Phase Difference Optimization of Dual-Wavelength Excitation for the CW-Photoacoustic-Based Noninvasive and Selective Investigation of Aqueous Solutions of Glucose
Abstract
:1. Introduction
2. Experimental Section
2.1. OPBS Method
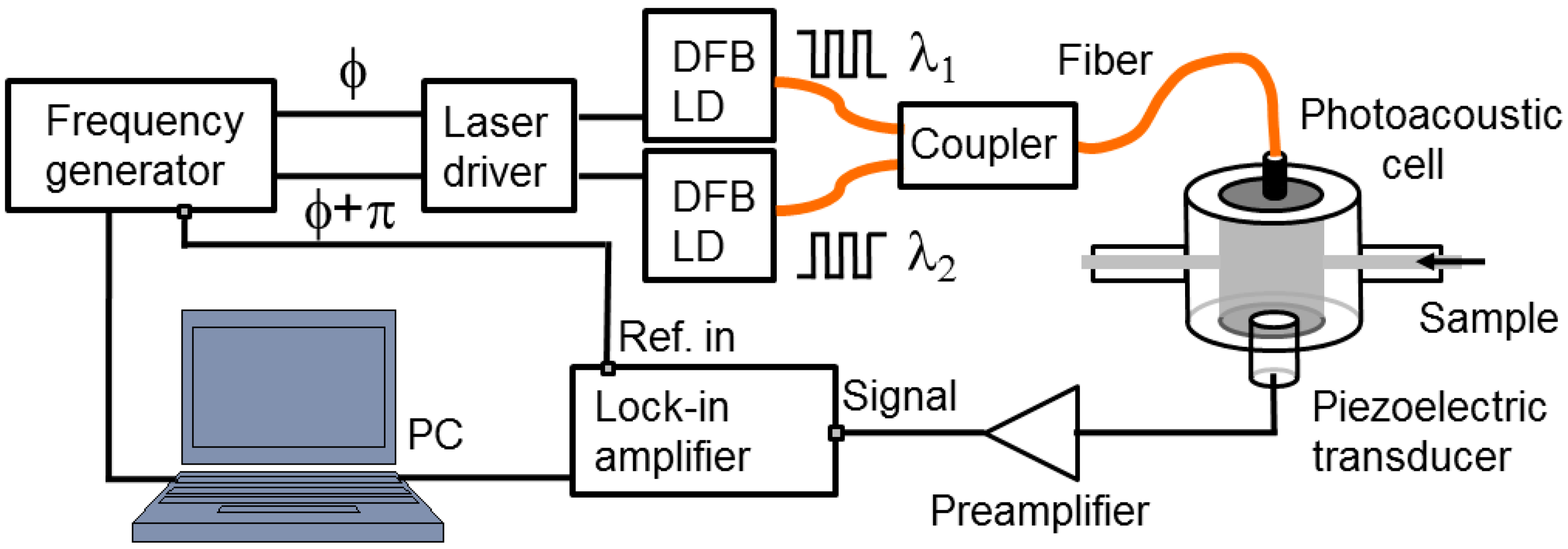
2.2. Experimental Setup
2.3. Glucose Solution Preparation
2.4. Experimental Sequence
3. Results and Discussion
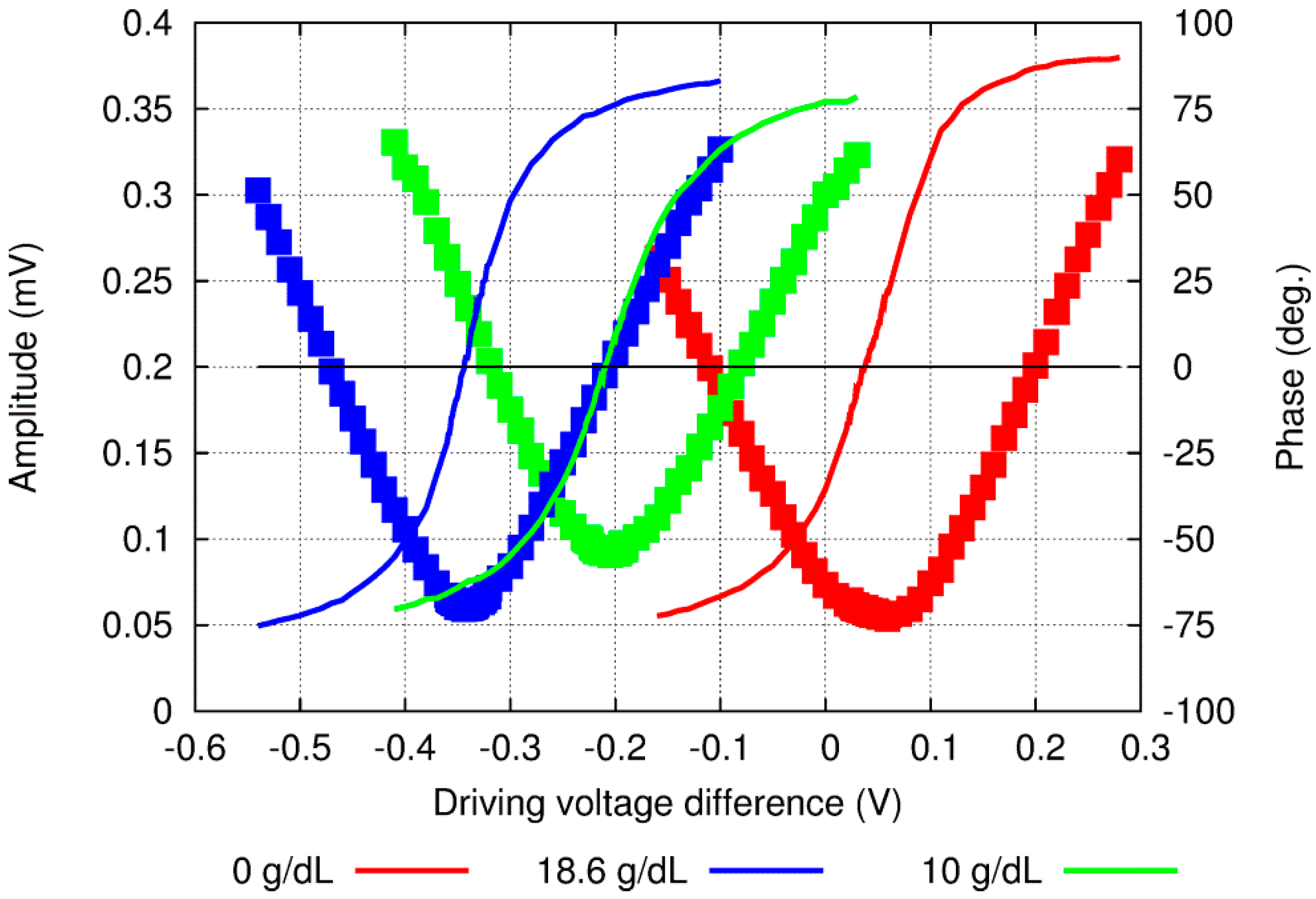
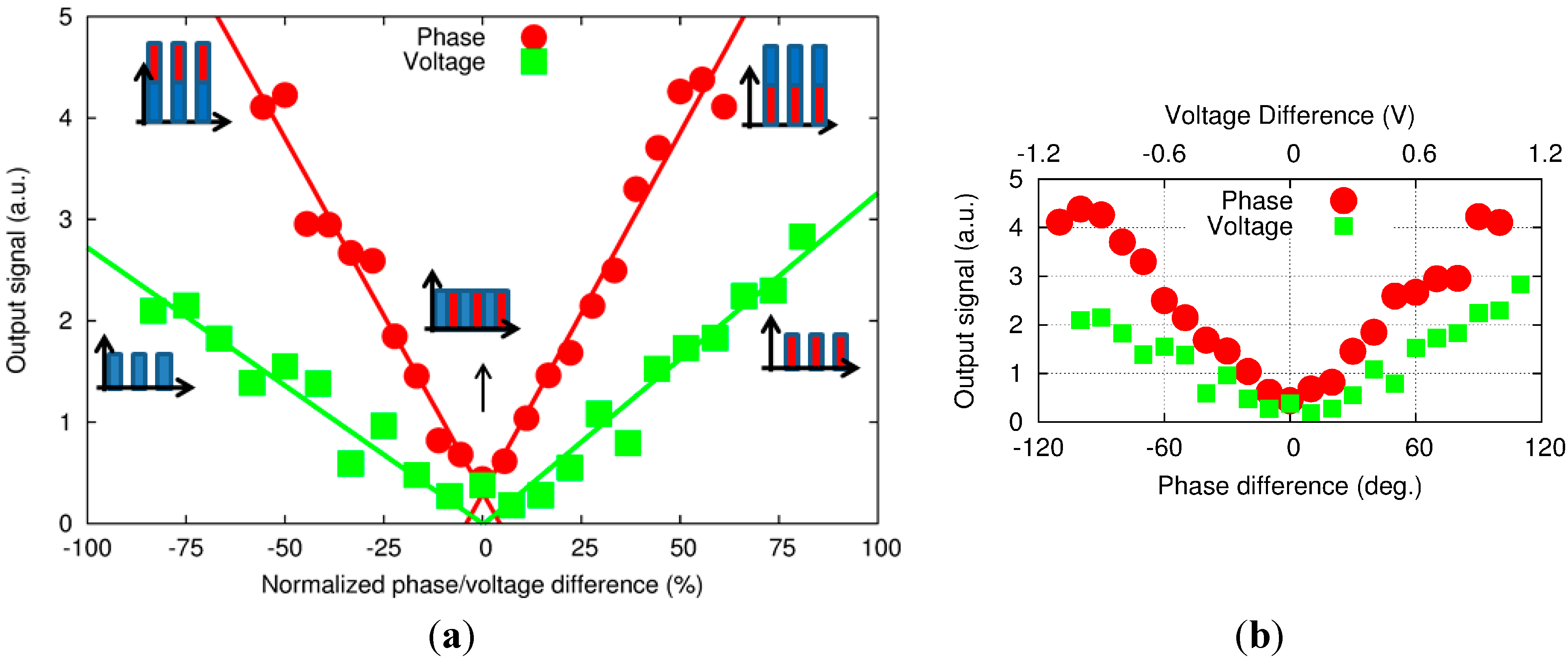
3.1. PA Signal for Wide Range of Phase Differences and Driving Voltages
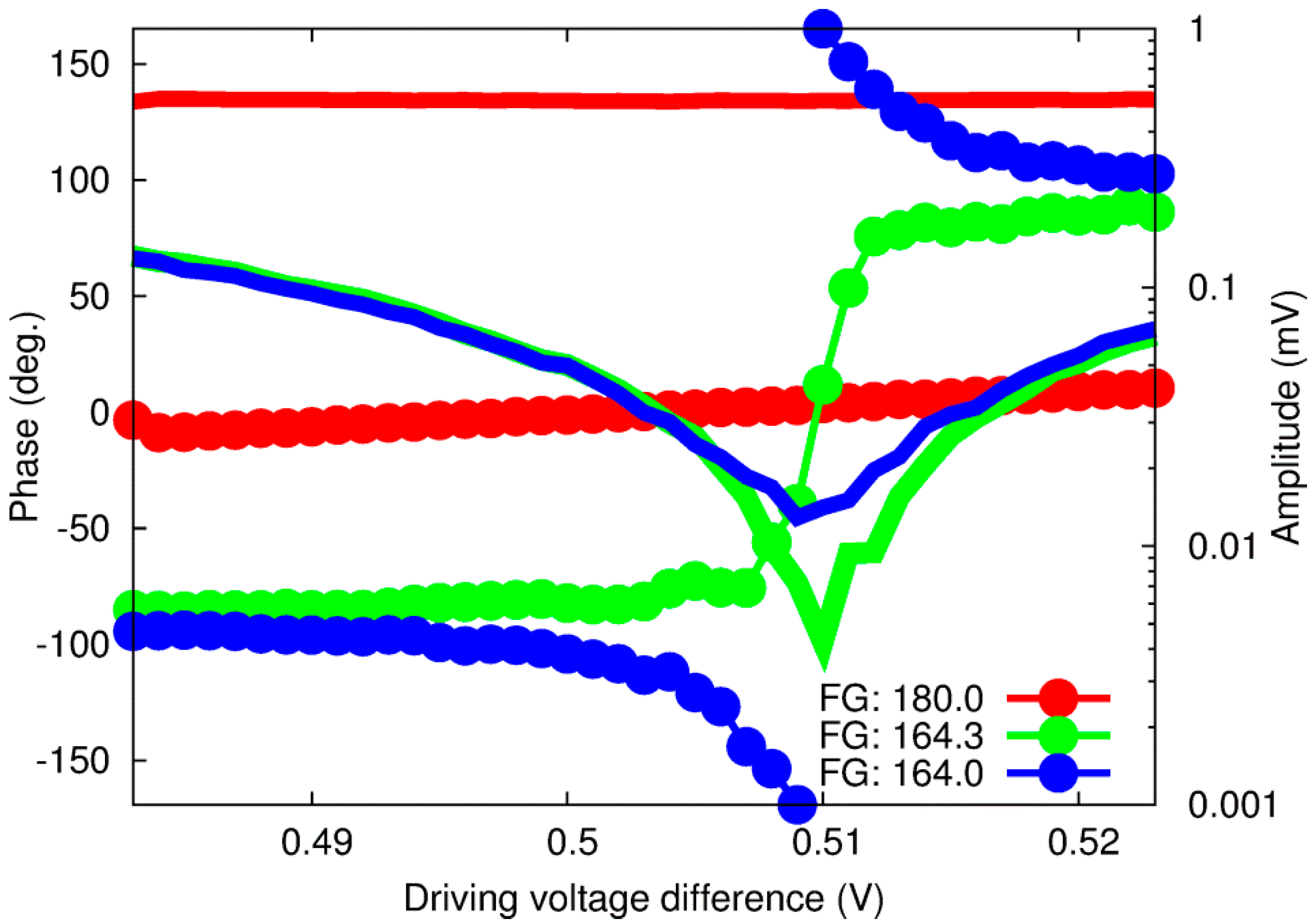

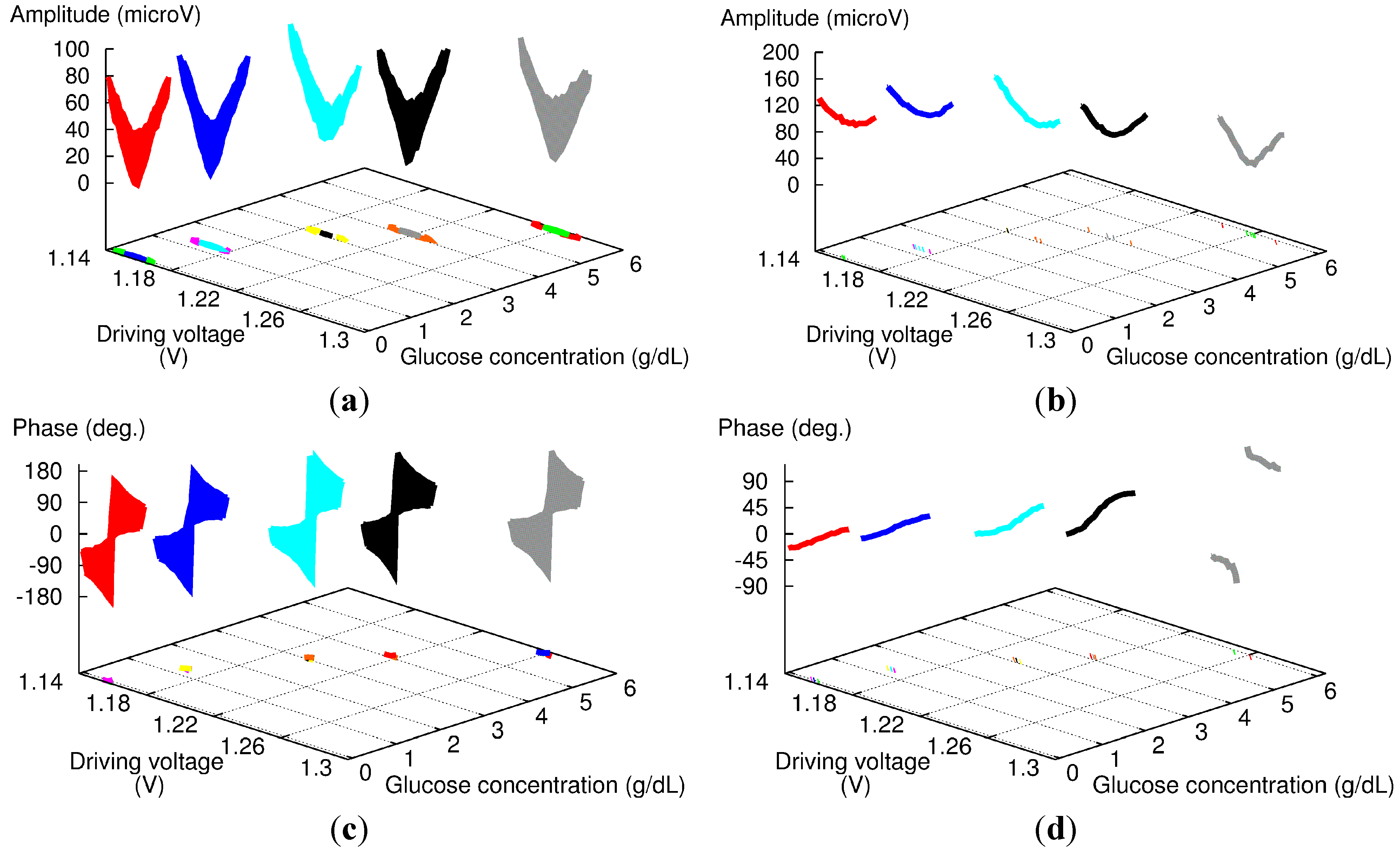
3.2. Analysis in the Frequency Domain
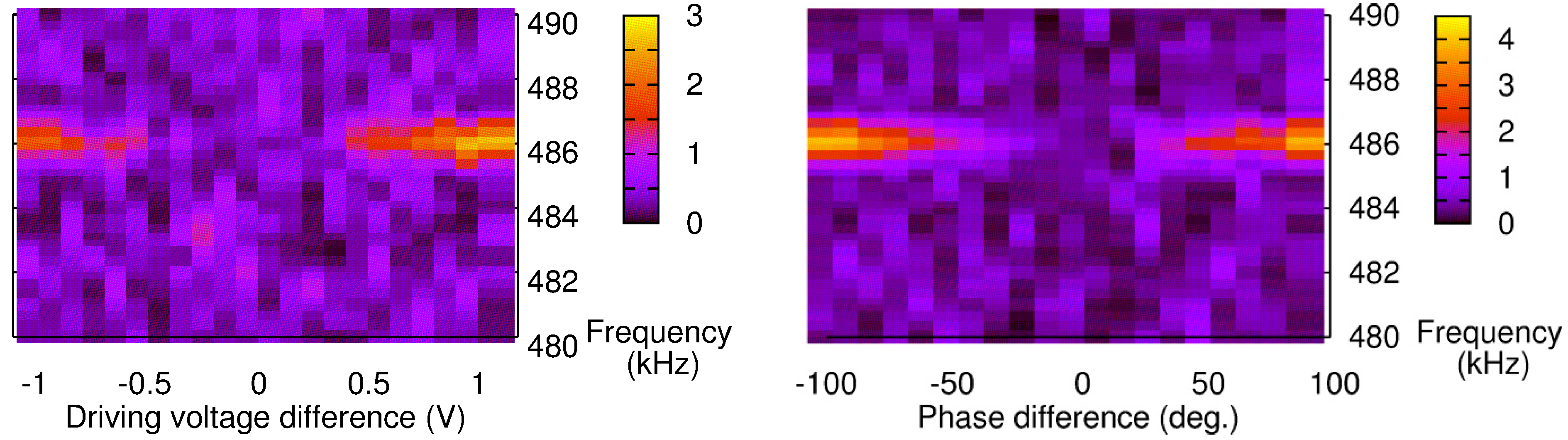
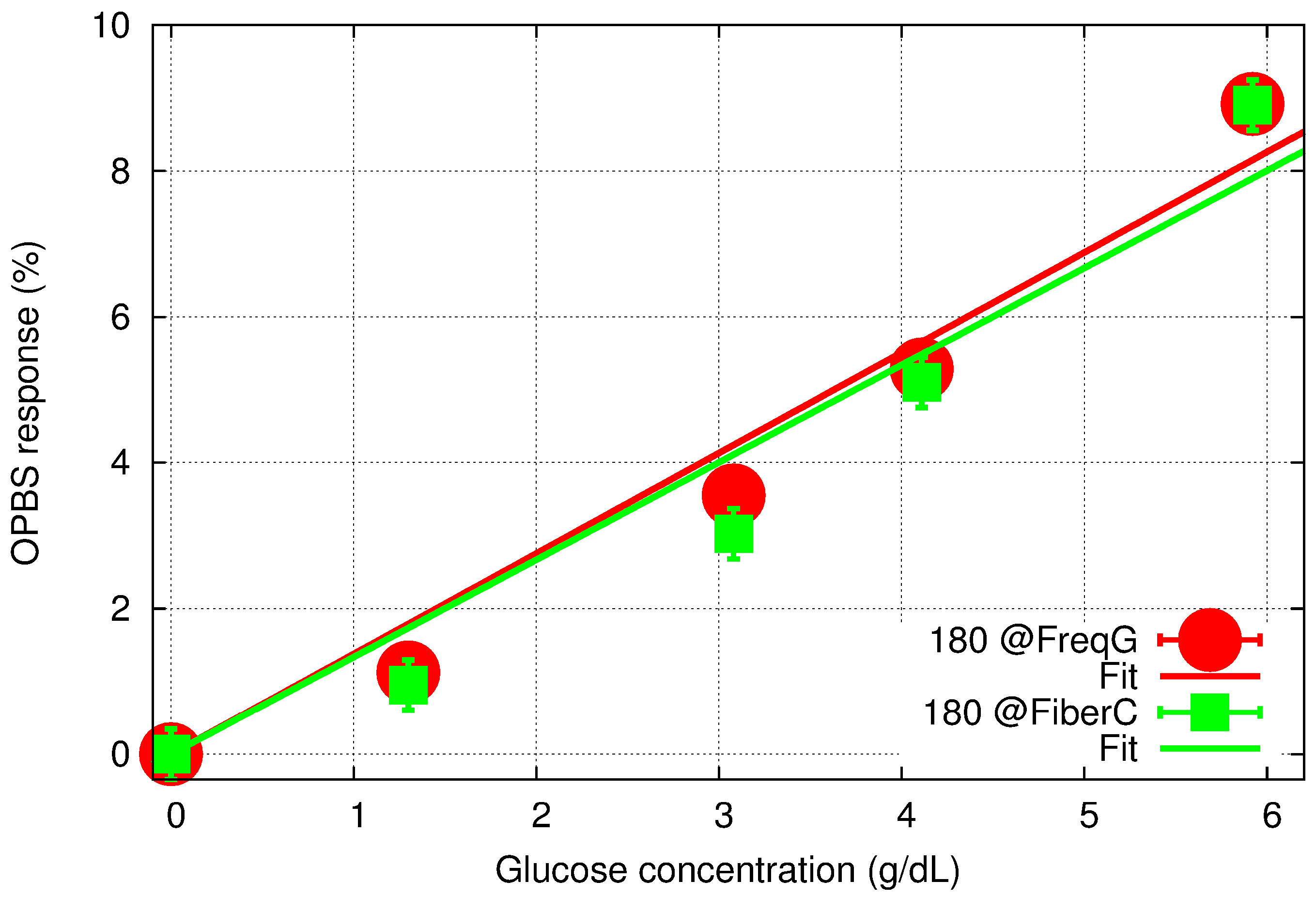
3.3. Measurements of Aqueous Glucose Solution
3.4. Remaining Issues
4. Conclusions
Conflicts of Interest
References
- Wild, S.; Roglic, G.; Green, A.; Sicree, R.; King, H. Global Prevalence of Diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care 2004, 27, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization and International Diabetes Federation. