1. Introduction
Mitochondria are essential organelles for energy production in eukaryotic cells. Their function is regulated by both nuclear DNA and mitochondrial DNA (mtDNA), which encodes key components of the respiratory chain and ATP synthase, as well as RNA molecules required for mitochondrial protein synthesis. Each cell contains multiple copies of mtDNA. The default is homoplasmy, which means that the mtDNA is the same in all, but mutated and wildtype mtDNA copies can also coexist within the same cell, which is known as heteroplasmy. In cases of mitochondrial disease due to a heteroplasmic mtDNA mutation, symptoms typically arise when heteroplasmic mutation load exceeds a tissue-specific threshold. High energy-demanding tissues like brain and skeletal muscles are most commonly affected [
1]. Patients with mitochondrial myopathy suffer from fatigue, muscle weakness, and exercise intolerance [
2]. Jeppesen et al. showed in a study with 50 m.3243A>G mutation carriers that all carriers with <50% m.3243A>G mutation in skeletal muscle showed no exercise intolerance, while part of the 50–80% mutation load carriers and most mutation carriers with >80% mutation load did show exercise intolerance, showing a clear relationship between m.3243A>G mutation load and skeletal muscle functioning [
3]. Currently, there is no effective cure for mitochondrial myopathies, and patients are supported with symptomatic management by receiving dietary supplements, medication for muscle pain, physical therapy, and respiratory support [
4].
To combat mitochondrial myopathy caused by an mtDNA mutation, our group is developing a therapy using autologous muscle stem cells, called mesoangioblasts, with a low mtDNA mutation load. Mesoangioblasts can be efficiently isolated from skeletal muscles and expanded ex vivo till sufficient numbers for systemic administration to treat all muscles. Upon intra-arterial delivery, mesoangioblasts migrate to damaged skeletal muscles where they can form new fibers or fuse with existing muscle fibers. Preclinical studies demonstrated that mesoangioblasts of about half of analyzed mtDNA mutation carriers displayed a low mtDNA mutation load and fulfilled all criteria for therapeutic application, allowing transplantation of autologous mesoangioblasts [
5]. The first in-human clinical study demonstrated that one intra-arterial administration of autologous mesoangioblasts in the lower leg of m.3243A>G mutation carriers is safe [
6], and a currently ongoing phase IIa clinical study aims to assess the effect of three mesoangioblast administrations on muscle strength, exercise intolerance, and m.3243A>G mutation load in the arm of m.3243A>G patients with a measurable functional deficit.
In a previous in vitro study, we have reported that the addition of healthy mesangioblasts to myotubes with a high mtDNA mutation load leads to a proportional reduction in mtDNA mutation load [
7]. Therefore, the current in vitro study assesses possible changes in mitochondrial morphology and membrane potential in myotubes of mtDNA patients and the effect of fusion with healthy mesoangioblasts. To this end, we used confocal spinning disk microscopy in combination with mitochondrial staining using tetramethylrhodamine methyl ester (TMRM), as described before [
8], to study myotubes derived from mesoangioblasts of two female mtDNA mutation carriers (M02 with 96% m.3271T>C and M11 with 73% m.3291T>C) and one male control without the m.3271T>C or m.3291T>C mutation.
2. Results
First, we determined mitochondrial volume, number of individual mitochondrial objects, and membrane potential in non-hybrid myotubes, i.e., directly derived from 11 days differentiated mesoangioblasts with a high mtDNA mutation load (M02 and M11) and a control (M06) to assess a possible effect of the high mtDNA mutation load. Next, we assessed the effect on these parameters following addition of control male mesoangioblasts (mM06) at differentiation day 5 to female myotubes of M02 and M11 with an mtDNA mutation, i.e., hybrid myotubes. These analyses were performed in one single experiment which contained both hybrid and non-hybrid myotubes.
2.1. Analysis of Myotube Fusion Index
First, the Myotube Fusion Index (MFI) was assessed (
Table 1). MFI was calculated from eight fields of view per culture for non-hybrid (M02, M11, and M06) and hybrid myotubes (M02+mM06 and M11+mM06). The fusion index was defined as the percentage of nuclei located within multinucleated myotubes relative to the total number of nuclei per field of view.
In addition, we compared if there were significant differences in the number of nuclei or in sarcoplasm volume per myotube between these cell cultures. One-way ANOVA of these variables showed no statistically significant differences (
p > 0.05) within the non-hybrid myotubes. Next, hybrid and non-hybrid cell culture pairs were analyzed using
t-test. While no significant changes on MFI were observed, addition of mM06 to M02 myotubes resulted in myotubes with significantly increased (
p < 0.05) number of nuclei/myotube, sarcoplasm volume/nucleus, and total sarcoplasm volume per myotube (
Table 1). In contrast, mM06 fusion with M11 only significantly increased the number of nuclei/myotube and sarcoplasm volume/nucleus, but not total myotube sarcoplasm volume.
