Cisplatin in Ovarian Cancer Treatment—Known Limitations in Therapy Force New Solutions
Abstract
1. Introduction
2. The History of Cisplatin
3. Cisplatin—Mechanisms of Its Cytotoxic Action
3.1. Damaging the Genomic DNA
3.2. Damaging the Mitochondrial DNA
3.3. Induction of Oxidative Stress in Cells
4. Disadvantages and Limitations of Cisplatin
4.1. Toxic Side Effects
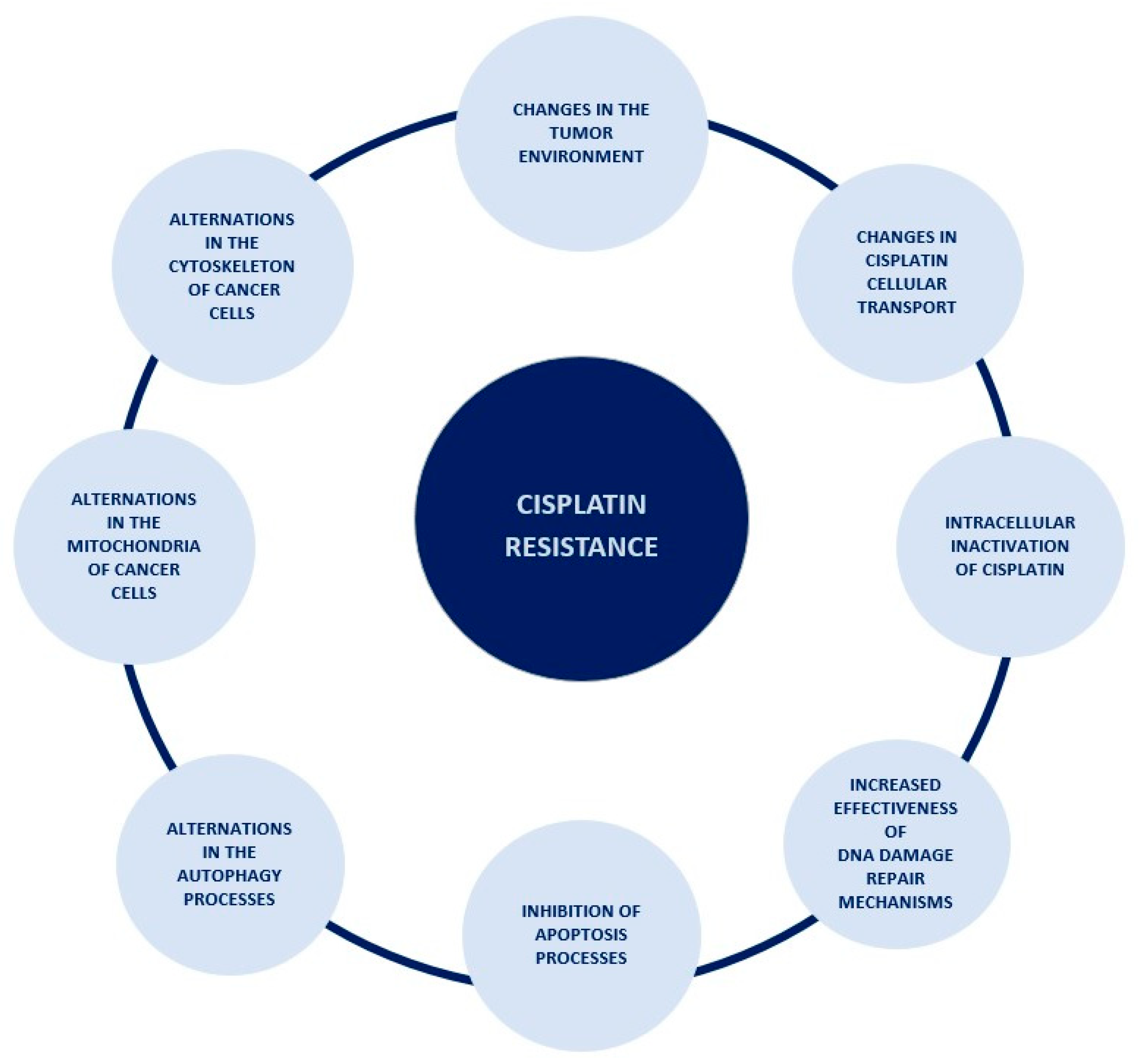
4.2. Acquisition of Resistance to Cisplatin by Cancer Cells
4.2.1. Changes in Cisplatin Cellular Transport
4.2.2. Intracellular Inactivation of Cisplatin
4.2.3. Increased Effectiveness of DNA Damage Repair Mechanisms
4.2.4. Inhibition of Apoptosis Processes
4.2.5. Changes in the Autophagy Processes
4.2.6. Changes in the Mitochondria of Cancer Cells
4.2.7. Changes in the Cytoskeleton of Cancer Cells
4.2.8. Changes in the Tumor Microenvironment
5. Strategies to Increase the Effectiveness of Cisplatin in the Treatment of Ovarian Cancer
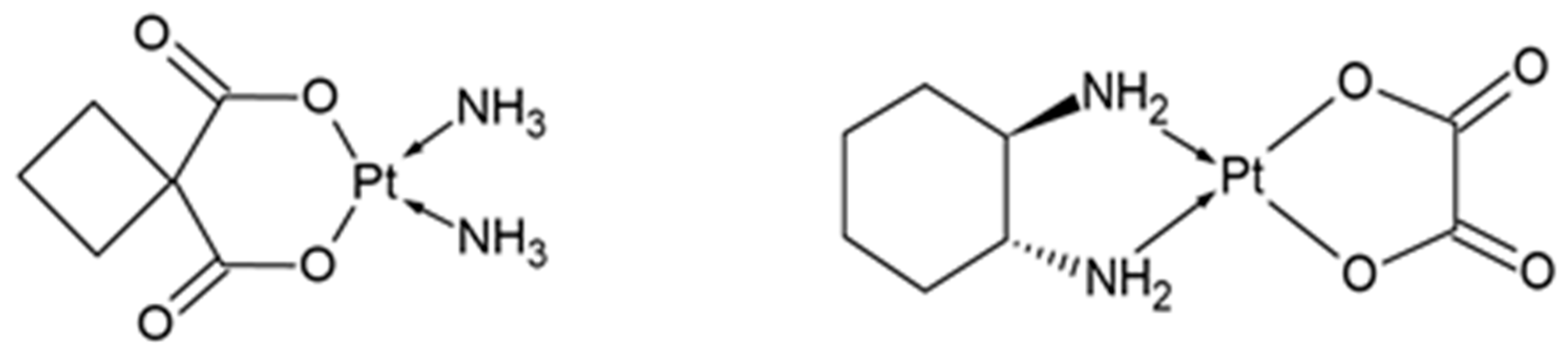
5.1. Designing of Cisplatin Analogs
5.2. Combination Therapy with Other Drugs
5.3. Combination Therapy with Substances Derived from Plants
5.4. Combination Therapy with Cisplatin and Radiotherapy
5.5. Combination Therapy with Cisplatin and Hyperthermia
5.6. Nanocarriers for Controlled Delivery of Cisplatin
| Components of Combination Therapy | Possible Applications | References |
|---|---|---|
| Cisplatin + paclitaxel | Ovarian cancer Cervical cancer Gastric cancer Non-small-cell lung cancer | [7,8,80,95] |
| Cisplatin + docetaxel | Ovarian cancer Head and neck cancer Non-small-cell lung cancer Breast cancer | [80,98,121,122] |
| Cisplatin + cardamonin | Ovarian cancer | [99] |
| Cisplatin + berberine | Ovarian cancer Breast cancer Gastric cancer | [100,123,124] |
| Cisplatin + emodin | Ovarian cancer Non-small-cell lung cancer Bladder cancer Gastric cancer Endometrial cancer | [101,125,126,127,128] |
| Cisplatin + thymoquinone | Ovarian cancer Lung cancer | [102,129] |
| Cisplatin + genistein | Ovarian cancer Cervical cancer Non-small-cell lung cancer | [103,130,131] |
| Cisplatin + luteolin | Ovarian cancer Colorectal cancer | [104,132] |
| Cisplatin + saikosaponin-D | Ovarian cancer Gastric cancer Cervical cancer Non-small-cell lung cancer | [105,133,134] |
| Cisplatin + radiotherapy | Ovarian cancer Head and neck cancer Cervical cancer | [19,120] |
| Cisplatin + hyperthermia | Ovarian cancer Bladder cancer Oral cancer | [108,135,136] |
| Platinum Complex | Possible Applications | Current Approval Status | References |
