Special Issue: Antibody Therapy for Hematologic Malignancies
Funding
Acknowledgments
Conflicts of Interest
References
- Sun, K.; Wu, H.; Zhu, Q.; Gu, K.; Wei, H.; Wang, S.; Li, L.; Wu, C.; Chen, R.; Pang, Y.; et al. Global landscape and trends in lifetime risks of haematologic malignancies in 185 countries: Population-based estimates from GLOBOCAN 2022. eClinicalMedicine 2025, 83, 103193. [Google Scholar] [CrossRef]
- Li, Z.; Chen, G.; Du, G. Global, regional, and national economic burden of hematologic malignancies (1990–2021) with projections to 2050. Front. Public Health 2025, 13, 1570792. [Google Scholar] [CrossRef]
- Cui, Z.X.; Yao, S.X.; Zhang, Y.X.; Lu, H.Y.; Sun, L.P.; Shi, L. Bruton’s tyrosine kinase (BTK) inhibitors: An updated patent review (2019–2024). Expert Opin. Ther. Pat. 2025, 1–25. [Google Scholar] [CrossRef]
- Das, D.; Xie, L.; Qiao, D.; Cao, Y.; Jiang, S.; Zheng, M.; Liu, Z.; Li, Y.; Jia, J.; Lv, Y.; et al. Discovery of Reversible, Noncovalent Bruton’s Tyrosine Kinase Inhibitors Targeting BTK C481S Mutation. ACS Med. Chem. Lett. 2025, 16, 1038–1047. [Google Scholar] [CrossRef]
- Cappell, K.M.; Kochenderfer, J.N. Long-term outcomes following CAR T cell therapy: What we know so far. Nat. Rev. Clin. Oncol. 2023, 20, 359–371. [Google Scholar] [CrossRef]
- Jiang, N.; Yang, Z.; Miao, H.; Xing, S.; Wang, S.; Li, N. Recent advances in universal chimeric antigen receptor T cell therapy. J. Hematol. Oncol. 2025, 18, 82. [Google Scholar] [CrossRef]
- Bilgihan, M.T.; Eryigit, A.N.; Ciftciler, R. Efficacy and Safety of Immune Checkpoint Inhibitors in Hematologic Malignancies. Clin. Lymphoma Myeloma Leuk. 2024, 24, 23–31. [Google Scholar] [CrossRef]
- Olsen, T.A.; Barnum, K.J.; Avigan, D.; Rosenblatt, J. Cancer vaccines in hematologic malignancy: A systematic review of the rational and evidence for clinical use. Best Pract. Res. Clin. Haematol. 2025, 38, 101650. [Google Scholar] [CrossRef]
- Sousa-Pimenta, M.; Dos Santos, N.R. Cytokine-based immunotherapy in hematolymphoid malignancies. Int. Rev. Cell Mol. Biol. 2025, 396, 55–79. [Google Scholar]
