Propolis Protects GC-1spg Spermatogonial Cells against Tert-Butyl Hydroperoxide-Induced Oxidative Damage
Abstract
1. Introduction
2. Results
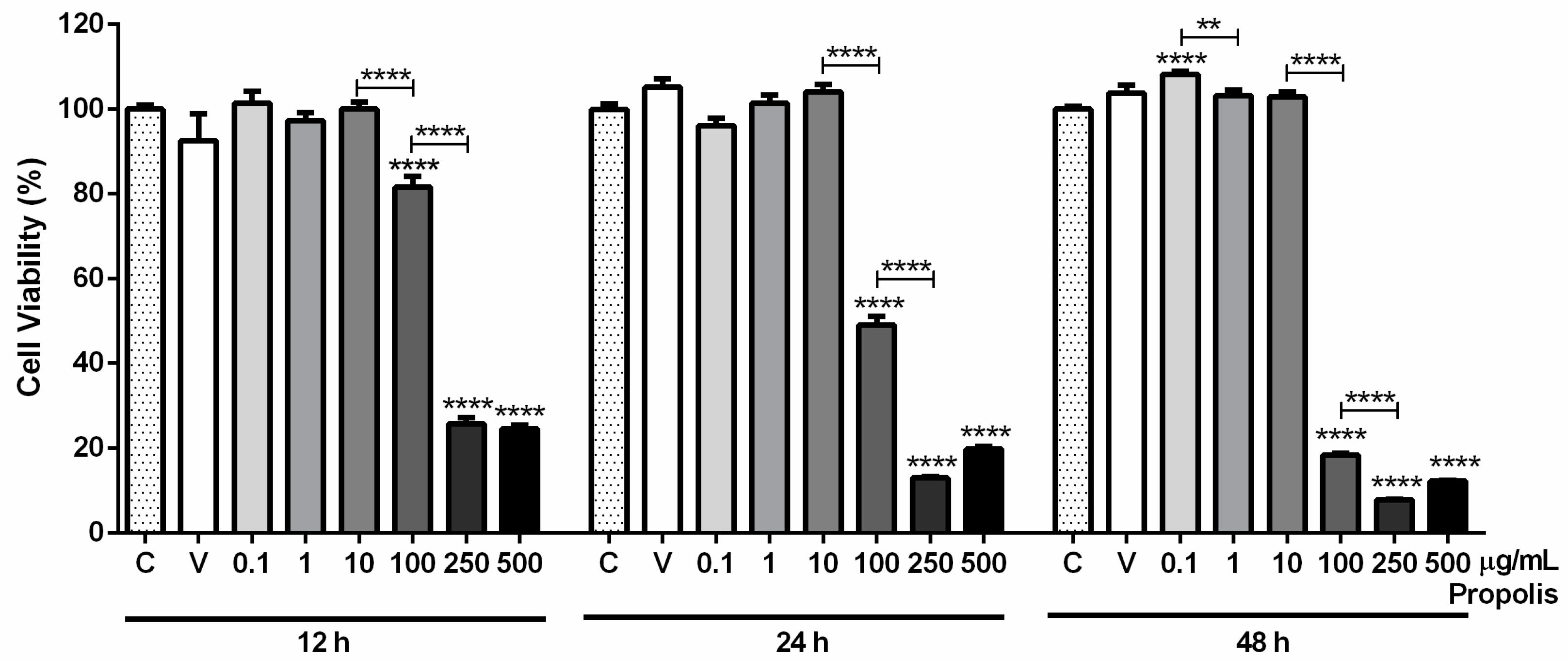
2.1. Propolis’ Characterization: Phytochemical Composition, Antioxidant Properties and Cytotoxicity
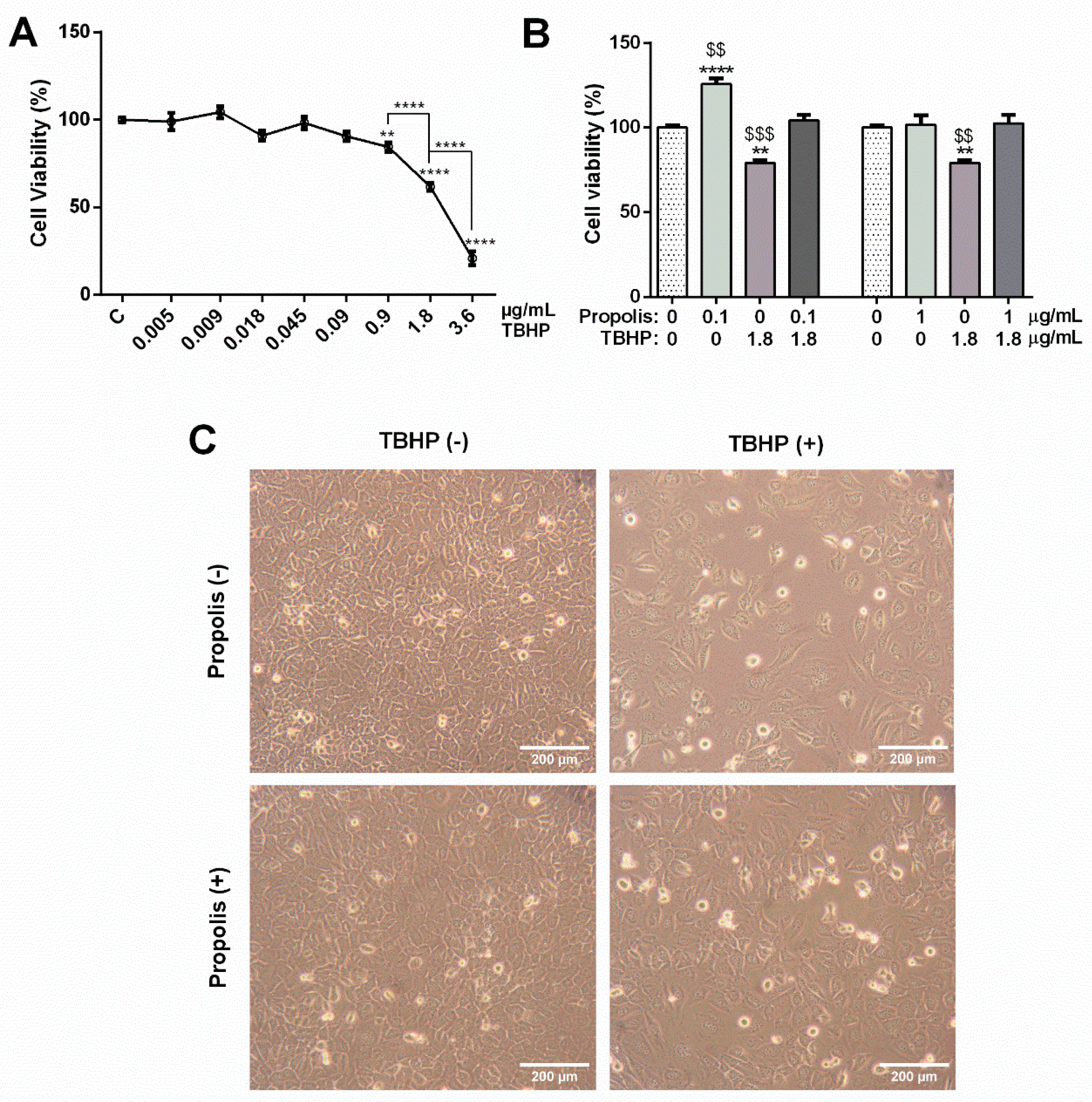
2.2. Propolis Attenuated the Impact of the OS Inducer Tert-Butyl Hydroperoxide (TBHP) in the Viability of GC-1spg Cells
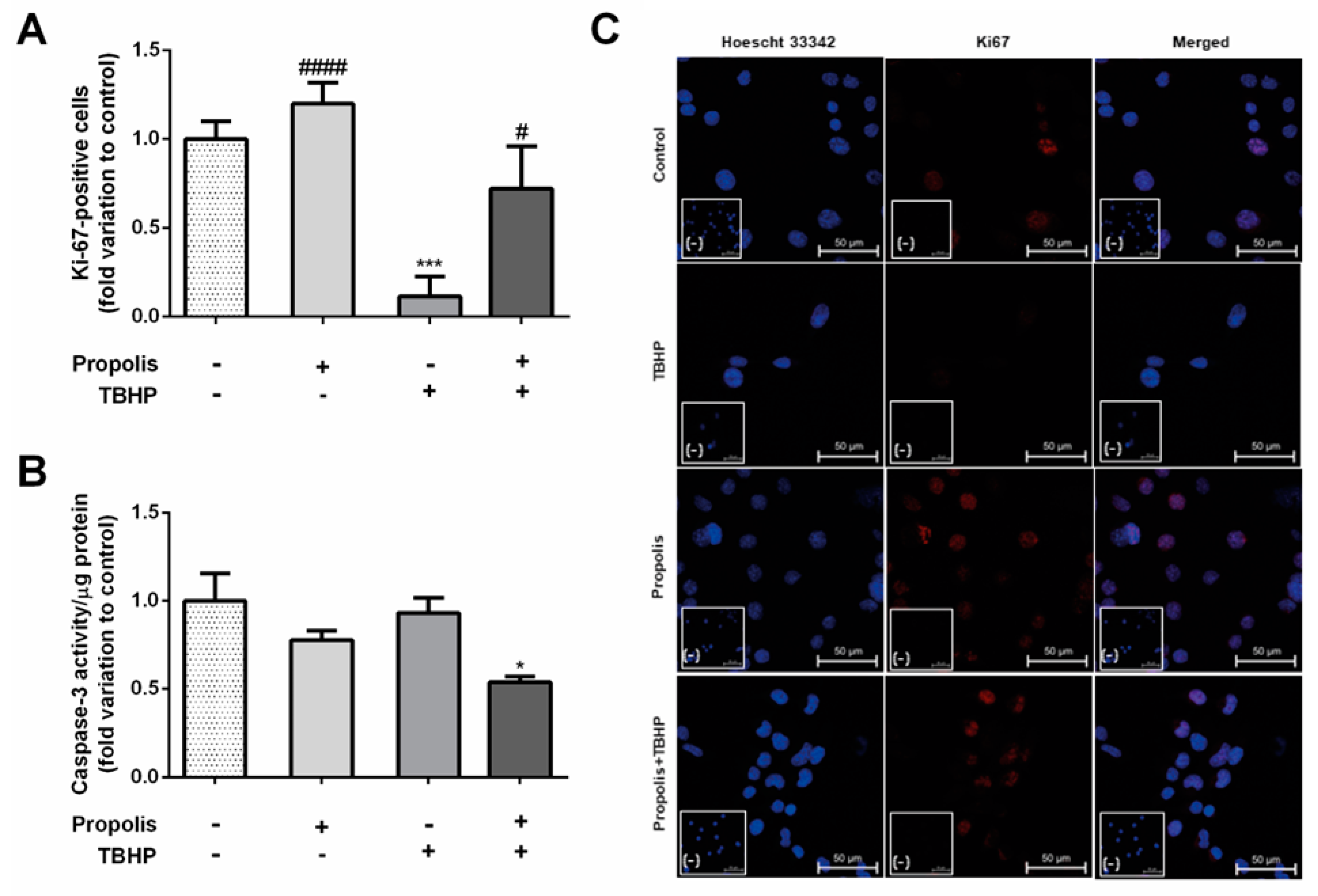
2.3. Propolis Prevented the Antiproliferative Effect of TBHP in GC-1spg Cells, Reducing Caspase-3 Activity Only in the Presence of TBHP Stimuli
2.4. Propolis Reduced Reactive Oxygen Species (ROS) Levels in GC-1spg Cells, Raising Glutathione Peroxidase (GPx) Activity in Cells Exposed to TBHP
3. Discussion
4. Materials and Methods
4.1. Propolis and TBHP
4.2. Total Phenolic Compounds Determination
4.3. Flavonoid Content Assessment
4.4. 2,2-Diphenyl-1-picrylhydrazyl (DPPH) Free Radical Scavenging Assay
4.5. Cell Culture
4.6. Propolis and TBHP Treatments
4.7. 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium Bromide (MTT) Assay
4.8. Ki-67 Fluorescent Immunohistochemistry
4.9. Dihydroethidium (DHE) Assay
4.10. Total Protein Extraction and Quantification
4.11. Evaluation of Antioxidant Enzyme Activity
4.12. Caspase-3-like Activity Assay
4.13. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zabaiou, N.; Fouache, A.; Trousson, A.; Baron, S.; Zellagui, A.; Lahouel, M.; Lobaccaro, J.A. Biological properties of propolis extracts: Something new from an ancient product. Chem. Phys. Lipids 2017, 207, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Hallajzadeh, J.; Milajerdi, A.; Amirani, E.; Attari, V.E.; Maghsoudi, H.; Mirhashemi, S.M. Effects of propolis supplementation on glycemic status, lipid profiles, inflammation and oxidative stress, liver enzymes, and body weight: A systematic review and meta-analysis of randomized controlled clinical trials. J. Diabetes Metab. Disord. 2021, 20, 831–843. [Google Scholar] [CrossRef] [PubMed]
- Anjum, S.I.; Ullah, A.; Khan, K.A.; Attaullah, M.; Khan, H.; Ali, H.; Bashir, M.A.; Tahir, M.; Ansari, M.J.; Ghramh, H.A.; et al. Composition and functional properties of propolis (bee glue): A review. Saudi J. Biol. Sci. 2019, 26, 1695–1703. [Google Scholar] [CrossRef] [PubMed]
- Bankova, V.; Dyulgerov, A.; Popov, S.; Evstatieva, L.; Kuleva, L.; Pureb, O.; Zamjansan, Z. Propolis produced in Bulgaria and Mongolia: Phenolic compounds and plant origin. Apidologie 1992, 23, 79–85. [Google Scholar] [CrossRef]
