Gulf War Illness, Fibromyalgia, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Long COVID Overlap in Common Symptoms and Underlying Biological Mechanisms: Implications for Future Therapeutic Strategies
Abstract
1. Introduction
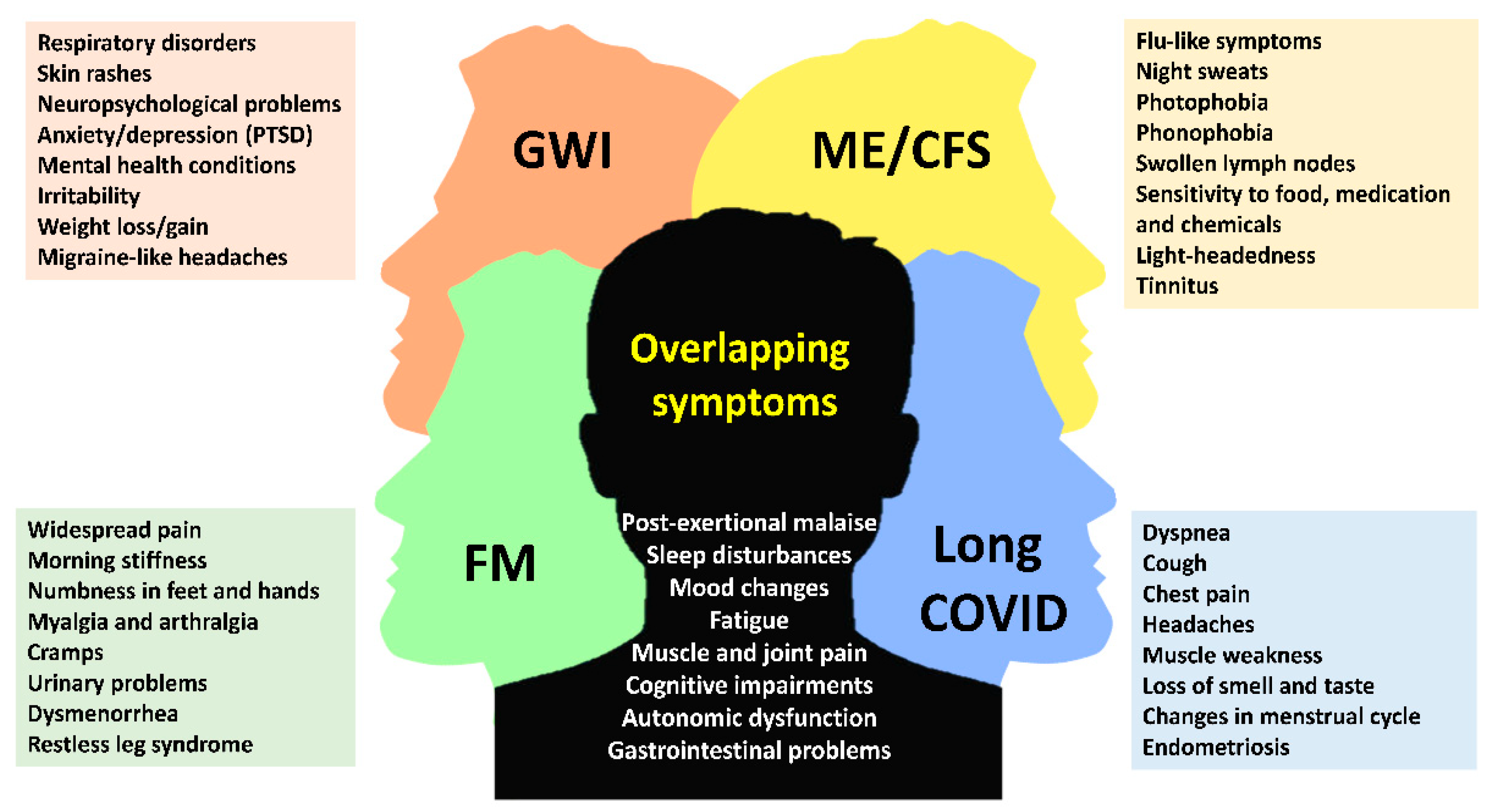
2. Common Symptoms in Low-Energy Associated Disorders
2.1. Fatigue and Post-Exertional Malaise
2.2. Autonomic Dysfunction
2.3. Cognitive Impairment
2.4. Unrefreshing Sleep
2.5. Muscle and Joint Pain
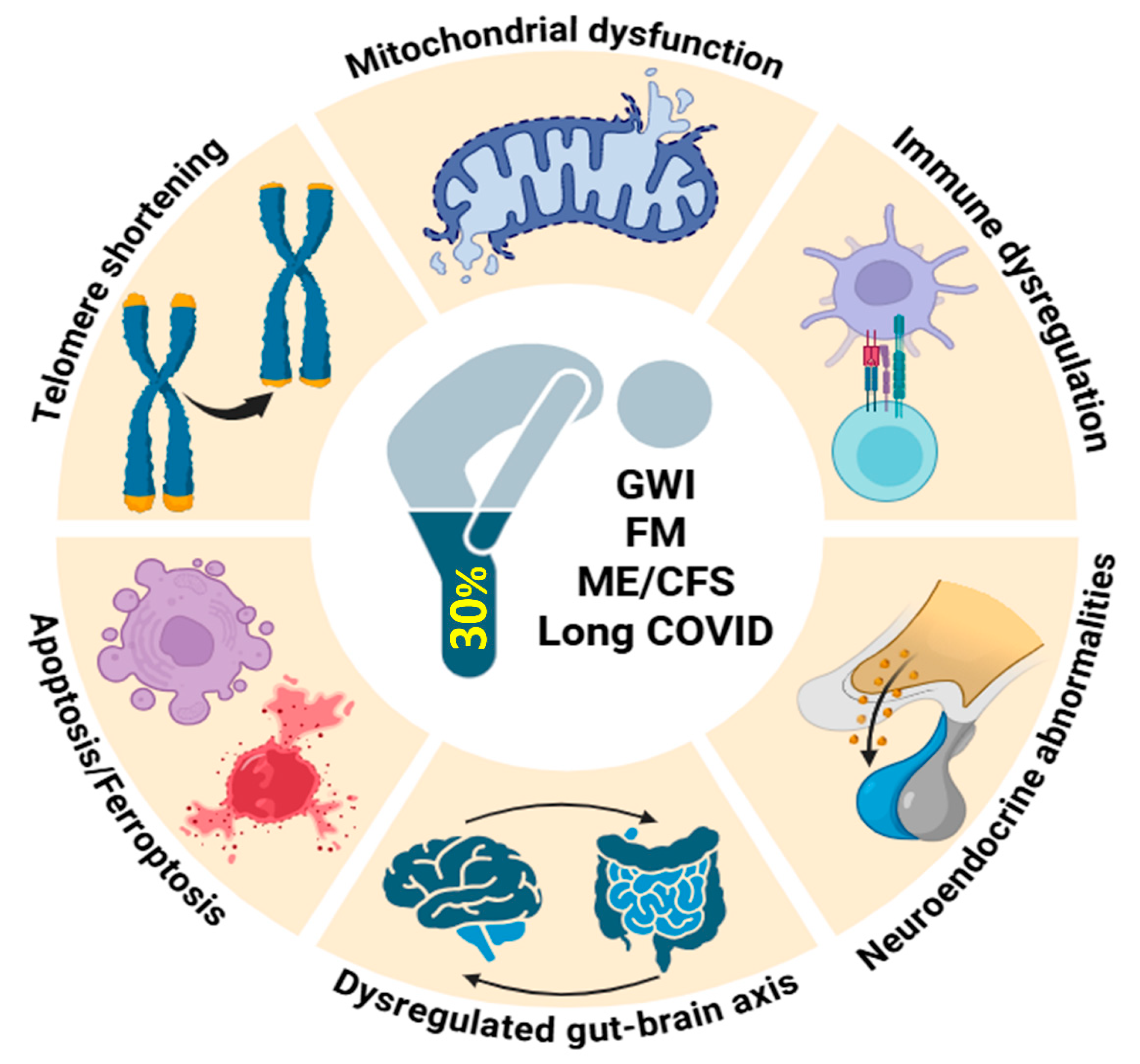
3. Understanding the Biological Mechanisms Shared Between These Disorders
3.1. Mitochondrial Dysfunction, Oxidative Stress and Inflammation
3.2. Immune Dysregulation
3.3. Neuroendocrine Abnormalities
3.4. Dysregulated Gut–Brain Axis
3.5. Apoptosis and Ferroptosis
3.6. Telomere Shortening
4. Implications for Current and Promising Therapeutic Strategies
4.1. Current Therapeutic Approaches
4.2. Stem Cell Therapy
4.3. Coenzyme Q10 Supplementation
5. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANS | Autonomic nervous system |
| ATP | Adenosine triphosphate |
| BMSC | Bone marrow-derived mesenchymal stem cells |
| CBT-I | Cognitive behavior therapy-insomnia |
| CDC | Centers for Disease Control and Prevention |
| CoQ10 | Coenzyme Q10 |
| ENS | Enteric nervous system |
| FM | Fibromyalgia |
| FDA | Food and Drug Administration |
| FTH1 | Ferritin heavy chain 1 |
| GET | Graded exercise therapy |
| GPX4 | Glutathione peroxidase 4 |
| GWI | Gulf War Illness |
| HRV | Heart rate variability |
| HPA | Hypothalamic–pituitary–adrenal axis |
| HO-1 | Heme-oxygenase-1 |
| IBS | Irritable bowel syndrome |
| IL | Interleukin |
| MAOI | Monoamine oxidase inhibitors |
| ME/CFS | Myalgic encephalomyelitis/chronic fatigue syndrome |
| MPP+ | 1-methyl-4-phenylpyridinium |
| NADH | Nicotinamide adenine dinucleotide |
| NK | Natural killer cells |
| PEM | Post-exertional malaise |
| PESE | Post-exertional symptom exacerbation |
| PI3K | Phosphatidylinositol-3-kinase |
| POTS | Postural orthostatic tachycardia syndrome |
| iPSC | Induced-pluripotent stem cells |
| RCT | Randomized controlled trial |
| ROS | Reactive oxygen species |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| SLC7A11 | Solute carrier family 7 member 11 |
| SSRI | Selective serotonin reuptake inhibitors |
| TRPV1 | Transient receptor potential vanilloid 1 |
| TRPM2 | Transient receptor potential melastatin 2 |
| TRF1 | Telomeric repeat-binding factor 1 |
| TRF2 | Telomeric repeat-binding factor 2 |
References
- Queiroz, L.P. Worldwide epidemiology of fibromyalgia. Curr. Pain Headache Rep. 2013, 17, 356. [Google Scholar] [CrossRef]
- Lim, E.J.; Ahn, Y.C.; Jang, E.S.; Lee, S.W.; Lee, S.H.; Son, C.G. Systematic review and meta-analysis of the prevalence of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). J. Transl. Med. 2020, 18, 100. [Google Scholar] [CrossRef]
- Dehlia, A.; Guthridge, M.A. The persistence of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) after SARS-CoV-2 infection: A systematic review and meta-analysis. J. Infect. 2024, 89, 106297. [Google Scholar] [CrossRef]
- Bast, E.; Jester, D.J.; Palacio, A.; Krengel, M.; Reinhard, M.; Ashford, J.W. Gulf War Illness: A Historical Review and Considerations of a Post-Viral Syndrome. Mil. Med. 2025, usaf092. [Google Scholar] [CrossRef]
- Annesley, S.J.; Missailidis, D.; Heng, B.; Josev, E.K.; Armstrong, C.W. Unravelling shared mechanisms: Insights from recent ME/CFS research to illuminate long COVID pathologies. Trends Mol. Med. 2024, 30, 443–458. [Google Scholar] [CrossRef]
- Goldenberg, D.L. The pivotal role of central sensitization in long COVID, fibromyalgia and myalgic encephalomyelitis/chronic fatigue syndrome. Expert Rev. Neurother. 2025, 25, 973–989. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, K.; Nisenbaum, R.; Stewart, G.; Thompson, W.W.; Robin, L.; Washko, R.M.; Noah, D.L.; Barrett, D.H.; Randall, B.; Herwaldt, B.L.; et al. Chronic multisymptom illness affecting Air Force veterans of the Gulf War. Jama 1998, 280, 981–988. [Google Scholar] [CrossRef] [PubMed]
- Steele, L. Prevalence and patterns of Gulf War illness in Kansas veterans: Association of symptoms with characteristics of person, place, and time of military service. Am. J. Epidemiol. 2000, 152, 992–1002. [Google Scholar] [CrossRef] [PubMed]
- Clauw, D.J.; D’Arcy, Y.; Gebke, K.; Semel, D.; Pauer, L.; Jones, K.D. Normalizing fibromyalgia as a chronic illness. Postgrad. Med. 2018, 130, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.P. A Historical Review of Chronic Fatigue Syndrome. J. Humanit. Soc. Sci. 2018, 23, 23–28. [Google Scholar]
- Komaroff, A.L.; Lipkin, W.I. ME/CFS and Long COVID share similar symptoms and biological abnormalities: Road map to the literature. Front. Med. 2023, 10, 1187163. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, D.L. How to understand the overlap of long COVID, chronic fatigue syndrome/myalgic encephalomyelitis, fibromyalgia and irritable bowel syndromes. Semin. Arthritis Rheum. 2024, 67, 152455. [Google Scholar] [CrossRef] [PubMed]
- Khakban, I.; Jain, S.; Gallab, J.; Dharmaraj, B.; Zhou, F.; Lokker, C.; Abdelkader, W.; Zeraatkar, D.; Busse, J.W. Impact of the COVID-19 Pandemic and the 2021 National Institute for Health and Care Excellence Guidelines on Public Perspectives Toward Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Thematic and Sentiment Analysis on Twitter (Rebranded as X). J. Med. Internet Res. 2025, 27, e65087. [Google Scholar] [CrossRef]
- Davis, L.; Higgs, M.; Snaith, A.; Lodge, T.A.; Strong, J.; Espejo-Oltra, J.A.; Kujawski, S.; Zalewski, P.; Pretorius, E.; Hoerger, M.; et al. Dysregulation of lipid metabolism, energy production, and oxidative stress in myalgic encephalomyelitis/chronic fatigue syndrome, Gulf War Syndrome and fibromyalgia. Front. Neurosci. 2025, 19, 1498981. [Google Scholar] [CrossRef]
- Mantle, D.; Hargreaves, I.P.; Domingo, J.C.; Castro-Marrero, J. Mitochondrial Dysfunction and Coenzyme Q10 Supplementation in Post-Viral Fatigue Syndrome: An Overview. Int. J. Mol. Sci. 2024, 25, 574. [Google Scholar] [CrossRef]
- James, L.M.; Georgopoulos, A.P. At the Root of 3 “Long” Diseases: Persistent Antigens Inflicting Chronic Damage on the Brain and Other Organs in Gulf War Illness, Long-COVID-19, and Chronic Fatigue Syndrome. Neurosci. Insights 2022, 17, 26331055221114817. [Google Scholar] [CrossRef]
- León-Moreno, L.C.; Reza-Zaldívar, E.E.; Hernández-Sapiéns, M.A.; Villafaña-Estarrón, E.; García-Martin, M.; Ojeda-Hernández, D.D.; Matias-Guiu, J.A.; Gomez-Pinedo, U.; Matias-Guiu, J.; Canales-Aguirre, A.A. Mesenchymal Stem Cell-Based Therapies in the Post-Acute Neurological COVID Syndrome: Current Landscape and Opportunities. Biomolecules 2023, 14, 8. [Google Scholar] [CrossRef]
- Padda, J.; Khalid, K.; Zubair, U.; Al Hennawi, H.; Yadav, J.; Almanie, A.H.; Mehta, K.A.; Tasnim, F.; Cooper, A.C.; Jean-Charles, G. Stem Cell Therapy and Its Significance in Pain Management. Cureus 2021, 13, e17258. [Google Scholar] [CrossRef]
