Nano-Based Vaccine Delivery Systems: Innovative Therapeutics Against Cancer and Neurological Disorders
Abstract
1. Introduction
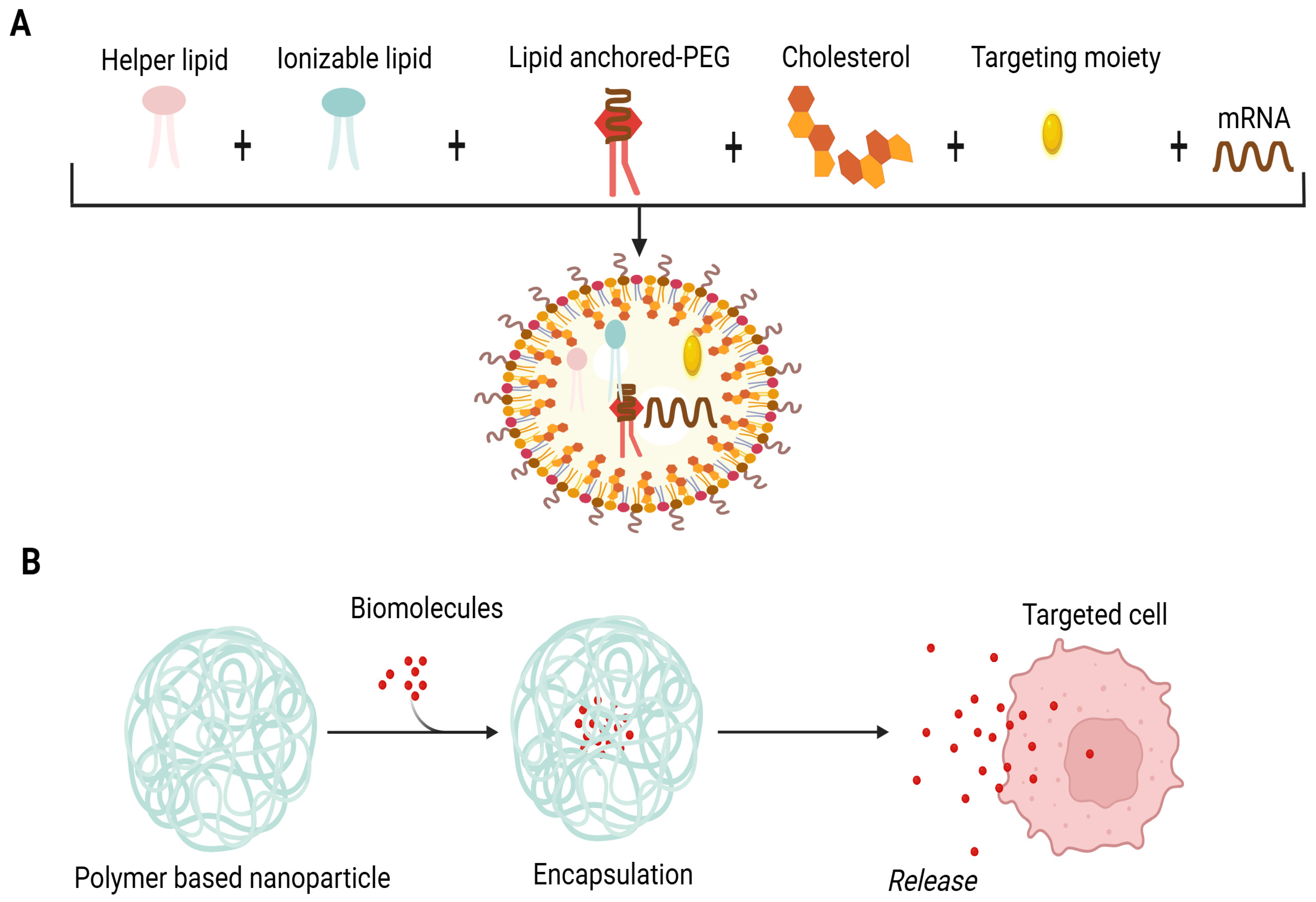
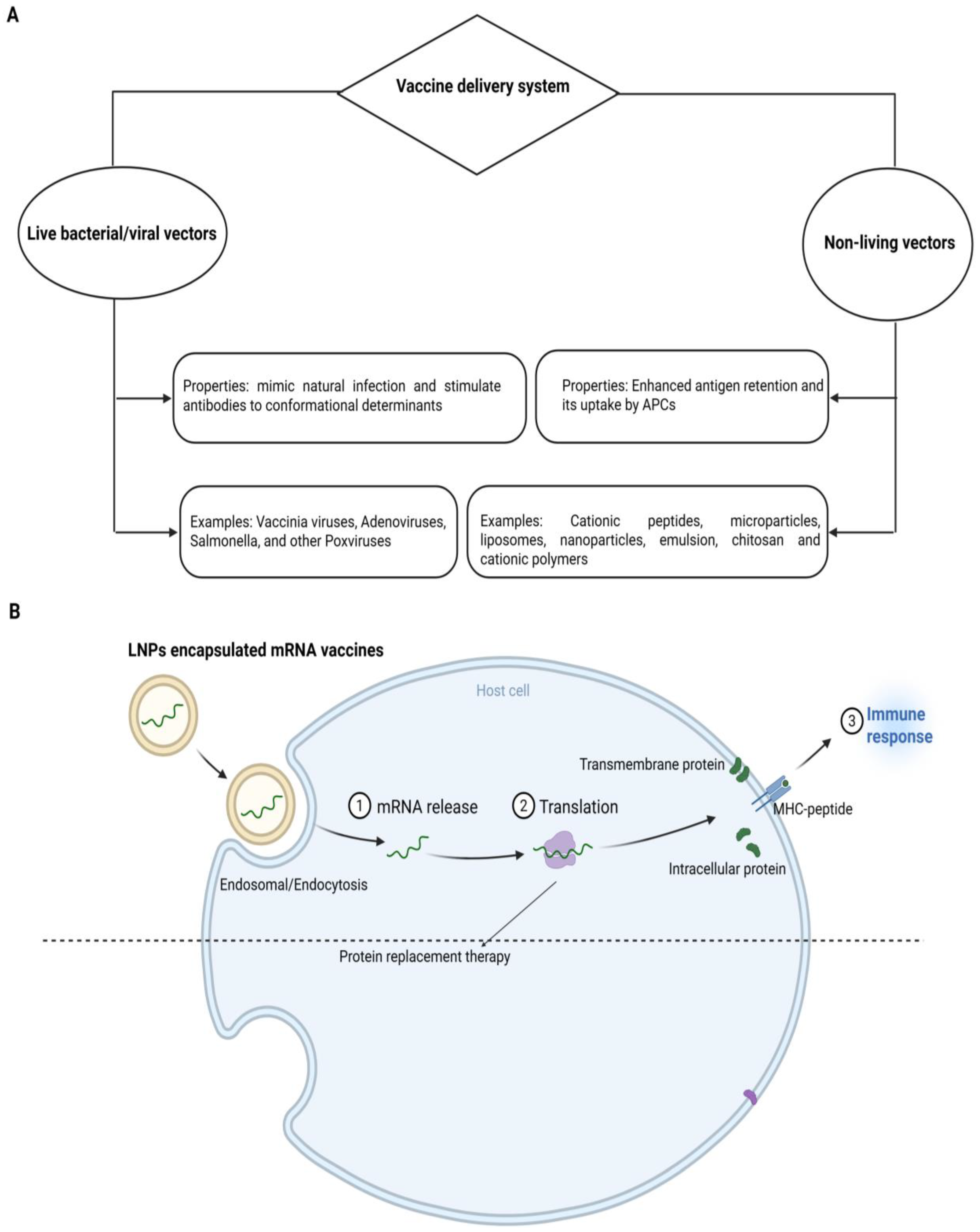
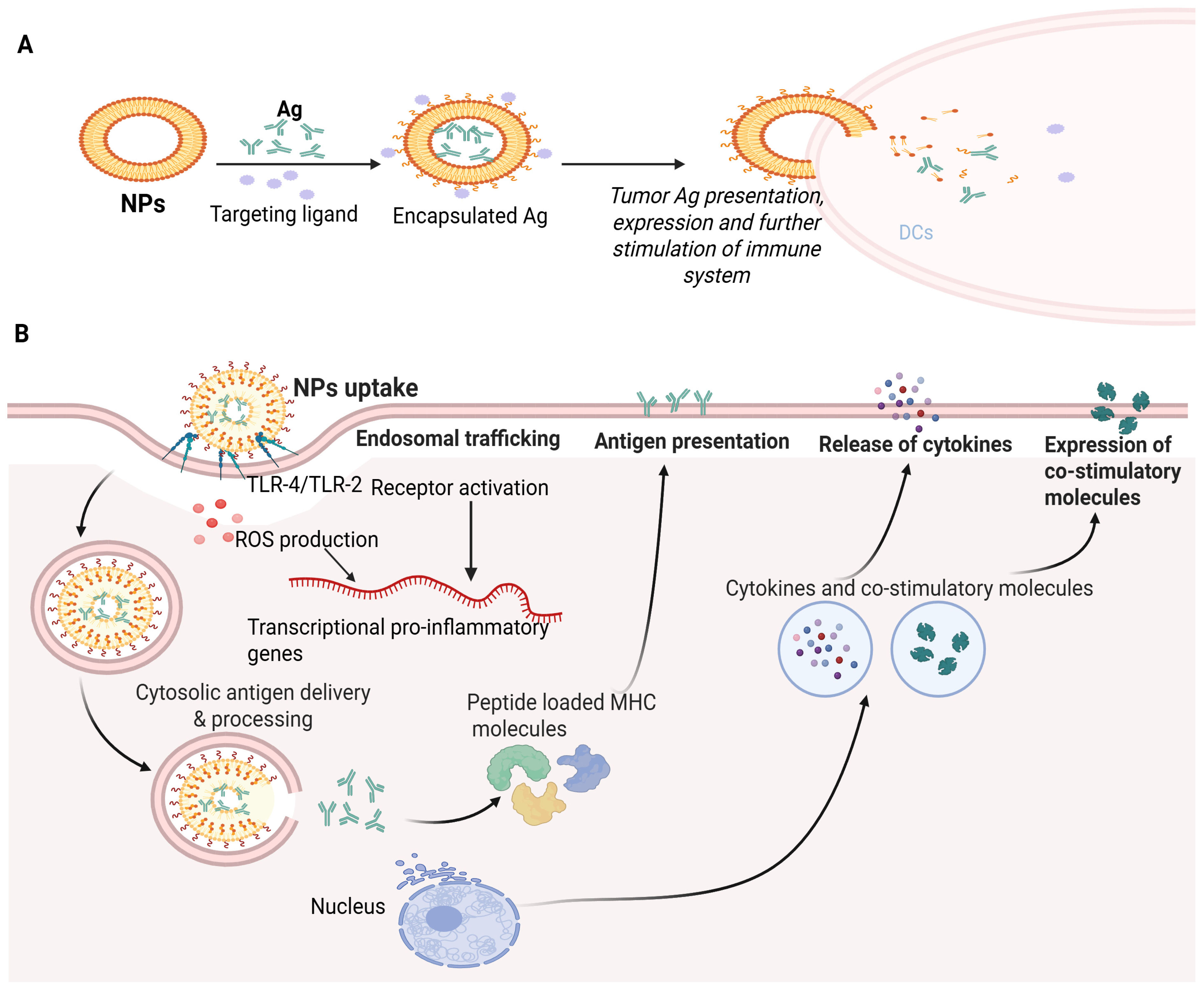
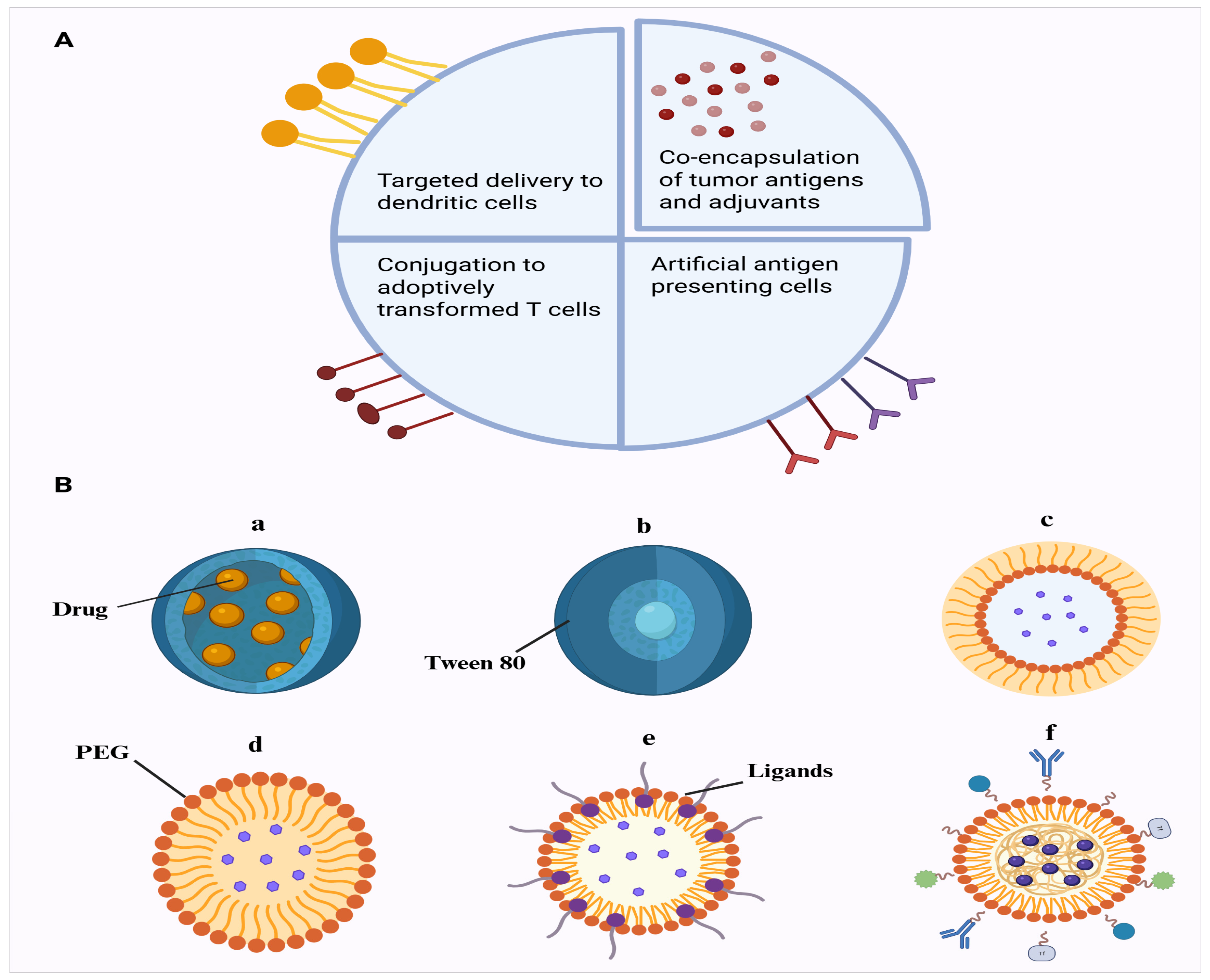
1.1. Lipid NPs and Liposomes
1.2. Polymeric NPs
1.3. Dendrimer NPs
1.4. Micelles and Emulsion
1.5. Inorganic NPs
1.6. Immune-Stimulatory Complexes
1.7. Exosomes as Vaccine Carriers
2. Mechanisms of Nanomaterials for Enhancement of Vaccines’ Efficacy
2.1. NPs and Vaccine Permeability and Efficacy at Tissue Level
2.2. NPs and Vaccine Permeability and Efficacy at Cellular Level
2.3. Enhancement of Vaccine Targeting
2.4. Stimulation of Immune Responses
2.5. Augmentation of Vaccine Cellular Utilization
3. Advancement in Cancer Vaccine Development
3.1. Cancer or Tumor Peptide Vaccines
3.2. Exosome-Based Nanovaccines Against Cancer
4. Nano-Based Carrier Systems for Neurological Disorders
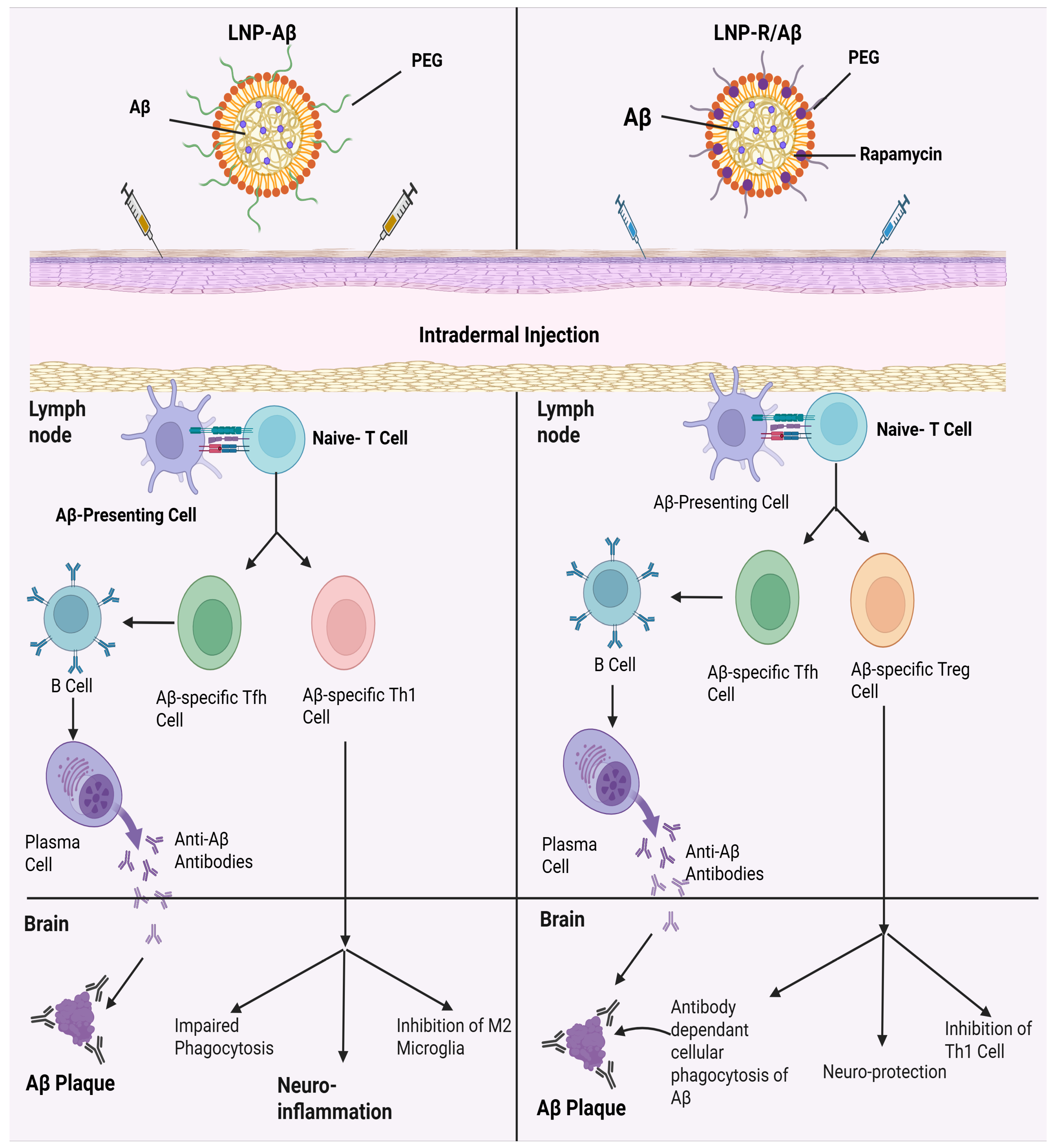
4.1. Alzheimer’s Disease
4.2. Parkinson’s Disease (PD)
4.3. Huntington’s Disease
4.4. Multiple Sclerosis
4.5. Sleep Apnea
4.6. Brain Tumors
4.7. Epilepsy
4.8. Ischemic Stroke
4.9. Autoimmune Encephalomyelitis
4.10. Other Reports in Neurodegenerative Disorders
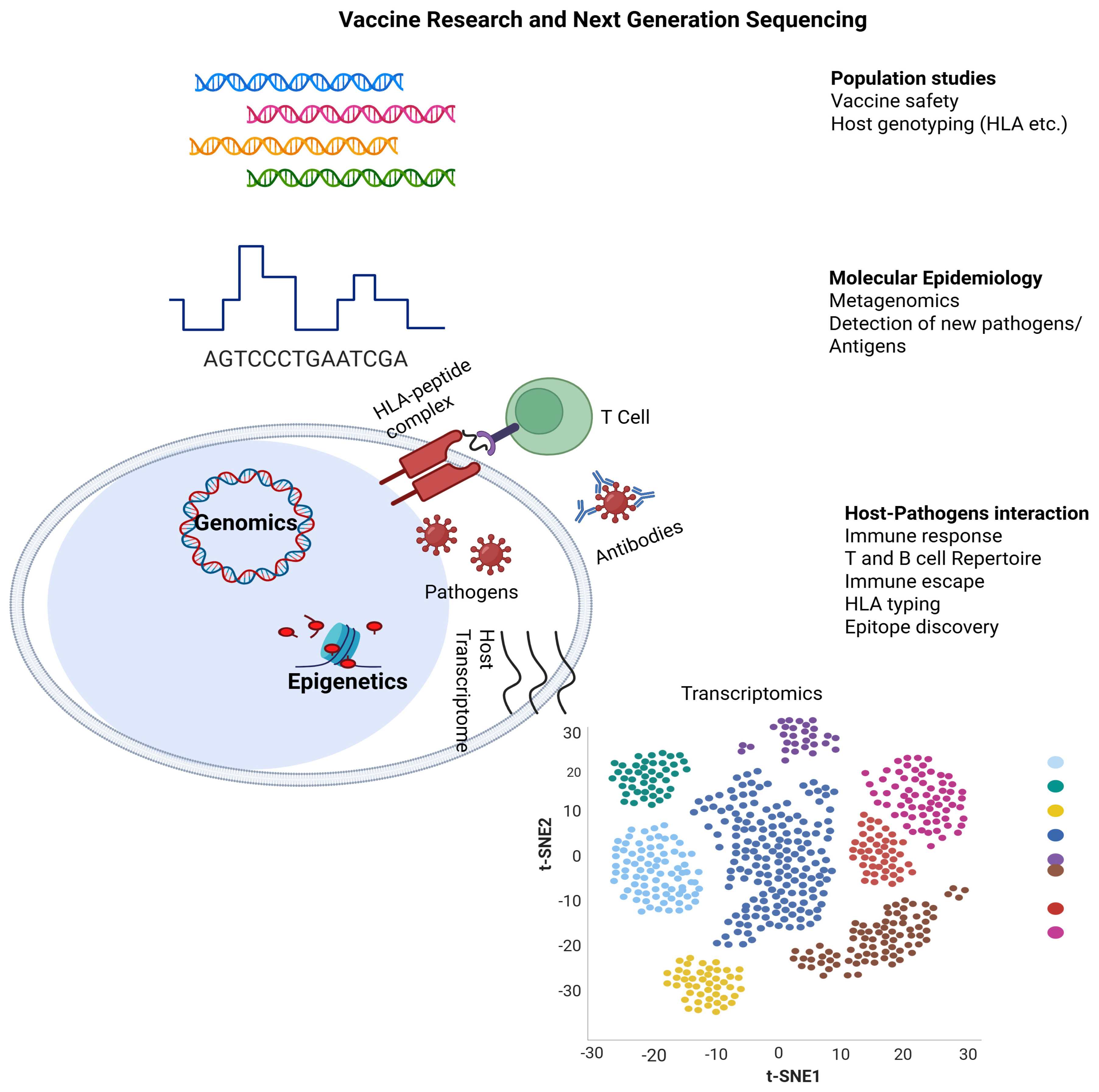
5. Next-Generation Deep Sequencing in Vaccine Delivery Systems Today and Tomorrow
| Study Reference | Nanoparticles/Nanocarriers Used | Size/Composition | Circulation/Persistence/Release Profile/Delivery Mechanism | Immune Response Initiated and Advantage | Regulatory Status | Disorder Type |
|---|---|---|---|---|---|---|
| Lei et al., 2024 [210] | mRNA-loaded mannosylated LNPs (Man-LNPs) | ~100–150 nm; ionizable cationic lipids with mannose ligands for DC targeting, helper lipids (DSPC), cholesterol PEG-lipids; encapsulating uridine-modified mRNA neoantigens | IM injection; mannose receptor-mediated DC uptake (3–5-fold enhanced vs. non-targeted LNPs); sustained antigen expression in 24–48 h; biodegradable, low toxicity | Potent CD8+ T cell responses, 10-fold higher IFN-γ, Th1-biased immunity, tumor regression in E.G7-OVA lymphoma model; targeted DC activation, improved efficacy at low doses, reduced off-target effects | Pre-clinical | Cancer (lymphoma) |
| Mendez-Gomez et al., 2024 [191] | mRNA loaded-LNPs | Aggregates > 1 μm (individual LNPs ~100 nm; onion-like multilamellar structure); ionizable lipids, cholesterol, PEG-lipids; encapsulating tumor mRNA antigens/neoantigens | Intravenous (IV) systemic administration; mimics emboli for lymphoreticular entrapment and RIG-I activation in stromal cells; rapid distribution (cytokine release within hours); no detailed pharmacokinetics (e.g., clearance, bioavailability) reported; well-tolerated in mice and dogs | Elicits rapid IFN-α/β via RIG-I/IFNAR1, enhances monocytes and lymphocytes activation, induces antigen-specific CD8+ T cell responses (↑ effector T cells, ↓ regulatory cells); potent immunity in glioma tumors | Pre-clinical study | Cancer (glioma) |
| Chen et al., 2023 [211] | Acid-ionizable iron nano-adjuvant (PEIM; IONPs with STING agonist) | ~50–100 nm; iron oxide nanoparticles (IONPs) coated with acid-ionizable copolymers like PEI, co-assembled with STING agonist MSA-2; encapsulating personalized tumor antigens | Intratumoral injection; concentrates in draining lymph nodes; acid-responsive release of Fe3+ for ROS generation and STING activation; facilitates APCs uptake | Augments STING/IFN-I pathway, enhances antigen cross-presentation, elicits 55-fold higher CD8+ T cell response; advantages: 16-fold STING agonist dosage-sparing, potent anti-tumor immunity in melanoma and colorectal carcinoma models | Pre-clinical | Cancer (melanoma and colorectal carcinoma) |
| Pan et al., 2023 [212] | Stearic acid-doped LNPs (sLNPs-OVA/MPLA) | ~100–150 nm; ionizable cationic lipid, DSPC, cholesterol, DMG-PEG2000, stearic acid (anionic); co-loaded with OVA-mRNA and MPLA (TLR4 agonist) | IV injection; spleen-selective mRNA translation via stearic acid; sustained antigen expression in 24–48 h | Enhanced DC activation, Th1-biased CD8+ T cell responses (↑ IFN-γ), persistent immune memory; potent tumor growth inhibition in E.G7-OVA lymphoma and B16F10-OVA melanoma models; synergistic TLR4 activation | Pre-clinical | Cancer (lymphoma and melanoma) |
| Cao et al., 2023 [61] | Dendrimers; GT-Mn2+ coordinative dendrimers | ~100–200 nm; amine-terminated PAMAM dendrimers (G5) coordinated with Mn2+ ions for self-assembly; encapsulates peptide antigens | Subcutaneous (SC) injection; DC internalization via macropinocytosis/lipid-raft pathways; gradual dissociation for antigen release and Mn2+ activation | Efficient antigen cross-presentation on MHC-I, activates cGAS-STING pathway (↑ IFN-β, cytokines); induces robust CD8+ T cell responses, Th1 immunity; advantages: personalized neoantigen packaging, potent tumor regression in melanoma or lymphoma models | Pre-clinical | Cancer (lymphoma and melanoma) |
| Shen et al., 2023 [62] | Dendrimers; photothermal-triggered dendrimers (IR780-PAMAM-OVA) | ~100–150 nm; PAMAM dendrimer (G5) conjugated with IR780 (photothermal agent) and OVA peptide antigen; self-assembled nanoparticles | SC injection; photothermal-triggered antigen release under NIR (near infrared) laser (808 nm); lymph node drainage; sustained release post-NIR-exposure; well-tolerated | Activates DCs via photothermal effect, enhances antigen-specific CD8+ T cell responses, Th1 immunity (↑ IFN-γ, IL-12); NIR-controlled release boosts immunity, significant tumor suppression in B16-OVA melanoma model | Pre-clinical | Cancer (melanoma) |
| Sasaki et al., 2022 [213] | mRNA-loaded LNPs (A-11-LNP; DC-targeted) | ~200 nm (optimal range; A-11: 547 nm); pH-sensitive cationic lipid CL4H6 (60%), DOPE (10%), cholesterol (28.5%), PEG-DSG (1.5%); encapsulating mRNA containing antigens | IV administration; targets splenic DCs; higher uptake/gene expression vs. smaller LNPs; transgene expression peaks at 24 h; multi-dosing tolerated | Induces DC-specific transgene expression (↑ CD40/CD80/CD86), antigen-specific CD8+ T cell responses; superior anti-tumor efficacy in E.G7-OVA lymphoma model; low toxicity | Pre-clinical | Cancer (lymphoma) |
| Kozaka et al., 2019 [65] | Micelles (reverse micellar antigen carriers) | ~10–20 nm; reverse micelles with sucrose erucate (ER-290), cholesterol and phosphatidylcholine; encapsulates OVA protein or tumor antigens | Intradermal; reverse micelles penetrate stratum corneum, target cutaneous DCs; sustained antigen release; well-tolerated | Induces antigen-specific CD8+ T cell responses, Th1-biased immunity (↑ IFN-γ); non-invasive transcutaneous delivery, effective tumor suppression in melanoma model, simpler than invasive methods | Pre-clinical | Cancer (melanoma) |
| Kranz et al., 2016 [214] | Liposomes/LNPs/RNA-lipoplex (RNA-LPX) | ~200–400 nm; ionizable cationic lipids, tumor antigen mRNA | IV delivery; targets spleen DCs via net negative charge; rapid uptake (within hours) into lymphoid DCs or macrophages; measurable half-life in circulation; persists in lymphoid organs; protects RNA from degradation | Induces IFN-α release, antigen-specific CD4+/CD8+ effector/memory T cell responses; IFNα-dependent tumor rejection in B16-OVA melanoma mouse models; ligand-free DC targeting, potent innate or adaptive immunity, broad antigen applicability | Pre-clinical | Cancer (melanoma) |
| Lee et al., 2023 [154] | Dendrimers | ~100–150 nm; polyamidoamine (PAMAM) dendrimers conjugated with amyloid-beta (Aβ) peptide (1–42) | SC injection; lymph node drainage for DC uptake; sustained antigen presentation; well-tolerated | Induces anti-Aβ antibodies (IgG) and Aβ-specific regulatory T cells (Tregs); reduces Aβ plaques, neuroinflammation and cognitive deficits in APP/PS1 mouse model of Alzheimer’s; balances humoral immunity and immune regulation to avoid excessive inflammation | Pre-clinical | Neurological disorder (Alzheimer’s) |
| Gomi et al. [169] | PS-LNPs (phosphatidylserine lipid nanoparticles) | ~131–133 nm; negative zeta potential ≈ −21 mV; encapsulating MOG35–55 mRNA antigen | IV injection; spleen-targeting; antigen presentation of self-antigen; low dose (1 µg) temporal dosing on days 7, 10, and 13 post-immunization; sustained release, well tolerated | Induces antigen-specific tolerance; lowers EAE (experimental autoimmune encephalomyelitis clinical score) scores, reduces IL-17A and pro-inflammatory cytokines; Treg induction; antigen specificity and low dose | Pre-clinical | Neurological disorder (multiple sclerosis) |
