Kidney Transplantation in Patients with Multiple Myeloma: Current Evidence, Challenges, and Future Directions
Abstract
1. Introduction
2. Methods
3. Renal Involvement in Multiple Myeloma
3.1. Pathophysiological Mechanisms
3.1.1. Light Chain Cast Nephropathy
3.1.2. Monoclonal Immunoglobulin Deposition and Aggregation Disorders
3.1.3. Renal Involvement Without Monoclonal Immunoglobulin Deposits
3.1.4. Indirect Mechanisms
3.2. Epidemiology of Kidney Injury in Multiple Myeloma
3.3. Prognostic Implications
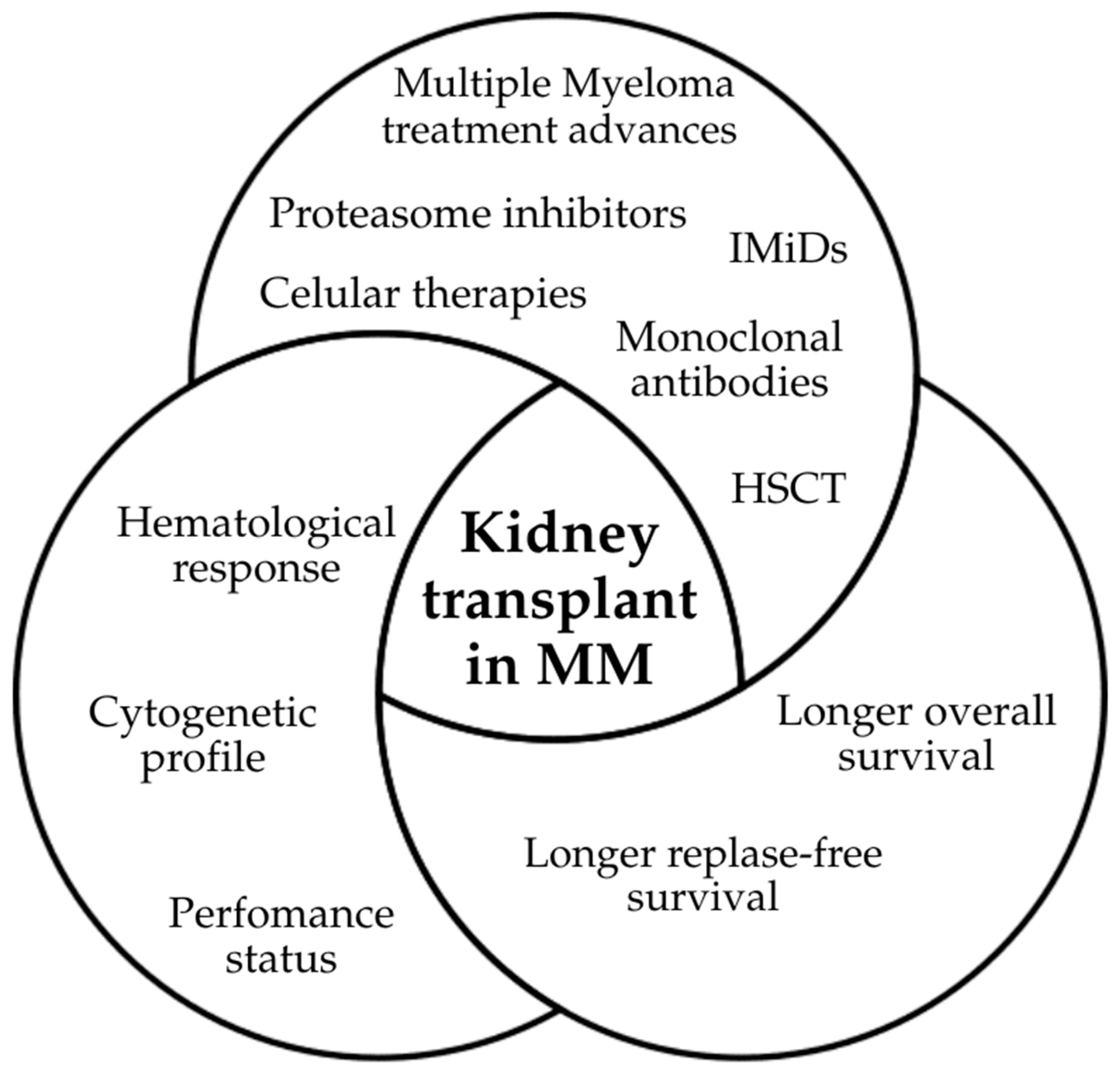
4. Advances in Myeloma Therapy and Impact on Transplant Candidacy
4.1. Evolution of Multiple Myeloma Therapy
4.2. Hematopoietic Stem Cell Transplantation
4.3. Implications for Kidney Transplant Eligibility
5. Kidney Transplantation in Patients with Multiple Myeloma
5.1. Rationale for Kidney Transplantation in Patients with Multiple Myeloma
5.2. Historical Case Reports
5.3. Current Evidence
5.4. Kidney Transplantation in Particular Situations
5.5. Combined Approaches
6. Eligibility Criteria for Kidney Transplantation in Multiple Myeloma
6.1. Hematological Criteria
6.2. Nephrological Criteria
- Clinical stability and absence of active infection, absence of active neoplasms;
- Absence of uncontrolled comorbidities;
- Capacity for adherence to immunosuppressive therapy and follow-up [2].