- Zheng, Y.-Z.; Deng, G.; Liang, Q.; Chen, D.-F.; Guo, R.; Lai, R.-C. Antioxidant activity of quercetin and its glucosides from propolis: A theoretical study. Sci. Rep. 2017, 7, 7543. [Google Scholar] [CrossRef] [PubMed]
- Martinotti, S.; Ranzato, E. Propolis: A new frontier for wound healing? Burns Trauma 2015, 3, 9. [Google Scholar] [CrossRef] [PubMed]
- Kuropatnicki, A.K.; Szliszka, E.; Krol, W. Historical aspects of propolis research in modern times. Evid.-Based Complement. Altern. Med. 2013, 2013, 964149. [Google Scholar] [CrossRef]
- Šuran, J.; Cepanec, I.; Mašek, T.; Radić, B.; Radić, S.; Tlak Gajger, I.; Vlainić, J. Propolis extract and its bioactive compounds—From traditional to modern extraction technologies. Molecules 2021, 26, 2930. [Google Scholar] [CrossRef]
- Braakhuis, A.A.-O. Evidence on the Health Benefits of Supplemental Propolis. Nutrients 2019, 11, 2705. [Google Scholar] [CrossRef]
- Ramos, A.F.N.; Miranda, J.L.D. Propolis: A review of its anti-inflammatory and healing actions. J. Venom. Anim. Toxins Incl. Trop. Dis. 2007, 13, 697–710. [Google Scholar] [CrossRef]
- Chandna, P.; Adlakha, V.K.; Das, S.; Singh, S. Complementary and Alternative Medicine (CAM): A review of propolis in dentistry. Technology 2014, 4, 675–685. [Google Scholar]
- Wagh, V.D. Propolis: A wonder bees product and its pharmacological potentials. Adv. Pharmacol. Sci. 2013, 2013, 308249. [Google Scholar] [CrossRef] [PubMed]
- Forma, E.; Brys, M. Anticancer Activity of Propolis and Its Compounds. Nutrients 2021, 13, 2594. [Google Scholar] [CrossRef] [PubMed]
- Jasprica, I.; Mornar, A.; Debeljak, Ž.; Smolčić-Bubalo, A.; Medić-Šarić, M.; Mayer, L.; Romić, Ž.; Bućan, K.; Balog, T.; Sobočanec, S. In vivo study of propolis supplementation effects on antioxidative status and red blood cells. J. Ethnopharmacol. 2007, 110, 548–554. [Google Scholar] [CrossRef] [PubMed]
- Osés, S.M.; Pascual-Maté, A.; Fernández-Muiño, M.A.; López-Díaz, T.M.; Sancho, M.T. Bioactive properties of honey with propolis. Food Chem. 2016, 196, 1215–1223. [Google Scholar] [CrossRef] [PubMed]
- Bazmandegan, G.; Boroushaki, M.T.; Shamsizadeh, A.; Ayoobi, F.; Hakimizadeh, E.; Allahtavakoli, M. Brown propolis attenuates cerebral ischemia-induced oxidative damage via affecting antioxidant enzyme system in mice. Biomed. Pharmacother. 2017, 85, 503–510. [Google Scholar] [CrossRef]
