Unified Methodology for the Primary Preclinical In Vivo Screening of New Anticoagulant Pharmaceutical Agents from Hematophagous Organisms
Abstract
1. Introduction
2. Results
2.1. Assessment of Pharmacodynamic Profile
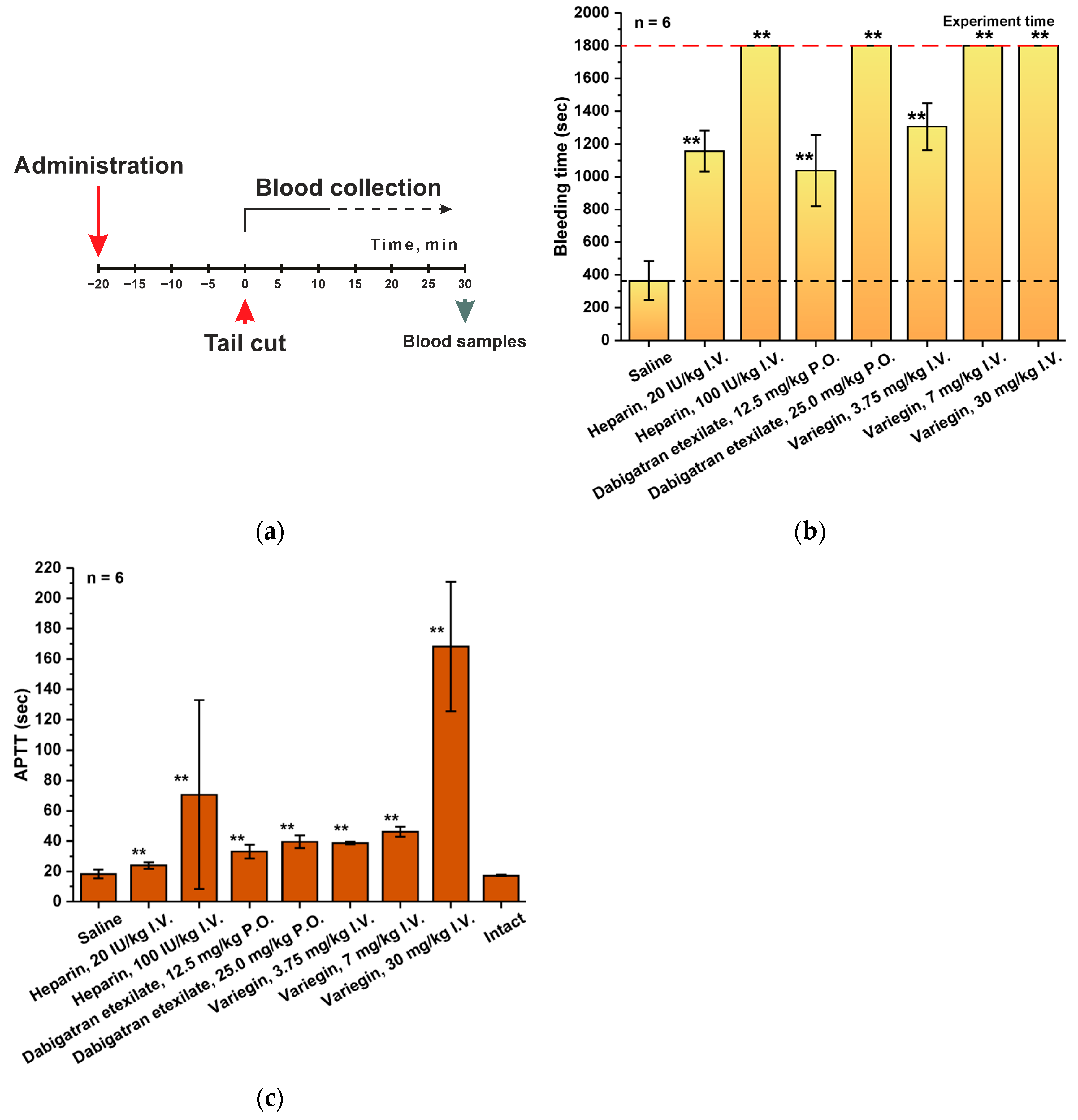
2.2. Rat Tail-Cut Bleeding Model
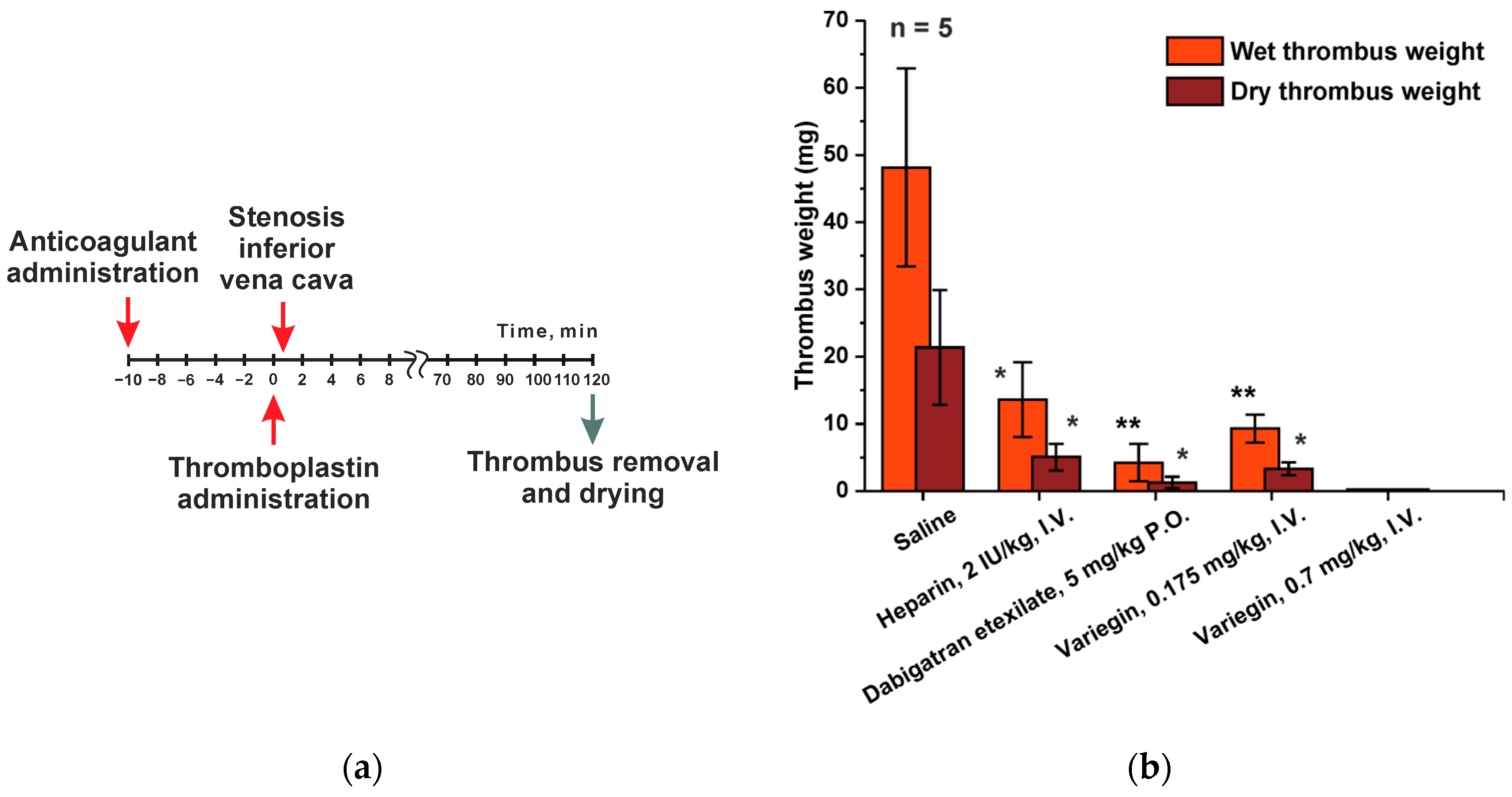
2.3. Rat Inferior Vena Cava (IVC) Incomplete Stenosis Model of Venous Thrombosis Associated with Hypercoagulation
3. Discussion
4. Materials and Methods
4.1. Reagents
4.2. Animals
4.3. Drugs Administration
4.4. Assessment of Pharmacodynamic Profile
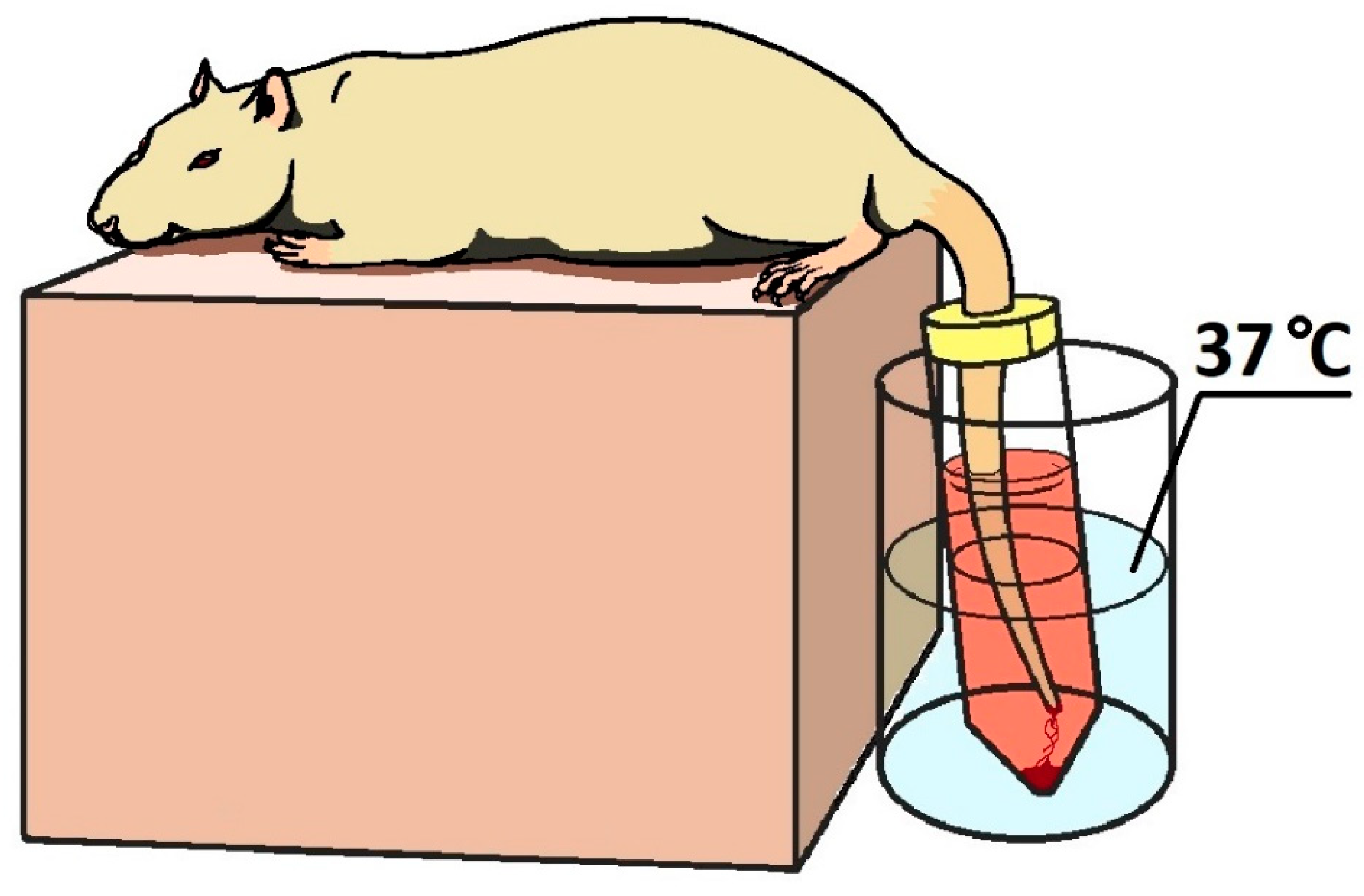
4.5. Tail-Cut Bleeding Model
4.6. Rat Inferior Vena Cava (IVC) Incomplete Stenosis Model of Venous Thrombosis
4.7. Blood Sample Analysis
4.8. Statistical Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hirsh, J.; Eikelboom, J.W.; Chan, N.C. Fifty years of research on antithrombotic therapy: Achievements and disappointments. Eur. J. Intern. Med. 2019, 70, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bartholomew, J.R. Update on the management of venous thromboembolism. Clevel. Clin. J. Med. 2017, 84 (Suppl. S3), 39–46. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.A. Antithrombotic therapy. Top. Companion Anim. Med. 2012, 27, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Chernysh, I.N.; Nagaswami, C.; Kosolapova, S.; Peshkova, A.D.; Cuker, A.; Cines, D.B.; Cambor, C.L.; Litvinov, R.I.; Weisel, J.W. The distinctive structure and composition of arterial and venous thrombi and pulmonary emboli. Sci. Rep. 2020, 10, 5112. [Google Scholar] [CrossRef] [PubMed]
