Serum Levels of Adiponectin Are Strongly Associated with Lipoprotein Subclasses in Healthy Volunteers but Not in Patients with Metabolic Syndrome
Abstract
1. Introduction
2. Results
2.1. Demographic and Clinical Characteristics and Laboratory Data in HVs and Patients with MS
2.2. Correlation Analyses between Adiponectin and the Serum Levels of VLDL, IDL, and LDL
2.3. Correlation Analyses between Adiponectin and the Serum Levels of HDL
2.4. Associations of Lipoprotein Parameters with Low and High Adiponectin Levels in HVs and Patients with MS
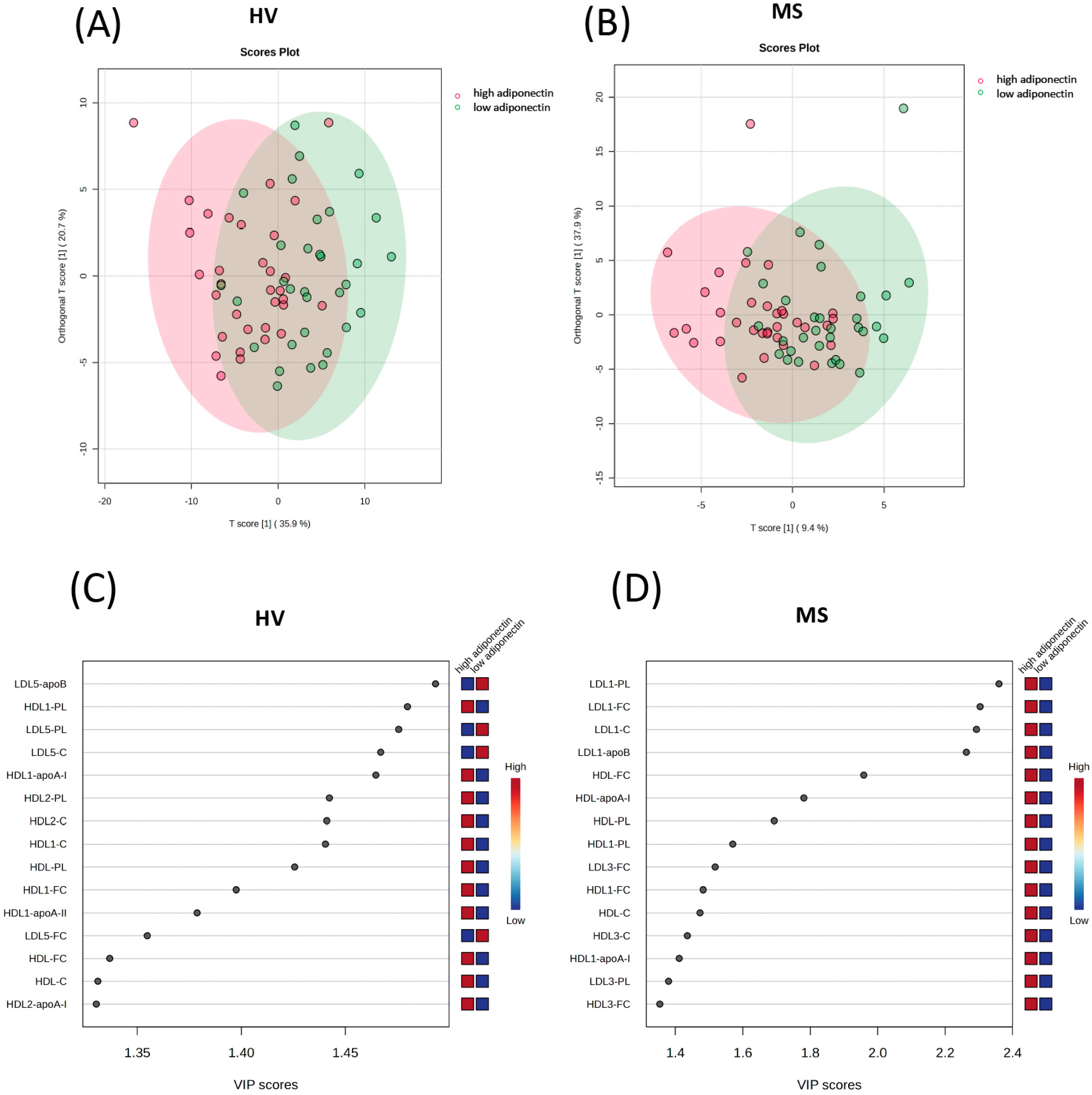
2.4.1. Orthogonal Partial Least-Squares Discriminant Analysis (OPLS-DA)
2.4.2. Logistic Regression Analysis
3. Discussion
4. Materials and Methods
4.1. Study Design, Participants, and Routine Laboratory Procedures
4.2. Adiponectin Measurements
4.3. Lipoprotein Profiling Using Nuclear Magnetic Resonance (NMR) Spectroscopy
4.4. Statistics
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kahn, B.B.; Flier, J.S. Obesity and insulin resistance. J. Clin. Investig. 2000, 106, 473–481. [Google Scholar] [CrossRef]
- Fujioka, S.; Matsuzawa, Y.; Tokunaga, K.; Tarui, S. Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metab. Clin. Exp. 1987, 36, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar]
- Choubey, M.; Ranjan, A.; Krishna, A. Adiponectin/AdipoRs signaling as a key player in testicular aging and associated metabolic disorders. Vitam. Horm. 2021, 115, 611–634. [Google Scholar] [PubMed]
- Dai, W.; Choubey, M.; Patel, S.; Singer, H.A.; Ozcan, L. Adipocyte CAMK2 deficiency improves obesity-associated glucose intolerance. Mol. Metab. 2021, 53, 101300. [Google Scholar] [CrossRef] [PubMed]
- Adiels, M.; Olofsson, S.O.; Taskinen, M.R.; Boren, J. Overproduction of very low-density lipoproteins is the hallmark of the dyslipidemia in the metabolic syndrome. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 1225–1236. [Google Scholar] [CrossRef]
- Hirano, T. Pathophysiology of Diabetic Dyslipidemia. J. Atheroscler. Thromb. 2018, 25, 771–782. [Google Scholar] [CrossRef]
- Christou, G.A.; Kiortsis, D.N. Adiponectin and lipoprotein metabolism. Obes. Rev. 2013, 14, 939–949. [Google Scholar] [CrossRef]
- Hafiane, A.; Gasbarrino, K.; Daskalopoulou, S.S. The role of adiponectin in cholesterol efflux and HDL biogenesis and metabolism. Metab. Clin. Exp. 2019, 100, 153953. [Google Scholar] [CrossRef]
- Zocchi, M.; Della Porta, M.; Lombardoni, F.; Scrimieri, R.; Zuccotti, G.V.; Maier, J.A.; Cazzola, R. A Potential Interplay between HDLs and Adiponectin in Promoting Endothelial Dysfunction in Obesity. Biomedicines 2022, 10, 1344. [Google Scholar] [CrossRef]
- Lara-Castro, C.; Fu, Y.; Chung, B.H.; Garvey, W.T. Adiponectin and the metabolic syndrome: Mechanisms mediating risk for metabolic and cardiovascular disease. Curr. Opin. Lipidol. 2007, 18, 263–270. [Google Scholar] [CrossRef]
- Yanai, H.; Yoshida, H. Beneficial Effects of Adiponectin on Glucose and Lipid Metabolism and Atherosclerotic Progression: Mechanisms and Perspectives. Int. J. Mol. Sci. 2019, 20, 1190. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Choubey, M.; Bora, P.; Krishna, A. Adiponectin and Chemerin: Contrary Adipokines in Regulating Reproduction and Metabolic Disorders. Reprod. Sci. 2018, 25, 1462–1473. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, M.; Shimomura, I. Roles of adiponectin and oxidative stress in obesity-associated metabolic and cardiovascular diseases. Rev. Endocr. Metab. Disord. 2014, 15, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, T.; Kamon, J.; Minokoshi, Y.; Ito, Y.; Waki, H.; Uchida, S.; Yamashita, S.; Noda, M.; Kita, S.; Ueki, K.; et al. Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat. Med. 2002, 8, 1288–1295. [Google Scholar] [CrossRef] [PubMed]
