CDK4/6 Inhibitors in Breast Cancer—Who Should Receive Them?
Abstract
Author Contributions
Funding
Conflicts of Interest
References
- Klein, M.E.; Kovatcheva, M.; Davis, L.E.; Tap, W.D.; Koff, A. CDK4/6 Inhibitors: The Mechanism of Action May Not Be as Simple as Once Thought. Cancer Cell 2018, 34, 9–20. [Google Scholar] [CrossRef]
- Sherr, C.J.; Beach, D.; Shapiro, G.I. Targeting CDK4 and CDK6: From Discovery to Therapy. Cancer Discov. 2016, 6, 353–367. [Google Scholar] [CrossRef]
- Feng, Q.; O’Malley, B.W. Nuclear receptor modulation—Role of coregulators in selective estrogen receptor modulator (SERM) actions. Steroids 2014, 90, 39–43. [Google Scholar] [CrossRef]
- Shang, Y.; Hu, X.; DiRenzo, J.; Lazar, M.A.; Brown, M. Cofactor dynamics and sufficiency in estrogen receptor-regulated transcription. Cell 2000, 103, 843–852. [Google Scholar] [CrossRef]
- Cossetti, R.J.; Tyldesley, S.K.; Speers, C.H.; Zheng, Y.; Gelmon, K.A. Comparison of breast cancer recurrence and outcome patterns between patients treated from 1986 to 1992 and from 2004 to 2008. J. Clin. Oncol. 2015, 33, 65–73. [Google Scholar] [CrossRef]
- Global Burden of Disease Cancer Collaboration; Fitzmaurice, C.; Akinyemiju, T.F.; Al Lami, F.H.; Alam, T.; Alizadeh-Navaei, R.; Allen, C.; Alsharif, U.; Alvis-Guzman, N.; Amini, E.; et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2016: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2018, 4, 1553–1568. [Google Scholar] [CrossRef] [PubMed]
- Finn, R.S.; Dering, J.; Conklin, D.; Kalous, O.; Cohen, D.J.; Desai, A.J.; Ginther, C.; Atefi, M.; Chen, I.; Fowst, C.; et al. PD 0332991, a selective cyclin D kinase 4/6 inhibitor, preferentially inhibits proliferation of luminal estrogen receptor-positive human breast cancer cell lines in vitro. Breast Cancer Res. 2009, 11, R77. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, C.C.; Clarke, R.; Goetz, M.P.; Robertson, J. Cyclin-Dependent Kinase 4/6 Inhibitors for Treatment of Hormone Receptor-Positive, ERBB2-Negative Breast Cancer: A Review. JAMA Oncol. 2023, 9, 1273–1282. [Google Scholar] [CrossRef] [PubMed]
- Masurkar, P.P.; Damgacioglu, H.; Deshmukh, A.A.; Trivedi, M.V. Cost Effectiveness of CDK4/6 Inhibitors in the First-Line Treatment of HR+/HER2- Metastatic Breast Cancer in Postmenopausal Women in the USA. Pharmacoeconomics 2023, 41, 709–718. [Google Scholar] [CrossRef]