- Cao, X.-P.; Chen, Y.-F.; Zhang, J.-L.; You, M.-M.; Wang, K.; Hu, F.-L. Mechanisms underlying the wound healing potential of propolis based on its in vitro antioxidant activity. Phytomedicine 2017, 34, 76–84. [Google Scholar] [CrossRef]
- Bhargava, P.; Mahanta, D.; Kaul, A.; Ishida, Y.; Terao, K.; Wadhwa, R.; Kaul, S.C. Experimental Evidence for Therapeutic Potentials of Propolis. Nutrients 2021, 13, 2528. [Google Scholar] [CrossRef]
- Yousef, M.I.; Kamel, K.I.; Hassan, M.S.; El-Morsy, A.M.A. Protective role of propolis against reproductive toxicity of triphenyltin in male rabbits. Food Chem. Toxicol. 2010, 48, 1846–1852. [Google Scholar] [CrossRef]
- Aitken, R.J.; Smith, T.B.; Jobling, M.S.; Baker, M.A.; De Iuliis, G.N. Oxidative stress and male reproductive health. Asian J. Androl. 2014, 16, 31–38. [Google Scholar] [CrossRef]
- Martins, R.V.L.; Silva, A.M.S.; Duarte, A.P.; Socorro, S.; Correia, S.; Maia, C.J. Natural Products as Protective Agents for Male Fertility. BioChem 2021, 1, 122–147. [Google Scholar] [CrossRef]
- Capucho, C.; Sette, R.; de Souza Predes, F.; de Castro Monteiro, J.; Pigoso, A.A.; Barbieri, R.; Dolder, M.A.H.; Severi-Aguiar, G.D.C. Green Brazilian propolis effects on sperm count and epididymis morphology and oxidative stress. Food Chem. Toxicol. 2012, 50, 3956–3962. [Google Scholar] [CrossRef] [PubMed]
- Gholaminejad, F.; Javadi, M.; Karami, A.A.; Alizadeh, F.; Kavianpour, M.; Khadem Haghighian, H. Propolis Supplementation Effects on Semen Parameters, Oxidative Stress, Inflammatory Biomarkers and Reproductive Hormones in Infertile Men with Asthenozoospermia; A Randomized Clinical Trial. Int. J. Med. Lab. 2019, 6, 21–32. [Google Scholar] [CrossRef]
- Seven, I.A.-O.; Tatli Seven, P.A.-O.; Gul Baykalir, B.A.-O.; Parlak Ak, T.A.-O.; Ozer Kaya, S.A.-O.; Yaman, M.A.-O. Bee glue (propolis) improves reproductive organs, sperm quality and histological changes and antioxidant parameters of testis tissues in rats exposed to excess copper. Andrologia 2020, 52, e13540. [Google Scholar] [CrossRef] [PubMed]
- Çilenk, K.T.; Öztürk, İ.; Sönmez, M.F. Ameliorative effect of propolis on the cadmium-induced reproductive toxicity in male albino rats. Exp. Mol. Pathol. 2016, 101, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Nagy, W.; Ghoneim, H.; El-Aziz, A.; Alsenosy, A.E. Dietary Propolis Supplement Improves Semen Characteristics in Egyptian Buffaloes. Damanhour J. Vet. Sci. 2020, 4, 11–15. [Google Scholar] [CrossRef]
