ADHD in Adulthood: Clinical Presentation, Comorbidities, and Treatment Perspectives
Abstract
1. Introduction
1.1. Significance of the Problem
1.2. Aim of the Study
1.3. Methodology
2. Epidemiology of Adult ADHD
2.1. Prevalence
| Disorder Category | Estimated Comorbidity (%) | Clinical Implications (Interpretation) | Source |
|---|---|---|---|
| Mood Disorders | 30–50% | ADHD symptoms (e.g., emotional dysregulation) may be masked by depression or misdiagnosed as bipolar disorder. | [51,52] |
| Anxiety Disorders | 30–50% | Anxiety may be both a consequence (e.g., life failures related to ADHD) and a separate condition. It significantly complicates the clinical picture. | [41] |
| Substance Use Disorders (SUD) | 25–50% | Often interpreted as attempts at “self-medication” of ADHD symptoms (impulsivity, attention deficits). Significantly worsens prognosis. | [53,54] |
| Personality Disorders | Increased risk | Shared features (impulsivity, emotional dysregulation), especially with Borderline and Antisocial types, make the diagnostic process extremely complex. | [55] |
| Learning Difficulties/Executive Function Deficits | Frequent | Highlights the neurodevelopmental nature of ADHD; executive function deficits are often at the core of academic and occupational impairments. | [56] |
| Autism Spectrum Disorder (ASD) | 15–50% | Reflects shared neurodevelopmental and genetic origins; leads to compounded functional impairment and emotional dysregulation. | [50] |
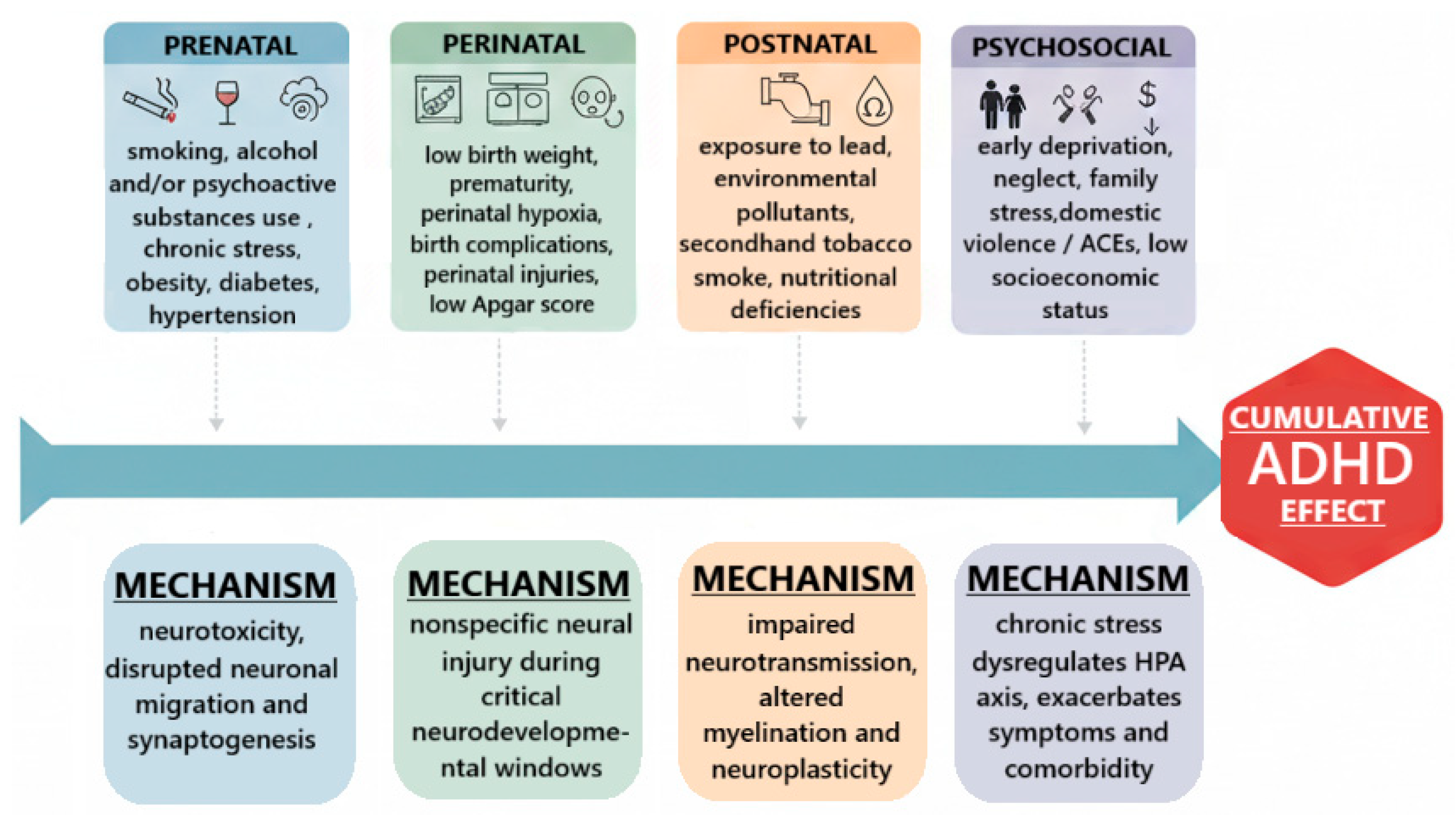
2.2. Risk Factors and Predictors
3. Etiology and Neurobiology of Adult ADHD
3.1. Neurobiological Models
3.2. Neurotransmitter System Dysfunctions
3.3. Structural and Functional Brain Abnormalities
3.4. Aberrant Large-Scale Brain Network Functioning
3.5. Additional Neuroimaging Findings in ADHD
4. Neuropsychological Features of Adult ADHD: Comorbidity and Diagnostic Challenges
4.1. Neuropsychological Perspective on Symptoms of Adult ADHD
4.2. Comorbidities and Diagnostic Differentiation
4.3. Diagnostic Approaches and Challenges
5. Sex-Dependent Differences in Adult ADHD
5.1. Epidemiology and Diagnosis
5.2. Clinical and Psychosocial Differences
5.3. Neurobiological Correlates
5.4. Diagnostic and Therapeutic Implications
6. Treatment of Adult ADHD
6.1. Pharmacotherapy
6.1.1. Stimulant Medications
6.1.2. Non-Stimulant Medications
6.2. Psychological and Behavioral Interventions
6.3. Supportive Treatments
| Intervention | Outcome Measure | Summary Effect (SMD/g) | 95% CI | N (Adults) | Quality (GRADE) | Clinical Interpretation |
|---|---|---|---|---|---|---|
| Amphetamines (stimulant, e.g., lisdexamfetamine, dextroamphetamine) | Clinician-rated ADHD symptoms (≈12 weeks) [142] | SMD − 0.79 | −0.99 to −0.58 | n ≈ 8131 | Moderate–High | Large effect on core ADHD symptoms; rapid onset; guideline first-line [142] |
| Methylphenidate (stimulant) | Clinician-rated ADHD symptoms (≈12 weeks) | SMD − 0.49 | −0.64 to −0.35 | n ≈ 2600 | Moderate–High | Moderate effect size; widely recommended as first-line [142] |
| Atomoxetine (non-stimulant) | Clinician-rated ADHD symptoms (10–12 weeks; longer-term effects accrue) | SMD − 0.45 | −0.58 to −0.32 | n ≈ 2050 | Moderate | Small–moderate effect; slower onset; useful when stimulants contraindicated or misuse risk [142,171] |
| Cognitive–Behavioral Therapy (adjunct or monotherapy) | ADHD symptoms and functional outcomes | Hedges’ g ≈ 0.65 vs. control | 0.44 to 0.86 | n ≈ 896 | Moderate | Moderate benefit for symptoms/function; smaller vs. active controls; valuable for residual deficits [172,173] |
| Adverse Effect/Safety Domain | Lisdexamfetamine | Methylphenidate | Atomoxetine | Viloxazine | Clinical Action/Monitoring |
|---|---|---|---|---|---|
| Insomnia/sleep disturbance | 27% (N = 358; insomnia 27% vs. placebo 8%) [174]. | 12.3% (CONCERTA adults; insomnia 12.3% vs. placebo 6.1%) [178]. | 15% (STRATTERA adults; insomnia 15% vs. placebo 8%) [176]. | 23% insomnia (Qelbree adults; 23% vs. placebo 7%). | Ask about dosing time; prefer morning dosing for stimulants; counsel on sleep hygiene; consider switching to less activating agent or non-stimulant if persistent. Monitor sleep and daytime function. |
| Decreased appetite/anorexia/weight decrease | Decreased appetite 27%; decreased weight 3% (adult ADHD Study 7) [174]. | Decreased appetite 25.3%; weight decreased 6.5% (CONCERTA adults) [175]. | Decreased appetite 16%; weight decreased 2% (STRATTERA adults) [176]. | Decreased appetite 10% (Qelbree adults). | Baseline weight; periodic weight monitoring (especially early treatment/children); dietary counselling; assess for clinically significant weight loss → consider dose change/alternative. |
| Dry mouth/xerostomia | 26% (VYVANSE adults) [174]. | 14.0% (CONCERTA adults) [175]. | 20% (STRATTERA adults) [176]. | 10% (Qelbree adults) [177] | Encourage fluids, sugar-free gum/lozenges, oral hygiene; consider symptomatic measures. |
| Nausea/GI adverse events | Nausea 7% (adult ADHD Study 7) [174]. | Nausea 12.8% (CONCERTA adults) [175]. | Nausea 26% (STRATTERA adults) [176]. | Nausea 12% (Qelbree adults) [177]. | Take with food if tolerated; antiemetic strategies rarely needed; monitor for persistent GI symptoms and weight loss; check labs if indicated. |
| Headache | Headache reported (adult ADHD trial: ~1% leading to discontinuation; post-market data show higher rates in other indications)—see label [174]. | Headache 22.2% (CONCERTA adults) [175]. | Headache 19% (STRATTERA adults table) [176]. | Headache 17% (Qelbree adults) [177]. | Symptomatic treatment (analgesia); monitor for severe or new/worsening headaches—consider cardiovascular assessment if concerning features. |
| Cardiovascular (↑ HR, ↑ BP, tachycardia, palpitations) | Increased HR 2%; ↑ BP 3%; palpitations 2% in adult ADHD Study; note higher heart-rate signals in some adult BED/adult flexible-dose studies [174]. | Tachycardia 4.8%; palpitations 3.1% (CONCERTA adults); mean small increases in BP/HR reported [175]. | Palpitations 3%; some adults experienced potentially clinically important HR/BP changes (~5–10% in some analyses); label recommends monitoring [176]. | Tachycardia 4% (Qelbree adults; also 29% had >20 bpm increases at any time point in adult flexible-dose trial—see label) [177]. | Baseline CV history, baseline BP and HR prior to initiation, recheck after titration and periodically; avoid stimulants in uncontrolled CVD; cardiology referral if symptomatic or marked changes. Consider non-stimulant in high CV risk. |
| Somnolence/sedation/fatigue | Somnolence reported infrequently in adult ADHD Study 7 (labels show low % in that adult ADHD study), but somnolence common in some adult BED trials [174]. | Sedation not a leading AE for methylphenidate ER in adults (some sedation/sleep disruption reported) [175]. | Somnolence 8% (STRATTERA adults) [176]. | Somnolence 6% (Qelbree adults) [177]. | Counsel re: driving/operating machinery especially with guanfacine and viloxazine; consider dosing time adjustments; avoid co-administration with other sedating meds where possible. |
| Abuse/diversion potential | High (controlled substance, Schedule II)—lisdexamfetamine associated with misuse/diversion risk; note prodrug reduces immediate abuse potential but controlled substance status remains [174]. | High (methylphenidate-controlled substance) risk of misuse/diversion; label warns about dependence [175]. | Low (atomoxetine not a controlled substance); low abuse potential [176]. | Low (Qelbree/viloxazine not scheduled; low abuse potential) [177]. | Screen for current or past SUD at baseline; if active SUD, prefer non-stimulants (atomoxetine, viloxazine) and structured SUD care; if stimulants required, use ER formulations, close monitoring and controlled dispensing. |
| Hepatic injury/LFT signals | Rare post-marketing hepatotoxicity signals are possible; follow label for post-marketing reports [174]. | Rare; monitor if clinically indicated [175]. | Labeled: rare cases of severe hepatic injury reported—monitor (STRATTERA label includes hepatic injury warnings) [176]. | Limited long-term adult data; monitor per label; follow LFTs if clinically indicated [177]. | Obtain baseline LFTs if liver disease or symptoms; for atomoxetine consider LFT monitoring if symptoms or risk factors (per label). |