- Ceddia, R.B.; Somwar, R.; Maida, A.; Fang, X.; Bikopoulos, G.; Sweeney, G. Globular adiponectin increases GLUT4 translocation and glucose uptake but reduces glycogen synthesis in rat skeletal muscle cells. Diabetologia 2005, 48, 132–139. [Google Scholar] [CrossRef]
- Combs, T.P.; Berg, A.H.; Obici, S.; Scherer, P.E.; Rossetti, L. Endogenous glucose production is inhibited by the adipose-derived protein Acrp30. J. Clin. Investig. 2001, 108, 1875–1881. [Google Scholar] [CrossRef] [PubMed]
- Combs, T.P.; Marliss, E.B. Adiponectin signaling in the liver. Rev. Endocr. Metab. Disord. 2014, 15, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Berg, A.H.; Combs, T.P.; Du, X.; Brownlee, M.; Scherer, P.E. The adipocyte-secreted protein Acrp30 enhances hepatic insulin action. Nat. Med. 2001, 7, 947–953. [Google Scholar] [CrossRef]
- Christou, G.A.; Tellis, K.C.; Elisaf, M.C.; Tselepis, A.D.; Kiortsis, D.N. High density lipoprotein is positively correlated with the changes in circulating total adiponectin and high molecular weight adiponectin during dietary and fenofibrate treatment. Hormones 2012, 11, 178–188. [Google Scholar] [CrossRef]
- Riestra, P.; Garcia-Anguita, A.; Lasuncion, M.A.; Cano, B.; de Oya, M.; Garces, C. Relationship of adiponectin with metabolic syndrome components in pubertal children. Atherosclerosis 2011, 216, 467–470. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.J.; Kim, O.Y. Plasma adiponectin is associated with less atherogenic lipoprotein phenotype. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 770–775. [Google Scholar] [CrossRef] [PubMed]
- Tsubakio-Yamamoto, K.; Sugimoto, T.; Nishida, M.; Okano, R.; Monden, Y.; Kitazume-Taneike, R.; Yamashita, T.; Nakaoka, H.; Kawase, R.; Yuasa-Kawase, M.; et al. Serum adiponectin level is correlated with the size of HDL and LDL particles determined by high performance liquid chromatography. Metab. Clin. Exp. 2012, 61, 1763–1770. [Google Scholar] [CrossRef] [PubMed]
- Qiao, L.; Zou, C.; van der Westhuyzen, D.R.; Shao, J. Adiponectin reduces plasma triglyceride by increasing VLDL triglyceride catabolism. Diabetes 2008, 57, 1824–1833. [Google Scholar] [CrossRef] [PubMed]
- Weiss, R.; Otvos, J.D.; Flyvbjerg, A.; Miserez, A.R.; Frystyk, J.; Sinnreich, R.; Kark, J.D. Adiponectin and lipoprotein particle size. Diabetes Care 2009, 32, 1317–1319. [Google Scholar] [CrossRef]
- Oku, H.; Matsuura, F.; Koseki, M.; Sandoval, J.C.; Yuasa-Kawase, M.; Tsubakio-Yamamoto, K.; Masuda, D.; Maeda, N.; Ohama, T.; Ishigami, M.; et al. Adiponectin deficiency suppresses ABCA1 expression and ApoA-I synthesis in the liver. FEBS Lett. 2007, 581, 5029–5033. [Google Scholar] [CrossRef] [PubMed]
- Verges, B.; Petit, J.M.; Duvillard, L.; Dautin, G.; Florentin, E.; Galland, F.; Gambert, P. Adiponectin is an important determinant of apoA-I catabolism. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 1364–1369. [Google Scholar] [CrossRef] [PubMed]
- von Eynatten, M.; Schneider, J.G.; Humpert, P.M.; Rudofsky, G.; Schmidt, N.; Barosch, P.; Hamann, A.; Morcos, M.; Kreuzer, J.; Bierhaus, A.; et al. Decreased plasma lipoprotein lipase in hypoadiponectinemia: An association independent of systemic inflammation and insulin resistance. Diabetes Care 2004, 27, 2925–2929. [Google Scholar] [CrossRef] [PubMed]
