Abstract
Disruption of the microbiota resulting in pathogenicity is known as dysbiosis and is key in the pathogenesis of inflammatory bowel disease [IBD]. The microbiome of patients with IBD is characterized by depletion of commensal bacteria, in particular Bacteroidetes and the Lachnospiraceae subgroup of Firmicutes, and by the concomitant increase in Proteobacteria and the Bacillus subgroup of Firmicutes. These changes reflect a decrease in microbial diversity with a concomitant decrease in health-promoting bacteria like Faecalibacterium and Roseburia. Treatment with biologic agents has changed the natural course of disease, improving patient outcomes. Changes in gut microbiota occur under treatment with biologic agents and act towards reversal of dysbiosis. These changes are more striking in patients achieving remission and specific gut microbiota signatures may be predictive of treatment response and a step towards precision medicine, since, despite advances in medical treatment, some patients are at risk of surgery and subsequent complications such as anastomotic leakage. This review summarizes current available evidence on the interplay of gut microbiota and biologic agents, surgery, and surgical complications in patients with IBD.
1. Introduction
Inflammatory bowel disease (IBD) encompasses a variety of intestinal conditions that lead to long-lasting inflammation in the digestive system. The primary forms of IBD include ulcerative colitis (UC) and Crohn′s disease (CD), and their incidence is increasing worldwide [,]. IBD is thought to occur in people with a genetic predisposition following environmental exposure; gut epithelial barrier defects, the microbiota, and a dysregulated immune response are strongly implicated. Patients usually present with bloody diarrhoea, abdominal pain, weight loss, and fatigue, and the diagnosis is based on a combination of clinical and laboratory findings, such as abnormalities in the complete blood count (leucocytosis, anaemia, and thrombocytosis), elevated C-reactive protein (CRP), elevated faecal calprotectin, hypoalbuminemia, and micronutrient deficiencies. Endoscopy remains the diagnostic gold standard. The goal of medical treatment is to achieve a swift clinical response and to sustain clinical remission. Management of IBD has changed considerably in parallel with newly available therapies, and now consists of immunosuppressive agents as well as biologicals. In some patients, surgical treatment may still be required [,].
The gut microbiome is considered to play a key role in the pathogenesis of IBD as well as in the prediction and follow-up of treatment response. More precisely, the gut microbiome is increasingly recognized as a central factor in the development and progression of inflammatory bowel disease (IBD). It is believed to influence both the initiation and perpetuation of the disease through complex interactions with the host immune system, intestinal epithelial cells, and environmental triggers. Furthermore, alterations in the composition and function of the gut microbiota are being explored not only as potential biomarkers for diagnosing IBD but also for predicting patients’ responses to various therapeutic interventions. Consequently, monitoring the microbiome over time may offer valuable insights into treatment efficacy and disease remission or relapse, thereby playing a critical role in both personalized treatment strategies and long-term disease management. In this review, we aim to summarize current available evidence on the interplay between the gut microbiome with biologic agents, surgery, and surgical complications in patients with IBD.
2. Materials and Methods
A search was conducted across MEDLINE [PubMed] on 1 June 2025 under the terms “Surgical Procedures, Colorectal”[Mesh], “Anastomosis, Surgical”[Mesh], “gut microbio*”, “faecalibacterium”, “dysbiosis”, “infliximab”, “adalimumab”, “ustekinumab”, and “vedolizumab” for studies published in English without publication time restriction. The search was performed by two independent authors and the same authors assessed all articles generated by the electronic search, by title, abstract, and complete text, to find those meeting the eligibility criteria. Publications retrieved from electronic databases were imported into reference management software [EndNoteX6, Thomson Reuters, New York, NY, USA], and duplicates were removed. The search strategy is shown in Figure 1.
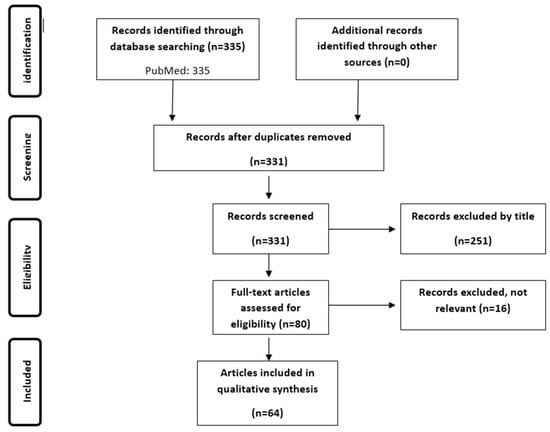
Figure 1.
Search strategy.
3. Results and Discussion
3.1. The Gut Microbiota in Inflammatory Bowel Disease
3.1.1. Dysbiosis
The gut microbiota, as the endogenous gastrointestinal microbial flora is called, plays a fundamentally important role in health and disease, yet it is not completely defined and understood. There is significant intersubject variability and differences between the stool and mucosa community composition, partially attributable to variations in time, diet, and health status []. In IBD, major changes in the composition of the gut microbiota, compared to that of healthy individuals, have already been described. Frank and colleagues examined tissue samples from patients with Crohn′s disease (CD) and ulcerative colitis (UC), along with samples from non-inflammatory bowel disease (IBD) controls []. The microbiota of individuals with IBD was found to have a reduced abundance of beneficial bacteria, especially those from the Bacteroidetes phylum and the Lachnospiraceae family of Firmicutes, while showing a corresponding increase in Proteobacteria and the Bacillus group of Firmicutes. Moreover, the small-intestine samples, as a whole, contained less overall phylogenetic diversity of Bacteroidetes and Firmicutes than did the large intestine. These changes reflect a decrease in microbial diversity, both alpha-diversity (the number of different species found as a measure of local species richness) and beta-diversity (the ratio between regional and local species diversity), whereas other studies have found a concomitant decrease in health-promoting bacteria like Faecalibacterium and Roseburia [,]. Both bacteria of the Firmicutes phylum are producers of the short-chain fatty acid [SCFA] butyrate, and in the presence of butyrate and other SCFAs, such as propionic and acetic acid, tissue macrophages differentiate and display enhanced antimicrobial activity []. Most of the studies on microbiota in IBD report separately and focus on changes seen in Faecalibacterium prausnitzii abundance; thus, these changes are provided in more detail below.