As analyzed myotubes contained varying numbers of nuclei per myotube (range 3–36), which was associated with varying sarcoplasm volume, this needs to be corrected to enable analysis of mitochondrial parameters. To compare non-hybrid M02, M11, and M06, we first verified that the sarcoplasm volume increases proportionally with the number of nuclei per myotube. This was supported by a strong linear relationship (R
2 values between 0.78 and 0.89), intercepts that were not significantly different from zero, and less than 10% variation in slope between the three cell cultures (
Supplemental Figure S2). This indicates that in non-hybrid cells, mitochondrial parameters can be normalized to either myotube sarcoplasm volume or number of nuclei per myotube. However, in hybrid myotubes, 33% variation between slopes of M02 and M02+mM06 (y = 4025.5x vs. y = 5342.9x) and between slopes of M11 and M11+mM06 (y = 4157.9x vs. y = 2773.2x) was observed. This substantial variation excludes normalization of mitochondrial parameters to sarcoplasm volume in these hybrid myotubes. Therefore, the number of nuclei was used for analysis of hybrid myotubes and the sarcoplasmic volume and/or number of nuclei was used for analysis of the non-hybrid myotubes.
2.2. Analysis of Mitochondrial Morphology and Membrane Potential in Non-Hybrid Myotubes with High Mutation Load (M02, M11) and a Healthy Control (M06)
First, total mitochondrial volume and organization (number of individual mitochondrial objects) was analyzed in myotubes derived from mesoangioblasts with a high mutation load (M02, M11) and from control mesoangioblasts (M06). The parameters were mitochondrial volume (µm
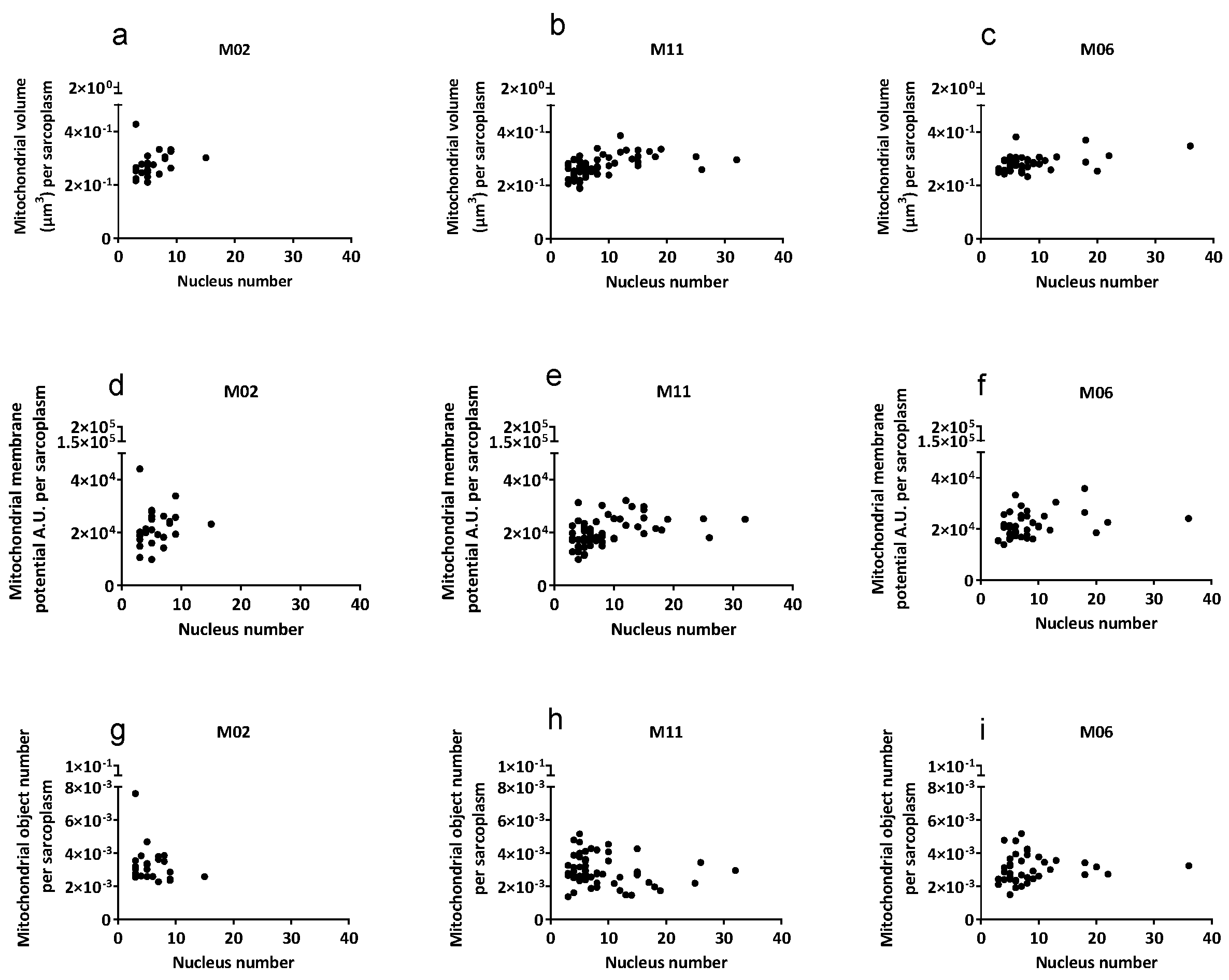
3) per myotube, mitochondrial membrane potential (A.U.), and the number of mitochondrial objects per myotube normalized to myotube cytoplasm volume (sarcoplasm). As shown in
Table 2 and
Figure 1, when corrected for sarcoplasm volume, no significant differences were apparent in mitochondrial volume, mitochondrial membrane potential, and mitochondrial object number between myotubes of three different cell cultures. Given the differences in size among individual myotubes, mitochondrial parameters were normalized to sarcoplasmic volume and plotted against the number of nuclei per myotube (
Figure 1). After normalization, mitochondrial parameters remained comparable across myotubes with increasing nucleus number, indicating proportional scaling with myotube size rather than changes in mitochondrial function per unit sarcoplasm.
