Astatine-211-Labeled Therapy Targeting Amino Acid Transporters: Overcoming Drug Resistance in Non-Small Cell Lung Cancer
Abstract
1. Introduction
2. Therapeutic Approaches and Mechanisms of Drug Resistance in NSCLC
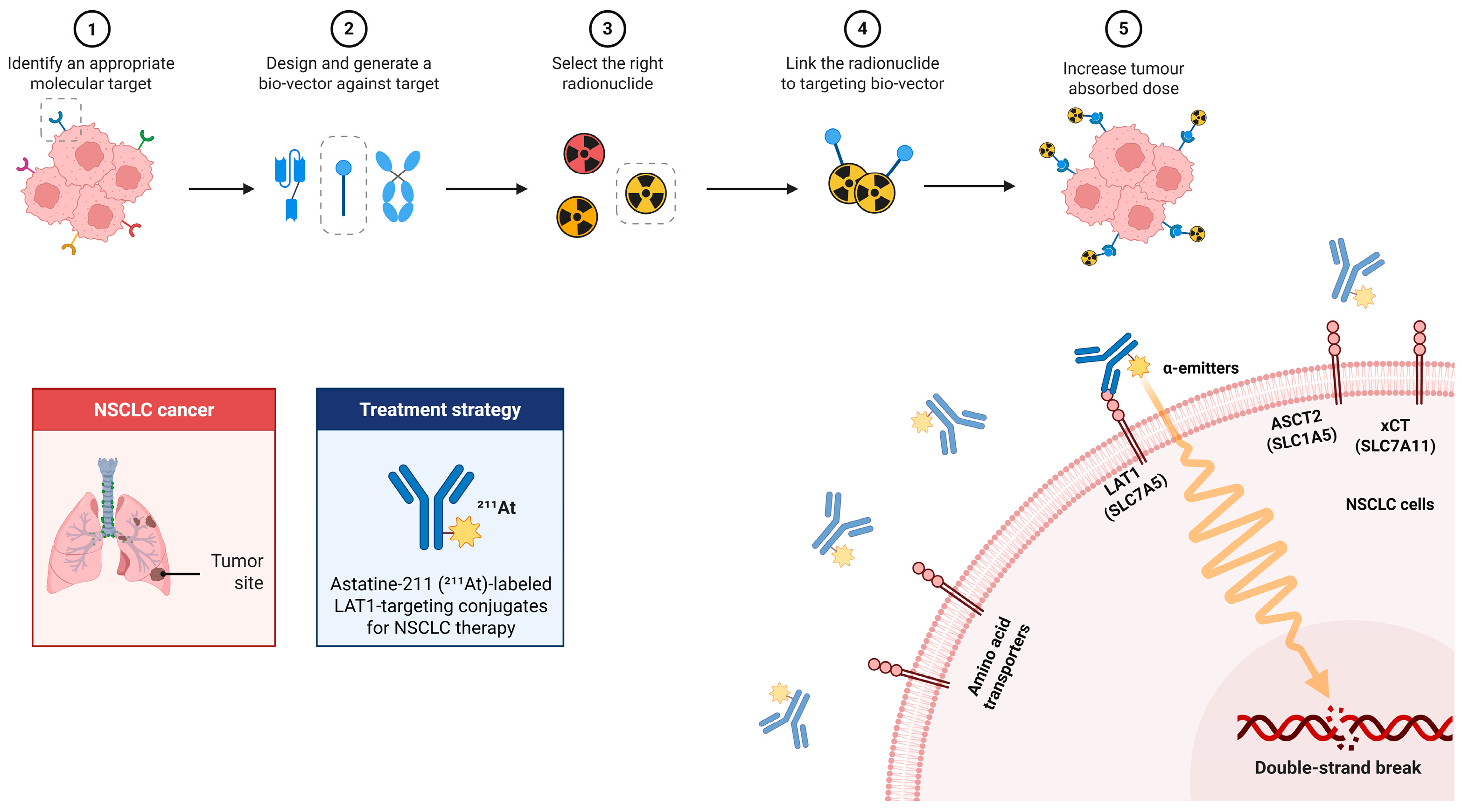
2.1. Therapeutic Approaches
2.2. Resistance Mechanisms
2.3. Modality-Specific Resistance Examples
2.4. Shared Adaptive Programs Across Modalities
3. Amino Acid Transporters in NSCLC: Structure, Function, and Therapeutic Targeting
3.1. Overview and Structural Features
3.2. Roles in Tumor Metabolism and the Microenvironment
3.3. Immune and Expression Profiles in NSCLC
4. Physical and Radiobiological Basis of 211At Therapy
4.1. Physical & Radiobiological Properties
4.2. Comparison with Other Therapeutic Radionuclides
4.3. Radiolabeling Strategies of 211At
4.4. Targeting Amino Acid Transporters with 211At
4.5. Applications in Other Malignancies
4.6. Delivery Platforms for Enhanced Retention
4.6.1. Antibodies and ADCs
4.6.2. Peptides
4.6.3. Nanocarriers
4.7. Toward Clinical Translation
4.7.1. Dosimetry and Pharmacokinetics
4.7.2. Safety and Toxicity Mitigation
4.7.3. Patient Selection and Trial Design
5. Integration with Existing NSCLC Therapies
5.1. Integration with Targeted Agents
5.2. Therapeutic Synergy with Radiotherapy and Chemotherapy
5.3. Synergy with Immunotherapy
5.4. Synergies with Ferroptosis and DNA Damage
5.5. Theranostic Framework
6. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 131I | Iodine-131 |
| 177Lu | Lutetium-177 |
| 18F | Fluorine-18 |
| 18F-FAMT | 18F-L-3-fluoro-α-methyl-tyrosine |
| 18F-FBPA | 18F-fluoro-boronophenylalanine |
| [18F]FSPG | (4S)-4-(3-fluoropropyl)-L-glutamate |
| 211At | Astatine-211 |
| 213Bi | Bismuth-213 |
| 223Ra | Radium-223 |
| 225Ac | Actinium-225 |
| AA | Amino acid |
| AAMP | 2-[211At]AAMP (LAT1-targeted analogue) |
| AAMT | 211At-labeled α-methyl-L-tyrosine |
| ABCB1 | ATP-binding cassette subfamily B member 1 (P-glycoprotein) |
| ABCG2 | ATP-binding cassette subfamily G member 2 (BCRP) |
| ADC | Antibody–drug conjugate |
| ADCC | Antibody-dependent cellular cytotoxicity |
| AHR | Aryl hydrocarbon receptor |
| AKT | Protein kinase B |
| ALK | Anaplastic lymphoma kinase |
| ASCT2 | Alanine-serine-cysteine transporter 2 (SLC1A5) |
| ATF4 | Activating transcription factor 4 |
| ATR | Ataxia telangiectasia and Rad3-related protein |
| B2M | Beta-2-microglobulin |
| BCH | 2-Aminobicyclo[2.2.1]heptane-2-carboxylic acid |
| BenSer | Benzylserine |
| CD98hc/4F2hc | Heavy chain of CD98 (SLC3A2) |
| CDC | Complement-dependent cytotoxicity |
| CHK1 | Checkpoint kinase 1 |
| CSC | Cancer stem cell |
| CYP | Cytochrome P450 |
| DDR | DNA damage response |
| DM1 | Maytansinoid DM1 |
| DNA | Deoxyribonucleic acid |
| DSB(s) | Double-strand break(s) |
| DTP | Drug-tolerant persister(s) |
| EBRT | External-beam radiotherapy |
| EGFR | Epidermal growth factor receptor |
| EMT | Epithelial–mesenchymal transition |
| ERBB3 | Erb-B2 receptor tyrosine kinase 3 (HER3) |
| ERK | Extracellular signal-regulated kinase |
| EZH2 | Enhancer of zeste homolog 2 |
| F(ab′)2 | Antibody fragment F(ab′)2 |
| FIN(s) | Ferroptosis inducer(s) |
| GPX4 | Glutathione peroxidase 4 |
| GMP | Good Manufacturing Practice |
| GSH | Glutathione |
| GATOR2 | GAP activity toward Rags complex 2 |
| HIF-1 | Hypoxia-inducible factor 1 |
| HIF-2α | Hypoxia-inducible factor 2 alpha |
| HLA-I | Human leukocyte antigen class I |
| HMGB1 | High mobility group box 1 |
| HR | Homologous recombination |
| ICI(s) | Immune checkpoint inhibitor(s) |
| ICD | Immunogenic cell death |
| IDO1 | Indoleamine 2,3-dioxygenase 1 |
| IEDDA | Inverse electron-demand Diels–Alder reaction |
| iRGD | Internalizing the RGD peptide |
| JPH203 | Nanvuranlat (LAT1 inhibitor) |
| KEAP1 | Kelch-like ECH-associated protein 1 |
| KRASG12C | KRAS p.G12C mutation |
| LAG-3 | Lymphocyte-activation gene 3 |
| LAT1 | L-type amino acid transporter 1 (SLC7A5) |
| LET | Linear energy transfer |
| MABG | meta-Astatobenzylguanidine |
| MAPK | Mitogen-activated protein kinase |
| mAb | Monoclonal antibody |
| mCRPC | Metastatic castration-resistant prostate cancer |
| MeV | Mega-electron volt |
| MDSC(s) | Myeloid-derived suppressor cell(s) |
| MMAE | Monomethyl auristatin E |
| mTOR | Mechanistic target of rapamycin |
| mTORC1 | mTOR complex 1 |
| NaAt | Sodium astatide ([211At]NaAt) |
| NAD(P)H | Nicotinamide adenine dinucleotide (phosphate), reduced form |
| NFE2L2 | Nuclear factor erythroid-derived 2-like 2 |
| NHEJ | Non-homologous end-joining |
| NRF2 | Nuclear factor erythroid 2-related factor 2 |
| NSCLC | Non-small cell lung cancer |
| OER | Oxygen-enhancement ratio |
| OS | Overall survival |
| PD-L1 | Programmed death-ligand 1 |
| PEG | Polyethylene glycol |
| PET | Positron emission tomography |
| PI3K | Phosphoinositide 3-kinase |
| PK | Pharmacokinetics |
| PLGA | Poly(lactic-co-glycolic acid) |
| PBD | Pyrrolobenzodiazepine |
| PRIT | Pretargeted radioimmunotherapy |
| PSMA | Prostate-specific membrane antigen |
| Rag GTPases | Ras-related GTP-binding proteins A–D |
| RGD | Arg-Gly-Asp peptide |
| ROS | Reactive oxygen species |
| ROS1 | c-ros oncogene 1 (receptor tyrosine kinase) |
| RT | Radiotherapy |
| SAB | N-succinimidyl astatobenzoate |
| SAGMB | Guanidinomethyl-substituted succinimidyl astatobenzoate |
| SBRT | Stereotactic body radiotherapy |
| SLC1A5 | Solute carrier family one member 5 (ASCT2) |
| SLC3A2 | Solute carrier family three member 2 (CD98hc/4F2hc) |
| SLC7A5 | Solute carrier family seven member 5 (LAT1) |
| SLC7A11 | Solute carrier family seven member 11 (xCT) |
| SLC38A2 (SNAT2) | Sodium-coupled neutral amino acid transporter 2 |
| SLC43A2 | Solute carrier family 43 member 2 |
| SNAT2 | See SLC38A2 |
| TAZ | WW domain-containing transcription regulator 1 |
| TIGIT | T cell immunoreceptor with Ig and ITIM domains |
| TIM-3 | T cell immunoglobulin and mucin domain 3 |
| TKI(s) | Tyrosine kinase inhibitor(s) |
| TME | Tumor microenvironment |
| Treg(s) | Regulatory T cell(s) |
| TRT | Targeted radionuclide therapy |
| V-9302 | Small-molecule glutamine transport inhibitor |
| VISTA | V-domain Ig suppressor of T-cell activation |
| WEE1 | WEE1 G2 checkpoint kinase |
| xCT | Cystine/glutamate antiporter (SLC7A11) |
| YAP | Yes-associated protein |
References
- Zhou, J.; Xu, Y.; Liu, J.; Feng, L.; Yu, J.; Chen, D. Global burden of lung cancer in 2022 and projections to 2050: Incidence and mortality estimates from GLOBOCAN. Cancer Epidemiol. 2024, 93, 102693. [Google Scholar] [CrossRef]
- Tang, F.H.; Wong, H.Y.T.; Tsang, P.S.W.; Yau, M.; Tam, S.Y.; Law, L.; Yau, K.; Wong, J.; Farah, F.H.M.; Wong, J. Recent advancements in lung cancer research: A narrative review. Transl. Lung Cancer Res. 2025, 14, 975–990. [Google Scholar] [CrossRef]
- Ganti, A.K.; Klein, A.B.; Cotarla, I.; Seal, B.; Chou, E. Update of incidence, prevalence, survival, and initial treatment in patients with non-small cell lung cancer in the US. JAMA Oncol. 2021, 7, 1824–1832. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Y.; Liu, X.; Wang, Y.; Zheng, D.; Meng, Q.; Jiang, L.; Yang, S.; Zhang, S.; Zhang, X.; Liu, Y.; et al. Mechanisms of resistance to targeted therapy and immunotherapy in non-small cell lung cancer: Promising strategies to overcome challenges. Front. Immunol. 2024, 15, 1366260. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Li, Y.; Huang, Y.; Wu, J.; Bao, W.; Xue, C.; Li, X.; Dong, S.; Dong, Z.; Hu, S. Advances in molecular pathology and therapy of non-small cell lung cancer. Signal Transduct. Target. Ther. 2025, 10, 186. [Google Scholar] [CrossRef]
- Liu, S.; Zhang, X.; Wang, W.; Li, X.; Sun, X.; Zhao, Y.; Wang, Q.; Li, Y.; Hu, F.; Ren, H. Metabolic reprogramming and therapeutic resistance in primary and metastatic breast cancer. Mol. Cancer 2024, 23, 261. [Google Scholar] [CrossRef]
- Chen, J.; Cui, L.; Lu, S.; Xu, S. Amino acid metabolism in tumor biology and therapy. Cell Death Dis. 2024, 15, 42. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Zhang, F.; Xu, F.; Yang, C. Metabolic reprogramming and therapeutic targeting in non-small cell lung cancer: Emerging insights beyond the Warburg effect. Front. Oncol. 2025, 15, 1564226. [Google Scholar] [CrossRef]
- Furuse, J.; Ikeda, M.; Ueno, M.; Furukawa, M.; Morizane, C.; Takehara, T.; Nishina, T.; Todaka, A.; Okano, N.; Hara, K.; et al. A phase II placebo-controlled study of the effect and safety of nanvuranlat in patients with advanced biliary tract cancers previously treated by systemic chemotherapy. Clin. Cancer Res. 2024, 30, 3990–3995. [Google Scholar] [CrossRef]
- Morozova, V.; Pellegata, D.; Singer, S.; Charles, R.-P.; Müller, J.; Altmann, K.-H.; Gertsch, J. Pharmacodynamic analyses of LAT1 inhibitors in vitro and in vivo by targeted metabolomics reveal target-independent effects. Biomed. Pharmacother. 2025, 190, 118402. [Google Scholar] [CrossRef]
- Maris, M.; Salles, G.; Kim, W.S.; Kim, T.M.; Lyons, R.M.; Arellano, M.; Karmali, R.; Schiller, G.; Cull, E.; Abboud, C.N.; et al. ASCT2-targeting antibody-drug conjugate MEDI7247 in adult patients with relapsed/refractory hematological malignancies: A first-in-human, phase 1 study. Target. Oncol. 2024, 19, 321–332. [Google Scholar] [CrossRef]