| Study Reference | Nanoparticles/Nanocarriers Used | Size/Composition | Circulation/Persistence/Release Profile/Delivery Mechanism | Immune Response Initiated and Advantage | Regulatory Status | Disorder Type |
|---|---|---|---|---|---|---|
| Weber et al., 2024 [215] | LNP formulation, personalized neoantigen lipid nanoparticles | ~80–100 nm; lipid nanoparticle (LNP) formulation with ionizable cationic lipids, cholesterol, PEG-lipids; synthetic mRNA encoding up to 34 patient-specific neoantigens | Intramuscular (IM) injection; designed for lymph node drainage and DC uptake; sustained antigen expression in days; well-tolerated | Induces neoantigen-specific CD4+/CD8+ T cell responses; individualized for melanoma tumor mutations | Phase II clinical trial completed (2024, positive); multiple Phase III ongoing; not FDA approved yet; patented | Cancer (melanoma) |
| Mendez-Gomez et al., 2024 [191] | RNA lipid particle aggregates (RNA-LPAs; multi-lamellar mRNA aggregates) | Aggregates > 1 μm (individual LNPs 100 nm, onion-like multilamellar); composed of ionizable lipids, cholesterol, PEG-lipids; encapsulating patient-derived tumor mRNA antigens like IL13Rα2 | Intravenous (IV) systemic administration; rapid systemic distribution; well-tolerated with multi-dosing | Stimulated rapid cytokines, chemokines release, monocytes and lymphocytes activation and antigen-specific CD8+ T cell expansion, reduced regulatory cells, increased effector T cells; enhanced immunogenicity for glioblastoma | Phase I clinical trial completed; safe; not FDA approved; not patented yet | Cancer (glioblastoma) |
| Rojas et al., 2023 [216] | RNA-lipoplex nanoparticles (iNeST; autogene cevumeran RO7198457/BNT12) | ~200–400 nm; proprietary ionizable cationic lipids, patient-derived tumor neoantigen mRNA (up to 20 neoantigens) | IV delivery; targets splenic DCs via net negative charge; rapid uptake in hours; sustained T cell persistence up to 3 years; well-tolerated in multi-dosing | Induces neoantigen-specific CD8+ T cells responses detected up to 3 years; fully personalized for tumor mutations, enhances anti-tumor immunity in pancreatic and melanoma tumors | Phase I clinical trial completed; multiple Phase II trials ongoing; not FDA approved; not patented yet | Cancer (melanoma and pancreatic cancer) |
| Sahin et al., 2020 [217] | Liposomes; RNA-lipoplex (RNA-LPX; FixVac BNT111) | 200–400 nm; proprietary ionizable cationic lipids, uridine-modified mRNA encoding four melanoma antigens (NY-ESO-1, MAGE-A3, tyrosinase, TPTE) | IV delivery; targets splenic dendritic cells via net negative charge; rapid uptake in hours; sustained antigen expression; well-tolerated up to 400 µg doses in multi-dosing regimens | Induces IFN-α, durable antigen-specific CD4+/CD8+ T cell responses in melanoma, enhances pre-existing immunity | Phase I clinical trial completed (2020); Phase 2 ongoing (2024 topline positive); not FDA approved; not patented yet | Cancer (melanoma) |
| T. Gargett et al., 2018 [30] | Liposomes/LNPs (dendritic-cell-targeted nanocarriers) | ~100–150 nm; MM200 melanoma cell vesicles, POPC liposomes, anti-DC-SIGN antibodies, IFN-γ | IV delivery; targets DC-SIGN on DCs for antigen presentation; multi-dose tolerated | Induced antigen-specific T cell responses (CD4+ and CD8+) and antibody production; strategy designed to enhance presentation and overcome immune tolerance in melanoma | Phase I clinical trial completed; safe; not FDA approved; patented | Cancer (melanoma) |
| Kranz et al., 2016 [214] | Liposomes/LNPs, RNA-lipoplex (RNA-LPX) | ~200–400 nm; ionizable cationic lipids, tumor antigen mRNA | IV delivery; targets spleen DCs via negative charge; well-tolerated | Induces IFN-α, antigen-specific CD4+/CD8+ T cell responses; systemic DC targeting, potent T cell priming for melanoma | Phase I clinical trial completed; safe; not FDA approved; not patented yet | Cancer (melanoma) |
| Palmer et al., 2001 [218] | Liposome/LNPs | ~100–200 nm (multilamellar); BLP25 lipopeptide (25-aa MUC1 core peptide), MPL adjuvant, DPPC, DMPG, cholesterol | Intradermal; prolonged circulation (PEGylated)/controlled antigen/drug release, cyclophosphamide pretreatment; facilitates APC uptake for MHC presentation; well-tolerated multi-dosing | Induces MUC1-specific T cell (IFN-γ, proliferation) and humoral responses; safe with minimal toxicity; targets overexpressed MUC1 in NSCLC (non-small-cell lung cancer) for active specific immunotherapy | Phase I and II clinical trials completed; advanced to Phase III; not approved by FDA; patented | Cancer (non-small-cell lung cancer) |
| Ciccone, 2024 [159] | B-312 nano synthetic peptides/antigens | Synthetic peptides derived from α-synuclein | IM injection; doses tested: 300/100/100 µg and 300/300/300 µg; antibody titers peaked around week 21, detectable up to ~45 weeks; antibodies cross blood–brain barrier | Induces antibodies selectively against aggregated α-synuclein; reduces pathological α-synuclein seeding activity in CSF | Phase I clinical trial completed; not approved by FDA; not patented yet | Neurological disorder (Parkinson’s) |
| Eijsvogel et al., 2024 [160] | LNPs | ~80–100 nm; ionizable lipid, DSPC, cholesterol, PEG-lipid; peptide delivery as antigens | Intramuscular injection; induces anti-α-synuclein antibodies; well tolerated; crossed BBB | Induces antibodies selectively against aggregated α-synuclein; reduces pathological α-synuclein seeding activity in CSF, improves cognitive behavior | Phase II clinical trial completed; not approved by FDA; not patented yet | Neurological disorder (Parkinson’s) |
| Volc et al., 2020 [161] | Active peptides/nano antigens | Synthetic peptides derived from α-synuclein | IM injection (300/100/100 μg or 300/300/300 μg doses, 3 doses over 8 weeks); systemic distribution for immune activation; antibodies detectable in serum and CSF up to 44 weeks | Induces anti-α-Syn antibodies; reduces pathological α-Syn seeding in CSF, improves MDS-UPDRS Part II scores (daily living activities), stable motor/cognitive function; potentially disease-modifying for early PD | Phase I clinical trial completed but not approved by FDA; not patented yet | Neurological disorder (Parkinson’s) |
| Yu et al., 2023 [219] | Peptides (synthetic Aβ1–14 B cell epitope peptides linked to UBITh® helper T cell epitopes; alum + CpG adjuvants) | Synthetic micro/nano peptides | Intramuscular injection; distribution for immune activation; antibodies detectable in serum and CSF | Induces robust anti-amyloid β antibodies; high responder rate; has shown trends toward slowing cognitive decline; favorable safety profile | Phase II clinical trial completed; not approved by FDA; patented | Neurological disorder (Alzheimer’s) |
6. Future Challenges and Perspectives
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Butterfield, L.H. Cancer Vaccines. BMJ 2015, 350, h988. [Google Scholar] [CrossRef]
- Dumurgier, J.; Tzourio, C. Epidemiology of Neurological Diseases in Older Adults. Rev. Neurol. 2020, 176, 642–648. [Google Scholar] [CrossRef]
- Krishnamachari, Y.; Salem, A.K. Innovative Strategies for Co-Delivering Antigens and Cpg Oligonucleotides. Adv. Drug Deliv. Rev. 2009, 61, 205–217. [Google Scholar] [CrossRef]
- Igarashi, Y.; Sasada, T. Cancer Vaccines: Toward the Next Breakthrough in Cancer Immunotherapy. J. Immunol. Res. 2020, 2020, 5825401. [Google Scholar] [CrossRef] [PubMed]
- Poddar, M.K.; Chakraborty, A.; Banerjee, S. Neurodegeneration: Diagnosis, Prevention, and Therapy. In Oxidoreductase; IntechOpen: London, UK, 2021. [Google Scholar]
- Lingineni, K.; Belekar, V.; Tangadpalliwar, S.R.; Garg, P. Tangadpalliwar, and Prabha Garg. The Role of Multidrug Resistance Protein (Mrp-1) as an Active Efflux Transporter on Blood–Brain Barrier (Bbb) Permeability. Mol. Divers. 2017, 21, 355–365. [Google Scholar] [CrossRef]
- Irvine, D.J.; Swartz, M.A.; Szeto, G.L. Engineering Synthetic Vaccines Using Cues from Natural Immunity. Nat. Mater. 2013, 12, 978–990. [Google Scholar] [CrossRef]
- Goetz, M.; Thotathil, N.; Zhao, Z.; Mitragotri, S. Vaccine Adjuvants for Infectious Disease in the Clinic. Bioeng. Transl. Med. 2024, 9, e10663. [Google Scholar] [CrossRef]
