1. Introduction
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder and the leading cause of dementia worldwide [
1]. Its pathological hallmarks include extracellular aggregation of amyloid-β (Aβ) peptides into plaques and intracellular accumulation of hyperphosphorylated tau in the form of neurofibrillary tangles, both of which disrupt synaptic integrity and neuronal homeostasis, leading to widespread neurodegeneration [
2]. Recently, several disease-modifying anti-Aβ monoclonal antibody therapies have entered the clinic; however, significant challenges remain due to their relatively modest effects, the need for serial MRI monitoring to detect potentially severe side effects and the fact that only patients in the early stages of AD can be treated [
3,
4,
5,
6,
7,
8]. Targeting tau has been proposed as a potentially superior therapeutic strategy to amyloid, as the formation of neurofibrillary tangles closely coincides with the onset of dementia symptoms and more accurately predicts patterns of clinical decline [
9,
10,
11]. Various strategies to target tau pathology in AD have previously been explored with multiple approaches in late-stage clinical trials [
8,
12,
13]. Nucleic acid-based therapeutics, such as antisense oligonucleotides (ASOs), provide an opportunity to modify disease progression in AD by downregulating overexpressed genes [
14]. ASOs targeting the
MAPT gene (MAPT-ASOs), which encodes for the tau protein, reduce expression by binding to tau mRNA and recruiting RNase H1, which degrades the transcript and prevents tau protein synthesis [
14]. In a Phase 1b clinical study, the MAPT-ASO candidate BIIB080 demonstrated a dose-dependent and sustained reduction in cerebrospinal fluid (CSF) total tau and phosphorylated tau (p-tau) and is currently being further evaluated in a Phase 2 trial, thus highlighting the clinical potential of MAPT-ASOs in treating AD [
15,
16].
A major obstacle in the development of AD therapies is the limited penetration of drugs into the brain due to the restrictive nature of the blood–brain barrier (BBB) [
17]. The BBB is a highly selective interface at the brain microvasculature, composed of brain microvascular endothelial cells (BMECs), astrocytes, pericytes, and extracellular matrix components such as the vascular basement membrane and the intraluminal glycocalyx [
18]. BMECs are interconnected by complex tight junctions that strongly limit paracellular transport, forcing most therapeutics to rely on the transcellular pathway for entry into the central nervous system (CNS) [
19]. As a result, drug penetration is poor, often necessitating high systemic doses to achieve therapeutic concentrations in the brain [
17]. ASOs are no exception, as their relatively large size, strong negative charge, and hydrophilicity prevent passive diffusion across the BBB [
20]. Consequently, current clinical trials of MAPT-ASOs employ intrathecal administration, an invasive and repeated procedure associated with uneven brain distribution, procedural risks, and limited patient tolerability [
15,
16]. To address these limitations and enable systemic delivery, ASOs can be incorporated into lipid nanoparticles such as liposomes, which provide protection against nuclease degradation, improve pharmacokinetic properties, and enhance cellular uptake and endosomal escape [
21]. Functionalizing these liposomes with surface ligands that bind to receptors overexpressed at BMECs facilitates BBB crossing through receptor-mediated transcytosis, thus allowing for CNS-specific systemic delivery [
22,
23,
24].
Transferrin receptor 1 (TFR1) is preferentially expressed on the luminal surface of BMECs compared to peripheral endothelium, making it an attractive and relatively specific target for delivering substances across the BBB to the CNS [
25]. The physiological role of TFR1 in mediating essential iron transport across the BBB highlights its powerful and active endocytic transport pathway for the delivery of drugs for the treatment of AD. One of the most important features of TFR1 in AD is that its expression levels and functional integrity at the BBB appear to be largely preserved despite AD neuropathology. This is a crucial distinction because many other BBB components, such as tight junctions and efflux transporters, exhibit dysfunction or altered expression in AD, which may complicate the delivery of drugs that rely on their normal function [
26]. Given that transferrin (TF) is a widely tolerated endogenous protein and its conjugates are compatible with scalable chemical systems (EDC/NHS: carboxyl-to-amine; maleimide–thiol; click: fast azide–alkyne), which facilitate its conjugation to various carriers and reduces immunogenicity, in order to allow TF to compete with abundant plasma transferrin and avoid random lysine conjugation interfering with iron binding [
27], TF can be placed on a flexible PEG tether, and the surface density of TF can be manipulated to achieve the required affinity for entering endothelial cells.
To evaluate ASO drug delivery strategies, animal models can be used [
21]. However, due to species-specific differences in BBB properties, such as tight junction complexity and TFR1 density, distribution, and ligand-binding characteristics, the translatability of these studies is limited [
28]. In vitro BBB models provide an alternative, yet conventional transwell systems fail to capture the 3D architecture, lack dynamic flow and are further biased by introducing a stiff membrane with non-physiological properties at a critical location in the BBB model [
29]. Self-assembled BBB organoids offer potential high-throughput tools for permeability studies, including nanoparticle evaluation, but they lack a full BBB architecture, allow only for semi-quantitative assessments and may be complex and lengthy to establish [
30,
31]. Hydrogel-based approaches present significant advantages, as cells can organize with cell–cell and cell–extracellular matrix (ECM) interactions that reflect in vivo BBB anatomy. Previous studies have evaluated nanoparticles using hydrogel-based transwell-like systems or self-assembled capillary structures in wells with perfusable openings [
32,
33]. However, these systems still lack fluid flow, an essential factor in BBB physiology and nanoparticle attachment. Microfluidic BBB chips address this limitation by incorporating micro-sized channels that allow controlled fluid flow and simultaneous cell culture [
29,
34,
35,
36,
37]. Previously, a perfusable BBB microvasculature network (MVN) model has been developed through self-assembly of BMECs, astrocytes, and pericytes within a fibrin hydrogel in a microfluidic chip [
38,
39]. This model accurately recapitulates in vivo BBB architecture, including the formation of luminal microvessels with astrocytes and pericytes actively aligning and interacting with the endothelium [
38,
39]. Moreover, physiologically relevant expression and localization of BBB membrane transporters, tight junction proteins, and extracellular matrix components, as well as cytokine production, were observed, with permeability values comparable to those observed in rat brains [
38,
39]. Importantly, TFR1 expression in BMECs increases during the formation of the MVNs [
39] and is ultimately higher in BMECs cultured as MVNs than in 2D monocultures [
38], highlighting how such approaches enhance physiological relevance and are therefore particularly suitable for studying TF-mediated delivery. Previous studies have shown that nanoparticle size and functionalization can be effectively evaluated for BBB permeability using this BBB MVN model alone or combined with a tumour spheroid [
40,
41].