- Tsilibary, E.C.; Carlson, D.; Georgopoulos, A.P. Protective Effect of Stem Cells from Toxicity Induced by Gulf War Illness (GWI) Serum in N2A Neuroblastoma Cells. J. Neurol. Neuromedicine 2021, 6, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Hodges, L. Repeated Cardiopulmonary Exercise Testing of ME/CFS Patients. Methods Mol. Biol. 2025, 2920, 163–172. [Google Scholar] [CrossRef]
- Risbano, M.G. From fatigue to physiology: Submaximal 2-day cardiopulmonary exercise test and emerging standards in long COVID. Exp. Physiol. 2025. [Google Scholar] [CrossRef]
- Frank, J.; Tehrani, L.; Gamer, J.; Van Booven, D.J.; Ballarin, S.; Rossman, R.; Edelstein, A.; Uppalati, S.; Reuthebuck, A.; Collado, F.; et al. Gulf War Illness Induced Sex-Specific Transcriptional Differences Under Stressful Conditions. Int. J. Mol. Sci. 2025, 26, 3610. [Google Scholar] [CrossRef]
- Vink, M.; Partyka-Vink, K. The PACE Trial’s GET Manual for Therapists Exposes the Fixed Incremental Nature of Graded Exercise Therapy for ME/CFS. Life 2025, 15, 584. [Google Scholar] [CrossRef]
- Boruch, A.; Branchaw, G.; O’Connor, P.J.; Cook, D.B. Physical Activity and Fatigue Symptoms: Neurotypical Adults and People with Chronic Multisymptom Illnesses. Curr. Top. Behav. Neurosci. 2024, 67, 281–308. [Google Scholar] [CrossRef]
- Di Bari, A.; Demo, G.; Patron, E. Unravelling the relationship between anxiety, autonomic nervous system dysfunction and fibromyalgia: A systematic review. Clin. Exp. Rheumatol. 2025, 43, 1136–1145. [Google Scholar] [CrossRef]
- Escorihuela, R.M.; Capdevila, L.; Castro, J.R.; Zaragozà, M.C.; Maurel, S.; Alegre, J.; Castro-Marrero, J. Reduced heart rate variability predicts fatigue severity in individuals with chronic fatigue syndrome/myalgic encephalomyelitis. J. Transl. Med. 2020, 18, 4. [Google Scholar] [CrossRef]
- Avery, T.J.; Mathersul, D.C.; Schulz-Heik, R.J.; Mahoney, L.; Bayley, P.J. Self-Reported Autonomic Dysregulation in Gulf War Illness. Mil. Med. 2023, 188, e1462–e1467. [Google Scholar] [CrossRef]
- Garner, R.S.; Rayhan, R.U.; Baraniuk, J.N. Verification of exercise-induced transient postural tachycardia phenotype in Gulf War Illness. Am. J. Transl. Res. 2018, 10, 3254–3264. [Google Scholar] [PubMed]
- Verne, Z.T.; Fields, J.Z.; Zhang, B.B.; Zhou, Q. Autonomic dysfunction and gastroparesis in Gulf War veterans. J. Investig. Med. 2023, 71, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Kemp, J.; Sunnquist, M.; Jason, L.A.; Newton, J.L. Autonomic dysfunction in myalgic encephalomyelitis and chronic fatigue syndrome: Comparing self-report and objective measures. Clin. Auton. Res. 2019, 29, 475–477. [Google Scholar] [CrossRef] [PubMed]
- Ziaja, C.P.; Young, S.; Stark, M. Dysregulation of the autonomic nervous system in ME/CFS and post-COVID syndrome: Insights from 48-h heart rate variability monitoring. J. Neurol. Sci. 2023, 455, 121241. [Google Scholar] [CrossRef]
- El-Sawy, N.; El-Tantawi, G.; Achmawi, G.A.H.; Sultan, H.; Younis, S. Autonomic changes in fibromyalgia: Clinical and electrophysiological study. Alexandria J. Med. 2012, 48, 215–222. [Google Scholar] [CrossRef][Green Version]
- Kingsley, J.D. Autonomic dysfunction in women with fibromyalgia. Arthritis Res. Ther. 2012, 14, 103. [Google Scholar] [CrossRef]
- Staud, R. Autonomic dysfunction in fibromyalgia syndrome: Postural orthostatic tachycardia. Curr. Rheumatol. Rep. 2008, 10, 463–466. [Google Scholar] [CrossRef]
- Dani, M.; Dirksen, A.; Taraborrelli, P.; Torocastro, M.; Panagopoulos, D.; Sutton, R.; Lim, P.B. Autonomic dysfunction in ‘long COVID’: Rationale, physiology and management strategies. Clin. Med. 2021, 21, e63–e67. [Google Scholar] [CrossRef] [PubMed]
- Fedorowski, A.; Sutton, R. Autonomic dysfunction and postural orthostatic tachycardia syndrome in post-acute COVID-19 syndrome. Nat. Rev. Cardiol. 2023, 20, 281–282. [Google Scholar] [CrossRef]
- Giunta, S.; Giordani, C.; De Luca, M.; Olivieri, F. Long-COVID-19 autonomic dysfunction: An integrated view in the framework of inflammaging. Mech. Ageing Dev. 2024, 218, 111915. [Google Scholar] [CrossRef] [PubMed]
- Domingo, J.C.; Battistini, F.; Cordobilla, B.; Zaragoza, M.C.; Sanmartin-Sentanes, R.; Alegre-Martin, J.; Cambras, T.; Castro-Marrero, J. Association of circulating biomarkers with illness severity measures differentiates myalgic encephalomyelitis/chronic fatigue syndrome and post-COVID-19 condition: A prospective pilot cohort study. J. Transl. Med. 2024, 22, 343. [Google Scholar] [CrossRef] [PubMed]
- Golomb, B.A. Oxidative Stress and Mitochondrial Injury in Chronic Multisymptom Conditions: From Gulf War Illness to Autism Spectrum Disorder. Nat. Prec. 2012. [Google Scholar] [CrossRef]
- Alshelh, Z.; Albrecht, D.S.; Bergan, C.; Akeju, O.; Clauw, D.J.; Conboy, L.; Edwards, R.R.; Kim, M.; Lee, Y.C.; Protsenko, E.; et al. In-vivo imaging of neuroinflammation in veterans with Gulf War illness. Brain Behav. Immun. 2020, 87, 498–507. [Google Scholar] [CrossRef]
- Butterick, T.A.; Trembley, J.H.; Hocum Stone, L.L.; Muller, C.J.; Rudquist, R.R.; Bach, R.R. Gulf War Illness-associated increases in blood levels of interleukin 6 and C-reactive protein: Biomarker evidence of inflammation. BMC Res. Notes 2019, 12, 816. [Google Scholar] [CrossRef]
- Chao, L.L.; Sullivan, K.; Krengel, M.H.; Killiany, R.J.; Steele, L.; Klimas, N.G.; Koo, B.B. The prevalence of mild cognitive impairment in Gulf War veterans: A follow-up study. Front. Neurosci. 2023, 17, 1301066. [Google Scholar] [CrossRef]
- Cheng, C.H.; Alshelh, Z.; Guan, Y.; Sullivan, K.; Loggia, M.L.; Koo, B.B. Association of the tissue microstructural diffusivity and translocator protein PET in Gulf War Illness. Brain Behav. Immun. Health 2021, 18, 100364. [Google Scholar] [CrossRef]
- Cheng, C.H.; Koo, B.B.; Calderazzo, S.; Quinn, E.; Aenlle, K.; Steele, L.; Klimas, N.; Krengel, M.; Janulewicz, P.; Toomey, R.; et al. Alterations in high-order diffusion imaging in veterans with Gulf War Illness is associated with chemical weapons exposure and mild traumatic brain injury. Brain Behav. Immun. 2020, 89, 281–290. [Google Scholar] [CrossRef]
- Dickey, B.; Madhu, L.N.; Shetty, A.K. Gulf War Illness: Mechanisms Underlying Brain Dysfunction and Promising Therapeutic Strategies. Pharmacol. Ther. 2021, 220, 107716. [Google Scholar] [CrossRef]
- Godlewska, B.R.; Sylvester, A.L.; Emir, U.E.; Sharpley, A.L.; Clarke, W.T.; Williams, S.R.; Gonçalves, A.J.; Raman, B.; Valkovič, L.; Cowen, P.J. Brain and muscle chemistry in myalgic encephalitis/chronic fatigue syndrome (ME/CFS) and long COVID: A 7T magnetic resonance spectroscopy study. Mol. Psychiatry 2025, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jonsjö, M.A.; Olsson, G.L.; Wicksell, R.K.; Alving, K.; Holmström, L.; Andreasson, A. The role of low-grade inflammation in ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome)—Associations with symptoms. Psychoneuroendocrinology 2020, 113, 104578. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Sato, W.; Son, C.G. Brain-regional characteristics and neuroinflammation in ME/CFS patients from neuroimaging: A systematic review and meta-analysis. Autoimmun. Rev. 2024, 23, 103484. [Google Scholar] [CrossRef] [PubMed]