6.3. Timing for Kidney Transplantation
- Standard-risk, MRD-negative patients may be considered after 6 months;
- Standard-risk, MRD-positive patients or high-risk, MRD-negative patients are advised to wait at least 12 months;
- High-risk, MRD-positive patients without remission are unlikely to benefit from kidney transplant.
6.4. Multidisciplinary Context
7. Proposed Algorithm for Patient Selection and Follow Up
- Standard-risk, MRD-negative: consider ≥6 months post-therapy/HSCT.
- High-risk cytogenetics or MRD-positive: wait ≥12 months.
8. Immunosuppression and Maintenance Strategies
8.1. Challenges of Immunosuppression in Multiple Myeloma
8.2. Strategies for Maintenance Therapy
8.3. Proposed Monitoring Strategies
9. Discussion and Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AL | Amyloid light chain |
| AKI | Acute Kidney Injury |
| CR | Complete response |
| ECOG | Eastern Cooperative Oncology Group (performance status) |
| eGFR | Estimated glomerular filtration rate |
| ESD/ESRD | End-stage renal disease |
| FISH | Fluorescence in situ hybridization |
| FLCs | Free light chains |
| HSCT | Hematopoietic stem cell transplantation |
| IMiD | Immunomodulatory drugs |
| IMWG | International Myeloma Working Group |
| KDIGO | Kidney Disease: Improving Global Outcomes |
| KPS | Karnofsky Performance Status |
| LCDD | Light chain deposition disease |
| LCCN | Light chain cast nephropathy |
| MGRS | Monoclonal gammopathy of renal significance |
| MM | Multiple myeloma |
| MRD | Minimal residual disease |
| OS | Overall survival |
| PFS | Progression-free survival |
| PR | Partial response |
| RRT | Renal replacement therapy |
| sCR | Stringent complete response |
| SMM | Smoldering multiple myeloma |
| VGPR | Very good partial response |
References
- Ávila, G.; Roldão, M.; Ferreira, H.; Coelho, I.; Chuva, T.; Paiva, A.; Costa, J.M. Kidney Transplantation in Multiple Myeloma in 2023: A Short Review. Clin. Nephrol. 2024, 102, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Chadban, S.J.; Ahn, C.; Axelrod, D.A.; Foster, B.J.; Kasiske, B.L.; Kher, V.; Kumar, D.; Oberbauer, R.; Pascual, J.; Pilmore, H.L.; et al. KDIGO Clinical Practice Guideline on the Evaluation and Management of Candidates for Kidney Transplantation. Transplantation 2020, 104, S11–S103. [Google Scholar] [CrossRef] [PubMed]
- Mella, A.; Clari, R.; Deiana, V.; Giraudi, R.; Giovinazzo, G.; Gallo, E.; Dolla, C.; Lavacca, A.; Manzione, A.M.; Fop, F.; et al. Pre-Existing Oncohematological Disease in Kidney Transplant Recipients: Impact on Graft Survival, Acute Rejection, and Long-Term Clinical Outcomes. Front. Immunol. 2025, 16, 1629521. [Google Scholar] [CrossRef]
- Murakami, N.; Webber, A.B.; Nair, V. Transplant Onconephrology in Patients with Kidney Transplants. Adv. Chronic Kidney Dis. 2022, 29, 188–200.e1. [Google Scholar] [CrossRef] [PubMed]
- Kitchlu, A.; McArthur, E.; Amir, E.; Booth, C.M.; Sutradhar, R.; Majeed, H.; Nash, D.M.; Silver, S.A.; Garg, A.X.; Chan, C.T.; et al. Acute Kidney Injury in Patients Receiving Systemic Treatment for Cancer: A Population-Based Cohort Study. JNCI J. Natl. Cancer Inst. 2019, 111, 727–736. [Google Scholar] [CrossRef]
- Sprangers, B. Aetiology and Management of Acute Kidney Injury in Multiple Myeloma. Nephrol. Dial. Transplant. 2018, 33, 722–724. [Google Scholar] [CrossRef]
- Sulu, C.; Yalın, S.F.; Gürer, T.; Ar, M.C.; Altıparmak, M.R. Renal Recovery after Acute Kidney Injury Requiring Urgent Hemodialysis Is not Associated with Improved Survival of Patients with Multiple Myeloma. Ir. J. Med. Sci. 2023, 192, 757–763. [Google Scholar] [CrossRef]
