Strategies of Classical Swine Fever Immune Evasion
Abstract
1. Introduction
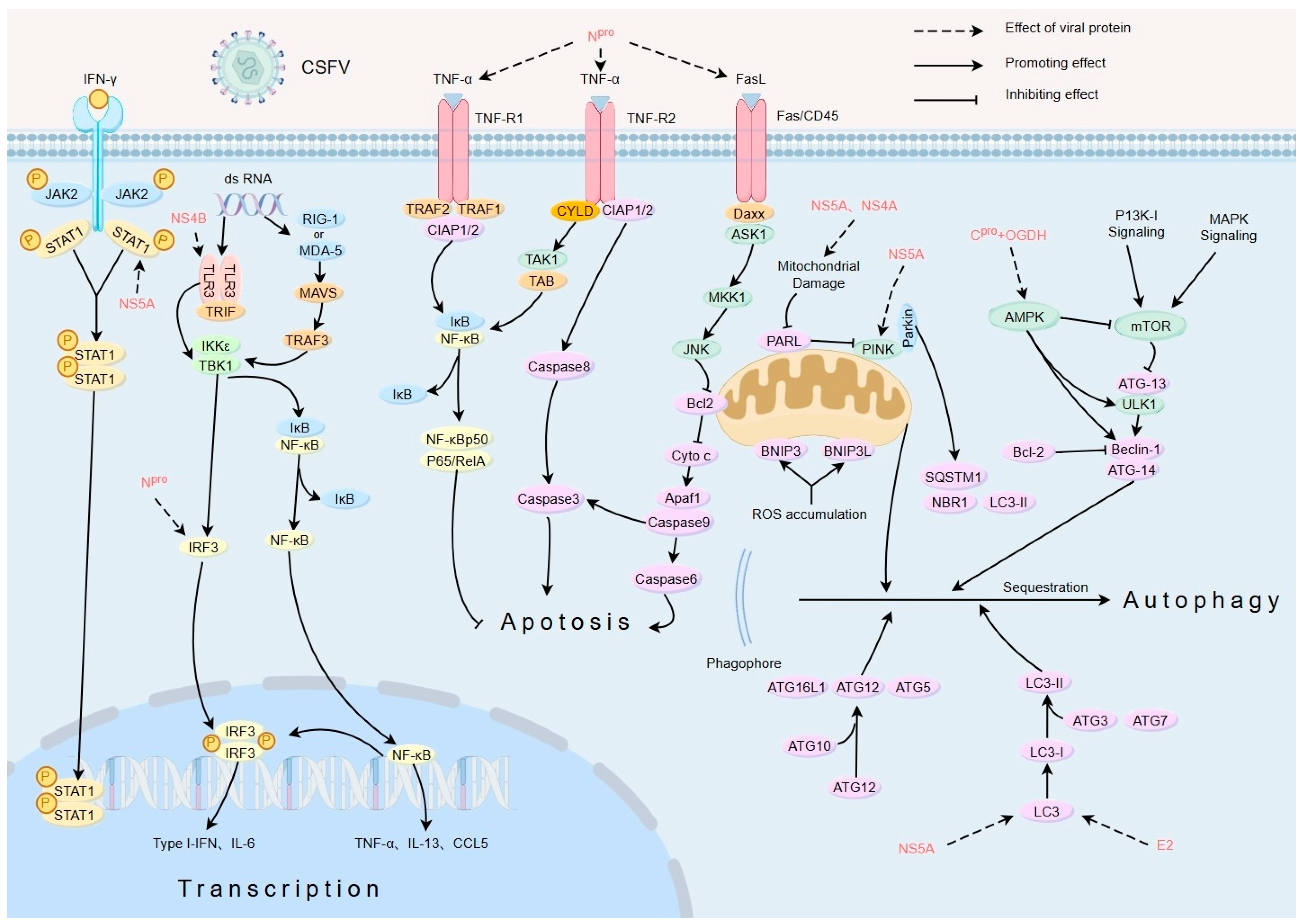
2. Regulation of Innate Immune Response
2.1. Suppressing Interferons (IFNs)
2.2. Blocking the Signalling Pathways Affected by PRRs
2.3. Regulating Interleukin (IL)
3. Regulation of Adaptive Immune Response
3.1. Suppressing Antigen Presentation
3.2. Suppressing T-Cell Immune Responses
3.3. Suppressing B-Cell Immune Responses
4. Regulation of Apoptosis
4.1. CSFV Infection Induces Apoptosis in Target Cells
4.2. CSFV Indirectly Induces Apoptosis
5. Regulation of Autophagy
6. Conclusions and Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Van Oirschot, J.T. Classical swine fever (hog cholera). In Disease of Swine, 8th ed.; Straw, B.E., D’Allaire, S., Mengeling, W.L., Taylor, D.J., Eds.; A Blackwell Publishing Company: Hoboken, NJ, USA; Iowa State University Press: Ames, IA, USA, 1999; pp. 159–172. [Google Scholar]
- Shope, R.E. The swine lungworm as a reservoir and intermediate host for hog cholera virus I. The provocation of masked hog cholera virus in lungworm-infested swine by ascaris larvae. J. Exp. Med. 1958, 107, 609–622. [Google Scholar] [CrossRef] [PubMed]
- WOAH. Infection with classical swine Fever virus. In Terrestrial Animal Health Code, 28th ed.; WOAH: Paris, France, 2023; Chapter 15.2. [Google Scholar]
- Ganges, L.; Crooke, H.R.; Bohórquez, J.A.; Postel, A.; Sakoda, Y.; Becher, P.; Ruggli, N. Classical swine fever virus: The past, present and future. Virus Res. 2020, 289, 198151. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, P.; Adams, M.J.; Benkő, M.; Breitbart, M.; Brister, J.R.; Carstens, E.B.; Davison, A.J.; Delwart, E.; Gorbalenya, A.E.; Harrach, B.; et al. Consensus statement: Virus taxonomy in the age of metagenomics. Nat. Rev. Microbiol. 2017, 15, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Summerfield, A.; Knoetig, S.M.; Tschudin, R.; McCullough, K.C. Pathogenesis of granulocytopenia and bone marrow atrophy during classical swine fever involves apoptosis and necrosis of uninfected cells. Virology 2000, 272, 50–60. [Google Scholar] [CrossRef]
- Sánchez-Cordón, P.J.; Núñez, A.; Salguero, F.J.; Pedrera, M.; Fernández de Marco, M.; Gómez-Villamandos, J.C. Lymphocyte apoptosis and thrombocytopenia in spleen during classical swine fever: Role of macrophages and cytokines. Vet. Pathol. 2005, 42, 477–488. [Google Scholar] [CrossRef]
- Borca, M.V.; Gudmundsdottir, I.; Fernández-Sainz, I.J.; Holinka, L.G.; Risatti, G.R. Patterns of cellular gene expression in swine macrophages infected with highly virulent classical swine fever virus strain Brescia. Virus Res. 2008, 138, 89–96. [Google Scholar] [CrossRef]
- La Rocca, S.A.; Herbert, R.J.; Crooke, H.; Drew, T.W.; Wileman, T.E.; Powell, P.P. Loss of interferon regulatory factor 3 in cells infected with classical swine fever virus involves the N-terminal protease, Npro. J. Virol. 2005, 79, 7239–7247. [Google Scholar] [CrossRef]
- Fiebach, A.R.; Guzylack-Piriou, L.; Python, S.; Summerfield, A.; Ruggli, N. Classical swine fever virus Npro limits type I interferon induction in plasmacytoid dendritic cells by interacting with interferon regulatory factor 7. J. Virol. 2011, 85, 8002–8011. [Google Scholar] [CrossRef]
