Lactiplantibacillus (Lactobacillus) plantarum as a Complementary Treatment to Improve Symptomatology in Neurodegenerative Disease: A Systematic Review of Open Access Literature
Abstract
1. Introduction
1.1. The Neurodegenerative Disease
1.2. The Impact of Gut Microbiota in Neurodegenerative Disease
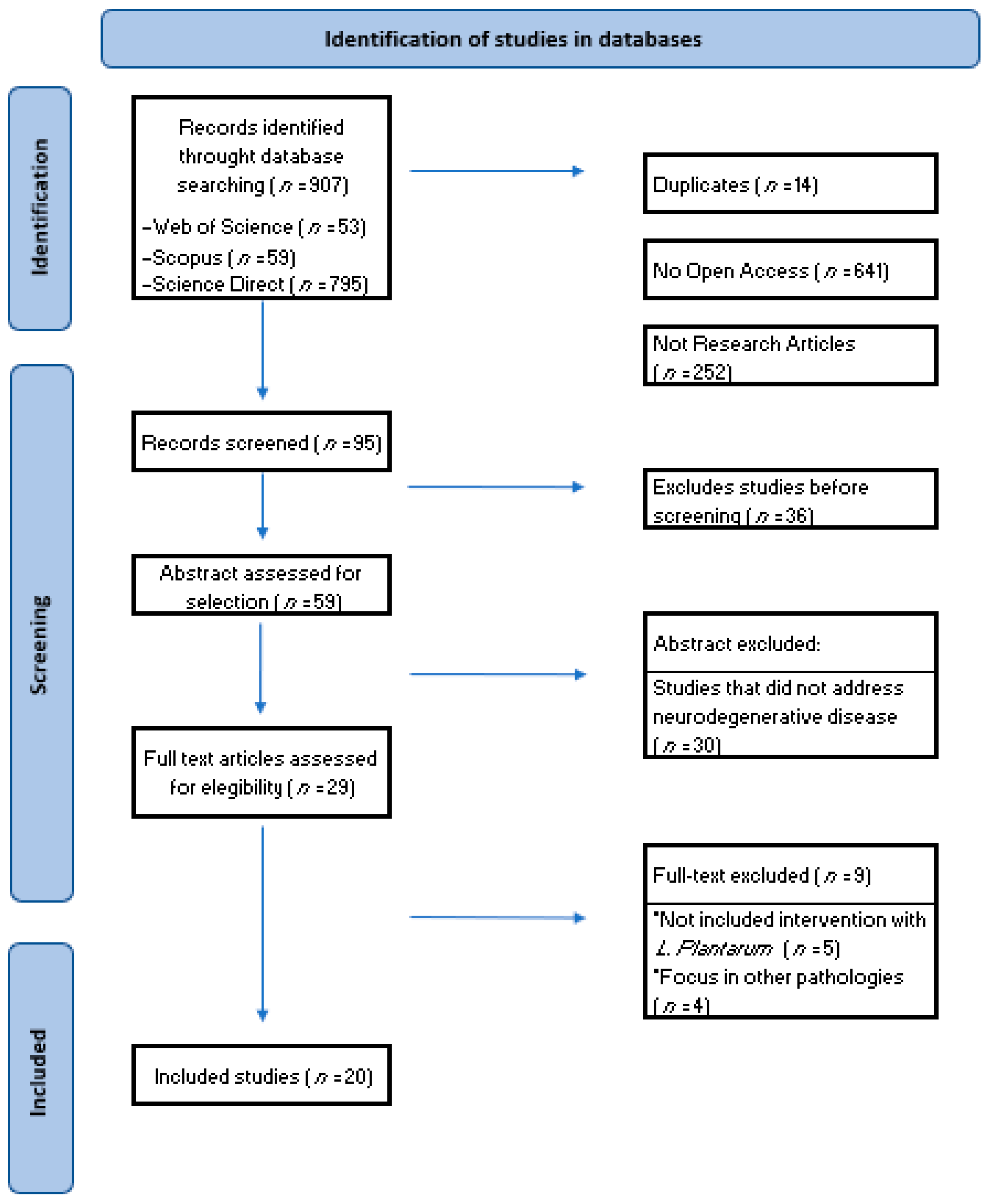
2. Methods
2.1. Literature Search
2.2. Study Selection
3. Results
3.1. Data Extraction
- ▪
- Type of study (human or animal models);
- ▪
- Type of probiotic used (Lactobacillus plantarum or Lactiplantibacillus plantarum alone or in combination);
- ▪
- Neurodegenerative pathology addressed in the research;
- ▪
- Population (description);
- ▪
- Methodology of the research carried out;
- ▪
- Intervention (dose administered, time);
- ▪
- Results obtained after the intervention with Lactobacillus plantarum or Lactiplantibacillus plantarum.
3.2. Human Model
3.2.1. Parkinson’s Disease
3.2.2. Mild Cognitive Impairment
3.3. Animal Model
3.3.1. Alzheimer’s Disease
3.3.2. Parkinson’s Disease
3.3.3. Multiple Sclerosis
3.3.4. Oxidative Stress
3.3.5. Cognitive Decline and Oxidative Stress
3.3.6. Neurodegenerative Process
4. Discussion
Limitations and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tam, O.H.; Ostrow, L.W.; Hammell, M.G. Diseases of the nERVous system: Retrotransposon activity in neurodegenerative disease. Mob. DNA 2019, 10, 32. [Google Scholar] [CrossRef]
- Guzman-Martinez, L.; Maccioni, R.B.; Andrade, V.; Navarrete, L.P.; Pastor, M.G.; Ramos-Escobar, N. Neuroinflammation as a Common Feature of Neurodegenerative Disorders. Front. Pharmacol. 2019, 10, 1008. [Google Scholar] [CrossRef]
- Muddapu, V.R.; Dharshini, S.A.P.; Chakravarthy, V.S.; Gromiha, M.M. Neurodegenerative Diseases—Is Metabolic Deficiency the Root Cause? Front. Neurosci. 2020, 14, 213. [Google Scholar] [CrossRef]
- Rekatsina, M.; Paladini, A.; Piroli, A.; Zis, P.; Pergolizzi, J.V.; Varrassi, G. Pathophysiology and Therapeutic Perspectives of Oxidative Stress and Neurodegenerative Diseases: A Narrative Review. Adv. Ther. 2020, 37, 113–139. [Google Scholar] [CrossRef]
- Nichols, E.; Steinmetz, J.D.; Vollset, S.E.; Fukutaki, K.; Chalek, J.; Abd-Allah, F.; Abdoli, A.; Abualhasan, A.; Abu-Gharbieh, E.; Akram, T.T.; et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef] [PubMed]
- Harciarek, M.; Kertesz, A. The Prevalence of Misidentification Syndromes in Neurodegenerative Diseases. Alzheimer Dis. Assoc. Disord. 2008, 22, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhou, Y.; Gao, Q.; Ping, D.; Wang, Y.; Wu, W.; Lin, X.; Fang, Y.; Zhang, J.; Shao, A. The Role of Exosomal microRNAs and Oxidative Stress in Neurodegenerative Diseases. Oxidative Med. Cell. Longev. 2020, 2020, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Teleanu, D.M.; Niculescu, A.G.; Lungu, I.I.; Radu, C.I.; Vladâcenco, O.; Roza, E.; Costăchescu, B.; Grumezescu, A.M.; Teleanu, R.I. An Overview of Oxidative Stress, Neuroinflammation, and Neurodegenerative Diseases. Int. J. Mol. Sci. 2022, 23, 5938. [Google Scholar] [CrossRef] [PubMed]
- Rehman, M.U.; Sehar, N.; Dar, N.J.; Khan, A.; Arafah, A.; Rashid, S.; Rashid, S.M.; Ganaie, M.A. Mitochondrial dysfunctions, oxidative stress and neuroinflammation as therapeutic targets for neurodegenerative diseases: An update on current advances and impediments. Neurosci. Biobehav. Rev. 2023, 144, 104961. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Redondo-Flórez, L.; Beltrán-Velasco, A.I.; Ramos-Campo, D.J.; Belinchón-deMiguel, P.; Martinez-Guardado, I.; Dalamitros, A.A.; Yáñez-Sepúlveda, R.; Martín-Rodríguez, A.; Tornero-Aguilera, J.F. Mitochondria and Brain Disease: A Comprehensive Review of Pathological Mechanisms and Therapeutic Opportunities. Biomedicines 2023, 11, 2488. [Google Scholar] [CrossRef]
- Cenini, G.; Lloret, A.; Cascella, R. Oxidative Stress in Neurodegenerative Diseases: From a Mitochondrial Point of View. Oxidative Med. Cell. Longev. 2019, 2019, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Konovalova, J.; Gerasymchuk, D.; Parkkinen, I.; Chmielarz, P.; Domanskyi, A. Interplay between MicroRNAs and Oxidative Stress in Neurodegenerative Diseases. Int. J. Mol. Sci. 2019, 20, 6055. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Kukreti, R.; Saso, L.; Kukreti, S. Oxidative Stress: A Key Modulator in Neurodegenerative Diseases. Molecules 2019, 24, 1583. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Chen, M.; Jiang, J. Mitochondrial dysfunction in neurodegenerative diseases and drug targets via apoptotic signaling. Mitochondrion 2019, 49, 35–45. [Google Scholar] [CrossRef]
- Callizot, N.; Combes, M.; Henriques, A.; Poindron, P. Necrosis, apoptosis, necroptosis, three modes of action of dopaminergic neuron neurotoxins. PLoS ONE 2019, 14, e0215277. [Google Scholar] [CrossRef]
- Saleem, S. Apoptosis, Autophagy, Necrosis and Their Multi Galore Crosstalk in Neurodegeneration. Neuroscience 2021, 469, 162–174. [Google Scholar] [CrossRef]
- Shandilya, S.; Kumar, S.; Jha, N.K.; Kesari, K.K.; Ruokolainen, J. Interplay of gut microbiota and oxidative stress: Perspective on neurodegeneration and neuroprotection. J. Adv. Res. 2022, 38, 223–244. [Google Scholar] [CrossRef]
- Shang, H.; Zhao, X.; Zhang, X. Neurodegenerative Diseases. In Pediatric Neuroimaging; Springer: Singapore, 2022; pp. 211–214. [Google Scholar]
- Mohammadi, A.; Colagar, A.H.; Khorshidian, A.; Amini, S.M. The Functional Roles of Curcumin on Astrocytes in Neurodegenerative Diseases. Neuroimmunomodulation 2022, 29, 4–14. [Google Scholar] [CrossRef]
- Litke, R.; Garcharna, L.C.; Jiwani, S.; Neugroschl, J. Modifiable Risk Factors in Alzheimer Disease and Related Dementias: A Review. Clin. Ther. 2021, 43, 953–965. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Fact Sheets of Dementia; World Health Organization: Geneva, Switzerland, 2021; Available online: https:// www.who.int/news-room/fact-sheets/detail/dementia (accessed on 2 March 2024).