- Franchini, M.; Mannucci, P.M. Venous and arterial thrombosis: Different sides of the same coin? Eur. J. Intern. Med. 2008, 19, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Chan, N.; Sobieraj-Teague, M.; Eikelboom, J.W. Direct oral anticoagulants: Evidence and unresolved issues. Lancet 2020, 396, 1767–1776. [Google Scholar] [CrossRef] [PubMed]
- Alquwaizani, M.; Buckley, L.; Adams, C.; Fanikos, J. Anticoagulants: A Review of the Pharmacology, Dosing, and Complications. Curr. Emerg. Hosp. Med. Rep. 2013, 1, 83–97. [Google Scholar] [CrossRef] [PubMed]
- Mulloy, B.; Hogwood, J.; Gray, E.; Lever, R.; Page, C.P. Pharmacology of Heparin and Related Drugs. Pharmacol. Rev. 2016, 68, 76–141. [Google Scholar] [CrossRef] [PubMed]
- Selleng, K.; Warkentin, T.E.; Greinacher, A. Heparin-induced thrombocytopenia in intensive care patients. Crit. Care Med. 2007, 35, 1165–1176. [Google Scholar] [CrossRef]
- Junqueira, D.R.; Zorzela, L.M.; Perini, E. Unfractionated heparin versus low molecular weight heparins for avoiding heparin-induced thrombocytopenia in postoperative patients. Cochrane Database Syst. Rev. 2017, 4, CD007557. [Google Scholar] [CrossRef]
- Junren, C.; Xiaofang, X.; Huiqiong, Z.; Gangmin, L.; Yanpeng, Y.; Xiaoyu, C.; Yuqing, G.; Yanan, L.; Yue, Z.; Fu, P.; et al. Pharmacological Activities and Mechanisms of Hirudin and Its Derivatives—A Review. Front. Pharmacol. 2021, 12, 660757. [Google Scholar] [CrossRef]