- Franklin, J.; Eichenauer, D.A.; Becker, I.; Monsef, I.; Engert, A. Optimisation of chemotherapy and radiotherapy for untreated Hodgkin lymphoma patients with respect to second malignant neoplasms, overall and progression-free survival: Individual participant data analysis. Cochrane Database Syst. Rev. 2017, 9, CD008814. [Google Scholar] [CrossRef]
- Watts, J.M.; Baer, M.R.; Yang, J.; Prebet, T.; Lee, S.; Schiller, G.J.; Dinner, S.N.; Pigneux, A.; Montesinos, P.; Wang, E.S.; et al. Olutasidenib alone or with azacitidine in IDH1-mutated acute myeloid leukaemia and myelodysplastic syndrome: Phase 1 results of a phase 1/2 trial. Lancet Haematol. 2023, 10, e46–e58, Erratum in Lancet Haematol. 2023, 10, e9. [Google Scholar] [CrossRef]
- Goldkuhle, M.; Kreuzberger, N.; von Tresckow, B.; Eichenauer, D.A.; Specht, L.; Monsef, I.; Skoetz, N. Chemotherapy alone versus chemotherapy plus radiotherapy for adults with early-stage Hodgkin’s lymphoma. Cochrane Database Syst. Rev. 2024, 12, CD007110. [Google Scholar]
- Jonas, B.A.; Fisch, S.C.; Curtin, P.T.; Schiller, G.J.; Jeyakumar, D.; Tzachanis, D.; Bejar, R.; Qi, L.; Wieduwilt, M.J.; Tuscano, J.M.; et al. University of California Hematologic Malignancies, C. A phase 1 trial of ibrutinib and azacitidine for higher risk myelodysplastic syndromes (University of California Hematologic Malignancies Consortium Study 1503). Leuk. Res. 2025, 155, 107717. [Google Scholar] [CrossRef]
- Yuan, X.; Wang, F.; Zhao, P.; Yang, B.; Yang, X.; Tian, T.; Li, B.; Liu, G.; Wang, S.; Tang, D.; et al. Efficacy and safety of CD19 combined with CD22 or CD20 chimeric antigen receptor T-cell therapy for hematological malignancies. Front. Immunol. 2025, 16, 1577360. [Google Scholar] [CrossRef]
- Grillo-Lopez, A.J. Rituximab: An insider’s historical perspective. Semin. Oncol. 2000, 27 (Suppl. 12), 9–16. [Google Scholar]
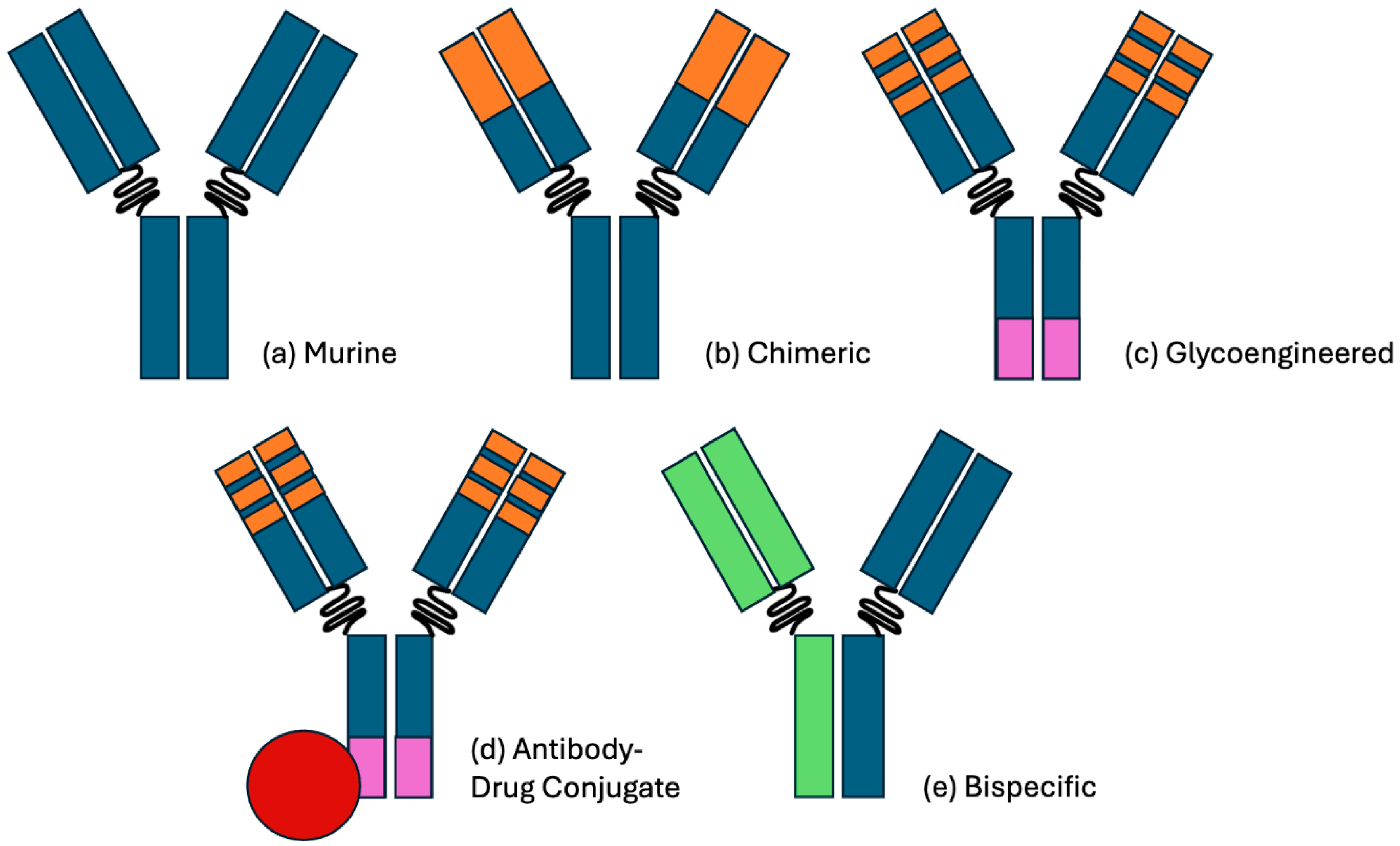
- Naman, J.; Shah, N.; Heyman, B.M. Antibody Therapy for Patients with Lymphoid Malignancies: Past and Present. Int. J. Mol. Sci. 2025, 26, 1711. [Google Scholar] [CrossRef]