- Shahnawaz, M.; Mukherjee, A.; Pritzkow, S.; Mendez, N.; Rabadia, P.; Liu, X.; Hu, B.; Schmeichel, A.; Singer, W.; Wu, G.; et al. Discriminating α-synuclein strains in Parkinson’s disease and multiple system atrophy. Nature 2020, 578, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Mus, L.; Siani, F.; Giuliano, C.; Ghezzi, C.; Cerri, S.; Blandini, F. Development and biochemical characterization of a mouse model of Parkinson’s disease bearing defective glucocerebrosidase activity. Neurobiol. Dis. 2019, 124, 289–296. [Google Scholar] [CrossRef]
- Meoni, S.; Cury, R.G.; Moro, E. New players in basal ganglia dysfunction in Parkinson’s disease. Prog. Brain Res. 2020, 252, 307–327. [Google Scholar]
- Navarro-López, E.M.; Çelikok, U.; Şengör, N.S. A dynamical model for the basal ganglia-thalamo-cortical oscillatory activity and its implications in Parkinson’s disease. Cogn. Neurodyn. 2021, 15, 693–720. [Google Scholar] [CrossRef]
- Adler, A.F.; Cardoso, T.; Nolbrant, S.; Mattsson, B.; Hoban, D.B.; Jarl, U.; Wahlestedt, J.N.; Grealish, S.; Björklund, A.; Parmar, M. hESC-Derived Dopaminergic Transplants Integrate into Basal Ganglia Circuitry in a Preclinical Model of Parkinson’s Disease. Cell Rep. 2019, 28, 3462–3473.e5. [Google Scholar] [CrossRef]
- Park, Y.W.; Shin, N.; Chung, S.J.; Kim, J.; Lim, S.M.; Lee, P.H.; Lee, S.; Ahn, K.J. Magnetic Resonance Imaging–Visible Perivascular Spaces in Basal Ganglia Predict Cognitive Decline in Parkinson’s Disease. Mov. Disord. 2019, 34, 1672–1679. [Google Scholar] [CrossRef]
- Weintraub, D.; Aarsland, D.; Chaudhuri, K.R.; Dobkin, R.D.; Leentjens, A.F.; Rodriguez-Violante, M.; Schrag, A. The neuropsychiatry of Parkinson’s disease: Advances and challenges. Lancet Neurol. 2022, 21, 89–102. [Google Scholar] [CrossRef]
- Armstrong, M.J.; Okun, M.S. Diagnosis and Treatment of Parkinson Disease. JAMA 2020, 323, 548–560. [Google Scholar] [CrossRef] [PubMed]
- Peball, M.; Krismer, F.; Knaus, H.; Djamshidian, A.; Werkmann, M.; Carbone, F.; Ellmerer, P.; Heim, B.; Marini, K.; Valent, D.; et al. Non-Motor Symptoms in Parkinson’s Disease are Reduced by Nabilone. Ann. Neurol. 2020, 88, 712–722. [Google Scholar] [CrossRef] [PubMed]
- Babiloni, A.H.; Bellemare, A.; Beetz, G.; Vinet, S.-A.; Martel, M.O.; Lavigne, G.J.; De Beaumont, L. The effects of non-invasive brain stimulation on sleep disturbances among different neurological and neuropsychiatric conditions: A systematic review. Sleep Med. Rev. 2021, 55, 101381. [Google Scholar] [CrossRef]
- Maggi, G.; Trojano, L.; Barone, P.; Santangelo, G. Sleep Disorders and Cognitive Dysfunctions in Parkinson’s Disease: A Meta-Analytic Study. Neuropsychol. Rev. 2021, 31, 643–682. [Google Scholar] [CrossRef]
- Adiele, R.C.; Adiele, C.A. Metabolic defects in multiple sclerosis. Mitochondrion 2019, 44, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Sasso, B.L.; Agnello, L.; Bivona, G.; Bellia, C.; Ciaccio, M. Cerebrospinal Fluid Analysis in Multiple Sclerosis Diagnosis: An Update. Medicina 2019, 55, 245. [Google Scholar] [CrossRef] [PubMed]
- Absinta, M.; Sati, P.; Masuzzo, F.; Nair, G.; Sethi, V.; Kolb, H.; Ohayon, J.; Wu, T.; Cortese, I.C.M.; Reich, D.S. Association of Chronic Active Multiple Sclerosis Lesions With Disability In Vivo. JAMA Neurol. 2019, 76, 1474–1483. [Google Scholar] [CrossRef] [PubMed]
- Zeng, C.; Gu, L.; Liu, Z.; Zhao, S. Review of Deep Learning Approaches for the Segmentation of Multiple Sclerosis Lesions on Brain MRI. Front. Neurosci. 2020, 14, 610967. [Google Scholar] [CrossRef]
- Calvi, A.; Haider, L.; Prados, F.; Tur, C.; Chard, D.; Barkhof, F. In vivo imaging of chronic active lesions in multiple sclerosis. Mult. Scler. J. 2022, 28, 683–690. [Google Scholar] [CrossRef]
- Villarreal, J.V.; Abraham, M.J.; Acevedo, J.A.; Rai, P.K.; Thottempudi, N.; Fang, X.; Gogia, B. Tumefactive multiple sclerosis (TMS): A case series of this challenging variant of MS. Mult. Scler. Relat. Disord. 2021, 48, 102699. [Google Scholar] [CrossRef]
- Vaddepally, R.; Sodavarapu, S.; Kutadi, A.; Taylor, W.; Kumar, N. Case Report: A case of immune checkpoint inhibitor therapy in a patient with multiple sclerosis. F1000Research 2020, 9, 1167. [Google Scholar] [CrossRef]
- McGinley, M.P.; Goldschmidt, C.H.; Rae-Grant, A.D. Diagnosis and Treatment of Multiple Sclerosis. JAMA 2021, 325, 765–779. [Google Scholar] [CrossRef]
- Silveira, C.; Guedes, R.; Maia, D.; Curral, R.; Coelho, R. Neuropsychiatric Symptoms of Multiple Sclerosis: State of the Art. Psychiatry Investig. 2019, 16, 877–888. [Google Scholar] [CrossRef]
- Rommer, P.S.; Eichstädt, K.; Ellenberger, D.; Flachenecker, P.; Friede, T.; Haas, J.; Kleinschnitz, C.; Pöhlau, D.; Rienhoff, O.; Stahmann, A.; et al. Symptomatology and symptomatic treatment in multiple sclerosis: Results from a nationwide MS registry. Mult. Scler. J. 2019, 25, 1641–1652. [Google Scholar] [CrossRef]
- Uceda, S.; Echeverry-Alzate, V.; Reiriz-Rojas, M.; Martínez-Miguel, E.; Pérez-Curiel, A.; Gómez-Senent, S.; Beltrán-Velasco, A.I. Gut Microbial Metabolome and Dysbiosis in Neurodegenerative Diseases: Psychobiotics and Fecal Microbiota Transplantation as a Therapeutic Approach—A Comprehensive Narrative Review. Int. J. Mol. Sci. 2023, 24, 13294. [Google Scholar] [CrossRef]
- Rinninella, E.; Raoul, P.; Cintoni, M.; Franceschi, F.; Miggiano, G.A.; Gasbarrini, A.; Mele, M.C. What Is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms 2019, 7, 14. [Google Scholar] [CrossRef] [PubMed]
- Al Bander, Z.; Nitert, M.D.; Mousa, A.; Naderpoor, N. The Gut Microbiota and Inflammation: An Overview. Int. J. Environ. Res. Public Health 2020, 17, 7618. [Google Scholar] [CrossRef] [PubMed]
- Verhaar, B.J.H.; Hendriksen, H.M.A.; de Leeuw, F.A.; Doorduijn, A.S.; van Leeuwenstijn, M.; Teunissen, C.E.; Barkhof, F.; Scheltens, P.; Kraaij, R.; van Duijn, C.M.; et al. Gut Microbiota Composition Is Related to AD Pathology. Front. Immunol. 2022, 12, 794519. [Google Scholar] [CrossRef] [PubMed]
