Reduced Expression of SATB2 in Colorectal Cancer and Its Association with Demographic and Clinicopathological Parameters
Abstract
1. Introduction
2. Results
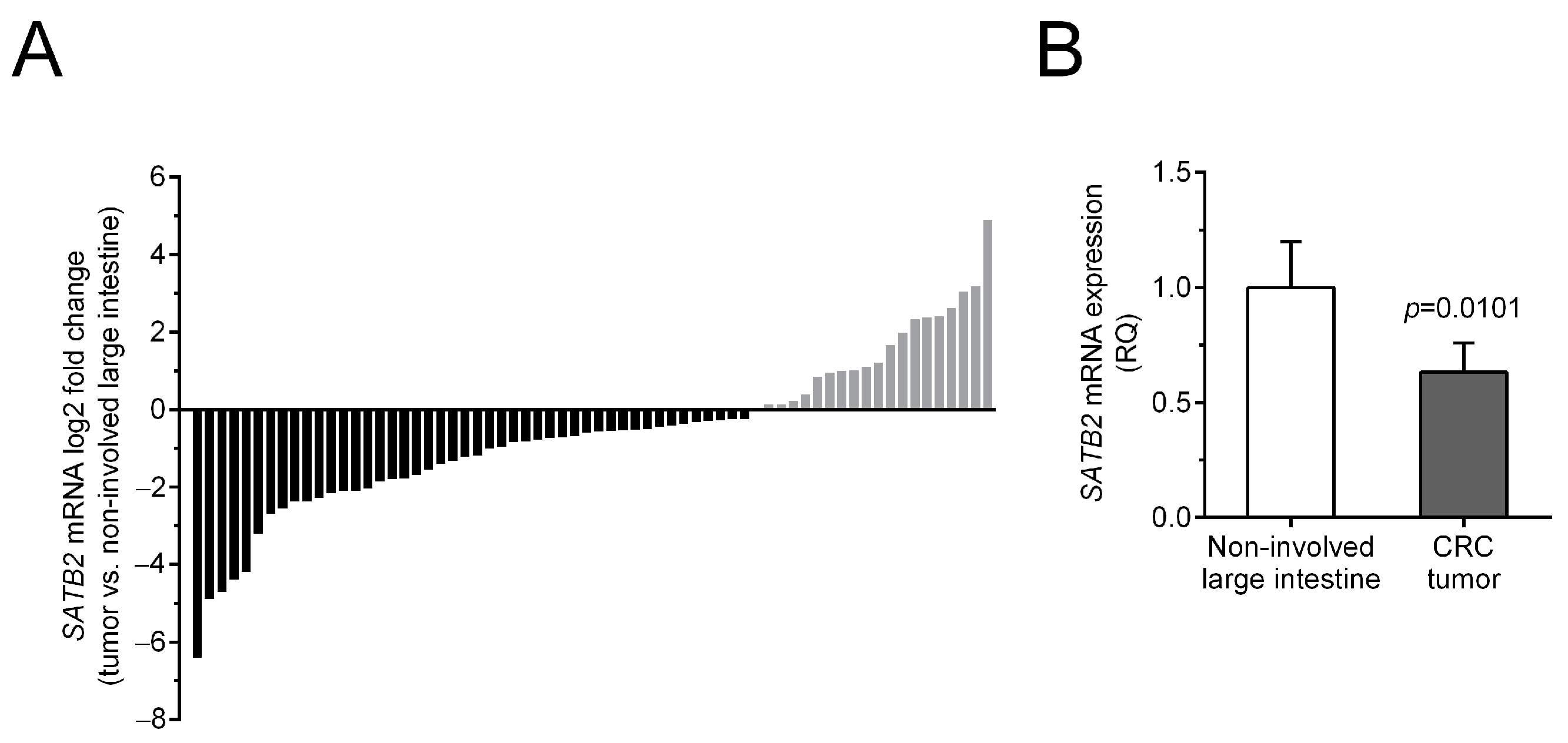
2.1. Reduced SATB2 mRNA Levels in CRC Tissues
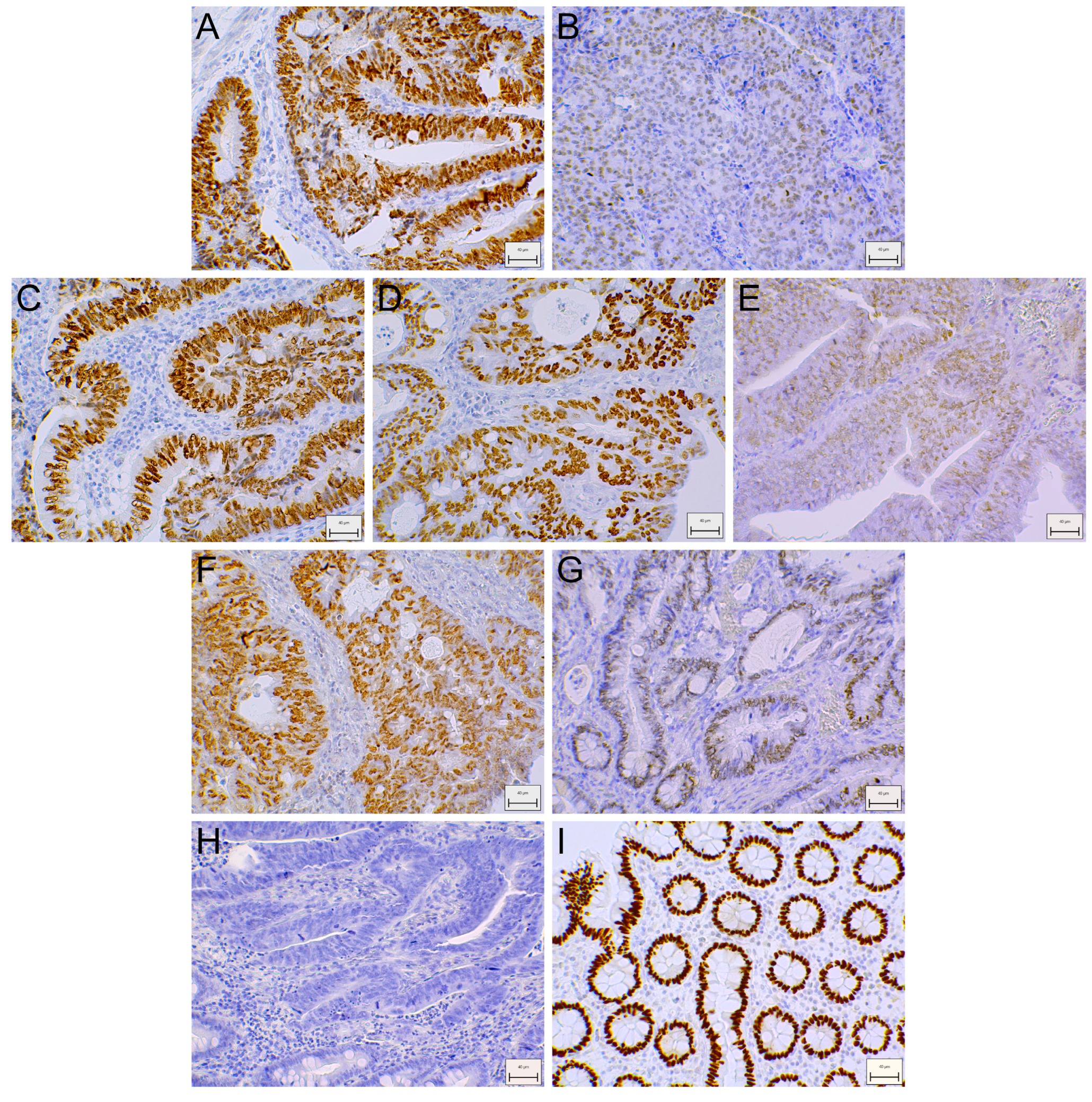
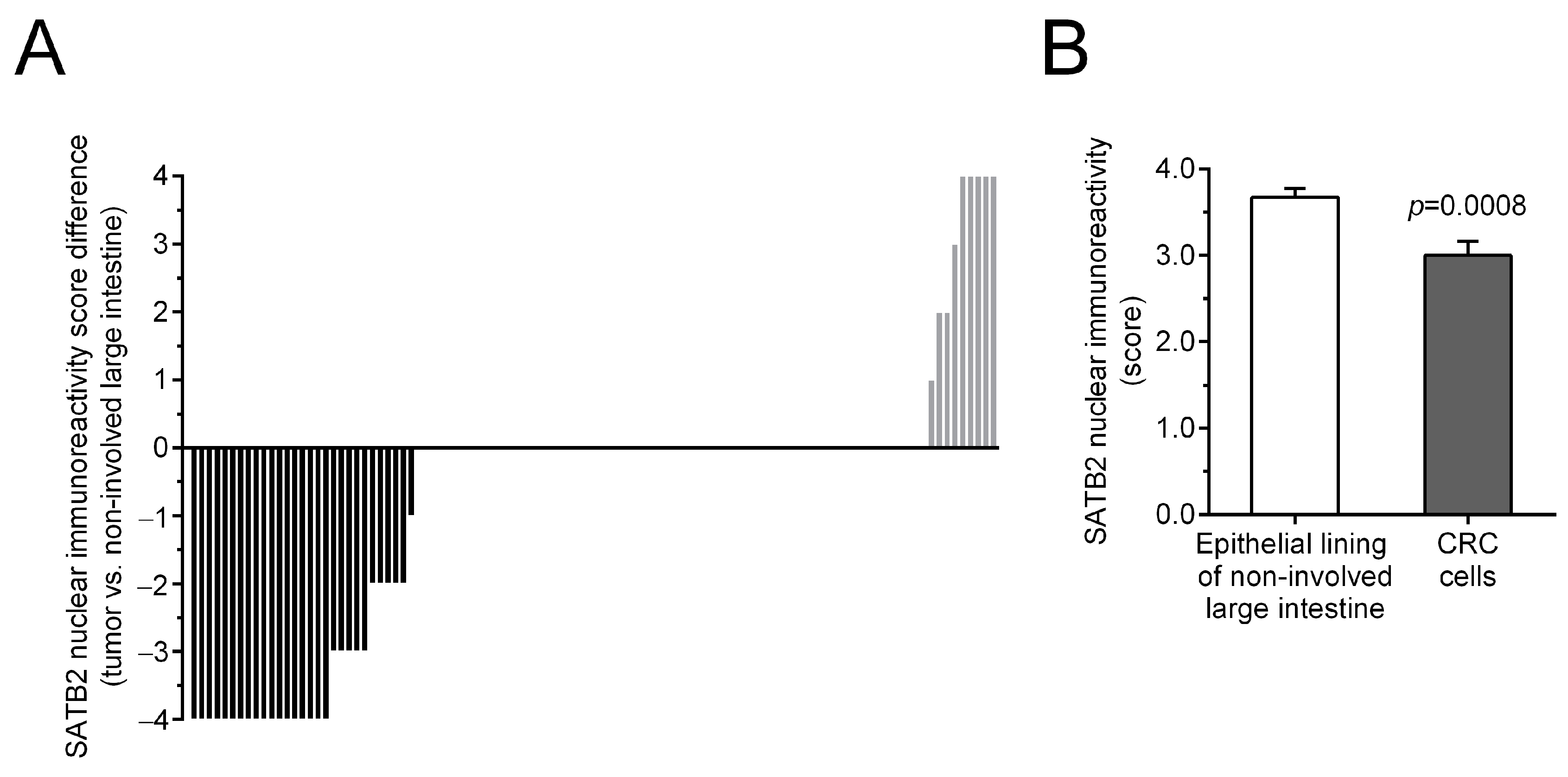
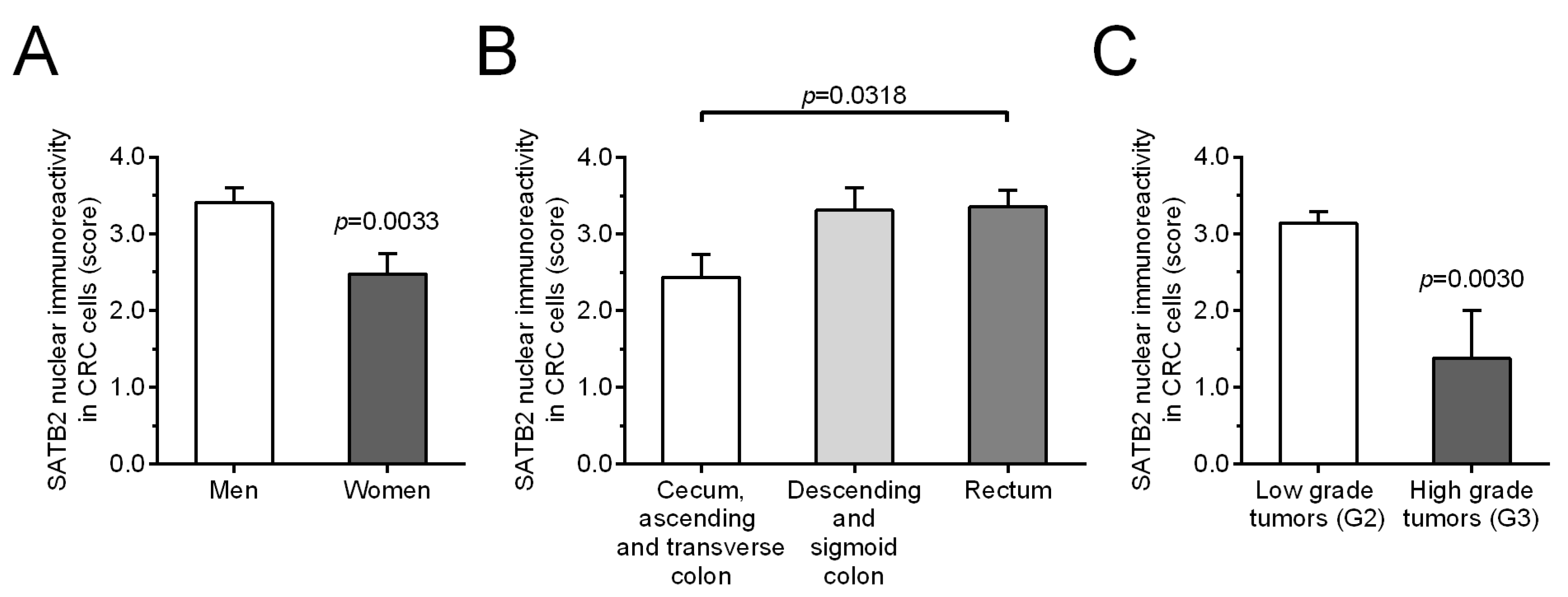
2.2. Downregulated SATB2 Immunoreactivity (SATB2-Ir) in CRC Tissues and Its Association with Sex, Tumor Localization, and Histological Grade
2.3. No Association of SATB2 mRNA and Protein Levels with Overall Survival of CRC Patients
3. Discussion
4. Materials and Methods
4.1. Patients and Tissue Sample Collection
4.2. Total RNA Isolation, Reverse Transcription, and QPCR
4.3. Immunohistochemistry and Staining Evaluation
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SATB2 | Special AT-rich sequence-binding protein 2 |
| CRC | Colorectal cancer |
| qPCR | Quantitative polymerase chain reaction |
| IHC | Immunohistochemical |
| HCC | Hepatocellular carcinoma |
| HNSCC | Head and neck squamous cell carcinoma |
| EMT | Epithelial-mesenchymal transition |
| OS | Overall survival |
| SATB2-Ir | SATB2-immunoreactivity |
| RQ | Relative quantification |
| HR | Hazard ratio |
| CI | Confidence interval |
| MANECs/NECs | Mixed adenoneuroendocrine carcinomas/neuroendocrine carcinomas |
| lncRNA SATB2-AS1 | Long non-coding RNA antisense transcript of SATB2 |
| TMA | Tissue microarray |
| miRs | MicroRNAs |
| MSI | Microsatellite instability |
| KRAS | Kirsten rat sarcoma virus |
| ACTB | β-actin |
| HPRT1 | Hypoxanthine phosphoribosyltransferase 1 |
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef]
- Rawla, P.; Sunkara, T.; Barsouk, A. Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Gastroenterol. Rev. 2019, 14, 89–103. [Google Scholar] [CrossRef] [PubMed]
- Ewing, I.; Hurley, J.J.; Josephides, E.; Millar, A. The molecular genetics of colorectal cancer. Frontline Gastroenterol. 2014, 5, 26–30. [Google Scholar] [CrossRef]
- Huang, X.; Chen, Q.; Luo, W.; Pakvasa, M.; Zhang, Y.; Zheng, L.; Li, S.; Yang, Z.; Zeng, H.; Liang, F.; et al. SATB2: A versatile transcriptional regulator of craniofacial and skeleton development, neurogenesis and tumorigenesis, and its applications in regenerative medicine. Genes Dis. 2020, 9, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Dum, D.; Kromm, D.; Lennartz, M.; De Wispelaere, N.; Büscheck, F.; Luebke, A.M.; Burandt, E.; Menz, A.; Kluth, M.; Hube-Magg, C.; et al. SATB2 Expression in Human Tumors: A Tissue Microarray Study on More Than 15 000 Tumors. Arch. Pathol. Lab. Med. 2023, 147, 451–464. [Google Scholar] [CrossRef]