- Tannock, I.F.; Khan, Q.J.; Fojo, T. Why We Do Not Recommend That Women With Breast Cancer Receive Adjuvant Treatment With a CDK4/6 Inhibitor. J. Clin. Oncol. 2025, 43, 2456–2460. [Google Scholar] [CrossRef]
- Asghar, U.S.; Kanani, R.; Roylance, R.; Mittnacht, S. Systematic Review of Molecular Biomarkers Predictive of Resistance to CDK4/6 Inhibition in Metastatic Breast Cancer. JCO Precis. Oncol. 2022, 6, e2100002. [Google Scholar] [CrossRef]
- O’Leary, B.; Cutts, R.J.; Liu, Y.; Hrebien, S.; Huang, X.; Fenwick, K.; Andre, F.; Loibl, S.; Loi, S.; Garcia-Murillas, I.; et al. The Genetic Landscape and Clonal Evolution of Breast Cancer Resistance to Palbociclib plus Fulvestrant in the PALOMA-3 Trial. Cancer Discov. 2018, 8, 1390–1403. [Google Scholar] [CrossRef]
- Wander, S.A.; Cohen, O.; Gong, X.; Johnson, G.N.; Buendia-Buendia, J.E.; Lloyd, M.R.; Kim, D.; Luo, F.; Mao, P.; Helvie, K.; et al. The Genomic Landscape of Intrinsic and Acquired Resistance to Cyclin-Dependent Kinase 4/6 Inhibitors in Patients with Hormone Receptor-Positive Metastatic Breast Cancer. Cancer Discov. 2020, 10, 1174–1193. [Google Scholar] [CrossRef]
- Schwartz, C.J.; Marra, A.; Selenica, P.; Gazzo, A.; Tan, K.; Ross, D.; Razavi, P.; Chandarlapaty, S.; Weigelt, B.; Reis-Filho, J.S.; et al. RB1 Genetic Alterations in Estrogen Receptor-Positive Breast Carcinomas: Correlation With Neuroendocrine Differentiation. Mod. Pathol. 2024, 37, 100541. [Google Scholar] [CrossRef] [PubMed]
- Finn, R.S.; Liu, Y.; Zhu, Z.; Martin, M.; Rugo, H.S.; Dieras, V.; Im, S.A.; Gelmon, K.A.; Harbeck, N.; Lu, D.R.; et al. Biomarker Analyses of Response to Cyclin-Dependent Kinase 4/6 Inhibition and Endocrine Therapy in Women with Treatment-Naive Metastatic Breast Cancer. Clin. Cancer Res. 2020, 26, 110–121. [Google Scholar] [CrossRef]
- Turner, N.C.; Liu, Y.; Zhu, Z.; Loi, S.; Colleoni, M.; Loibl, S.; DeMichele, A.; Harbeck, N.; Andre, F.; Bayar, M.A.; et al. Cyclin E1 Expression and Palbociclib Efficacy in Previously Treated Hormone Receptor-Positive Metastatic Breast Cancer. J. Clin. Oncol. 2019, 37, 1169–1178, Erratum in J. Clin. Oncol. 2019, 37, 2956. https://doi.org/10.1200/JCO.19.02416. [Google Scholar] [CrossRef]
- Cristofanilli, M.; Rugo, H.S.; Im, S.-A.; Slamon, D.J.; Harbeck, N.; Bondarenko, I.; Masuda, N.; Colleoni, M.; DeMichele, A.; Loi, S.; et al. Overall Survival with Palbociclib and Fulvestrant in Women with HR+/HER2− ABC: Updated Exploratory Analyses of PALOMA-3, a Double-blind, Phase III Randomized Study. Clin. Cancer Res. 2022, 28, 3433–3442. [Google Scholar] [CrossRef]