- Michaudel, C.; Sokol, H. The Gut Microbiota at the Service of Immunometabolism. Cell Metab. 2020, 32, 514–523. [Google Scholar] [CrossRef]
- Gomaa, E.Z. Human gut microbiota/microbiome in health and diseases: A review. Antonie van Leeuwenhoek 2020, 113, 2019–2040. [Google Scholar] [CrossRef]
- Chen, Y.; Zhou, J.; Wang, L. Role and Mechanism of Gut Microbiota in Human Disease. Front. Cell. Infect. Microbiol. 2021, 11, 86. [Google Scholar] [CrossRef]
- Dingeo, G.; Brito, A.; Samouda, H.; Iddir, M.; La Frano, M.R.; Bohn, T. Phytochemicals as modifiers of gut microbial communities. Food Funct. 2020, 11, 8444–8471. [Google Scholar] [CrossRef]
- Marć, M.A.; Jastrząb, R.; Mytych, J. Does the Gut Microbial Metabolome Really Matter? The Connection between GUT Metabolome and Neurological Disorders. Nutrients 2022, 14, 3967. [Google Scholar] [CrossRef]
- Chen, Z.; Maqbool, J.; Sajid, F.; Hussain, G.; Sun, T. Human gut microbiota and its association with pathogenesis and treatments of neurodegenerative diseases. Microb. Pathog. 2021, 150, 104675. [Google Scholar] [CrossRef]
- Ning, J.; Huang, S.Y.; Chen, S.D.; Zhang, Y.R.; Huang, Y.Y.; Yu, J.T. Investigating Casual Associations Among Gut Microbiota, Metabolites, and Neurodegenerative Diseases: A Mendelian Randomization Study. J. Alzheimer’s Dis. 2022, 87, 211–222. [Google Scholar] [CrossRef]
- Wallace, T.C.; Guarner, F.; Madsen, K.; Cabana, M.D.; Gibson, G.; Hentges, E.; Sanders, M.E. Human gut microbiota and its relationship to health and disease. Nutr. Rev. 2011, 69, 392–403. [Google Scholar] [CrossRef]
- Lozupone, C.A.; Stombaugh, J.I.; Gordon, J.I.; Jansson, J.K.; Knight, R. Diversity, stability and resilience of the human gut microbiota. Nature 2012, 489, 220–230. [Google Scholar] [CrossRef]
- Harmsen, H.J.M.; de Goffau Marcus, C. The Human Gut Microbiota. In Microbiota of the Human Body: Implications in Health and Disease; Springer: Berlin/Heidelberg, Germany, 2016; pp. 95–108. [Google Scholar]
- Al-Rashidi, H.E. Gut microbiota and immunity relevance in eubiosis and dysbiosis. Saudi J. Biol. Sci. 2022, 29, 1628–1643. [Google Scholar] [CrossRef]
- Jurjus, A.; Eid, A.; Al Kattar, S.; Zeenny, M.N.; Gerges-Geagea, A.; Haydar, H.; Hilal, A.; Oueidat, D.; Matar, M.; Tawilah, J.; et al. Inflammatory bowel disease, colorectal cancer and type 2 diabetes mellitus: The links. BBA Clin. 2016, 5, 16–24. [Google Scholar] [CrossRef]
- Borrego-Ruiz, A.; Borrego, J.J. An updated overview on the relationship between human gut microbiome dysbiosis and psychiatric and psychological disorders. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2024, 128, 110861. [Google Scholar] [CrossRef]
- Aponte, M.; Murru, N.; Shoukat, M. Therapeutic, Prophylactic, and Functional Use of Probiotics: A Current Perspective. Front. Microbiol. 2020, 11, 562048. [Google Scholar] [CrossRef]
- Tremblay, A.; Lingrand, L.; Maillard, M.; Feuz, B.; Tompkins, T.A. The effects of psychobiotics on the microbiota-gut-brain axis in early-life stress and neuropsychiatric disorders. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 105, 110142. [Google Scholar] [CrossRef]
- Ağagündüz, D.; Kocaadam-Bozkurt, B.; Bozkurt, O.; Sharma, H.; Esposito, R.; Özoğul, F.; Capasso, R. Microbiota alteration and modulation in Alzheimer’s disease by gerobiotics: The gut-health axis for a good mind. Biomed. Pharmacother. 2022, 153, 113430. [Google Scholar] [CrossRef]
- Faulin, T.d.E.S.; Estadella, D. Alzheimer’s disease and its relationship with the microbiota-gut-brain axis. Arq. Gastroenterol. 2023, 60, 144–154. [Google Scholar] [CrossRef]
- Morella, I.; Negro, M.; Dossena, M.; Brambilla, R.; D’Antona, G. Gut-muscle-brain axis: Molecular mechanisms in neurodegenerative disorders and potential therapeutic efficacy of probiotic supplementation coupled with exercise. Neuropharmacology 2023, 240, 109718. [Google Scholar] [CrossRef]
- Kumar, H.; Dhalaria, R.; Guleria, S.; Cimler, R.; Sharma, R.; Siddiqui, S.A.; Valko, M.; Nepovimova, E.; Dhanjal, D.S.; Singh, R.; et al. Anti-oxidant potential of plants and probiotic spp. in alleviating oxidative stress induced by H2O2. Biomed. Pharmacother. 2023, 165, 115022. [Google Scholar] [CrossRef]
- Suganya, K.; Koo, B.-S. Gut–Brain Axis: Role of Gut Microbiota on Neurological Disorders and How Probiotics/Prebiotics Beneficially Modulate Microbial and Immune Pathways to Improve Brain Functions. Int. J. Mol. Sci. 2020, 21, 7551. [Google Scholar] [CrossRef]
- Shabbir, U.; Arshad, M.S.; Sameen, A.; Oh, D.-H. Crosstalk between Gut and Brain in Alzheimer’s Disease: The Role of Gut Microbiota Modulation Strategies. Nutrients 2021, 13, 690. [Google Scholar] [CrossRef]
- Wang, P.; Gao, J.; Ke, W.; Wang, J.; Li, D.; Liu, R.; Jia, Y.; Wang, X.; Chen, X.; Chen, F.; et al. Resveratrol reduces obesity in high-fat diet-fed mice via modulating the composition and metabolic function of the gut microbiota. Free Radic. Biol. Med. 2020, 156, 83–98. [Google Scholar] [CrossRef]
- Fan, Y.; Pedersen, O. Gut microbiota in human metabolic health and disease. Nat. Rev. Microbiol. 2021, 19, 55–71. [Google Scholar] [CrossRef]
- Leta, V.; Chaudhuri, K.R.; Milner, O.; Chung-Faye, G.; Metta, V.; Pariante, C.M.; Borsini, A. Neurogenic and anti-inflammatory effects of probiotics in Parkinson’s disease: A systematic review of preclinical and clinical evidence. Brain Behav. Immun. 2021, 98, 59–73. [Google Scholar] [CrossRef]
- Socała, K.; Doboszewska, U.; Szopa, A.; Serefko, A.; Włodarczyk, M.; Zielińska, A.; Poleszak, E.; Fichna, J.; Wlaź, P. The role of microbiota-gut-brain axis in neuropsychiatric and neurological disorders. Pharmacol. Res. 2021, 172, 105840. [Google Scholar] [CrossRef]
- Korf, J.M.; Ganesh, B.P.; McCullough, L.D. Gut dysbiosis and age-related neurological diseases in females. Neurobiol. Dis. 2022, 168, 105695. [Google Scholar] [CrossRef]
