In Vitro and Ex Vivo Models to Study Molecular Trafficking Across the Human Intestinal Barrier
Abstract
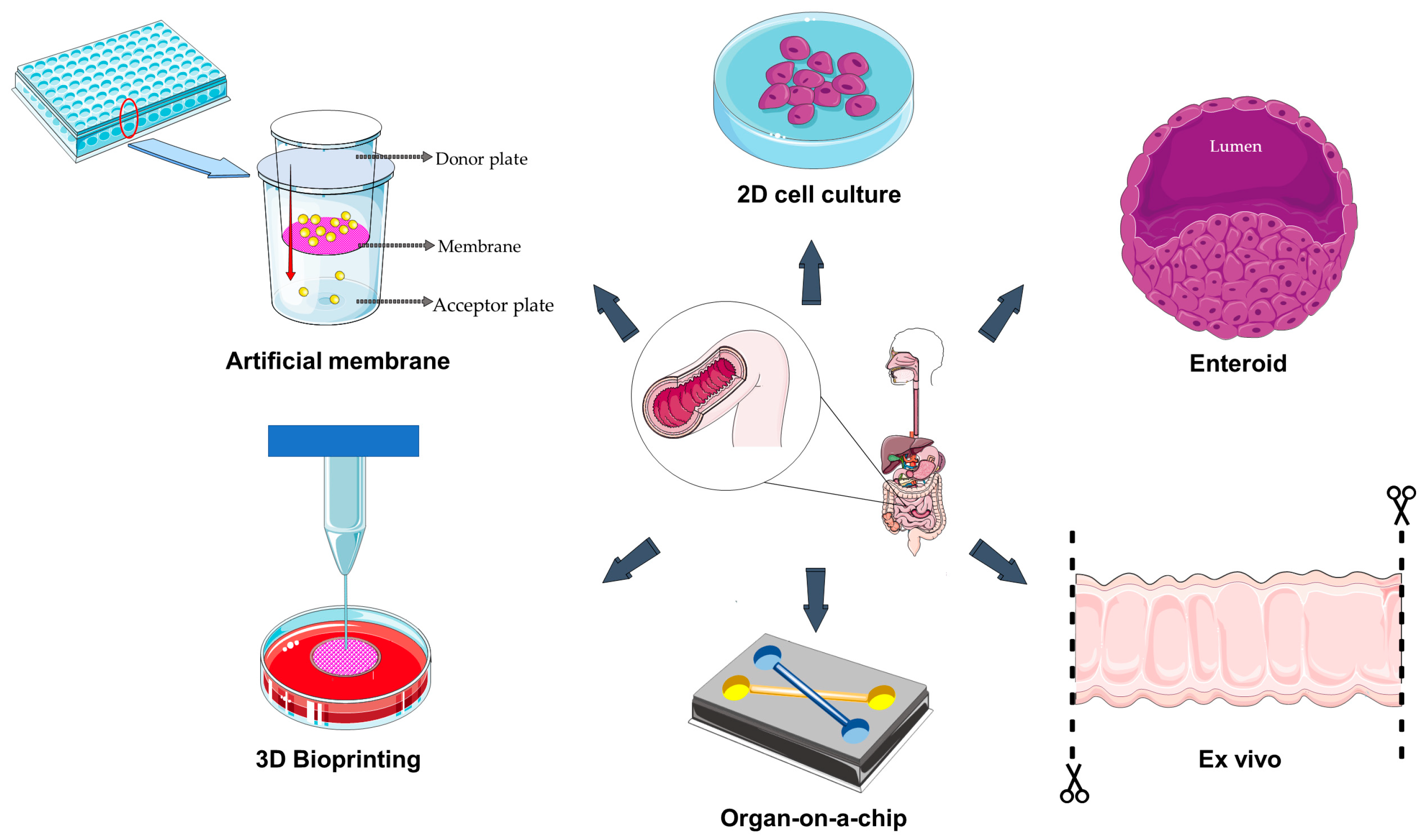
1. Introduction
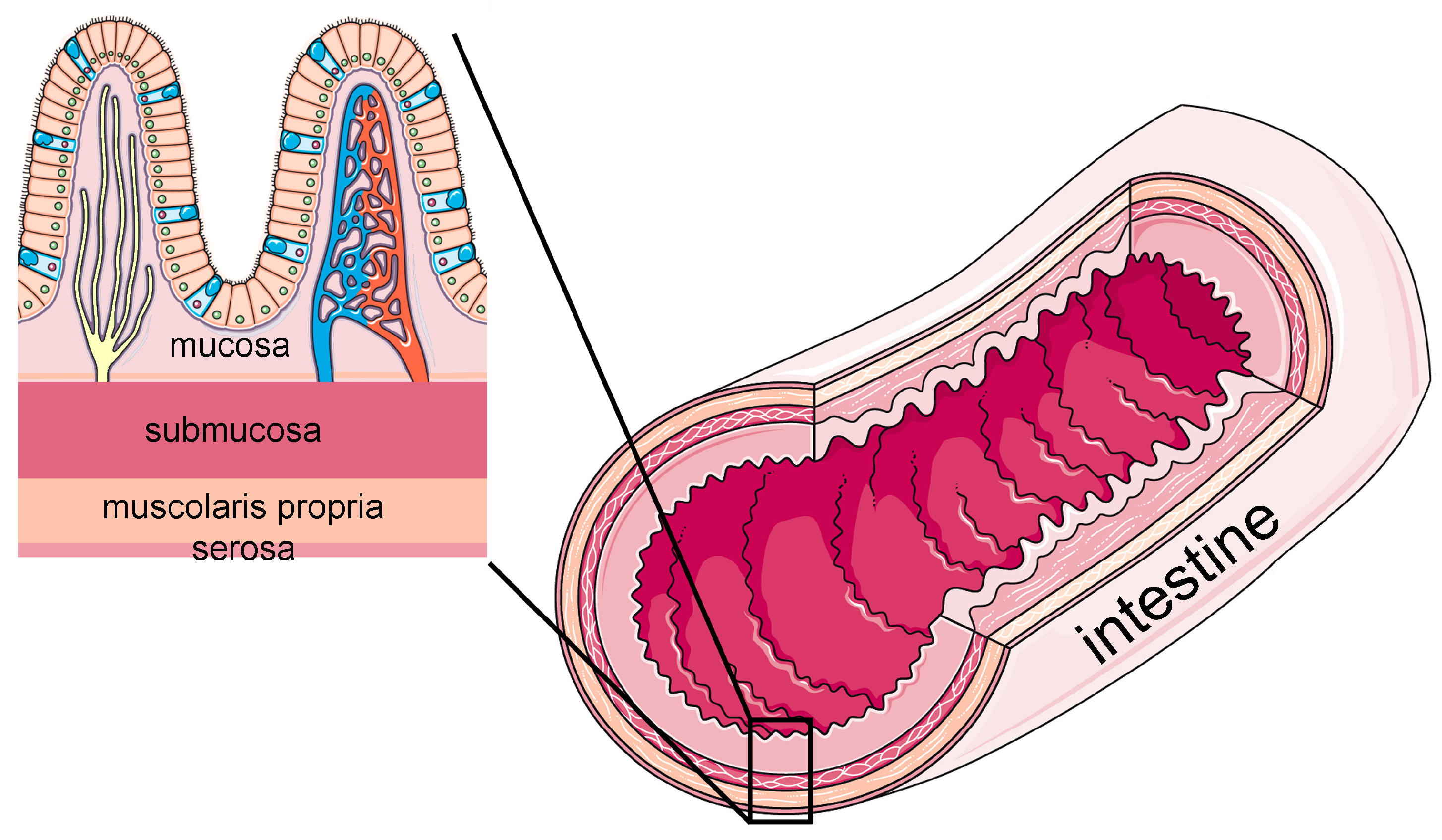
1.1. Structural and Functional Features of the Human Intestinal Barrier
1.2. Scope of the Review
2. Artificial Membranes
3. Two-Dimensional and Three-Dimensional Cell Cultures
4. Three-Dimensional Bioprinting
5. Organ-on-a-Chip
6. Ex Vivo
7. Future Perspectives
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Costa, J.; Ahluwalia, A. Advances and Current Challenges in Intestinal in vitro Model Engineering: A Digest. Front. Bioeng. Biotechnol. 2019, 7, 144. [Google Scholar] [CrossRef]
- Donkers, J.M.; Amirabadi, H.E.; Van de Steeg, E. Intestine-on-a-chip: Next level in vitro research model of the human intestine. Curr. Opin. Toxicol. 2021, 25, 6–14. [Google Scholar] [CrossRef]
- Hua, S. Advances in Oral Drug Delivery for Regional Targeting in the Gastrointestinal Tract—Influence of Physiological, Pathophysiological and Pharmaceutical Factors. Front. Pharmacol. 2020, 11, 524. [Google Scholar] [CrossRef] [PubMed]
- Drori, E.; Rahamim, V.; Patel, D.; Anker, Y.; Meir, S.; Uzan, G.; Somech, S.; Drori, C.; Tzadok, T.; Azagury, A. An In vitro Caco2-Based Model for Measuring Intestinal Bioadhesion Comparable to Ex vivo Models. Small Sci. 2024, 5, 2400461. [Google Scholar] [CrossRef] [PubMed]
- Moran, E.T. Anatomy, Microbes, and Fiber: Small Versus Large Intestine. J. Appl. Poult. Res. 2006, 15, 154–160. [Google Scholar] [CrossRef]
- Di Sabatino, A.; Santacroce, G.; Rossi, C.M.; Broglio, G.; Lenti, M.V. Role of mucosal immunity and epithelial-vascular barrier in modulating gut homeostasis. Intern. Emerg. Med. 2023, 18, 1635–1646. [Google Scholar] [CrossRef]
- Turner, H.L.; Turner, J.R. Good fences make good neighbors: Gastrointestinal mucosal structure. Gut Microbes 2010, 1, 22–29. [Google Scholar] [CrossRef][Green Version]
- Groschwitz, K.R.; Hogan, S.P. Intestinal barrier function: Molecular regulation and disease pathogenesis. J. Allergy Clin. Immunol. 2009, 124, 3–20, quiz 21–22. [Google Scholar] [CrossRef]
- Collins, J.T.; Nguyen, A.; Omole, A.E.; Badireddy, M. Anatomy, Abdomen and Pelvis, Small Intestine; StatPearls Publishing: Treasure Island, Finland, 2025. [Google Scholar]
- Ensari, A.; Marsh, M.N. Exploring the villus. Gastroenterol. Hepatol. Bed Bench. 2018, 11, 181–190. [Google Scholar]
- Schoultz, I.; Keita, Å.V. The Intestinal Barrier and Current Techniques for the Assessment of Gut Permeability. Cells 2020, 9, 1909. [Google Scholar] [CrossRef]
- Di Tommaso, N.; Santopaolo, F.; Gasbarrini, A.; Ponziani, F.R. The Gut-Vascular Barrier as a New Protagonist in Intestinal and Extraintestinal Diseases. Int. J. Mol. Sci. 2023, 24, 1470. [Google Scholar] [CrossRef]
- Cifarelli, V.; Eichmann, A. The Intestinal Lymphatic System: Functions and Metabolic Implications. Cell Mol. Gastroenterol. Hepatol. 2019, 7, 503–513. [Google Scholar] [CrossRef]
- Colombo, R.; Paolillo, M.; Papetti, A. A Dynamic In Vitro Model for Testing Intestinal Absorption of Different Vegetable Food Secondary Metabolites. Appl. Sci. 2023, 13, 5033. [Google Scholar] [CrossRef]
- Park, J.; Lee, H.; Park, K. Gastrointestinal tract and skin permeability of chemicals in consumer products using parallel artificial membrane permeability assay (PAMPA). Environ. Anal. Health Toxicol. 2021, 36, e2021021. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, M.; Tsuneishi, S.; Maeda, Y.; Masaoka, Y.; Sakuma, S.; Yamashita, S. A new in vitro system for evaluation of passive intestinal drug absorption: Establishment of a double artificial membrane permeation assay. Eur. J. Pharm. Biopharm. 2014, 88, 840–846. [Google Scholar] [CrossRef] [PubMed]
- Petit, C.; Bujard, A.; Skalicka-Woźniak, K.; Cretton, S.; Houriet, J.; Christen, P.; Carrupt, P.A.; Wolfender, J.L. Prediction of the Passive Intestinal Absorption of Medicinal Plant Extract Constituents with the Parallel Artificial Membrane Permeability Assay (PAMPA). Planta Med. 2016, 82, 424–431. [Google Scholar] [CrossRef]
- He, S.; Zhiti, A.; Barba-Bon, A.; Hennig, A.; Nau, W.M. Real-Time Parallel Artificial Membrane Permeability Assay Based on Supramolecular Fluorescent Artificial Receptors. Front. Chem. 2020, 8, 597927. [Google Scholar] [CrossRef]
- Dobričić, V.; Marodi, M.; Marković, B.; Tomašič, T.; Durcik, M.; Zidar, N.; Mašič, L.P.; Ilaš, J.; Kikelj, D.; Čudina, O. Estimation of passive gastrointestinal absorption of new dual DNA gyrase and topoisomerase IV inhibitors using PAMPA and biopartitioning micellar chromatography and quantitative structure-retention relationship analysis. J. Chromatogr. B Analyt Technol. Biomed. Life Sci. 2024, 1240, 124158. [Google Scholar] [CrossRef]