- Dobreva, G.; Dambacher, J.; Grosschedl, R. SUMO modification of a novel MAR-binding protein, SATB2, modulates immunoglobulin mu gene expression. Genes Dev. 2003, 17, 3048–3061. [Google Scholar] [CrossRef] [PubMed]
- Seong, B.K.; Lau, J.; Adderley, T.; Kee, L.; Chaukos, D.; Pienkowska, M.; Malkin, D.; Thorner, P.; Irwin, M.S. SATB2 enhances migration and invasion in osteosarcoma by regulating genes involved in cytoskeletal organization. Oncogene 2015, 34, 3582–3592. [Google Scholar] [CrossRef]
- Xu, H.Y.; Fang, W.; Huang, Z.W.; Lu, J.C.; Wang, Y.Q.; Tang, Q.L.; Song, G.H.; Kang, Y.; Zhu, X.J.; Zou, C.Y.; et al. Metformin reduces SATB2-mediated osteosarcoma stem cell-like phenotype and tumor growth via inhibition of N-cadherin/NF-kB signaling. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 4516–4528. [Google Scholar]
- Yu, W.; Roy, S.K.; Ma, Y.; LaVeist, T.A.; Shankar, S.; Srivastava, R.K. Higher expression of SATB2 in hepatocellular carcinoma of African Americans determines more aggressive phenotypes than those of Caucasian Americans. J. Cell. Mol. Med. 2019, 23, 7999–8009. [Google Scholar] [CrossRef]
- Jiang, G.; Cui, Y.; Yu, X.; Wu, Z.; Ding, G.; Cao, L. miR-211 suppresses hepatocellular carcinoma by downregulating SATB2. Oncotarget 2015, 6, 9457–9466. [Google Scholar] [CrossRef]
- Patani, N.; Jiang, W.; Mansel, R.; Newbold, R.; Mokbel, K. The mRNA expression of SATB1 and SATB2 in human breast cancer. Cancer Cell Int. 2009, 9, 18. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Ma, Y.; Ochoa, A.C.; Shankar, S.; Srivastava, R.K. Cellular transformation of human mammary epithelial cells by SATB2. Stem Cell Res. 2017, 19, 139–147. [Google Scholar] [CrossRef]
- Chung, J.; Lau, J.; Cheng, L.S.; Grant, R.I.; Robinson, F.; Ketela, T.; Reis, P.P.; Roche, O.; Kamel-Reid, S.; Moffat, J.; et al. SATB2 augments ΔNp63α in head and neck squamous cell carcinoma. EMBO Rep. 2010, 11, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.R.; Xu, L.H.; Yang, A.K.; Zhong, Q.; Song, M.; Li, M.Z.; Hu, L.J.; Chen, F.J.; Hu, Z.D.; Han, P.; et al. Decreased expression of SATB2: A novel independent prognostic marker of worse outcome in laryngeal carcinoma patients. PLoS ONE 2012, 7, e40704. [Google Scholar] [CrossRef] [PubMed]
- Geng, G.J.; Li, N.; Mi, Y.J.; Yu, X.Y.; Luo, X.Y.; Gao, J.; Luo, Q.C.; Xie, J.D.; Fa, X.E.; Jiang, J. Prognostic value of SATB2 expression in patients with esophageal squamous cell carcinoma. Int. J. Clin. Exp. Pathol. 2015, 8, 423–431. [Google Scholar]