- Aizawa, E.; Tsuji, H.; Asahara, T.; Takahashi, T.; Teraishi, T.; Yoshida, S.; Koga, N.; Hattori, K.; Ota, M.; Kunugi, H. Bifidobacterium and Lactobacillus Counts in the Gut Microbiota of Patients With Bipolar Disorder and Healthy Controls. Front. Psychiatry 2019, 9, 730. [Google Scholar] [CrossRef]
- Monteiro, C.R.A.V.; Carmo, M.S.D.; Melo, B.O.; Alves, M.S.; dos Santos, C.I.; Monteiro, S.G.; Bomfim, M.R.Q.; Fernandes, E.S.; Monteiro-Neto, V. In Vitro Antimicrobial Activity and Probiotic Potential of Bifidobacterium and Lactobacillus against Species of Clostridium. Nutrients 2019, 11, 448. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Zhang, Y.; Li, H.; Liu, X. The potential of proteins, hydrolysates and peptides as growth factors for Lactobacillus and Bifidobacterium: Current research and future perspectives. Food Funct. 2020, 11, 1946–1957. [Google Scholar] [CrossRef]
- Wang, C.-H.; Yen, H.-R.; Lu, W.-L.; Ho, H.-H.; Lin, W.-Y.; Kuo, Y.-W.; Huang, Y.-Y.; Tsai, S.-Y.; Lin, H.-C. Adjuvant Probiotics of Lactobacillus salivarius subsp. salicinius AP-32, L. johnsonii MH-68, and Bifidobacterium animalis subsp. lactis CP-9 Attenuate Glycemic Levels and Inflammatory Cytokines in Patients With Type 1 Diabetes Mellitus. Front. Endocrinol. (Lausanne) 2022, 13, 754401. [Google Scholar] [CrossRef]
- Ni, Y.; Zhang, Y.; Zheng, L.; Rong, N.; Yang, Y.; Gong, P.; Yang, Y.; Siwu, X.; Zhang, C.; Zhu, L.; et al. Bifidobacterium and Lactobacillus improve inflammatory bowel disease in zebrafish of different ages by regulating the intestinal mucosal barrier and microbiota. Life Sci. 2023, 324, 121699. [Google Scholar] [CrossRef]
- Mohammadi, G.; Dargahi, L.; Peymani, A.; Mirzanejad, Y.; Alizadeh, S.A.; Naserpour, T.; Nassiri-Asl, M. The Effects of Probiotic Formulation Pretreatment (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) on a Lipopolysaccharide Rat Model. J. Am. Coll. Nutr. 2019, 38, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, G.; Dargahi, L.; Naserpour, T.; Mirzanejad, Y.; Alizadeh, S.A.; Peymani, A.; Nassiri-Asl, M. Probiotic mixture of Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 attenuates hippocampal apoptosis induced by lipopolysaccharide in rats. Int. Microbiol. 2019, 22, 317–323. [Google Scholar] [CrossRef]
- Un-Nisa, A.; Khan, A.; Zakria, M.; Siraj, S.; Ullah, S.; Tipu, M.K.; Ikram, M.; Kim, M.O. Updates on the Role of Probiotics against Different Health Issues: Focus on Lactobacillus. Int. J. Mol. Sci. 2022, 24, 142. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.-H.; Liu, Y.-W.; Wu, C.-C.; Wang, S.; Tsai, Y.-C. Psychobiotics in mental health, neurodegenerative and neurodevelopmental disorders. J. Food Drug Anal. 2019, 27, 632–648. [Google Scholar] [CrossRef]
- Kong, Y.; Wang, L.; Jiang, B. The Role of Gut Microbiota in Aging and Aging Related Neurodegenerative Disorders: Insights from Drosophila Model. Life 2021, 11, 855. [Google Scholar] [CrossRef]
- Sun, P.; Su, L.; Zhu, H.; Li, X.; Guo, Y.; Du, X.; Zhang, L.; Qin, C. Gut Microbiota Regulation and Their Implication in the Development of Neurodegenerative Disease. Microorganisms 2021, 9, 2281. [Google Scholar] [CrossRef]
- Ojha, S.; Patil, N.; Jain, M.; Kole, C.; Kaushik, P. Probiotics for Neurodegenerative Diseases: A Systemic Review. Microorganisms 2023, 11, 1083. [Google Scholar] [CrossRef]
- Patel, C.; Pande, S.; Acharya, S. Potentiation of anti-Alzheimer activity of curcumin by probiotic Lactobacillus rhamnosus UBLR-58 against scopolamine-induced memory impairment in mice. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2020, 393, 1955–1962. [Google Scholar] [CrossRef]
- Wang, L.; Zhao, Z.; Zhao, L.; Zhao, Y.; Yang, G.; Wang, C.; Gao, L.; Niu, C.; Li, S. Lactobacillus plantarum DP189 Reduces α-SYN Aggravation in MPTP-Induced Parkinson’s Disease Mice via Regulating Oxidative Damage, Inflammation, and Gut Microbiota Disorder. J. Agric. Food Chem. 2022, 70, 1163–1173. [Google Scholar] [CrossRef]
- Bi, M.; Liu, C.; Wang, Y.; Liu, S.-J. Therapeutic Prospect of New Probiotics in Neurodegenerative Diseases. Microorganisms 2023, 11, 1527. [Google Scholar] [CrossRef]
- Mateo, D.; Marquès, M.; Domingo, J.L.; Torrente, M. Influence of gut microbiota on the development of most prevalent neurodegenerative dementias and the potential effect of probiotics in elderly: A scoping review. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2023, 195, e32959. [Google Scholar] [CrossRef]
- Solanki, R.; Karande, A.; Ranganathan, P. Emerging role of gut microbiota dysbiosis in neuroinflammation and neurodegeneration. Front. Neurol. 2023, 14, 1149618. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Prisma-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Page, M.J.; E McKenzie, J.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Moher, D. Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J. Clin. Epidemiol. 2021, 134, 103–112. [Google Scholar] [CrossRef]
- Ghyselinck, J.; Verstrepen, L.; Moens, F.; Abbeele, P.V.D.; Bruggeman, A.; Said, J.; Smith, B.; Barker, L.A.; Jordan, C.; Leta, V.; et al. Influence of probiotic bacteria on gut microbiota composition and gut wall function in an in-vitro model in patients with Parkinson’s disease. Int. J. Pharm. X 2021, 3, 100087. [Google Scholar] [CrossRef]
- Lu, C.-S.; Chang, H.-C.; Weng, Y.-H.; Chen, C.-C.; Kuo, Y.-S.; Tsai, Y.-C. The Add-On Effect of Lactobacillus plantarum PS128 in Patients With Parkinson’s Disease: A Pilot Study. Front. Nutr. 2021, 8, 650053. [Google Scholar] [CrossRef]
- Fei, Y.; Wang, R.; Lu, J.; Peng, S.; Yang, S.; Wang, Y.; Zheng, K.; Li, R.; Lin, L.; Li, M. Probiotic intervention benefits multiple neural behaviors in older adults with mild cognitive impairment. Geriatr. Nurs. 2023, 51, 167–175. [Google Scholar] [CrossRef]
- Bonfili, L.; Cecarini, V.; Gogoi, O.; Berardi, S.; Scarpona, S.; Angeletti, M.; Rossi, G.; Eleuteri, A.M. Gut microbiota manipulation through probiotics oral administration restores glucose homeostasis in a mouse model of Alzheimer’s disease. Neurobiol. Aging 2020, 87, 35–43. [Google Scholar] [CrossRef]
