Network Controllability Reveals Key Mitigation Points for Tumor-Promoting Signaling in Tumor-Educated Platelets
Abstract
1. Introduction
2. Results
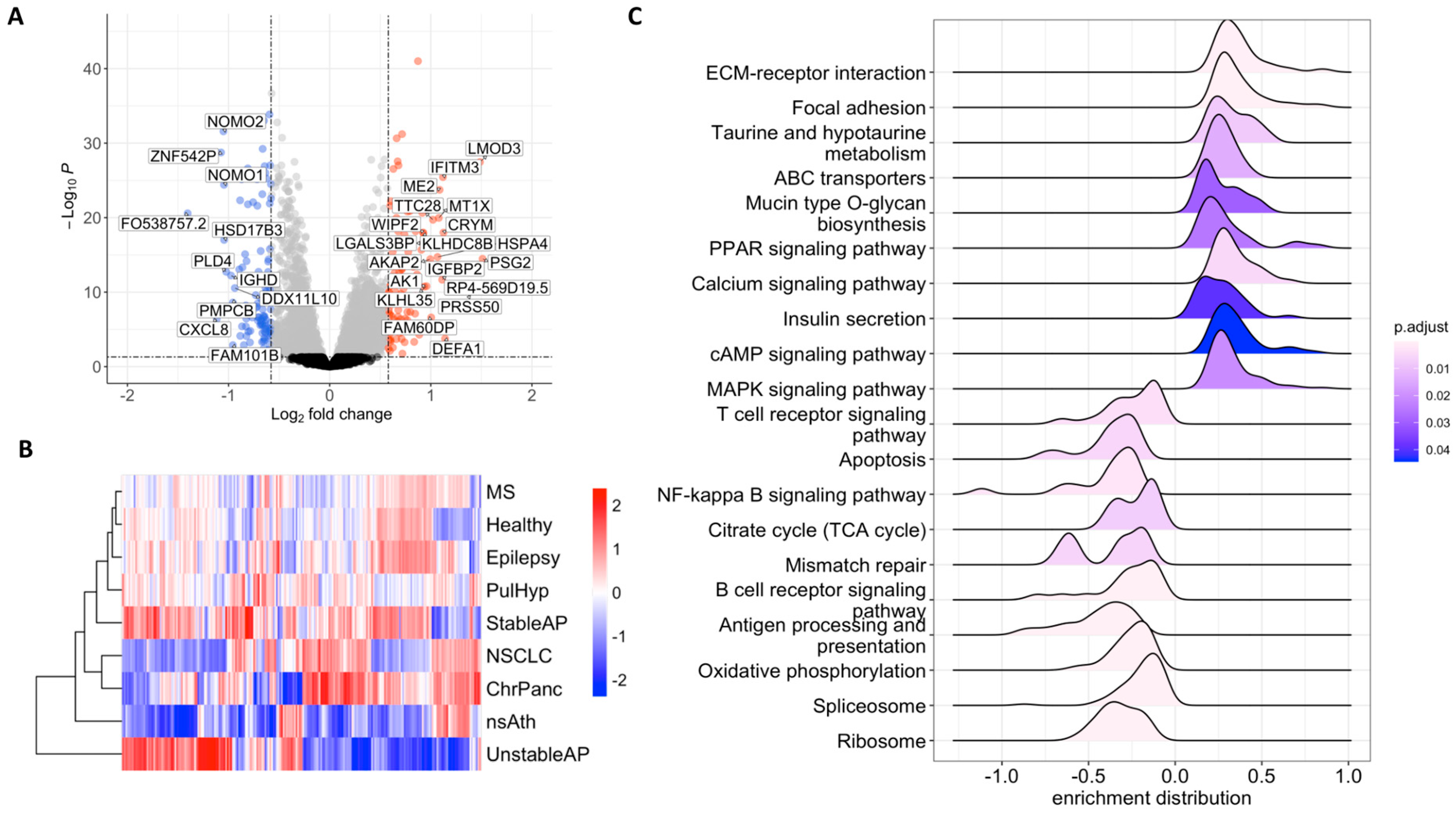
2.1. RNA Profiles of Tumor-Educated Platelets in NSCLC
2.2. Therapeutic Target Discovery Based on Transcriptome Data
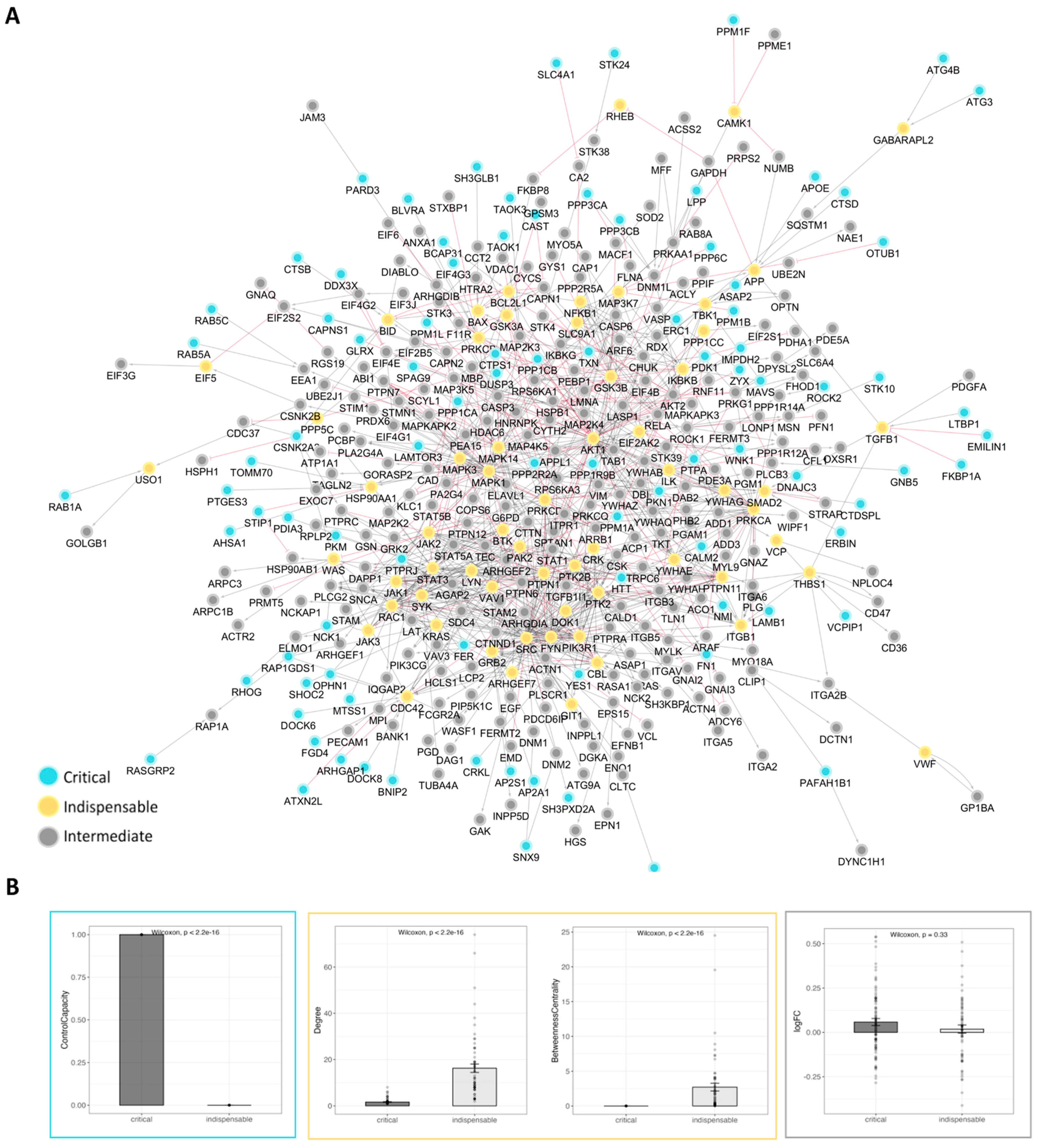
2.3. Therapeutic Target Discovery Based on Network Controllability
2.4. Expanded Platelet Interactome Reveals Novel Targetable Nodes
- -
- Datasheet S13 analyzes another TEP cohort (GSE68086; Best et al.) comparing breast cancer vs healthy. Results mirror our findings, with our top genes (ITGA2B, FLNA, GRB2, FCGR2A, APP) among the highest-ranking DEGs (|log2FC| ≈ 2–3).
- -
- Datasheet S14 reuses the same GEO cohort (GSE183635) to compare pancreatic cancer with healthy controls. Our genes appeared again with very similar differential expression (often with slightly higher logFC), both across datasets and relative to each other.