- Huskey, J.L.; Heilman, R.L.; Khamash, H.; Fonseca, R. Kidney Transplant in the Era of Modern Therapy for Multiple Myeloma. Transplantation 2018, 102, 1994–2001. [Google Scholar] [CrossRef]
- Mohyuddin, G.R.; Koehn, K.; Shune, L.; Aziz, M.; Abdallah, A.O.; McClune, B.; Kambhampati, S. Renal insufficiency in multiple myeloma: A systematic review and meta-analysis of all randomized trials from 2005–2019. Leuk. Lymphoma 2021, 62, 1386–1395. [Google Scholar] [CrossRef]
- Wang, L.; Liu, C.; Song, H.; Yuan, J.; Zha, Y.; Deng, Y. Update on kidney injury caused by multiple myeloma. Ann. Hematol. 2024, 103, 5007–5018. [Google Scholar] [CrossRef]
- Dimopoulos, M.A.; Merlini, G.; Bridoux, F.; Leung, N.; Mikhael, J.; Harrison, S.J.; Kastritis, E.; Garderet, L.; Gozzetti, A.; van de Donk, N.W.C.J.; et al. Management of multiple myeloma-related renal impairment: Recommendations from the International Myeloma Working Group. Lancet Oncol. 2023, 24, 293–311. [Google Scholar] [CrossRef]
- Bridoux, F.; Leung, N.; Nasrc, S.H.; Jaccardd, A.; Royale, V. Kidney disease in multiple myeloma. Presse Med. 2025, 54, 104264. [Google Scholar] [CrossRef] [PubMed]
- Ying, W.; Sanders, P.W. Mapping the Binding Domain of Immunoglobulin Light Chains for Tamm-Horsfall Protein. Am. J. Pathol. 2001, 158, 1859–1866. [Google Scholar] [CrossRef] [PubMed]
- Yadav, P.; Sathick, I.J.; Leung, N.; Brown, E.E.; Cook, M.; Sanders, P.W.; Cockwell, P. Serum free light chain level at diagnosis in myeloma cast nephropathy—A multicentre study. Blood Cancer J. 2020, 10, 28. [Google Scholar] [CrossRef]
- Leung, N.; Bridoux, F.; Batuman, V.; Chaidos, A.; Cockwell, P.; D’Agati, V.D.; Dispenzieri, A.; Fervenza, F.C.; Fermand, J.P.; Gibbs, S.; et al. The evaluation of monoclonal gammopathy of renal significance: A consensus report of the International Kidney and Monoclonal Gammopathy Research Group. Nat. Rev. Nephrol. 2019, 15, 45–59, Erratum in Nat. Rev. Nephrol. 2019, 15, 121. [Google Scholar] [CrossRef]
- Chauvet, S.; Fremeaux-Bacchi, V.; Petitprez, F.; Karras, A.; Daniel, L.; Burtey, S.; Choukroun, G.; Delmas, Y.; Guerrot, D.; Francois, A.; et al. Treatment of B-cell disorder improves renal outcome of patients with monoclonal gammopathy–associated C3 glomerulopathy. Blood 2017, 129, 11. [Google Scholar] [CrossRef]
- Ho, P.J.; Moore, E.M.; McQuilten, Z.K.; Wellard, C.; Bergin, K.; Augustson, B.; Blacklock, H.; Harrison, S.J.; Horvath, N.; King, T.; et al. Renal Impairment at Diagnosis in Myeloma: Patient Characteristics, Treatment, and Impact on Outcomes. Results From the Australia and New Zealand Myeloma and Related Diseases Registry. Clin. Lymphoma Myeloma Leuk. 2019, 19, e415–e424. [Google Scholar] [CrossRef]
- Eleutherakis-Papaiakovou, V.; Bamias, A.; Gika, D.; Simeonidis, A.; Pouli, A.; Anagnostopoulos, A.; Michali, E.; Economopoulos, T.; Zervas, K.; Dimopoulos, M.A. Renal failure in multiple myeloma: Incidence, correlations, and prognostic significance. Leuk. Lymphoma 2007, 48, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Knudsen, L.M.; Hippe, E.; Hjorth, M.; Holmberg, E.; Westin, J. Renal function in newly diagnosed multiple myeloma—A demographic study of 1353 patients. Eur. J. Haematol. 1994, 53, 207–212. [Google Scholar] [CrossRef]
- Branco, C.; Silva, M.; Rodrigues, N.; Vieira, J.; Forjaz Lacerda, J.; Lopes, J.A. The Role of High-Risk Cytogenetics in Acute Kidney Injury of Newly Diagnosed Multiple Myeloma: A Cohort Study. Int. J. Mol. Sci. 2025, 26, 6108. [Google Scholar] [CrossRef]