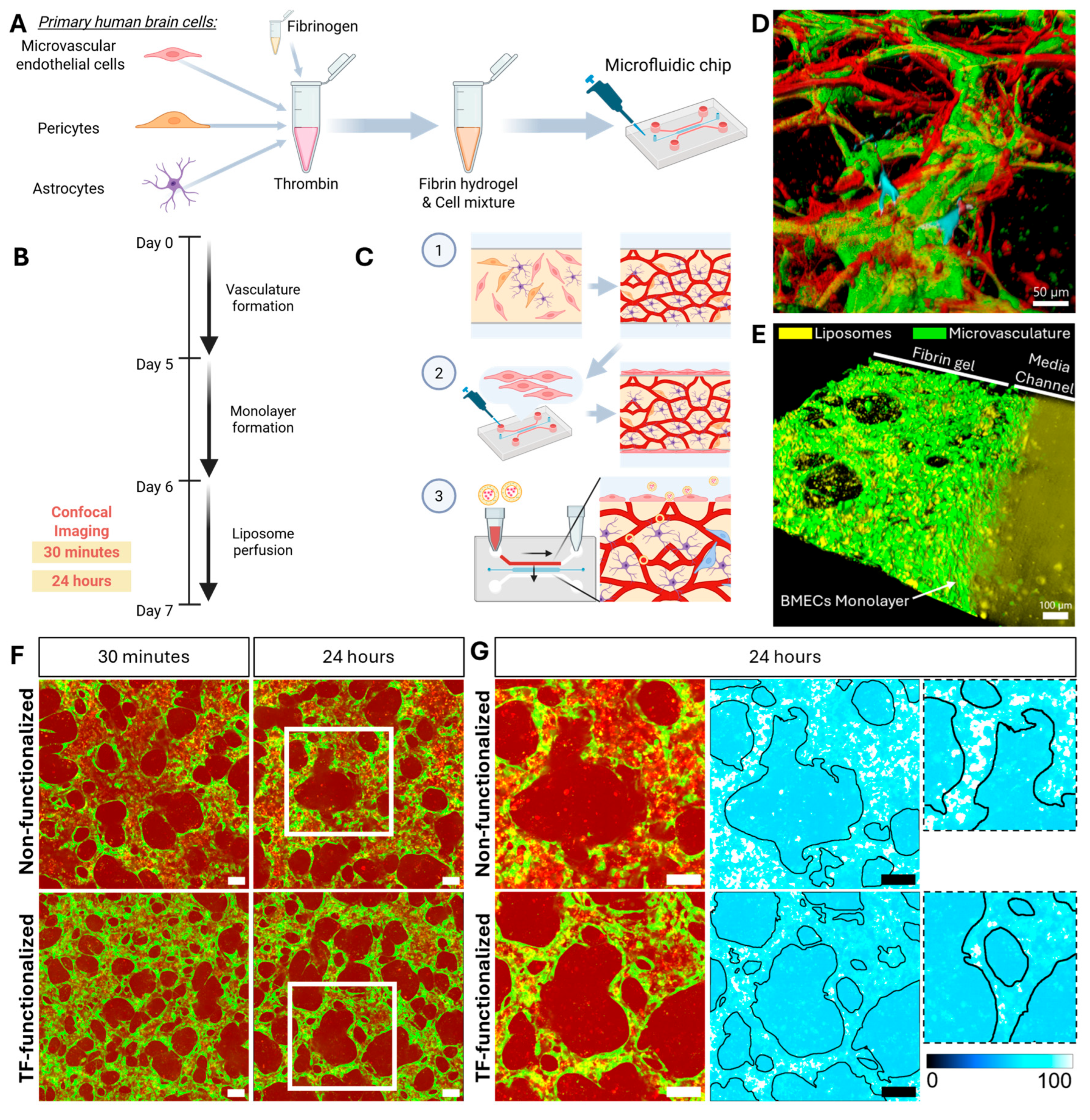
In this study, we investigated whether TF-functionalized liposomes encapsulating MAPT-ASOs could enhance BBB permeability using the previously published and well-characterized 3D BBB MVN in vitro model [
38,
39,
40]. We hypothesized that TF functionalization would enhance the permeability of MAPT-ASO-loaded liposomes across the BBB MVN in vitro model. To test this, TF-functionalized and control liposomes were perfused through the BBB MVNs, and MAPT-ASO delivery was monitored by fluorescent labelling and confocal microscopy to assess translocation across the BBB over 24 h. The results demonstrated that transferrin-functionalized liposomes enabled enhanced transport of the functionally effective MAPT-ASO to extravascular regions within the BBB MVN. These findings reveal a new strategy for MAPT-ASO brain delivery and provide novel methodologies for leveraging the 3D BBB MVN model as a versatile platform for nanoparticle evaluation.
3. Discussion
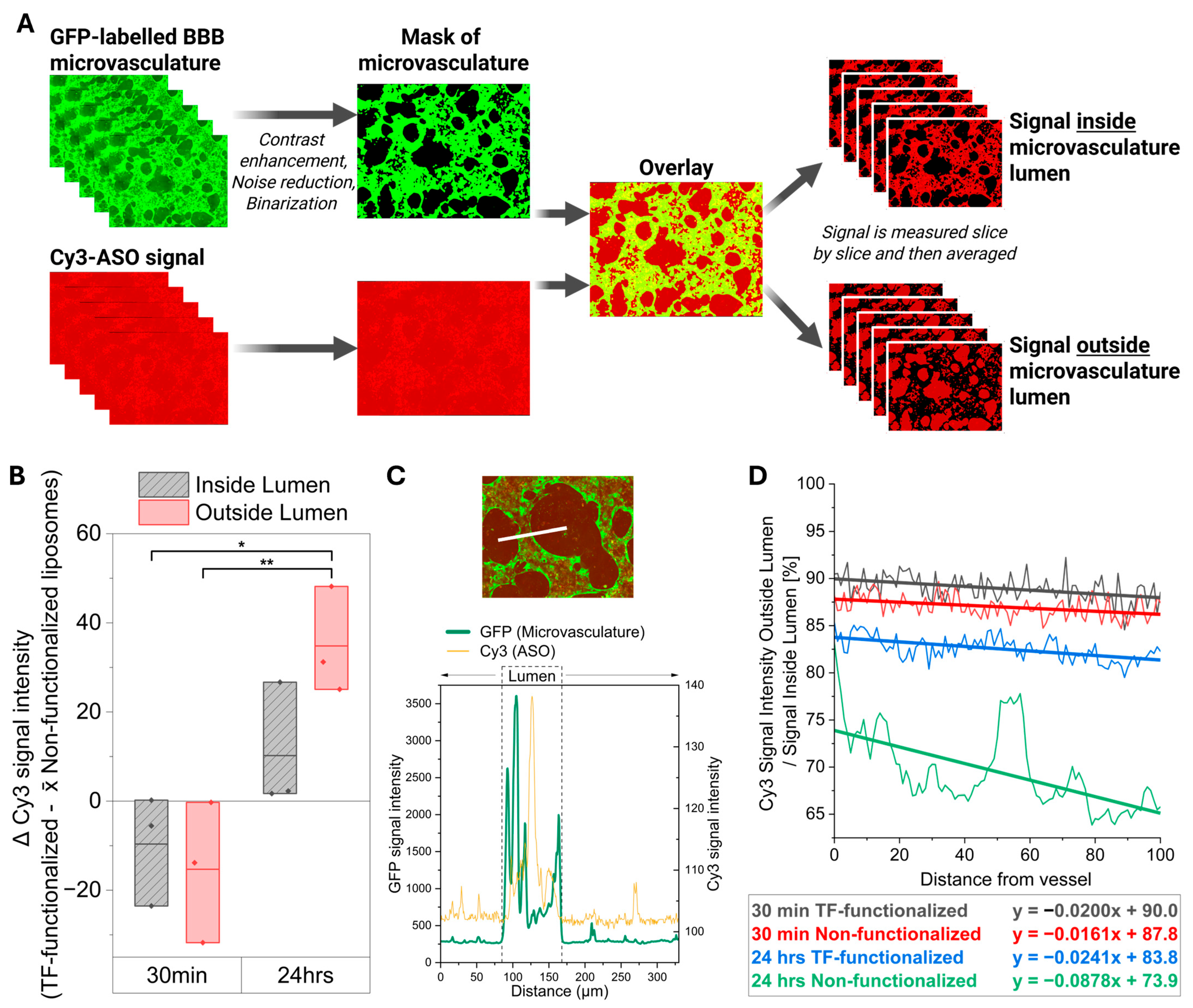
In this study, we evaluated whether transferrin-functionalized liposomes loaded with antisense oligonucleotides targeting the MAPT gene (MAPT-ASO) could enhance delivery across the BBB in a 3D in vitro model of human brain microvasculature. After demonstrating that the here-used MAPT-ASO was indeed effective in lowering tau levels and protecting against axonal degeneration, we then showed that transferrin-functionalized liposomes were able to enhance the delivery of the MAPT-ASO across the BBB after 24 h compared to the non-functionalized liposomes. Therefore, this study presents a novel delivery strategy for a functionally effective tau-targeting ASO, which could potentially enable systemic delivery of these promising therapeutics for Alzheimer’s disease. Furthermore, it highlights the utility of the 3D BBB microvasculature network in vitro model as a versatile and translational platform for evaluating the brain delivery of nucleic acid-based therapeutics.