3. Discussion
3.1. Targeting Tumor-Educated Platelet Signaling
3.2. Limitations and Outlook
4. Materials and Methods
4.1. RNAseq Data Analysis
4.2. Differential Gene Expression Analysis and Data Normalization
4.3. Volcano Plots and Heatmaps
4.4. Gene Set Enrichment Analysis
4.5. Clustering of DEGs
4.6. Construction of Platelet Signaling Network
4.7. Network Controllability and Subnetworks
4.8. Gene Scores and Subnetworks
4.9. Drug Repurposing
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Metharom, P.; Falasca, M.; Berndt, M.C. The History of Armand Trousseau and Cancer-Associated Thrombosis. Cancers 2019, 11, 158. [Google Scholar] [CrossRef]
- Crissman, J.D.; Hatfield, J.; Schaldenbrand, M.; Sloane, B.F.; Honn, K.V. Arrest and extravasation of B16 amelanotic melanoma in murine lungs. A light and electron microscopic study. Lab. Investig. 1985, 53, 470–478. [Google Scholar] [PubMed]
- Gasic, G.J.; Boettiger, D.; Catalfamo, J.L.; Gasic, T.B.; Stewart, G.J. Aggregation of platelets and cell membrane vesiculation by rat cells transformed in vitro by Rous sarcoma virus. Cancer Res. 1978, 38, 2950–2955. [Google Scholar]
- Stone, R.L.; Nick, A.M.; McNeish, I.A.; Balkwill, F.; Han, H.D.; Bottsford-Miller, J.; Rupaimoole, R.; Armaiz-Pena, G.N.; Pecot, C.V.; Coward, J.; et al. Paraneoplastic thrombocytosis in ovarian cancer. N. Engl. J. Med. 2012, 366, 610–618, Erratum in N. Engl. J. Med. 2012, 367, 1768.. [Google Scholar] [CrossRef]
- Menter, D.G.; Tucker, S.C.; Kopetz, S.; Sood, A.K.; Crissman, J.D.; Honn, K.V. Platelets and cancer: A casual or causal relationship: Revisited. Cancer Metastasis Rev. 2014, 33, 231–269. [Google Scholar] [CrossRef]
- Haemmerle, M.; Bottsford-Miller, J.; Pradeep, S.; Taylor, M.L.; Choi, H.-J.; Hansen, J.M.; Dalton, H.J.; Stone, R.L.; Cho, M.S.; Nick, A.M.; et al. FAK regulates platelet extravasation and tumor growth after antiangiogenic therapy withdrawal. J. Clin. Investig. 2016, 126, 1885–1896. [Google Scholar] [CrossRef]
- Varki, A. Trousseau’s syndrome: Multiple definitions and multiple mechanisms. Blood 2007, 110, 1723–1729. [Google Scholar] [CrossRef]
- Khorana, A.A.; Connolly, G.C. Assessing risk of venous thromboembolism in the patient with cancer. J. Clin. Oncol. 2009, 27, 4839–4847. [Google Scholar] [CrossRef] [PubMed]
- Lyman, G.H.; Khorana, A.A. Cancer, clots and consensus: New understanding of an old problem. J. Clin. Oncol. 2009, 27, 4821–4826. [Google Scholar] [CrossRef]
- Bailey, S.E.; Ukoumunne, O.C.; Shephard, E.; Hamilton, W. Clinical relevance of thrombocytosis in primary care: A prospective cohort study of cancer incidence using English electronic medical records and cancer registry data. Br. J. Gen. Pract. 2017, 67, e405–e413. [Google Scholar] [CrossRef] [PubMed]
- Abdulrahman, G.O.; Das, N.; Singh, K.L. The predictive role of thrombocytosis in benign, borderline and malignant ovarian tumors. Platelets 2020, 31, 795–800. [Google Scholar] [CrossRef]
- Skorek, P.; Stępień, K.; Fila, M.; Hauer, J.; Kużdżał, J. Preoperative thrombocytosis in surgically treated patients with non-small cell lung cancer. Pol. Arch. Intern. Med. 2018, 128, 512–517. [Google Scholar] [CrossRef]
- Li, N. Platelets in cancer metastasis: To help the “villain” to do evil. Int. J. Cancer 2016, 138, 2078–2087. [Google Scholar] [CrossRef]
- Sasaki, Y.; Takahashi, T.; Miyazaki, H.; Matsumoto, A.; Kato, T.; Nakamura, K.; Iho, S.; Okuno, Y.; Nakao, K. Production of thrombopoietin by human carcinomas and its novel isoforms. Blood 1999, 94, 1952–1960. [Google Scholar] [CrossRef]
- Calverley, D.C.; Phang, T.L.; Choudhury, Q.G.; Gao, B.; Oton, A.B.; Weyant, M.J.; Geraci, M.W. Significant downregulation of platelet gene expression in metastatic lung cancer. Clin. Transl. Sci. 2010, 3, 227–232. [Google Scholar] [CrossRef]
- Sabrkhany, S.; Kuijpers, M.J.E.; Knol, J.C.; Olde Damink, S.W.M.; Dingemans, A.C.; Verheul, H.M.; Piersma, S.R.; Pham, T.V.; Griffioen, A.W.; Oude Egbrink, M.G.A.; et al. Exploration of the platelet proteome in patients with early-stage cancer. J. Proteomics 2018, 177, 65–74. [Google Scholar] [CrossRef]
- Denis, M.M.; Tolley, N.D.; Bunting, M.; Schwertz, H.; Jiang, H.; Lindemann, S.; Yost, C.C.; Rubner, F.J.; Albertine, K.H.; Swoboda, K.J.; et al. Escaping the nuclear confines: Signal-dependent pre-mRNA splicing in anucleate platelets. Cell 2005, 122, 379–391. [Google Scholar] [CrossRef]
- Li, S.; Lu, Z.; Wu, S.; Chu, T.; Li, B.; Qi, F.; Zhao, Y.; Nie, G. The dynamic role of platelets in cancer progression and their therapeutic implications. Nat. Rev. Cancer 2024, 24, 72–87. [Google Scholar] [CrossRef]
- Skog, J.; Würdinger, T.; Van Rijn, S.; Meijer, D.H.; Gainche, L.; Curry, W.T., Jr.; Carter, B.S.; Krichevsky, A.M.; Breakefield, X.O. Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nat. Cell Biol. 2008, 10, 1470–1476. [Google Scholar] [CrossRef]
- Banerjee, M.; Whiteheart, S.W. The ins and outs of endocytic trafficking in platelet functions. Curr. Opin. Hematol. 2017, 24, 467–474. [Google Scholar] [CrossRef]
- Murphy, L.; Inchauspé, J.; Valenzano, G.; Holland, P.; Sousos, N.; Belnoue-Davis, H.L.; Li, R.; Jooss, N.J.; Benlabiod, C.; Murphy, E.; et al. Platelets sequester extracellular DNA, capturing tumor-derived and free fetal DNA. Science 2025, 389, eadp3971. [Google Scholar] [CrossRef]
- Kuznetsov, H.S.; Marsh, T.; Markens, B.A.; Castaño, Z.; Greene-Colozzi, A.; Hay, S.A.; Brown, V.E.; Richardson, A.L.; Signoretti, S.; Battinelli, E.M.; et al. Identification of luminal breast cancers that establish a tumor-supportive macroenvironment defined by proangiogenic platelets and bone marrow-derived cells. Cancer Discov. 2012, 2, 1150–1165. [Google Scholar] [CrossRef]
- Kerr, B.A.; McCabe, N.P.; Feng, W.; Byzova, T.V. Platelets govern pre-metastatic tumor communication to bone. Oncogene 2013, 32, 4319–4324. [Google Scholar] [CrossRef]
- Roweth, H.G.; Battinelli, E.M. Lessons to learn from tumor-educated platelets. Blood 2021, 137, 3174–3180. [Google Scholar] [CrossRef] [PubMed]
- Weyrich, A.S.; Dixon, D.A.; Pabla, R.; Elstad, M.R.; McIntyre, T.M.; Prescott, S.M.; Zimmerman, G.A. Signal-dependent translation of a regulatory protein, Bcl-3, in activated human platelets. Proc. Natl. Acad. Sci. USA 1998, 95, 5556–5561. [Google Scholar] [CrossRef]
- Nilsson, R.J.; Balaj, L.; Hulleman, E.; Van Rijn, S.; Pegtel, D.M.; Walraven, M.; Widmark, A.; Gerritsen, W.R.; Verheul, H.M.; Vandertop, W.P.; et al. Blood platelets contain tumor-derived RNA biomarkers. Blood 2011, 118, 3680–3683. [Google Scholar] [CrossRef] [PubMed]
- Ye, B.; Li, F.; Chen, M.; Weng, Y.; Qi, C.; Xie, Y.; Zhang, Q.; Ding, H.; Zhang, J.; Gao, X. A panel of platelet-associated circulating long non-coding RNAs as potential biomarkers for colorectal cancer. Genomics 2022, 114, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Tabaeian, S.P.; Eshkiki, Z.S.; Dana, F.; Fayyaz, F.; Baniasadi, M.; Agah, S.; Masoodi, M.; Safari, E.; Sedaghat, M.; Abedini, P.; et al. Evaluation of tumor-educated platelet long non-coding RNAs (lncRNAs) as potential diagnostic biomarkers for colorectal cancer. J. Cancer Res. Ther. 2024, 20, 1453–1458. [Google Scholar] [CrossRef]
- Moonmuang, S.; Chaiyawat, P.; Jantrapirom, S.; Pruksakorn, D.; Piccolo, L.L. Circulating Long Non-Coding RNAs as Novel Potential Biomarkers for Osteogenic Sarcoma. Cancers 2021, 13, 4214. [Google Scholar] [CrossRef]
- Yuan, M.; Jia, Y.; Xing, Y.; Wang, Y.; Liu, Y.; Liu, X.; Liu, D. Screening and validation of platelet activation-related lncRNAs as potential biomarkers for prognosis and immunotherapy in gastric cancer patients. Front. Genet. 2022, 13, 965033. [Google Scholar] [CrossRef]