6.4. Dietary Interventions in ADHD Therapy
7. Psychosocial Functioning and Quality of Life in Adults with ADHD
7.1. Occupational and Educational Performance
7.2. Social Relationships and Family Life
8. Future Research Directions
8.1. Better Understanding of Etiology and Neurobiology
8.2. Improvement of Diagnostic Methods
8.3. Trends and Future Directions in Pharmacotherapy for Adult ADHD
9. Limitations
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hrys, A.; Chepeleva, N.; Tkachuk, T.; Tor, L. Aдaптaцiйний пoтeнцiaл ociб дopocлoгo вiкy з poзлaдoм дeфiцитy yвaги/гiпepaктивнocтi (PДУГ). Insight Psychol. Dimens. Soc. 2024, 12, 471–494. [Google Scholar]
- Al-Yateem, N.; Slewa-Younan, S.; Halimi, A.; Saeed, S.A.; Tliti, D.; Mohammad, M.; Ridwan, M.; Zeidan, R.; Hammash, M.H.; Ahmed, F.R.; et al. Prevalence of Undiagnosed Attention Deficit Hyperactivity Disorder (ADHD) Symptoms in the Young Adult Population of the United Arab Emirates: A National Cross-Sectional Study. J. Epidemiol. Glob. Health 2023, 14, 45–53. [Google Scholar] [CrossRef]
- Johnson, J.; Morris, S.; George, S. Attention deficit hyperactivity disorder in adults: What the non-specialist needs to know. Br. J. Hosp. Med. 2020, 81, 1–11. [Google Scholar] [CrossRef]
- Kooij, J.; Bijlenga, D.; Salerno, L.; Jaeschke, R.; Bitter, I.; Balázs, J.; Thome, J.; Dom, G.; Kasper, S.; Filipe, C.N.; et al. Updated European Consensus Statement on diagnosis and treatment of adult ADHD. Eur. Psychiatry 2019, 56, 14–34. [Google Scholar] [CrossRef]
- Song, P.; Zha, M.; Yang, Q.; Zhang, Y.; Li, X.; Rudan, I. The prevalence of adult attention-deficit hyperactivity disorder: A global systematic review and meta-analysis. J. Glob. Health 2021, 11, 04009. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Taylor, M.J.; Larsson, H.; Gillberg, C.; Lichtenstein, P.; Lundström, S. Investigating the childhood symptom profile of community-based individuals diagnosed with attention-deficit/hyperactivity disorder as adults. J. Child Psychol. Psychiatry 2019, 60, 259–266. [Google Scholar] [CrossRef]
- Breda, V.; Rovaris, D.L.; Vitola, E.S.; Mota, N.R.; Blaya-Rocha, P.; Salgado, C.A.I.; Victor, M.M.; Picon, F.A.; Karam, R.G.; Silva, K.L.; et al. Does collateral retrospective information about childhood attention-deficit/hyperactivity disorder symptoms assist in the diagnosis of attention-deficit/hyperactivity disorder in adults? Findings from a large clinical sample. Aust. N. Zeal. J. Psychiatry 2016, 50, 557–565. [Google Scholar] [CrossRef]
- Lin, Y.-J.; Yang, L.-K.; Gau, S.S.-F. Psychiatric comorbidities of adults with early- and late-onset attention-deficit/hyperactivity disorder. Aust. N. Zeal. J. Psychiatry 2016, 50, 548–556. [Google Scholar] [CrossRef]
- Liu, C.-Y.; Asherson, P.; Viding, E.; Greven, C.U.; Pingault, J.-B. Early Predictors of De Novo and Subthreshold Late-Onset ADHD in a Child and Adolescent Cohort. J. Atten. Disord. 2021, 25, 1240–1250. [Google Scholar] [CrossRef] [PubMed]
- Turjeman-Levi, Y.; Itzchakov, G.; Engel-Yeger, B. Executive function deficits mediate the relationship between employees’ ADHD and job burnout. AIMS Public Health 2024, 11, 294–314. [Google Scholar] [CrossRef] [PubMed]
- Lauder, K.; McDowall, A.; Tenenbaum, H.R. A systematic review of interventions to support adults with ADHD at work—Implications from the paucity of context-specific research for theory and practice. Front. Psychol. 2022, 13, 893469. [Google Scholar] [CrossRef]
- Soares, L.S.; Alves, A.L.C.; Costa, D.d.S.; Malloy-Diniz, L.F.; de Paula, J.J.; Romano-Silva, M.A.; de Miranda, D.M. Common Venues in Romantic Relationships of Adults With Symptoms of Autism and Attention Deficit/Hyperactivity Disorder. Front. Psychiatry 2021, 12, 593150. [Google Scholar] [CrossRef] [PubMed]
- Oguchi, M.; Takahashi, T.; Nitta, Y.; Kumano, H. The Moderating Effect of Attention-Deficit Hyperactivity Disorder Symptoms on the Relationship Between Procrastination and Internalizing Symptoms in the General Adult Population. Front. Psychol. 2021, 12, 708579. [Google Scholar] [CrossRef] [PubMed]
- Katzman, M.A.; Bilkey, T.S.; Chokka, P.R.; Fallu, A.; Klassen, L.J. Adult ADHD and comorbid disorders: Clinical implications of a dimensional approach. BMC Psychiatry 2017, 17, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; A Hartman, C.; Haavik, J.; Harro, J.; Klungsøyr, K.; Hegvik, T.-A.; Wanders, R.; Ottosen, C.; Dalsgaard, S.; Faraone, S.V.; et al. Common psychiatric and metabolic comorbidity of adult attention-deficit/hyperactivity disorder: A population-based cross-sectional study. PLoS ONE 2018, 13, e0204516. [Google Scholar] [CrossRef]
- van de Glind, G.; Konstenius, M.; Koeter, M.W.J.; van Emmerik-van Oortmerssen, K.; Carpentier, P.-J.; Kaye, S.; Degenhardt, L.; Skutle, A.; Franck, J.; Bu, E.-T.; et al. Variability in the prevalence of adult ADHD in treatment seeking substance use disorder patients: Results from an international multi-center study exploring DSM-IV and DSM-5 criteria. Drug Alcohol Depend. 2014, 134, 158–166. [Google Scholar] [CrossRef]
- Weibel, S.; Bicego, F.; Muller, S.; Martz, E.; Costache, M.E.; Kraemer, C.; Bertschy, G.; Lopez, R.; Weiner, L. Two Facets of Emotion Dysregulation Are Core Symptomatic Domains in Adult ADHD: Results from the SR-WRAADDS, a Broad Symptom Self-Report Questionnaire. J. Atten. Disord. 2022, 26, 767–778. [Google Scholar] [CrossRef]
- Green, J.G.; DeYoung, G.; Wogan, M.E.; Wolf, E.J.; Lane, K.L.; Adler, L.A. Evidence for the reliability and preliminary validity of the Adult ADHD Self-Report Scale v1.1 (ASRS v1.1) Screener in an adolescent community sample. Int. J. Methods Psychiatr. Res. 2018, 28, e1751. [Google Scholar] [CrossRef]
- Cohen, M.B.-D.; Eldar, E.; Maeir, A.; Nahum, M. Emotional dysregulation and health related quality of life in young adults with ADHD: A cross sectional study. Health Qual. Life Outcomes 2021, 19, 270. [Google Scholar] [CrossRef]
- Widding-Havneraas, T.; Markussen, S.; Elwert, F.; Lyhmann, I.; Bjelland, I.; Halmøy, A.; Chaulagain, A.; Ystrom, E.; Mykletun, A.; Zachrisson, H.D. Geographical variation in ADHD: Do diagnoses reflect symptom levels? Eur. Child Adolesc. Psychiatry 2023, 32, 1795–1803. [Google Scholar] [CrossRef]
- Park, S.; Park, S. Prevalence, Correlates, and Comorbidities Among Young Adults Who Screened Positive for ADHD in South Korea During the COVID-19 Pandemic. J. Atten. Disord. 2024, 28, 1331–1339. [Google Scholar] [CrossRef]
- Stickley, A.; Leinsalu, M.; Ruchkin, V.; Oh, H.; Narita, Z.; Koyanagi, A. Attention-deficit/hyperactivity disorder symptoms and perceived mental health discrimination in adults in the general population. Eur. Psychiatry 2019, 56, 91–96. [Google Scholar] [CrossRef]
- Vater, C.H.; DiSalvo, M.; Ehrlich, A.; Parker, H.; O’cOnnor, H.; Faraone, S.V.; Biederman, J. ADHD in Adults: Does Age at Diagnosis Matter? J. Atten. Disord. 2024, 28, 614–624. [Google Scholar] [CrossRef]
- Al-Wardat, M.; Etoom, M.; A Almhdawi, K.; Hawamdeh, Z.; Khader, Y. Prevalence of attention-deficit hyperactivity disorder in children, adolescents and adults in the Middle East and North Africa region: A systematic review and meta-analysis. BMJ Open 2024, 14, e078849. [Google Scholar] [CrossRef]
- Caye, A.; Swanson, J.; Thapar, A.; Sibley, M.; Arseneault, L.; Hechtman, L.; Arnold, L.E.; Niclasen, J.; Moffitt, T.; Rohde, L.A. Life Span Studies of ADHD—Conceptual Challenges and Predictors of Persistence and Outcome. Curr. Psychiatry Rep. 2016, 18, 111. [Google Scholar] [CrossRef]
- Morkem, R.; Handelman, K.; Queenan, J.A.; Birtwhistle, R.; Barber, D. Validation of an EMR algorithm to measure the prevalence of ADHD in the Canadian Primary Care Sentinel Surveillance Network (CPCSSN). BMC Med. Inform. Decis. Mak. 2020, 20, 166. [Google Scholar] [CrossRef]
- Kessler, R.C.; Adler, L.; Barkley, R.; Biederman, J.; Conners, C.K.; Demler, O.; Faraone, S.V.; Greenhill, L.L.; Howes, M.J.; Secnik, K.; et al. The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey Replication. Am. J. Psychiatry 2006, 163, 716–723. [Google Scholar] [CrossRef]
