Mapping of Determinants of Urinary Sex Steroid Metabolites During Late Pregnancy: Results from Two Spanish Cohorts
Abstract
1. Introduction
2. Results
2.1. Participants’ Characteristics
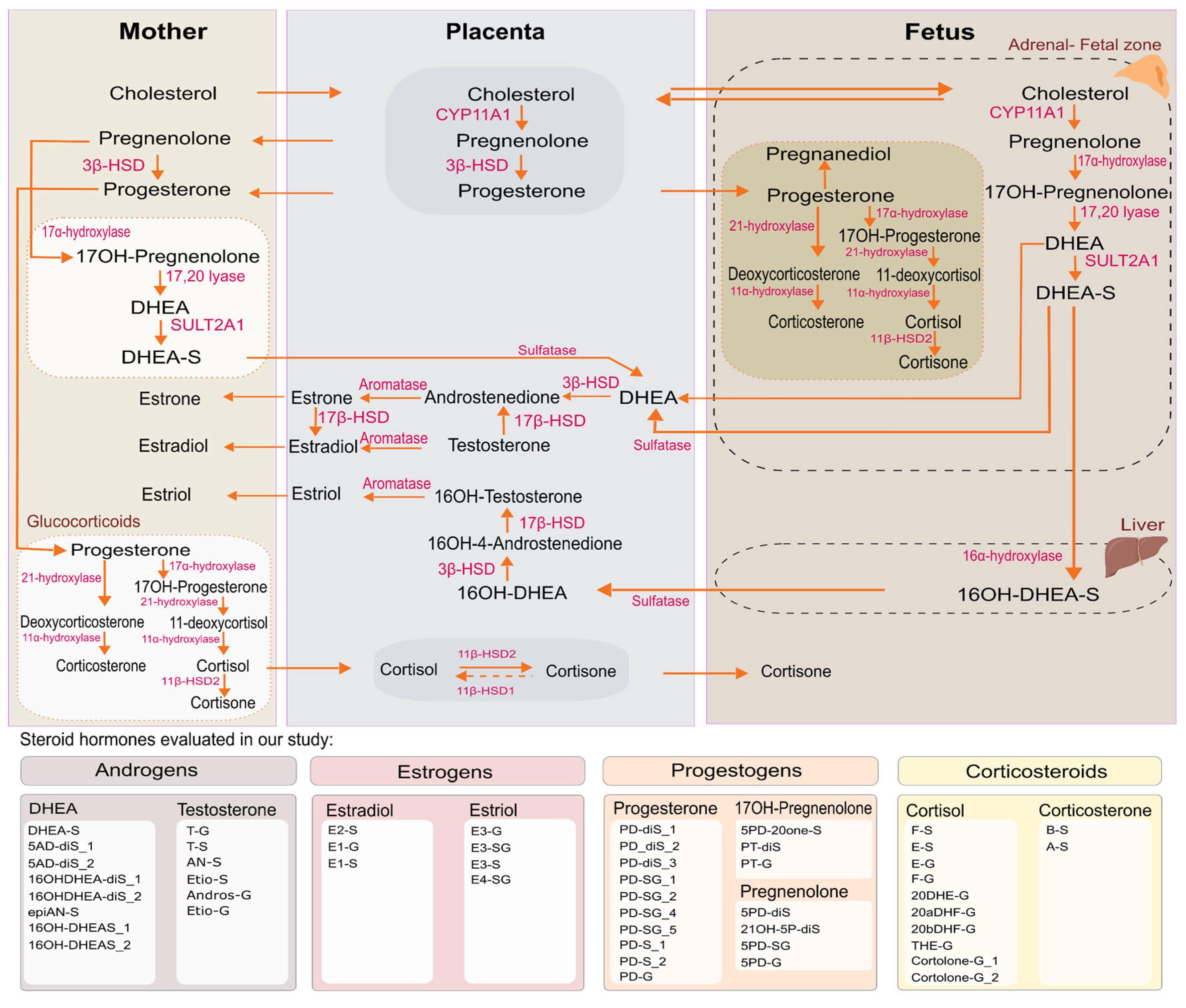
2.2. Identification of SH Metabolites
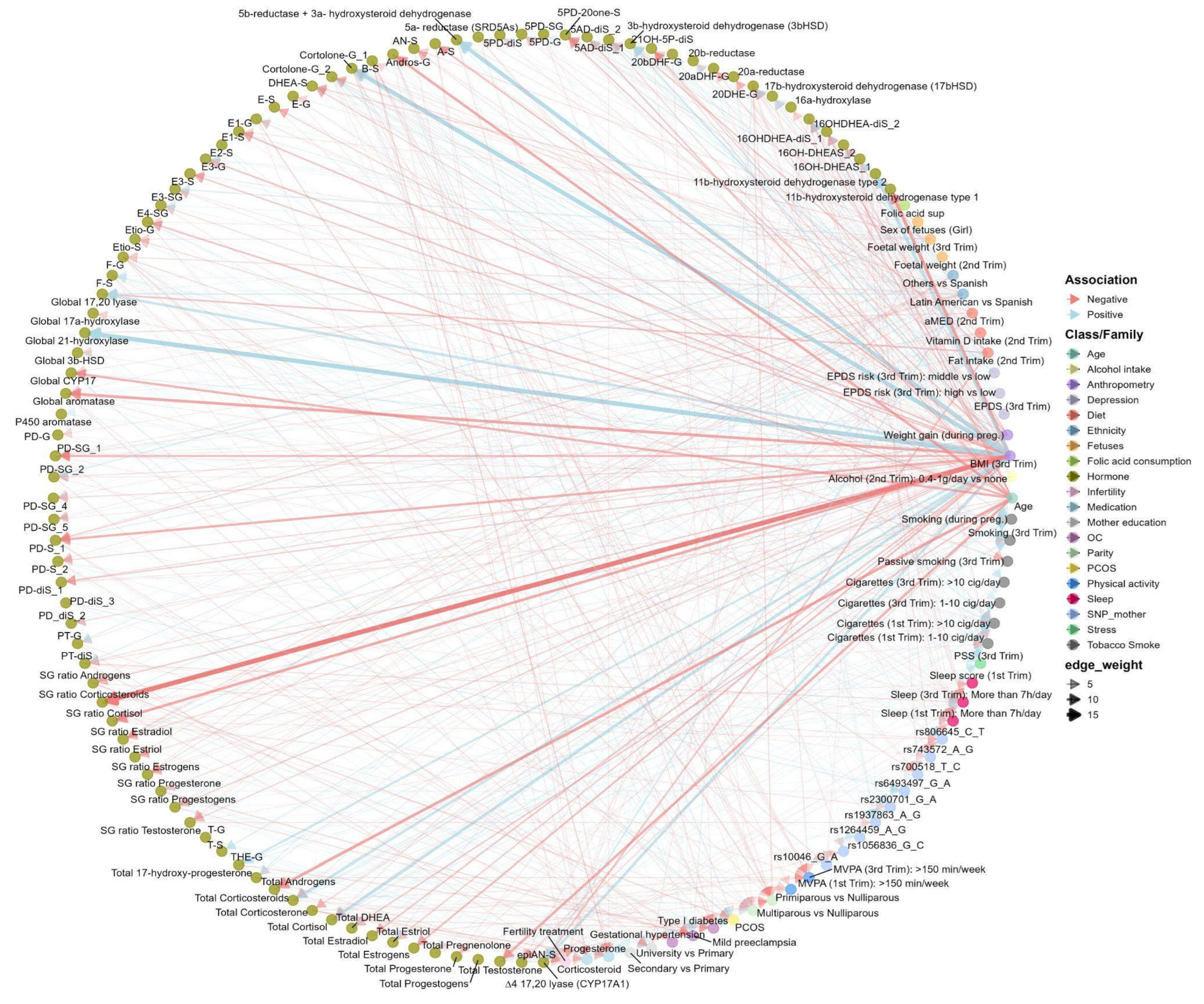
2.3. Main Determinant Selection of the SH Metabolome (BiSC): ExWAS and ENET Analyses
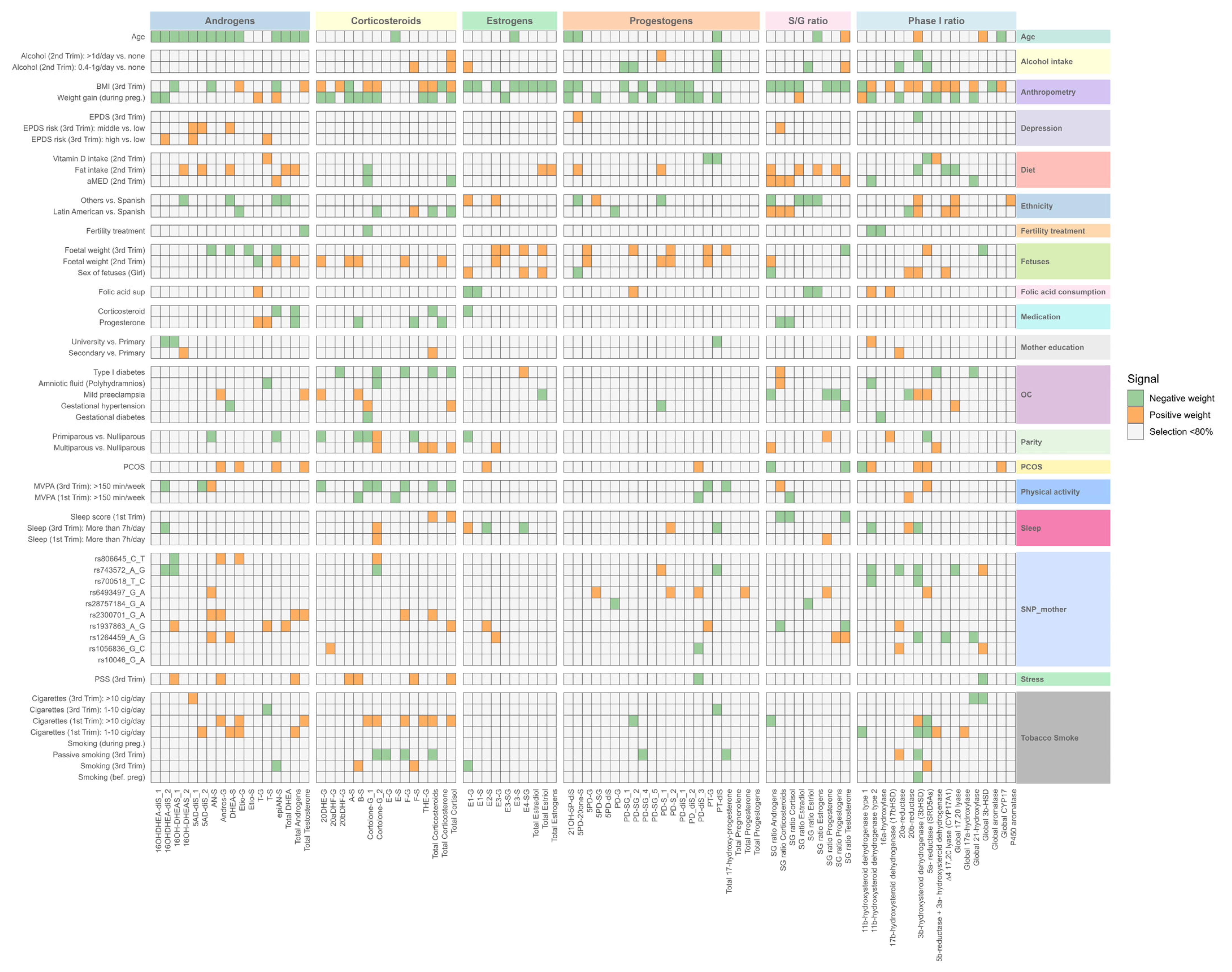
2.4. Determinants of Steroid Hormones: Relative Importance Analysis in the BiSC
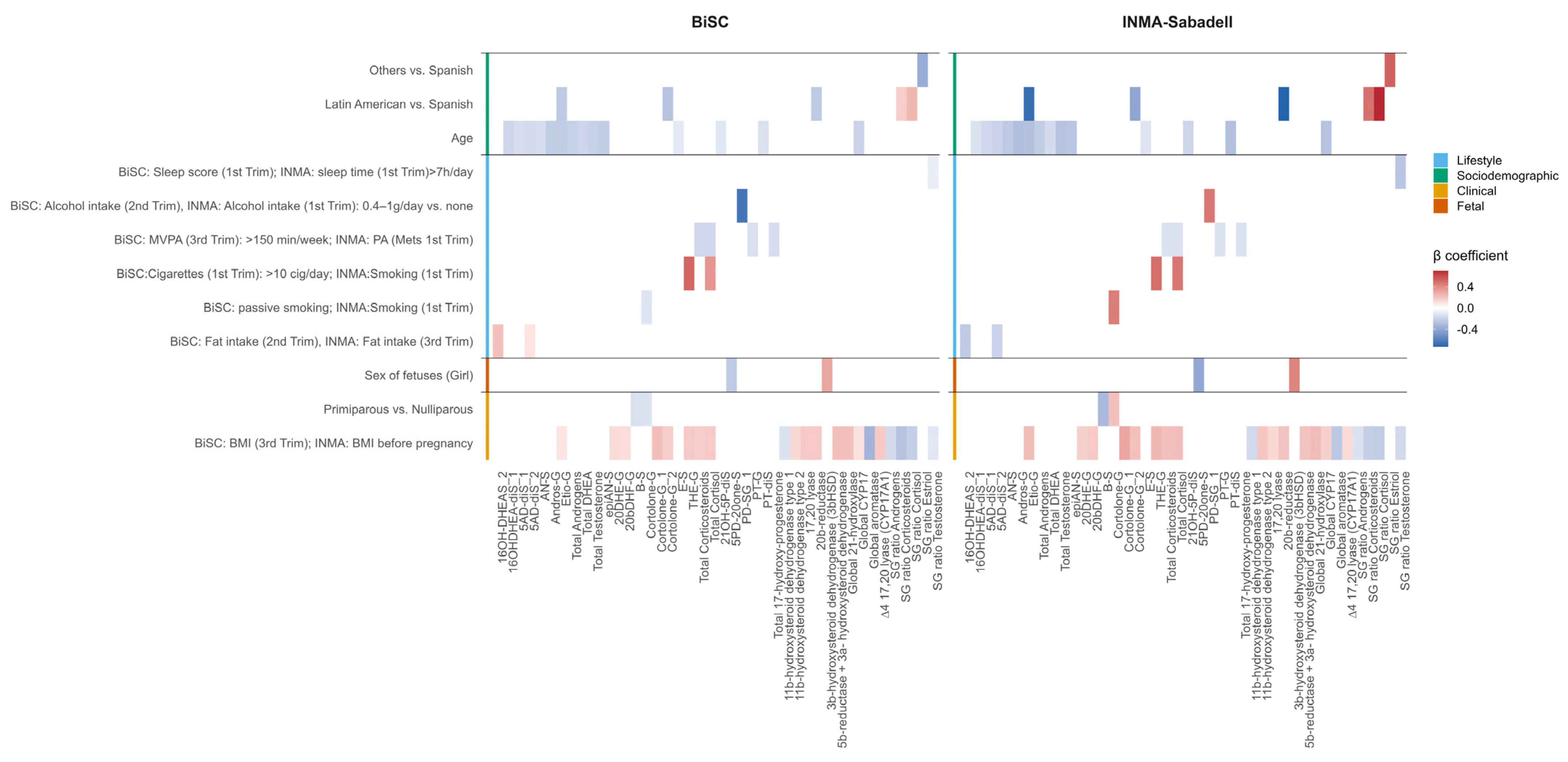
2.5. External Replication Analysis (INMA-Sabadell)
3. Discussion
3.1. A New Window into Maternal Steroid Metabolism
3.2. Clinical Factors Are Consistently Associated with SH-Level Differences
3.3. Lifestyle Behaviors: Physical Activity, Sleep, Smoking, Alcohol, and Diet Are Determinants of SH Levels
3.4. Maternal Age and Ethnicity as Sociodemographic Determinants Associated with SH Metabolism
3.5. Genetic: SNPs from Steroidogenesis Enzymes
3.6. Fetal Determinants: Sex
3.7. Strengths, Limitations, and Future Directions
4. Materials and Methods
4.1. Study Participants and Study Overview
4.2. Urine Collection and Steroid Targeted Metabolome Profiling
4.3. Determinants
4.3.1. Sociodemographic and Clinical Parameters
4.3.2. Fetal Sex and Growth
4.3.3. Genetic
4.3.4. Mental Health
4.3.5. Lifestyle
4.4. Statistical Analysis
4.4.1. Data Preparation
4.4.2. Primary Analysis—BiSC
ExWAS Analysis
Elastic Net Regression Analysis to Determinant Selection
Linear Regression Model and Variance Explained Estimation
4.4.3. Replication Analysis—INMA-Sabadell Cohort
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| A-S | 11-dehydrocorticosterone-Sulfate |
| AN-S | Androsterone-Sulfate |
| Andros-G | Androsterone-Glucuronide |
| B-S | Corticosterone-Sulfate |
| BMI | Body mass index |
| Cortolone-G_1 | 20a-Cortolone-Glucuronide |
| Cortolone-G_2 | 20b-Cortolone-Glucuronide |
| DHEA | Dehydroepiandrosterone |
| DHEA-S | DHEA-sulfate |
| E-S | Cortisone-Sulfate |
| E-G | Cortisone-Glucuronide |
| E2-S | Estradiol-Sulfate |
| E1-G | Estrone-Glucuronide |
| E1-S | Estrone-Sulfate |
| E3-G | Estriol-Glucuronide |
| E3-SG | Estriol-Sulfoglucoconjugated |
| E3-S | Estriol-Sulfate |
| E4-SG | Estetrol-Sulfoglucoconjugated |
| ExWAS | Exposome-Wide Analysis |
| ENT | Effective number of tests |
| ENET | Elastic net regression |
| epiAN-S | epiandrosterone-Sulfate |
| Etio-S | Etiocholanolone-Sulfate |
| Etio-G | Etiocholanolone-Glucuronide |
| F-S | Cortisol-Sulfate |
| F-G | Cortisol-Glucuronide |
| FFQ | Food Frequency Questionnaire |
| IQR | Interquartile range |
| LC-MS/MS | Liquid chromatography-tandem mass spectrometry |
| MEDAS | Mediterranean Diet Adherence Score |
| MVPA | Moderate-to-vigorous physical activity |
| OC | Obstetric complications |
| PCs | Principal components |
| PCOS | Polycystic Ovary Syndrome |
| rMED | Relative Mediterranean Diet score |
| S/G | Sulfate/Glucuronide |
| SNPs | Single-nucleotide polymorphism |
| SH | Steroid hormones |
| 5AD-diS_1 | 5-androsten-3β17β-diol-diSulfate |
| 5AD-diS_2 | 5-androsten-3α17β-diol-diSulfate |
| 16OHDHEA-diS_1 | 16β-hydroxy-DHEA-diSulfate |
| 16OHDHEA-diS_2 | 16α-hydroxy-DHEA-diSulfate |
| 16OH-DHEAS_1 | 16β-hydroxy-DHEA-Sulfate |
| 16OH-DHEAS_2 | 16α-hydroxy-DHEA-Sulfate |
| T-G | Testosterone-Glucuronide |
| T-S | Testosterone-Sulfate |
| 20DHE-G | 20dihydrocortisone-Glucuronide |
| 20aDHF-G | 20α-dihydrocortisol-Glucuronide |
| 20bDHF-G | 20β-dihydrocortisol-Glucuronide |
| THE-G | Tetrahydrocortisone-Glucuronide |
| 5PD-20one-S | 17-hydroxy-5-pregnenolone-3-sulfate |
| 5PD-diS | 5-Pregnendiol-DiSulfate |
| 21OH-5P-diS | 21-Hydroxypregnenolone-DiSulfate |
| 5PD-SG | 5-Pregnendiol-Sulfoglucoconjugated |
| 5PD-G | 5-Pregnendiol-Glucuronide |
| PD-diS_1 | 5α-Pregnan-3β,20α-diol-DiSulfate |
| PD_diS_2 | 5α-Pregnan-3α,20α-diol-DiSulfate |
| PD-diS_3 | 5β-Pregnan-3α,20α-diol-DiSulfate |
| PD-SG_1 | 5α-Pregnandiol-3β-sulfate-20α-Glucuronide |
| PD-SG_2 | Pregnandiol-sulfoglucoconjugate (unknown stereochemistry) |
| PD-SG_4 | Pregnandiol-sulfoglucoconjugate (unknown stereochemistry) |
| PD-SG_5 | Pregnandiol-sulfoglucoconjugate (unknown stereochemistry) |
| PD-S_1 | 5α-Pregnan-3β20α-diol-20-Sulfate |
| PD-S_2 | 5β-Pregnan-3α20α-diol-20-Sulfate |