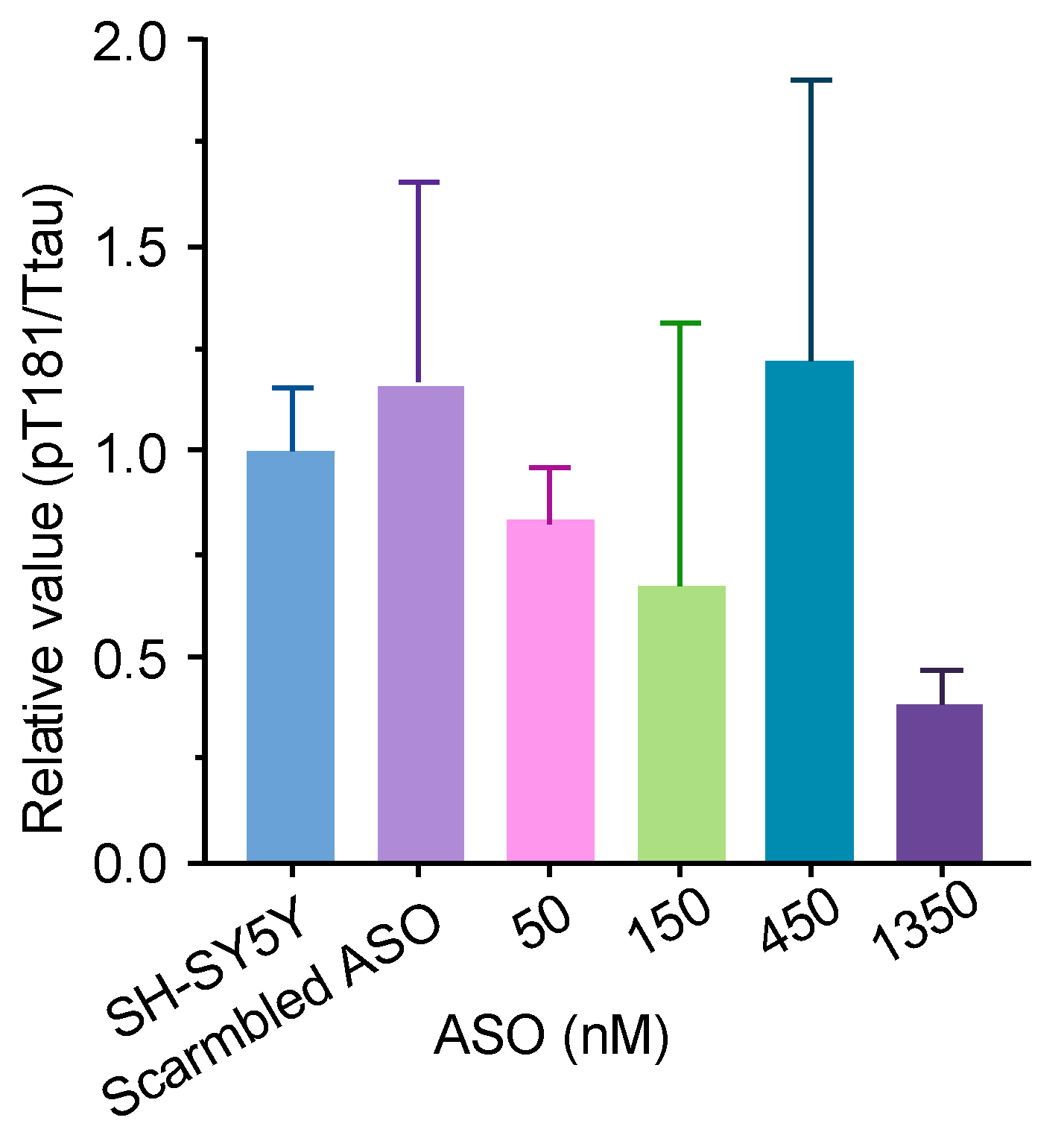
The ASO used here is a fully phosphorothioate oligo directly targeting human MAPT pre-mRNA. By hybridizing to MAPT mRNA, the ASO recruits RNase H1 to cleave the target transcripts, thereby lowering MAPT mRNA and reducing tau protein synthesis [
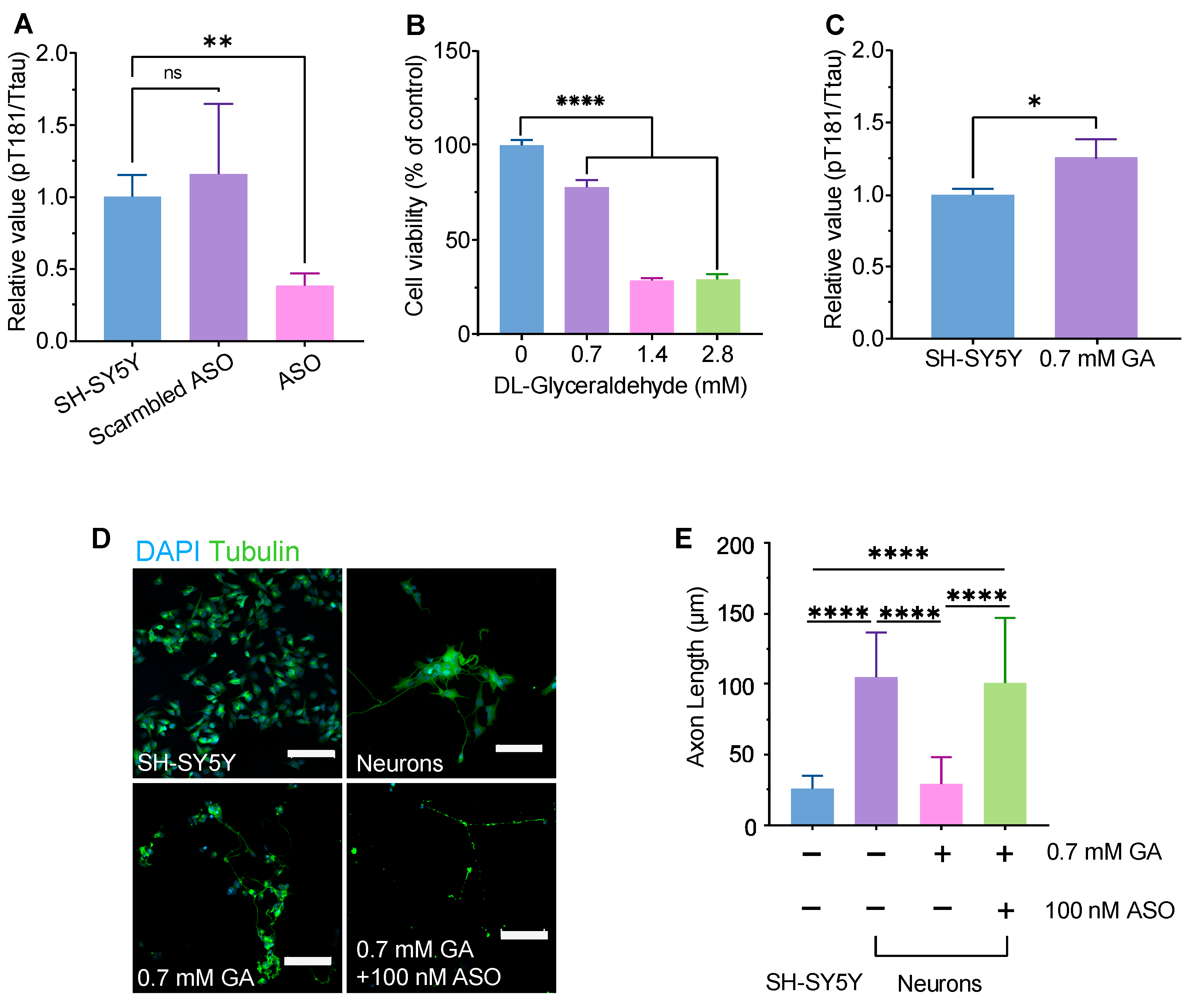
44]. Using a well-established GA-induced axonal degeneration approach in SH-SY5Y–derived neurons [
45], we found that GA reduced viability in a dose-dependent manner (0.7–2.8 mM). CLSM revealed marked neurite fragmentation after 0.7 mM GA, which was rescued by co-treatment with the MAPT-ASO. GA significantly shortened axons relative to untreated neurons, whereas GA + MAPT-ASO significantly increased axon length compared with GA alone. In parallel, the MAPT-ASO significantly lowered the pT181/total Tau ratio versus both untreated and scramble-ASO controls. These results illustrate that MAPT knockdown reduces pathogenic tau phosphorylation at Thr181 and mitigates axonal damage under metabolic stress in this neuronal model. These findings align with prior human data showing that intrathecal administration of this MAPT-targeting ASO produces reductions in CSF tau species and engages its intended RNase-H mechanism in patients with early AD [
16]. Future studies should evaluate the long-term effects of MAPT-ASO treatment on neuronal connectivity and synaptic function, as well as its efficacy in in vivo models of Alzheimer’s disease.