- Dass, R.; Kalia, M.; Harris, J.; Packham, T. Understanding the Experience and Impacts of Brain Fog in Chronic Pain: A Scoping Review. Can. J. Pain 2023, 7, 2217865. [Google Scholar] [CrossRef]
- García-Domínguez, M. Fibromyalgia and Inflammation: Unrevealing the Connection. Cells 2025, 14, 271. [Google Scholar] [CrossRef]
- Ferrés, S.; Serrat, M.; Auer, W.; Royuela-Colomer, E.; Almirall, M.; Lizama-Lefno, A.; Nijs, J.; Maes, M.; Luciano, J.V.; Borràs, X.; et al. Immune-inflammatory effects of the multicomponent intervention FIBROWALK in outdoor and online formats for patients with fibromyalgia. Brain Behav. Immun. 2025, 125, 184–197. [Google Scholar] [CrossRef]
- Zhang, C.; Zhang, P.; Zhao, Y.; Liu, Y.; Hu, Y.; Zhu, Z.; Xiao, H. The Effect of a Remote Network Technology Supervised Exercise Program Combined With Drug Treatment for Fibromyalgia: Randomized, Single-Blind, Controlled Trial. J. Med. Internet Res. 2025, 27, e71624. [Google Scholar] [CrossRef]
- Zhao, S.; Martin, E.M.; Reuken, P.A.; Scholcz, A.; Ganse-Dumrath, A.; Srowig, A.; Utech, I.; Kozik, V.; Radscheidt, M.; Brodoehl, S.; et al. Long COVID is associated with severe cognitive slowing: A multicentre cross-sectional study. EClinicalMedicine 2024, 68, 102434. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Cui, R.; Leng, L.; Wang, G.; Peng, G. Cognitive Impairment in the Post-Acute Phases of COVID-19 and Mechanisms: An Introduction and Narrative Review. J. Alzheimers Dis. Rep. 2024, 8, 647–658. [Google Scholar] [CrossRef]
- Liew, F.; Efstathiou, C.; Fontanella, S.; Richardson, M.; Saunders, R.; Swieboda, D.; Sidhu, J.K.; Ascough, S.; Moore, S.C.; Mohamed, N.; et al. Large-scale phenotyping of patients with long COVID post-hospitalization reveals mechanistic subtypes of disease. Nat. Immunol. 2024, 25, 607–621. [Google Scholar] [CrossRef] [PubMed]
- Lipsky, R.K.; Helmer, D.A.; Beckham, J.C.; Calhoun, P.S.; Pugh, M.J.; Kimbrel, N.A. The association between Gulf War Illness and suicidal thoughts and behaviors among Gulf War Era Veterans. J. Psychiatr. Res. 2025, 183, 302–307. [Google Scholar] [CrossRef]
- Van Wilgen, C.P.; Ucles-Juarez, R.; Krutko, D.; Li, Y.; Polli, A.; Syed, A.; Zampese, S.; Reis, F.J.J.; de Zeeuw, J. Knowledge on cause, clinical manifestation and treatment for fibromyalgia among medical doctors: A worldwide survey. Pain Pract. 2024, 24, 620–626. [Google Scholar] [CrossRef] [PubMed]
- Zeron-Rugerio, M.F.; Zaragoza, M.C.; Domingo, J.C.; Sanmartin-Sentanes, R.; Alegre-Martin, J.; Castro-Marrero, J.; Cambras, T. Sleep and circadian rhythm alterations in myalgic encephalomyelitis/chronic fatigue syndrome and post-COVID fatigue syndrome and its association with cardiovascular risk factors: A prospective cohort study. Chronobiol. Int. 2024, 41, 1104–1115. [Google Scholar] [CrossRef]
- Winograd, D.M.; Sullivan, N.L.; Thien, S.R.; Pigeon, W.R.; Litke, D.R.; Helmer, D.A.; Rath, J.F.; Lu, S.E.; McAndrew, L.M. Veterans with Gulf War Illness perceptions of management strategies. Life Sci. 2021, 279, 119219. [Google Scholar] [CrossRef]
- Karabey Aksalli, I.; Baygin, N.; Hagiwara, Y.; Paul, J.K.; Iype, T.; Barua, P.D.; Koh, J.E.W.; Baygin, M.; Dogan, S.; Tuncer, T.; et al. Automated characterization and detection of fibromyalgia using slow wave sleep EEG signals with glucose pattern and D’hondt pooling technique. Cogn. Neurodyn. 2024, 18, 383–404. [Google Scholar] [CrossRef]
- Lederman, S.; Arnold, L.M.; Vaughn, B.; Engels, J.M.; Kelley, M.; Sullivan, G.M. Pain Relief by Targeting Nonrestorative Sleep in Fibromyalgia: A Phase 3 Randomized Trial of Bedtime Sublingual Cyclobenzaprine. Pain Med. 2025, pnaf089. [Google Scholar] [CrossRef]
- Malluru, N.; Abdullah, Y.; Hackshaw, K.V. Early diagnostics of fibromyalgia: An overview of the challenges and opportunities. Expert Rev. Mol. Diagn. 2025, 25, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, N.Z.Y.; Parekh, R.S.; Inban, P.; Sakthi, S.; Tekuru, Y.; Prajjwal, P.; John, J.; Sharma, R. Fibromyalgia: Advances in pathophysiology, diagnostic biomarkers, genetic insights, multisystemic involvement, and treatment updates and multidisciplinary interventions. Dis. Mon. 2025, 71, 101965. [Google Scholar] [CrossRef] [PubMed]
- Climent-Sanz, C.; Valenzuela-Pascual, F.; Martínez-Navarro, O.; Blanco-Blanco, J.; Rubí-Carnacea, F.; García-Martínez, E.; Soler-González, J.; Barallat-Gimeno, E.; Gea-Sánchez, M. Cognitive behavioral therapy for insomnia (CBT-i) in patients with fibromyalgia: A systematic review and meta-analysis. Disabil. Rehabil. 2022, 44, 5770–5783. [Google Scholar] [CrossRef]
- Imamura, M.; Robertson, C.; Hudson, J.; Whibley, D.; Aucott, L.; Gillies, K.; Beasley, M.; Stevens, M.J.; Manson, P.; Dulake, D.; et al. Effects of pharmacological and non-pharmacological interventions for the management of sleep problems in people with fibromyalgia: A multi-methods evidence synthesis. Health Technol. Assess. 2025, 29, 1–228. [Google Scholar] [CrossRef]
- Castro-Marrero, J.; Zaragozá, M.C.; González-Garcia, S.; Aliste, L.; Sáez-Francàs, N.; Romero, O.; Ferré, A.; Fernández de Sevilla, T.; Alegre, J. Poor self-reported sleep quality and health-related quality of life in patients with chronic fatigue syndrome/myalgic encephalomyelitis. J. Sleep Res. 2018, 27, e12703. [Google Scholar] [CrossRef] [PubMed]
- Weigel, B.; Eaton-Fitch, N.; Thapaliya, K.; Marshall-Gradisnik, S. Illness presentation and quality of life in myalgic encephalomyelitis/chronic fatigue syndrome and post COVID-19 condition: A pilot Australian cross-sectional study. Qual. Life Res. 2024, 33, 2489–2507. [Google Scholar] [CrossRef]
- Mohamed, A.Z.; Andersen, T.; Radovic, S.; Del Fante, P.; Kwiatek, R.; Calhoun, V.; Bhuta, S.; Hermens, D.F.; Lagopoulos, J.; Shan, Z.Y. Objective sleep measures in chronic fatigue syndrome patients: A systematic review and meta-analysis. Sleep Med. Rev. 2023, 69, 101771. [Google Scholar] [CrossRef]
- Yin, J.; Xu, J.; Ren, T.L. Recent Progress in Long-Term Sleep Monitoring Technology. Biosensors 2023, 13, 395. [Google Scholar] [CrossRef]
- Chao, L.L. Examining the current health of Gulf War veterans with the veterans affairs frailty index. Front. Neurosci. 2023, 17, 1245811. [Google Scholar] [CrossRef]
- Pettersen, P.S.; Haugmark, T.; Berg, I.J.; Hammer, H.B.; Neogi, T.; Zangi, H.; Haugen, I.K.; Provan, S.A. Pain sensitization in fibromyalgia. Cross-sectional associations between quantitative sensory testing of pain sensitization and fibromyalgia disease burden. Eur. J. Pain 2025, 29, e4771. [Google Scholar] [CrossRef]
- Escalante, A.; Fischbach, M. Musculoskeletal manifestations, pain, and quality of life in Persian Gulf War veterans referred for rheumatologic evaluation. J. Rheumatol. 1998, 25, 2228–2235. [Google Scholar]
- Castro-Marrero, J.; Cordero, M.D.; Sáez-Francas, N.; Jimenez-Gutierrez, C.; Aguilar-Montilla, F.J.; Aliste, L.; Alegre-Martin, J. Could mitochondrial dysfunction be a differentiating marker between chronic fatigue syndrome and fibromyalgia? Antioxid. Redox Signal. 2013, 19, 1855–1860. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Meyer, J.N.; Hill, H.Z.; Lange, G.; Condon, M.R.; Klein, J.C.; Ndirangu, D.; Falvo, M.J. Role of mitochondrial DNA damage and dysfunction in veterans with Gulf War Illness. PLoS ONE 2017, 12, e0184832. [Google Scholar] [CrossRef]