|---|---|---|---|
| Cisplatin | Ovarian cancer Testicular cancer Head and neck cancer Bladder cancer | Approved and used in cancer therapy since 1978 | [6,85] |
| Carboplatin | Ovarian cancer Non-small-cell lung cancer Breast cancer Cervical cancer Testicular cancer | Approved and used in cancer therapy since 1989 | [85,137,138] |
| Oxaliplatin | Colon cancer Gastric cancer Esophageal cancer Ovarian cancer Testicular cancer | Approved and used in cancer therapy since 1999 in Europe and 2002 in the USA | [85,91] |
| Nedaplatin | Non-small-cell lung cancer Esophageal cancer Head and neck cancer Ovarian cancer Urothelial cancer | In clinical trials. Approved and used in cancer therapy since 1995 in Japan | [85,139] |
| Heptaplatin | Gastric cancer Head and neck cancer | In clinical trials. Approved and used in cancer therapy since 2005 in Korea | [6,85] |
| Lobaplatin | Breast cancer Small-cell lung cancer Ovarian cancer Cervical cancer Gastric cancer | In clinical trials. Approved and used in cancer therapy since 2004 in China | [85,140,141] |
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Today; International Agency for Research on Cancer: Lyon, France, 2020; Available online: https://gco.iarc.fr/today/onlineanalysistable?v=2020&mode=cancer&mode_population=continents&population=900&populations=908&key=asr&sex=2&cancer=39&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&group_cancer=1&include_nmsc=0&include_nmsc_other=1#collapse-group-0-4 (accessed on 24 September 2022).
- Ferlay, J.; Laversanne, M.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Tomorrow; International Agency for Research on Cancer: Lyon, France, 2020; Available online: https://gco.iarc.fr/tomorrow/en/dataviz/isotype?cancers=25&single_unit=10000&sexes=2&years=2040&types=1 (accessed on 24 September 2022).
- Chandra, A.; Pius, C.; Nabeel, M.; Nair, M.; Vishwanatha, J.K.; Ahmad, S.; Basha, R. Ovarian cancer: Current status and strategies for improving therapeutic outcomes. Cancer Med. 2019, 8, 7018–7031. [Google Scholar] [CrossRef] [PubMed]
- Winter, W.E., 3rd; Maxwell, G.L.; Tian, C.; Sundborg, M.J.; Rose, G.S.; Rose, P.G.; Rubin, S.C.; Muggia, F.; McGuire, W.P. Tumor residual after surgical cytoreduction in prediction of clinical outcome in stage IV epithelial ovarian cancer: A Gynecologic Oncology Group Study. J. Clin. Oncol. 2008, 26, 83–89. [Google Scholar] [CrossRef]
