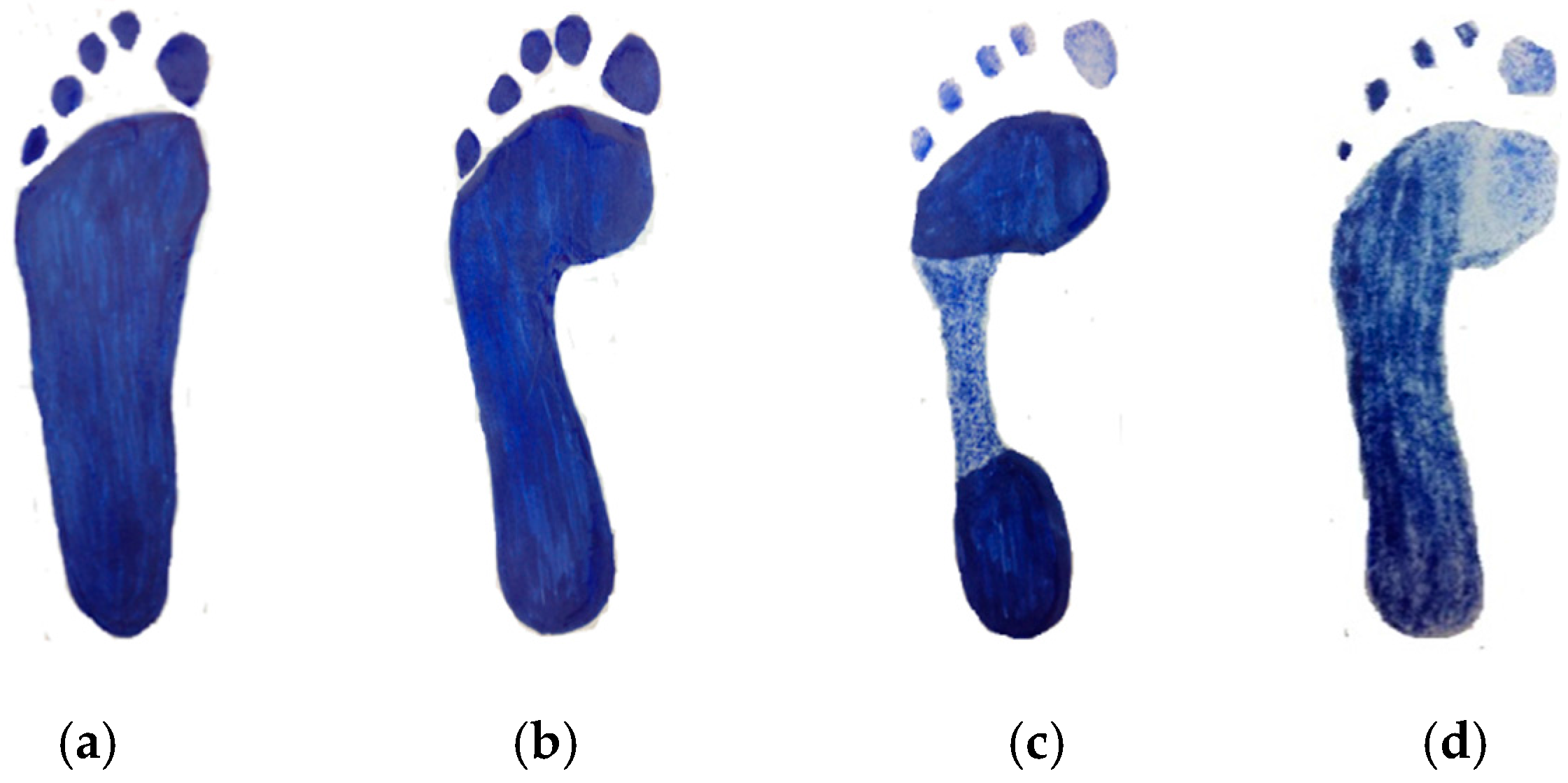
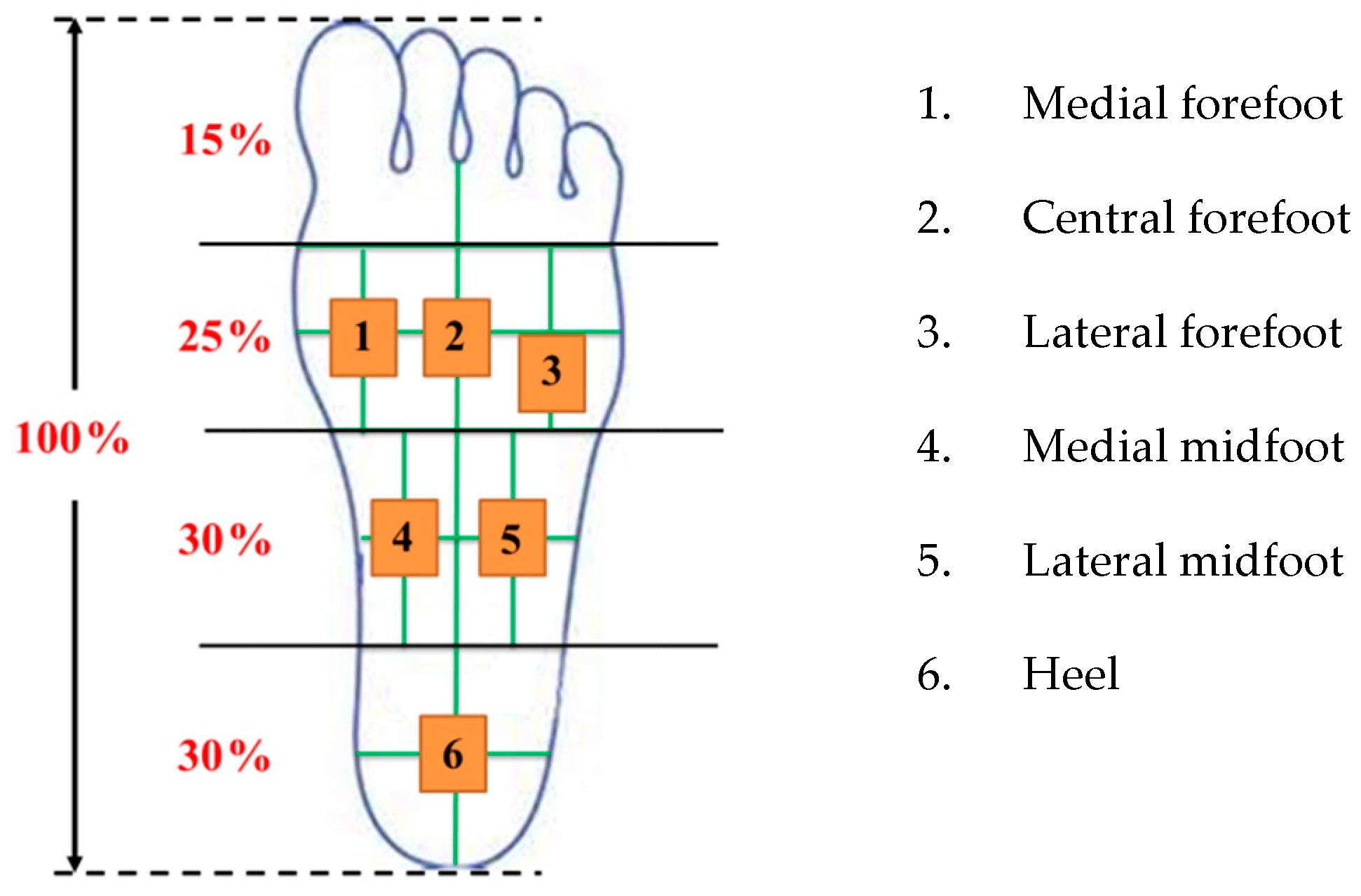
3.2. Plantar Foot Sensing Area Definition
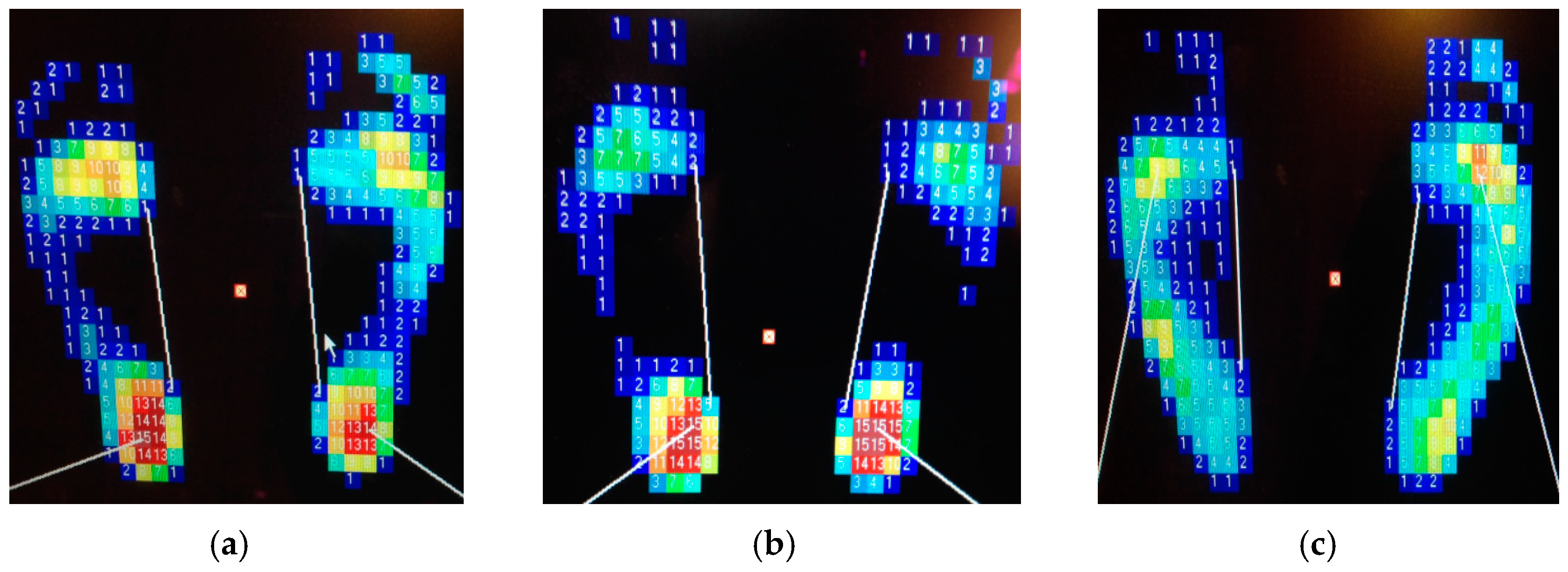
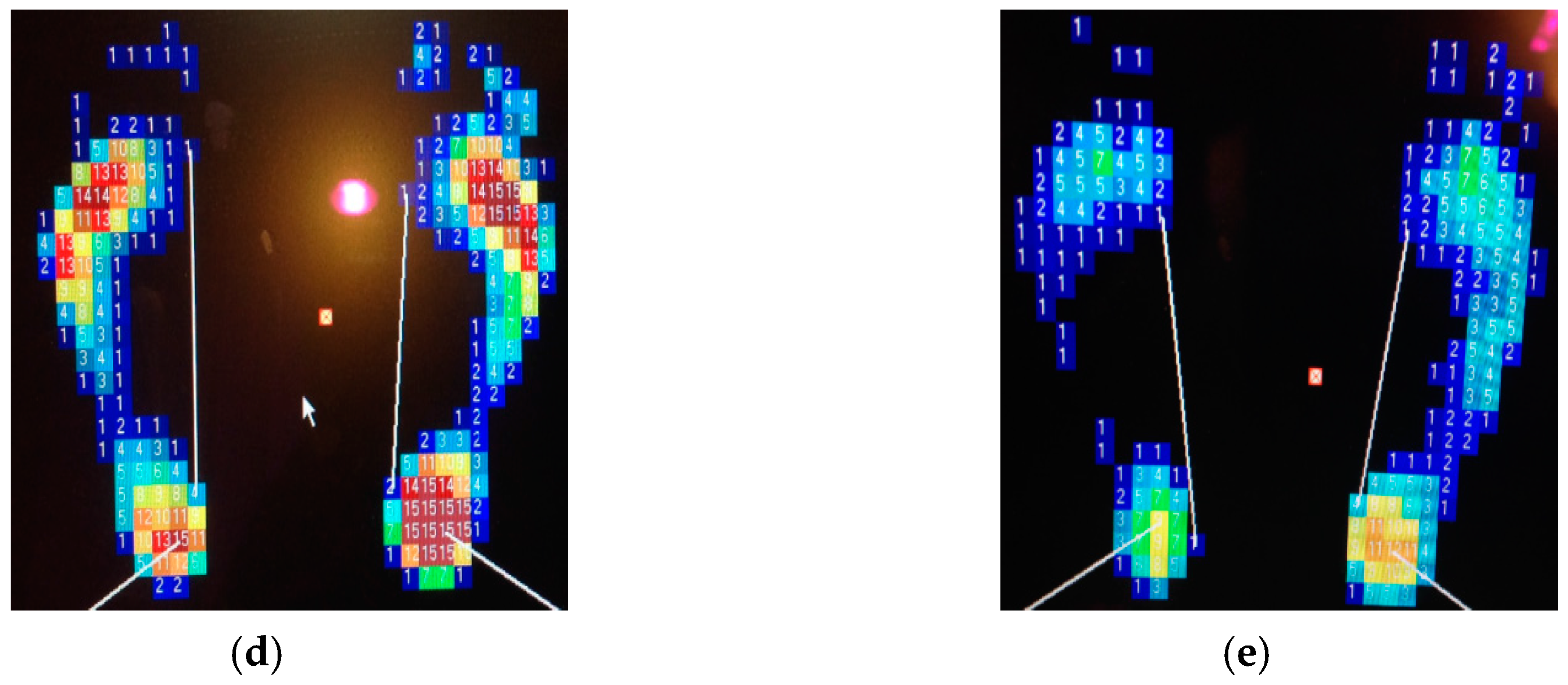
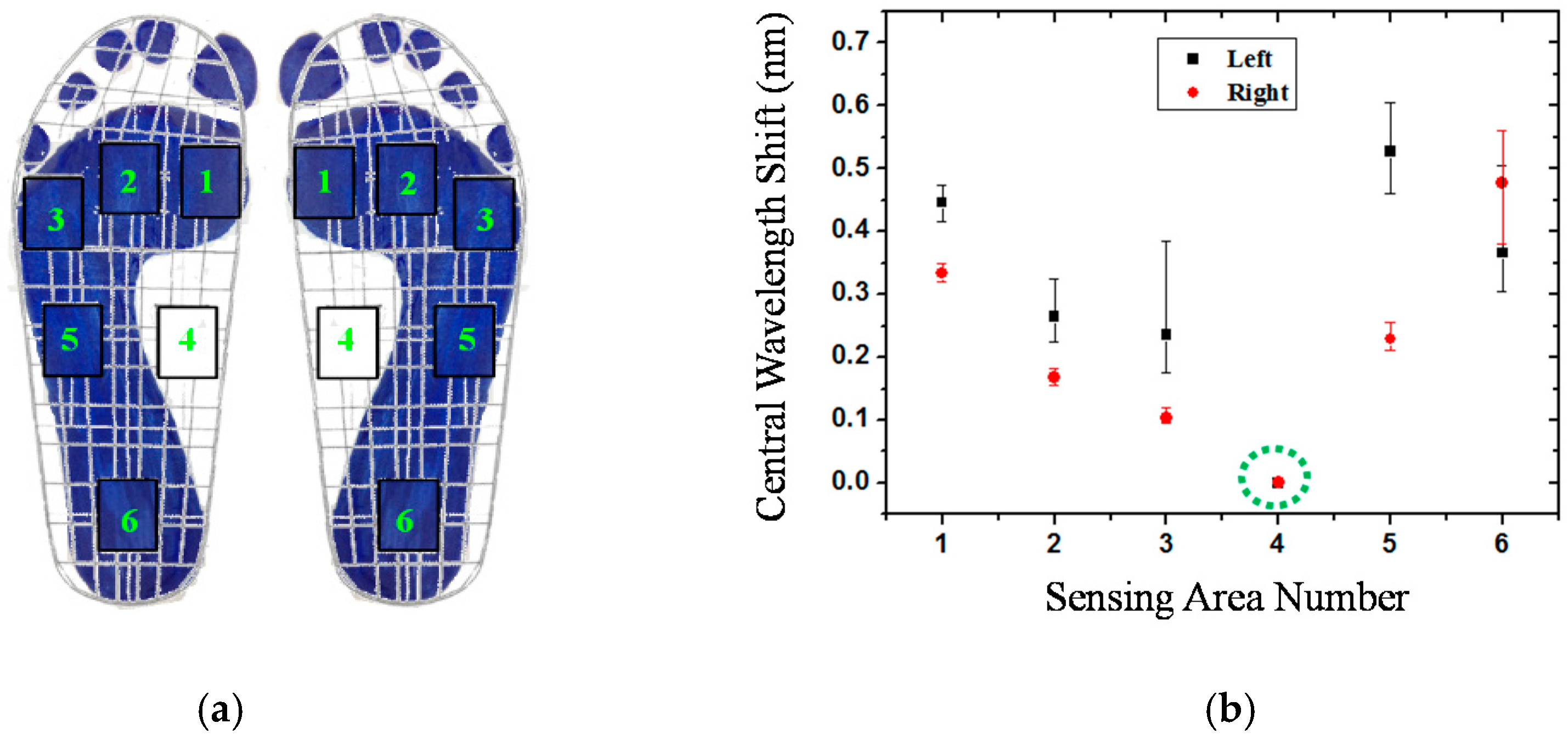
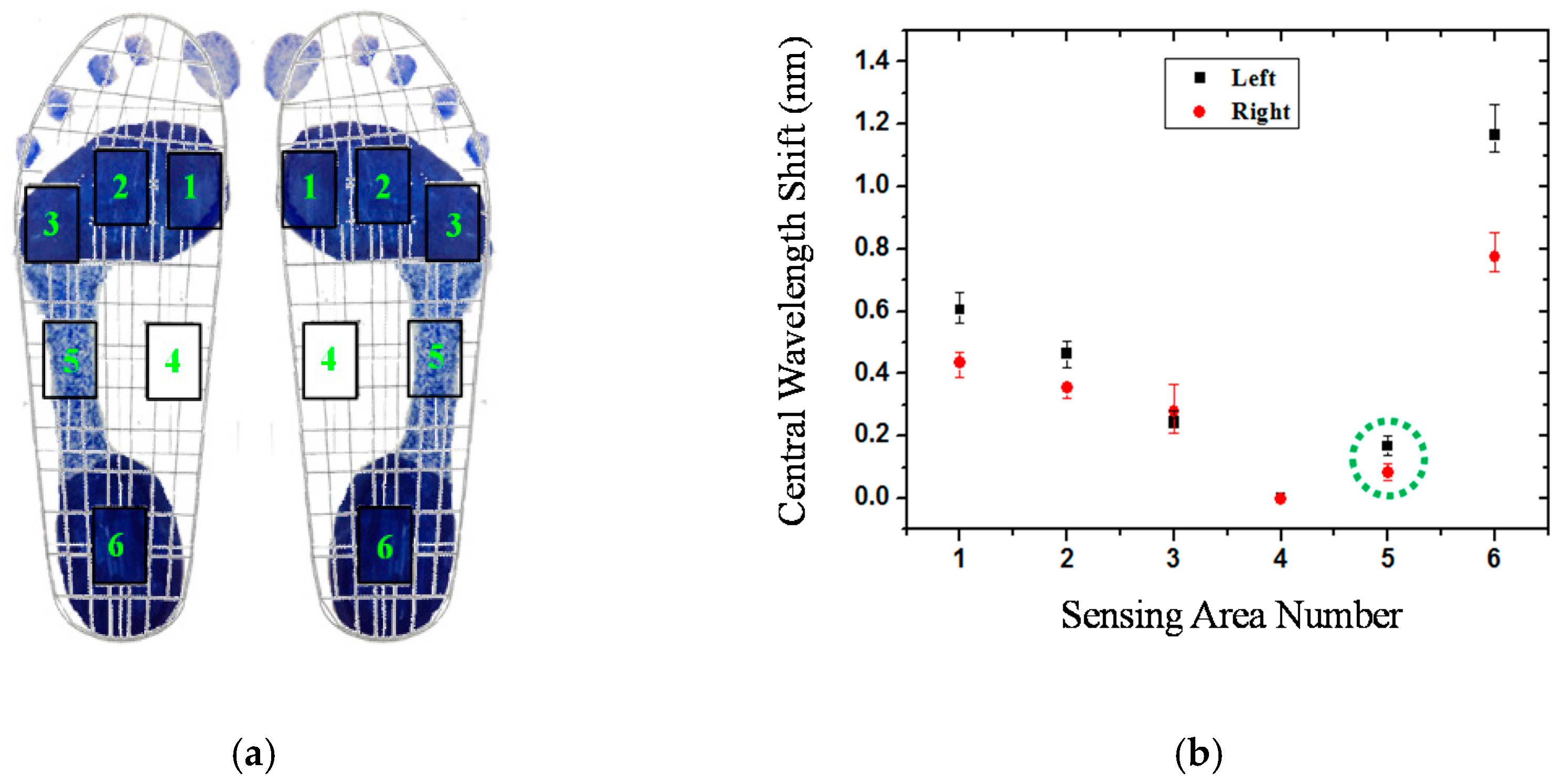
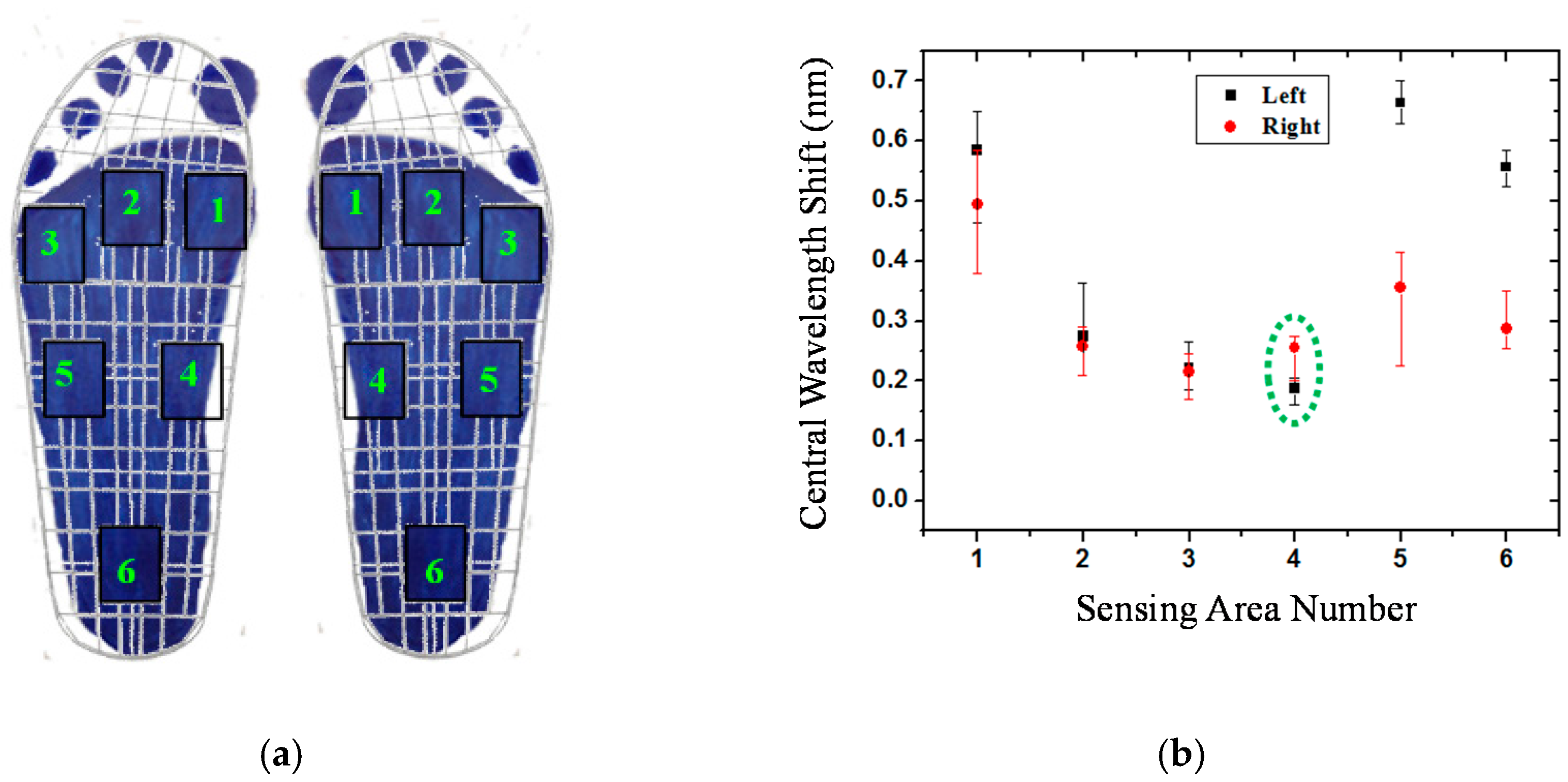
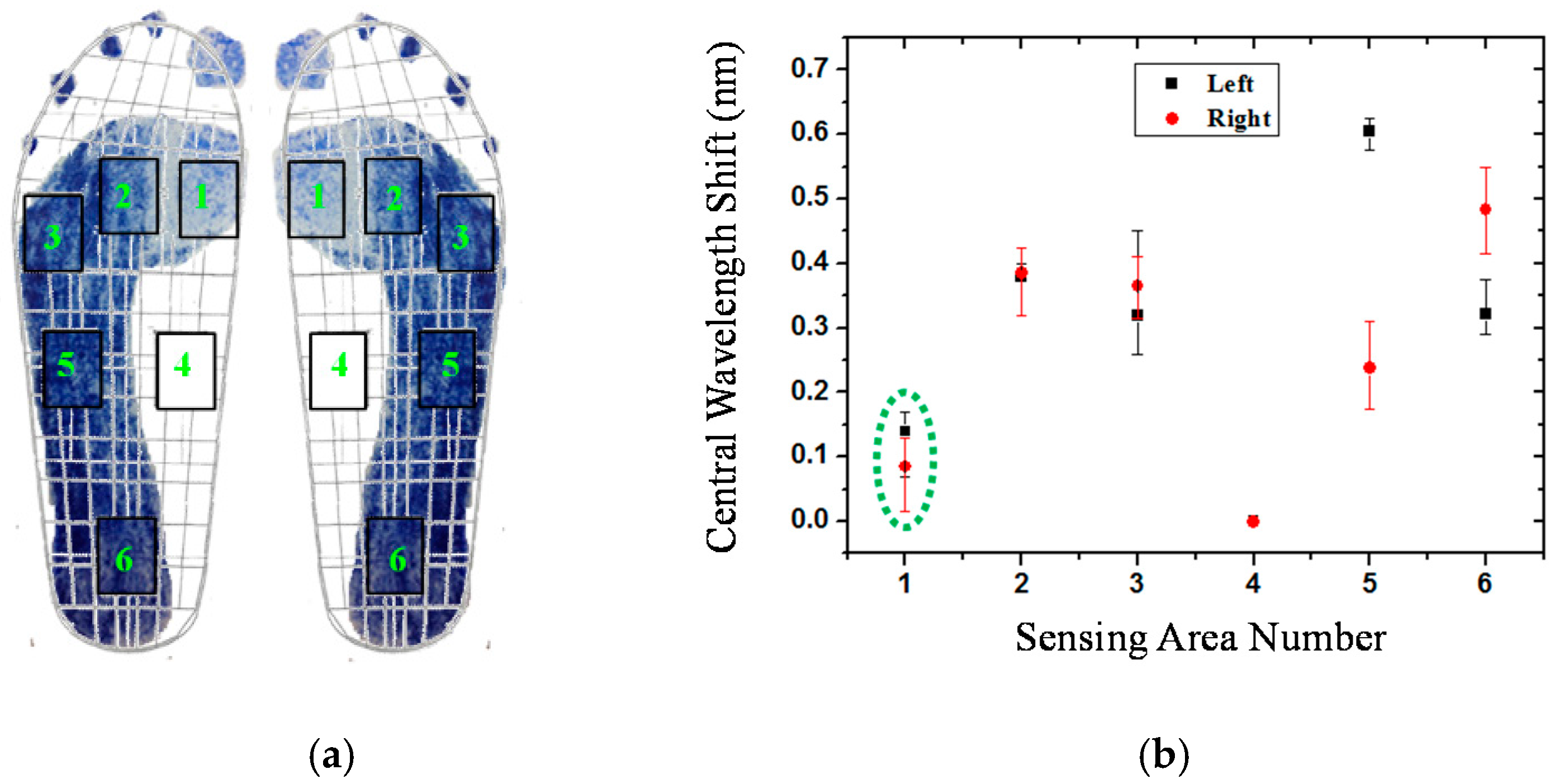
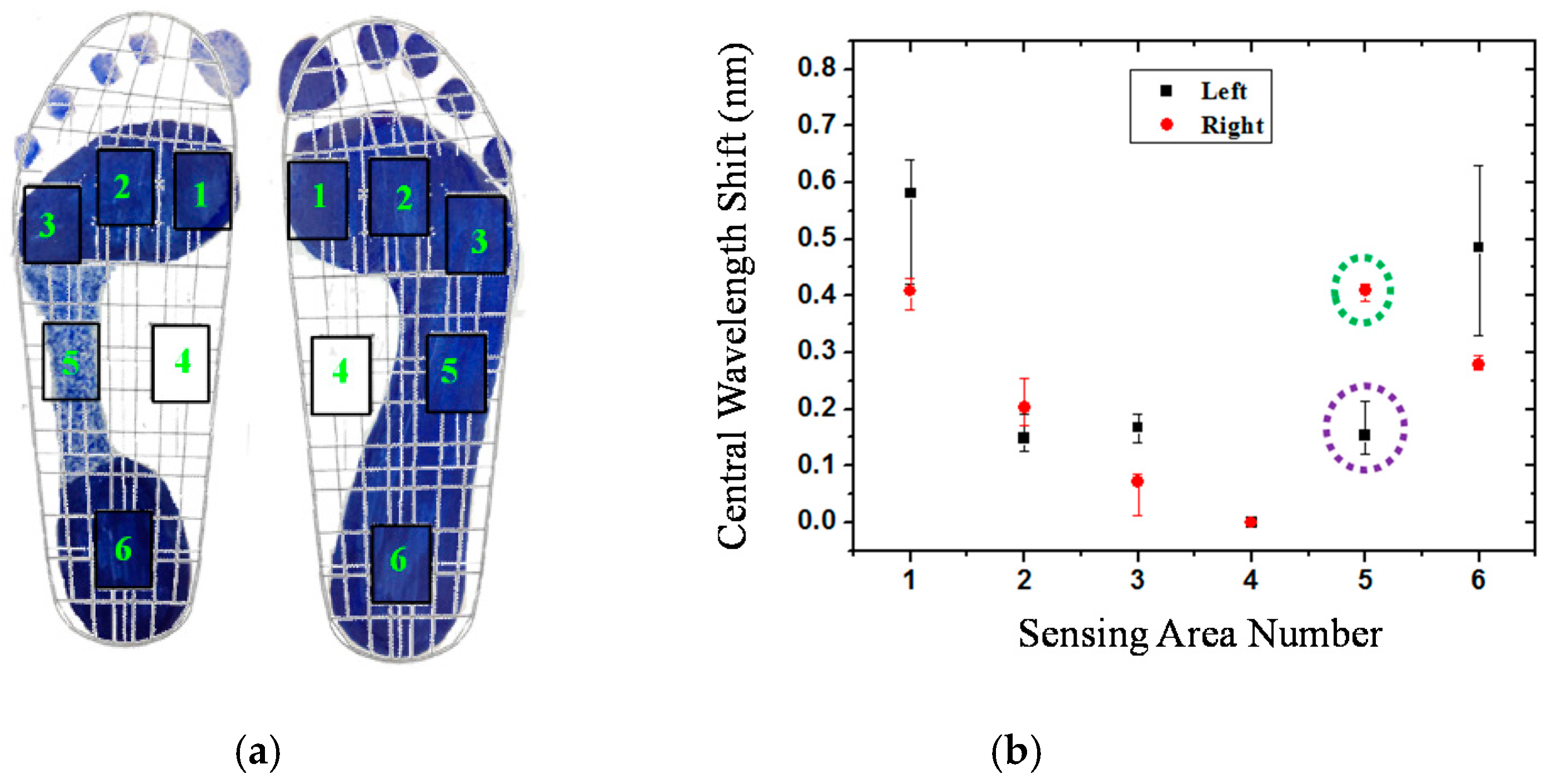
3.3. Experimental Results
3.4. Sensing Stability
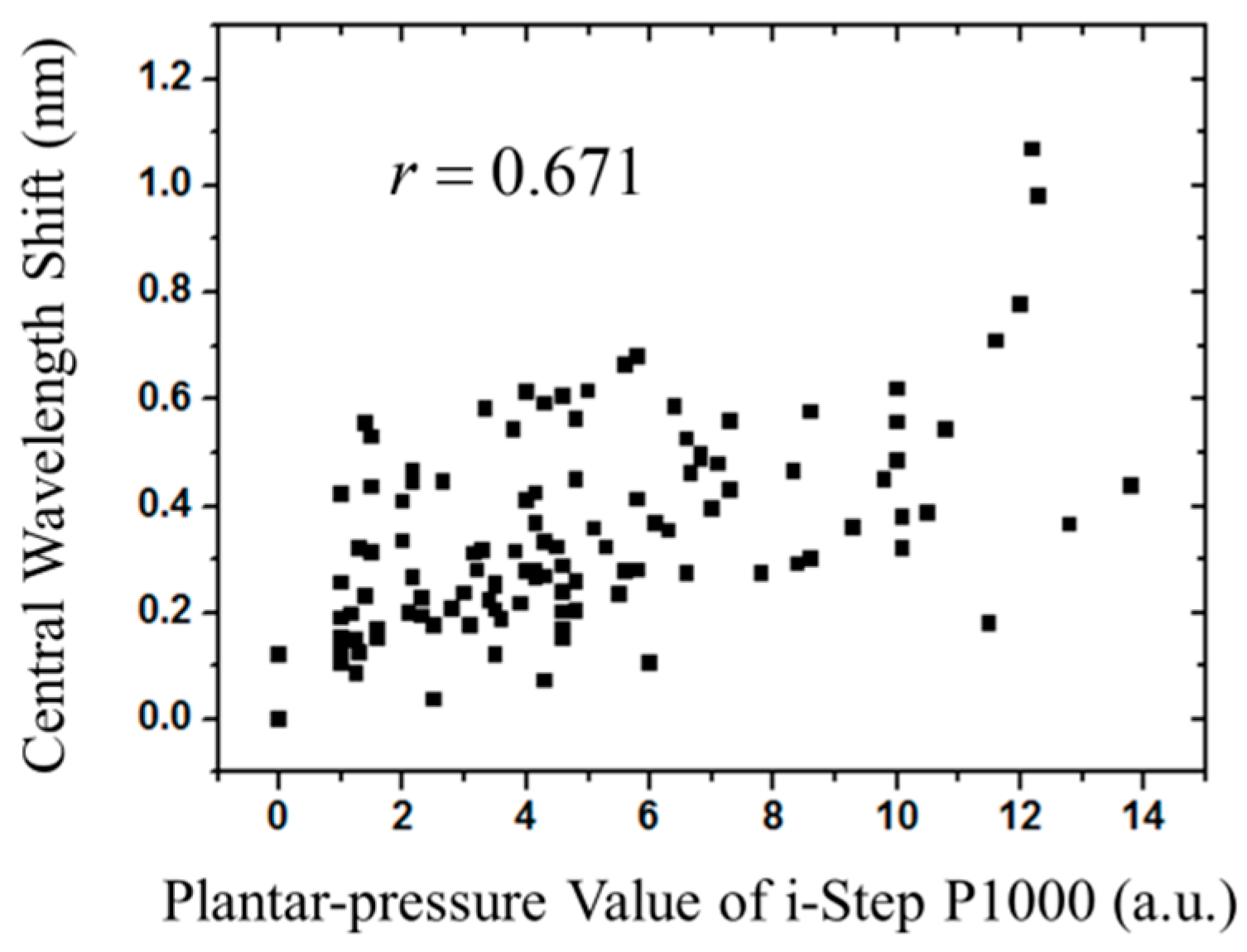
3.5. Statistical Verification
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Razeghi, M.; Batt, M.E. Foot type classification: A critical review of current methods. Gait Posture 2002, 15, 282–291. [Google Scholar] [CrossRef]