- Lee, D.-Y.; Shin, Y.-J.; Kim, J.-K.; Jang, H.-M.; Joo, M.-K.; Kim, D.-H. Alleviation of cognitive impairment by gut microbiota lipopolysaccharide production-suppressing Lactobacillus plantarum and Bifidobacterium longum in mice. Food Funct. 2021, 12, 10750–10763. [Google Scholar] [CrossRef] [PubMed]
- Mallikarjuna, N.; Praveen, K.; Yellamma, K. Role of Lactobacillus plantarum MTCC1325 in membrane-bound transport ATPases system in Alzheimer’s disease-induced rat brain. BioImpacts 2016, 6, 203–209. [Google Scholar] [CrossRef]
- Kaur, H.; Nookala, S.; Singh, S.; Mukundan, S.; Nagamoto-Combs, K.; Combs, C.K. Sex-Dependent Effects of Intestinal Microbiome Manipulation in a Mouse Model of Alzheimer’s Disease. Cells 2021, 10, 2370. [Google Scholar] [CrossRef]
- Liao, J.-F.; Cheng, Y.-F.; You, S.-T.; Kuo, W.-C.; Huang, C.-W.; Chiou, J.-J.; Hsu, C.-C.; Hsieh-Li, H.-M.; Wang, S.; Tsai, Y.-C. Lactobacillus plantarum PS128 alleviates neurodegenerative progression in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced mouse models of Parkinson’s disease. Brain Behav. Immun. 2020, 90, 26–46. [Google Scholar] [CrossRef]
- Lee, Y.Z.; Cheng, S.-H.; Chang, M.-Y.; Lin, Y.-F.; Wu, C.-C.; Tsai, Y.-C. Neuroprotective Effects of Lactobacillus plantarum PS128 in a Mouse Model of Parkinson’s Disease: The Role of Gut Microbiota and MicroRNAs. Int. J. Mol. Sci. 2023, 24, 6794. [Google Scholar] [CrossRef]
- Wang, L.; Li, S.; Jiang, Y.; Zhao, Z.; Shen, Y.; Zhang, J.; Zhao, L. Neuroprotective effect of Lactobacillus plantarum DP189 on MPTP-induced Parkinson’s disease model mice. J. Funct. Foods 2021, 85, 104635. [Google Scholar] [CrossRef]
- Perez Visñuk, D.; Savoy de Giori, G.; LeBlanc, J.G.; de Moreno de LeBlanc, A. Neuroprotective effects associated with immune modulation by selected lactic acid bacteria in a Parkinson’s disease model. Nutrition 2020, 79–80, 110995. [Google Scholar] [CrossRef]
- Perez Visñuk, D.; del Milagro Teran, M.; Savoy de Giori, G.; LeBlanc, J.G.; de Moreno de LeBlanc, A. Neuroprotective Effect of Riboflavin Producing Lactic Acid Bacteria in Parkinsonian Models. Neurochem. Res. 2022, 47, 1269–1279. [Google Scholar] [CrossRef]
- Xu, Y.; Xie, M.; Xue, J.; Xiang, L.; Li, Y.; Xiao, J.; Xiao, G.; Wang, H. EGCG ameliorates neuronal and behavioral defects by remodeling gut microbiota and TotM expression in Drosophila models of Parkinson’s disease. FASEB J. 2020, 34, 5931–5950. [Google Scholar] [CrossRef]
- Ilie, O.-D.; Duta, R.; Balmus, I.-M.; Savuca, A.; Petrovici, A.; Nita, I.-B.; Antoci, L.-M.; Jijie, R.; Mihai, C.-T.; Ciobica, A.; et al. Assessing the Neurotoxicity of a Sub-Optimal Dose of Rotenone in Zebrafish (Danio rerio) and the Possible Neuroactive Potential of Valproic Acid, Combination of Levodopa and Carbidopa, and Lactic Acid Bacteria Strains. Antioxidants 2022, 11, 2040. [Google Scholar] [CrossRef]
- Mestre, L.; Carrillo-Salinas, F.J.; Feliú, A.; Mecha, M.; Alonso, G.; Espejo, C.; Calvo-Barreiro, L.; Luque-García, J.L.; Estevez, H.; Villar, L.M.; et al. How oral probiotics affect the severity of an experimental model of progressive multiple sclerosis? Bringing commensal bacteria into the neurodegenerative process. Gut Microbes 2020, 12, 1813532. [Google Scholar] [CrossRef]
- Shang, X.; Geng, L.; Zhao, Z.; Luo, L.; Shi, X.; Zhang, Q.; Du, R.; Cong, Y.; Xu, W. Transcriptomics reveals the mechanism of selenium-enriched Lactobacillus plantarum alleviating brain oxidative stress under cadmium stress in Luciobarbus capito. Ecotoxicol. Environ. Saf. 2022, 242, 113890. [Google Scholar] [CrossRef]
- Xu, Z.; Zhang, J.; Wu, J.; Yang, S.; Li, Y.; Wu, Y.; Li, S.; Zhang, X.; Zuo, W.; Lian, X.; et al. Lactobacillus plantarum ST-III culture supernatant ameliorates alcohol-induced cognitive dysfunction by reducing endoplasmic reticulum stress and oxidative stress. Front. Neurosci. 2022, 16, 976358. [Google Scholar] [CrossRef] [PubMed]
- Westfall, S.; Lomis, N.; Prakash, S. Longevity extension in Drosophila through gut-brain communication. Sci. Rep. 2018, 8, 8362. [Google Scholar] [CrossRef]
- Zaydi, A.I.; Lew, L.C.; Hor, Y.Y.; Jaafar, M.H.; Chuah, L.O.; Yap, K.P.; Azlan, A.; Azzam, G.; Liong, M.T. Lactobacillus plantarum DR7 improved brain health in aging rats via the serotonin, inflammatory and apoptosis pathways. Benef. Microbes 2020, 11, 753–766. [Google Scholar] [CrossRef] [PubMed]
- Xia, Y.; Gong, Y.; Lin, X.; Yang, Y.; Song, X.; Wang, G.; Xiong, Z.; Qian, Y.; Liao, Z.; Zhang, H.; et al. Lactobacillus plantarum AR113 attenuates liver injury in D-galactose-induced aging mice via the inhibition of oxidative stress and endoplasmic reticulum stress. Food Sci. Hum. Wellness 2024, 13, 885–897. [Google Scholar] [CrossRef]
- Mirzaei, H.; Sedighi, S.; Kouchaki, E.; Barati, E.; Dadgostar, E.; Aschner, M.; Tamtaji, O.R. Probiotics and the Treatment of Parkinson’s Disease: An Update. Cell. Mol. Neurobiol. 2022, 42, 2449–2457. [Google Scholar] [CrossRef]
- Tan, A.H.; Hor, J.W.; Chong, C.W.; Lim, S. Probiotics for Parkinson’s disease: Current evidence and future directions. JGH Open 2021, 5, 414–419. [Google Scholar] [CrossRef]
- Metta, V.; Leta, V.; Mrudula, K.R.; Prashanth, L.K.; Goyal, V.; Borgohain, R.; Chung-Faye, G.; Chaudhuri, K.R. Gastrointestinal dysfunction in Parkinson’s disease: Molecular pathology and implications of gut microbiome, probiotics, and fecal microbiota transplantation. J. Neurol. 2022, 269, 1154–1163. [Google Scholar] [CrossRef]
- Felice, V.D.; Quigley, E.M.; Sullivan, A.M.; O’Keeffe, G.W.; O’Mahony, S.M. Microbiota-gut-brain signalling in Parkinson’s disease: Implications for non-motor symptoms. Park. Relat. Disord. 2016, 27, 1–8. [Google Scholar] [CrossRef]
- Dutta, S.K.; Verma, S.; Jain, V.; Surapaneni, B.K.; Vinayek, R.; Phillips, L.; Nair, P.P. Parkinson’s Disease: The Emerging Role of Gut Dysbiosis, Antibiotics, Probiotics, and Fecal Microbiota Transplantation. J. Neurogastroenterol. Motil. 2019, 25, 363–376. [Google Scholar] [CrossRef]