- Matsuura, F.; Oku, H.; Koseki, M.; Sandoval, J.C.; Yuasa-Kawase, M.; Tsubakio-Yamamoto, K.; Masuda, D.; Maeda, N.; Tsujii, K.; Ishigami, M.; et al. Adiponectin accelerates reverse cholesterol transport by increasing high density lipoprotein assembly in the liver. Biochem. Biophys. Res. Commun. 2007, 358, 1091–1095. [Google Scholar] [CrossRef]
- Chan, D.C.; Barrett, P.H.; Ooi, E.M.; Ji, J.; Chan, D.T.; Watts, G.F. Very low density lipoprotein metabolism and plasma adiponectin as predictors of high-density lipoprotein apolipoprotein A-I kinetics in obese and nonobese men. J. Clin. Endocrinol. Metab. 2009, 94, 989–997. [Google Scholar] [CrossRef]
- Schneider, J.G.; von Eynatten, M.; Schiekofer, S.; Nawroth, P.P.; Dugi, K.A. Low plasma adiponectin levels are associated with increased hepatic lipase activity in vivo. Diabetes Care 2005, 28, 2181–2186. [Google Scholar] [CrossRef] [PubMed]
- Loucif, Y.; Methot, J.; Tremblay, K.; Brisson, D.; Gaudet, D. Contribution of adiponectin to the cardiometabolic risk of postmenopausal women with loss-of-function lipoprotein lipase gene mutations. Menopause 2011, 18, 558–562. [Google Scholar] [CrossRef] [PubMed]
- Strauss, J.G.; Frank, S.; Kratky, D.; Hammerle, G.; Hrzenjak, A.; Knipping, G.; von Eckardstein, A.; Kostner, G.M.; Zechner, R. Adenovirus-mediated rescue of lipoprotein lipase-deficient mice. Lipolysis of triglyceride-rich lipoproteins is essential for high density lipoprotein maturation in mice. J. Biol. Chem. 2001, 276, 36083–36090. [Google Scholar] [CrossRef] [PubMed]
- Pilz, S.; Horejsi, R.; Moller, R.; Almer, G.; Scharnagl, H.; Stojakovic, T.; Dimitrova, R.; Weihrauch, G.; Borkenstein, M.; Maerz, W.; et al. Early atherosclerosis in obese juveniles is associated with low serum levels of adiponectin. J. Clin. Endocrinol. Metab. 2005, 90, 4792–4796. [Google Scholar] [CrossRef] [PubMed]
- Magge, S.N.; Stettler, N.; Koren, D.; Levitt Katz, L.E.; Gallagher, P.R.; Mohler, E.R., 3rd; Rader, D.J. Adiponectin is associated with favorable lipoprotein profile, independent of BMI and insulin resistance, in adolescents. J. Clin. Endocrinol. Metab. 2011, 96, 1549–1554. [Google Scholar] [CrossRef] [PubMed]
- Hallikainen, M.; Kolehmainen, M.; Schwab, U.; Laaksonen, D.E.; Niskanen, L.; Rauramaa, R.; Pihlajamaki, J.; Uusitupa, M.; Miettinen, T.A.; Gylling, H. Serum adipokines are associated with cholesterol metabolism in the metabolic syndrome. Clin. Chim. Acta 2007, 383, 126–132. [Google Scholar] [CrossRef]
- Okada, T.; Saito, E.; Kuromori, Y.; Miyashita, M.; Iwata, F.; Hara, M.; Harada, K. Relationship between serum adiponectin level and lipid composition in each lipoprotein fraction in adolescent children. Atherosclerosis 2006, 188, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Tomono, Y.; Hiraishi, C.; Yoshida, H. Age and sex differences in serum adiponectin and its association with lipoprotein fractions. Ann. Clin. Biochem. 2018, 55, 165–171. [Google Scholar] [CrossRef]
- Shirakawa, T.; Nakajima, K.; Yatsuzuka, S.; Shimomura, Y.; Kobayashi, J.; Machida, T.; Sumino, H.; Murakami, M. The role of circulating lipoprotein lipase and adiponectin on the particle size of remnant lipoproteins in patients with diabetes mellitus and metabolic syndrome. Clin. Chim. Acta 2015, 440, 123–132. [Google Scholar] [CrossRef]
- Ryo, M.; Nakamura, T.; Kihara, S.; Kumada, M.; Shibazaki, S.; Takahashi, M.; Nagai, M.; Matsuzawa, Y.; Funahashi, T. Adiponectin as a biomarker of the metabolic syndrome. Circ. J. 2004, 68, 975–981. [Google Scholar] [CrossRef]