- Song, Z.; Zhang, J.; Qin, S.; Luan, X.; Zhang, H.; Yang, M.; Jin, Y.; Yang, G.; Yu, F. Targeted alpha therapy: A comprehensive analysis of the biological effects from “local-regional-systemic” dimensions. Eur. J. Nucl. Med. Mol. Imaging 2025, 52, 2031–2048. [Google Scholar] [CrossRef]
- Vanermen, M.; Ligeour, M.; Oliveira, M.-C.; Gestin, J.-F.; Elvas, F.; Navarro, L.; Guérard, F. Astatine-211 radiolabelling chemistry: From basics to advanced biological applications. EJNMMI Radiopharm. Chem. 2024, 9, 69. [Google Scholar] [CrossRef]
- Jang, A.; Kendi, A.T.; Johnson, G.B.; Halfdanarson, T.R.; Sartor, O. Targeted alpha-particle therapy: A review of current trials. Int. J. Mol. Sci. 2023, 24, 11626. [Google Scholar] [CrossRef] [PubMed]
- Albertsson, P.; Bäck, T.; Bergmark, K.; Hallqvist, A.; Johansson, M.; Aneheim, E.; Lindegren, S.; Timperanza, C.; Smerud, K.; Palm, S. Astatine-211-based radionuclide therapy: Current clinical trial landscape. Front. Med. 2023, 9, 1076210. [Google Scholar] [CrossRef] [PubMed]
- Pu, X.; Zhou, Y.; Wang, J.; Wu, L. Immune checkpoint inhibitor-based therapy as the first-line treatment for advanced non-small cell lung cancer: Efficacy, challenges, and future perspectives. Thorac. Cancer 2025, 16, e70113. [Google Scholar] [CrossRef]
- Su, P.-L.; Furuya, N.; Asrar, A.; Rolfo, C.; Li, Z.; Carbone, D.P.; He, K. Recent advances in therapeutic strategies for non-small cell lung cancer. J. Hematol. Oncol. 2025, 18, 35. [Google Scholar] [CrossRef]
- Mirsky, M.M.; Myers, K.E.; Abul-Khoudoud, S.O.; Lee, J.Y.; Bruno, D.S. Systemic therapy for operable NSCLC: A review of the literature and discussion of future directions. J. Clin. Med. 2025, 14, 4127. [Google Scholar] [CrossRef] [PubMed]
- Abel, S.; Hasan, S.; Horne, Z.D.; Colonias, A.; Wegner, R.E. Stereotactic body radiation therapy in early-stage NSCLC: Historical review, contemporary evidence, and future implications. Lung Cancer Manag. 2019, 8, LMT09. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.N.; Owen, D. Advances in stereotactic body radiation therapy for lung cancer. Cancer J. 2024, 30, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Burcher, K.; Karukonda, P.; Kelsey, C.; Mullikin, T.; Antonia, S.J.; Oduah, E.I. A critical review of immunomodulation in the management of inoperable stage III NSCLC. Cancers 2025, 17, 1829. [Google Scholar] [CrossRef]
- Gálffy, G.; Morócz, É.; Korompay, R.; Hécz, R.; Bujdosó, R.; Puskás, R.; Lovas, T.; Gáspár, E.; Yahya, K.; Király, P.; et al. Targeted therapeutic options in early and metastatic NSCLC: Overview. Pathol. Oncol. Res. 2024, 30, 1611715. [Google Scholar] [CrossRef]
- Ahluwalia, V.S.; Parikh, R.B. Chemoimmunotherapy vs immunotherapy monotherapy receipt in advanced non-small cell lung cancer. JAMA Netw. Open 2025, 8, e2459380. [Google Scholar] [CrossRef]
- Tian, T.; Li, Y.; Li, J.; Xu, H.; Fan, H.; Zhu, J.; Wang, Y.; Peng, F.; Gong, Y.; Du, Y.; et al. Immunotherapy for patients with advanced non-small cell lung cancer harboring oncogenic driver alterations other than EGFR: A multicenter real-world analysis. Transl. Lung Cancer Res. 2024, 13, 861–874. [Google Scholar] [CrossRef] [PubMed]
- Attili, I.; Passaro, A.; Corvaja, C.; Aliaga, P.T.; Signore, E.D.; Spitaleri, G.; de Marinis, F. Immune checkpoint inhibitors in EGFR-mutant non-small cell lung cancer: A systematic review. Cancer Treat. Rev. 2023, 119, 102602. [Google Scholar] [CrossRef] [PubMed]
- Lisberg, A.; Cummings, A.; Goldman, J.W.; Bornazyan, K.; Reese, N.; Wang, T.; Coluzzi, P.; Ledezma, B.; Mendenhall, M.; Hunt, J.; et al. A phase II study of pembrolizumab in EGFR-mutant, PD-L1-positive, tyrosine kinase inhibitor-naïve patients with advanced NSCLC. J. Thorac. Oncol. 2018, 13, 1138–1145. [Google Scholar] [CrossRef]
- Addeo, A.; Passaro, A.; Malapelle, U.; Banna, G.L.; Subbiah, V.; Friedlaender, A. Immunotherapy in non-small cell lung cancer harbouring driver mutations. Cancer Treat. Rev. 2021, 96, 102179. [Google Scholar] [CrossRef]
- Liu, L.; Soler, J.; Reckamp, K.L.; Sankar, K. Emerging targets in non-small cell lung cancer. Int. J. Mol. Sci. 2024, 25, 10046. [Google Scholar] [CrossRef] [PubMed]
- Vander Velde, R.; Yoon, N.; Marusyk, V.; Durmaz, A.; Dhawan, A.; Miroshnychenko, D.; Lozano-Peral, D.; Desai, B.; Balynska, O.; Poleszhuk, J.; et al. Resistance to targeted therapies as a multifactorial, gradual adaptation to inhibitor-specific selective pressures. Nat. Commun. 2020, 11, 2393. [Google Scholar] [CrossRef]
- Lim, Z.-F.; Ma, P.C. Emerging insights of tumor heterogeneity and drug resistance mechanisms in lung cancer targeted therapy. J. Hematol. Oncol. 2019, 12, 134. [Google Scholar] [CrossRef]
- Liu, J.; Cai, Y.; Liu, J.; Chen, D.; Wu, X. Immunotherapy resistance and therapeutic strategies in PD-L1 high-expression non-small cell lung cancer. Onco Targets Ther. 2025, 18, 953–966. [Google Scholar] [CrossRef]
- Xie, J.; Gao, Y.; Xu, W.; Zhu, J. Mechanisms of resistance to ALK inhibitors and corresponding treatment strategies in lung cancer. Int. J. Gen. Med. 2025, 18, 2151–2171. [Google Scholar] [CrossRef]
- Yu, J.; Kong, X.; Feng, Y. Tumor microenvironment-driven resistance to immunotherapy in non-small cell lung cancer: Strategies for cold-to-hot tumor transformation. Cancer Drug Resist. 2025, 8, 14. [Google Scholar] [CrossRef]
- Morgillo, F.; Della Corte, C.M.; Fasano, M.; Ciardiello, F. Mechanisms of resistance to EGFR-targeted drugs: Lung cancer. ESMO Open 2016, 1, e000060. [Google Scholar] [CrossRef]
- Hatcher, J.M.; Bahcall, M.; Choi, H.G.; Gao, Y.; Sim, T.; George, R.; Jänne, P.A.; Gray, N.S. Discovery of inhibitors that overcome the G1202R anaplastic lymphoma kinase resistance mutation. J. Med. Chem. 2015, 58, 9296–9308. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, S.; Wang, K.; Sun, S.-Y. MET inhibitors for targeted therapy of EGFR TKI-resistant lung cancer. J. Hematol. Oncol. 2019, 12, 63. [Google Scholar] [CrossRef] [PubMed]
- Oxnard, G.R.; Yang, J.C.-H.; Yu, H.; Kim, S.-W.; Saka, H.; Horn, L.; Goto, K.; Ohe, Y.; Mann, H.; Thress, K.S.; et al. TATTON: A multi-arm, phase Ib trial of osimertinib combined with selumetinib, savolitinib, or durvalumab in EGFR-mutant lung cancer. Ann. Oncol. 2020, 31, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Huang, Y.; Zhao, Q. Epigenetic alterations and inflammation as emerging use for the advancement of treatment in non-small cell lung cancer. Front. Immunol. 2022, 13, 878740. [Google Scholar] [CrossRef]
- Lin, S.; Ruan, H.; Qin, L.; Zhao, C.; Gu, M.; Wang, Z.; Liu, B.; Wang, H.; Wang, J. Acquired resistance to EGFR-TKIs in NSCLC mediates epigenetic downregulation of MUC17 by facilitating NF-κB activity via UHRF1/DNMT1 complex. Int. J. Biol. Sci. 2023, 19, 832–851. [Google Scholar] [CrossRef]
- Zhang, Q.; Shi, Y.; Liu, S.; Yang, W.; Chen, H.; Guo, N.; Sun, W.; Zhao, Y.; Ren, Y.; Jia, L.; et al. EZH2/G9a interact to mediate drug resistance in non-small-cell lung cancer by regulating the SMAD4/ERK/c-Myc signaling axis. Cell Rep. 2024, 43, 113714. [Google Scholar] [CrossRef] [PubMed]
- Zang, H.; Qian, G.; Zong, D.; Fan, S.; Owonikoko, T.K.; Ramalingam, S.S.; Sun, S.-Y. Overcoming acquired resistance of epidermal growth factor receptor-mutant non-small cell lung cancer cells to osimertinib by combining osimertinib with the histone deacetylase inhibitor panobinostat (LBH589). Cancer 2020, 126, 2024–2033. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Ren, S.; Li, X.; Wang, Y.; Garfield, D.; Zhou, S.; Chen, X.; Su, C.; Chen, M.; Kuang, P.; et al. MiR-21 overexpression is associated with acquired resistance of EGFR-TKI in non-small cell lung cancer. Lung Cancer 2014, 83, 146–153. [Google Scholar] [CrossRef]
- Ji, Y.; Xiao, C.; Fan, T.; Deng, Z.; Wang, D.; Cai, W.; Li, J.; Liao, T.; Li, C.; He, J. The epigenetic hallmarks of immune cells in cancer. Mol. Cancer 2025, 24, 66. [Google Scholar] [CrossRef]
- Mahfoudhi, E.; Ricordel, C.; Lecuyer, G.; Mouric, C.; Lena, H.; Pedeux, R. Preclinical models for acquired resistance to third-generation EGFR inhibitors in NSCLC: Functional studies and drug combinations used to overcome resistance. Front. Oncol. 2022, 12, 853501. [Google Scholar] [CrossRef]
- Liang, H.; Xu, Y.; Zhao, J.; Chen, M.; Wang, M. Hippo pathway in non-small cell lung cancer: Mechanisms, potential targets, and biomarkers. Cancer Gene Ther. 2024, 31, 652–666. [Google Scholar] [CrossRef]
- Liaghat, M.; Ferdousmakan, S.; Mortazavi, S.H.; Yahyazadeh, S.; Irani, A.; Banihashemi, S.; Seyedi Asl, F.S.; Akbari, A.; Farzam, F.; Aziziyan, F.; et al. The impact of epithelial–mesenchymal transition induced by metabolic processes and intracellular signaling pathways on chemoresistance, metastasis, and recurrence in solid tumors. Cell Commun. Signal. 2024, 22, 575. [Google Scholar] [CrossRef]
- Yan, T.; Shi, J. Angiogenesis and EMT regulators in the tumor microenvironment in lung cancer and immunotherapy. Front. Immunol. 2024, 15, 1509195. [Google Scholar] [CrossRef]
- Zheng, Y.; Ma, L.; Sun, Q. Clinically relevant ABC transporter for anti-cancer drug resistance. Front. Pharmacol. 2021, 12, 648407. [Google Scholar] [CrossRef]