- Chen, X.; Luo, X.; Zu, Y.; Issa, H.A.; Li, L.; Ye, H.; Yang, T.; Hu, J.; Wei, L. Severe renal impairment as an adverse prognostic factor for survival in newly diagnosed multiple myeloma patients. J. Clin. Lab. Anal. 2020, 34, e23416. [Google Scholar] [CrossRef]
- Courant, M.; Orazio, S.; Monnereau, A.; Preterre, J.; Combe, C.; Rigothier, C. Incidence, prognostic impact and clinical outcomes of renal impairment in patients with multiple myeloma: A population-based registry. Nephrol. Dial. Transplant. 2021, 36, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Sana, M.K.; Abdullah, S.M.; Javed, S.; Ehsan, H.; Faizan, U.; Khalid, F.; Jaan, A.; Tayyeb, M.; Abdullah, S.; Anwer, F. Efficacy of Ixazomib and Bortezomib with Lenalidomide Combination Regimens for Multiple Myeloma: A Systematic Review. Blood 2020, 136, 40–41. [Google Scholar] [CrossRef]
- Krejcik, J.; Casneuf, T.; Nijhof, I.S.; Verbist, B.; Bald, J.; Plesner, T.; Syed, K.; Liu, K.; van de Donk, N.W.; Weiss, B.M.; et al. Daratumumab depletes CD38+ immune regulatory cells, promotes T-cell expansion, and skews T-cell repertoire in multiple myeloma. Blood 2016, 128, 384–394. [Google Scholar] [CrossRef]
- Munshi, N.C.; Anderson, L.D., Jr.; Shah, N.; Madduri, D.; Berdeja, J.; Lonial, S.; Raje, N.; Lin, Y.; Siegel, D.; Oriol, A.; et al. Idecabtagene Vicleucel in Relapsed and Refractory Multiple Myeloma. N. Engl. J. Med. 2021, 384, 705–716. [Google Scholar] [CrossRef]
- Kazandjian, D. Multiple myeloma epidemiology and survival: A unique malignancy. Semin. Oncol. 2016, 43, 676–681. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, N.; Costa, C.; Branco, C.; Martins, C.; Lopes, J.A. Acute kidney injury in multiple myeloma patients undergoing autologous hematopoietic stem cell transplant: A cohort study. J. Nephrol. 2024, 37, 419–428. [Google Scholar] [CrossRef]
- Rodrigues, N.; Branco, C.; Sousa, G.; Silva, M.; Costa, C.; Marques, F.; Vasconcelos, P.; Martins, C.; Lopes, J.A. Risk Factors and Long-Term Outcomes of Acute Kidney Disease in Hematopoietic Stem Cell Transplant—Cohort Study. Cancers 2025, 17, 538. [Google Scholar] [CrossRef]
- Ng, J.H.; Izard, S.; Murakami, N.; Jhaveri, K.D.; Sharma, A.; Nair, V. Outcomes of kidney transplantation in patients with myeloma and amyloidosis in the USA. Nephrol. Dial. Transplant. 2022, 37, 2569–2580. [Google Scholar] [CrossRef]
- Tsakiris, D.J.; Stel, V.S.; Finne, P.; Fraser, E.; Heaf, J.; de Meester, J.; Schmaldienst, S.; Dekker, F.; Verrina, E.; Jager, K.J. Incidence and outcome of patients starting renal replacement therapy for end-stage renal disease due to multiple myeloma or light-chain deposit disease: An ERA-EDTA Registry study. Nephrol. Dial. Transplant. 2010, 25, 1200–1206. [Google Scholar] [CrossRef]
- Heybeli, C.; Bentall, A.J.; Alexander, M.P.; Amer, H.; Buadi, F.K.; Dispenzieri, A.; Dingli, D.; Gertz, M.A.; Issa, N.; Kapoor, P. Kidney Transplant Outcomes of Patients with Multiple Myeloma. Kidney Int. Rep. 2022, 7, 752–762. [Google Scholar] [CrossRef]
- Penn, I. Evaluation of transplant candidates with pre-existing malignancies. Ann. Transplant. 1997, 2, 14–17. [Google Scholar] [PubMed]
- Leung, N.; Lager, D.J.; Gertz, M.A.; Wilson, K.; Kanakiriya, S.; Fervenza, F.C. Long-term outcome of renal transplantation in light-chain deposition disease. Am. J. Kidney Dis. 2004, 43, 147–153. [Google Scholar] [CrossRef]
- Kormann, R.; Pouteil-Noble, C.; Muller, C.; Arnulf, B.; Viglietti, D.; Sberro, R.; Sayegh, J.; Durrbach, A.; Dantal, J.; Girerd, S.; et al. Kidney transplantation for active multiple myeloma or smoldering myeloma: A case-control study. Clin. Kidney J. 2019, 14, 156–166. [Google Scholar] [CrossRef]