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Roglic, G.; Unwin, N.; Bennett, P.; Mathers, C.; Tuomilehto, J.; Satyajit, N.; Connilly, V.; King, H. The Burden of Mortality Attributable to Diabetes. Diabetes Care 2005, 28, 2130–2135. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. IDF Diabetes Atlas Sixth Edition, 6th ed.; International Diabetes Federation: Brussels, Belgium, 2013; p. 160. [Google Scholar]
- The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of Diabetes Mellitus. Diabetes Care 2003, 26, 3160–3167. [Google Scholar]
- American Diabetes Association. Standards of Medical Care in Diabetes. Diabetes Care 2005, 28, S4–S36. [Google Scholar]
- Rubin, A.L. Diabetes for Dummies, 3rd ed.; Wiley Publishing, Inc.: Hoboken, NJ, USA, 2008. [Google Scholar]
- American Diabetes Association. Consensus Statement on Self-Monitoring of Blood Glucose. Diabetes Care 1987, 10, 95–99. [Google Scholar]
- Kirk, J.K.; Stegner, J. Self-Monitoring of Blood Glucose: Practical Aspects. J. Diabetes Sci. Technol. 2010, 4, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Thorsell, A.; Gordon, M.; Jovanovic, L. Continuous glucose monitoring: A stepping stone in the journey towards a cure for diabetes. J. Matern. Fetal. Neonatal Med. 2004, 15, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Sachedina, N.; Pickup, J. Performance assessment of the Medtronic-MiniMed Continuous Glucose Monitoring System and its use for measurement of glycaemic control in Type 1 diabetic subjects. Diabet. Med. 2003, 20, 1012–1015. [Google Scholar] [CrossRef] [PubMed]
- Ginsberg, B.H. An Overview of Minimally Invasive Technologies. Clin. Chem. 1992, 38, 1596–1600. [Google Scholar] [PubMed]
- Kost, J.; Mitragotri, S.; Gabbay, R.; Pishko, M.; Langer, R. Transdermal monitoring of glucose and other analytes using ultrasound. Nat. Med. 2000, 6, 347–350. [Google Scholar] [CrossRef] [PubMed]
- Chuang, H.; Taylor, E.; Davison, T.W. Clinical evaluation of a continuous minimally invasive glucose flux sensor placed over ultrasonically permeated skin. Diabetes Technol. Ther. 2004, 6, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Voskerician, G.; Shive, M.S.; Shawgo, R.S.; von Recum, H.; Anderson, J.M.; Cima, M.J.; Langer, R. Biocompatibility and biofouling of MEMS drug delivery devices. Biomaterials 2003, 24, 1959–1967. [Google Scholar] [CrossRef]
- Ma, K.; Yuen, J.M.; Shah, N.C.; Walsh, J.T.; Glucksberg, M.R.; van Duyne, R.P. In vivo, transcutaneous glucose sensing using surface-enhanced spatially offset raman spectroscopy: Multiple rats, improved hypoglycemic accuracy, low incident power, and continuous monitoring for greater than 17 days. Anal. Chem. 2011, 83, 9146–9152. [Google Scholar] [CrossRef] [PubMed]
- Voskerician, G.; Anderson, J.M. Foreign Body Reaction. In Wiley Encyclopedia of Biomedical Engineering; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2006. [Google Scholar]
- Pickup, J.C.; Hussain, F.; Evans, N.D.; Sachedina, N. In vivo glucose monitoring: The clinical reality and the promise. Biosens. Bioelectron. 2005, 20, 1897–902. [Google Scholar] [CrossRef] [PubMed]
- Wagner, J.; Malchoff, C.; Abbott, G. Invasiveness as a barrier to self-monitoring of blood glucose in diabetes. Diabetes Technol. Ther. 2005, 7, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, L.; Schmelzeisen-Redeker, G. Non-invasive continuous glucose monitoring in Type I diabetic patients with optical glucose sensors. Diabetologia 1998, 41, 848–854. [Google Scholar] [CrossRef] [PubMed]
- Khalil, O. Spectroscopic and clinical aspects of noninvasive glucose measurements. Clin. Chem. 1999, 177, 165–177. [Google Scholar]