| PD-G | Pregnandiol-Glucuronide |
| PT-diS | Pregnantriol-diSulfate |
| PT-G | Pregnantriol-Glucuronide |
References
- Chatuphonprasert, W.; Jarukamjorn, K.; Ellinger, I. Physiology and Pathophysiology of Steroid Biosynthesis, Transport and Metabolism in the Human Placenta. Front. Pharmacol. 2018, 9, 1027. [Google Scholar] [CrossRef] [PubMed]
- Christakoudi, S.; Cowan, D.A.; Christakudis, G.; Taylor, N.F. 21-Hydroxylase Deficiency in the Neonate—Trends in Steroid Anabolism and Catabolism during the First Weeks of Life. J. Steroid Biochem. Mol. Biol. 2013, 138, 334–347. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.L.; Bose, H.S. Early Steps in Steroidogenesis: Intracellular Cholesterol Trafficking: Thematic Review Series: Genetics of Human Lipid Diseases. J. Lipid Res. 2011, 52, 2111–2135. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.L.; Auchus, R.J. The Molecular Biology, Biochemistry, and Physiology of Human Steroidogenesis and Its Disorders. Endocr. Rev. 2011, 32, 81–151. [Google Scholar] [CrossRef]
- Miller, W.L. Steroidogenesis: Unanswered Questions. Trends Endocrinol. Metab. 2017, 28, 771–793. [Google Scholar] [CrossRef]
- Miller, W.L. Steroid Hormone Synthesis in Mitochondria. Mol. Cell. Endocrinol. 2013, 379, 62–73. [Google Scholar] [CrossRef]
- Liang, L.; Rasmussen, M.-L.H.; Piening, B.; Shen, X.; Chen, S.; Röst, H.; Snyder, J.K.; Tibshirani, R.; Skotte, L.; Lee, N.C.Y.; et al. Metabolic Dynamics and Prediction of Gestational Age and Time to Delivery in Pregnant Women. Cell 2020, 181, 1680–1692.e15. [Google Scholar] [CrossRef]
- Thompson, A.L.; Lampl, M. Prenatal and Postnatal Energetic Conditions and Sex Steroids Levels across the First Year of Life. Am. J. Hum. Biol. 2013, 25, 643–654. [Google Scholar] [CrossRef]
- Lan, K.-C.; Lai, Y.-J.; Cheng, H.-H.; Tsai, N.-C.; Su, Y.-T.; Tsai, C.-C.; Hsu, T.-Y. Levels of Sex Steroid Hormones and Their Receptors in Women with Preeclampsia. Reprod. Biol. Endocrinol. 2020, 18, 12. [Google Scholar] [CrossRef]
- Chen, S.; Shen, X.; Liang, L.; Avina, M.; Zackriah, H.; Jelliffe-Pawlowski, L.; Rand, L.; Snyder, M. Longitudinal Urine Metabolic Profiling and Gestational Age Prediction in Pregnancy. bioRxiv 2022. [Google Scholar] [CrossRef]
- Soldin, O.P.; Guo, T.; Weiderpass, E.; Tractenberg, R.E.; Hilakivi-Clarke, L.; Soldin, S.J. Steroid Hormone Levels in Pregnancy and 1 Year Postpartum Using Isotope Dilution Tandem Mass Spectrometry. Fertil. Steril. 2005, 84, 701–710. [Google Scholar] [CrossRef]
- Cantonwine, D.E.; McElrath, T.F.; Trabert, B.; Xu, X.; Sampson, J.; Roberts, J.M.; Hoover, R.N.; Troisi, R. Estrogen Metabolism Pathways in Preeclampsia and Normal Pregnancy. Steroids 2019, 144, 8–14. [Google Scholar] [CrossRef]
- Kallak, T.K.; Hellgren, C.; Skalkidou, A.; Sandelin-Francke, L.; Ubhayasekhera, K.; Bergquist, J.; Axelsson, O.; Comasco, E.; Campbell, R.E.; Sundström Poromaa, I. Maternal and Female Fetal Testosterone Levels Are Associated with Maternal Age and Gestational Weight Gain. Eur. J. Endocrinol. 2017, 177, 379–388. [Google Scholar] [CrossRef]
- Barrett, E.S.; Mbowe, O.; Thurston, S.W.; Butts, S.; Wang, C.; Nguyen, R.; Bush, N.; Redmon, J.B.; Sheshu, S.; Swan, S.H.; et al. Predictors of Steroid Hormone Concentrations in Early Pregnancy: Results from a Multi-Center Cohort. Matern. Child Health J. 2019, 23, 397–407. [Google Scholar] [CrossRef]
- Lof, M.; Hilakivi-Clarke, L.; Sandin S, S.; de Assis, S.; Yu, W.; Weiderpass, E. Dietary Fat Intake and Gestational Weight Gain in Relation to Estradiol and Progesterone Plasma Levels during Pregnancy: A Longitudinal Study in Swedish Women. BMC Women Health 2009, 9, 10. [Google Scholar] [CrossRef] [PubMed]
- Petridou, E.; Katsouyanni, K.; Hsieh, C.; Antsaklis, A.; Trichopoulos, D. Diet, Pregnancy Estrogens and Their Possible Relevance to Cancer Risk in the Offspring. Oncology 2009, 49, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Bíró, I.; Bufa, A.; Wilhelm, F.; Mánfai, Z.; Kilár, F.; Gocze, P.M. Urinary Steroid Profile in Early Pregnancy after in Vitro Fertilization. Acta Obstet. Gynecol. Scand. 2012, 91, 625–629. [Google Scholar] [CrossRef]
- Maliqueo, M.; Lara, H.E.; Sánchez, F.; Echiburú, B.; Crisosto, N.; Sir-Petermann, T. Placental Steroidogenesis in Pregnant Women with Polycystic Ovary Syndrome. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 166, 151–155. [Google Scholar] [CrossRef]