2.3. Hybrid Myotubes: Fusion of Control Mesoangioblasts with Myotubes with High mtDNA Mutation Load
As shown in
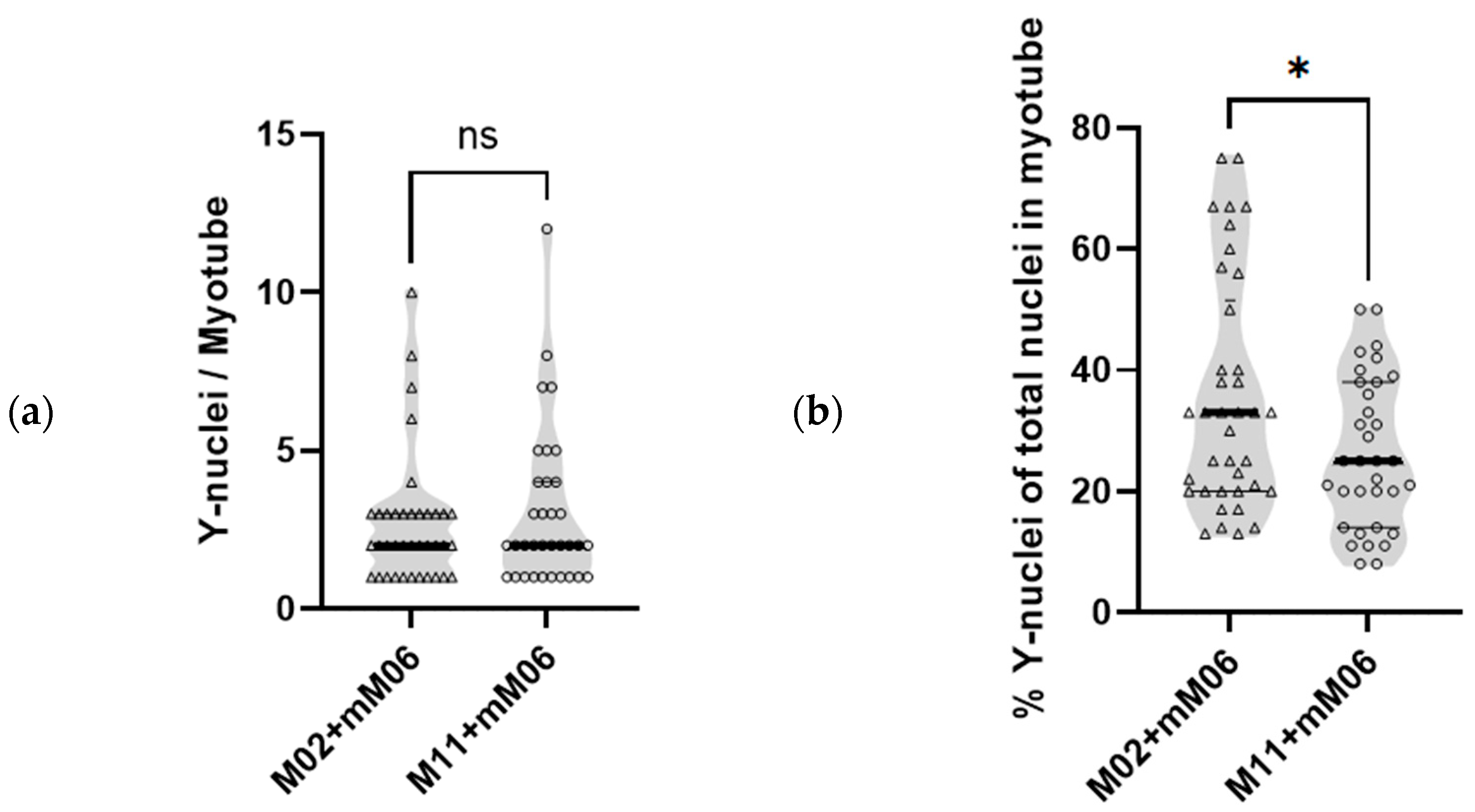
Table 1, hybrid myotubes (M02+mM06 and M11+mM06) contained on average 2.2 and 3.6 more nuclei per myotube, respectively, compared with non-hybrid M02 and M11 myotubes, corresponding to increases of 38% and 39%. As mM06 mesoangioblasts are derived from a male donor, their nuclei contain a Y-chromosome, which was fluorescently labeled to enable quantification of the contribution of mM06 mesoangioblasts to each individual hybrid myotube. As shown in
Figure 2a, the total number of Y-chromosome nuclei from mM06 per myotube was not significantly different in both groups of hybrids. However, due to non-hybrid M02 having less nuclei/myotube than non-hybrid M11 (5.8 ± 2.8 vs. 8.8 ± 6.1, mean ± SD, respectively), the relative contribution of control mM06 mesoangioblasts (Y) fused per total number of nuclei in the hybrid M02+mM06 myotubes is larger. As shown in
Figure 2b, the percentage of Y-nuclei in M02+mM06 hybrid myotubes was 35.5% ± 18.9% (mean ± SD, range: 12.5–75%), while M11+mM06 myotubes showed a significantly lower percentage of Y-nuclei 26.2% ± 12.3% (mean ± SD, range: 8.3–50%).