- Lei, J.T.; Shao, J.; Zhang, J.; Iglesia, M.; Chan, D.W.; Cao, J.; Anurag, M.; Singh, P.; He, X.; Kosaka, Y.; et al. Functional Annotation of ESR1 Gene Fusions in Estrogen Receptor-Positive Breast Cancer. Cell Rep. 2018, 24, 1434–1444 e1437. [Google Scholar] [CrossRef]
- Haricharan, S.; Punturi, N.; Singh, P.; Holloway, K.R.; Anurag, M.; Schmelz, J.; Schmidt, C.; Lei, J.T.; Suman, V.; Hunt, K.; et al. Loss of MutL Disrupts CHK2-Dependent Cell-Cycle Control through CDK4/6 to Promote Intrinsic Endocrine Therapy Resistance in Primary Breast Cancer. Cancer Discov. 2017, 7, 1168–1183. [Google Scholar] [CrossRef] [PubMed]
- Anurag, M.; Punturi, N.; Hoog, J.; Bainbridge, M.N.; Ellis, M.J.; Haricharan, S. Comprehensive Profiling of DNA Repair Defects in Breast Cancer Identifies a Novel Class of Endocrine Therapy Resistance Drivers. Clin. Cancer Res. 2018, 24, 4887–4899. [Google Scholar] [CrossRef] [PubMed]
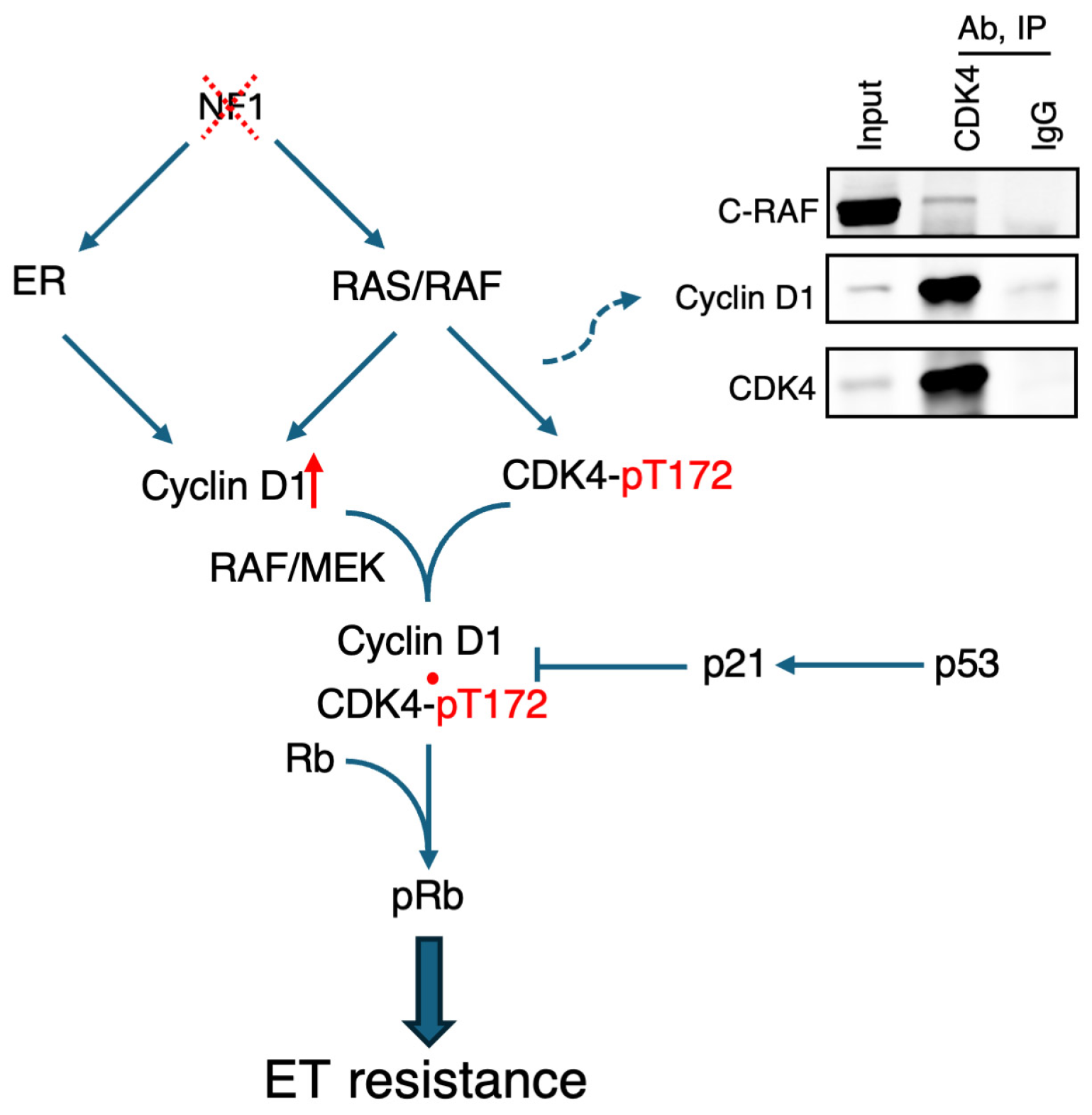
- Zheng, Z.-Y.; Chen, A.; Jaehnig, E.J.; Anurag, M.; Lei, J.T.; Feng, L.; Wang, C.; Fandino, D.; Singh, P.; Kennedy, H.; et al. NF1-depleted ER+ breast cancers are differentially sensitive to CDK4/6 inhibitors. Sci. Transl. Med. 2025, 17, eadq5492. [Google Scholar] [CrossRef]
- Zheng, Z.Y.; Anurag, M.; Lei, J.T.; Cao, J.; Singh, P.; Peng, J.; Kennedy, H.; Nguyen, N.C.; Chen, Y.; Lavere, P.; et al. Neurofibromin Is an Estrogen Receptor-alpha Transcriptional Co-repressor in Breast Cancer. Cancer Cell 2020, 37, 387–402 e387. [Google Scholar] [CrossRef] [PubMed]
- Wood, D.J.; Endicott, J.A. Structural insights into the functional diversity of the CDK-cyclin family. Open Biol. 2018, 8, 180112. [Google Scholar] [CrossRef]
- Bockstaele, L.; Bisteau, X.; Paternot, S.; Roger, P.P. Differential regulation of cyclin-dependent kinase 4 (CDK4) and CDK6, evidence that CDK4 might not be activated by CDK7, and design of a CDK6 activating mutation. Mol. Cell Biol. 2009, 29, 4188–4200. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Xu, H.; Lin, S.; Deng, W.; Zhou, J.; Zhang, Y.; Shi, Y.; Peng, D.; Xue, Y. GPS 5.0: An Update on the Prediction of Kinase-specific Phosphorylation Sites in Proteins. Genom. Proteom. Bioinform. 2020, 18, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.X.; Gao, F.; Luo, J.; Northfelt, D.W.; Goetz, M.; Forero, A.; Hoog, J.; Naughton, M.; Ademuyiwa, F.; Suresh, R.; et al. NeoPalAna: Neoadjuvant Palbociclib, a Cyclin-Dependent Kinase 4/6 Inhibitor, and Anastrozole for Clinical Stage 2 or 3 Estrogen Receptor-Positive Breast Cancer. Clin. Cancer Res. 2017, 23, 4055–4065. [Google Scholar] [CrossRef]