- Sheir, M.A.; Serrapica, F.; Ahmed, R.A.J.F. An Innovative Use of Propolis in the Production of Dipping Sauce Powder as a Functional Food to Mitigate Testicular Toxicity Induced by Cadmium Chloride: Technological and Biological Evidence. Foods 2023, 12, 3069. [Google Scholar] [CrossRef]
- Abd-Elrazek, A.M.; El-dash, H.A.; Said, N.I. The role of propolis against paclitaxel-induced oligospermia, sperm abnormality, oxidative stress and DNA damage in testes of male rats. Andrologia 2020, 52, e13394. [Google Scholar] [CrossRef]
- Özkök, A.A.-O.; Keskin, M.; Tanuğur Samancı, A.E.; Yorulmaz Önder, E.; Takma, Ç. Determination of antioxidant activity and phenolic compounds for basic standardization of Turkish propolis. Appl. Biol. Chem. 2021, 64, 37. [Google Scholar] [CrossRef]
- Falcão, S.I.; Vale, N.; Gomes, P.; Domingues, M.R.M.; Freire, C.; Cardoso, S.M.; Vilas-Boas, M. Phenolic profiling of Portuguese propolis by LC–MS spectrometry: Uncommon propolis rich in flavonoid glycosides. Phytochem. Anal. 2013, 24, 309–318. [Google Scholar] [CrossRef]
- Falcão, S.I.; Freire, C.; Vilas-Boas, M. A proposal for physicochemical standards and antioxidant activity of Portuguese propolis. J. Am. Oil Chem. Soc. 2013, 90, 1729–1741. [Google Scholar] [CrossRef]
- Kasiotis, K.M.; Anastasiadou, P.; Papadopoulos, A.; Machera, K. Revisiting Greek Propolis: Chromatographic Analysis and Antioxidant Activity Study. PLoS ONE 2017, 12, e0170077. [Google Scholar] [CrossRef] [PubMed]
- Miliauskas, G.; Venskutonis, P.R.; Van Beek, T.A. Screening of radical scavenging activity of some medicinal and aromatic plant extracts. Food Chem. 2004, 85, 231–237. [Google Scholar] [CrossRef]
- Viuda-Martos, M.; Ruiz-Navajas, Y.; Fernández-López, J.; Pérez-Álvarez, J.A. Functional properties of honey, propolis, and royal jelly. J. Food Sci. 2008, 73, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Tvrdá, E.; Árvay, J.; Ďuračka, M.; Kačániová, M. Mitochondria-Stimulating and Antioxidant Effects of Slovak Propolis Varieties on Bovine Spermatozoa. Oxygen 2023, 3, 179–189. [Google Scholar] [CrossRef]
- Mendez-Pfeiffer, P.; Alday, E.; Carreño, A.L.; Hernández-Tánori, J.; Montaño-Leyva, B.; Ortega-García, J.; Valdez, J.; Garibay-Escobar, A.; Hernandez, J.; Valencia, D. Seasonality modulates the cellular antioxidant activity and antiproliferative effect of sonoran desert propolis. Antioxidants 2020, 9, 1294. [Google Scholar] [CrossRef] [PubMed]