- Martin, L.J.; Woo, J.G.; Daniels, S.R.; Goodman, E.; Dolan, L.M. The relationships of adiponectin with insulin and lipids are strengthened with increasing adiposity. J. Clin. Endocrinol. Metab. 2005, 90, 4255–4259. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.C.; Watts, G.F.; Ooi, E.M.; Chan, D.T.; Wong, A.T.; Barrett, P.H. Apolipoprotein A-II and adiponectin as determinants of very low-density lipoprotein apolipoprotein B-100 metabolism in nonobese men. Metab. Clin. Exp. 2011, 60, 1482–1487. [Google Scholar] [CrossRef] [PubMed]
- Klobucar, I.; Stadler, J.T.; Klobucar, L.; Lechleitner, M.; Trbusic, M.; Pregartner, G.; Berghold, A.; Habisch, H.; Madl, T.; Marsche, G.; et al. Associations between Endothelial Lipase, High-Density Lipoprotein, and Endothelial Function Differ in Healthy Volunteers and Metabolic Syndrome Patients. Int. J. Mol. Sci. 2023, 24, 2073. [Google Scholar] [CrossRef] [PubMed]
- Klobucar, I.; Klobucar, L.; Lechleitner, M.; Trbusic, M.; Pregartner, G.; Berghold, A.; Habisch, H.; Madl, T.; Frank, S.; Degoricija, V. Associations between Endothelial Lipase and Apolipoprotein B-Containing Lipoproteins Differ in Healthy Volunteers and Metabolic Syndrome Patients. Int. J. Mol. Sci. 2023, 24, 10681. [Google Scholar] [CrossRef] [PubMed]
- Lucero, D.; Zago, V.; Lopez, G.H.; Cacciagiu, L.; Lopez, G.I.; Wikinski, R.; Nakajima, K.; Schreier, L. Predominance of large VLDL particles in metabolic syndrome, detected by size exclusion liquid chromatography. Clin. Biochem. 2012, 45, 293–297. [Google Scholar] [CrossRef]
- Brudasca, I.; Cucuianu, M. Pathogenic role of abnormal fatty acids and adipokines in the portal flow. Relevance for metabolic syndrome, hepatic steatosis and steatohepatitis. Rom. J. Intern. Med. 2007, 45, 149–157. [Google Scholar] [PubMed]
- Ng, T.W.; Watts, G.F.; Farvid, M.S.; Chan, D.C.; Barrett, P.H. Adipocytokines and VLDL metabolism: Independent regulatory effects of adiponectin, insulin resistance, and fat compartments on VLDL apolipoprotein B-100 kinetics? Diabetes 2005, 54, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Rashid, S.; Watanabe, T.; Sakaue, T.; Lewis, G.F. Mechanisms of HDL lowering in insulin resistant, hypertriglyceridemic states: The combined effect of HDL triglyceride enrichment and elevated hepatic lipase activity. Clin. Biochem. 2003, 36, 421–429. [Google Scholar] [CrossRef] [PubMed]
- James, R.W.; Hochstrasser, D.; Tissot, J.D.; Funk, M.; Appel, R.; Barja, F.; Pellegrini, C.; Muller, A.F.; Pometta, D. Protein heterogeneity of lipoprotein particles containing apolipoprotein A-I without apolipoprotein A-II and apolipoprotein A-I with apolipoprotein A-II isolated from human plasma. J. Lipid Res. 1988, 29, 1557–1571. [Google Scholar] [CrossRef]
- Rosenson, R.S.; Brewer, H.B., Jr.; Chapman, M.J.; Fazio, S.; Hussain, M.M.; Kontush, A.; Krauss, R.M.; Otvos, J.D.; Remaley, A.T.; Schaefer, E.J. HDL measures, particle heterogeneity, proposed nomenclature, and relation to atherosclerotic cardiovascular events. Clin. Chem. 2011, 57, 392–410. [Google Scholar] [CrossRef]
- Cnop, M.; Havel, P.J.; Utzschneider, K.M.; Carr, D.B.; Sinha, M.K.; Boyko, E.J.; Retzlaff, B.M.; Knopp, R.H.; Brunzell, J.D.; Kahn, S.E. Relationship of adiponectin to body fat distribution, insulin sensitivity and plasma lipoproteins: Evidence for independent roles of age and sex. Diabetologia 2003, 46, 459–469. [Google Scholar] [CrossRef]
- Stadler, J.T.; Lackner, S.; Morkl, S.; Trakaki, A.; Scharnagl, H.; Borenich, A.; Wonisch, W.; Mangge, H.; Zelzer, S.; Meier-Allard, N.; et al. Obesity Affects HDL Metabolism, Composition and Subclass Distribution. Biomedicines 2021, 9, 242. [Google Scholar] [CrossRef] [PubMed]
