Gene and lncRNA Profiling of ω3/ω6 Polyunsaturated Fatty Acid-Exposed Human Visceral Adipocytes Uncovers Different Responses in Healthy Lean, Obese and Colorectal Cancer-Affected Individuals
Abstract
1. Introduction
2. Results
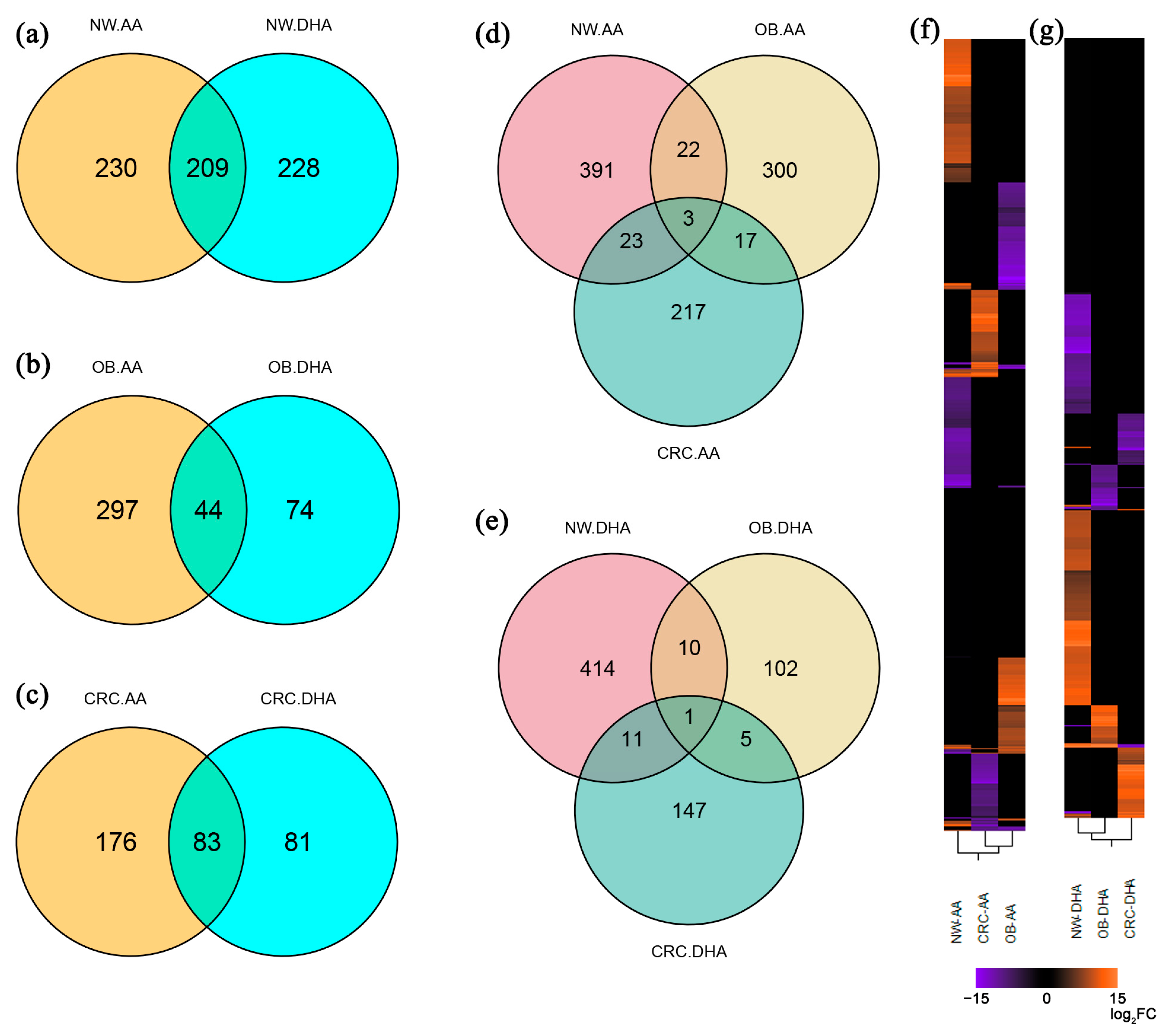
2.1. Arachidonic and Docosahexaenoic Acids Differently Affect Adipocyte Transcription in Healthy Lean, Obese and CRC-Affected Subjects
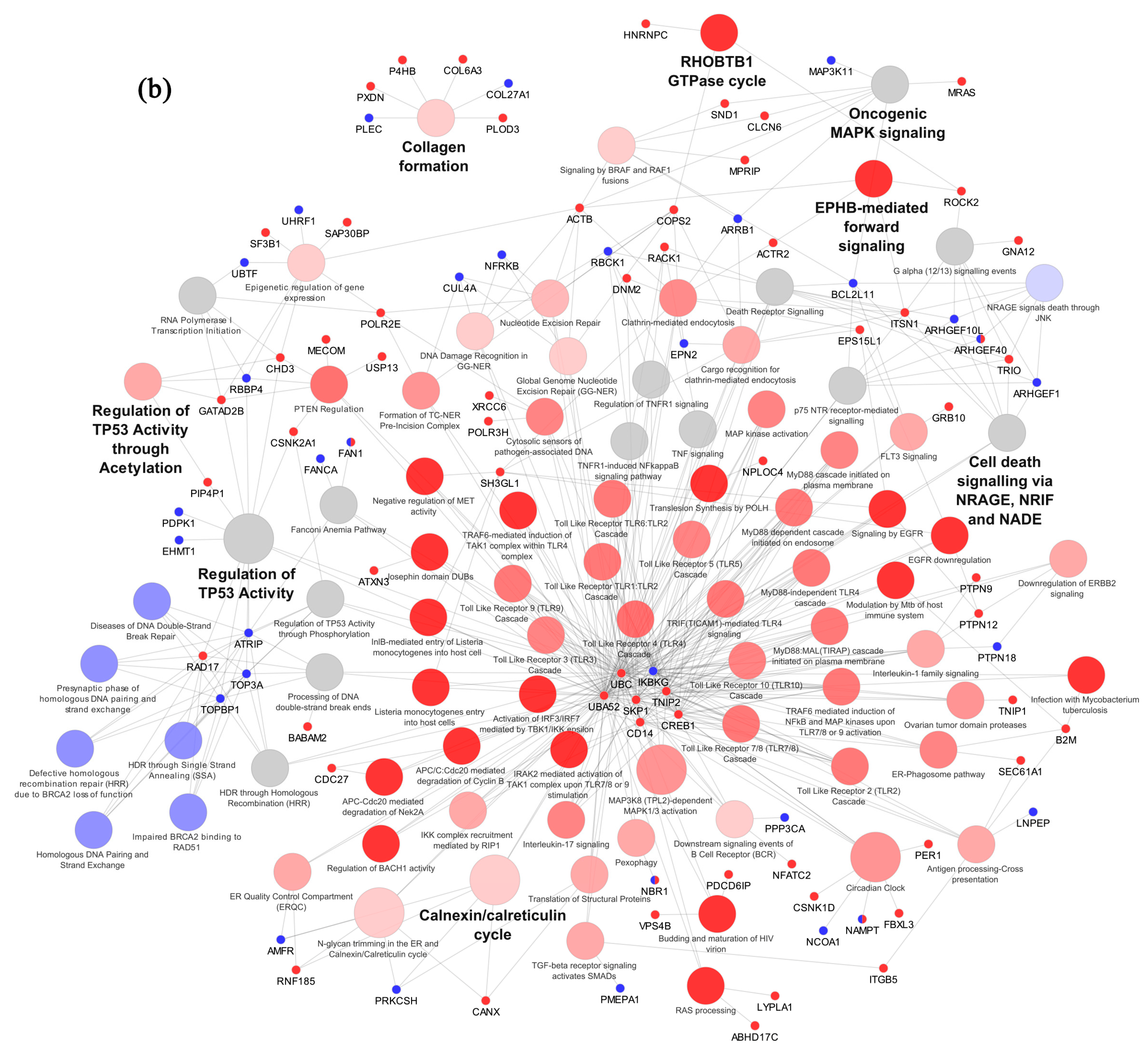
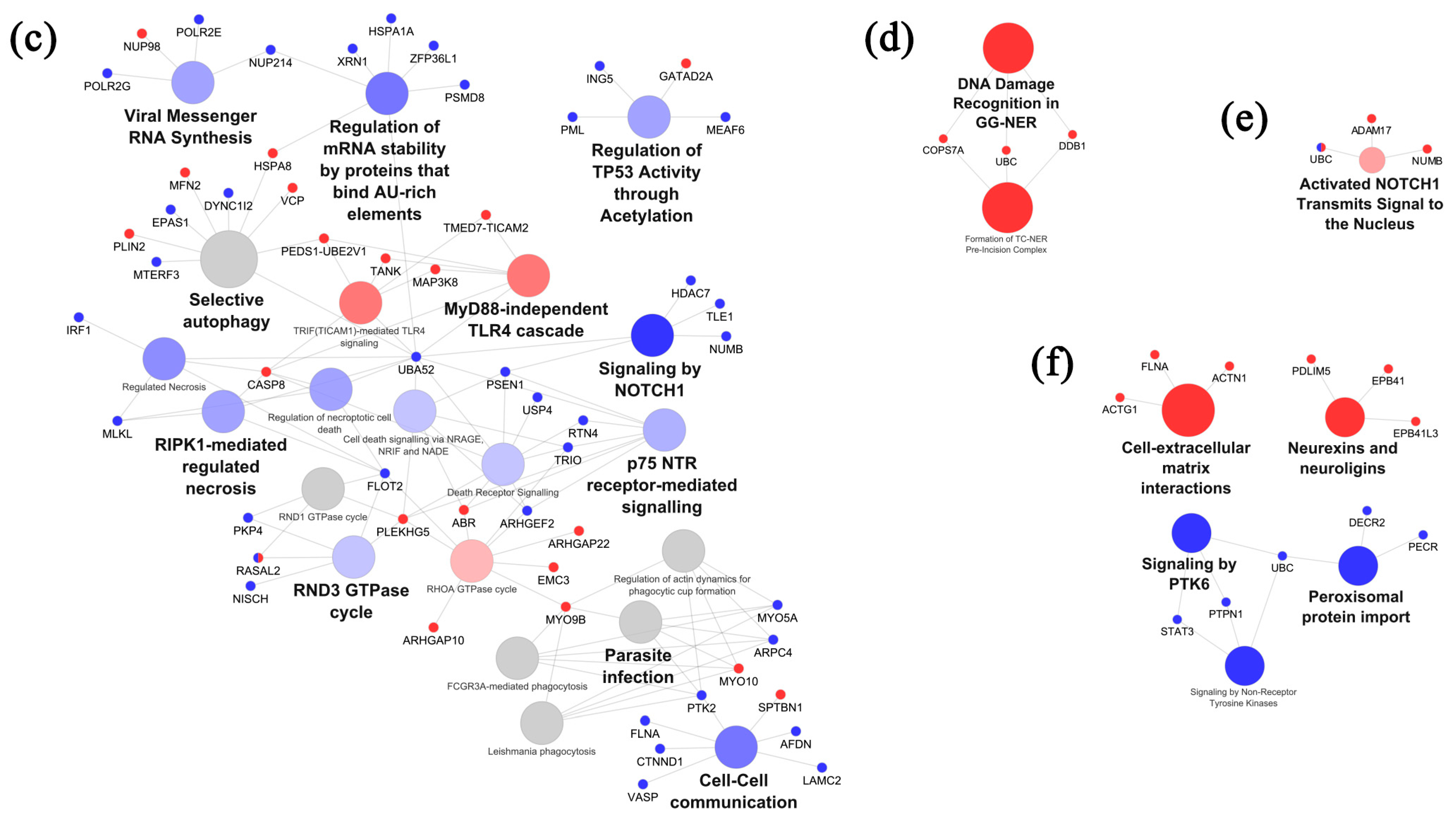
2.2. Pathway Enrichment Analysis of Differentially Expressed Genes Reveals Higher Number of PUFA-Modulated Pathways in Healthy Lean Individuals Compared to Obese and CRC-Affected Subjects
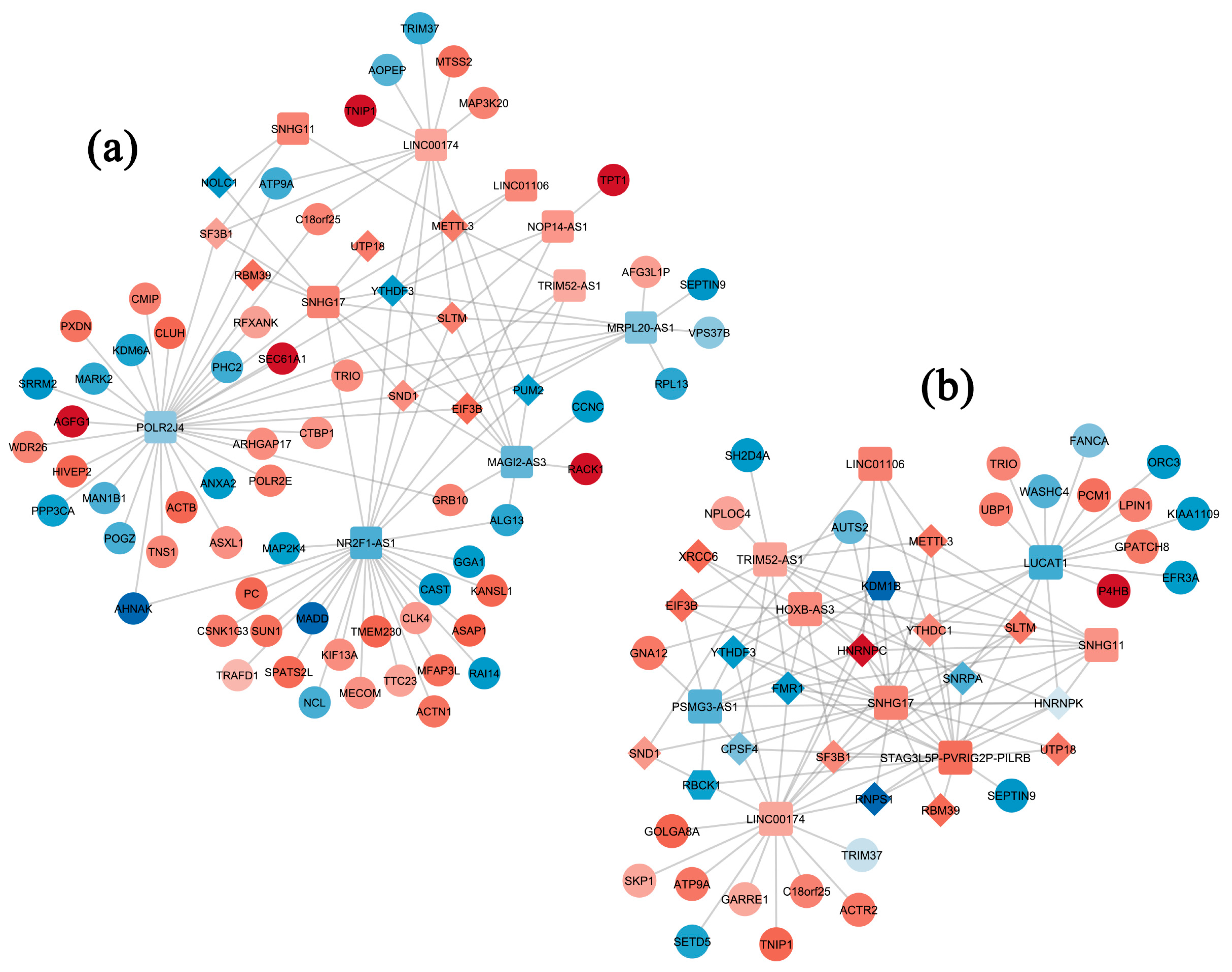
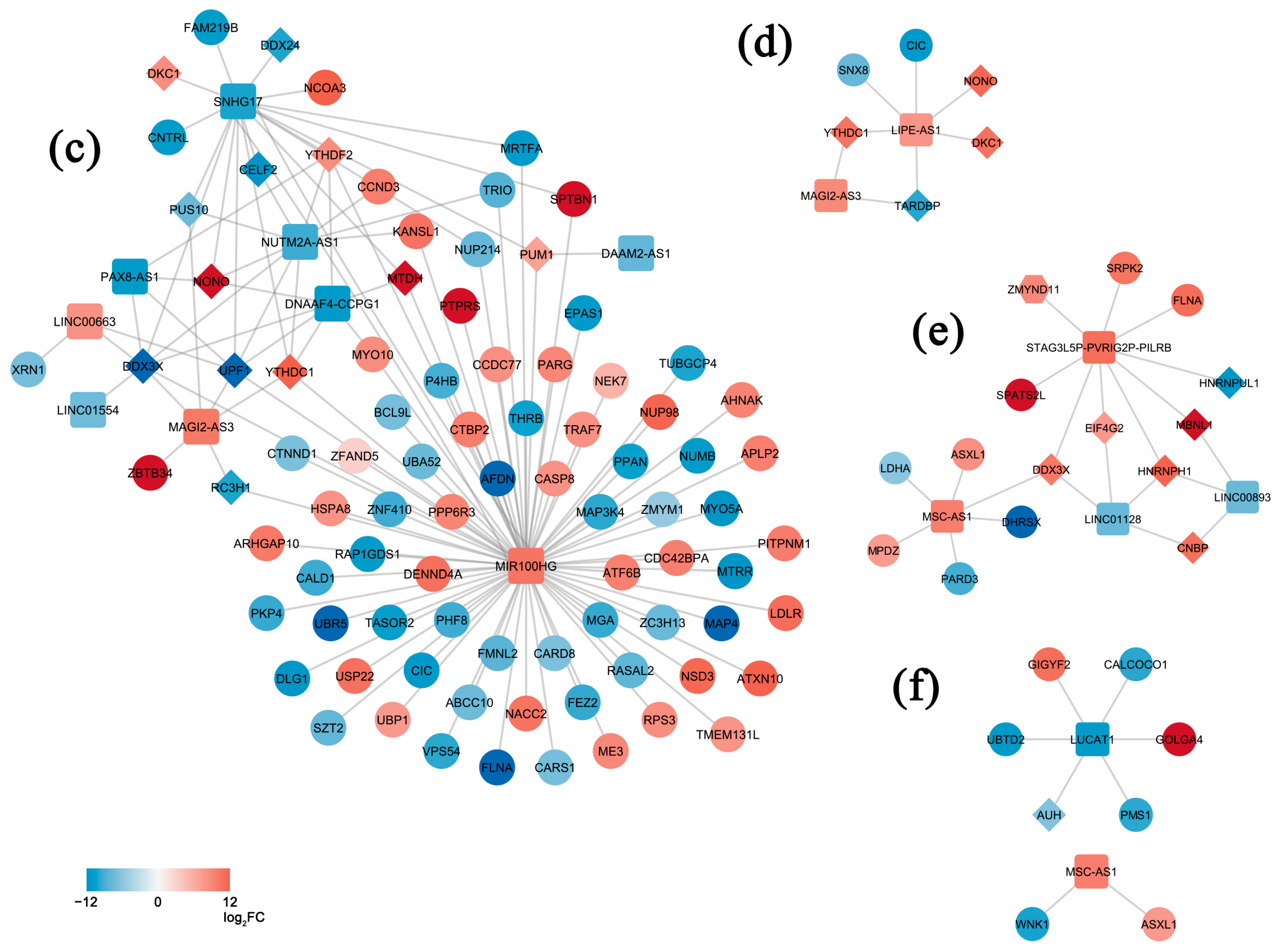
2.3. LncRNA Profiles and mRNA-lncRNA-RNA-Binding Protein Networks Are Specifically Associated with PUFA Stimulation in Healthy Lean, Obese and CRC-Affected Subjects
3. Discussion
4. Materials and Methods
4.1. Ethics Statement
4.2. Patient and Sample Collection
4.3. Adipocyte Isolation/Culture and RNA Preparation
4.4. RNASeq Data Preprocessing and Differential Expression Analysis
4.5. mRNA-lncRNA Regulation Network Construction
4.6. Functional Analysis
4.7. Real-Time Quantitative PCR Validation of Differentially Expressed Transcripts
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Keum, N.; Giovannucci, E. Global burden of colorectal cancer: Emerging trends, risk factors and prevention strategies. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 713–732. [Google Scholar] [CrossRef]
- Kumavath, R.; Pavithran, H.; Paul, S.; Anju, V.T.; Busi, S.; Dyavaiah, M. Effects of gut microbiome and obesity on the development, progression and prevention of cancer (Review). Int. J. Oncol. 2024, 64, 4. [Google Scholar] [CrossRef]
- Mitchelson, K.A.J.; O’Connell, F.; O’Sullivan, J.; Roche, H.M. Obesity, Dietary Fats, and Gastrointestinal Cancer Risk-Potential Mechanisms Relating to Lipid Metabolism and Inflammation. Metabolites 2024, 14, 42. [Google Scholar] [CrossRef]
- D’Archivio, M.; Scazzocchio, B.; Giammarioli, S.; Fiani, M.L.; Varì, R.; Santangelo, C.; Veneziani, A.; Iacovelli, A.; Giovannini, C.; Gessani, S.; et al. ω3-PUFAs exert anti-inflammatory activity in visceral adipocytes from colorectal cancer patients. PLoS ONE 2013, 8, e77432. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Del Cornò, M.; D’Archivio, M.; Conti, L.; Scazzocchio, B.; Varì, R.; Donninelli, G.; Varano, B.; Giammarioli, S.; De Meo, S.; Silecchia, G.; et al. Visceral fat adipocytes from obese and colorectal cancer subjects exhibit distinct secretory and ω6 polyunsaturated fatty acid profiles and deliver immunosuppressive signals to innate immunity cells. Oncotarget 2016, 7, 63093–63105. [Google Scholar] [CrossRef] [PubMed]
- Donninelli, G.; Del Cornò, M.; Pierdominici, M.; Scazzocchio, B.; Varì, R.; Varano, B.; Pacella, I.; Piconese, S.; Barnaba, V.; D’Archivio, M.; et al. Distinct Blood and Visceral Adipose Tissue Regulatory T Cell and Innate Lymphocyte Profiles Characterize Obesity and Colorectal Cancer. Front. Immunol. 2017, 8, 643. [Google Scholar] [CrossRef]
- Thanikachalam, K.; Khan, G. Colorectal Cancer and Nutrition. Nutrients 2019, 11, 164. [Google Scholar] [CrossRef] [PubMed]