- Koslik, H.J.; Hamilton, G.; Golomb, B.A. Mitochondrial dysfunction in Gulf War illness revealed by 31Phosphorus Magnetic Resonance Spectroscopy: A case-control study. PLoS ONE 2014, 9, e92887. [Google Scholar] [CrossRef] [PubMed]
- Golomb, B.A.; Han, J.H.; Fung, A.; Berg, B.K.; Miller, B.J.; Hamilton, G. Bioenergetic impairment in Gulf War illness assessed via (31)P-MRS. Sci. Rep. 2024, 14, 7418. [Google Scholar] [CrossRef]
- Golomb, B.A.; Kelley, R.I.; Han, J.H.; Miller, B.; Bui, L. Gulf war illness: A tale of two genomes. BMC Res. Notes 2024, 17, 230. [Google Scholar] [CrossRef] [PubMed]
- Golomb, B.A.; Sanchez Baez, R.; Schilling, J.M.; Dhanani, M.; Fannon, M.J.; Berg, B.K.; Miller, B.J.; Taub, P.R.; Patel, H.H. Mitochondrial impairment but not peripheral inflammation predicts greater Gulf War illness severity. Sci. Rep. 2023, 13, 10739. [Google Scholar] [CrossRef]
- Shetty, G.A.; Hattiangady, B.; Upadhya, D.; Bates, A.; Attaluri, S.; Shuai, B.; Kodali, M.; Shetty, A.K. Chronic Oxidative Stress, Mitochondrial Dysfunction, Nrf2 Activation and Inflammation in the Hippocampus Accompany Heightened Systemic Inflammation and Oxidative Stress in an Animal Model of Gulf War Illness. Front. Mol. Neurosci. 2017, 10, 182. [Google Scholar] [CrossRef]
- Cordero, M.D.; de Miguel, M.; Carmona-López, I.; Bonal, P.; Campa, F.; Moreno-Fernández, A.M. Oxidative stress and mitochondrial dysfunction in fibromyalgia. Neuro Endocrinol. Lett. 2010, 31, 169–173. [Google Scholar]
- Assavarittirong, C.; Samborski, W.; Grygiel-Górniak, B. Oxidative Stress in Fibromyalgia: From Pathology to Treatment. Oxid. Med. Cell. Longev. 2022, 2022, 1582432. [Google Scholar] [CrossRef]
- Holden, S.; Maksoud, R.; Eaton-Fitch, N.; Cabanas, H.; Staines, D.; Marshall-Gradisnik, S. A systematic review of mitochondrial abnormalities in myalgic encephalomyelitis/chronic fatigue syndrome/systemic exertion intolerance disease. J. Transl. Med. 2020, 18, 290. [Google Scholar] [CrossRef]
- Smits, B.; van den Heuvel, L.; Knoop, H.; Küsters, B.; Janssen, A.; Borm, G.; Bleijenberg, G.; Rodenburg, R.; van Engelen, B. Mitochondrial enzymes discriminate between mitochondrial disorders and chronic fatigue syndrome. Mitochondrion 2011, 11, 735–738. [Google Scholar] [CrossRef] [PubMed]
- Tomas, C.; Brown, A.; Strassheim, V.; Elson, J.L.; Newton, J.; Manning, P. Cellular bioenergetics is impaired in patients with chronic fatigue syndrome. PLoS ONE 2017, 12, e0186802. [Google Scholar] [CrossRef]
- Molnar, T.; Lehoczki, A.; Fekete, M.; Varnai, R.; Zavori, L.; Erdo-Bonyar, S.; Simon, D.; Berki, T.; Csecsei, P.; Ezer, E. Mitochondrial dysfunction in long COVID: Mechanisms, consequences, and potential therapeutic approaches. Geroscience 2024, 46, 5267–5286. [Google Scholar] [CrossRef]
- Szögi, T.; Borsos, B.N.; Masic, D.; Radics, B.; Bella, Z.; Bánfi, A.; Ördög, N.; Zsiros, C.; Kiricsi, Á.; Pankotai-Bodó, G.; et al. Novel biomarkers of mitochondrial dysfunction in Long COVID patients. Geroscience 2025, 47, 2245–2261. [Google Scholar] [CrossRef] [PubMed]
- Stufano, A.; Isgrò, C.; Palese, L.L.; Caretta, P.; De Maria, L.; Lovreglio, P.; Sardanelli, A.M. Oxidative Damage and Post-COVID Syndrome: A Cross-Sectional Study in a Cohort of Italian Workers. Int. J. Mol. Sci. 2023, 24, 7445. [Google Scholar] [CrossRef]
- Cox, B.; Goolkasian, P.; Palomo, I.M.; Williams, M.V.; Maloney, S.R.; Ariza, M.E. Reactivation of Latent Herpesviruses and a Faulty Antiviral Response may Contribute to Chronic Multi-Symptom and Multi-System Illnesses in U.S. Military Veterans. J. Med. Virol. 2025, 97, e70400. [Google Scholar] [CrossRef]
- Mettler, J.; Ming-Azevedo, P.; Hügle, T. Fibromyalgia with concomitant immune-mediated rheumatic diseases: An evaluation of clinical characteristics, diagnostic criteria and multimodal treatment outcomes. Adv. Rheumatol. 2025, 65, 27. [Google Scholar] [CrossRef] [PubMed]
- Burzynski, H.E.; Reagan, L.P. Exposing the latent phenotype of Gulf War Illness: Examination of the mechanistic mediators of cognitive dysfunction. Front. Immunol. 2024, 15, 1403574. [Google Scholar] [CrossRef]
- Trageser, K.J.; Sebastian-Valverde, M.; Naughton, S.X.; Pasinetti, G.M. The Innate Immune System and Inflammatory Priming: Potential Mechanistic Factors in Mood Disorders and Gulf War Illness. Front. Psychiatry 2020, 11, 704. [Google Scholar] [CrossRef]
- Whistler, T.; Fletcher, M.A.; Lonergan, W.; Zeng, X.R.; Lin, J.M.; Laperriere, A.; Vernon, S.D.; Klimas, N.G. Impaired immune function in Gulf War Illness. BMC Med. Genom. 2009, 2, 12. [Google Scholar] [CrossRef]
- Klein, J.; Wood, J.; Jaycox, J.R.; Dhodapkar, R.M.; Lu, P.; Gehlhausen, J.R.; Tabachnikova, A.; Greene, K.; Tabacof, L.; Malik, A.A.; et al. Distinguishing features of long COVID identified through immune profiling. Nature 2023, 623, 139–148. [Google Scholar] [CrossRef]
- Ruf, W. Immune damage in Long COVID. Science 2024, 383, 262–263. [Google Scholar] [CrossRef] [PubMed]
- Yin, K.; Peluso, M.J.; Luo, X.; Thomas, R.; Shin, M.G.; Neidleman, J.; Andrew, A.; Young, K.C.; Ma, T.; Hoh, R.; et al. Long COVID manifests with T cell dysregulation, inflammation and an uncoordinated adaptive immune response to SARS-CoV-2. Nat. Immunol. 2024, 25, 218–225. [Google Scholar] [CrossRef]
- Eaton-Fitch, N.; Rudd, P.; Er, T.; Hool, L.; Herrero, L.; Marshall-Gradisnik, S. Immune exhaustion in ME/CFS and long COVID. JCI Insight 2024, 9, e183810. [Google Scholar] [CrossRef] [PubMed]
- Lutz, L.; Rohrhofer, J.; Zehetmayer, S.; Stingl, M.; Untersmayr, E. Evaluation of Immune Dysregulation in an Austrian Patient Cohort Suffering from Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Biomolecules 2021, 11, 1359. [Google Scholar] [CrossRef] [PubMed]
- O’Neal, A.J.; Hanson, M.R. The Enterovirus Theory of Disease Etiology in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Critical Review. Front. Med. 2021, 8, 688486. [Google Scholar] [CrossRef]
- Vinker-Shuster, M.; Magen, E.; Green, I.; Merzon, E.; Golan-Cohen, A.; Israel, A. Increased Rates of Infectious Diseases in Fibromyalgia Patients: A Population-Based Case-Control Study. Biomedicines 2024, 12, 2821. [Google Scholar] [CrossRef]
- Clauw, D.; Sarzi-Puttini, P.; Pellegrino, G.; Shoenfeld, Y. Is fibromyalgia an autoimmune disorder? Autoimmun. Rev. 2024, 23, 103424. [Google Scholar] [CrossRef]
- Findeisen, K.; Guymer, E.; Littlejohn, G. Neuroinflammatory and Immunological Aspects of Fibromyalgia. Brain Sci. 2025, 15, 206. [Google Scholar] [CrossRef] [PubMed]
- Goebel, A.; Krock, E.; Gentry, C.; Israel, M.R.; Jurczak, A.; Urbina, C.M.; Sandor, K.; Vastani, N.; Maurer, M.; Cuhadar, U.; et al. Passive transfer of fibromyalgia symptoms from patients to mice. J. Clin. Investig. 2021, 131, e144201. [Google Scholar] [CrossRef] [PubMed]
- Camici, M.; Del Duca, G.; Brita, A.C.; Antinori, A. Connecting dots of long COVID-19 pathogenesis: A vagus nerve- hypothalamic-pituitary- adrenal-mitochondrial axis dysfunction. Front. Cell. Infect. Microbiol. 2024, 14, 1501949. [Google Scholar] [CrossRef]