- Kocot, J.; Kielczykowska, M.; Luchowska-Kocot, D.; Kurzepa, J.; Musik, I. Antioxidant Potential of Propolis, Bee Pollen, and Royal Jelly: Possible Medical Application. Oxid. Med. Cell Longev. 2018, 2018, 7074209. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Gachhui, R.; Sil, P.C. Hepatoprotective properties of kombucha tea against TBHP-induced oxidative stress via suppression of mitochondria dependent apoptosis. Pathophysiology 2011, 18, 221–234. [Google Scholar] [CrossRef]
- Sarkar, M.K.; Sil, P.C. Prevention of tertiary butyl hydroperoxide induced oxidative impairment and cell death by a novel antioxidant protein molecule isolated from the herb, Phyllanthus niruri. Toxicol In Vitro 2010, 24, 1711–1719. [Google Scholar] [CrossRef]
- Wang, X.; Ye, X.-l.; Liu, R.; Chen, H.-L.; Bai, H.; Liang, X.; Zhang, X.-D.; Wang, Z.; Li, W.-l.; Hai, C.-X. Antioxidant activities of oleanolic acid in vitro: Possible role of Nrf2 and MAP kinases. Chem. Biol. Interact. 2010, 184, 328–337. [Google Scholar] [CrossRef]
- Kent, K.D.; Harper, W.J.; Bomser, J.A. Effect of whey protein isolate on intracellular glutathione and oxidant-induced cell death in human prostate epithelial cells. Toxicol In Vitro 2003, 17, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Najafi, M.F.; Vahedy, F.; Seyyedin, M.; Jomehzadeh, H.R.; Bozary, K. Effect of the water extracts of propolis on stimulation and inhibition of different cells. Cytotechnology 2007, 54, 49–56. [Google Scholar] [CrossRef] [PubMed]
- de Francisco, L.; Pinto, D.; Rosseto, H.; Toledo, L.; Santos, R.; Tobaldini-Valério, F.; Svidzinski, T.; Bruschi, M.; Sarmento, B.; Oliveira, M.B.P.P. Evaluation of radical scavenging activity, intestinal cell viability and antifungal activity of Brazilian propolis by-product. Food Res. Int. 2018, 105, 537–547. [Google Scholar] [CrossRef] [PubMed]
- Aherne, S.A.; Kerry, J.P.; O’Brien, N.M. Effects of plant extracts on antioxidant status and oxidant-induced stress in Caco-2 cells. Br. J. Nutri. 2007, 97, 321–328. [Google Scholar] [CrossRef] [PubMed]
- ElMazoudy, R.H.; Attia, A.A.; El-Shenawy, N.S. Protective role of propolis against reproductive toxicity of chlorpyrifos in male rats. Pestic. Biochem. Phys. 2011, 101, 175–181. [Google Scholar] [CrossRef]
- Almeida, C.; Cunha, M.; Ferraz, L.; Silva, J.; Barros, A.; Sousa, M. Caspase-3 detection in human testicular spermatozoa from azoospermic and non-azoospermic patients. Int. J. Androl. 2011, 34, e407–e414. [Google Scholar] [CrossRef]
- Said, T.M.; Paasch, U.; Glander, H.J.; Agarwal, A. Role of caspases in male infertility. Hum. Reprod. Update 2004, 10, 39–51. [Google Scholar] [CrossRef]