- Wilens, T.E.; Martelon, M.; Joshi, G.; Bateman, C.; Fried, R.; Petty, C.; Biederman, J. Does ADHD Predict Substance-Use Disorders? A 10-Year Follow-up Study of Young Adults With ADHD. J. Am. Acad. Child Adolesc. Psychiatry 2011, 50, 543–553. [Google Scholar] [CrossRef] [PubMed]
- Vingilis, E.; Erickson, P.G.; Toplak, M.E.; Kolla, N.J.; Mann, R.E.; Seeley, J.; Vandermaas, M.; Daigle, D.S. Attention Deficit Hyperactivity Disorder Symptoms, Comorbidities, Substance Use, and Social Outcomes among Men and Women in a Canadian Sample. BioMed Res. Int. 2015, 2015, 982072. [Google Scholar] [CrossRef] [PubMed]
- Espinet, S.D.; Graziosi, G.; Toplak, M.E.; Hesson, J.; Minhas, P. A Review of Canadian Diagnosed ADHD Prevalence and Incidence Estimates Published in the Past Decade. Brain Sci. 2022, 12, 1051. [Google Scholar] [CrossRef] [PubMed]
- van de Glind, G.; van den Brink, W.; Koeter, M.W.; Carpentier, P.J.; van Emmerik-van Oortmerssen, K.; Kaye, S.; Skutle, A.; Bu, E.-T.H.; Franck, J.; Konstenius, M.; et al. Validity of the Adult ADHD Self-Report Scale (ASRS) as a screener for adult ADHD in treatment seeking substance use disorder patients. Drug Alcohol Depend. 2013, 132, 587–596. [Google Scholar] [CrossRef] [PubMed]
- Slobodin, O.; Crunelle, C.L. Mini Review: Socio-Cultural Influences on the Link Between ADHD and SUD. Front. Public Health 2019, 7, 173. [Google Scholar] [CrossRef]
- Ebejer, J.L.; E Medland, S.; Van Der Werf, J.; Gondro, C.; Henders, A.K.; Lynskey, M.; Martin, N.G.; Duffy, D.L. Attention deficit hyperactivity disorder in australian adults: Prevalence, persistence, conduct problems and disadvantage. PLoS ONE 2012, 7, e47404. [Google Scholar] [CrossRef] [PubMed]
- Caye, A.; Rocha, T.B.-M.; Anselmi, L.; Murray, J.; Menezes, A.M.B.; Barros, F.C.; Gonçalves, H.; Wehrmeister, F.; Jensen, C.M.; Steinhausen, H.-C.; et al. Attention-Deficit/Hyperactivity Disorder Trajectories From Childhood to Young Adulthood: Evidence From a Birth Cohort Supporting a Late-Onset Syndrome. JAMA Psychiatry 2016, 73, 705–712. [Google Scholar] [CrossRef]
- Staley, B.S.; Robinson, L.R.; Claussen, A.H.; Katz, S.M.; Danielson, M.L.; Summers, A.D.; Farr, S.L.; Blumberg, S.J.; Tinker, S.C. Attention-Deficit/Hyperactivity Disorder Diagnosis, Treatment, and Telehealth Use in Adults—National Center for Health Statistics Rapid Surveys System, United States, October–November 2023. MMWR Morb. Mortal Wkly. Rep. 2024, 73, 890–895. [Google Scholar] [CrossRef] [PubMed]
- Faraone, S.V.; Spencer, T.J.; Montano, C.B.; Biederman, J. Attention-deficit/hyperactivity disorder in adults: A survey of current practice in psychiatry and primary care. Arch. Intern Med. 2004, 164, 1221–1226. [Google Scholar] [CrossRef]
- Sasayama, D.; Kuge, R.; Toibana, Y.; Honda, H. Trends in Diagnosed Attention-Deficit/Hyperactivity Disorder Among Children, Adolescents, and Adults in Japan From April 2010 to March 2020. JAMA Netw. Open 2022, 5, e2234179. [Google Scholar] [CrossRef]
- Brod, M.; Pohlman, B.; Lasser, R.; Hodgkins, P. Comparison of the burden of illness for adults with ADHD across seven countries: A qualitative study. Health Qual. Life Outcomes 2012, 10, 47. [Google Scholar] [CrossRef]
- Mattos, P.; Louzã, M.R.; Palmini, A.L.F.; de Oliveira, I.R.; Rocha, F.L. A multicenter, open-label trial to evaluate the quality of life in adults with ADHD treated with long-acting methylphenidate (OROS MPH): Concerta Quality of Life (CONQoL) study. J. Atten. Disord. 2013, 17, 444–448. [Google Scholar] [CrossRef]
- Hesson, J.; Fowler, K. Prevalence and Correlates of Self-Reported ADD/ADHD in a Large National Sample of Canadian Adults. J. Atten. Disord. 2018, 22, 191–200. [Google Scholar] [CrossRef]
- Mao, A.R.; Findling, R.L. Comorbidities in adult attention-deficit/hyperactivity disorder: A practical guide to diagnosis in primary care. Postgrad. Med. 2014, 126, 42–51. [Google Scholar] [CrossRef]
- Zaleski, A.L.; Craig, K.J.T.; Khan, R.; Waber, R.; Xin, W.; Powers, M.; Ramey, U.; Verbrugge, D.J.; Fernandez-Turner, D. Real-world evaluation of prevalence, cohort characteristics, and healthcare utilization and expenditures among adults and children with autism spectrum disorder, attention-deficit hyperactivity disorder, or both. BMC Health Serv. Res. 2025, 25, 1048. [Google Scholar] [CrossRef]
- Lai, M.-C.; Kassee, C.; Besney, R.; Bonato, S.; Hull, L.; Mandy, W.; Szatmari, P.; Ameis, S.H. Prevalence of co-occurring mental health diagnoses in the autism population: A systematic review and meta-analysis. Lancet Psychiatry 2019, 6, 819–829. [Google Scholar] [CrossRef]
- Martinez, S.; Stoyanov, K.; Carcache, L. Unraveling the spectrum: Overlap, distinctions, and nuances of ADHD and ASD in children. Front. Psychiatry 2024, 15, 1387179. [Google Scholar] [CrossRef]
- Harikumar, A.; Evans, D.W.; Dougherty, C.C.; Carpenter, K.L.; Michael, A.M. A Review of the Default Mode Network in Autism Spectrum Disorders and Attention Deficit Hyperactivity Disorder. Brain Connect. 2021, 11, 253–263. [Google Scholar] [CrossRef]
- Rodenas-Cuadrado, P.; Ho, J.; Vernes, S.C. Shining a light on CNTNAP2: Complex functions to complex disorders. Eur. J. Hum. Genet. 2014, 22, 171–178. [Google Scholar] [CrossRef] [PubMed]
- E Yerys, B.; A McQuaid, G.; Lee, N.R.; Wallace, G.L. Co-occurring ADHD symptoms in autistic adults are associated with less independence in daily living activities and lower subjective quality of life. Autism 2022, 26, 2188–2195. [Google Scholar] [CrossRef]
- Deserno, M.K.; Bathelt, J.; Groenman, A.P.; Geurts, H.M. Probing the overarching continuum theory: Data-driven phenotypic clustering of children with ASD or ADHD. Eur. Child Adolesc. Psychiatry 2023, 32, 1909–1923. [Google Scholar] [CrossRef]
- Schweizer, T.; Endres, D.; Dziobek, I.; van Elst, L.T. Psychosocial therapeutic approaches for high-functioning autistic adults. Front. Psychiatry 2024, 14, 1265066. [Google Scholar] [CrossRef] [PubMed]
- Young, S.; Hollingdale, J.; Absoud, M.; Bolton, P.; Branney, P.; Colley, W.; Craze, E.; Dave, M.; Deeley, Q.; Farrag, E.; et al. Guidance for identification and treatment of individuals with attention deficit/hyperactivity disorder and autism spectrum disorder based upon expert consensus. BMC Med. 2020, 18, 146. [Google Scholar] [CrossRef] [PubMed]
- Yoshimasu, K.; Barbaresi, W.J.; Colligan, R.C.; Voigt, R.G.; Killian, J.M.; Weaver, A.L.; Katusic, S.K. Adults With Persistent ADHD: Gender and Psychiatric Comorbidities—A Population-Based Longitudinal Study. J. Atten. Disord. 2018, 22, 535–546. [Google Scholar] [CrossRef]
- Instanes, J.T.; Klungsøyr, K.; Halmøy, A.; Fasmer, O.B.; Haavik, J. Adult ADHD and Comorbid Somatic Disease: A Systematic Literature Review. J. Atten. Disord. 2018, 22, 203–228. [Google Scholar] [CrossRef] [PubMed]
- Surman, C.B.; Monuteaux, M.C.; Petty, C.R.; Faraone, S.V.; Spencer, T.J.; Chu, N.F.; Biederman, J. Representativeness of participants in a clinical trial for attention-deficit/hyperactivity disorder? Comparison with adults from a large observational study. J. Clin. Psychiatry 2010, 71, 1612–1616. [Google Scholar] [CrossRef]
- Kooij, J.J.S.; Huss, M.; Asherson, P.; Akehurst, R.; Beusterien, K.; French, A.; Sasané, R.; Hodgkins, P. Distinguishing comorbidity and successful management of adult ADHD. J. Atten. Disord. 2012, 16, 3S–19S. [Google Scholar] [CrossRef]
- Okada, T.; Sotodate, T.; Ogasawara-Shimizu, M.; Nishigaki, N. Psychiatric comorbidities of attention deficit/hyperactivity disorder in Japan: A nationwide population-based study. Front. Psychiatry 2024, 15, 1359872. [Google Scholar] [CrossRef]
- Kofler, M.J.; Singh, L.J.; Soto, E.F.; Chan, E.S.M.; Miller, C.E.; Harmon, S.L.; Spiegel, J.A. Working memory and short-term memory deficits in ADHD: A bifactor modeling approach. Neuropsychology 2020, 34, 686–698. [Google Scholar] [CrossRef]
- Faraone, S.V.; Larsson, H. Genetics of attention deficit hyperactivity disorder. Mol. Psychiatry 2019, 24, 562–575. [Google Scholar] [CrossRef] [PubMed]