- Kucuksayan, H.; Ozes, O.N.; Akca, H. Downregulation of SATB2 is critical for induction of epithelial-to-mesenchymal transition and invasion of NSCLC cells. Lung Cancer 2016, 98, 122–129. [Google Scholar] [CrossRef]
- Le Page, C.; Köbel, M.; Meunier, L.; Provencher, D.M.; Mes-Masson, A.M.; Rahimi, K. A COEUR cohort study of SATB2 expression and its prognostic value in ovarian endometrioid carcinoma. J. Pathol. Clin. Res. 2019, 5, 177–188. [Google Scholar] [CrossRef]
- Sliwinska-Jewsiewicka, A.; Kowalczyk, A.E.; Krazinski, B.E.; Godlewski, J.; Kwiatkowski, P.; Kiewisz, J.; Grzegrzolka, J.; Dziegiel, P.; Kmiec, Z. Decreased Expression of SATB2 Associates with Tumor Growth and Predicts Worse Outcome in Patients with Clear Cell Renal Cell Carcinoma. Anticancer Res. 2018, 38, 839–846. [Google Scholar] [CrossRef]
- Yu, W.; Ma, Y.; Shankar, S.; Srivastava, R.K. SATB2/β-catenin/TCF-LEF pathway induces cellular transformation by generating cancer stem cells in colorectal cancer. Sci. Rep. 2017, 7, 10939. [Google Scholar] [CrossRef]
- Sun, X.; Liu, S.; Chen, P.; Fu, D.; Hou, Y.; Hu, J.; Liu, Z.; Jiang, Y.; Cao, X.; Cheng, C.; et al. miR-449a inhibits colorectal cancer progression by targeting SATB2. Oncotarget 2016, 8, 100975–100988. [Google Scholar] [CrossRef]
- Yang, D.; Li, R.; Xia, J.; Li, W.; Zhou, H. miR-3666 suppresses cellular proliferation and invasion in colorectal cancer by targeting SATB2. Mol. Med. Rep. 2018, 18, 4847–4854. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhou, J.; Wang, X.Y.; Hao, J.M.; Chen, J.Z.; Zhang, X.M.; Jin, H.; Liu, L.; Zhang, Y.F.; Liu, J.; et al. Down-regulated expression of SATB2 is associated with metastasis and poor prognosis in colorectal cancer. J. Pathol. 2009, 219, 114–122. [Google Scholar] [CrossRef]
- Eberhard, J.; Gaber, A.; Wangefjord, S.; Nodin, B.; Uhlén, M.; Ericson Lindquist, K.; Jirström, K. A cohort study of the prognostic and treatment predictive value of SATB2 expression in colorectal cancer. Br. J. Cancer 2012, 106, 931–938. [Google Scholar] [CrossRef]
- Gu, J.; Wang, G.; Liu, H.; Xiong, C. SATB2 targeted by methylated miR-34c-5p suppresses proliferation and metastasis attenuating the epithelial-mesenchymal transition in colorectal cancer. Cell Prolif. 2018, 51, e12455. [Google Scholar] [CrossRef] [PubMed]
- Mansour, M.A.; Hyodo, T.; Ito, S.; Kurita, K.; Kokuryo, T.; Uehara, K.; Nagino, M.; Takahashi, M.; Hamaguchi, M.; Senga, T. SATB2 suppresses the progression of colorectal cancer cells via inactivation of MEK5/ERK5 signaling. FEBS J. 2015, 282, 1394–1405. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, Y.H.; Hu, Y.Y.; Chen, L.; Li, J.M. Special AT-rich sequence-binding protein 2 acts as a negative regulator of stemness in colorectal cancer cells. World J. Gastroenterol. 2016, 22, 8528–8539. [Google Scholar] [CrossRef]
