Chemokines in Cartilage Regeneration and Degradation: New Insights
Abstract
1. Introduction
2. Method
3. Results and Discussion
3.1. Monocyte Chemotactic Proteins (MCPs)
3.1.1. MCP-1
3.1.2. MCP-2 and MCP-3
3.2. Regulated on Activation, Normal T-Cell Expressed, and Secreted (RANTES)
3.3. Macrophage Inflammatory Proteins (MIPs)
3.3.1. MIP-1α and MIP-1β
3.3.2. MIP-3
3.4. CCL21
3.5. CCL22
3.6. ELR+ CXC Chemokines
3.7. CXCL12
3.8. CX3CL1
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hu, J.C.; Athanasiou, K.A. Low-Density Cultures of Bovine Chondrocytes: Effects of Scaffold Material and Culture System. Biomaterials 2005, 26, 2001–2012. [Google Scholar] [CrossRef] [PubMed]
- Secor, E.J.; Grzanna, M.W.; Rashmir-Raven, A.M.; Frondoza, C.G. Chondrocyte Production of Pro-Inflammatory Chemokine MCP-1 (CCL-2) and Prostaglandin E-2 Is Inhibited by Avocado/Soybean Unsaponifiables, Glucosamine, Chondroitin Sulfate Combination. Pharmacol. Pharm. 2018, 9, 10–26. [Google Scholar] [CrossRef]
- Zlotnik, A.; Yoshie, O. Chemokines: A New Classification System and Their Role in Immunity. Immunity 2000, 12, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Lloyd, C.; Zhou, H.; Dolich, S.; Deeds, J.; Gonzalo, J.A.; Vath, J.; Gosselin, M.; Ma, J.; Dussault, B.; et al. Neurotactin, a Membrane-Anchored Chemokine Upregulated in Brain Inflammation. Nature 1997, 387, 611–617. [Google Scholar] [CrossRef] [PubMed]
- Raghu, H.; Lepus, C.M.; Wang, Q.; Wong, H.H.; Lingampalli, N.; Oliviero, F.; Punzi, L.; Giori, N.J.; Goodman, S.B.; Chu, C.R.; et al. CCL2/CCR2, but Not CCL5/CCR5, Mediates Monocyte Recruitment, Inflammation and Cartilage Destruction in Osteoarthritis. Ann. Rheum. Dis. 2017, 76, 914–922. [Google Scholar] [CrossRef] [PubMed]
- Córdova, L.A.; Loi, F.; Lin, T.H.; Gibon, E.; Pajarinen, J.; Nabeshima, A.; Lu, L.; Yao, Z.; Goodman, S.B. CCL2, CCL5, and IGF-1 Participate in the Immunomodulation of Osteogenesis during M1/M2 Transition in Vitro. J. Biomed. Mater. Res. A 2017, 105, 3069–3076. [Google Scholar] [CrossRef] [PubMed]
- Deshmane, S.L.; Kremlev, S.; Amini, S.; Sawaya, B.E. Monocyte Chemoattractant Protein-1 (MCP-1): An Overview. J. Interferon Cytokine Res. 2009, 29, 313–325. [Google Scholar] [CrossRef]
- Ni, F.; Zhang, Y.; Peng, X.; Li, J. Correlation between Osteoarthritis and Monocyte Chemotactic Protein-1 Expression: A Meta-Analysis. J. Orthop. Surg. Res. 2020, 15, 516. [Google Scholar] [CrossRef]
- Cuéllar, V.G.; Cuéllar, J.M.; Kirsch, T.; Strauss, E.J. Correlation of Synovial Fluid Biomarkers with Cartilage Pathology and Associated Outcomes in Knee Arthroscopy. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 475–485. [Google Scholar] [CrossRef]
- Ren, G.; Lutz, I.; Railton, P.; Wiley, J.P.; McAllister, J.; Powell, J.; Krawetz, R.J. Serum and Synovial Fluid Cytokine Profiling in Hip Osteoarthritis: Distinct from Knee Osteoarthritis and Correlated with Pain. BMC Musculoskelet. Disord. 2018, 19, 39. [Google Scholar] [CrossRef]
- Poo, Y.S.; Nakaya, H.; Gardner, J.; Larcher, T.; Schroder, W.A.; Le, T.T.; Major, L.D.; Suhrbier, A. CCR2 Deficiency Promotes Exacerbated Chronic Erosive Neutrophil-Dominated Chikungunya Virus Arthritis. J. Virol. 2014, 88, 6862–6872. [Google Scholar] [CrossRef] [PubMed]
- Ajuebor, M.N.; Das, A.M.; Virág, L.; Flower, R.J.; Szabó, C.; Perretti, M. Role of Resident Peritoneal Macrophages and Mast Cells in Chemokine Production and Neutrophil Migration in Acute Inflammation: Evidence for an Inhibitory Loop Involving Endogenous IL-10. J. Immunol. 1999, 162, 1685–1691. [Google Scholar] [CrossRef] [PubMed]
- Girbl, T.; Lenn, T.; Perez, L.; Rolas, L.; Barkaway, A.; Thiriot, A.; del Fresno, C.; Lynam, E.; Hub, E.; Thelen, M.; et al. Distinct Compartmentalization of the Chemokines CXCL1 and CXCL2 and the Atypical Receptor ACKR1 Determine Discrete Stages of Neutrophil Diapedesis. Immunity 2018, 49, 1062–1076.e6. [Google Scholar] [CrossRef] [PubMed]