- Faraone, S.V.; Banaschewski, T.; Coghill, D.; Zheng, Y.; Biederman, J.; Bellgrove, M.A.; Newcorn, J.H.; Gignac, M.; Al Saud, N.M.; Manor, I.; et al. The World Federation of ADHD International Consensus Statement: 208 Evidence-based conclusions about the disorder. Neurosci. Biobehav. Rev. 2021, 128, 789–818. [Google Scholar] [CrossRef]
- Demontis, D.; Walters, R.K.; Martin, J.; Mattheisen, M.; Als, T.D.; Agerbo, E.; Baldursson, G.; Belliveau, R.; Bybjerg-Grauholm, J.; Bækvad-Hansen, M.; et al. Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat. Genet. 2019, 51, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Grünblatt, E.; Werling, A.M.; Roth, A.; Romanos, M.; Walitza, S. Association study and a systematic meta-analysis of the VNTR polymorphism in the 3′-UTR of dopamine transporter gene and attention-deficit hyperactivity disorder. J. Neural Transm. 2019, 126, 517–529. [Google Scholar] [CrossRef]
- Acosta, H.; Kantojärvi, K.; Tuulari, J.J.; Lewis, J.D.; Hashempour, N.; Scheinin, N.M.; Lehtola, S.J.; Nolvi, S.; Fonov, V.S.; Collins, D.L.; et al. Association of cumulative prenatal adversity with infant subcortical structure volumes and child problem behavior and its moderation by a coexpression polygenic risk score of the serotonin system. Dev. Psychopathol. 2023, 36, 1027–1042. [Google Scholar] [CrossRef]
- Ni, M.; Li, L.; Li, W.; Zhang, Q.; Zhao, J.; Shen, Q.; Yao, D.; Wang, T.; Li, B.; Ding, X.; et al. Examining the relationship between birth weight and attention-deficit hyperactivity disorder diagnosis. Front. Psychiatry 2023, 14, 1074783. [Google Scholar] [CrossRef]
- Sánchez-Mora, C.; Richarte, V.; Garcia-Martínez, I.; Pagerols, M.; Corrales, M.; Bosch, R.; Vidal, R.; Viladevall, L.; Casas, M.; Cormand, B.; et al. Dopamine receptor DRD4 gene and stressful life events in persistent attention deficit hyperactivity disorder. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2015, 168, 480–491. [Google Scholar] [CrossRef] [PubMed]
- Todd, R.D.; Neuman, R.J. Gene–Environment interactions in the development of combined type ADHD: Evidence for a synapse-based model. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2007, 144B, 971–975. [Google Scholar] [CrossRef]
- Lundström, S.; Chang, Z.; Kerekes, N.; Gumpert, C.H.; Råstam, M.; Gillberg, C.; Lichtenstein, P.; Anckarsäter, H. Autistic-like traits and their association with mental health problems in two nationwide twin cohorts of children and adults. Psychol. Med. 2011, 41, 2423–2433. [Google Scholar] [CrossRef] [PubMed]
- Fusar-Poli, P.; Rubia, K.; Rossi, G.; Sartori, G.; Balottin, U. Striatal dopamine transporter alterations in ADHD: Pathophysiology or adaptation to psychostimulants? A meta-analysis. Am. J. Psychiatry 2012, 169, 264–272. [Google Scholar] [CrossRef]
- Véronneau-Veilleux, F.; Robaey, P.; Ursino, M.; Nekka, F. A mechanistic model of ADHD as resulting from dopamine phasic/tonic imbalance during reinforcement learning. Front. Comput. Neurosci. 2022, 16, 849323. [Google Scholar] [CrossRef] [PubMed]
- Van Dessel, J.; Sonuga-Barke, E.; Mies, G.; Lemiere, J.; Van der Oord, S.; Morsink, S.; Danckaerts, M. Delay aversion in attention deficit/hyperactivity disorder is mediated by amygdala and prefrontal cortex hyper-activation. J. Child Psychol. Psychiatry 2018, 59, 888–899. [Google Scholar] [CrossRef]
- Gamo, N.J.; Wang, M.; Arnsten, A.F. Methylphenidate and atomoxetine enhance prefrontal function through α2-adrenergic and dopamine D1 receptors. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 1011–1023. [Google Scholar] [CrossRef]
- Vidor, M.V.; Panzenhagen, A.C.; Martins, A.R.; Cupertino, R.B.; Bandeira, C.E.; Picon, F.A.; da Silva, B.S.; Vitola, E.S.; Rohde, L.A.; Rovaris, D.L.; et al. Emerging findings of glutamate–glutamine imbalance in the medial prefrontal cortex in attention deficit/hyperactivity disorder: Systematic review and meta-analysis of spectroscopy studies. Eur. Arch. Psychiatry Clin. Neurosci. 2022, 272, 1395–1411. [Google Scholar] [CrossRef]
- Faraone, S.V.; Ward, C.L.; Boucher, M.; Elbekai, R.; Brunner, E. Role of serotonin in psychiatric and somatic comorbidities of attention-deficit/hyperactivity disorder: A systematic literature review. Neurosci. Biobehav. Rev. 2025, 176, 106275. [Google Scholar] [CrossRef]
- Hoogman, M.; Muetzel, R.; Guimaraes, J.P.; Shumskaya, E.; Mennes, M.; Zwiers, M.P.; Jahanshad, N.; Sudre, G.; Wolfers, T.; Earl, E.A.; et al. Brain Imaging of the Cortex in ADHD: A Coordinated Analysis of Large-Scale Clinical and Population-Based Samples. Am. J. Psychiatry 2019, 176, 531–542. [Google Scholar] [CrossRef]
- Shaw, P.; Eckstrand, K.; Sharp, W.; Blumenthal, J.; Lerch, J.P.; Greenstein, D.; Clasen, L.; Evans, A.; Giedd, J.; Rapoport, J.L. Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proc. Natl. Acad. Sci. USA 2007, 104, 19649–19654. [Google Scholar] [CrossRef]
- van Ewijk, H.; Heslenfeld, D.J.; Zwiers, M.P.; Buitelaar, J.K.; Oosterlaan, J. Diffusion tensor imaging in attention deficit/hyperactivity disorder: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2012, 36, 1093–1106. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, L.S.; Levitt, J.G.; O’Neill, J.; Alger, J.R.; Luders, E.; Phillips, O.R.; Caplan, R.; Toga, A.W.; McCracken, J.; Narr, K.L. Reduced white matter integrity in attention-deficit hyperactivity disorder. Neuroreport 2008, 19, 1705–1708. [Google Scholar] [CrossRef] [PubMed]
- Stephan, K.E.; Friston, K.J. Analyzing effective connectivity with functional magnetic resonance imaging. WIREs Cogn. Sci. 2010, 1, 446–459. [Google Scholar] [CrossRef]
- Stoodley, C.J. The Cerebellum and Neurodevelopmental Disorders. Cerebellum 2016, 15, 34–37. [Google Scholar] [CrossRef]
- Hilger, K.; Fiebach, C.J. ADHD symptoms are associated with the modular structure of intrinsic brain networks in a representative sample of healthy adults. Netw. Neurosci. 2019, 3, 567–588. [Google Scholar] [CrossRef]
- Castellanos, F.X.; Proal, E. Large-scale brain systems in ADHD: Beyond the prefrontal–striatal model. Trends Cogn. Sci. 2012, 16, 17–26. [Google Scholar] [CrossRef]
- Lin, H.-Y.; Tseng, W.-Y.I.; Lai, M.-C.; Matsuo, K.; Gau, S.S.-F. Altered Resting-State Frontoparietal Control Network in Children with Attention-Deficit/Hyperactivity Disorder. J. Int. Neuropsychol. Soc. 2015, 21, 271–284. [Google Scholar] [CrossRef] [PubMed]
- Vera, J.D.; Freichel, R.; Michelini, G.; Loo, S.K.; Lenartowicz, A. A Network Approach to Understanding the Role of Executive Functioning and Alpha Oscillations in Inattention and Hyperactivity-Impulsivity Symptoms of ADHD. J. Atten. Disord. 2024, 28, 1357–1367. [Google Scholar] [CrossRef]
- Ishii-Takahashi, A.; Takizawa, R.; Nishimura, Y.; Kawakubo, Y.; Kuwabara, H.; Matsubayashi, J.; Hamada, K.; Okuhata, S.; Yahata, N.; Igarashi, T.; et al. Prefrontal activation during inhibitory control measured by near-infrared spectroscopy for differentiating between autism spectrum disorders and attention deficit hyperactivity disorder in adults. Neuroimage Clin. 2013, 4, 53–63. [Google Scholar] [CrossRef]
- Sáenz, A.A.; Villemonteix, T.; Massat, I. Structural and functional neuroimaging in attention-deficit/hyperactivity disorder. Dev. Med. Child Neurol. 2019, 61, 399–405. [Google Scholar] [CrossRef]
- Salomone, S.; Fleming, G.R.; Bramham, J.; O’cOnnell, R.G.; Robertson, I.H. Neuropsychological Deficits in Adult ADHD: Evidence for Differential Attentional Impairments, Deficient Executive Functions, and High Self-Reported Functional Impairments. J. Atten. Disord. 2020, 24, 1413–1424. [Google Scholar] [CrossRef] [PubMed]
- Dunn, G.A.; Nigg, J.T.; Sullivan, E.L. Neuroinflammation as a risk factor for attention deficit hyperactivity disorder. Pharmacol. Biochem. Behav. 2019, 182, 22–34. [Google Scholar] [CrossRef]
- Lewis, N.; Villani, A.; Lagopoulos, J. Gut dysbiosis as a driver of neuroinflammation in attention-deficit/hyperactivity disorder: A review of current evidence. Neuroscience 2025, 569, 298–321. [Google Scholar] [CrossRef] [PubMed]
- DSM. Available online: https://www.psychiatry.org:443/psychiatrists/practice/dsm (accessed on 5 August 2025).