- Sayed, R.H.; Wechalekar, A.D.; Gilbertson, J.A.; Bass, P.; Mahmood, S.; Sachchithanantham, S.; Fontana, M.; Patel, K.; Whelan, C.J.; Lachmann, H.J. Natural history and outcome of light chain deposition disease. Blood 2015, 126, 2805–2810. [Google Scholar] [CrossRef] [PubMed]
- Kourelis, T.V.; Nasr, S.H.; Dispenzieri, A.; Kumar, S.K.; Gertz, M.A.; Fervenza, F.C.; Buadi, F.K.; Lacy, M.Q.; Erickson, S.B.; Cosio, F.G.; et al. Outcomes of patients with renal monoclonal immunoglobulin deposition disease. Am. J. Hematol. 2016, 91, 1123–1128. [Google Scholar] [CrossRef]
- Molina-Andújar, A.; Tovar, N.; Cuadrado, E.; Castrejón de Anta, N.; Revuelta, I.; Cucchiari, D.; Cofan, F.; Esforzado, N.; Cibeira, M.T.; Rosiñol, L.; et al. Kidney Transplantation in Monoclonal Immunoglobulin Deposition Disease: A Report of 6 Cases. Am. J. Kidney Dis. 2021, 78, 755–759. [Google Scholar] [CrossRef]
- Havasi, A.; Heybeli, C.; Leung, N.; Angel-Korman, A.; Sanchorawala, V.; Cohen, O.; Wechalekar, A.; Bridoux, F.; Jaffer, I.; Gutgarts, V.; et al. Outcomes of renal transplantation in patients with AL amyloidosis: An international collaboration through The International Kidney and Monoclonal Gammopathy Research Group. Blood Cancer J. 2022, 12, 119. [Google Scholar] [CrossRef]
- Sethi, J.; Sulaiman, S.; Ramachandran, R.; Prakash, G.; Kanwar, D.; Nada, R.; Rathi, M.; Kohli, H.S. Bortezomib-based Chemotherapy and Bone-marrow Followed by Renal Transplantation in Multiple Myeloma: A Literature Review. Indian J. Transplant. 2025, 19, 150–156. [Google Scholar] [CrossRef]
- Baraldi, O.; Grandinetti, V.; Donati, G.; Comai, G.; Battaglino, G.; Cuna, V.; Capelli, I.; Sala, E.; La Manna, G. Hematopoietic Cell and Renal Transplantation in Plasma Cell Dyscrasia Patients. Cell Transplant. 2016, 25, 995–1005. [Google Scholar] [CrossRef] [PubMed]
- Humphrey, R.L.; Wright, J.R.; Zachary, J.B.; Sterioff, S.; DeFronzo, R.A. Renal transplantation in multiple myeloma. A case report. Ann. Intern. Med. 1975, 83, 651–653. [Google Scholar] [CrossRef]
- Hanamura, I. Multiple myeloma with high-risk cytogenetics and its treatment approach. Int. J. Hematol. 2022, 115, 762–777. [Google Scholar] [CrossRef]
- Rajkumar, S.V.; Harousseau, J.-L.; Durie, B.G.M.; Anderson, K.C.; Dimopoulos, M.A.; Kyle, R.A.; Blade, J.; Richardson, P.G.; Orlowski, R.Z.; Siegel, D.S.; et al. Consensus recommendations for the uniform reporting of clinical trials: International Myeloma Working Group consensus statement. Blood 2011, 117, 4691–4695. [Google Scholar] [CrossRef]
- Paiva, B.; Puig, N.; Cedena, M.-T.; Martínez-López, J.; Cordon, L.; Vidriales, M.-B.; Flores-Montero, J.; Gutierrez, N.C.; Martín-Ramos, M.L.; Oriol, A.; et al. Measurable residual disease by flow cytometry in multiple myeloma: A consensus approach from the European Myeloma Network. Leukemia 2017, 31, 555–564. [Google Scholar] [CrossRef]
- Oken, M.M.; Creech, R.H.; Tormey, D.C.; Horton, J.; Davis, T.E.; McFadden, E.T.; Carbone, P.P. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 1982, 5, 649–655. [Google Scholar] [CrossRef]
- Knoll, G.; Cockfield, S.; Blydt-Hansen, T.; Baran, D.; Kiberd, B.; Landsberg, D.; Rush, D.; Cole, E. Kidney Transplant Working Group of the Canadian Society of Transplantation. Canadian Society of Transplantation consensus guidelines on eligibility for kidney transplantation. Can. Med. Assoc. J. 2005, 173, 1181–1184. [Google Scholar] [CrossRef]
- Van den Bosch, I.; Sprangers, B.; Gertz, M. Multiple myeloma and kidney transplantation: The beginning of a new era. Clin. Kidney J. 2019, 12, 213–215. [Google Scholar] [CrossRef]
