Effects of Near-Infrared Diode Laser Irradiation on Pain Relief and Neuropeptide Markers During Experimental Tooth Movement in the Periodontal Ligament Tissues of Rats: A Pilot Study
Abstract
1. Introduction
2. Results
2.1. Effects of Diode Laser Irradiation on Nociceptive Behaviors in ETM
2.2. Effects of Diode Laser Irradiation on Temperature
2.3. Immunohistochemical Staining
2.3.1. Substance P Immunohistochemical Staining
2.3.2. CGRP IHC Staining
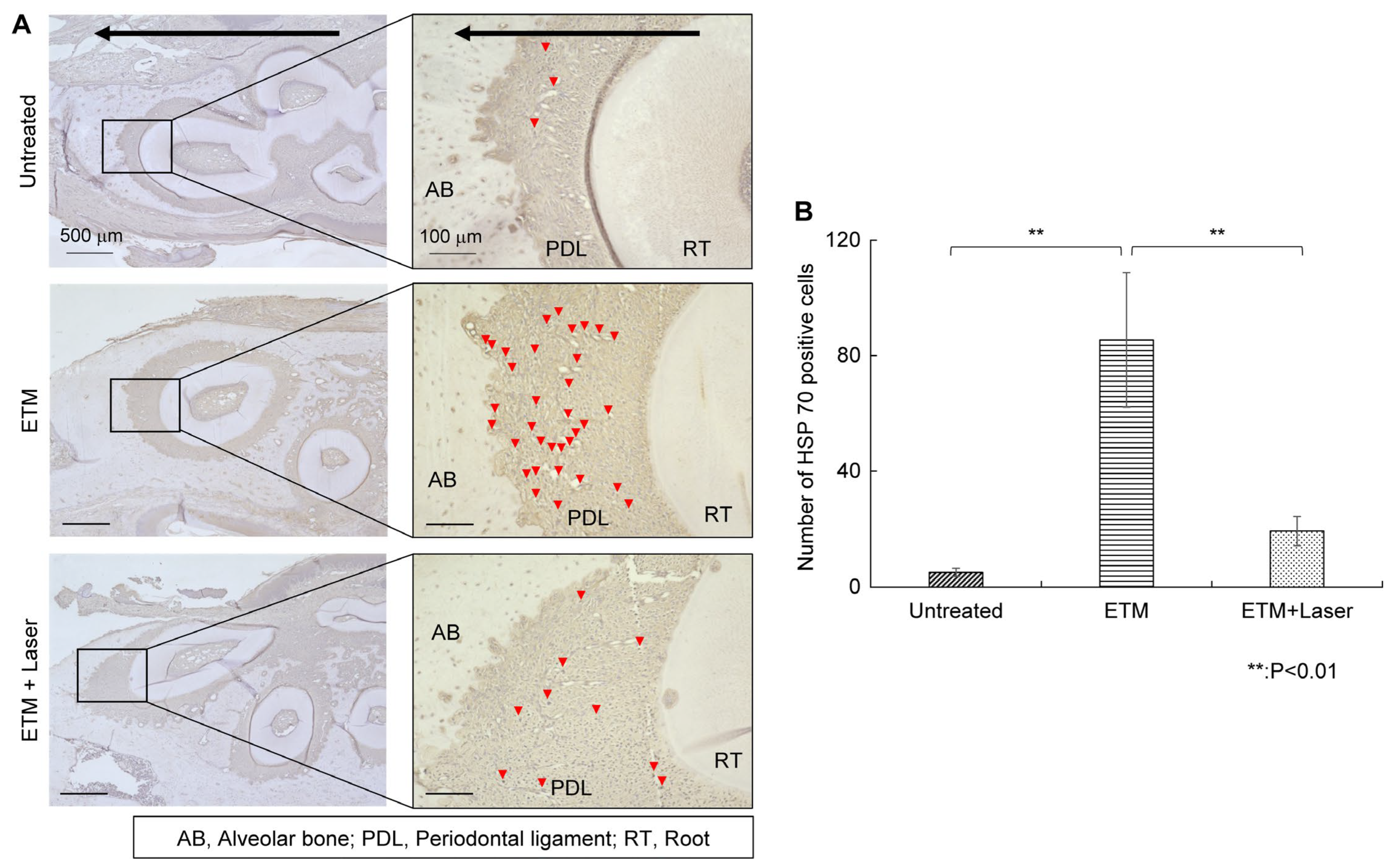
2.3.3. HSP 70 IHC Staining
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. ETM Model of Rats
4.3. Laser Irradiation
4.4. Behavior Testing
4.5. Temperature Measurement
4.6. Examination of Histological Changes
4.7. Immunohistochemical Staining
4.8. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HSP | heat shock protein |
| ETM | experimental tooth movement |
| VCM | vacuous chewing movement |
| IL | interleukin |
| SP | substance P |
| ASIC3 | acid-sensing ion channel 3 |
| TRPV1 | transient receptor potential vanilloid 1 |
| CGRP | calcitonin gene-related peptide |
| TG | trigeminal ganglion |
| SGCs | satellite glial cells |
| TNFα | tumor necrosis factor-α |
| MAPK | mitogen-activated protein kinase |
| NIR | frequency near-infrared |
References
- Long, H.; Wang, Y.; Jian, F.; Liao, L.-N.; Yang, X.; Lai, W.-L. Current advances in orthodontic pain. Int. J. Oral Sci. 2016, 8, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, V. Orthodontic pain: From causes to management—a review. Eur. J. Orthod. 2007, 29, 170–179. [Google Scholar] [CrossRef]
- Kavaliauskiene, A.; Smailiene, D.; Buskiene, I.; Keriene, D. Pain and discomfort perception among patients undergoing orthodontic treatment: Results from one month follow-up study. Stomatologija 2012, 14, 118–125. [Google Scholar]
- Krukemeyer, A.M.; Arruda, A.O.; Rohr Inglehart, M. Pain and Orthodontic Treatment Patient Experiences and Provider Assessments. Angle Orthod. 2009, 79, 1175–1181. [Google Scholar] [CrossRef]
- Wang, S.; Ko, C.C.; Chung, M.K. Nociceptor mechanisms underlying pain and bone remodeling via orthodontic forces: Toward no pain, big gain. Front. Pain Res. 2024, 5, 1365194. [Google Scholar] [CrossRef]
- Johal, A.; Fleming, P.S.; Al Jawad, F.A. A prospective longitudinal controlled assessment of pain experience and oral health-related quality of life in adolescents undergoing fixed appliance treatment. Orthod. Craniofacial Res. 2014, 17, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Chae, H.S.; Park, H.J.; Hwang, H.R.; Kwon, A.; Lim, W.H.; Yi, W.J.; Han, D.H.; Kim, Y.H.; Baek, J.H. The effect of antioxidants on the production of pro-inflammatory cytokines and orthodontic tooth movement. Mol. Cells 2011, 32, 189–196. [Google Scholar] [CrossRef]