- Piltonen, T.T.; Giacobini, P.; Edvinsson, Å.; Hustad, S.; Lager, S.; Morin-Papunen, L.; Tapanainen, J.S.; Sundström-Poromaa, I.; Arffman, R.K. Circulating Antimüllerian Hormone and Steroid Hormone Levels Remain High in Pregnant Women with Polycystic Ovary Syndrome at Term. Fertil. Steril. 2019, 111, 588–596.e1. [Google Scholar] [CrossRef]
- Liu, Y.; Zhao, X.-X.; Hu, X.-J.; Yang, F.; Lin, P.; Cui, S.-C.; Zhao, W.; Cao, X.-Y.; Wang, Y.-S. Effect of Sex Hormone–Binding Globulin Polymorphisms on the Outcome of in Vitro Fertilization-Embryo Transfer for Polycystic Ovary Syndrome Patients: A Case-Control Study. J. Cell. Biochem. 2019, 120, 4675–4686. [Google Scholar] [CrossRef] [PubMed]
- Koskivuori, J.; Voutilainen, R.; Storvik, M.; Häkkinen, M.R.; Uusitalo, L.; Keski-Nisula, L.; Backman, K.; Auriola, S.; Lehtonen, M. Comparative Steroid Profiling of Newborn Hair and Umbilical Cord Serum Highlights the Role of Fetal Adrenals, Placenta, and Pregnancy Outcomes in Fetal Steroid Metabolism. J. Steroid Biochem. Mol. Biol. 2023, 232, 106357. [Google Scholar] [CrossRef] [PubMed]
- Mullen, J.; Gadot, Y.; Eklund, E.; Andersson, A.; Schulze, J.J.; Ericsson, M.; Hirschberg, A.L.; Rane, A.; Ekström, L. Pregnancy Greatly Affects the Steroidal Module of the Athlete Biological Passport. Drug Test. Anal. 2018, 10, 1070–1075. [Google Scholar] [CrossRef] [PubMed]
- Farhan, S.H.; Abdul-Hassan, I.A.; Mohammed, N. Association of Polymorphism Rs1264459 in the HLA-E Gene Promoter with Incidence of (RSA) and Its Consequences to Steroid Hormones in Iraqi Women. Iraqi J. Biotechnol. 2020, 3. [Google Scholar]
- Piasek, M.; Škrgatić, L.; Sulimanec, A.; Orct, T.; Sekovanić, A.; Kovačić, J.; Katić, A.; Branović Čakanić, K.; Pizent, A.; Brajenović, N.; et al. Effects of Maternal Cigarette Smoking on Trace Element Levels and Steroidogenesis in the Maternal–Placental–Fetal Unit. Toxics 2023, 11, 714. [Google Scholar] [CrossRef]
- Rauramo, I.; Andersson, B.; Laatikainen, T.; Pettersson, J. Stress Hormones and Placental Steroids in Physical Exercise during Pregnancy. BJOG Int. J. Obstet. Gynaecol. 1982, 89, 921–925. [Google Scholar] [CrossRef]
- Crowley, S.K.; O’Buckley, T.K.; Schiller, C.E.; Stuebe, A.; Morrow, A.L.; Girdler, S.S. Blunted Neuroactive Steroid and HPA Axis Responses to Stress Are Associated with Reduced Sleep Quality and Negative Affect in Pregnancy: A Pilot Study. Psychopharmacology 2016, 233, 1299–1310. [Google Scholar] [CrossRef]
- Halmesmäki, E.; Autti, I.; Granström, M.-L.; Stenman, U.-H.; Ylikorkala, O. Estradiol, Estriol, Progesterone, Prolactin, and Human Chorionic Gonadotropin in Pregnant Women with Alcohol Abuse. J. Clin. Endocrinol. Metab. 1987, 64, 153–156. [Google Scholar] [CrossRef]
- Hansel, M.C.; Murphy, H.R.; Brunner, J.; Wang, C.; Miller, R.K.; O’Connor, T.G.; Barrett, E.S.; Rivera-Núñez, Z. Associations between Neighborhood Stress and Maternal Sex Steroid Hormones in Pregnancy. BMC Pregnancy Childbirth 2023, 23, 730. [Google Scholar] [CrossRef]
- Toriola, A.T.; Vääräsmäki, M.; Lehtinen, M.; Zeleniuch-Jacquotte, A.; Lundin, E.; Rodgers, K.-G.; Lakso, H.-A.; Chen, T.; Schock, H.; Hallmans, G.; et al. Determinants of Maternal Sex Steroids During the First Half of Pregnancy. Obstet. Gynecol. 2011, 118, 1029–1036. [Google Scholar] [CrossRef]
- Chen, M.; Guan, Y.; Huang, R.; Duan, J.; Zhou, J.; Chen, T.; Wang, X.; Xia, Y.; London, S.J. Associations between the Maternal Exposome and Metabolome during Pregnancy. Environ. Health Perspect. 2022, 130, 037003. [Google Scholar] [CrossRef] [PubMed]
- Deltourbe, L.G.; Sugrue, J.; Maloney, E.; Dubois, F.; Jaquaniello, A.; Bergstedt, J.; Patin, E.; Quintana-Murci, L.; Ingersoll, M.A.; Duffy, D.; et al. Steroid Hormone Levels Vary with Sex, Aging, Lifestyle, and Genetics. Sci. Adv. 2025, 11, eadu6094. [Google Scholar] [CrossRef]
- Pozo, O.J.; Marcos, J.; Khymenets, O.; Pranata, A.; Fitzgerald, C.C.; McLeod, M.D.; Shackleton, C. SULFATION PATHWAYS: Alternate Steroid Sulfation Pathways Targeted by LC–MS/MS Analysis of Disulfates: Application to Prenatal Diagnosis of Steroid Synthesis Disorders. J. Mol. Endocrinol. 2018, 61, M1–M12. [Google Scholar] [CrossRef]