2.4. Analysis of Mitochondrial Morphology and Membrane Potential in Hybrid Myotubes Formed by Fusion of High mtDNA Mutation Load Myotubes with Control Mesoangioblasts
Hybrid M02+mM06 and M11+mM06 myotubes were compared with their respective non-hybrid counterparts (M02 and M11) to evaluate the contribution of control mM06 mesoangioblasts to mitochondrial properties following fusion with mtDNA-mutated myotubes. Mitochondrial parameters were calculated per myotube volume, per μm
3 sarcoplasm volume, and per myotube nucleus (
Table 3). However, as previously explained, the slope of the relationship between sarcoplasm volume and nuclei number differed significantly between hybrid and non-hybrid cultures (
Supplementary Table S1); therefore, we considered normalization per nucleus to be most appropriate.
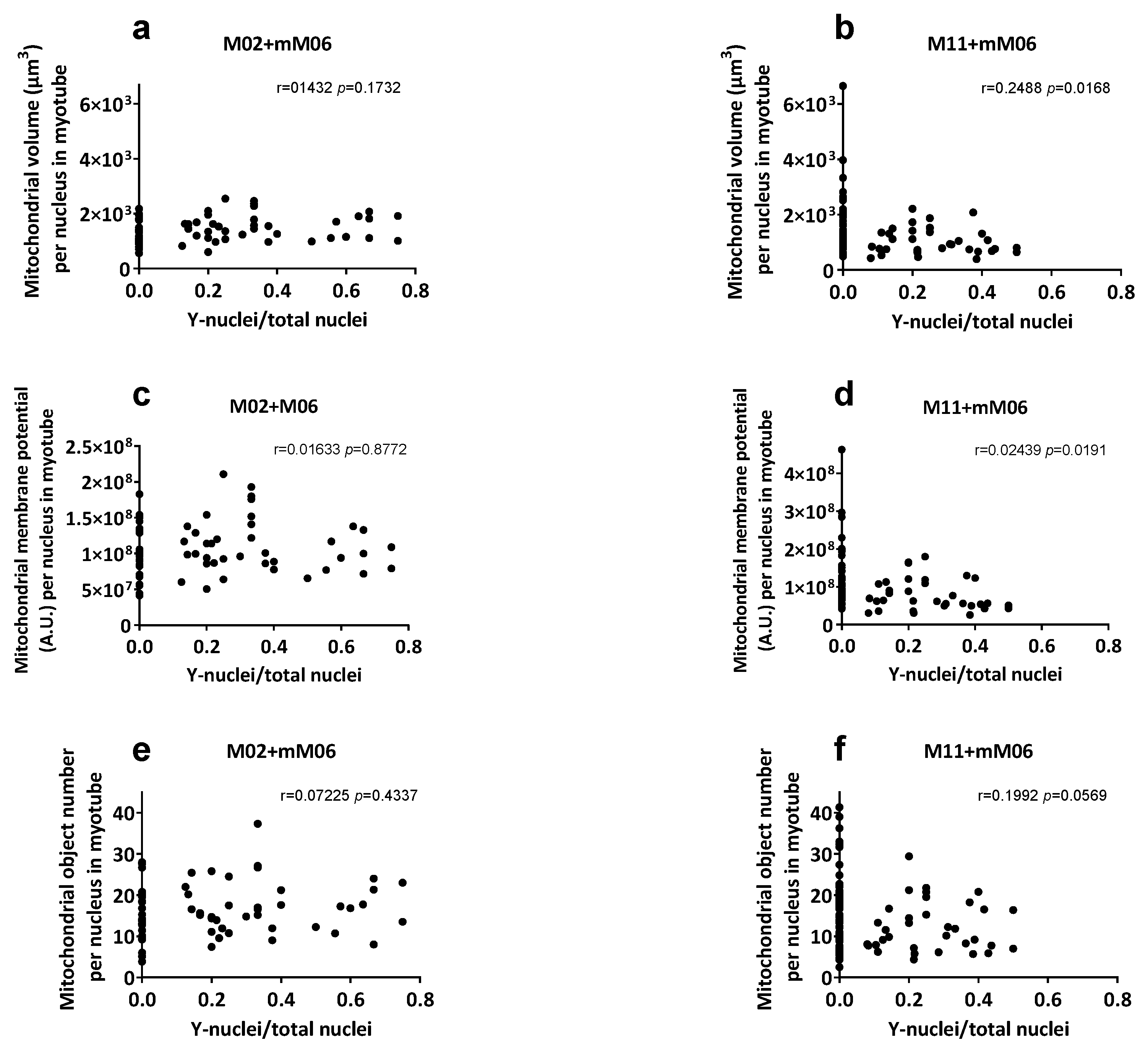
In comparisons between M11 vs. M11+mM06 hybrids, no differences were detected in total myotube volume, membrane potential, or number of mitochondrial objects when normalized per myotube or per sarcoplasm volume. When correcting for nuclei number, both mitochondrial volume and membrane potential were significantly reduced in M11+mM06, indicating reduced contribution of M06 mitochondria (
Table 3). Analysis of these parameters relative to the proportion of mM06 nuclei within hybrid myotubes (
Figure 3) showed a significant negative correlation in M11+mM06 for mitochondrial volume and membrane potential. In M11+mM06 hybrid myotubes, the number of mitochondrial objects per myotube nucleus was reduced, whereas the total number of mitochondrial objects per myotube remained unchanged, suggesting fusion of mM06-derived mitochondria with M11 mitochondria.