- Nelson, R.S.; Seligson, N.D.; Bottiglieri, S.; Carballido, E.; Del Cueto, A.; Imanirad, I.; Levine, R.; Parker, A.S.; Swain, S.M.; Tillman, E.M.; et al. UGT1A1-guided cancer therapy: Review of the evidence and considerations for clinical implementation. Cancers 2021, 13, 1566. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, Z.; Wang, Y.; Jin, W.; Zhang, Z.; Jin, L.; Qian, J.; Zheng, L. CYP3A4 and CYP3A5: The crucial roles in clinical drug metabolism and the significant implications of genetic polymorphisms. PeerJ 2024, 12, e18636. [Google Scholar] [CrossRef] [PubMed]
- Conrad, J.; Vaz, R.J. Validating the use of rational modification of compounds to reduce P-gp efflux. Arch. Pharmacol. Ther. 2024, 6, 34–39. [Google Scholar] [CrossRef]
- Yoo, H.; Kim, Y.; Kim, J.; Cho, H.; Kim, K. Overcoming cancer drug resistance with nanoparticle strategies for key protein inhibition. Molecules 2024, 29, 3994. [Google Scholar] [CrossRef]
- van der Kleij, M.B.A.; Guchelaar, N.A.D.; Meertens, M.; Westerdijk, K.; Giraud, E.L.; Bleckman, R.F.; Groenland, S.L.; van Eerden, R.A.G.; Imholz, A.L.T.; Vulink, A.J.E.; et al. Reasons for non-feasibility of therapeutic drug monitoring of oral targeted therapies in oncology: An analysis of the closed cohorts of a multicentre prospective study. Br. J. Cancer 2024, 131, 843–851. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Li, W.; Zhang, P.; Guo, F.; Liu, M. Current trends in sensitizing immune checkpoint inhibitors for cancer treatment. Mol. Cancer 2024, 23, 279. [Google Scholar] [CrossRef]
- Zhang, A.; Fan, T.; Liu, Y.; Yu, G.; Li, C.; Jiang, Z. Regulatory T cells in immune checkpoint blockade antitumor therapy. Mol. Cancer 2024, 23, 251. [Google Scholar] [CrossRef]
- Kurt, F.G.O.; Lasser, S.; Arkhypov, I.; Utikal, J.; Umansky, V. Enhancing immunotherapy response in melanoma: Myeloid-derived suppressor cells as a therapeutic target. J. Clin. Investig. 2023, 133, e170762. [Google Scholar] [CrossRef]
- Liu, Y.-T.; Sun, Z.-J. Turning cold tumors into hot tumors by improving T-cell infiltration. Theranostics 2021, 11, 5365–5386. [Google Scholar] [CrossRef] [PubMed]
- Achmad, A.; Hanaoka, H.; Holik, H.A.; Endo, K.; Tsushima, Y.; Kartamihardja, A.H.S. LAT1-specific PET radiotracers: Development and clinical experiences of a new class of cancer-specific radiopharmaceuticals. Theranostics 2025, 15, 1864–1878. [Google Scholar] [CrossRef]
- Cormerais, Y.; Massard, P.A.; Vucetic, M.; Giuliano, S.; Tambutté, E.; Durivault, J.; Vial, V.; Endou, H.; Wempe, M.F.; Parks, S.K.; et al. The glutamine transporter ASCT2 (SLC1A5) promotes tumor growth independently of the amino acid transporter LAT1 (SLC7A5). J. Biol. Chem. 2018, 293, 2877–2887. [Google Scholar] [CrossRef] [PubMed]
- Koppula, P.; Zhuang, L.; Gan, B. Cystine transporter SLC7A11/xCT in cancer: Ferroptosis, nutrient dependency, and cancer therapy. Protein Cell 2021, 12, 599–620. [Google Scholar] [CrossRef]
- Wang, B.; Pei, J.; Xu, S.; Liu, J.; Yu, J. A glutamine tug-of-war between cancer and immune cells: Recent advances in unraveling the ongoing battle. J. Exp. Clin. Cancer Res. 2024, 43, 74. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Leekha, A.; Nandy, S.; Kulkarni, R.; Martinez-Paniagua, M.; Sefat, K.M.S.R.; Willson, R.C.; Varadarajan, N. Enzymatic depletion of circulating glutamine is immunosuppressive in cancers. iScience 2024, 27, 109817. [Google Scholar] [CrossRef] [PubMed]
- Kaneda-Nakashima, K.; Zhang, Z.; Manabe, Y.; Shimoyama, A.; Kabayama, K.; Watabe, T.; Kanai, Y.; Ooe, K.; Toyoshima, A.; Shirakami, Y.; et al. α-Emitting cancer therapy using 211At-AAMT targeting LAT1. Cancer Sci. 2021, 112, 1132–1140. [Google Scholar] [CrossRef]
- Gong, X.; Zhou, Y.; Deng, Y. Targeting DNA damage response-mediated resistance in non-small cell lung cancer: From mechanistic insights to drug development. Curr. Oncol. 2025, 32, 367. [Google Scholar] [CrossRef]
- da Costa, A.A.B.A.; Chowdhury, D.; Shapiro, G.I.; D’Andrea, A.D.; Konstantinopoulos, P.A. Targeting replication stress in cancer therapy. Nat. Rev. Drug Discov. 2023, 22, 38–58. [Google Scholar] [CrossRef] [PubMed]
- Nickoloff, J.A. Targeting replication stress response pathways to enhance genotoxic chemo- and radiotherapy. Molecules 2022, 27, 4736. [Google Scholar] [CrossRef]
- Gralewska, P.; Gajek, A.; Marczak, A.; Rogalska, A. Participation of the ATR/CHK1 pathway in replicative stress targeted therapy of high-grade ovarian cancer. J. Hematol. Oncol. 2020, 13, 39. [Google Scholar] [CrossRef]
- Lohberger, B.; Glänzer, D.; Eck, N.; Stasny, K.; Falkner, A.; Leithner, A.; Georg, D. The ATR inhibitor VE-821 enhances the radiosensitivity and suppresses DNA repair mechanisms of human chondrosarcoma cells. Int. J. Mol. Sci. 2023, 24, 2315. [Google Scholar] [CrossRef]
- Liu, S.; Jiang, A.; Tang, F.; Duan, M.; Li, B. Drug-induced tolerant persisters in tumor: Mechanism, vulnerability and perspective implication for clinical treatment. Mol. Cancer 2025, 24, 150. [Google Scholar] [CrossRef]
- Prasanna, P.G.; Citrin, D.E.; Hildesheim, J.; Ahmed, M.M.; Venkatachalam, S.; Riscuta, G.; Xi, D.; Zheng, G.; van Deursen, J.; Goronzy, J.; et al. Therapy-induced senescence: Opportunities to improve anticancer therapy. J. Natl. Cancer Inst. 2021, 113, 1285–1298. [Google Scholar] [CrossRef]
- Barnieh, F.M.; Morton, J.; Olanrewaju, O.; El-Khamisy, S.F. Decoding the adaptive survival mechanisms of breast cancer dormancy. Oncogene 2025, 44, 3759–3773. [Google Scholar] [CrossRef] [PubMed]
- Saleh, T.; Greenberg, E.F.; Faber, A.C.; Harada, H.; Gewirtz, D.A. A critical appraisal of the utility of targeting therapy-induced senescence for cancer treatment. Cancer Res. 2025, 85, 1755–1768. [Google Scholar] [CrossRef]
- Li, Y.; Mao, T.; Wang, J.; Zheng, H.; Hu, Z.; Cao, P.; Yang, S.; Zhu, L.; Guo, S.; Zhao, X.; et al. Toward the next generation EGFR inhibitors: An overview of osimertinib resistance mediated by EGFR mutations in non-small cell lung cancer. Cell Commun. Signal. 2023, 21, 71. [Google Scholar] [CrossRef] [PubMed]
- Zhou, K.; Li, S.; Zhao, Y.; Cheng, K. Mechanisms of drug resistance to immune checkpoint inhibitors in non-small cell lung cancer. Front. Immunol. 2023, 14, 1127071. [Google Scholar] [CrossRef]
- Alsaafeen, B.H.; Ali, B.R.; Elkord, E. Resistance mechanisms to immune checkpoint inhibitors: Updated insights. Mol. Cancer 2025, 24, 20. [Google Scholar] [CrossRef]
- Koyama, S.; Akbay, E.A.; Li, Y.Y.; Herter-Sprie, G.S.; Buczkowski, K.A.; Richards, W.G.; Gandhi, L.; Redig, A.J.; Rodig, S.J.; Asahina, H.; et al. Adaptive resistance to therapeutic PD-1 blockade is associated with upregulation of alternative immune checkpoints. Nat. Commun. 2016, 7, 10501. [Google Scholar] [CrossRef]
- Telarovic, I.; Wenger, R.H.; Pruschy, M. Interfering with tumor hypoxia for radiotherapy optimization. J. Exp. Clin. Cancer Res. 2021, 40, 197. [Google Scholar] [CrossRef]
- Catania, C.; Liu, S.V.; Garassino, M.; Delmonte, A.; Scotti, V.; Cappuzzo, F.; Genova, C.; Russo, A.; Russano, M.; Bennati, C.; et al. Correlation between treatments and outcomes of patients with EGFR-mutated non-small-cell lung cancer that transitioned into small-cell lung cancer: An international retrospective study. ESMO Open 2025, 10, 105326. [Google Scholar] [CrossRef]
- Lailler, C.; Didelot, A.; Garinet, S.; Berthou, H.; Sroussi, M.; de Reyniès, A.; Dedhar, S.; Martin-Lannerée, S.; Fabre, E.; Le Pimpec-Barthes, F.; et al. PrPC controls epithelial-to-mesenchymal transition in EGFR-mutated NSCLC: Implications for TKI resistance and patient follow-up. Oncogene 2024, 43, 2781–2794. [Google Scholar] [CrossRef]
- Rumde, P.H.; Burns, T.F. A path to persistence after EGFR inhibition. Cancer Res. 2024, 84, 1188–1190. [Google Scholar] [CrossRef] [PubMed]
- Tufail, M.; Jiang, C.-H.; Li, N. Altered Metabolism in Cancer: Insights into Energy Pathways and Therapeutic Targets. Mol. Cancer 2024, 23, 203. [Google Scholar] [CrossRef]
- Jakobsen, S.; Nielsen, C.U. Exploring amino acid transporters as therapeutic targets for cancer: An examination of inhibitor structures, selectivity issues, and discovery approaches. Pharmaceutics 2024, 16, 197. [Google Scholar] [CrossRef]
- Hushmandi, K.; Einollahi, B.; Saadat, S.H.; Lee, E.H.C.; Farani, M.R.; Okina, E.; Huh, Y.S.; Nabavi, N.; Salimimoghadam, S.; Kumar, A.P. Amino acid transporters within the solute carrier superfamily: Underappreciated proteins and novel opportunities for cancer therapy. Mol. Metab. 2024, 84, 101952. [Google Scholar] [CrossRef]
- Kahlhofer, J.; Teis, D. The human LAT1–4F2hc (SLC7A5–SLC3A2) transporter complex: Physiological and pathophysiological implications. Basic Clin. Pharmacol. Toxicol. 2023, 133, 459–472. [Google Scholar] [CrossRef]
- Scalise, M.; Pochini, L.; Console, L.; Losso, M.A.; Indiveri, C. The human SLC1A5 (ASCT2) amino acid transporter: From function to structure and role in cell biology. Front. Cell Dev. Biol. 2018, 6, 96. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Dong, Z.; Wang, J. Circ_0000808 promotes the development of non-small cell lung cancer by regulating glutamine metabolism via the miR-1827/SLC1A5 axis. World J. Surg. Oncol. 2022, 20, 329. [Google Scholar] [CrossRef]