- Marelli, U.K.; Bezençon, J.; Puig, E.; Ernst, B.; Kessler, H. Enantiomeric cyclic peptides with different Caco-2 permeability suggest carrier-mediated transport. Chemistry 2015, 21, 8023–8027. [Google Scholar] [CrossRef]
- Berben, P.; Brouwers, J.; Augustijns, P. Assessment of Passive Intestinal Permeability Using an Artificial Membrane Insert System. J. Pharm. Sci. 2018, 107, 250–256. [Google Scholar] [CrossRef]
- Đanić, M.; Pavlović, N.; Stanimirov, B.; Lazarević, S.; Vukmirović, S.; Al-Salami, H.; Mikov, M. PAMPA model of gliclazide permeability: The impact of probiotic bacteria and bile acids. Eur. J. Pharm. Sci. 2021, 158, 105668. [Google Scholar] [CrossRef] [PubMed]
- Đanić, M.; Pavlović, N.; Dedić, N.; Zaklan, D.; Lazarević, S.; Stanimirov, B.; Mikov, M. Influence of probiotics and deoxycholate on azathioprine transport in the PAMPA model: Insights into pharmacomicrobiomics and interindividual variability in drug response. Front. Pharmacol. 2025, 16, 1608110. [Google Scholar] [CrossRef] [PubMed]
- Billat, P.A.; Roger, E.; Faure, S.; Lagarce, F. Models for drug absorption from the small intestine: Where are we and where are we going? Drug Discov. Today 2017, 22, 761–775. [Google Scholar] [CrossRef] [PubMed]
- An, Y.; Ji, C.; Zhang, H.; Jiang, Q.; Maitz, M.F.; Pan, J.; Luo, R.; Wang, Y. Engineered Cell Membrane Coating Technologies for Biomedical Applications: From Nanoscale to Macroscale. ACS Nano 2025, 19, 11517–11546. [Google Scholar] [CrossRef]
- Moyer, H.L.; Vergara, L.; Stephan, C.; Sakolish, C.; Lin, H.C.; Chiu, W.A.; Villenave, R.; Hewitt, P.; Ferguson, S.S.; Rusyn, I. Human Small Intestinal Tissue Models to Assess Barrier Permeability: Comparative Analysis of Caco-2 Cells, Jejunal and Duodenal Enteroid-Derived Cells, and EpiIntestinalTM Tissues in Membrane-Based Cultures with and Without Flow. Bioengineering 2025, 12, 809. [Google Scholar] [CrossRef]
- Eslami Amirabadi, H.; Donkers, J.M.; Wierenga, E.; Ingenhut, B.; Pieters, L.; Stevens, L.; Donkers, T.; Westerhout, J.; Masereeuw, R.; Bobeldijk-Pastorova, I.; et al. Intestinal explant barrier chip: Long-term intestinal absorption screening in a novel microphysiological system using tissue explants. Lab Chip 2022, 22, 326–342. [Google Scholar] [CrossRef]
- Navarro Del Hierro, J.; Reglero, G.; Martin, D. Chemical Characterization and Bioaccessibility of Bioactive Compounds from Saponin-Rich Extracts and Their Acid-Hydrolysates Obtained from Fenugreek and Quinoa. Foods 2020, 9, 1159. [Google Scholar] [CrossRef]
- Zhang, M.; Su, Y.; Li, J.; Chang, C.; Gu, L.; Yang, Y. Fabrication of phosphatidylcholine-EGCG nanoparticles with sustained release in simulated gastrointestinal digestion and their transcellular permeability in a Caco-2 monolayer model. Food Chem. 2023, 437 Pt 1, 137580. [Google Scholar] [CrossRef]
- Verhoeckx, K.; Cotter, P.; López-Expósito, I.; Kleiveland, C.; Lea, T.; Mackie, A.; Requena, T.; Swiatecka, D.; Wichers, H. The Impact of Food Bioactives on Health: In Vitro and Ex Vivo Models; Springer: Cham, Switzerland, 2015. [Google Scholar]
- Park, H.Y.; Yu, J.H. Mitigation effect of hesperidin on X-ray radiation-induced intestinal barrier dysfunction in Caco-2 cell monolayers. Food Chem. Toxicol. 2024, 186, 114549. [Google Scholar] [CrossRef]
- Bergmann, H.; Rogoll, D.; Scheppach, W.; Melcher, R.; Richling, E. The Ussing type chamber model to study the intestinal transport and modulation of specific tight-junction genes using a colonic cell line. Mol. Nutr. Food Res. 2009, 53, 1211–1225. [Google Scholar] [CrossRef]
- Streekstra, E.J.; Keuper-Navis, M.; van den Heuvel, J.J.M.W.; van den Broek, P.; Stommel, M.W.J.; Bervoets, S.; O’Gorman, L.; Greupink, R.; Russel, F.G.M.; van de Steeg, E.; et al. Human enteroid monolayers as a potential alternative for Ussing chamber and Caco-2 monolayers to study passive permeability and drug efflux. Eur. J. Pharm. Sci. 2024, 201, 106877. [Google Scholar] [CrossRef] [PubMed]
- Strugari, A.F.G.; Stan, M.S.; Gharbia, S.; Hermenean, A.; Dinischiotu, A. Characterization of Nanoparticle Intestinal Transport Using an In Vitro Co-Culture Model. Nanomaterials 2018, 9, 5. [Google Scholar] [CrossRef] [PubMed]
- Small, J. Modelling Shiga Toxin-Producing Escherichia coli Infection Using Intestinal Stem Cells. Ph.D. Thesis, University of Cincinnati, Cincinnati, OH, USA, 2023. [Google Scholar]