- Tura, A.; Maran, A.; Pacini, G. Non-invasive glucose monitoring: Assessment of technologies and devices according to quantitative criteria. Diabetes Res. Clin. Pract. 2007, 77, 16–40. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, P.; Quan, K.M.; MacKenzie, H.A.; Freeborn, S.S.; Hannigan, J.; Johnston, E.M.; Greig, F.; Binnie, T.D. Application of pulsed laser photoacoustic sensors in monitoring oil contamination in water. Sens. Actuators B Chem. 1995, 29, 339–344. [Google Scholar] [CrossRef]
- Christison, G.B.; MacKenzie, H.A. Laser photoacoustic determination of physiological glucose concentrations in human whole blood. Med. Biol. Eng. Comput. 1993, 31, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Kottmann, J.; Grob, U.; Rey, J.M.; Sigrist, M.W. Mid-infrared fiber-coupled photoacoustic sensor for biomedical applications. Sensors 2013, 13, 535–549. [Google Scholar] [CrossRef] [PubMed]
- Pleitez, M.A.; Lieblein, T.; Bauer, A.; Hertzberg, O.; von Lilienfeld-Toal, H.; Ma, W.; Mäntele, W. In vivo noninvasive monitoring of glucose concentration in human epidermis by mid-infrared pulsed photoacoustic spectroscopy. Anal. Chem. 2013, 85, 1013–1020. [Google Scholar] [CrossRef] [PubMed]