- Wang, Y.; Hemmelder, M.H.; Bos, W.J.W.; Snoep, J.D.; de Vries, A.P.J.; Dekker, F.W.; Meuleman, Y. Mapping health-related quality of life after kidney transplantation by group comparisons: A systematic review. Nephrol. Dial. Transplant. 2021, 36, 2327–2339. [Google Scholar] [CrossRef] [PubMed]
- Vardell, V.A.; Horns, J.J.; Daud, A.A.; Sborov, D.W. Cardiovascular Events in Multiple Myeloma: A Retrospective Review of the SEER-Medicare Claims Database. Blood 2024, 144, 6942. [Google Scholar] [CrossRef]
- Plummer, C.; Driessen, C.; Szabo, Z.; Mateos, M.V. Management of cardiovascular risk in patients with multiple myeloma. Blood Cancer J. 2019, 9, 26. [Google Scholar] [CrossRef] [PubMed]
- Issa, Z.A.; Zantout, M.S.; Azar, S.T. Multiple myeloma and diabetes. ISRN Endocrinol. 2011, 1, 815013. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Palumbo, A.; Bringhen, S.; Mateos, M.V.; Larocca, A.; Facon, T.; Kumar, S.K.; Offidani, M.; McCarthy, P.; Evangelista, A.; Lonial, S.; et al. Geriatric assessment predicts survival and toxicities in elderly myeloma patients: An International Myeloma Working Group report. Blood 2015, 125, 2068–2074, Erratum in Blood 2016, 127, 1213; Erratum in Blood 2016, 128, 1020. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Poh, C.; Keegan, T.; Rosenberg, A.S. Second primary malignancies in multiple myeloma: A review. Blood Rev. 2021, 46, 100757. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maldonado, J.R. Why It is Important to Consider Social Support When Assessing Organ Transplant Candidates? Am. J. Bioeth. 2019, 19, 1–8. [Google Scholar] [CrossRef]
- Shah, S.; Ibrahim, M.; Delaney, M.; Schey, S.; Bygrave, C.; Streetly, M.; Benjamin, R. Risk of Relapse of Multiple Myeloma Following Kidney Transplantation. Clin. Kidney J. 2019, 12, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Geraldes, C.; Roque, A.; Sarmento-Ribeiro, A.B.; Neves, M.; Ionita, A.; Gerivaz, R.; Tomé, A.; Afonso, S.; Silveira, M.P.; Sousa, P.; et al. Practical Management of Disease-Related Manifestations and Drug Toxicities in Patients with Multiple Myeloma. Front. Oncol. 2024, 14, 1282300. [Google Scholar] [CrossRef]
- Caro, J.; Braunstein, M.; Williams, L.; Bruno, B.; Kaminetzky, D.; Siegel, A.; Razzo, B.; Alfandari, S.; Morgan, G.J.; Davies, F.E.; et al. Inflammation and Infection in Plasma Cell Disorders: How Pathogens Shape the Fate of Patients. Leukemia 2022, 36, 613–624. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.; Sinha, P.; Harrison, S.J.; Quach, H.; Slavin, M.A.; Teh, B.W. Epidemiology and Risks of Infections in Patients with Multiple Myeloma Managed with New Generation Therapies. Clin. Lymphoma Myeloma Leuk. 2021, 21, 444–450.e3. [Google Scholar] [CrossRef] [PubMed]
- Tete, S.M.; Bijl, M.; Sahota, S.S.; Bos, N.A. Immune Defects in the Risk of Infection and Response to Vaccination in Monoclonal Gammopathy of Undetermined Significance and Multiple Myeloma. Front. Immunol. 2014, 5, 257. [Google Scholar] [CrossRef]
- Parrondo, R.D.; Reljic, T.; Iqbal, M.; Ayala, E.; Kharfan-Dabaja, M.A.; Kumar, A.; Murthy, H.S. Efficacy of Proteasome Inhibitor-based Maintenance Following Autologous Transplantation in Multiple Myeloma: A Systematic Review and Meta-analysis. Eur. J. Haematol. 2021, 106, 40–48. [Google Scholar] [CrossRef]
- Han, X.; Jin, C.; Zheng, G.; He, D.; Zhao, Y.; Li, Y.; Wu, W.; Zheng, W.; Wei, G.; Zhang, E.; et al. Different Patient Subgroup Different Maintenance, Proteasome Inhibitors or Immunomodulators Maintenance for Newly Diagnosed Multiple Myeloma: A 7-Year Single-Center Data in China. Front. Oncol. 2021, 11, 665217, Erratum in Front. Oncol. 2021, 11, 740715. [Google Scholar] [CrossRef]