- Saxena, K.; Blutt, S.E.; Ettayebi, K.; Zeng, X.L.; Broughman, J.R.; Crawford, S.E.; Karandikar, U.C.; Sastri, N.P.; Conner, M.E.; Opekun, A.R.; et al. Human Intestinal Enteroids: A New Model To Study Human Rotavirus Infection, Host Restriction, and Pathophysiology. J. Virol. 2015, 90, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Parente, I.A.; Chiara, L.; Bertoni, S. Exploring the potential of human intestinal organoids: Applications, challenges, and future directions. Life Sci. 2024, 352, 122875. [Google Scholar] [CrossRef]
- Sharma, A.; Lee, J.; Fonseca, A.G.; Moshensky, A.; Kothari, T.; Sayed, I.M.; Ibeawuchi, S.R.; Pranadinata, R.F.; Ear, J.; Sahoo, D.; et al. E-cigarettes compromise the gut barrier and trigger inflammation. iScience 2021, 24, 102035. [Google Scholar] [CrossRef]
- Meir, M.; Salm, J.; Fey, C.; Schweinlin, M.; Kollmann, C.; Kannapin, F.; Germer, C.T.; Waschke, J.; Beck, C.; Burkard, N.; et al. Enteroids Generated from Patients with Severe Inflammation in Crohn’s Disease Maintain Alterations of Junctional Proteins. J. Crohns Colitis 2020, 14, 1473–1487. [Google Scholar] [CrossRef]
- Kourula, S.; Derksen, M.; Jardi, F.; Jonkers, S.; van Heerden, M.; Verboven, P.; Theuns, V.; Van Asten, S.; Huybrechts, T.; Kunze, A.; et al. Intestinal organoids as an in vitro platform to characterize disposition, metabolism, and safety profile of small molecules. Eur. J. Pharm. Sci. 2023, 188, 106481. [Google Scholar] [CrossRef]
- Min, S.; Kim, S.; Cho, S.W. Gastrointestinal tract modeling using organoids engineered with cellular and microbiota niches. Exp. Mol. Med. 2020, 52, 227–237. [Google Scholar] [CrossRef]
- Haga, K.; Ettayebi, K.; Tenge, V.R.; Karandikar, U.C.; Lewis, M.A.; Lin, S.C.; Neill, F.H.; Ayyar, B.V.; Zeng, X.L.; Larson, G.; et al. Genetic Manipulation of Human Intestinal Enteroids Demonstrates the Necessity of a Functional Fucosyltransferase 2 Gene for Secretor-Dependent Human Norovirus Infection. mBio 2020, 11, e00251-20. [Google Scholar] [CrossRef]
- Kasendra, M.; Tovaglieri, A.; Sontheimer-Phelps, A.; Jalili-Firoozinezhad, S.; Bein, A.; Chalkiadaki, A.; Scholl, W.; Zhang, C.; Rickner, H.; Richmond, C.A.; et al. Development of a primary human Small Intestine-on-a-Chip using biopsy-derived organoids. Sci. Rep. 2018, 8, 2871. [Google Scholar] [CrossRef]
- Hospodiuk, M.; Dey, M.; Sosnoski, D.; Ozbolat, I.T. The bioink: A comprehensive review on bioprintable materials. Biotechnol. Adv. 2017, 35, 217–239. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Gao, L.; Ma, L.; Luo, Y.; Yang, H.; Cui, Z. 3D Bioprinting: A Novel Avenue for Manufacturing Tissues and Organs. Engineering 2019, 5, 777–794. [Google Scholar] [CrossRef]
- Macedo, M.H.; Torras, N.; García-Díaz, M.; Barrias, C.; Sarmento, B.; Martínez, E. The shape of our gut: Dissecting its impact on drug absorption in a 3D bioprinted intestinal model. Biomater. Adv. 2023, 153, 213564. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhou, W.; Roh, T.; Estes, M.K.; Kaplan, D.L. In vitro enteroid-derived three-dimensional tissue model of human small intestinal epithelium with innate immune responses. PLoS ONE 2017, 12, e0187880. [Google Scholar] [CrossRef]
- Madden, L.R.; Nguyen, T.V.; Garcia-Mojica, S.; Shah, V.; Le, A.V.; Peier, A.; Visconti, R.; Parker, E.M.; Presnell, S.C.; Nguyen, D.G.; et al. Bioprinted 3D Primary Human Intestinal Tissues Model Aspects of Native Physiology and ADME/Tox Functions. iScience 2018, 2, 156–167. [Google Scholar] [CrossRef]
- Tofani, L.B.; Avelino, T.M.; de Azevedo, R.J.; Elias, G.B.; Ganzerla, M.D.; Terra, M.F.; Rodrigues, V.K.T.; Rabelo, R.S.; Harb, S.V.; Figueira, A.C.M. Biofabricated 3D Intestinal Models as an Alternative to Animal-Based Approaches for Drug Toxicity Assays. Tissue Eng. Regen. Med. 2025, 22, 181–194. [Google Scholar] [CrossRef]
- Li, Y.; Cheng, S.; Shi, H.; Yuan, R.; Gao, C.; Wang, Y.; Zhang, Z.; Deng, Z.; Huang, J. 3D embedded bioprinting of large-scale intestine with complex structural organization and blood capillaries. Biofabrication 2024, 16, 045001. [Google Scholar] [CrossRef]
- Tripathi, S.; Mandal, S.S.; Bauri, S.; Maiti, P. 3D bioprinting and its innovative approach for biomedical applications. MedComm 2022, 4, e194. [Google Scholar] [CrossRef]
- Hewes, S.A.; Wilson, R.L.; Estes, M.K.; Shroyer, N.F.; Blutt, S.E.; Grande-Allen, K.J. In Vitro Models of the Small Intestine: Engineering Challenges and Engineering Solutions. Tissue Eng. Part B Rev. 2020, 26, 313–326. [Google Scholar] [CrossRef]
- Creff, J.; Courson, R.; Mangeat, T.; Foncy, J.; Souleille, S.; Thibault, C.; Besson, A.; Malaquin, L. Fabrication of 3D scaffolds reproducing intestinal epithelium topography by high-resolution 3D stereolithography. Biomaterials 2019, 221, 119404. [Google Scholar] [CrossRef]