- Reff, M.E.; Carner, K.; Chambers, K.S.; Chinn, P.C.; Leonard, J.E.; Raab, R.; Newman, R.A.; Hanna, N.; Anderson, D.R. Depletion of B cells in vivo by a chimeric mouse human monoclonal antibody to CD20. Blood 1994, 83, 435–445. [Google Scholar] [CrossRef]
- Harjunpaa, A.; Junnikkala, S.; Meri, S. Rituximab (anti-CD20) therapy of B-cell lymphomas: Direct complement killing is superior to cellular effector mechanisms. Scand. J. Immunol. 2000, 51, 634–641. [Google Scholar] [CrossRef]
- Shan, D.; Ledbetter, J.A.; Press, O.W. Apoptosis of malignant human B cells by ligation of CD20 with monoclonal antibodies. Blood 1998, 91, 1644–1652. [Google Scholar] [CrossRef]
- Byrd, J.C.; Kitada, S.; Flinn, I.W.; Aron, J.L.; Pearson, M.; Lucas, D.; Reed, J.C. The mechanism of tumor cell clearance by rituximab in vivo in patients with B-cell chronic lymphocytic leukemia: Evidence of caspase activation and apoptosis induction. Blood 2002, 99, 1038–1043. [Google Scholar] [CrossRef]
- Mossner, E.; Brunker, P.; Moser, S.; Puntener, U.; Schmidt, C.; Herter, S.; Grau, R.; Gerdes, C.; Nopora, A.; van Puijenbroek, E.; et al. Increasing the efficacy of CD20 antibody therapy through the engineering of a new type II anti-CD20 antibody with enhanced direct and immune effector cell-mediated B-cell cytotoxicity. Blood 2010, 115, 4393–4402. [Google Scholar] [CrossRef]
- Agliardi, S.; Veronese, C.; Panzeri, F.; Palazzini, S.; Guarnieri, G.; Loiacono, S.; Martinelli, V.; Potenza, A.M.; Sbraga, E.; Rissotto, E.; et al. Immunocytokines in cancer treatment: A systematic review. Cancer Treat. Rev. 2025, 139, 102978. [Google Scholar] [CrossRef]
- Caserta, S.; Campo, C.; Cancemi, G.; Neri, S.; Stagno, F.; Mannina, D.; Allegra, A. Bispecific Antibodies and Antibody-Drug Conjugates in Relapsed/Refractory Aggressive Non-Hodgkin Lymphoma, Focusing on Diffuse Large B-Cell Lymphoma. Cancers 2025, 17, 2479. [Google Scholar] [CrossRef]
- Jensen, M.; Winkler, U.; Manzke, O.; Diehl, V.; Engert, A. Rapid tumor lysis in a patient with B-cell chronic lymphocytic leukemia and lymphocytosis treated with an anti-CD20 monoclonal antibody (IDEC-C2B8, rituximab). Ann. Hematol. 1998, 77, 89–91. [Google Scholar] [CrossRef]