- Hausmann, Y.; Roman-Sosa, G.; Thiel, H.J.; Rümenapf, T. Classical swine fever virus glycoprotein Erns is an endoribonuclease with an unusual base specificity. J. Virol. 2004, 78, 5507–5512. [Google Scholar] [CrossRef]
- Python, S.; Gerber, M.; Suter, R.; Ruggli, N.; Summerfield, A. Correction: Efficient Sensing of Infected Cells in Absence of Virus Particles by Plasmacytoid Dendritic Cells Is Blocked by the Viral Ribonuclease Erns. PLoS Pathog. 2013, 9, e1003412. [Google Scholar] [CrossRef]
- Spink, C.F.; Gray, L.C.; Davies, F.E.; Morgan, G.J.; Bidwell, J.L. Haplotypic structure across the I kappa B alpha gene (NFKBIA) and association with multiple myeloma. Cancer Lett. 2007, 246, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Doceul, V.; Charleston, B.; Crooke, H.; Reid, E.; Powell, P.P.; Seago, J. The Npro product of classical swine fever virus interacts with IkappaBalpha, the NF-kappaB inhibitor. J. Gen. Virol. 2008, 89 Pt 8, 1881–1889. [Google Scholar] [CrossRef]
- Li, C.; Wang, Y.; Zheng, H.; Dong, W.; Lv, H.; Lin, J.; Guo, K.; Zhang, Y. Antiviral activity of ISG15 against classical swine fever virus replication in porcine alveolar macrophages via inhibition of autophagy by ISGylating BECN1. Vet. Res. 2020, 51, 22. [Google Scholar] [CrossRef]
- Dong, X.Y.; Tang, S.Q. Erratum to: Classical swine fever virus NS5A protein changed inflammatory cytokine secretion in porcine alveolar macrophages by inhibiting the NF-κB signaling pathway. J. Virol. 2016, 13, 135. [Google Scholar] [CrossRef]
- Brubaker, S.W.; Bonham, K.S.; Zanoni, I.; Kagan, J.C. Innate immune pattern recognition: A cell biological perspective. Annu. Rev. Immunol. 2015, 33, 257–290. [Google Scholar] [CrossRef] [PubMed]
- Cao, X. Self-regulation and cross-regulation of pattern-recognition receptor signalling in health and disease. Nat. Rev. Immunol. 2016, 16, 35–50. [Google Scholar] [CrossRef]
- Hüsser, L.; Alves, M.P.; Ruggli, N.; Summerfield, A. Identification of the role of RIG-I, MDA-5 and TLR3 in sensing RNA viruses in porcine epithelial cells using lentivirus-driven RNA interference. Virus Res. 2011, 159, 9–16. [Google Scholar] [CrossRef]
- Cao, Z.; Yang, Q.; Zheng, M.; Lv, H.; Kang, K.; Zhang, Y. Classical swine fever virus non-structural proteins modulate Toll-like receptor signaling pathways in porcine monocyte-derived macrophages. Vet Microbiol. 2019, 230, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Dong, H.; Li, S.; Munir, M.; Chen, J.; Luo, Y.; Sun, Y.; Liu, L.; Qiu, H.J. Hemoglobin subunit beta interacts with the capsid protein and antagonizes the growth of classical swine fever virus. J. Virol. 2013, 87, 5707–5717. [Google Scholar] [CrossRef]
- Li, L.F.; Yu, J.; Zhang, Y.; Yang, Q.; Li, Y.; Zhang, L.; Wang, J.; Li, S.; Luo, Y.; Sun, Y.; et al. Interferon-Inducible Oligoadenylate Synthetase-Like Protein Acts as an Antiviral Effector against Classical Swine Fever Virus via the MDA5-Mediated Type I Interferon-Signaling Pathway. J. Virol. 2017, 91, e01514-16. [Google Scholar] [CrossRef]