- Mansour, M.A.; Hyodo, T.; Akter, K.A.; Kokuryo, T.; Uehara, K.; Nagino, M.; Senga, T. SATB1 and SATB2 play opposing roles in c-Myc expression and progression of colorectal cancer. Oncotarget 2016, 7, 4993–5006. [Google Scholar] [CrossRef][Green Version]
- Hrudka, J.; Matěj, R.; Nikov, A.; Tomyak, I.; Fišerová, H.; Jelínková, K.; Waldauf, P. Loss of SATB2 expression correlates with cytokeratin 7 and PD-L1 tumor cell positivity and aggressiveness in colorectal cancer. Sci. Rep. 2022, 12, 19152. [Google Scholar] [CrossRef]
- Mezheyeuski, A.; Ponten, F.; Edqvist, P.H.; Sundström, M.; Thunberg, U.; Qvortrup, C.; Pfeiffer, P.; Sorbye, H.; Glimelius, B.; Dragomir, A. Metastatic colorectal carcinomas with high SATB2 expression are associated with better prognosis and response to chemotherapy: A population-based Scandinavian study. Acta Oncol. 2020, 59, 284–290. [Google Scholar] [CrossRef]
- Li, J.; Zeng, Q.; Lin, J.; Huang, H.; Chen, L. Loss of SATB2 and CDX2 expression is associated with DNA mismatch repair protein deficiency and BRAF mutation in colorectal cancer. Med. Mol. Morphol. 2024, 57, 1–10. [Google Scholar] [CrossRef]
- Ma, C.; Olevian, D.; Miller, C.; Herbst, C.; Jayachandran, P.; Kozak, M.M.; Chang, D.T.; Pai, R.K. SATB2 and CDX2 are prognostic biomarkers in DNA mismatch repair protein deficient colon cancer. Mod. Pathol. 2019, 32, 1217–1231. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, M.; Silva, M.; Konukiewitz, B.; Lang, C.; Steiger, K.; Halfter, K.; Engel, J.; Jank, P.; Pfarr, N.; Wilhelm, D.; et al. Loss of SATB2 Occurs More Frequently Than CDX2 Loss in Colorectal Carcinoma and Identifies Particularly Aggressive Cancers in High-Risk Subgroups. Cancers 2021, 13, 6177. [Google Scholar] [CrossRef]
- Cígerová, V.; Adamkov, M.; Drahošová, S.; Grendár, M. Immunohistochemical expression and significance of SATB2 protein in colorectal cancer. Ann. Diagn. Pathol. 2021, 52, 151731. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Sierra, M.S.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017, 66, 683–691. [Google Scholar] [CrossRef]
- Pradhan, S.J.; Reddy, P.C.; Smutny, M.; Sharma, A.; Sako, K.; Oak, M.S.; Shah, R.; Pal, M.; Deshpande, O.; Dsilva, G.; et al. Satb2 acts as a gatekeeper for major developmental transitions during early vertebrate embryogenesis. Nat. Commun. 2021, 12, 6094. [Google Scholar] [CrossRef]