- Laffont, B.; Corduan, A.; Plé, H.; Duchez, A.-C.; Cloutier, N.; Boilard, E.; Provost, P. Activated platelets can deliver mRNA regulatory Ago2*microRNA complexes to endothelial cells via microparticles. Blood 2013, 122, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Mammadova-Bach, E.; Gil-Pulido, J.; Sarukhanyan, E.; Burkard, P.; Shityakov, S.; Schonhart, C.; Stegner, D.; Remer, K.; Nurden, P.; Nurden, A.T.; et al. Platelet glycoprotein VI promotes metastasis through interaction with cancer cell-derived galectin-3. Blood 2020, 135, 1146–1160. [Google Scholar] [CrossRef]
- Ichikawa, J.; Ando, T.; Kawasaki, T.; Sasaki, T.; Shirai, T.; Tsukiji, N.; Kimura, Y.; Aoki, K.; Hayakawa, K.; Suzuki-Inoue, K.; et al. Role of Platelet C-Type Lectin-Like Receptor 2 in Promoting Lung Metastasis in Osteosarcoma. J. Bone Miner. Res. 2020, 35, 1738–1750. [Google Scholar] [CrossRef]
- Mitrugno, A.; Williams, D.; Kerrigan, S.W.; Moran, N. A novel and essential role for FcγRIIa in cancer cell-induced platelet activation. Blood 2014, 123, 249–260. [Google Scholar] [CrossRef]
- Miao, S.; Shu, D.; Zhu, Y.; Lu, M.; Zhang, Q.; Pei, Y.; He, A.-D.; Ma, R.; Zhang, B.; Ming, Z.-Y. Cancer cell-derived immunoglobulin G activates platelets by binding to platelet FcγRIIa. Cell Death Dis. 2019, 10, 87. [Google Scholar] [CrossRef]
- Strasenburg, W.; Jóźwicki, J.; Durślewicz, J.; Kuffel, B.; Kulczyk, M.P.; Kowalewski, A.; Grzanka, D.; Drewa, T.; Adamowicz, J. Tumor Cell-Induced Platelet Aggregation as an Emerging Therapeutic Target for Cancer Therapy. Front. Oncol. 2022, 12, 909767. [Google Scholar] [CrossRef]
- Heinmoller, E.; Weinel, R.J.; Heidtmann, H.H.; Salge, U.; Seitz, R.; Schmitz, I.; Müller, K.M.; Zirngibl, H. Studies on tumor-cell-induced platelet aggregation in human lung cancer cell lines. J. Cancer Res. Clin. Oncol. 1996, 122, 735–744. [Google Scholar] [CrossRef] [PubMed]
- Jurasz, P.; Alonso-Escolano, D.; Radomski, M.W. Platelet-Cancer interactions: Mechanisms and pharmacology of tumour cell-induced platelet aggregation. Br. J. Pharmacol. 2004, 143, 819–826. [Google Scholar] [CrossRef]
- Cooke, N.M.; Egan, K.; McFadden, S.; Grogan, L.; Breathnach, O.S.; O’Leary, J.; Hennessy, B.T.; Kenny, D. Increased platelet reactivity in patients with late-stage metastatic cancer. Cancer Med. 2013, 2, 564–570. [Google Scholar] [CrossRef]
- Tesfamariam, B. Involvement of platelets in tumor cell metastasis. Pharmacol. Ther. 2016, 157, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Mammadova-Bach, E.; Mangin, P.; Lanza, F.; Gachet, C. Platelets in cancer. From basic research to therapeutic implications. Hamostaseologie 2015, 35, 325–336. [Google Scholar] [CrossRef] [PubMed]
- Palacios-Acedo, A.L.; Mège, D.; Crescence, L.; Dignat-George, F.; Dubois, C.; Panicot-Dubois, L. Platelets, Thrombo-Inflammation, and Cancer: Collaborating with the Enemy. Front. Immunol. 2019, 10, 1805. [Google Scholar] [CrossRef]
- Filippelli, A.; Del Gaudio, C.; Simonis, V.; Ciccone, V.; Spini, A.; Donnini, S. Scoping Review on Platelets and Tumor Angiogenesis: Do We Need More Evidence or Better Analysis? Int. J. Mol. Sci. 2022, 23, 13401. [Google Scholar] [CrossRef] [PubMed]
- Haemmerle, M.; Stone, R.L.; Menter, D.G.; Afshar-Kharghan, V.; Sood, A.K. The Platelet Lifeline to Cancer: Challenges and Opportunities. Cancer Cell 2018, 33, 965–983. [Google Scholar] [CrossRef] [PubMed]
- von Hundelshausen, P.; Koenen, R.R.; Sack, M.; Mause, S.F.; Adriaens, W.; Proudfoot, A.E.; Hackeng, T.M.; Weber, C. Heterophilic interactions of platelet factor 4 and RANTES promote monocyte arrest on endothelium. Blood 2005, 105, 924–930. [Google Scholar] [CrossRef]
- Ansari, M.J.; Bokov, D.; Markov, A.; Jalil, A.T.; Shalaby, M.N.; Suksatan, W.; Chupradit, S.; Al-Ghamdi, H.S.; Shomali, N.; Zamani, A.; et al. Cancer combination therapies by angiogenesis inhibitors; a comprehensive review. Cell Commun. Signal 2022, 20, 49. [Google Scholar] [CrossRef]
- Pinedo, H.M.; Verheul, H.; D’Amato, R.; Folkman, J. Involvement of platelets in tumour angiogenesis? Lancet 1998, 352, 1775–1777. [Google Scholar] [CrossRef]
- Maurer, S.; Ferrari de Andrade, L. NK Cell Interaction with Platelets and Myeloid Cells in the Tumor Milieu. Front. Immunol. 2020, 11, 608849. [Google Scholar] [CrossRef]
- Placke, T.; Örgel, M.; Schaller, M.; Jung, G.; Rammensee, H.-G.; Kopp, H.-G.; Salih, H.R. Platelet-derived MHC class I confers a pseudonormal phenotype to cancer cells that subverts the antitumor reactivity of natural killer immune cells. Cancer Res. 2012, 72, 440–448. [Google Scholar] [CrossRef]
- Plantureux, L.; Crescence, L.; Dignat-George, F.; Panicot-Dubois, L.; Dubois, C. Effects of platelets on cancer progression. Thromb. Res. 2018, 164 (Suppl. 1), S40–S47. [Google Scholar] [CrossRef]
- Gay, L.J.; Felding-Habermann, B. Contribution of platelets to tumour metastasis. Nat. Rev. Cancer 2011, 11, 123–134. [Google Scholar] [CrossRef] [PubMed]
- Erpenbeck, L.; Schon, M.P. Deadly allies: The fatal interplay between platelets and metastasizing cancer cells. Blood 2010, 115, 3427–3436. [Google Scholar] [CrossRef]
- Lonsdorf, A.S.; Krämer, B.F.; Fahrleitner, M.; Schönberger, T.; Gnerlich, S.; Ring, S.; Gehring, S.; Schneider, S.W.; Kruhlak, M.J.; Meuth, S.G.; et al. Engagement of αIIbβ3 (GPIIb/IIIa) with ανβ3 integrin mediates interaction of melanoma cells with platelets: A connection to hematogenous metastasis. J. Biol. Chem. 2012, 287, 2168–2178. [Google Scholar] [CrossRef]
- Labelle, M.; Begum, S.; Hynes, R.O. Platelets guide the formation of early metastatic niches. Proc. Natl. Acad. Sci. USA 2014, 111, E3053–E3061. [Google Scholar] [CrossRef]
- Foss, A.; Muñoz-Sagredo, L.; Sleeman, J.; Thiele, W. The contribution of platelets to intravascular arrest, extravasation, and outgrowth of disseminated tumor cells. Clin. Exp. Metastasis 2020, 37, 47–67. [Google Scholar] [CrossRef]
- Schumacher, D.; Strilic, B.; Sivaraj, K.K.; Wettschureck, N.; Offermanns, S. Platelet-derived nucleotides promote tumor-cell transendothelial migration and metastasis via P2Y2 receptor. Cancer Cell 2013, 24, 130–137. [Google Scholar] [CrossRef]
- Sierko, E.; Wojtukiewicz, M.Z. Inhibition of platelet function: Does it offer a chance of better cancer progression control? Semin. Thromb. Hemost. 2007, 33, 712–721. [Google Scholar] [CrossRef] [PubMed]
- Seizer, P.; May, A.E. Platelets and matrix metalloproteinases. Thromb. Haemost. 2013, 110, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Vlodavsky, I.; Eldor, A.; Haimovitz-Friedman, A.; Matzner, Y.; Ishai-Michaeli, R.; Lider, O.; Naparstek, Y.; Cohen, I.R.; Fuks, Z. Expression of heparanase by platelets and circulating cells of the immune system: Possible involvement in diapedesis and extravasation. Invasion Metastasis 1992, 12, 112–127. [Google Scholar]
- Giannakeas, V.; Kotsopoulos, J.; Cheung, M.C.; Rosella, L.; Brooks, J.D.; Lipscombe, L.; Akbari, M.R.; Austin, P.C.; Narod, S.A. Analysis of Platelet Count and New Cancer Diagnosis Over a 10-Year Period. JAMA Netw. Open 2022, 5, e2141633. [Google Scholar] [CrossRef]
- Sabrkhany, S.; Kuijpers, M.J.E.; Egbrink, M.G.A.O.; Griffioen, A.W. Platelets as messengers of early-stage cancer. Cancer Metastasis Rev. 2021, 40, 563–573. [Google Scholar] [CrossRef] [PubMed]
- Huong, P.T.; Nguyen, L.T.; Nguyen, X.-B.; Lee, S.K.; Bach, D.-H. The Role of Platelets in the Tumor-Microenvironment and the Drug Resistance of Cancer Cells. Cancers 2019, 11, 240. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Guo, Y.; Chang, Z.; Zhang, D.; Zhang, S.; Pei, H.; Pang, J.; Zhao, Z.J.; Chen, Y. Bidirectional Interaction Between Cancer Cells and Platelets Provides Potential Strategies for Cancer Therapies. Front. Oncol. 2021, 11, 764119. [Google Scholar] [CrossRef]