In contrast, M02+mM06 hybrids displayed a significant increase in mitochondrial volume (FC 1.70), membrane potential (FC 1.57), and number of mitochondrial objects (FC 1.55) per myotube, together with a significantly larger sarcoplasm volume (FC 1.72). When normalized per myotube nucleus, only total mitochondrial volume remained significantly increased by 1.15-fold, and no change was seen per sarcoplasm volume, indicating regulation by sarcoplasm volume.
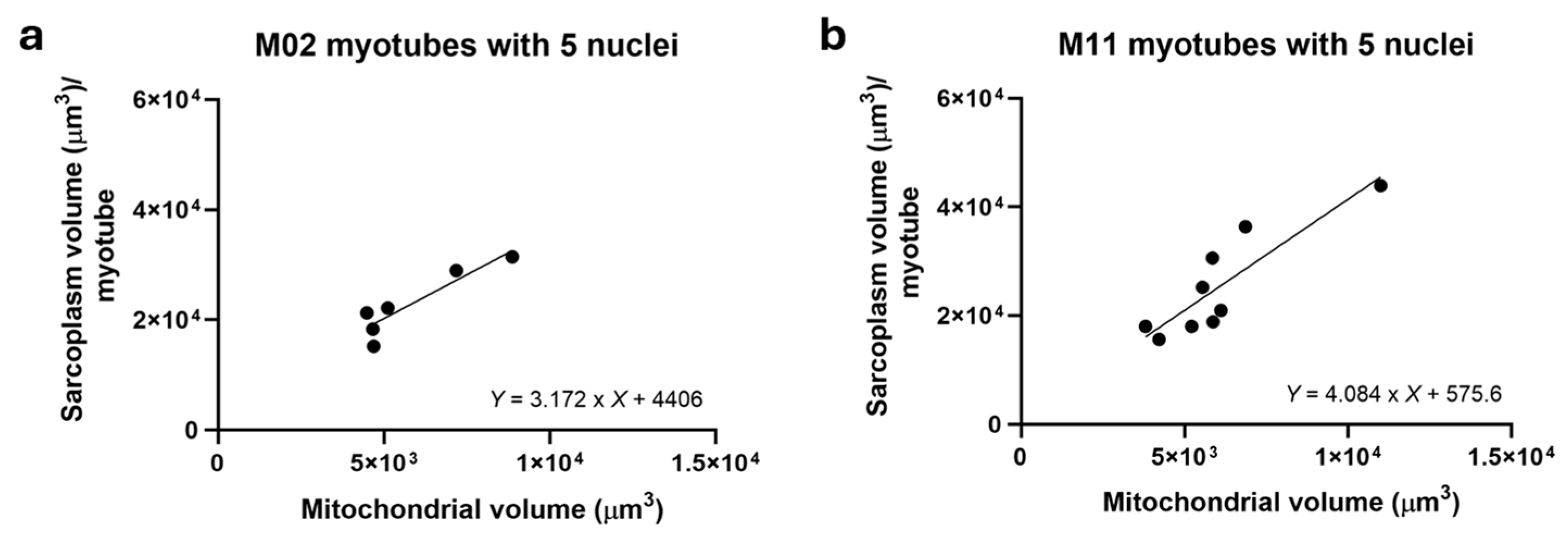
To further explore the relationship between mitochondrial volume and sarcoplasmic volume, non-hybrid M02 (
n = 7) and M11 (
n = 9) myotubes containing five nuclei were analyzed. As shown in
Figure 4, mitochondrial volume strongly correlated with sarcoplasm volume in both, supporting the conclusion that sarcoplasm volume governs mitochondrial volume.
3. Discussion
In this study, we investigated how pathogenic mtDNA mutations affect mitochondrial morphology and membrane potential in mesoangioblast-derived myotubes, and examined the behavior of mitochondria following fusion with healthy mesoangioblasts. By using a combination of live-cell imaging and FISH techniques, we were able to track and analyze specific myotubes that had fused with healthy mesoangioblasts. We first studied mitochondrial morphology and membrane potential of mesoangioblast-derived myotubes of M02 with 96% m.3271T>C and M11 with 73% m.3291T>C and M06 with 3% m.3243A>G as a healthy control. The results from this study showed that mitochondrial morphology (total mitochondrial volume and number of individual mitochondrial objects) and membrane potential were similar across myotubes derived from both high mtDNA mutation load (M02, M11) and healthy control (M06) mesoangioblasts when normalized to sarcoplasm size. Normalization to sarcoplasm size was necessary for valid comparisons across cell cultures, as sarcoplasm volume correlated with the number of nuclei and as we compared myotubes with varying nuclear content. After correction, no statistically significant differences in mitochondrial volume, membrane potential, or mitochondrial object number were observed between the groups. Although M02 myotubes had a lower nucleus count compared to M11 and M06, this did not translate into differences in mitochondrial parameters after normalization. These findings indicate that, despite the presence of pathogenic mtDNA mutations at levels exceeding 70%, the baseline mitochondrial characteristics of in vitro differentiated myotubes do not differ from those of healthy controls.