- Graetz, T.J.; Tellor, B.R.; Smith, J.R.; Avidan, M.S. Desirudin: A review of the pharmacology and clinical application for the prevention of deep vein thrombosis. Expert Rev. Cardiovasc. Ther. 2011, 9, 1101–1109. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, B.I.; Ekman, S.; Lindbratt, S.; Baur, M.; Bach, D.; Torholm, C.; Kälebo, P.; Close, P. Prevention of thromboembolism with use of recombinant hirudin. Results of a double-blind, multicenter trial comparing the efficacy of desirudin (Revasc) with that of unfractionated heparin in patients having a total hip replacement. J. Bone Jt. Surg. Am 1997, 79, 326–333. [Google Scholar] [CrossRef]
- Adkins, J.C.; Wilde, M.I. Lepirudin: A review of its potential place in the management of thrombotic disorders. BioDrugs 1998, 10, 227–255. [Google Scholar] [CrossRef]
- Lubenow, N.; Eichler, P.; Lietz, T.; Greinacher, A.; Group, H.I. Lepirudin in patients with heparin-induced thrombocytopenia—Results of the third prospective study (HAT-3) and a combined analysis of HAT-1, HAT-2, and HAT-3. J. Thromb. Haemost. 2005, 3, 2428–2436. [Google Scholar] [CrossRef] [PubMed]
- Grubb, K.J.; Salehi, P.; Chedrawy, E.G. Bivalirudin: Alternative anticoagulation during cardiopulmonary bypass in patients with heparin-induced thrombocytopenia. Recent Pat. Cardiovasc. Drug Discov. 2010, 5, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Jove, M.; Maslanka, M.; Minkowitz, H.S.; Jaffer, A.K.; Investigators, D.-A. Safety of desirudin in thrombosis prevention after total knee arthroplasty: The DESIR-ABLE study. Am. J. Ther. 2014, 21, 496–499. [Google Scholar] [CrossRef]