- Posner, J.; Polanczyk, G.V.; Sonuga-Barke, E. Attention-deficit hyperactivity disorder. Lancet 2020, 395, 450–462. [Google Scholar] [CrossRef] [PubMed]
- Bedawi, R.M.; Al-Farsi, Y.; Mirza, H.; Al-Huseini, S.; Al-Mahrouqi, T.; Al-Kiyumi, O.; Al-Azri, M.; Al-Adawi, S. Prevalence and Clinical Profile of Adults with ADHD Attending a Tertiary Care Hospital for Five Years. Int. J. Environ. Res. Public Health 2024, 21, 566. [Google Scholar] [CrossRef]
- LeRoy, A.; Jacova, C.; Young, C. Neuropsychological Performance Patterns of Adult ADHD Subtypes. J. Atten. Disord. 2019, 23, 1136–1147. [Google Scholar] [CrossRef]
- Hackett, A.P.-C.; Joseph, R.P.-C.; Robinson, K.P.-C.; Welsh, J.D.; Nicholas, J.; Schmidt, E. Adult attention deficit/hyperactivity disorder in the ambulatory care setting. J. Am. Acad. Physician Assist. 2020, 33, 12–16. [Google Scholar] [CrossRef]
- Mostert, J.C.; Onnink, A.M.H.; Klein, M.; Dammers, J.; Harneit, A.; Schulten, T.; van Hulzen, K.J.; Kan, C.C.; Slaats-Willemse, D.; Buitelaar, J.K.; et al. Cognitive heterogeneity in adult attention deficit/hyperactivity disorder: A systematic analysis of neuropsychological measurements. Eur. Neuropsychopharmacol. 2015, 25, 2062–2074. [Google Scholar] [CrossRef]
- Senkowski, D.; Ziegler, T.; Singh, M.; Heinz, A.; He, J.; Silk, T.; Lorenz, R.C. Assessing Inhibitory Control Deficits in Adult ADHD: A Systematic Review and Meta-analysis of the Stop-signal Task. Neuropsychol. Rev. 2024, 34, 548–567. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Jiménez, R.; Cubillo, A.; A Jiménez-Arriero, M.; Ponce, G.; Aragüés-Figuero, M.; Palomo, T. Executive dysfunctions in adults with attention deficit hyperactivity disorder. Rev. Neurol. 2006, 43, 678–684. [Google Scholar] [PubMed]
- Yue, X.; Liu, L.; Chen, W.; Preece, D.A.; Liu, Q.; Li, H.; Wang, Y.; Qian, Q. Affective-cognitive-behavioral heterogeneity of Attention-Deficit/Hyperactivity Disorder (ADHD): Emotional dysregulation as a sentinel symptom differentiating “ADHD-simplex” and “ADHD-complex” syndromes? J. Affect. Disord. 2022, 307, 133–141. [Google Scholar] [CrossRef]
- Alaghband-Rad, J.; Dashti, B.; Tehranidoost, M.; Zargarinejad, G.M.; FarhadBeigi, P.M. A Preliminary Investigation of Deficits in Executive Functions of Adults With Attention Deficit Hyperactivity Disorder. J. Nerv. Ment. Dis. 2021, 209, 35–39. [Google Scholar] [CrossRef]
- Chan, E.S.M.; Langberg, J.M. Predicting Occupational Outcomes for Individuals with ADHD: The Role of Hyperactivity/Impulsivity and Executive Functioning. J. Occup. Rehabil. 2024. [Google Scholar] [CrossRef] [PubMed]
- Guo, N.; Fuermaier, A.B.M.; Koerts, J.; Mueller, B.W.; Diers, K.; Mroß, A.; Mette, C.; Tucha, L.; Tucha, O. Neuropsychological functioning of individuals at clinical evaluation of adult ADHD. J. Neural Transm. 2021, 128, 877–891. [Google Scholar] [CrossRef]
- Yáñez-Téllez, G.; Romero-Romero, H.; Rivera-García, L.; Prieto-Corona, B.; Bernal-Hernandez, J.; Marosi-Holczberger, E.; Guerrero-Juárez, V.; Rodríguez-Camacho, M.; Silva-Pereyra, J.F. Cognitive and executive functions in ADHD. Actas Esp. Psiquiatr. 2012, 40, 293–298. [Google Scholar]
- Holst, Y.; Thorell, L.B. Neuropsychological Functioning in Adults With ADHD and Adults With Other Psychiatric Disorders. J. Atten. Disord. 2017, 21, 137–148. [Google Scholar] [CrossRef]
- Pettersson, R.; Söderström, S.; Nilsson, K.W. Diagnosing ADHD in Adults: An Examination of the Discriminative Validity of Neuropsychological Tests and Diagnostic Assessment Instruments. J. Atten. Disord. 2018, 22, 1019–1031. [Google Scholar] [CrossRef]
- de Braek, D.I.; Dijkstra, J.B.; Jolles, J. Cognitive Complaints and Neuropsychological Functioning in Adults With and Without Attention-Deficit Hyperactivity Disorder Referred for Multidisciplinary Assessment. Appl. Neuropsychol. 2011, 18, 127–135. [Google Scholar] [CrossRef]
- Shaw, P.; Stringaris, A.; Nigg, J.; Leibenluft, E. Emotion Dysregulation in Attention Deficit Hyperactivity Disorder. Am. J. Psychiatry 2014, 171, 276–293. [Google Scholar] [CrossRef]
- Soler-Gutiérrez, A.-M.; Pérez-González, J.-C.; Mayas, J. Evidence of emotion dysregulation as a core symptom of adult ADHD: A systematic review. PLoS ONE 2023, 18, e0280131. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, O.; Chavanon, M.; Riechmann, E.; Christiansen, H. Emotional dysregulation is a primary symptom in adult Attention-Deficit/Hyperactivity Disorder (ADHD). J. Affect. Disord. 2018, 232, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Wu, W.; Wu, Y.; Liu, X.; Liang, W.; Wu, R.; Li, Y. Adult ADHD and comorbid anxiety and depressive disorders: A review of etiology and treatment. Front. Psychiatry 2025, 16, 1597559. [Google Scholar] [CrossRef]
- Choi, W.-S.; Woo, Y.S.; Wang, S.-M.; Lim, H.K.; Bahk, W.-M. The prevalence of psychiatric comorbidities in adult ADHD compared with non-ADHD populations: A systematic literature review. PLoS ONE 2022, 17, e0277175. [Google Scholar] [CrossRef] [PubMed]
- Moldekleiv, C.D.; Lundervold, A.J.; Solberg, B.S.; Engeland, A.; Fadnes, L.T.; Chalabianloo, F.; Klungsøyr, K. Prevalence of substance use disorder in individuals with attention deficit/hyperactivity disorder: Associations with sex and psychiatric comorbidity. BMC Psychiatry 2025, 25, 936. [Google Scholar] [CrossRef]
- Shaker, N.M.; Mahmoud, D.A.M.; Ahmed, M.M.; Rabie, E.S. Frequency of binge eating in medication adherent patients with ADHD and its relation to impulsivity. Middle East Curr. Psychiatry 2025, 32, 28. [Google Scholar] [CrossRef]
- Hambleton, A.; Pepin, G.; Le, A.; Maloney, D.; Touyz, S.; Maguire, S. Psychiatric and medical comorbidities of eating disorders: Findings from a rapid review of the literature. J. Eat. Disord. 2022, 10, 132. [Google Scholar] [CrossRef]
- Baby, M.; Priya, V.; Pallavi, J.; Chand, B.K.; Srinivasan, L.V.; Rana, S.S.; Tawil, S.; Haque, S.; Ghosh, P.; Bhattacharya, P.; et al. A Narrative Review of Outcomes, Comorbidities, and Alternative Behavioral Interventions in Adolescent and Adult Women with ADHD. Int. J. Women’s Health 2025, 17, 3201–3228. [Google Scholar] [CrossRef]
- Alarachi, A.; Merrifield, C.; Rowa, K.; McCabe, R.E. Are We Measuring ADHD or Anxiety? Examining the Factor Structure and Discriminant Validity of the Adult ADHD Self-Report Scale in an Adult Anxiety Disorder Population. Assessment 2024, 31, 1508–1524. [Google Scholar] [CrossRef]
- Barbuti, M.; Maiello, M.; Spera, V.; Pallucchini, A.; Brancati, G.E.; Maremmani, A.G.I.; Perugi, G.; Maremmani, I. Challenges of Treating ADHD with Comorbid Substance Use Disorder: Considerations for the Clinician. J. Clin. Med. 2023, 12, 3096. [Google Scholar] [CrossRef] [PubMed]
- Overview|Attention Deficit Hyperactivity Disorder: Diagnosis and Management|Guidance|NICE. 2018. Available online: https://www.nice.org.uk/guidance/ng87 (accessed on 6 August 2025).
- Table 7, DSM-IV to DSM-5 Attention-Deficit/Hyperactivity Disorder Comparison. 2016. Available online: https://www.ncbi.nlm.nih.gov/books/NBK519712/table/ch3.t3/ (accessed on 6 August 2025).
- Recommendations|Attention Deficit Hyperactivity Disorder: Diagnosis and Management|Guidance|NICE. 2018. Available online: https://www.nice.org.uk/guidance/ng87/chapter/Recommendations#diagnosis# (accessed on 6 August 2025).
