Heterogeneity of Cellular Senescence, Senotyping, and Targeting by Senolytics and Senomorphics in Lung Diseases
Abstract
1. Introduction
2. Molecular Mechanisms of Cellular Senescence
2.1. DNA Damage Response (DDR) and Telomere Attrition
2.2. Mitochondrial Dysfunction and Oxidative Stress
2.3. Epigenetic Regulation of Senescence in Lung Cells
2.4. Biological States of Cellular Senescence
3. The Dichotomous Role of Senescence in Lung Health and Disease
3.1. Beneficial Roles
3.2. Detrimental Roles
4. Roles of Cellular Senescence in Lung Diseases: Role of Cellular Senescence in Lung Diseases Based on Cellular Heterogeneity
4.1. Senescence in COPD
Cellular Senescence Across Different COPD Stages and Severities
4.2. Senescence in IPF
4.3. Lung Cancer
4.4. Senescence in Acute Lung InjuryALI and Acute Respiratory Distress Syndrome (ARDS) (Including COVID-19)
4.5. Cystic Fibrosis (CF)
4.6. Pulmonary Arterial Hypertension
4.7. Senescence in Asthma
4.8. Key Proteins Implicated in Cellular Senescence in Lung Diseases
4.8.1. IL-10 (Interleukin 10)
4.8.2. TP53 (p53)
4.8.3. H2AX (H2A.X Variant Histone)
4.8.4. Cyclin-Dependent Kinase Inhibitor 2A (CDKN2A; p16INK4a)
4.8.5. GDF15
4.8.6. CDKN1A (p21)
4.8.7. TNFRSF1B (TNF Receptor Superfamily Member 1B)
4.8.8. Bcl2 L1 (BCL2 Like 1)
4.8.9. CXCL8 (IL-8)
4.8.10. IL1A (Interleukin 1 Alpha)
4.8.11. MMP12 (Matrix Metallopeptidase 12)
4.8.12. SERPINE1 (PAI-1)
4.8.13. TGFβ1 (Transforming Growth Factor Beta 1)
4.8.14. TNF (Tumor Necrosis Factor)
4.8.15. IL-6 (Interleukin 6)
4.8.16. IL-1βa (Interleukin 1 Beta)
4.8.17. MMP-8 (Matrix Metallopeptidase 8)
4.8.18. VEGFA (Vascular Endothelial Growth Factor A)
4.8.19. SIRT1
5. Therapeutics of Cellular Senescence
5.1. Senolytics
5.2. Mechanisms of Senolytic Action
5.3. Major Classes and Examples of Senolytic Agents
5.4. Early Senolytics (Dasatinib and Quercetin)
5.5. Natural Products
5.5.1. Fisetin
5.5.2. Gingerenone A
5.5.3. Bcl-2 Family Inhibitors
5.5.4. Navitoclax (ABT-263)
5.5.5. Selective Bcl-xL Inhibitors
5.5.6. HSP90 Inhibitors
5.6. Additional Classes of Senolytics
5.7. Novel Therapeutic Modalities
Senolytic CAR-T Cells
5.8. Senomorphics
5.9. Mechanisms of Senomorphic Action: Targeting SASP Regulation
5.9.1. NF-κB Pathway
5.9.2. mTOR Pathway
5.9.3. p38 MAPK Pathway
5.9.4. JAK/STAT Pathway
5.9.5. ATM Pathway
5.10. Natural Compounds and Derivatives
5.10.1. Rapamycin (Sirolimus)
5.10.2. Resveratrol
5.10.3. Curcumin
5.10.4. Other Flavonoids (Apigenin, Kaempferol, Quercetin)
5.10.5. Niacinamide (Vitamin B3) and Hyaluronic Acid
5.11. Repurposed Drugs
5.11.1. Metformin
5.11.2. Statins
5.11.3. Aspirin
5.11.4. JAK Inhibitors (Ruxolitinib)
5.11.5. ATM Inhibitors (KU-55933, KU-60019)
5.11.6. p38 MAPK Inhibitors (SB203580, UR13756, BIRB796)
5.12. Novel Synthetic Compounds
NF-κB Inhibitors (SR12343)
5.13. Therapeutic Potential and Limitations of Senomorphism
5.14. Delivery Mechanisms for Senotherapeutics
5.14.1. Nanoparticles
5.14.2. Exosomes
5.14.3. Galactose-Modified Prodrugs
5.14.4. Antibody-Drug Conjugates (ADCs)
5.15. Therapeutic Applications and Strategies
5.15.1. Current Status of Clinical Trials
5.15.2. Senotherapeutics Challenges and Opportunities
5.15.3. Biomarker Gaps: Need for In Vivo Markers of Senescence in Lungs
6. Cellular Senescence in Lung Cells and Lung Diseases: Underexplored Aspects
6.1. Senescence and Immune Cell Crosstalk in the Lung
6.1.1. Modulation of Alveolar Macrophages
6.1.2. Modulation of T Cells
6.1.3. Modulation of Neutrophils
6.1.4. The Role of Immunosenescence in Worsening Chronic Lung Disease Outcomes
6.1.5. SASP as a Driver of Immune Dysfunction in Aging Lungs
6.2. Senescence Heterogeneity and Senescence States Across Lung Cell Types
6.2.1. Fibroblasts, Endothelial Cells, Pericytes, and Club Cells May Undergo Functionally Distinct Senescence
6.2.2. Mapping Senescent Cell Subtypes with Single-Cell RNA-seq or Spatial Transcriptomics
6.3. Reversibility of Senescence and Plasticity
Pseudosenescence: Senescence Marker Expression Without Stable Growth Arrest
6.4. Role of Mechanical Stress and ECM Stiffness
6.5. Senescence-Associated Metabolic Reprogramming
6.6. Potential Target for Therapy: Metabolic Senolytics
7. Emerging Directions and Unmet Needs
7.1. Personalized Medicine: Identifying Senescent Cell Burden in Individual Patients
7.2. Role of Environmental Pollutants, Microbiome, and Circadian Rhythms in Lung Senescence
7.3. Clinical Translation of Senescence-Targeted Therapies: Challenges and Progresses
8. Future Perspectives
9. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviation
| Abbreviation | Full Form |
| DDR | DNA Damage Response |
| SASP | Senescence-Associated Secretory Phenotype |
| COPD | Chronic Obstructive Pulmonary Disease |
| IPF | Idiopathic Pulmonary Fibrosis |
| OIS | Oncogene-Induced Senescence |
| TIS | Therapy-Induced Senescence |
| MiDAS | Mitochondrial Dysfunction-Associated Senescence |
| AMPK | AMP-activated Protein Kinase |
| AT2 | Alveolar Type II Cells |
| ECM | Extracellular Matrix |
| ROS | Reactive Oxygen Species |
| PDGF-AA | Platelet-Derived Growth Factor-AA |
| MMPs | Matrix Metalloproteinases |
| p53 | Tumor Suppressor Protein 53 |
| p21 | Cyclin-Dependent Kinase Inhibitor 1 |
| p16 | Cyclin-Dependent Kinase Inhibitor 4A |
| Rb | Retinoblastoma |
| ALI | Acute Lung Injury |
| ARDS | Acute Respiratory Distress Syndrome |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome Coronavirus 2 |
| EVs | Extracellular Vesicles |
| rhCC16 | Recombinant Human Clara Cell Protein 16 |
| SIRT1 | Sirtuin 1 |
| PAI-1 | Plasminogen Activator Inhibitor-1 |
| TGF-β | Transforming Growth Factor Beta |
| CTGF | Connective Tissue Growth Factor |
| PDGF | Platelet-Derived Growth Factor |
| PAECs | Pulmonary Artery Endothelial Cells |
| PASMCs | Pulmonary Artery Smooth Muscle Cells |
| YWHAZ | Tyrosine 3-Monooxygenase/Tryptophan 5-Monooxygenase Activation Protein Zeta |
| ABT-737 | Senolytic Therapy Drug |
| FOXO4-DRI | Forkhead Box O4-Drug Resistance Inhibitor |
| SA-β-Gal | Senescence-Associated β-Galactosidase |
| γH2A.X | Gamma-Histone H2A Variant X |
| DNAmAge | DNA Methylation Age |
| AgeAcc | Age Acceleration |
| WGCNA | Weighted Gene Co-Expression Network Analysis |
| IL-10 | Interleukin 10 |
| TP53 | Tumor Protein 53 |
| H2AX | H2A.X Variant Histone |
| CDKN2A | Cyclin-Dependent Kinase Inhibitor 2A |
| GDF15 | Growth Differentiation Factor 15 |
| CDKN1A | Cyclin-Dependent Kinase Inhibitor 1A |
| TNFRSF1B | Tumor Necrosis Factor Receptor Superfamily Member 1B |
| Bcl2 L1 | BCL2 Like 1 |
| CXCL8 | C-X-C Motif Chemokine Ligand 8 |
| IL1A | Interleukin 1 Alpha |
| MMP12 | Matrix Metallopeptidase 12 |
| SERPINE1 | Serine Protease Inhibitor, Clade E, Member 1 (Plasminogen Activator Inhibitor-1) |
| TGFβ1 | Transforming Growth Factor Beta 1 |
| TNF | Tumor Necrosis Factor |
| IL-6 | Interleukin 6 |
| IL-1β | Interleukin 1 Beta |
| MMP-8 | Matrix Metallopeptidase 8 |
| VEGFA | Vascular Endothelial Growth Factor A |
| SnCs | Senescent Cells |
| NF-κB | Nuclear Factor Kappa B |
| mTOR | Mammalian Target of Rapamycin |
| p38 MAPK | p38 Mitogen-Activated Protein Kinase |
| JAK/STAT | Janus Kinase/Signal Transducer and Activator of Transcription |
| ATM | Ataxia Telangiectasia Mutated |
| STACs | Sirtuin-Activating Compounds |
| Nrf2 | Nuclear Factor Erythroid 2-Related Factor 2 |
| DAMPs | Damage-Associated Molecular Patterns |
| TAME | Targeting Aging with Metformin |
| eNOS | Endothelial Nitric Oxide Synthase |
| Ruxolitinib | JAK Inhibitor |
| Rapalogs | Rapamycin Analogs |
| SR12343 | NF-κB Inhibitor |
References
- Gorgoulis, V.; Adams, P.D.; Alimonti, A.; Bennett, D.C.; Bischof, O.; Bishop, C.; Campisi, J.; Collado, M.; Evangelou, K.; Ferbeyre, G.; et al. Cellular Senescence: Defining a Path Forward. Cell 2019, 179, 813–827. [Google Scholar] [CrossRef]
- Herranz, N.; Gil, J. Mechanisms and functions of cellular senescence. J. Clin. Investig. 2018, 128, 1238–1246. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Ji, S. Cellular senescence: Molecular mechanisms and pathogenicity. J. Cell. Physiol. 2018, 233, 9121–9135. [Google Scholar] [CrossRef] [PubMed]
- Calabrò, A.; Accardi, G.; Aiello, A.; Caruso, C.; Galimberti, D.; Candore, G. Senotherapeutics to Counteract Senescent Cells Are Prominent Topics in the Context of Anti-Ageing Strategies. Int. J. Mol. Sci. 2024, 25, 1792. [Google Scholar] [CrossRef] [PubMed]
- Dimri, G.P.; Lee, X.; Basile, G.; Acosta, M.; Scott, G.; Roskelley, C.; Medrano, E.E.; Linskens, M.; Rubelj, I.; Pereira-Smith, O.; et al. A biomarker that identifies senescent human cells in culture and in aging skin in vivo. Proc. Natl. Acad. Sci. USA 1995, 92, 9363–9367. [Google Scholar] [CrossRef]
- Coppé, J.-P.; Desprez, P.-Y.; Krtolica, A.; Campisi, J. The senescence-associated secretory phenotype: The dark side of tumor suppression. Annu. Rev. Pathol. 2010, 5, 99–118. [Google Scholar] [CrossRef]
- Basisty, N.; Kale, A.; Jeon, O.H.; Kuehnemann, C.; Payne, T.; Rao, C.; Holtz, A.; Shah, S.; Sharma, V.; Ferrucci, L.; et al. A proteomic atlas of senescence-associated secretomes for aging biomarker development. PLoS Biol. 2020, 18, e3000599. [Google Scholar] [CrossRef]
- Borghesan, M.; Hoogaars, W.; Varela-Eirin, M.; Talma, N.; Demaria, M. A Senescence-Centric View of Aging: Implications for Longevity and Disease. Trends Cell Biol. 2020, 30, 777–791. [Google Scholar] [CrossRef]
- d’Adda di Fagagna, F.; Reaper, P.M.; Clay-Farrace, L.; Fiegler, H.; Carr, P.; Von Zglinicki, T.; Jackson, S.P. A DNA damage checkpoint response in telomere-initiated senescence. Nature 2003, 426, 194–198. [Google Scholar] [CrossRef]
- Hayflick, L.; Moorhead, P.S. The serial cultivation of human diploid cell strains. Exp. Cell Res. 1961, 25, 585–621. [Google Scholar] [CrossRef]
- Parimon, T.; Chen, P.; Stripp, B.R.; Liang, J.; Jiang, D.; Noble, P.W.; Parks, W.C.; Yao, C. Senescence of alveolar epithelial progenitor cells: A critical driver of lung fibrosis. Am. J. Physiol. Physiol. 2023, 325, C483–C495. [Google Scholar] [CrossRef] [PubMed]
- Okuda, R.; Aoshiba, K.; Matsushima, H.; Ogura, T.; Okudela, K.; Ohashi, K. Cellular senescence and senescence-associated secretory phenotype: Comparison of idiopathic pulmonary fibrosis, connective tissue disease-associated interstitial lung disease, and chronic obstructive pulmonary disease. J. Thorac. Dis. 2019, 11, 857–864. [Google Scholar] [CrossRef] [PubMed]
- Sundar, I.K.; Rashid, K.; Gerloff, J.; Li, D.; Rahman, I. Genetic Ablation of p16INK4a Does Not Protect against Cellular Senescence in Mouse Models of Chronic Obstructive Pulmonary Disease/Emphysema. Am. J. Respir. Cell Mol. Biol. 2018, 59, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Rashid, K.; Sundar, I.K.; Gerloff, J.; Li, D.; Rahman, I. Lung cellular senescence is independent of aging in a mouse model of COPD/emphysema. Sci. Rep. 2018, 8, 9023. [Google Scholar] [CrossRef]
- Serrano, M.; Lin, A.W.; McCurrach, M.E.; Beach, D.; Lowe, S.W. Oncogenic ras Provokes Premature Cell Senescence Associated with Accumulation of p53 and p16INK4a. Cell 1997, 88, 593–602. [Google Scholar] [CrossRef]
- Pribluda, A.; Elyada, E.; Wiener, Z.; Hamza, H.; Goldstein, R.E.; Biton, M.; Burstain, I.; Morgenstern, Y.; Brachya, G.; Billauer, H.; et al. A senescence-inflammatory switch from cancer-inhibitory to cancer-promoting mechanism. Cancer Cell 2013, 24, 242–256. [Google Scholar] [CrossRef]
- Ewald, J.A.; Desotelle, J.A.; Wilding, G.; Jarrard, D.F. Therapy-induced senescence in cancer. J. Natl. Cancer Inst. 2010, 102, 1536–1546. [Google Scholar] [CrossRef]
- Schmitt, C.A.; Fridman, J.S.; Yang, M.; Lee, S.; Baranov, E.; Hoffman, R.M.; Lowe, S.W. A senescence program controlled by p53 and P16INK4a contributes to the outcome of cancer therapy. Cell 2002, 109, 335–346. [Google Scholar] [CrossRef]
- Bajtai, E.; Kiss, C.; Bakos, É.; Langó, T.; Lovrics, A.; Schád, É.; Tisza, V.; Hegedűs, K.; Fürjes, P.; Szabó, Z.; et al. Therapy-induced senescence is a transient drug resistance mechanism in breast cancer. Mol. Cancer 2025, 24, 128. [Google Scholar] [CrossRef]
- Wiley, C.D.; Velarde, M.C.; Lecot, P.; Liu, S.; Sarnoski, E.A.; Freund, A.; Shirakawa, K.; Lim, H.W.; Davis, S.S.; Ramanathan, A.; et al. Mitochondrial Dysfunction Induces Senescence with a Distinct Secretory Phenotype. Cell Metab. 2016, 23, 303–314. [Google Scholar] [CrossRef]