- Dukic, J.; Ehlert, U. Longitudinal Course of Sex Steroids From Pregnancy to Postpartum. Endocrinology 2023, 164, bqad108. [Google Scholar] [CrossRef]
- Jin, C.; Peng, Y.; Luo, X.; Zhu, Q.; Lin, L.; Yang, J.; Wang, P. Dynamic Change of Estrogen and Progesterone Metabolites in Human Urine during Pregnancy. Sci. Rep. 2025, 15, 8409. [Google Scholar] [CrossRef]
- Mistry, H.D.; Eisele, N.; Escher, G.; Dick, B.; Surbek, D.; Delles, C.; Currie, G.; Schlembach, D.; Mohaupt, M.G.; Gennari-Moser, C. Gestation-Specific Reference Intervals for Comprehensive Spot Urinary Steroid Hormone Metabolite Analysis in Normal Singleton Pregnancy and 6 Weeks Postpartum. Reprod. Biol. Endocrinol. 2015, 13, 101. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Swift, T.A.; West, C.A.; Rosano, T.G.; Rej, R. Immunoassay of Estradiol: Unanticipated Suppression by Unconjugated Estriol. Clin. Chem. 2004, 50, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Perng, W.; Aslibekyan, S. Find the Needle in the Haystack, Then Find It Again: Replication and Validation in the ‘Omics Era. Metabolites 2020, 10, 286. [Google Scholar] [CrossRef] [PubMed]
- Maitre, L.; Jedynak, P.; Gallego, M.; Ciaran, L.; Audouze, K.; Casas, M.; Vrijheid, M. Integrating-Omics Approaches into Population-Based Studies of Endocrine Disrupting Chemicals: A Scoping Review. Environ. Res. 2023, 228, 115788. [Google Scholar] [CrossRef]
- Wang, R.; Hartmann, M.F.; Tiosano, D.; Wudy, S.A. Characterizing the Steroidal Milieu in Amniotic Fluid of Mid-Gestation: A GC-MS Study. J. Steroid Biochem. Mol. Biol. 2019, 193, 105412. [Google Scholar] [CrossRef]
- Krone, N.; Hughes, B.A.; Lavery, G.G.; Stewart, P.M.; Arlt, W.; Shackleton, C.H.L. Gas Chromatography/Mass Spectrometry (GC/MS) Remains a Pre-Eminent Discovery Tool in Clinical Steroid Investigations Even in the Era of Fast Liquid Chromatography Tandem Mass Spectrometry (LC/MS/MS). J. Steroid Biochem. Mol. Biol. 2010, 121, 496–504. [Google Scholar] [CrossRef]
- Servin-Barthet, C.; Martínez-García, M.; Paternina-Die, M.; Marcos-Vidal, L.; Martín de Blas, D.; Soler, A.; Khymenets, O.; Bergé, D.; Casals, G.; Prats, P.; et al. Pregnancy Entails a U-Shaped Trajectory in Human Brain Structure Linked to Hormones and Maternal Attachment. Nat. Commun. 2025, 16, 730. [Google Scholar] [CrossRef]
- Jäntti, S.E.; Hartonen, M.; Hilvo, M.; Nygren, H.; Hyötyläinen, T.; Ketola, R.A.; Kostiainen, R. Steroid and Steroid Glucuronide Profiles in Urine during Pregnancy Determined by Liquid Chromatography–Electrospray Ionization-Tandem Mass Spectrometry. Anal. Chim. Acta 2013, 802, 56–66. [Google Scholar] [CrossRef]
- Lahti-Pulkkinen, M.; Räikkönen, K.; Basiukajc, A.; Lee, P.; Denham, S.G.; Simpson, J.P.; Villa, P.; Hämäläinen, E.; Laivuori, H.; Kajantie, E.; et al. Determination of Steroid Reference Intervals in a Pregnancy Population. J. Steroid Biochem. Mol. Biol. 2025, 248, 106691. [Google Scholar] [CrossRef]
- Costantine, M. Physiologic and Pharmacokinetic Changes in Pregnancy. Front. Pharmacol. 2014, 5, 65. [Google Scholar] [CrossRef]
- Pasqualini, J.R. Enzymes Involved in the Formation and Transformation of Steroid Hormones in the Fetal and Placental Compartments. J. Steroid Biochem. Mol. Biol. 2005, 97, 401–415. [Google Scholar] [CrossRef]
- Volqvartz, T.; Andersen, H.H.B.; Pedersen, L.H.; Larsen, A. Obesity in Pregnancy—Long-Term Effects on Offspring Hypothalamic-Pituitary-Adrenal Axis and Associations with Placental Cortisol Metabolism: A Systematic Review. Eur. J. Neurosci. 2023, 58, 4393–4422. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, S.L.; Mitchell, A.M.; Kowalsky, J.M.; Christian, L.M. Maternal Parity and Perinatal Cortisol Adaptation: The Role of Pregnancy-Specific Distress and Implications for Postpartum Mood. Psychoneuroendocrinology 2018, 97, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Marteinsdottir, I.; Sydsjö, G.; Faresjö, Å.; Theodorsson, E.; Josefsson, A. Parity—Related Variation in Cortisol Concentrations in Hair during Pregnancy. BJOG Int. J. Obstet. Gynaecol. 2021, 128, 637–644. [Google Scholar] [CrossRef] [PubMed]