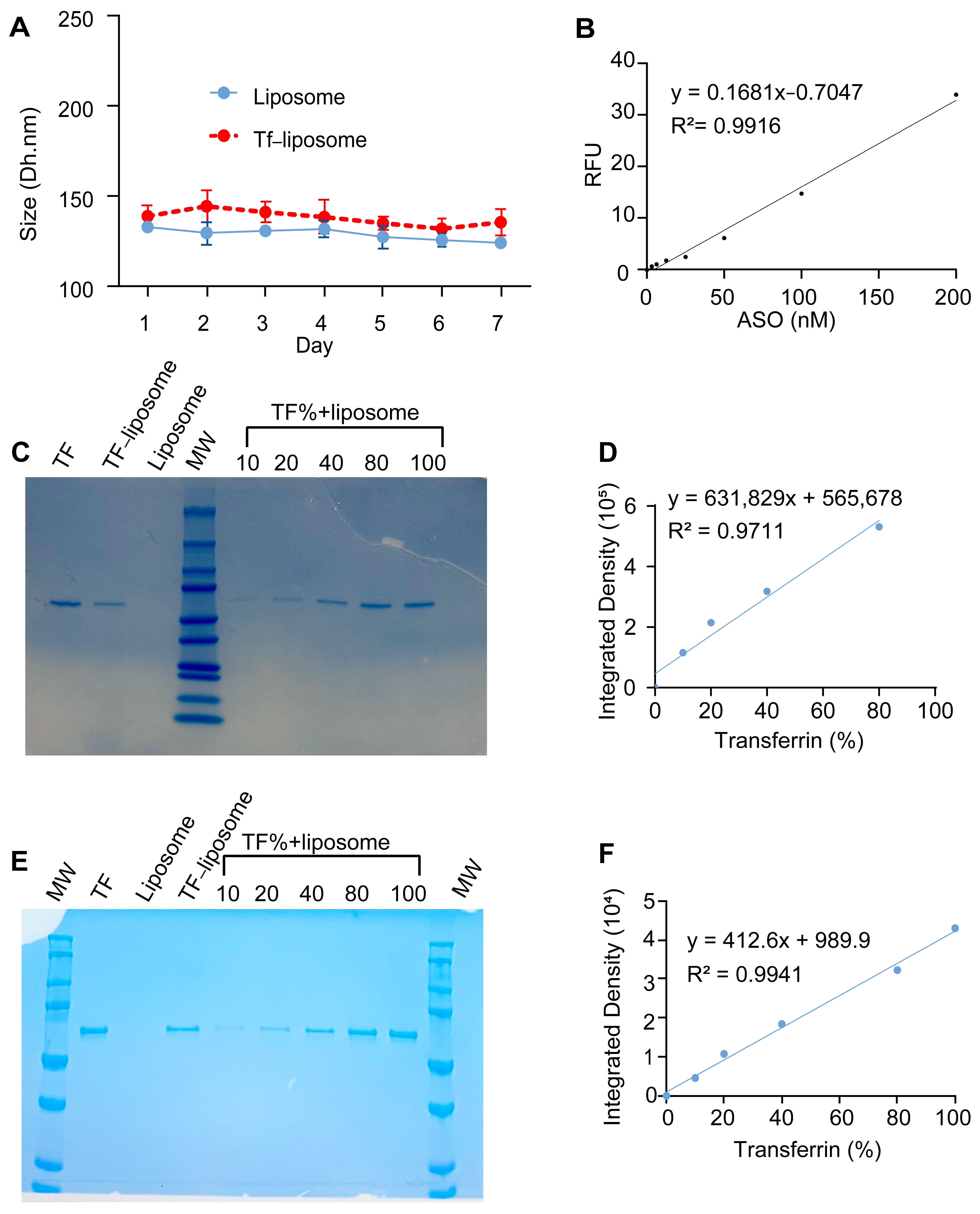
The liposomes prepared in this study exhibited a particle size of 132.8 nm, which increased only modestly to 139.4 nm after TF functionalization. This size falls within the optimal range for crossing the BBB via receptor-mediated transcytosis and is also favourable for efficient endocytosis by neuronal cells. The slight decrease in PDI from 0.201 to 0.189 further confirms that the liposome population remained highly monodisperse and uniform during TF attachment. The slightly negative ζ-potential (−4.04 and −4.65 mV) indicates minimal electrostatic stabilization; however, steric hindrance from PEG chains likely ensures colloidal stability, while near-neutral charge may reduce nonspecific interactions and improve biocompatibility. During perfusion in the microvasculature BBB network model, some aggregation was visible, further highlighting the need for additional improvements in colloidal stability in future formulations. However, during storage at 4 °C, the liposomes remained stable over 7 days, showing no significant change in size, confirming the robustness of the formulation. Transferrin was covalently conjugated to the liposome surface via the carboxyl group of DSPE-PEG(2000)-COOH, allowing stable grafting while preserving the protein’s orientation and functionality for receptor recognition, which is critical for efficient receptor-mediated uptake. The MAPT-ASO encapsulation efficiency (48.3 ± 1.6%) and TF grafting rate (39.2 ± 11.2%) are sufficient to demonstrate payload delivery and receptor-mediated targeting in this study, though affinity-based or density-based separation techniques could further improve payload retention and reduce variability. Overall, these physicochemical characteristics, combined with TF functionalization, support receptor-mediated transport across the BBB and effective MAPT-ASO delivery to neuronal cells.
As expected, TF-functionalized liposomes improved MAPT-ASO delivery across the BBB within the microvascular network model. While transferrin receptor-mediated delivery has been previously explored, this study advances the field by integrating TF-functionalized liposomes with a perfusable 3D in vitro BBB microvascular platform that recapitulates key anatomical and physiological features of the human neurovascular unit. Unlike conventional 2D monolayer models, this system enables dynamic assessment of ASO transport under flow conditions, provides spatial resolution of liposomal distribution across vascular and extravascular compartments, and offers a more predictive representation of human BBB behaviour due to the use of human cells that interact in a physiologically relevant manner. This combination of targeted nanocarrier design and a biomimetic microvascular model offers a novel and translationally relevant strategy for preclinical evaluation of CNS-directed therapeutics, bridging the gap between in vitro screening and in vivo application. In contrast to prior work using a 3D microvasculature BBB model with iPSC-derived endothelial cells (iPSC-ECs), we employed human primary brain microvascular endothelial cells (BMECs) to evaluate nanoparticle transport. In 2D cultures, BBB-relevant genes, including genes of interest for drug delivery such as TFR1 and Low-Density Lipoprotein Receptor-Related Protein 1 (LRP1), were higher in BMECs compared to iPSC-ECs and human umbilical vein endothelial cells (HUVECs) [
40]. However, the difference between iPSC-ECs and BMECs diminished when cultured in the 3D co-culture model, suggesting that interactions with astrocytes and pericytes may play a more critical role than the endothelial cell source, a notion we similarly observed recently, also in HUVECs [
38,
46]. However, BMECs can sustain microvascular networks for longer periods than iPSC-ECs and, in our experience, are easier to incorporate into the microvasculature model [
38].
Earlier studies assessed liposome permeability based on changes in fluorescence intensity within the first 5–30 min after nanoparticle administration, a strategy commonly used for barrier integrity testing with tracers such as dextran. However, while this approach is appropriate for detecting paracellular leakiness of small tracer molecules, TF-functionalized liposomes, being substantially larger in size, primarily cross the BBB via receptor-mediated transcytosis [
47]. This process involves luminal binding and endocytic internalization, followed by vesicular trafficking through endosomal compartments and subsequent abluminal fusion to release the cargo into the perivascular space, a sequence of events that involves complex kinetics, which are likely very different from paracellular transport [
48,
49]. Moreover, PEGylated liposomes in humans (e.g., Doxil
®) exhibit a circulation half-life of approximately 20 to 50 h, further supporting that longer assessment periods are necessary to capture this sustained exposure. Indeed, we observed a marked increase in MAPT-ASO delivery efficiency across the extravascular space only after 24 h. Within the immediate perivascular region, TF-functionalized liposomes provided only a modest improvement after 30 min, but this effect became much more pronounced by 24 h. This finding is particularly relevant as neurons in vivo are typically located within 10–20 µm of brain capillaries, underscoring that TF-functionalized liposomes can substantially enhance MAPT-ASO delivery to their potential neuronal targets over time.
The hereby observed gradual increase in extravascular accumulation of the labelled-MAPT-ASO is likely the result of rate-limiting processes during receptor-mediated transcytosis. For example, limited availability and oversaturation of TFR1s may initially restrict the number of liposomes that can be transported across the endothelium. However, as TFR1s are actively recycled at the BBB [
50], continuous receptor-mediated transcytosis could occur over the 24 h period, leading to the observed gradual increase in MAPT-ASO accumulation within the extravascular space. Other factors, such as exocytosis, which has been proposed as the rate-limiting process during receptor-mediated transport of anti-TFR1 monoclonal antibodies, could also be important [
49]. Future studies could employ this platform to further investigate and optimize liposomal and cargo trafficking kinetics, as well as TFR1 recycling dynamics, which have previously been shown to be strongly influenced by ligand–receptor binding affinity [
50].
Although liposomes consistently enter cells and exhibit enhanced BBB permeability in in vitro models, studies have demonstrated that, when nanoparticles are handled in complex environments, they are rapidly covered by a layer of adsorbed plasma proteins or interact with other proteins in the culture medium and form protein coronas [
51]. For transferrin-targeted formulations, several studies have shown that corona formation can sterically shield surface-bound TF and reduce its effective affinity for the transferrin receptor, leading to diminished receptor-mediated uptake and attenuated brain delivery [
52]. In this study, we performed preliminary stability assessments in a PBS and FBS mixture. Both liposomes and TF–liposomes maintained relatively stable particle sizes and ζ potential at 37 °C in serum, indicating that the formulations remain stable under simplified physiological conditions. Nevertheless, such in vitro assays cannot fully reproduce the dynamic and compositionally diverse protein corona that forms in vivo, and therefore do not fully predict the extent to which TF will remain functionally accessible in the bloodstream. Future work may focus on determining how its composition influences TF receptor binding and subsequent biodistribution. In addition, formulation strategies such as adjusting PEG architecture or incorporating surface chemistries that mitigate ligand masking will be explored to better preserve the specificity of transferrin–receptor interactions after systemic administration [
53].