- Franco, A.T.; Corken, A.; Ware, J. Platelets at the interface of thrombosis, inflammation, and cancer. Blood 2015, 126, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Battinelli, E.M.; Markens, B.A.; Italiano, J.E., Jr. Release of angiogenesis regulatory proteins from platelet alpha granules: Modulation of physiologic and pathologic angiogenesis. Blood 2011, 118, 1359–1369. [Google Scholar] [CrossRef]
- Guillem-Llobat, P.; Dovizio, M.; Bruno, A.; Ricciotti, E.; Cufino, V.; Sacco, A.; Grande, R.; Alberti, S.; Arena, V.; Cirillo, M.; et al. Aspirin prevents colorectal cancer metastasis in mice by splitting the crosstalk between platelets and tumor cells. Oncotarget 2016, 7, 32462–32477. [Google Scholar] [CrossRef]
- Lucotti, S.; Cerutti, C.; Soyer, M.; Gil-Bernabé, A.M.; Gomes, A.L.; Allen, P.D.; Smart, S.; Markelc, B.; Watson, K.; Armstrong, P.C.; et al. Aspirin blocks formation of metastatic intravascular niches by inhibiting platelet-derived COX-1/thromboxane A2. J. Clin. Investig. 2019, 129, 1845–1862. [Google Scholar] [CrossRef]
- Gebremeskel, S.; LeVatte, T.; Liwski, R.S.; Johnston, B.; Bezuhly, M. The reversible P2Y12 inhibitor ticagrelor inhibits metastasis and improves survival in mouse models of cancer. Int. J. Cancer 2015, 136, 234–240. [Google Scholar] [CrossRef]
- Zhang, W.; Dang, S.; Hong, T.; Tang, J.; Fan, J.; Bu, D.; Sun, Y.; Wang, Z.; Wisniewski, T. A humanized single-chain antibody against beta 3 integrin inhibits pulmonary metastasis by preferentially fragmenting activated platelets in the tumor microenvironment. Blood 2012, 120, 2889–2898. [Google Scholar] [CrossRef]
- Amirkhosravi, A.; Mousa, S.A.; Amaya, M.; Blaydes, S.; Desai, H.; Meyer, T.; Francis, J.L. Inhibition of tumor cell-induced platelet aggregation and lung metastasis by the oral GpIIb/IIIa antagonist XV454. Thromb. Haemost. 2003, 90, 549–554. [Google Scholar]
- Khorana, A.A.; Francis, C.W.; Culakova, E.; Kuderer, N.M.; Lyman, G.H. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J. Thromb. Haemost. 2007, 5, 632–634. [Google Scholar] [CrossRef] [PubMed]
- Riedl, J.; Preusser, M.; Nazari, P.M.S.; Posch, F.; Panzer, S.; Marosi, C.; Birner, P.; Thaler, J.; Brostjan, C.; Lötsch, D.; et al. Podoplanin expression in primary brain tumors induces platelet aggregation and increases risk of venous thromboembolism. Blood 2017, 129, 1831–1839. [Google Scholar] [CrossRef] [PubMed]
- Sasano, T.; Gonzalez-Delgado, R.; Muñoz, N.M.; Carlos-Alcade, W.; Cho, M.S.; Sheth, R.A.; Sood, A.K.; Afshar-Kharghan, V. Podoplanin promotes tumor growth, platelet aggregation, and venous thrombosis in murine models of ovarian cancer. J. Thromb. Haemost. 2022, 20, 104–114. [Google Scholar] [CrossRef]
- Wojtukiewicz, M.Z.; Hempel, D.; Sierko, E.; Tucker, S.C.; Honn, K.V. Antiplatelet agents for cancer treatment: A real perspective or just an echo from the past? Cancer Metastasis Rev. 2017, 36, 305–329. [Google Scholar] [CrossRef]
- Best, M.G.; Sol, N.; Veld, S.G.I. ‘.; Vancura, A.; Muller, M.; Niemeijer, A.-L.N.; Fejes, A.V.; Fat, L.-A.T.K.; In ‘t Veld, A.E.H.; Leurs, C.; et al. Swarm Intelligence-Enhanced Detection of Non-Small-Cell Lung Cancer Using Tumor-Educated Platelets. Cancer Cell 2017, 32, 238–252.E9. [Google Scholar] [CrossRef]
- Turei, D.; Korcsmaros, T.; Saez-Rodriguez, J. OmniPath: Guidelines and gateway for literature-curated signaling pathway resources. Nat. Methods 2016, 13, 966–967. [Google Scholar] [CrossRef]
- Osmanoglu, O.; Gupta, S.K.; Almasi, A.; Yagci, S.; Srivastava, M.; Araujo, G.H.M.; Nagy, Z.; Balkenhol, J.; Dandekar, T. Signaling network analysis reveals fostamatinib as a potential drug to control platelet hyperactivation during SARS-CoV-2 infection. Front. Immunol. 2023, 14, 1285345. [Google Scholar] [CrossRef]
- Gaillard, S.; Wilkinson, M.; Martin, L.P.; Deery, A.; Langsdale, A.; Bayable, A.; Zahurak, M.; Huang, P.; Armstrong, D.K.; Shih, I.-M.; et al. A phase 1 study of the SYK inhibitor fostamatinib and weekly paclitaxel for recurrent platinum-resistant ovarian cancer. Am. Soc. Clin. Oncol. 2023, 41, 5574. [Google Scholar] [CrossRef]
- Rolf, M.G.; Curwen, J.O.; Veldman-Jones, M.; Eberlein, C.; Wang, J.; Harmer, A.; Hellawell, C.J.; Braddock, M. In vitro pharmacological profiling of R406 identifies molecular targets underlying the clinical effects of fostamatinib. Pharmacol. Res. Perspect. 2015, 3, e00175. [Google Scholar] [CrossRef]
- Cornish, A.J.; Markowetz, F. SANTA: Quantifying the functional content of molecular networks. PLoS Comput. Biol. 2014, 10, e1003808. [Google Scholar] [CrossRef] [PubMed]
- Knox, C.; Wilson, M.; Klinger, C.M.; Franklin, M.; Oler, E.; Wilson, A.; Pon, A.; Cox, J.; Chin, N.E.L.; Strawbridge, S.A.; et al. DrugBank 6.0: The DrugBank Knowledgebase for 2024. Nucleic Acids Res. 2024, 52, D1265–D1275. [Google Scholar] [CrossRef] [PubMed]
- Mai, S.; Inkielewicz-Stepniak, I. Pancreatic Cancer and Platelets Crosstalk: A Potential Biomarker and Target. Front. Cell Dev. Biol. 2021, 9, 749689. [Google Scholar] [CrossRef]
- Xing, S.; Zeng, T.; Xue, N.; He, Y.; Lai, Y.-Z.; Li, H.-L.; Huang, Q.; Chen, S.-L.; Liu, W.-L. Development and Validation of Tumor-educated Blood Platelets Integrin Alpha 2b (ITGA2B) RNA for Diagnosis and Prognosis of Non-small-cell Lung Cancer through RNA-seq. Int. J. Biol. Sci. 2019, 15, 1977–1992. [Google Scholar] [CrossRef]
- Goswami, C.; Chawla, S.; Thakral, D.; Pant, H.; Verma, P.; Malik, P.S.; Jayadeva, J.; Gupta, R.; Ahuja, G.; Sengupta, D. Molecular signature comprising 11 platelet-genes enables accurate blood-based diagnosis of NSCLC. BMC Genom. 2020, 21, 744, Erratum in BMC Genom. 2020, 21, 877.. [Google Scholar]
- Best, M.G.; Sol, N.; Kooi, I.E.; Tannous, J.; Westerman, B.A.; Rustenburg, F.; Schellen, P.; Verschueren, H.; Post, E.; Koster, J.; et al. RNA-Seq of Tumor-Educated Platelets Enables Blood-Based Pan-Cancer, Multiclass, and Molecular Pathway Cancer Diagnostics. Cancer Cell 2015, 28, 666–676. [Google Scholar] [CrossRef] [PubMed]
- Ge, X.; Yuan, L.; Cheng, B.; Dai, K. Identification of seven tumor-educated platelets RNAs for cancer diagnosis. J. Clin. Lab. Anal. 2021, 35, e23791. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Hong, C.; Luo, Y.; Wei, L.; Luo, Y.; Peng, Y.; Xu, Y. Prognostic value of IGFBP2 in various cancers: A systematic review and meta-analysis. Cancer Med. 2022, 11, 3035–3047. [Google Scholar] [CrossRef] [PubMed]
- Moore, T.; Dveksler, G.S. Pregnancy-specific glycoproteins: Complex gene families regulating maternal-fetal interactions. Int. J. Dev. Biol. 2014, 58, 273–280. [Google Scholar] [CrossRef]
- Ingman, W.V.; Robertson, S.A. The essential roles of TGFB1 in reproduction. Cytokine Growth Factor. Rev. 2009, 20, 233–239. [Google Scholar] [CrossRef]
- Zhao, M.R.; Qiu, W.; Li, Y.-X.; Zhang, Z.-B.; Li, D.; Wang, Y.-L. Dual effect of transforming growth factor beta1 on cell adhesion and invasion in human placenta trophoblast cells. Reproduction 2006, 132, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, S.; Andersen, J.; Norgaard, T. Pregnancy-specific beta 1-glycoprotein (SP1) in serum and tissue from patients with benign and malignant breast tumours. Br. J. Cancer 1984, 49, 663–667. [Google Scholar] [CrossRef][Green Version]
- Skinner, J.M.; Whitehead, R. Pregnancy-specific beta glycoprotein (SP1) in tumours of the human gastrointestinal tract. Br. J. Cancer 1981, 44, 476–478. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhao, J.; Rabadan, R.; Levine, A.J. Pregnancy specific glycoproteins: A possible mediator of immune tolerance of cancers. J. Cell. Immunol. 2021, 3, 109–117. [Google Scholar]
- Pang, J.H.; Coupland, L.A.; Freeman, C.; Chong, B.H.; Parish, C.R. Activation of tumour cell ECM degradation by thrombin-activated platelet membranes: Potentially a P-selectin and GPIIb/IIIa-dependent process. Clin. Exp. Metastasis 2015, 32, 495–505. [Google Scholar] [CrossRef]