- Tak, L.M.; Cleare, A.J.; Ormel, J.; Manoharan, A.; Kok, I.C.; Wessely, S.; Rosmalen, J.G. Meta-analysis and meta-regression of hypothalamic-pituitary-adrenal axis activity in functional somatic disorders. Biol. Psychol. 2011, 87, 183–194. [Google Scholar] [CrossRef]
- O’Callaghan, J.P.; Miller, D.B. Neuroinflammation disorders exacerbated by environmental stressors. Metabolism 2019, 100, 153951. [Google Scholar] [CrossRef]
- Golier, J.A.; Caramanica, K.; Yehuda, R. Neuroendocrine response to CRF stimulation in veterans with and without PTSD in consideration of war zone era. Psychoneuroendocrinology 2012, 37, 350–357. [Google Scholar] [CrossRef]
- Tomic, S.; Brkic, S.; Lendak, D.; Maric, D.; Medic Stojanoska, M.; Novakov Mikic, A. Neuroendocrine disorder in chronic fatigue syndrome. Turk. J. Med. Sci. 2017, 47, 1097–1103. [Google Scholar] [CrossRef]
- Demori, I.; Losacco, S.; Giordano, G.; Mucci, V.; Blanchini, F.; Burlando, B. Fibromyalgia pathogenesis explained by a neuroendocrine multistable model. PLoS ONE 2024, 19, e0303573. [Google Scholar] [CrossRef] [PubMed]
- Sasikumar, S.; Unniappan, S. SARS-CoV-2 Infection and the Neuroendocrine System. Neuroendocrinology 2024, 114, 1158–1175. [Google Scholar] [CrossRef]
- Kimono, D.A. Gastrointestinal problems, mechanisms and possible therapeutic directions in Gulf war illness: A mini review. Mil. Med. Res. 2021, 8, 50. [Google Scholar] [CrossRef]
- Trivedi, A.; Bose, D.; Moffat, K.; Pearson, E.; Walsh, D.; Cohen, D.; Skupsky, J.; Chao, L.; Golier, J.; Janulewicz, P.; et al. Gulf War Illness Is Associated with Host Gut Microbiome Dysbiosis and Is Linked to Altered Species Abundance in Veterans from the BBRAIN Cohort. Int. J. Environ. Res. Public Health 2024, 21, 1102. [Google Scholar] [CrossRef]
- Keating, J.A.; Shaughnessy, C.; Baubie, K.; Kates, A.E.; Putman-Buehler, N.; Watson, L.; Dominguez, N.; Watson, K.; Cook, D.B.; Rabago, D.; et al. Characterising the gut microbiome in veterans with Gulf War Illness: A protocol for a longitudinal, prospective cohort study. BMJ Open 2019, 9, e031114. [Google Scholar] [CrossRef]
- Nono Djotsa, A.B.S.; Nguyen Wenker, T.H.; Ahmed, S.T.; Ghosh, S.; Malhotra, D.; Boyle, S.H.; Gifford, E.J.; Sims, K.J.; White, D.L.; Steele, L.; et al. Irritable Bowel Syndrome in Veterans With Gulf War Illness Evaluated at VA’s War-Related Illness and Injury Study Center. Mil. Med. 2024, 189, e2644–e2654. [Google Scholar] [CrossRef]
- Malhotra, D.; Boyle, S.H.; Gifford, E.J.; Sullivan, B.A.; Nguyen Wenker, T.H.; Abs, N.D.; Ahmed, S.T.; Upchurch, J.; Vahey, J.; Stafford, C.; et al. Self-reported gastrointestinal disorders among veterans with gulf war illness with and without posttraumatic stress disorder. Neurogastroenterol Motil. 2023, 35, e14548. [Google Scholar] [CrossRef]
- Chatterjee, S.; Bose, D.; Seth, R. Host gut microbiome and potential therapeutics in Gulf War Illness: A short review. Life Sci. 2021, 280, 119717. [Google Scholar] [CrossRef] [PubMed]
- Saha, P.; Skidmore, P.T.; Holland, L.A.; Mondal, A.; Bose, D.; Seth, R.K.; Sullivan, K.; Janulewicz, P.A.; Horner, R.; Klimas, N.; et al. Andrographolide Attenuates Gut-Brain-Axis Associated Pathology in Gulf War Illness by Modulating Bacteriome-Virome Associated Inflammation and Microglia-Neuron Proinflammatory Crosstalk. Brain Sci. 2021, 11, 905. [Google Scholar] [CrossRef] [PubMed]
- Collier, C.A.; Salikhova, A.; Sabir, S.; Raghavan, S.A. Persistent enteric neuroinflammation chronically impairs colonic motility in a pyridostigmine bromide-induced mouse model of Gulf War illness. Biol. Open 2025, 14, bio061867. [Google Scholar] [CrossRef]
- Martín, F.; Blanco-Suárez, M.; Zambrano, P.; Cáceres, O.; Almirall, M.; Alegre-Martín, J.; Lobo, B.; González-Castro, A.M.; Santos, J.; Domingo, J.C.; et al. Increased gut permeability and bacterial translocation are associated with fibromyalgia and myalgic encephalomyelitis/chronic fatigue syndrome: Implications for disease-related biomarker discovery. Front. Immunol. 2023, 14, 1253121. [Google Scholar] [CrossRef]
- Shtrozberg, S.; Bazzichi, L.; Sarzi-Puttini, P.; Aloush, V.; Ablin, J.N. Is the gut microbiome of importance in fibromyalgia? A critical review of emerging evidence. Clin. Exp. Rheumatol. 2025, 43, 990–998. [Google Scholar] [CrossRef] [PubMed]
- Waterman, A.; Doumas, S.A.; Fischer, M.; Mattar, M.; Charbel, S.; Jennings, J.; Doman, D.B. Uncovering the Hidden Link Between the Aberrant Intestinal Microbiome and Fibromyalgia. Gastroenterol. Hepatol. 2025, 21, 111–121. [Google Scholar]
- Iannuccelli, C.; Favretti, M.; Dolcini, G.; Di Carlo, M.; Pellegrino, G.; Bazzichi, L.; Atzeni, F.; Lucini, D.; Varassi, G.; Leoni, M.L.G.; et al. Fibromyalgia: One year in review 2025. Clin. Exp. Rheumatol. 2025, 43, 957–969. [Google Scholar] [CrossRef]
- Jurek, J.M.; Castro-Marrero, J. A Narrative Review on Gut Microbiome Disturbances and Microbial Preparations in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Implications for Long COVID. Nutrients 2024, 16, 1545. [Google Scholar] [CrossRef] [PubMed]
- Trautmann, A. Core features and inherent diversity of post-acute infection syndromes. Front. Immunol. 2025, 16, 1509131. [Google Scholar] [CrossRef]
- Guo, C.; Che, X.; Briese, T.; Ranjan, A.; Allicock, O.; Yates, R.A.; Cheng, A.; March, D.; Hornig, M.; Komaroff, A.L.; et al. Deficient butyrate-producing capacity in the gut microbiome is associated with bacterial network disturbances and fatigue symptoms in ME/CFS. Cell Host Microbe 2023, 31, 288–304.e288. [Google Scholar] [CrossRef] [PubMed]
- Tian, H.; Wang, L.; Aiken, E.; Ortega, R.J.V.; Hardy, R.; Placek, L.; Kozhaya, L.; Unutmaz, D.; Oh, J.; Yao, X. Fast Targeted Metabolomics for Analyzing Metabolic Diversity of Bacterial Indole Derivatives in ME/CFS Gut Microbiome. bioRxiv 2024. [Google Scholar] [CrossRef] [PubMed]
- Xiong, R.; Gunter, C.; Fleming, E.; Vernon, S.D.; Bateman, L.; Unutmaz, D.; Oh, J. Multi-’omics of gut microbiome-host interactions in short- and long-term myalgic encephalomyelitis/chronic fatigue syndrome patients. Cell Host Microbe 2023, 31, 273–287.e275. [Google Scholar] [CrossRef]
- Lau, R.I.; Su, Q.; Ng, S.C. Long COVID and gut microbiome: Insights into pathogenesis and therapeutics. Gut Microbes 2025, 17, 2457495. [Google Scholar] [CrossRef]
- Oh, S.; An, S.; Park, K.; Lee, S.; Han, Y.M.; Koh, S.J.; Lee, J.; Gim, H.; Kim, D.; Seo, H. Gut Microbial Signatures in Long COVID: Potential Biomarkers and Therapeutic Targets. Infect. Dis. Ther. 2025, 14, 1461–1475. [Google Scholar] [CrossRef]
- Smail, S.W.; Albarzinji, N.; Salih, R.H.; Taha, K.O.; Hirmiz, S.M.; Ismael, H.M.; Noori, M.F.; Azeez, S.S.; Janson, C. Microbiome dysbiosis in SARS-CoV-2 infection: Implication for pathophysiology and management strategies of COVID-19. Front. Cell. Infect. Microbiol. 2025, 15, 1537456. [Google Scholar] [CrossRef]
- Yao, L.; Devotta, H.; Li, J.; Lunjani, N.; Sadlier, C.; Lavelle, A.; Albrich, W.C.; Walter, J.; O’Toole, P.W.; O’Mahony, L. Dysrupted microbial tryptophan metabolism associates with SARS-CoV-2 acute inflammatory responses and long COVID. Gut Microbes 2024, 16, 2429754. [Google Scholar] [CrossRef]