- Kisner, C.; Colby, L.A. The Ankle and Foot. In Therapeutic Exercise: Foundations and Techniques, 4th ed.; A. Davis Company: Philadelphia, PA, USA, 2002; p. 566. [Google Scholar]
- Grech, C.; Formosa, C.; Gatt, A. Shock attenuation properties at heel strike: Implications for the clinical management of the cavus foot. J. Orthop. 2016, 13, 148–151. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.; Weil, R.; Boer, E.D. Standardizing foot-type classification using arch index values. Physiother. Can. 2012, 64, 280–283. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, M.K.; Friis, R.; Michaelsen, M.S.; Jakobsen, P.A.; Nielsen, R.O. Classification of the height and flexibility of the medial longitudinal arch of the foot. J. Foot Ankle Res. 2012, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Franco, A.H. Pes cavus and pes planus analyses and treatment. Phys. Ther. 1987, 67, 688–694. [Google Scholar] [PubMed]
- Periyasamy, R.; Anand, S. The effect of foot arch on plantar pressure distribution during standing. J. Med. Eng. Technol. 2013, 37, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Tang, U.H.; Zügner, R.; Lisovskaja, V.; Karlsson, J.; Hagberg, K.; Tranberg, R. Comparison of plantar pressure in three types of insole given to patients with diabetes at risk of developing foot ulcers—A two-year, randomized trial. J. Clin. Trans. Endocrinol. 2014, 1, 121–132. [Google Scholar]