- Winkler, U.; Jensen, M.; Manzke, O.; Schulz, H.; Diehl, V.; Engert, A. Cytokine-release syndrome in patients with B-cell chronic lymphocytic leukemia and high lymphocyte counts after treatment with an anti-CD20 monoclonal antibody (rituximab, IDEC-C2B8). Blood 1999, 94, 2217–2224. [Google Scholar] [CrossRef]
- Lim, L.C.; Koh, L.P.; Tan, P. Fatal cytokine release syndrome with chimeric anti-CD20 monoclonal antibody rituximab in a 71-year-old patient with chronic lymphocytic leukemia. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 1999, 17, 1962–1963. [Google Scholar]
- Amitai, I.; Gafter-Gvili, A.; Shargian-Alon, L.; Raanani, P.; Gurion, R. Obinutuzumab-related adverse events: A systematic review and meta-analysis. Hematol. Oncol. 2021, 39, 215–221. [Google Scholar] [CrossRef]
- Kou, K.; Zhou, Q.; Du, L.; Xu, F. Obinutuzumab-induced severe acute thrombocytopenia: A case report and literature review. Front. Immunol. 2025, 16, 1609862. [Google Scholar] [CrossRef]
- Davis, T.A.; Czerwinski, D.K.; Levy, R. Therapy of B-cell lymphoma with anti-CD20 antibodies can result in the loss of CD20 antigen expression. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 1999, 5, 611–615. [Google Scholar]
- Kinoshita, T.; Nagai, H.; Murate, T.; Saito, H. CD20-negative relapse in B-cell lymphoma after treatment with Rituximab. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 1998, 16, 3916. [Google Scholar]
- Donati, G.; Amati, B. MYC and therapy resistance in cancer: Risks and opportunities. Mol. Oncol. 2022, 16, 3828–3854. [Google Scholar] [CrossRef]
- de Jonge, A.V.; Csikos, T.; Eken, M.; Bulthuis, E.P.; Poddighe, P.J.; Roemer, M.G.M.; Chamuleau, M.E.D.; Mutis, T. Delineating MYC-Mediated Escape Mechanisms from Conventional and T Cell-Redirecting Therapeutic Antibodies. Int. J. Mol. Sci. 2024, 25, 12094. [Google Scholar] [CrossRef]
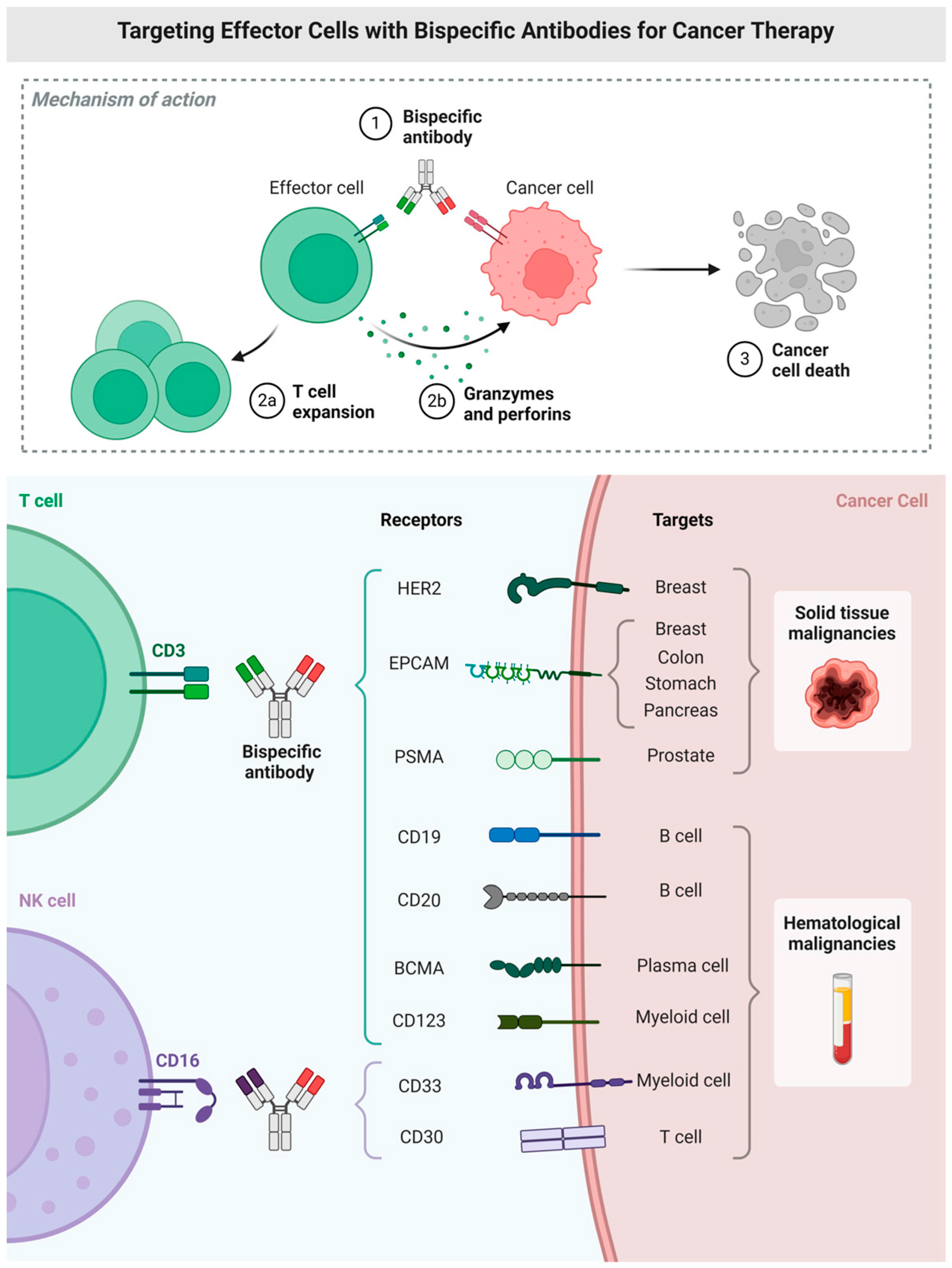
- Staerz, U.D.; Bevan, M.J. Hybrid hybridoma producing a bispecific monoclonal antibody that can focus effector T-cell activity. Proc. Natl. Acad. Sci. USA 1986, 83, 1453–1457, Erratum in Proc. Natl. Acad. Sci. USA 1986, 83, 4972.. [Google Scholar] [CrossRef]