- Capranzano, P.; Dangas, G. Bivalirudin for primary percutaneous coronary intervention in acute myocardial infarction: The HORIZONS-AMI trial. Expert Rev. Cardiovasc. Ther. 2012, 10, 411–422. [Google Scholar] [CrossRef]
- El Khoury, M.; Karam, B.; Tabet, R.; Lafferty, J.C.; Snyder, S.T. Current Practice of Percutaneous Coronary Intervention in Patients With Coagulation Disorders. Cureus 2021, 13, e18284. [Google Scholar] [CrossRef]
- Al-Abdouh, A.; Mhanna, M.; Jabri, A.; Mdanat, L.; Alhuneafat, L.; Mostafa, M.R.; Kundu, A.; Gupta, V. Bivalirudin versus unfractionated heparin in patients with myocardial infarction undergoing percutaneous coronary intervention: A systematic review and meta-analysis of randomized controlled trials. Cardiovasc. Revascularization Med. 2023, 61, 52–61. [Google Scholar] [CrossRef]
- Bikdeli, B.; Erlinge, D.; Valgimigli, M.; Kastrati, A.; Han, Y.; Steg, P.G.; Stables, R.H.; Mehran, R.; James, S.K.; Frigoli, E.; et al. Bivalirudin Versus Heparin During PCI in NSTEMI: Individual Patient Data Meta-Analysis of Large Randomized Trials. Circulation 2023, 148, 1207–1219. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Bernardi, M.; Ortega-Paz, L.; Nerla, R.; D’Amario, D.; Franchi, F.; Biondi-Zoccai, G.; Angiolillo, D.J. Bivalirudin in acute coronary syndromes. Expert Rev. Cardiovasc. Ther. 2023, 21, 901–911. [Google Scholar] [CrossRef] [PubMed]
- Oli, P.R.; Shrestha, D.B.; Shtembari, J.; Gyawali, P.; Regmi, L.; Bhandari, A.; Dhungel, S.; Mattumpuram, J.; Pant, K.; Mungee, S. Bivalirudin versus heparin in STEMI after BRIGHT-4 trial: An updated meta-analysis. Coron. Artery Dis. 2023, 34, 562–579. [Google Scholar] [CrossRef] [PubMed]