- Felding-Habermann, B.; Habermann, R.; Saldívar, E.; Ruggeri, Z.M. Role of beta3 integrins in melanoma cell adhesion to activated platelets under flow. J. Biol. Chem. 1996, 271, 5892–5900. [Google Scholar] [CrossRef] [PubMed]
- Burdick, M.M.; Konstantopoulos, K. Platelet-induced enhancement of LS174T colon carcinoma and THP-1 monocytoid cell adhesion to vascular endothelium under flow. Am. J. Physiol. Cell Physiol. 2004, 287, C539–C547. [Google Scholar] [CrossRef]
- Koch, A.E.; Polverini, P.J.; Kunkel, S.L.; Harlow, L.A.; DiPietro, L.A.; Elner, V.M.; Elner, S.G.; Strieter, R.M. Interleukin-8 as a macrophage-derived mediator of angiogenesis. Science 1992, 258, 1798–1801. [Google Scholar] [CrossRef]
- Strieter, R.M.; Polverini, P.J.; Kunkel, S.L.; Arenberg, D.A.; Burdick, M.D.; Kasper, J.; Dzuiba, J.; Van Damme, J.; Walz, A.; Marriott, D.; et al. The functional role of the ELR motif in CXC chemokine-mediated angiogenesis. J. Biol. Chem. 1995, 270, 27348–27357. [Google Scholar] [CrossRef]
- Cambier, S.; Gouwy, M.; Proost, P. The chemokines CXCL8 and CXCL12: Molecular and functional properties, role in disease and efforts towards pharmacological intervention. Cell. Mol. Immunol. 2023, 20, 217–251. [Google Scholar] [CrossRef]
- Zhu, Y.M.; Webster, S.J.; Flower, D.; Woll, P.J. Interleukin-8/CXCL8 is a growth factor for human lung cancer cells. Br. J. Cancer 2004, 91, 1970–1976. [Google Scholar] [CrossRef]
- Zhang, W.; Qu, H.; Ma, X.; Li, L.; Wei, Y.; Wang, Y.; Zeng, R.; Nie, Y.; Zhang, C.; Yin, K.; et al. Identification of cuproptosis and immune-related gene prognostic signature in lung adenocarcinoma. Front. Immunol. 2023, 14, 1179742. [Google Scholar] [CrossRef]
- Tyagi, T.; Jain, K.; Yarovinsky, T.O.; Chiorazzi, M.; Du, J.; Castro, C.; Griffin, J.; Korde, A.; Martin, K.A.; Takyar, S.S.; et al. Platelet-derived TLT-1 promotes tumor progression by suppressing CD8+ T cells. J. Exp. Med. 2023, 220, e20212218. [Google Scholar] [CrossRef]
- Pandey, P.; Khan, F.; Upadhyay, T.K.; Seungjoon, M.; Park, M.N.; Kim, B. New insights about the PDGF/PDGFR signaling pathway as a promising target to develop cancer therapeutic strategies. Biomed Pharmacother. 2023, 161, 114491, Erratum in Biomed Pharmacother. 2023, 167, 115388.. [Google Scholar] [CrossRef]
- Hers, I. Insulin-like growth factor-1 potentiates platelet activation via the IRS/PI3Kalpha pathway. Blood 2007, 110, 4243–4252. [Google Scholar] [CrossRef] [PubMed]
- Mantini, G.; Meijer, L.L.; Glogovitis, I.; In ‘t Veld, S.G.J.G.; Paleckyte, R.; Capula, M.; Le Large, T.Y.S.; Morelli, L.; Pham, T.V.; Piersma, S.R.; et al. Omics Analysis of Educated Platelets in Cancer and Benign Disease of the Pancreas. Cancers 2020, 13, 66. [Google Scholar] [CrossRef]
- Eslami, S.Z.; Cortés-Hernández, L.E.; Glogovitis, I.; Antunes-Ferreira, M.; D’ambrosi, S.; Kurma, K.; Garima, F.; Cayrefourcq, L.; Best, M.G.; Koppers-Lalic, D.; et al. In vitro cross-talk between metastasis-competent circulating tumor cells and platelets in colon cancer: A malicious association during the harsh journey in the blood. Front. Cell Dev. Biol. 2023, 11, 1209846. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Forbes, M.E.; Fuller, G.N.; Li, J.; Yang, X.; Zhang, W. IGFBP2: Integrative hub of developmental and oncogenic signaling network. Oncogene 2020, 39, 2243–2257. [Google Scholar] [CrossRef] [PubMed]
- Haschemi, R.; Kobelt, D.; Steinwarz, E.; Schlesinger, M.; Stein, U.; Bendas, G. Insulin-like Growth Factor Binding Protein-2 (IGFBP2) Is a Key Molecule in the MACC1-Mediated Platelet Communication and Metastasis of Colorectal Cancer Cells. Int. J. Mol. Sci. 2021, 22, 12195. [Google Scholar] [CrossRef]
- Wei, L.F.; Weng, X.; Huang, X.; Peng, Y.; Guo, H.; Xu, Y. IGFBP2 in cancer: Pathological role and clinical significance (Review). Oncol. Rep. 2021, 45, 427–438. [Google Scholar] [CrossRef]
- Guo, C.; Lu, H.; Gao, W.; Wang, L.; Lu, K.; Wu, S.; Pataer, A.; Huang, M.; El-Zein, R.; Lin, T.; et al. Insulin-like growth factor binding protein-2 level is increased in blood of lung cancer patients and associated with poor survival. PLoS ONE 2013, 8, e74973. [Google Scholar] [CrossRef]
- Wang, J.; Hu, Z.G.; Li, D.; Xu, J.X.; Zeng, Z.G. Gene expression and prognosis of insulin-like growth factor-binding protein family members in non-small cell lung cancer. Oncol. Rep. 2019, 42, 1981–1995. [Google Scholar] [CrossRef]
- Lu, H.; Ai, J.; Zheng, Y.; Zhou, W.; Zhang, L.; Zhu, J.; Zhang, H.; Wang, S. IGFBP2/ITGA5 promotes gefitinib resistance via activating STAT3/CXCL1 axis in non-small cell lung cancer. Cell Death Dis. 2024, 15, 447. [Google Scholar] [CrossRef]
- Saci, A.; Liu, W.Q.; Vidal, M.; Garbay, C.; Rendu, F.; Bachelot-Loza, C. Differential effect of the inhibition of Grb2-SH3 interactions in platelet activation induced by thrombin and by Fc receptor engagement. Biochem. J. 2002, 363, 717–725. [Google Scholar] [CrossRef]
- Vogtle, T.; Baig, A.A.; Volz, J.; Duchow, T.B.; Pleines, I.; Dütting, S.; Nitschke, L.; Watson, S.P.; Nieswandt, B. Critical redundant functions of the adapters Grb2 and Gads in platelet (hem)ITAM signaling in mice. Platelets 2020, 31, 801–811. [Google Scholar] [CrossRef] [PubMed]
- Visconte, C.; Canino, J.; Guidetti, G.F.; Zarà, M.; Seppi, C.; Abubaker, A.A.; Pula, G.; Torti, M.; Canobbio, I. Amyloid precursor protein is required for in vitro platelet adhesion to amyloid peptides and potentiation of thrombus formation. Cell Signal 2018, 52, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.; Michael, J.V.; Naik, U.P.; McKenzie, S.E. Platelet FcγRIIA in immunity and thrombosis: Adaptive immunothrombosis. J. Thromb. Haemost. 2021, 19, 1149–1160. [Google Scholar] [CrossRef]
- Camerer, E.; Qazi, A.A.; Duong, D.N.; Cornelissen, I.; Advincula, R.; Coughlin, S.R. Platelets, protease-activated receptors, and fibrinogen in hematogenous metastasis. Blood 2004, 104, 397–401. [Google Scholar] [CrossRef]
- Palumbo, J.S.; Talmage, K.E.; Massari, J.V.; La Jeunesse, C.M.; Flick, M.J.; Kombrinck, K.W.; Jirousková, M.; Degen, J.L. Platelets and fibrin(ogen) increase metastatic potential by impeding natural killer cell-mediated elimination of tumor cells. Blood 2005, 105, 178–185. [Google Scholar] [CrossRef]
- Trikha, M.; Zhou, Z.; Timar, J.; Raso, E.; Kennel, M.; Emmell, E.; Nakada, M.T. Multiple roles for platelet GPIIb/IIIa and alphavbeta3 integrins in tumor growth, angiogenesis, and metastasis. Cancer Res. 2002, 62, 2824–2833. [Google Scholar] [PubMed]
- Jain, S.; Zuka, M.; Liu, J.; Russell, S.; Dent, J.; Guerrero, J.A.; Forsyth, J.; Maruszak, B.; Gartner, T.K.; Felding-Habermann, B.; et al. Platelet glycoprotein Ibα supports experimental lung metastasis. Proc. Natl. Acad. Sci. USA 2007, 104, 9024–9028. [Google Scholar] [CrossRef]
- Spalton, J.C.; Mori, J.; Pollitt, A.Y.; Hughes, C.E.; Eble, J.A.; Watson, S.P. The novel Syk inhibitor R406 reveals mechanistic differences in the initiation of GPVI and CLEC-2 signaling in platelets. J. Thromb. Haemost. 2009, 7, 1192–1199. [Google Scholar] [CrossRef]
- Harbi, M.H.; Smith, C.W.; Alenazy, F.O.; Nicolson, P.L.R.; Tiwari, A.; Watson, S.P.; Thomas, M.R. Antithrombotic Effects of Fostamatinib in Combination with Conventional Antiplatelet Drugs. Int. J. Mol. Sci. 2022, 23, 6982. [Google Scholar] [CrossRef]
- Apostolidis, S.A.; Sarkar, A.; Giannini, H.M.; Goel, R.R.; Mathew, D.; Suzuki, A.; Baxter, A.E.; Greenplate, A.R.; Alanio, C.; Abdel-Hakeem, M.; et al. Signaling Through FcγRIIA and the C5a-C5aR Pathway Mediate Platelet Hyperactivation in COVID-19. Front. Immunol. 2022, 13, 834988. [Google Scholar] [CrossRef] [PubMed]