The alteration of microbiota composition that leads to pathogenicity is referred to as dysbiosis, and it is suggested that this may be influenced by interactions with environmental stressors in individuals genetically predisposed to develop IBD []. Since the intestinal epithelial layer is crucial for maintaining the symbiotic relationship between microbiota and host and for preventing inappropriate immune and inflammatory reactions, this connection is disrupted in IBD. The mucosal barrier becomes permeable due to changes in epithelial tight junctions, cell death, and damage to the intestinal lining, allowing the invasion of pathogenic microorganisms in a dysbiotic setting [].
3.1.2. Faecalibacterium Prausnitzii
F. prausnitzii is one of the largest butyrate producers. Initially classified as Bacteroides prausnitzii in 1937, it was reclassified as Fusobacterium prausnitzii in 1974 and then as Faecalibacterium prausnitzii in 2002 []. It is imperative for sustaining health and luminal homeostasis and its abundance has been found to be altered across a wide range of diseases and disorders; in IBD, it tends to be diminished. F. prausnitzii consists of two main phylogroups. Phylogroup I was observed in 87% of healthy individuals, while it was present in less than 50% of patients with IBD. On the other hand, phylogroup II was found in over 75% of IBD patients but only in 52% of healthy individuals. Consequently, even though the main members of the F. prausnitzii population are present in both healthy and IBD individuals, richness is reduced in the latter and an altered phylotype distribution exists []. Reductions in the abundance of Faecalibacterium have been associated with a decline in the circulation of CD4+ CD8α+ Foxp3+ regulatory T [Treg] lymphocytes, as well as with an increase in various disease activity metrics []. Moreover, SCFA production by F. prausnitzii inhibits the enzyme HDAC1 in CD4+ T cells resulting in the downregulation of some proinflammatory cytokines, while also promoting Forkhead box P3 [Foxp3] which induces Th17/Treg balance by encouraging Th17 cells to differentiate []. Considering all of the above, it is understood that alterations in the composition and function of the gut microbiota may lead to alterations in gut microbiota-derived metabolites, such as bile acids, SCFA, and tryptophan metabolites, also implicated in the pathogenesis of IBD []. In health, SCFAs mediate diverse effects on mucosal immunity, including supporting B cell development, differentiation and expansion of regulatory T (Treg) cells, maintenance of mucosal integrity by means of inflammasome activation and IL-18 production, and on colonic dendritic cells and macrophages, which promote differentiation of Treg cells. All of these are impaired in IBD []. Bile acids that reach the colon are normally transformed into secondary bile acids by bacteria; in IBD, dysbiosis leads to loss of this transformation to secondary bile acids and an imbalance of primary and secondary bile acids in the colon []. Lastly, the major pathway for dietary tryptophan is the kynurenine pathway, with tryptophan also being used to generate serotonin and associated metabolites. Tryptophan can be metabolized by commensal microbiota to produce indoles with diverse effects on mucosal immunity and homeostasis. In IBD, dysbiosis leads to the loss of the microbial activation of tryptophan, causing increased metabolism down the kynurenine pathway [].
In a cross-sectional study of 116 UC patients in remission, 29 first-degree relatives, and 31 healthy controls, F. prausnitzii was reduced in patients but also their relatives compared to controls. A low abundance of F. prausnitzii was also associated with less than 12 months of remission. F. prausnitzii increased steadily until reaching similar levels to those of controls if remission persisted, whereas it remained low if patients relapsed []. In a study involving UC patients who had not previously received biological therapy prior to starting anti-tumour necrosis factor [TNF] therapy, F. prausnitzii was more abundant at the start in those who responded positively compared to non-responders, and its levels increased during the induction therapy for responders []. Beneficial microbes like F. prausnitzii and Roseburia have been consistently associated with positive clinical outcomes [].
3.2. Fluctuation of Gut Microbiota and Implications for Treatment Response Prediction
Recently, it has been acknowledged that gut microbiota in IBD fluctuates more than that of healthy individuals, periodically exhibiting the pattern of healthy individuals and deviating away from it. Some fluctuations of the gut microbiota correlate with disease severity, while others have been associated with intensified medication due to a flare-up of the disease, implying a future direction for microbiota composition guided therapies [,,]. In a recent systematic review focusing on biomarkers for response to advanced therapies in IBD, baseline microbial analyses and therapeutic response data were available for a total of 1232 individuals, making up 46% of the overall study population []. Parameters evaluated as biomarkers for treatment response in the individual studies were diversity, abundance of specific microbial taxa, presence of opportunistic organisms, SCFA-producing organisms and butyrate synthesis pathways, and other metabolomic analysis []. Evidence from individual studies suggests that dysbiosis, characterized by a decrease in Firmicutes, and/or enterotyping correlate with the risk and time to relapse after anti-TNF treatment [,,]. Moreover, a range of metabolic biomarkers involving lipid, bile acid, and amino acid pathways may contribute to prediction of response to anti-TNF therapy in IBD []. In a proof-of-concept investigation, Busquets et al. examined the ability to predict who would respond to anti-TNF therapy. The RAID algorithm, which combines four bacterial markers, demonstrated a strong ability to differentiate between responders and non-responders, achieving sensitivity and specificity rates of 93.33% and 100%, respectively, with a positive predictive value of 100% and a negative predictive value of 75% [].
3.3. Longitudinal Changes in Gut Microbiota in IBD Patients Treated with Biologic Agents
In order to achieve the double goal in IBD treatment of rapid clinical response and sustained clinical remission, a variety of immunomodulating therapies are available (corticosteroids, thiopurines and newer biologic agents such as TNF inhibitors). Anti-TNF-α agents are among the most effective therapies to induce and maintain remission in IBD, as a T-cell mediated response is the hallmark of the pathogenesis of intestinal inflammation, which is facilitated by increased proinflammatory cytokines, interferon gamma, interleukin 12, and TNF-α. Increased secretion of TNF-α from lamina propria mononuclear cells has been found in the intestinal mucosa and TNF-α positive cells have been found deeper in the lamina propria and in the submucosa [].
As dysbiosis is also considered to play a key role in IBD, several studies so far have investigated possible changes in the composition of gut microbiota during and/or after treatment with biologic agents compared to baseline; these studies are summarized in Table 1 [,,,,,,,,,,,,,,,,,]. The evidence relates mainly to microbiota changes under treatment with TNF inhibitors but also with other treatments, discussed below in more detail.

Table 1.
Longitudinal changes in gut microbiota in patients with inflammatory bowel diseases treated with biologic agents.