- Diaz, D.; Martinez, J.; Bushman, G.; Wolowich, W.R. Anticoagulation strategies in COVID-19 infected patients receiving ECMO support. J. Extracorpor. Technol. 2023, 55, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Hamzah, M.; Jarden, A.M.; Ezetendu, C.; Stewart, R. Evaluation of Bivalirudin As an Alternative to Heparin for Systemic Anticoagulation in Pediatric Extracorporeal Membrane Oxygenation. Pediatr. Crit. Care Med. 2020, 21, 827–834. [Google Scholar] [CrossRef]
- Stangier, J.; Clemens, A. Pharmacology, pharmacokinetics, and pharmacodynamics of dabigatran etexilate, an oral direct thrombin inhibitor. Clin. Appl. Thromb. 2009, 15 (Suppl. S1), 9S–16S. [Google Scholar] [CrossRef] [PubMed]
- Yasaka, M.; Yokota, H.; Suzuki, M.; Asakura, H.; Yamane, T.; Ogi, Y.; Kimoto, T.; Nakayama, D. Idarucizumab for Emergency Reversal of the Anticoagulant Effects of Dabigatran: Final Results of a Japanese Postmarketing Surveillance Study. Cardiol. Ther. 2023, 12, 723–740. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency. Dabigatran Etexilate. Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/dabigatran-etexilate-accord (accessed on 11 November 2023).
- U.S. Food and Drug Administration. Pradaxa. Full Prescribing Information. Medication Guide. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiJotuRz7qCAxUXLRAIHaoOC20QFnoECAgQAQ&url=https%3A%2F%2Fwww.accessdata.fda.gov%2Fdrugsatfda_docs%2Flabel%2F2011%2F022512s007lbl.pdf&usg=AOvVaw0EzRfiMGzbiENy8lhc4joQ&opi=89978449 (accessed on 11 November 2023).