- Ginsberg, Y.; Quintero, J.; Anand, E.; Casillas, M.; Upadhyaya, H.P. Underdiagnosis of Attention-Deficit/Hyperactivity Disorder in Adult Patients: A Review of the Literature. Prim Care Companion CNS Disord. 2014, 16, PCC.13r01600. [Google Scholar] [CrossRef] [PubMed]
- Christensen, K.S.; Storebø, O.J.; Bach, B. Assessing the Construct Validity of the Adult ADHD Self-report Scale for DSM-5 and Prevalence of ADHD in a Danish Population Sample. J. Atten. Disord. 2025, 29, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Brevik, E.J.; Lundervold, A.J.; Haavik, J.; Posserud, M. Validity and accuracy of the Adult Attention-Deficit/Hyperactivity Disorder (ADHD) Self-Report Scale (ASRS) and the Wender Utah Rating Scale (WURS) symptom checklists in discriminating between adults with and without ADHD. Brain Behav. 2020, 10, e01605. [Google Scholar] [CrossRef]
- Hong, M.; Kooij, J.S.; Kim, B.; Joung, Y.-S.; Yoo, H.K.; Kim, E.-J.; Lee, S.I.; Bhang, S.-Y.; Lee, S.Y.; Han, D.H.; et al. Validity of the Korean Version of DIVA-5: A Semi-Structured Diagnostic Interview for Adult ADHD. Neuropsychiatr. Dis. Treat. 2020, 16, 2371–2376. [Google Scholar] [CrossRef]
- Lovett, B.J.; Harrison, A.G. Assessing adult ADHD: New research and perspectives. J. Clin. Exp. Neuropsychol. 2021, 43, 333–339. [Google Scholar] [CrossRef]
- Mestres, F.; Richarte, V.; Crespín, J.J.; Torrent, C.; Biel, S.; Ramos, C.; Ibáñez, P.; Oltra-Arañó, L.; Corrales, M.; Amoretti, S.; et al. Sex differences in adults with attention-deficit/hyperactivity disorder: A population-based study. Eur. Psychiatry 2025, 68, e90. [Google Scholar] [CrossRef]
- Solberg, B.S.; Halmøy, A.; Engeland, A.; Igland, J.; Haavik, J.; Klungsøyr, K. Gender differences in psychiatric comorbidity: A population-based study of 40 000 adults with attention deficit hyperactivity disorder. Acta Psychiatr. Scand. 2018, 137, 176–186. [Google Scholar] [CrossRef]
- Quinn, P.O.; Madhoo, M. A review of attention-deficit/hyperactivity disorder in women and girls: Uncovering this hidden diagnosis. Prim Care Companion CNS Disord. 2014, 16, PCC.13r01596. [Google Scholar] [CrossRef]
- Vildalen, V.U.; Brevik, E.J.; Haavik, J.; Lundervold, A.J. Females With ADHD Report More Severe Symptoms Than Males on the Adult ADHD Self-Report Scale. J. Atten. Disord. 2019, 23, 959–967. [Google Scholar] [CrossRef]
- Kao, P.-H.; Ho, C.-H.; Huang, C.L.-C. Sex differences in psychiatric comorbidities of attention-deficit/hyperactivity disorder among children, adolescents, and adults: A nationwide population-based cohort study. PLoS ONE 2025, 20, e0315587. [Google Scholar] [CrossRef]
- Frodl, T.; Skokauskas, N. Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects. Acta Psychiatr. Scand. 2012, 125, 114–126. [Google Scholar] [CrossRef]
- Valera, E.M.; Faraone, S.V.; Murray, K.E.; Seidman, L.J. Meta-analysis of structural imaging findings in attention-deficit/hyperactivity disorder. Biol. Psychiatry 2007, 61, 1361–1369. [Google Scholar] [CrossRef]
- Ellison-Wright, I.; Ellison-Wright, Z.; Bullmore, E. Structural brain change in Attention Deficit Hyperactivity Disorder identified by meta-analysis. BMC Psychiatry 2008, 8, 51. [Google Scholar] [CrossRef]
- Nakao, T.; Radua, J.; Rubia, K.; Mataix-Cols, D. Gray matter volume abnormalities in ADHD: Voxel-based meta-analysis exploring the effects of age and stimulant medication. Am. J. Psychiatry 2011, 168, 1154–1163. [Google Scholar] [CrossRef] [PubMed]
- Qiu, A.; Crocetti, D.; Adler, M.; Mahone, E.M.; Denckla, M.B.; Miller, M.I.; Mostofsky, S.H. Basal ganglia volume and shape in children with attention deficit hyperactivity disorder. Am. J. Psychiatry 2009, 166, 74–82. [Google Scholar] [CrossRef]
- Onnink, A.M.H.; Zwiers, M.P.; Hoogman, M.; Mostert, J.C.; Kan, C.C.; Buitelaar, J.; Franke, B. Brain alterations in adult ADHD: Effects of gender, treatment and comorbid depression. Eur. Neuropsychopharmacol. 2014, 24, 397–409. [Google Scholar] [CrossRef] [PubMed]
- Villemonteix, T.; De Brito, S.A.; Kavec, M.; Balériaux, D.; Metens, T.; Slama, H.; Baijot, S.; Mary, A.; Peigneux, P.; Massat, I. Grey matter volumes in treatment naïve vs. chronically treated children with attention deficit/hyperactivity disorder: A combined approach. Eur. Neuropsychopharmacol. 2015, 25, 1118–1127. [Google Scholar] [CrossRef] [PubMed]
- Dupont, G.; van Rooij, D.; Buitelaar, J.K.; Reif, A.; Grimm, O. Sex-related differences in adult attention-deficit hyperactivity disorder patients—An analysis of external globus pallidus functional connectivity in resting-state functional MRI. Front. Psychiatry 2022, 13, 962911. [Google Scholar] [CrossRef]
- Rosch, K.S.; Mostofsky, S.H.; Nebel, M.B. ADHD-Related Sex Differences in Fronto-Subcortical Intrinsic Functional Connectivity and Associations with Delay Discounting. J. Neurodev. Disord. 2018, 10, 34. [Google Scholar] [CrossRef] [PubMed]
- Jung, B.; Ahn, K.; Justice, C.; Norman, L.; Price, J.; Sudre, G.; Shaw, P. Rare copy number variants in males and females with childhood attention-deficit/hyperactivity disorder. Mol. Psychiatry 2022, 28, 1240–1247. [Google Scholar] [CrossRef]
- de Jong, M.; Wynchank, D.S.M.R.; van Andel, E.; Beekman, A.T.F.; Kooij, J.J.S. Female-specific pharmacotherapy in ADHD: Premenstrual adjustment of psychostimulant dosage. Front. Psychiatry 2023, 14, 1306194. [Google Scholar] [CrossRef] [PubMed]
- Haimov-Kochman, R.; Berger, I. Cognitive functions of regularly cycling women may differ throughout the month, depending on sex hormone status; a possible explanation to conflicting results of studies of ADHD in females. Front. Hum. Neurosci. 2014, 8, 191. [Google Scholar] [CrossRef]
- Roberts, B.; Eisenlohr-Moul, T.; Martel, M.M. Reproductive steroids and ADHD symptoms across the menstrual cycle. Psychoneuroendocrinology 2018, 88, 105–114. [Google Scholar] [CrossRef]
- Shanmugan, S.; Epperson, C.N. Estrogen and the prefrontal cortex: Towards a new understanding of estrogen’s effects on executive functions in the menopause transition. Hum. Brain Mapp. 2014, 35, 847–865. [Google Scholar] [CrossRef] [PubMed]
- Young, S.; Adamo, N.; Ásgeirsdóttir, B.B.; Branney, P.; Beckett, M.; Colley, W.; Cubbin, S.; Deeley, Q.; Farrag, E.; Gudjonsson, G.; et al. Females with ADHD: An expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/ hyperactivity disorder in girls and women. BMC Psychiatry 2020, 20, 404. [Google Scholar] [CrossRef]
- Cortese, S.; Adamo, N.; Del Giovane, C.; Mohr-Jensen, C.; Hayes, A.J.; Carucci, S.; Atkinson, L.Z.; Tessari, L.; Banaschewski, T.; Coghill, D.; et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: A systematic review and network meta-analysis. Lancet Psychiatry 2018, 5, 727–738. [Google Scholar] [CrossRef]
- Castells, X.; Blanco-Silvente, L.; Cunill, R. Amphetamines for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst. Rev. 2018, 2018, CD007813. [Google Scholar] [CrossRef]
- Knouse, L.E.; Safren, S.A. Current status of cognitive behavioral therapy for adult attention-deficit hyperactivity disorder. Psychiatr. Clin. N. Am. 2010, 33, 497–509. [Google Scholar] [CrossRef]
- Aoshima, K.A.; Banu, S.; Udoetuk, S.; Shah, A.A.; Moukaddam, N. To Prescribe or Not? Pharmacological Options in Adult Attention-Deficit/Hyperactivity Disorder. Psychiatr. Ann. 2017, 47, 303–308. [Google Scholar] [CrossRef]
- Treatment in adult ADHD|Oxford Textbook of Attention Deficit Hyperactivity Disorder|Oxford Academic. Available online: https://academic.oup.com/book/24517/chapter-abstract/187669990?redirectedFrom=fulltext (accessed on 10 August 2025).
- Schoeman, R.; de Klerk, M. Adult attention-deficit hyperactivity disorder: A database analysis of South African private health insurance. S. Afr. J. Psychiatr. 2017, 23, 1010. [Google Scholar]
- Thomsen, P.H.; Houmann, T.; Ishøy, P.L. Pharmacological treatment of ADHD in children and adults. Ugeskr Laeger 2025, 187, V10240755. [Google Scholar] [CrossRef]
- Levin, C.J.; Goodman, D.W.; Adler, L.A. Review of Cardiovascular Effects of ADHD Medications. Psychiatr. Ann. 2018, 48, 323–327. [Google Scholar] [CrossRef]
- Wojnowski, N.M.; Zhou, E.; Jee, Y.H. Effect of stimulants on final adult height. J. Pediatr. Endocrinol. Metab. 2022, 35, 1337–1344. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Attention-Deficit/Hyperactivity Disorder Medications for Adults: Drugs; Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2024.