- Rothbauer, M.; Rosser, J.M.; Zirath, H.; Ertl, P. Tomorrow today: Organ-on-a-chip advances towards clinically relevant pharmaceutical and medical in vitro models. Curr. Opin. Biotechnol. 2019, 55, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Özkan, A.; LoGrande, N.T.; Feitor, J.F.; Goyal, G.; Ingber, D.E. Intestinal organ chips for disease modelling and personalized medicine. Nat. Rev. Gastroenterol. Hepatol. 2024, 21, 751–773. [Google Scholar] [CrossRef] [PubMed]
- Fois, C.A.M.; Schindeler, A.; Valtchev, P.; Dehghani, F. Dynamic flow and shear stress as key parameters for intestinal cells morphology and polarization in an organ-on-a-chip model. Biomed. Microdevices 2021, 23, 55. [Google Scholar] [CrossRef] [PubMed]
- Cherwin, A.E.; Templeton, H.N.; Ehrlich, A.T.; Patlin, B.H.; Henry, C.S.; Tobet, S.A. Microfluidic organotypic device to test intestinal mucosal barrier permeability ex vivo. Lab Chip 2023, 23, 4126–4133. [Google Scholar] [CrossRef]
- Morelli, M.; Cabezuelo Rodríguez, M.; Queiroz, K. A high-throughput gut-on-chip platform to study the epithelial responses to enterotoxins. Sci. Rep. 2024, 14, 5797. [Google Scholar] [CrossRef]
- Yin, J.; Sunuwar, L.; Kasendra, M.; Yu, H.; Tse, C.M.; Talbot, C.C., Jr.; Boronina, T.; Cole, R.; Karalis, K.; Donowitz, M. Fluid shear stress enhances differentiation of jejunal human enteroids in Intestine-Chip. Am. J. Physiol. Gastrointest. Liver Physiol. 2021, 320, G258–G271. [Google Scholar] [CrossRef]
- Gleeson, J.P.; Zhang, S.Y.; Subelzu, N.; Ling, J.; Nissley, B.; Ong, W.; Nofsinger, R.; Kesisoglou, F. Head-to-Head Comparison of Caco-2 Transwell and Gut-on-a-Chip Models for Assessing Oral Peptide Formulations. Mol. Pharm. 2024, 21, 3880–3888. [Google Scholar] [CrossRef]
- Beaurivage, C.; Kanapeckaite, A.; Loomans, C.; Erdmann, K.S.; Stallen, J.; Janssen, R.A.J. Development of a human primary gut-on-a-chip to model inflammatory processes. Sci. Rep. 2020, 10, 21475. [Google Scholar] [CrossRef]
- Marr, E.E.; Mulhern, T.J.; Welch, M.; Keegan, P.; Caballero-Franco, C.; Johnson, B.G.; Kasaian, M.; Azizgolshani, H.; Petrie, T.; Charest, J.; et al. A platform to reproducibly evaluate human colon permeability and damage. Sci. Rep. 2023, 13, 8922. [Google Scholar] [CrossRef]
- Wang, X.; Zhu, Y.; Cheng, Z.; Zhang, C.; Liao, Y.; Liu, B.; Zhang, D.; Li, Z.; Fang, Y. Emerging microfluidic gut-on-a-chip systems for drug development. Acta Biomater. 2024, 188, 48–64. [Google Scholar] [CrossRef]
- Li, X.G.; Chen, M.X.; Zhao, S.Q.; Wang, X.Q. Intestinal Models for Personalized Medicine: From Conventional Models to Microfluidic Primary Intestine-on-a-chip. Stem Cell Rev. Rep. 2022, 18, 2137–2151. [Google Scholar] [CrossRef]
- Wheeler, A.E.; Stoeger, V.; Owens, R.M. Lab-on-chip technologies for exploring the gut-immune axis in metabolic disease. Lab Chip 2024, 24, 1266–1292. [Google Scholar] [CrossRef]
- Pimenta, J.; Ribeiro, R.; Almeida, R.; Costa, P.F.; da Silva, M.A.; Pereira, B. Organ-on-Chip Approaches for Intestinal 3D In Vitro Modeling. Cell Mol. Gastroenterol. Hepatol. 2022, 13, 351–367. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.H.; Wiseman, G. The use of sacs of everted small intestine for the study of the transference of substances from the mucosal to the serosal surface. J. Physiol. 1954, 123, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Carrillo, J.C.; Penman, M.G.; Manton, J.; Fioravanzo, E.; Powrie, R.H.; Elcombe, C.R.; Borsboom-Patel, T.; Tian, Y.; Shen, H.; et al. Assessment of the Intestinal Absorption of Higher Olefins by the Everted Gut Sac Model in Combination with In Silico New Approach Methodologies. Chem. Res. Toxicol. 2022, 35, 1383–1392. [Google Scholar] [CrossRef] [PubMed]
- Doppalapudi, S.; Suryadevara, V.; Ramineni, S.R.; Chadalavada, A.K. Assessment of the Effect of Bromelain on Glucose Uptake Using Everted Gut Sac Technique. Pharmacophore 2023, 14, 33–39. [Google Scholar] [CrossRef]
- Bhat, W.H.; Ahmed, S.S. Evaluation of in-vitro antidiabetic activity using silver nanoparticles of Galinsoga parviflora leaf extract. Int. J. Basic Clin. Pharmacol. 2024, 13, 629–635. [Google Scholar] [CrossRef]
- Pol, K.D.; Jagtap, P.N.; Musle, S.K.; Bobade, S.S.; Kadam, A.M.; More, V.P.; Deshmukh, P.P.; Kunjir, A.M. Effect of orange peel extract on intestinal absorption of aspirin using everted sac technique. J. Adv. Sci. Res. 2023, 14, 51–56. [Google Scholar] [CrossRef]
- Joshi, A.; Soni, A.; Acharya, S. In vitro models and ex vivo systems used in inflammatory bowel disease. Vitr. Models 2022, 1, 213–227. [Google Scholar] [CrossRef]