- Fanikos, J.; Murwin, D.; Gruenenfelder, F.; Tartakovsky, I.; França, L.R.; Reilly, P.A.; Kermer, P.; Wowern, F.V.; Lane, D.A.; Butcher, K. Global Use of Idarucizumab in Clinical Practice: Outcomes of the RE-VECTO Surveillance Program. Thromb. Haemost. 2020, 120, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Kostromina, M.A.; Tukhovskaya, E.A.; Shaykhutdinova, E.R.; Slashcheva, G.A.; Ismailova, A.M.; Palikov, V.A.; Palikova, Y.A.; Dyachenko, I.A.; Kravchenko, I.N.; Sadovnikova, E.S.; et al. Screening of the Promising Direct Thrombin Inhibitors from Haematophagous Organisms. Part I: Recombinant Analogues and Their Antithrombotic Activity In Vitro. Biomedicines 2021, 10, 11. [Google Scholar] [CrossRef]
- Esipov, R.S.; Kostromina, M.A. Comparative analysis of the effectiveness of C-terminal cleavage intein-based constructs in producing a recombinant analog of anophelin, an anticoagulant from Anopheles albimanus. Appl. Biochem. Biotechnol. 2015, 175, 2468–2488. [Google Scholar] [CrossRef]
- Koh, C.Y.; Kazimirova, M.; Trimnell, A.; Takac, P.; Labuda, M.; Nuttall, P.A.; Kini, R.M. Variegin, a novel fast and tight binding thrombin inhibitor from the tropical bont tick. J. Biol. Chem. 2007, 282, 29101–29113. [Google Scholar] [CrossRef] [PubMed]
- Dejana, E.; Callioni, A.; Quintana, A.; de Gaetano, G. Bleeding time in laboratory animals. II—A comparison of different assay conditions in rats. Thromb. Res. 1979, 15, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Dejana, E.; Villa, S.; de Gaetano, G. Bleeding time in rats: A comparison of different experimental conditions. Thromb. Haemost. 1982, 48, 108–111. [Google Scholar] [CrossRef] [PubMed]
- Bagot, C.N.; Arya, R. Virchow and his triad: A question of attribution. Br. J. Haematol. 2008, 143, 180–190. [Google Scholar] [CrossRef]
- Jagadeeswaran, P.; Cooley, B.C.; Gross, P.L.; Mackman, N. Animal Models of Thrombosis from Zebrafish to Nonhuman Primates: Use in the Elucidation of New Pathologic Pathways and the Development of Antithrombotic Drugs. Circ. Res. 2016, 118, 1363–1379. [Google Scholar] [CrossRef]


| Group | Subgroup (for Each Subgroup n = 5) | Drug and Route of Administration | Dose and Volume of Administration | Time Point after Injection, min |
|---|---|---|---|---|
| 1 | 1 | Saline | 5 mL/kg | 15 |
| 2 | 30 | |||
| 3 | 60 | |||
| 4 | 90 | |||
| 2 | 5 | Heparin, intravenously | 20 IU/kg, 5 mL/kg | 15 |
| 6 | 30 | |||
| 7 | 60 | |||
| 8 | 90 | |||
| 3 | 9 | Variegin, intravenously | 3 mg/kg, 5 mL/kg | 15 |
| 10 | 30 | |||
| 11 | 60 | |||
| 12 | 90 | |||
| 4 | 13 | Dabigatran etexilate, peroral | 10 mg/kg, 10 mL/kg | 15 |
| 14 | 30 | |||
| 15 | 60 | |||
| 16 | 90 | |||
| 17 | 120 | |||
| 18 | 180 | |||
| 5 | 19 | Dabigatran etexilate, peroral | 25 mg/kg, 10 mL/kg | 15 |
| 20 | 30 | |||
| 21 | 60 | |||
| 22 | 90 | |||
| 23 | 120 | |||
| 24 | 180 |
| Group | Drug | Route of Administration | Dose and Volume of Administration |
|---|---|---|---|
| 1 (n = 6) | Saline | Intravenously | 5 mL/kg |
| 2 (n = 6) | Heparin | Intravenously | 100 IU/kg, 5 mL/kg |