- Yu, L.C. Gastrointestinal pathophysiology in long COVID: Exploring roles of microbiota dysbiosis and serotonin dysregulation in post-infectious bowel symptoms. Life Sci. 2024, 358, 123153. [Google Scholar] [CrossRef] [PubMed]
- El-Sehrawy, A.; Ayoub, I.I.; Uthirapathy, S.; Ballal, S.; Gabble, B.C.; Singh, A.; V, K.; Panigrahi, R.; Kamali, M.; Khosravi, M. The microbiota-gut-brain axis in myalgic encephalomyelitis/chronic fatigue syndrome: A narrative review of an emerging field. Eur. J. Transl. Myol. 2025, 35, 13690. [Google Scholar] [CrossRef]
- Elmore, S. Apoptosis: A review of programmed cell death. Toxicol. Pathol. 2007, 35, 495–516. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Kang, R.; Tang, D. Monitoring autophagy-dependent ferroptosis. Methods Cell Biol. 2021, 165, 163–176. [Google Scholar] [CrossRef] [PubMed]
- Georgopoulos, A.P.; James, L.M.; Carpenter, A.F.; Engdahl, B.E.; Leuthold, A.C.; Lewis, S.M. Gulf War illness (GWI) as a neuroimmune disease. Exp. Brain Res. 2017, 235, 3217–3225. [Google Scholar] [CrossRef]
- Tsilibary, E.C.; Souto, E.P.; Kratzke, M.; James, L.M.; Engdahl, B.E.; Georgopoulos, A.P. Anthrax Protective Antigen 63 (PA63): Toxic Effects in Neural Cultures and Role in Gulf War Illness (GWI). Neurosci. Insights 2020, 15, 2633105520931966. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Lavín, M. Dorsal root ganglia: Fibromyalgia pain factory? Clin. Rheumatol. 2021, 40, 783–787. [Google Scholar] [CrossRef]
- Yüksel, E.; Nazıroğlu, M.; Şahin, M.; Çiğ, B. Involvement of TRPM2 and TRPV1 channels on hyperalgesia, apoptosis and oxidative stress in rat fibromyalgia model: Protective role of selenium. Sci. Rep. 2017, 7, 17543. [Google Scholar] [CrossRef]
- Gheita, T.A.; El Sisi, R.W.; Raafat, H.A.; Khalil, H.M. Anti-annexin V antibodies in primary fibromyalgia syndrome: Relation to associated Sjögren’s syndrome. J. Clin. Immunol. 2013, 33, 311–312. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Z.; Jiao, W.; Wang, Y.; Wang, X.; Zhao, Y.; Fan, X.; Tian, L.; Li, X.; Mi, J. Ferroptosis and its role in skeletal muscle diseases. Front. Mol. Biosci. 2022, 9, 1051866. [Google Scholar] [CrossRef]
- Jiang, L.; Zhu, Z.; Han, K.; Chen, D.; Huang, L.; Hu, N.; Du, J.; Zhang, B.; Su, Y.; Li, T.; et al. Magnesium hexacyanoferrate nanocatalysts alleviates fibromyalgia syndrome by reversing cellular ferroptosis. J. Chem. Eng. 2024, 498, 155019. [Google Scholar] [CrossRef]
- Kennedy, G.; Khan, F.; Hill, A.; Underwood, C.; Belch, J.J. Biochemical and vascular aspects of pediatric chronic fatigue syndrome. Arch. Pediatr. Adolesc. Med. 2010, 164, 817–823. [Google Scholar] [CrossRef]
- Cezar, R.; Kundura, L.; André, S.; Lozano, C.; Vincent, T.; Muller, L.; Lefrant, J.Y.; Roger, C.; Claret, P.G.; Duvnjak, S.; et al. T4 apoptosis in the acute phase of SARS-CoV-2 infection predicts long COVID. Front. Immunol. 2023, 14, 1335352. [Google Scholar] [CrossRef]
- Biamonte, F.; Botta, C.; Mazzitelli, M.; Rotundo, S.; Trecarichi, E.M.; Foti, D.; Torti, C.; Viglietto, G.; Torella, D.; Costanzo, F. Combined lymphocyte/monocyte count, D-dimer and iron status predict COVID-19 course and outcome in a long-term care facility. J. Transl. Med. 2021, 19, 79. [Google Scholar] [CrossRef]
- Sousa, R.A.L.; Yehia, A.; Abulseoud, O.A. Attenuation of ferroptosis as a potential therapeutic target for neuropsychiatric manifestations of post-COVID syndrome. Front. Neurosci. 2023, 17, 1237153. [Google Scholar] [CrossRef]
- Yang, L.; Wu, Y.; Jin, W.; Mo, N.; Ye, G.; Su, Z.; Tang, L.; Wang, Y.; Li, Y.; Du, J. The potential role of ferroptosis in COVID-19-related cardiovascular injury. Biomed. Pharmacother. 2023, 168, 115637. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Wang, S.; Han, Y.; Zhang, H.; Cao, J.; Dong, S.; Li, D.; Lei, M.; Liu, C.; Gao, Y. Role of Ferroptosis in the Progression of COVID-19 and the Development of Long COVID. Curr. Med. Chem. 2024, 32, 4324–4342. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.M.; Pendlebury, D.F.; Nandakumar, J. Structural biology of telomeres and telomerase. Cell. Mol. Life Sci. 2020, 77, 61–79. [Google Scholar] [CrossRef] [PubMed]
- Starkweather, A.R.; Alhaeeri, A.A.; Montpetit, A.; Brumelle, J.; Filler, K.; Montpetit, M.; Mohanraj, L.; Lyon, D.E.; Jackson-Cook, C.K. An integrative review of factors associated with telomere length and implications for biobehavioral research. Nurs. Res. 2014, 63, 36–50. [Google Scholar] [CrossRef]
- Gao, X.; Yu, X.; Zhang, C.; Wang, Y.; Sun, Y.; Sun, H.; Zhang, H.; Shi, Y.; He, X. Telomeres and Mitochondrial Metabolism: Implications for Cellular Senescence and Age-related Diseases. Stem Cell Rev. Rep. 2022, 18, 2315–2327. [Google Scholar] [CrossRef]
- Nassour, J.; Przetocka, S.; Karlseder, J. Telomeres as hotspots for innate immunity and inflammation. DNA Repair 2024, 133, 103591. [Google Scholar] [CrossRef]
- Opresko, P.L.; Sanford, S.L.; De Rosa, M. Oxidative Stress and DNA Damage at Telomeres. Cold Spring Harb. Perspect. Biol. 2025, 17, a041707. [Google Scholar] [CrossRef] [PubMed]
- Armanios, M. The Role of Telomeres in Human Disease. Annu. Rev. Genom. Hum. Genet. 2022, 23, 363–381. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.T.; Janak, J.C.; Santos-Lozada, A.R.; McEvilla, S.; Ansley, S.D.; Walker, L.E.; Spiro, A.; Stewart, I.J. Telomere Shortening and Accelerated Aging in US Military Veterans. Int. J. Environ. Res. Public Health 2021, 18, 1743. [Google Scholar] [CrossRef]
- Charatan, F. Nerve gas antidote a possible cause of gulf war illness. BMJ 1999, 319, 1154. [Google Scholar] [CrossRef]
- Mantle, D.; Golomb, B.A. Coenzyme Q10 and Xenobiotic Metabolism: An Overview. Int. J. Mol. Sci. 2025, 26, 5788. [Google Scholar] [CrossRef]
- Rajeevan, M.S.; Murray, J.; Oakley, L.; Lin, J.S.; Unger, E.R. Association of chronic fatigue syndrome with premature telomere attrition. J. Transl. Med. 2018, 16, 44. [Google Scholar] [CrossRef]
- Hassett, A.L.; Epel, E.; Clauw, D.J.; Harris, R.E.; Harte, S.E.; Kairys, A.; Buyske, S.; Williams, D.A. Pain is associated with short leukocyte telomere length in women with fibromyalgia. J. Pain 2012, 13, 959–969. [Google Scholar] [CrossRef]
- Dos Reis, G.G.; Silvestre, R.T.; Alves, G.; Delmonico, L.; Chantre-Justino, M.; Moreira, A.D.S.; Müller, B.L.A.; do Nascimento, C.R.; da Silva, D.L.P.; Dos Santos, L.S.; et al. Leukocyte telomere length and telomerase activity in Long COVID patients from Rio de Janeiro, Brazil. Mem. Inst. Oswaldo Cruz 2025, 120, e240129. [Google Scholar] [CrossRef]
- Mongelli, A.; Barbi, V.; Gottardi Zamperla, M.; Atlante, S.; Forleo, L.; Nesta, M.; Massetti, M.; Pontecorvi, A.; Nanni, S.; Farsetti, A.; et al. Evidence for Biological Age Acceleration and Telomere Shortening in COVID-19 Survivors. Int. J. Mol. Sci. 2021, 22, 6151. [Google Scholar] [CrossRef] [PubMed]
- Polli, A.; Godderis, L.; Martens, D.S.; Patil, M.S.; Hendrix, J.; Wyns, A.; Van Campenhout, J.; Richter, E.; Fanning, L.; Vandekerckhove, O.; et al. Exploring DNA methylation, telomere length, mitochondrial DNA, and immune function in patients with Long-COVID. BMC Med. 2025, 23, 60. [Google Scholar] [CrossRef]