- Hull, M.A. Nutritional prevention of colorectal cancer. Proc. Nutr. Soc. 2021, 80, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Mallick, R.; Basak, S.; Das, R.K.; Banerjee, A.; Paul, S.; Pathak, S.; Duttaroy, A.K. Fatty Acids and Their Proteins in Adipose Tissue Inflammation. Cell Biochem. Biophys. 2023, 82, 35–51. [Google Scholar] [CrossRef] [PubMed]
- Del Cornò, M.; Varì, R.; Scazzocchio, B.; Varano, B.; Masella, R.; Conti, L. Dietary Fatty Acids at the Crossroad between Obesity and Colorectal Cancer: Fine Regulators of Adipose Tissue Homeostasis and Immune Response. Cells 2021, 10, 1738. [Google Scholar] [CrossRef]
- Harwood, J.L. Polyunsaturated Fatty Acids: Conversion to Lipid Mediators, Roles in Inflammatory Diseases and Dietary Sources. Int. J. Mol. Sci. 2023, 24, 8838. [Google Scholar] [CrossRef] [PubMed]
- Moon, Y.A. Emerging roles of polyunsaturated fatty acid synthesis pathway in colorectal cancer. Anim. Cells Syst. 2023, 27, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.; Hussain, M.; Jiang, B.; Zheng, L.; Pan, Y.; Hu, J.; Khan, A.; Ashraf, A.; Zou, X. Omega-3 long-chain polyunsaturated fatty acids: Metabolism and health implications. Prog. Lipid Res. 2023, 92, 101255. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C. Omega-3 fatty acids and inflammatory processes: From molecules to man. Biochem. Soc. Trans. 2017, 45, 1105–1115. [Google Scholar] [CrossRef] [PubMed]
- Ulven, S.M.; Christensen, J.J.; Nygård, O.; Svardal, A.; Leder, L.; Ottestad, I.; Lysne, V.; Laupsa-Borge, J.; Ueland, P.M.; Midttun, Ø.; et al. Using metabolic profiling and gene expression analyses to explore molecular effects of replacing saturated fat with polyunsaturated fat-a randomized controlled dietary intervention study. Am. J. Clin. Nutr. 2019, 109, 1239–1250. [Google Scholar] [CrossRef] [PubMed]
- Bouwens, M.; van de Rest, O.; Dellschaft, N.; Bromhaar, M.G.; de Groot, L.C.; Geleijnse, J.M.; Müller, M.; Afman, L.A. Fish-oil supplementation induces antiinflammatory gene expression profiles in human blood mononuclear cells. Am. J. Clin. Nutr. 2009, 90, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Bouwens, M.; Grootte Bromhaar, M.; Jansen, J.; Müller, M.; Afman, L.A. Postprandial dietary lipid-specific effects on human peripheral blood mononuclear cell gene expression profiles. Am. J. Clin. Nutr. 2010, 91, 208–217. [Google Scholar] [CrossRef]
- Skulas-Ray, A.C.; Kris-Etherton, P.M.; Harris, W.S.; Vanden Heuvel, J.P.; Wagner, P.R.; West, S.G. Dose-response effects of omega-3 fatty acids on triglycerides, inflammation, and endothelial function in healthy persons with moderate hypertriglyceridemia. Am. J. Clin. Nutr. 2011, 93, 243–252. [Google Scholar] [CrossRef]
- Myhrstad, M.C.; Ulven, S.M.; Günther, C.C.; Ottestad, I.; Holden, M.; Ryeng, E.; Borge, G.I.; Kohler, A.; Brønner, K.W.; Thoresen, M.; et al. Fish oil supplementation induces expression of genes related to cell cycle, endoplasmic reticulum stress and apoptosis in peripheral blood mononuclear cells: A transcriptomic approach. J. Intern. Med. 2014, 276, 498–511. [Google Scholar] [CrossRef]
- Rundblad, A.; Holven, K.B.; Bruheim, I.; Myhrstad, M.C.; Ulven, S.M. Effects of fish and krill oil on gene expression in peripheral blood mononuclear cells and circulating markers of inflammation: A randomised controlled trial. J. Nutr. Sci. 2018, 7, e10. [Google Scholar] [CrossRef]