- Muñoz-Espín, D.; Cañamero, M.; Maraver, A.; Gómez-López, G.; Contreras, J.; Murillo-Cuesta, S.; Rodríguez-Baeza, A.; Varela-Nieto, I.; Ruberte, J.; Collado, M.; et al. Programmed cell senescence during mammalian embryonic development. Cell 2013, 155, 1104–1118. [Google Scholar] [CrossRef]
- Acosta, J.C.; Banito, A.; Wuestefeld, T.; Georgilis, A.; Janich, P.; Morton, J.P.; Athineos, D.; Kang, T.-W.; Lasitschka, F.; Andrulis, M.; et al. A complex secretory program orchestrated by the inflammasome controls paracrine senescence. Nat. Cell Biol. 2013, 15, 978–990. [Google Scholar] [CrossRef]
- Rattanavirotkul, N.; Kirschner, K.; Chandra, T. Induction and transmission of oncogene-induced senescence. Cell. Mol. Life Sci. 2021, 78, 843–852. [Google Scholar] [CrossRef] [PubMed]
- Mastri, M.; Tracz, A.; Lee, C.R.; Dolan, M.; Attwood, K.; Christensen, J.G.; Liu, S.; Ebos, J.M. A Transient Pseudosenescent Secretome Promotes Tumor Growth after Antiangiogenic Therapy Withdrawal. Cell Rep. 2018, 25, 3706–3720.e8. [Google Scholar] [CrossRef] [PubMed]
- Reimann, M.; Lee, S.; Schmitt, C.A. Cellular senescence: Neither irreversible nor reversible. J. Exp. Med. 2024, 221, e20232136. [Google Scholar] [CrossRef]
- Campisi, J.; d’Adda di Fagagna, F. Cellular senescence: When bad things happen to good cells. Nat. Rev. Mol. Cell Biol. 2007, 8, 729–740. [Google Scholar] [CrossRef] [PubMed]
- Chang-Chien, J.; Huang, J.-L.; Tsai, H.-J.; Wang, S.-L.; Kuo, M.-L.; Yao, T.-C. Particulate matter causes telomere shortening and increase in cellular senescence markers in human lung epithelial cells. Ecotoxicol. Environ. Saf. 2021, 222, 112484. [Google Scholar] [CrossRef]
- Eckhardt, C.M.; Wu, H. Environmental Exposures and Lung Aging: Molecular Mechanisms and Implications for Improving Respiratory Health. Curr. Environ. Health Rep. 2021, 8, 281–293. [Google Scholar] [CrossRef]
- Tsuji, T.; Aoshiba, K.; Nagai, A. Cigarette smoke induces senescence in alveolar epithelial cells. Am. J. Respir. Cell Mol. Biol. 2004, 31, 643–649. [Google Scholar] [CrossRef]
- Miwa, S.; Kashyap, S.; Chini, E.; von Zglinicki, T. Mitochondrial dysfunction in cell senescence and aging. J. Clin. Investig. 2022, 132, e158447. [Google Scholar] [CrossRef]
- Ahmad, T.; Sundar, I.K.; Lerner, C.A.; Gerloff, J.; Tormos, A.M.; Yao, H.; Rahman, I. Impaired mitophagy leads to cigarette smoke stress-induced cellular senescence: Implications for chronic obstructive pulmonary disease. FASEB J. 2015, 29, 2912–2929. [Google Scholar] [CrossRef]
- O’rEilly, S.; Markiewicz, E.; Idowu, O.C. Aging, senescence, and cutaneous wound healing—A complex relationship. Front. Immunol. 2024, 15, 1429716. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.; Wallace, J.; Peterson, A.L.; Scaffa, A.; Rizal, S.; Hegarty, K.; Maeda, H.; Chang, J.L.; Oulhen, N.; Kreiling, J.A.; et al. Timing and cell specificity of senescence drives postnatal lung development and injury. Nat. Commun. 2023, 14, 273. [Google Scholar] [CrossRef] [PubMed]
- Dennery, P.A.; Yao, H. Emerging role of cellular senescence in normal lung development and perinatal lung injury. Chin. Med. J.-Pulm. Crit. Care Med. 2024, 2, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Schafer, M.J.; White, T.A.; Iijima, K.; Haak, A.J.; Ligresti, G.; Atkinson, E.J.; Oberg, A.L.; Birch, J.; Salmonowicz, H.; Zhu, Y.; et al. Cellular senescence mediates fibrotic pulmonary disease. Nat. Commun. 2017, 8, 14532. [Google Scholar] [CrossRef]
- Woldhuis, R.R.; Heijink, I.H.; van den Berge, M.; Timens, W.; Oliver, B.G.G.; de Vries, M.; Brandsma, C.-A. COPD-derived fibroblasts secrete higher levels of senescence-associated secretory phenotype proteins. Thorax 2021, 76, 508–511. [Google Scholar] [CrossRef]
- Wisman, M.; Kruk, D.M.L.W.; Kooistra, W.; Heijink, I.H.; Woldhuis, R.R. Lower levels of senescence in human lung mesenchymal stromal cells compared with lung fibroblasts: Implications for tissue regeneration in COPD. Am. J. Physiol. Cell. Mol. Physiol. 2025, 328, L858–L865. [Google Scholar] [CrossRef]
- Tsuji, T.; Aoshiba, K.; Nagai, A. Alveolar cell senescence in patients with pulmonary emphysema. Am. J. Respir. Crit. Care Med. 2006, 174, 886–893. [Google Scholar] [CrossRef]
- Waters, D.W.; Blokland, K.E.C.; Pathinayake, P.S.; Burgess, J.K.; Mutsaers, S.E.; Prele, C.M.; Schuliga, M.; Grainge, C.L.; Knight, D.A. Fibroblast senescence in the pathology of idiopathic pulmonary fibrosis. Am. J. Physiol. Lung Cell. Mol. Physiol. 2018, 315, L162–L172. [Google Scholar] [CrossRef]
- Nyunoya, T.; Monick, M.; Lysek, G.; Aykinburns, N. Cigarette smoke induces cellular senescence. Am. J. Respir. Cell Mol. Biol. 2006, 35, 681–688. [Google Scholar] [CrossRef]
- Alder, J.K.; Chen, J.J.-L.; Lancaster, L.; Danoff, S.; Su, S.-C.; Cogan, J.D.; Vulto, I.; Xie, M.; Qi, X.; Tuder, R.M.; et al. Short telomeres are a risk factor for idiopathic pulmonary fibrosis. Proc. Natl. Acad. Sci. USA 2008, 105, 13051–13056. [Google Scholar] [CrossRef]
- Baek, K.-H.; Bhang, D.; Zaslavsky, A.; Wang, L.-C.; Vachani, A.; Kim, C.F.; Albelda, S.M.; Evan, G.I.; Ryeom, S. Thrombospondin-1 mediates oncogenic Ras–induced senescence in premalignant lung tumors. J. Clin. Investig. 2013, 123, 4375–4389. [Google Scholar] [CrossRef]
- Tripathi, U.; Nchioua, R.; Prata, L.G.P.L.; Zhu, Y.; Gerdes, E.O.W.; Giorgadze, N.; Pirtskhalava, T.; Parker, E.; Xue, A.; Espindola-Netto, J.M.; et al. SARS-CoV-2 causes senescence in human cells and exacerbates the senescence-associated secretory phenotype through TLR-3. Aging 2021, 13, 21838–21854. [Google Scholar] [CrossRef]
- Matthay, M.A.; Hendrickson, C.M. Viral pathogens and acute lung injury: Investigations inspired by the SARS epidemic and the 2009 H1N1 influenza pandemic. Semin. Respir. Crit. Care Med. 2013, 34, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Kellogg, D.L.; Musi, N.; Nambiar, A.M. Cellular Senescence in Idiopathic Pulmonary Fibrosis. Curr. Mol. Biol. Rep. 2021, 7, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Woldhuis, R.R.; De Vries, M.; Timens, W.; van den Berge, M.; DeMaria, M.; Oliver, B.G.G.; Heijink, I.H.; Brandsma, C.-A. Link between increased cellular senescence and extracellular matrix changes in COPD. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2020, 319, L48–L60. [Google Scholar] [CrossRef] [PubMed]
- Barkauskas, C.E.; Cronce, M.J.; Rackley, C.R.; Bowie, E.J.; Keene, D.R.; Stripp, B.R.; Randell, S.H.; Noble, P.W.; Hogan, B.L.M. Type 2 alveolar cells are stem cells in adult lung. J. Clin. Investig. 2013, 123, 3025–3036. [Google Scholar] [CrossRef]
- Ruysseveldt, E.; Martens, K.; Steelant, B. Airway Basal Cells, Protectors of Epithelial Walls in Health and Respiratory Diseases. Front. Allergy 2021, 2, 787128. [Google Scholar] [CrossRef]
- Desai, T.J.; Brownfield, D.G.; Krasnow, M.A. Alveolar progenitor and stem cells in lung development, renewal and cancer. Nature 2014, 507, 190–194. [Google Scholar] [CrossRef]
- Han, S.; Budinger, G.S.; Gottardi, C.J. Alveolar epithelial regeneration in the aging lung. J. Clin. Investig. 2023, 133, e170504. [Google Scholar] [CrossRef]
- Gurkar, A.U.; Gerencser, A.A.; Mora, A.L.; Nelson, A.C.; Zhang, A.R.; Lagnado, A.B.; Enninful, A.; Benz, C.; Furman, D.; Beaulieu, D.; et al. Spatial mapping of cellular senescence: Emerging challenges and opportunities. Nat. Aging 2023, 3, 776–790. [Google Scholar] [CrossRef]
- Cohn, R.L.; Gasek, N.S.; Kuchel, G.A.; Xu, M. The heterogeneity of cellular senescence: Insights at the single-cell level. Trends Cell Biol. 2023, 33, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Sanborn, M.A.; Wang, X.; Gao, S.; Dai, Y.; Rehman, J. Unveiling the cell-type-specific landscape of cellular senescence through single-cell transcriptomics using SenePy. Nat. Commun. 2025, 16, 1884. [Google Scholar] [CrossRef] [PubMed]
- Bueno, M.; Calyeca, J.; Rojas, M.; Mora, A.L. Mitochondria dysfunction and metabolic reprogramming as drivers of idiopathic pulmonary fibrosis. Redox Biol. 2020, 33, 101509. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Xi, Q.; Li, X.; Liu, H. Mitochondrial dysfunction and alveolar type II epithelial cell senescence: The destroyer and rescuer of idiopathic pulmonary fibrosis. Front. Cell Dev. Biol. 2025, 13, 1535601. [Google Scholar] [CrossRef]
- Cuevas-Mora, K.; Roque, W.; Shaghaghi, H.; Gochuico, B.R.; Rosas, I.O.; Summer, R.; Romero, F. Hermansky-Pudlak syndrome-2 alters mitochondrial homeostasis in the alveolar epithelium of the lung. Respir. Res. 2021, 22, 49. [Google Scholar] [CrossRef]
- Su, W.; Guo, Y.; Wang, Q.; Ma, L.; Zhang, Q.; Zhang, Y.; Geng, Y.; Jin, T.; Guo, J.; Yang, R.; et al. YAP1 inhibits the senescence of alveolar epithelial cells by targeting Prdx3 to alleviate pulmonary fibrosis. Exp. Mol. Med. 2024, 56, 1643–1654. [Google Scholar] [CrossRef]
- Yu, Y.; Chu, C.; Wang, K.; Li, Y.; Mao, Z.; Hu, L.; Chen, F. YAP/TAZ activation mediates PQ-induced lung fibrosis by sustaining senescent pulmonary epithelial cells. Respir. Res. 2024, 25, 212. [Google Scholar] [CrossRef]
- Ovadya, Y.; Landsberger, T.; Leins, H.; Vadai, E.; Gal, H.; Biran, A.; Yosef, R.; Sagiv, A.; Agrawal, A.; Shapira, A.; et al. Impaired immune surveillance accelerates accumulation of senescent cells and aging. Nat. Commun. 2018, 9, 5435. [Google Scholar] [CrossRef]
- Parikh, P.; Wicher, S.; Khandalavala, K.; Pabelick, C.M.; Britt, R.D., Jr.; Prakash, Y.S. Cellular senescence in the lung across the age spectrum. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2019, 316, L826–L842. [Google Scholar] [CrossRef]
- Freund, A.; Patil, C.K.; Campisi, J. p38MAPK is a novel DNA damage response-independent regulator of the senescence-associated secretory phenotype. EMBO J. 2011, 30, 1536–1548. [Google Scholar] [CrossRef] [PubMed]
- Ajoolabady, A.; Pratico, D.; Bahijri, S.; Eldakhakhny, B.; Tuomilehto, J.; Wu, F.; Ren, J. Hallmarks and mechanisms of cellular senescence in aging and disease. Cell Death Discov. 2025, 11, 364. [Google Scholar] [CrossRef] [PubMed]
- Di Micco, R.; Krizhanovsky, V.; Baker, D.; d’Adda di Fagagna, F. Cellular senescence in ageing: From mechanisms to therapeutic opportunities. Nat. Rev. Mol. Cell Biol. 2021, 22, 75–95. [Google Scholar] [CrossRef]
- Di Micco, R.; Krizhanovsky, V.; Baker, D.; d’Adda di Fagagna, F. HDAC4 degradation during senescence unleashes an epigenetic program driven by AP-1/p300 at selected enhancers and super-enhancers. Genome Biol. 2021, 22, 129. [Google Scholar] [CrossRef]
- Ferrucci, L.; Zampino, M. A mitochondrial root to accelerated ageing and frailty. Nat. Rev. Endocrinol. 2020, 16, 133–134. [Google Scholar] [CrossRef]
- Kuwano, K.; Araya, J.; Hara, H.; Minagawa, S.; Takasaka, N.; Ito, S.; Kobayashi, K.; Nakayama, K. Cellular senescence and autophagy in the pathogenesis of chronic obstructive pulmonary disease (COPD) and idiopathic pulmonary fibrosis (IPF). Respir. Investig. 2016, 54, 397–406. [Google Scholar] [CrossRef]
- Oit-Wiscombe, I.; Virag, L.; Soomets, U.; Altraja, A. Increased DNA damage in progression of COPD: A response by poly(ADP-Ribose) polymerase-1. PLoS ONE 2013, 8, e70333. [Google Scholar] [CrossRef]
- Romaniello, D.; Gelfo, V.; Pagano, F.; Sgarzi, M.; Morselli, A.; Girone, C.; Filippini, D.M.; D’uVa, G.; Lauriola, M. IL-1 and senescence: Friends and foe of EGFR neutralization and immunotherapy. Front. Cell Dev. Biol. 2022, 10, 1083743. [Google Scholar] [CrossRef]
- Brandsma, C.-A.; de Vries, M.; Costa, R.; Woldhuis, R.R.; Königshoff, M.; Timens, W. Lung ageing and COPD: Is there a role for ageing in abnormal tissue repair? Eur. Respir. Rev. 2017, 26, 170073. [Google Scholar] [CrossRef]
- Mora, A.L.; Bueno, M.; Rojas, M. Mitochondria in the spotlight of aging and idiopathic pulmonary fibrosis. J. Clin. Investig. 2017, 127, 405–414. [Google Scholar] [CrossRef]
- Bueno, M.; Lai, Y.-C.; Romero, Y.; Brands, J.; Croix, C.M.S.; Kamga, C.; Corey, C.; Herazo-Maya, J.D.; Sembrat, J.; Lee, J.S.; et al. PINK1 deficiency impairs mitochondrial homeostasis and promotes lung fibrosis. J. Clin. Investig. 2015, 125, 521–538. [Google Scholar] [CrossRef]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The hallmarks of aging. Cell 2013, 153, 1194–1217. [Google Scholar] [CrossRef]