Since liposomes circulate through the brain microvasculature under flow, which likely affects margination and ligand-receptor binding [
54,
55], we applied transient fluid flow using a simple hydrostatic pressure-driven setup, as previously described [
56,
57,
58]. This approach produced a more homogeneous distribution of liposomes across the MVNs compared to static conditions. Consistent with prior reports, we observed that transient fluid flow also promoted larger vessel diameters [
57]. Due to the induced shear stress and the associated beneficial signalling in BMECs [
59], previous studies have shown that fluid flow can extend BBB MVN model viability and enhance MVN perfusability [
56,
57,
60]. Therefore, future studies incorporating stable flow generated by micropumps could support long-term liposome testing, including pre-conditioning and repeated dosing. Integrating such flow systems with robotic handling and automated image analysis would convert the BBB MVN model into a predictive high-throughput platform, as exemplified by other commercially available BBB organ-on-chip systems [
34]. The self-assembled BBB MVN model recapitulates essential microvascular architecture and employs human-derived cell types, features that are expected to enhance translational fidelity relative to simpler BBB in vitro models. Future studies should pursue rigorous validation and directly benchmark the model’s predictive accuracy against in vivo and human clinical data, thereby establishing its suitability as a high-throughput platform for systematic evaluation of BBB drug delivery strategies [
29].
Our study is limited by its focus on liposome-mediated MAPT-ASO delivery in healthy conditions as well as the lack of in vivo investigations. Given that BBB dysfunction is a key feature of AD pathology, future work should evaluate liposome-mediated MAPT-ASO delivery in an AD context. Previous studies have modelled AD in BBB MVNs by co-culture with neurons carrying familial AD (FAD) mutations, resulting in significantly altered gene expression and permeability in MVNs [
56,
58]. However, MVN morphology and perfusability were also significantly altered, making efficient nanoparticle perfusion in AD-impacted MVNs difficult to achieve. Future in vivo studies should focus on evaluating whether intravenously administered TF-functionalized liposomes enhance the transport of MAPT-ASO into the brain parenchyma and whether this results in effective reduction in tau mRNA, total tau, and phosphorylated tau levels. Using humanized transgenic animal models, for example, TfR
mu/hu knock-in (KI) mice, which express a humanized transferrin receptor 1 at the BBB, and human tau
tg/− mice, which express the human MAPT gene on a murine tau null background, allows simultaneous assessment of receptor-mediated BBB transport and target engagement of MAPT-directed therapeutics under human-relevant conditions [
61,
62,
63,
64]. In combination with quantitative methods to assess MAPT-ASO penetration across the BBB, such as the capillary depletion technique, fluorescent labelling with co-localization analysis, and blocking or competition studies to confirm transferrin receptor dependence, these experiments would provide comprehensive validation of the liposomal delivery strategy presented here. Given the enhanced biomimicry of the 3D BBB model used in this study, the presented results are expected to have improved translatability to in vivo systems.
4. Materials and Methods
4.1. Study Design
This study was designed to (1). evaluate the effectiveness of a MAPT-ASO in reducing tau levels and protecting against GA-induced axonal degeneration and (2). assess the ability of TF-functionalized liposomes to deliver the MAPT-ASO across a 3D in vitro BBB model. To assess MAPT-ASO efficacy, pT181/total tau ratios were quantified following treatment with MAPT-ASO, scrambled ASO, or vehicle-only controls, while protection against GA-induced axonal degeneration was evaluated relative to untreated samples. For BBB transport experiments, Cy3-MAPT-ASO-loaded liposomes with or without TF-functionalization were compared. Cy3-MAPT-ASO delivery was assessed at two timepoints: 30 min and 24 h post-perfusion through the BBB model.
4.2. Materials
Cells: SH-SY5Y cells (Manassas, ATCC, VA, USA), green fluorescent protein (GFP)-labelled human BMECs (AngioProteomie, Boston, MA, USA; #cAP-0002GFP, Lot: 2022062302), human brain vascular pericytes (ScienCell, Carlsbad, CA, USA; Cat#1200, Lot: 33155), and human brain astrocytes (ScienCell, #1800, Lot: 34727).
Cell culture media: SH-SY5Y media (Essential Medium Eagle Medium (EMEM, Sigma Life Science, St. Louis, MO, USA), 10% (v/v) fetal bovine serum (FBS, Sigma Life Science), 1% (v/v) Penicillin–Streptomycin (P/S, Sigma Life Science)), BMEC media (VascuLife VEGF medium (Lifeline Cell Technology, Frederick, MD, USA), 10% FBS (Life Technologies, Carlsbad, CA, USA), pericyte medium (ScienCell), and astrocyte medium (ScienCell).
Other reagents for cell culture: 0.25% trypsin-EDTA (Gibco, Paisley, UK), Phosphate-buffered saline (PBS, Gibco), human fibronectin (Life Technologies), TrypLE Express (Life Technologies), and 0.05% trypsin-EDTA (ScienCell).
ASOs: Scrambled ASO (sequence: 5′-ACCCTTCGAGCTTGAGAGTT-3′) or MAPT-ASO (sequence: 5′-GCTTTTACTGACCATGCGAG-3′), unlabelled or labelled with Cyanine3 (Cyanine3) (Genscript, Oxford, UK). Synthesized with a phosphorothioate backbone.
Liposome preparation: DSPC, CHOL, DSPE-PEG(2000) and DSPE-PEG(2000)-COOH (Avanti Polar Lipids, Alabaster, AL, USA), chloroform (Thermo Fisher, Paisley, UK), 1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide hydrochloride (EDC·HCl) and N-hydroxysulfosuccinimide (sulfo-NHS, Thermo Fisher), transferrin (TF, Sigma, Life Science), 300,000 MWCO Spectra/Por® Dialysis Membrane (Cole-Parmer, St. Neots, UK), 10,000 molecular weight cut-off (MWCO) SnakeSkin™ Dialysis Tubing (Thermo Fisher), Zetasizer Nano (Malvern Instruments Ltd., Malvern, UK).
Microfluidic BBB in vitro model: Polydimethylsiloxane (PDMS, Sylgard 184 Silicone Elastomer Kit Dow, Dow, Cheadle, UK), #1 glass coverslips (Agar Scientific, Stansted, UK), bovine fibrinogen (Merck Life Science, Gillingham, UK), PBS (calcium/magnesium free, Life Technologies), thrombin (Sigma-Aldrich, St. Louis, MO, USA), BBB model culture medium (Vasculife VEGF endothelial medium (Lifeline Cell Technology) prepared with 0.1875 U/mL of heparin and 2% FBS).
Immunofluorescence staining: Paraformaldehyde (PFA; Electron Microscopy Sciences, Hatfield, PA, USA), BSA (Sigma-Aldrich), Triton X-100 (Sigma-Aldrich), normal goat serum (Abcam, Cambridge, UK), Alexa Fluor® 488 anti-beta III Tubulin antibody (#ab195879, Abcam), anti-glial fibrillary acidic protein antibody (#ab33922, Abcam), anti-rabbit Alexa Fluor 647 (#4414, Cell Signaling, Danvers, MA, USA), Phalloidin labelling probe (#A12381, Invitrogen, Paisley, UK), and DAPI (Sigma-Aldrich).
Other reagents: Lipofectamine 2000 (Thermo Fisher, UK), Cell lysis buffer (Radio-Immunoprecipitation Assay buffer (RIPA, Thermo Fisher), phosphatase and protease inhibitor (Thermo Fisher)), pT181 tau and total tau ELISA assay kits (Thermo Fisher), glyceraldehyde (GA, Thermo Fisher), 3-(4,5-Dimethylthiazol-2-yl)-2,5-Diphenyltetrazolium Bromide (MTT, Thermo Fisher), and dimethyl sulfoxide (DMSO, Thermo Fisher).