- Budnik-Przybylska, D.; Laskowski, R.; Pawlicka, P.; Anikiej-Wiczenbach, P.; Łada-Maśko, A.; Szumilewicz, A.; Makurat, F.; Przybylski, J.; Soya, H.; Kaźmierczak, M. Do Physical Activity and Personality Matter for Hair Cortisol Concentration and Self-Reported Stress in Pregnancy? A Pilot Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 8050. [Google Scholar] [CrossRef]
- Hernández-Pérez, J.G.; Taha, S.; Torres-Sánchez, L.E.; Villasante-Tezanos, A.; Milani, S.A.; Baillargeon, J.; Canfield, S.; Lopez, D.S. Association of Sleep Duration and Quality with Serum Testosterone Concentrations among Men and Women: NHANES 2011–2016. Andrology 2024, 12, 518–526. [Google Scholar] [CrossRef]
- Rizwan, S.; Manning, J.T.; Brabin, B.J. Maternal Smoking during Pregnancy and Possible Effects of in Utero Testosterone: Evidence from the 2D:4D Finger Length Ratio. Early Hum. Dev. 2007, 83, 87–90. [Google Scholar] [CrossRef]
- Cajachagua-Torres, K.N.; Jaddoe, V.W.V.; de Rijke, Y.B.; van den Akker, E.L.T.; Reiss, I.K.M.; van Rossum, E.F.C.; El Marroun, H. Parental Cannabis and Tobacco Use during Pregnancy and Childhood Hair Cortisol Concentrations. Drug Alcohol Depend. 2021, 225, 108751. [Google Scholar] [CrossRef] [PubMed]
- Hill, M.; Popov, P.; Havlikova, H.; Kancheva, L.; Vrbikova, J.; Meloun, M.; Kancheva, R.; Cibula, D.; Pouzar, V.; Cerny, I.; et al. Reinstatement of Serum Pregnanolone Isomers and Progesterone During Alcohol Detoxification Therapy in Premenopausal Women. Alcohol. Clin. Exp. Res. 2005, 29, 1010–1017. [Google Scholar] [CrossRef]
- Cui, X.; Rosner, B.; Willett, W.C.; Hankinson, S.E. Dietary Fat, Fiber, and Carbohydrate Intake and Endogenous Hormone Levels in Premenopausal Women. Horm. Cancer 2010, 1, 265–276. [Google Scholar] [CrossRef]
- Soltani, S.; Hejazi, M.; Meshkini, F.; Torabinasab, K.; Zeraattalab-Motlagh, S.; Sangsefidi, Z.S.; Sikaroudi, M.K.; Razmpoosh, E.; Ansari, A.; Abdollahi, S. The Effect of Low-Fat Diets Versus High-Fat Diet on Sex Hormones: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Food Sci. 2025, 90, e70266. [Google Scholar] [CrossRef]
- Glynn, L.M.; Schetter, C.D.; Chicz-DeMet, A.; Hobel, C.J.; Sandman, C.A. Ethnic Differences in Adrenocorticotropic Hormone, Cortisol and Corticotropin-Releasing Hormone during Pregnancy. Peptides 2007, 28, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Thayer, Z.M.; Kuzawa, C.W. Ethnic Discrimination Predicts Poor Self-Rated Health and Cortisol in Pregnancy: Insights from New Zealand. Soc. Sci. Med. 2015, 128, 36–42. [Google Scholar] [CrossRef]
- Urizar, G.G.; Yim, I.S.; Kofman, Y.B.; Tilka, N.; Miller, K.; Freche, R.; Johnson, A. Ethnic Differences in Stress-Induced Cortisol Responses:Increased Risk for Depression during Pregnancy. Biol. Psychol. 2019, 147, 107630. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Coates, R.J.; Gwinn, M.; Khoury, M.J. Steroid 5-α-Reductase Type 2 (SRD5a2) Gene Polymorphisms and Risk of Prostate Cancer: A HuGE Review. Am. J. Epidemiol. 2010, 171, 1–13. [Google Scholar] [CrossRef]
- Colicino, E.; Cowell, W.; Pedretti, N.F.; Joshi, A.; Petrick, L.; Niedzwiecki, M.; Wright, R.O.; Wright, R.J. Maternal Steroids during Pregnancy and Their Associations with Exposure to Lifetime Stressful Life Events, Prenatal Stress Appraisal and Psychological Functioning. Psychoneuroendocrinology 2023, 158, 106395. [Google Scholar] [CrossRef]
- Colicino, E.; Cowell, W.; Foppa Pedretti, N.; Joshi, A.; Youssef, O.; Just, A.C.; Kloog, I.; Petrick, L.; Niedzwiecki, M.; Wright, R.O.; et al. Maternal Steroids during Pregnancy and Their Associations with Ambient Air Pollution and Temperature during Preconception and Early Gestational Periods. Environ. Int. 2022, 165, 107320. [Google Scholar] [CrossRef]
- Rivera-Núñez, Z.; Hansel, M.; Capurro, C.; Kozlosky, D.; Wang, C.; Doherty, C.L.; Buckley, B.; Ohman-Strickland, P.; Miller, R.K.; O’Connor, T.G.; et al. Prenatal Cadmium Exposure and Maternal Sex Steroid Hormone Concentrations across Pregnancy. Toxics 2023, 11, 589. [Google Scholar] [CrossRef]
- Kolatorova, L.; Vitku, J.; Hampl, R.; Adamcova, K.; Skodova, T.; Simkova, M.; Parizek, A.; Starka, L.; Duskova, M. Exposure to Bisphenols and Parabens during Pregnancy and Relations to Steroid Changes. Environ. Res. 2018, 163, 115–122. [Google Scholar] [CrossRef]