- Eyles, J.L.; Hickey, M.J.; Norman, M.U.; Croker, B.A.; Roberts, A.W.; Drake, S.F.; James, W.G.; Metcalf, D.; Campbell, I.K.; Wicks, I.P. A Key Role for G-CSF-Induced Neutrophil Production and Trafficking during Inflammatory Arthritis. Blood 2008, 112, 5193–5201. [Google Scholar] [CrossRef]
- Michael, B.D.; Bricio-Moreno, L.; Sorensen, E.W.; Miyabe, Y.; Lian, J.; Solomon, T.; Kurt-Jones, E.A.; Luster, A.D. Astrocyte- and Neuron-Derived CXCL1 Drives Neutrophil Transmigration and Blood-Brain Barrier Permeability in Viral Encephalitis. Cell Rep. 2020, 32, 108150. [Google Scholar] [CrossRef]
- White, G.E.; Iqbal, A.J.; Greaves, D.R. CC Chemokine Receptors and Chronic Inflammation—Therapeutic Opportunities and Pharmacological Challenges. Pharmacol. Rev. 2013, 65, 47–89. [Google Scholar] [CrossRef]
- Sambamurthy, N.; Nguyen, V.; Smalley, R.; Xiao, R.; Hankenson, K.; Gan, J.; Miller, R.E.; Malfait, A.M.; Dodge, G.R.; Scanzello, C.R. Chemokine Receptor-7 (CCR7) Deficiency Leads to Delayed Development of Joint Damage and Functional Deficits in a Murine Model of Osteoarthritis. J. Orthop. Res. 2018, 36, 864–875. [Google Scholar] [CrossRef]
- Joutoku, Z.; Onodera, T.; Matsuoka, M.; Homan, K.; Momma, D.; Baba, R.; Hontani, K.; Hamasaki, M.; Matsubara, S.; Hishimura, R.; et al. CCL21/CCR7 Axis Regulating Juvenile Cartilage Repair Can Enhance Cartilage Healing in Adults. Sci. Rep. 2019, 9, 5165. [Google Scholar] [CrossRef]
- Xu, Y.K.; Ke, Y.; Wang, B.; Lin, J.H. The Role of MCP-1-CCR2 Ligand-receptor Axis in Chondrocyte Degradation and Disease Progress in Knee Osteoarthritis. Biol. Res. 2015, 48, 64. [Google Scholar] [CrossRef]
- Quincey, A.; Mohan, S.; Edderkaoui, B. Monocyte Chemotactic Proteins Mediate the Effects of Hyperglycemia in Chondrocytes: In Vitro Studies. Life 2022, 12, 836. [Google Scholar] [CrossRef]
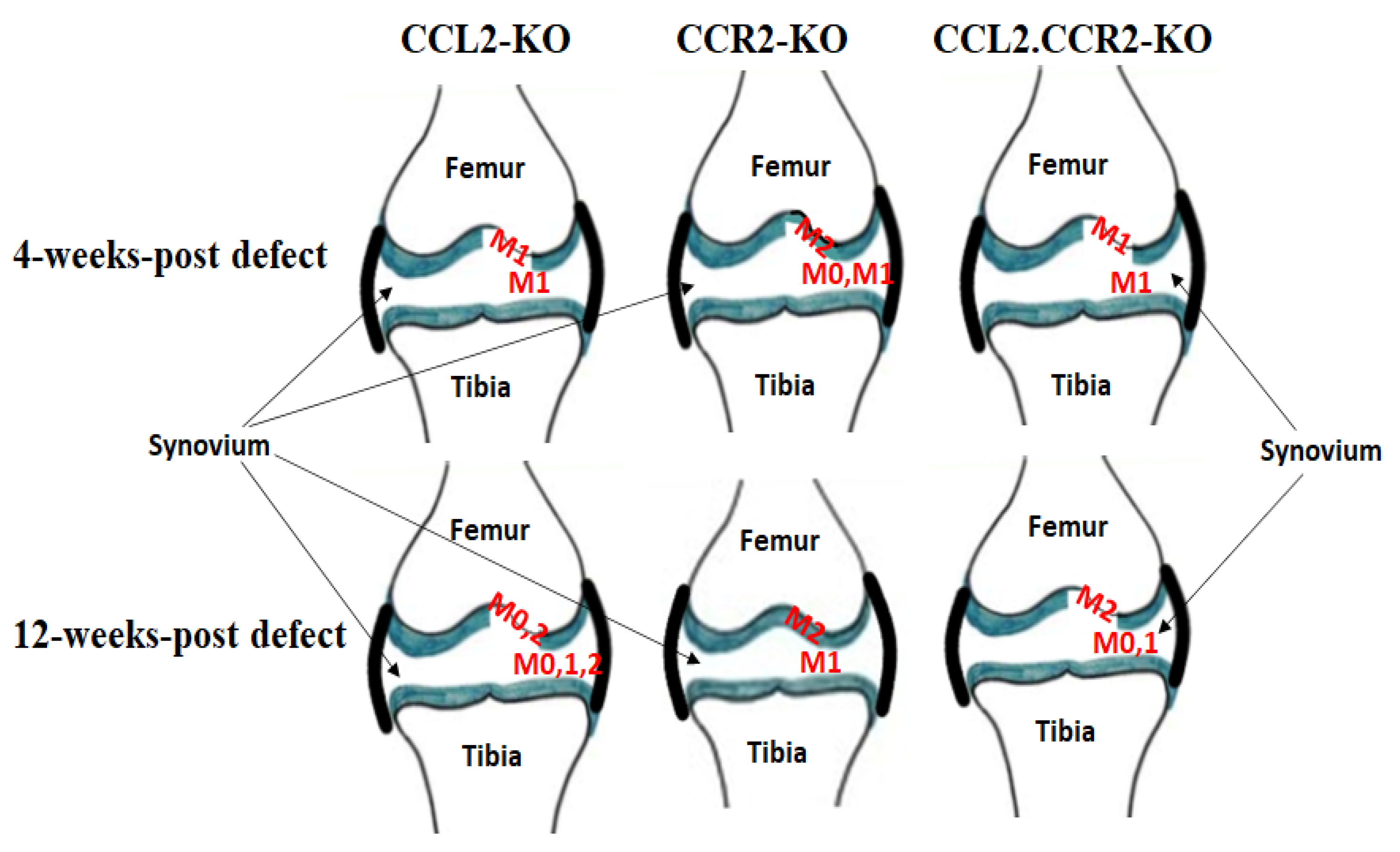
- Jablonski, C.L.; Leonard, C.; Salo, P.; Krawetz, R.J. CCL2 but Not CCR2 Is Required for Spontaneous Articular Cartilage Regeneration Post-Injury. J. Orthop. Res. 2019, 37, 2561–2574. [Google Scholar] [CrossRef] [PubMed]
- Fahy, N.; de Vries-van Melle, M.L.; Lehmann, J.; Wei, W.; Grotenhuis, N.; Farrell, E.; van der Kraan, P.M.; Murphy, J.M.; Bastiaansen-Jenniskens, Y.M.; van Osch, G.J.V.M. Human Osteoarthritic Synovium Impacts Chondrogenic Differentiation of Mesenchymal Stem Cells via Macrophage Polarisation State. Osteoarthr. Cartil. 2014, 22, 1167–1175. [Google Scholar] [CrossRef] [PubMed]
- Phillips, K.L.E.; Cullen, K.; Chiverton, N.; Michael, A.L.R.; Cole, A.A.; Breakwell, L.M.; Haddock, G.; Bunning, R.A.D.; Cross, A.K.; Le Maitre, C.L. Potential Roles of Cytokines and Chemokines in Human Intervertebral Disc Degeneration: Interleukin-1 Is a Master Regulator of Catabolic Processes. Osteoarthr. Cartil. 2015, 23, 1165–1177. [Google Scholar] [CrossRef]
- Marçais, A.; Coupet, C.-A.; Walzer, T.; Tomkowiak, M.; Ghittoni, R.; Marvel, J. Cell-Autonomous CCL5 Transcription by Memory CD8 T Cells Is Regulated by IL-4. J. Immunol. 2006, 177, 4451–4457. [Google Scholar] [CrossRef] [PubMed]
- Scott, K.M.; Cohen, D.J.; Hays, M.; Nielson, D.W.; Grinstaff, M.W.; Lawson, T.B.; Snyder, B.D.; Boyan, B.D.; Schwartz, Z. Regulation of Inflammatory and Catabolic Responses to IL-1β in Rat Articular Chondrocytes by MicroRNAs MiR-122 and MiR-451. Osteoarthr. Cartil. 2021, 29, 113–123. [Google Scholar] [CrossRef]
- Assirelli, E.; Pulsatelli, L.; Dolzani, P.; Platano, D.; Olivotto, E.; Filardo, G.; Trisolino, G.; Facchini, A.; Borzì, R.M.; Meliconi, R. Human Osteoarthritic Cartilage Shows Reduced In Vivo Expression of IL-4, a Chondroprotective Cytokine That Differentially Modulates IL-1β-Stimulated Production of Chemokines and Matrix-Degrading Enzymes In Vitro. PLoS ONE 2014, 9, e96925. [Google Scholar] [CrossRef]