3.3.1. Adalimumab
Adalimumab is a TNF-blocker used in the treatment of IBD. In a prospective study in Italy, microbiota of 20 patients with CD under adalimumab was investigated prior to and after 6 months of treatment []. In the whole population, there was a trend towards increased abundance of some main phyla such as Firmicutes and Bacteroides, and a decreased abundance of Proteobacteria. These differences reached statistical significance only in patients with treatment success, suggesting that response to adalimumab may be associated with reversal of dysbiosis. No notable alterations were detected in the population of Faecalibacterium prausnitzii. Comparable findings have also been documented by other researchers in both CD [,] and UC [,].
3.3.2. Infliximab
Infliximab is another anti-TNF for the treatment of IBD. In a German study, among patients with IBD and rheumatic diseases and healthy controls, Aden et al. reported significant baseline differences among the three groups; dysbiosis was present in both the IBD and rheumatic groups []. Interestingly, treatment with infliximab shifted the diversity of faecal microbiota in patients with IBD, but not with rheumatic disease, toward that of controls, suggesting that other factors may interfere with biologicals and induce clinical remission. Ditto et al. focused on microbiota changes under treatment with TNF-inhibitors [TNFi] in a small cohort of patients with enteropathic spondylarthritis. Although no differences were observed in α- or β-diversity, abundance of Lachnospiraceae and Coprococcus increased and there was a decreasing trend in Proteobacteria and Gammaproteobacteria []. Similar studies confirm the restoration of gut dysbiosis in IBD patients under infliximab treatment, reflected in the increase in α-diversity, increased abundance of Bacteroidetes and Firmicutes, and decreased abundance of Enterobacterales, as well as an increased abundance of SCFA-producing taxa such as Lachnospira, Roseburia, and Blautia [family Lachnospiraceae] []. These changes are more pronounced in treatment-responders and specific alterations like the ratio of F. prausnitzii/E. coli are accurate biomarkers for predicting clinical remission, performing even better than calprotectin and the Harvey–Bradshaw index [,,].
3.3.3. Ustekinumab
Ustekinumab is a fully human IgG1κ monoclonal antibody that targets the shared p40 subunit of interleukin [IL]-12 and IL-23. By preventing these cytokines from attaching to their receptors, it diminishes the maturation and proliferation of Th-1 and Th-17 cells. In a limited study involving patients with IBD, no significant long-term effects of ustekinumab treatment were observed on alpha- and beta-diversity, nor on the abundance of other phyla or genera []. In a secondary analysis of a randomized, double-blind, placebo-controlled phase 2b clinical trial, among 306 anti-TNF-refractory CD patients, a high relative abundance of Faecalibacterium was associated with remission 6 weeks later. The median α-diversity of responders observed after the introduction of ustekinumab showed a significant evolution over time, increasing from baseline to 4 weeks post-induction. It then declined from 4 to 6 weeks after treatment initiation, but was notably higher than the baseline at 22 weeks post-induction, indicating that changes in the microbiota may reflect treatment response []. Xu et al. have even reported changes in the oral microbiota under ustekinumab treatment in responders and non-responders; oral samples are easier than faecal samples to obtain for follow-up of treatment response [].
3.3.4. Vedolizumab
Vedolizumab is a human-derived IgG1 monoclonal antibody that targets α4β7 integrin, specifically inhibiting the movement of leukocytes into the gastrointestinal tract by binding to the α4β7 integrin. In a small study of 29 participants, patients in remission under anti-integrin therapy had a higher abundance of the phylum Verrucomicrobiota and metabolomic analysis showed higher levels of two SCFA, namely butyric acid and isobutyric acid, in these patients compared to non-responders []. Ananthakrishnan et al. studied, longitudinally, the gut microbiota of 85 patients with IBD under vedolizumab and observed very few changes in microbial composition under treatment [].
Nevertheless, there were markedly greater changes in microbial function at the metagenomic level. In patients with Crohn′s disease, 17 pathways showed a significant reduction at the 14-week follow-up compared to the baseline, with 15 of these reductions occurring exclusively in individuals who reached remission. Among these were declines in various tricarboxylic acid cyclic pathways and the nicotinamide adenine dinucleotide salvage pathway, indicating a reduction in oxidative stress for those achieving remission. The changes were less striking in UC.
3.4. Surgery in Inflammatory Bowel Disease, Surgical Complications, and Gut Microbiota
3.4.1. Surgery and the Role of Gut Microbiota
Over the last two decades, although advances have improved the course and outcomes of IBD, like earlier diagnosis, introduction of disease-modifying immunosuppressive therapy and biologic agents, earlier detection, and endoscopic management of colorectal neoplasia, there is still a considerable 5-year cumulative risk of surgery for such patients, reaching 7% in UC and 18.0% in CD []. Recently, Lewis et al. [] described an association of dysbiosis and surgery for CD. They identified patients with prior surgery in two different cohorts, namely the Study of a Prospective Adult Research Cohort with Inflammatory Bowel Disease [SPARC IBD] and the Diet to Induce Remission in Crohn′s Disease [DINE-CD] study, and reported that intestinal resection was associated with reduced alpha-diversity and altered beta-diversity with increased Proteobacteria and reduced Bacteroidetes and Firmicutes.
Additionally, the potentially beneficial Egerthella lenta, Adlercreutzia equalofaciens, and Gordonibacter pamelaeae were lower in abundance among patients with prior surgery in both cohorts []. In a separate study examining alterations in microbiota and metabolome following various surgeries for IBD, it appears that intestinal surgery leads to a decrease in the diversity of the gut microbiota and metabolome. Colectomy had a greater effect compared to ileocolonic resection and the type of surgery explained the greater variation in the microbiota data than any other variable, followed by disease subtype, antibiotic use, and disease activity [].
3.4.2. Anastomotic Leakage and the Role of Gut Microbiota
Complications following intestinal surgery affect roughly one in three patients. The most prevalent short-term complications are infection and ileus, while pouchitis and faecal incontinence are the most commonly observed long-term complications []. Anastomotic leakage is a major complication, leading to high morbidity and mortality. Anastomotic leakage is quite common after colorectal surgical procedures with an incidence of 2–20%, depending on the location of the anastomosis, with the highest rates being observed in low rectal anastomoses. Common predisposing factors are mainly host-derived [male gender, increasing age, comorbidities, and malnutrition] but operation characteristics [duration of surgery, small distance of the anastomosis from the anal verge, and positive intraoperative leak test] are of paramount importance []. Mechanical bowel preparation and antimicrobial prophylaxis may decrease the risk []. The underlying pathophysiology is yet unclear but microbiota changes have been proposed as a potential contributor.