Baseline differences were expected because morphological and biochemical abnormalities were reported for both mutations. The m.3271T>C mutation in MT-TL1, encoding mitochondrial tRNA^Leu(UUR), typically impairs mitochondrial translation and complex I activity, often reflecting reduced membrane potential and abnormal cristae in sensitive cell types when heteroplasmy exceeds ~70% [
9]. Similarly, m.3291T>C, also affecting MT-TL1, impairs translation of subunits of the mitochondrial respiratory chain complexes, particularly complex I, III, and IV [
10]. This causes complex I and III deficiencies, morphological abnormalities, and a decrease in membrane potential. In our study, despite >80% mutation load, we did not observe any change in mitochondrial morphology and membrane potential. Several factors may explain the absence of detectable differences. First, analysis at the level of individual hybrid myotubes necessitated the use of imaging-based approaches. Mitochondrial membrane potential was therefore assessed using TMRM as a functional readout linked to ATP production. Other mitochondrial functional assays would be informative but are not technically feasible in individual myotubes or cannot be performed on the same cell. Second, the choice for the spinning disk confocal microscopy was dictated by the need to image in living cells without any photodamage. However, as a drawback, this imaging approach is not sensitive enough to identify subtle subcellular structural changes in mitochondrial cristae architecture. This is supported by Stephan et al. [
11] and Ren et al. [
12], who demonstrated that super-resolution microscopy (e.g., STED nanoscopy) is required to visualize fine cristae changes in mitochondria. Therefore, we could only look at more general characteristics such as volume, number of mitochondrial objects, and mitochondrial membrane potential. Third, the timing of measurements (day 11 of differentiation) may be too early to observe pronounced mitochondrial dysfunction, which often becomes evident under prolonged differentiation or metabolic stress [
13]. Myotubes at this stage may not have reached full contractile or metabolic maturity. Immature myotubes often lack organized sarcomeres and exhibit limited contraction activity, which reduces their energetic demand [
14]. As mitochondrial membrane potential is closely tied to ATP turnover, this reduced metabolic activity may contribute to the absence of detectable depolarization despite high mutation load. Fourth, the culture conditions, specifically usage of high glucose medium, might introduce insufficient metabolic stressors, such as nutrient deprivation or high energy demand, which are known to unmask mitochondrial defects in high-heteroplasmy models [
15,
16]. As no mitochondrial abnormalities were observed, we could not test if the fusion would lead to the expected improvement of mitochondrial function. However, still a number of interesting observations were made.
First, we showed that fusion of control mM06 mesoangioblasts with mutant myotubes did not have a negative effect on myotube formation, as MFI did not significantly differ between non-hybrid and hybrid conditions of M02 or M11 cell cultures. Secondly, changes in mitochondrial volume and membrane potential of hybrid myotubes were observed. M02+mM06 hybrid myotubes displayed a significant increase with respect to all analyzed mitochondrial parameters and increased sarcoplasm volume. When calculating mitochondrial volume per nucleus, a significant increase of 1.15-fold is observed, while no significant change is observed when calculating mitochondrial volume per sarcoplasm volume, indicating that mitochondrial volume is controlled by the sarcoplasm volume. In line with this, in [
17], resistance training was found to result in a reduction in both mitochondrial volume as well as sarcoplasmic volume in biceps brachii muscle of previously untrained individuals. The increases in mitochondrial parameters observed in M02+mM06 hybrids were not observed in M11+mM06 hybrid myotubes. This can likely be explained by the cell size, as non-hybrid M06 myotubes are substantially bigger (~17%) with respect to sarcoplasm volume and mitochondrial volume per nucleus compared to M02, while being similar to M11. Fusion of mM06 to M11 rather resulted in a proportional reduction in mitochondrial volume and membrane potential when corrected for myotube nuclei number. This is likely the consequence of different maturation stages, as M11 was differentiated for 11 days, while mM06 was added on day 5 and only had the opportunity to differentiate for a maximum of 6 days. To verify this, longer myogenic differentiation is required, which is not feasible in 2d culture, but could be achieved using 3d tissue-engineered myogenic culture [
18]. Taken together, our data demonstrated a strong relation between mitochondrial content and sarcoplasm volume, which should be taken into consideration when analyzing mitochondrial parameters.
Thirdly, after fusing mM06 mesoangioblasts with M11 myotubes, the number of mitochondrial objects per nucleus is reduced, while the total number of mitochondrial objects per myotube is not changed compared to M11, indicating integration and formation of bigger mitochondrial networks. In line with this, the number of mitochondrial objects per myotube nucleus is unchanged in M02+mM06 hybrid myotubes, despite a 1.15-fold increase in mitochondrial volume per nucleus. This data suggests fusion of the mM06-derived mitochondria with M11/M02 mitochondria, which is obviously something we would like to achieve in our therapy. Our prior work with Zelissen et al. demonstrated a proportional reduction in mtDNA mutation load after fusion [
7] and the current data suggest that this is a fusion with existing mitochondria and not an addition of healthy ones. This is consistent with previous studies demonstrating that mitochondria fuse following cell–cell fusion or nanotube-mediated mitochondrial transfer, with the resulting mitochondrial population being stably propagated [
19,
20].