- Staerz, U.D.; Kanagawa, O.; Bevan, M.J. Hybrid antibodies can target sites for attack by T cells. Nature 1985, 314, 628–631. [Google Scholar] [CrossRef]
- Ma, J.; Mo, Y.; Tang, M.; Shen, J.; Qi, Y.; Zhao, W.; Huang, Y.; Xu, Y.; Qian, C. Bispecific Antibodies: From Research to Clinical Application. Front. Immunol. 2021, 12, 626616. [Google Scholar] [CrossRef]
- Nagorsen, D.; Kufer, P.; Baeuerle, P.A.; Bargou, R. Blinatumomab: A historical perspective. Pharmacol. Ther. 2012, 136, 334–342. [Google Scholar] [CrossRef]
- Topp, M.S.; Gokbuget, N.; Zugmaier, G.; Degenhard, E.; Goebeler, M.E.; Klinger, M.; Neumann, S.A.; Horst, H.A.; Raff, T.; Viardot, A.; et al. Long-term follow-up of hematologic relapse-free survival in a phase 2 study of blinatumomab in patients with MRD in B-lineage ALL. Blood 2012, 120, 5185–5187. [Google Scholar] [CrossRef]
- Fischer, C.; Chen, S.S.; Nimmerfroh, J.; Eugster, A.; Stucheli, S.; Schultheiss, C.; Widmer, C.; Heim, D.; Kasenda, B.; Passweg, J.; et al. IGLV3-21(R110)-directed bispecific antibodies activate T cells and promote killing in a high-risk subset of chronic lymphocytic leukemia. Haematologica 2025. [Google Scholar] [CrossRef]
- Markl, F.; Schultheiss, C.; Ali, M.; Chen, S.S.; Zintchenko, M.; Egli, L.; Mietz, J.; Chijioke, O.; Paschold, L.; Spajic, S.; et al. Mutation-specific CAR T cells as precision therapy for IGLV3-21(R110) expressing high-risk chronic lymphocytic leukemia. Nat. Commun. 2024, 15, 993. [Google Scholar] [CrossRef]
- Amoozgar, B.; Bangolo, A.; Habibi, M.; Cho, C.; Goy, A. From Molecular Precision to Clinical Practice: A Comprehensive Review of Bispecific and Trispecific Antibodies in Hematologic Malignancies. Int. J. Mol. Sci. 2025, 26, 5319. [Google Scholar] [CrossRef]
- Chang, A.; Pelletier, A.N.; McGuire, D.J.; Tsagiopoulou, M.; Karipidou, M.; Ayers, A.; Leal, A.M.K.; Churnetski, M.C.; O’Leary, C.B.; Switchenko, J.M.; et al. PD-1 expression identifies proliferating malignant CLL B cells and is a potential biomarker of response to BTK inhibitor therapy. Proc. Natl. Acad. Sci. USA 2025, 122, e2426935122. [Google Scholar] [CrossRef]