- Rudkowska, I.; Ponton, A.; Jacques, H.; Lavigne, C.; Holub, B.J.; Marette, A.; Vohl, M.C. Effects of a supplementation of n-3 polyunsaturated fatty acids with or without fish gelatin on gene expression in peripheral blood mononuclear cells in obese, insulin-resistant subjects. J. Nutr. Nutr. 2011, 4, 192–202. [Google Scholar] [CrossRef]
- Rudkowska, I.; Paradis, A.M.; Thifault, E.; Julien, P.; Tchernof, A.; Couture, P.; Lemieux, S.; Barbier, O.; Vohl, M.C. Transcriptomic and metabolomic signatures of an n-3 polyunsaturated fatty acids supplementation in a normolipidemic/normocholesterolemic Caucasian population. J. Nutr. Biochem. 2013, 24, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Polus, A.; Zapala, B.; Razny, U.; Gielicz, A.; Kiec-Wilk, B.; Malczewska-Malec, M.; Sanak, M.; Childs, C.E.; Calder, P.C.; Dembinska-Kiec, A. Omega-3 fatty acid supplementation influences the whole blood transcriptome in women with obesity, associated with pro-resolving lipid mediator production. Biochim. Biophys. Acta 2016, 1861, 1746–1755. [Google Scholar] [CrossRef]
- Tojjari, A.; Choucair, K.; Sadeghipour, A.; Saeed, A. Anti-Inflammatory and Immune Properties of Polyunsaturated Fatty Acids (PUFAs) and Their Impact on Colorectal Cancer (CRC) Prevention and Treatment. Cancers 2023, 15, 4294. [Google Scholar] [CrossRef] [PubMed]
- Itariu, B.K.; Zeyda, M.; Hochbrugger, E.E.; Neuhofer, A.; Prager, G.; Schindler, K.; Bohdjalian, A.; Mascher, D.; Vangala, S.; Schranz, M.; et al. Long-chain n-3 PUFAs reduce adipose tissue and systemic inflammation in severely obese nondiabetic patients: A randomized controlled trial. Am. J. Clin. Nutr. 2012, 96, 1137–1149. [Google Scholar] [CrossRef] [PubMed]
- Kratz, M.; Kuzma, J.N.; Hagman, D.K.; van Yserloo, B.; Matthys, C.C.; Callahan, H.S.; Weigle, D.S. n3 PUFAs do not affect adipose tissue inflammation in overweight to moderately obese men and women. J. Nutr. 2013, 143, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Holt, P.R.; Alemán, J.O.; Walker, J.M.; Jiang, C.S.; Liang, Y.; de Rosa, J.C.; Giri, D.D.; Iyengar, N.M.; Milne, G.L.; Hudis, C.A.; et al. Docosahexaenoic Acid Supplementation is Not Anti-Inflammatory in Adipose Tissue of Healthy Obese Postmenopausal Women. Int. J. Nutr. 2017, 1, 31–49. [Google Scholar] [CrossRef] [PubMed]
- Huerta, A.E.; Prieto-Hontoria, P.L.; Fernández-Galilea, M.; Escoté, X.; Martínez, J.A.; Moreno-Aliaga, M.J. Effects of dietary supplementation with EPA and/or α-lipoic acid on adipose tissue transcriptomic profile of healthy overweight/obese women following a hypocaloric diet. Biofactors 2017, 43, 117–131. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, J.F.; Xue, C.; Hu, Y.; Li, M.; Reilly, M.P. Adipose tissue RNASeq reveals novel gene-nutrient interactions following n-3 PUFA supplementation and evoked inflammation in humans. J. Nutr. Biochem. 2016, 30, 126–132. [Google Scholar] [CrossRef]
- Shah, R.D.; Xue, C.; Zhang, H.; Tuteja, S.; Li, M.; Reilly, M.P.; Ferguson, J.F. Expression of Calgranulin Genes S100A8, S100A9 and S100A12 Is Modulated by n-3 PUFA during Inflammation in Adipose Tissue and Mononuclear Cells. PLoS ONE 2017, 12, e0169614. [Google Scholar] [CrossRef]