- Kim, B.J.; Zheng, Z.Y.; Lei, J.T.; Holt, M.V.; Chen, A.; Peng, J.; Fandino, D.; Singh, P.; Kennedy, H.; Dou, Y.; et al. Proteogenomic Approaches for the Identification of NF1/Neurofibromin-depleted Estrogen Receptor-positive Breast Cancers for Targeted Treatment. Cancer Res. Commun. 2023, 3, 1366–1377. [Google Scholar] [CrossRef]
- Curtis, C.; Shah, S.P.; Chin, S.F.; Turashvili, G.; Rueda, O.M.; Dunning, M.J.; Speed, D.; Lynch, A.G.; Samarajiwa, S.; Yuan, Y.; et al. The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 2012, 486, 346–352. [Google Scholar] [CrossRef]
- Tashakori, M.; Kadia, T.; Loghavi, S.; Daver, N.; Kanagal-Shamanna, R.; Pierce, S.; Sui, D.; Wei, P.; Khodakarami, F.; Tang, Z.; et al. TP53 copy number and protein expression inform mutation status across risk categories in acute myeloid leukemia. Blood 2022, 140, 58–72. [Google Scholar] [CrossRef]
- Redig, A.J.; Capelletti, M.; Dahlberg, S.E.; Sholl, L.M.; Mach, S.; Fontes, C.; Shi, Y.; Chalasani, P.; Janne, P.A. Clinical and Molecular Characteristics of NF1-Mutant Lung Cancer. Clin. Cancer Res. 2016, 22, 3148–3156. [Google Scholar] [CrossRef]
- Sangha, N.; Wu, R.; Kuick, R.; Powers, S.; Mu, D.; Fiander, D.; Yuen, K.; Katabuchi, H.; Tashiro, H.; Fearon, E.R.; et al. Neurofibromin 1 (NF1) defects are common in human ovarian serous carcinomas and co-occur with TP53 mutations. Neoplasia 2008, 10, 1362–1372. [Google Scholar] [CrossRef]
- Griffith, O.L.; Spies, N.C.; Anurag, M.; Griffith, M.; Luo, J.; Tu, D.; Yeo, B.; Kunisaki, J.; Miller, C.A.; Krysiak, K.; et al. The prognostic effects of somatic mutations in ER-positive breast cancer. Nat. Commun. 2018, 9, 3476, Erratum in Nat. Commun. 2018, 9, 850. [Google Scholar] [CrossRef]
- Fillbrunn, M.; Signorovitch, J.; Andre, F.; Wang, I.; Lorenzo, I.; Ridolfi, A.; Park, J.; Dua, A.; Rugo, H.S. PIK3CA mutation status, progression and survival in advanced HR+ /HER2- breast cancer: A meta-analysis of published clinical trials. BMC Cancer 2022, 22, 1002. [Google Scholar] [CrossRef] [PubMed]