- Li, W.; Zhang, Z.; Zhang, L.; Li, H.; Fan, S.; Zhu, E.; Fan, J.; Li, Z.; Chen, W.; Yi, L.; et al. Antiviral Role of Serine Incorporator 5 (SERINC5) Proteins in Classical Swine Fever Virus Infection. Front. Microbiol. 2020, 11, 580233. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.Y.; Liu, W.J.; Zhao, M.Q.; Wang, J.Y.; Pei, J.J.; Luo, Y.W.; Ju, C.M.; Chen, J.D. Correction: Classical swine fever virus triggers RIG-I and MDA5-dependent signaling pathway to IRF-3 and NF-κB activation to promote secretion of interferon and inflammatory cytokines in porcine alveolar macrophages. J. Virol. 2024, 21, 137. [Google Scholar] [CrossRef]
- Zaffuto, K.M.; Piccone, M.E.; Burrage, T.G.; Balinsky, C.A.; Risatti, G.R.; Borca, M.V.; Holinka, L.G.; Rock, D.L.; Afonso, C.L. Classical swine fever virus inhibits nitric oxide production in infected macrophages. J. Gen. Virol. 2007, 88 Pt 11, 3007–3012. [Google Scholar] [CrossRef]
- Sánchez-Cordón, P.J.; Romanini, S.; Salguero, F.J.; Núñez, A.; Bautista, M.J.; Jover, A.; Gómez-Villamos, J.C. Apoptosis of thymocytes related to cytokine expression in experimental classical swine fever. J. Comp. Pathol. 2002, 127, 239–248. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Liang, W.; Kang, K.; Li, H.; Cao, Z.; Zhang, Y. Classical swine fever virus and p7 protein induce secretion of IL-1β in macrophages. J. Gen. Virol. 2014, 95 Pt 12, 2693–2699. [Google Scholar] [CrossRef]
- Fan, S.; Yuan, J.; Deng, S.; Chen, Y.; Xie, B.; Wu, K.; Zhu, M.; Xu, H.; Huang, Y.; Yang, J.; et al. Activation of Interleukin-1β Release by the Classical Swine Fever Virus Is Dependent on the NLRP3 Inflammasome, Which Affects Virus Growth in Monocytes. Front. Cell Infect. Microbiol. 2018, 8, 225. [Google Scholar] [CrossRef] [PubMed]
- Zhao, F.; Huang, Y.; Ji, J.; Liu, X.; Li, X.; Zou, L.; Wu, K.; Liu, X.D.; Zeng, S.; Wang, X.; et al. IDO1 promotes CSFV replication by mediating tryptophan metabolism to inhibit NF-κB signaling. J. Virol. 2024, 98, e0045824. [Google Scholar] [CrossRef]
- Dong, W.; Jing, H.; Wang, H.; Cao, S.; Sun, Y.; Zhang, Y.; Lv, H. Classical swine fever virus NS4B protein interacts with MAVS and inhibits IL-8 expression in PAMs. Virus Res. 2022, 307, 198622. [Google Scholar] [CrossRef]
- Dong, W.; Lv, H.; Guo, K.; Wang, T.; Ouyang, Y.; Jin, M.; Zhang, Y. Classical Swine Fever Virus Infection and Its NS4A Protein Expression Induce IL-8 Production through MAVS Signaling Pathway in Swine Umbilical Vein Endothelial Cells. Front. Microbiol. 2018, 8, 2687. [Google Scholar] [CrossRef]
- Jamin, A.; Gorin, S.; Cariolet, R.; Le Potier, M.F.; Kuntz-Simon, G. Classical swine fever virus induces activation of plasmacytoid and conventional dendritic cells in tonsil, blood, and spleen of infected pigs. Vet. Res. 2008, 39, 7. [Google Scholar] [CrossRef]
- Renson, P.; Le Dimna, M.; Keranflech, A.; Cariolet, R.; Koenen, F.; Le Potier, M.F. CP7_E2alf oral vaccination confers partial protection against early classical swine fever virus challenge and interferes with pathogeny-related cytokine responses. Vet. Res. 2013, 44, 9. [Google Scholar] [CrossRef]
- Wienhold, D.; Armengol, E.; Marquardt, A.; Marquardt, C.; Voigt, H.; Büttner, M.; Saalmüller, A.; Pfaff, E. Immunomodulatory effect of plasmids co-expressing cytokines in classical swine fever virus subunit gp55/E2-DNA vaccination. Vet. Res. 2005, 36, 571–587. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, G.G.; Liu, L.M. Dendritic cells and Langerhans cells in the uptake of mucosal antigens. Curr. Top Microbiol. Immunol. 1999, 236, 33–53. [Google Scholar]