- Parker, J.L.; Deme, J.C.; Kolokouris, D.; Kuteyi, G.; Biggin, P.C.; Lea, S.M.; Newstead, S. Molecular basis for redox control by the human cystine/glutamate antiporter system Xc−. Nat. Commun. 2021, 12, 7147. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Lu, Z.; Sun, R.; Guo, S.; Gao, F.; Cao, B.; Aa, J. The role of SLC7A11 in cancer: Friend or foe? Cancers 2022, 14, 3059. [Google Scholar] [CrossRef]
- Ishimoto, T.; Nagano, O.; Yae, T.; Tamada, M.; Motohara, T.; Oshima, H.; Oshima, M.; Ikeda, T.; Asaba, R.; Yagi, H.; et al. CD44 variant regulates redox status in cancer cells by stabilizing the xCT subunit of system Xc− and thereby promotes tumor growth. Cancer Cell 2011, 19, 387–400. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Liu, Y.; Cao, J.; Wu, C.; Tang, L.; Bian, W.; Chen, Y.; Yu, L.; Wu, Y.; Li, S.; et al. Targeting epigenetic and post-translational modifications of NRF2: Key regulatory factors in disease treatment. Cell Death Discov. 2025, 11, 189. [Google Scholar] [CrossRef]
- Wang, J.; Hao, S.; Song, G.; Wang, Y.; Hao, Q. The prognostic and clinicopathological significance of SLC7A11 in human cancers: A systematic review and meta-analysis. PeerJ 2023, 11, e14931. [Google Scholar] [CrossRef]
- Hu, K.; Li, K.; Lv, J.; Feng, J.; Chen, J.; Wu, H.; Cheng, F.; Jiang, W.; Wang, J.; Pei, H.; et al. Suppression of the SLC7A11/glutathione axis causes synthetic lethality in KRAS-mutant lung adenocarcinoma. J. Clin. Investig. 2020, 130, 1752–1766. [Google Scholar] [CrossRef]
- Wu, D.; Yan, R.; Song, S.; Swansiger, A.K.; Li, Y.; Prell, J.S.; Zhou, Q.; Robinson, C.V. The complete assembly of human LAT1-4F2hc complex provides insights into its regulation, function and localisation. Nat. Commun. 2024, 15, 3711. [Google Scholar] [CrossRef]
- Wang, Q.; Holst, J. L-type amino acid transport and cancer: Targeting the mTORC1 pathway to inhibit neoplasia. Am. J. Cancer Res. 2015, 5, 1281–1294. [Google Scholar] [PubMed]
- Imai, H.; Kaira, K.; Oriuchi, N.; Yanagitani, N.; Sunaga, N.; Ishizuka, T.; Kanai, Y.; Endou, H.; Nakajima, T.; Mori, M. L-type amino acid transporter 1 expression is a prognostic marker in patients with surgically resected stage I non-small cell lung cancer. Histopathology 2009, 54, 804–813. [Google Scholar] [CrossRef] [PubMed]
- Scalise, M.; Mazza, T.; Pappacoda, G.; Pochini, L.; Cosco, J.; Rovella, F.; Indiveri, C. The human SLC1A5 neutral amino acid transporter catalyzes a pH-dependent glutamate/glutamine antiport, as well. Front. Cell Dev. Biol. 2020, 8, 603. [Google Scholar] [CrossRef]
- Liu, Y.; Ge, X.; Pang, J.; Zhang, Y.; Zhang, H.; Wu, H.; Fan, F.; Liu, H. Restricting glutamine uptake enhances NSCLC sensitivity to third-generation EGFR-TKI almonertinib. Front. Pharmacol. 2021, 12, 671328. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, K.; Kaira, K.; Tomizawa, Y.; Sunaga, N.; Kawashima, O.; Oriuchi, N.; Tominaga, H.; Nagamori, S.; Kanai, Y.; Yamada, M.; et al. ASC amino acid transporter 2 (ASCT2) as a novel prognostic marker in non-small cell lung cancer. Br. J. Cancer 2014, 110, 2030–2039. [Google Scholar] [CrossRef]
- Huang, Y.; Dai, Z.; Barbacioru, C.; Sadée, W. Cystine-glutamate transporter SLC7A11 in cancer chemosensitivity and chemoresistance. Cancer Res. 2005, 65, 7446–7454. [Google Scholar] [CrossRef]
- Jyotsana, N.; Ta, K.T.; DelGiorno, K.E. The role of cystine/glutamate antiporter SLC7A11/xCT in the pathophysiology of cancer. Front. Oncol. 2022, 12, 858462. [Google Scholar] [CrossRef]
- Ji, X.; Qian, J.; Rahman, S.M.J.; Siska, P.J.; Zou, Y.; Harris, B.K.; Hoeksema, M.D.; Trenary, I.A.; Chen, H.; Eisenberg, R.; et al. xCT (SLC7A11)-mediated metabolic reprogramming promotes non-small cell lung cancer progression. Oncogene 2018, 37, 5007–5019. [Google Scholar] [CrossRef]
- Wolfson, R.L.; Chantranupong, L.; Saxton, R.A.; Shen, K.; Scaria, S.M.; Cantor, J.R.; Sabatini, D.M. Sestrin2 is a leucine sensor for the mTORC1 pathway. Science 2016, 351, 43–48. [Google Scholar] [CrossRef]
- Lama-Sherpa, T.D.; Jeong, M.-H.; Jewell, J.L. Regulation of mTORC1 by the Rag GTPases. Biochem. Soc. Trans. 2023, 51, 655–664. [Google Scholar] [CrossRef] [PubMed]
- Durán, R.V.; Oppliger, W.; Robitaille, A.M.; Heiserich, L.; Skendaj, R.; Gottlieb, E.; Hall, M.N. Glutaminolysis activates Rag-mTORC1 signaling. Mol. Cell 2012, 47, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Kandasamy, P.; Zlobec, I.; Nydegger, D.T.; Pujol-Giménez, J.; Bhardwaj, R.; Shirasawa, S.; Tsunoda, T.; Hediger, M.A. Oncogenic KRAS mutations enhance amino acid uptake by colorectal cancer cells via the Hippo signaling effector YAP1. Mol. Oncol. 2021, 15, 2782–2800. [Google Scholar] [CrossRef] [PubMed]
- Imai, H.; Kaira, K.; Oriuchi, N.; Shimizu, K.; Tominaga, H.; Yanagitani, N.; Sunaga, N.; Ishizuka, T.; Nagamori, S.; Promchan, K.; et al. Inhibition of L-type amino acid transporter 1 has antitumor activity in non-small cell lung cancer. Anticancer. Res. 2010, 30, 4819–4828. [Google Scholar]
- Zhang, Z.; Liu, R.; Shuai, Y.; Huang, Y.; Jin, R.; Wang, X.; Luo, J. ASCT2 (SLC1A5)-dependent glutamine uptake is involved in the progression of head and neck squamous cell carcinoma. Br. J. Cancer 2020, 122, 82–93. [Google Scholar] [CrossRef]
- Wang, W.; Guo, M.-N.; Li, N.; Pang, D.-Q.; Wu, J.-H. Glutamine deprivation impairs function of infiltrating CD8+ T cells in hepatocellular carcinoma by inducing mitochondrial damage and apoptosis. World J. Gastrointest. Oncol. 2022, 14, 1124–1140. [Google Scholar] [CrossRef]
- Edwards, D.N.; Ngwa, V.M.; Raybuck, A.L.; Wang, S.; Hwang, Y.; Kim, L.C.; Cho, S.H.; Paik, Y.; Wang, Q.; Zhang, S.; et al. Selective glutamine metabolism inhibition in tumor cells improves antitumor T lymphocyte activity in triple-negative breast cancer. J. Clin. Investig. 2021, 131, e140100. [Google Scholar] [CrossRef]
- Li, Q.; Zhong, X.; Yao, W.; Yu, J.; Wang, C.; Li, Z.; Lai, S.; Qu, F.; Fu, X.; Huang, X.; et al. Inhibitor of Glutamine Metabolism V9302 Promotes ROS-Induced Autophagic Degradation of B7H3 to Enhance Antitumor Immunity. J. Biol. Chem. 2022, 298, 101753. [Google Scholar] [CrossRef]
- Liu, J.; Xia, X.; Huang, P. xCT: A critical molecule that links cancer metabolism to redox signaling. Mol. Ther. 2020, 28, 2358–2366. [Google Scholar] [CrossRef]
- Greenwood, H.E.; Barber, A.R.; Edwards, R.S.; Tyrrell, W.E.; George, M.E.; dos Santos, S.N.; Baark, F.; Tanc, M.; Khalil, E.; Falzone, A.; et al. Imaging NRF2 activation in non-small cell lung cancer with positron emission tomography. Nat. Commun. 2024, 15, 10484. [Google Scholar] [CrossRef]
- Nagane, M.; Kanai, E.; Shibata, Y.; Shimizu, T.; Yoshioka, C.; Maruo, T.; Yamashita, T. Sulfasalazine, an inhibitor of the cystine-glutamate antiporter, reduces DNA damage repair and enhances radiosensitivity in murine B16F10 melanoma. PLoS ONE 2018, 13, e0195151. [Google Scholar] [CrossRef] [PubMed]
- Sendo, K.; Seino, M.; Ohta, T.; Nagase, S. Impact of the glutathione synthesis pathway on sulfasalazine-treated endometrial cancer. Oncotarget 2022, 13, 224–236. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Kang, R.; Klionsky, D.J.; Tang, D. GPX4 in cell death, autophagy, and disease. Autophagy 2023, 19, 2621–2638. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Zhong, R.; Wei, T.; Jin, Y.; He, C.; Li, H.; Cheng, Y. Mechanism of targeting the mTOR pathway to regulate ferroptosis in NSCLC with different EGFR mutations. Oncol. Lett. 2024, 28, 1–9. [Google Scholar] [CrossRef]
- Li, F.-J.; Long, H.-Z.; Zhou, Z.-W.; Luo, H.-Y.; Xu, S.-G.; Gao, L.-C. System Xc−/GSH/GPX4 axis: An important antioxidant system for the ferroptosis in drug-resistant solid tumor therapy. Front. Pharmacol. 2022, 13, 910292. [Google Scholar] [CrossRef]
- Sinclair, L.V.; Neyens, D.; Ramsay, G.; Taylor, P.M.; Cantrell, D.A. Single cell analysis of kynurenine and system L amino acid transport in T cells. Nat. Commun. 2018, 9, 1981. [Google Scholar] [CrossRef]
- Solvay, M.; Holfelder, P.; Klaessens, S.; Pilotte, L.; Stroobant, V.; Lamy, J.; Naulaerts, S.; Spillier, Q.; Frédérick, R.; De Plaen, E.; et al. Tryptophan depletion sensitizes the AHR pathway by increasing AHR expression and GCN2/LAT1-mediated kynurenine uptake, and potentiates induction of regulatory T lymphocytes. J. Immunother. Cancer 2023, 11, e006728. [Google Scholar] [CrossRef]
- Sinclair, L.V.; Rolf, J.; Emslie, E.; Shi, Y.-B.; Taylor, P.M.; Cantrell, D.A. Control of amino acid transport by antigen receptors coordinates the metabolic reprogramming essential for T cell differentiation. Nat. Immunol. 2013, 14, 500–508. [Google Scholar] [CrossRef]
- Saini, N.; Naaz, A.; Metur, S.P.; Gahlot, P.; Walvekar, A.; Dutta, A.; Davathamizhan, U.; Sarin, A.; Laxman, S. Methionine uptake via the SLC43A2 transporter is essential for regulatory T-cell survival. Life Sci. Alliance 2022, 5, e202201663. [Google Scholar] [CrossRef]
- Ma, G.; Liang, Y.; Chen, Y.; Wang, L.; Li, D.; Liang, Z.; Wang, X.; Tian, D.; Yang, X.; Niu, H. Glutamine deprivation induces PD-L1 expression via activation of EGFR/ERK/c-Jun signaling in renal cancer. Mol. Cancer Res. 2020, 18, 324–339. [Google Scholar] [CrossRef]