- Andre, F.; Ciruelos, E.; Rubovszky, G.; Campone, M.; Loibl, S.; Rugo, H.S.; Iwata, H.; Conte, P.; Mayer, I.A.; Kaufman, B.; et al. Alpelisib for PIK3CA-Mutated, Hormone Receptor-Positive Advanced Breast Cancer. N. Engl. J. Med. 2019, 380, 1929–1940. [Google Scholar] [CrossRef]
- Vora, S.R.; Juric, D.; Kim, N.; Mino-Kenudson, M.; Huynh, T.; Costa, C.; Lockerman, E.L.; Pollack, S.F.; Liu, M.; Li, X.; et al. CDK 4/6 inhibitors sensitize PIK3CA mutant breast cancer to PI3K inhibitors. Cancer Cell 2014, 26, 136–149. [Google Scholar] [CrossRef] [PubMed]
- el-Deiry, W.S.; Tokino, T.; Velculescu, V.E.; Levy, D.B.; Parsons, R.; Trent, J.M.; Lin, D.; Mercer, W.E.; Kinzler, K.W.; Vogelstein, B. WAF1, a potential mediator of p53 tumor suppression. Cell 1993, 75, 817–825. [Google Scholar] [CrossRef]
- Harper, J.W.; Adami, G.R.; Wei, N.; Keyomarsi, K.; Elledge, S.J. The p21 Cdk-interacting protein Cip1 is a potent inhibitor of G1 cyclin-dependent kinases. Cell 1993, 75, 805–816. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Y.; Hannon, G.J.; Zhang, H.; Casso, D.; Kobayashi, R.; Beach, D. p21 is a universal inhibitor of cyclin kinases. Nature 1993, 366, 701–704. [Google Scholar] [CrossRef]
- Hortobagyi, G.N.; Stemmer, S.M.; Burris, H.A.; Yap, Y.S.; Sonke, G.S.; Paluch-Shimon, S.; Campone, M.; Petrakova, K.; Blackwell, K.L.; Winer, E.P.; et al. Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann. Oncol. 2018, 29, 1541–1547, Erratum in Ann. Oncol. 2019, 30, 1842. [Google Scholar] [CrossRef]
- Chiu, J.; Su, F.; Joshi, M.; Masuda, N.; Ishikawa, T.; Aruga, T.; Zarate, J.P.; Babbar, N.; Balbin, O.A.; Yap, Y.S. Potential value of ctDNA monitoring in metastatic HR + /HER2- breast cancer: Longitudinal ctDNA analysis in the phase Ib MONALEESASIA trial. BMC Med. 2023, 21, 306. [Google Scholar] [CrossRef]
- Anderson, S.A.; Bartow, B.B.; Harada, S.; Siegal, G.P.; Wei, S.; Dal Zotto, V.L.; Huang, X. p53 protein expression patterns associated with TP53 mutations in breast carcinoma. Breast Cancer Res. Treat. 2024, 207, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Tsherniak, A.; Vazquez, F.; Montgomery, P.G.; Weir, B.A.; Kryukov, G.; Cowley, G.S.; Gill, S.; Harrington, W.F.; Pantel, S.; Krill-Burger, J.M.; et al. Defining a Cancer Dependency Map. Cell 2017, 170, 564–576 e516. [Google Scholar] [CrossRef]
- Palmer, C.L.; Boras, B.; Pascual, B.; Li, N.; Li, D.; Garza, S.; Huser, N.; Yuan, J.T.; Cianfrogna, J.A.; Sung, T.; et al. CDK4 selective inhibition improves preclinical anti-tumor efficacy and safety. Cancer Cell 2025, 43, 464–481 e414. [Google Scholar] [CrossRef]