- Weiss, R.; Yegorchikov, Y.; Shusterman, A.; Raz, I. Noninvasive continuous glucose monitoring using photoacoustic technology—Results from the first 62 subjects. Diabetes Technol. Ther. 2007, 9, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z. Pulsed Photoacoustic Techniques and Glucose Determination in Human Blood and Tissue; Oulu University Press: Oulu, Finland, 2002. [Google Scholar]
- Camou, S.; Haga, T.; Tajima, T.; Tamechika, E. Detection of aqueous glucose based on a cavity size- and optical-wavelength-independent continuous-wave photoacoustic technique. Anal. Chem. 2012, 84, 4718–4724. [Google Scholar] [CrossRef] [PubMed]
- Camou, S.; Ueno, Y.; Tamechika, E. Simulation Tool for the Prediction of Compound Dependence of CW-Photoacoustic-Based Sensor Using Dual Differential Optical Excitation. Procedia Eng. 2012, 47, 474–477. [Google Scholar] [CrossRef]
- Camou, S. Continuous-wave Photoacoustic-based Sensor for the Detection of Aqueous Glucose: Towards Non-invasive and Continuous Glycemia Sensing. In Pervasive and Mobile Sensing and Computing for Healthcare; Mukhopadhyay, S.C., Postolache, O.A., Eds.; Springe-Verlag: Berlin/Heidelberg, Germany, 2013; pp. 111–134. [Google Scholar]