- Yao, H.; Rahman, I. Role of histone deacetylase 2 in epigenetics and cellular senescence: Implications in lung inflammaging and COPD. Am. J. Physiol. Lung Cell. Mol. Physiol. 2012, 303, L557–L566. [Google Scholar] [CrossRef]
- Rezwan, F.I.; Imboden, M.; Amaral, A.F.; Wielscher, M.; Jeong, A.; Triebner, K.; Real, F.G.; Jarvelin, M.-R.; Jarvis, D.; Probst-Hensch, N.M.; et al. Association of adult lung function with accelerated biological aging. Aging 2020, 12, 518–542. [Google Scholar] [CrossRef]
- Wang, C.; Just, A.; Heiss, J.; Coull, B.A.; Hou, L.; Zheng, Y.; Sparrow, D.; Vokonas, P.S.; Baccarelli, A.; Schwartz, J. Biomarkers of aging and lung function in the normative aging study. Aging 2020, 12, 11942–11966. [Google Scholar] [CrossRef] [PubMed]
- Hodge, G.; Tran, H.B.; Reynolds, P.N.; Jersmann, H.; Hodge, S. Lymphocyte senescence in COPD is associated with decreased sirtuin 1 expression in steroid resistant pro-inflammatory lymphocytes. Ther. Adv. Respir. Dis. 2020, 14, 1753466620905280. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Pitcher, L.E.; Prahalad, V.; Niedernhofer, L.J.; Robbins, P.D. Targeting cellular senescence with senotherapeutics: Senolytics and senomorphics. FEBS J. 2023, 290, 1362–1383. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.; Yuan, H.; Soifer, I.; Maile, T.M.; Wang, R.Y.; Ireland, A.; O’Brien, J.J.; Goudeau, J.; Chan, L.J.; Vijay, T.; et al. Novel insights from a multiomics dissection of the Hayflick limit. eLife 2022, 11, e70283. [Google Scholar] [CrossRef]
- Shay, J.W.; Wright, W.E. Hayflick, his limit, and cellular ageing. Nat. Rev. Mol. Cell Biol. 2000, 1, 72–76. [Google Scholar] [CrossRef]
- Van Nguyen, T.; Puebla-Osorio, N.; Pang, H.; Dujka, M.E.; Zhu, C. DNA damage-induced cellular senescence is sufficient to suppress tumorigenesis: A mouse model. J. Exp. Med. 2007, 204, 1453–1461. [Google Scholar] [CrossRef]
- Yao, H.; Edirisinghe, I.; Rajendrasozhan, S.; Yang, S.-R.; Caito, S.; Adenuga, D.; Rahman, I. Cigarette smoke-mediated inflammatory and oxidative responses are strain-dependent in mice. Am. J. Physiol. Cell. Mol. Physiol. 2008, 294, L1174–L1186. [Google Scholar] [CrossRef]
- Cottage, C.T.; Peterson, N.; Kearley, J.; Berlin, A.; Xiong, X.; Huntley, A.; Zhao, W.; Brown, C.; Migneault, A.; Zerrouki, K.; et al. Targeting p16-induced senescence prevents cigarette smoke-induced emphysema by promoting IGF1/Akt1 signaling in mice. Commun. Biol. 2019, 2, 307. [Google Scholar] [CrossRef]
- Kaur, G.; Sundar, I.K.; Rahman, I. p16-3MR: A Novel Model to Study Cellular Senescence in Cigarette Smoke-Induced Lung Injuries. Int. J. Mol. Sci. 2021, 22, 4834. [Google Scholar] [CrossRef] [PubMed]
- Majewska, J.; Agrawal, A.; Mayo, A.; Roitman, L.; Chatterjee, R.; Kralova, J.S.; Landsberger, T.; Katzenelenbogen, Y.; Meir-Salame, T.; Hagai, E.; et al. p16-dependent increase of PD-L1 stability regulates immunosurveillance of senescent cells. Nat. Cell Biol. 2024, 26, 1336–1345. [Google Scholar] [CrossRef] [PubMed]
- Storer, M.; Mas, A.; Robert-Moreno, À.; Pecoraro, M.; Ortells, M.C.; Di Giacomo, V.; Yosef, R.; Pilpel, N.; Krizhanovsky, V.; Sharpe, J.; et al. Senescence Is a Developmental Mechanism that Contributes to Embryonic Growth and Patterning. Cell 2013, 155, 1119–1130. [Google Scholar] [CrossRef] [PubMed]
- Blázquez-Prieto, J.; Huidobro, C.; López-Alonso, I.; Amado-Rodriguez, L.; Martín-Vicente, P.; López-Martínez, C.; Crespo, I.; Pantoja, C.; Fernandez-Marcos, P.J.; Serrano, M.; et al. Activation of p21 limits acute lung injury and induces early senescence after acid aspiration and mechanical ventilation. Transl. Res. 2021, 233, 104–116. [Google Scholar] [CrossRef] [PubMed]
- Huidobro, C.; Martín-Vicente, P.; López-Martínez, C.; Alonso-López, I.; Amado-Rodríguez, L.; Crespo, I.; Albaiceta, G.M. Cellular and molecular features of senescence in acute lung injury. Mech. Ageing Dev. 2021, 193, 111410. [Google Scholar] [CrossRef] [PubMed]
- Feller, D.; Kun, J.; Ruzsics, I.; Rapp, J.; Sarosi, V.; Kvell, K.; Helyes, Z.; Pongracz, J.E. Cigarette Smoke-Induced Pulmonary Inflammation Becomes Systemic by Circulating Extracellular Vesicles Containing Wnt5a and Inflammatory Cytokines. Front. Immunol. 2018, 9, 1724. [Google Scholar] [CrossRef]
- Huvenne, W.; Pérez-Novo, C.A.; Derycke, L.; De Ruyck, N.; Krysko, O.; Maes, T.; Pauwels, N.; Robays, L.; Bracke, K.R.; Joos, G.; et al. Different regulation of cigarette smoke induced inflammation in upper versus lower airways. Respir. Res. 2010, 11, 100. [Google Scholar] [CrossRef]
- Tsuji, T.; Aoshiba, K.; Nagai, A. Alveolar cell senescence exacerbates pulmonary inflammation in patients with chronic obstructive pulmonary disease. Respiration 2010, 80, 59–70. [Google Scholar] [CrossRef]
- Hernandez-Gonzalez, F.; Faner, R.; Rojas, M.; Agustí, A.; Serrano, M.; Sellarés, J. Cellular Senescence in Lung Fibrosis. Int. J. Mol. Sci. 2021, 22, 7012. [Google Scholar] [CrossRef]
- Salem, I.H.; Dubé, J.; Boulet, L.; Chakir, J. Telomere shortening correlates with accelerated replicative senescence of bronchial fibroblasts in asthma. Clin. Exp. Allergy 2015, 45, 1713–1715. [Google Scholar] [CrossRef] [PubMed]
- Goyal, A.; Afzal, M.; Khan, N.H.; Goyal, K.; Srinivasamurthy, S.K.; Gupta, G.; Kumar, K.B.; Ali, H.; Rana, M.; Wong, L.S.; et al. Targeting p53-p21 signaling to enhance mesenchymal stem cell regenerative potential. Regen. Ther. 2025, 29, 352–363. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Liu, G.; Luckhardt, T.; Antony, V.; Zhou, Y.; Carter, A.B.; Thannickal, V.J.; Liu, R. Serpine 1 induces alveolar type II cell senescence through activating p53-p21-Rb pathway in fibrotic lung disease. Aging Cell 2017, 16, 1114–1124. [Google Scholar] [CrossRef] [PubMed]
- Álvarez, D.; Cárdenes, N.; Sellarés, J.; Bueno, M.; Corey, C.; Hanumanthu, V.S.; Rojas, M. IPF lung fibroblasts have a senescent phenotype. Am. J. Physiol. Lung Cell Mol. Physiol. 2017, 313, L1164–L1173. [Google Scholar] [CrossRef]
- Hernandez-Segura, A.; de Jong, T.V.; Melov, S.; Guryev, V.; Campisi, J.; DeMaria, M. Unmasking Transcriptional Heterogeneity in Senescent Cells. Curr. Biol. 2017, 27, 2652–2660.e4. [Google Scholar] [CrossRef]
- Neri, F.; Zheng, S.; Watson, M.; Desprez, P.Y.; Gerencser, A.A.; Campisi, J.; Wirtz, D.; Wu, P.H.; Schilling, B. Senescent cell heterogeneity and responses to senolytic treatment are related to cell cycle status during senescence induction. Aging (Albany NY) 2025, 17, 2063–2078. [Google Scholar] [CrossRef]
- Sun, Y. An updated landscape of cellular senescence heterogeneity: Mechanisms, technologies and senotherapies. Transl. Med. Aging 2023, 7, 46–51. [Google Scholar] [CrossRef]
- Tao, W.; Yu, Z.; Han, J.-D.J. Single-cell senescence identification reveals senescence heterogeneity, trajectory, and modulators. Cell Metab. 2024, 36, 1126–1143.e5. [Google Scholar] [CrossRef]
- Bitencourt, T.C.; Vargas, J.E.; Silva, A.O.; Fraga, L.R.; Filippi-Chiela, E. Subcellular structure, heterogeneity, and plasticity of senescent cells. Aging Cell 2024, 23, e14154. [Google Scholar] [CrossRef]
- Chien, Y.; Scuoppo, C.; Wang, X.; Fang, X.; Balgley, B.; Bolden, J.E.; Premsrirut, P.; Luo, W.; Chicas, A.; Lee, C.S.; et al. Control of the senescence-associated secretory phenotype by NF-κB promotes senescence and enhances chemosensitivity. Genes Dev. 2011, 25, 2125–2136. [Google Scholar] [CrossRef] [PubMed]
- Sundar, I.K.; Rashid, K.; Gerloff, J.; Rangel-Moreno, J.; Li, D.; Rahman, I. Genetic ablation of histone deacetylase 2 leads to lung cellular senescence and lymphoid follicle formation in COPD/emphysema. FASEB J. 2018, 32, 4955–4971. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Pitcher, L.E.; Yousefzadeh, M.J.; Niedernhofer, L.J.; Robbins, P.D.; Zhu, Y. Cellular senescence: A key therapeutic target in aging and diseases. J. Clin. Investig. 2022, 132, e158450. [Google Scholar] [CrossRef]
- Paez-Ribes, M.; González-Gualda, E.; Doherty, G.J.; Muñoz-Espín, D. Targeting senescent cells in translational medicine. EMBO Mol. Med. 2019, 11, e10234. [Google Scholar] [CrossRef]
- Demaria, M.; Ohtani, N.; Youssef, S.A.; Rodier, F.; Toussaint, W.; Mitchell, J.R.; Laberge, R.-M.; Vijg, J.; Van Steeg, H.; Dollé, M.E.; et al. An essential role for senescent cells in optimal wound healing through secretion of PDGF-AA. Dev. Cell 2014, 31, 722–733. [Google Scholar] [CrossRef]
- Krizhanovsky, V.; Yon, M.; Dickins, R.A.; Hearn, S.; Simon, J.; Miething, C.; Yee, H.; Zender, L.; Lowe, S.W. Senescence of activated stellate cells limits liver fibrosis. Cell 2008, 134, 657–667. [Google Scholar] [CrossRef]
- Cho, H.-J.; Hwang, J.-A.; Yang, E.J.; Kim, E.-C.; Kim, J.-R.; Kim, S.Y.; Kim, Y.Z.; Park, S.C.; Lee, Y.-S. Nintedanib induces senolytic effect via STAT3 inhibition. Cell Death Dis. 2022, 13, 760. [Google Scholar] [CrossRef]
- Palmer, A.K.; Xu, M.; Zhu, Y.; Pirtskhalava, T.; Weivoda, M.M.; Hachfeld, C.M.; Prata, L.G.; van Dijk, T.H.; Verkade, E.; Casaclang-Verzosa, G.; et al. Targeting senescent cells alleviates obesity-induced metabolic dysfunction. Aging Cell 2019, 18, e12950. [Google Scholar] [CrossRef]
- Du, D.; Tang, X.; Li, Y.; Gao, Y.; Chen, R.; Chen, Q.; Wen, J.; Wu, T.; Zhang, Y.; Lu, H.; et al. Senotherapy Protects against Cisplatin-Induced Ovarian Injury by Removing Senescent Cells and Alleviating DNA Damage. Oxidative Med. Cell. Longev. 2022, 2022, 9144644. [Google Scholar] [CrossRef]
- Lee, S.; Islam, M.N.; Boostanpour, K.; Aran, D.; Jin, G.; Christenson, S.; Matthay, M.A.; Eckalbar, W.L.; DePianto, D.J.; Arron, J.R.; et al. Molecular programs of fibrotic change in aging human lung. Nat. Commun. 2021, 12, 6309. [Google Scholar] [CrossRef]
- Wu, J.; Dong, F.; Wang, R.-A.; Wang, J.; Zhao, J.; Yang, M.; Gong, W.; Cui, R.; Dong, L. Central role of cellular senescence in TSLP-induced airway remodeling in asthma. PLoS ONE 2013, 8, e77795. [Google Scholar] [CrossRef]
- Sinha, S.; Castillo, V.; Espinoza, C.R.; Tindle, C.; Fonseca, A.G.; Dan, J.M.; Katkar, G.D.; Das, S.; Sahoo, D.; Ghosh, P. COVID-19 lung disease shares driver AT2 cytopathic features with Idiopathic pulmonary fibrosis. EBioMedicine 2022, 82, 104185. [Google Scholar] [CrossRef] [PubMed]
- Alder, J.K.; Barkauskas, C.E.; Limjunyawong, N.; Stanley, S.E.; Kembou, F.; Tuder, R.M.; Hogan, B.L.M.; Mitzner, W.; Armanios, M. Telomere dysfunction causes alveolar stem cell failure. Proc. Natl. Acad. Sci. USA 2015, 112, 5099–5104. [Google Scholar] [CrossRef] [PubMed]
- Orjalo, A.V.; Bhaumik, D.; Gengler, B.K.; Scott, G.K.; Campisi, J. Cell surface-bound IL-1α is an upstream regulator of the senescence-associated IL-6/IL-8 cytokine network. Proc. Natl. Acad. Sci. USA 2009, 106, 17031–17036. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Montero, P.; Londoño-Vallejo, A.; Vernot, J.-P. Senescence-associated IL-6 and IL-8 cytokines induce a self- and cross-reinforced senescence/inflammatory milieu strengthening tumorigenic capabilities in the MCF-7 breast cancer cell line. Cell Commun. Signal. 2017, 15, 17. [Google Scholar] [CrossRef]
- Rana, T.; Jiang, C.; Liu, G.; Miyata, T.; Antony, V.; Thannickal, V.J.; Liu, R.-M. PAI-1 Regulation of TGF-β1–induced Alveolar Type II Cell Senescence, SASP Secretion, and SASP-mediated Activation of Alveolar Macrophages. Am. J. Respir. Cell Mol. Biol. 2020, 62, 319–330. [Google Scholar] [CrossRef]
- Rivas, M.; Gupta, G.; Costanzo, L.; Ahmed, H.; Wyman, A.E.; Geraghty, P. Senescence: Pathogenic Driver in Chronic Obstructive Pulmonary Disease. Medicina 2022, 58, 817. [Google Scholar] [CrossRef]
- Zhou, F.; Onizawa, S.; Nagai, A.; Aoshiba, K. Epithelial cell senescence impairs repair process and exacerbates inflammation after airway injury. Respir. Res. 2011, 12, 78. [Google Scholar] [CrossRef]
- Kuźnar-Kamińska, B.; Mikuła-Pietrasik, J.; Witucka, A.; Romaniuk, A.; Konieczna, N.; Rubiś, B.; Książek, K.; Tykarski, A.; Batura-Gabryel, H. Serum from patients with chronic obstructive pulmonary disease induces senescence-related phenotype in bronchial epithelial cells. Sci. Rep. 2018, 8, 12940. [Google Scholar] [CrossRef]
- Wendisch, D.; Dietrich, O.; Mari, T.; von Stillfried, S.; Ibarra, I.L.; Mittermaier, M.; Mache, C.; Chua, R.L.; Knoll, R.; Timm, S.; et al. SARS-CoV-2 infection triggers profibrotic macrophage responses and lung fibrosis. Cell 2021, 184, 6243–6261.e27. [Google Scholar] [CrossRef]