- Cancer Genome Atlas, N. Comprehensive molecular portraits of human breast tumours. Nature 2012, 490, 61–70. [Google Scholar] [CrossRef]
- Lanman, R.B.; Mortimer, S.A.; Zill, O.A.; Sebisanovic, D.; Lopez, R.; Blau, S.; Collisson, E.A.; Divers, S.G.; Hoon, D.S.; Kopetz, E.S.; et al. Analytical and Clinical Validation of a Digital Sequencing Panel for Quantitative, Highly Accurate Evaluation of Cell-Free Circulating Tumor DNA. PLoS ONE 2015, 10, e0140712. [Google Scholar] [CrossRef] [PubMed]
| Gene | p Value | FDR | Odds Ratio | Trend |
|---|---|---|---|---|
| TP53 | 1.1 × 10−58 | 1.9 × 10−56 | 5.3 | Co-occurring |
| NF1 | 7.5 × 10−8 | 6.5 × 10−6 | 3.2 | Co-occurring |
| USH2A | 1.3 × 10−3 | 3.3 × 10−2 | 1.7 | Co-occurring |
| MUC16 | 7.3 × 10−4 | 2.1 × 10−2 | 1.5 | Co-occurring |
| PIK3CA | 4.7 × 10−4 | 1.6 × 10−2 | 0.7 | Mutually Exclusive |
| GATA3 | 1.1 × 10−4 | 4.6 × 10−3 | 0.5 | Mutually Exclusive |
| MAP3K1 | 4.4 × 10−4 | 2.5 × 10−3 | 0.5 | Mutually Exclusive |
| Tumor Type | Hazard Ratio (HR) | HR 95% CI | p Value |
|---|---|---|---|
| NF1 Loss, TP53 Wildtype (n = 148) | 1.64 | 1.27–2.13 | 0.000185 |
| NF1 Normal, TP53 Mutated (n = 127) | 1.62 | 1.22–2.15 | 0.00077 |
| NF1 Loss, TP53 Mutated (n = 106) | 1.74 | 1.3–2.35 | 0.000248 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, A.; Zheng, Z.-Y.; Anurag, M.; Elkhanany, A.; Chen, N.C.; Chang, E.C. CDK4/6 Inhibitors in Breast Cancer—Who Should Receive Them? Int. J. Mol. Sci. 2025, 26, 10322. https://doi.org/10.3390/ijms262110322
Chen A, Zheng Z-Y, Anurag M, Elkhanany A, Chen NC, Chang EC. CDK4/6 Inhibitors in Breast Cancer—Who Should Receive Them? International Journal of Molecular Sciences. 2025; 26(21):10322. https://doi.org/10.3390/ijms262110322
Chicago/Turabian StyleChen, Anran, Ze-Yi Zheng, Meenakshi Anurag, Ahmed Elkhanany, Natalie C. Chen, and Eric C. Chang. 2025. "CDK4/6 Inhibitors in Breast Cancer—Who Should Receive Them?" International Journal of Molecular Sciences 26, no. 21: 10322. https://doi.org/10.3390/ijms262110322
APA StyleChen, A., Zheng, Z.-Y., Anurag, M., Elkhanany, A., Chen, N. C., & Chang, E. C. (2025). CDK4/6 Inhibitors in Breast Cancer—Who Should Receive Them? International Journal of Molecular Sciences, 26(21), 10322. https://doi.org/10.3390/ijms262110322