- Spanner, G.; Niessner, R. New concept for the non-invasive determination of physiological glucose concentrations using modulated laser diodes. Anal. Bioanal. Chem. 1996, 354, 306–310. [Google Scholar] [CrossRef] [PubMed]
- Spanner, G.; Niessner, R. Noninvasive determination of blood constituents using an array of modulated laser diodes and a photoacoustic sensor head. Anal. Bioanal. Chem. 1996, 355, 327–328. [Google Scholar] [CrossRef] [PubMed]
- Patel, C.; Tam, A. Pulsed optoacoustic spectroscopy of condensed matter. Rev. Mod. Phys. 1981, 53, 517–550. [Google Scholar] [CrossRef]
- Camou, S.; Ueno, Y.; Tamechika, E. Isothermic determination of aqueous solution glucose concentration in low mg/dL range by CW-photoacoustic-based protocol. Sens. Actuators B Chem. 2013, 185, 568–574. [Google Scholar] [CrossRef]
- Niemz, M.H. Laser-Tissue Interactions: Fundamentals and Applications, 3rd ed.; Springer: Heidelberg, Germany, 2003. [Google Scholar]
- Yoon, G.; Amerov, A.K.; Jeon, K. Optical measurement of glucose levels in scattering media. In Proceedings of the 20th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Hong Kong, China, 29 October–1 November 1998; Volume 20, pp. 1897–1899.
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Camou, S. Phase Difference Optimization of Dual-Wavelength Excitation for the CW-Photoacoustic-Based Noninvasive and Selective Investigation of Aqueous Solutions of Glucose. Sensors 2015, 15, 16358-16371. https://doi.org/10.3390/s150716358
Camou S. Phase Difference Optimization of Dual-Wavelength Excitation for the CW-Photoacoustic-Based Noninvasive and Selective Investigation of Aqueous Solutions of Glucose. Sensors. 2015; 15(7):16358-16371. https://doi.org/10.3390/s150716358
Chicago/Turabian StyleCamou, Serge. 2015. "Phase Difference Optimization of Dual-Wavelength Excitation for the CW-Photoacoustic-Based Noninvasive and Selective Investigation of Aqueous Solutions of Glucose" Sensors 15, no. 7: 16358-16371. https://doi.org/10.3390/s150716358
APA StyleCamou, S. (2015). Phase Difference Optimization of Dual-Wavelength Excitation for the CW-Photoacoustic-Based Noninvasive and Selective Investigation of Aqueous Solutions of Glucose. Sensors, 15(7), 16358-16371. https://doi.org/10.3390/s150716358