- Mester, P.; Rath, U.; Schmid, S.; Muller, M.; Buechler, C.; Pavel, V. Exploring the Relationship between Plasma Adiponectin, Gender, and Underlying Diseases in Severe Illness. Biomedicines 2023, 11, 3287. [Google Scholar] [CrossRef]
- Boren, J.; Chapman, M.J.; Krauss, R.M.; Packard, C.J.; Bentzon, J.F.; Binder, C.J.; Daemen, M.J.; Demer, L.L.; Hegele, R.A.; Nicholls, S.J.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: Pathophysiological, genetic, and therapeutic insights: A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2020, 41, 2313–2330. [Google Scholar] [CrossRef]
- Balling, M.; Nordestgaard, B.G.; Langsted, A.; Varbo, A.; Kamstrup, P.R.; Afzal, S. Small Dense Low-Density Lipoprotein Cholesterol Predicts Atherosclerotic Cardiovascular Disease in the Copenhagen General Population Study. J. Am. Coll. Cardiol. 2020, 75, 2873–2875. [Google Scholar] [CrossRef]
- Balling, M.; Afzal, S.; Varbo, A.; Langsted, A.; Davey Smith, G.; Nordestgaard, B.G. VLDL Cholesterol Accounts for One-Half of the Risk of Myocardial Infarction Associated With apoB-Containing Lipoproteins. J. Am. Coll. Cardiol. 2020, 76, 2725–2735. [Google Scholar] [CrossRef]
- Kontush, A. HDL particle number and size as predictors of cardiovascular disease. Front. Pharmacol. 2015, 6, 218. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Wiley, J.F.; Carrington, M.J. A metabolic syndrome severity score: A tool to quantify cardio-metabolic risk factors. Prev. Med. 2016, 88, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Maher, A.D.; Crockford, D.; Toft, H.; Malmodin, D.; Faber, J.H.; McCarthy, M.I.; Barrett, A.; Allen, M.; Walker, M.; Holmes, E.; et al. Optimization of human plasma 1H NMR spectroscopic data processing for high-throughput metabolic phenotyping studies and detection of insulin resistance related to type 2 diabetes. Anal. Chem. 2008, 80, 7354–7362. [Google Scholar] [CrossRef]
- Blaise, B.J.; Correia, G.D.S.; Haggart, G.A.; Surowiec, I.; Sands, C.; Lewis, M.R.; Pearce, J.T.M.; Trygg, J.; Nicholson, J.K.; Holmes, E.; et al. Statistical analysis in metabolic phenotyping. Nat. Protoc. 2021, 16, 4299–4326. [Google Scholar] [CrossRef] [PubMed]
- Pang, Z.; Chong, J.; Zhou, G.; de Lima Morais, D.A.; Chang, L.; Barrette, M.; Gauthier, C.; Jacques, P.E.; Li, S.; Xia, J. MetaboAnalyst 5.0: Narrowing the gap between raw spectra and functional insights. Nucleic Acids Res. 2021, 49, W388–W396. [Google Scholar] [CrossRef] [PubMed]
- Thevenot, E.A.; Roux, A.; Xu, Y.; Ezan, E.; Junot, C. Analysis of the Human Adult Urinary Metabolome Variations with Age, Body Mass Index, and Gender by Implementing a Comprehensive Workflow for Univariate and OPLS Statistical Analyses. J. Proteome Res. 2015, 14, 3322–3335. [Google Scholar] [CrossRef] [PubMed]

| Variable | All (N = 130) | HV (N = 65) | MS (N = 65) | p |
|---|---|---|---|---|
| Age (years) | 56.0 (50.0, 60.0) | 56.0 (50.0, 59.0) | 57.0 (50.0, 60.0) | 0.440 |
| Sex (female) | 62 (47.7%) | 31 (47.7%) | 31 (47.7%) | 1.000 |
| Body weight (kg) | 87.5 (75.2, 102.8) | 77.0 (68.0, 88.0) | 98.0 (86.0, 113.5) | <0.001 |
| Body height (m) | 1.74 ± 0.10 | 1.75 ± 0.10 | 1.73 ± 0.11 | 0.243 |
| BMI (kg/m2) | 28.8 (25.1, 32.7) | 25.1 (23.7, 28.1) | 32.6 (29.8, 35.9) | <0.001 |
| Waist circumference (cm) | 103.1 ± 16.5 | 92.2 ± 11.6 | 113.9 ± 13.2 | <0.001 |
| SBP (mmHg) | 130.0 (120.0, 140.0) | 120.0 (115.0, 130.0) | 140.0 (130.0, 145.0) | <0.001 |
| DBP (mmHg) | 80.0 (70.0, 80.0) | 70.0 (70.0, 80.0) | 80.0 (70.0, 80.0) | <0.001 |
| MAP (mmHg) | 96.7 (88.3, 100.0) | 88.3 (85.0, 96.7) | 98.3 (96.7, 101.7) | <0.001 |