- Bateman, G.; Guo-Parke, H.; Rodgers, A.M.; Linden, D.; Bailey, M.; Weldon, S.; Kidney, J.C.; Taggart, C.C. Airway Epithelium Senescence as a Driving Mechanism in COPD Pathogenesis. Biomedicines 2023, 11, 2072. [Google Scholar] [CrossRef] [PubMed]
- Aghali, A.; Khalfaoui, L.; Lagnado, A.B.; Drake, L.Y.; Teske, J.J.; Pabelick, C.M.; Passos, J.F.; Prakash, Y.S. Cellular senescence is increased in airway smooth muscle cells of elderly persons with asthma. Am. J. Physiol. Cell. Mol. Physiol. 2022, 323, L558–L568. [Google Scholar] [CrossRef] [PubMed]
- Kyi, P.; Hendee, K.; Hunyenyiwa, T.; Matus, K.; Mammoto, T.; Mammoto, A. Endothelial senescence mediates hypoxia-induced vascular remodeling by modulating PDGFB expression. Front. Med. 2022, 9, 908639. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, C.A.; Tchkonia, T.; Niedernhofer, L.J.; Robbins, P.D.; Kirkland, J.L.; Lee, S. COVID-19 and cellular senescence. Nat. Rev. Immunol. 2023, 23, 251–263. [Google Scholar] [CrossRef]
- Lehmann, M.; Korfei, M.; Mutze, K.; Klee, S.; Skronska-Wasek, W.; Alsafadi, H.N.; Ota, C.; Costa, R.; Schiller, H.B.; Lindner, M.; et al. Senolytic drugs target alveolar epithelial cell function and attenuate experimental lung fibrosis ex vivo. Eur. Respir. J. 2017, 50, 1602367. [Google Scholar] [CrossRef]
- Evangelou, K.; Veroutis, D.; Paschalaki, K.; Foukas, P.G.; Lagopati, N.; Dimitriou, M.; Papaspyropoulos, A.; Konda, B.; Hazapis, O.; Polyzou, A.; et al. Pulmonary infection by SARS-CoV-2 induces senescence accompanied by an inflammatory phenotype in severe COVID-19: Possible implications for viral mutagenesis. Eur. Respir. J. 2022, 60, 2102951. [Google Scholar] [CrossRef]
- Justice, J.N.; Nambiar, A.M.; Tchkonia, T.; LeBrasseur, N.K.; Pascual, R.; Hashmi, S.K.; Prata, L.; Masternak, M.M.; Kritchevsky, S.B.; Musi, N.; et al. Senolytics in idiopathic pulmonary fibrosis: Results from a first-in-human, open-label, pilot study. EBioMedicine 2019, 40, 554–563. [Google Scholar] [CrossRef]
- Childs, B.G.; Gluscevic, M.; Baker, D.J.; Laberge, R.-M.; Marquess, D.; Dananberg, J.; van Deursen, J.M. Senescent cells: An emerging target for diseases of ageing. Nat. Rev. Drug Discov. 2017, 16, 718–735. [Google Scholar] [CrossRef]
- MacNee, W. Is Chronic Obstructive Pulmonary Disease an Accelerated Aging Disease? Ann. Am. Thorac. Soc. 2016, 13 (Suppl. 5), s429–s437. [Google Scholar] [CrossRef]
- Wang, T.; Jia, Z.; Li, S.; Li, Y.; Yu, T.; Lu, T.; Shi, Y. The association between leukocyte telomere length and chronic obstructive pulmonary disease is partially mediated by inflammation: A meta-analysis and population-based mediation study. BMC Pulm. Med. 2022, 22, 320. [Google Scholar] [CrossRef]
- Yi, X.; Li, T.; Wei, X.; He, Z. Erythromycin attenuates oxidative stress-induced cellular senescence via the PI3K-mTOR signaling pathway in chronic obstructive pulmonary disease. Front. Pharmacol. 2022, 13, 1043474. [Google Scholar]
- Yao, H.; Yang, S.-R.; Edirisinghe, I.; Rajendrasozhan, S.; Caito, S.; Adenuga, D.; O’Reilly, M.A.; Rahman, I. Disruption of p21 attenuates lung inflammation induced by cigarette smoke, LPS, and fMLP in mice. Am. J. Respir. Cell Mol. Biol. 2008, 39, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Kaur, G.; Muthumalage, T.; Rahman, I. Clearance of senescent cells reverts the cigarette smoke-induced lung senescence and airspace enlargement in p16-3MR mice. Aging Cell 2023, 22, e13850. [Google Scholar] [CrossRef] [PubMed]
- Devulder, J.V.; Baker, J.R.; Fenwick, P.S.; Odqvist, L.; Donnelly, L.E.; Barnes, P.J. COPD Airway Epithelial Cell-derived Extracellular Vesicles Spread Cellular Senescence via MicroRNA-34a. Am. J. Respir. Cell Mol. Biol. 2025, 73, 210–220. [Google Scholar] [CrossRef]
- Ren, Y.J.; Sun, T.Q.; Lu, Y.; Liu, D.L.; Gao, R.; Li, T.; Pang, M. rhCC16 Suppresses Cellular Senescence and Ameliorates COPD-Like Symptoms by Activating the AMPK/Sirt1-PGC-1-α-TFAM Pathway to Promote Mitochondrial Function. J. Cell. Mol. Med. 2025, 29, e70566. [Google Scholar] [CrossRef]
- Norheim, K.L.; Ben Ezra, M.; Heckenbach, I.; Andreasson, L.M.; Eriksen, L.L.; Dyhre-Petersen, N.; Damgaard, M.V.; Berglind, M.; Pricolo, L.; Sampson, D.; et al. Effect of nicotinamide riboside on airway inflammation in COPD: A randomized, placebo-controlled trial. Nat. Aging 2024, 4, 1772–1781. [Google Scholar] [CrossRef]
- Yao, H.; Chung, S.; Hwang, J.-W.; Rajendrasozhan, S.; Sundar, I.K.; Dean, D.A.; McBurney, M.W.; Guarente, L.; Gu, W.; Rönty, M.; et al. SIRT1 protects against emphysema via FOXO3-mediated reduction of premature senescence in mice. J. Clin. Investig. 2012, 122, 2032–2045. [Google Scholar] [CrossRef]
- Rajendrasozhan, S.; Yang, S.-R.; Kinnula, V.L.; Rahman, I. SIRT1, an antiinflammatory and antiaging protein, is decreased in lungs of patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2008, 177, 861–870. [Google Scholar] [CrossRef]
- Luo, X.; Zeng, W.; Tang, J.; Liu, W.; Yang, J.; Chen, H.; Jiang, L.; Zhou, X.; Huang, J.; Zhang, S.; et al. Multi-modal transcriptomic analysis reveals metabolic dysregulation and immune responses in chronic obstructive pulmonary disease. Sci. Rep. 2024, 14, 22699. [Google Scholar] [CrossRef]
- Alfaro, E.; Díaz-García, E.; García-Tovar, S.; Galera, R.; Casitas, R.; Martínez-Cerón, E.; Torres-Vargas, M.; Padilla, J.M.; López-Fernández, C.; Pérez-Moreno, P.; et al. Effect of physical activity in lymphocytes senescence burden in patients with COPD. Am. J. Physiol. Cell. Mol. Physiol. 2024, 327, L464–L472. [Google Scholar] [CrossRef]
- Campisi, M.; Liviero, F.; Maestrelli, P.; Guarnieri, G.; Pavanello, S. DNA Methylation-Based Age Prediction and Telomere Length Reveal an Accelerated Aging in Induced Sputum Cells Compared to Blood Leukocytes: A Pilot Study in COPD Patients. Front. Med. 2021, 8, 690312. [Google Scholar] [CrossRef]
- He, Y.; Thummuri, D.; Zheng, G.; Okunieff, P.; Citrin, D.E.; Vujaskovic, Z.; Zhou, D. Cellular senescence and radiation-induced pulmonary fibrosis. Transl. Res. 2019, 209, 14–21. [Google Scholar] [CrossRef]
- Borie, R.; Crestani, B.; Bichat, H. Prevalence of telomere shortening in familial and sporadic pulmonary fibrosis is increased in men. Am. J. Respir. Crit. Care Med. 2009, 179, 1073. [Google Scholar] [CrossRef]
- Oldham, J.M. Interstitial Lung Abnormalities and Aging Biomarkers: A Mediation. Am. J. Respir. Crit. Care Med. 2021, 203, 1058–1060. [Google Scholar] [CrossRef] [PubMed]
- Pardo, A.; Selman, M. Lung Fibroblasts, Aging, and Idiopathic Pulmonary Fibrosis. Ann. Am. Thorac. Soc. 2016, 13 (Suppl. 5), S417–S421. [Google Scholar] [CrossRef] [PubMed]
- Yosef, R.; Pilpel, N.; Tokarsky-Amiel, R.; Biran, A.; Ovadya, Y.; Cohen, S.; Vadai, E.; Dassa, L.; Shahar, E.; Condiotti, R.; et al. Directed elimination of senescent cells by inhibition of BCL-W and BCL-XL. Nat. Commun. 2016, 7, 11190. [Google Scholar] [CrossRef] [PubMed]
- Sanders, Y.Y.; Hagood, J.S.; Liu, H.; Zhang, W.; Ambalavanan, N.; Thannickal, V.J. Histone deacetylase inhibition promotes fibroblast apoptosis and ameliorates pulmonary fibrosis in mice. Eur. Respir. J. 2014, 43, 1448–1458. [Google Scholar] [CrossRef]
- Sisson, T.H.; Osterholzer, J.J.; Leung, L.; Basrur, V.; Nesvizhskii, A.I.; Subbotina, N.; Warnock, M.; Torrente, D.; Virk, A.Q.; Gutor, S.S.; et al. PAI-1 interaction with sortilin-related receptor 1 is required for lung fibrosis. J. Clin. Investig. 2025, 10, e186131. [Google Scholar] [CrossRef]
- Marudamuthu, A.S.; Shetty, S.K.; Bhandary, Y.P.; Karandashova, S.; Thompson, M.; Sathish, V.; Florova, G.; Hogan, T.B.; Pabelick, C.M.; Prakash, Y.S.; et al. Plasminogen activator inhibitor-1 suppresses profibrotic responses in fibroblasts from fibrotic lungs. J. Biol. Chem. 2015, 290, 9428–9441. [Google Scholar] [CrossRef]
- Wiley, C.D.; Brumwell, A.N.; Davis, S.S.; Jackson, J.R.; Valdovinos, A.; Calhoun, C.; Alimirah, F.; Castellanos, C.A.; Ruan, R.; Wei, Y.; et al. Secretion of leukotrienes by senescent lung fibroblasts promotes pulmonary fibrosis. J. Clin. Investig. 2019, 4, e130056. [Google Scholar] [CrossRef]
- Jun, J.-I.; Lau, L.F. CCN2 induces cellular senescence in fibroblasts. J. Cell Commun. Signal. 2017, 11, 15–23. [Google Scholar] [CrossRef]
- Tsukui, T.; Sun, K.-H.; Wetter, J.B.; Wilson-Kanamori, J.R.; Hazelwood, L.A.; Henderson, N.C.; Adams, T.S.; Schupp, J.C.; Poli, S.D.; Rosas, I.O.; et al. Collagen-producing lung cell atlas identifies multiple subsets with distinct localization and relevance to fibrosis. Nat. Commun. 2020, 11, 1920. [Google Scholar] [CrossRef] [PubMed]
- Habermann, A.C.; Gutierrez, A.J.; Bui, L.T.; Yahn, S.L.; Winters, N.I.; Calvi, C.L.; Peter, L.; Chung, M.-I.; Taylor, C.J.; Jetter, C.; et al. Single-cell RNA sequencing reveals profibrotic roles of distinct epithelial and mesenchymal lineages in pulmonary fibrosis. Sci. Adv. 2020, 6, eaba1972. [Google Scholar] [CrossRef] [PubMed]
- Reyfman, P.A.; Walter, J.M.; Joshi, N.; Anekalla, K.R.; McQuattie-Pimentel, A.C.; Chiu, S.; Fernandez, R.; Akbarpour, M.; Chen, C.-I.; Ren, Z.; et al. Single-Cell Transcriptomic Analysis of Human Lung Provides Insights into the Pathobiology of Pulmonary Fibrosis. Am. J. Respir. Crit. Care Med. 2019, 199, 1517–1536. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Espín, D.; Serrano, M. Cellular senescence: From physiology to pathology. Nat. Rev. Mol. Cell Biol. 2014, 15, 482–496. [Google Scholar] [CrossRef]
- Wang, H.; Yu, Y.; Li, R.; Zhang, H.; Chen, Z.-S.; Sun, C.; Zhuang, J. Immunoregulatory mechanisms in the aging microenvironment: Targeting the senescence-associated secretory phenotype for cancer immunotherapy. Acta Pharm. Sin. B 2025, 15, 4476–4496. [Google Scholar] [CrossRef]
- Saleh, T.; Bloukh, S.; Carpenter, V.J.; Alwohoush, E.; Bakeer, J.; Darwish, S.; Azab, B.; Gewirtz, D.A. Therapy-Induced Senescence: An “Old” Friend Becomes the Enemy. Cancers 2020, 12, 822. [Google Scholar] [CrossRef]
- Coppé, J.-P.; Patil, C.K.; Rodier, F.; Sun, Y.; Muñoz, D.P.; Goldstein, J.; Nelson, P.S.; Desprez, P.-Y.; Campisi, J. Senescence-associated secretory phenotypes reveal cell-nonautonomous functions of oncogenic RAS and the p53 tumor suppressor. PLoS Biol. 2008, 6, 2853–2868. [Google Scholar] [CrossRef]
- Wang, L.; Lankhorst, L.; Bernards, R. Exploiting senescence for the treatment of cancer. Nat. Rev. Cancer 2022, 22, 340–355. [Google Scholar] [CrossRef]
- Lei, Y.; Zhong, C.; Zhang, J.; Zheng, Q.; Xu, Y.; Li, Z.; Huang, C.; Ren, T. Senescent lung fibroblasts in idiopathic pulmonary fibrosis facilitate non-small cell lung cancer progression by secreting exosomal MMP1. Oncogene 2025, 44, 769–781. [Google Scholar] [CrossRef]
- DeMaria, M.; O’Leary, M.N.; Chang, J.; Shao, L.; Liu, S.; Alimirah, F.; Koenig, K.; Le, C.; Mitin, N.; Deal, A.M.; et al. Cellular Senescence Promotes Adverse Effects of Chemotherapy and Cancer Relapse. Cancer Discov. 2017, 7, 165–176. [Google Scholar] [CrossRef]
- Haston, S.; Gonzalez-Gualda, E.; Morsli, S.; Ge, J.; Reen, V.; Calderwood, A.; Moutsopoulos, I.; Panousopoulos, L.; Deletic, P.; Carreno, G.; et al. Clearance of senescent macrophages ameliorates tumorigenesis in KRAS-driven lung cancer. Cancer Cell 2023, 41, 1242–1260.e6. [Google Scholar] [CrossRef] [PubMed]
- Gerdes, E.O.W.; Vanichkachorn, G.; Verdoorn, B.P.; Hanson, G.J.; Joshi, A.Y.; Murad, M.H.; Rizza, S.A.; Hurt, R.T.; Tchkonia, T.; Kirkland, J.L. Role of senescence in the chronic health consequences of COVID-19. Transl. Res. 2022, 241, 96–108. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, S.; Minami, S.; Hashimoto, R.; Konishi, Y.; Suzuki, T.; Kondo, T.; Sasai, M.; Torii, S.; Ono, C.; Shichinohe, S.; et al. SARS-CoV-2 infection triggers paracrine senescence and leads to a sustained senescence-associated inflammatory response. Nat. Aging 2022, 2, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Torres Acosta, M.A.; Singer, B.D. Pathogenesis of COVID-19-induced ARDS: Implications for an ageing population. Eur. Respir. J. 2020, 56, 2002049. [Google Scholar] [CrossRef]
- Künzi, L.; Easter, M.; Hirsch, M.J.; Krick, S. Cystic Fibrosis Lung Disease in the Aging Population. Front. Pharmacol. 2021, 12, 601438. [Google Scholar] [CrossRef]