- Fisk, H.L.; Childs, C.E.; Miles, E.A.; Ayres, R.; Noakes, P.S.; Paras-Chavez, C.; Kuda, O.; Kopecký, J.; Antoun, E.; Lillycrop, K.A.; et al. Modification of subcutaneous white adipose tissue inflammation by omega-3 fatty acids is limited in human obesity-a double blind, randomised clinical trial. eBioMedicine 2022, 77, 103909. [Google Scholar] [CrossRef] [PubMed]
- Murumalla, R.K.; Gunasekaran, M.K.; Padhan, J.K.; Bencharif, K.; Gence, L.; Festy, F.; Césari, M.; Roche, R.; Hoareau, L. Fatty acids do not pay the toll: Effect of SFA and PUFA on human adipose tissue and mature adipocytes inflammation. Lipids Health Dis. 2012, 11, 175. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, J.F.; Roberts-Lee, K.; Borcea, C.; Smith, H.M.; Midgette, Y.; Shah, R. Omega-3 polyunsaturated fatty acids attenuate inflammatory activation and alter differentiation in human adipocytes. J. Nutr. Biochem. 2019, 64, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.R.; Midgette, Y.; Shah, R. Fish Oil Derived Omega 3 Fatty Acids Suppress Adipose NLRP3 Inflammasome Signaling in Human Obesity. J. Endocr. Soc. 2019, 3, 504–515. [Google Scholar] [CrossRef] [PubMed]
- Del Cornò, M.; Baldassarre, A.; Calura, E.; Conti, L.; Martini, P.; Romualdi, C.; Varì, R.; Scazzocchio, B.; D’Archivio, M.; Masotti, A.; et al. Transcriptome Profiles of Human Visceral Adipocytes in Obesity and Colorectal Cancer Unravel the Effects of Body Mass Index and Polyunsaturated Fatty Acids on Genes and Biological Processes Related to Tumorigenesis. Front. Immunol. 2019, 10, 265. [Google Scholar] [CrossRef] [PubMed]
- Maass, P.G.; Luft, F.C.; Bähring, S. Long non-coding RNA in health and disease. J. Mol. Med. 2014, 92, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Shakhpazyan, N.K.; Mikhaleva, L.M.; Bedzhanyan, A.L.; Sadykhov, N.K.; Midiber, K.Y.; Konyukova, A.K.; Kontorschikov, A.S.; Maslenkina, K.S.; Orekhov, A.N. Long Non-Coding RNAs in Colorectal Cancer: Navigating the Intersections of Immunity, Intercellular Communication, and Therapeutic Potential. Biomedicines 2023, 11, 2411. [Google Scholar] [CrossRef]
- Lorente-Cebrián, S.; González-Muniesa, P.; Milagro, F.I.; Martínez, J.A. MicroRNAs and other non-coding RNAs in adipose tissue and obesity: Emerging roles as biomarkers and therapeutic targets. Clin. Sci. 2019, 133, 23–40. [Google Scholar] [CrossRef]
- Gao, H.; Kerr, A.; Jiao, H.; Hon, C.C.; Rydén, M.; Dahlman, I.; Arner, P. Long Non-Coding RNAs Associated with Metabolic Traits in Human White Adipose Tissue. eBioMedicine 2018, 30, 248–260. [Google Scholar] [CrossRef]
- Sun, L.; Lin, J.D. Function and Mechanism of Long Noncoding RNAs in Adipocyte Biology. Diabetes 2019, 68, 887–896. [Google Scholar] [CrossRef]
- Tait, S.; Baldassarre, A.; Masotti, A.; Calura, E.; Martini, P.; Varì, R.; Scazzocchio, B.; Gessani, S.; Del Cornò, M. Integrated Transcriptome Analysis of Human Visceral Adipocytes Unravels Dysregulated microRNA-Long Non-coding RNA-mRNA Networks in Obesity and Colorectal Cancer. Front. Oncol. 2020, 10, 1089. [Google Scholar] [CrossRef] [PubMed]
- Djuricic, I.; Calder, P.C. Beneficial Outcomes of Omega-6 and Omega-3 Polyunsaturated Fatty Acids on Human Health: An Update for 2021. Nutrients 2021, 13, 2421. [Google Scholar] [CrossRef]