- Bondeson, J.; Lauder, S.; Wainwright, S.; Amos, N.; Evans, A.; Hughes, C.; Feldmann, M.; Caterson, B. Adenoviral Gene Transfer of the Endogenous Inhibitor IkappaB Alpha into Human Osteoarthritis Synovial Fibroblasts Demonstrates That Several Matrix Metalloproteinases and Aggrecanases Are Nuclear Factor-KappaB-Dependent. J. Rheumatol. 2007, 34, 523–533. [Google Scholar]
- Du, J.; Long, R.G.; Nakai, T.; Sakai, D.; Benneker, L.M.; Zhou, G.; Li, B.; Eglin, D.; Iatridis, J.C.; Alini, M.; et al. Functional Cell Phenotype Induction with TGF-B1 and Collagen-Polyurethane Scaffold for Annulus Fibrosus Rupture Repair. Eur. Cell Mater. 2020, 39, 1–17. [Google Scholar] [CrossRef]
- Lu, L.; Zhang, X.; Zhang, M.; Zhang, H.; Liao, L.; Yang, T.; Zhang, J.; Xian, L.; Chen, D.; Wang, M. RANTES and SDF-1 Are Keys in Cell-Based Therapy of TMJ Osteoarthritis. J. Dent. Res. 2015, 94, 1601–1609. [Google Scholar] [CrossRef]
- Zhang, Z.; Xing, X.; Hensley, G.; Chang, L.W.; Liao, W.; Abu-Amer, Y.; Sandell, L.J. Resistin Induces Expression of Proinflammatory Cytokines and Chemokines in Human Articular Chondrocytes via Transcription and Messenger RNA Stabilization. Arthritis Rheum. 2010, 62, 1993–2003. [Google Scholar] [CrossRef]
- Yang, D.W.; Qian, G.B.; Jiang, M.J.; Wang, P.; Wang, K.Z. Inhibition of MicroRNA-495 Suppresses Chondrocyte Apoptosis through Activation of the NF-ΚB Signaling Pathway by Regulating CCL4 in Osteoarthritis. Gene Ther. 2019, 26, 217–229. [Google Scholar] [CrossRef] [PubMed]
- Alaaeddine, N.; Antoniou, J.; Moussa, M.; Hilal, G.; Kreichaty, G.; Ghanem, I.; Abouchedid, W.; Saghbini, E.; Di Battista, J.A. The Chemokine CCL20 Induces Proinflammatory and Matrix Degradative Responses in Cartilage. Inflamm. Res. 2015, 64, 721–731. [Google Scholar] [CrossRef]
- Subburaman, M.; Edderkaoui, B. Evaluation of CCL21 Role in Post-Knee Injury Inflammation and Early Cartilage Degeneration. PLoS ONE 2021, 16, e0247913. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Lin, S.; Huang, H. Involvement of Increased Expression of Chemokine C–C Motif Chemokine 22 (CCL22)/CC Chemokine Receptor 4 (CCR4) in the Inflammatory Injury and Cartilage Degradation of Chondrocytes. Cytotechnology 2021, 73, 715–726. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Wang, P.; Xie, Z.; Wang, S.; Ma, M.; Li, J.; Li, M.; Cen, S.; Tang, S.; Zheng, G.; et al. Abnormal Inhibition of Osteoclastogenesis by Mesenchymal Stem Cells through the MiR-4284/CXCL5 Axis in Ankylosing Spondylitis. Cell Death Dis. 2019, 10, 188. [Google Scholar] [CrossRef] [PubMed]
- Kawata, K.; Koga, H.; Tsuji, K.; Miyatake, K.; Nakagawa, Y.; Yokota, T.; Sekiya, I.; Katagiri, H. Extracellular Vesicles Derived from Mesenchymal Stromal Cells Mediate Endogenous Cell Growth and Migration via the CXCL5 and CXCL6/CXCR2 Axes and Repair Menisci. Stem Cell Res. Ther. 2021, 12, 414. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Shi, J.; Zhang, J.; Lv, Z.; Guo, F.; Huang, H.; Zhu, W.; Chen, A. CXCL12/CXCR4 Axis Regulates Aggrecanase Activation and Cartilage Degradation in a Post-Traumatic Osteoarthritis Rat Model. Int. J. Mol. Sci. 2016, 17, 1522. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, J.; Fan, W.; Zhang, J.; Hua, B.; Sun, B.; Zhu, L.; Niu, X.; Yan, Z.; Guo, C. Stromal Cell-Derived Factor-1α and Transforming Growth Factor-β 1 Synergistically Facilitate Migration and Chondrogenesis of Synovium-Derived Stem Cells through MAPK Pathways. Am. J. Transl. Res. 2017, 9, 2656. [Google Scholar]