- Uhlén, M.; Fagerberg, L.; Hallström, B.M.; Lindskog, C.; Oksvold, P.; Mardinoglu, A.; Sivertsson, Å.; Kampf, C.; Sjöstedt, E.; Asplund, A.; et al. Proteomics. Tissue-based map of the human proteome. Science 2015, 347, 1260419. [Google Scholar] [CrossRef]
- Magnusson, K.; de Wit, M.; Brennan, D.J.; Johnson, L.B.; McGee, S.F.; Lundberg, E.; Naicker, K.; Klinger, R.; Kampf, C.; Asplund, A.; et al. SATB2 in combination with cytokeratin 20 identifies over 95% of all colorectal carcinomas. Am. J. Surg. Pathol. 2011, 35, 937–948. [Google Scholar] [CrossRef] [PubMed]
- Brocato, J.; Costa, M. SATB1 and 2 in colorectal cancer. Carcinogenesis 2015, 36, 186–191. [Google Scholar] [CrossRef]
- Dragomir, A.; de Wit, M.; Johansson, C.; Uhlen, M.; Pontén, F. The role of SATB2 as a diagnostic marker for tumors of colorectal origin: Results of a pathology-based clinical prospective study. Am. J. Clin. Pathol. 2014, 141, 630–638. [Google Scholar] [CrossRef]
- Lin, F.; Shi, J.; Zhu, S.; Chen, Z.; Li, A.; Chen, T.; Wang, H.L.; Liu, H. Cadherin-17 and SATB2 are sensitive and specific immunomarkers for medullary carcinoma of the large intestine. Arch. Pathol. Lab. Med. 2014, 138, 1015–1026. [Google Scholar] [CrossRef]
- Maguire, B.; Duggan, W.P.; Prehn, J.H.M.; Burke, J.P. Meta-analysis of SATB2 immunohistochemical expression in colorectal cancer versus primary ovarian mucinous neoplasms. Ann. Diagn. Pathol. 2024, 71, 152302. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Koshino, A.; Lasota, J.; Komura, M.; Wang, C.; Ebi, M.; Ogasawara, N.; Kojima, K.; Tsuzuki, T.; Kasai, K.; et al. Use of SATB2 and CDX2 Immunohistochemistry to Characterize and Diagnose Colorectal Cancer. Appl. Immunohistochem. Mol. Morphol. 2024, 32, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Berg, K.B.; Schaeffer, D.F. SATB2 as an Immunohistochemical Marker for Colorectal Adenocarcinoma: A Concise Review of Benefits and Pitfalls. Arch. Pathol. Lab. Med. 2017, 141, 1428–1433. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Sun, L.; Zhang, L.; Zhou, L.; Niu, D.; Cao, W.; Li, Z.; Huang, X.; Kang, Q.; Jia, L.; et al. SATB2 Shows Different Profiles Between Appendiceal Adenocarcinomas Ex Goblet Cell Carcinoids and Appendiceal/Colorectal Conventional Adenocarcinomas: An Immunohistochemical Study With Comparison to CDX2. Gastroenterol. Res. 2018, 11, 221–230. [Google Scholar] [CrossRef]
- Kim, C.J.; Baruch-Oren, T.; Lin, F.; Fan, X.S.; Yang, X.J.; Wang, H.L. Value of SATB2 immunostaining in the distinction between small intestinal and colorectal adenocarcinomas. J. Clin. Pathol. 2016, 69, 1046–1050. [Google Scholar] [CrossRef]