- Ryva, B.A.; Pacyga, D.C.; Anderson, K.Y.; Calafat, A.M.; Whalen, J.; Aung, M.T.; Gardiner, J.C.; Braun, J.M.; Schantz, S.L.; Strakovsky, R.S. Associations of Urinary Non-Persistent Endocrine Disrupting Chemical Biomarkers with Early-to-Mid Pregnancy Plasma Sex-Steroid and Thyroid Hormones. Environ. Int. 2024, 183, 108433. [Google Scholar] [CrossRef]
- Bedrak, E.; Brandes, O.; Fried, K. Profiles of Steroids during Third Trimester of Pregnancy in Women: Effect of Hot, Dry Desert Environment. J. Therm. Biol. 1980, 5, 235–241. [Google Scholar] [CrossRef]
- Diviccaro, S.; Giatti, S.; Cioffi, L.; Chrostek, G.; Melcangi, R.C. The Gut-Microbiota-Brain Axis: Focus on Gut Steroids. J. Neuroendocrinol. 2025, 37, e13471. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; Gascon, M.; Bustamante, M.; Rivas, I.; Foraster, M.; Basagaña, X.; Cosín, M.; Eixarch, E.; Ferrer, M.; Gratacós, E.; et al. Cohort Profile: Barcelona Life Study Cohort (BiSC). Int. J. Epidemiol. 2024, 53, dyae063. [Google Scholar] [CrossRef] [PubMed]
- Guxens, M.; Ballester, F.; Espada, M.; Fernández, M.F.; Grimalt, J.O.; Ibarluzea, J.; Olea, N.; Rebagliato, M.; Tardón, A.; Torrent, M.; et al. Cohort Profile: The INMA-INfancia y Medio Ambiente-(Environment and Childhood) Project. Int. J. Epidemiol. 2012, 41, 930–940. [Google Scholar] [CrossRef]
- Lubin, J.H.; Colt, J.S.; Camann, D.; Davis, S.; Cerhan, J.R.; Severson, R.K.; Bernstein, L.; Hartge, P. Epidemiologic Evaluation of Measurement Data in the Presence of Detection Limits. Environ. Health Perspect. 2004, 112, 1691–1696. [Google Scholar] [CrossRef]
- Magyar, B.P.; Santi, M.; Sommer, G.; Nuoffer, J.-M.; Leichtle, A.; Grössl, M.; Fluck, C.E. Short-Term Fasting Attenuates Overall Steroid Hormone Biosynthesis in Healthy Young Women. J. Endocr. Soc. 2022, 6, bvac075. [Google Scholar] [CrossRef]
- Ondřejíková, L.; Pařízek, A.; Šimják, P.; Vejražková, D.; Velíková, M.; Anderlová, K.; Vosátková, M.; Krejčí, H.; Koucký, M.; Kancheva, R.; et al. Altered Steroidome in Women with Gestational Diabetes Mellitus: Focus on Neuroactive and Immunomodulatory Steroids from the 24th Week of Pregnancy to Labor. Biomolecules 2021, 11, 1746. [Google Scholar] [CrossRef]
- Lobmaier, S.M.; Figueras, F.; Mercade, I.; Crovetto, F.; Peguero, A.; Parra-Saavedra, M.; Ortiz, J.U.; Crispi, F.; Gratacós, E. Levels of Maternal Serum Angiogenic Factors in Third-Trimester Normal Pregnancies: Reference Ranges, Influence of Maternal and Pregnancy Factors and Fetoplacental Doppler Indices. Fetal Diagn. Ther. 2014, 36, 38–43. [Google Scholar] [CrossRef]
- Hadlock, F.P.; Harrist, R.B.; Sharman, R.S.; Deter, R.L.; Park, S.K. Estimation of Fetal Weight with the Use of Head, Body, and Femur Measurements—A Prospective Study. Am. J. Obstet. Gynecol. 1985, 151, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Salomon, L.J.; Alfirevic, Z.; Da Silva Costa, F.; Deter, R.L.; Figueras, F.; Ghi, T.A.; Glanc, P.; Khalil, A.; Lee, W.; Napolitano, R.; et al. ISUOG Practice Guidelines: Ultrasound Assessment of Fetal Biometry and Growth. Ultrasound Obstet. Gynecol. 2019, 53, 715–723. [Google Scholar] [CrossRef] [PubMed]
- Iñiguez, C.; Esplugues, A.; Sunyer, J.; Basterrechea, M.; Fernández-Somoano, A.; Costa, O.; Estarlich, M.; Aguilera, I.; Lertxundi, A.; Tardón, A.; et al. Prenatal Exposure to NO2 and Ultrasound Measures of Fetal Growth in the Spanish INMA Cohort. Environ. Health Perspect. 2016, 124, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Hellgren, C.; Comasco, E.; Skalkidou, A.; Sundström-Poromaa, I. Allopregnanolone Levels and Depressive Symptoms during Pregnancy in Relation to Single Nucleotide Polymorphisms in the Allopregnanolone Synthesis Pathway. Horm. Behav. 2017, 94, 106–113. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of Postnatal Depression: Development of the 10-Item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Remor, E. Psychometric Properties of a European Spanish Version of the Perceived Stress Scale (PSS). Span. J. Psychol. 2006, 9, 86–93. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Coll-Risco, I.; Camiletti-Moirón, D.; Acosta-Manzano, P.; Aparicio, V.A. Translation and Cross-Cultural Adaptation of the Pregnancy Physical Activity Questionnaire (PPAQ) into Spanish. J. Matern. Fetal Neonatal Med. 2019, 32, 3954–3961. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour, 1st ed.; World Health Organization: Geneva, Switzerland, 2020; ISBN 978-92-4-001512-8. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Vioque, J.; Navarrete-Muñoz, E.-M.; Gimenez-Monzó, D.; García-de-la-Hera, M.; Granado, F.; Young, I.S.; Ramón, R.; Ballester, F.; Murcia, M.; Rebagliato, M.; et al. Reproducibility and Validity of a Food Frequency Questionnaire among Pregnant Women in a Mediterranean Area. Nutr. J. 2013, 12, 26. [Google Scholar] [CrossRef]