- Wang, W.A.; Groenendyk, J.; Michalak, M. Calreticulin signaling in health and disease. Int. J. Biochem. Cell Biol. 2012, 44, 842–846. [Google Scholar] [CrossRef] [PubMed]
- Mathers, J.C. Obesity and bowel cancer: From molecular mechanisms to interventions. Nutr. Res. 2019, 70, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Tabuso, M.; Homer-Vanniasinkam, S.; Adya, R.; Arasaradnam, R.P. Role of tissue microenvironment resident adipocytes in colon cancer. World J. Gastroenterol. 2017, 23, 5829–5835. [Google Scholar] [CrossRef] [PubMed]
- Bernard, J.J.; Wellberg, E.A. The Tumor Promotional Role of Adipocytes in the Breast Cancer Microenvironment and Macroenvironment. Am. J. Pathol. 2021, 191, 1342–1352. [Google Scholar] [CrossRef] [PubMed]
- Holowatyj, A.N.; Haffa, M.; Lin, T.; Scherer, D.; Gigic, B.; Ose, J.; Warby, C.A.; Himbert, C.; Abbenhardt-Martin, C.; Achaintre, D.; et al. Multi-Omics Analysis Reveals Adipose-tumor Crosstalk in Patients with Colorectal Cancer. Cancer Prev. Res. 2020, 13, 817–828. [Google Scholar] [CrossRef]
- Alves, M.G.; Moreira, Â.; Guimarães, M.; Nora, M.; Sousa, M.; Oliveira, P.F.; Monteiro, M.P. Body mass index is associated with region-dependent metabolic reprogramming of adipose tissue. BBA Clin. 2017, 8, 1–6. [Google Scholar] [CrossRef]
- Fleckenstein-Elsen, M.; Dinnies, D.; Jelenik, T.; Roden, M.; Romacho, T.; Eckel, J. Eicosapentaenoic acid and arachidonic acid differentially regulate adipogenesis, acquisition of a brite phenotype and mitochondrial function in primary human adipocytes. Mol. Nutr. Food Res. 2016, 60, 2065–2075. [Google Scholar] [CrossRef]
- Engin, A. Circadian Rhythms in Diet-Induced Obesity. Adv. Exp. Med. Biol. 2017, 960, 19–52. [Google Scholar] [CrossRef]
- Kinouchi, K.; Sassone-Corsi, P. Metabolic rivalry: Circadian homeostasis and tumorigenesis. Nat. Rev. Cancer 2020, 20, 645–661. [Google Scholar] [CrossRef] [PubMed]
- Ribas-Latre, A.; Eckel-Mahan, K. Nutrients and the Circadian Clock: A Partnership Controlling Adipose Tissue Function and Health. Nutrients 2022, 14, 2084. [Google Scholar] [CrossRef] [PubMed]
- Boden, G.; Duan, X.; Homko, C.; Molina, E.J.; Song, W.; Perez, O.; Cheung, P.; Merali, S. Increase in endoplasmic reticulum stress-related proteins and genes in adipose tissue of obese, insulin-resistant individuals. Diabetes 2008, 57, 2438–2444. [Google Scholar] [CrossRef] [PubMed]
- Mak, I.L.; Lavery, P.; Agellon, S.; Rauch, F.; Murshed, M.; Weiler, H.A. Arachidonic acid exacerbates diet-induced obesity and reduces bone mineral content without impacting bone strength in growing male rats. J. Nutr. Biochem. 2019, 73, 108226. [Google Scholar] [CrossRef] [PubMed]
- Xing, C.; Sun, S.G.; Yue, Z.Q.; Bai, F. Role of lncRNA LUCAT1 in cancer. Biomed. Pharmacother. 2021, 134, 111158. [Google Scholar] [CrossRef]