- Parmar, M.K.; Ledermann, J.A.; Colombo, N.; du Bois, A.; Delaloye, J.-F.; Kristensen, G.B.; Wheeler, S.; Swart, A.M.; Qian, W.; Torri, V.; et al. Paclitaxel plus platinum-based chemotherapy versus conventional platinum-based chemotherapy in women with relapsed ovarian cancer: The ICON4/AGO-OVAR-2.2 trial. Lancet 2003, 361, 2099–2106. [Google Scholar]
- Ghosh, S. Cisplatin: The first metal based anticancer drug. Bioorg. Chem. 2019, 88, 102925. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.J.; Chun, S.H.; Kim, K.O.; Kim, M.K.; Lee, K.H.; Hyun, M.S.; Bae, S.H.; Ryoo, H.M.; Do, Y.R.; Kwon, K.Y.; et al. The Efficacy of Paclitaxel and Cisplatin Combination Chemotherapy for the Treatment of Metastatic or Recurrent Gastric Cancer: A Multicenter Phase II Study. Korean J. Intern. Med. 2005, 20, 135–140. [Google Scholar] [CrossRef]
- Sohn, J.H.; Kim, Y.T.; Rha, S.Y.; Yoo, N.C.; Roh, J.K.; Kim, B.S.; Suh, C.O.; Kim, G.E.; Jang, W.I.; Chung, H.C. Paclitaxel and Cisplatin Combination Chemotherapy in Pretreated Breast Cancer. Cancer Res. Treat. 2003, 35, 267–273. [Google Scholar] [CrossRef]
- Ciccarelli, R.B.; Solomon, M.J.; Varshavsky, A.; Lippard, S.J. In vivo effects of cis- and trans-diamminedichloroplatinum(II) on SV40 chromosomes: Differential repair, DNA-protein crosslinking, and inhibition of replication. Biochemistry 1985, 24, 7533–7540. [Google Scholar] [CrossRef]
- Skowron, M.A.; Melnikova, M.; Van Roermund, J.G.H.; Romano, A.; Albers, P.; Thomale, J.; Schulz, W.A.; Niegisch, G.; Hoffmann, M.J. Multifaceted Mechanisms of Cisplatin Resistance in Long-Term Treated Urothelial Carcinoma Cell Lines. Int. J. Mol. Sci. 2018, 19, 590. [Google Scholar] [CrossRef]
- Dentino, M.; Luft, F.; Yum, M.N.; Williams, S.D.; Einhorn, L.H. Long term effect of Cis-Diamminedichloride platinum (CDDP) on renal function and structure in man. Cancer 1978, 41, 1274–1281. [Google Scholar] [CrossRef] [PubMed]
- Breglio, A.M.; Rusheen, A.E.; Shide, E.D.; Fernandez, K.A.; Spielbauer, K.K.; McLachlin, K.M.; Hall, M.D.; Amable, L.; Cunningham, L.L. Cisplatin is retained in the cochlea indefinitely following chemotherapy. Nat. Commun. 2017, 8, 1654. [Google Scholar] [CrossRef]
- Bearcroft, C.P.; Domizio, P.; Mourad, F.H.; André, E.A.; Farthing, M.J.G. Cisplatin impairs fluid and electrolyte absorption in rat small intestine: A role for 5-hydroxytryptamine. Gut 1999, 44, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Siddik, Z.H. Cisplatin Resistance. In Cancer Drug Resistance. Cancer Drug Discovery and Development; Teicher, B.A., Ed.; Humana Press: Totowa, NJ, USA, 2006. [Google Scholar] [CrossRef]