- Yong, J.; Elisabeth Groeger, S.; Ruf, S.; Ruiz-Heiland, G. Influence of leptin and compression in GAS-6 mediated homeostasis of periodontal ligament cell. Oral Dis. 2023, 29, 1172–1183. [Google Scholar] [CrossRef] [PubMed]
- Ashizawa, Y.; Sahara, N. Quantitative evaluation of newly formed bone in the alveolar wall surrounding the root during the initial stage of experimental tooth movement in the rat. Arch. Oral Biol. 1998, 43, 473–484. [Google Scholar] [CrossRef]
- Nakatani, A.; Kunimatsu, R.; Tsuka, Y.; Sakata, S.; Horie, K.; Gunji, H.; Ito, S.; Kado, I.; Putranti, N.A.R.; Terayama, R.; et al. Effects of high-frequency near infrared laser irradiation on experimental tooth movement–induced pain in rats. Lasers Med. Sci. 2022, 37, 2697–2706. [Google Scholar] [CrossRef]
- Nakatani, A.; Kunimatsu, R.; Tsuka, Y.; Sakata, S.; Ito, S.; Kado, I.; Putranti, N.A.R.; Terayama, R.; Tanimoto, K. High-frequency near-infrared semiconductor laser irradiation suppressed experimental tooth movement-induced inflammatory pain markers in the periodontal ligament tissues of rats. Lasers Med. Sci. 2023, 38, 109. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Long, H.; Ye, N.; Liao, L.; Yang, X.; Jian, F.; Wang, Y.; Lai, W. The effect of capsaicin on expression patterns of CGRP in trigeminal ganglion and trigeminal nucleus caudalis following experimental tooth movement in rats. J. Appl. Oral Sci. 2016, 24, 597–606. [Google Scholar] [CrossRef]
- Sacerdote, P.; Levrini, L. Peripheral mechanisms of dental pain: The role of substance P. Mediat. Inflamm. 2012, 2012, 951920. [Google Scholar] [CrossRef]
- Long, H.; Liao, L.; Gao, M.; Ma, W.; Zhou, Y.; Jian, F.; Wang, Y.; Lai, W. Periodontal CGRP contributes to orofacial pain following experimental tooth movement in rats. Neuropeptides 2015, 52, 31–37. [Google Scholar] [CrossRef]
- Norevall, L.I.; Forsgren, S.; Matsson, L. Expression of neuropeptides (CGRP, substance P) during and after orthodontic tooth movement in the rat. Eur. J. Orthod. 1995, 17, 311–325. [Google Scholar] [CrossRef] [PubMed]
- Narmada, I.B.; Rubianto, M.; Putra, S.T. The effect of low-level light therapy on orthodontic tooth movement rate, HSP70, MMP-8. Dent. Res. J. 2020, 17, 73–79. [Google Scholar] [CrossRef]