- Saha, B.; Mathur, T.; Tronolone, J.J.; Chokshi, M.; Lokhande, G.K.; Selahi, A.; Gaharwar, A.K.; Afshar-Kharghan, V.; Sood, A.K.; Bao, G.; et al. Human tumor microenvironment chip evaluates the consequences of platelet extravasation and combinatorial antitumor-antiplatelet therapy in ovarian cancer. Sci. Adv. 2021, 7, eabg5283. [Google Scholar] [CrossRef]
- Iba, T.; Levy, J.H. The roles of platelets in COVID-19-associated coagulopathy and vaccine-induced immune thrombotic thrombocytopenia. Trends Cardiovasc. Med. 2022, 32, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bye, A.P.; Hoepel, W.; Mitchell, J.L.; Jégouic, S.M.; Loureiro, S.; Sage, T.; Vidarsson, G.; Nouta, J.; Wuhrer, M.; de Taeye, S.W.; et al. Aberrant glycosylation of anti-SARS-CoV-2 spike IgG is a prothrombotic stimulus for platelets. Blood 2021, 138, 1481–1489. [Google Scholar] [CrossRef]
- Gonzalez-Lopez, T.J.; Bermejo-Vega, N.; Cardesa-Cabrera, R.; Martínez-Robles, V.; Aguilar-Monserrate, G.; Pérez-Segura, G.; Domingo, A.; Luis-Navarro, J.; Lakhwani, S.; Acedo, N.; et al. Fostamatinib effectiveness and safety for immune thrombocytopenia in clinical practice. Blood 2024, 144, 646–656. [Google Scholar] [CrossRef]
- Hu, M.; Yin, R.; Deng, K.; Xu, N. Drug repurposing of fostamatinib against cancer via potential cytotoxicity and immune checkpoint regulation. Front. Immunol. 2025, 16, 1602189. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.; Lee, H.; Beck, B.R.; Lee, B.; Lee, J.H.; Kim, S.; Chun, S.H.; Won, H.S.; Ko, Y.H. Repurposing of the Syk inhibitor fostamatinib using a machine learning algorithm. Exp. Ther. Med. 2025, 29, 110. [Google Scholar] [CrossRef]
- Park, S.R.; Speranza, G.; Piekarz, R.; Wright, J.J.; Kinders, R.J.; Wang, L.; Pfister, T.; Trepel, J.B.; Lee, M.-J.; Alarcon, S.; et al. A multi-histology trial of fostamatinib in patients with advanced colorectal, non-small cell lung, head and neck, thyroid, and renal cell carcinomas, and pheochromocytomas. Cancer Chemother. Pharmacol. 2013, 71, 981–990. [Google Scholar] [CrossRef]
- Schror, K. Aspirin and platelets: The antiplatelet action of aspirin and its role in thrombosis treatment and prophylaxis. Semin. Thromb. Hemost. 1997, 23, 349–356. [Google Scholar] [CrossRef]
- Pulcinelli, F.M.; Pignatelli, P.; Celestini, A.; Riondino, S.; Gazzaniga, P.P.; Violi, F. Inhibition of platelet aggregation by aspirin progressively decreases in long-term treated patients. J. Am. Coll. Cardiol. 2004, 43, 979–984. [Google Scholar] [CrossRef]
- van Zijverden, L.M.; Schutte, M.H.; Madsen, M.C.; Bonten, T.N.; Smulders, Y.M.; Wiepjes, C.M.; van Diemen, J.J.K.; Thijs, A. The efficacy of aspirin to inhibit platelet aggregation in patients hospitalised with a severe infection: A multicentre, open-label, randomised controlled trial. Clin. Exp. Med. 2023, 23, 3501–3508. [Google Scholar] [CrossRef]
- Florensa, D.; Mateo, J.; Solsona, F.; Galván, L.; Mesas, M.; Piñol, R.; Espinosa-Leal, L.; Godoy, P. Low-dose acetylsalicylic acid for cancer prevention considering risk factors: A retrospective cohort study. Ann. Epidemiol. 2023, 84, 60–66. [Google Scholar] [CrossRef]
- Yang, J.; Yamashita-Kanemaru, Y.; Morris, B.I.; Contursi, A.; Trajkovski, D.; Xu, J.; Patrascan, I.; Benson, J.; Evans, A.C.; Conti, A.G.; et al. Aspirin prevents metastasis by limiting platelet TXA(2) suppression of T cell immunity. Nature 2025, 640, 1052–1061. [Google Scholar] [CrossRef] [PubMed]
- Sevigny, J.; Chiao, P.; Bussière, T.; Weinreb, P.H.; Williams, L.; Maier, M.; Dunstan, R.; Salloway, S.; Chen, T.; Ling, Y.; et al. The antibody aducanumab reduces Abeta plaques in Alzheimer’s disease. Nature 2016, 537, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Mussbacher, M.; Salzmann, M.; Brostjan, C.; Hoesel, B.; Schoergenhofer, C.; Datler, H.; Hohensinner, P.; Basílio, J.; Petzelbauer, P.; Assinger, A.; et al. Cell Type-Specific Roles of NF-kappaB Linking Inflammation and Thrombosis. Front. Immunol. 2019, 10, 85. [Google Scholar] [CrossRef] [PubMed]
- Crimmins, E.M. Lifespan and Healthspan: Past, Present, and Promise. Gerontologist 2015, 55, 901–911. [Google Scholar] [CrossRef]
- Finch, C.E. Evolution in health and medicine Sackler colloquium: Evolution of the human lifespan and diseases of aging: Roles of infection, inflammation, and nutrition. Proc. Natl. Acad. Sci. USA 2010, 107 (Suppl. S1), 1718–1724. [Google Scholar] [CrossRef]
- Wendelboe, A.M.; Raskob, G.E. Global Burden of Thrombosis: Epidemiologic Aspects. Circ. Res. 2016, 118, 1340–1347. [Google Scholar] [CrossRef]
- Gu, S.X.; Dayal, S. Inflammation mediated platelet hyperactivity in aging. Ann. Blood 2020, 5, 10. [Google Scholar] [CrossRef]
- Price, J.; Lord, J.M.; Harrison, P. Inflammaging and platelet hyperreactivity: A new therapeutic target? J. Thromb. Haemost. 2020, 18, 3–5. [Google Scholar] [CrossRef]
- Klavina, P.A.; Leon, G.; Curtis, A.M.; Preston, R.J. Dysregulated haemostasis in thrombo-inflammatory disease. Clin. Sci. 2022, 136, 1809–1829. [Google Scholar] [CrossRef] [PubMed]
- Byun, J.S.; Gardner, K. Wounds that will not heal: Pervasive cellular reprogramming in cancer. Am. J. Pathol. 2013, 182, 1055–1064. [Google Scholar] [CrossRef]
- Martins Castanheira, N.; Spanhofer, A.K.; Wiener, S.; Bobe, S.; Schillers, H. Uptake of platelets by cancer cells and recycling of the platelet protein CD42a. J. Thromb. Haemost. 2022, 20, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Anaconda Documentation, 2020. Version 2020.x. Available online: https://www.anaconda.com/docs/getting-started/anaconda/release/2020.x (accessed on 29 October 2025).
- Wilke, C. cowplot: Streamlined Plot Theme and Plot Annotations for ‘ggplot2’_. 2024. Cowplot 1.2.0.. Available online: https://wilkelab.org/cowplot/ (accessed on 29 October 2025).
- Wu, L.; Li, M.; Wang, J.; Wu, F.-X. CytoCtrlAnalyser: A Cytoscape app for biomolecular network controllability analysis. Bioinformatics 2018, 34, 1428–1430. [Google Scholar] [CrossRef]
- Shannon, P.; Markiel, A.; Ozier, O.; Baliga, N.S.; Wang, J.T.; Ramage, D.; Amin, N.; Schwikowski, B.; Ideker, T. Cytoscape: A software environment for integrated models of biomolecular interaction networks. Genome Res. 2003, 13, 2498–2504. [Google Scholar] [CrossRef]
- Ceccarelli, F.; Turei, D.; Gabor, A.; Saez-Rodriguez, J. Bringing data from curated pathway resources to Cytoscape with OmniPath. Bioinformatics 2020, 36, 2632–2633. [Google Scholar] [CrossRef] [PubMed]
- Oleś, A. DEFormats: Differential Gene Expression Data Formats Converter. R package version 1.30.0. 2024. Available online: https://rdrr.io/bioc/DEFormats/ (accessed on 29 October 2025).
- Love, M.I.; Huber, W.; Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014, 15, 550. [Google Scholar]
- Chen, Y.; Chen, L.; Lun, A.T.; Baldoni, P.L.; Smyth, G.K. edgeR 4.0: Powerful differential analysis of sequencing data with expanded functionality and improved support for small counts and larger datasets. Nucleic Acids Res. 2025, 53, gkaf018. [Google Scholar] [CrossRef]
- Blighe, K.; Rana, S.; Lewis, M. EnhancedVolcano: Publication-Ready Volcano Plots with Enhanced Colouring and Labeling. 2023. Available online: https://bioconductor.org/packages/release/bioc/html/EnhancedVolcano.html (accessed on 28 October 2025).
- Rainer, J. EnsDb.Hsapiens.v86: Ensembl Based Annotation Package, Version 86. 2017. Available online: https://bioconductor.org/packages/release/data/annotation/html/EnsDb.Hsapiens.v86.html (accessed on 29 October 2025).
- Chen, S.; Zhou, Y.; Chen, Y.; Gu, J. fastp: An ultra-fast all-in-one FASTQ preprocessor. Bioinformatics 2018, 34, i884–i890. [Google Scholar] [CrossRef]
- Andrews, S. FastQC: A Quality Control Tool for High Throughput Sequence Data. 2010. Available online: http://www.bioinformatics.babraham.ac.uk/projects/fastqc (accessed on 29 October 2025).