- Wang, Y.; Hong, Z.; Wei, S.; Ye, Z.; Chen, L.; Qiu, C. Investigating the role of LncRNA PSMG3-AS1 in gastric cancer: Implications for prognosis and therapeutic intervention. Cell Cycle 2023, 22, 2161–2171. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Liu, Y.; Yuan, S.; Bi, X.; Yang, Y.; Zhu, H.; Li, Z.; Ji, L.; Yu, X. The emerging role of NR2F1-AS1 in the tumorigenesis and progression of human cancer. Pathol. Res. Pract. 2022, 235, 153938. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Yu, Y.; Liao, F.; Tan, S. Homo Sapiens Circular RNA 0079993 (hsa_circ_0079993) of the POLR2J4 Gene Acts as an Oncogene in Colorectal Cancer Through the microRNA-203a-3p.1 and CREB1 Axis. Med. Sci. Monit. 2019, 25, 6872–6883. [Google Scholar] [CrossRef]
- Lu, C.; Liao, W.; Huang, Y.; Luo, Y. Increased expression of NOP14 is associated with improved prognosis due to immune regulation in colorectal cancer. BMC Gastroenterol. 2022, 22, 207. [Google Scholar] [CrossRef]
- Ren, H.; Li, Z.; Tang, Z.; Li, J.; Lang, X. Long noncoding MAGI2-AS3 promotes colorectal cancer progression through regulating miR-3163/TMEM106B axis. J. Cell. Physiol. 2020, 235, 4824–4833. [Google Scholar] [CrossRef]
- Ma, L.; Gao, J.; Zhang, N.; Wang, J.; Xu, T.; Lei, T.; Zou, X.; Wei, C.; Wang, Z. Long noncoding RNA SNHG17: A novel molecule in human cancers. Cancer Cell Int. 2022, 22, 104. [Google Scholar] [CrossRef]
- Wu, Y.; Wang, Z.; Yu, S.; Liu, D.; Sun, L. LncmiRHG-MIR100HG: A new budding star in cancer. Front. Oncol. 2022, 12, 997532. [Google Scholar] [CrossRef]
- Liu, J.X.; Li, W.; Li, J.T.; Liu, F.; Zhou, L. Screening key long non-coding RNAs in early-stage colon adenocarcinoma by RNA-sequencing. Epigenomics 2018, 10, 1215–1228. [Google Scholar] [CrossRef]
- Peng, J.; Ma, Y.; Zhao, X.; Yang, X.; Wang, H. Constitutive β-Catenin Overexpression Represses Lncrna MIR100HG Transcription via HDAC6-Mediated Histone Modification in Colorectal Cancer. Mol. Cancer Res. 2022, 20, 949–959. [Google Scholar] [CrossRef]
- Thunen, A.; La Placa, D.; Zhang, Z.; Shively, J.E. Role of lncRNA LIPE-AS1 in adipogenesis. Adipocyte 2022, 11, 11–27. [Google Scholar] [CrossRef]
- Zhu, J.; Jiang, C.; Hui, H.; Sun, Y.; Tao, M.; Liu, Y.; Qian, X. Overexpressed lncRNA LINC00893 Suppresses Progression of Colon Cancer by Binding with miR-146b-3p to Upregulate PRSS8. J. Oncol. 2022, 2022, 8002318. [Google Scholar] [CrossRef] [PubMed]
- Pan, S.; Chen, Y.; Yan, J.; Li, F.; Chen, X.; Xu, X.; Xing, H. The emerging roles and mechanisms of exosomal non-coding RNAs in the mutual regulation between adipose tissue and other related tissues in obesity and metabolic diseases. Front. Endocrinol. 2022, 13, 975334. [Google Scholar] [CrossRef] [PubMed]
- Norreen-Thorsen, M.; Struck, E.C.; Öling, S.; Zwahlen, M.; Von Feilitzen, K.; Odeberg, J.; Lindskog, C.; Pontén, F.; Uhlén, M.; Dusart, P.J.; et al. A human adipose tissue cell-type transcriptome atlas. Cell Rep. 2022, 40, 111046. [Google Scholar] [CrossRef] [PubMed]
- Rey, F.; Urrata, V.; Gilardini, L.; Bertoli, S.; Calcaterra, V.; Zuccotti, G.V.; Cancello, R.; Carelli, S. Role of long non-coding RNAs in adipogenesis: State of the art and implications in obesity and obesity-associated diseases. Obes. Rev. 2021, 22, e13203. [Google Scholar] [CrossRef] [PubMed]
- Squillaro, T.; Peluso, G.; Galderisi, U.; Di Bernardo, G. Long non-coding RNAs in regulation of adipogenesis and adipose tissue function. eLife 2020, 9, e59053. [Google Scholar] [CrossRef] [PubMed]
- Giuliani, A.; Ferrara, F.; Scimò, M.; Angelico, F.; Olivieri, L.; Basso, L. Adipose tissue fatty acid composition and colon cancer: A case-control study. Eur. J. Nutr. 2014, 53, 1029–1037. [Google Scholar] [CrossRef]