- Guan, C.; Yang, Y.; Tian, D.; Jiang, Z.; Zhang, H.; Li, Y.; Yan, J.; Zhang, C.; Chen, C.; Zhang, J.; et al. Evaluation of an Ussing Chamber System Equipped with Rat Intestinal Tissues to Predict Intestinal Absorption and Metabolism in Humans. Eur. J. Drug Metab. Pharmacokinet. 2022, 47, 639–652. [Google Scholar] [CrossRef]
- Taebnia, N.; Römling, U.; Lauschke, V.M. In vitro and ex vivo modeling of enteric bacterial infections. Gut Microbes 2023, 15, 2158034. [Google Scholar] [CrossRef] [PubMed]
- Duarte, V.; Mallmann, A.O.; Liberalesso, D.; Simões, C.T.; Gressler, L.T.; Molossi, F.A.; Bracarense, A.P.F.R.L.; Mallmann, C.A. Impact of deoxynivalenol on intestinal explants of broiler chickens: An ex vivo model to assess antimycotoxins additives. Toxicon 2021, 200, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Streekstra, E.J.; Kiss, M.; van den Heuvel, J.; Nicolaï, J.; van den Broek, P.; Botden, S.M.B.I.; Stommel, M.W.J.; van Rijssel, L.; Ungell, A.L.; van de Steeg, E.; et al. A proof of concept using the Ussing chamber methodology to study pediatric intestinal drug transport and age-dependent differences in absorption. Clin. Transl. Sci. 2022, 15, 2392–2402. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; van Weerden, W.M.; de Ridder, C.M.A.; Erkens-Schulze, S.; Schönfeld, E.; Meijer, T.G.; Kanaar, R.; van Gent, D.C.; Nonnekens, J. Ex vivo treatment of prostate tumor tissue recapitulates in vivo therapy response. Prostate 2019, 79, 390–402. [Google Scholar] [CrossRef]
- Ng, K.W.; Pearton, M.; Coulman, S.; Anstey, A.; Gateley, C.; Morrissey, A.; Allender, C.; Birchall, J. Development of an ex vivo human skin model for intradermal vaccination: Tissue viability and Langerhans cell behaviour. Vaccine 2009, 27, 5948–5955. [Google Scholar] [CrossRef]
- Costa, C.M.; de Carvalho, N.M.; de Oliveira, D.L.; Madureira, A.R. A Critical Review on In Vitro and Ex Vivo Models of the Intestinal Epithelium of Humans and Monogastric Animals. Gastrointest. Disord. 2024, 6, 337–358. [Google Scholar] [CrossRef]
- Alam, M.A.; Al-Jenoobi, F.I.; Al-Mohizea, A.M. Everted gut sac model as a tool in pharmaceutical research: Limitations and applications. J. Pharm. Pharmacol. 2012, 64, 326–336. [Google Scholar] [CrossRef]
- Mehta, K.; Maass, C.; Cucurull-Sanchez, L.; Pichardo-Almarza, C.; Subramanian, K.; Androulakis, I.P.; Gobburu, J.; Schaller, S.; Sherwin, C.M. Modernizing Preclinical Drug Development: The Role of New Approach Methodologies. ACS Pharmacol. Transl. Sci. 2025, 8, 1513–1525. [Google Scholar] [CrossRef]
- Jalili-Firoozinezhad, S.; Gazzaniga, F.S.; Calamari, E.L.; Camacho, D.M.; Fadel, C.W.; Bein, A.; Swenor, B.; Nestor, B.; Cronce, M.J.; Tovaglieri, A.; et al. A complex human gut microbiome cultured in an anaerobic intestine-on-a-chip. Nat. Biomed. Eng. 2019, 3, 520–531, Erratum in Nat. Biomed. Eng. 2019, 3, 583. [Google Scholar] [CrossRef]
- Almalla, A.; Alzain, N.; Elomaa, L.; Richter, F.; Scholz, J.; Lindner, M.; Siegmund, B.; Weinhart, M. Hydrogel-Integrated Millifluidic Systems: Advancing the Fabrication of Mucus-Producing Human Intestinal Models. Cells 2024, 13, 1080. [Google Scholar] [CrossRef]
- Shi, H.; Kowalczewski, A.; Vu, D.; Liu, X.; Salekin, A.; Yang, H.; Ma, Z. Organoid intelligence: Integration of organoid technology and artificial intelligence in the new era of in vitro models. Med. Nov. Technol. Devices 2024, 21, 100276. [Google Scholar] [CrossRef]
| Experimental Model | Investigated Molecules | Applications | Results | References |
|---|---|---|---|---|
| PAMPA | parabens, bisphenols, isothiazolinones, phthalates | To test the permeability of chemical compounds | Log P is a key factor in permeability, but also molecular weight, pKa, chemical structure, and interactions with membrane lipids also influence permeation | [15] |
| PAMPA | DNA gyrase and topoisomerase IV inhibitors | To estimate the passive gastrointestinal absorption of 13 DNA gyrase inhibitor compounds | PAMPA showed low permeability for acidic compounds and high permeability for neutral and more lipophilic compounds | [19] |
| real-time PAMPA | 1,2-dioleoyl-sn-glycero-3-phosphocholine (DOPC), DOPC + stearic acid | To propose a new RT-PAMPA method for real-time measurement of passive drug permeability using fluorescent artificial receptors | The method quickly distinguishes drugs with different permeabilities, is compatible with various solvents and membranes, and improves efficiency compared to traditional PAMPA | [18] |