- Smith, D.M.; Jakub, K.S.; James, R.B., Jr. Applications of Nanotechnology for Immunology. Nat. Rev. Immunol. 2013, 13, 592–605. [Google Scholar] [CrossRef] [PubMed]
- Hayat, G.; Mohammad, S.; Darroudi, M. Nanovaccine: A Novel Approach in Immunization. J. Cell. Physiol. 2019, 234, 12530–12536. [Google Scholar] [CrossRef]
- Xie, L.; Xie, D.; Du, Z.; Xue, S.; Wang, K.; Yu, X.; Liu, X.; Peng, Q.; Fang, C. A Novel Therapeutic Outlook: Classification, Applications and Challenges of Inhalable Micron/Nanoparticle Drug Delivery Systems in Lung Cancer. Int. J. Oncol. 2024, 64, 38. [Google Scholar] [CrossRef] [PubMed]
- Hristova-Panusheva, K.; Xenodochidis, C.; Georgieva, M.; Krasteva, N. Nanoparticle-Mediated Drug Delivery Systems for Precision Targeting in Oncology. Pharmaceuticals 2024, 17, 677. [Google Scholar] [CrossRef] [PubMed]
- Rajashri, B.; Chavda, V.P.; Nongrang, L.; Alom, S.; Deka, K.; Kalita, T.; Ali, F.; Bhattacharjee, B.; Vora, L. Nanoparticle-Based Delivery Systems for Vaccines. Vaccines 2022, 10, 1946. [Google Scholar] [CrossRef] [PubMed]
- Ewii, U.E.; Attama, A.A.; Olorunsola, E.O.; Onugwu, A.L.; Nwakpa, F.U.; Anyiam, C.; Chijioke, C.; Ogbulie, T. Nanoparticles for Drug Delivery: Insight into in Vitro and in Vivo Drug Release from Nanomedicines. Nano TransMed 2025, 4, 100083. [Google Scholar] [CrossRef]
- Parvin, N.; Mandal, T.K.; Joo, S.-W. The Impact of COVID-19 on Rna Therapeutics: A Surge in Lipid Nanoparticles and Alternative Delivery Systems. Pharmaceutics 2024, 16, 1366. [Google Scholar] [CrossRef]
- Xiao, W.; Jiang, W.; Chen, Z.; Huang, Y.; Mao, J.; Zheng, W.; Hu, Y.; Shi, J. Advance in Peptide-Based Drug Development: Delivery Platforms, Therapeutics and Vaccines. Signal Transduct. Target. Ther. 2025, 10, 74. [Google Scholar] [CrossRef]
- Sahdev, P.; Ochyl, L.J.; Moon, J.J. Biomaterials for Nanoparticle Vaccine Delivery Systems. Pharm. Res. 2014, 31, 2563–2582. [Google Scholar] [CrossRef]
- Zhuo, Y.; Zeng, H.; Su, C.; Lv, Q.; Cheng, T.; Lei, L. Tailoring Biomaterials for Vaccine Delivery. J. Nanobiotechnol. 2024, 22, 480. [Google Scholar] [CrossRef]
- Hussein, M.; Mumtaz, M.; Nasir, I.; Abdullahi, A. Nanotechnology-Based Vaccines. Biol. Med. Nat. Prod. Chem. 2023, 12, 343–361. [Google Scholar] [CrossRef]
- Panda, A.K. Nanotechnology in Vaccine Development. Proc. Natl. Acad. Sci. India Sect. B Biol. Sci. 2012, 82, 13–27. [Google Scholar] [CrossRef]
- Ahmad, M.Z.; Ahmad, J.; Haque, A.; Alasmary, M.Y.; Abdel-Wahab, B.A.; Akhter, S. Emerging Advances in Synthetic Cancer Nano-Vaccines: Opportunities and Challenges. Expert Rev. Vaccines 2020, 19, 1053–1071. [Google Scholar] [CrossRef] [PubMed]
- Assefi, M.; Ataeinaeini, M.; Nazari, A.; Gholipour, A.; Vertiz-Osores, J.J.; Calla-Vásquez, K.M.; Al-Naqeeb, B.Z.T.; Jassim, K.H.; Kalajahi, H.G.; Yasamineh, S.; et al. A State-of-the-Art Review on Solid Lipid Nanoparticles as a Nanovaccines Delivery System. J. Drug Deliv. Sci. Technol. 2023, 86, 104623. [Google Scholar] [CrossRef]
- Francis, J.E.; Skakic, I.; Majumdar, D.; Taki, A.C.; Shukla, R.; Walduck, A.; Smooker, P.M. Solid Lipid Nanoparticles Delivering a DNA Vaccine Encoding Helicobacter Pylori Urease a Subunit: Immune Analyses before and after a Mouse Model of Infection. Int. J. Mol. Sci. 2024, 25, 1076. [Google Scholar] [CrossRef]
- Minz, S.; Pandey, R.S. Development of Adjuvanted Solid Fat Nanoemulsions for Pulmonary Hepatitis B Vaccination. J. Pharm. Sci. 2018, 107, 1701–1712. [Google Scholar] [CrossRef]
- Swetha, K.; Kotla, N.G.; Tunki, L.; Jayaraj, A.; Bhargava, S.K.; Hu, H.; Bonam, S.R.; Kurapati, R. Recent Advances in the Lipid Nanoparticle-Mediated Delivery of Mrna Vaccines. Vaccines 2023, 11, 658. [Google Scholar] [CrossRef] [PubMed]
- Shahzamani, K.; Mahmoudian, F.; Ahangarzadeh, S.; Ranjbar, M.M.; Beikmohammadi, L.; Bahrami, S.; Mohammadi, E.; Esfandyari, S.; Alibakhshi, A.; Javanmard, S.H. Vaccine Design and Delivery Approaches for COVID-19. Int. Immunopharmacol. 2021, 100, 108086. [Google Scholar] [CrossRef] [PubMed]
- Tosha, P.; Joshi, P.; Pathak, R.; Shah, S. Nano-Vaccination Strategies: Applications and Challenges for Intranasal Immunization. Curr. Pharm. Biotechnol. 2023, 24, 946–969. [Google Scholar] [CrossRef]
- Feather, L.A.J.; Nadella, V.; Kastner, E.; Perrie, Y.; Hilton, A.C.; Devitt, A. Development of a Rapid in Vitro Pre-Screen for Distinguishing Effective Liposome-Adjuvant Delivery Systems. Sci. Rep. 2022, 12, 12448. [Google Scholar] [CrossRef]
- Wallis, J.; Katti, P.; Martin, A.M.; Hills, T.; Seymour, L.W.; Shenton, D.P.; Carlisle, R.C. A Liposome-Based Cancer Vaccine for a Rapid and High-Titre Anti-Erbb-2 Antibody Response. Eur. J. Pharm. Sci. 2020, 152, 105456. [Google Scholar] [CrossRef]
- Gargett, T.; Abbas, M.N.; Rolan, P.; Price, J.D.; Gosling, K.M.; Ferrante, A.; Ruszkiewicz, A.; Atmosukarto, I.I.C.; Altin, J.; Parish, C.R.; et al. Phase I Trial of Lipovaxin-Mm, a Novel Dendritic Cell-Targeted Liposomal Vaccine for Malignant Melanoma. Cancer Immunol. Immunother. 2018, 67, 1461–1472. [Google Scholar] [CrossRef]
- Abdellatif, A.A.; Younis, M.A.; Alsowinea, A.F.; Abdallah, E.M.; Abdel-Bakky, M.S.; Al-Subaiyel, A.; Hassan, Y.A.; Tawfeek, H.M. Lipid Nanoparticles Technology in Vaccines: Shaping the Future of Prophylactic Medicine. Colloids Surf. B Biointerfaces 2023, 222, 113111. [Google Scholar] [CrossRef]
- Wang, J.-H.; Gessler, D.J.; Zhan, W.; Gallagher, T.L.; Gao, G. Adeno-Associated Virus as a Delivery Vector for Gene Therapy of Human Diseases. Signal Transduct. Target. Ther. 2024, 9, 78. [Google Scholar] [CrossRef]
- Sandgren, K.J.; Truong, N.R.; Smith, J.B.; Bertram, K.; Cunningham, A.L. Vaccines for Herpes Simplex: Recent Progress Driven by Viral and Adjuvant Immunology. In Herpes Simplex Virus: Methods and Protocols; Springer: Berlin/Heidelberg, Germany, 2020; pp. 31–56. [Google Scholar]
- Ramamoorth, M.; Narvekar, A. Non Viral Vectors in Gene Therapy-an Overview. J. Clin. Diagn. Res. JCDR 2015, 9, GE01–GE06. [Google Scholar] [CrossRef]
- Folegatti, P.M.; Ewer, K.J.; Aley, P.K.; Angus, B.; Becker, S.; Belij-Rammerstorfer, S.; Bellamy, D.; Bibi, S.; Bittaye, M.; Clutterbuck, E.A.; et al. Safety and Immunogenicity of the Chadox1 nCoV-19 Vaccine against SARS-CoV-2: A Preliminary Report of a Phase 1/2, Single-Blind, Randomised Controlled Trial. Lancet 2020, 396, 467–478. [Google Scholar] [CrossRef] [PubMed]
- Logunov, D.Y.; Dolzhikova, I.V.; Zubkova, O.V.; Tukhvatullin, A.I.; Shcheblyakov, D.V.; Dzharullaeva, A.S.; Grousova, D.M.; Erokhova, A.S.; Kovyrshina, A.V.; Botikov, A.G.; et al. Safety and Immunogenicity of an rAd26 and rAd5 Vector-Based Heterologous Prime-Boost COVID-19 Vaccine in Two Formulations: Two Open, Non-Randomised Phase 1/2 Studies from Russia. Lancet 2021, 396, 887–897, Erratum in Lancet 2021, 397, 98. [Google Scholar] [CrossRef] [PubMed]
- Clark, M.A.; Blair, H.; Liang, L.; Brey, R.N.; Brayden, D.; Hirst, B.H. Targeting Polymerised Liposome Vaccine Carriers to Intestinal M Cells. Vaccine 2001, 20, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Hardee, C.L.; Arévalo-Soliz, L.M.; Hornstein, B.D.; Zechiedrich, L. Advances in Non-Viral DNA Vectors for Gene Therapy. Genes 2017, 8, 65. [Google Scholar] [CrossRef]
- Peres, C.; Matos, A.I.; Conniot, J.; Sainz, V.; Zupančič, E.; Silva, J.M.; Graça, L.; Gaspar, R.S.; Préat, V.; Florindo, H.F. Poly (Lactic Acid)-Based Particulate Systems Are Promising Tools for Immune Modulation. Acta Biomater. 2017, 48, 41–57. [Google Scholar] [CrossRef]
- Gutjahr, A.; Phelip, C.; Coolen, A.-L.; Monge, C.; Boisgard, A.-S.; Paul, S.; Verrier, B. Biodegradable Polymeric Nanoparticles-Based Vaccine Adjuvants for Lymph Nodes Targeting. Vaccines 2016, 4, 34. [Google Scholar] [CrossRef]
- Huang, Z.; Zhuang, X.; Liu, L.; Zhao, J.; Ma, S.; Si, X.; Zhu, Z.; Wu, F.; Jin, N.; Tian, M.; et al. Modularized Viromimetic Polymer Nanoparticle Vaccines (Vpnvaxs) to Elicit Durable and Effective Humoral Immune Responses. Natl. Sci. Rev. 2023, 11, nwad310. [Google Scholar] [CrossRef]
- Majumder, J.; Minko, T. Multifunctional and Stimuli-Responsive Nanocarriers for Targeted Therapeutic Delivery. Expert Opin. Drug Deliv. 2021, 18, 205–227. [Google Scholar] [CrossRef]
- Yoo, J.; Park, C.; Yi, G.; Lee, D.; Koo, H. Active Targeting Strategies Using Biological Ligands for Nanoparticle Drug Delivery Systems. Cancers 2019, 11, 640. [Google Scholar] [CrossRef]
- Thakur, R.; Arora, V. Comprehensive Review on Polymeric and Metal Nanoparticles: Possible Therapeutic Avenues. Int. J. Polym. Mater. Polym. Biomater. 2023, 72, 1489–1509. [Google Scholar] [CrossRef]