- Szita, V.R.; Mikala, G.; Kozma, A.; Fábián, J.; Hardi, A.; Alizadeh, H.; Rajnics, P.; Rejtő, L.; Szendrei, T.; Váróczy, L.; et al. Targeted Venetoclax Therapy in t(11;14) Multiple Myeloma: Real World Data From Seven Hungarian Centers. Pathol. Oncol. Res. 2022, 28, 1610276. [Google Scholar] [CrossRef]
- Chitty, D.W.; Hartley-Brown, M.A.; Abate, M.; Thakur, R.; Wanchoo, R.; Jhaveri, K.D.; Nair, V. Kidney Transplantation in Patients with Multiple Myeloma: Narrative Analysis and Review of the Last Two Decades. Nephrol. Dial. Transplant. 2022, 37, 1616–1626. [Google Scholar] [CrossRef]
- Teh, B.W.; Reynolds, G.; Slavin, M.A.; Cooley, L.; Roberts, M.; Liu, E.; Thursky, K.; Talaulikar, D.; Mollee, P.; Szabo, F.; et al. Executive Summary of Consensus Clinical Practice Guidelines for the Prevention of Infection in Patients with Multiple Myeloma. Intern. Med. J. 2023, 53, 1469–1477. [Google Scholar] [CrossRef] [PubMed]
- Alhuraiji, A.; Al Farsi, K.; Mheidly, K.; Elsabah, H.; Cherif, H.; Hamad, A.; Marashi, M.; Al Hateeti, H.; Osman, H.; Mohty, M. Relapsed/Refractory Multiple Myeloma: Standard of Care Management of Patients in the Gulf Region. Clin. Hematol. Int. 2025, 7, 20–33. [Google Scholar] [CrossRef] [PubMed]
- Sonneveld, P. Management of Multiple Myeloma in the Relapsed/Refractory Patient. Hematology 2017, 2017, 508–517. [Google Scholar] [CrossRef] [PubMed]

| Reference | Number of Patients | Renal Lesion | Pre-Transplant Treatment (Chemo/Autologous HSCT) | Main Outcomes |
|---|---|---|---|---|
| Humphrey 1975 (Pre-bortezomib) [41] | 1 | LCCN | Chemotherapy | Patient died from infection at 3 months; graft outcome not specified |
| Penn 1997 (Pre-bortezomib) [32] | 12 | MM (various) | Various | 8/12 relapsed (67%); poor overall patient survival (most died within a few years); graft survival variably reported |
| Leung 2004 (Pre-bortezomib) [33] | 7 | LCDD | Melphalan + prednisone (3 patients) | Median graft survival 11 months; 5/7 relapsed; 4 patients died; 1 patient alive with functioning graft at 13 years |
| Tsakiris 2010 (Pre-bortezomib) [30] | 35 (from 2453 RRT) | MM/LDD | Not specified (1986–2005) | Mean overall patient survival 9.6 years (vs 19.6 years in non-MM); graft survival not reported |
| Huskey 2018 (Modern era) [8] | 4 | MM | Bortezomib, Lenalidomide, thalidomide, dexamethasone; 2 autologous HSCT | Follow-up 46 months; 1 death at 5.5 years (patient survival); 1 acute rejection at 10 months (graft loss); 1 hematological relapse at 8 months without renal relapse; 1 stable |
| Kormann 2019 (Modern era) [34] | 13 (vs. 65 controls) | MM/SMM, LCDD, AL amyloidosis | Chemotherapy ± autologous HSCT | Median patient survival 117 months; median graft survival 80 months; no significant difference vs. controls; higher infection rates |
| Heybeli 2022 (Modern era) [31] | 11 (12 kidney transplants) | MM | Bortezomib-based ± lenalidomide; 8 CR, 2 VGPR, 2 PR | 5-year graft survival 66%; 5-year progression-free survival 44%; 5-year overall patient survival 61%; 75% hematological relapse; 25% graft failure |
| Ng 2022 (Modern era) [29] | National United States cohort | MM and amyloidosis | Registry data | Overall patient survival worse in plasma cell dyscrasias vs. non-PCD; outcomes worse in amyloidosis; MM survival closer to controls |
| Sethi 2025 (Modern era) [39] | 18 | MM post-Autologous HSCT | Autologous HSCT + bortezomib-based chemotherapy | Median interval HSCT to transplant: 29.5 mo; pre-transplant 5 VGPR, 6 CR, 5 sCR; relapse rate 27.7%; rejection 16.6%; graft loss 16.6%; 5-year overall patient survival 50% |