- Bessede, A.; Peyraud, F.; Le Moulec, S.; Cousin, S.; Cabart, M.; Chomy, F.; Rey, C.; Lara, O.; Odin, O.; Nafia, I.; et al. Upregulation of indoleamine 2,3-dioxygenase 1 in tumor cells and tertiary lymphoid structures is a hallmark of inflamed non-small cell lung cancer. Clin. Cancer Res. 2023, 29, 4883–4893. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Li, Y.; Yang, X.; Zhang, X.; Xie, J.; Li, S.; Liu, H.; Guo, J.; He, L.; Chen, W.; et al. T lymphocyte infiltration in association with IDO1 expression in resected lung adenocarcinoma and normal adjacent lung tissues. Biomed. Res. Int. 2022, 2022, 2381018. [Google Scholar] [CrossRef] [PubMed]
- Kaira, K.; Oriuchi, N.; Imai, H.; Shimizu, K.; Yanagitani, N.; Sunaga, N.; Hisada, T.; Tanaka, S.; Ishizuka, T.; Kanai, Y.; et al. Prognostic significance of L-type amino acid transporter 1 expression in resectable stage I–III nonsmall cell lung cancer. Br. J. Cancer 2008, 98, 742–748. [Google Scholar] [CrossRef]
- Yazawa, T.; Shimizu, K.; Kaira, K.; Nagashima, T.; Ohtaki, Y.; Atsumi, J.; Obayashi, K.; Nagamori, S.; Kanai, Y.; Oyama, T.; et al. Clinical significance of coexpression of L-type amino acid transporter 1 (LAT1) and ASC amino acid transporter 2 (ASCT2) in lung adenocarcinoma. Am. J. Transl. Res. 2015, 7, 1126–1139. [Google Scholar]
- Robert, S.M.; Buckingham, S.C.; Campbell, S.L.; Robel, S.; Holt, K.T.; Ogunrinu-Babarinde, T.; Warren, P.P.; White, D.M.; Reid, M.A.; Eschbacher, J.M.; et al. SLC7A11 expression is associated with seizures and predicts poor survival in patients with malignant glioma. Sci. Transl. Med. 2015, 7, 289ra86. [Google Scholar] [CrossRef]
- Stine, Z.E.; Walton, Z.E.; Altman, B.J.; Hsieh, A.L.; Dang, C.V. MYC, metabolism, and cancer. Cancer Discov. 2015, 5, 1024–1039. [Google Scholar] [CrossRef]
- Onishi, Y.; Hiraiwa, M.; Kamada, H.; Iezaki, T.; Yamada, T.; Kaneda, K.; Hinoi, E. Hypoxia affects Slc7a5 expression through HIF-2α in differentiated neuronal cells. FEBS Open Bio 2019, 9, 241–247. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, X.; Chen, D.; Liu, Y.; Li, Z.; Duan, S.; Zhang, Z.; Jiang, X.; Stockwell, B.R.; Gu, W. GAS41 modulates ferroptosis by anchoring NRF2 on chromatin. Nat. Commun. 2024, 15, 2531. [Google Scholar] [CrossRef]
- Gu, Z.; Liu, Y.; Cai, F.; Patrick, M.; Zmajkovic, J.; Cao, H.; Zhang, Y.; Tasdogan, A.; Chen, M.; Qi, L.; et al. Loss of EZH2 reprograms BCAA metabolism to drive leukemic transformation. Cancer Discov. 2019, 9, 1228–1247. [Google Scholar] [CrossRef]
- Console, L.; Scalise, M.; Tarmakova, Z.; Coe, I.R.; Indiveri, C. N-linked glycosylation of human SLC1A5 (ASCT2) transporter is critical for trafficking to membrane. Biochim. Biophys. Acta Mol. Cell Res. 2015, 1853, 1636–1645. [Google Scholar] [CrossRef]
- Dickens, D.; Chiduza, G.N.; Wright, G.S.; Pirmohamed, M.; Antonyuk, S.V.; Hasnain, S.S. Modulation of LAT1 (SLC7A5) transporter activity and stability by membrane cholesterol. Sci. Rep. 2017, 7, 43580. [Google Scholar] [CrossRef] [PubMed]
- Lieu, E.L.; Nguyen, T.; Rhyne, S.; Kim, J. Amino acids in cancer. Exp. Mol. Med. 2020, 52, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Tian, L.; Liu, C.; Zheng, S.; Shi, H.; Wei, F.; Jiang, W.; Dong, Y.; Xu, H.; Yin, E.; Sun, N.; et al. KEAP1 mutations as key crucial prognostic biomarkers for resistance to KRAS-G12C inhibitors. J. Transl. Med. 2025, 23, 82. [Google Scholar] [CrossRef] [PubMed]
- Roncali, L.; Hindré, F.; Samarut, E.; Lacoeuille, F.; Rousseau, A.; Lemée, J.-M.; Garcion, E.; Chérel, M. Current landscape and future directions of targeted alpha therapy for glioblastoma treatment. Theranostics 2025, 15, 4861–4889. [Google Scholar] [CrossRef]
- Li, F.; Yang, Y.; Liao, J.; Liu, N. Recent progress of astatine-211 in endoradiotherapy: Great advances from fundamental properties to targeted radiopharmaceuticals. Chin. Chem. Lett. 2022, 33, 3325–3338. [Google Scholar] [CrossRef]
- Eriksson, S.E.; Bäck, T.; Elgström, E.; Jensen, H.; Nilsson, R.; Lindegren, S.; Tennvall, J. Successful radioimmunotherapy of established syngeneic rat colon carcinoma with 211At-mAb. EJNMMI Res. 2013, 3, 23. [Google Scholar] [CrossRef]
- Guerra Liberal, F.D.C.; Moreira, H.; Redmond, K.M.; O’Sullivan, J.M.; Alshehri, A.H.D.; Wright, T.C.; Dunne, V.L.; Campfield, C.; Biggart, S.; McMahon, S.J.; et al. Differential responses to 223Ra and alpha-particles exposure in prostate cancer driven by mitotic catastrophe. Front. Oncol. 2022, 12, 877302. [Google Scholar] [CrossRef]
- Tronchin, S.; Forster, J.; Hickson, K.; Bezak, E. Modeling the effect of daughter migration on dosimetry estimates for unlabeled actinium-225. Med. Phys. 2024, 51, 5032–5044. [Google Scholar] [CrossRef]
- Hooijman, E.L.; Radchenko, V.; Ling, S.W.; Konijnenberg, M.; Brabander, T.; Koolen, S.L.W.; de Blois, E. Implementing Ac-225 labelled radiopharmaceuticals: Practical considerations and (pre-)clinical perspectives. EJNMMI Radiopharm. Chem. 2024, 9, 9. [Google Scholar] [CrossRef]
- Ahenkorah, S.; Cassells, I.; Deroose, C.M.; Cardinaels, T.; Burgoyne, A.R.; Bormans, G.; Ooms, M.; Cleeren, F. Bismuth-213 for targeted radionuclide therapy: From atom to bedside. Pharmaceutics 2021, 13, 599. [Google Scholar] [CrossRef]
- Stokke, C.; Kvassheim, M.; Blakkisrud, J. Radionuclides for targeted therapy: Physical properties. Molecules 2022, 27, 5429. [Google Scholar] [CrossRef]
- Piccardo, A.; Ugolini, M.; Altrinetti, V.; Bottoni, G.; Lupi, I.; Tonacchera, M.; Vitti, P.; Trimboli, P. Radioiodine therapy of Graves’ disease. Q. J. Nucl. Med. Mol. Imaging 2021, 65, 132–137. [Google Scholar] [CrossRef]
- Meyer, C.; Stuparu, A.; Lueckerath, K.; Calais, J.; Czernin, J.; Slavik, R.; Dahlbom, M. Tandem isotope therapy with 225Ac- and 177Lu-PSMA-617 in a murine model of prostate cancer. J. Nucl. Med. 2023, 64, 1772–1778. [Google Scholar] [CrossRef] [PubMed]
- Sjögreen Gleisner, K.; Chouin, N.; Minguez Gabina, P.; Cicone, F.; Gnesin, S.; Stokke, C.; Konijnenberg, M.; Cremonesi, M.; Verburg, F.A.; Bernhardt, P.; et al. EANM dosimetry committee recommendations for dosimetry of 177Lu-labelled somatostatin-receptor- and PSMA-targeting ligands. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 1778–1809. [Google Scholar] [CrossRef] [PubMed]
- Palangka, C.R.A.P.; Mahendra, I.; Ritawidya, R.; Kondo, N.; Nakajima, T. Alpha particle emitter radiolabeled antibodies in cancer therapy: Current status, challenges, and future prospects. Pharmaceuticals 2025, 18, 1316. [Google Scholar] [CrossRef]
- Miederer, M.; Benešová-Schäfer, M.; Mamat, C.; Kästner, D.; Pretze, M.; Michler, E.; Brogsitter, C.; Kotzerke, J.; Kopka, K.; Scheinberg, D.A.; et al. Alpha-emitting radionuclides: Current status and future perspectives. Pharmaceuticals 2024, 17, 76. [Google Scholar] [CrossRef] [PubMed]
- Bolcaen, J.; Kleynhans, J.; Nair, S.; Verhoeven, J.; Goethals, I.; Sathekge, M.; Vandevoorde, C.; Ebenhan, T. A perspective on the radiopharmaceutical requirements for imaging and therapy of glioblastoma. Theranostics 2021, 11, 7911–7947. [Google Scholar] [CrossRef] [PubMed]
- Raval, A.D.; Zhang, Y.; Korn, M.; Constantinovici, N.; McKay, R.R. Real-world utilization patterns and survival in men with metastatic prostate cancer treated with radium-223 in the United States. Prostate Cancer Prostatic Dis. 2025, 1–8. [Google Scholar] [CrossRef]
- Gao, J.; Li, M.; Yin, J.; Liu, M.; Wang, H.; Du, J.; Li, J. The different strategies for the radiolabeling of [211At]-astatinated radiopharmaceuticals. Pharmaceutics 2024, 16, 738. [Google Scholar] [CrossRef]
- Shirakami, Y.; Watabe, T.; Obata, H.; Kaneda, K.; Ooe, K.; Liu, Y.; Teramoto, T.; Toyoshima, A.; Shinohara, A.; Shimosegawa, E.; et al. Synthesis of [211At]4-astato-L-phenylalanine by dihydroxyboryl-astatine substitution reaction in aqueous solution. Sci. Rep. 2021, 11, 12982. [Google Scholar] [CrossRef]
- Guérard, F.; Lee, Y.-S.; Baidoo, K.; Gestin, J.-F.; Brechbiel, M.W. Unexpected behavior of the heaviest halogen astatine in the nucleophilic substitution of aryliodonium salts. Chem. Eur. J. 2016, 22, 12332–12339. [Google Scholar] [CrossRef]
- Ohshima, Y.; Suzuki, H.; Hanaoka, H.; Sasaki, I.; Watanabe, S.; Haba, H.; Arano, Y.; Tsushima, Y.; Ishioka, N.S. Preclinical evaluation of new α-radionuclide therapy targeting LAT1: 2-[211At]astato-α-methyl-L-phenylalanine in tumor-bearing model. Nucl. Med. Biol. 2020, 90–91, 15–22. [Google Scholar] [CrossRef]
- Hanaoka, H.; Ohshima, Y.; Suzuki, H.; Sasaki, I.; Watabe, T.; Ooe, K.; Watanabe, S.; Ishioka, N.S. Enhancing the therapeutic effect of 2-211At-astato-α-methyl-L-phenylalanine with probenecid loading. Cancers 2021, 13, 5514. [Google Scholar] [CrossRef]
- Lee, Y.; Jin, C.; Ohgaki, R.; Xu, M.; Ogasawara, S.; Warshamanage, R.; Yamashita, K.; Murshudov, G.; Nureki, O.; Murata, T.; et al. Structural basis of anticancer drug recognition and amino acid transport by LAT1. Nat. Commun. 2025, 16, 1635. [Google Scholar] [CrossRef]
- Kanai, A.; Hanaoka, H.; Yamaguchi, A.; Mahendra, I.; Palangka, C.; Ohshima, Y.; Higuchi, T.; Tsushima, Y. Enhancing the accumulation level of 3-[18F]fluoro-L-α-methyltyrosine in tumors by preloading probenecid. Nucl. Med. Biol. 2022, 104–105, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Nishikubo, K.; Ohgaki, R.; Okanishi, H.; Okuda, S.; Xu, M.; Endou, H.; Kanai, Y. Pharmacologic inhibition of LAT1 predominantly suppresses transport of large neutral amino acids and downregulates global translation in cancer cells. J. Cell. Mol. Med. 2022, 26, 5246–5256. [Google Scholar] [CrossRef]