- Fung, T.T.; McCullough, M.L.; Newby, P.; Manson, J.E.; Meigs, J.B.; Rifai, N.; Willett, W.C.; Hu, F.B. Diet-Quality Scores and Plasma Concentrations of Markers of Inflammation and Endothelial Dysfunction2. Am. J. Clin. Nutr. 2005, 82, 163–173. [Google Scholar] [CrossRef]
- SR28—Page Reports: USDA ARS. Available online: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/methods-and-application-of-food-composition-laboratory/mafcl-site-pages/sr28-page-reports/ (accessed on 24 July 2025).
- Palma-Linares, I.; Farrán Codina, A.; Cervera Ral, P. Tablas de Composición de Alimentos por Medidas Caseras de Consumo Habitual en España: = Taules de Composició D’aliments per Mesures Casolanes de Consum Habitual a Espanya; Mc Graw-Hill: Madrid, Spain, 2005; ISBN 978-84-609-7033-0. [Google Scholar]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for Total Energy Intake in Epidemiologic Studies. Am. J. Clin. Nutr. 1997, 65, 1220S–1228S. [Google Scholar] [CrossRef]
- Gebhardt, S.; Lemar, L.; Haytowitz, D.; Pehrsson, P.; Nickle, M.; Showell, B.; Thomas, R.; Exler, J.; Holden, J. USDA National Nutrient Database for Standard Reference, Release 21; United States Department of Agriculture Agricultural Research Service: Washington, DC, USA, 2006. [Google Scholar]
- Zou, H.; Hastie, T. Regularization and Variable Selection Via the Elastic Net. J. R. Stat. Soc. Ser. B Stat. Methodol. 2005, 67, 301–320. [Google Scholar] [CrossRef]
- Groemping, U. Relative Importance for Linear Regression in R: The Package Relaimpo. J. Stat. Softw. 2007, 17, 1–27. [Google Scholar] [CrossRef]




| BiSC (n = 721) | INMA-Sabadell (n = 500) | |
|---|---|---|
| Maternal age (year) | 34.8 [5.2] 1 | 31.2 [5.7] 1 |
| Missing | 0 | 1 |
| Gestational age at sampling collection | 34.7 [2] 1 | 34.1 [1.4] 1 |
| BMI * (kg/m2) | 23.2 [4.9] 1 | 22.7 [4.5] 1 |
| Underweight (<18.5 kg/m2), n (%) | 22 (4) | 25 (5) |
| Normal weight (18.5–25 kg/m2) n (%) | 434 (64) | 331 (66) |
| Overweight (25–30 kg/m2), n (%) | 155 (23) | 102 (20) |
| Obese (>30 kg/m2), n (%) | 63 (9) | 42 (8) |
| Missing | 47 | 0 |
| Mother country of birth, n (%) | ||
| Spain | 498 (69) | 446 (89) |
| Latin America | 165 (23) | 36 (7) |
| Others | 57 (8) | 18 (4) |
| Missing | 1 | 0 |
| Maternal education, n (%) | ||
| Primary or without education | 27 (4) | 4 (1) |
| Secondary | 175 (24) | 132 (27) |
| Technical or University | 519 (72) | 362 (73) |
| Missing | 1 | 2 |
| Parity, n (%) | ||
| Nulliparous | 443 (61) | 282 (57) |
| Primiparous | 229 (32) | 185 (37) |
| Multiparous | 49 (7) | 31 (6) |
| Missing | 0 | 2 |
| Alcohol during pregnancy (daily intake), n (%) | ||
| 0.4–1 g/day | 18 (3) | 33 (7) |
| 1 g/day or more | 13 (2) | 36 (7) |
| None | 593 (95) | 429 (86) |
| Missing | 97 | 2 |
| Smoking at the beginning of pregnancy, n (%) | ||
| between 1 and 10 cig/day | 10 (2) | 48 (10) |
| more than 10 cig/day | 15 (2) | 19 (4) |
| No smoking | 684 (96) | 427 (86) |
| Missing | 12 | 6 |
| Physical activity, n (%) | ||
| More than 150 min/week | 151 (22%) | - |
| Missing | 21 | - |
| Physical activity (mets) | - | 37.5 [5.6] |
| Missing | - | 2 |
| Sleep time, n (%) | ||
| More than 7 h/day | 554 (79%) | 431 (87%) |
| Missing | 20 | 2 |
| Folic acid supplementation, n (%) | ||
| Yes | 380 (74%) | 408 (82%) |
| Missing | 209 | 0 |
| Mediterranean Diet Score | 4.0 [2.0] | 4.0 [2.0] |
| Missing | 97 | 6 |
| Contraceptive, n (%) | ||
| Yes | 627 (87%) | 452 (90%) |
| Missing | 8 | 1 (0.2%) |
| Type of contraceptive, n (%) | ||
| Hormonal | 145 (20%) | 175 (35%) |
| Season, n (%) | ||
| Autumn | 179 (25) | 139 (28) |
| Spring | 175 (24) | 139 (28) |
| Summer | 214 (30) | 107 (22) |
| Winter | 153 (21) | 111 (22) |
| Missing | - | 4 |
| COVID confinement, n (%) | - | |
| Yes | 194 (27) | - |
| BiSC (n = 721) | INMA (n = 500) | |
|---|---|---|
| Hormone (µmol/L) | Median (IQR) | Median (IQR) |