An increasing volume of research indicates that undergoing surgery can lead to a notable shift in the composition of the gut microbiota due to ischemia-reperfusion injury occurring from the constriction of intestinal blood vessels during the procedure []. Following colorectal surgery, the relative abundance of oral anaerobic bacteria, including Parvimonas micra, Peptoanaerobacter stomatis, Peptostreptococcus anaerobius, Dorea longicatena, and Porphyromonas uenonis, as well as obligate anaerobes like bifidobacteria, is significantly decreased. Conversely, the levels of pathogenic bacteria such as Enterobacteriaceae, Enterococcus, Staphylococcus, and Pseudomonas substantially increase after the procedure. []. Anastomotic leakage is considered to be associated with gut microbiota changes, and has already been shown in various animal models, suggesting common pathogens like Pseudomonas aeruginosa and Enterococcus faecalis as factors contributing to leakage [,,]. A recent study using a mouse model suggests that gut microbiota influence anastomotic healing in colorectal surgery through modulation of mucosal proinflammatory cytokines, such as mucosal MIP-1α, MIP-2, MCP-1, and IL-17A/F [], so that biopsy samples from surgical margins, rather than faecal samples, may be appropriate to explore the contribution of the intestinal microbiota to leakage [].
In a small cohort of 21 colon cancer patients, five developed anastomotic leak and showed an array of bacterial species which promoted dysbiosis, such as Acinetobacter lwoffii and Hafnia alvei. Patients with appropriate mucosal healing had a microbiota abundant in species with a protective function like Faecalibacterium prausnitzii and Barnesiella intestinihominis []. Lehr et al. [] concluded that after colorectal surgery, overall bacterial diversity and the abundance of some genera such as Faecalibacterium or Alistipes decreased over time, while the genera Enterococcus and Escherichia_Shigella increased.
Marked variations have been observed in the abundance of genera including Prevotella, Faecalibacterium, and Phocaeicola. Ruminococcus2 and Blautia demonstrated notable differences in their abundance, even among preoperative samples, suggesting that they may also serve as predictors for postoperative complications []. A recent systematic review on the role of the gut microbiota in anastomotic leakage after colorectal resection summarized results from seven clinical and five experimental studies. The authors conclude that patients experiencing anastomotic leakage show a reduced α-diversity in their gut microbiota, and certain genera of microbes, such as Lachnospiraceae, Bacteroidaceae, Bifidobacterium, Acinetobacter, Fusobacterium, Dielma, Elusimicronium, Prevotella, and Faecalibacterium, appear to be linked to this condition. In contrast, genera like Streptococcus, Eubacterium, Enterobacteriaceae, Klebsiella, Actinobacteria, Gordonibacter, Phocaeicola, and Ruminococcus seem to provide a protective effect [].
3.4.3. Anastomotic Leakage and the Role of Biologic Agents
Since TNF is involved in angiogenesis and collagen production, which are crucial for wound healing, there are concerns that pre-operative treatment with anti-TNF could affect the body′s response to surgical stress and elevate the likelihood of complications during surgery. In a prospective, multi-centre cohort pilot study, 46 IBD patients undergoing major abdominal operations were analysed, with 18 of them having undergone anti-TNF therapy prior to the procedure. Concentrations of immunological and other biomarkers of the surgical stress response [TNF, IL-6, IL-10, IL-8, IL-17A, C-reactive protein, white blood cells, cortisol, transferrin, ferritin, and D-Dimer] were measured and no difference in the concentrations was found between anti-TNF-treated and anti-TNF-naïve patients postoperatively.
Moreover, no difference in the rate of postoperative complications or length of stay was observed []. In a retrospective study of 282 IBD patients, of whom 73 patients were treated with anti-TNF therapy within 8 weeks of surgery, 30-day anastomotic leak, intra-abdominal abscess, wound infection, extra-abdominal infection, readmission, and mortality rates did not differ significantly []. Similar results have been reported by others [,]. In a cohort of 417 surgically treated patients with CD in Demark in 2000–2007, however, prednisolone, rather than biologic agents, had a negative impact on post-surgical anastomotic leak rates []. In a meta-analysis of six studies including 1159 patients, among whom 413 complications were identified, there was no significant difference in the major complication rate [OR, 1.59; 95% CI, 0.89–2.86], minor complication rate [OR,1.80; 95% CI, 0.87–3.71], reoperation rate [OR, 1.33; 95% CI, 0.55–3.20], or 30-day mortality rate [OR, 3.74; 95% CI, 0.56–25.16] between the infliximab-treated and control groups []. Importantly, timing of the last dose of anti-TNF agents does not appear to affect the rate of postoperative complications in patients with IBD [].
4. Conclusions
Dysbiosis plays a central role in the pathogenesis of IBD. Biologic therapies have significantly altered the disease course, leading to improved patient outcomes. These treatments also induce changes in the gut microbiota, and specific microbial signatures may help predict treatment response, paving the way for precision medicine. Despite therapeutic advances, some IBD patients still require surgery and remain at risk of complications such as anastomotic leakage, which has been linked to alterations in the gut microbiota []. To date, no studies have specifically examined the relationship between gut microbiota and anastomotic leakage in patients with IBD.
Given the evidence, biologic treatment may offer additional benefits to surgical candidates by modulating the gut microbiota toward eubiosis, potentially reducing the risk of anastomotic leakage [Figure 2]. This hypothesis warrants further investigation, and the complex interplay between gut microbiota, biologic therapy, and postoperative outcomes in IBD should be explored in future animal and clinical studies.
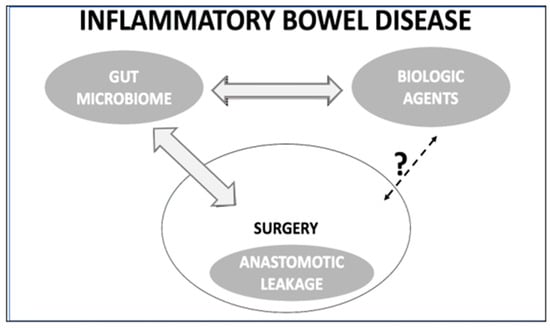
Figure 2.
The concept of interplay among the gut microbiota, biologic agents, and the postoperative anastomotic leakage in patients with inflammatory bowel disease.