4. Methods and Material
4.1. Cell Culture
Mesoangioblast isolation and culture were performed as described before [
5]. Mesoangioblasts were cultured between passage number 4 and 15 in a 37 °C humidified incubator in 4% O
2 and 5% CO
2, using IMDM medium supplemented with 10% fetal bovine serum (Bodinco, Alkmaar, The Netherlands), 1× glutamine, 1× sodium-pyruvate, 1× non-essential amino acids, 1× insulin transferase selenium X, 0.2% 2-mercaptoethanol, 5 ng/mL FGF2 (Miltenyi Biotec, Teterow, Germany), and 0.1% gentamycin. To allow later spinning disk confocal microscopy of myotubes, mesoangioblasts (25,000 cells/cm
2) were subsequently seeded on a 1:27 dilution of Matrigel (hESC-qualified Matrix (5 mL LDEV-free))-coated 4-well microscopy µ-slides (Ibidi). All three mesoangioblast cultures were subsequently differentiated to myotubes by allowing them to reach 100% confluence and at day 0 replacing mesangioblast growth medium with myogenic differentiation medium, which consists of DMEM containing 2% horse serum. At day 5 after starting myogenic differentiation, mesoangioblasts (20,000 cell/cm
2) from the healthy male control, (mM06), resuspended in DMEM 2% horse serum were added to initiate fusion of these cells with the M02/M11 forming myotubes. At day 11, cells were stained with 200 nM tetramethyl rhodamine methyl ester (mitochondria, red, TMRM), 2 μM Calcein AM (cell cytoplasm, green), and 2 μM Hoechst 34580 (Cell nuclei, blue) in medium for 30 min at 37 °C and 5% CO
2. After incubation, medium was replaced with fresh differentiation medium and live imaging was performed using spinning disk confocal microscope as described below. All materials in this study were purchased from ThermoFisher Scientific (Waltham, MA, USA) unless stated otherwise.
4.2. Confocal Imaging of Mesoangioblasts and Myotubes and Image Analysis
Myotubes were imaged using CorrSight SDCM using a Zeiss 63× oil immersion (White Plains, NY, USA) with numerical aperture (NA) 1.3. Myotubes were imaged using a 20× air objective (Waltham, MA, USA) with NA 0.9. The microscope was equipped with an Andromeda spinning disk module, and a Hamamatsu ORCA-Flash 4.0 V2 camera (Hamamatsu, Japan) with a laser light source that emits at different wavelengths of 405, 488, 561, and 640 nm. Excitation at 561 nm was used for acquiring images for mitochondria stained with TMRM (red), excitation at 488 was used to image the cytoplasm stained with Calcein–AM (green), and excitation at 405 nm was used to image the nuclei stained with Hoechst 34580 (blue). Emission filters FF01 593/46-25, FF01 523/30-25, and FF01 446 nm were used, respectively. Live-cell imaging of mesoangioblasts and myotubes was carried out inside a 37 °C and 5% CO2 controlled chamber (Ibidi). For live-cell imaging of myotubes, 150 Z-stacks were acquired. All images were deconvoluted using Huygens Professional version 21.10 (SVI) using the Classic Maximum Likelihood Estimation algorithm with a signal-to-noise ratio of 7.0, maximum iterations of 40, and quality threshold of 0.001.
4.3. FISH and Imaging of Fixed Samples
To identify male control mesoangioblast (mM06) nuclei in myotubes of female myotubes (M02/m11), FISH staining of Y-chromosome was used. Immediately after live-cell imaging of the myotubes, cells were fixed in 4% formaldehyde in PBS for 5 min, then permeabilized in 0.2% Triton X-100 in PBS for 30 min, dehydrated with 70, 96, 100% Ethanol. Subsequently, 5 ng/µL of the Y-chromosome probe (DYZ3 probe: targets Y-chromosome centromeric DNA [
21]) conjugated to Y-ATTO 550 dissolved in 10% dextran sulfate and 60% formamide and 2XSSC (1 xSSC is 0.15 M NaCl, 0.015 M sodium citrate, pH 7.0) was added to each well of the plate. The plate was placed for 10 min on a preheated hotplate at 80 °C, after which in situ hybridization was allowed overnight in 37 °C incubator, followed by PBS washes and 1 µg/mL DAPI staining on the following day. Using the DAPI and Y-ATTO 550 channels, the same field of views of the fixed samples were imaged using SDCM and the previously recorded live images of myotubes were overlayed. The distinction between hybrid (M02+mM06, M11+mM06) and non-hybrid (M02, M11) myotubes could now be made based on the presence of the stained Y-chromosomes in the overlay images.