- Fernando, M.E.; Crowther, R.G.; Pappas, E.; Lazzarini, P.A.; Cunningham, M.; Sangla, K.S.; Buttner, P.; Golledge, J. Plantar pressure in diabetic peripheral neuropathy patients with active foot ulceration, previous ulceration and no history of ulceration: A meta-analysis of observational studies. PLoS ONE 2014, 9, e99050. [Google Scholar] [CrossRef] [PubMed]
- Bacarin, T.A.; Sacco, I.C.N.; Hennig, E.M. Plantar pressure distribution patterns during gait in diabetic neuropathy patients with a history of foot ulcers. Clinics 2009, 64, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.A.; Aziz, Z.; Acharya, U.R.; Ha, T.P.; Kannathal, N.; Ng, E.Y.K.; Law, C.; Subramaniam, T.; Shuen, W.Y.; Fang, S.C. Analysis of plantar pressure in diabetic type 2 subjects with and without neuropathy. ITBM-RBM 2006, 27, 46–55. [Google Scholar] [CrossRef]
- Telfer, S.; Erdemir, A.; Woodburn, J.; Cavanagh, P.R. Simplified versus geometrically accurate models of forefoot anatomy to predict plantar pressures: A finite element study. J. Biomech. 2016, 49, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Shu, L.; Hua, T.; Wang, Y.; Li, Q.; Feng, D.D.; Tao, X. In-shoe plantar pressure measurement and analysis system based on fabric pressure sensing array. IEEE Trans. Inform. Technol. Biomed. 2010, 14, 767–775. [Google Scholar]