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016. [Google Scholar]
- Kassambara, A. ggpubr: ‘ggplot2’ Based Publication Ready Plots. 2023. Available online: https://CRAN.R-project.org/package=ggpubr (accessed on 29 October 2025).
- Pedersen, T.L. ggraph: An Implementation of Grammar of Graphics for Graphs and Networks. 2024. Available online: https://CRAN.R-project.org/package=ggraph (accessed on 29 October 2025).
- Ahlmann-Eltze, C.; Huber, W. glmGamPoi: Fitting Gamma-Poisson generalized linear models on single cell count data. Bioinformatics 2021, 36, 5701–5702. [Google Scholar] [CrossRef]
- Kolberg, L.; Raudvere, U.; Kuzmin, I.; Vilo, J.; Peterson, H. gprofiler2—An R package for gene list functional enrichment analysis and namespace conversion toolset g: Profiler. F1000Research 2020, 9, ELIXIR-709. Available online: https://CRAN.R-project.org/package=gprofiler2 (accessed on 29 October 2025). [CrossRef] [PubMed]
- Iannone, R.; Cheng, J.; Schloerke, B.; Hughes, E.; Lauer, A.; Seo, J.; Brevoort, K.; Roy, O. gt: Easily Create Presentation-Ready Display Tables. 2024. Available online: https://CRAN.R-project.org/package=gt (accessed on 29 October 2025).
- Antonov, M.; Csárdi, G.; Horvát, S.; Müller, K.; Nepusz, T.; Noom, D.; Salmon, M.; Traag, V.; Welles, B.F.; Zanini, F. igraph enables fast and robust network analysis across programming languages. arXiv 2023, arXiv:2311.10260. [Google Scholar] [CrossRef]
- Bray, N.L.; Pimentel, H.; Melsted, P.; Pachter, L. Near-optimal probabilistic RNA-seq quantification. Nat. Biotechnol. 2016, 34, 525–527, Erratum in Nat. Biotechnol. 2016, 34, 888. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, M.E.; Phipson, B.; Wu, D.; Hu, Y.; Law, C.W.; Shi, W.; Smyth, G.K. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015, 43, e47. [Google Scholar] [CrossRef]
- Mills, B. MetBrewer: Color Palettes Inspired by Works at the Metropolitan Museum of Art, R package version 0.2.0. 2022. Available online: https://github.com/BlakeRMills/MetBrewer (accessed on 28 October 2025).
- Ewels, P.; Magnusson, M.; Lundin, S.; Käller, M. MultiQC: Summarize analysis results for multiple tools and samples in a single report. Bioinformatics 2016, 32, 3047–3048. [Google Scholar] [CrossRef]
- Valdeolivas, A.; Turei, D.; Gabor, A. OmnipathR: Client for the OmniPath Web Service. R package version 3.10.1. 2019. Available online: https://r.omnipathdb.org (accessed on 28 October 2025).
- Carlson, M. org.Hs.eg.db: Genome Wide Annotation for Human. R package version 3.18.0. 2023. Available online: https://bioconductor.org/packages/release/data/annotation/html/org.Hs.eg.db.html (accessed on 28 October 2025).
- Kolde, R. pheatmap: Pretty Heatmaps. R package version 1.0.12. 2019. Available online: https://cran.r-project.org/web/packages/pheatmap/pheatmap.pdf (accessed on 28 October 2025).
- Sievert, C. Interactive Web-Based Data Visualization with R, Plotly, and Shiny; Chapman and Hall/CRC Florida: Boca Raton, FL, USA, 2020; eBook ISBN 9780429447273. [Google Scholar]
- Fischer, B.S.M.; Pau, G. rhdf5: R Interface to HDF5, R Package Version 2.48.0. 2024. Available online: https://www.bioconductor.org/packages/release/bioc/html/rhdf5.html (accessed on 28 October 2025).
- Posit Team. RStudio: Integrated Development Environment for R; Posit Software; PBC: Boston, MA, USA, 2024; Available online: https://posit.co/products/open-source/rstudio/?sid=1 (accessed on 28 October 2025).
- Risso, D.; Ngai, J.; Speed, T.P.; Dudoit, S. Normalization of RNA-seq data using factor analysis of control genes or samples. Nat. Biotechnol. 2014, 32, 896–902. [Google Scholar] [CrossRef]
- Wickham, H.; Averick, M.; Bryan, J.; Chang, W.; McGowan, L.D.; François, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J.; et al. Welcome to the tidyverse. J. Open Source Softw. 2019, 4, 1686. [Google Scholar] [CrossRef]
- Soneson, C.; Love, M.I.; Robinson, M.D. Differential analyses for RNA-seq: Transcript-level estimates improve gene-level inferences. F1000Research 2015, 4, 1521. [Google Scholar] [CrossRef] [PubMed]
- Lauss, M. swamp: Visualization, Analysis and Adjustment of High-Dimensional Data in Respect to Sample Annotations. R Package Version 1.5.1. 2019. Available online: https://cran.r-project.org/web/packages/swamp/swamp.pdf (accessed on 28 October 2025).
- Vinayagam, A.; Gibson, T.E.; Lee, H.-J.; Yilmazel, B.; Roesel, C.; Hu, Y.; Kwon, Y.; Sharma, A.; Liu, Y.-Y.; Perrimon, N.; et al. Controllability analysis of the directed human protein interaction network identifies disease genes and drug targets. Proc. Natl. Acad. Sci. USA 2016, 113, 4976–4981. [Google Scholar] [CrossRef] [PubMed]
- Jia, T.; Liu, Y.-Y.; Csóka, E.; Pósfai, M.; Slotine, J.-J.; Barabási, A.-L. Emergence of bimodality in controlling complex networks. Nat. Commun. 2013, 4, 2002. [Google Scholar] [CrossRef]
- Garrido-Mesa, N.; Zarzuelo, A.; Galvez, J. Minocycline: Far beyond an antibiotic. Br. J. Pharmacol. 2013, 169, 337–352. [Google Scholar] [CrossRef]
- Sapadin, A.N.; Fleischmajer, R. Tetracyclines: Nonantibiotic properties and their clinical implications. J. Am. Acad. Dermatol. 2006, 54, 258–265. [Google Scholar] [CrossRef]
- Wei, X.; Zhao, L.; Liu, J.; Dodel, R.; Farlow, M.; Du, Y. Minocycline prevents gentamicin-induced ototoxicity by inhibiting p38 MAP kinase phosphorylation and caspase 3 activation. Neuroscience 2005, 131, 513–521. [Google Scholar] [CrossRef]
- Chen, M.; Ona, V.O.; Li, M.; Ferrante, R.J.; Fink, K.B.; Zhu, S.; Bian, J.; Guo, L.; Farrell, L.A.; Hersch, S.M.; et al. Minocycline inhibits caspase-1 and caspase-3 expression and delays mortality in a transgenic mouse model of Huntington disease. Nat. Med. 2000, 6, 797–801. [Google Scholar] [CrossRef]
- Wang, X.; Zhu, S.; Drozda, M.; Zhang, W.; Stavrovskaya, I.G.; Cattaneo, E.; Ferrante, R.J.; Kristal, B.S.; Friedlander, R.M. Minocycline inhibits caspase-independent and -dependent mitochondrial cell death pathways in models of Huntington’s disease. Proc. Natl. Acad. Sci. USA 2003, 100, 10483–10487. [Google Scholar] [CrossRef] [PubMed]
- Festoff, B.W.; Ameenuddin, S.; Arnold, P.M.; Wong, A.; Santacruz, K.S.; Citron, B.A. Minocycline neuroprotects, reduces microgliosis, and inhibits caspase protease expression early after spinal cord injury. J. Neurochem. 2006, 97, 1314–1326. [Google Scholar] [CrossRef] [PubMed]
- Berens, S.C.; Bird, C.M.; Harrison, N.A. Minocycline differentially modulates human spatial memory systems. Neuropsychopharmacology 2020, 45, 2162–2169. [Google Scholar] [CrossRef]


| Target Name 1 | Description | Drugs 2 | Module |
|---|---|---|---|
| CACNA1D | calcium voltage-gated channel subunit alpha1 D | Ergocalciferol, Enflurane, Ranolazine, Phenytoin, Isradipine, Topiramate, Nimodipine, Nisoldipine, Spironolactone, Nicardipine, Magnesium sulfate, Verapamil, Levomenthol, Ethanol, Felodipine, Miconazole, Nifedipine, Amiodarone, Dronedarone, Clevidipine, Levamlodipine, Fish oil | 1 |
| PPARA | peroxisome proliferator-activated receptor alpha | Valproic acid, Indomethacin, Rosiglitazone, Fenoprofen, Fenofibrate, Ibuprofen, Amiodarone, Gemfibrozil, Prasterone, Palmitic Acid, Soybean oil, Fenofibric acid, Fish oil | 1 |
| LPAR4 | lysophosphatidic acid receptor 4 | Promethazine | 1 |
| ME2 | malic enzyme 2 | NADH | 1 |
| MAOB | monoamine oxidase B | Amphetamine, Phentermine, Procaine, Tranylcypromine, Phenelzine, Zonisamide, Selegiline, Pioglitazone, Procarbazine, Isocarboxazid, Rasagiline, Metamfetamine, Flavin adenine dinucleotide, Safinamide, Viloxazine, Flortaucipir F-18 | 3 |