- Hoshino-Negishi, K.; Ohkuro, M.; Nakatani, T.; Kuboi, Y.; Nishimura, M.; Ida, Y.; Kakuta, J.; Hamaguchi, A.; Kumai, M.; Kamisako, T.; et al. Role of Anti-Fractalkine Antibody in Suppression of Joint Destruction by Inhibiting Migration of Osteoclast Precursors to the Synovium in Experimental Arthritis. Arthritis Rheumatol. 2019, 71, 222–231. [Google Scholar] [CrossRef]
- Mora, E.; Guglielmotti, A.; Biondi, G.; Sassone-Corsi, P. Bindarit: An Anti-Inflammatory Small Molecule That Modulates the NFκB Pathway. Cell Cycle 2012, 11, 159–169. [Google Scholar] [CrossRef]
- Borzì, R.M.; Mazzetti, I.; Macor, S.; Silvestri, T.; Bassi, A.; Cattini, L.; Facchini, A. Flow Cytometric Analysis of Intracellular Chemokines in Chondrocytes In Vivo: Constitutive Expression and Enhancement in Osteoarthritis and Rheumatoid Arthritis. FEBS Lett. 1999, 455, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Abu-Amer, Y. IL-4 Abrogates Osteoclastogenesis through STAT6-Dependent Inhibition of NF-KappaB. J. Clin. Investig. 2001, 107, 1375–1385. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, T.A.; Ohmori, Y.; Tebo, J. Regulation of Chemokine Expression by Antiinflammatory Cytokines. Immunol. Res. 2002, 25, 229–245. [Google Scholar] [CrossRef]
- Ohmori, Y.; Hamilton, T.A. IL-4-Induced STAT6 Suppresses IFN-Gamma-Stimulated STAT1-Dependent Transcription in Mouse Macrophages. J. Immunol. 1997, 159, 5474–5482. [Google Scholar] [CrossRef] [PubMed]
- Ohmori, Y.; Hamilton, T.A. Interleukin-4/STAT6 Represses STAT1 and NF-Kappa B-Dependent Transcription through Distinct Mechanisms. J. Biol. Chem. 2000, 275, 38095–38103. [Google Scholar] [CrossRef] [PubMed]
- Wangler, S.; Menzel, U.; Li, Z.; Ma, J.; Hoppe, S.; Benneker, L.M.; Alini, M.; Grad, S.; Peroglio, M. CD146/MCAM Distinguishes Stem Cell Subpopulations with Distinct Migration and Regenerative Potential in Degenerative Intervertebral Discs. Osteoarthr. Cartil. 2019, 27, 1094–1105. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Zeiter, S.; Schmid, T.; Sakai, D.; Iatridis, J.C.; Zhou, G.; Richards, R.G.; Alini, M.; Grad, S.; Li, Z. Effect of the CCL5-Releasing Fibrin Gel for Intervertebral Disc Regeneration. Cartilage 2020, 11, 169–180. [Google Scholar] [CrossRef]
- Frapin, L.; Clouet, J.; Chédeville, C.; Moraru, C.; Samarut, E.; Henry, N.; André, M.; Bord, E.; Halgand, B.; Lesoeur, J.; et al. Controlled Release of Biological Factors for Endogenous Progenitor Cell Migration and Intervertebral Disc Extracellular Matrix Remodelling. Biomaterials 2020, 253, 120107. [Google Scholar] [CrossRef]
- Zhao, X.Y.; Yang, Z.B.; Zhang, Z.J.; Zhang, Z.Q.; Kang, Y.; Huang, G.X.; Wang, S.W.; Huang, H.; Liao, W.M. CCL3 Serves as a Potential Plasma Biomarker in Knee Degeneration (Osteoarthritis). Osteoarthr. Cartil. 2015, 23, 1405–1411. [Google Scholar] [CrossRef]
- Lee, J.H.; Ort, T.; Ma, K.; Picha, K.; Carton, J.; Marsters, P.A.; Lohmander, L.S.; Baribaud, F.; Song, X.Y.R.; Blake, S. Resistin Is Elevated Following Traumatic Joint Injury and Causes Matrix Degradation and Release of Inflammatory Cytokines from Articular Cartilage In Vitro. Osteoarthr. Cartil. 2009, 17, 613–620. [Google Scholar] [CrossRef]
- Staikos, C.; Ververidis, A.; Drosos, G.; Manolopoulos, V.G.; Verettas, D.A.; Tavridou, A. The Association of Adipokine Levels in Plasma and Synovial Fluid with the Severity of Knee Osteoarthritis. Rheumatology 2013, 52, 1077–1083. [Google Scholar] [CrossRef] [PubMed]