Author Contributions
Conceptualization, K.K. and A.-E.M.; methodology, G.T. and E.K. (Evdoxia Kyriazopoulou); software, G.T.; validation, E.K. (Eleni Karakike), A.-E.M., and E.F.; formal analysis, A.-E.M.; investigation, E.K. (Evdoxia Kyriazopoulou); resources, E.K. (Eleni Karakike); data curation, E.F.; writing—original draft preparation, A.-E.M. and E.K. (Evdoxia Kyriazopoulou); writing—review and editing, E.K. (Evdoxia Kyriazopoulou); visualization, E.F.; supervision, K.K.; project administration, K.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Not applicable.
Acknowledgments
The Novo Nordisk Foundation Center for Stem Cell Medicine is supported by a Novo Nordisk Foundation grant (NNF21CC0073729) and we gratefully acknowledge Anne D. Shrewsbury BA for her English language editing of our manuscript, drawing on her expertise as a native English speaker.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| IBD | Inflammatory Bowel Disease |
| SCFA | Short-chain Fatty Acids |
| CD | Crohn’s Disease |
| UC | Ulcerative Colitis |
References
- Dolinger, M.; Torres, J.; Vermeire, S. Crohn’s disease. Lancet 2024, 403, 1177–1191. [Google Scholar] [CrossRef] [PubMed]
- Le Berre, C.; Honap, S.; Peyrin-Biroulet, L. Ulcerative colitis. Lancet 2023, 402, 571–584. [Google Scholar] [CrossRef] [PubMed]
- Eckburg, P.B.; Bik, E.M.; Bernstein, C.N.; Purdom, E.; Dethlefsen, L.; Sargent, M.; Gill, S.R.; Nelson, K.E.; Relman, D.A. Diversity of the human intestinal microbial flora. Science 2005, 308, 1635–1638. [Google Scholar] [CrossRef] [PubMed]
- Frank, D.N.; St Amand, A.L.; Feldman, R.A.; Boedeker, E.C.; Harpaz, N.; Pace, N.R. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc. Natl. Acad. Sci. USA 2007, 104, 13780–13785. [Google Scholar] [CrossRef] [PubMed]
- Pisani, A.; Rausch, P.; Bang, C.; Ellul, S.; Tabone, T.; Marantidis Cordina, C.; Zahra, G.; Franke, A.; Ellul, P. Dysbiosis in the Gut Microbiota in Patients with Inflammatory Bowel Disease during Remission. Microbiol. Spectr. 2022, 10, e0061622. [Google Scholar] [CrossRef] [PubMed]
- Machiels, K.; Joossens, M.; Sabino, J.; De Preter, V.; Arijs, I.; Eeckhaut, V.; Ballet, V.; Claes, K.; Van Immerseel, F.; Verbeke, K.; et al. A decrease of the butyrate-producing species Roseburia hominis and Faecalibacterium prausnitzii defines dysbiosis in patients with ulcerative colitis. Gut 2014, 63, 1275–1283. [Google Scholar] [CrossRef] [PubMed]
- Schulthess, J.; Pandey, S.; Capitani, M.; Rue-Albrecht, K.C.; Arnold, I.; Franchini, F.; Chomka, A.; Ilott, N.E.; Johnston, D.G.W.; Pires, E.; et al. The Short Chain Fatty Acid Butyrate Imprints an Antimicrobial Program in Macrophages. Immunity 2019, 50, 432–445.e7. [Google Scholar] [CrossRef] [PubMed]
- Khalaf, R.; Sciberras, M.; Ellul, P. The role of the fecal microbiota in inflammatory bowel disease. Eur. J. Gastroenterol. Hepatol. 2024, 36, 1249–1258. [Google Scholar] [CrossRef] [PubMed]
- Martín, R.; Rios-Covian, D.; Huillet, E.; Auger, S.; Khazaal, S.; Bermúdez-Humarán, L.G.; Sokol, H.; Chatel, J.M.; Langella, P. Faecalibacterium: A bacterial genus with promising human health applications. FEMS Microbiol. Rev. 2023, 47, fuad039. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Siles, M.; Martinez-Medina, M.; Abellà, C.; Busquets, D.; Sabat-Mir, M.; Duncan, S.H.; Aldeguer, X.; Flint, H.J.; Garcia-Gil, L.J. Mucosa-associated Faecalibacterium prausnitzii phylotype richness is reduced in patients with inflammatory bowel disease. Appl. Environ. Microbiol. 2015, 81, 7582–7592. [Google Scholar] [CrossRef] [PubMed]
- Touch, S.; Godefroy, E.; Rolhion, N.; Danne, C.; Oeuvray, C.; Straube, M.; Galbert, C.; Brot, L.; Salgueiro, I.A.; Chadi, S.; et al. Human CD4+CD8α+ Tregs induced by Faecalibacterium prausnitzii protect against intestinal inflammation. JCI Insight. 2022, 7, e154722. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Zhang, M.; Wang, Y.; Dorfman, R.G.; Liu, H.; Yu, T.; Chen, X.; Tang, D.; Xu, L.; Yin, Y.; et al. Faecalibacterium prausnitzii Produces Butyrate to Maintain Th17/Treg Balance and to Ameliorate Colorectal Colitis by Inhibiting Histone Deacetylase 1. Inflamm. Bowel Dis. 2018, 24, 1926–1940. [Google Scholar] [CrossRef] [PubMed]
- Lavelle, A.; Sokol, H. Gut microbiota-derived metabolites as key actors in inflammatory bowel disease. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 223–237. [Google Scholar] [CrossRef] [PubMed]
- Varela, E.; Manichanh, C.; Gallart, M.; Torrejón, A.; Borruel, N.; Casellas, F.; Guarner, F.; Antolin, M. Colonisation by Faecalibacterium prausnitzii and maintenance of clinical remission in patients with ulcerative colitis. Aliment. Pharmacol. Ther. 2013, 38, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Magnusson, M.K.; Strid, H.; Sapnara, M.; Lasson, A.; Bajor, A.; Ung, K.A.; Öhman, L. Anti-TNF Therapy Response in Patients with Ulcerative Colitis Is Associated with Colonic Antimicrobial Peptide Expression and Microbiota Composition. J. Crohn’s Colitis 2016, 10, 943–952. [Google Scholar] [CrossRef] [PubMed]