- Cottet, V.; Vaysse, C.; Scherrer, M.L.; Ortega-Deballon, P.; Lakkis, Z.; Delhorme, J.B.; Deguelte-Lardière, S.; Combe, N.; Bonithon-Kopp, C. Fatty acid composition of adipose tissue and colorectal cancer: A case-control study. Am. J. Clin. Nutr. 2015, 101, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Vaittinen, M.; Männistö, V.; Käkelä, P.; Ågren, J.; Tiainen, M.; Schwab, U.; Pihlajamäki, J. Interorgan cross talk between fatty acid metabolism, tissue inflammation, and FADS2 genotype in humans with obesity. Obesity 2017, 25, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Garaulet, M.; Pérez-Llamas, F.; Pérez-Ayala, M.; Martínez, P.; de Medina, F.S.; Tebar, F.J.; Zamora, S. Site-specific differences in the fatty acid composition of abdominal adipose tissue in an obese population from a Mediterranean area: Relation with dietary fatty acids, plasma lipid profile, serum insulin, and central obesity. Am. J. Clin. Nutr. 2001, 74, 585–591. [Google Scholar] [CrossRef] [PubMed]
- Arner, P.; Rydén, M. Fatty Acids, Obesity and Insulin Resistance. Obes Facts 2015, 8, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Hodson, L.; McQuaid, S.E.; Karpe, F.; Frayn, K.N.; Fielding, B.A. Differences in partitioning of meal fatty acids into blood lipid fractions: A comparison of linoleate, oleate, and palmitate. Am. J. Physiol. Endocrinol. Metab. 2009, 296, E64–E71. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Han, L.; He, J.; Lv, J.; Pan, R.; Lv, T. A high serum-free fatty acid level is associated with cancer. J. Cancer Res. Clin. Oncol. 2020, 146, 705–710. [Google Scholar] [CrossRef] [PubMed]
- Ameer, F.; Scandiuzzi, L.; Hasnain, S.; Kalbacher, H.; Zaidi, N. De novo lipogenesis in health and disease. Metabolism 2014, 63, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Worthmann, A.; Ridder, J.; Piel, S.Y.L.; Evangelakos, I.; Musfeldt, M.; Voß, H.; O’Farrell, M.; Fischer, A.W.; Adak, S.; Sundd, M.; et al. Fatty acid synthesis suppresses dietary polyunsaturated fatty acid use. Nat. Commun. 2024, 15, 45. [Google Scholar] [CrossRef]
- Roynette, C.E.; Calder, P.C.; Dupertuis, Y.M.; Pichard, C. n-3 polyunsaturated fatty acids and colon cancer prevention. Clin. Nutr. 2004, 23, 139–151. [Google Scholar] [CrossRef]
- González-Becerra, K.; Ramos-Lopez, O.; Barrón-Cabrera, E.; Riezu-Boj, J.I.; Milagro, F.I.; Martínez-López, E.; Martínez, J.A. Fatty acids, epigenetic mechanisms and chronic diseases: A systematic review. Lipids Health Dis. 2019, 18, 178. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Langmead, B.; Salzberg, S.L. HISAT: A fast spliced aligner with low memory requirements. Nat. Methods 2015, 12, 357–360. [Google Scholar] [CrossRef] [PubMed]
- Pertea, M.; Pertea, G.M.; Antonescu, C.M.; Chang, T.C.; Mendell, J.T.; Salzberg, S.L. StringTie enables improved reconstruction of a transcriptome from RNA-seq reads. Nat. Biotechnol. 2015, 33, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Pertea, G.; Pertea, M. GFF Utilities: GffRead and GffCompare. F1000Research 2020, 9, 304. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. Available online: https://www.R-project.org/ (accessed on 12 March 2024).