- Deng, S.; Yang, C.; Nie, K.; Fan, S.; Zhu, M.; Zhu, J.; Chen, Y.; Yuan, J.; Zhang, J.; Xu, H.; et al. Host cell protein PSMB10 interacts with viral NS3 protein and inhibits the growth of classical swine fever virus. Virology 2019, 537, 74–83. [Google Scholar] [CrossRef]
- Armengol, E.; Wiesmüller, K.H.; Wienhold, D.; Büttner, M.; Pfaff, E.; Jung, G.; Saalmüller, A. Identification of T-cell epitopes in the structural and non-structural proteins of classical swine fever virus. J. Gen. Virol. 2002, 83 Pt 3, 551–560. [Google Scholar] [CrossRef]
- Fan, Y.H.; Lin, Y.L.; Hwang, Y.C.; Yang, H.C.; Chiu, H.C.; Chiou, S.H.; Jong, M.H.; Chow, K.C.; Lin, C.C. T-cell factor-4 and MHC upregulation in pigs receiving a live attenuated classical swine fever virus (CSFV) vaccine strain with interferon-gamma adjuvant. Vet. J. 2016, 216, 148–156. [Google Scholar] [CrossRef]
- Chen, L.J.; Dong, X.Y.; Shen, H.Y.; Zhao, M.Q.; Ju, C.M.; Yi, L.; Zhang, X.T.; Kang, Y.M.; Chen, J.D. Classical swine fever virus suppresses maturation and modulates functions of monocyte-derived dendritic cells without activating nuclear factor kappa B. Res. Vet. Sci. 2012, 93, 529–537. [Google Scholar] [CrossRef]
- Ferry, J.A.; Hill, B.; Hsi, E.D. Correction: Mature B, T and NK-cell, plasma cell and histiocytic/dendritic cell neoplasms: Classification according to the World Health Organization and International Consensus Classification. Hematol. Oncol. J. 2024, 17, 75. [Google Scholar] [CrossRef]
- Masopust, D.; Schenkel, J.M. The integration of T cell migration, differentiation and function. Nat. Rev. Immunol. 2013, 13, 309–320. [Google Scholar] [CrossRef]
- Markowska-Daniel, I.; Pejsak, Z.; Winnicka, A.; Collins, R.A. Phenotypic analysis of peripheral leukocytes in piglets infected with classical swine fever virus. Res. Vet. Sci. 1999, 67, 53–57. [Google Scholar] [CrossRef]
- Piriou, L.; Chevallier, S.; Hutet, E.; Charley, B.; Le Potier, M.F.; Albina, E. Humoral and cell-mediated immune responses of d/d histocompatible pigs against classical swine fever (CSF) virus. Vet. Res. 2003, 34, 389–404. [Google Scholar] [CrossRef] [PubMed]
- Suradhat, S.; Sada, W.; Buranapraditkun, S.; Damrongwatanapokin, S. The kinetics of cytokine production and CD25 expression by porcine lymphocyte subpopulations following exposure to classical swine fever virus (CSFV). Vet. Immunol. Immunopathol. 2005, 106, 197–208. [Google Scholar] [CrossRef]
- Soldevila, F.; Edwards, J.C.; Graham, S.P.; Crooke, H.R.; Werling, D.; Steinbach, F. Activation of Dendritic Cells in Tonsils Is Associated with CD8 T Cell Responses following Vaccination with Live Attenuated Classical Swine Fever Virus. Int. J. Mol. Sci. 2021, 22, 8795. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Wang, X.; Yuan, M.; Zhang, X.; Yang, X.; Guan, X.; Li, S.; Ma, J.; Qiu, H.J.; Li, Y. Identification of two novel T cell epitopes on the E2 protein of classical swine fever virus C-strain. Vet. Microbiol. 2023, 284, 109814. [Google Scholar] [CrossRef]
- Tarradas, J.; de la Torre, M.E.; Rosell, R.; Perez, L.J.; Pujols, J.; Muñoz, M.; Muñoz, I.; Muñoz, S.; Abad, X.; Domingo, M.; et al. The impact of CSFV on the immune response to control infection. Virus Res. 2014, 185, 82–91. [Google Scholar] [CrossRef]