- Koirala, P.; Chen, S.R.; Boer, J.C.; Khalil, Z.G.; Deceneux, C.; Goodchild, G.; Lu, L.; Faruck, M.O.; Shalash, A.O.; Bashiri, S.; et al. Polymeric Nanoparticles as a Self-Adjuvanting Peptide Vaccine Delivery System: The Role of Shape. Adv. Funct. Mater. 2023, 33, 2209304. [Google Scholar] [CrossRef]
- Zhao, H.; Li, Y.; Zhao, B.; Zheng, C.; Niu, M.; Song, Q.; Liu, X.; Feng, Q.; Zhang, Z.; Wang, L. Orchestrating Antigen Delivery and Presentation Efficiency in Lymph Node by Nanoparticle Shape for Immune Response. Acta Pharm. Sin. B 2023, 13, 3892–3905. [Google Scholar] [CrossRef]
- Wibowo, D.; Jorritsma, S.H.; Gonzaga, Z.J.; Evert, B.; Chen, S.; Rehm, B.H. Polymeric Nanoparticle Vaccines to Combat Emerging and Pandemic Threats. Biomaterials 2021, 268, 120597. [Google Scholar] [CrossRef]
- Eivazzadeh-Keihan, R.; Noruzi, E.B.; Mehrban, S.F.; Aliabadi, H.A.M.; Karimi, M.; Mohammadi, A.; Maleki, A.; Mahdavi, M.; Larijani, B.; Shalan, A.E. The Latest Advances in Biomedical Applications of Chitosan Hydrogel as a Powerful Natural Structure with Eye-Catching Biological Properties. J. Mater. Sci. 2022, 57, 3855–3891. [Google Scholar] [CrossRef]
- Sarah, G.; Saupe, A.; McBurney, W.; Rades, T.; Hook, S. Comparison of Chitosan Nanoparticles and Chitosan Hydrogels for Vaccine Delivery. J. Pharm. Pharmacol. 2008, 60, 1591–1600. [Google Scholar] [CrossRef] [PubMed]
- Rasim, M.; Wasan, E.K. Chitosan Non-Particulate Vaccine Delivery Systems. J. Pharm. Pharm. Sci. 2024, 27, 12921. [Google Scholar] [CrossRef]
- Erdal, C.; Stefan, K.S.; Satyanarayana, S.; Steve, B.; Alpar, H.O. Development of Chitosan–Pullulan Composite Nanoparticles for Nasal Delivery of Vaccines: In Vivo Studies. J. Microencapsul. 2015, 32, 769–783. [Google Scholar]
- Mohsen, D.; Negahdari, B.; Eslam, H.M.; Zare, H.; Ghanaat, M.; Koushali, S.S.; Malekshahi, Z.V. Polymeric Nanoparticles for DNA Vaccine-Based Cancer Immunotherapy: A Review. Biotechnol. Lett. 2023, 45, 1053–1072. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.A.; McCrudden, C.M.; McCaffrey, J.; McBride, J.W.; Cole, G.; Dunne, N.J.; Robson, T.; Kissenpfennig, A.; Donnelly, R.F.; McCarthy, H.O. DNA Vaccination for Cervical Cancer; a Novel Technology Platform of Rala Mediated Gene Delivery Via Polymeric Microneedles. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 921–932. [Google Scholar] [CrossRef]
- Alexandra, S.; Grun, M.K.; Mao, T.; Israelow, B.; Reschke, M.; Grundler, J.; Akhtar, L.; Lee, T.; Shin, K.; Piotrowski-Daspit, A.S. Polymer Nanoparticles Deliver Mrna to the Lung for Mucosal Vaccination. Sci. Transl. Med. 2023, 15, eabq0603. [Google Scholar] [CrossRef] [PubMed]
- Hyunjoon, K.; Kirtane, A.R.; Kim, N.Y.; Rajesh, N.U.; Tang, C.; Ishida, K.; Hayward, A.M.; Langer, R.; Traverso, G. Gastrointestinal Delivery of an Mrna Vaccine Using Immunostimulatory Polymeric Nanoparticles. AAPS J. 2023, 25, 81. [Google Scholar] [CrossRef] [PubMed]
- Francisca, D.; Azevedo, M.; Sousa, F.; Osório, H.; Campos, D.; Sampaio, P.; Gomes, J.; Sarmento, B.; Reis, C.A. Polymeric Nanoparticles Targeting Sialyl-Tn in Gastric Cancer: A Live Tracking under Flow Conditions. Mater. Today Bio 2022, 16, 100417. [Google Scholar] [CrossRef]
- Prashant, K.; Jain, K.; Jain, N.K. Dendrimer as Nanocarrier for Drug Delivery. Prog. Polym. Sci. 2014, 39, 268–307. [Google Scholar] [CrossRef]
- Fatemeh, N.; Fanaei, H.; Imani, A.; Vahedian, J.; Amoli, F.A.; Ghorbi, J.; Sohanaki, H.; Mohammadi, S.M.; Golchoobian, R. Evaluation of Nanocarrier Targeted Drug Delivery of Capecitabine-Pamam Dendrimer Complex in a Mice Colorectal Cancer Model. Acta Medica Iran. 2016, 54, 485–493. [Google Scholar]
- Rasha, I.; Tobaiqy, M.; Al Faraj, A. Optimizing Use of Theranostic Nanoparticles as a Life-Saving Strategy for Treating COVID-19 Patients. Theranostics 2020, 10, 5932. [Google Scholar] [CrossRef]
- Lyubov, A.K.; Apartsin, E.K.; Nizolenko, L.F.; Karpenko, L.I. Dendrimer-Mediated Delivery of DNA and Rna Vaccines. Pharmaceutics 2023, 15, 1106. [Google Scholar] [CrossRef]
- Cao, Z.; Ren, L.; Niu, L.; Zhao, R.; Liu, N.; Zhuang, Q.; Pan, F.; Liu, Z.; Cheng, Y.; Yang, Y. A Coordinative Dendrimer-Based Nanovaccine for Cancer Treatment. Matter 2023, 6, 3574–3597. [Google Scholar] [CrossRef]
- Shen, S.; Gao, Y.; Ouyang, Z.; Jia, B.; Shen, M.; Shi, X. Photothermal-Triggered Dendrimer Nanovaccines Boost Systemic Antitumor Immunity. J. Control. Release 2023, 355, 171–183, Erratum in J. Control. Release 2025, 386, 114112. [Google Scholar] [CrossRef]
- Laredj-Bourezg, F.; Bolzinger, M.-A.; Pelletier, J.; Chevalier, Y. Pickering Emulsions Stabilized by Biodegradable Block Copolymer Micelles for Controlled Topical Drug Delivery. Int. J. Pharm. 2017, 531, 134–142. [Google Scholar] [CrossRef]
- Zhang, J.; Ratanasirintrawoot, S.; Chandrasekaran, S.; Wu, Z.; Ficarro, S.B.; Yu, C.; Ross, C.A.; Cacchiarelli, D.; Xia, Q.; Seligson, M.; et al. Lin28 Regulates Stem Cell Metabolism and Conversion to Primed Pluripotency. Cell Stem Cell 2016, 19, 66–80. [Google Scholar] [CrossRef]
- Kozaka, S.; Tahara, Y.; Wakabayashi, R.; Nakata, T.; Ueda, T.; Kamiya, N.; Goto, M. Transcutaneous Cancer Vaccine Using a Reverse Micellar Antigen Carrier. Mol. Pharm. 2020, 17, 645–655. [Google Scholar] [CrossRef]
- Qin, Y.; Zeng, W.-F.; Liang, W. Development of Therapeutic Cancer Vaccines Using Nanomicellar Preparations. Oncol. Transl. Med. 2023, 9, 265–268. [Google Scholar] [CrossRef]
- Wang, C.; Xue, Y.; Markovic, T.; Li, H.; Wang, S.; Zhong, Y.; Du, S.; Zhang, Y.; Hou, X.; Yu, Y.; et al. Blood–Brain-Barrier-Crossing Lipid Nanoparticles for Mrna Delivery to the Central Nervous System. Nat. Mater. 2025, 24, 1653–1663. [Google Scholar] [CrossRef]
- Han, E.L.; Tang, S.; Kim, D.; Murray, A.M.; Swingle, K.L.; Hamilton, A.G.; Mrksich, K.; Padilla, M.S.; Palanki, R.; Li, J.J.; et al. Peptide-Functionalized Lipid Nanoparticles for Targeted Systemic Mrna Delivery to the Brain. Nano Lett. 2025, 25, 800–810. [Google Scholar] [CrossRef]
- Silberstein, S.; Spierings, E.L.H.; Kunkel, T. Celecoxib Oral Solution and the Benefits of Self-Microemulsifying Drug Delivery Systems (Smedds) Technology: A Narrative Review. Pain Ther. 2023, 12, 1109–1119. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Li, X.; Zhou, L.; Chen, W.; Marchioni, E. Protein-Based High Internal Phase Pickering Emulsions: A Review of Their Fabrication, Composition and Future Perspectives in the Food Industry. Foods 2023, 12, 482. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Wu, F.; Xu, Y.; Tang, X.; Xie, X.; Hu, R.; Ou, Y.; Wei, H.; Ye, L.; He, C.; et al. Double-Metal Ion Adjuvant Stabilized Pickering Emulsion to Amplify Humoral and Cellular Immune Responses. Nano Res. 2025, 18, 94907237. [Google Scholar] [CrossRef]
- Willi, P.; Sharma, C.P. Inorganic Nanoparticles for Targeted Drug Delivery. In Biointegration of Medical Implant Materials; Woodhead Publishing: Cambridge, UK, 2020; pp. 333–373. [Google Scholar]
- Zheng, J.; Ren, W.; Chen, T.; Jin, Y.; Li, A.; Yan, K.; Wu, Y.; Wu, A. Recent Advances in Superparamagnetic Iron Oxide Based Nanoprobes as Multifunctional Theranostic Agents for Breast Cancer Imaging and Therapy. Curr. Med. Chem. 2018, 25, 3001–3016. [Google Scholar] [CrossRef]
- Chaves, L.L.; Dourado, D.; Prunache, I.-B.; da Silva, P.M.M.; Lucena, G.T.d.S.; de Souza, Z.C.; de Moura, P.M.M.F.; Bordallo, H.N.; Formiga, F.R.; Rebouças, J.d.S. Nanocarriers of Antigen Proteins for Vaccine Delivery. Int. J. Pharm. 2024, 659, 124162. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Zhang, Y.; Yin, X.; He, Y.; Zhang, Q.; Chen, C. Layered Double Hydroxide Nanoparticles as an Adjuvant for Inactivated Foot-and-Mouth Disease Vaccine in Pigs. BMC Vet. Res. 2020, 16, 474. [Google Scholar] [CrossRef]
- Verma, N.K.; Crosbie-Staunton, K.; Satti, A.; Gallagher, S.; Ryan, K.B.; Doody, T.; McAtamney, C.; MacLoughlin, R.; Galvin, P.; Burke, C.S.; et al. Magnetic Core-Shell Nanoparticles for Drug Delivery by Nebulization. J. Nanobiotechnol. 2013, 11, 1. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.-X.; Xie, Y.; Ye, Y.-P. Iscoms and Iscomatrix. Vaccine 2009, 27, 4388–4401. [Google Scholar] [CrossRef] [PubMed]
- Barr, I.G.; Sjölander, A.; Cox, J.C. Iscoms and Other Saponin Based Adjuvants. Adv. Drug Deliv. Rev. 1998, 32, 247–271. [Google Scholar] [CrossRef]