- Chu, C.; Yu, L.; Li, Y.; Guo, H.; Zhai, Q.; Chen, W.; Tian, F. Meta-analysis of randomized controlled trials of the effects of probiotics in Parkinson’s disease. Food Funct. 2023, 14, 3406–3422. [Google Scholar] [CrossRef]
- Park, J.M.; Lee, S.C.; Ham, C.; Kim, Y.W. Effect of probiotic supplementation on gastrointestinal motility, inflammation, motor, non-motor symptoms and mental health in Parkinson’s disease: A meta-analysis of randomized controlled trials. Gut Pathog. 2023, 15, 9. [Google Scholar] [CrossRef]
- van Wamelen, D.J.; Martinez-Martin, P.; Weintraub, D.; Schrag, A.; Antonini, A.; Falup-Pecurariu, C.; Odin, P.; Ray Chaudhuri, K. The Non-Motor Symptoms Scale in Parkinson’s disease: Validation and use. Acta Neurol. Scand. 2021, 143, 3–12. [Google Scholar] [CrossRef]
- Hermanowicz, N.; Jones, S.A.; Hauser, R.A. Impact of non-motor symptoms in Parkinson’s disease: A PMDAlliance survey. Neuropsychiatr. Dis. Treat. 2019, 15, 2205–2212. [Google Scholar] [CrossRef]
- Goya, M.E.; Xue, F.; Sampedro-Torres-Quevedo, C.; Arnaouteli, S.; Riquelme-Dominguez, L.; Romanowski, A.; Brydon, J.; Ball, K.L.; Stanley-Wall, N.R.; Doitsidou, M. Probiotic Bacillus subtilis Protects against α-Synuclein Aggregation in C. elegans. Cell Rep. 2020, 30, 367–380.e7. [Google Scholar] [CrossRef]
- Liu, X.; Du, Z.R.; Wang, X.; Sun, X.R.; Zhao, Q.; Zhao, F.; Wong, W.T.; Wong, K.H.; Dong, X.-L. Polymannuronic acid prebiotic plus Lacticaseibacillus rhamnosus GG probiotic as a novel synbiotic promoted their separate neuroprotection against Parkinson’s disease. Food Res. Int. 2022, 155, 111067. [Google Scholar] [CrossRef]
- Chen, Z.; Zhong, C. Oxidative stress in Alzheimer’s disease. Neurosci. Bull. 2014, 30, 271–281. [Google Scholar] [CrossRef]
- Nimgampalle, M.; Kuna, Y. Anti-Alzheimer Properties of Probiotic, Lactobacillus plantarum MTCC 1325 in Alzheimer’s Disease induced Albino Rats. J. Clin. Diagn. Res. JCDR 2017, 11, KC01. [Google Scholar] [CrossRef]
- Cekanaviciute, E.; Yoo, B.B.; Runia, T.F.; Debelius, J.W.; Singh, S.; Nelson, C.A.; Kanner, R.; Bencosme, Y.; Lee, Y.K.; Hauser, S.L.; et al. Gut bacteria from multiple sclerosis patients modulate human T cells and exacerbate symptoms in mouse models. Proc. Natl. Acad. Sci. USA 2017, 114, 10713–10718. [Google Scholar] [CrossRef]
- Amini, M.E.; Shomali, N.; Bakhshi, A.; Rezaei, S.; Hemmatzadeh, M.; Hosseinzadeh, R.; Eslami, S.; Babaie, F.; Aslani, S.; Torkamandi, S.; et al. Gut microbiome and multiple sclerosis: New insights and perspective. Int. Immunopharmacol. 2020, 88, 107024. [Google Scholar] [CrossRef]
- Brown, J.; Quattrochi, B.; Everett, C.; Hong, B.-Y.; Cervantes, J. Gut commensals, dysbiosis, and immune response imbalance in the pathogenesis of multiple sclerosis. Mult. Scler. J. 2021, 27, 807–811. [Google Scholar] [CrossRef]
- Pilotto, S.; Zoledziewska, M.; Fenu, G.; Cocco, E.; Lorefice, L. Disease-modifying therapy for multiple sclerosis: Implications for gut microbiota. Mult. Scler. Relat. Disord. 2023, 73, 104671. [Google Scholar] [CrossRef]
- Zhang, L.; Liu, C.; Li, D.; Zhao, Y.; Zhang, X.; Zeng, X.; Yang, Z.; Li, S. Antioxidant activity of an exopolysaccharide isolated from Lactobacillus plantarum C88. Int. J. Biol. Macromol. 2013, 54, 270–275. [Google Scholar] [CrossRef]
- Gao, D.; Gao, Z.; Zhu, G. Antioxidant effects of Lactobacillus plantarum via activation of transcription factor Nrf2. Food Funct. 2013, 4, 982–989. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.; Xing, Z.; Li, C.; Wang, J.; Wang, Y. Molecular mechanisms and in vitro antioxidant effects of Lactobacillus plantarum MA2. Food Chem. 2017, 221, 1642–1649. [Google Scholar] [CrossRef] [PubMed]
- Izuddin, W.I.; Humam, A.M.; Loh, T.C.; Foo, H.L.; Samsudin, A.A. Dietary Postbiotic Lactobacillus plantarum Improves Serum and Ruminal Antioxidant Activity and Upregulates Hepatic Antioxidant Enzymes and Ruminal Barrier Function in Post-Weaning Lambs. Antioxidants 2020, 9, 250. [Google Scholar] [CrossRef] [PubMed]
- Ge, Q.; Yang, B.; Liu, R.; Jiang, D.; Yu, H.; Wu, M.; Zhang, W. Antioxidant activity of Lactobacillus plantarum NJAU-01 in an animal model of aging. BMC Microbiol. 2021, 21, 182. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.J.; Chen, J.L.; Liao, J.F.; Chen, Y.H.; Chieu, M.W.; Ke, Y.Y.; Hsu, C.C.; Tsai, Y.C.; Hsieh-Li, H.M. Lactobacillus plantarum PS128 prevents cognitive dysfunction in Alzheimer’s disease mice by modulating propionic acid levels, glycogen synthase kinase 3 beta activity, and gliosis. BMC Complement. Med Ther. 2021, 21, 259. [Google Scholar] [CrossRef]
- Lin, S.-W.; Tsai, Y.-S.; Chen, Y.-L.; Wang, M.-F.; Chen, C.-C.; Lin, W.-H.; Fang, T.J. Lactobacillus plantarum GKM3 Promotes Longevity, Memory Retention, and Reduces Brain Oxidation Stress in SAMP8 Mice. Nutrients 2021, 13, 2860. [Google Scholar] [CrossRef]
- Al, K.F.; Craven, L.J.; Gibbons, S.; Parvathy, S.N.; Wing, A.C.; Graf, C.; A Parham, K.; Kerfoot, S.M.; Wilcox, H.; Burton, J.P.; et al. Fecal microbiota transplantation is safe and tolerable in patients with multiple sclerosis: A pilot randomized controlled trial. Mult. Scler. J. Exp. Transl. Clin. 2022, 8, 20552173221086662. [Google Scholar] [CrossRef]
- Rosa, F.; Michelotti, T.C.; St-Pierre, B.; Trevisi, E.; Osorio, J.S. Early Life Fecal Microbiota Transplantation in Neonatal Dairy Calves Promotes Growth Performance and Alleviates Inflammation and Oxidative Stress during Weaning. Animals 2021, 11, 2704. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Ning, J.; Bao, X.-Q.; Shang, M.; Ma, J.; Li, G.; Zhang, D. Fecal microbiota transplantation protects rotenone-induced Parkinson’s disease mice via suppressing inflammation mediated by the lipopolysaccharide-TLR4 signaling pathway through the microbiota-gut-brain axis. Microbiome 2021, 9, 226. [Google Scholar] [CrossRef] [PubMed]
- Xiang, W.; Xiang, H.; Wang, J.; Jiang, Y.; Pan, C.; Ji, B.; Zhang, A. Fecal microbiota transplantation: A novel strategy for treating Alzheimer’s disease. Front. Microbiol. 2023, 14, 1281233. [Google Scholar] [CrossRef] [PubMed]