- Cousins, S.D.; Morrison, S.C.; Drechsler, W.I. The reliability of plantar pressure assessment during barefoot level walking in children aged 7–11 years. J. Foot Ankle Res. 2012, 5, 8. [Google Scholar] [CrossRef] [PubMed]
- Orlin, M.N.; McPoil, T.G. Plantar pressure assessment. Phys. Ther. 2000, 80, 399–409. [Google Scholar] [PubMed]
- Razak, A.H.A.; Zayegh, A.; Begg, R.K.; Wahab, Y. Foot plantar pressure measurement system: A review. Sensors 2012, 12, 9884–9912. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.M.; Fuss, F.K.; Weizman, Y.; Woudstra, Y.; Troynikov, O. Design of low cost smart insole for real time measurement of plantar pressure. Procedia Technol. 2015, 20, 117–122. [Google Scholar] [CrossRef]
- Mann, R.; Malisoux, L.; Urhausen, A.; Meijer, K.; Theisen, D. Plantar pressure measurements and running-related injury: A systematic review of methods and possible associations. Gait Posture 2016, 47, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Prasad, A.S.G.; Omkar, S.N.; Vikranth, H.N.; Anil, V.; Chethana, K.; Asokan, S. Design and development of Fiber Bragg Grating sensing plate for plantar strain measurement and postural stability analysis. Measurement 2014, 47, 789–793. [Google Scholar] [CrossRef]
- Ahmadi, R.; Dargahi, J.; Packirisamy, M.; Cecere, R. A new hybrid catheter-tip tactile sensor with relative hardness measuring capability for use in catheter-based heart surgery. In Proceedings of the IEEE Sensors, Waikoloa, HI, USA, 1–4 November 2010; pp. 1592–1595.