- Damia, G.; Imperatori, L.; Stefanini, M.; D’Incalci, M. Sensitivity of CHO mutant cell lines with specific defects in nucleotide excision repair to different anti-cancer agents. Int. J. Cancer 1996, 66, 779–783. [Google Scholar] [CrossRef]
- Schoeberl, A.; Gutmann, M.; Theiner, S.; Corte-Rodríguez, M.; Braun, G.; Vician, P.; Berger, W.; Koellensperger, G. The copper transporter CTR1 and cisplatin accumulation at the single-cell level by LA-ICP-TOFMS. Front. Mol. Biosci. 2022, 9, 1055356. [Google Scholar] [CrossRef]
- Song, M.; Cui, M.; Liu, K. Therapeutic strategies to overcome cisplatin resistance in ovarian cancer. Eur. J. Med. Chem. 2022, 232, 114205. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.-Y.; Zhang, Q.-Y.; Zheng, G.-J.; Feng, B. Phytochemicals: Current strategy to sensitize cancer cells to cisplatin. Biomed. Pharmacother. 2018, 110, 518–527. [Google Scholar] [CrossRef]
- Zhao, L.; Liu, S.; Liang, D.; Jiang, T.; Yan, X.; Zhao, S.; Liu, Y.; Zhao, W.; Yu, H. Resensitization of cisplatin resistance ovarian cancer cells to cisplatin through pretreatment with low-dose fraction radiation. Cancer Med. 2019, 8, 2442–2448. [Google Scholar] [CrossRef]
- Sukovas, A.; Silkuniene, G.; Trumbeckaite, S.; Jasukaitiene, A.; Degutyte-Fomins, L.; Mildaziene, V.; Gulbinas, A.; Baniene, R.; Dambrauskas, Z.; Paskauskas, S. Hyperthermia potentiates cisplatin cytotoxicity and negative effects on mitochondrial functions in OVCAR-3 cells. J. Bioenerg. Biomembr. 2019, 51, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Avendaño, C.; Menéndez, C.J. Medicinal Chemistry of Anticancer Drugs, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2015; p. 230. [Google Scholar]
- Makovec, T. Cisplatin and beyond: Molecular mechanisms of action and drug resistance development in cancer chemotherapy. Radiol. Oncol. 2019, 53, 148–158. [Google Scholar] [CrossRef]
- Alderden, R.A.; Hall, M.D.; Hambley, T. The Discovery and Development of Cisplatin. J. Chem. Educ. 2006, 83, 728–734. [Google Scholar] [CrossRef]
- Rosenberg, B.; Van Camp, L.; Grimley, E.B.; Thomson, A.J. The Inhibition of Growth or Cell Division in Escherichia coli by Different Ionic Species of Platinum(IV) Complexes. J. Biol. Chem. 1967, 242, 1347–1352. [Google Scholar] [CrossRef]
- Rosenberg, B.; Vancamp, L.; Trosko, J.E.; Mansour, V.H. Platinum Compounds: A New Class of Potent Antitumour Agents. Nature 1969, 222, 385–386. [Google Scholar] [CrossRef] [PubMed]
- Dhara, S.C. A Rapid Method for the Synthesis of cis-Pt(NH3)2Cl2]. Indian J. Chem. 1970, 8, 193–194. [Google Scholar]