- Castro-Marrero, J.; Sáez-Francàs, N.; Santillo, D.; Alegre, J. Treatment and management of chronic fatigue syndrome/myalgic encephalomyelitis: All roads lead to Rome. Br. J. Pharmacol. 2017, 174, 345–369. [Google Scholar] [CrossRef] [PubMed]
- Chandan, J.S.; Brown, K.R.; Simms-Williams, N.; Bashir, N.Z.; Camaradou, J.; Heining, D.; Turner, G.M.; Rivera, S.C.; Hotham, R.; Minhas, S.; et al. Non-Pharmacological Therapies for Post-Viral Syndromes, Including Long COVID: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 3477. [Google Scholar] [CrossRef] [PubMed]
- Mengshoel, A.M.; Helland, I.B.; Meeus, M.; Castro-Marrero, J.; Pheby, D.; Bolle Strand, E. Patients’ experiences and effects of non-pharmacological treatment for myalgic encephalomyelitis/chronic fatigue syndrome—A scoping mixed methods review. Int. J. Qual. Stud. Health Well-Being 2020, 15, 1764830. [Google Scholar] [CrossRef] [PubMed]
- Nugent, S.M.; Freeman, M.; Ayers, C.K.; Winchell, K.A.; Press, A.M.; O’Neil, M.E.; Paynter, R.; Kansagara, D. A Systematic Review of Therapeutic Interventions and Management Strategies for Gulf War Illness. Mil. Med. 2021, 186, e169–e178. [Google Scholar] [CrossRef]
- Hetta, H.F.; Elsaghir, A.; Sijercic, V.C.; Ahmed, A.K.; Gad, S.A.; Zeleke, M.S.; Alanazi, F.E.; Ramadan, Y.N. Clinical Progress in Mesenchymal Stem Cell Therapy: A Focus on Rheumatic Diseases. Immun. Inflamm. Dis. 2025, 13, e70189. [Google Scholar] [CrossRef]
- Safina, I.; Embree, M.C. Biomaterials for recruiting and activating endogenous stem cells in situ tissue regeneration. Acta Biomater. 2022, 143, 26–38. [Google Scholar] [CrossRef]
- Liu, K.; Zhou, Z.; Pan, M.; Zhang, L. Stem cell-derived mitochondria transplantation: A promising therapy for mitochondrial encephalomyopathy. CNS Neurosci. Ther. 2021, 27, 733–742. [Google Scholar] [CrossRef]
- Xu, Z.; Zhang, L.; Fei, X.; Yi, X.; Li, W.; Wang, Q. The miR-29b-Sirt1 axis regulates self-renewal of mouse embryonic stem cells in response to reactive oxygen species. Cell. Signal. 2014, 26, 1500–1505. [Google Scholar] [CrossRef]
- Mahrouf-Yorgov, M.; Augeul, L.; Da Silva, C.C.; Jourdan, M.; Rigolet, M.; Manin, S.; Ferrera, R.; Ovize, M.; Henry, A.; Guguin, A.; et al. Mesenchymal stem cells sense mitochondria released from damaged cells as danger signals to activate their rescue properties. Cell Death Differ. 2017, 24, 1224–1238. [Google Scholar] [CrossRef]
- Ennis, W.J.; Sui, A.; Bartholomew, A. Stem Cells and Healing: Impact on Inflammation. Adv. Wound Care 2013, 2, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Rebelatto, C.L.K.; Boldrini-Leite, L.M.; Daga, D.R.; Marsaro, D.B.; Vaz, I.M.; Jamur, V.R.; de Aguiar, A.M.; Vieira, T.B.; Furman, B.P.; Aguiar, C.O.; et al. Quality Control Optimization for Minimizing Security Risks Associated with Mesenchymal Stromal Cell-Based Product Development. Int. J. Mol. Sci. 2023, 24, 12955. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Huang, H.; Lu, X.; Yan, X.; Jiang, X.; Xu, R.; Wang, S.; Zhang, C.; Yuan, X.; Xu, Z.; et al. Effect of human umbilical cord-derived mesenchymal stem cells on lung damage in severe COVID-19 patients: A randomized, double-blind, placebo-controlled phase 2 trial. Signal Transduct. Target Ther. 2021, 6, 58. [Google Scholar] [CrossRef]
- Yuan, M.Q.; Song, L.; Wang, Z.R.; Zhang, Z.Y.; Shi, M.; He, J.; Mo, Q.; Zheng, N.; Yao, W.Q.; Zhang, Y.; et al. Long-term outcomes of mesenchymal stem cell therapy in severe COVID-19 patients: 3-year follow-up of a randomized, double-blind, placebo-controlled trial. Stem Cell Res. Ther. 2025, 16, 94. [Google Scholar] [CrossRef]
- Mokhemer, S.A.; Desouky, M.K.; Abdelghany, A.K.; Ibrahim, M.F.G. Stem cells therapeutic effect in a reserpine-induced fibromyalgia rat model: A possible NLRP3 inflammasome modulation with neurogenesis promotion in the cerebral cortex. Life Sci. 2023, 325, 121784. [Google Scholar] [CrossRef]
- Golomb, B.A.; Allison, M.; Koperski, S.; Koslik, H.J.; Devaraj, S.; Ritchie, J.B. Coenzyme Q10 benefits symptoms in Gulf War veterans: Results of a randomized double-blind study. Neural Comput 2014, 26, 2594–2651. [Google Scholar] [CrossRef]
- Castro-Marrero, J.; Segundo, M.J.; Lacasa, M.; Martinez-Martinez, A.; Sentañes, R.S.; Alegre-Martin, J. Effect of Dietary Coenzyme Q10 Plus NADH Supplementation on Fatigue Perception and Health-Related Quality of Life in Individuals with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Prospective, Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients 2021, 13, 2658. [Google Scholar] [CrossRef]
- Nacul, L.; Authier, F.J.; Scheibenbogen, C.; Lorusso, L.; Helland, I.B.; Martin, J.A.; Sirbu, C.A.; Mengshoel, A.M.; Polo, O.; Behrends, U.; et al. European Network on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (EUROMENE): Expert Consensus on the Diagnosis, Service Provision, and Care of People with ME/CFS in Europe. Medicina 2021, 57, 510. [Google Scholar] [CrossRef]
- Cordero, M.D.; Alcocer-Gómez, E.; de Miguel, M.; Culic, O.; Carrión, A.M.; Alvarez-Suarez, J.M.; Bullón, P.; Battino, M.; Fernández-Rodríguez, A.; Sánchez-Alcazar, J.A. Can coenzyme q10 improve clinical and molecular parameters in fibromyalgia? Antioxid. Redox Signal. 2013, 19, 1356–1361. [Google Scholar] [CrossRef]
- Sawaddiruk, P.; Apaijai, N.; Paiboonworachat, S.; Kaewchur, T.; Kasitanon, N.; Jaiwongkam, T.; Kerdphoo, S.; Chattipakorn, N.; Chattipakorn, S.C. Coenzyme Q10 supplementation alleviates pain in pregabalin-treated fibromyalgia patients via reducing brain activity and mitochondrial dysfunction. Free Radic Res. 2019, 53, 901–909. [Google Scholar] [CrossRef] [PubMed]
- Barletta, M.A.; Marino, G.; Spagnolo, B.; Bianchi, F.P.; Falappone, P.C.F.; Spagnolo, L.; Gatti, P. Coenzyme Q10 + alpha lipoic acid for chronic COVID syndrome. Clin. Exp. Med. 2023, 23, 667–678. [Google Scholar] [CrossRef] [PubMed]
- Hansen, K.S.; Mogensen, T.H.; Agergaard, J.; Schiøttz-Christensen, B.; Østergaard, L.; Vibholm, L.K.; Leth, S. High-dose coenzyme Q10 therapy versus placebo in patients with post COVID-19 condition: A randomized, phase 2, crossover trial. Lancet Reg. Health Eur. 2023, 24, 100539. [Google Scholar] [CrossRef] [PubMed]
- Opstad, T.B.; Alexander, J.; Aaseth, J.O.; Larsson, A.; Seljeflot, I.; Alehagen, U. Selenium and Coenzyme Q(10) Intervention Prevents Telomere Attrition, with Association to Reduced Cardiovascular Mortality-Sub-Study of a Randomized Clinical Trial. Nutrients 2022, 14, 3346. [Google Scholar] [CrossRef]
- Zhang, D.; Yan, B.; Yu, S.; Zhang, C.; Wang, B.; Wang, Y.; Wang, J.; Yuan, Z.; Zhang, L.; Pan, J. Coenzyme Q10 inhibits the aging of mesenchymal stem cells induced by D-galactose through Akt/mTOR signaling. Oxid. Med. Cell. Longev. 2015, 2015, 867293. [Google Scholar] [CrossRef]
- Li, X.; Zhan, J.; Hou, Y.; Hou, Y.; Chen, S.; Luo, D.; Luan, J.; Wang, L.; Lin, D. Coenzyme Q10 Regulation of Apoptosis and Oxidative Stress in H2O2 Induced BMSC Death by Modulating the Nrf-2/NQO-1 Signaling Pathway and Its Application in a Model of Spinal Cord Injury. Oxid. Med. Cell. Longev. 2019, 2019, 6493081. [Google Scholar] [CrossRef]