- Šenolt, L.; Housa, D.; Vernerová, Z.; Jirásek, T.; Svobodová, R.; Veigl, D.; Anderlová, K.; Müller-Ladner, U.; Pavelka, K.; Haluzík, M. Resistin in Rheumatoid Arthritis Synovial Tissue, Synovial Fluid and Serum. Ann. Rheum. Dis. 2007, 66, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Presle, N.; Pottie, P.; Dumond, H.; Guillaume, C.; Lapicque, F.; Pallu, S.; Mainard, D.; Netter, P.; Terlain, B. Differential Distribution of Adipokines between Serum and Synovial Fluid in Patients with Osteoarthritis. Contribution of Joint Tissues to Their Articular Production. Osteoarthr. Cartil. 2006, 14, 690–695. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, Z.; Kang, Y.; Hou, C.; Duan, X.; Sheng, P.; Sandell, L.J.; Liao, W. Resistin Stimulates Expression of Chemokine Genes in Chondrocytes via Combinatorial Regulation of c/EBPβ and NF-ΚB. Int. J. Mol. Sci. 2014, 15, 17242–17255. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.; Gan, J.; Bush-Joseph, C.; Verma, N.; Tetreault, M.W.; Saha, K.; Margulis, A.; Fogg, L.; Scanzello, C.R. Synovial Chemokine Expression and Relationship with Knee Symptoms in Patients with Meniscal Tears. Osteoarthr. Cartil. 2015, 23, 1158–1164. [Google Scholar] [CrossRef][Green Version]
- Yamashita, M.; Iwama, N.; Date, F.; Shibata, N.; Miki, H.; Yamauchi, K.; Sawai, T.; Sato, S.; Takahashi, T.; Ono, M. Macrophages Participate in Lymphangiogenesis in Idiopathic Diffuse Alveolar Damage through CCL19-CCR7 Signal. Hum. Pathol. 2009, 40, 1553–1563. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, E.; Oberbarnscheidt, M.; Bulfone-Paus, S.; Förster, R.; Kunzendorf, U.; Krautwald, S. CCR7 Signaling Inhibits T Cell Proliferation. J. Immunol. 2007, 179, 6485–6493. [Google Scholar] [CrossRef]
- Luther, S.A.; Tang, H.L.; Hyman, P.L.; Farr, A.G.; Cyster, J.G. Coexpression of the Chemokines ELC and SLC by T Zone Stromal Cells and Deletion of the ELC Gene in the plt/plt Mouse. Proc. Natl. Acad. Sci. USA 2000, 97, 12694–12699. [Google Scholar] [CrossRef]
- Beckmann, J.H.; Yan, S.; Lührs, H.; Heid, B.; Skubich, S.; Förster, R.; Hoffmann, M.W. Prolongation of Allograft Survival in CCR7-Deficient Mice. Transplantation 2004, 77, 1809–1814. [Google Scholar] [CrossRef]
- Loeser, R.F.; Olex, A.L.; McNulty, M.A.; Carlson, C.S.; Callahan, M.F.; Ferguson, C.M.; Chou, J.; Leng, X.; Fetrow, J.S. Microarray Analysis Reveals Age-Related Differences in Gene Expression during the Development of Osteoarthritis in Mice. Arthritis Rheum. 2012, 64, 705–717. [Google Scholar] [CrossRef]
- Loeser, R.F.; Olex, A.L.; McNulty, M.A.; Carlson, C.S.; Callahan, M.; Ferguson, C.; Fetrow, J.S. Disease Progression and Phasic Changes in Gene Expression in a Mouse Model of Osteoarthritis. PLoS ONE 2013, 8, e54633. [Google Scholar] [CrossRef] [PubMed]
- Olex, A.L.; Turkett, W.H.; Fetrow, J.S.; Loeser, R.F. Integration of Gene Expression Data with Network-Based Analysis to Identify Signaling and Metabolic Pathways Regulated during the Development of Osteoarthritis. Gene 2014, 542, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Godiska, R.; Chantry, D.; Raport, C.J.; Sozzani, S.; Allavena, P.; Leviten, D.; Mantovani, A.; Gray, P.W. Human Macrophage-Derived Chemokine (MDC), a Novel Chemoattractant for Monocytes, Monocyte-Derived Dendritic Cells, and Natural Killer Cells. J. Exp. Med. 1997, 185, 1595–1604. [Google Scholar] [CrossRef] [PubMed]
- Imai, T.; Chantry, D.; Raport, C.J.; Wood, C.L.; Nishimura, M.; Godiska, R.; Yoshie, O.; Gray, P.W. Macrophage-Derived Chemokine Is a Functional Ligand for the CC Chemokine Receptor 4. J. Biol. Chem. 1998, 273, 1764–1768. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.J.; Haraldsen, G.; Pan, J.; Rottman, J.; Qin, S.; Ponath, P.; Andrew, D.P.; Warnke, R.; Ruffing, N.; Kassam, N.; et al. The Chemokine Receptor CCR4 in Vascular Recognition by Cutaneous but Not Intestinal Memory T Cells. Nature 1999, 400, 776–780. [Google Scholar] [CrossRef] [PubMed]
- Ren, G.; Whittaker, J.L.; Leonard, C.; De Rantere, D.; Pang, D.S.J.; Salo, P.; Fritzler, M.; Kapoor, M.; de Koning, A.P.J.; Jaremko, J.L.; et al. CCL22 Is a Biomarker of Cartilage Injury and Plays a Functional Role in Chondrocyte Apoptosis. Cytokine 2019, 115, 32–44. [Google Scholar] [CrossRef] [PubMed]