| MetSSS | 2.4 (0.8, 4.2) | 0.7 (0.0, 2.3) | 3.8 (2.6, 4.8) | <0.001 |
| Chronic diseases | ||||
| Arterial hypertension | 60 (46.2%) | 0 (0.0%) | 60 (92.3%) | <0.001 |
| Diabetes mellitus type 2 | 27 (20.8%) | 0 (0.0%) | 27 (41.5%) | <0.001 |
| Stable angina pectoris | 2 (1.5%) | 0 (0.0%) | 2 (3.1%) | 0.496 |
| Atrial fibrillation | 2 (1.5%) | 0 (0.0%) | 2 (3.1%) | 0.496 |
| CVI and TIA | 1 (0.8%) | 0 (0.0%) | 1 (1.5%) | 1.000 |
| Intermittent claudications | 4 (3.1%) | 0 (0.0%) | 4 (6.2%) | 0.119 |
| Deep venous thrombosis | 6 (4.6%) | 1 (1.5%) | 5 (7.7%) | 0.208 |
| Pulmonary embolism | 2 (1.5%) | 0 (0.0%) | 2 (3.1%) | 0.496 |
| Functions and habits | ||||
| Smoking | 34 (26.2%) | 16 (24.6%) | 18 (27.7%) | 0.842 |
| Physical activity (≥3 times/week) | 105 (80.8%) | 58 (89.2%) | 47 (72.3%) | 0.025 |
| Menstrual cycle (female) | 18/62 (29.0%) | 12/31 (38.7%) | 6/31 (19.4%) | 0.161 |
| Variable | All (N = 130) | HV (N = 65) | MS (N = 65) | p |
|---|---|---|---|---|
| Adiponectin (µg/mL) | 14.0 (10.4, 19.4) | 15.1 (11.6, 22.2) | 13.0 (9.9, 17.2) | 0.006 |
| Triglycerides (mmol/L) | 1.3 (0.9, 1.9) | 1.0 (0.8, 1.4) | 1.6 (1.1, 2.2) | <0.001 |
| Total cholesterol (mmol/L) | 5.3 (4.7, 6.1) | 5.5 (5.1, 6.0) | 5.0 (4.3, 6.2) | 0.057 |
| LDL-C (mmol/L) | 3.2 (2.5, 3.7) | 3.3 (2.8, 3.7) | 3.0 (2.3, 3.7) | 0.077 |
| HDL-C (mmol/L) | 1.4 (1.1, 1.7) | 1.6 (1.4, 1.8) | 1.2 (1.0, 1.4) | <0.001 |
| Glucose (mmol/L) | 5.3 (4.9, 5.7) | 4.9 (4.8, 5.2) | 5.7 (5.3, 6.5) | <0.001 |
| Protein (g/L) | 73.0 (70.0, 76.0) | 72.0 (69.0, 75.0) | 75.0 (71.0, 77.0) | 0.002 |
| Albumin (g/L) | 48.0 (46.0, 49.0) | 47.0 (46.0, 49.0) | 48.0 (45.0, 49.0) | 0.465 |
| CRP (µg/mL) | 1.8 (0.8, 3.7) | 1.2 (0.6, 2.3) | 2.4 (1.2, 5.5) | <0.001 |
| IL-6 (pg/mL) | 3.0 (2.1, 5.3) | 2.3 (1.7, 3.0) | 4.1 (2.7, 6.8) | <0.001 |
| Bilirubin (µmol/L) | 8.5 (6.0, 11.6) | 9.6 (7.4, 13.3) | 7.4 (5.5, 10.4) | 0.012 |
| AST (U/L) | 23.0 (20.0, 27.0) | 23.0 (20.0, 25.0) | 23.0 (19.0, 32.0) | 0.244 |
| ALT (U/L) | 24.0 (19.0, 36.0) | 22.0 (18.0, 29.0) | 30.0 (22.0, 43.0) | <0.001 |
| AP (U/L) | 61.0 (51.0, 73.0) | 60.0 (49.0, 70.0) | 65.0 (52.0, 81.0) | 0.065 |
| GGT (U/L) | 24.5 (15.2, 38.0) | 16.0 (13.0, 30.0) | 31.0 (21.0, 44.0) | <0.001 |
| CK (U/L) | 124.5 (83.0, 186.8) | 115.0 (81.0, 153.0) | 133.0 (86.0, 226.0) | 0.048 |
| LDH (U/L) | 172.0 (150.5, 192.0) | 168.0 (147.0, 191.0) | 176.0 (158.0, 193.0) | 0.365 |
| Urea (mmol/L) | 5.3 (4.5, 6.3) | 5.0 (4.2, 6.0) | 5.6 (4.8, 6.5) | 0.004 |
| Urate (µmol/L) | 297.5 (249.9, 345.1) | 273.7 (232.0, 327.2) | 315.3 (279.7, 362.9) | <0.001 |
| Creatinine (µmol/L) | 77.9 (67.3, 87.6) | 77.9 (69.0, 89.4) | 76.6 (65.5, 87.0) | 0.414 |
| eGFR (mL/min/1.73 m2) | 88.0 (78.0, 97.1) | 87.5 (77.2, 93.6) | 88.9 (79.1, 98.0) | 0.358 |
| Sodium (mmol/L) | 139.0 (138.0, 141.0) | 140.0 (138.0, 141.0) | 139.0 (138.0, 140.0) | 0.041 |
| Potassium (mmol/L) | 4.2 (4.1, 4.6) | 4.3 (4.1, 4.5) | 4.2 (4.1, 4.6) | 0.703 |
| Chloride (mmol/L) | 100.0 (98.2, 102.8) | 101.0 (99.0, 103.0) | 100.0 (98.0, 101.0) | 0.006 |
| Adiponectin (µg/mL) | ||||
|---|---|---|---|---|
| HV (N = 65) | MS (N = 65) | |||
| Variable (mg/dL) | r | p | r | p |
| VLDL-C | −0.44 | 0.0003 | −0.15 | 0.2406 |
| VLDL1-C | −0.44 | 0.0002 | −0.18 | 0.1565 |
| VLDL2-C | −0.42 | 0.0005 | −0.16 | 0.2099 |
| VLDL3-C | −0.45 | 0.0002 | −0.15 | 0.2334 |
| VLDL4-C | −0.37 | 0.0021 | −0.09 | 0.4980 |
| VLDL5-C | 0.02 | 0.8480 | 0.19 | 0.1281 |
| VLDL-FC | −0.44 | 0.0003 | −0.15 | 0.2456 |
| VLDL1-FC | −0.52 | <0.0001 | −0.22 | 0.0724 |
| VLDL2-FC | −0.44 | 0.0002 | −0.21 | 0.0932 |
| VLDL3-FC | −0.43 | 0.0004 | −0.19 | 0.1381 |