- Asadi, M.; Taghizadeh, S.; Kaviani, E.; Vakili, O.; Taheri-Anganeh, M.; Tahamtan, M.; Savardashtaki, A. Caspase-3: Structure, function, and biotechnological aspects. Biotechnol. Appl. Biochem. 2022, 69, 1633–1645. [Google Scholar] [CrossRef]
- Kumari, S.; Nayak, G.; Lukose, S.T.; Kalthur, S.G.; Bhat, N.; Hegde, A.R.; Mutalik, S.; Kalthur, G.; Adiga, S.K. Indian propolis ameliorates the mitomycin C-induced testicular toxicity by reducing DNA damage and elevating the antioxidant activity. Biomed. Pharmacother. 2017, 95, 252–263. [Google Scholar] [CrossRef]
- Rizk, S.M.; Zaki, H.F.; Mina, M.A.M. Propolis attenuates doxorubicin-induced testicular toxicity in rats. Food Chem. Toxicol. 2014, 67, 176–186. [Google Scholar] [CrossRef]
- Khayyal, M.T.; Abdel-Naby, D.H.; El-Ghazaly, M.A. Propolis extract protects against radiation-induced intestinal mucositis through anti-apoptotic mechanisms. Environ. Sci. Pollut. Res. 2019, 26, 24672–24682. [Google Scholar] [CrossRef] [PubMed]
- de Rooij, D.G. Proliferation and differentiation of spermatogonial stem cells. Reproduction 2001, 121, 347–354. [Google Scholar] [CrossRef]
- Lushchak, V.I. Free radicals, reactive oxygen species, oxidative stress and its classification. Chem.-Biol. Interact. 2014, 224, 164–175. [Google Scholar] [CrossRef] [PubMed]
- Fatemi, N.; Sanati, M.H.; Jamali Zavarehei, M.; Ayat, H.; Esmaeili, V.; Golkar-Narenji, A.; Zarabi, M.; Gourabi, H. Effect of tertiary-butyl hydroperoxide (TBHP)-induced oxidative stress on mice sperm quality and testis histopathology. Andrologia 2013, 45, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Correia, S.; Vaz, C.V.; Silva, A.M.; Cavaco, J.E.; Socorro, S. Regucalcin counteracts tert-butyl hydroperoxide and cadmium-induced oxidative stress in rat testis. J. Appl. Toxicol. 2017, 37, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Kumar, T.R.; Muralidhara. Induction of oxidative stress by organic hydroperoxides in testis and epididymal sperm of rats in vivo. J. Androl. 2013, 28, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Fatemi, N.; Sanati, M.H.; Shamsara, M.; Moayer, F.; Zavarehei, M.J.; Pouya, A.; Sayyahpour, F.; Ayat, H.; Gourabi, H. TBHP-induced oxidative stress alters microRNAs expression in mouse testis. J. Assist. Reprod. Genet. 2014, 31, 1287–1293. [Google Scholar] [CrossRef]