- Bröer, A.; Fairweather, S.; Bröer, S. Disruption of amino acid homeostasis by novel ASCT2 inhibitors involves multiple targets. Front. Pharmacol. 2018, 9, 785. [Google Scholar] [CrossRef] [PubMed]
- Hara, Y.; Minami, Y.; Yoshimoto, S.; Hayashi, N.; Yamasaki, A.; Ueda, S.; Masuko, K.; Masuko, T. Anti-tumor effects of an antagonistic mAb against the ASCT2 amino acid transporter on KRAS-mutated human colorectal cancer cells. Cancer Med. 2019, 9, 302–312. [Google Scholar] [CrossRef] [PubMed]
- Koppula, P.; Olszewski, K.; Zhang, Y.; Kondiparthi, L.; Liu, X.; Lei, G.; Das, M.; Fang, B.; Poyurovsky, M.V.; Gan, B. KEAP1 deficiency drives glucose dependency and sensitizes lung cancer cells and tumors to GLUT inhibition. iScience 2021, 24, 102649. [Google Scholar] [CrossRef]
- Cobler, L.; Zhang, H.; Suri, P.; Park, C.; Timmerman, L.A. xCT inhibition sensitizes tumors to γ-radiation via glutathione reduction. Oncotarget 2018, 9, 32280–32297. [Google Scholar] [CrossRef]
- Gan, B. How erastin assassinates cells by ferroptosis revealed. Protein Cell 2023, 14, 84–86. [Google Scholar] [CrossRef]
- Sun, S.; Shen, J.; Jiang, J.; Wang, F.; Min, J. Targeting ferroptosis opens new avenues for the development of novel therapeutics. Signal Transduct. Target. Ther. 2023, 8, 372. [Google Scholar] [CrossRef]
- Watabe, T.; Kaneda-Nakashima, K.; Shirakami, Y.; Liu, Y.; Ooe, K.; Teramoto, T.; Toyoshima, A.; Shimosegawa, E.; Nakano, T.; Kanai, Y.; et al. Targeted alpha therapy using astatine (211At)-labeled phenylalanine: A preclinical study in glioma bearing mice. Oncotarget 2020, 11, 1388–1398. [Google Scholar] [CrossRef] [PubMed]
- Roncali, L.; Marionneau-Lambot, S.; Roy, C.; Eychenne, R.; Gouard, S.; Avril, S.; Chouin, N.; Riou, J.; Allard, M.; Rousseau, A.; et al. Brain intratumoural astatine-211 radiotherapy targeting syndecan-1 leads to durable glioblastoma remission and immune memory in female mice. EBioMedicine 2024, 105, 105202. [Google Scholar] [CrossRef]
- Takami, H.; Imura, Y.; Outani, H.; Nakai, S.; Inoue, A.; Kotani, Y.; Okada, S.; Kaneda-Nakashima, K. LAT1-targeted alpha therapy using 211At-AAMT for bone and soft tissue sarcomas. Int. J. Mol. Sci. 2025, 26, 8599. [Google Scholar] [CrossRef] [PubMed]
- Xia, P.; Dubrovska, A. CD98 heavy chain as a prognostic biomarker and target for cancer treatment. Front. Oncol. 2023, 13, 1251100. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Wiriyasermkul, P.; Jin, C.; Quan, L.; Ohgaki, R.; Okuda, S.; Kusakizako, T.; Nishizawa, T.; Oda, K.; Ishitani, R.; et al. Cryo-EM structure of the human L-type amino acid transporter 1 in complex with glycoprotein CD98hc. Nat. Struct. Mol. Biol. 2019, 26, 510–517. [Google Scholar] [CrossRef]
- Hayashi, N.; Yamasaki, A.; Ueda, S.; Okazaki, S.; Ohno, Y.; Tanaka, T.; Endo, Y.; Tomioka, Y.; Masuko, K.; Masuko, T.; et al. Oncogenic transformation of NIH/3T3 cells by the overexpression of L-type amino acid transporter 1, a promising anti-cancer target. Oncotarget 2021, 12, 1256–1270. [Google Scholar] [CrossRef]
- Hayes, G.M.; Chinn, L.; Cantor, J.M.; Cairns, B.; Levashova, Z.; Tran, H.; Velilla, T.; Duey, D.; Lippincott, J.; Zachwieja, J.; et al. Antitumor activity of an anti-CD98 antibody. Int. J. Cancer 2015, 137, 710–720. [Google Scholar] [CrossRef]
- Zheng, M.; Wang, Z.; Li, M.; Yang, N.; Lu, H.; Zhang, Z.; Dong, Y.; Chen, Y.; Zhu, Z.; Tong, A.; et al. A novel SLC3A2-targeting antibody-drug conjugate exerts potent antitumor efficacy in head and neck squamous cell cancer. Transl. Oncol. 2024, 45, 101981. [Google Scholar] [CrossRef]
- Montero, J.C.; Calvo-Jiménez, E.; del Carmen, S.; Abad, M.; Ocaña, A.; Pandiella, A. Surfaceome analyses uncover CD98hc as an antibody drug-conjugate target in triple negative breast cancer. J. Exp. Clin. Cancer Res. 2022, 41, 106. [Google Scholar] [CrossRef]
- Montero, J.C.; del Carmen, S.; Abad, M.; Sayagués, J.M.; Barbáchano, A.; Fernández-Barral, A.; Muñoz, A.; Pandiella, A. An amino acid transporter subunit as an antibody–drug conjugate target in colorectal cancer. J. Exp. Clin. Cancer Res. 2023, 42, 200. [Google Scholar] [CrossRef] [PubMed]
- Hingorani, D.V.; Allevato, M.M.; Camargo, M.F.; Lesperance, J.; Quraishi, M.A.; Aguilera, J.; Franiak-Pietryga, I.; Scanderbeg, D.J.; Wang, Z.; Molinolo, A.A.; et al. Monomethyl auristatin antibody and peptide drug conjugates for trimodal cancer chemo-radio-immunotherapy. Nat. Commun. 2022, 13, 3869. [Google Scholar] [CrossRef]
- Hartley, J.A. Antibody-drug conjugates (ADCs) delivering pyrrolobenzodiazepine (PBD) dimers for cancer therapy. Expert Opin. Biol. Ther. 2021, 21, 931–943. [Google Scholar] [CrossRef]
- Gerber, H.-P.; Gangwar, S.; Betts, A. Therapeutic index improvement of antibody-drug conjugates. MAbs 2023, 15, 2230618. [Google Scholar] [CrossRef]
- Metrangolo, V.; Engelholm, L.H. Antibody–drug conjugates: The dynamic evolution from conventional to next-generation constructs. Cancers 2024, 16, 447. [Google Scholar] [CrossRef] [PubMed]
- Vadevoo, S.M.P.; Gurung, S.; Lee, H.-S.; Gunassekaran, G.R.; Lee, S.-M.; Yoon, J.-W.; Lee, Y.-K.; Lee, B. Peptides as multifunctional players in cancer therapy. Exp. Mol. Med. 2023, 55, 1099–1109. [Google Scholar] [CrossRef] [PubMed]
- Echigo, H.; Munekane, M.; Fuchigami, T.; Washiyama, K.; Mishiro, K.; Wakabayashi, H.; Takahashi, K.; Kinuya, S.; Ogawa, K. Optimizing the pharmacokinetics of an 211At-labeled RGD peptide with an albumin-binding moiety via the administration of an albumin-binding inhibitor. Eur. J. Nucl. Med. Mol. Imaging 2024, 51, 2663–2671. [Google Scholar] [CrossRef]
- Echigo, H.; Mishiro, K.; Fuchigami, T.; Shiba, K.; Kinuya, S.; Ogawa, K. Synthesis and evaluation of a dimeric RGD peptide as a preliminary study for radiotheranostics with radiohalogens. Molecules 2021, 26, 6107. [Google Scholar] [CrossRef]
- Bo, T.; Kobayashi, S.; Inanami, O.; Fujii, J.; Nakajima, O.; Ito, T.; Yasui, H. LAT1 inhibitor JPH203 sensitizes cancer cells to radiation by enhancing radiation-induced cellular senescence. Transl. Oncol. 2021, 14, 101212. [Google Scholar] [CrossRef]
- van Geldermalsen, M.; Quek, L.-E.; Turner, N.; Freidman, N.; Pang, A.; Guan, Y.F.; Krycer, J.R.; Ryan, R.; Wang, Q.; Holst, J. Benzylserine inhibits breast cancer cell growth by disrupting intracellular amino acid homeostasis and triggering amino acid response pathways. BMC Cancer 2018, 18, 689. [Google Scholar] [CrossRef]
- Schulte, M.L.; Fu, A.; Zhao, P.; Li, J.; Geng, L.; Smith, S.T.; Kondo, J.; Coffey, R.J.; Johnson, M.O.; Rathmell, J.C.; et al. Pharmacological blockade of ASCT2-dependent glutamine transport leads to antitumor efficacy in preclinical models. Nat. Med. 2018, 24, 194–202. [Google Scholar] [CrossRef]
- Pillai, R.; LeBoeuf, S.E.; Hao, Y.; New, C.; Blum, J.L.E.; Rashidfarrokhi, A.; Huang, S.M.; Bahamon, C.; Wu, W.L.; Karadal-Ferrena, B.; et al. Glutamine antagonist DRP-104 suppresses tumor growth and enhances response to checkpoint blockade in KEAP1 mutant lung cancer. Sci. Adv. 2024, 10, eadm9859. [Google Scholar] [CrossRef] [PubMed]
- Ohno, Y.; Suda, K.; Masuko, K.; Yagi, H.; Hashimoto, Y.; Masuko, T. Production and characterization of highly tumor-specific rat monoclonal antibodies recognizing the extracellular domain of human L-type amino acid transporter 1. Cancer Sci. 2008, 99, 1000–1007. [Google Scholar] [CrossRef]
- Ueda, S.; Hayashi, H.; Miyamoto, T.; Abe, S.; Hirai, K.; Matsukura, K.; Yagi, H.; Hara, Y.; Yoshida, K.; Okazaki, S.; et al. Anti-tumor effects of mAb against L-type amino acid transporter 1 (LAT1) bound to human and monkey LAT1 with dual avidity modes. Cancer Sci. 2019, 110, 674–685. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Byun, J.-K.; Choi, Y.-K.; Park, K.-G. Targeting glutamine metabolism as a therapeutic strategy for cancer. Exp. Mol. Med. 2023, 55, 706–715. [Google Scholar] [CrossRef] [PubMed]
- Herth, M.M.; Hvass, L.; Poulie, C.B.M.; Müller, M.; García-Vázquez, R.; Gustavsson, T.; Shalgunov, V.; Clausen, A.S.; Jørgensen, J.T.; Hansson, E.; et al. An 211At-labeled tetrazine for pretargeted therapy. J. Med. Chem. 2025, 68, 4410–4425. [Google Scholar] [CrossRef]
- Timperanza, C.; Jensen, H.; Bäck, T.; Lindegren, S.; Aneheim, E. Pretargeted alpha therapy of disseminated cancer combining click chemistry and astatine-211. Pharmaceuticals 2023, 16, 595. [Google Scholar] [CrossRef]
- Bhunia, S.; Vangala, V.; Bhattacharya, D.; Ravuri, H.G.; Kuncha, M.; Chakravarty, S.; Sistla, R.; Chaudhuri, A. Large amino acid transporter 1 selective liposomes of L-DOPA functionalized amphiphile for combating glioblastoma. Mol. Pharm. 2017, 14, 3834–3847. [Google Scholar] [CrossRef]
- Li, L.; Di, X.; Wu, M.; Sun, Z.; Zhong, L.; Wang, Y.; Fu, Q.; Kan, Q.; Sun, J.; He, Z. Targeting tumor highly-expressed LAT1 transporter with amino acid-modified nanoparticles: Toward a novel active targeting strategy in breast cancer therapy. Nanomedicine 2017, 13, 987–998. [Google Scholar] [CrossRef] [PubMed]
- De, K.; Prasad, P.; Sinha, S.; Mukhopadhyay, S.; Roy, S.S. Synthesis, characterization, and biological evaluation of radiolabeled glutamine conjugated polymeric nanoparticles: A simple approach for tumor imaging. ACS Appl. Bio Mater. 2023, 6, 2172–2183. [Google Scholar] [CrossRef]