- Robinson, M.D.; McCarthy, D.J.; Smyth, G.K. edgeR: A Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics 2010, 26, 139–140. [Google Scholar] [CrossRef]
- Risso, D.; Ngai, J.; Speed, T.P.; Dudoit, S. Normalization of RNA-seq data using factor analysis of control genes or samples. Nat. Biotechnol. 2014, 32, 896–902. [Google Scholar] [CrossRef]
- Durinck, S.; Spellman, P.T.; Birney, E.; Huber, W. Mapping identifiers for the integration of genomic datasets with the R/Bioconductor package biomaRt. Nat. Protoc. 2009, 4, 1184–1191. [Google Scholar] [CrossRef]
- Li, J.H.; Liu, S.; Zhou, H.; Qu, L.H.; Yang, J.H. starBase v2.0: Decoding miRNA-ceRNA, miRNA-ncRNA and protein-RNA interaction networks from large-scale CLIP-Seq data. Nucleic Acids Res. 2014, 42, D92–D97. [Google Scholar] [CrossRef]
- Lin, Y.; Liu, T.; Cui, T.; Wang, Z.; Zhang, Y.; Tan, P.; Huang, Y.; Yu, J.; Wang, D. RNAInter in 2020: RNA interactome repository with increased coverage and annotation. Nucleic Acids Res. 2020, 48, D189–D197. [Google Scholar] [CrossRef] [PubMed]
- Shannon, P.; Markiel, A.; Ozier, O.; Baliga, N.S.; Wang, J.T.; Ramage, D.; Amin, N.; Schwikowski, B.; Ideker, T. Cytoscape: A software environment for integrated models of biomolecular interaction networks. Genome Res. 2003, 13, 2498–2504. [Google Scholar] [CrossRef] [PubMed]
- Bindea, G.; Mlecnik, B.; Hackl, H.; Charoentong, P.; Tosolini, M.; Kirilovsky, A.; Fridman, W.H.; Pagès, F.; Trajanoski, Z.; Galon, J. ClueGO: A Cytoscape plug-in to decipher functionally grouped gene ontology and pathway annotation networks. Bioinformatics 2009, 25, 1091–1093. [Google Scholar] [CrossRef] [PubMed]

| Total Transcripts | DEGs | DELs | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Subject category | Treatment | Up | Down | TOT | Up | Down | TOT | Up | Down | TOT |
| NW | AA | 272 | 196 | 468 | 201 | 150 | 351 | 7 | 5 | 12 |
| DHA | 280 | 176 | 456 | 265 | 167 | 432 | 7 | 4 | 11 | |
| OB | AA | 159 | 193 | 352 | 152 | 184 | 335 | 6 | 7 | 13 |
| DHA | 57 | 62 | 119 | 54 | 61 | 115 | 2 | 0 | 2 | |
| CRC | AA | 144 | 126 | 270 | 138 | 114 | 252 | 2 | 5 | 7 |
| DHA | 95 | 73 | 168 | 92 | 69 | 161 | 1 | 1 | 2 | |
| NW | OB | CRC | ||||
|---|---|---|---|---|---|---|
| AA | DHA | AA | DHA | AA | DHA | |
| Annotated lncRNAs | ||||||
| DAAM2-AS1 | −7.56 | |||||
| DNAAF4-CCPG1 | −10.76 | |||||
| FAM88B | −8.61 | |||||
| HOXB-as3 | 8.34 | |||||
| LINC00174 | 6.40 | 6.31 | ||||
| LINC00663 | 7.84 | |||||
| LINC00884 | 8.65 | |||||
| LINC00893 | −7.22 | |||||
| LINC01106 | 8.54 | 9.19 | ||||
| LINC01128 | −7.30 | |||||
| LINC01554 | −7.02 | |||||
| LIPE-AS1 | 7.61 | |||||
| LUCAT1 | −8.84 | −10.57 | ||||
| MAGI2-AS3 | −7.67 | 9.66 | 8.41 | |||
| MIR100HG | 10.06 | |||||
| MRPL20-AS1 | −6.14 | |||||
| MSC-AS1 | 9.36 | 9.24 | ||||
| NOP14-AS1 | 7.51 | |||||
| NR2F1-AS1 | −8.53 | |||||
| NUTM2A-AS1 | −8.84 | |||||
| PAX8-AS1 | −10.64 | |||||
| POLR2J4 | −5.80 | |||||
| PSMG3-AS1 | −8.17 | |||||
| SNHG11 | 8.91 | 7.75 | ||||
| SNHG17 | 9.02 | 8.96 | −8.26 | |||
| STAG3L5P-PVRIG2P-PILRB | 10.54 | −8.06; 10.46 | ||||
| TICAM2-AS1 | 6.53 | |||||
| TRIM52-AS1 | 6.01 | 6.51 | ||||
| Novel lncRNAs | ||||||
| HSALNG0010842 | −6.76 | |||||
| HSALNG0056067 | −8.63 | |||||
| HSALNG0088518 | 6.11 | |||||
| HSALNG0101929 | 6.68 | |||||
| HSALNG0114326 | −11.64 | |||||
| HSALNG0132632 | −6.07 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tait, S.; Calura, E.; Baldassarre, A.; Masotti, A.; Varano, B.; Gessani, S.; Conti, L.; Del Cornò, M. Gene and lncRNA Profiling of ω3/ω6 Polyunsaturated Fatty Acid-Exposed Human Visceral Adipocytes Uncovers Different Responses in Healthy Lean, Obese and Colorectal Cancer-Affected Individuals. Int. J. Mol. Sci. 2024, 25, 3357. https://doi.org/10.3390/ijms25063357
Tait S, Calura E, Baldassarre A, Masotti A, Varano B, Gessani S, Conti L, Del Cornò M. Gene and lncRNA Profiling of ω3/ω6 Polyunsaturated Fatty Acid-Exposed Human Visceral Adipocytes Uncovers Different Responses in Healthy Lean, Obese and Colorectal Cancer-Affected Individuals. International Journal of Molecular Sciences. 2024; 25(6):3357. https://doi.org/10.3390/ijms25063357
Chicago/Turabian StyleTait, Sabrina, Enrica Calura, Antonella Baldassarre, Andrea Masotti, Barbara Varano, Sandra Gessani, Lucia Conti, and Manuela Del Cornò. 2024. "Gene and lncRNA Profiling of ω3/ω6 Polyunsaturated Fatty Acid-Exposed Human Visceral Adipocytes Uncovers Different Responses in Healthy Lean, Obese and Colorectal Cancer-Affected Individuals" International Journal of Molecular Sciences 25, no. 6: 3357. https://doi.org/10.3390/ijms25063357
APA StyleTait, S., Calura, E., Baldassarre, A., Masotti, A., Varano, B., Gessani, S., Conti, L., & Del Cornò, M. (2024). Gene and lncRNA Profiling of ω3/ω6 Polyunsaturated Fatty Acid-Exposed Human Visceral Adipocytes Uncovers Different Responses in Healthy Lean, Obese and Colorectal Cancer-Affected Individuals. International Journal of Molecular Sciences, 25(6), 3357. https://doi.org/10.3390/ijms25063357