| PAMPA and Caco-2 cells | polar N-methylated cyclic hexaalanines, lipophilic tri-N-methylated Veber–Hirschmann peptides, lipophilic peptide | To study pairs of enantiomeric peptides of 3 polar peptides and 2 lipophilic peptides to investigate the possible involvement of stereospecific biological transporters | The spatial structure of peptides has a significant influence on their intestinal permeability through carrier-mediated transporters | [20] |
| AMI-system and Caco-2 cells | Carvedilol, felodipine, fenofibrate, ibuprofen, indomethacin, itraconazole, JNJ39393406, ketoconazole, metroprolol, naproxen, piroxicam, posoconazole, tadalafil, zafirlukast | To evaluate AMI as a rapid, cost-effective, and simple alternative to the Caco-2 cell model for estimating the passive intestinal permeability of poorly soluble drugs | The AMI system demonstrated a high correlation with the Caco-2 model in assessing passive intestinal permeability, representing a rapid, cost-effective, and simple alternative, although it does not replicate active transport or the mucus barrier | [21] |
| DAMPA | Atenolol, carbamazepine, cimetidine, ketoprofen, metoprolol, piroxicam, propranolol, acyclovir, alprenolol, antipyrine, chlorotiazide, famotidine, methotrexate, nadolol, pindolol, salicyclic acid, sulfas atrazine, sulpiride, terbut aline, warfarin | To develop and validate the DAMPA method for predicting human intestinal drug permeability in vitro | DAMPA showed a strong correlation with human data representing an efficient and accurate alternative to traditional cell-based models | [16] |
| PAMPA + probiotic bacteria and bile acids | gliclazide | To estimate the influence of bile acids and intestinal bacteria on intestinal absorption of gliclazide | pH, probiotics, and bile acids affect the permeability and bioavailability of gliclazide | [22] |
| PAMPA + probiotic bacteria and deoxycholate | azathioprine | To evaluate the permeability of azathioprine at different pH levels, both alone and in combination with deoxycholic acid and probiotics | Azathioprine shows higher permeability at acidic pH; probiotics increase its permeability but reduce its overall amount, while deoxycholic acid decreases permeability | [23] |
| Experimental Model | Investigated Molecules | Applications | Cell Source | Culture Duration | Results | References |
|---|---|---|---|---|---|---|
| Transwell membrane (cell monolayer) | Epigallocatechin gallate (EGCG) | To develop phosphatidylcholine-based nanoparticles to enhance the oral bioavailability of EGCG and investigate its intestinal absorption using Caco-2 cell models | Human | Up to 72 h | The nanoparticles improved digestive stability, promoted cellular uptake, and inhibited efflux, thereby enhancing overall EGCG absorption | [29] |
| Ussing chamber | Hesperidin | To evaluate whether pretreatment with hesperidin mitigates X-ray (2 Gy)-induced damage to intestinal barrier function | Human | Up to 72 h | Hesperidin pre-treatment protected intestinal barrier integrity from X-ray damage by improving cell survival, reducing permeability, and restoring tight junction proteins | [31] |
| Ussing chamber | Polyphenols | To study the transport, metabolism, and effect of apple polyphenols on the intestinal barrier, particularly on tight junctions and the transepithelial resistance of cells | Human | Up to 24 h | Apple polyphenols improve the intestinal barrier by increasing transepithelial resistance and stimulating tight junction proteins, also promoting epithelial damage repair | [32] |
| Transwell membrane (co-culture) | Silicon quantum dots and iron oxide nanoparticles | To develop an in vitro intestinal model to study nanoparticle transport | Human | Up to 21 days | The nanoparticles did not cross the model due to aggregation | [34] |
| Enteroid cell model | Escherichia coli | To develop an in vitro human intestinal model to analyze infection by E. coli O157:H7 and compare it with probiotic and commensal strains | Human | Up to 15.5 days | The model remained intact with apical saline. Non-pathogenic E. coli strains did not damage the epithelium, while E. coli O157:H7 caused loss of barrier integrity, strong bacterial adhesion, epithelial damage, and bacterial translocation after 24–36 h | [35] |
| Enteroid cell model | E-cigarette | To analyze the effects of chronic exposure to e-cigarette aerosols (with or without nicotine) on the intestinal barrier, using murine models and human organoids | Murine and human | Up to 24 h | Prolonged use of e-cigarettes damages the intestinal barrier, increases inflammation, and heightens susceptibility to bacterial infections | [38] |