- Bezzerri, V.; Piacenza, F.; Caporelli, N.; Malavolta, M.; Provinciali, M.; Cipolli, M. Is cellular senescence involved in cystic fibrosis? Respir. Res. 2019, 20, 32. [Google Scholar] [CrossRef]
- Easter, M.; Hirsch, M.J.; Harris, E.; Howze, P.H.; Matthews, E.L.; Jones, L.I.; Bollenbecker, S.; Vang, S.; Tyrrell, D.J.; Sanders, Y.Y.; et al. FGF receptors mediate cellular senescence in the cystic fibrosis airway epithelium. J. Clin. Investig. 2024, 9, e174888. [Google Scholar] [CrossRef]
- Laucirica, D.R.; Garratt, L.W.; Kicic, A. Progress in Model Systems of Cystic Fibrosis Mucosal Inflammation to Understand Aberrant Neutrophil Activity. Front. Immunol. 2020, 11, 595. [Google Scholar] [CrossRef]
- Voynow, J.A.; Shinbashi, M. Neutrophil Elastase and Chronic Lung Disease. Biomolecules 2021, 11, 1065. [Google Scholar] [CrossRef]
- Barnes, P.J.; Baker, J.; Donnelly, L.E. Cellular Senescence as a Mechanism and Target in Chronic Lung Diseases. Am. J. Respir. Crit. Care Med. 2019, 200, 556–564. [Google Scholar] [CrossRef] [PubMed]
- Roger, I.; Milara, J.; Belhadj, N.; Cortijo, J. Senescence Alterations in Pulmonary Hypertension. Cells 2021, 10, 3456. [Google Scholar] [CrossRef] [PubMed]
- Culley, M.K.; Chan, S.Y. Endothelial Senescence: A New Age in Pulmonary Hypertension. Circ. Res. 2022, 130, 928–941. [Google Scholar] [CrossRef] [PubMed]
- Qamsari, E.S.; Stewart, D.J. Cellular senescence in the pathogenesis of pulmonary arterial hypertension: The good, the bad and the uncertain. Front. Immunol. 2024, 15, 1403669. [Google Scholar] [CrossRef]
- Born, E.; Lipskaia, L.; Breau, M.; Houssaini, A.; Beaulieu, D.P.; Marcos, E.; Pierre, R.; Cruzeiro, M.D.; Lefevre, M.; Derumeaux, G.; et al. Eliminating Senescent Cells Can Promote Pulmonary Hypertension Development and Progression. Circulation 2023, 147, 650–666. [Google Scholar] [CrossRef]
- Wang, A.-P.; Yang, F.; Tian, Y.; Su, J.-H.; Gu, Q.; Chen, W.; Gong, S.-X.; Ma, X.-F.; Qin, X.-P.; Jiang, Z.-S. Pulmonary Artery Smooth Muscle Cell Senescence Promotes the Proliferation of PASMCs by Paracrine IL-6 in Hypoxia-Induced Pulmonary Hypertension. Front. Physiol. 2021, 12, 656139. [Google Scholar] [CrossRef]
- Ramadhiani, R.; Ikeda, K.; Miyagawa, K.; Ryanto, G.R.T.; Tamada, N.; Suzuki, Y.; Kirita, Y.; Matoba, S.; Hirata, K.-I.; Emoto, N. Endothelial cell senescence exacerbates pulmonary hypertension by inducing juxtacrine Notch signaling in smooth muscle cells. iScience 2023, 26, 106662. [Google Scholar] [CrossRef]
- Meng, Z.-Y.; Lu, C.-H.; Li, J.; Liao, J.; Wen, H.; Li, Y.; Huang, F.; Zeng, Z.-Y. Identification and experimental verification of senescence-related gene signatures and molecular subtypes in idiopathic pulmonary arterial hypertension. Sci. Rep. 2024, 14, 22157. [Google Scholar] [CrossRef]
- Gan, Y.; Ye, F.; He, X.-X. The role of YWHAZ in cancer: A maze of opportunities and challenges. J. Cancer 2020, 11, 2252–2264. [Google Scholar] [CrossRef]
- Van Der Feen, D.E.; Bossers, G.P.; Hagdorn, Q.A.; Moonen, J.R.; Kurakula, K.; Szulcek, R.; Bartelds, B. Cellular senescence impairs the reversibility of pulmonary arterial hypertension. Sci. Transl. Med. 2020, 12, eaaw4974. [Google Scholar] [CrossRef]
- Wan, R.; Srikaram, P.; Guntupalli, V.; Hu, C.; Chen, Q.; Gao, P. Cellular senescence in asthma: From pathogenesis to therapeutic challenges. EBioMedicine 2023, 94, 104717. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Tata, A.; Konkimalla, A.; Katsura, H.; Lee, R.F.; Ou, J.; Banovich, N.E.; Kropski, J.A.; Tata, P.R. Persistence of a regeneration-associated, transitional alveolar epithelial cell state in pulmonary fibrosis. Nat. Cell Biol. 2020, 22, 934–946. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Chen, H.; Liang, J.; Gu, X.; Zhou, J.; Xie, C.; Jin, J. TGF-β1/IL-11/MEK/ERK signaling mediates senescence-associated pulmonary fibrosis in a stress-induced premature senescence model of Bmi-1 deficiency. Exp. Mol. Med. 2020, 52, 130–151. [Google Scholar] [CrossRef] [PubMed]
- Gessner, C.; Scheibe, R.; Wötzel, M.; Hammerschmidt, S.; Kuhn, H.; Engelmann, L.; Hoheisel, G.; Gillissen, A.; Sack, U.; Wirtz, H. Exhaled breath condensate cytokine patterns in chronic obstructive pulmonary disease. Respir. Med. 2005, 99, 1229–1240. [Google Scholar] [CrossRef] [PubMed]
- Kristan, S.S.; Marc, M.M.; Kern, I.; Flezar, M.; Suskovic, S.; Kosnik, M.; Korosec, P. Airway angiogenesis in stable and exacerbated chronic obstructive pulmonary disease. Scand. J. Immunol. 2012, 75, 109–114. [Google Scholar] [CrossRef]
- Lim, S.; Roche, N.; Oliver, B.G.; Mattos, W.; Barnes, P.J.; Chung, K.F. Balance of matrix metalloprotease-9 and tissue inhibitor of metalloprotease-1 from alveolar macrophages in cigarette smokers. Regulation by interleukin-10. Am. J. Respir. Crit. Care Med. 2000, 162 Pt 1, 1355–1360. [Google Scholar] [CrossRef]
- Betsuyaku, T.; Nishimura, M.; Takeyabu, K.; Tanino, M.; Venge, P.; Xu, S.; Kawakami, Y. Neutrophil granule proteins in bronchoalveolar lavage fluid from subjects with subclinical emphysema. Am. J. Respir. Crit. Care Med. 1999, 159, 1985–1991. [Google Scholar] [CrossRef]
- Lv, X.; Liu, C.; Liu, S.; Li, Y.; Wang, W.; Li, K.; Hua, F.; Cui, B.; Zhang, X.; Yu, J.; et al. The cell cycle inhibitor P21 promotes the development of pulmonary fibrosis by suppressing lung alveolar regeneration. Acta Pharm. Sin. B 2022, 12, 735–746. [Google Scholar] [CrossRef]
- Ma, J.-H.; Zhang, Y.-T.; Wang, L.-P.; Sun, Q.-Y.; Zhang, H.; Li, J.-J.; Han, N.-N.; Zhu, Y.-Y.; Xie, X.-Y.; Li, X. K63 Ubiquitination of P21 Can Facilitate Pellino-1 in the Context of Chronic Obstructive Pulmonary Disease and Lung Cellular Senescence. Cells 2022, 11, 3115. [Google Scholar] [CrossRef]
- Reyes, N.S.; Krasilnikov, M.; Allen, N.C.; Lee, J.Y.; Hyams, B.; Zhou, M.; Peng, T. Sentinel p16(INK4a+) cells in the basement membrane form a reparative niche in the lung. Science 2022, 378, 192–201. [Google Scholar] [CrossRef]
- Verhamme, F.; Seys, L.J.M.; De Smet, E.; Provoost, S.; Janssens, W.; Elewaut, D.; Joos, G.; Brusselle, G.; Bracke, K. Elevated GDF-15 contributes to pulmonary inflammation upon cigarette smoke exposure. Mucosal Immunol. 2017, 10, 1400–1411. [Google Scholar] [CrossRef] [PubMed]
- Jiang, G.; Liu, C.; Zhang, W. IL-17A and GDF15 are able to induce epithelial-mesenchymal transition of lung epithelial cells in response to cigarette smoke. Exp. Ther. Med. 2018, 16, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Radwanska, A.; Cottage, C.T.; Piras, A.; Overed-Sayer, C.; Sihlbom, C.; Budida, R.; Wrench, C.; Connor, J.; Monkley, S.; Hazon, P.; et al. Increased expression and accumulation of GDF15 in IPF extracellular matrix contribute to fibrosis. J. Clin. Investig. 2022, 7, e153058. [Google Scholar] [CrossRef]
- Shaghaghi, H.; Cuevas-Mora, K.; Para, R.; Tran, C.; Roque, W.; Robertson, M.J.; Rosas, I.O.; Summer, R.; Romero, F. A model of the aged lung epithelium in idiopathic pulmonary fibrosis. Aging 2021, 13, 16922–16937. [Google Scholar] [CrossRef]
- Zhang, Y.; Jiang, M.; Nouraie, M.; Roth, M.G.; Tabib, T.; Winters, S.; Chen, X.; Sembrat, J.; Chu, Y.; Cardenes, N.; et al. GDF15 is an epithelial-derived biomarker of idiopathic pulmonary fibrosis. Am. J. Physiol. Cell. Mol. Physiol. 2019, 317, L510–L521. [Google Scholar] [CrossRef]
- Zhou, Y.; Höti, N.; Ao, M.; Zhang, Z.; Zhu, H.; Li, L.; Askin, F.; Gabrielson, E.; Zhang, H.; Li, Q.K. Expression of P16 and P53 in non-small-cell lung cancer: Clinicopathological correlation and potential prognostic impact. Biomarkers Med. 2019, 13, 761–771. [Google Scholar] [CrossRef]
- Keow, J.; Cecchini, M.J.; Jayawardena, N.; Zompatori, M.; Joseph, M.G.; Mura, M. Digital quantification of p16-positive foci in fibrotic interstitial lung disease is associated with a phenotype of idiopathic pulmonary fibrosis with reduced survival. Respir. Res. 2022, 23, 147. [Google Scholar] [CrossRef]
- Khan, S.S.; Shah, S.J.; Klyachko, E.; Baldridge, A.S.; Eren, M.; Place, A.T.; Aviv, A.; Puterman, E.; Lloyd-Jones, D.M.; Heiman, M.; et al. A null mutation in SERPINE1 protects against biological aging in humans. Sci. Adv. 2017, 3, eaao1617. [Google Scholar] [CrossRef]
- Malinina, A.; Dikeman, D.; Westbrook, R.; Moats, M.; Gidner, S.; Poonyagariyagorn, H.; Walston, J.; Neptune, E.R. IL10 deficiency promotes alveolar enlargement and lymphoid dysmorphogenesis in the aged murine lung. Aging Cell 2020, 19, e13130. [Google Scholar] [CrossRef]
- McDonough, J.E.; Martens, D.S.; Tanabe, N.; Ahangari, F.; Verleden, S.E.; Maes, K.; Verleden, G.M.; Kaminski, N.; Hogg, J.C.; Nawrot, T.S.; et al. A role for telomere length and chromosomal damage in idiopathic pulmonary fibrosis. Respir. Res. 2018, 19, 132. [Google Scholar] [CrossRef]
- Russo, R.C.; Guabiraba, R.; Garcia, C.C.; Barcelos, L.S.; Roffê, E.; Souza, A.L.S.; Amaral, F.A.; Cisalpino, D.; Cassali, G.D.; Doni, A.; et al. Role of the chemokine receptor CXCR2 in bleomycin-induced pulmonary inflammation and fibrosis. Am. J. Respir. Cell Mol. Biol. 2009, 40, 410–421. [Google Scholar] [CrossRef]
- Robbins, P.D.; Jurk, D.; Khosla, S.; Kirkland, J.L.; LeBrasseur, N.K.; Miller, J.D.; Passos, J.F.; Pignolo, R.J.; Tchkonia, T.; Niedernhofer, L.J. Senolytic Drugs: Reducing Senescent Cell Viability to Extend Health Span. Annu. Rev. Pharmacol. Toxicol. 2021, 61, 779–803. [Google Scholar] [CrossRef]
- Lewinska, A.; Adamczyk-Grochala, J.; Bloniarz, D.; Olszowka, J.; Kulpa-Greszta, M.; Litwinienko, G.; Tomaszewska, A.; Wnuk, M.; Pazik, R. AMPK-mediated senolytic and senostatic activity of quercetin surface functionalized Fe3O4 nanoparticles during oxidant-induced senescence in human fibroblasts. Redox Biol. 2020, 28, 101337. [Google Scholar] [CrossRef]
- Zhu, Y.; Tchkonia, T.; Fuhrmann-Stroissnigg, H.; Dai, H.M.; Ling, Y.Y.; Stout, M.B.; Pirtskhalava, T.; Giorgadze, N.; Johnson, K.O.; Giles, C.B.; et al. Identification of a novel senolytic agent, navitoclax, targeting the Bcl-2 family of anti-apoptotic factors. Aging Cell 2016, 15, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.I.; Tchkonia, T.; Pirtskhalava, T.; Gower, A.C.; Ding, H.; Giorgadze, N.; Palmer, A.K.; Ikeno, Y.; Hubbard, G.B.; Lenburg, M.; et al. The Achilles’ heel of senescent cells: From transcriptome to senolytic drugs. Aging Cell 2015, 14, 644–658. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Sun, C.; Mao, L.; Ma, P.; Liu, F.; Yang, J.; Gao, Y. The biological activities, chemical stability, metabolism and delivery systems of quercetin: A review. Trends Food Sci. Technol. 2016, 56, 21–38. [Google Scholar] [CrossRef]
- Zhu, Y.; Doornebal, E.J.; Pirtskhalava, T.; Giorgadze, N.; Wentworth, M.; Fuhrmann-Stroissnigg, H.; Niedernhofer, L.J.; Robbins, P.D.; Tchkonia, T.; Kirkland, J.L. New agents that target senescent cells: The flavone, fisetin, and the BCL-XL inhibitors, A1331852 and A1155463. Aging 2017, 9, 955–963. [Google Scholar] [CrossRef]
- Yousefzadeh, M.J.; Zhu, Y.; McGowan, S.J.; Angelini, L.; Fuhrmann-Stroissnigg, H.; Xu, M.; Ling, Y.Y.; Melos, K.I.; Pirtskhalava, T.; Inman, C.L.; et al. Fisetin is a senotherapeutic that extends health and lifespan. EBioMedicine 2018, 36, 18–28. [Google Scholar] [CrossRef]
- Moaddel, R.; Rossi, M.; Rodriguez, S.; Munk, R.; Khadeer, M.; Abdelmohsen, K.; Gorospe, M.; Ferrucci, L. Identification of gingerenone A as a novel senolytic compound. PLoS ONE 2022, 17, e0266135. [Google Scholar] [CrossRef]
- Rawat, L.; Hegde, H.; Hoti, S.L.; Nayak, V. Piperlongumine induces ROS mediated cell death and synergizes paclitaxel in human intestinal cancer cells. Biomed. Pharmacother. 2020, 128, 110243. [Google Scholar] [CrossRef]
- Chang, J.; Wang, Y.; Shao, L.; Laberge, R.-M.; DeMaria, M.; Campisi, J.; Janakiraman, K.; Sharpless, N.E.; Ding, S.; Feng, W.; et al. Clearance of senescent cells by ABT263 rejuvenates aged hematopoietic stem cells in mice. Nat. Med. 2016, 22, 78–83. [Google Scholar] [CrossRef]
- Fuhrmann-Stroissnigg, H.; Niedernhofer, L.J.; Robbins, P.D. Hsp90 inhibitors as senolytic drugs to extend healthy aging. Cell Cycle 2018, 17, 1048–1055. [Google Scholar] [CrossRef]
- Fuhrmann-Stroissnigg, H.; Ling, Y.Y.; Zhao, J.; McGowan, S.J.; Zhu, Y.; Brooks, R.W.; Grassi, D.; Gregg, S.Q.; Stripay, J.L.; Dorronsoro, A.; et al. Identification of HSP90 inhibitors as a novel class of senolytics. Nat. Commun. 2017, 8, 422. [Google Scholar] [CrossRef]