- Li, Z.; Zhao, T.; Ding, J.; Gu, H.; Wang, Q.; Wang, Y.; Zhang, D.; Gao, C. A reactive oxygen species-responsive hydrogel encapsulated with bone marrow derived stem cells promotes repair and regeneration of spinal cord injury. Bioact. Mater. 2023, 19, 550–568. [Google Scholar] [CrossRef]
- Li, T.; Li, X.; Han, G.; Liang, M.; Yang, Z.; Zhang, C.; Huang, S.; Tai, S.; Yu, S. The Therapeutic Potential and Clinical Significance of Exosomes as Carriers of Drug Delivery System. Pharmaceutics 2022, 15, 21. [Google Scholar] [CrossRef]
- Saka, O.M.; Dora, D.D.; Kibar, G.; Tevlek, A. Expanding the role of exosomes in drug, biomolecule, and nanoparticle delivery. Life Sci. 2025, 368, 123499. [Google Scholar] [CrossRef]
- Sheykhhasan, M.; Amini, R.; Soleimani Asl, S.; Saidijam, M.; Hashemi, S.M.; Najafi, R. Neuroprotective effects of coenzyme Q10-loaded exosomes obtained from adipose-derived stem cells in a rat model of Alzheimer’s disease. Biomed. Pharmacother. 2022, 152, 113224. [Google Scholar] [CrossRef]
- Sun, J.; Yang, F.; Wang, L.; Yu, H.; Yang, Z.; Wei, J.; Vasilev, K.; Zhang, X.; Liu, X.; Zhao, Y. Delivery of coenzyme Q10 loaded micelle targets mitochondrial ROS and enhances efficiency of mesenchymal stem cell therapy in intervertebral disc degeneration. Bioact. Mater. 2023, 23, 247–260, Erratum in Bioact. Mater. 2023, 24, 171–173. [Google Scholar] [CrossRef] [PubMed]
- Maruo, Y.; Shiraishi, M.; Hibino, M.; Abe, J.; Takeda, A.; Yamada, Y. Activation of Mitochondria in Mesenchymal Stem Cells by Mitochondrial Delivery of Coenzyme Q(10). Biol. Pharm. Bull. 2024, 47, 1415–1421. [Google Scholar] [CrossRef]
- Li, X.; Wang, X.; Zhang, C.; Wang, J.; Wang, S.; Hu, L. Dysfunction of metabolic activity of bone marrow mesenchymal stem cells in aged mice. Cell Prolif. 2022, 55, e13191. [Google Scholar] [CrossRef]
- Park, J.; Park, H.H.; Choi, H.; Kim, Y.S.; Yu, H.J.; Lee, K.Y.; Lee, Y.J.; Kim, S.H.; Koh, S.H. Coenzyme Q10 protects neural stem cells against hypoxia by enhancing survival signals. Brain Res. 2012, 1478, 64–73. [Google Scholar] [CrossRef]
- Choi, H.; Park, H.H.; Lee, K.Y.; Choi, N.Y.; Yu, H.J.; Lee, Y.J.; Park, J.; Huh, Y.M.; Lee, S.H.; Koh, S.H. Coenzyme Q10 restores amyloid beta-inhibited proliferation of neural stem cells by activating the PI3K pathway. Stem Cells Dev. 2013, 22, 2112–2120. [Google Scholar] [CrossRef]
- Lee, H.J.; Park, M.J.; Joo, B.S.; Joo, J.K.; Kim, Y.H.; Yang, S.W.; Kim, C.W.; Kim, K.H. Effects of coenzyme Q10 on ovarian surface epithelium-derived ovarian stem cells and ovarian function in a 4-vinylcyclohexene diepoxide-induced murine model of ovarian failure. Reprod. Biol. Endocrinol. 2021, 19, 59. [Google Scholar] [CrossRef]
- Velichkovska, M.; Surnar, B.; Nair, M.; Dhar, S.; Toborek, M. Targeted Mitochondrial COQ(10) Delivery Attenuates Antiretroviral-Drug-Induced Senescence of Neural Progenitor Cells. Mol. Pharm. 2019, 16, 724–736. [Google Scholar] [CrossRef]
- Liu, H.; Liu, S.; Jiang, J.; Zhang, Y.; Luo, Y.; Zhao, J.; Xu, J.; Xie, Y.; Liao, W.; Wang, W.; et al. CoQ10 enhances the efficacy of airway basal stem cell transplantation on bleomycin-induced idiopathic pulmonary fibrosis in mice. Respir. Res. 2022, 23, 39. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Pérez, O.R.; Juárez-Navarro, K.J.; Diaz, N.F.; Padilla-Camberos, E.; Beltran-Garcia, M.J.; Cardenas-Castrejon, D.; Corona-Perez, H.; Hernández-Jiménez, C.; Díaz-Martínez, N.E. Biomolecules resveratrol + coenzyme Q10 recover the cell state of human mesenchymal stem cells after 1-methyl-4-phenylpyridinium-induced damage and improve proliferation and neural differentiation. Front. Neurosci. 2022, 16, 929590. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Wang, X.; Ouyang, L.; Chen, W.; Zhang, L.; Cao, Y. Antioxidants Improve the Proliferation and Efficacy of hUC-MSCs against H2O2-Induced Senescence. Antioxidants 2023, 12, 1334. [Google Scholar] [CrossRef] [PubMed]
| Study Refs. | Models | Outcomes |
|---|---|---|
| Park et al. (2012) [193] | Neural stem cells (rat) | Improved cell viability and intracellular signaling proteins during hypoxia-reperfusion |
| Choi et al. (2013) [194] | Neural stem cells (mouse) | CoQ10 restored amyloid beta-inhibited proliferation by activating the PI3K pathway |
| Zhang et al. (2015) [184] | Mesenchymal stem cells (rat) | Inhibition of oxidative stress and cell aging induced by D-galactose |
| Lee et al. (2021) [195] | Ovarian stem cells (mouse) | Improved stem cell function in vinylcyclohexene-diepoxide induced model of ovarian failure |
| Velichkovska et al. (2019) [196] | Neural progenitor cells (mouse) | Mitochondrial dysfunction induced by anti-retroviral drugs (tenofovir and emtricitabine) improved |
| Liu et al. (2022) [197] | Airway basal stem cells (human) | Reduced oxidative stress induced by hydrogen peroxide; improved efficiency of transplanted cells in bleomycin-induced model of pulmonary fibrosis |
| Sun et al. (2023) [190] | Mesenchymal stem cells (rat) | Improved efficiency of transplanted cells in rat model of intervertebral disk degeneration |
| Hernández-Perez et al. (2022) [198] | Mesenchymal stem cells (human) | Reduced oxidative stress, improved cell viability and proliferation following exposure to MPP+ |
| Zheng et al. (2023) [199] | Umbilical cord mesenchymal stem cells (human) | Reduced oxidative stress induced by hydrogen peroxide, cell senescence reduced and proliferation capacity improved |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mantle, D.; Domingo, J.C.; Golomb, B.A.; Castro-Marrero, J. Gulf War Illness, Fibromyalgia, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Long COVID Overlap in Common Symptoms and Underlying Biological Mechanisms: Implications for Future Therapeutic Strategies. Int. J. Mol. Sci. 2025, 26, 9044. https://doi.org/10.3390/ijms26189044
Mantle D, Domingo JC, Golomb BA, Castro-Marrero J. Gulf War Illness, Fibromyalgia, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Long COVID Overlap in Common Symptoms and Underlying Biological Mechanisms: Implications for Future Therapeutic Strategies. International Journal of Molecular Sciences. 2025; 26(18):9044. https://doi.org/10.3390/ijms26189044
Chicago/Turabian StyleMantle, David, Joan Carles Domingo, Beatrice Alexandra Golomb, and Jesús Castro-Marrero. 2025. "Gulf War Illness, Fibromyalgia, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Long COVID Overlap in Common Symptoms and Underlying Biological Mechanisms: Implications for Future Therapeutic Strategies" International Journal of Molecular Sciences 26, no. 18: 9044. https://doi.org/10.3390/ijms26189044
APA StyleMantle, D., Domingo, J. C., Golomb, B. A., & Castro-Marrero, J. (2025). Gulf War Illness, Fibromyalgia, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Long COVID Overlap in Common Symptoms and Underlying Biological Mechanisms: Implications for Future Therapeutic Strategies. International Journal of Molecular Sciences, 26(18), 9044. https://doi.org/10.3390/ijms26189044