| Reference | Number of Patients | Renal Lesion | Pre-Transplant Treatment (Chemo/Autologous HSCT) | Main Outcomes |
|---|---|---|---|---|
| Leung 2004 (Pre-bortezomib) [33] | 7 | LCDD | Melphalan + prednisone (3 patients) | Median follow up 33.3 months; 5/7 relapse; mean graft loss 11 months; 4 deaths; 1 alive 13 years |
| Sayed 2015 (Modern era) [35] | 7 | LCDD | 4 chemotherapy/Autologous HSCT; 3 none | 3 graft losses (2 relapse at 1.6 and 1.9 yrs, 1 rejection); 4 functioning grafts (eGFR > 40 mL/min) |
| Kourelis 2016 (Modern era) [36] | 9 | LCDD | Chemotherapy ± bortezomib | 3 graft recurrences (2–9 yrs); 1 bortezomib + CR relapsed at 9 years; others without hematological response relapsed earlier |
| Molina-Andújar 2021 (Modern era) [37] | 6 | LCDD | Bortezomib + melphalan + Autologous HSCT | All CR pre-transplant; follow up 20.5 months; 1 hematological relapse; 2 disease progressions (1 graft loss); 5 patients alive with functioning grafts |
| Category | Green (Eligible/Favorable) | Yellow (Conditional/Caution) | Red (Contraindicated/Unfavorable) |
|---|---|---|---|
| Hematological Response | Complete response (CR) or very good partial response (VGPR) with MRD negativity; standard-risk cytogenetics | VGPR with MRD positivity high-risk cytogenetics but in sustained remission | Active disease high-risk with persistent MRD positivity |
| Timing | ≥6 months post-HSCT with stable remission (standard risk, MRD-negative) | 12 months post-HSCT for high-risk or MRD-positive patients | <6 months from therapy Relapsed/refractory disease |
| Performance Status | ECOG 0–2 or KPS ≥ 70% | ECOG 2–3 with potentially reversible frailty/comorbidities | ECOG ≥ 3 Severe, irreversible frailty |
| Comorbidities | Controlled cardiovascular disease Well-managed diabetes No active infections or cancer | Controlled but significant comorbidities (e.g., stable ischemic heart disease, mild frailty) | Severe cardiovascular disease Uncontrolled diabetes Active infection/other cancers |
| Psychosocial factors | Strong social support Demonstrated adherence to therapy and follow-up | Limited support systems but improving with intervention | Active substance abuse Major untreated psychiatric illness |
| Patient preferences | Fully informed and motivated; engaged in shared decision-making | Uncertain adherence or ambivalence | Refusal of therapy Inability to comply with follow-up |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodrigues, N.; Silva, M.; Branco, C.; Barreto, S.; Pais, T.; Lopes, J.A. Kidney Transplantation in Patients with Multiple Myeloma: Current Evidence, Challenges, and Future Directions. Int. J. Mol. Sci. 2025, 26, 9358. https://doi.org/10.3390/ijms26199358
Rodrigues N, Silva M, Branco C, Barreto S, Pais T, Lopes JA. Kidney Transplantation in Patients with Multiple Myeloma: Current Evidence, Challenges, and Future Directions. International Journal of Molecular Sciences. 2025; 26(19):9358. https://doi.org/10.3390/ijms26199358
Chicago/Turabian StyleRodrigues, Natacha, Manuel Silva, Carolina Branco, Sofia Barreto, Telma Pais, and José António Lopes. 2025. "Kidney Transplantation in Patients with Multiple Myeloma: Current Evidence, Challenges, and Future Directions" International Journal of Molecular Sciences 26, no. 19: 9358. https://doi.org/10.3390/ijms26199358
APA StyleRodrigues, N., Silva, M., Branco, C., Barreto, S., Pais, T., & Lopes, J. A. (2025). Kidney Transplantation in Patients with Multiple Myeloma: Current Evidence, Challenges, and Future Directions. International Journal of Molecular Sciences, 26(19), 9358. https://doi.org/10.3390/ijms26199358