- Petrovic, M.; Todorovic, M. Biochemical and molecular mechanisms of action of cisplatin in cancer cells. Med. Biol. 2016, 18, 12–18. [Google Scholar]
- Nagai, N.; Okuda, R.; Kinoshita, M.; Ogata, H. Decomposition Kinetics of Cisplatin in Human Biological Fluids. J. Pharm. Pharmacol. 1996, 48, 918–924. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.S.; Berners-Price, S.J.; Hambley, T.W. Slowing of Cisplatin Aquation in the Presence of DNA but Not in the Presence of Phosphate: Improved Understanding of Sequence Selectivity and the Roles of Monoaquated and Diaquated Species in the Binding of Cisplatin to DNA. Inorg. Chem. 2000, 39, 5603–5613. [Google Scholar] [CrossRef]
- Rocha, C.R.R.; Silva, M.M.; Quinet, A.; Cabral-Neto, J.B.; Menck, C.F.M. DNA repair pathways and cisplatin resistance: An intimate relationship. Clinics 2018, 73, e478s. [Google Scholar] [CrossRef]
- Fichtinger-Schepman, A.M.J.; Van der Veer, J.L.; Hartog, J.H.J.D.; Lohman, P.H.M.; Reedijk, J. Adducts of the antitumor drug cis-diamminedichloroplatinum(II) with DNA: Formation, identification, and quantitation. Biochemistry 1985, 24, 707–713. [Google Scholar] [CrossRef]
- Baik, M.-H.; Friesner, R.A.; Lippard, S.J. Theoretical Study of Cisplatin Binding to Purine Bases: Why Does Cisplatin Prefer Guanine over Adenine? J. Am. Chem. Soc. 2003, 125, 14082–14092. [Google Scholar] [CrossRef]
- Reardon, J.T.; Vaisman, A.; Chaney, S.G.; Sancar, A. Efficient nucleotide excision repair of cisplatin, oxaliplatin, and Bis-aceto-ammine-dichloro-cyclohexylamine-platinum(IV) (JM216) platinum intrastrand DNA diadducts. Cancer Res 1999, 59, 3968–3971. [Google Scholar]
- Borkar, P.; Bhandari, P.; Yadav, S.; Prabhu, A. Cisplatin Resistance in Ovarian Cancer: Classical Outlook and Newer Perspectives. Biomed. Pharmacol. J. 2021, 14, 1993–2005. [Google Scholar] [CrossRef]
- Fuertes, M.A.; Alonso, C.; Pérez, J.M. Biochemical Modulation of Cisplatin Mechanisms of Action: Enhancement of Antitumor Activity and Circumvention of Drug Resistance. Chem. Rev. 2003, 103, 645–662. [Google Scholar] [CrossRef] [PubMed]
- Brozovic, A.; Ambriović-Ristov, A.; Osmak, M. The relationship between cisplatin-induced reactive oxygen species, glutathione, and BCL-2 and resistance to cisplatin. Crit. Rev. Toxicol. 2010, 40, 347–359. [Google Scholar] [CrossRef]
- Scheel-Toellner, D.; Wang, K.; Craddock, R.; Webb, P.R.; McGettrick, H.; Assi, L.K.; Parkes, N.; Clough, L.E.; Gulbins, E.; Salmon, M.; et al. Reactive oxygen species limit neutrophil life span by activating death receptor signaling. Blood 2004, 104, 2557–2564. [Google Scholar] [CrossRef]