- Lovgren, K.; Morein, B. The Requirement of Lipids for the Formation of Immunostimulating Complexes (Iscoms). Biotechnol. Appl. Biochem. 1988, 10, 161–172. [Google Scholar] [CrossRef]
- Buglione-Corbett, R.; Pouliot, K.; Marty-Roix, R.; Li, W.; West, K.; Wang, S.; Morelli, A.B.; Lien, E.; Lu, S. Reduced Myd88 Dependency of Iscomatrix™ Adjuvant in a DNA Prime-Protein Boost Hiv Vaccine. Hum. Vaccines Immunother. 2014, 10, 1078–1090. [Google Scholar] [CrossRef]
- Pearse, M.; Drane, D. Iscomatrix® Adjuvant for Antigen Delivery. Adv. Drug Deliv. Rev. 2005, 57, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Kersten, G.F.A.; Crommelin, D.J.A. Liposomes and Iscoms. Vaccine 2003, 21, 915–920. [Google Scholar] [CrossRef] [PubMed]
- Santos, P.; Almeida, F. Exosome-Based Vaccines: History, Current State, and Clinical Trials. Front. Immunol. 2021, 12, 711565. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Dong, H.; Cao, H.; Ji, X.; Luan, S.; Liu, J. Exosomes in Pathogenesis, Diagnosis, and Treatment of Alzheimer’s Disease. Med. Sci. Monit. 2019, 25, 3329. [Google Scholar] [CrossRef]
- Sun, D.; Zhuang, X.; Xiang, X.; Liu, Y.; Zhang, S.; Liu, C.; Barnes, S.; Grizzle, W.; Miller, D.; Zhang, H.-G. A Novel Nanoparticle Drug Delivery System: The Anti-Inflammatory Activity of Curcumin Is Enhanced When Encapsulated in Exosomes. Mol. Ther. 2010, 18, 1606–1614. [Google Scholar] [CrossRef]
- Saleh, A.F.; Lázaro-Ibáñez, E.; Forsgard, M.A.-M.; Shatnyeva, O.; Osteikoetxea, X.; Karlsson, F.; Heath, N.; Ingelsten, M.; Rose, J.; Harris, J.; et al. Extracellular Vesicles Induce Minimal Hepatotoxicity and Immunogenicity. Nanoscale 2019, 11, 6990–7001. [Google Scholar] [CrossRef]
- Krishnan, A.; Gangadaran, P.; Chavda, V.P.; Jogalekar, M.P.; Muthusamy, R.; Valu, D.; Vadivalagan, C.; Ramani, P.; Laishevtcev, A.; Katari, N.K.; et al. Convalescent Serum-Derived Exosomes: Attractive Niche as COVID-19 Diagnostic Tool and Vehicle for Mrna Delivery. Exp. Biol. Med. 2022, 247, 1244–1252. [Google Scholar] [CrossRef]
- Thakur, A.; Parra, D.C.; Motallebnejad, P.; Brocchi, M.; Chen, H.J. Exosomes: Small Vesicles with Big Roles in Cancer, Vaccine Development, and Therapeutics. Bioact. Mater. 2022, 10, 281–294. [Google Scholar] [CrossRef] [PubMed]
- Balachandran, B.; Yuana, Y. Extracellular Vesicles-Based Drug Delivery System for Cancer Treatment. Cogent Med. 2019, 6, 1635806. [Google Scholar] [CrossRef]
- Draz, M.S.; Wang, Y.; Chen, F.F.; Xu, Y.; Shafiee, H. Electrically Oscillating Plasmonic Nanoparticles for Enhanced DNA Vaccination against Hepatitis C Virus. Adv. Funct. Mater. 2017, 27, 1604139. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Rai, B. Effect of Size and Surface Charge of Gold Nanoparticles on Their Skin Permeability: A Molecular Dynamics Study. Sci. Rep. 2017, 7, srep45292. [Google Scholar] [CrossRef]
- Bernocchi, B.; Carpentier, R.; Lantier, I.; Ducournau, C.; Dimier-Poisson, I.; Betbeder, D. Mechanisms Allowing Protein Delivery in Nasal Mucosa Using Npl Nanoparticles. J. Control. Release 2016, 232, 42–50. [Google Scholar] [CrossRef]
- Ji, Z.; Xie, Z.; Zhang, Z.; Gong, T.; Sun, X. Engineering Intravaginal Vaccines to Overcome Mucosal and Epithelial Barriers. Biomaterials 2017, 128, 8–18. [Google Scholar] [CrossRef]
- López-Espinosa, J.; Park, P.; Holcomb, M.; Godin, B.; Villapol, S. Nanotechnology-Driven Therapies for Neurodegenerative Diseases: A Comprehensive Review. Ther. Deliv. 2024, 15, 997–1024. [Google Scholar] [CrossRef]
- Ereej, N.; Hameed, H.; Khan, M.A.; Faheem, S.; Hameed, A. Nanoparticle-Based Gene Therapy for Neurodegenerative Disorders. Mini Rev. Med. Chem. 2024, 24, 1723–1745. [Google Scholar] [CrossRef]
- Mittal, K.R.; Pharasi, N.; Sarna, B.; Singh, M.; Haider, S.; Singh, S.K.; Dua, K.; Jha, S.K.; Dey, A.; Ojha, S.; et al. Nanotechnology-Based Drug Delivery for the Treatment of Cns Disorders. Transl. Neurosci. 2022, 13, 527–546. [Google Scholar] [CrossRef]
- De Jong, W.H.; Borm, P.J. Drug Delivery and Nanoparticles: Applications and Hazards. Int. J. Nanomed. 2008, 3, 133–149. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.J.; Cutler, E.G.; Cho, H. Therapeutic Nanoplatforms and Delivery Strategies for Neurological Disorders. Nano Converg. 2018, 5, 35. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, K.; Kumar, P.S.; Rangasamy, G.; Ankitha, K.; Niyathi, V.; Manivasagan, V.; Saranya, K. Recent Advances in Nanotechnology and Its Application for Neuro-Disease: A Review. Appl. Nanosci. 2023, 13, 6631–6665. [Google Scholar] [CrossRef]
- Greish, K. Cancer Nanotechnology. In Methods in Molecular Biology; Humana Press: New York, NY, USA, 2010; p. 624. [Google Scholar]
- Mangas-Sanjuan, V.; González-Alvarez, M.; Gonzalez-Alvarez, I.; Bermejo, M. Drug Penetration across the Blood-Brain Barrier: An Overview. Ther. Deliv. 2010, 1, 535–562. [Google Scholar] [CrossRef]
- Fakhoury, M.; Takechi, R.; Al-Salami, H. Drug Permeation across the Blood-Brain Barrier: Applications of Nanotechnology. Br. J. Med. Med Res. 2015, 6, 547–556. [Google Scholar] [CrossRef]
- Zhu, Q.; Wu, S.-D.; Wu, S.-S.; Yang, P.; Sun, J.-Z.; Kang, J.-B. Biodegradable Nano-Hybrid Vehicles for Combinatorial and Targeted Drug Delivery for Glioma Treatment. J. Biomater. Tissue Eng. 2017, 7, 363–370. [Google Scholar] [CrossRef]
- Orunoğlu, M.; Kaffashi, A.; Pehlivan, S.B.; Şahin, S.; Söylemezoğlu, F.; Oğuz, K.K.; Mut, M. Effects of Curcumin-Loaded Plga Nanoparticles on the Rg2 Rat Glioma Model. Mater. Sci. Eng. C 2017, 78, 32–38. [Google Scholar] [CrossRef]
- Chung, J.Y.; Thone, M.N.; Kwon, Y.J. COVID-19 Vaccines: The Status and Perspectives in Delivery Points of View. Adv. Drug Deliv. Rev. 2021, 170, 1–25. [Google Scholar] [CrossRef]
- Bolhassani, A.; Safaiyan, S.; Rafati, S. Improvement of Different Vaccine Delivery Systems for Cancer Therapy. Mol. Cancer 2011, 10, 3. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, C. Role of Nanotechnology in Hiv/Aids Vaccine Development. Adv. Drug Deliv. Rev. 2016, 103, 76–89. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, T.; Aljaeid, B.M. Preparation, Characterization, and Potential Application of Chitosan, Chitosan Derivatives, and Chitosan Metal Nanoparticles in Pharmaceutical Drug Delivery. Drug Des. Dev. Ther. 2016, 10, 483–507. [Google Scholar] [CrossRef] [PubMed]
- Dinda, S.C.; Pattnaik, G. Nanobiotechnology-Based Drug Delivery in Brain Targeting. Curr. Pharm. Biotechnol. 2013, 14, 1264–1274. [Google Scholar] [CrossRef]
- Huo, M.; Zhao, Y.; Satterlee, A.B.; Wang, Y.; Xu, Y.; Huang, L. Tumor-Targeted Delivery of Sunitinib Base Enhances Vaccine Therapy for Advanced Melanoma by Remodeling the Tumor Microenvironment. J. Control. Release 2017, 245, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Hu, X.; Xiang, D. Nanoparticle Drug Delivery Systems: An Excellent Carrier for Tumor Peptide Vaccines. Drug Deliv. 2018, 25, 1319–1327. [Google Scholar] [CrossRef]
- Sun, W.; Khare, P.; Wang, X.; Challa, D.K.; Greenberg, B.M.; Ober, R.J.; Ward, E.S. Selective Depletion of Antigen-Specific Antibodies for the Treatment of Demyelinating Disease. Mol. Ther. 2021, 29, 1312–1323. [Google Scholar] [CrossRef]
- Sun, B.; Xia, T. Nanomaterial-Based Vaccine Adjuvants. J. Mater. Chem. B 2016, 4, 5496–5509. [Google Scholar] [CrossRef]
- Gato, W.E.; Hunter, D.A.; Byrd, I.C.; Mays, C.A.; Yau, W.; Wu, J. Assessment of the Short-Term Toxicity of TiO2 Nanofiber in Sprague Dawley Rats. Environ. Toxicol. 2017, 32, 1775–1783. [Google Scholar] [CrossRef]
- Alsaleh, N.B.; Persaud, I.; Brown, J.M. Silver Nanoparticle-Directed Mast Cell Degranulation Is Mediated through Calcium and Pi3k Signaling Independent of the High Affinity Ige Receptor. PLoS ONE 2016, 11, e0167366. [Google Scholar] [CrossRef]
- Marquardt, C.; Fritsch-Decker, S.; Al-Rawi, M.; Diabaté, S.; Weiss, C. Autophagy Induced by Silica Nanoparticles Protects Raw264. 7 Macrophages from Cell Death. Toxicology 2017, 379, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Li, P.; Liu, L.; Pan, H.; Li, H.; Cai, L.; Ma, Y. Self-Adjuvanted Nanovaccine for Cancer Immunotherapy: Role of Lysosomal Rupture-Induced Ros in Mhc Class I Antigen Presentation. Biomaterials 2016, 79, 88–100. [Google Scholar] [CrossRef] [PubMed]
- Klippstein, R.; Pozo, D. Nanotechnology-Based Manipulation of Dendritic Cells for Enhanced Immunotherapy Strategies. Nanomed. Nanotechnol. Biol. Med. 2010, 6, 523–529. [Google Scholar] [CrossRef]