- Amor, C.; Fernández-Maestre, I.; Chowdhury, S.; Ho, Y.-J.; Nadella, S.; Graham, C.; Carrasco, S.E.; Nnuji-John, E.; Feucht, J.; Hinterleitner, C.; et al. Prophylactic and long-lasting efficacy of senolytic CAR T cells against age-related metabolic dysfunction. Nat. Aging 2024, 4, 336–349. [Google Scholar] [CrossRef] [PubMed]
- Baar, M.P.; Brandt, R.M.C.; Putavet, D.A.; Klein, J.D.D.; Derks, K.W.J.; Bourgeois, B.R.M.; Stryeck, S.; Rijksen, Y.; Van Willigenburg, H.; Feijtel, D.A.; et al. Targeted Apoptosis of Senescent Cells Restores Tissue Homeostasis in Response to Chemotoxicity and Aging. Cell 2017, 169, 132–147.e16. [Google Scholar] [CrossRef] [PubMed]
- González-Gualda, E.; Baker, A.G.; Fruk, L.; Muñoz-Espín, D. A guide to assessing cellular senescence in vitro and in vivo. Febs J. 2021, 288, 56–80. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Kumar, A.; Xie, K.; Schaaf, K.; Scifo, E.; Morsy, S.; Li, T.; Ehninger, A.; Bano, D.; Ehninger, D. Targeting senescent cells with NKG2D-CAR T cells. Cell Death Discov. 2024, 10, 217. [Google Scholar] [CrossRef]
- Huang, Y.; Liu, T. Step further towards targeted senolytic therapy: Therapeutic potential of uPAR-CAR T cells for senescence-related diseases. Signal Transduct. Target. Ther. 2020, 5, 155. [Google Scholar] [CrossRef]
- Kotschy, A.; Szlavik, Z.; Murray, J.; Davidson, J.; Maragno, A.L.; Le Toumelin-Braizat, G.; Chanrion, M.; Kelly, G.L.; Gong, J.-N.; Moujalled, D.M.; et al. The MCL1 inhibitor S63845 is tolerable and effective in diverse cancer models. Nature 2016, 538, 477–482. [Google Scholar] [CrossRef]
- Partridge, L.; Fuentealba, M.; Kennedy, B.K. The quest to slow ageing through drug discovery. Nat. Rev. Drug Discov. 2020, 19, 513–532. [Google Scholar] [CrossRef]
- Xu, M.; Tchkonia, T.; Ding, H.; Ogrodnik, M.; Lubbers, E.R.; Pirtskhalava, T.; White, T.A.; Johnson, K.O.; Stout, M.B.; Mezera, V.; et al. JAK inhibition alleviates the cellular senescence-associated secretory phenotype and frailty in old age. Proc. Natl. Acad. Sci. USA 2015, 112, E6301–E6310. [Google Scholar] [CrossRef]
- Walters, H.E.; Deneka-Hannemann, S.; Cox, L.S. Reversal of phenotypes of cellular senescence by pan-mTOR inhibition. Aging 2016, 8, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Bogdanowicz, P.; Bensadoun, P.; Noizet, M.; Béganton, B.; Philippe, A.; Alvarez-Georges, S.; Doat, G.; Tourette, A.; Bessou-Touya, S.; Lemaitre, J.-M.; et al. Senomorphic activity of a combination of niacinamide and hyaluronic acid: Correlation with clinical improvement of skin aging. Sci. Rep. 2024, 14, 16321. [Google Scholar] [CrossRef] [PubMed]
- Moiseeva, O.; Deschênes-Simard, X.; St-Germain, E.; Igelmann, S.; Huot, G.; Cadar, A.E.; Ferbeyre, G. Metformin inhibits the senescence-associated secretory phenotype by interfering with IKK/NF-κB activation. Aging Cell 2013, 12, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Gomari, H.; Moghadam, M.F.; Soleimani, M. Targeted cancer therapy using engineered exosome as a natural drug delivery vehicle. OncoTargets Ther. 2018, 11, 5753–5762. [Google Scholar] [CrossRef]
- Cai, Y.; Zhou, H.; Zhu, Y.; Sun, Q.; Ji, Y.; Xue, A.; Wang, Y.; Chen, W.; Yu, X.; Wang, L.; et al. Elimination of senescent cells by β-galactosidase-targeted prodrug attenuates inflammation and restores physical function in aged mice. Cell Res. 2020, 30, 574–589. [Google Scholar] [CrossRef]
- Poblocka, M.; Bassey, A.L.; Smith, V.M.; Falcicchio, M.; Manso, A.S.; Althubiti, M.; Sheng, X.; Kyle, A.; Barber, R.; Frigerio, M.; et al. Targeted clearance of senescent cells using an antibody-drug conjugate against a specific membrane marker. Sci. Rep. 2021, 11, 20358. [Google Scholar] [CrossRef]
- Gerdes, E.O.W.; Misra, A.; Netto, J.M.E.; Tchkonia, T.; Kirkland, J.L. Strategies for late phase preclinical and early clinical trials of senolytics. Mech. Ageing Dev. 2021, 200, 111591. [Google Scholar] [CrossRef]
- de Vos, S.; Leonard, J.P.; Friedberg, J.W.; Zain, J.; Dunleavy, K.; Humerickhouse, R.; Wilson, W.H. Safety and efficacy of navitoclax, a BCL-2 and BCL-X(L) inhibitor, in patients with relapsed or refractory lymphoid malignancies: Results from a phase 2a study. Leuk Lymphoma 2021, 62, 810–818. [Google Scholar] [CrossRef]
- Cai, Y.; Song, W.; Li, J.; Jing, Y.; Liang, C.; Zhang, L.; Liu, G.H. The landscape of aging. Sci. China Life Sci. 2022, 65, 2354–2454. [Google Scholar] [CrossRef]
- Muñoz-Espín, D.; Rovira, M.; Galiana, I.; Giménez, C.; Lozano-Torres, B.; Paez-Ribes, M.; Llanos, S.; Chaib, S.; Muñoz-Martín, M.; Ucero, A.C.; et al. A versatile drug delivery system targeting senescent cells. EMBO Mol. Med. 2018, 10, e9355. [Google Scholar] [CrossRef]
- Schafer, M.J.; Zhang, X.; Kumar, A.; Atkinson, E.J.; Zhu, Y.; Jachim, S.; Mazula, D.L.; Brown, A.K.; Berning, M.; Aversa, Z.; et al. The senescence-associated secretome as an indicator of age and medical risk. J. Clin. Investig. 2020, 5, e133668. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Niu, Z.; Wang, Y.; Zheng, Y.; Zhu, Y.; Wang, C.; Gao, X.; Gao, L.; Zhang, W.; Zhang, K.; et al. Senescence as a dictator of patient outcomes and therapeutic efficacies in human gastric cancer. Cell Death Discov. 2022, 8, 13. [Google Scholar] [CrossRef] [PubMed]
- Bian, R.; Zhang, L.; Li, D.; Xu, X. CDKN1A as a target of senescence in heart failure: Insights from a multiomics study. Front. Pharmacol. 2024, 15, 1446300. [Google Scholar] [CrossRef] [PubMed]
- Suryadevara, V.; Hudgins, A.D.; Rajesh, A.; Pappalardo, A.; Karpova, A.; Dey, A.K.; Hertzel, A.; Agudelo, A.; Rocha, A.; Soygur, B.; et al. SenNet recommendations for detecting senescent cells in different tissues. Nat. Rev. Mol. Cell Biol. 2024, 25, 1001–1023. [Google Scholar] [CrossRef]
- Prieto, L.I.; Sturmlechner, I.; Graves, S.I.; Zhang, C.; Goplen, N.P.; Yi, E.S.; Sun, J.; Li, H.; Baker, D.J. Senescent alveolar macrophages promote early-stage lung tumorigenesis. Cancer Cell 2023, 41, 1261–1275.e6. [Google Scholar] [CrossRef]
- Smith, R.; Bassand, K.; Dussol, A.; Piesse, C.; Duplus, E.; El Hadri, K. A new model and precious tool to study molecular mechanisms of macrophage aging. Aging 2024, 16, 12697–12725. [Google Scholar] [CrossRef]
- Maus, M.; López-Polo, V.; Mateo, L.; Lafarga, M.; Aguilera, M.; De Lama, E.; Meyer, K.; Sola, A.; Lopez-Martinez, C.; López-Alonso, I.; et al. Iron accumulation drives fibrosis, senescence and the senescence-associated secretory phenotype. Nat. Metab. 2023, 5, 2111–2130. [Google Scholar] [CrossRef]
- Zhou, B.-W.; Liu, H.-M.; Xu, F.; Jia, X.-H. The role of macrophage polarization and cellular crosstalk in the pulmonary fibrotic microenvironment: A review. Cell Commun. Signal. 2024, 22, 172. [Google Scholar] [CrossRef]
- Campbell, R.A.; Docherty, M.-H.; Ferenbach, D.A.; Mylonas, K.J. The Role of Ageing and Parenchymal Senescence on Macrophage Function and Fibrosis. Front. Immunol. 2021, 12, 700790. [Google Scholar] [CrossRef]
- Salminen, A. Inhibitory immune checkpoints suppress the surveillance of senescent cells promoting their accumulation with aging and in age-related diseases. Biogerontology 2024, 25, 749–773. [Google Scholar] [CrossRef]
- Marin, I.; Serrano, M.; Pietrocola, F. Recent insights into the crosstalk between senescent cells and CD8 T lymphocytes. npj Aging 2023, 9, 8. [Google Scholar] [CrossRef]
- Melo-Narváez, M.C.; Stegmayr, J.; Wagner, D.E.; Lehmann, M. Lung regeneration: Implications of the diseased niche and ageing. Eur. Respir. Rev. 2020, 29, 200222. [Google Scholar] [CrossRef]
- Ruhland, M.K.; Loza, A.J.; Capietto, A.-H.; Luo, X.; Knolhoff, B.L.; Flanagan, K.C.; Belt, B.A.; Alspach, E.; Leahy, K.; Luo, J.; et al. Stromal senescence establishes an immunosuppressive microenvironment that drives tumorigenesis. Nat. Commun. 2016, 7, 11762. [Google Scholar] [CrossRef]
- Li, X.; Li, C.; Zhang, W.; Wang, Y.; Qian, P.; Huang, H. Inflammation and aging: Signaling pathways and intervention therapies. Signal Transduct. Target. Ther. 2023, 8, 239. [Google Scholar] [CrossRef]
- Favaretto, G.; Rossi, M.N.; Cuollo, L.; Laffranchi, M.; Cervelli, M.; Soriani, A.; Sozzani, S.; Santoni, A.; Antonangeli, F. Neutrophil-activating secretome characterizes palbociclib-induced senescence of breast cancer cells. Cancer Immunol. Immunother. 2024, 73, 113. [Google Scholar] [CrossRef] [PubMed]
- Rolas, L.; Stein, M.; Barkaway, A.; Reglero-Real, N.; Sciacca, E.; Yaseen, M.; Wang, H.; Vazquez-Martinez, L.; Golding, M.; A Blacksell, I.; et al. Senescent endothelial cells promote pathogenic neutrophil trafficking in inflamed tissues. Embo Rep. 2024, 25, 3842–3869. [Google Scholar] [CrossRef] [PubMed]
- Cai, C.; Guan, L.; Wang, C.; Hu, R.; Ou, L.; Jiang, Q. The role of fibroblast-neutrophil crosstalk in the pathogenesis of inflammatory diseases: A multi-tissue perspective. Front. Immunol. 2025, 16, 1588667. [Google Scholar] [CrossRef]
- Fulop, T.; Larbi, A.; Dupuis, G.; Le Page, A.; Frost, E.H.; Cohen, A.A.; Witkowski, J.M.; Franceschi, C. Immunosenescence and Inflamm-Aging As Two Sides of the Same Coin: Friends or Foes? Front. Immunol. 2017, 8, 1960. [Google Scholar] [CrossRef]
- Wynn, T.A.; Vannella, K.M. Macrophages in Tissue Repair, Regeneration, and Fibrosis. Immunity 2016, 44, 450–462. [Google Scholar] [CrossRef]
- Simmons, S.R.; Bhalla, M.; Herring, S.E.; Tchalla, E.Y.I.; Ghanem, E.N.B. Older but Not Wiser: The Age-Driven Changes in Neutrophil Responses during Pulmonary Infections. Infect. Immun. 2021, 89, e00653-20. [Google Scholar] [CrossRef]
- Yang, S.-C.; Tsai, Y.-F.; Pan, Y.-L.; Hwang, T.-L. Understanding the role of neutrophils in acute respiratory distress syndrome. Biomed. J. 2021, 44, 439–446. [Google Scholar] [CrossRef]
- Wang, Y.; Huang, X.; Luo, G.; Xu, Y.; Deng, X.; Lin, Y.; Wang, Z.; Zhou, S.; Wang, S.; Chen, H.; et al. The aging lung: Microenvironment, mechanisms, and diseases. Front. Immunol. 2024, 15, 1383503. [Google Scholar] [CrossRef]
- Soto-Heredero, G.; Gabandé-Rodríguez, E.; Carrasco, E.; Escrig-Larena, J.I.; Heras, M.M.G.d.L.; Delgado-Pulido, S.; Francos-Quijorna, I.; Blanco, E.M.; Fernández-Almeida, Á.; Abia, D.; et al. KLRG1 identifies regulatory T cells with mitochondrial alterations that accumulate with aging. Nat. Aging 2025, 5, 799–815. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Liang, Q.; Ren, Y.; Guo, C.; Ge, X.; Wang, L.; Han, X. Immunosenescence: Molecular mechanisms and diseases. Signal. Transduct. Target Ther. 2023, 8, 200. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Lu, Q.; Liu, X. Advances in cellular senescence in idiopathic pulmonary fibrosis (Review). Exp. Ther. Med. 2023, 25, 145. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Dong, C.; Han, Y.; Gu, Z.; Sun, C. Immunosenescence, aging and successful aging. Front. Immunol. 2022, 13, 942796. [Google Scholar] [CrossRef]
- Devulder, J.V. Unveiling mechanisms of lung aging in COPD: A promising target for therapeutics development. Chin. Med. J.-Pulm. Crit. Care Med. 2024, 2, 133–141. [Google Scholar] [CrossRef]
- Xie, C.; Likun, M.M.Y.; Luo, Q.-L.; Dong, J.-C. Role of cellular senescence in inflammatory lung diseases. Cytokine Growth Factor Rev. 2023, 70, 26–40. [Google Scholar] [CrossRef]
- Wan, R.; Wang, L.; Zhu, M.; Li, W.; Duan, Y.; Yu, G. Cellular Senescence: A Troy Horse in Pulmonary Fibrosis. Int. J. Mol. Sci. 2023, 24, 16410. [Google Scholar] [CrossRef]
- D’aGnillo, F.; Walters, K.-A.; Xiao, Y.; Sheng, Z.-M.; Scherler, K.; Park, J.; Gygli, S.; Rosas, L.A.; Sadtler, K.; Kalish, H.; et al. Lung epithelial and endothelial damage, loss of tissue repair, inhibition of fibrinolysis, and cellular senescence in fatal COVID-19. Sci. Transl. Med. 2021, 13, eabj7790. [Google Scholar] [CrossRef]
- Zhou, S.; Zhu, J.; Zhou, P.-K.; Gu, Y. Alveolar type 2 epithelial cell senescence and radiation-induced pulmonary fibrosis. Front. Cell Dev. Biol. 2022, 10, 999600. [Google Scholar] [CrossRef] [PubMed]
- Beidokhti, M.N.; Villalba, N.; Ma, Y.; Reynolds, A.; Villamil, J.H.; Yuan, S.Y. Lung endothelial cell senescence impairs barrier function and promotes neutrophil adhesion and migration. GeroScience 2025, 47, 2655–2671. [Google Scholar] [CrossRef] [PubMed]