- Alexandrescu, L.; Nicoara, A.D.; Tofolean, D.E.; Herlo, A.; Nelson Twakor, A.; Tocia, C.; Trandafir, A.; Dumitru, A.; Dumitru, E.; Aftenie, C.F.; et al. Healing from Within: How Gut Microbiota Predicts IBD Treatment Success—A Systematic Review. Int. J. Mol. Sci. 2024, 25, 8451. [Google Scholar] [CrossRef] [PubMed]
- Schierova, D.; Roubalova, R.; Kolar, M.; Stehlikova, Z.; Rob, F.; Jackova, Z.; Coufal, S.; Thon, T.; Mihula, M.; Modrak, M.; et al. Fecal Microbiota Changes and Specific Anti-Bacterial Response in Patients with IBD during Anti-TNF Therapy. Cells 2021, 10, 3188. [Google Scholar] [CrossRef] [PubMed]
- Halfvarson, J.; Brislawn, C.J.; Lamendella, R.; Vázquez-Baeza, Y.; Walters, W.A.; Bramer, L.M.; D’Amato, M.; Bonfiglio, F.; McDonald, D.; Gonzalez, A.; et al. Dynamics of the human gut microbiota in inflammatory bowel disease. Nat. Microbiol. 2017, 2, 17004. [Google Scholar] [CrossRef] [PubMed]
- Eckenberger, J.; Butler, J.C.; Bernstein, C.N.; Shanahan, F.; Claesson, M.J. Interactions between Medications and the Gut Microbiota in Inflammatory Bowel Disease. Microorganisms 2022, 10, 1963. [Google Scholar] [CrossRef] [PubMed]
- Meade, S.; Liu Chen Kiow, J.; Massaro, C.; Kaur, G.; Squirell, E.; Bressler, B.; Lunken, G. Gut microbiota-associated predictors as biomarkers of response to advanced therapies in inflammatory bowel disease: A systematic review. Gut Microbes. 2023, 15, 2287073. [Google Scholar] [CrossRef] [PubMed]
- Rajca, S.; Grondin, V.; Louis, E.; Vernier-Massouille, G.; Grimaud, J.C.; Bouhnik, Y.; Laharie, D.; Dupas, J.L.; Pillant, H.; Picon, L.; et al. Alterations in the intestinal microbiota [dysbiosis] as a predictor of relapse after infliximab withdrawal in Crohn’’s disease. Inflamm. Bowel Dis. 2014, 20, 978–986. [Google Scholar] [PubMed]
- Caenepeel, C.; Falony, G.; Machiels, K.; Verstockt, B.; Goncalves, P.J.; Ferrante, M.; Sabino, J.; Raes, J.; Vieira-Silva, S.; Vermeire, S. Dysbiosis and Associated Stool Features Improve Prediction of Response to Biological Therapy in Inflammatory Bowel Disease. Gastroenterology 2024, 166, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Xu, Z.Z.; He, Y.; Yang, Y.; Liu, L.; Lin, Q.; Nie, Y.; Li, M.; Zhi, F.; Liu, S.; et al. Gut Microbiota Offers Universal Biomarkers across Ethnicity in Inflammatory Bowel Disease Diagnosis and Infliximab Response Prediction. mSystem 2018, 3, e00188-17. [Google Scholar] [CrossRef] [PubMed]
- Ding, N.S.; McDonald, J.A.K.; Perdones-Montero, A.; Rees, D.N.; Adegbola, S.O.; Misra, R.; Hendy, P.; Penez, L.; Marchesi, J.R.; Holmes, E.; et al. Metabonomics and the Gut Microbiota Associated with Primary Response to Anti-TNF Therapy in Crohn’s Disease. J. Crohn’s Colitis 2020, 14, 1090–1102. [Google Scholar] [CrossRef] [PubMed]
- Busquets, D.; Mas-de-Xaxars, T.; López-Siles, M.; Martínez-Medina, M.; Bahí, A.; Sàbat, M.; Louvriex, R.; Miquel-Cusachs, J.O.; Garcia-Gil, J.L.; Aldeguer, X.; et al. Anti-tumour Necrosis Factor Treatment with Adalimumab Induces Changes in the Microbiota of Crohn’s Disease. J. Crohn’s Colitis 2015, 9, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Ribaldone, D.G.; Caviglia, G.P.; Abdulle, A.; Pellicano, R.; Ditto, M.C.; Morino, M.; Fusaro, E.; Saracco, G.M.; Bugianesi, E.; Astegiano, M. Adalimumab Therapy Improves Intestinal Dysbiosis in Crohn’’s Disease. J. Clin. Med. 2019, 8, 1646. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Lu, Z.; Kang, D.; Feng, Z.; Li, G.; Sun, M.; Liu, Z.; Wu, W.; Fang, L. Distinct alterations of fecal microbiota refer to the efficacy of adalimumab in Crohn’’s disease. Front. Pharmacol. 2022, 13, 913720. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.N.; Shin, S.Y.; Kim, J.H.; Baek, J.; Kim, H.J.; Lee, K.M.; Park, S.J.; Kim, S.Y.; Choi, H.K.; Kim, W.; et al. Dynamic changes in the gut microbiota composition during adalimumab therapy in patients with ulcerative colitis: Implications for treatment response prediction and therapeutic targets. Gut Pathog. 2024, 16, 44. [Google Scholar] [CrossRef] [PubMed]
- Sakurai, T.; Nishiyama, H.; Sakai, K.; De Velasco, M.A.; Nagai, T.; Komeda, Y.; Kashida, H.; Okada, A.; Kawai, I.; Nishio, K.; et al. Mucosal microbiota and gene expression are associated with long-term remission after discontinuation of adalimumab in ulcerative colitis. Sci. Rep. 2020, 10, 19186. [Google Scholar] [CrossRef] [PubMed]
- Aden, K.; Rehman, A.; Waschina, S.; Pan, W.H.; Walker, A.; Lucio, M.; Nunez, A.M.; Bharti, R.; Zimmerman, J.; Bethge, J.; et al. Metabolic Functions of Gut Microbes Associate with Efficacy of Tumor Necrosis Factor Antagonists in Patients With Inflammatory Bowel Diseases. Gastroenterology 2019, 157, 1279–1292.e11. [Google Scholar] [CrossRef] [PubMed]
- Ditto, M.C.; Parisi, S.; Landolfi, G.; Borrelli, R.; Realmuto, C.; Finucci, A.; Caviglia, G.P.; Ribaldone, D.G.; Astegiano, M.; Zanetti, A.; et al. Intestinal microbiota changes induced by TNF-inhibitors in IBD-related spondyloarthritis. RMD Open 2021, 7, e001755. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, X.; Tian, Z.; Feng, R.; Li, M.; Li, T.; Zhou, G.; Qiu, Y.; Chen, B.; He, Y.; Chen, M.; et al. Fecal Microbiota Alterations Associated With Clinical and Endoscopic Response to Infliximab Therapy in Crohn’s Disease. Inflamm. Bowel Dis. 2020, 26, 1636–1647. [Google Scholar] [CrossRef] [PubMed]