| Enteroids from donor tissue | Ketoprofen, valacyclovir, propranolol, digoxin, atenolol | To evaluate the use of human intestinal organoids as in vitro models for studying drug absorption, metabolism, and intestinal toxicity | Murine and human | Up to 21 days | Intestinal organoids represent an effective and translational model for absorption, distribution, metabolism, and excretion, and intestinal safety studies | [40] |
| Enteroid cell model | Fucosyltransferase 2 (FUT2) gene | Study the role of the FUT2 gene in susceptibility to human norovirus infection using genetically modified human intestinal organoids | Human | Up to 5 days | FUT2 is necessary and sufficient to enable human norovirus to infect intestinal cells, affecting viral binding and replication | [42] |
| Experimental Model | Investigated Molecules | Applications | Results | References |
|---|---|---|---|---|
| 3D biopinted intestine model enriched with human intestinal fibroblasts. Intestinal epithelial cells (Caco-2 and HT29-MTX) | metoprolol, atenolol, colchicine | To create a 3D in vitro model of human small intestine that includes villus architecture and stromal compartment to better study drug absorption | The 3D model exhibits barrier and permeability functions more similar to the human intestine compared to flat models | [46] |
| 3D bioprinted intestine model with human primary intestinal epithelial cells and myofibroblasts | digoxin, topotecan, lucifer yellow, propranolol, mitoxantrone, indomethacin | To develop a 3D human small intestine model using primary cells to improve preclinical prediction of drug absorption, metabolism, transport, and toxicity | The model replicates intestinal architecture and function with physiological barrier properties, active expression of metabolic enzymes and transporters, and realistic responses to drugs and toxins | [48] |
| 3D bioprinted intestine model enriched with HT-29 and Caco-2 cells | ibuprofen | To create a 3D bioprinted intestinal model for preclinical drug testing studies | The bioprinted model containing fibroblasts replicates more accurately the human intestine compared to a 3D model without fibroblasts and traditional 2D models | [49] |
| 3D bioprinted intestine-like scaffold with large tube-like and ring folds enriched with Caco-2 cells and human umbilical vein endothelial cells | FITC-dextrans (4 kDa and 70 kDa) | To develop a realistic and large-scale 3D in vitro intestinal model that faithfully reproduces the complex anatomical structure of the human intestine, including hollow lumen, folds, crypts, villi, microvilli, and capillary network | A vascularized intestinal tissue populated with epithelial and endothelial cells, and capable of mimicking the intestinal barrier was created | [50] |
| Experimental Model | Investigated Molecules | Applications | Cell Source | Culture Duration | Results | References |
|---|---|---|---|---|---|---|
| OrganoReady® Colon Caco-2 | Nigericin, patulin, ochratoxin A, mellitin | To evaluate the effects of different enterotoxins on the intestinal epithelial barrier | Human | Up to 8 days before toxin exposure | The model showed greater sensitivity compared to conventional models, allowing the differentiation of the toxins’ pathogenic mechanisms in terms of permeability, cytotoxicity, and cell morphology | [58] |
| Primary human intestine chip | Lucifer yellow | To provide a more realistic and functional tool for studying intestinal physiology, cellular interactions, intestinal diseases, pharmacology, and personalized medicine | Human | Up to 12 days | The chip recapitulates key structures such as intestinal villi, maintains a functional epithelial barrier, and reproduces multilineage cell differentiation; it provides a more sensitive and relevant system compared to 2D models | [43] |
| Emulate Bio, Inc. | Sodium caprate and monolaurate with dextran, insulin and octreotide | To evaluate the effectiveness of intestinal permeation enhancers to improve the oral delivery of peptide drugs | Human | Up to 21 days | The model shows more realistic permeability and greater resistance to bile salts compared to a transwell model, making it a useful tool for the development of oral peptide drugs | [60] |
| PREDICT96 | IFN-γ, TNF-α | To study the colonic epithelial barrier, assessing damage and recovery in response to inflammatory cytokines relevant to inflammatory bowel disease | Human | Up to 14 days | Exposure to the inflammatory cytokines TNF-α and IFN-γ induced dose-dependent barrier damage, with variations in sensitivity among donors | [62] |
| Experimental Model | Investigated Molecules | Applications | Results | References |
|---|---|---|---|---|