4.3. Cell Culture, ASO Transfection and Protein Extraction
SH-SY5Y cells (ATCC, VA, USA) were cultured in Essential Medium Eagle Medium (EMEM, Sigma Life Science) supplemented with 10% (v/v) fetal bovine serum (FBS, Sigma Life Science) and 1% (v/v) Penicillin–Streptomycin (P/S, Sigma Life Science) in 6-well plates for 24 h. Cells were then transfected with 1.35 mM of scrambled ASO or ASO using Lipofectamine 2000 (Thermo Fisher). Scrambled ASO sequence: 5′-ACCCTTCGAGCTTGAGAGTT-3′; ASO sequence: 5′-GCTTTTACTGACCATGCGAG-3′. After an additional 72 h of incubation, cell lysates were prepared. First, SH-SY5Y cells were detached by 0.25% trypsin-EDTA (Gibco) for 2 min. After the cells were centrifuged at 125× g for 5 min, the resulting pellets were washed twice with ice-cold PBS (Gibco). Radio-Immunoprecipitation Assay buffer (RIPA, Thermo Fisher) supplemented with 1× phosphatase and protease inhibitor (Thermo Fisher) was prepared as the lysis buffer to lyse cell pellets for 30 min on ice. Then, the lysates were centrifuged at 12,500 rpm for 15 min at 4 °C. Subsequently, the supernatant was collected and transferred into a new microcentrifuge tube for subsequent use.
4.4. Enzyme-Linked Immunosorbent (ELISA) Assay
ELISA assays for pT181 and total tau (Thermo Fisher) were performed according to the manufacturer’s protocols. For pT181 quantification, 50 µL of each sample was mixed with 50 µL of detection antibody solution and incubated at 4 °C for 17 h. For total tau quantification, 50 µL of each sample was mixed with 50 µL of standard dilution buffer and incubated at room temperature for 2 h. Following incubation, wells were aspirated and washed four times with 1× Wash Buffer. Subsequently, 100 µL of the corresponding conjugate solution (anti-rabbit IgG HRP for pT181; human total tau–biotin conjugate followed by streptavidin–HRP for total tau) was added to each well and incubated for 30 min at room temperature. After washing, 100 µL of stabilized chromogen was added and incubated for 30 min in the dark. Reactions were terminated with 100 µL of Stop Solution, and absorbance was measured at 450 nm within 2 h.
4.5. Cell Viability Assay
SH-SY5Y cells were cultured in minimum essential medium supplemented with 10% v/v FBS and 1% v/v P/S in 96-well plates for 24 h, followed by treatment with glyceraldehyde (GA, Thermo Fisher) at a concentration of 0, 0.7, 1.4, and 2.8 mM. All assays were performed after an additional 24 h of incubation. MTT solution was then added to each well to a final concentration of 0.455 mg/mL. After 2 h of incubation, the 3-(4,5-Dimethylthiazol-2-yl)-2,5-Diphenyltetrazolium Bromide (MTT, Thermo Fisher) solution was removed, and 100 µL of dimethyl sulfoxide (DMSO, Thermo Fisher) was added to each well. The absorbance was measured at 490 nm by a Tecan plate reader. Data was analyzed using One-way analysis of variance (ANOVA).
4.6. Neuron Differentiation
Based on slight modifications of methods previously reported by Uras et al. [
45], SH-SY5Y cells were differentiated using the established three-stage protocol and then challenged with GA to generate the GA-induced neuronal model. Specifically, SH-SY5Y cells were diluted to 1.5 × 10
5 cells/mL, and 2 mL of the suspension was seeded into 35 mm Petri dishes. After 2 days, the medium was replaced with differentiation medium #1 and subsequently changed every 48 h for 5 days. After that, the cells were cultured in differentiation medium #2 for 2 days. Cells were then detached and seeded onto extracellular matrix (ECM) coated dishes. For ECM coating, the ECM solution was diluted 1:100 in cold DMEM, and 2 mL of the mixture was added to each 35 mm dish. After overnight incubation, the solution was aspirated and the dishes were air-dried. One day after seeding on ECM-coated dishes, the medium was replaced with differentiation medium #3 and then changed every 3 days to maintain neuronal health. Neurons were treated either with 0.7 mM GA alone or with GA plus 100 nM of ASO delivered using Lipofectamine 2000 and incubated for 72 h.
4.7. Two-Dimensional Immunofluorescence Staining, Imaging, and Neurite Analysis
Glass coverslips were coated with poly-L-lysine for 1 h at room temperature, rinsed three times with sterile water, and then dried completely. SH-SY5Y cells were seeded on a glass-based dish for differentiation. Before fixation, cells were rinsed briefly in PBS-T and were fixed in 4% PFA for 10 min at room temperature. Samples were washed three times with PBS-T and blocked with 1% BSA for 30 min. After blocking, samples were incubated overnight at 4 °C with Alexa Fluor® 488 anti-beta III Tubulin antibody (#ab195879, Abcam) and washed three times in PBS-T. Samples were subsequently stained with DAPI for 15 min and then washed three times in PBS-T. The samples were imaged by Axio Observer Z1/7 Confocal Microscope. Z-stack images were acquired covering a distance of 138 μm. NeuronJ plug-in was performed after background subtraction, with distinct colours assigned to individual traces. Neurite lengths were quantified with the Measure tracing function, and results were analyzed by ANOVA.
4.8. Liposome Preparation
The liposomes were prepared by the thin-film hydration method. DSPC, CHOL, DSPE-PEG(2000) and DSPE-PEG(2000)-COOH (Avanti Polar Lipids) were dissolved in chloroform (Thermo Fisher) with a molar ratio of 2:1:0.11:0.021; then, the solution was evaporated at 35 °C under a vacuum condition to remove the organic solvent until the thin film formed. Residual chloroform was further removed by overnight incubation in a vacuum desiccator at room temperature. The thin film was then hydrated with 4 mL of PBS with Cyanine3-MAPT-ASO (Cy3-MAPT-ASO). The suspension was vortexed and sonicated (40 kHz, 25 °C, Allendale Ultrasonics, Hoddesdon, UK) at room temperature for 10 min to prepare liposomes containing ASO and followed by extrusion 21 times through a 100 nm polycarbonate membrane to reduce particle size. Free Cy3-MAPT-ASOs were separated from liposomes by dialysis through 10,000 molecular weight cut-off (MWCO) SnakeSkin™ Dialysis Tubing (Thermo Fisher). After the MAPT-ASO-loaded liposome was prepared, it was activated by 1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide hydrochloride (EDC·HCl) and N-hydroxysulfosuccinimide (sulfo-NHS, Thermo Fisher) for 15 min at room temperature at pH 5.5. TF was added to the active liposome solution and incubated overnight at 4 °C at pH 7.5. Free TF was separated from TF-ASO–liposome by dialysis through 300,000 MWCO Spectra/Por® Dialysis Membrane (Cole-Parmer).
4.9. Particle Size Determination and Morphology Observation of Liposomes
The Zetasizer Nano (Malvern Instruments Ltd.) was used to characterize the particle size and ζ-potential of the liposomes. The morphology of the liposome was determined by cryogenic transmission electron microscopy (JEM 2100+, JEOL, Tokyo, Japan). Liposomes and TF–liposomes (n = 3) were resuspended in PBS, PBS-FBS (1:1, v/v) to mimic the condition in biological fluids and examine the stability for 7 days and 24 h. The variations in the average diameter in these suspensions were determined by DLS.
4.10. Determination of Encapsulation Efficiency and Conjugation of Transferrin
The fluorescence intensity of Cy3-MAPT-ASO was used to prepare a calibration curve. After dialysis, the fluorescence intensity of samples was determined via Plate Reader (Tecan, Männedorf, Switzerland), the Cy3 excitation spectrum was obtained at 585 nm emission, and the emission spectrum was obtained at 540 nm excitation, gain was 100. The encapsulation efficiency, expressed as entrapment percentage, was calculated through the following relationship (1):
where C
A is the MAPT-ASO concentration in dialysed liposomes, and C
At is the MAPT-ASO concentration initially introduced.
Total TF (Thermo Fisher) input was normalized to 100%. A TF calibration curve was generated from serial dilutions of TF. Each standard was mixed 1:1 with liposomes and processed identically to samples. Liposomes and TF served as control groups. Equal volumes were resolved by SDS–PAGE on the same gel, followed by Coomassie staining. Band intensity of TF was quantified in ImageJ (version 1.54r) and fitted to the TF calibration curve. The TF grafting yield on liposomes was calculated from the calibrated TF amount relative to the 100% input.
4.11. Stability Study
The stability of liposomes and TF–liposomes was evaluated after storage at 4 °C for 14 days. Particle size was determined by ZetaSizer Nano with DTS1070 folded capillary zeta cell. Results were then processed using one-way Analysis of Variance (ANOVA). Ordinary one-way ANOVA followed by Tukey’s post hoc test was used to compare size differences between samples at different timepoints (Day 7 and Day 14, respectively). In addition to storage stability, the particle size and ζ-potential of liposomes and TF–liposomes were evaluated during incubation at 37 °C in PBS:FBS (1:1, v/v) for 24 h to assess colloidal stability in a physiologically relevant environment.