- Strieter, R.M.; Polverini, P.J.; Kunkel, S.L.; Arenberg, D.A.; Burdick, M.D.; Kasper, J.; Dzuiba, J.; Van Damme, J.; Walz, A.; Marriott, D.; et al. The Functional Role of the ELR Motif in CXC Chemokine-Mediated Angiogenesis. J. Biol. Chem. 1995, 270, 27348–27357. [Google Scholar] [CrossRef]
- Sherwood, J.; Bertrand, J.; Nalesso, G.; Poulet, B.; Pitsillides, A.; Brandolini, L.; Karystinou, A.; De Bari, C.; Luyten, F.P.; Pitzalis, C.; et al. A Homeostatic Function of CXCR2 Signalling in Articular Cartilage. Ann. Rheum. Dis. 2015, 74, 2207–2215. [Google Scholar] [CrossRef]
- Caxaria, S.; Kouvatsos, N.; Eldridge, S.E.; Alvarez-Fallas, M.; Thorup, A.; Cici, D.; Barawi, A.; Arshed, A.; Strachan, D.; Carletti, G.; et al. Disease Modification and Symptom Relief in Osteoarthritis Using a Mutated GCP-2/CXCL6 Chemokine. EMBO Mol. Med. 2023, 15, e16218. [Google Scholar] [CrossRef]
- Eldridge, S.; Nalesso, G.; Ismail, H.; Vicente-Greco, K.; Kabouridis, P.; Ramachandran, M.; Niemeier, A.; Herz, J.; Pitzalis, C.; Perretti, M.; et al. Agrin Mediates Chondrocyte Homeostasis and Requires Both LRP4 and α-Dystroglycan to Enhance Cartilage Formation in Vitro and In Vivo. Ann. Rheum. Dis. 2016, 75, 1228–1235. [Google Scholar] [CrossRef]
- Rot, A. Endothelial Cell Binding of NAP-1/IL-8: Role in Neutrophil Emigration. Immunol. Today 1992, 13, 291–294. [Google Scholar] [CrossRef] [PubMed]
- Middleton, J.; Neil, S.; Wintle, J.; Clark-Lewis, I.; Moore, H.; Lam, C.; Auer, M.; Hub, E.; Rot, A. Transcytosis and Surface Presentation of IL-8 by Venular Endothelial Cells. Cell 1997, 91, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Luster, A.D. Chemokines—Chemotactic Cytokines That Mediate Inflammation. N. Engl. J. Med. 1998, 338, 436–445. [Google Scholar] [CrossRef] [PubMed]
- Bizzarri, C.; Beccari, A.R.; Bertini, R.; Cavicchia, M.R.; Giorgini, S.; Allegretti, M. ELR+ CXC Chemokines and Their Receptors (CXC Chemokine Receptor 1 and CXC Chemokine Receptor 2) as New Therapeutic Targets. Pharmacol. Ther. 2006, 112, 139–149. [Google Scholar] [CrossRef] [PubMed]
- Proudfoot, A.E.I.; Johnson, Z.; Bonvin, P.; Handel, T.M. Glycosaminoglycan Interactions with Chemokines Add Complexity to a Complex System. Pharmaceuticals 2017, 10, 70. [Google Scholar] [CrossRef] [PubMed]
- Handel, T.M.; Dyer, D.P. Perspectives on the Biological Role of Chemokine:Glycosaminoglycan Interactions. J. Histochem. Cytochem. 2021, 69, 87–91. [Google Scholar] [CrossRef]
- Vicente, R.; Noël, D.; Pers, Y.M.; Apparailly, F.; Jorgensen, C. Deregulation and Therapeutic Potential of MicroRNAs in Arthritic Diseases. Nat. Rev. Rheumatol. 2016, 12, 211–220. [Google Scholar] [CrossRef]
- Lakshmipathy, U.; Hart, R.P. Concise Review: MicroRNA Expression in Multipotent Mesenchymal Stromal Cells. Stem Cells 2008, 26, 356–363. [Google Scholar] [CrossRef]
- Clark, E.A.; Kalomoiris, S.; Nolta, J.A.; Fierro, F.A. Concise Review: MicroRNA Function in Multipotent Mesenchymal Stromal Cells. Stem Cells 2014, 32, 1074–1082. [Google Scholar] [CrossRef]
- Chen, Q.; Shou, P.; Zheng, C.; Jiang, M.; Cao, G.; Yang, Q.; Cao, J.; Xie, N.; Velletri, T.; Zhang, X.; et al. Fate Decision of Mesenchymal Stem Cells: Adipocytes or Osteoblasts? Cell Death Differ. 2016, 23, 1128–1139. [Google Scholar] [CrossRef]
- Yu, L.; Cecil, J.; Peng, S.B.; Schrementi, J.; Kovacevic, S.; Paul, D.; Su, E.W.; Wang, J. Identification and Expression of Novel Isoforms of Human Stromal Cell-Derived Factor 1. Gene 2006, 374, 174–179. [Google Scholar] [CrossRef]
- Righetti, A.; Giulietti, M.; Šabanović, B.; Occhipinti, G.; Principato, G.; Piva, F. CXCL12 and Its Isoforms: Different Roles in Pancreatic Cancer? J. Oncol. 2019, 2019, 9681698. [Google Scholar] [CrossRef] [PubMed]
- Janssens, R.; Struyf, S.; Proost, P. Pathological Roles of the Homeostatic Chemokine CXCL12. Cytokine Growth Factor Rev. 2018, 44, 51–68. [Google Scholar] [CrossRef] [PubMed]