- Xu, Y.; Deng, L.; Ren, H.; Zhang, X.; Huang, F.; Yue, T. Transport of Nanoparticles across Pulmonary Surfactant Monolayer: A Molecular Dynamics Study. Phys. Chem. Chem. Phys. 2017, 19, 17568–17576. [Google Scholar] [CrossRef] [PubMed]
- Siefert, A.L.; Ehrlich, A.; Corral, M.J.; Goldsmith-Pestana, K.; McMahon-Pratt, D.; Fahmy, T.M. Immunomodulatory Nanoparticles Ameliorate Disease in the Leishmania (Viannia) Panamensis Mouse Model. Biomaterials 2016, 108, 168–176. [Google Scholar] [CrossRef]
- Jain, A.; Cheng, K. The Principles and Applications of Avidin-Based Nanoparticles in Drug Delivery and Diagnosis. J. Control. Release 2017, 245, 27–40. [Google Scholar] [CrossRef]
- Shimoni, O.; Postma, A.; Yan, Y.; Scott, A.M.; Heath, J.K.; Nice, E.C.; Zelikin, A.N.; Caruso, F. Macromolecule Functionalization of Disulfide-Bonded Polymer Hydrogel Capsules and Cancer Cell Targeting. ACS Nano 2012, 6, 1463–1472. [Google Scholar] [CrossRef]
- Zahedipour, F.; Jamialahmadi, K.; Zamani, P.; Jaafari, M.R. Improving the Efficacy of Peptide Vaccines in Cancer Immunotherapy. Int. Immunopharmacol. 2023, 123, 110721. [Google Scholar] [CrossRef]
- Bijker, M.S.; Eeden, S.J.F.v.D.; Franken, K.L.; Melief, C.J.M.; van der Burg, S.H.; Offringa, R. Superior Induction of Anti-Tumor Ctl Immunity by Extended Peptide Vaccines Involves Prolonged, Dc-Focused Antigen Presentation. Eur. J. Immunol. 2008, 38, 1033–1042. [Google Scholar] [CrossRef]
- Kwon, S.; Kim, Y.-E.; Park, J.-A.; Kim, D.-S.; Kwon, H.-J.; Lee, Y. Therapeutic Effect of a Tm4sf5-Specific Peptide Vaccine against Colon Cancer in a Mouse Model. BMB Rep. 2014, 47, 215. [Google Scholar] [CrossRef]
- Nava-Parada, P.; Forni, G.; Knutson, K.L.; Pease, L.R.; Celis, E. Peptide Vaccine Given with a Toll-Like Receptor Agonist Is Effective for the Treatment and Prevention of Spontaneous Breast Tumors. Cancer Res. 2007, 67, 1326–1334. [Google Scholar] [CrossRef]
- Melero, I.; Berman, D.M.; Aznar, M.A.; Korman, A.J.; Gracia, J.L.P.; Haanen, J. Evolving Synergistic Combinations of Targeted Immunotherapies to Combat Cancer. Nat. Rev. Cancer 2015, 15, 457–472. [Google Scholar] [CrossRef]
- Vonderheide, R.H.; Domchek, S.M.; Clark, A.S. Immunotherapy for Breast Cancer: What Are We Missing? Clin. Cancer Res. 2017, 23, 2640–2646. [Google Scholar] [CrossRef] [PubMed]
- Sen, K.; Mandal, M. Second Generation Liposomal Cancer Therapeutics: Transition from Laboratory to Clinic. Int. J. Pharm. 2013, 448, 28–43. [Google Scholar] [CrossRef] [PubMed]
- Prasad, S.; Cody, V.; Saucier-Sawyer, J.K.; Saltzman, W.M.; Sasaki, C.T.; Edelson, R.L.; Birchall, M.A.; Hanlon, D.J. Polymer Nanoparticles Containing Tumor Lysates as Antigen Delivery Vehicles for Dendritic Cell–Based Antitumor Immunotherapy. Nanomed. Nanotechnol. Biol. Med. 2011, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Mocan, T.; Matea, C.; Tabaran, F.; Iancu, C.; Orasan, R.; Mocan, L. In Vitro Administration of Gold Nanoparticles Functionalized with Muc-1 Protein Fragment Generates Anticancer Vaccine Response Via Macrophage Activation and Polarization Mechanism. J. Cancer 2015, 6, 583. [Google Scholar] [CrossRef]
- Valente, F.; Astolfi, L.; Simoni, E.; Danti, S.; Franceschini, V.; Chicca, M.; Martini, A. Nanoparticle Drug Delivery Systems for Inner Ear Therapy: An Overview. J. Drug Deliv. Sci. Technol. 2017, 39, 28–35. [Google Scholar] [CrossRef]
- Chiang, C.H.; Hosseinkhani, H.; Cheng, W.S.; Chen, G.W.; Wang, C.H.; Lo, Y.L. Improving Drug Loading Efficiency and Delivery Performance of Micro–and Nanoparticle Preparations through Optimising Formulation Variables. Int. J. Nanotechnol. 2013, 10, 996–1006. [Google Scholar] [CrossRef]
- Friede, M.; Aguado, M. Need for New Vaccine Formulations and Potential of Particulate Antigen and DNA Delivery Systems. Adv. Drug Deliv. Rev. 2005, 57, 325–331. [Google Scholar] [CrossRef]
- Fan, Y.; Moon, J.J. Nanoparticle Drug Delivery Systems Designed to Improve Cancer Vaccines and Immunotherapy. Vaccines 2015, 3, 662–685. [Google Scholar] [CrossRef]
- Meir, R.; Shamalov, K.; Betzer, O.; Motiei, M.; Horovitz-Fried, M.; Yehuda, R.; Popovtzer, A.; Popovtzer, R.; Cohen, C.J. Nanomedicine for Cancer Immunotherapy: Tracking Cancer-Specific T-Cells in Vivo with Gold Nanoparticles and Ct Imaging. ACS Nano 2015, 9, 6363–6372. [Google Scholar] [CrossRef]
- Betzer, O.; Gao, Y.; Shamul, A.; Motiei, M.; Sadan, T.; Yehuda, R.; Atkins, A.; Cohen, C.J.; Shen, M.; Shi, X.; et al. Multifunctional Nanoprobe for Real-Time in Vivo Monitoring of T Cell Activation. Nanomed. Nanotechnol. Biol. Med. 2022, 46, 102596. [Google Scholar] [CrossRef]
- Rosalia, R.A.; Silva, A.L.; Camps, M.; Allam, A.; Jiskoot, W.; van der Burg, S.H.; Ossendorp, F.; Oostendorp, J. Efficient Ex Vivo Induction of T Cells with Potent Anti-Tumor Activity by Protein Antigen Encapsulated in Nanoparticles. Cancer Immunol. Immunother. 2013, 62, 1161–1173. [Google Scholar] [CrossRef]
- Heuts, J.; Jiskoot, W.; Ossendorp, F.; van der Maaden, K. Cationic Nanoparticle-Based Cancer Vaccines. Pharmaceutics 2021, 13, 596. [Google Scholar] [CrossRef]
- Liu, Y. Nanoparticle Mediated Chemo-Immunotherapy for Triple Negative Breast Cancer. Ph.D. Thesis, The University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, 2020. [Google Scholar]
- Schumacher, T.N.; Schreiber, R.D. Neoantigens in Cancer Immunotherapy. Science 2015, 348, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Besse, B.; Charrier, M.; Lapierre, V.; Dansin, E.; Lantz, O.; Planchard, D.; Le Chevalier, T.; Livartoski, A.; Barlesi, F.; Laplanche, A.; et al. Dendritic Cell-Derived Exosomes as Maintenance Immunotherapy after First Line Chemotherapy in Nsclc. Oncoimmunology 2016, 5, e1071008. [Google Scholar] [CrossRef] [PubMed]
- Bhatta, R.; Han, J.; Liu, Y.; Bo, Y.; Lee, D.; Zhou, J.; Wang, Y.; Nelson, E.R.; Chen, Q.; Zhang, X.S.; et al. Metabolic Tagging of Extracellular Vesicles and Development of Enhanced Extracellular Vesicle Based Cancer Vaccines. Nat. Commun. 2023, 14, 8047. [Google Scholar] [CrossRef] [PubMed]
- Santos-Sacchi, J. Cochlear Mechanics: No Shout but a Twist in the Absence of Prestin. Curr. Biol. 2008, 18, R304–R306. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Mehta, A.; Tong, Z.; Esser, L.; Voelcker, N.H. Development of Polymeric Nanoparticles for Blood–Brain Barrier Transfer—Strategies and Challenges. Adv. Sci. 2021, 8, 2003937. [Google Scholar] [CrossRef]
- Chan, K.L.; Poller, W.C.; Swirski, F.K.; Russo, S.J. Central Regulation of Stress-Evoked Peripheral Immune Responses. Nat. Rev. Neurosci. 2023, 24, 591–604. [Google Scholar] [CrossRef]
- Pasha, S.; Gupta, K. Various Drug Delivery Approaches to the Central Nervous System. Expert Opin. Drug Deliv. 2010, 7, 113–135. [Google Scholar] [CrossRef]
- Nance, E.; Pun, S.H.; Saigal, R.; Sellers, D.L. Drug Delivery to the Central Nervous System. Nat. Rev. Mater. 2022, 7, 314–331. [Google Scholar] [CrossRef]
- Iliff, J.J.; Wang, M.; Liao, Y.; Plogg, B.A.; Peng, W.; Gundersen, G.A.; Benveniste, H.; Vates, G.E.; Deane, R.; Goldman, S.A.; et al. A Paravascular Pathway Facilitates CSF Flow through the Brain Parenchyma and the Clearance of Interstitial Solutes, Including Amyloid β. Sci. Transl. Med. 2012, 4, 147ra11. [Google Scholar] [CrossRef]
- Park, J.; Le, Q.; Wu, Y.; Lee, J.; Oh, Y. Tolerogenic Nanovaccine for Prevention and Treatment of Autoimmune Encephalomyelitis. Adv. Mater. 2023, 35, 2202670. [Google Scholar] [CrossRef]
- Garbayo, E.; Ansorena, E.; Blanco-Prieto, M. Brain Drug Delivery Systems for Neurodegenerative Disorders. Curr. Pharm. Biotechnol. 2012, 13, 2388–2402. [Google Scholar] [CrossRef] [PubMed]
- Palmer, A.M. The Role of the Blood–Cns Barrier in Cns Disorders and Their Treatment. Neurobiol. Dis. 2010, 37, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.; Lee, S.; Park, S.; Hong, J.; Kim, C.; Cho, I.; Sohn, H.S.; Kim, K.; Park, I.W.; Yoon, S.; et al. A Therapeutic Nanovaccine That Generates Anti-Amyloid Antibodies and Amyloid-Specific Regulatory T Cells for Alzheimer’s Disease. Adv. Mater. 2023, 35, 2207719. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Jung, M.; Kim, B.-S.; Kim, Y. The Development of Therapeutic Nanovaccine That Elicits Anti-Aβ Antibodies and Aβ-Specific Regulatory T Cells for the Treatment of Alzheimer’s Disease. Alzheimer’s Dement. 2023, 19, e076411. [Google Scholar] [CrossRef]
- Hovakimyan, A.; Chilingaryan, G.; King, O.; Capocchi, J.K.; Chadarevian, J.P.; Davtyan, H.; Kniazev, R.; Agadjanyan, M.G.; Ghochikyan, A. Mrna Vaccine for Alzheimer’s Disease: Pilot Study. Vaccines 2024, 12, 659. [Google Scholar] [CrossRef]