- Elnady, M.S.; Eltatawy, F.A.; Nosseir, A.G.; Zamzam, Y.A.; El-Guindya, D.M. Diagnostic accuracy of SATB2 in identifying primary and metastatic colorectal carcinoma: A comparative immunohistochemical study. Ecancermedicalscience 2022, 16, 1491. [Google Scholar] [CrossRef]
- Liu, F.; Gao, Z.; Shen, D.; Zhao, H.; Wang, C.; Ye, Y.; Ma, Y.; Kong, F. Significance of SATB2 expression in colon cancer and its differential diagnosis in digestive tract adenocarcinoma and ovarian primary and metastatic carcinoma. Pathol. Res. Pract. 2019, 215, 152430. [Google Scholar] [CrossRef]
- Yang, M.H.; Yu, J.; Chen, N.; Wang, X.Y.; Liu, X.Y.; Wang, S.; Ding, Y.Q. Elevated microRNA-31 expression regulates colorectal cancer progression by repressing its target gene SATB2. PLoS ONE 2013, 8, e85353. [Google Scholar] [CrossRef]
- Yang, M.H.; Yu, J.; Jiang, D.M.; Li, W.L.; Wang, S.; Ding, Y.Q. microRNA-182 targets special AT-rich sequence-binding protein 2 to promote colorectal cancer proliferation and metastasis. J. Transl. Med. 2014, 12, 109. [Google Scholar] [CrossRef]
- Clancy, H.A.; Sun, H.; Passantino, L.; Kluz, T.; Muñoz, A.; Zavadil, J.; Costa, M. Gene expression changes in human lung cells exposed to arsenic, chromium, nickel or vanadium indicate the first steps in cancer. Metallomics 2012, 4, 784–793. [Google Scholar] [CrossRef]
- Eldeeb, S.A.; Salem, M.M.; Morsi, D.F.; Soliman, N.A. Immunohistochemical expression of SATB2 and clinicopathological correlation in colorectal adenocarcinoma. Merit Res. J. Med. Med. Sci. 2022, 10, 115–124. [Google Scholar] [CrossRef]
- Dekker, E.; Tanis, P.J.; Vleugels, J.L.A.; Kasi, P.M.; Wallace, M.B. Colorectal cancer. Lancet 2019, 394, 1467–1480. [Google Scholar] [CrossRef] [PubMed]
- Kowalczyk, A.E.; Krazinski, B.E.; Godlewski, J.; Kiewisz, J.; Kwiatkowski, P.; Sliwinska-Jewsiewicka, A.; Kiezun, J.; Wierzbicki, P.M.; Bodek, G.; Sulik, M.; et al. Altered expression of the PLAGL1 (ZAC1/LOT1) gene in colorectal cancer: Correlations to the clinicopathological parameters. Int. J. Oncol. 2015, 47, 951–962. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kowalczyk, A.E.; Godlewski, J.; Krazinski, B.E.; Kiewisz, J.; Sliwinska-Jewsiewicka, A.; Kwiatkowski, P.; Pula, B.; Dziegiel, P.; Janiszewski, J.; Wierzbicki, P.M.; et al. Divergent expression patterns of SATB1 mRNA and SATB1 protein in colorectal cancer and normal tissues. Tumour Biol. 2015, 36, 4441–4452. [Google Scholar] [CrossRef][Green Version]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]