| 17-hydroxy-pregnenolone: 5PD-20one-S | 1.99 (2.64) | 2.75 (3.85) |
| 17-hydroxy-progesterone: PT-G | 3.27 (2.09) | 4.30 (3.84) |
| 17-hydroxy-progesterone: PT-diS | 0.05 (0.07) | 0.07 (0.12) |
| Corticosterone: A-S | 0.30 (0.20) | 0.35 (0.46) |
| Corticosterone: B-S | 0.39 (0.30) | 0.59 (0.70) |
| Cortisol: 20DHE-G | 0.10 (0.10) | 0.11 (0.15) |
| Cortisol: 20αDHF-G | 0.03 (0.04) | 0.07 (0.08) |
| Cortisol: 20βDHF-G | 0.31 (0.30) | 0.33 (0.48) |
| Cortisol: Cortolone-G_1 | 2.33 (1.76) | 3.85 (4.31) |
| Cortisol: Cortolone-G_2 | 1.08 (0.86) | 2.50 (2.96) |
| Cortisol: E-G | 0.33 (0.22) | 0.58 (0.69) |
| Cortisol: E-S | 0.03 (0.02) | 0.04 (0.04) |
| Cortisol: F-G | 0.08 (0.06) | 0.22 (0.21) |
| Cortisol: F-S | 0.18 (0.12) | 0.28 (0.30) |
| Cortisol: THE-G | 1.74 (1.46) | 3.56 (3.78) |
| DHEA: 16OH-DHEAS_1 | 0.87 (0.65) | 0.63 (0.86) |
| DHEA: 16OH-DHEAS_2 | 0.60 (0.85) | 0.85 (1.44) |
| DHEA: 16OHDHEA-diS_1 | 0.34 (0.38) | 0.39 (0.51) |
| DHEA: 16OHDHEA-diS_2 | 0.12 (0.13) | 0.14 (0.21) |
| DHEA: 5AD-diS_1 | 0.04 (0.04) | 0.05 (0.07) |
| DHEA: 5AD-diS_2 | 0.11 (0.10) | 0.16 (0.20) |
| DHEA: DHEA-S | 0.12 (0.33) | 0.26 (0.97) |
| DHEA: epiAN-S | 0.07 (0.14) | 0.13 (0.26) |
| Estradiol: E1-G | 0.73 (0.70) | 1.12 (1.25) |
| Estradiol: E1-S | 1.59 (3.22) | 2.22 (4.89) |
| Estradiol: E2-S | 0.02 (0.03) | 0.03 (0.05) |
| Estriol: E3-G | 2.69 (1.82) | 2.93 (2.18) |
| Estriol: E3-S | 0.76 (0.90) | 1.02 (1.31) |
| Estriol: E3-SG | 1.05 (1.22) | 1.19 (1.46) |
| Estriol: E4-SG | 0.03 (0.04) | 0.03 (0.05) |
| Pregnenolone: 21OH-5P-diS | 0.20 (0.15) | 0.28 (0.24) |
| Pregnenolone: 5PD-G | 45.04 (30.24) | 52.53 (48.78) |
| Pregnenolone: 5PD-SG | 0.47 (0.44) | 0.52 (0.62) |
| Pregnenolone: 5PD-diS | 2.46 (1.80) | 3.17 (2.95) |
| Progesterone: PD-G | 72.62 (43.54) | 76.60 (57.04) |
| Progesterone: PD-SG_1 | 1.93 (2.27) | 1.64 (2.07) |
| Progesterone: PD-SG_2 | 0.95 (1.36) | 0.68 (1.17) |
| Progesterone: PD-SG_4 | 2.66 (2.46) | 2.82 (3.15) |
| Progesterone: PD-SG_5 | 1.09 (0.98) | 1.14 (1.20) |
| Progesterone: PD-S_1 | 0.61 (0.73) | 0.77 (1.22) |
| Progesterone: PD-S_2 | 6.06 (7.89) | 7.06 (11.94) |
| Progesterone: PD-diS_1 | 1.61 (1.05) | 1.75 (1.28) |
| Progesterone: PD-diS_3 | 0.04 (0.04) | 0.07 (0.09) |
| Progesterone: PD_diS_2 | 0.43 (0.41) | 0.52 (0.67) |
| Testosterone: AN-S | 0.46 (0.63) | 0.83 (1.29) |
| Testosterone: Andros-G | 3.25 (2.63) | 5.62 (6.00) |
| Testosterone: Etio-G | 1.09 (1.12) | 2.27 (2.82) |
| Testosterone: Etio-S | 0.36 (0.45) | 0.78 (1.09) |
| Testosterone: T-G | 0.01 (0.01) | 0.02 (0.02) |
| Testosterone: T-S | 0.02 (0.02) | 0.02 (0.03) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laveriano-Santos, E.P.; Renard-Dausset, E.; Bustamante, M.; Pelegri, D.; García-Ruiz, Z.; Ruiz-Rivera, M.; Cosin-Tomas, M.; Llurba-Olive, E.; Gomez-Roig, M.D.; Haro, N.; et al. Mapping of Determinants of Urinary Sex Steroid Metabolites During Late Pregnancy: Results from Two Spanish Cohorts. Int. J. Mol. Sci. 2025, 26, 11598. https://doi.org/10.3390/ijms262311598
Laveriano-Santos EP, Renard-Dausset E, Bustamante M, Pelegri D, García-Ruiz Z, Ruiz-Rivera M, Cosin-Tomas M, Llurba-Olive E, Gomez-Roig MD, Haro N, et al. Mapping of Determinants of Urinary Sex Steroid Metabolites During Late Pregnancy: Results from Two Spanish Cohorts. International Journal of Molecular Sciences. 2025; 26(23):11598. https://doi.org/10.3390/ijms262311598
Chicago/Turabian StyleLaveriano-Santos, Emily P., Estelle Renard-Dausset, Mariona Bustamante, Dolors Pelegri, Zoraida García-Ruiz, Marina Ruiz-Rivera, Marta Cosin-Tomas, Elisa Llurba-Olive, Maria Dolores Gomez-Roig, Noemi Haro, and et al. 2025. "Mapping of Determinants of Urinary Sex Steroid Metabolites During Late Pregnancy: Results from Two Spanish Cohorts" International Journal of Molecular Sciences 26, no. 23: 11598. https://doi.org/10.3390/ijms262311598
APA StyleLaveriano-Santos, E. P., Renard-Dausset, E., Bustamante, M., Pelegri, D., García-Ruiz, Z., Ruiz-Rivera, M., Cosin-Tomas, M., Llurba-Olive, E., Gomez-Roig, M. D., Haro, N., Pozo, Ó. J., Dadvand, P., Vrijheid, M., & Maitre, L. (2025). Mapping of Determinants of Urinary Sex Steroid Metabolites During Late Pregnancy: Results from Two Spanish Cohorts. International Journal of Molecular Sciences, 26(23), 11598. https://doi.org/10.3390/ijms262311598