| VLDL4-FC | −0.37 | 0.0025 | −0.08 | 0.5392 |
| VLDL5-FC | 0.02 | 0.8595 | −0.02 | 0.8983 |
| VLDL-TG | −0.51 | <0.0001 | −0.23 | 0.0625 |
| VLDL1-TG | −0.53 | <0.0001 | −0.27 | 0.0305 |
| VLDL2-TG | −0.48 | 0.0001 | −0.21 | 0.0957 |
| VLDL3-TG | −0.44 | 0.0003 | −0.18 | 0.1401 |
| VLDL4-TG | −0.40 | 0.0010 | −0.17 | 0.1778 |
| VLDL5-TG | 0.03 | 0.8010 | 0.05 | 0.6917 |
| VLDL-PL | −0.47 | 0.0001 | −0.22 | 0.0847 |
| VLDL1-PL | −0.55 | <0.0001 | −0.26 | 0.0335 |
| VLDL2-PL | −0.49 | <0.0001 | −0.22 | 0.0778 |
| VLDL3-PL | −0.45 | 0.0001 | −0.21 | 0.0942 |
| VLDL4-PL | −0.42 | 0.0005 | −0.14 | 0.2809 |
| VLDL5-PL | −0.10 | 0.4176 | 0.07 | 0.5612 |
| VLDL-apoB | −0.44 | 0.0002 | −0.18 | 0.1623 |
| Adiponectin (µg/mL) | ||||
|---|---|---|---|---|
| HV (N = 65) | MS (N = 65) | |||
| Variable (mg/dL) | r | p | r | p |
| IDL-C | −0.42 | 0.0005 | −0.07 | 0.5765 |
| IDL-FC | −0.43 | 0.0003 | −0.09 | 0.4883 |
| IDL-TG | −0.43 | 0.0004 | −0.16 | 0.1988 |
| IDL-PL | −0.41 | 0.0006 | −0.11 | 0.3826 |
| IDL-apoB | −0.39 | 0.0015 | −0.08 | 0.5405 |
| Adiponectin (µg/mL) | ||||
|---|---|---|---|---|
| HV (N = 65) | MS (N = 65) | |||
| Variable (mg/dL) | r | p | r | p |
| LDL-C | −0.17 | 0.1788 | 0.14 | 0.2695 |
| LDL1-C | 0.18 | 0.1421 | 0.40 | 0.0011 |
| LDL2-C | 0.29 | 0.0175 | 0.16 | 0.2032 |
| LDL3-C | 0.05 | 0.6650 | 0.24 | 0.0579 |
| LDL4-C | −0.44 | 0.0002 | 0.15 | 0.2264 |
| LDL5-C | −0.58 | <0.0001 | −0.05 | 0.7202 |
| LDL6-C | −0.39 | 0.0012 | −0.19 | 0.1245 |
| LDL-FC | −0.07 | 0.5977 | 0.19 | 0.1221 |
| LDL1-FC | 0.17 | 0.1826 | 0.39 | 0.0012 |
| LDL2-FC | 0.33 | 0.0072 | 0.19 | 0.1389 |
| LDL3-FC | 0.18 | 0.1521 | 0.28 | 0.0226 |
| LDL4-FC | −0.33 | 0.0075 | 0.22 | 0.0854 |
| LDL5-FC | −0.52 | <0.0001 | 0.04 | 0.7578 |
| LDL6-FC | −0.33 | 0.0076 | −0.14 | 0.2724 |
| LDL-TG | −0.19 | 0.1251 | 0.03 | 0.7852 |
| LDL1-TG | 0.00 | 0.9788 | 0.16 | 0.2032 |
| LDL2-TG | 0.16 | 0.2017 | 0.16 | 0.2084 |
| LDL3-TG | 0.17 | 0.1729 | 0.22 | 0.0752 |
| LDL4-TG | −0.37 | 0.0021 | 0.09 | 0.4614 |
| LDL5-TG | −0.47 | 0.0001 | −0.10 | 0.4094 |
| LDL6-TG | −0.17 | 0.1709 | −0.17 | 0.1716 |
| LDL-PL | −0.14 | 0.2730 | 0.21 | 0.0993 |
| LDL1-PL | 0.20 | 0.1185 | 0.42 | 0.0004 |
| LDL2-PL | 0.32 | 0.0090 | 0.20 | 0.1074 |
| LDL3-PL | 0.08 | 0.5141 | 0.27 | 0.0328 |
| LDL4-PL | −0.46 | 0.0001 | 0.16 | 0.2024 |
| LDL5-PL | −0.59 | <0.0001 | −0.02 | 0.9014 |
| LDL6-PL | −0.32 | 0.0083 | −0.17 | 0.1644 |
| LDL-apoB | −0.26 | 0.0384 | 0.09 | 0.4987 |
| LDL1-apoB | 0.21 | 0.0956 | 0.40 | 0.0010 |
| LDL2-apoB | 0.29 | 0.0182 | 0.16 | 0.2153 |
| LDL3-apoB | 0.04 | 0.7334 | 0.25 | 0.0444 |
| LDL4-apoB | −0.49 | <0.0001 | 0.14 | 0.2495 |
| LDL5-apoB | −0.58 | <0.0001 | −0.07 | 0.5689 |
| LDL6-apoB | −0.41 | 0.0007 | −0.18 | 0.1539 |
| Adiponectin (µg/mL) | ||||
|---|---|---|---|---|
| HV (N = 65) | MS (N = 65) | |||
| Variable (mg/dL) | r | p | r | p |
| HDL-C | 0.53 | <0.0001 | 0.32 | 0.0099 |
| HDL1-C | 0.58 | <0.0001 | 0.27 | 0.0304 |
| HDL2-C | 0.57 | <0.0001 | 0.38 | 0.0018 |
| HDL3-C | 0.40 | 0.0009 | 0.34 | 0.0057 |
| HDL4-C | −0.15 | 0.2239 | 0.13 | 0.3129 |
| HDL-FC | 0.55 | <0.0001 | 0.42 | 0.0005 |
| HDL1-FC | 0.52 | <0.0001 | 0.32 | 0.0087 |
| HDL2-FC | 0.47 | 0.0001 | 0.33 | 0.0065 |
| HDL3-FC | 0.20 | 0.1123 | 0.37 | 0.0027 |
| HDL4-FC | −0.14 | 0.2639 | 0.26 | 0.0385 |
| HDL-TG | 0.16 | 0.1958 | 0.24 | 0.0508 |
| HDL1-TG | 0.44 | 0.0002 | 0.30 | 0.0136 |
| HDL2-TG | 0.18 | 0.1434 | 0.23 | 0.0685 |
| HDL3-TG | −0.09 | 0.4864 | 0.10 | 0.4067 |
| HDL4-TG | −0.42 | 0.0005 | 0.00 | 0.9834 |
| HDL-PL | 0.59 | <0.0001 | 0.43 | 0.0004 |