4.12. Microfluidic Device Making
Soft lithography techniques were applied to fabricate microfluidic devices made from polydimethylsiloxane (PDMS, Sylgard 184 Silicone Elastomer Kit Dow, Dow, Cheadle, UK), following approaches similar to those described in previous studies [
65,
66,
67]. An acrylic mould (Weatherall Equipment and Instruments, Wendover, UK), 1000 µm thick, was laser-cut based on a design (see
Appendix A Figure A3A) created in AutoCAD (version 2025.0.1, Autodesk, San Francisco, CA, USA) and subsequently affixed to an acrylic base. PDMS was prepared by combining the base elastomer with its curing agent in a 10:1 ratio, following the manufacturer’s guidelines. The resulting mixture was degassed for 30 min in a desiccator to eliminate trapped air. After degassing, the PDMS was poured into the moulds to a depth of 8 mm and cured in an oven at 80 °C for 1.5 h. Once cured, the PDMS structures were extracted from the moulds, and 2 mm and 1.5 mm diameter inlet and outlet ports were created for the medium and hydrogel channels, respectively, using a biopsy puncher. The PDMS components were then soaked in deionized water and sterilized via autoclaving. After drying overnight at 80 °C, the PDMS chips were bonded to #1 glass coverslips using a Corona plasma treatment system (Elveflow, Paris, France). Before device seeding, hydrophobicity was restored by placing the microfluidic chips at 80 °C for at least 4 h.
4.13. Two-Dimensional Cell Culture of BMECs, Astrocytes and Pericytes
Cells were maintained in a humidified incubator (37 °C, 5% CO2). Green fluorescent protein (GFP) labelled human brain microvascular cells (BMECs) (AngioProteomie; #cAP-0002GFP, Lot: 2022062302) were cultured in VascuLife vascular endothelial growth factor (VEGF) medium (Lifeline Cell Technology) supplemented with 10% FBS (Life Technologies). Cells were expanded in human fibronectin-coated (3 µg/cm2, Life Technologies) flasks, and media were changed every other day. Cells were passaged using TrypLE Express (Life Technologies) and used at passages 2–4 for experiments.
Primary human brain vascular pericytes (ScienCell; Cat#1200, Lot: 33155) and human brain astrocytes (ScienCell; #1800, Lot: 34727) were cultured as recommended by the manufacturer. Pericytes and astrocytes were expanded using pericyte medium (ScienCell, #1201) and astrocyte medium (ScienCell) in flasks coated with poly-L-lysine (2 μg/cm2, ScienCell). Cells were used at passages 2 or 3 for experiments and detached using 0.05% trypsin/EDTA (ScienCell).
4.14. BBB MVN Model Establishment
To establish the 3D microvascular BBB in vitro model, cells were incorporated into a fibrin hydrogel consisting of fibrinogen and thrombin, as described previously [
38]. A 6 mg/mL bovine fibrinogen (Merck Life Science) was prepared in PBS (calcium/magnesium free, Life Technologies) by incubation for 2 h at 37 °C, followed by filtration through a 0.2 μm filter. Thrombin (Sigma-Aldrich) was initially prepared at a concentration of 100 U/mL by dissolving 1 KU thrombin powder in 10 mL PBS (calcium/magnesium free), followed by a 1:25 dilution in Vasculife VEGF endothelial medium prepared with 0.1875 U/mL of heparin and 2% FBS. Thrombin and fibrinogen solutions were prepared under sterile conditions and kept on ice during all procedures.
BMECs, astrocytes and pericytes were detached, centrifuged, and resuspended in culture media to be counted. Cells were spun down again separately and resuspended in thrombin and then combined. The thrombin–cell mixture was mixed in equal parts with fibrinogen to form the fibrin hydrogel. Cells were seeded within the fibrin hydrogel at a final concentration of 20 million cells/mL, 1.5 million cells/mL and 3 million cells/mL for BMECs, pericytes and astrocytes, respectively. The fibrin–cell mixture was immediately injected into the central channel of the microfluidic device. Seeded devices were placed in a sterile humidified Petri dish, and fibrin was allowed to polymerize for 30 min within an incubator (37 °C, 5% CO2). Finally, Vasculife VEGF endothelial medium prepared with 0.1875 U/mL of heparin and 2% FBS was added to the media channels. Media were changed every day in the devices.
To prevent liposomes from freely diffusing into the hydrogel without entering the MVN first, a monolayer of BMECs was seeded along the gel interface at day 5 of device culture. To improve cell attachment, media channels were emptied and coated with human fibronectin diluted in culture media (0.03 mg/mL, Life Technologies) for 10 min. BMECs were detached and seeded into one media channel at a concentration of 1.5 million cells/mL in device culture media. The device was tilted 45° for 10 min to improve monolayer formation along the gel via gravity. Subsequently, the same was performed for the opposing media channel.
4.15. Three-Dimensional Immunofluorescence Staining and Imaging
At day 7 of BBB MVN culture, immunofluorescence staining was performed in a similar fashion as described previously [
38]. Briefly, media were removed, and devices were washed and then fixed with 4% paraformaldehyde (PFA; Electron Microscopy Sciences) overnight at room temperature (RT). Subsequently, devices were washed 3 times for 5 min with PBS at RT. Cell membranes were permeabilized with 0.1% Triton X-100 (Sigma-Aldrich) in PBS for 20 min at RT, followed by blocking in 0.1% normal goat serum (Abcam) prepared in 0.1% Triton X-100 for 1.5 h at RT. Immunostaining was performed using a primary antibody against glial fibrillary acidic protein (GFAP; #ab33922, Abcam) diluted 1:100 in the blocking buffer and incubated for 24 h at 4 °C. Devices were washed 3 times for 5 min. Subsequently, secondary antibodies (anti-rabbit Alexa Fluor 647; #4414, Cell Signalling) were diluted in PBS and applied for 2 h at RT. For visualization of filamentous actin, samples were incubated with phalloidin probes (165 nmol; #A12381, Invitrogen) for 20 min at RT. Nuclear staining was performed with DAPI (1:1000; Sigma-Aldrich) for 15 min. Finally, samples were washed again with PBS (3 times, 5 min each at RT) before imaging on an inverted confocal microscope (BC43, Olympus, Tokyo, Japan).
4.16. Liposome Perfusion Across the BBB MVNs
Six days after BBB microfluidic devices were seeded, TF-functionalized liposomes and non-functionalized liposomes were perfused through the MVNs at a concentration of 30 μg/mL. All liposomes were freshly prepared before each experiment and vortexed for 10 s before their use. For liposome perfusion, all media were removed, and on one side, the filled media channel (~100 μL) was replaced with 80 μL. Then pipette tips, with the ends cut to fit tightly, were inserted into the openings of the media channels. On the side where no media were present, 250 μL of liposome solution was added to one tip. This setup allowed liposomes to flow across the media channel (similarly to arterial flow) but also into the MVNs (capillary flow) due to the hydrostatic pressure difference between the two media channels.