| 3 (n = 6) | Heparin | Intravenously | 20 IU/kg, 5 mL/kg |
| 4 (n = 6) | Dabigatran etexilate | Peroral | 25 mg/kg, 10 mL/kg |
| 5 (n = 6) | Dabigatran etexilate | Peroral | 12.5 mg/kg, 10 mL/kg |
| 6 (n = 6) | Variegin | Intravenously | 30 mg/kg, 5 mL/kg |
| 7 (n = 6) | Variegin | Intravenously | 7.5 mg/kg, 5 mL/kg |
| 8 (n = 6) | Variegin | Intravenously | 3.75 mg/kg, 5 mL/kg |
| 9 (n = 6) | Intact | - | - |
| Group (for Each Group n = 5) | Drug | Route of Administration | Dose and Volume of Administration |
|---|---|---|---|
| 1 | Saline | Intravenously | 2 mL/kg |
| 2 | Heparin | Intravenously | 2 IU/kg, 2 mL/kg |
| 3 | Dabigatran etexilate | Peroral | 5 mg/kg, 2 mL/kg |
| 4 | Variegin | Intravenously | 0.7 mg/kg, 2 mL/kg |
| 5 | Variegin | Intravenously | 0.175 mg/kg, 2 mL/kg |
| Parameters of Hematological Analysis | |
|---|---|
| Leucocyte, 109/L | Hemoglobin, g/L |
| Lymphocyte, 109/L | Hematocrit, l/L |
| Monocyte, 109/L | Mean cell volume, fl |
| Granulocyte, 109/L | Mean cell hemoglobin, pg |
| Lymphocyte, % | Mean corpuscular hemoglobin concentration, g/L |
| Monocyte, % | RBC distribution width, % |
| Granulocyte, % | RDW standard deviation, fl |
| Red blood cell, 1012/L | Platelet count, 109/L |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kostromina, M.A.; Tukhovskaya, E.A.; Shaykhutdinova, E.R.; Palikova, Y.A.; Palikov, V.A.; Slashcheva, G.A.; Ismailova, A.M.; Kravchenko, I.N.; Dyachenko, I.A.; Zayats, E.A.; et al. Unified Methodology for the Primary Preclinical In Vivo Screening of New Anticoagulant Pharmaceutical Agents from Hematophagous Organisms. Int. J. Mol. Sci. 2024, 25, 3986. https://doi.org/10.3390/ijms25073986
Kostromina MA, Tukhovskaya EA, Shaykhutdinova ER, Palikova YA, Palikov VA, Slashcheva GA, Ismailova AM, Kravchenko IN, Dyachenko IA, Zayats EA, et al. Unified Methodology for the Primary Preclinical In Vivo Screening of New Anticoagulant Pharmaceutical Agents from Hematophagous Organisms. International Journal of Molecular Sciences. 2024; 25(7):3986. https://doi.org/10.3390/ijms25073986
Chicago/Turabian StyleKostromina, Maria A., Elena A. Tukhovskaya, Elvira R. Shaykhutdinova, Yuliya A. Palikova, Viktor A. Palikov, Gulsara A. Slashcheva, Alina M. Ismailova, Irina N. Kravchenko, Igor A. Dyachenko, Evgeniy A. Zayats, and et al. 2024. "Unified Methodology for the Primary Preclinical In Vivo Screening of New Anticoagulant Pharmaceutical Agents from Hematophagous Organisms" International Journal of Molecular Sciences 25, no. 7: 3986. https://doi.org/10.3390/ijms25073986
APA StyleKostromina, M. A., Tukhovskaya, E. A., Shaykhutdinova, E. R., Palikova, Y. A., Palikov, V. A., Slashcheva, G. A., Ismailova, A. M., Kravchenko, I. N., Dyachenko, I. A., Zayats, E. A., Abramchik, Y. A., Murashev, A. N., & Esipov, R. S. (2024). Unified Methodology for the Primary Preclinical In Vivo Screening of New Anticoagulant Pharmaceutical Agents from Hematophagous Organisms. International Journal of Molecular Sciences, 25(7), 3986. https://doi.org/10.3390/ijms25073986