- Huang, X.; Kaneda-Nakashima, K.; Kadonaga, Y.; Kabayama, K.; Shimoyama, A.; Ooe, K.; Kato, H.; Toyoshima, A.; Shinohara, A.; Haba, H.; et al. Astatine-211-labeled gold nanoparticles for targeted alpha-particle therapy via intravenous injection. Pharmaceutics 2022, 14, 2705. [Google Scholar] [CrossRef]
- Ruoslahti, E. Tumor-penetrating peptides for improved drug delivery. Adv. Drug Deliv. Rev. 2017, 110–111, 3–12. [Google Scholar] [CrossRef]
- Makharadze, D.; Valle, L.J.D.; Katsarava, R.; Puiggalí, J. The art of PEGylation: From simple polymer to sophisticated drug delivery system. Int. J. Mol. Sci. 2025, 26, 3102. [Google Scholar] [CrossRef]
- Salgueiro, M.J.; Zubillaga, M. Theranostic nanoplatforms in nuclear medicine: Current advances, emerging trends, and perspectives for personalized oncology. J. Nanotheranostics 2025, 6, 27. [Google Scholar] [CrossRef]
- Chakravarty, R.; Hong, H.; Cai, W. Positron emission tomography image-guided drug delivery: Current status and future perspectives. Mol. Pharm. 2014, 11, 3777–3797. [Google Scholar] [CrossRef] [PubMed]
- Mellhammar, E.; Dahlbom, M.; Vilhelmsson-Timmermand, O.; Strand, S.-E. Tumor Control Probability and Small-Scale Monte Carlo Dosimetry: Effects of Heterogenous Intratumoral Activity Distribution in Radiopharmaceutical Therapy. J. Nucl. Med. 2023, 64, 1632–1637. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Lu, C.; Wang, X.; Wu, D. PSMA Targeted Therapy: From Molecular Mechanisms to Clinical Breakthroughs in Castration-Resistant Prostate Cancer. Eur. J. Med. Chem. 2025, 296, 117829. [Google Scholar] [CrossRef]
- Zhang, C.; Liu, J.; Wu, J.; Ranjan, K.; Cui, X.; Wang, X.; Zhang, D.; Zhu, S. Key Molecular DNA Damage Responses of Human Cells to Radiation. Front. Cell Dev. Biol. 2024, 12, 1422520. [Google Scholar] [CrossRef] [PubMed]
- Rama, E.; May, J.-N.; Rix, A.; Lammers, T.; Kiessling, F. Image-guided strategies to improve drug delivery to tumors beyond using the enhanced permeability and retention (EPR) effect. Biochem. Biophys. Res. Commun. 2025, 778, 152346. [Google Scholar] [CrossRef] [PubMed]
- Kahya, U.; Lukiyanchuk, V.; Gorodetska, I.; Weigel, M.M.; Köseer, A.S.; Alkan, B.; Savic, D.; Linge, A.; Löck, S.; Peitzsch, M.; et al. Disruption of Glutamine Transport Uncouples the NUPR1 Stress-Adaptation Program and Induces Prostate Cancer Radiosensitivity. Cell Commun. Signal. 2025, 23, 351. [Google Scholar] [CrossRef]
- Müller, M.; Pedersen, N.B.; Shalgunov, V.; Jensen, A.I.; Battisti, U.M.; Herth, M.M. Astatine-211—Towards in vivo stable astatine-211 labeled radiopharmaceuticals and their (pre)clinical applications. Med. Res. Rev. 2025; in press. [Google Scholar] [CrossRef]
- Oriuchi, N.; Aoki, M.; Ukon, N.; Washiyama, K.; Tan, C.; Shimoyama, S.; Nishijima, K.; Takahashi, K.; Ito, H.; Ikezoe, T.; et al. Possibility of cancer-stem-cell-targeted radioimmunotherapy for acute myelogenous leukemia using 211At-CXCR4 monoclonal antibody. Sci. Rep. 2020, 10, 6810. [Google Scholar] [CrossRef]
- Larsen, R.H.; Slade, S.; Zalutsky, M.R. Blocking [211At]astatide accumulation in normal tissues: Preliminary evaluation of seven potential compounds. Nucl. Med. Biol. 1998, 25, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Sudo, H.; Tsuji, A.B.; Sugyo, A.; Nagatsu, K.; Minegishi, K.; Ishioka, N.S.; Ito, H.; Yoshinaga, K.; Higashi, T. Preclinical evaluation of the acute radiotoxicity of the α-emitting molecular-targeted therapeutic agent 211At-MABG for the treatment of malignant pheochromocytoma in normal mice. Transl. Oncol. 2019, 12, 879–888. [Google Scholar] [CrossRef]
- Yssartier, T.; Liu, L.; Pardoue, S.; Le Questel, J.-Y.; Guérard, F.; Montavon, G.; Galland, N. In vivo stability of 211At-radiopharmaceuticals: On the impact of halogen bond formation. RSC Med. Chem. 2024, 15, 223–233. [Google Scholar] [CrossRef]
- Andersson, H.; Cederkrantz, E.; Bäck, T.; Divgi, C.; Elgqvist, J.; Himmelman, J.; Horvath, G.; Jacobsson, L.; Jensen, H.; Lindegren, S.; et al. Intraperitoneal α-particle radioimmunotherapy of ovarian cancer patients: Pharmacokinetics and dosimetry of 211At-MX35 F(ab′)2—A phase I study. J. Nucl. Med. 2009, 50, 1153–1160. [Google Scholar] [CrossRef]
- Kaizuka, Y.; Suzuki, H.; Watabe, T.; Ooe, K.; Toyoshima, A.; Takahashi, K.; Sawada, K.; Iimori, T.; Masuda, Y.; Uno, T.; et al. Neopentyl glycol-based radiohalogen-labeled amino acid derivatives for cancer radiotheranostics. EJNMMI Radiopharm. Chem. 2024, 9, 17. [Google Scholar] [CrossRef]
- Ling, S.W.; van der Veldt, A.A.M.; Konijnenberg, M.; Segbers, M.; Hooijman, E.; Bruchertseifer, F.; Morgenstern, A.; de Blois, E.; Brabander, T. Evaluation of the tolerability and safety of [225Ac]Ac-PSMA-I&T in patients with metastatic prostate cancer: A phase I dose escalation study. BMC Cancer 2024, 24, 146. [Google Scholar] [CrossRef]
- Zhao, T.; Liang, S.H. Enhancing the stability of 211At radiopharmaceuticals: Insights from ortho-substituent strategies. ACS Med. Chem. Lett. 2025, 16, 504–507. [Google Scholar] [CrossRef]
- Thurber, G.M.; Weissleder, R. A systems approach for tumor pharmacokinetics. PLoS ONE 2011, 6, e24696. [Google Scholar] [CrossRef]
- Wei, L.; Tominaga, H.; Ohgaki, R.; Wiriyasermkul, P.; Hagiwara, K.; Okuda, S.; Kaira, K.; Oriuchi, N.; Nagamori, S.; Kanai, Y. Specific transport of 3-fluoro-L-α-methyl-tyrosine by LAT1 explains its specificity to malignant tumors in imaging. Cancer Sci. 2016, 107, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Bao, M.; Gu, X.; Tong, K.; Chu, F.; Ye, P.; Kaneda-Nakashima, K.; Hou, W.; Li, Y.; Wei, L. L-3-[18F]-fluoro-α-methyl tyrosine as a PET tracer for tumor diagnosis: A systematic review from mechanisms to clinical applications. Int. J. Mol. Sci. 2025, 26, 5848. [Google Scholar] [CrossRef] [PubMed]
- Watabe, T.; Ose, N.; Naka, S.; Fukui, E.; Kimura, T.; Kanou, T.; Funaki, S.; Sasaki, H.; Kamiya, T.; Kurimoto, K.; et al. Evaluation of LAT1 expression in patients with lung cancer and mediastinal tumors: 18F-FBPA PET study with immunohistological comparison. Clin. Nucl. Med. 2023, 48, 853–860. [Google Scholar] [CrossRef] [PubMed]
- Bednarz, B. Theranostics and patient-specific dosimetry. Semin. Radiat. Oncol. 2023, 33, 317–326. [Google Scholar] [CrossRef]
- Naka, S.; Ooe, K.; Shirakami, Y.; Kurimoto, K.; Sakai, T.; Takahashi, K.; Toyoshima, A.; Wang, Y.; Haba, H.; Kato, H.; et al. Production of [211At]NaAt solution under GMP compliance for investigator-initiated clinical trial. EJNMMI Radiopharm. Chem. 2024, 9, 29. [Google Scholar] [CrossRef] [PubMed]
- Kondo, Y.; Joho, T.; Sasaki, S.; Mochizuki, K.; Hasegawa, N.; Ukon, N.; Nishijima, K.; Washiyama, K.; Tanaka, H.; Higashi, T.; et al. Production of 211At and automated radiosynthesis of [211At]MABG via electrophilic astatodesilylation. EJNMMI Radiopharm. Chem. 2025, 10, 52. [Google Scholar] [CrossRef]
- Liu, Y.-H.; Li, Y.-L.; Shen, H.-T.; Chien, P.-J.; Sheu, G.-T.; Wang, B.-Y.; Chang, W.-W. L-type amino acid transporter 1 regulates cancer stemness and the expression of programmed cell death 1 ligand 1 in lung cancer cells. Int. J. Mol. Sci. 2021, 22, 10955. [Google Scholar] [CrossRef]
- Cheng, Z.; Cui, H.; Wang, Y.; Yang, J.; Lin, C.; Shi, X.; Zou, Y.; Chen, J.; Jia, X.; Su, L. The advance of the third-generation EGFR-TKI in the treatment of non-small cell lung cancer: A review. Oncol. Rep. 2024, 51, 16. [Google Scholar] [CrossRef]
- Awad, M.M.; Liu, S.; Rybkin, I.I.; Arbour, K.C.; Dilly, J.; Zhu, V.W.; Johnson, M.L.; Heist, R.S.; Patil, T.; Riely, G.J.; et al. Acquired resistance to KRASG12C inhibition in cancer. N. Engl. J. Med. 2021, 384, 2382–2393. [Google Scholar] [CrossRef]
- Poty, S.; Francesconi, L.C.; McDevitt, M.R.; Morris, M.J.; Lewis, J.S. α-emitters for radiotherapy: From basic radiochemistry to clinical studies—Part 1. J. Nucl. Med. 2018, 59, 878–884. [Google Scholar] [CrossRef]
- Mladenova, V.; Mladenov, E.; Stuschke, M.; Iliakis, G. DNA damage clustering after ionizing radiation and consequences in the processing of chromatin breaks. Molecules 2022, 27, 1540. [Google Scholar] [CrossRef] [PubMed]
- Lüdeking, M.; Stemwedel, K.; Ramachandran, D.; Grosche, S.; Christiansen, H.; Merten, R.; Henkenberens, C.; Bogdanova, N.V. Efficiency of moderately hypofractionated radiotherapy in NSCLC cell model. Front. Oncol. 2024, 14, 1293745. [Google Scholar] [CrossRef]
- Ogihara, K.; Kikuchi, E.; Okazaki, S.; Hagiwara, M.; Takeda, T.; Matsumoto, K.; Kosaka, T.; Mikami, S.; Saya, H.; Oya, M. Sulfasalazine could modulate the CD44v9-xCT system and enhance cisplatin-induced cytotoxic effects in metastatic bladder cancer. Cancer Sci. 2019, 110, 1431–1441. [Google Scholar] [CrossRef] [PubMed]
- Kleinendorst, S.C.; Oosterwijk, E.; Bussink, J.; Westdorp, H.; Konijnenberg, M.W.; Heskamp, S. Combining targeted radionuclide therapy and immune checkpoint inhibition for cancer treatment. Clin. Cancer Res. 2022, 28, 3652–3657. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Liu, H.; Lou, J.; Zhang, J.; Zuo, C.; Zhu, M.; Zhang, X.; Yin, Y.; Zhang, Y.; Qin, S.; et al. Alpha-emitter radium-223 induces STING-dependent pyroptosis to trigger robust antitumor immunity. Small 2024, 20, e2307448. [Google Scholar] [CrossRef]
- Lin, W.; Wang, C.; Liu, G.; Bi, C.; Wang, X.; Zhou, Q.; Jin, H. SLC7A11/xCT in cancer: Biological functions and therapeutic implications. Am. J. Cancer Res. 2020, 10, 3106–3126. [Google Scholar]