- Murphy, P.M.; Heusinkveld, L. Multisystem Multitasking by CXCL12 and Its Receptors CXCR4 and ACKR3. Cytokine 2018, 109, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Loetscher, M.; Geiser, T.; O’Reilly, T.; Zwahlen, R.; Baggiolini, M.; Moser, B. Cloning of a Human Seven-Transmembrane Domain Receptor, LESTR, That Is Highly Expressed in Leukocytes. J. Biol. Chem. 1994, 269, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Naumann, U.; Cameroni, E.; Pruenster, M.; Mahabaleshwar, H.; Raz, E.; Zerwes, H.G.; Rot, A.; Thelen, M. CXCR7 Functions as a Scavenger for CXCL12 and CXCL11. PLoS ONE 2010, 5, e9175. [Google Scholar] [CrossRef] [PubMed]
- Askari, A.T.; Unzek, S.; Popovic, Z.B.; Goldman, C.K.; Forudi, F.; Kiedrowski, M.; Rovner, A.; Ellis, S.G.; Thomas, J.D.; DiCorleto, P.E.; et al. Effect of Stromal-Cell-Derived Factor 1 on Stem-Cell Homing and Tissue Regeneration in Ischaemic Cardiomyopathy. Lancet 2003, 362, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Ceradini, D.J.; Kulkarni, A.R.; Callaghan, M.J.; Tepper, O.M.; Bastidas, N.; Kleinman, M.E.; Capla, J.M.; Galiano, R.D.; Levine, J.P.; Gurtner, G.C. Progenitor Cell Trafficking Is Regulated by Hypoxic Gradients through HIF-1 Induction of SDF-1. Nat. Med. 2004, 10, 858–864. [Google Scholar] [CrossRef]
- Teicher, B.A.; Fricker, S.P. CXCL12 (SDF-1)/CXCR4 Pathway in Cancer. Clin. Cancer Res. 2010, 16, 2927–2931. [Google Scholar] [CrossRef]
- Abdelouahab, H.; Zhang, Y.; Wittner, M.; Oishi, S.; Fujii, N.; Besancenot, R.; Plo, I.; Ribrag, V.; Solary, E.; Vainchenker, W.; et al. CXCL12/CXCR4 Pathway Is Activated by Oncogenic JAK2 in a PI3K-Dependent Manner. Oncotarget 2017, 8, 54082. [Google Scholar] [CrossRef]
- Fang, Z.; Meng, Q.; Xu, J.; Wang, W.; Zhang, B.; Liu, J.; Liang, C.; Hua, J.; Zhao, Y.; Yu, X.; et al. Signaling Pathways in Cancer-Associated Fibroblasts: Recent Advances and Future Perspectives. Cancer Commun. 2023, 43, 3–41. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Liang, G.; Huang, Z.; Doty, S.B.; Boskey, A.L. Conditional Inactivation of the CXCR4 Receptor in Osteoprecursors Reduces Postnatal Bone Formation Due to Impaired Osteoblast Development. J. Biol. Chem. 2011, 286, 26794–26805. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, Y.; Ii, M.; Matsumoto, T.; Kuroda, R.; Kuroda, T.; Kwon, S.M.; Kawamoto, A.; Akimaru, H.; Mifune, Y.; Shoji, T.; et al. SDF-1/CXCR4 Axis in Tie2-Lineage Cells Including Endothelial Progenitor Cells Contributes to Bone Fracture Healing. J. Bone Miner. Res. 2015, 30, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Tzeng, Y.S.; Chung, N.C.; Chen, Y.R.; Huang, H.Y.; Chuang, W.P.; Lai, D.M. Imbalanced Osteogenesis and Adipogenesis in Mice Deficient in the Chemokine Cxcl12/Sdf1 in the Bone Mesenchymal Stem/Progenitor Cells. J. Bone Miner. Res. 2018, 33, 679–690. [Google Scholar] [CrossRef] [PubMed]
- Blom, A.B.; Brockbank, S.M.; van Lent, P.L.; van Beuningen, H.M.; Geurts, J.; Takahashi, N.; van der Kraan, P.M.; van de Loo, F.A.; Schreurs, B.W.; Clements, K.; et al. Involvement of the Wnt Signaling Pathway in Experimental and Human Osteoarthritis: Prominent Role of Wnt-Induced Signaling Protein 1. Arthritis Rheum. 2009, 60, 501–512. [Google Scholar] [CrossRef]
- Yaykasli, K.O.; Hatipoglu, O.F.; Yaykasli, E.; Yildirim, K.; Kaya, E.; Ozsahin, M.; Uslu, M.; Gunduz, E. Leptin Induces ADAMTS-4, ADAMTS-5, and ADAMTS-9 Genes Expression by Mitogen-Activated Protein Kinases and NF-ĸB Signaling Pathways in Human Chondrocytes. Cell Biol. Int. 2015, 39, 104–112. [Google Scholar] [CrossRef]
- Prasadam, I.; Crawford, R.; Xiao, Y. Aggravation of ADAMTS and Matrix Metalloproteinase Production and Role of ERK1/2 Pathway in the Interaction of Osteoarthritic Subchondral Bone Osteoblasts and Articular Cartilage Chondrocytes—Possible Pathogenic Role in Osteoarthritis. J. Rheumatol. 2012, 39, 621–634. [Google Scholar] [CrossRef]