- Schoenmaker, L.; Witzigmann, D.; Kulkarni, J.A.; Verbeke, R.; Kersten, G.; Jiskoot, W.; Crommelin, D.J. Mrna-Lipid Nanoparticle COVID-19 Vaccines: Structure and Stability. Int. J. Pharm. 2021, 601, 120586. [Google Scholar] [CrossRef]
- Kumar, R.; Aadil, K.R.; Mondal, K.; Mishra, Y.K.; Oupicky, D.; Ramakrishna, S.; Kaushik, A. Neurodegenerative Disorders Management: State-of-Art and Prospects of Nano-Biotechnology. Crit. Rev. Biotechnol. 2022, 42, 1180–1212. [Google Scholar] [CrossRef]
- Melamed, E.; Offen, D.; Shirvan, A.; Djaldetti, R.; Barzilai, A.; Ziv, I. Levodopa Toxicity and Apoptosis. Ann. Neurol. 1998, 44, S149–S154. [Google Scholar] [CrossRef]
- Ciccone, I. Ub-312 Reduces A-Synuclein in Parkinson Disease in Phase 1 Trial. Available online: https://www.neurologylive.com/view/ub-312-reduces-alpha-synuclein-pd-phase-1-trial (accessed on 25 July 2025).
- Eijsvogel, P.; Misra, P.; Concha-Marambio, L.; Boyd, J.D.; Ding, S.; Fedor, L.; Hsieh, Y.-T.; Sun, Y.S.; Vroom, M.M.; Farris, C.M.; et al. Target Engagement and Immunogenicity of an Active Immunotherapeutic Targeting Pathological A-Synuclein: A Phase 1 Placebo-Controlled Trial. Nat. Med. 2024, 30, 2631–2640. [Google Scholar] [CrossRef]
- Volc, D.; Poewe, W.; Kutzelnigg, A.; Lührs, P.; Thun-Hohenstein, C.; Schneeberger, A.; Galabova, G.; Majbour, N.; Vaikath, N.; El-Agnaf, O.; et al. Safety and Immunogenicity of the A-Synuclein Active Immunotherapeutic Pd01a in Patients with Parkinson’s Disease: A Randomised, Single-Blinded, Phase 1 Trial. Lancet Neurol. 2020, 19, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Frim, D.M.; Yee, W.M.; Isacson, O. Ngf Reduces Striatal Excitotoxic Neuronal Loss without Affecting Concurrent Neuronal Stress. NeuroReport 1993, 4, 655–658. [Google Scholar] [CrossRef] [PubMed]
- Buonaguro, L.; Tagliamonte, M. Peptide-Based Vaccine for Cancer Therapies. Front. Immunol. 2023, 14, 1210044, Erratum in Front. Immunol. 2023, 14, 1324894. [Google Scholar] [CrossRef] [PubMed]
- Satapathy, M.K.; Yen, T.-L.; Jan, J.-S.; Tang, R.-D.; Wang, J.-Y.; Taliyan, R.; Yang, C.-H. Solid Lipid Nanoparticles (Slns): An Advanced Drug Delivery System Targeting Brain through Bbb. Pharmaceutics 2021, 13, 1183. [Google Scholar] [CrossRef]
- Salzer, J.; Svenningsson, A.; Sundström, P. Neurofilament Light as a Prognostic Marker in Multiple Sclerosis. Mult. Scler. J. 2010, 16, 287–292. [Google Scholar] [CrossRef]
- Li, X.; Naeem, A.; Xiao, S.; Hu, L.; Zhang, J.; Zheng, Q. Safety Challenges and Application Strategies for the Use of Dendrimers in Medicine. Pharmaceutics 2022, 14, 1292. [Google Scholar] [CrossRef]
- Michaeli, M.F.; Ahi, G.; Ramazani, F.; Behnejad, S. The Effect of a Pain Management Program in Reducing the Pain in Patients with Multiple Sclerosis. J. Res. Health 2016, 6, 336–344. [Google Scholar]
- Luo, M.; Samandi, L.Z.; Wang, Z.; Chen, Z.J.; Gao, J. Synthetic Nanovaccines for Immunotherapy. J. Control. Release 2017, 263, 200–210. [Google Scholar] [CrossRef]
- Gomi, M.; Nakayama, Y.; Sakurai, Y.; Oyama, R.; Iwasaki, K.; Doi, M.; Liu, Y.; Hori, M.; Watanabe, H.; Hashimoto, K.; et al. Tolerogenic Lipid Nanoparticles for Delivering Self-Antigen Mrna for the Treatment of Experimental Autoimmune Encephalomyelitis. Pharmaceuticals 2023, 16, 1270. [Google Scholar] [CrossRef] [PubMed]
- Yan, L.; Park, H.R.; Kezirian, E.J.; Yook, S.; Kim, J.-H.; Joo, E.Y.; Kim, H. Altered Regional Cerebral Blood Flow in Obstructive Sleep Apnea Is Associated with Sleep Fragmentation and Oxygen Desaturation. J. Cereb. Blood Flow Metab. 2021, 41, 2712–2724. [Google Scholar] [CrossRef] [PubMed]
- Macchitella, L.; Romano, D.L.; Marinelli, C.V.; Toraldo, D.M.; Arigliani, M.; De Benedetto, M.; Angelelli, P. Neuropsychological and Socio–Cognitive Deficits in Patients with Obstructive Sleep Apnea. J. Clin. Exp. Neuropsychol. 2021, 43, 514–533. [Google Scholar] [CrossRef]
- Lal, C.; Strange, C.; Bachman, D. Neurocognitive Impairment in Obstructive Sleep Apnea. Chest 2012, 141, 1601–1610. [Google Scholar] [CrossRef] [PubMed]
- Sforza, E.; Roche, F. Sleep Apnea Syndrome and Cognition. Front. Neurol. 2012, 3, 87. [Google Scholar] [CrossRef]
- Urbano, F.; Roux, F.; Schindler, J.; Mohsenin, V. Impaired Cerebral Autoregulation in Obstructive Sleep Apnea. J. Appl. Physiol. 2008, 105, 1852–1857. [Google Scholar] [CrossRef]
- Yadav, S.K.; Kumar, R.; Macey, P.M.; Richardson, H.L.; Wang, D.J.; Woo, M.A.; Harper, R.M. Regional Cerebral Blood Flow Alterations in Obstructive Sleep Apnea. Neurosci. Lett. 2013, 555, 159–164. [Google Scholar] [CrossRef]
- Dimitrova, M.; Genov, K. Global Cognitive Performance and Assessment of Memory Functions in Obstructive Sleep Apnea. Folia Medica 2020, 62, 539–545. [Google Scholar] [CrossRef]
- Menzies, B.; Teng, A.; Burns, M.; Lah, S. Neurocognitive Outcomes of Children with Sleep Disordered Breathing: A Systematic Review with Meta-Analysis. Sleep Med. Rev. 2022, 63, 101629. [Google Scholar] [CrossRef] [PubMed]
- Sun, B.; Ma, Q.; Shen, J.; Meng, Z.; Xu, J. Up-to-Date Advance in the Relationship between Osa and Stroke: A Narrative Review. Sleep Breath 2024, 28, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Carneiro-Barrera, A.; Amaro-Gahete, F.J.; Guillén-Riquelme, A.; Jurado-Fasoli, L.; Sáez-Roca, G.; Martín-Carrasco, C.; Buela-Casal, G.; Ruiz, J.R. Effect of an Interdisciplinary Weight Loss and Lifestyle Intervention on Obstructive Sleep Apnea Severity: The Interapnea Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e228212. [Google Scholar] [CrossRef] [PubMed]
- Bailly, S.; Trzepizur, W.; Gagnadoux, F. Cardiovascular Protection in Sleep Apnea: Is It a Question of Cpap Adherence? Arch. Bronconeumol. 2023, 59, 277–279. [Google Scholar] [CrossRef]
- Robertson, C.; Herbison, P.; Harkness, M. Dental and Occlusal Changes During Mandibular Advancement Splint Therapy in Sleep Disordered Patients. Eur. J. Orthod. 2003, 25, 371–376. [Google Scholar] [CrossRef]
- Mohammadieh, A.; Sutherland, K.; Cistulli, P.A. Sleep Disordered Breathing: Management Update. Intern. Med. J. 2017, 47, 1241–1247. [Google Scholar] [CrossRef]
- Malhotra, A.; Grunstein, R.R.; Fietze, I.; Weaver, T.E.; Redline, S.; Azarbarzin, A.; Sands, S.A.; Schwab, R.J.; Dunn, J.P.; Chakladar, S.; et al. Tirzepatide for the Treatment of Obstructive Sleep Apnea and Obesity. N. Engl. J. Med. 2024, 391, 1193–1205, Erratum in N. Engl. J. Med. 2024, 391, 1464. [Google Scholar] [CrossRef]
- Andrade, A.G.; Bubu, O.M.; Varga, A.W.; Osorio, R.S. The Relationship between Obstructive Sleep Apnea and Alzheimer’s Disease. J. Alzheimer’s Dis. 2018, 64, S255–S270. [Google Scholar] [CrossRef]
- Sharma, R.A.; Varga, A.W.; Bubu, O.M.; Pirraglia, E.; Kam, K.; Parekh, A.; Wohlleber, M.; Miller, M.D.; Andrade, A.; Lewis, C.; et al. Obstructive Sleep Apnea Severity Affects Amyloid Burden in Cognitively Normal Elderly. A Longitudinal Study. Am. J. Respir. Crit. Care Med. 2018, 197, 933–943. [Google Scholar] [CrossRef]
- Jin, Y.; Du, Q.; Song, M.; Kang, R.; Zhou, J.; Zhang, H.; Ding, Y. Amyloid-Β-Targeting Immunotherapies for Alzheimer’s Disease. J. Control. Release 2024, 375, 346–365. [Google Scholar] [CrossRef]
- Balachandran, D.D.; Bashoura, L.; Sheshadri, A.; Manzullo, E.; Faiz, S.A. The Impact of Immunotherapy on Sleep and Circadian Rhythms in Patients with Cancer. Front. Oncol. 2023, 13, 1295267. [Google Scholar] [CrossRef] [PubMed]
- Gursoy-Ozdemir, Y.; Bozdag-Pehlivan, S.; Sekerdag, M. Nanotechnology Methods for Neurological Diseases and Brain Tumors Drug Delivery Across the Blood-Brain Barrier; Academic Press: Cambridge, MA, USA, 2017. [Google Scholar]
- Li, H.; Luo, Q.; Zhang, H.; Ma, X.; Gu, Z.; Gong, Q.; Luo, K. Nanomedicine Embraces Cancer Radio-Immunotherapy: Mechanism, Design, Recent Advances, and Clinical Translation. Chem. Soc. Rev. 2023, 52, 47–96. [Google Scholar] [CrossRef]
- Lee, T.J.; Haque, F.; Shu, D.; Yoo, J.Y.; Li, H.; Yokel, R.A.; Horbinski, C.; Kim, T.H.; Kim, S.-H.; Kwon, C.-H.; et al. Rna Nanoparticle as a Vector for Targeted Sirna Delivery into Glioblastoma Mouse Model. Oncotarget 2015, 6, 14766. [Google Scholar] [CrossRef]
- Mendez-Gomez, H.R.; DeVries, A.; Castillo, P.; von Roemeling, C.; Qdaisat, S.; Stover, B.D.; Xie, C.; Weidert, F.; Zhao, C.; Moor, R.; et al. Rna Aggregates Harness the Danger Response for Potent Cancer Immunotherapy. Cell 2024, 187, 2521–2535.e21. [Google Scholar] [CrossRef] [PubMed]