- Hulst, M.; Loeffen, W.; Weesendorp, E. Pathway analysis in blood cells of pigs infected with classical swine fever virus: Comparison of pigs that develop a chronic form of infection or recover. Arch. Virol. 2013, 158, 325–339. [Google Scholar] [CrossRef]
- Lee, W.C.; Wang, C.S.; Chien, M.S. Virus antigen expression and alterations in peripheral blood mononuclear cell subpopulations after classical swine fever virus infection. Vet. Microbiol. 1999, 67, 17–29. [Google Scholar] [CrossRef]
- Summerfield, A.; McNeilly, F.; Walker, I.; Allan, G.; Knoetig, S.M.; McCullough, K.C. Depletion of CD4(+) and CD8(high+) T-cells before the onset of viraemia during classical swine fever. Vet. Immunol. Immunopathol. 2001, 78, 3–19. [Google Scholar] [CrossRef]
- Obeng, E. Apoptosis (programmed cell death) and its signals—A review. Braz. J. Biol. 2021, 81, 1133–1143. [Google Scholar] [CrossRef]
- Ruggli, N.; Tratschin, J.D.; Schweizer, M.; McCullough, K.C.; Hofmann, M.A.; Summerfield, A. Classical swine fever virus interferes with cellular antiviral defense: Evidence for a novel function of Npro. J. Virol. 2003, 77, 7645–7654. [Google Scholar] [CrossRef]
- Bensaude, E.; Turner, J.L.E.; Wakeley, P.R.; Sweetman, D.A.; Pardieu, C.; Drew, T.W.; Wileman, T.; Powell, P.P. Classical swine fever virus induces proinflammatory cytokines and tissue factor expression and inhibits apoptosis and interferon synthesis during the establishment of long-term infection of porcine vascular endothelial cells. J. Gen. Virol. 2004, 85 Pt 4, 1029–1037. [Google Scholar] [CrossRef] [PubMed]
- Dastoor, Z.; Dreyer, J.L. Potential role of nuclear translocation of glyceraldehyde-3-phosphate dehydrogenase in apoptosis and oxidative stress. J. Cell Sci. 2001, 114 Pt 9, 1643–1653. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Jiang, Y.; Shi, Z.; Yan, Y.; Guo, H.; He, F.; Tu, C. Proteomic alteration of PK-15 cells after infection by classical swine fever virus. J. Proteome Res. 2008, 7, 5263–5269. [Google Scholar] [CrossRef]
- Suradhat, S.; Thanawongnuwech, R.; Poovorawan, Y. Upregulation of IL-10 gene expression in porcine peripheral blood mononuclear cells by porcine reproductive and respiratory syndrome virus. J. Gen. Virol. 2003, 84 Pt 2, 453–459. [Google Scholar] [CrossRef]
- Summerfield, A.; Zingle, K.; Inumaru, S.; McCullough, K.C. Induction of apoptosis in bone marrow neutrophil-lineage cells by classical swine fever virus. J. Gen. Virol. 2001, 82 Pt 6, 1309–1318. [Google Scholar] [CrossRef]
- Renson, P.; Blanchard, Y.; Le Dimna, M.; Felix, H.; Cariolet, R.; Jestin, A.; Le Potier, M.F. Acute induction of cell death-related IFN stimulated genes (ISG) differentiates highly from moderately virulent CSFV strains. Vet. Res. 2010, 41, 7. [Google Scholar] [CrossRef]
- Nielsen, J.; Lohse, L.; Rasmussen, T.B.; Uttenthal, A. Classical swine fever in 6- and 11-week-old pigs: Haematological and immunological parameters are modulated in pigs with mild clinical disease. Vet. Immunol. Immunopathol. 2010, 138, 159–173. [Google Scholar] [CrossRef]