| SATB2 mRNA RQ (CRC vs. Non-Involved Colon Tissue) | ||||
|---|---|---|---|---|
| Parameters | Number of Cases | RQ < 1 n (%) | RQ > 1 n (%) | p-Value a |
| Total | 66 | 46 (69.7) | 20 (30.3) | |
| Sex | ||||
| Men | 34 | 24 (70.6) | 10 (29.4) | 1.0000 |
| Women | 32 | 22 (68.7) | 10 (31.3) | |
| Localization | ||||
| Cecum, ascending and transverse colon | 24 | 20 (83.3) | 4 (16.7) | 0.1892 |
| Descending and sigmoid colon | 18 | 11 (61.1) | 7 (38.9) | |
| Rectum | 24 | 15 (62.5) | 9 (37.5) | |
| Grade of differentiation (G) | ||||
| G2 | 60 | 41 (68.3) | 19 (31.7) | 0.6588 |
| G3 | 6 | 5 (83.3) | 1 (16.7) | |
| Depth of invasion (T status) | ||||
| T1 + T2 | 9 | 8 (88.9) | 1 (11.1) | 0.2573 |
| T3 + T4 | 57 | 38 (66.7) | 19 (33.3) | |
| Lymph node metastasis (N status) | ||||
| N0 | 35 | 27 (77.1) | 8 (22.9) | 0.1292 |
| N1 + N2 | 31 | 19 (61.3) | 12 (38.7) | |
| Distant metastasis (M status) | ||||
| M0 | 56 | 42 (75.0) | 14 (25.0) | 0.0555 |
| M1 | 10 | 4 (40.0) | 6 (60.0) | |
| TNM stage | ||||
| I + II | 31 | 25 (80.6) | 6 (19.4) | 0.1068 |
| III + IV | 35 | 21 (60.0) | 14 (40.0) | |
| Quantitative parameter | r | p-Value b | ||
| Age c | 66 | −0.0699 | 0.5769 | |
| Nuclear SATB2 Immunoreactivity in CRC Cells | ||||
|---|---|---|---|---|
| Parameters | Number of Patients | Score ≤ 2 n (%) | Score > 2 n (%) | p-Value a |
| Total | 104 | 30 (28.8) | 74 (71.2) | |
| Sex | ||||
| Men | 58 | 9 (15.5) | 49 (84.5) | 0.0010 |
| Women | 46 | 21 (45.7) | 25 (54.3) | |
| Localization | ||||
| Cecum, ascending and transverse colon | 39 | 17 (43.6) | 22 (56.4) | 0.0365 |
| Descending and sigmoid colon | 26 | 5 (19.2) | 21 (80.8) | |
| Rectum | 39 | 8 (20.5) | 31 (79.5) | |
| Grade of differentiation (G) | ||||
| G2 | 96 | 24 (25.0) | 72 (75.0) | 0.0068 |
| G3 | 8 | 6 (75.0) | 2 (25.0) | |
| Depth of invasion (T status) | ||||
| T1 + T2 | 16 | 6 (37.5) | 10 (62.5) | 0.5489 |
| T3 + T4 | 88 | 24 (27.3) | 64 (72.7) | |
| Lymph node metastasis (N status) | ||||
| N0 | 56 | 14 (25.0) | 42 (75.0) | 0.3904 |
| N1 + N2 | 48 | 16 (33.3) | 32 (66.7) | |
| Distant metastasis (M status) | ||||
| M0 | 91 | 28 (30.8) | 63 (69.2) | 0.3384 |
| M1 | 13 | 2 (15.4) | 11 (84.6) | |
| TNM stage | ||||
| I + II | 52 | 13 (25.0) | 39 (75.0) | 0.5165 |
| III + IV | 52 | 17 (32.7) | 35 (67.3) | |
| Quantitative parameter | r | p-Value b | ||
| Age c | 104 | −0.0076 | 0.9389 | |
| Parameter | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| SATB2 mRNA RQ | 0.98 | 0.88–1.08 | 0.6406 | |||
| SATB2 immunoreactivity in CRC | 1.02 | 0.85–1.22 | 0.8492 | |||