- Hayday, A.; Dechanet-Merville, J.; Rossjohn, J.; Silva-Santos, B. Cancer immunotherapy by gammadelta T cells. Science 2024, 386, eabq7248. [Google Scholar] [CrossRef]
- Marischen, L.; Fritsch, J.; Ilic, J.; Wahl, L.; Bertsch, T.; Knop, S.; Bold, A. Two Are Better than One: The Bi-Specific Antibody Mosunetuzumab Reveals an Improved Immune Response of Vgamma9Vdelta2 T Cells Targeting CD20 in Malignant B Cells in Comparison to the Mono-Specific Antibody Obinutuzumab. Int. J. Mol. Sci. 2025, 26, 1262. [Google Scholar] [CrossRef]
- Budde, L.E.; Assouline, S.; Sehn, L.H.; Schuster, S.J.; Yoon, S.S.; Yoon, D.H.; Matasar, M.J.; Bosch, F.; Kim, W.S.; Nastoupil, L.J.; et al. Single-Agent Mosunetuzumab Shows Durable Complete Responses in Patients with Relapsed or Refractory B-Cell Lymphomas: Phase I Dose-Escalation Study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2022, 40, 481–491. [Google Scholar] [CrossRef]
- Budde, L.E.; Sehn, L.H.; Matasar, M.; Schuster, S.J.; Assouline, S.; Giri, P.; Kuruvilla, J.; Canales, M.; Dietrich, S.; Fay, K.; et al. Safety and efficacy of mosunetuzumab, a bispecific antibody, in patients with relapsed or refractory follicular lymphoma: A single-arm, multicentre, phase 2 study. Lancet Oncol. 2022, 23, 1055–1065. [Google Scholar] [CrossRef]
- Bayly-McCredie, E.; Treisman, M.; Fiorenza, S. Safety and Efficacy of Bispecific Antibodies in Adults with Large B-Cell Lymphomas: A Systematic Review of Clinical Trial Data. Int. J. Mol. Sci. 2024, 25, 9736. [Google Scholar] [CrossRef]
- Juarez-Salcedo, L.M.; Nimkar, S.; Corazon, A.M.; Dalia, S. Loncastuximab Tesirine in the Treatment of Relapsed or Refractory Diffuse Large B-Cell Lymphoma. Int. J. Mol. Sci. 2024, 25, 7580. [Google Scholar] [CrossRef]
- Mullard, A. FDA approves ADC Therapeutics’ loncastuximab tesirine, ushering in a new cytotoxic payload. Nat. Rev. Drug Discov. 2021, 20, 414. [Google Scholar] [CrossRef]