- Santosh, P.J.; Sattar, S.; Canagaratnam, M. Efficacy and tolerability of pharmacotherapies for attention-deficit hyperactivity disorder in adults. CNS Drugs 2011, 25, 737–763. [Google Scholar] [CrossRef]
- Sogard, A.S.; Mickleborough, T.D. The therapeutic potential of exercise and caffeine on attention-deficit/hyperactivity disorder in athletes. Front. Neurosci. 2022, 16, 978336. [Google Scholar] [CrossRef]
- Kazarov, C.; Peasah, S.K.; McConnell, E.; Fischer, K.K.; Good, C.B. Trends in Pediatric Attention-Deficit Hyperactive Disorder Diagnoses and Prescription Utilization: 2016 to 2019. J. Dev. Behav. Pediatr. 2024, 45, e397–e405. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Raga, J.; Knecht, C.; de Alvaro, R. Profile of guanfacine extended release and its potential in the treatment of attention-deficit hyperactivity disorder. Neuropsychiatr. Dis. Treat 2015, 11, 1359–1370. [Google Scholar] [CrossRef]
- Tan, X.; Xu, Y.; Wang, S.; Li, J.; Hu, C.; Chen, Z.; Cheng, Q.; Wang, Z. Efficacy and Safety of SPN-812 (Extended-Release Viloxazine) in Children and Adolescents with Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Brain Sci. 2023, 13, 1627. [Google Scholar] [CrossRef]
- Kawabe, K.; Horiuchi, F.; Matsumoto, Y.; Inoue, S.; Okazawa, M.; Hosokawa, R.; Nakachi, K.; Soga, J.; Ueno, S. Practical clinical guidelines and pharmacological treatment for attention-deficit hyperactivity disorder in Asia. Neuropsychopharmacol. Rep. 2024, 44, 29–33. [Google Scholar] [CrossRef]
- Pan, N.; Ma, T.; Liu, Y.; Zhang, S.; Hu, S.; Shekara, A.; Cao, H.; Gong, Q.; Chen, Y. Overlapping and differential neuropharmacological mechanisms of stimulants and nonstimulants for attention-deficit/hyperactivity disorder: A comparative neuroimaging analysis. Psychol. Med. 2025, 54, 4676–4690. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.H.; Mazursky-Horowitz, H.; Chronis-Tuscano, A. Delivering Evidence-Based Treatments for Child Attention-Deficit/Hyperactivity Disorder (ADHD) in the Context of Parental ADHD. Curr. Psychiatry Rep. 2014, 16, 474. [Google Scholar] [CrossRef]
- Stevenson, C.S.; Whitmont, S.; Bornholt, L.; Livesey, D.; Stevenson, R.J. A cognitive remediation programme for adults with Attention Deficit Hyperactivity Disorder. Aust. N. Zeal. J. Psychiatry 2002, 36, 610–616. [Google Scholar] [CrossRef]
- Leaberry, K.D.; Rosen, P.J.; Fogleman, N.D.; Walerius, D.M.; Slaughter, K.E. Comorbid Internalizing and Externalizing Disorders Predict Lability of Negative Emotions Among Children With ADHD. J. Atten. Disord. 2020, 24, 1989–2001. [Google Scholar] [CrossRef]
- Prevatt, F.; Yelland, S. An Empirical Evaluation of ADHD Coaching in College Students. J. Atten. Disord. 2015, 19, 666–677. [Google Scholar] [CrossRef]
- Ing, C.; Mills, J.P. ‘Hey, look at me’: An {auto}ethnographic account of experiencing ADHD symptoms within sport. Qual. Res. Sport, Exerc. Health 2017, 11, 274–283. [Google Scholar] [CrossRef]
- Mitchell, J.T.; Benson, J.W.; Knouse, L.E.; Kimbrel, N.A.; Anastopoulos, A.D. Are Negative Automatic Thoughts Associated with ADHD in Adulthood? Cogn. Ther. Res. 2013, 37, 851–859. [Google Scholar] [CrossRef]
- Waxmonsky, J.G.; Waschbusch, D.A.; Belin, P.; Li, T.; Babocsai, L.; Humphery, H.; Pariseau, M.E.; Babinski, D.E.; Hoffman, M.T.; Haak, J.L.; et al. A Randomized Clinical Trial of an Integrative Group Therapy for Children With Severe Mood Dysregulation. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 196–207. [Google Scholar] [CrossRef] [PubMed]
- López-Pinar, C.; Martínez-Sanchís, S.; Carbonell-Vayá, E.; Sánchez-Meca, J.; Fenollar-Cortés, J. Efficacy of Nonpharmacological Treatments on Comorbid Internalizing Symptoms of Adults With Attention-Deficit/Hyperactivity Disorder: A Meta-Analytic Review. J. Atten. Disord. 2020, 24, 456–478. [Google Scholar] [CrossRef]
- Gaur, S.; Pallanti, S. Treatment Outcomes in an Adult Attention Deficit Hyperactivity Disorder Clinic With a Focus on Executive Functioning and Sluggish Cognitive Tempo. Cureus 2020, 12, e9814. [Google Scholar] [CrossRef]
- Seery, C.; Cochrane, R.H.; Mulcahy, M.; Kilbride, K.; Wrigley, M.; Bramham, J. “A one-stop shop”: Real-world use and app-users’ experiences of a psychoeducational smartphone app for adults with ADHD. Internet Interv. 2025, 39, 100807. [Google Scholar] [CrossRef]
- Weusten, L.H.; Heijnen-Kohl, S.M.J.; Ellison, J.; van Alphen, S.P.J. Interference of attention-deficit hyperactivity disorder in an older adult with a severe personality disorder and dermatillomania. Int. Psychogeriatrics 2014, 26, 341–343. [Google Scholar] [CrossRef]
- Kiraz, S.; Sertçelik, S. Adult attention deficit hyperactivity disorder and early maladaptive schemas. Clin. Psychol. Psychother. 2021, 28, 1055–1064. [Google Scholar] [CrossRef] [PubMed]
- Wietecha, L.A.; Clemow, D.B.; Buchanan, A.S.; Young, J.L.; Sarkis, E.H.; Findling, R.L. Atomoxetine Increased Effect over Time in Adults with Attention-Deficit/Hyperactivity Disorder Treated for up to 6 Months: Pooled Analysis of Two Double-Blind, Placebo-Controlled, Randomized Trials. CNS Neurosci. Ther. 2016, 22, 546–557. [Google Scholar] [CrossRef]
- Knouse, L.E.; Teller, J.; Brooks, M.A. Meta-analysis of cognitive–behavioral treatments for adult ADHD. J. Consult. Clin. Psychol. 2017, 85, 737–750. [Google Scholar] [CrossRef] [PubMed]
- Strålin, E.E.; Thorell, L.B.; Lundgren, T.; Bölte, S.; Bohman, B. Cognitive behavioral therapy for ADHD predominantly inattentive presentation: Randomized controlled trial of two psychological treatments. Front. Psychiatry 2025, 16, 1564506. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food & Drug Administration. Drugs@FDA: FDA-Approved Drugs—New Drug Application 021977; VYVANSE (Lisdexamfetamine Dimesylate). Available online: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=021977 (accessed on 6 November 2025).
- U.S. Food & Drug Administration. Janssen-Cilag Manufacturing, LLC. CONCERTA® (Methylphenidate HCl) Extended-Release Tablets—Prescribing Information, Label Edition 2015; Application No. 021121, Supplement s035. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/021121s035lbl.pdf (accessed on 6 November 2025).
- U.S. Food & Drug Administration. Eli Lilly and Company. STRATTERA® (Atomoxetine Hydrochloride) Capsules—Prescribing Information, NDA 21-411 Package Insert. 2002. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2002/21411_strattera_lbl.pdf (accessed on 6 November 2025).
- U.S. Food & Drug Administration. Adhansia XR® (methylphenidate hydrochloride) Extended-Release Capsules—Prescribing Information, NDA 211964 s000. 2021. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/211964s000lbl.pdf (accessed on 6 November 2025).
- Drug Safety Communications. FDA. 2025. Available online: https://www.fda.gov/drugs/drug-safety-and-availability/drug-safety-communications (accessed on 11 August 2025).
- Pinto, S.; Correia-De-Sá, T.; Sampaio-Maia, B.; Vasconcelos, C.; Moreira, P.; Ferreira-Gomes, J. Eating Patterns and Dietary Interventions in ADHD: A Narrative Review. Nutrients 2022, 14, 4332. [Google Scholar] [CrossRef]
- Catalá-López, F.; Hutton, B.; Núñez-Beltrán, A.; Page, M.J.; Ridao, M.; Saint-Gerons, D.M.; A Catalá, M.; Tabarés-Seisdedos, R.; Moher, D. The pharmacological and non-pharmacological treatment of attention deficit hyperactivity disorder in children and adolescents: A systematic review with network meta-analyses of randomised trials. PLoS ONE 2017, 12, e0180355. [Google Scholar] [CrossRef]
- De Crescenzo, F.; Cortese, S.; Adamo, N.; Janiri, L. Pharmacological and non-pharmacological treatment of adults with ADHD: A meta-review. Évid. Based Ment. Health 2017, 20, 4–11. [Google Scholar] [CrossRef]
- Pelsser, L.; Frankena, K.; Toorman, J.; Pereira, R.R. Retrospective Outcome Monitoring of ADHD and Nutrition (ROMAN): The Effectiveness of the Few-Foods Diet in General Practice. Front. Psychiatry 2020, 11, 96. [Google Scholar] [CrossRef]
- Khoshbakht, Y.; Moghtaderi, F.; Bidaki, R.; Hosseinzadeh, M.; Salehi-Abargouei, A. The effect of dietary approaches to stop hypertension (DASH) diet on attention-deficit hyperactivity disorder (ADHD) symptoms: A randomized controlled clinical trial. Eur. J. Nutr. 2021, 60, 3647–3658. [Google Scholar] [CrossRef] [PubMed]
- Renoux, C.; Shin, J.; Dell’ANiello, S.; Fergusson, E.; Suissa, S. Prescribing trends of attention-deficit hyperactivity disorder (ADHD) medications in UK primary care, 1995–2015. Br. J. Clin. Pharmacol. 2016, 82, 858–868. [Google Scholar] [CrossRef]
- Li, L.; Zhu, N.; Zhang, L.; Kuja-Halkola, R.; D’onofrio, B.M.; Brikell, I.; Lichtenstein, P.; Cortese, S.; Larsson, H.; Chang, Z. ADHD Pharmacotherapy and Mortality in Individuals With ADHD. JAMA 2024, 331, 850–860. [Google Scholar] [CrossRef]
- Kenter, R.M.F.; Gjestad, R.; Lundervold, A.J.; Nordgreen, T. A self-guided internet-delivered intervention for adults with ADHD: Results from a randomized controlled trial. Internet Interv. 2023, 32, 100614. [Google Scholar] [CrossRef]
- Seery, C.; Leonard-Curtin, A.; Naismith, L.; King, N.; O’DOnnell, F.; Byrne, B.; Boyd, C.; Kilbride, K.; Wrigley, M.; McHugh, L.; et al. Feasibility of the Understanding and Managing Adult ADHD Programme: Open-access online group psychoeducation and acceptance and commitment therapy for adults with attention-deficit hyperactivity disorder. BJPsych Open 2024, 10, e163. [Google Scholar] [CrossRef]
- Bozzatello, P.; Rocca, P.; Mantelli, E.; Bellino, S. Polyunsaturated Fatty Acids: What is Their Role in Treatment of Psychiatric Disorders? Int. J. Mol. Sci. 2019, 20, 5257. [Google Scholar] [CrossRef] [PubMed]
- Landaas, E.T.; Aarsland, T.I.M.; Ulvik, A.; Halmøy, A.; Ueland, P.M.; Haavik, J. Vitamin levels in adults with ADHD. BJPsych Open 2016, 2, 377–384. [Google Scholar] [CrossRef] [PubMed]