| Sex (women vs. men) | 0.80 | 0.44–1.46 | 0.4648 | |||
| Age (years) a | 1.04 | 1.01–1.07 | 0.0082 | 1.04 | 1.01–1.08 | 0.0140 |
| Localization | ||||||
| (rectum vs. cecum, ascending and transverse colon) | 1.42 | 0.71–2.85 | 0.4221 | |||
| (descending and sigmoid colon vs. cecum, ascending and transverse colon) | 1.56 | 0.72–3.38 | 0.6825 | |||
| Grade of differentiation (G3 vs. G2) | 1.02 | 0.31–3.28 | 0.9776 | |||
| Depth of invasion (T3 + T4 vs. T1 + T2) | 4.77 | 1.16–19.73 | 0.0308 | 1.87 | 0.42–8.28 | 0.4098 |
| Lymph node metastasis (N1 + N2 vs. N0) | 3.56 | 1.88–6.74 | 0.0001 | 2.30 | 0.54–9.69 | 0.2582 |
| Distant metastases (M1 vs. M0) | 7.09 | 3.48–14.4 | <0.0001 | 4.84 | 1.98–11.78 | 0.0005 |
| TNM stage (III + IV vs. I + II) | 5.34 | 2.62–10.86 | <0.0001 | 1.58 | 0.31–7.97 | 0.5784 |
| Gene | Primer Sequences |
|---|---|
| SATB2 | F: 5′-AGGAGTTTGGGAGATGGTAT-3′ |
| R: 5′-CCCAGAACACAATAGTCTGAA-3′ | |
| ACTB | F: 5′-TGTGCCCATCTACGAGGGGTATGC-3′ |
| R: 5′-GGTACATGGTGGTGCCGCCAGACA-3′ | |
| HPRT1 | F: 5′-GACTTTGCTTTCCTTGGTCAGGC-3′ |
| R: 5′-TGGCGATGTCAATAGGACTCCAG-3′ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kowalczyk, A.E.; Śliwińska-Jewsiewicka, A.; Kraziński, B.E.; Piotrowska, A.; Grzegrzółka, J.; Godlewski, J.; Dzięgiel, P.; Kmieć, Z. Reduced Expression of SATB2 in Colorectal Cancer and Its Association with Demographic and Clinicopathological Parameters. Int. J. Mol. Sci. 2025, 26, 2374. https://doi.org/10.3390/ijms26052374
Kowalczyk AE, Śliwińska-Jewsiewicka A, Kraziński BE, Piotrowska A, Grzegrzółka J, Godlewski J, Dzięgiel P, Kmieć Z. Reduced Expression of SATB2 in Colorectal Cancer and Its Association with Demographic and Clinicopathological Parameters. International Journal of Molecular Sciences. 2025; 26(5):2374. https://doi.org/10.3390/ijms26052374
Chicago/Turabian StyleKowalczyk, Anna Ewa, Agnieszka Śliwińska-Jewsiewicka, Bartłomiej Emil Kraziński, Aleksandra Piotrowska, Jędrzej Grzegrzółka, Janusz Godlewski, Piotr Dzięgiel, and Zbigniew Kmieć. 2025. "Reduced Expression of SATB2 in Colorectal Cancer and Its Association with Demographic and Clinicopathological Parameters" International Journal of Molecular Sciences 26, no. 5: 2374. https://doi.org/10.3390/ijms26052374
APA StyleKowalczyk, A. E., Śliwińska-Jewsiewicka, A., Kraziński, B. E., Piotrowska, A., Grzegrzółka, J., Godlewski, J., Dzięgiel, P., & Kmieć, Z. (2025). Reduced Expression of SATB2 in Colorectal Cancer and Its Association with Demographic and Clinicopathological Parameters. International Journal of Molecular Sciences, 26(5), 2374. https://doi.org/10.3390/ijms26052374