- Sanchis-Artero, L.; Martínez-Blanch, J.F.; Manresa-Vera, S.; Cortés-Castell, E.; Valls-Gandia, M.; Iborra, M.; Paredes-Arquiola, J.M.; Boscá-Watts, M.; Huguet, J.M.; Gil-Borrás, R.; et al. Evaluation of changes in intestinal microbiota in Crohn’s disease patients after anti-TNF alpha treatment. Sci. Rep. 2021, 11, 10016. [Google Scholar] [CrossRef] [PubMed]
- Seong, G.; Kim, N.; Joung, J.G.; Kim, E.R.; Chang, D.K.; Chun, J.; Hong, S.N.; Kim, Y.H. Changes in the Intestinal Microbiota of Patients with Inflammatory Bowel Disease with Clinical Remission during an 8-Week Infliximab Infusion Cycle. Microorganisms 2020, 8, 874. [Google Scholar] [CrossRef] [PubMed]
- Tamburini, F.B.; Tripathi, A.; Gold, M.P.; Yang, J.C.; Biancalani, T.; McBride, J.M.; Keir, M.E. Gardenia Study Group. Gut Microbial Species and Endotypes Associate with Remission in Ulcerative Colitis Patients Treated with Anti-TNF or Anti-integrin Therapy. J. Crohn’s Colitis 2024, 18, 1819–1831. [Google Scholar] [CrossRef] [PubMed]
- Rob, F.; Schierova, D.; Stehlikova, Z.; Kreisinger, J.; Roubalova, R.; Coufal, S.; Mihula, M.; Jackova, Z.; Kverka, M.; Thon, T.; et al. Association between ustekinumab therapy and changes in specific anti-microbial response, serum biomarkers, and microbiota composition in patients with IBD: A pilot study. PLoS ONE 2022, 17, e0277576. [Google Scholar] [CrossRef] [PubMed]
- Doherty, M.K.; Ding, T.; Koumpouras, C.; Telesco, S.E.; Monast, C.; Das, A.; Brodmerkel, C.; Schloss, P.D. Fecal Microbiota Signatures Are Associated with Response to Ustekinumab Therapy among Crohn’s Disease Patients. mBio 2018, 9, e02120-17. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Xie, R.; He, L.; Wang, H.; Zhu, Y.; Yang, X.; Yu, H. Oral Microbiota Associated with Clinical Efficacy of Ustekinumab in Crohn’s Disease. Endocr. Metab. Immune Disord. Drug Targets. 2025; Advance online publication. [Google Scholar] [CrossRef]
- Liu, J.; Fang, H.; Hong, N.; Lv, C.; Zhu, Q.; Feng, Y.; Wang, B.; Tian, J.; Yu, Y. Gut Microbiota and Metabonomic Profile Predict Early Remission to Anti-Integrin Therapy in Patients with Moderate to Severe Ulcerative Colitis. Microbiol. Spectr. 2023, 11, e0145723. [Google Scholar] [CrossRef] [PubMed]
- Ananthakrishnan, A.N.; Luo, C.; Yajnik, V.; Khalili, H.; Garber, J.J.; Stevens, B.W.; Cleland, T.; Xavier, R.J. Gut Microbiota Function Predicts Response to Anti-integrin Biologic Therapy in Inflammatory Bowel Diseases. Cell Host Microbe 2017, 21, 603–610.e3. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Wu, Z.; Yang, X.; Ding, J.; Wang, Q.; Fang, H.; Zhu, L.; Hu, M. Reduced gut microbiota diversity in ulcerative colitis patients with latent tuberculosis infection during vedolizumab therapy: Insights on prophylactic anti-tuberculosis effects. BMC Microbiol. 2024, 24, 543. [Google Scholar] [CrossRef] [PubMed]
- Tsai, L.; Ma, C.; Dulai, P.S.; Prokop, L.J.; Eisenstein, S.; Ramamoorthy, S.L.; Feagan, B.G.; Jairath, V.; Sandborn, W.J.; Singh, S. Contemporary Risk of Surgery in Patients With Ulcerative Colitis and Crohn’s Disease: A Meta-Analysis of Population-Based Cohorts. Clin. Gastroenterol. Hepatol. 2021, 19, 2031–2045.e11. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.D.; Daniel, S.G.; Li, H.; Hao, F.; Patterson, A.D.; Hecht, A.L.; Brensinger, C.M.; Wu, G.D.; Bittinger, K.; Wolf, D.C.; et al. Surgery for Crohn’s Disease Is Associated With a Dysbiotic Microbiota and Metabolome: Results From Two Prospective Cohorts. Cell. Mol. Gastroenterol. Hepatol. 2024, 18, 101357. [Google Scholar] [CrossRef] [PubMed]
- Fang, X.; Vázquez-Baeza, Y.; Elijah, E.; Vargas, F.; Ackermann, G.; Humphrey, G.; Lau, R.; Weldon, K.C.; Sanders, J.G.; Panitchpakdi, M.; et al. Gastrointestinal Surgery for Inflammatory Bowel Disease Persistently Lowers Microbiota and Metabolome Diversity. Inflamm. Bowel Dis. 2021, 27, 603–616. [Google Scholar] [CrossRef] [PubMed]
- Murphy, P.B.; Khot, Z.; Vogt, K.N.; Ott, M.; Dubois, L. Quality of Life After Total Proctocolectomy With Ileostomy or IPAA: A Systematic Review. Dis. Colon. Rectum. 2015, 58, 899–908. [Google Scholar] [CrossRef] [PubMed]
- McDermott, F.D.; Heeney, A.; Kelly, M.E.; Steele, R.J.; Carlson, G.L.; Winter, D.C. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br. J. Surg. 2015, 102, 462–479. [Google Scholar] [CrossRef] [PubMed]
- Hansen, R.B.; Balachandran, R.; Valsamidis, T.N.; Iversen, L.H. The role of preoperative mechanical bowel preparation and oral antibiotics in prevention of anastomotic leakage following restorative resection for primary rectal cancer—A systematic review and meta-analysis. Int. J. Color. Dis. 2023, 38, 129. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, B.; Wei, Y. New understanding of gut microbiota and colorectal anastomosis leak: A collaborative review of the current concepts. Front. Cell. Infect. Microbiol. 2022, 12, 1022603. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Cui, H.; Wang, F.; Zhang, Y.; Xu, Q.; Liu, D.; Wang, K.; Hou, S. Role of gut microbiota in postoperative complications and prognosis of gastrointestinal surgery: A narrative review. Medicine 2022, 101, e29826. [Google Scholar] [CrossRef] [PubMed]