- Imai, T.; Hieshima, K.; Haskell, C.; Baba, M.; Nagira, M.; Nishimura, M.; Kakizaki, M.; Takagi, S.; Nomiyama, H.; Schall, T.J.; et al. Identification and Molecular Characterization of Fractalkine Receptor CX3CR1, Which Mediates Both Leukocyte Migration and Adhesion. Cell 1997, 91, 521–530. [Google Scholar] [CrossRef]
- Hundhausen, C.; Misztela, D.; Berkhout, T.A.; Broadway, N.; Saftig, P.; Reiss, K.; Hartmann, D.; Fahrenholz, F.; Postina, R.; Matthews, V.; et al. The Disintegrin-like Metalloproteinase ADAM10 Is Involved in Constitutive Cleavage of CX3CL1 (Fractalkine) and Regulates CX3CL1-Mediated Cell-Cell Adhesion. Blood 2003, 102, 1186–1195. [Google Scholar] [CrossRef]
- Goda, S.; Imai, T.; Yoshie, O.; Yoneda, O.; Inoue, H.; Nagano, Y.; Okazaki, T.; Imai, H.; Bloom, E.T.; Domae, N.; et al. CX3C-Chemokine, Fractalkine-Enhanced Adhesion of THP-1 Cells to Endothelial Cells Through Integrin-Dependent and -Independent Mechanisms. J. Immunol. 2000, 164, 4313–4320. [Google Scholar] [CrossRef]
- Matsunawa, M.; Isozaki, T.; Odai, T.; Yajima, N.; Takeuchi, H.T.; Negishi, M.; Ide, H.; Adachi, M.; Kasama, T. Increased Serum Levels of Soluble Fractalkine (CX3CL1) Correlate with Disease Activity in Rheumatoid Vasculitis. Arthritis Rheum. 2006, 54, 3408–3416. [Google Scholar] [CrossRef] [PubMed]
| Chemokine/Receptor | KO Phenotype | References | ||
|---|---|---|---|---|
| Chemokine Name | Specific Receptors * | Chemokine | Receptor | |
| MCP-1/CCL2 | CCR2 |
|
| * [16] [5,11] [11] |
| MIP-3β/CCL19 | CCR7 | - | Delayed cartilage degeneration post-MMD. | * [16] [17] |
| CCL21 | CCR7 | - |
| * [16] [17] [18] |
| Chemokines | Regulators of Chemokine Expression/Synthesis | Role | References | ||
|---|---|---|---|---|---|
| Chemokine Name | Inhibitors | Stimulators | Degradation | Formation | |
| MCP-1/CCL2 | Bindarit | Il-1β, LPS High glucose | Yes | Yes | [20] |
| [2] | |||||
| [19] | |||||
| [21] | |||||
| MCP2/CCL8 | Bindarit | High glucose | - | - | [20] |
| MCP3/CCL7 | Bindarit | High glucose Il-1β | - | - | [20] |
| [23] | |||||
| RANTES/CCL5 | Il-4, STAT6 miR-122 | Il-1β NF-kB | - | CCL5 + TGF-β1 CCL5 + CXCL12 | [24] |
| [25] | |||||
| [26] | |||||
| [27] | |||||
| [28] | |||||
| [29] | |||||
| MIP-1α/CCL3 | miR-122 | Resistin, Il-1β miR-451 | Yes | - | [25] |
| [30] | |||||
| MIP-1β/CCL4 | miR-495 | Resistin Il-1β | - | Yes | [31] |
| [30] | |||||
| MIP-3α/CCL20 | - | - | CCL20 | - | [32] |
| CCL21 | - | - | CCL21-CCR7 in MMD | CCL21-CCR7 in FTCD in juvenile | [33] |
| [17] | |||||
| [18] | |||||
| CCL22 | - | - | Yes | - | [34] |
| CXCL5 | miR-4284 | MSC-DEV | - | CXCL5/CXCL6-CXCR2 | [35] |
| [36] | |||||
| CXCL6/GCP2 | MSC-DEV | - | - | CXCL5/CXCL6-CXCR2 | [36] |
| CXCL12 | - | - | CXCL12 | CXCL12 + CCL5 CXCL12 + TGF-β1 | [37] |
| [29] | |||||
| [38] | |||||
| CX3CL1/Fractalin | - | - | CX3CL1 | - | [39] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Edderkaoui, B. Chemokines in Cartilage Regeneration and Degradation: New Insights. Int. J. Mol. Sci. 2024, 25, 381. https://doi.org/10.3390/ijms25010381
Edderkaoui B. Chemokines in Cartilage Regeneration and Degradation: New Insights. International Journal of Molecular Sciences. 2024; 25(1):381. https://doi.org/10.3390/ijms25010381
Chicago/Turabian StyleEdderkaoui, Bouchra. 2024. "Chemokines in Cartilage Regeneration and Degradation: New Insights" International Journal of Molecular Sciences 25, no. 1: 381. https://doi.org/10.3390/ijms25010381
APA StyleEdderkaoui, B. (2024). Chemokines in Cartilage Regeneration and Degradation: New Insights. International Journal of Molecular Sciences, 25(1), 381. https://doi.org/10.3390/ijms25010381