- Tosi, D.; Saccomandi, P.; Schena, E.; Duraibabu, D.B.; Poeggel, S.; Leen, G.; Lewis, E. Intra-tissue pressure measurement in ex vivo liver undergoing laser ablation with fiber-optic Fabry-Perot probe. Sensors 2016, 16, 544. [Google Scholar] [CrossRef] [PubMed]
- Saccomandi, P.; Oddo, C.M.; Zollo, L.; Formica, D.; Romeo, R.A.; Massaroni, C.; Caponero, M.A.; Vitiello, N.; Guglielmelli, E.; Silvestri, S.; Schena, E. Feedforward neural network for force coding of an MPI-compatible tactile sensor array based on fiber Bragg grating. J. Sens. 2015, 2015, 367194. [Google Scholar] [CrossRef]
- Liang, T.C.; Lin, Y.L. A fiber-optic sensor for the ground vibration detection. Opt. Commun. 2013, 306, 190–197. [Google Scholar] [CrossRef]
- Feng, M.Q.; Kim, D.H. Novel fiber optic accelerometer system using geometric moire fringe. Sens. Actuators A Phys. 2006, 128, 37–142. [Google Scholar] [CrossRef]
- Huang, H.S.; Liang, T.C. The fabrication and analysis of lateral pressure fiber sensor based on fiber Bragg grating. Microw. Opt. Technol. Lett. 2008, 50, 2535–2537. [Google Scholar] [CrossRef]
- Liang, T.C.; Huang, H.S.; Chuang, M.H. Study on fiber grating sensors for concentration measurement of cottonseed oil adulteration in pure olive oil. Microelectron. Eng. 2015, 148, 21–24. [Google Scholar] [CrossRef]
- Dziuda, L.; Skibniewski, F.W.; Krej, M.; Lewandowski, J. Monitoring respiration and cardiac activity using fiber Bragg grating-based sensor. IEEE Trans. Biomed. Eng. 2012, 59, 1934–1942. [Google Scholar] [CrossRef] [PubMed]
- Al-Fakih, E.A.; Osman, N.A.A.; Adikan, F.R.M.; Eshraghi, A.; Jahanshahi, P. Development and validation of fiber Bragg grating sensing pad for interface pressure measurements within prosthetic sockets. IEEE Sens. J. 2016, 16, 965–974. [Google Scholar] [CrossRef]
- Chang, Y.T.; Yen, C.T.; Wu, Y.S.; Cheng, H.C. Using a fiber loop and fiber Bragg grating as a fiber optic sensor to simultaneously measure temperature and displacement. Sensors 2013, 13, 6542–6551. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Zhou, Z.; Wen, X.; Zhang, D. A diaphragm-type fiber Bragg grating pressure sensor with temperature compensation. Measurement 2013, 46, 1041–1046. [Google Scholar] [CrossRef]
- Li, J.; Neumann, H.; Ramalingam, R. Design, fabrication, and testing of fiber Bragg grating sensors for cryogenic long-range displacement measurement. Cryogenics 2015, 68, 36–43. [Google Scholar] [CrossRef]
- Zhao, Z.G.; Zhang, Y.J.; Li, C.; Wan, Z.; Li, Y.N.; Wang, K.; Xu, J.F. Monitoring of coal mine roadway roof separation based on fiber Bragg grating displacement sensors. Int. J. Rock Mech. Min. Sci. 2015, 74, 128–132. [Google Scholar] [CrossRef]
- Cavaiola, C.; Saccomandi, P.; Massaroni, C.; Tosi, D.; Giurazza, F.; Frauenfelder, G.; Zobel, B.B.; Matteo, F.M.D.; Caponero, M.A.; Polimadei, A.; et al. Error of a temperature probe for cancer ablation monitoring caused by respiratory movements: Ex vivo and in vivo analysis. IEEE Sens. J. 2016, 16, 5934–5941. [Google Scholar] [CrossRef]
- Park, H.J.; Song, M. Linear FBG temperature sensor interrogation with Fabry-Perot ITU multi-wavelength reference. Sensors 2008, 8, 6769–6776. [Google Scholar] [CrossRef]
- Marques, R.D.S.; Prado, A.R.; Antunes, P.F.D.C.; André, P.S.D.B.; Ribeiro, M.R.N.; Frizera-Neto, A.; Pontes, M.J. Corrosion Resistant FBG-based quasi-distributed sensor for crude oil tank dynamic temperature profile monitoring. Sensors 2015, 15, 30693–30703. [Google Scholar] [CrossRef] [PubMed]
- Ma, G.M.; Li, C.R.; Quan, J.T.; Jiang, J.; Cheng, Y.C. A fiber Bragg grating tension and tilt sensor applied to icing monitoring on overhead transmission lines. IEEE Trans. Power Deliv. 2011, 26, 2163–2170. [Google Scholar] [CrossRef]
- Bao, H.; Dong, X.; Shao, L.Y.; Zhao, C.L.; Jin, S. Temperature-insensitive 2-D tilt sensor by incorporating fiber Bragg gratings with a hybrid pendulum. Opt. Commun. 2010, 283, 5021–5024. [Google Scholar] [CrossRef]
- Liang, T.C.; Lin, Y.L. Ground vibrations detection with fiber optic sensor. Opt. Commun. 2012, 285, 2363–2367. [Google Scholar] [CrossRef]
- Melle, S.M.; Liu, K.; Measures, R.M. Practical fiber-optic Bragg grating strain gauge system. Appl. Opt. 1993, 32, 3601–3609. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Li, J.X.; Hong, Y.; Wang, L. Characteristics of plantar loads in maximum forward lunge tasks in badminton. PLoS ONE 2015, 10, e0137558. [Google Scholar] [CrossRef] [PubMed]
- Ho, I.J.; Hou, Y.Y.; Yang, C.H.; Wu, W.L.; Chen, S.K.; Guo, L.Y. Comparison of plantar pressure distribution between different speed and incline during treadmill jogging. J. Sports Sci. Med. 2010, 9, 154–160. [Google Scholar] [PubMed]
- Puth, M.T.; Neuhauser, M.; Ruxton, G.D. Effective use of Pearson's product-moment correlation coefficient. Anim. Behav. 2014, 93, 183–189. [Google Scholar] [CrossRef]

| No. | Foot Type | |
|---|---|---|
| Left | Right | |
| 1 | neutral | neutral |
| 2 | neutral | neutral |
| 3 | neutral | neutral |
| 4 | cavus | cavus |
| 5 | cavus | cavus |
| 6 | cavus | cavus |
| 7 | cavus | cavus |
| 8 | flat | flat |
| 9 | flat | flat |
| 10 | supinated | supinated |
| 11 | cavus | neutral |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liang, T.-C.; Lin, J.-J.; Guo, L.-Y. Plantar Pressure Detection with Fiber Bragg Gratings Sensing System. Sensors 2016, 16, 1766. https://doi.org/10.3390/s16101766
Liang T-C, Lin J-J, Guo L-Y. Plantar Pressure Detection with Fiber Bragg Gratings Sensing System. Sensors. 2016; 16(10):1766. https://doi.org/10.3390/s16101766
Chicago/Turabian StyleLiang, Tsair-Chun, Jhe-Jhun Lin, and Lan-Yuen Guo. 2016. "Plantar Pressure Detection with Fiber Bragg Gratings Sensing System" Sensors 16, no. 10: 1766. https://doi.org/10.3390/s16101766
APA StyleLiang, T.-C., Lin, J.-J., & Guo, L.-Y. (2016). Plantar Pressure Detection with Fiber Bragg Gratings Sensing System. Sensors, 16(10), 1766. https://doi.org/10.3390/s16101766