| HDL1-PL | 0.61 | <0.0001 | 0.35 | 0.0042 |
| HDL2-PL | 0.59 | <0.0001 | 0.40 | 0.0011 |
| HDL3-PL | 0.42 | 0.0004 | 0.36 | 0.0030 |
| HDL4-PL | −0.11 | 0.3640 | 0.20 | 0.1132 |
| HDL-apoA-I | 0.49 | <0.0001 | 0.37 | 0.0022 |
| HDL1-apoA-I | 0.58 | <0.0001 | 0.33 | 0.0082 |
| HDL2-apoA-I | 0.54 | <0.0001 | 0.31 | 0.0110 |
| HDL3-apoA-I | 0.38 | 0.0021 | 0.32 | 0.0084 |
| HDL4-apoA-I | −0.22 | 0.0760 | 0.19 | 0.1328 |
| HDL-apoA-II | −0.06 | 0.6577 | 0.12 | 0.3386 |
| HDL1-apoA-II | 0.46 | 0.0001 | 0.20 | 0.1069 |
| HDL2-apoA-II | 0.36 | 0.0031 | 0.14 | 0.2698 |
| HDL3-apoA-II | −0.08 | 0.5036 | 0.13 | 0.2986 |
| HDL4-apoA-II | −0.37 | 0.0027 | 0.00 | 0.9822 |
| Adiponectin (µg/mL) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
| Variable (mg/dL) | r | p | r | p | r | p | r | p |
| HDL-C | 0.42 | 0.0007 | 0.42 | 0.0009 | 0.40 | 0.0015 | 0.34 | 0.0064 |
| HDL1-C | 0.44 | 0.0004 | 0.43 | 0.0005 | 0.42 | 0.0007 | 0.41 | 0.0009 |
| HDL2-C | 0.45 | 0.0003 | 0.45 | 0.0003 | 0.44 | 0.0004 | 0.39 | 0.0015 |
| HDL-FC | 0.40 | 0.0012 | 0.40 | 0.0015 | 0.38 | 0.0023 | 0.33 | 0.0080 |
| HDL1-FC | 0.38 | 0.0025 | 0.37 | 0.0030 | 0.35 | 0.0049 | 0.34 | 0.0076 |
| HDL2-FC | 0.33 | 0.0088 | 0.34 | 0.0077 | 0.31 | 0.0134 | 0.27 | 0.0334 |
| HDL1-TG | 0.19 | 0.1425 | 0.19 | 0.1515 | 0.17 | 0.1811 | 0.21 | 0.1045 |
| HDL-PL | 0.43 | 0.0006 | 0.43 | 0.0006 | 0.40 | 0.0012 | 0.36 | 0.0042 |
| HDL1-PL | 0.45 | 0.0002 | 0.45 | 0.0003 | 0.43 | 0.0005 | 0.43 | 0.0005 |
| HDL2-PL | 0.44 | 0.0004 | 0.44 | 0.0003 | 0.43 | 0.0006 | 0.40 | 0.0014 |
| HDL3-PL | 0.28 | 0.0283 | 0.28 | 0.0267 | 0.27 | 0.0366 | 0.21 | 0.1004 |
| HDL-apoA-I | 0.32 | 0.0110 | 0.32 | 0.0129 | 0.29 | 0.0225 | 0.24 | 0.0648 |
| HDL1-apoA-I | 0.41 | 0.0009 | 0.41 | 0.0011 | 0.39 | 0.0017 | 0.39 | 0.0016 |
| HDL2-apoA-I | 0.37 | 0.0027 | 0.37 | 0.0031 | 0.35 | 0.0057 | 0.32 | 0.0124 |
| HDL1-apoA-II | 0.28 | 0.0281 | 0.28 | 0.0319 | 0.25 | 0.0462 | 0.29 | 0.0231 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klobučar, I.; Habisch, H.; Klobučar, L.; Trbušić, M.; Pregartner, G.; Berghold, A.; Kostner, G.M.; Scharnagl, H.; Madl, T.; Frank, S.; et al. Serum Levels of Adiponectin Are Strongly Associated with Lipoprotein Subclasses in Healthy Volunteers but Not in Patients with Metabolic Syndrome. Int. J. Mol. Sci. 2024, 25, 5050. https://doi.org/10.3390/ijms25095050
Klobučar I, Habisch H, Klobučar L, Trbušić M, Pregartner G, Berghold A, Kostner GM, Scharnagl H, Madl T, Frank S, et al. Serum Levels of Adiponectin Are Strongly Associated with Lipoprotein Subclasses in Healthy Volunteers but Not in Patients with Metabolic Syndrome. International Journal of Molecular Sciences. 2024; 25(9):5050. https://doi.org/10.3390/ijms25095050
Chicago/Turabian StyleKlobučar, Iva, Hansjörg Habisch, Lucija Klobučar, Matias Trbušić, Gudrun Pregartner, Andrea Berghold, Gerhard M. Kostner, Hubert Scharnagl, Tobias Madl, Saša Frank, and et al. 2024. "Serum Levels of Adiponectin Are Strongly Associated with Lipoprotein Subclasses in Healthy Volunteers but Not in Patients with Metabolic Syndrome" International Journal of Molecular Sciences 25, no. 9: 5050. https://doi.org/10.3390/ijms25095050
APA StyleKlobučar, I., Habisch, H., Klobučar, L., Trbušić, M., Pregartner, G., Berghold, A., Kostner, G. M., Scharnagl, H., Madl, T., Frank, S., & Degoricija, V. (2024). Serum Levels of Adiponectin Are Strongly Associated with Lipoprotein Subclasses in Healthy Volunteers but Not in Patients with Metabolic Syndrome. International Journal of Molecular Sciences, 25(9), 5050. https://doi.org/10.3390/ijms25095050