| Probiotics | Population | Methodology | Intervention | Results | References | ||
|---|---|---|---|---|---|---|---|
| Parkinson’s Disease | |||||||
| HUMAN MODEL | Lactobacillus acidophilus NCIMB 30175, Lactobacillus plantarum NCIMB 30173, Lactobacillus rhamnosus NCIMB 30174 and Enterococcus faecium NCIMB 30176 | Fecal samples from six donors (three healthy control subjects, three diagnosed with PD) | In vitro dynamic, multi-compartment gastrointestinal model | Fermentation with probiotic for 48 h | Increased levels of Firmicutes, Actinobacteria and Bacteroidetes in PD patients. Modulation of the intestinal microbiota that delays pathology progression | 10.1016/j.ijpx.2021.100087 | [92] |
| Lactobacillus plantarum PS128 | 25 patients | Open-label, single-arm, baseline-controlled trial | PS128 (2 capsules containing 30 billion colony-forming units per capsule) daily for 12 weeks | Improved motor scores and quality of life | 10.3389/fnut.2021.650053 | [93] | |
| MCI (Mild Cognitive Impairment) | |||||||
| Lactobacillus plantarum BioF-228, Lactococcus lactis BioF-224, Bifidobacterium lactis CP-9, Lactobacillus rhamnosus Bv-77, Lactobacillus johnsonii MH-68, Lactobacillus paracasei MP137, Lactobacillus salivarius AP-32, Lactobacillus acidophilus TYCA06, Lactococcus lactis LY-66, Bifidobacterium lactis HNO19, Lactobacillus rhamnosus HNO01, Lactobacillus paracasei GL-156, Bifidobacterium animalis BB-115, Lactobacillus casei CS-773, Lactobacillus reuteri TSR332, Lactobacillus fermentum TSF331, Bifidobacterium infantis BLI-02, and Lactobacillus plantarum CN2018 | 42 patients | Pilot randomized controlled trial (RCT) | 2 g (>2 × 1010 CFU/g) probiotics daily for 12 weeks | Cognitive function and sleep quality were improved | 10.1016/j.gerinurse.2023.03.006 | [94] | |
| Alzheimer’s Disease | |||||||
| ANIMAL MODEL | SLAB51: Streptococcus thermophilus DSM 32245, Bifidobacterium lactis DSM 32246, B. lactis DSM 32247, Lactobacillus acidophilus DSM 32241, Lactobacillus helveticus DSM 32242, Lactobacillus paracasei DSM 32243, Lactobacillus plantarum DSM 32244 and Lactobacillus brevis DSM 27961 | 48 AD male mice triple-transgenic, B6; 129-Psen1tm1Mpm Tg (amyloid precursor protein [APP] Swe, tauP301L) 1Lfa/J (named 3xTg-AD) and the wt B6129SF2 mice | Treatment with probiotic vs. Sham | SLAB51 (200 billion bacteria/kg/d) daily for 16 and 48 weeks | It improved impaired brain glucose metabolism implicated in AD pathogenesis, delaying disease progression | 10.1016/j.neurobiolaging.2019.11.004 | [95] |
| NK151: Lactobacillus plantarum; NK173: Bifidobacterium longum | 35 specific pathogen-free C57BL/6 mice | Treatment with probiotic vs. Sham | Escherichiacoli K1 (EC, 1 × 109 CFU per mouse per day) were orally gavage daily for 5 days | Reduced memory impairment and modulated gut microbial profile | 10.1039/d1fo02167b | [96] | |
| Lactobacillus plantarum MTCC1325 | 48 healthy adult male Wistar rats | The hippocampal (HP) and cerebral cortex (CC) brain regions of each animal were isolated | Lactobacillus plantarum MTCC1325 daily for 60 days | Neurodegeneration was reduced by the protective effect on the ATPase system in the brain | 10.15171/bi.2016.27 | [97] | |
| VSL#3 ®: Lactobacillus plantarum, Lactobacillus delbrueckii subsp. Bulgaricus, Lactobacillus paracasei, Lactobacillus acidophilus, Bifidobacterium breve, Bifidobacterium longum, Bifidobacterium infantis and Streptococcus salivarius subsp. Thermophilus | 140 mice: 70 male and female AppNL-G-F (AD) and 70 male and female C57BL/6J (wild type, WT) | Treatment with probiotic vs. Sham vs. ABX (antibiotic) vs. ABX+probiotic | VSL#3 ® (4 × 109 UFC/día/mice) for 8 weeks | All groups of female mice with intervention improved mnesic ability but none affected memory in male mice; reduced brain levels of TNF-α in female AppNL-G-F mice | 10.3390/cells10092370 | [98] | |
| Parkinson’s Disease | |||||||
| Lactobacillus plantarum PS128 | 90 six-week-old male C57BL/6J mice | Treatment with probiotic vs. Sham | PS128 (109 CFU in 200 μL saline) daily for 28 days | Motor deficits were improved and dopaminergic neuronal death was alleviated. Glial reactivity is reduced and striatal neurotrophic factors are increased | 10.1016/j.bbi.2020.07.036 | [99] | |
| Lactobacillus plantarum PS128 | 40 eight-week-old male C57BL/6J mice | Treatment with probiotic vs. Sham | PS128 (109 CFU/d) (week 1 to 6) and rotenone | Modified the microbial profile and maintained neuroprotective effects by increasing the expression of the suppressor of cytokine signaling | 10.3390/ijms24076794 | [100] | |
| Lactobacillus plantarum DP189 | 90 male C57BL/6 mice | Treatment with probiotic vs. Sham | DP189 (0.2 mL) daily for 14 days | Improved motor symptoms and increased levels of monoamines in the nervous system. In addition, it promoted neuronal survival | 10.1016/j.jff.2021.104635 | [101] | |
| Lactobacillus plantarum CRL 2130, Streptococcus thermophilus CRL 808, and Streptococcus thermophilus CRL 807 | 56 eight-week-old male C57BL/6 mice | Treatment with probiotic vs. Sham | L. plantarum CRL 2130, S. thermophilus CRL 808, S. thermophilus CRL 807 or the bacterial mixture (100 µL that contain 8 ± 2 × 108 CFU/mL of each strain, individually or as a mixture daily) for 4 days | Both alone or in combination, the strains produced significantly improved motor skills, with possible involvement of vitamin B interaction, and protective immune response to organ inflammation | 10.1016/j.nut.2020.110995 | [102] | |
| Lactobacillus plantarum CRL2130, Lactobacillus plantarum CRL725 | 35 neuro-2a (N2a) neuroblastoma cell line (ATCC CCL131) mice | In vitro: Half of each brain was removed for the determination of cytokines; The other half of the brain was stored in 10% paraformaldehyde/PBS during 24 h and then embedded in paraffin; In vivo: Treatment with probiotic vs. Sham | In vitro: N2a cells were incubated with intracellular extract from L. plantarum CRL2130. In vivo: Lactobacillus plantarum CRL2130, Lactobacillus plantarum CRL725 (100 μL) once | In vitro: cells-maintained viability and significantly decreased IL-6 release and reactive oxygen species (ROS) formation. In vivo: attenuated motor deficits and prevented dopaminergic neuronal death | 10.1007/s11064-021-03520-w | [103] | |