- Ikwegbue, P.C.; Masamba, P.; Oyinloye, B.E.; Kappo, A.P. Roles of heat shock proteins in apoptosis, oxidative stress, human inflammatory diseases, and cancer. Pharmaceuticals 2017, 11, 2. [Google Scholar] [CrossRef] [PubMed]
- Muraoka, R.; Nakano, K.; Kawakami, T. Heat Shock Protein Overexpression-mediated periodontal ligament regeneration: A fundamental approach to generate a potential biomaterial. Materials 2022, 15, 809. [Google Scholar] [CrossRef]
- Morii, A.; Miyamura, Y.; Sago, M.I.; Mizuhara, M.; Shikayama, T.; Naniwa, M.; Hitomi, S.; Ujihara, I.; Kuroishi, K.N.; Gunjigake, K.K.; et al. Orthodontic force-induced oxidative stress in the periodontal tissue and dental pulp elicits nociception via activation/sensitization of TRPA1 on nociceptive fibers. Free. Radic. Biol. Med. 2020, 147, 175–186. [Google Scholar] [CrossRef]
- Yang, Z.; Luo, W.; Hou, J.; Zhao, Z.; Jian, F.; Wamalwa, P.; Lai, W.; Wang, J.; Wang, Y.; Liao, Z. Development of a behavior model of pain induced by experimental tooth movement in rats. Eur. J. Oral Sci. 2009, 117, 380–384. [Google Scholar] [CrossRef]
- Yang, Z.; Cao, Y.; Wang, Y.; Luo, W.; Hua, X.; Lu, Y.; Liao, Z.; Lai, W.; Zhao, Z. Behavioural responses and expression of P2X3 receptor in trigeminal ganglion after experimental tooth movement in rats. Arch. Oral Biol. 2009, 54, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Fu, R.; Tan, Y.; Fang, B.; Yang, Z. Chemokine CCL2 up-regulated in the medullary dorsal horn astrocytes contributes to nocifensive behaviors induced by experimental tooth movement. Eur. J. Oral Sci. 2014, 122, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Qiao, H.; Gao, Y.; Zhang, C.; Zhou, H. Increased expression of TRPV1 in the trigeminal ganglion is involved in orofacial pain during experimental tooth movement in rats. Eur. J. Oral Sci. 2015, 123, 17–23. [Google Scholar] [CrossRef]
- Gao, Y.; Liu, Y.; Zhu, K.; Zhang, Z.; Qiao, H.; Lu, Z.; Zhong, T.; Liu, Y.; Zhou, H. Blocking of TRPV-1 in the parodontium relieves orthodontic pain by inhibiting the expression of TRPV-1 in the trigeminal ganglion during experimental tooth movement in rats. Neurosci. Lett. 2016, 628, 67–72. [Google Scholar] [CrossRef]
- Gao, Y.; Duan, Y.Z. Increased COX2 in the trigeminal nucleus caudalis is involved in orofacial pain induced by experimental tooth movement. Anat. Rec. 2010, 293, 485–491. [Google Scholar] [CrossRef]
- Noda, K.; Nakamura, Y.; Kogure, K.; Nomura, Y. Morphological changes in the rat periodontal ligament and its vascularity after experimental tooth movement using superelastic forces. Eur. J. Orthod. 2009, 31, 37–45. [Google Scholar] [CrossRef]