- Mebratu, Y.A.; Soni, S.; Rosas, L.; Rojas, M.; Horowitz, J.C.; Nho, R. The aged extracellular matrix and the profibrotic role of senescence-associated secretory phenotype. Am. J. Physiol. Cell. Physiol. 2023, 325, C565–C579. [Google Scholar] [CrossRef] [PubMed]
- Saul, D.; Kosinsky, R.L.; Atkinson, E.J.; Doolittle, M.L.; Zhang, X.; LeBrasseur, N.K.; Pignolo, R.J.; Robbins, P.D.; Niedernhofer, L.J.; Ikeno, Y.; et al. A new gene set identifies senescent cells and predicts senescence-associated pathways across tissues. Nat. Commun. 2022, 13, 4827. [Google Scholar] [CrossRef]
- Melo-Narváez, M.C.; Bramey, N.; See, F.; Heinzelmann, K.; Ballester, B.; Steinchen, C.; Jain, E.; Federl, K.; Hu, Q.; Dhakad, D.; et al. Stimuli-Specific Senescence of Primary Human Lung Fibroblasts Modulates Alveolar Stem Cell Function. Cells 2024, 13, 1129. [Google Scholar] [CrossRef]
- Liao, Y.-L.; Fang, Y.-F.; Sun, J.-X.; Dou, G.-R. Senescent endothelial cells: A potential target for diabetic retinopathy. Angiogenesis 2024, 27, 663–679. [Google Scholar] [CrossRef]
- Morton, L.; Garza, A.P.; Debska-Vielhaber, G.; Villafuerte, L.E.; Henneicke, S.; Arndt, P.; Meuth, S.G.; Schreiber, S.; Dunay, I.R. Pericytes and Extracellular Vesicle Interactions in Neurovascular Adaptation to Chronic Arterial Hypertension. J. Am. Heart Assoc. 2025, 14, e038457. [Google Scholar] [CrossRef]
- Blackburn, J.B.; Li, N.F.; Bartlett, N.W.; Richmond, B.W. An update in club cell biology and its potential relevance to chronic obstructive pulmonary disease. Am. J. Physiol. Cell. Mol. Physiol. 2023, 324, L652–L665. [Google Scholar] [CrossRef]
- Jia, M.; Garcia, P.A.A.; Ovando-Ricardez, J.A.; Tabib, T.; Bittar, H.T.; Lafyatis, R.A.; Mora, A.L.; Benos, P.V.; Rojas, M. Transcriptional changes of the aging lung. Aging Cell 2023, 22, e13969. [Google Scholar] [CrossRef]
- Jia, H.; Chang, Y.; Chen, Y.; Chen, X.; Zhang, H.; Hua, X.; Xu, M.; Sheng, Y.; Zhang, N.; Cui, H.; et al. A single-cell atlas of lung homeostasis reveals dynamic changes during development and aging. Commun. Biol. 2024, 7, 427. [Google Scholar] [CrossRef] [PubMed]
- Kasmani, M.Y.; Topchyan, P.; Brown, A.K.; Brown, R.J.; Wu, X.; Chen, Y.; Khatun, A.; Alson, D.; Wu, Y.; Burns, R.; et al. A spatial sequencing atlas of age-induced changes in the lung during influenza infection. Nat. Commun. 2023, 14, 6597. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhou, X.; Yu, P.; Yao, J.; Guo, P.; Xu, Q.; Zhao, Y.; Wang, G.; Li, Q.; Zhu, X.; et al. A transcriptome-based human universal senescence index (hUSI) robustly predicts cellular senescence under various conditions. Nat. Aging 2025, 5, 1159–1175. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.D.; Rosas, L.; Khaliullin, T.; Jiang, P.; Hasanaj, E.; Ovando-Ricardez, J.A.; Bueno, M.; Rahman, I.; Pryhuber, G.S.; Li, D.; et al. scDOT: Optimal transport for mapping senescent cells in spatial transcriptomics. Genome Biol. 2024, 25, 288. [Google Scholar] [CrossRef]
- Ashraf, H.M.; Fernandez, B.; Spencer, S.L. The intensities of canonical senescence biomarkers integrate the duration of cell-cycle withdrawal. Nat. Commun. 2023, 14, 4527. [Google Scholar] [CrossRef]
- Nacarelli, T.; Lau, L.; Fukumoto, T.; Zundell, J.; Fatkhutdinov, N.; Wu, S.; Aird, K.M.; Iwasaki, O.; Kossenkov, A.V.; Schultz, D.; et al. NAD+ metabolism governs the proinflammatory senescence-associated secretome. Nat. Cell Biol. 2019, 21, 397–407. [Google Scholar] [CrossRef]
- Ritschka, B.; Knauer-Meyer, T.; Gonçalves, D.S.; Mas, A.; Plassat, J.-L.; Durik, M.; Jacobs, H.; Pedone, E.; Di Vicino, U.; Cosma, M.P.; et al. The senotherapeutic drug ABT-737 disrupts aberrant p21 expression to restore liver regeneration in adult mice. Genes Dev. 2020, 34, 489–494. [Google Scholar] [CrossRef]
- Saleh, T.; Tyutyunyk-Massey, L.; Murray, G.F.; Alotaibi, M.R.; Kawale, A.S.; Elsayed, Z.; Henderson, S.C.; Yakovlev, V.; Elmore, L.W.; Toor, A.; et al. Tumor cell escape from therapy-induced senescence. Biochem. Pharmacol. 2019, 162, 202–212. [Google Scholar] [CrossRef]
- Sladitschek-Martens, H.L.; Guarnieri, A.; Brumana, G.; Zanconato, F.; Battilana, G.; Xiccato, R.L.; Panciera, T.; Forcato, M.; Bicciato, S.; Guzzardo, V.; et al. YAP/TAZ activity in stromal cells prevents ageing by controlling cGAS–STING. Nature 2022, 607, 790–798. [Google Scholar] [CrossRef]
- Blokland, K.E.C.; Waters, D.W.; Schuliga, M.; Read, J.; Pouwels, S.D.; Grainge, C.L.; Jaffar, J.; Westall, G.; Mutsaers, S.E.; Prêle, C.M.; et al. Senescence of IPF Lung Fibroblasts Disrupt Alveolar Epithelial Cell Proliferation and Promote Migration in Wound Healing. Pharmaceutics 2020, 12, 389. [Google Scholar] [CrossRef]
- Suki, B.; Bates, J.H.; Bartolák-Suki, E. Remodeling of the Aged and Emphysematous Lungs: Roles of Microenvironmental Cues. Compr. Physiol. 2022, 12, 3559–3574. [Google Scholar] [CrossRef]
- Zhang, Y.; Tang, J.; Jiang, C.; Yi, H.; Guang, S.; Yin, G.; Wang, M. Metabolic reprogramming in cancer and senescence. Medcomm 2025, 6, e70055. [Google Scholar] [CrossRef] [PubMed]
- Lian, H.; Zhang, Y.; Zhu, Z.; Wan, R.; Wang, Z.; Yang, K.; Ma, S.; Wang, Y.; Xu, K.; Cheng, L.; et al. Fatty acid synthase inhibition alleviates lung fibrosis via β-catenin signal in fibroblasts. Life Sci. Alliance 2025, 8, e202402805. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.L.; Rowe, J.H.; Garcia-De-Alba, C.; Kim, C.F.; Sharpe, A.H.; Haigis, M.C. The aging lung: Physiology, disease, and immunity. Cell 2021, 184, 1990–2019. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Meng, Q.; Gao, X.; Sun, H.; Xu, Z.; Wang, Y.; Zhou, H. Lipid and glucose metabolism in senescence. Front. Nutr. 2023, 10, 1157352. [Google Scholar] [CrossRef]
- Correia-Melo, C.; Marques, F.D.M.; Anderson, R.; Hewitt, G.; Hewitt, R.; Cole, J.; Carroll, B.M.; Miwa, S.; Birch, J.; Merz, A.; et al. Mitochondria are required for pro-ageing features of the senescent phenotype. EMBO J. 2016, 35, 724–742. [Google Scholar] [CrossRef]
- Summer, R.; Shaghaghi, H.; Schriner, D.; Roque, W.; Sales, D.; Cuevas-Mora, K.; Desai, V.; Bhushan, A.; Ramirez, M.I.; Romero, F. Activation of the mTORC1/PGC-1 axis promotes mitochondrial biogenesis and induces cellular senescence in the lung epithelium. Erratum in. Am. J. Physiol. Lung Cell. Mol. Physiol. 2019, 316, L1049–L1060. [Google Scholar] [CrossRef]
- Chen, X.-Y.; Wang, D.-M.; Zhou, Y.; Liu, L.; Zhu, T.; Ran, Z.; Lu, M.-H.; Mu, B.-R. The critical role of mitophagy in cell senescence-mediated pulmonary fibrosis and potential therapeutic strategies. Mol. Biol. Rep. 2025, 52, 565. [Google Scholar] [CrossRef]
- Sabbatinelli, J.; Prattichizzo, F.; Olivieri, F.; Procopio, A.D.; Rippo, M.R.; Giuliani, A. Where Metabolism Meets Senescence: Focus on Endothelial Cells. Front. Physiol. 2019, 10, 1523. [Google Scholar] [CrossRef]
- Wiley, C.D.; Campisi, J. The metabolic roots of senescence: Mechanisms and opportunities for intervention. Nat. Metab. 2021, 3, 1290–1301. [Google Scholar] [CrossRef]
- Singh, R.; Gupta, V.; Kumar, A.; Singh, K. 2-Deoxy-D-Glucose: A Novel Pharmacological Agent for Killing Hypoxic Tumor Cells, Oxygen Dependence-Lowering in COVID-19, and Other Pharmacological Activities. Adv. Pharmacol. Pharm. Sci. 2023, 2023, 9993386. [Google Scholar] [CrossRef]
- Zong, Y.; Li, H.; Liao, P.; Chen, L.; Pan, Y.; Zheng, Y.; Zhang, C.; Liu, D.; Zheng, M.; Gao, J. Mitochondrial dysfunction: Mechanisms and advances in therapy. Signal Transduct. Target. Ther. 2024, 9, 124. [Google Scholar] [CrossRef]
- Duran, I.; Pombo, J.; Sun, B.; Gallage, S.; Kudo, H.; McHugh, D.; Bousset, L.; Avila, J.E.B.; Forlano, R.; Manousou, P.; et al. Detection of senescence using machine learning algorithms based on nuclear features. Nat. Commun. 2024, 15, 1041. [Google Scholar] [CrossRef]
- Abdelmohsen, K.; Mazan-Mamczarz, K.; Munk, R.; Tsitsipatis, D.; Meng, Q.; Rossi, M.; Pal, A.; Shin, C.H.; Martindale, J.L.; Piao, Y.; et al. Identification of senescent cell subpopulations by CITE-seq analysis. Aging Cell 2024, 23, e14297. [Google Scholar] [CrossRef]
- Viswanathan, V.S.; Toro, P.; Corredor, G.; Mukhopadhyay, S.; Madabhushi, A. The state of the art for artificial intelligence in lung digital pathology. J. Pathol. 2022, 257, 413–429. [Google Scholar] [CrossRef]
- Kokosi, M.A.; Margaritopoulos, G.A.; Wells, A.U. Personalised medicine in interstitial lung diseases: Number 6 in the Series “Personalised medicine in respiratory diseases” Edited by Renaud Louis and Nicolas Roche. Eur. Respir. Rev. 2018, 27, 170117. [Google Scholar] [CrossRef] [PubMed]
- Misawa, T.; Hitomi, K.; Miyata, K.; Tanaka, Y.; Fujii, R.; Chiba, M.; Loo, T.M.; Hanyu, A.; Kawasaki, H.; Kato, H.; et al. Identification of Novel Senescent Markers in Small Extracellular Vesicles. Int. J. Mol. Sci. 2023, 24, 2421. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Jiang, D.; Matsuda, J.L.; Ternyak, K.; Zhang, B.; Chu, H.W. Cigarette Smoke Induces Human Airway Epithelial Senescence via Growth Differentiation Factor 15 Production. Am. J. Respir. Cell Mol. Biol. 2016, 55, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Ma, L.; Wu, T.; Tian, Y.; Wu, L. Assessment of cellular senescence potential of PM2.5 using 3D human lung fibroblast spheroids in vitro model. Toxicol. Res. 2024, 13, tfae037. [Google Scholar] [CrossRef]
- Martic, I.; Jansen-Dürr, P.; Cavinato, M. Effects of Air Pollution on Cellular Senescence and Skin Aging. Cells 2022, 11, 2220. [Google Scholar] [CrossRef]
- Yang, D.; Xing, Y.; Song, X.; Qian, Y. The impact of lung microbiota dysbiosis on inflammation. Immunology 2020, 159, 156–166. [Google Scholar] [CrossRef]
- Jang, D.; Shin, J.; Shim, E.; Ohtani, N.; Jeon, O.H. The connection between aging, cellular senescence and gut microbiome alterations: A comprehensive review. Aging Cell 2024, 23, e14315. [Google Scholar] [CrossRef]
- Zhang, W.; Xiong, Y.; Tao, R.; Panayi, A.C.; Mi, B.; Liu, G. Emerging Insight Into the Role of Circadian Clock Gene BMAL1 in Cellular Senescence. Front. Endocrinol. 2022, 13, 915139. [Google Scholar] [CrossRef] [PubMed]
- Chhunchha, B.; Kubo, E.; Singh, D.P. Clock Protein Bmal1 and Nrf2 Cooperatively Control Aging or Oxidative Response and Redox Homeostasis by Regulating Rhythmic Expression of Prdx6. Cells 2020, 9, 1861. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Sundar, I.K.; Lucas, J.H.; Park, J.-G.; Nogales, A.; Martinez-Sobrido, L.; Rahman, I. Circadian clock molecule REV-ERBα regulates lung fibrotic progression through collagen stabilization. Nat. Commun. 2023, 14, 1295. [Google Scholar] [CrossRef] [PubMed]
- Fu, T.E.; Zhou, Z. Senescent cells as a target for anti-aging interventions: From senolytics to immune therapies. J. Transl. Intern. Med. 2025, 13, 33–47. [Google Scholar] [CrossRef]
- Nambiar, A.; Kellogg, D.; Justice, J.; Goros, M.; Gelfond, J.; Pascual, R.; Hashmi, S.; Masternak, M.; Prata, L.; LeBrasseur, N.; et al. Senolytics dasatinib and quercetin in idiopathic pulmonary fibrosis: Results of a phase I, single-blind, single-center, randomized, placebo-controlled pilot trial on feasibility and tolerability. EBioMedicine 2023, 90, 104481. [Google Scholar] [CrossRef]
- Mansfield, L.; Ramponi, V.; Gupta, K.; Stevenson, T.; Mathew, A.B.; Barinda, A.J.; Herbstein, F.; Morsli, S. Emerging insights in senescence: Pathways from preclinical models to therapeutic innovations. npj Aging 2024, 10, 53. [Google Scholar] [CrossRef]
- Bendani, H.; Boumajdi, N.; Belyamani, L.; Ibrahimi, A. Revolutionizing breast cancer immunotherapy by integrating AI and nanotechnology approaches: Review of current applications and future directions. Bioelectron. Med. 2025, 11, 13. [Google Scholar] [CrossRef]
- Baker, J.R.; Daly, L.; Hassibi, S.; Kimura, G.; Nishimoto, Y.; Kizawa, Y.; Ito, K. Senolytic therapy reduces inflammation in epithelial cells from COPD patients and in smoke-exposure mice. Front. Med. 2025, 12, 1451056. [Google Scholar] [CrossRef]
- Yang, C.; Han, Z.; Zhan, W.; Wang, Y.; Feng, J. Predictive investigation of idiopathic pulmonary fibrosis subtypes based on cellular senescence-related genes for disease treatment and management. Front. Genet. 2023, 14, 1157258. [Google Scholar] [CrossRef]
- de Godoy, M.C.X.; Macedo, J.A.; Gambero, A. Researching New Drug Combinations with Senolytic Activity Using Senescent Human Lung Fibroblasts MRC-5 Cell Line. Pharmaceuticals 2024, 17, 70. [Google Scholar] [CrossRef]