- Ertveldt, T.; Krasniqi, A.; Ceuppens, H.; Puttemans, J.; Dekempeneer, Y.; De Jonghe, K.; de Mey, W.; Lecocq, Q.; De Vlaeminck, Y.; Awad, R.M.; et al. Targeted α-therapy using 225Ac radiolabeled single-domain antibodies induces antigen-specific immune responses and instills immunomodulation both systemically and at the tumor microenvironment. J. Nucl. Med. 2023, 64, 751–758. [Google Scholar] [CrossRef]
- Chen, H.; Zhao, L.; Fu, K.; Lin, Q.; Wen, X.; Jacobson, O.; Sun, L.; Wu, H.; Zhang, X.; Guo, Z.; et al. Integrin αvβ3-targeted radionuclide therapy combined with immune checkpoint blockade immunotherapy synergistically enhances anti-tumor efficacy. Theranostics 2019, 9, 7948–7960. [Google Scholar] [CrossRef]
- Kim, J.-W.; Kim, M.-J.; Han, T.-H.; Lee, J.-Y.; Kim, S.; Kim, H.; Oh, K.-J.; Kim, W.K.; Han, B.-S.; Bae, K.-H.; et al. FSP1 confers ferroptosis resistance in KEAP1-mutant non-small cell lung carcinoma in NRF2-dependent and -independent manner. Cell Death Dis. 2023, 14, 567. [Google Scholar] [CrossRef] [PubMed]
- Koppula, P.; Lei, G.; Zhang, Y.; Yan, Y.; Mao, C.; Kondiparthi, L.; Shi, J.; Liu, X.; Horbath, A.; Das, M.; et al. A targetable CoQ–FSP1 axis drives ferroptosis- and radiation-resistance in KEAP1-inactive lung cancers. Nat. Commun. 2022, 13, 2206. [Google Scholar] [CrossRef]
- Nelson, B.J.B.; Krol, V.; Bansal, A.; Andersson, J.D.; Wuest, F.; Pandey, M.K. Aspects and prospects of preclinical theranostic radiopharmaceutical development. Theranostics 2024, 14, 6446–6470. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, A.R.; Koglin, N.; Mittra, E.S.; Han, S.; Cook, G.J.R.; Witney, T.H. Clinical [18F]FSPG positron emission tomography imaging reveals heterogeneity in tumor-associated system xC− activity. Cancers 2024, 16, 1437. [Google Scholar] [CrossRef]
- Cheng, Q.; Wållberg, H.; Grafström, J.; Lu, L.; Thorell, J.-O.; Hägg Olofsson, M.; Linder, S.; Johansson, K.; Tegnebratt, T.; Arnér, E.S.J.; et al. Preclinical PET imaging of EGFR levels: Pairing a targeting with a non-targeting Sel-tagged affibody-based tracer to estimate the specific uptake. EJNMMI Res. 2016, 6, 58. [Google Scholar] [CrossRef]
- Hellyer, J.A.; Padda, S.K.; Diehn, M.; Wakelee, H.A. Clinical implications of KEAP1–NFE2L2 mutations in NSCLC. J. Thorac. Oncol. 2021, 16, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.-S.; Kang, H.-M.; Na, K.; Kim, J.; Kim, T.-W.; Jung, J.; Lim, H.; Seo, H.; Lee, S.H. KEAP1–NRF2 pathway as a novel therapeutic target for EGFR-mutant non-small cell lung cancer. Tuberc. Respir. Dis. 2025, 88, 138–149. [Google Scholar] [CrossRef]
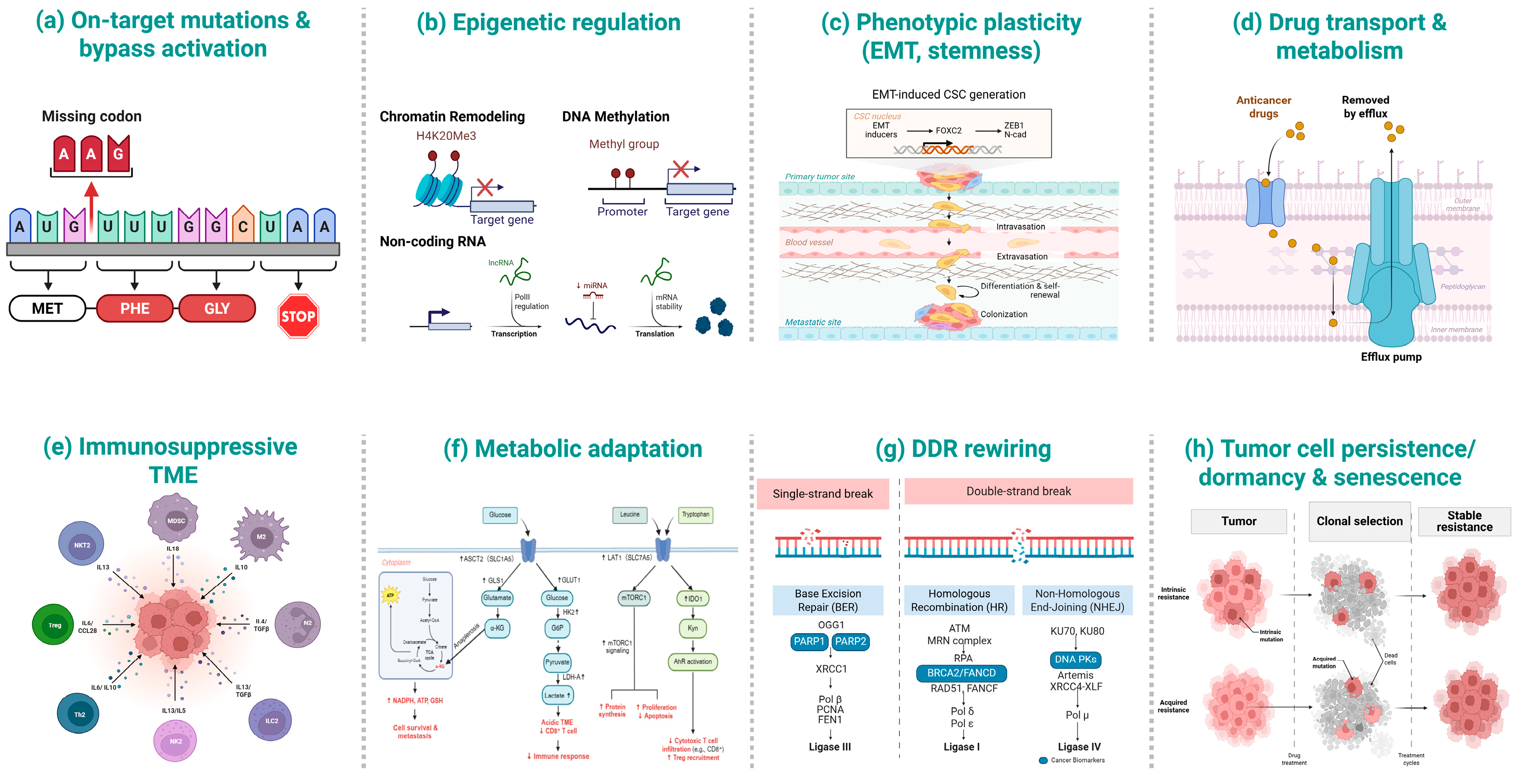
| Mechanism | Key Alterations/Molecules | Functional Consequences | Clinical/Therapeutic Relevance |
|---|---|---|---|
| On-target mutations & bypass activation | EGFR T790M/C797S [34]; ALK G1202R [35]; MET amplification [36] | Impaired drug binding [34,35]; bypass reactivation of PI3K/AKT and MAPK signaling [36] | Supports next-generation TKIs and combinatorial regimens (e.g., osimertinib + MET inhibitors [37]) |
| Epigenetic regulation | DNMT1/3A [38,39]; EZH2 [40]; HDACs [41]; miR-21 [42] | TSG silencing [38,39]; drug-tolerant state maintenance [40] | Provides rationale for DNMT/HDAC/EZH2 inhibitors and epigenetic–TKI/ICI combinations [43] |
| Phenotypic plasticity (EMT, stemness) | EMT-TFs [44], YAP/TAZ [45] | Promotes migration, invasion, and drug tolerance [46] | Highlights EMT/CSC-targeted and microenvironmental interventions [47] |
| Drug transport & metabolism | ABCB1/ABCG2 (efflux) [48]; CYP/UGT variants [49,50] | Reduced intracellular drug levels [48]; altered clearance/exposure [49,50] | Informs transporter-sparing drug design [51], nanoparticle delivery [52], and PK-guided dosing [53] |
| Immunosuppressive TME | PD-L1 upregulation [54]; Treg/MDSC infiltration [55,56] | CD8+ T-cell exclusion and impaired antigen presentation [57] | Supports next-generation ICIs (e.g., PD-1 + LAG-3) and myeloid/Treg-targeted strategies [54] |
| Metabolic adaptation | LAT1 [58], ASCT2 [59], xCT [60] | Enhanced glutamine/cystine influx → redox control, biosynthesis, immune modulation [60,61,62] | Creates vulnerabilities for metabolic inhibitors and radiolabeled strategies (e.g., LAT1-directed α-therapy [63] |
| DNA damage response (DDR) rewiring | HR/NHEJ modulation [64]; ATR–CHK1–WEE1 axis [65] | Enhanced repair and replication-stress tolerance [66] | Provides rationale for DDR inhibitors combined with chemo/radiotherapy or TKIs [67,68] |
| Tumor cell persistence/dormancy & senescence | Drug-tolerant persister (DTP) states [69]; therapy-induced senescence (SASP) [70] | Minimal-residual disease survival and relapse risk [69,71] | Supports persister eradication and senolytic strategies to prevent recurrence [72] |
| Transporter | Structural Features | Functional Role | Clinical Relevance |
|---|---|---|---|
| LAT1 (SLC7A5) | Disulfide-linked heterodimer with CD98hc/4F2hc (SLC3A2) [93] | Leucine uptake → mTORC1 activation [94] | Overexpressed/prognostic in NSCLC; therapeutic target [94,95] |
| ASCT2 (SLC1A5) | Na+-dependent obligatory antiporter [96]; N-glycosylation at N163/N212 [85] | Glutamine uptake sustaining NSCLC proliferation [97] | Correlates with stage, lymphatic/vascular invasion; independent poor-prognosis marker (NSCLC/AC) [98] |
| xCT (SLC7A11) | Light chain of system Xc−; heterodimer with 4F2hc [99] | Cystine/Glutamate exchange → GSH synthesis/antioxidant defense [100] | Upregulated in NSCLC; linked to poor prognosis and drug resistance [100]; therapeutic target [101] |
| Therapeutic Strategy | Representative Agents | Mechanism of Action | Evidence/Preclinical Findings |
|---|---|---|---|
| LAT1 (SLC7A5) inhibitors | JPH203 (nanvuranlat) [182], BCH [106], benzylserine [183] | Block leucine influx via LAT1 → dampen mTORC1 [182]; cytostatic G0/G1 arrest [183] | JPH203 radiosensitizes cancer cells via mTOR downregulation [182]; BenSer inhibits Leu/Gln uptake and cell cycle progression [183]. |
| ASCT2 (SLC1A5) inhibitors | V-9302 [158], benzylserine [183] | Reduce glutamine influx, limiting anaplerosis [184]; condition TME for ICI (note: V-9302 target selectivity debated [159]) | V-9302 attenuates tumor growth [184]; glutamine blockade enhances the efficacy of checkpoint blockade in lung cancer models [185]. |
| xCT (SLC7A11) inhibitors | Erastin [164], sulfasalazine [161], sorafenib [164] | Block cystine uptake → deplete GSH → induce ferroptosis [163] | Erastin sensitizes xCT+ tumors to ionizing radiation [162]; SSZ limits cystine uptake via xCT, thereby lowering GSH and increasing oxidative stress, resulting in growth inhibition [100]. |
| Monoclonal antibodies & ADCs | Anti-LAT1 mAbs (SOL22, SOL69) [186]; IGN523 (anti-CD98hc) [171]; CD98hc-ADCs [173] | mAb internalization → AA uptake decrease ↓; ADCC [187]; ADC payload delivery [173] | Anti-LAT1 mAbs: internalization/ADCC and in vivo antitumor effects [184]; IGN523: lymphoma xenograft activity; AML clinically evaluated; CD98 broadly expressed, incl. NSCLC [171]; CD98hc-ADC active in vivo [173]. |
| 211At-LAT1 radioligands | 211At-AAMT [188]; 211At-AAMP [155] | LAT1-mediated uptake delivers α-tracks, causing clustered DSBs [63] | 211At-AAMT: high LAT1 affinity, induces DSBs [63]; 211At-AAMP: growth inhibition and survival benefit in vivo [155]. |
| Pretargeted strategies (PRIT) | 211At-tetrazine [189] + inverse electron-demand Diels–Alder (IEDDA) [189] | Decouple carrier/radionuclide → improve tumor-to-blood ratios [189] | 211At-labeled pretargeting agent shows higher tumor-to-blood ratios vs. directly labeled mAbs [186]; IEDDA PRIT supports α-therapy [190]. |
| Combination approaches | LAT1 inhibitors + RT/mTOR inhibitors [116]; xCT inhibitors [82] + RT/FINs | Synthetic lethality via DNA damage + metabolic stress; radiosensitization [182] | JPH203 + RT radiosensitization [182]; xCT inhibition enhances RT response [162]; glutamine blockade augments ICI efficacy [185]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feng, S.; Hisada, K.; Yorifuji, H.; Shirakami, Y.; Kaneda-Nakashima, K. Astatine-211-Labeled Therapy Targeting Amino Acid Transporters: Overcoming Drug Resistance in Non-Small Cell Lung Cancer. Int. J. Mol. Sci. 2025, 26, 10736. https://doi.org/10.3390/ijms262110736
Feng S, Hisada K, Yorifuji H, Shirakami Y, Kaneda-Nakashima K. Astatine-211-Labeled Therapy Targeting Amino Acid Transporters: Overcoming Drug Resistance in Non-Small Cell Lung Cancer. International Journal of Molecular Sciences. 2025; 26(21):10736. https://doi.org/10.3390/ijms262110736
Chicago/Turabian StyleFeng, Sifan, Kentaro Hisada, Haruna Yorifuji, Yoshifumi Shirakami, and Kazuko Kaneda-Nakashima. 2025. "Astatine-211-Labeled Therapy Targeting Amino Acid Transporters: Overcoming Drug Resistance in Non-Small Cell Lung Cancer" International Journal of Molecular Sciences 26, no. 21: 10736. https://doi.org/10.3390/ijms262110736
APA StyleFeng, S., Hisada, K., Yorifuji, H., Shirakami, Y., & Kaneda-Nakashima, K. (2025). Astatine-211-Labeled Therapy Targeting Amino Acid Transporters: Overcoming Drug Resistance in Non-Small Cell Lung Cancer. International Journal of Molecular Sciences, 26(21), 10736. https://doi.org/10.3390/ijms262110736