- Olivas, A.D.; Shogan, B.D.; Valuckaite, V.; Zaborin, A.; Belogortseva, N.; Musch, M.; Meyer, F.; Trimble, W.L.; An, G.; Gilbert, J.; et al. Intestinal tissues induce an SNP mutation in Pseudomonas aeruginosa that enhances its virulence: Possible role in anastomotic leak. PLoS ONE 2012, 7, e44326. [Google Scholar] [CrossRef] [PubMed]
- Shogan, B.D.; Belogortseva, N.; Luong, P.M.; Zaborin, A.; Lax, S.; Bethel, C.; Ward, M.; Muldoon, J.P.; Singer, M.; An, G.; et al. Collagen degradation and MMP9 activation by Enterococcus faecalis contribute to intestinal anastomotic leak. Sci. Transl. Med. 2015, 7, 286ra68. [Google Scholar] [CrossRef] [PubMed]
- Schardey, H.M.; Kamps, T.; Rau, H.G.; Gatermann, S.; Baretton, G.; Schildberg, F.W. Bacteria: A major pathogenic factor for anastomotic insufficiency. Antimicrob. Agents Chemother. 1994, 38, 2564–2567. [Google Scholar] [CrossRef] [PubMed]
- Hajjar, R.; Gonzalez, E.; Fragoso, G.; Oliero, M.; Alaoui, A.A.; Calvé, A.; Vennin Rendos, H.; Djediai, S.; Cuisiniere, T.; Laplante, P.; et al. Gut microbiota influence anastomotic healing in colorectal cancer surgery through modulation of mucosal proinflammatory cytokines. Gut 2023, 72, 1143–1154. [Google Scholar] [CrossRef] [PubMed]
- Hernández-González, P.I.; Barquín, J.; Ortega-Ferrete, A.; Patón, V.; Ponce-Alonso, M.; Romero-Hernández, B.; Ocaña, J.; Caminoa, A.; Conde-Moreno, E.; Galeano, J.; et al. Anastomotic leak in colorectal cancer surgery: Contribution of gut microbiota and prediction approaches. Color. Dis. 2023, 25, 2187–2197. [Google Scholar] [CrossRef] [PubMed]
- Palmisano, S.; Campisciano, G.; Iacuzzo, C.; Bonadio, L.; Zucca, A.; Cosola, D.; Comar, M.; de Manzini, N. Role of preoperative gut microbiota on colorectal anastomotic leakage: Preliminary results. Updates Surg. 2020, 72, 1013–1022. [Google Scholar] [CrossRef] [PubMed]
- Lehr, K.; Lange, U.G.; Hipler, N.M.; Vilchez-Vargas, R.; Hoffmeister, A.; Feisthammel, J.; Buchloh, D.; Schanze, D.; Zenker, M.; Gockel, I.; et al. Prediction of anastomotic insufficiency based on the mucosal microbiota prior to colorectal surgery: A proof-of-principle study. Sci. Rep. 2024, 14, 15335. [Google Scholar] [CrossRef] [PubMed]
- Lianos, G.D.; Frountzas, M.; Kyrochristou, I.D.; Sakarellos, P.; Tatsis, V.; Kyrochristou, G.D.; Bali, C.D.; Gazouli, M.; Mitsis, M.; Schizas, D. What Is the Role of the Gut Microbiota in Anastomotic Leakage After Colorectal Resection? A Scoping Review of Clinical and Experimental Studies. J. Clin. Med. 2024, 13, 6634. [Google Scholar] [CrossRef] [PubMed]
- El-Hussuna, A.; Qvist, N.; Zangenberg, M.S.; Langkilde, A.; Siersma, V.; Hjort, S.; Gögenur, I. No effect of anti-TNF-α agents on the surgical stress response in patients with inflammatory bowel disease undergoing bowel resections: A prospective multi-center pilot study. BMC Surg. 2018, 18, 91. [Google Scholar] [CrossRef] [PubMed]
- Shwaartz, C.; Fields, A.C.; Sobrero, M.; Cohen, B.D.; Divino, C.M. Effect of Anti-TNF Agents on Postoperative Outcomes in Inflammatory Bowel Disease Patients: A Single Institution Experience. J. Gastrointest. Surg. 2016, 20, 1636–1642. [Google Scholar] [CrossRef] [PubMed]
- El-Hussuna, A.; Andersen, J.; Bisgaard, T.; Jess, P.; Henriksen, M.; Oehlenschlager, J.; Thorlacius-Ussing, O.; Olaison, G. Biologic treatment or immunomodulation is not associated with postoperative anastomotic complications in abdominal surgery for Crohn’s disease. Scand. J. Gastroenterol. 2012, 47, 662–668. [Google Scholar] [CrossRef] [PubMed]
- Kunitake, H.; Hodin, R.; Shellito, P.C.; Sands, B.E.; Korzenik, J.; Bordeianou, L. Perioperative treatment with infliximab in patients with Crohn’s disease and ulcerative colitis is not associated with an increased rate of postoperative complications. J. Gastrointest. Surg. 2008, 12, 1730–1737. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, G.; Qian, H.; Bressler, B. The risks of post-operative complications following pre-operative infliximab therapy for Crohn’s disease in patients undergoing abdominal surgery: A systematic review and meta-analysis. J. Crohn’s Colitis 2013, 7, 868–877. [Google Scholar] [CrossRef] [PubMed]
- Alsaleh, A.; Gaidos, J.K.; Kang, L.; Kuemmerle, J.F. Timing of Last Preoperative Dose of Infliximab Does Not Increase Postoperative Complications in Inflammatory Bowel Disease Patients. Dig. Dis. Sci. 2016, 61, 2602–2607. [Google Scholar] [CrossRef] [PubMed]
- Gaines, S.; Hyoju, S.; Williamson, A.J.; van Praagh, J.B.; Zaborina, O.; Rubin, D.T.; Alverdy, J.C.; Shogan, B.D.; Hyman, N. Infliximab Does Not Promote the Presence of Collagenolytic Bacteria in a Mouse Model of Colorectal Anastomosis. J. Gastrointest. Surg. 2020, 24, 2637–2642. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).