- Hardy, S.; Jackson, B.; Goodbourn, S.; Seago, J. Classical swine fever virus Npro antagonises IRF3 to prevent IFN-independent TLR3 and RIG-I-mediated apoptosis. J. Virol. 2020, 95, e01136-20. [Google Scholar] [PubMed]
- Xie, J.; Guo, H.; Gong, W.; Jiang, D.; Zhang, L.; Jia, J.; Tu, C. Identification of cleavage of NS5A of C-strain classical swine fever virus. Arch. Virol. 2017, 162, 391–400. [Google Scholar] [CrossRef]
- He, L.; Zhang, Y.; Fang, Y.; Liang, W.; Lin, J.; Cheng, M. Classical swine fever virus induces oxidative stress in swine umbilical vein endothelial cells. BMC Vet. Res. 2014, 10, 279. [Google Scholar] [CrossRef]
- Qian, G.; Lv, H.; Lin, J.; Li, X.; Lv, Q.; Wang, T.; Zhang, J.; Dong, W.; Guo, K.; Zhang, Y. FHC, an NS4B-interacting Protein, Enhances Classical Swine Fever Virus Propagation and Acts Positively in Viral Anti-apoptosis. Sci. Rep. 2018, 8, 8318. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Shi, Z.; Guo, H.; Tu, C. Changes in the porcine peripheral blood mononuclear cell proteome induced by infection with highly virulent classical swine fever virus. J. Gen. Virol. 2010, 91 Pt 9, 2254–2262. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.X.; Sun, J.F.; Guo, H.C.; Tu, C.C. Expression profiles of apoptotic genes of pig peripheral blood leukocytes caused by classical swine fever virus infection. Bing Du Xue Bao 2008, 24, 456–463. (In Chinese) [Google Scholar] [PubMed]
- Galluzzi, L.; Vitale, I.; Aaronson, S.A.; Abrams, J.M.; Adam, D.; Agostinis, P.; Alnemri, E.S.; Altucci, L.; Amelio, I.; Andrews, D.W.; et al. Molecular mechanisms of cell death: Recommendations of the Nomenclature Committee on Cell Death 2018. Cell Death Differ. 2018, 25, 486–541. [Google Scholar]
- Wang, B.; Pareek, G.; Kundu, M. ULK/Atg1: Phasing in and out of autophagy. Trends Biochem. Sci. 2024, 49, 494–505. [Google Scholar] [CrossRef]
- Jewell, J.L.; Russell, R.C.; Guan, K.L. Amino acid signalling upstream of mTOR. Nat. Rev. Mol. Cell Biol. 2013, 14, 133–139. [Google Scholar] [CrossRef]
- Pei, J.; Zhao, M.; Ye, Z.; Gou, H.; Wang, J.; Yi, L.; Dong, X.; Liu, W.; Luo, Y.; Liao, M.; et al. Autophagy enhances the replication of classical swine fever virus in vitro. Autophagy 2014, 10, 93–110. [Google Scholar] [CrossRef]
- Pei, J.; Deng, J.; Ye, Z.; Wang, J.; Gou, H.; Liu, W.; Zhao, M.; Liao, M.; Yi, L.; Chen, J. Absence of autophagy promotes apoptosis by modulating the ROS-dependent RLR signaling pathway in classical swine fever virus-infected cells. Autophagy 2016, 12, 1738–1758. [Google Scholar] [CrossRef]
- Gou, H.; Zhao, M.; Xu, H.; Wang, J.; Gou, H.; Liu, W.; Zhao, M.; Liao, M.; Yi, L.; Chen, J. CSFV induced mitochondrial fission and mitophagy to inhibit apoptosis. Oncotarget 2017, 8, 39382–39400. [Google Scholar] [CrossRef]
- Luo, Q.; Zhang, L.; Wei, F.; Fang, Q.; Bao, F.; Mi, S.; Li, N.; Wang, C.; Liu, Y.; Tu, C. mTORC1 Negatively Regulates the Replication of Classical Swine Fever Virus Through Autophagy and IRES-Dependent Translation. Science 2018, 3, 87–101. [Google Scholar] [CrossRef]
- Li, W.; Zhang, Z.; Zhang, L.; Zhou, Q.; Li, Y.; Yi, L.; Ding, H.; Zhao, M.; Chen, J.; Fan, S. Interaction of SERINC5 and IFITM1/2/3 regulates the autophagy-apoptosis-immune network under CSFV infection. Virulence 2022, 13, 1720–1740. [Google Scholar] [CrossRef] [PubMed]