| Lactobacillus plantarum KJ01, Acetobacter pomorum KJ02, Lactobacillus brevis KJ03, and Acetobacter pasteurianus KJ04 | 30 to 40 adult Drosophila | Treatment with probiotic vs. EGCG | Lactobacillus plantarum o Acetobacter pomorum (5 g food/1 mL of bacterial suspension) for 20 days (OD600 = 1, approximately 5 × 107 viable cells/mL) | LP KJ01 exacerbated PD symptoms and eliminated EGCG (eigallocatechin-3-gallate)-mediated symptom enhancement. In addition, it aggravated neuronal loss and hindered EGCG-mediated enhancement. | 10.1096/fj.201903125RR | [104] | |
| PROBIO: Lactobacillus casei W56, Lactobacillus acidophilus W22, Lactobacillus paracasei W20, Lactobacillus salivarius W24, Lactobacillus lactis W19, Lactobacillus plantarum W62, Bifidobacterium lactis W51, Bifidobacterium lactis W52, and Bifidobacterium bifidum W23 | 120 adult (6–8 months) wild-type AB (WT, genetic line) zebrafish | Treatment with probiotic vs. Sham | PROBIO (3 g × 28 envelopes) were dissolved directly into 100 mL distilled water as a unique dose per day | ROT triggers apoptosis and increases PARKIN and PINK1 expression. LEV/CARB and PROBIO maintain neurogenesis and angiogenesis, exerting neuroprotective functions and decreasing the impact of ROT | 10.3390/antiox11102040 | [105] | |
| Multiple Sclerosis | |||||||
| Lactobacillus paracasei DSM 24734, Lactobacillus plantarum DSM 24730, Lactobacillus acidophilus DSM 24735, Lactobacillus delbruckeii subspecies bulgaricus DSM 24734, Bifidobacterium longum DSM 24736, Bifidobacterium infantis DSM 24737, Bifidobacterium breve 24732 and Streptococcus thermophilus DSM 24731 | Fecal samples freshly obtained from each mouse on day 70 and 85 | Treatment with probiotic vs. Sham | 2 times a week: 3 × 108 CFU (100 μL) of Vivomixx for 70 to 85 days | Motor function was improved. Increased anti-inflammatory activation in the microglia | 10.1080/19490976.2020.1813532 | [106] | |
| Oxidative Stress | |||||||
| Se-enriched Lactobacillus plantarum CCFM8610 | 270 Luciobarbus capito | Treatment with probiotic vs. Sham | Diet of 1–2% body weight twice a day for 30 days | Reversed Cd toxicity in the blood and brain, improving antioxidant capacity and reducing memory loss | 10.1016/j.ecoenv.2022.113890 | [107] | |
| Lactobacillus plantarum ST-III AB161 (CGMCC 22782) | 24 male ICR mice | Treatment with probiotic vs. Sham | Free access for 28 days | Significantly improved cognitive dysfunction (memory and learning). Modifications in hippocampal morphology and synaptic dysfunction were found, reducing the impact of oxidative stress | 10.3389/fnins.2022.976358 | [108] | |
| Lactobacillus plantarum NCIMB 8826 (Lp8826), Lactobacillus fermentum NCIMB 5221 (Lf5221) and Bifidobacteria longum spp. infantis NCIMB 702255 (Bi702255) | Wildtype Drosophila melanogaster (Oregon R) | Treatment with probiotic vs. synbiotic | Probiotic formulation: 3.0 × 109 CFU/mL of probiotics with equal distribution between Lp8826 (1.0 × 109 CFU/mL), Lf5221 (1.0 × 109 CFU/mL) and Bi702255 (1.0 × 109 CFU/mL). Synbiotic formulation: probiotic formulation + 0.5% of TFLA powder | The probiotic and synbiotic reduced metabolic stress levels and inflammation, improved oxidative stress and loss of mitochondrial integrity. Synbiotic formulation maintains results better than separate formulation | 10.1038/s41598-018-25382-z | [109] | |
| Cognitive decline and oxidative stress | |||||||
| Lactobacillus plantarum DR7 | 6 Male Sprague Dawley rats | Treatment with probiotic vs. Sham | DR7 (109 CFU/day) for 12 weeks | Memory capacity improved. Anxiety also improved in the DR7-treated group. In addition, protective effects on serotonergic pathways were demonstrated | 10.3920/BM2019.0200 | [110] | |
| Neurodegenerative process | |||||||
| Lactobacillus plantarum AR113 | 32 male C57BL/6J mice | Treatment with probiotic vs. Sham | AR113 (1 × 109 CFU/mL) daily | It significantly reduced oxidative stress injury induced by D-galactose, decreasing its cytotoxicity. In addition, cell membrane integrity was maintained and antioxidant enzyme activity was increased | 10.26599/fshw.2022.9250076 | [111] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beltrán-Velasco, A.I.; Reiriz, M.; Uceda, S.; Echeverry-Alzate, V. Lactiplantibacillus (Lactobacillus) plantarum as a Complementary Treatment to Improve Symptomatology in Neurodegenerative Disease: A Systematic Review of Open Access Literature. Int. J. Mol. Sci. 2024, 25, 3010. https://doi.org/10.3390/ijms25053010
Beltrán-Velasco AI, Reiriz M, Uceda S, Echeverry-Alzate V. Lactiplantibacillus (Lactobacillus) plantarum as a Complementary Treatment to Improve Symptomatology in Neurodegenerative Disease: A Systematic Review of Open Access Literature. International Journal of Molecular Sciences. 2024; 25(5):3010. https://doi.org/10.3390/ijms25053010
Chicago/Turabian StyleBeltrán-Velasco, Ana Isabel, Manuel Reiriz, Sara Uceda, and Víctor Echeverry-Alzate. 2024. "Lactiplantibacillus (Lactobacillus) plantarum as a Complementary Treatment to Improve Symptomatology in Neurodegenerative Disease: A Systematic Review of Open Access Literature" International Journal of Molecular Sciences 25, no. 5: 3010. https://doi.org/10.3390/ijms25053010
APA StyleBeltrán-Velasco, A. I., Reiriz, M., Uceda, S., & Echeverry-Alzate, V. (2024). Lactiplantibacillus (Lactobacillus) plantarum as a Complementary Treatment to Improve Symptomatology in Neurodegenerative Disease: A Systematic Review of Open Access Literature. International Journal of Molecular Sciences, 25(5), 3010. https://doi.org/10.3390/ijms25053010