| Chicken everted intestine | Silver nanoparticles from Galinsoga parviflora | To evaluate the in vitro antidiabetic activity of silver nanoparticles from G. parviflora by analyzing their inhibition of α-amylase and α-glucosidase, as well as glucose uptake using the everted gut sac method with chicken ileum | Silver nanoparticles of G. parviflora showed strong in vitro antidiabetic activity, outperforming Acarbose in inhibiting α-amylase and α-glucosidase enzymes, and reducing short-term glucose absorption, indicating potential for managing postprandial blood glucose | [70] |
| Goat everted intestine | Citrus aurantium dulcis peel extract with aspirin | To evaluate how orange peel extract can improve the intestinal absorption of aspirin | The flavonoids present in orange peel extract enhanced its ability to improve aspirin absorption | [71] |
| Chicken intestine explants in Ussing chambers | Deoxynivalenol (DON) | To study the toxic effects of the mycotoxin DON on the intestinal barrier and to evaluate the efficacy of an antimycotoxin additive in protecting it | The mycotoxin DON rapidly damaged the integrity of the intestinal epithelium, and the tested antimycotoxin additive mitigated these damages by reducing cytoplasmic vacuolization and apoptosis | [75] |
| Human intestine explants in Ussing chambers | Talinolol, rosuvastatin, enalaprilat, propranolol | To study intestinal drug absorption in children and compare it to adults | Passive permeability is similar to that of adults, while active transport may be reduced in younger children | [76] |
| Mouse intestine explants in microfluidic chip | Collagen-1, claudin-1 | To evaluate the alterations induced by bacterial collagenase on the integrity and permeability of the intestinal barrier | Collagenase increases intestinal permeability, damages tight junction proteins, alters collagen structure, and modifies goblet cells by reducing mucus production, thereby compromising the barrier | [57] |
| In vitro Models | Advantages | Limitations | Primary Applications |
|---|---|---|---|
| Artificial membranes | Inexpensive, easy to use, and effective for high-throughput screening | Lack living cells, do not reproduce tissue complexity, and paracellular and active transports | Study of passive transport and molecular diffusion |
| 2D cultures | Easy to culture and manipulate, relative low cost, and good reproducibility | Lack 3D structure and interactions between the different intestinal cell types | Toxicity testing and absorption studies |
| 3D cultures | Better representation of tissue structure and interactions between different cell types than 2D cultures | More costly, generally with an enclosed luminal space, limited scalability, reproducibility, and long-term culture | Toxicity testing and absorption studies in a barrier with a more realistic functionality |
| 3D Bioprinting | Precise cell–matrix arrangement and possibility to develop personalized models | Expensive, complex technology that requires specialized operators | Reconstruction of complex tissues, tissue regeneration, drug testing, toxicity, and microbiota interactions |
| Organ-on-a-chip | Microfluidic environment with all the derived physical stimuli, real-time monitoring | Technical complexity, high costs and lack of immune cells | Assessment of safety, efficacy, and absorption of drugs and active compounds |
| Ex vivo | Original architecture very close to biological reality | Limited lifespan and high inter-donor variability | Pharmacological and physiological studies on human or animal tissues |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galvan, A.; Guidorizzi, E.; Carton, F.; Malatesta, M.; Calderan, L. In Vitro and Ex Vivo Models to Study Molecular Trafficking Across the Human Intestinal Barrier. Int. J. Mol. Sci. 2025, 26, 10535. https://doi.org/10.3390/ijms262110535
Galvan A, Guidorizzi E, Carton F, Malatesta M, Calderan L. In Vitro and Ex Vivo Models to Study Molecular Trafficking Across the Human Intestinal Barrier. International Journal of Molecular Sciences. 2025; 26(21):10535. https://doi.org/10.3390/ijms262110535
Chicago/Turabian StyleGalvan, Andrea, Elsa Guidorizzi, Flavia Carton, Manuela Malatesta, and Laura Calderan. 2025. "In Vitro and Ex Vivo Models to Study Molecular Trafficking Across the Human Intestinal Barrier" International Journal of Molecular Sciences 26, no. 21: 10535. https://doi.org/10.3390/ijms262110535
APA StyleGalvan, A., Guidorizzi, E., Carton, F., Malatesta, M., & Calderan, L. (2025). In Vitro and Ex Vivo Models to Study Molecular Trafficking Across the Human Intestinal Barrier. International Journal of Molecular Sciences, 26(21), 10535. https://doi.org/10.3390/ijms262110535