- Zhu, E.; Wu, H.; Chen, W.; Zhou, Q.; Li, Y.; Yi, L.; Ding, H.; Zhao, M.; Chen, J.; Fan, S. Classical swine fever virus employs the PERK- and IRE1-dependent autophagy for viral replication in cultured cells. Virulence 2021, 12, 130–149. [Google Scholar] [CrossRef]
- Xie, B.; Zhao, M.; Song, D.; Wu, K.; Yi, L.; Li, W.; Li, X.; Wang, K.; Chen, J. Induction of autophagy and suppression of type I IFN secretion by CSFV. Autophagy 2021, 17, 925–947. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Zhang, L.; Liang, W.; Liu, S.; Deng, W.; Liu, Y.; Liu, Y.; Song, M.; Guo, K.; Zhang, Y. Extracellular vesicles originating from autophagy mediate an antibody-resistant spread of classical swine fever virus in cell culture. Autophagy 2022, 18, 1433–1449. [Google Scholar] [CrossRef] [PubMed]
- Fan, S.; Wu, K.; Luo, C.; Liu, S.; Deng, W.; Liu, Y.; Liu, Y.; Song, M.; Guo, K.; Zhang, Y. Dual NDP52 Function in Persistent CSFV Infection. Front. Microbiol. 2020, 10, 2962. [Google Scholar] [CrossRef]
- Fan, S.; Wu, K.; Zhao, M.; Yuan, J.; Ma, S.; Zhu, E.; Chen, Y.; Ding, H.; Yi, L.; Chen, J. LDHB inhibition induces mitophagy and facilitates the progression of CSFV infection. Autophagy 2021, 17, 2305–2324. [Google Scholar] [CrossRef]
- Zeng, S.; Zhu, W.; Luo, Z.; Wu, K.; Lu, Z.; Li, X.; Wang, W.; Hu, W.; Qin, Y.; Chen, W.; et al. Role of OGDH in Atophagy-IRF3-IFN-β pathway during classical swine fever virus infection. Int. J. Biol. Macromol. 2023, 249, 126443. [Google Scholar] [CrossRef]
- Li, X.; Song, Y.; Wang, X.; Fu, C.; Zhao, F.; Zou, L.; Wu, K.; Chen, W.; Li, Z.; Fan, J.; et al. The regulation of cell homeostasis and antiviral innate immunity by autophagy during classical swine fever virus infection. Emerg. Microbes Infect. 2023, 12, 2164217. [Google Scholar] [CrossRef]
- Liu, X.; Yan, Q.; Liu, X.; Wei, W.; Zou, L.; Zhao, F.; Zeng, S.; Yi, L.; Ding, H.; Zhao, M.; et al. PKM2 induces mitophagy through the AMPK-mTOR pathway promoting CSFV proliferation. J. Virol. 2024, 98, e0175123. [Google Scholar] [CrossRef]
- Zhang, C.; Wang, X.; Sun, J.; Guo, M.; Zhang, X.; Wu, Y. Autophagy Induced by the N-Terminus of the Classic Swine Fever Virus Nonstructural Protein 5A Protein Promotes Viral Replication. Front. Microbiol. 2021, 12, 733385. [Google Scholar] [CrossRef]
- Zhang, C.; Wu, X.; Sun, J.; Guo, M.; Zhang, X.; Wu, Y. Mitophagy induced by classical swine fever virus nonstructural protein 5A promotes viral replication. Virus Res. 2022, 320, 198886. [Google Scholar]
- Sun, J.; Yu, H.; Wang, Y.; Li, L.; Zhu, J.; Ma, P.; Feng, Z.; Tu, C. Classical swine fever virus NS5A protein activates autophagy via the PP2A-DAPK3-Beclin 1 axis. J. Virol. 2023, 97, e0098823. [Google Scholar] [CrossRef]
- Lv, H.; Peng, Z.; Jia, B.; Jing, H.; Cao, S.; Xu, Z.; Dong, W. Transcriptome analysis of PK-15 cells expressing CSFV NS4A. BMC Vet. Res. 2022, 18, 434. [Google Scholar] [CrossRef]
- Wu, K.; Li, B.; Zhang, X.; Fang, Y.; Zeng, S.; Hu, W.; Liu, X.; Liu, X.; Lu, Z.; Li, X.; et al. Correction for Wu et al.; CSFV restricts necroptosis to sustain infection by inducing autophagy/mitophagy-targeted degradation of RIPK3. Microbiol. Spectr. 2024, 12, e0275823. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.M.; Mao, Q.; Yi, L.; Zhao, M.Q.; Chen, J.D. Apoptosis, Autophagy, and Pyroptosis: Immune Escape Strategies for Persistent Infection and Pathogenesis of Classical Swine Fever Virus. Pathogens 2019, 8, 239. [Google Scholar] [CrossRef]