- Matsubayashi, S.; Ito, S.; Araya, J.; Kuwano, K. Drugs against metabolic diseases as potential senotherapeutics for aging-related respiratory diseases. Front. Endocrinol. 2023, 14, 1079626. [Google Scholar] [CrossRef]
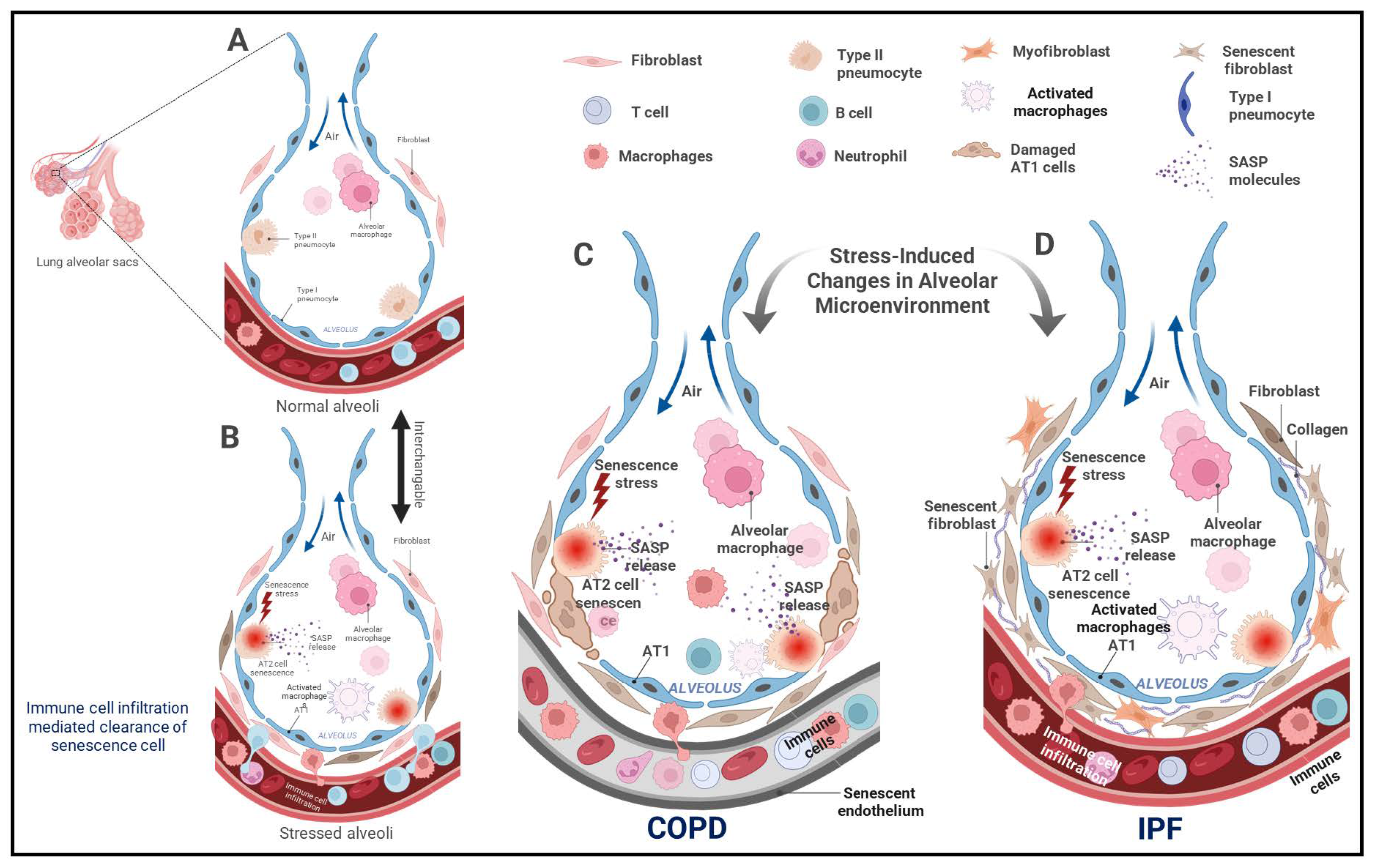
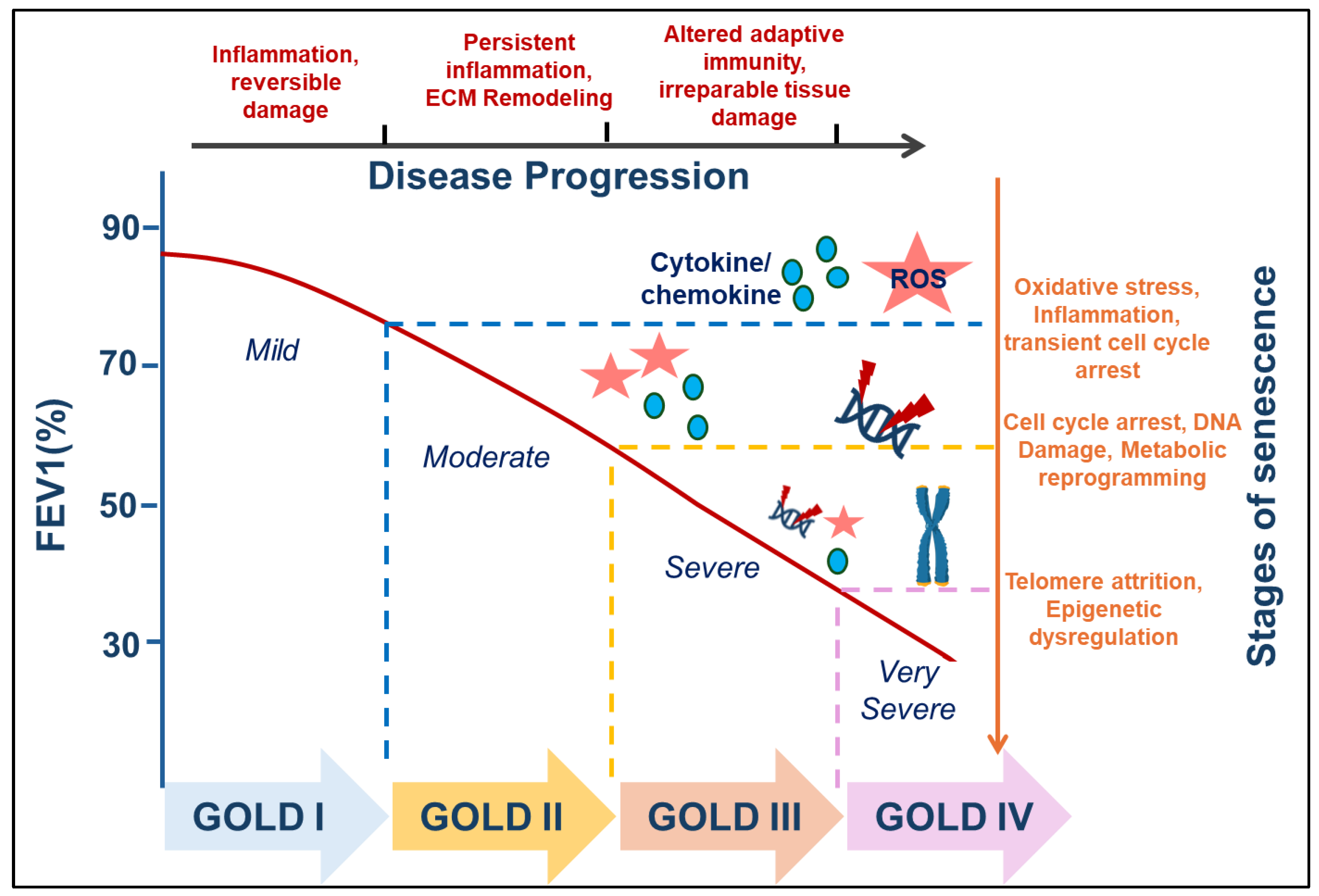
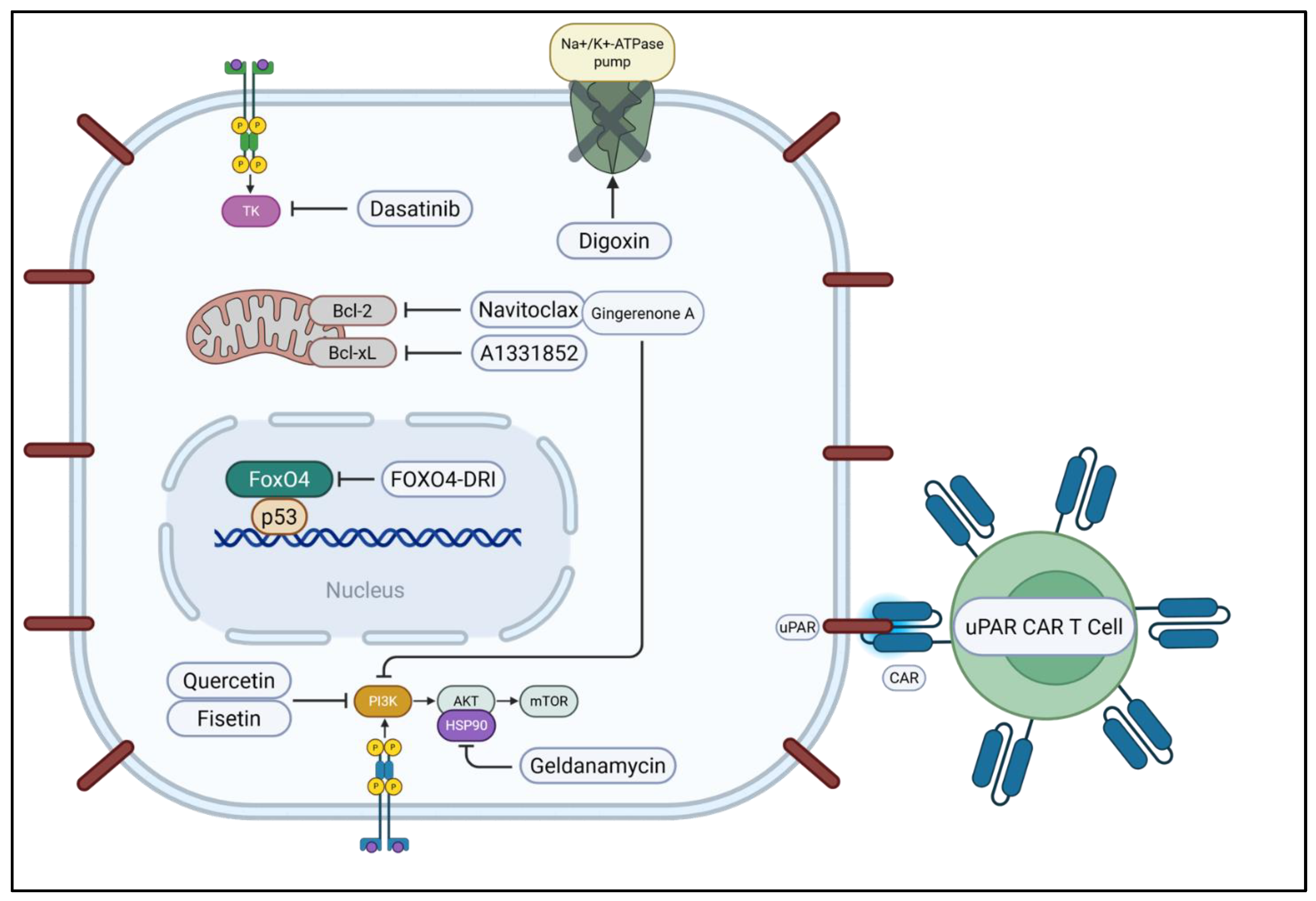
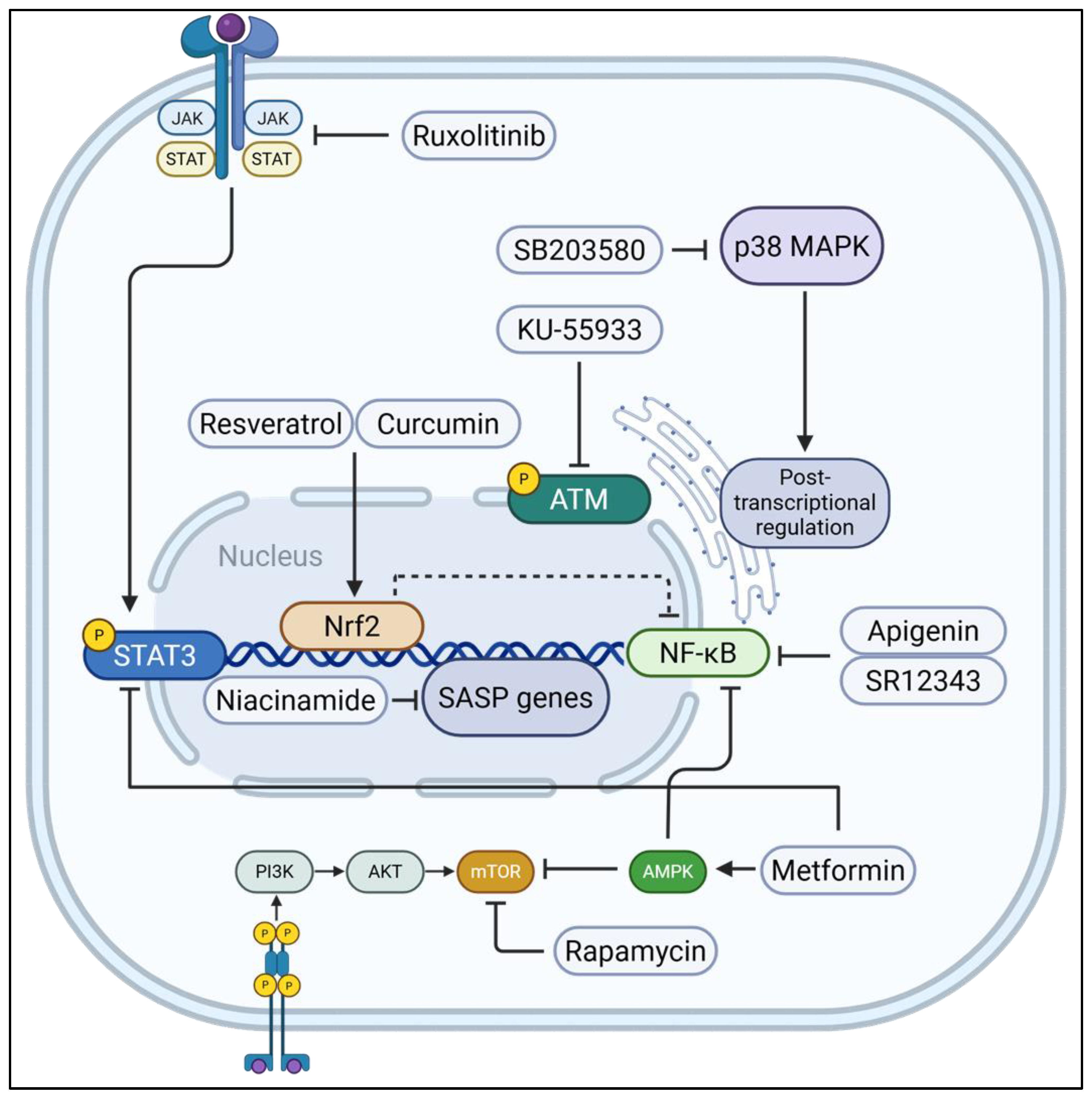
| Human/Mouse | Tissue | Marker | Cell | Disease | Hallmark | Upregulated/ Downregulated Protein | References |
|---|---|---|---|---|---|---|---|
| Mouse | Lungs | TNF | Not available | IPF | SASP | upregulated | [35] |
| Human | Lungs | MMP12 | Not available | IPF | SASP | upregulated | [35] |
| Mouse | Lungs | Bcl-2 | Fibroblast | IPF | SASP | downregulated | [147] |
| Mouse | Lungs | TGFB1 | Pulmonary fibroblasts | IPF | SASP | upregulated | [35,182,183] |
| Human | Lungs | TNF | Not available | IPF | SASP | upregulated | [35] |
| Mouse | Lungs | IL1A | Epithelial cells | IPF | SASP | upregulated | [183] |
| Human | Lungs | TGFB1/2 | Not available | IPF | SASP | downregulated | [35] |
| Mouse | Lungs | SERPINE1 | Not available | IPF | SASP | upregulated | [35,94] |
| COPD | |||||||
| Human | Lungs | IL-6 | Not available | COPD | SASP | upregulated | [184,185] |
| Human | Lungs | IL-10 | Not available | COPD | SASP | upregulated | [184,186] |
| Human | Lungs | VEGFA | Not available | COPD | SASP | upregulated | [185] |
| Human | Lungs | IL-1B | Not available | COPD | SASP | upregulated | [184] |
| Human | Lungs | MMP8 | Not available | COPD | SASP | upregulated | [187] |
| Human | Lungs | CXCL8 | Not available | COPD | SASP | upregulated | [185,187] |
| Human | Lungs | SIRT1 | Macrophages and Epithelial cells | COPD | SASP | downregulated | [137,138] |
| Mixed Diseases/Experimental Conditions | |||||||
| Mouse | Lungs | TP53 | Not available | Aging, ARDS, IPF, COPD | Cell cycle arrest | upregulated | [83,86,94,131,182,183] |
| Mouse | Lungs | CDKN1A | Not available | Aging, Pulmonary fibrosis, ARDS, COPD | Cell cycle arrest | upregulated | [13,29,33,83,86,94,131,183,188,189] |
| Human | Lungs | H2AX | Not available | Aging, COPD | Other | upregulated | [110] |
| Mouse | Lungs | CDKN2A | Not available | Aging, emphysema | Cell cycle arrest | upregulated | [82,83,133,183,190] |
| Human | Lungs | GDF15 | Not available | Aging, ILD, COPD, IPF | SASP | upregulated | [191,192,193] |
| Mouse | Lungs | H2AX | Not available | Development, Aging, IPF | DDR | upregulated | [33] |
| Mouse | Lungs | TNFRSF1B | Hyperoxia | SASP | upregulated | [33] | |
| Mouse | Lungs | MMP12 | Not available | IPF, CS exposure | SASP | upregulated | [35,83] |
| Mouse | Lungs | IL-6 | Not available | IPF, CS exposure | SASP | upregulated | [35,83,194], |
| Human | Lungs | CDKN1A | Epithelial cells | ARDS, IPF, COPD | Cell cycle arrest | upregulated | [35,86] |
| Mouse | Lungs | GDF15 | Not available | Pulmonary Emphysema, IPF | SASP | upregulated | [191,193,195] |
| Mouse | Lungs | IL-1A | Not available | IPF, Tobacco/cigarette smoke (CS) exposure | SASP | upregulated | [35,83,194] |
| Human | Lungs | CDKN2A | Not available | Non-small cell lung, IPF | Cell cycle arrest | upregulated | [196,197], |
| Aging/ARDS | |||||||
| Human | Lungs | TP53 | Fibroblast | ARDS | Cell cycle arrest | upregulated | [35,86] |
| Human | Lungs | SERPINE1 | Aging | SASP | upregulated | [198] | |
| Mouse | Lungs | IL-10 | Immune cells and alveolar epithelial cells | Aging | SASP | upregulated | [199] |
| Class | Compound | Primary Target |
|---|---|---|
| Tyrosine Kinase Inhibitor | Dasatinib | Tyrosine kinases, SCAP survival pathways |
| Flavonoid | Quercetin | PI3K pathway, mitochondria (via Bcl-2 family) |
| Fisetin | PI3K/AKT pathway, mitochondria | |
| Bcl-2 Family Inhibitor | Navitoclax (ABT-263) | Mitochondrial apoptosis regulators (Bcl-2 family) |
| Bcl-xL Selective Inhibitor | A1331852/A1155463 | Mitochondrial apoptosis pathway (Bcl-xL) |
| HSP90 Inhibitor | 17-DMAG/17-AAG/Geldanamycin | Chaperone protein complexes (HSP90-AKT axis) |
| Natural Product | Gingerenone A | Mitochondria, caspase cascade |
| Peptide | FOXO4-DRI | Nucleus (p53 signaling) |
| Immunotherapy | uPAR-targeted CAR T Cells | Cell surface receptor (uPAR) |
| Cardiac Glycoside | Ouabain/Digoxin | Plasma membrane (Na+/K+-ATPase pump) |
| Class | Compound | Primary Target |
|---|---|---|
| mTOR Inhibitor | Rapamycin (Sirolimus) | mTORC1 complex |
| SIRT1 Activator | Resveratrol | Nucleus (SIRT1, NF-κB, Nrf2) |
| Polyphenol | Curcumin | Nucleus (NF-κB, Nrf2) |
| Flavonoid | Apigenin/Kaempferol | NF-κB signaling pathway |
| Vitamin | Niacinamide (Vitamin B3) | Nucleus/Gene transcription |
| Topical Agent | Niacinamide + Hyaluronic Acid | Gene expression in skin cells |
| Biguanide | Metformin | AMPK, NF-κB, STAT3 pathways |
| Statin | Atorvastatin/Pravastatin/Simvastatin | Mitochondria, NF-κB, eNOS |
| JAK Inhibitor | Ruxolitinib | JAK/STAT pathway |
| ATM Inhibitor | KU-55933/KU-60019 | DDR pathway (ATM, NF-κB) |
| p38 MAPK Inhibitor | SB203580/UR13756/BIRB796 | p38 MAPK signaling |
| NF-κB Inhibitor | SR12343 | NF-κB signaling pathway |
| NCT Number | Condition(s) | Intervention(s) | Status | Focus of the Study |
|---|---|---|---|---|
| NCT02874989 | IPF | Dasatinib + Quercetin (senolytic) | Completed | Pilot trial testing intermittent senolytic dosing in IPF patients for safety, feasibility, and initial efficacy signals. |
| NCT01708278 | COPD | Quercetin (senomorphic/antioxidant) | Completed | 1-week dose-escalation study to establish safety and tolerability in COPD patients. |
| NCT03989271 | COPD | Quercetin (senomorphic) | Completed | Placebo-controlled study evaluating long-term safety and effects on airway epithelial gene expression. |
| NCT06003270 | COPD | Quercetin (senomorphic) | Recruiting (Phase II) | Testing whether quercetin improves inflammation and clinical outcomes in COPD patients. |
| NCT03651895 | COPD (non-diabetic) | Metformin (senomorphic; AMPK/mTOR axis) | Active, not recruiting | Studying metformin’s effects on airway glucose and senescence-linked pathways. |
| NCT00414648 | Lymphangioleiomyomatosis (LAM) | Sirolimus (rapamycin, senomorphic) | Completed (MILES trial) | Pivotal Phase III trial showing sirolimus stabilizes lung function in LAM patients. |
| NCT02432560 | LAM | Sirolimus | Active | Evaluating long-term safety and durability of sirolimus treatment. |
| NCT03150914 | LAM | Low-dose Sirolimus | Active | Testing early, long-term sirolimus to prevent disease progression in LAM. |
| NCT03253913 | LAM | Sirolimus ± Resveratrol | Completed/Active follow-up | Focused on biomarker changes (e.g., VEGF-D) in response to sirolimus with or without resveratrol. |
| NCT04537299 | COVID-19 (older adults, hospitalized) | Fisetin (senolytic) | Active | Assessing whether fisetin reduces complications in older adults hospitalized with COVID-19. |
| NCT04771611 | COVID-19 | Fisetin (senolytic) | Active | Evaluating fisetin’s role in reducing disease severity and complications in COVID-19. |
| Terms | Definition |
|---|---|
| Senescent cell (SnC) | A cell in the senescent state. |
| Senescence-associated secretory phenotype (SASP) | The context-dependent set of cytokines, chemokines, growth factors, proteases, lipids, and extracellular vesicles secreted by senescent cells. |
| Senotype | The subtype/identity of senescence in a given context (defined by trigger, markers, and SASP profile). |
| Senotyping | Experimental characterization of a senotype. |
| Replicative senescence (RS) | Senescence triggered by telomere attrition after repeated divisions, engaging DNA damage checkpoints. |
| Stress-induced premature senescence (SIPS) | Senescence caused by non-telomeric stressors (e.g., oxidative, inflammatory, toxicant exposure). |
| Oncogene-induced senescence (OIS) | Senescence elicited by oncogene hyperactivation as an early tumor-suppressive barrier. |
| Therapy-induced senescence (TIS) | Senescence induced by chemo- or radiotherapy in normal or malignant cells. |
| Mitochondrial dysfunction-associated senescence (MiDAS) | A senescence program driven by mitochondrial/metabolic stress with a distinct SASP signature. |
| Paracrine (bystander) senescence | Senescence induced in neighboring cells by SASP factors released from senescent cells. |
| Pseudosenescence | A reversible state that mimics some senescence markers (e.g., SA-β-gal, p16^INK4a) without establishing stable, irreversible cell-cycle arrest. |
| Immunosenescence | Age-associated decline of immune function, including impaired clearance of senescent cells. |
| Inflammaging | Chronic, low-grade sterile inflammation associated with aging and sustained SASP activity. |
| Senolytics | Agents that preferentially eliminate senescent cells. |
| Senomorphics (senostatics) | Agents that suppress deleterious SASP/signaling without killing senescent cells. |
| Senotherapy/Senotherapeutics | Umbrella term for therapeutic strategies targeting senescence (senolytics and senomorphics). |
| SA-β-gal (senescence-associated β-galactosidase) | A commonly used senescence activity readout measured at pH 6.0. |
| DNA damage response (DDR) | Checkpoint and repair signaling activated by DNA damage that helps enforce senescence. |
| SAHF (senescence-associated heterochromatin foci) | Repressive chromatin structures that stabilize proliferation arrest. |
| DNA-SCARS | DNA segments with chromatin alterations that reinforce persistent DDR signaling in senescence. |
| cGAS–STING signaling | Cytosolic DNA sensing pathway that amplifies SASP and innate immune signaling in senescence. |
| YAP–TAZ mechanotransduction | Matrix- and stiffness-responsive transcriptional regulators that can modulate fibroblast activation and senescence. |
| AT2 (AEC2) and AT1 cells | Alveolar type II progenitor cells and flattened type I gas-exchange cells of the distal lung. |
| Epithelial–mesenchymal transition (EMT) | A cell-state change linked to fibrosis and, in some contexts, senescence-associated remodeling. |
| TGF-β signaling | Profibrotic pathway frequently intersecting with senescence programs and SASP output. |
| NF-κB/JAK–STAT/mTOR | Canonical inflammatory and growth pathways that regulate SASP composition and intensity. |
| p16INK4a | CDK inhibitor that enforces RB-mediated cell-cycle arrest in senescence. |
| p21Cip1/Waf1 | CDK inhibitor downstream of p53 that enforces G1/S arrest in senescence. |
| TP53 (p53) | Tumor-suppressor transcription factor that initiates cell-cycle arrest and senescence upon stress/DNA damage. |
| Telomere attrition | Progressive telomere shortening that precipitates replicative senescence. |
| Autophagy/Mitophagy | Catabolic pathways that remodel proteostasis and mitochondria during senescence. |
| BCL-2 family dependency | Anti-apoptotic reliance (e.g., BCL-xL, BCL-2, MCL-1) common in senescent cells and targetable by senolytics. |
| Senescence escape | Loss of stable arrest and re-entry into the cell cycle from a senescent-like state. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ozdemir, S.A.; Faizan, M.I.; Kaur, G.; Shaikh, S.B.; Ul Islam, K.; Rahman, I. Heterogeneity of Cellular Senescence, Senotyping, and Targeting by Senolytics and Senomorphics in Lung Diseases. Int. J. Mol. Sci. 2025, 26, 9687. https://doi.org/10.3390/ijms26199687
Ozdemir SA, Faizan MI, Kaur G, Shaikh SB, Ul Islam K, Rahman I. Heterogeneity of Cellular Senescence, Senotyping, and Targeting by Senolytics and Senomorphics in Lung Diseases. International Journal of Molecular Sciences. 2025; 26(19):9687. https://doi.org/10.3390/ijms26199687
Chicago/Turabian StyleOzdemir, Said Ali, Md Imam Faizan, Gagandeep Kaur, Sadiya Bi Shaikh, Khursheed Ul Islam, and Irfan Rahman. 2025. "Heterogeneity of Cellular Senescence, Senotyping, and Targeting by Senolytics and Senomorphics in Lung Diseases" International Journal of Molecular Sciences 26, no. 19: 9687. https://doi.org/10.3390/ijms26199687
APA StyleOzdemir, S. A., Faizan, M. I., Kaur, G., Shaikh, S. B., Ul Islam, K., & Rahman, I. (2025). Heterogeneity of Cellular Senescence, Senotyping, and Targeting by Senolytics and Senomorphics in Lung Diseases. International Journal of Molecular Sciences, 26(19), 9687. https://doi.org/10.3390/ijms26199687