- Kurek-Górecka, A.; Rzepecka-Stojko, A.; Górecki, M.; Stojko, J.; Sosada, M.; Świerczek-Zięba, G. Structure and antioxidant activity of polyphenols derived from propolis. Molecules 2013, 19, 78–101. [Google Scholar] [CrossRef]
- Nattagh-Eshtivani, E.; Pahlavani, N.; Ranjbar, G.; Gholizadeh Navashenaq, J.; Salehi-Sahlabadi, A.; Mahmudiono, T.; Nader Shalaby, M.; Jokar, M.; Nematy, M.; Barghchi, H. Does propolis have any effect on rheumatoid arthritis? A review study. Food Sci. Nut 2022, 10, 1003–1020. [Google Scholar] [CrossRef]
- Mujica, V.; Orrego, R.; Pérez, J.; Romero, P.; Ovalle, P.; Zúñiga-Hernández, J.; Arredondo, M.; Leiva, E. The role of propolis in oxidative stress and lipid metabolism: A randomized controlled trial. Evid.-Based Complement. Altern. Med. 2017, 2017, 4272940. [Google Scholar] [CrossRef]
- Russo, A.; Troncoso, N.; Sanchez, F.; Garbarino, J.A.; Vanella, A. Propolis protects human spermatozoa from DNA damage caused by benzo [a] pyrene and exogenous reactive oxygen species. Life Sci. 2006, 78, 1401–1406. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.B.; Yoo, B.S. Propolis inhibits UVA-induced apoptosis of human keratinocyte HaCaT cells by scavenging ROS. Toxicol. Res. 2016, 32, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.Z.; Liu, Y.C.; Zheng, Y.F.; Chen, Y.F.; Si, J.J.; Chen, M.L.; Shou, Q.Y.; Zheng, H.Q.; Hu, F.L. Ethanol extract of chinese propolis attenuates early diabetic retinopathy by protecting the blood–retinal barrier in streptozotocin-induced diabetic rats. J. Food Sci. 2019, 84, 358–369. [Google Scholar] [CrossRef] [PubMed]
- Lubos, E.; Loscalzo, J.; Handy, D.E. Glutathione peroxidase-1 in health and disease: From molecular mechanisms to therapeutic opportunities. Antioxid. Redox Signal. 2011, 15, 1957–1997. [Google Scholar] [CrossRef]
- Agarwal, A.; Makker, K.; Sharma, R. Clinical relevance of oxidative stress in male factor infertility: An update. Am. J. Reprod. Immunol. 2008, 59, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Yasui, K.; Baba, A. Therapeutic potential of superoxide dismutase (SOD) for resolution of inflammation. Inflamm. Res. 2006, 55, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.; Sil, P.C. Tertiary butyl hydroperoxide induced oxidative damage in mice erythrocytes: Protection by taurine. Pathophysiology 2012, 19, 137–148. [Google Scholar] [CrossRef]
- Attia, A.A.; ElMazoudy, R.H.; El-Shenawy, N.S. Antioxidant role of propolis extract against oxidative damage of testicular tissue induced by insecticide chlorpyrifos in rats. Pestic. Biochem. Phys. 2012, 103, 87–93. [Google Scholar] [CrossRef]