- Le, T.M.D.; Yoon, A.-R.; Thambi, T.; Yun, C.-O. Polymeric Systems for Cancer Immunotherapy: A Review. Front. Immunol. 2022, 13, 826876. [Google Scholar] [CrossRef]
- Jabir, N.; Tabrez, S.; Firoz, C.K.; Zaidi, S.; Baeesa, S.; Gan, S.; Shakil, S.; Kamal, M. A Synopsis of Nano-Technological Approaches toward Anti-Epilepsy Therapy: Present and Future Research Implications. Curr. Drug Metab. 2015, 16, 336–345. [Google Scholar] [CrossRef]
- Samia, O.; Hanan, R.; Kamal, E.T. Carbamazepine Mucoadhesive Nanoemulgel (Mneg) as Brain Targeting Delivery System Via the Olfactory Mucosa. Drug Deliv. 2012, 19, 58–67. [Google Scholar] [CrossRef]
- Thompson, B.J.; Ronaldson, P.T. Drug Delivery to the Ischemic Brain. Adv. Pharmacol. 2014, 71, 165–202. [Google Scholar]
- González-Nieto, D.; Fernández-Serra, R.; Pérez-Rigueiro, J.; Panetsos, F.; Martinez-Murillo, R.; Guinea, G.V. Biomaterials to Neuroprotect the Stroke Brain: A Large Opportunity for Narrow Time Windows. Cells 2020, 9, 1074. [Google Scholar] [CrossRef] [PubMed]
- Hassanzadeh, P.; Arbabi, E.; Atyabi, F.; Dinarvand, R. Ferulic Acid-Loaded Nanostructured Lipid Carriers: A Promising Nanoformulation against the Ischemic Neural Injuries. Life Sci. 2018, 193, 64–76. [Google Scholar] [CrossRef]
- Sozio, P.; D’AUrizio, E.; Iannitelli, A.; Cataldi, A.; Zara, S.; Cantalamessa, F.; Nasuti, C.; Di Stefano, A. Ibuprofen and Lipoic Acid Diamides as Potential Codrugs with Neuroprotective Activity. Arch. Pharm. 2010, 343, 133–142. [Google Scholar] [CrossRef]
- Laserra, S.; Basit, A.; Sozio, P.; Marinelli, L.; Fornasari, E.; Cacciatore, I.; Ciulla, M.; Türkez, H.; Geyikoglu, F.; Di Stefano, A. Solid Lipid Nanoparticles Loaded with Lipoyl–Memantine Codrug: Preparation and Characterization. Int. J. Pharm. 2015, 485, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Cacciatore, I.; Ciulla, M.; Fornasari, E.; Marinelli, L.; Di Stefano, A. Solid Lipid Nanoparticles as a Drug Delivery System for the Treatment of Neurodegenerative Diseases. Expert Opin. Drug Deliv. 2016, 13, 1121–1131. [Google Scholar] [CrossRef]
- Dang, H.; Meng, M.H.W.; Zhao, H.; Iqbal, J.; Dai, R.; Deng, Y.; Lv, F. Luteolin-Loaded Solid Lipid Nanoparticles Synthesis, Characterization, & Improvement of Bioavailability, Pharmacokinetics in Vitro and Vivo Studies. J. Nanoparticle Res. 2014, 16, 2347. [Google Scholar] [CrossRef]
- Loureiro, J.A.; Andrade, S.; Duarte, A.; Neves, A.R.; Queiroz, J.F.; Nunes, C.; Sevin, E.; Fenart, L.; Gosselet, F.; Coelho, M.A.N.; et al. Resveratrol and Grape Extract-Loaded Solid Lipid Nanoparticles for the Treatment of Alzheimer’s Disease. Molecules 2017, 22, 277. [Google Scholar] [CrossRef]
- Rong, H.; Qi, M.; Pan, J.; Sun, Y.; Gao, J.; Zhang, X.; Li, W.; Zhang, B.; Zhang, X.-E.; Cui, Z. Self-Assembling Nanovaccine Confers Complete Protection against Zika Virus without Causing Antibody-Dependent Enhancement. Front. Immunol. 2022, 13, 905431. [Google Scholar] [CrossRef]
- Shen, Q.; Yang, J.; Liu, R.; Liu, L.; Zhang, J.; Shen, S.; Zhang, X. Hybrid ‘Clusterbombs’ as Multifunctional Nanoplatforms Potentiate Brain Tumor Immunotherapy. Mater. Horiz. 2019, 6, 810–816. [Google Scholar] [CrossRef]
- Nie, T.; He, Z.; Zhu, J.; Chen, K.; Howard, G.P.; Pacheco-Torres, J.; Minn, I.; Zhao, P.; Bhujwalla, Z.M.; Mao, H.-Q.; et al. Non-Invasive Delivery of Levodopa-Loaded Nanoparticles to the Brain Via Lymphatic Vasculature to Enhance Treatment of Parkinson’s Disease. Nano Res. 2021, 14, 2749–2761. [Google Scholar] [CrossRef]
- Alisha, D. Next-Gen Sequencing-Driven Antigen Screening Technology in Vaccine Development. In Reverse Vaccinology; Elsevier: Amsterdam, The Netherlands, 2024; pp. 237–261. [Google Scholar]
- Ward, A.B.; Wilson, I.A. Innovations in Structure-Based Antigen Design and Immune Monitoring for Next Generation Vaccines. Curr. Opin. Immunol. 2020, 65, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Lu, G.; Shan, S.; Zainab, B.; Ayaz, Z.; He, J.; Xie, Z.; Rashid, U.; Zhang, D.; Abbasi, A.M. Novel Vaccine Design Based on Genomics Data Analysis: A Review. Scand. J. Immunol. 2021, 93, e12986. [Google Scholar] [CrossRef]
- Guimaraes, L.C.; Costa, P.A.C.; Júnior, S.R.A.S.; Ferreira, H.A.S.; Braga, A.C.S.; de Oliveira, L.C.; Figueiredo, M.M.; Shepherd, S.; Hamilton, A.; Queiroz-Junior, C.M.; et al. Nanoparticle-Based DNA Vaccine Protects against SARS-CoV-2 Variants in Female Preclinical Models. Nat. Commun. 2024, 15, 590. [Google Scholar] [CrossRef]
- Lei, J.; Qi, S.; Yu, X.; Gao, X.; Yang, K.; Zhang, X.; Cheng, M.; Bai, B.; Feng, Y.; Lu, M.; et al. Development of Mannosylated Lipid Nanoparticles for Mrna Cancer Vaccine with High Antigen Presentation Efficiency and Immunomodulatory Capability. Angew. Chem. 2024, 136, e202318515. [Google Scholar] [CrossRef]
- Chen, F.; Li, T.; Zhang, H.; Saeed, M.; Liu, X.; Huang, L.; Wang, X.; Gao, J.; Hou, B.; Lai, Y.; et al. Acid-Ionizable Iron Nanoadjuvant Augments Sting Activation for Personalized Vaccination Immunotherapy of Cancer. Adv. Mater. 2023, 35, 2209910. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Zhang, L.; Deng, W.; Lou, J.; Gao, X.; Lou, X.; Liu, Y.; Yao, X.; Sheng, Y.; Yan, Y.; et al. Spleen-Selective Co-Delivery of Mrna and Tlr4 Agonist-Loaded Lnps for Synergistic Immunostimulation and Th1 Immune Responses. J. Control. Release 2023, 357, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, K.; Sato, Y.; Okuda, K.; Iwakawa, K.; Harashima, H. Mrna-Loaded Lipid Nanoparticles Targeting Dendritic Cells for Cancer Immunotherapy. Pharmaceutics 2022, 14, 1572. [Google Scholar] [CrossRef] [PubMed]
- Kranz, L.M.; Diken, M.; Haas, H.; Kreiter, S.; Loquai, C.; Reuter, K.C.; Meng, M.; Fritz, D.; Vascotto, F.; Hefesha, H.; et al. Systemic Rna Delivery to Dendritic Cells Exploits Antiviral Defence for Cancer Immunotherapy. Nature 2016, 534, 396–401. [Google Scholar] [CrossRef]
- Weber, J.S.; Carlino, M.S.; Khattak, A.; Meniawy, T.; Ansstas, G.; Taylor, M.H.; Kim, K.B.; McKean, M.; Long, G.V.; Sullivan, R.J.; et al. Individualised Neoantigen Therapy Mrna-4157 (V940) Plus Pembrolizumab Versus Pembrolizumab Monotherapy in Resected Melanoma (Keynote-942): A Randomised, Phase 2b Study. Lancet 2024, 403, 632–644. [Google Scholar] [CrossRef]
- Rojas, L.A.; Sethna, Z.; Soares, K.C.; Olcese, C.; Pang, N.; Patterson, E.; Lihm, J.; Ceglia, N.; Guasp, P.; Chu, A.; et al. Personalized Rna Neoantigen Vaccines Stimulate T Cells in Pancreatic Cancer. Nature 2023, 618, 144–150. [Google Scholar] [CrossRef]
- Sahin, U.; Oehm, P.; Derhovanessian, E.; Jabulowsky, R.A.; Vormehr, M.; Gold, M.; Maurus, D.; Schwarck-Kokarakis, D.; Kuhn, A.N.; Omokoko, T.; et al. An Rna Vaccine Drives Immunity in Checkpoint-Inhibitor-Treated Melanoma. Nature 2020, 585, 107–112. [Google Scholar] [CrossRef]
- Palmer, M.; Parker, J.; Modi, S.; Butts, C.; Smylie, M.; Meikle, A.; Kehoe, M.; MacLean, G.; Longenecker, M. Phase I Study of the Blp25 (Muc1 Peptide) Liposomal Vaccine for Active Specific Immunotherapy in Stage Iiib/Iv Non–Small-Cell Lung Cancer. Clin. Lung Cancer 2001, 3, 49–57. [Google Scholar] [CrossRef]
- Yu, H.J.; Dickson, S.P.; Wang, P.-N.; Chiu, M.-J.; Huang, C.-C.; Chang, C.-C.; Liu, H.; Hendrix, S.B.; Dodart, J.-C.; Verma, A.; et al. Safety, Tolerability, Immunogenicity, and Efficacy of Ub-311 in Participants with Mild Alzheimer’s Disease: A Randomised, Double-Blind, Placebo-Controlled, Phase 2a Study. eBioMedicine 2023, 94, 104665. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmed, S.; Gozal, D.; Khalyfa, A. Nano-Based Vaccine Delivery Systems: Innovative Therapeutics Against Cancer and Neurological Disorders. Int. J. Mol. Sci. 2025, 26, 10316. https://doi.org/10.3390/ijms262110316
Ahmed S, Gozal D, Khalyfa A. Nano-Based Vaccine Delivery Systems: Innovative Therapeutics Against Cancer and Neurological Disorders. International Journal of Molecular Sciences. 2025; 26(21):10316. https://doi.org/10.3390/ijms262110316
Chicago/Turabian StyleAhmed, Sarfraz, David Gozal, and Abdelnaby Khalyfa. 2025. "Nano-Based Vaccine Delivery Systems: Innovative Therapeutics Against Cancer and Neurological Disorders" International Journal of Molecular Sciences 26, no. 21: 10316. https://doi.org/10.3390/ijms262110316
APA StyleAhmed, S., Gozal, D., & Khalyfa, A. (2025). Nano-Based Vaccine Delivery Systems: Innovative Therapeutics Against Cancer and Neurological Disorders. International Journal of Molecular Sciences, 26(21), 10316. https://doi.org/10.3390/ijms262110316