- Zhang, J.; Li, F.; Chen, W.; Li, Y.; Zhang, Z.; Hua, R.; Liu, R.; Zhu, Y.; Sun, E.; Qiu, H.; et al. An attenuated African swine fever virus expressing the E2 glycoprotein of classical swine fever virus protects pigs against challenge of both viruses. Emerg. Microbes Infect. 2025, 14, 2469636. [Google Scholar] [CrossRef]
- Du, F.; Cao, Z.; Ye, Z.; He, J.; Zhang, W.; Zhang, K.; Ning, P. Production and immunogenicity of a deoxyribonucleic acid Alphavirus vaccine expressing classical swine fever virus E2-Erns protein and porcine Circovirus Cap-Rep protein. Front. Microbiol. 2022, 13, 1065532. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.Y.; Liu, K.S.; Zhang, C.; Ni, Z.; Zhu, Y.C.; Bao, H.L.; Chen, L.; Ye, W.C.; Hua, J.G.; Huo, S.X.; et al. Recombinant pseudorabies virus (PRV) expressing stabilized E2 of classical swine fever virus (CSFV) protects against both PRV and CSFV. Antivir. Res. 2023, 211, 105548. [Google Scholar] [CrossRef]
- Mi, S.; Wang, L.; Li, H.; Bao, F.; Madera, R.; Shi, X.; Zhang, L.; Mao, Y.; Yan, R.; Xia, X.; et al. Characterization of monoclonal antibodies that specifically differentiate field isolates from vaccine strains of classical swine fever virus. Front. Immunol. 2022, 13, 930631. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, W.; Cheng, J.; Liu, X.; Miao, S.; Tan, W.S.; Zhao, L. Designing a novel E2-IFN-γ fusion protein against CSFV by immunoinformatics and structural vaccinology approaches. Appl. Microbiol. Biotechnol. 2022, 106, 3611–3623. [Google Scholar] [CrossRef]
- Wang, F.; Hu, M.; Li, N.; Sun, X.; Xing, G.; Zheng, G.; Jin, Q.; Liu, Y.; Cui, C.; Zhang, G. Precise Assembly of Multiple Antigens on Nanoparticles with Specially Designed Affinity Peptides. ACS Appl. Mater. Interfaces 2022, 14, 39843–39857. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.H.; Deng, Z.F.; Lu, Y.; Fang, W.H.; He, F. A modular and self-adjuvanted multivalent vaccine platform based on porcine circovirus virus-like nanoparticles. J. Nanobiotechnol. 2022, 20, 493. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhu, J.; Wang, S.; Li, M.; Sun, X.; Liu, S.; Wang, Y.; Li, R.; Zhang, G. Modular Nano-Antigen Display Platform for Pigs Induces Potent Immune Responses. ACS Nano 2024, 18, 29152–29177. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Li, F.; Liu, Y. Strategies of Classical Swine Fever Immune Evasion. Int. J. Mol. Sci. 2025, 26, 7838. https://doi.org/10.3390/ijms26167838
Zhang Y, Li F, Liu Y. Strategies of Classical Swine Fever Immune Evasion. International Journal of Molecular Sciences. 2025; 26(16):7838. https://doi.org/10.3390/ijms26167838
Chicago/Turabian StyleZhang, Yuanji, Fangtao Li, and Yebing Liu. 2025. "Strategies of Classical Swine Fever Immune Evasion" International Journal of Molecular Sciences 26, no. 16: 7838. https://doi.org/10.3390/ijms26167838
APA StyleZhang, Y., Li, F., & Liu, Y. (2025). Strategies of Classical Swine Fever Immune Evasion. International Journal of Molecular Sciences, 26(16), 7838. https://doi.org/10.3390/ijms26167838