4.17. Liposome Permeability Measurements Using Automated Image Processing
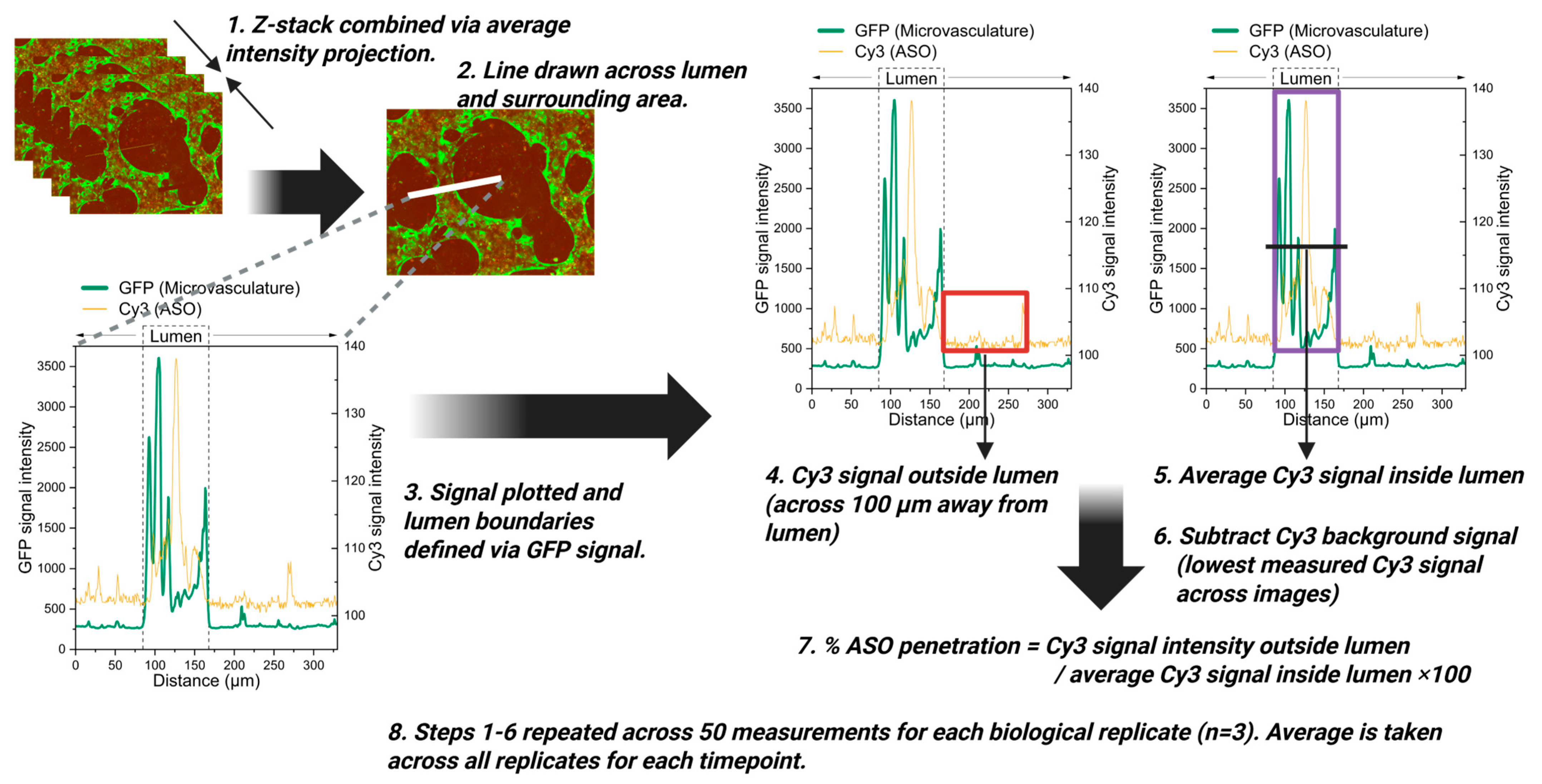
Thirty minutes after liposomes were perfused into the microvasculature, z-stacks of a region of interest (ROI) (1223 μm × 1583 μm) in the central part of the gel channel were taken by confocal microscopy (BC43, Olympus, Tokyo, Japan). Z-stacks covered the whole depth of the microvasculature. The same procedure was performed again 24 h later with the same imaging settings.
To quantify whether liposomes travelled outside the microvasculature, a FIJI [
68] macro was applied to each of the z-stacks (
Figure 4A) [
43]. In summary, the binary mask of the vasculature was used to either quantify the signal intensity of liposomes within this outline or outside of this outline to obtain information about the mean fluorescent signal intensity inside or outside the vasculature, respectively [
43]. Mean signal intensity for each z-slice was then averaged across the z-stack to obtain overall intensity values. Because the analysis was performed using an automated macro, all measurements were effectively blinded to experimental conditions. Raw measurements from TF–liposomes were normalized to the control measurement for each measurement day to prevent day-to-day variability in microscope imaging intensity, using Equation (2) below:
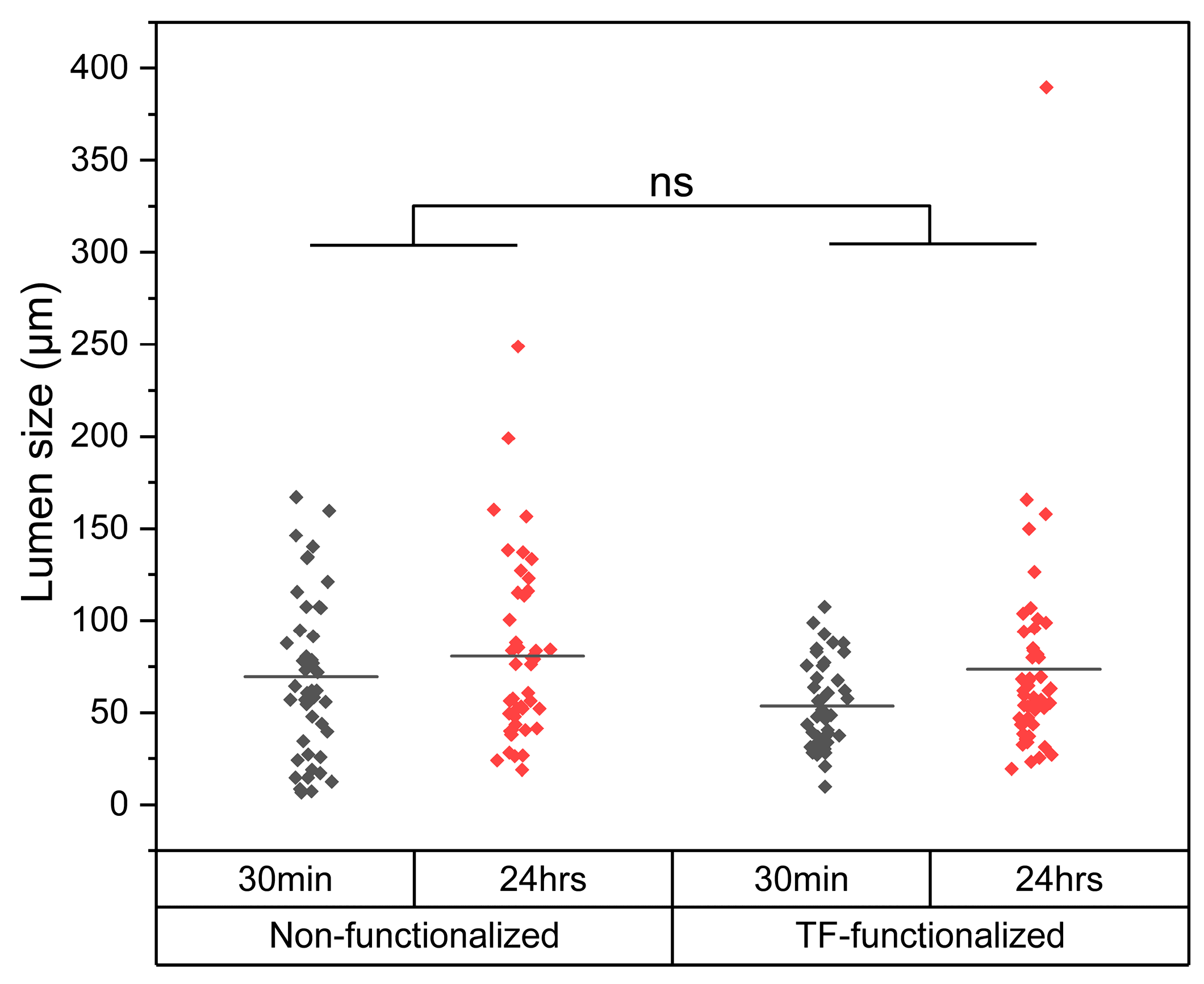
4.18. Liposome Permeability Assessment with Manual Signal Measurements up to 100 µm from the Vessel Lumen
To characterize the kinetics of Cy3-MAPT-ASO-loaded liposome transport across the microvasculature, fluorescence intensity profiles were quantified across the vessel lumen and the surrounding 100 µm of tissue, as shown in
Appendix A Figure A5. Confocal z-stacks were first merged using average intensity projections in FIJI [
68]. In a blinded manner, line scans were drawn perpendicular to selected vessel segments, and the fluorescence intensity of both GFP (microvasculature marker) and Cy3 (ASO signal) was measured using the ‘Line’ and ‘Plot profile’ functions in FIJI. The vessel boundaries were defined based on the GFP intensity profile, which was analyzed in Origin Pro (version 2024b, OriginLab Corporation, Northampton, MA, USA) using the ‘Level Crossing’ application to identify luminal borders (
Figure 4C). The Cy3 fluorescence intensity was then plotted over a 100 µm distance extending outward from the vessel wall, normalized (%) to the mean luminal intensity, and corrected by subtracting background fluorescence. For each condition, at least 50 evenly distributed measurements were collected across three biological replicates and averaged to generate representative intensity profiles.
4.19. Liposome Toxicity Assessment via Microvasculature Network Analysis
Following the same workflow in Origin Pro as described in the previous section, vessel size was measured by determining the borders of the microvasculature via the intensity profile from the GFP expressed at the microvasculature. Vessel sizes were compared between different experimental conditions.
4.20. Statistics
All statistical analyses were performed using GraphPad Prism (version 10, GraphPad Software, Boston, MA, USA) or Origin Pro software. The ANOVA test is used to compare the differences between three or more groups of normally distributed samples. Results with a p value < 0.05 were considered significant. * p < 0.05; ** p < 0.01; *** p < 0.001; **** p < 0.0001. n indicates the number of independent experiments performed for the same procedure.