- Bowen, E.J.; Schmidt, T.W.; Firm, C.S.; Russo, A.F.; Durham, P.L. Tumor Necrosis Factor-α Stimulation of Calcitonin Gene-Related Peptide Expression and Secretion from Rat Trigeminal Ganglion Neurons. J. Neurochem. 2006, 96, 65–77. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Long, H.; Ma, W.; Liao, L.; Yang, X.; Zhou, Y.; Shan, D.; Huang, R.; Jian, F.; Wang, Y.; et al. The role of periodontal ASIC3 in orofacial pain induced by experimental tooth movement in rats. Eur. J. Orthod. 2016, 38, 577–583. [Google Scholar] [CrossRef]
- Ohkura, M.; Ohkura, N.; Yoshiba, N.; Yoshiba, K.; Ida-Yonemochi, H.; Ohshima, H.; Saito, I.; Okiji, T. Orthodontic force application upregulated pain-associated prostaglandin-I2/PGI2-receptor/TRPV1 pathway-related gene expression in rat molars. Odontology 2018, 106, 2–10. [Google Scholar] [CrossRef]
- Guo, R.; Zhou, Y.; Long, H.; Shan, D.; Wen, J.; Hu, H.; Yang, H.; Wu, Z.; Lai, W. Transient receptor potential Vanilloid 1-based gene therapy alleviates orthodontic pain in rats. Int. J. Oral Sci. 2019, 11, 11. [Google Scholar] [CrossRef]
- Seybold, V.S. The role of peptides in central sensitization. In Sensory Nerves; Handbook of Experimental Pharmacology; Canning, B., Spina, D., Eds.; Springer: Berlin/Heidelberg, Germany, 2009; Volume 194, pp. 451–491. [Google Scholar] [CrossRef]
- Mistrova, E.; Kruzliak, P.; Chottova Dvorakova, M. Role of Substance P in the Cardiovascular System. Neuropeptides 2016, 58, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.K.; Pi, S.H.; Kim, S.H.; Min, K.S.; Lee, H.J.; Chang, H.S.; Kang, K.H.; Kim, H.R.; Shin, H.I.; Lee, S.K.; et al. Substance P regulates macrophage inflammatory protein 3α/chemokine C-C ligand 20 (CCL20) with heme oxygenase-1 in human periodontal ligament cells. Clin. Exp. Immunol. 2007, 150, 567–575. [Google Scholar] [CrossRef] [PubMed]
- Yong, J.; Gröger, S.; VON Bremen, J.; Martins Marques, M.; Braun, A.; Chen, X.; Ruf, S.; Chen, Q. Photobiomodulation therapy assisted orthodontic tooth movement: Potential implications, challenges, and new perspectives. J. Zhejiang Univ.-Sci. B 2023, 24, 957–973. [Google Scholar] [CrossRef] [PubMed]
- Sharp, F.R.; Zhan, X.; Liu, D.Z. Heat shock proteins in the brain: Role of Hsp70, Hsp 27, and HO-1 (Hsp32) and their therapeutic potential. Transl. Stroke Res. 2013, 4, 685–692. [Google Scholar] [CrossRef]
- Tsuchiya, T.; Hasegawa, N.; Yugawa, M.; Sasaki, A.; Suda, N.; Adachi, K. Different therapeutic effects of CO2 and diode laser irradiation on tooth movement-related pain. Front. Neurol. 2020, 11, 481. [Google Scholar] [CrossRef]