| FCGR2A | Fc gamma receptor IIa | Cetuximab, Etanercept, Human immunoglobulin G, Abciximab, Alemtuzumab, Bevacizumab, Sarilumab | 3 |
| SMPD1 | sphingomyelin phosphodiesterase 1 | Amlodipine, Chlorpromazine, Desipramine | 3 |
| GSTM3 | glutathione S-transferase mu 3 | Glutathione disulfide, Deoxycholic acid | 3 |
| ITGA2B | integrin subunit alpha 2b | Abciximab, Tirofiban | 3 |
| CA1 | carbonic anhydrase 1 | Topiramate, Chlorthalidone, Amlodipine, Methocarbamol, Bendroflumethiazide, Methazolamide, Hydroflumethiazide, Acetazolamide, Dorzolamide, Chlorothiazide, Zonisamide, Diclofenamide, Brinzolamide, Sodium sulfate | 7 |
| HBA1 | hemoglobin subunit alpha 1 | Iron Dextran, Nitrous acid, Copper, Sodium ferric gluconate complex, Ferric pyrophosphate citrate, Zinc acetate, Ferrous fumarate, Zinc chloride, Voxelotor, Ferric derisomaltose | 7 |
| SEC14L2 | SEC14-like lipid binding 2 | Vitamin E | 7 |
| ALAS2 | 5′-aminolevulinate synthase 2 | Glycine | 7 |
| ATOX1 | antioxidant 1 copper chaperone | Cisplatin | 8 |
| MAP1A | Microtubule-associated protein 1A | Estramustine | 8 |
| ID | Description | Drug Targets |
|---|---|---|
| R-HSA-445095 | Interaction between L1 and ankyrins | SCN1A (sodium channel protein type 1 subunit alpha), SCN2A (sodium channel protein type 2 subunit alpha), SCN9A (sodium channel protein type 9 subunit alpha), SCN3A (sodium channel protein type 3 subunit alpha), SCN11A (sodium channel protein type 11 subunit alpha), SCN8A (sodium channel protein type 8 subunit alpha), SCN1B (sodium channel regulatory subunit beta-1), SCN3B (sodium channel regulatory subunit beta-3) |
| R-HSA-3000178 | ECM proteoglycans | APP (amyloid-beta precursor protein), FN1 (fibronectin), HAPLN1 (hyaluronan and proteoglycan link protein 1), HSPG2 (basement membrane-specific heparan sulfate proteoglycan core protein), ITGA2B (integrin alpha-IIb) |
| R-HAS-1474228 | Degradation of the extracellular matrix | ELN (elastin), FBN2 (fibrillin-2), FN1 (fibronectin), HSPG2 (basement membrane-specific heparan sulfate proteoglycan core protein), NID1 (nidogen-1), PLG (plasminogen) |
| R-HSA-446728 | Cell junction organization | CDH11 (cadherin-11), FLNA (filamin-A), TESK1 (dual specificity testis-specific protein kinase 1) |
| R-HSA-381426 | Regulation of fIGF transport and uptake by IGFBPs | APP (amyloid-beta precursor protein), CP (ceruloplasmin), F5 (coagulation factor V), FN1 (fibronectin), ITIH2 (inter-alpha-trypsin inhibitor heavy chain H2), PLG (plasminogen), SERPIND1 (heparin cofactor 2) |
| R-HSA-5173105 | O-linked glycosylation | MUC16 (mucin-16) |
| R-HSA-1474290 | Collagen formation | P3H2 (prolyl 3-hydroxylase 2), P4HB (protein disulfide-isomerase), PLOD1 (procollagen-lysine,2-oxoglutarate 5-dioxygenase 1), PLOD2 (procollagen-lysine,2-oxoglutarate 5-dioxygenase 2) |
| R-HSA-1592389 | Activation of matrix metalloproteinases | no FDA-approved drugs found. |
| Drug Name 1 | Number of Targets | Targets 2 |
|---|---|---|
| Fostamatinib | 5 | CAMK1, JAK2, MAPK14, PRKCD, PTK2 |
| Minocycline | 4 | CASP3, MAPK1, MAPK14, MAPK3 |
| Acetylsalicylic acid | 3 | CASP3, MAPK1, MAPK3 |
| Arsenic trioxide | 3 | MAPK3, MAPK1, AKT1 |
| Copper | 3 | APP, GAPDH, HSP90AA1 |
| Benzoyl peroxide | 2 | PRKCA, PRKCD |
| Dequalinium * | 2 | PRKCA, PRKCD |
| Ingenol mebutate | 2 | PRKCD, PRKCA |
| Tamoxifen | 2 | PRKCA, PRKCD |
| Abrocitinib | 1 | JAK2 |
| Drug Name 1 | Degree | Log2FC | Weight | Gene Score | Drugs 2 |
|---|---|---|---|---|---|
| LYN | 48 | −0.24 | 11.34 | 0.48 | Dasatinib, Bosutinib, Ponatinib, Nintedanib, Fostamatinib |
| JAK1 | 21 | -- | 0 | 0.47 | Ruxolitinib, Tofacitinib, Momelotinib, Baricitinib, Fostamatinib, Fedratinib, Filgotinib, Abrocitinib, Upadacitinib, Pralsetinib |
| FCGR2A | 4 | 0.68 | 2.71 | 0.46 | Cetuximab, Etanercept, Human immunoglobulin G, Abciximab, Alemtuzumab, Bevacizumab, Catumaxomab, Sarilumab |
| TEC | 10 | 0.25 | 2.47 | 0.46 | Bosutinib, Fostamatinib, Ritlecitinib, Zanubrutinib |
| TUBA4A | 1 | −0.13 | 0.13 | 0.45 | Vincristine, Podofilox |
| PTPN6 | 29 | −0.09 | 2.73 | 0.45 | Tiludronic acid |
| SYK | 37 | −0.1 | 3.84 | 0.45 | Fostamatinib |
| ITGA5 | 5 | -- | 0 | 0.45 | Tauroursodeoxycholic acid |
| GRB2 | 37 | -- | 0 | 0.45 | Pegademase |
| JAK3 | 16 | 0.45 | 7.3 | 0.44 | Ruxolitinib, Tofacitinib, Momelotinib, Baricitinib, Fostamatinib, Ritlecitinib, Abrocitinib, Zanubrutinib |
| P2RY12 | 1 | −0.49 | 0.49 | 0.44 | Ticlopidine, Treprostinil, Clopidogrel, Promethazine, Epoprostenol, Prasugrel, Cangrelor, Ticagrelor |
| BTK | 19 | −0.271 | 5.08 | 0.44 | Dasatinib, Ibrutinib, Acalabrutinib, Fostamatinib, Ritlecitinib, Zanubrutinib, Pirtobrutinib |
| PPIA | 1 | -- | 0 | 0.44 | Cyclosporine, Copper, Artenimol |
| PIK3CB | 1 | 0.13 | 0.13 | 0.44 | Caffeine, Copanlisib |
| CSK | 18 | 0.11 | 1.95 | 0.44 | Dasatinib, Fostamatinib |
| PTK2B | 37 | 0.18 | 6.76 | 0.44 | Leflunomide, Fostamatinib |
| Gene | GSE89843 (NSCLC) | GSE183635 (NSCLC) | GSE68086 (Pancreatic Cancer) | GSE183635 (Breast Cancer) | Values |
|---|---|---|---|---|---|
| ITGA2B | 0.728134021 | 0.4243767 | 2.073708 | 0.6252545 | LogFC 1 |
| 1.40 × 10−29 | 2.20 × 10−4 | 1.25 × 10−13 | 1.72 × 10−3 | adj.p-value 2 | |
| 142/14545 | 3458/14608 | 2598/14784 | 407/17851 | DEG ranking 3 | |
| FLNA | 0.808899158 | 0.354511 | 3.144132 | 0.7036141 | LogFC |
| 1.22 × 10−31 | 7.92 × 10−4 | 1.43 × 10−21 | 1.48 × 10−4 | adj.p-value | |
| 102/14545 | 5047/14608 | 409/14784 | 247/17851 | DEG ranking | |
| GRB2 | 0.030350283 | −0.1527763 | 1.188885 | 0.229971 | LogFC |
| Not significant | 3.79 × 10−2 | 7.34 × 10−11 | 1.15 × 10−1 | adj.p-value | |
| Not among top | 10092/14608 | 5890/14784 | 5659/17851 | DEG ranking | |
| FCGR2A | 0.786305852 | 0.8687625 | 1.745807 | 0.633244 | LogFC |
| 4.03 × 10−19 | 1.21 × 10−24 | 1.62 × 10−12 | 1.95 × 10−6 | adj.p-value | |
| 118/14545 | 159/14608 | 3523/14784 | 387/17851 | DEG ranking | |
| APP | 0.336303527 | 0.2051573 | 1.344015 | 0.4870745 | LogFC |
| 5.93 × 10−8 | 2.23 × 10−2 | 3.48 × 10−13 | 4.25 × 10−3 | adj.p-value | |
| 2257/14545 | 8645/14608 | 5126/14784 | 992/17851 | DEG ranking |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osmanoglu, Ö.; Özer, E.; Gupta, S.K.; Heinze, K.G.; Schulze, H.; Dandekar, T. Network Controllability Reveals Key Mitigation Points for Tumor-Promoting Signaling in Tumor-Educated Platelets. Int. J. Mol. Sci. 2025, 26, 10780. https://doi.org/10.3390/ijms262110780
Osmanoglu Ö, Özer E, Gupta SK, Heinze KG, Schulze H, Dandekar T. Network Controllability Reveals Key Mitigation Points for Tumor-Promoting Signaling in Tumor-Educated Platelets. International Journal of Molecular Sciences. 2025; 26(21):10780. https://doi.org/10.3390/ijms262110780
Chicago/Turabian StyleOsmanoglu, Özge, Elif Özer, Shishir K. Gupta, Katrin G. Heinze, Harald Schulze, and Thomas Dandekar. 2025. "Network Controllability Reveals Key Mitigation Points for Tumor-Promoting Signaling in Tumor-Educated Platelets" International Journal of Molecular Sciences 26, no. 21: 10780. https://doi.org/10.3390/ijms262110780
APA StyleOsmanoglu, Ö., Özer, E., Gupta, S. K., Heinze, K. G., Schulze, H., & Dandekar, T. (2025). Network Controllability Reveals Key Mitigation Points for Tumor-Promoting Signaling in Tumor-Educated Platelets. International Journal of Molecular Sciences, 26(21), 10780. https://doi.org/10.3390/ijms262110780