- Sobocanec, S.; Šverko, V.; Balog, T.; Šarić, A.; Rusak, G.; Likić, S.; Kušić, B.; Katalinić, V.; Radić, S.; Marotti, T. Oxidant/antioxidant properties of Croatian native propolis. J. Agric. Food Chem. 2006, 54, 8018–8026. [Google Scholar] [CrossRef]
- Sakai, Y.; Aminaka, M.; Takata, A.; Kudou, Y.; Yamauchi, H.; Aizawa, Y.; Sakagami, H. Oxidative stress in mature rat testis and its developmental changes. Dev. Growth Differ. 2010, 52, 657–663. [Google Scholar] [CrossRef]
- Luis, A.; Neiva, D.; Pereira, H.; Gominho, J.; Domingues, F.; Duarte, A.P. Stumps of Eucalyptus globulus as a source of antioxidant and antimicrobial polyphenols. Molecules 2014, 19, 16428–16446. [Google Scholar] [CrossRef] [PubMed]
- Glutathione Peroxidase Assay Kit. Available online: https://www.caymanchem.com/product/703102/glutathione-peroxidase-assay-kit (accessed on 7 January 2023).
- Superoxide Dismutase, SOD, Activity Assay Kit. Available online: https://www.sigmaaldrich.com/PT/en/product/sigma/cs0009 (accessed on 7 January 2023).


| Total phenolics (mg GAE/g Propolis) | Flavonoids (mg QE/g Propolis) | IC50 (µg/mL) | Antioxidant Activity Index | Antioxidant Activity Classification |
|---|---|---|---|---|
| 168.70 ± 0.08 | 36.90 ± 0.19 | 63.32 ± 13.04 | 0.77 ± 0.13 | Moderate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duarte, F.; Feijó, M.; Luís, Â.; Socorro, S.; Maia, C.J.; Correia, S. Propolis Protects GC-1spg Spermatogonial Cells against Tert-Butyl Hydroperoxide-Induced Oxidative Damage. Int. J. Mol. Sci. 2024, 25, 614. https://doi.org/10.3390/ijms25010614
Duarte F, Feijó M, Luís Â, Socorro S, Maia CJ, Correia S. Propolis Protects GC-1spg Spermatogonial Cells against Tert-Butyl Hydroperoxide-Induced Oxidative Damage. International Journal of Molecular Sciences. 2024; 25(1):614. https://doi.org/10.3390/ijms25010614
Chicago/Turabian StyleDuarte, Filipa, Mariana Feijó, Ângelo Luís, Sílvia Socorro, Cláudio J. Maia, and Sara Correia. 2024. "Propolis Protects GC-1spg Spermatogonial Cells against Tert-Butyl Hydroperoxide-Induced Oxidative Damage" International Journal of Molecular Sciences 25, no. 1: 614. https://doi.org/10.3390/ijms25010614
APA StyleDuarte, F., Feijó, M., Luís, Â., Socorro, S., Maia, C. J., & Correia, S. (2024). Propolis Protects GC-1spg Spermatogonial Cells against Tert-Butyl Hydroperoxide-Induced Oxidative Damage. International Journal of Molecular Sciences, 25(1), 614. https://doi.org/10.3390/ijms25010614