- A Gordon, H.; Rucklidge, J.J.; Blampied, N.M.; Johnstone, J.M. Clinically Significant Symptom Reduction in Children with Attention-Deficit/Hyperactivity Disorder Treated with Micronutrients: An Open-Label Reversal Design Study. J. Child Adolesc. Psychopharmacol. 2015, 25, 783–798. [Google Scholar] [CrossRef]
- French, B.; Nalbant, G.; Wright, H.; Sayal, K.; Daley, D.; Groom, M.J.; Cassidy, S.; Hall, C.L. The impacts associated with having ADHD: An umbrella review. Front. Psychiatry 2024, 15, 1343314. [Google Scholar] [CrossRef]
- Cherkasova, M.V.; Roy, A.; Molina, B.S.; Scott, G.; Weiss, G.; Barkley, R.A.; Biederman, J.; Uchida, M.; Hinshaw, S.P.; Owens, E.B.; et al. Review: Adult Outcome as Seen Through Controlled Prospective Follow-up Studies of Children With Attention-Deficit/Hyperactivity Disorder Followed Into Adulthood. J. Am. Acad. Child Adolesc. Psychiatry 2022, 61, 378–391. [Google Scholar] [CrossRef]
- Biederman, J.; Faraone, S.V. The Effects of Attention-Deficit/Hyperactivity Disorder on Employment and Household Income. MedGenMed 2006, 8, 12. [Google Scholar]
- Adamou, M.; Arif, M.; Asherson, P.; Aw, T.-C.; Bolea, B.; Coghill, D.; Guðjónsson, G.; Halmøy, A.; Hodgkins, P.; Müller, U.; et al. Occupational issues of adults with ADHD. BMC Psychiatry 2013, 13, 59. [Google Scholar] [CrossRef]
- Ahlberg, R.; Du Rietz, E.; Ahnemark, E.; Andersson, L.M.; Werner-Kiechle, T.; Lichtenstein, P.; Larsson, H. Real-life instability in ADHD from young to middle adulthood: A nationwide register-based study of social and occupational problems. BMC Psychiatry 2023, 23, 336. [Google Scholar] [CrossRef]
- Young, S.; Morris, R.; Toone, B.; Tyson, C. Planning ability in adults with attention-deficit/hyperactivity disorder. Neuropsychology 2007, 21, 581–589. [Google Scholar] [CrossRef]
- Young, S.; Morris, R.; Toone, B.; Tyson, C. Spatial working memory and strategy formation in adults diagnosed with attention deficit hyperactivity disorder. Pers. Individ. Differ. 2006, 41, 653–661. [Google Scholar] [CrossRef]
- Fuermaier, A.B.M.; Tucha, L.; Butzbach, M.; Weisbrod, M.; Aschenbrenner, S.; Tucha, O. ADHD at the workplace: ADHD symptoms, diagnostic status, and work-related functioning. J. Neural Transm. 2021, 128, 1021–1031. [Google Scholar] [CrossRef]
- Oscarsson, M.; Nelson, M.; Rozental, A.; Ginsberg, Y.; Carlbring, P.; Jönsson, F. Stress and work-related mental illness among working adults with ADHD: A qualitative study. BMC Psychiatry 2022, 22, 751. [Google Scholar] [CrossRef] [PubMed]
- Kubik, J.A. Efficacy of ADHD coaching for adults with ADHD. J. Atten. Disord. 2010, 13, 442–453. [Google Scholar] [CrossRef] [PubMed]
- Kahveci Öncü, B.; Tutarel Kişlak, Ş. Marital Adjustment and Marital Conflict in Individuals Diagnosed with ADHD and Their Spouses. Noro Psikiyatr Ars 2022, 59, 127–132. [Google Scholar] [CrossRef]
- Ginapp, C.M.; Greenberg, N.R.; Macdonald-Gagnon, G.; Angarita, G.A.; Bold, K.W.; Potenza, M.N. The experiences of adults with ADHD in interpersonal relationships and online communities: A qualitative study. SSM-Qual. Res. Health 2023, 3, 100223. [Google Scholar] [CrossRef]
- Mokrova, I.; O’Brien, M.; Calkins, S.; Keane, S. Parental ADHD Symptomology and Ineffective Parenting: The Connecting Link of Home Chaos. Parenting 2010, 10, 119–135. [Google Scholar] [CrossRef]
- Støre, S.J.; Van Zalk, N.; Schwartz, W.G.; Nilsson, V.; Tillfors, M. The Relationship Between Social Anxiety Disorder and ADHD in Adolescents and Adults: A Systematic Review. J. Atten. Disord. 2024, 28, 1299–1319. [Google Scholar] [CrossRef]
- Nyström, A.; Petersson, K.; Janlöv, A.-C. Being Different but Striving to Seem Normal: The Lived Experiences of People Aged 50+ with ADHD. Issues Ment. Health Nurs. 2020, 41, 476–485. [Google Scholar] [CrossRef] [PubMed]
- Young, S.; Klassen, L.J.; Reitmeier, S.D.; Matheson, J.D.; Gudjonsson, G.H. Let’s Talk about Sex… and ADHD: Findings from an Anonymous Online Survey. Int. J. Environ. Res. Public Health 2023, 20, 2037. [Google Scholar] [CrossRef] [PubMed]
- Cortese, S.; Kelly, C.; Chabernaud, C.; Proal, E.; Di Martino, A.; Milham, M.P.; Castellanos, F.X. Toward systems neuroscience of ADHD: A meta-analysis of 55 fMRI studies. Am. J. Psychiatry 2012, 169, 1038–1055. [Google Scholar] [CrossRef]
- Hoogman, M.; Bralten, J.; Hibar, D.P.; Mennes, M.; Zwiers, M.P.; Schweren, L.S.J.; van Hulzen, K.J.E.; Medland, S.E.; Shumskaya, E.; Jahanshad, N.; et al. Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: A cross-sectional mega-analysis. Lancet Psychiatry 2017, 4, 310–319. [Google Scholar] [CrossRef]
- Oades, R.D.; Dauvermann, M.R.; Schimmelmann, B.G.; Schwarz, M.J.; Myint, A.-M. Attention-deficit hyperactivity disorder (ADHD) and glial integrity: S100B, cytokines and kynurenine metabolism-effects of medication. Behav. Brain Funct. 2010, 6, 29. [Google Scholar] [CrossRef]
- Thapar, A.; Cooper, M.; Eyre, O.; Langley, K. Practitioner Review: What have we learnt about the causes of ADHD? J. Child Psychol. Psychiatry 2013, 54, 3–16. [Google Scholar] [CrossRef] [PubMed]
| Region | Estimated Prevalence (%) | Methodological and Clinical Interpretation | Source |
|---|---|---|---|
| Globally | 2.5–6.7% (Average approx. 2.8%) | Very large variability; lower values (~2.5%) reflect strict clinical diagnoses, higher values (up to 6.7%) come from screening studies based on self-report. | [2,5] |
| Europe (EU) | 2.0–5.0% (Typically 3–4%) | Likely underestimation due to differences in access to diagnosis and variation in healthcare systems. | [5,24,25] |
| North America (USA) | ~4.4% | Higher rate than in Europe, likely reflecting greater clinical awareness and more developed diagnostic infrastructure. | [26,27,28] |
| North America (Canada) | ~3.3% | Heterogeneous results, similar to European estimates. | [29,30] |
| South America | 2.0–10.0% | Limited and highly inconsistent methodological data; reliable conclusions cannot be drawn. | [5] |
| Asia | 2.0–6.9% | High variability; reporting strongly influenced by cultural factors, including mental health stigma. | [31,32] |
| Middle East and North Africa | ~13.5% | Rate appears extremely high compared to other regions; requires urgent methodological verification. | [24] |
| Australia | ~3.4% | Consistent with other high-income countries with developed healthcare systems (Europe, Canada). | [33] |
| Region | Sample (Type) | Age | Key Finding: % First Diagnosed in Adulthood | Source |
|---|---|---|---|---|
| USA (national) | Population survey (NCHS RSS, N ≈ 7000) | ≥18 years | 55.9% of adults with ADHD were first diagnosed at age ≥ 18 | [35] |
| USA | Psychiatrists/PCPs chart review (N = 854) | ≥18 years | ~75% were first diagnosed in adulthood (only 25% had a childhood diagnosis) | [36] |
| Japan | National insurance claims (N = 838,265 new ADHD) | ≥20 years | 40% of all new ADHD cases were in adults | [37] |
| Domain | Functional Component | DSM-5 Symptom Examples | Common Clinical Features and Underlying Deficits | Source |
|---|---|---|---|---|
| Cognitive (Inattention) | Sustained Attention | “Fails to give close attention to details” | Difficulty maintaining focus during monotonous tasks (e.g., lectures, reading); high susceptibility to distraction | [87,91] |
| Executive Function (Working Memory) | Working Memory Capacity | “Often forgetful in daily activities” | Forgets multi-step directions; difficulty holding and manipulating information (e.g., mental math, instructions) | [87,91] |
| Executive Function (Organization) | Task Planning and Organization | “Difficulty organizing tasks and activities” | Poor time management; chronic lateness; disorganized environment; difficulty initiating tasks (procrastination). | [87,91] |
| Cognitive (Hyperactivity/Impulsivity) | Behavioral Inhibitory Control | “Often interrupts or intrudes on others” | Blurting out answers; hasty decisions without adequate information; difficulty waiting in line. | [92,93] |
| Hyperactivity (Internalized) | Internal Restlessness | “Is often ‘on the go’ acting as if ‘driven by a motor’” | Subjective inner restlessness; difficulty relaxing; fidgeting (e.g., tapping pen, shaking leg). | [92,94] |
| Emotional (Non-DSM Core Criteria) | Emotional Instability/Dysregulation | Not listed as core DSM-5 symptom (classified as “associated feature”) | Low frustration tolerance; rapid, intense mood swings; irritability; difficulty calming down. | [95] |
| Emotional Impulsivity | Emotional Urgency/Affective Impulsivity | Not listed as core DSM-5 symptom | “Negative urgency”; rash actions under emotional stress (e.g., angry emails, impulsive purchases). | [95] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bogdańska-Chomczyk, E.; Majewski, M.K.; Kozłowska, A. ADHD in Adulthood: Clinical Presentation, Comorbidities, and Treatment Perspectives. Int. J. Mol. Sci. 2025, 26, 11020. https://doi.org/10.3390/ijms262211020
Bogdańska-Chomczyk E, Majewski MK, Kozłowska A. ADHD in Adulthood: Clinical Presentation, Comorbidities, and Treatment Perspectives. International Journal of Molecular Sciences. 2025; 26(22):11020. https://doi.org/10.3390/ijms262211020
Chicago/Turabian StyleBogdańska-Chomczyk, Ewelina, Mariusz Krzysztof Majewski, and Anna Kozłowska. 2025. "ADHD in Adulthood: Clinical Presentation, Comorbidities, and Treatment Perspectives" International Journal of Molecular Sciences 26, no. 22: 11020. https://doi.org/10.3390/ijms262211020
APA StyleBogdańska-Chomczyk, E., Majewski, M. K., & Kozłowska, A. (2025). ADHD in Adulthood: Clinical Presentation, Comorbidities, and Treatment Perspectives. International Journal of Molecular Sciences, 26(22), 11020. https://doi.org/10.3390/ijms262211020