4.4. Analysis
Analysis of the mitochondrial network was performed manually on the segmented images of the fused myotubes using a script in Matlab R2021a (The Mathworks, Inc.) with additional DipImage toolbox (TU Delft) developed previously in our group, which was adopted from Koopman group [
22]. Deconvoluted images were filtered both with Median 3D filter and top-hat and masked using thresholding at a constant value as described in [
8,
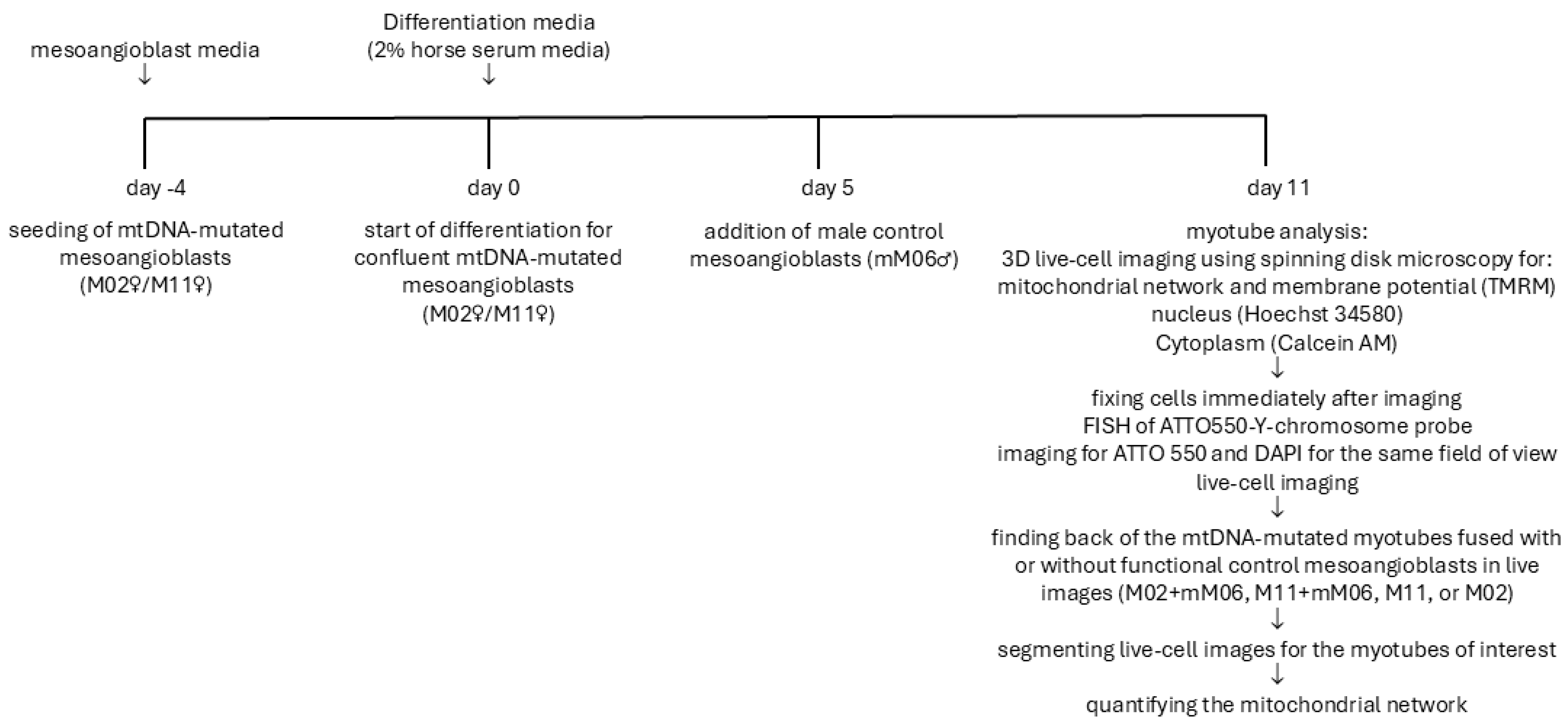
22]. Cytoplasm volume was calculated by subtracting the hole-filled nuclear volume using the Hoechst staining from the hole-filled cell volume defined by Calcein AM staining. The full schematic representation of the study design is presented in
Figure 5 and presents a schematic representation of the experimental workflow. It outlines the differentiation of mesoangioblasts into myotubes, the fusion of male control mesoangioblasts with both control and mtDNA-mutant myotubes, live imaging for mitochondrial morphology and membrane potential, and FISH analysis to distinguish hybrid from non-hybrid myotubes.
Supplementary Figure S1 illustrates the process of identifying fused control mesoangioblasts within mutated myotubes. Live-cell imaging visualized mitochondrial networks (TMRM), nuclei (Hoechst), and cytoplasm (Calcein AM). FISH using a Y-chromosome-specific probe confirmed fusion by detecting male nuclei within female-origin myotubes. Segmentation of live images allowed classification of mitochondrial structures and membrane potential. Mitochondria in fused myotubes were segmented and color-coded to represent discrete objects, and TMRM intensity maps provided qualitative assessment of membrane potential.
4.5. Myotube Fusion Index
The Myotube Fusion Index (MFI) represents the proportion of nuclei incorporated into multinucleated myotubes compared to the total nuclear count within an observed microscopic field. This metric is expressed as a percentage, calculated by dividing the count of nuclei found within myotubes by the total number of nuclei present in the field of view and multiplied by 100%.
4.6. Statistical Analysis
All data were initially checked for normality using the D’Agostino and Pearson test. Once normality was confirmed, comparisons among three groups were conducted using ordinary one-way ANOVA. To identify specific differences between groups, Tukey’s multiple comparisons test was applied as a post hoc analysis. For comparisons between two groups, an unpaired t-test was used. Analysis was performed by GraphPad Prism 8.4.