- Gunji, H.; Kunimatsu, R.; Tsuka, Y.; Yoshimi, Y.; Sumi, K.; Awada, T.; Nakajima, K.; Kimura, A.; Hiraki, T.; Hirose, N.; et al. Effect of high-frequency near-infrared diode laser irradiation on periodontal tissues during experimental tooth movement in rats. Lasers Surg. Med. 2018, 50, 772–780. [Google Scholar] [CrossRef]
- Kawasaki, K.; Shimizu, N. Effects of low-energy laser irradiation on bone remodeling during experimental tooth movement in rats. Lasers Surg. Med. 2000, 26, 282–291. [Google Scholar] [CrossRef]





| Parameter | Value |
|---|---|
| Wavelength | 808 nm |
| Operation mode | Pulse |
| Pulse duration | 20 ms |
| Peak power | 7 W |
| Average power | 560 mW |
| Frequency | 5 Hz |
| Power density | 1.12 W/cm2 |
| Irradiation diameter | 0.8 cm |
| Beam area | 0.5024 cm2 |
| Irradiation time | 45 s |
| Energy density | 50.4 J/cm2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okazaki, K.; Nakatani, A.; Kunimatsu, R.; Kado, I.; Sakata, S.; Kiridoshi, H.; Tanimoto, K. Effects of Near-Infrared Diode Laser Irradiation on Pain Relief and Neuropeptide Markers During Experimental Tooth Movement in the Periodontal Ligament Tissues of Rats: A Pilot Study. Int. J. Mol. Sci. 2025, 26, 7404. https://doi.org/10.3390/ijms26157404
Okazaki K, Nakatani A, Kunimatsu R, Kado I, Sakata S, Kiridoshi H, Tanimoto K. Effects of Near-Infrared Diode Laser Irradiation on Pain Relief and Neuropeptide Markers During Experimental Tooth Movement in the Periodontal Ligament Tissues of Rats: A Pilot Study. International Journal of Molecular Sciences. 2025; 26(15):7404. https://doi.org/10.3390/ijms26157404
Chicago/Turabian StyleOkazaki, Kanako, Ayaka Nakatani, Ryo Kunimatsu, Isamu Kado, Shuzo Sakata, Hirotaka Kiridoshi, and Kotaro Tanimoto. 2025. "Effects of Near-Infrared Diode Laser Irradiation on Pain Relief and Neuropeptide Markers During Experimental Tooth Movement in the Periodontal Ligament Tissues of Rats: A Pilot Study" International Journal of Molecular Sciences 26, no. 15: 7404. https://doi.org/10.3390/ijms26157404
APA StyleOkazaki, K., Nakatani, A., Kunimatsu, R., Kado, I., Sakata, S., Kiridoshi, H., & Tanimoto, K. (2025). Effects of Near-Infrared Diode Laser Irradiation on Pain Relief and Neuropeptide Markers During Experimental Tooth Movement in the Periodontal Ligament Tissues of Rats: A Pilot Study. International Journal of Molecular Sciences, 26(15), 7404. https://doi.org/10.3390/ijms26157404