- Xu, J.; Gewirtz, D.A. Is Autophagy Always a Barrier to Cisplatin Therapy? Biomolecules 2022, 12, 463. [Google Scholar] [CrossRef] [PubMed]
- Qi, L.; Luo, Q.; Zhang, Y.; Jia, F.; Zhao, Y.; Wang, F. Advances in Toxicological Research of the Anticancer Drug Cisplatin. Chem. Res. Toxicol. 2019, 32, 1469–1486. [Google Scholar] [CrossRef]
- Podratz, J.L.; Knight, A.M.; Ta, L.E.; Staff, N.P.; Gass, J.M.; Genelin, K.; Schlattau, A.; Lathroum, L.; Windebank, A.J. Cisplatin induced Mitochondrial DNA damage in dorsal root ganglion neurons. Neurobiol. Dis. 2011, 41, 661–668. [Google Scholar] [CrossRef]
- Oun, R.; Rowan, E. Cisplatin induced arrhythmia; electrolyte imbalance or disturbance of the SA node? Eur. J. Pharmacol. 2017, 811, 125–128. [Google Scholar] [CrossRef] [PubMed]
- Nowrousian, M.R.; Schmidt, C.G. Effects of cisplatin on different haemopoietic progenitor cells in mice. Br. J. Cancer 1982, 46, 397–402. [Google Scholar] [CrossRef]
- Amable, L. Cisplatin resistance and opportunities for precision medicine. Pharmacol. Res. 2016, 106, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Öhrvik, H.; Thiele, D.J. The role of Ctr1 and Ctr2 in mammalian copper homeostasis and platinum-based chemotherapy. J. Trace Elem. Med. Biol. 2015, 31, 178–182. [Google Scholar] [CrossRef]
- Du, X.; Li, H.; Wang, X.; Liu, Q.; Ni, J.; Sun, H. Kinetics and thermodynamics of metal binding to the N-terminus of a human copper transporter, hCTR1. Chem. Commun. 2013, 49, 9134–9136. [Google Scholar] [CrossRef] [PubMed]
- Crider, S.E.; Holbrook, R.J.; Franz, K.J. Coordination of platinum therapeutic agents to met-rich motifs of human copper transport protein1. Metallomics 2010, 2, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Öhrvik, H.; Nose, Y.; Wood, L.K.; Kim, B.-E.; Gleber, S.-C.; Ralle, M.; Thiele, D.J. Ctr2 regulates biogenesis of a cleaved form of mammalian Ctr1 metal transporter lacking the copper- and cisplatin-binding ecto-domain. Proc. Natl. Acad. Sci. USA 2013, 110, E4279–E4288. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-Y.; Choi, C.H.; Do, I.-G.; Song, S.Y.; Lee, W.; Park, H.S.; Song, T.J.; Kim, M.K.; Kim, T.-J.; Lee, J.-W.; et al. Prognostic value of the copper transporters, CTR1 and CTR2, in patients with ovarian carcinoma receiving platinum-based chemotherapy. Gynecol. Oncol. 2011, 122, 361–365. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, H.; Teramae, M.; Yamauchi, M.; Fukuda, T.; Yasui, T.; Sumi, T.; Honda, K.-I.; Ishiko, O. Association of copper transporter expression with platinum resistance in epithelial ovarian cancer. Anticancer. Res. 2013, 33, 1409–1414. [Google Scholar]