- Cremasco, F.; Menietti, E.; Speziale, D.; Sam, J.; Sammicheli, S.; Richard, M.; Varol, A.; Klein, C.; Umana, P.; Bacac, M.; et al. Cross-linking of T cell to B cell lymphoma by the T cell bispecific antibody CD20-TCB induces IFNgamma/CXCL10-dependent peripheral T cell recruitment in humanized murine model. PLoS ONE 2021, 16, e0241091. [Google Scholar] [CrossRef]
- Sun, L.L.; Ellerman, D.; Mathieu, M.; Hristopoulos, M.; Chen, X.; Li, Y.; Yan, X.; Clark, R.; Reyes, A.; Stefanich, E.; et al. Anti-CD20/CD3 T cell-dependent bispecific antibody for the treatment of B cell malignancies. Sci. Transl. Med. 2015, 7, 287ra70. [Google Scholar] [CrossRef]
- Pfeifer, M.; Zheng, B.; Erdmann, T.; Koeppen, H.; McCord, R.; Grau, M.; Staiger, A.; Chai, A.; Sandmann, T.; Madle, H.; et al. Anti-CD22 and anti-CD79B antibody drug conjugates are active in different molecular diffuse large B-cell lymphoma subtypes. Leukemia 2015, 29, 1578–1586. [Google Scholar] [CrossRef] [PubMed]
- Damiani, D.; Tiribelli, M. Monoclonal Antibodies Against Myeloid Leukemia Cells: Current Knowledge and Future Directions. Int. J. Mol. Sci. 2025, 26, 4571. [Google Scholar] [CrossRef] [PubMed]
- Woyach, J.A.; Furman, R.R.; Liu, T.M.; Ozer, H.G.; Zapatka, M.; Ruppert, A.S.; Xue, L.; Li, D.H.; Steggerda, S.M.; Versele, M.; et al. Resistance mechanisms for the Bruton’s tyrosine kinase inhibitor ibrutinib. N. Engl. J. Med. 2014, 370, 2286–2294. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Butchar, J.P. Special Issue: Antibody Therapy for Hematologic Malignancies. Int. J. Mol. Sci. 2025, 26, 9463. https://doi.org/10.3390/ijms26199463
Butchar JP. Special Issue: Antibody Therapy for Hematologic Malignancies. International Journal of Molecular Sciences. 2025; 26(19):9463. https://doi.org/10.3390/ijms26199463
Chicago/Turabian StyleButchar, Jonathan P. 2025. "Special Issue: Antibody Therapy for Hematologic Malignancies" International Journal of Molecular Sciences 26, no. 19: 9463. https://doi.org/10.3390/ijms26199463
APA StyleButchar, J. P. (2025). Special Issue: Antibody Therapy for Hematologic Malignancies. International Journal of Molecular Sciences, 26(19), 9463. https://doi.org/10.3390/ijms26199463