- Li, Y.-Q.; Yin, J.-Y.; Liu, Z.-Q.; Li, X.-P. Copper efflux transporters ATP7A and ATP7B: Novel biomarkers for platinum drug resistance and targets for therapy. IUBMB Life 2018, 70, 183–191. [Google Scholar] [CrossRef]
- Samimi, G.; Varki, N.M.; Wilczynski, S.; Safaei, R.; Alberts, D.S.; Howell, S.B. Increase in expression of the copper transporter ATP7A during platinum drug-based treatment is associated with poor survival in ovarian cancer patients. Clin. Cancer Res. 2003, 9, 5853–5859. [Google Scholar]
- Samimi, G.; Safaei, R.; Katano, K.; Holzer, A.K.; Rochdi, M.; Tomioka, M.; Goodman, M.; Howell, S.B. Increased Expression of the Copper Efflux Transporter ATP7A Mediates Resistance to Cisplatin, Carboplatin, and Oxaliplatin in Ovarian Cancer Cells. Clin. Cancer Res. 2004, 10, 4661–4669. [Google Scholar] [CrossRef]
- Komatsu, M.; Sumizawa, T.; Mutoh, M.; Chen, Z.S.; Terada, K.; Furukawa, T.; Yang, X.L.; Gao, H.; Miura, N.; Sugiyama, T.; et al. Copper-transporting P-type adenosine triphosphatase (ATP7B) is associated with cisplatin resistance. Cancer Res. 2000, 60, 1312–1316. [Google Scholar]
- Nakayama, K.; Kanzaki, A.; Terada, K.; Mutoh, M.; Ogawa, K.; Sugiyama, T.; Takenoshita, S.; Itoh, K.; Yaegashi, N.; Miyazaki, K.; et al. Prognostic Value of the Cu-Transporting ATPase in Ovarian Carcinoma Patients Receiving Cisplatin-Based Chemotherapy. Clin. Cancer Res. 2004, 10, 2804–2811. [Google Scholar] [CrossRef]
- Goto, S.; Iida, T.; Cho, S.; Oka, M.; Kohno, S.; Kondo, T. Overexpression of glutathione S-transferase pi enhances the adduct formation of cisplatin with glutathione in human cancer cells. Free Radic. Res. 1999, 31, 549–558. [Google Scholar] [CrossRef] [PubMed]
- Godwin, A.K.; Meister, A.; O’Dwyer, P.J.; Huang, C.S.; Hamilton, T.C.; Anderson, M.E. High resistance to cisplatin in human ovarian cancer cell lines is associated with marked increase of glutathione synthesis. Proc. Natl. Acad. Sci. USA 1992, 89, 3070–3074. [Google Scholar] [CrossRef] [PubMed]
- Kelley, S.L.; Basu, A.; Teicher, B.A.; Hacker, M.P.; Hamer, D.H.; Lazo, J.S. Overexpression of Metallothionein Confers Resistance to Anticancer Drugs. Science 1988, 241, 1813–1815. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Gao, S.; Hou, J. ERCC1 expression and platinum chemosensitivity in patients with ovarian cancer: A meta-analysis. Int. J. Biol. Markers 2020, 35, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Geisler, J.P.; Goodheart, M.J.; Sood, A.K.; Holmes, R.J.; Hatterman-Zogg, M.A.; Buller, R.E. Mismatch repair gene expression defects contribute to microsatellite instability in ovarian carcinoma. Cancer 2003, 98, 2199–2206. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.A.; Lord, C.J.; Ashworth, A. Therapeutic Targeting of the DNA Mismatch Repair Pathway. Clin. Cancer Res. 2010, 16, 5107–5113. [Google Scholar] [CrossRef] [PubMed]
- Eliopoulos, A.G.; Kerr, D.J.; Herod, J.; Hodgkins, L.; Krajewski, S.; Reed, J.C.; Young, L. The control of apoptosis and drug resistance in ovarian cancer: Influence of p53 and Bcl-2. Oncogene 1995, 11, 1217–1228. [Google Scholar]
- Asselin, E.; Mills, G.B.; Tsang, B.K. XIAP regulates Akt activity and caspase-3-dependent cleavage during cisplatin-induced apoptosis in human ovarian epithelial cancer cells. Cancer Res 2001, 61, 1862–1868. [Google Scholar]
- Gąsiorkiewicz, B.M.; Koczurkiewicz-Adamczyk, P.; Piska, K.; Pękala, E. Autophagy modulating agents as chemosensitizers for cisplatin therapy in cancer. Investig. New Drugs 2020, 39, 538–563. [Google Scholar] [CrossRef]
- Cocetta, V.; Ragazzi, E.; Montopoli, M. Mitochondrial Involvement in Cisplatin Resistance. Int. J. Mol. Sci. 2019, 20, 3384. [Google Scholar] [CrossRef]
- Mei, H.; Sun, S.; Bai, Y.; Chen, Y.; Chai, R.; Li, H. Reduced mtDNA copy number increases the sensitivity of tumor cells to chemotherapeutic drugs. Cell Death Dis. 2015, 6, e1710. [Google Scholar] [CrossRef] [PubMed]
- Kong, B.; Wang, Q.; Fung, E.; Xue, K.; Tsang, B.K. p53 Is Required for Cisplatin-induced Processing of the Mitochondrial Fusion Protein L-Opa1 That Is Mediated by the Mitochondrial Metallopeptidase Oma1 in Gynecologic Cancers. J. Biol. Chem. 2014, 289, 27134–27145. [Google Scholar] [CrossRef] [PubMed]
- Frezza, C.; Cipolat, S.; de Brito, O.M.; Micaroni, M.; Beznoussenko, G.V.; Rudka, T.; Bartoli, D.; Polishuck, R.S.; Danial, N.N.; De Strooper, B.; et al. OPA1 Controls Apoptotic Cristae Remodeling Independently from Mitochondrial Fusion. Cell 2006, 126, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Farrand, L.; Byun, S.; Kim, J.Y.; Im-Aram, A.; Lee, J.; Lim, S.; Lee, K.W.; Suh, J.-Y.; Lee, H.J.; Tsang, B.K. Piceatannol Enhances Cisplatin Sensitivity in Ovarian Cancer via Modulation of p53, X-linked Inhibitor of Apoptosis Protein (XIAP), and Mitochondrial Fission. J. Biol. Chem. 2013, 288, 23740–23750. [Google Scholar] [CrossRef]
- Shimizu, T.; Fujii, T.; Sakai, H. The Relationship Between Actin Cytoskeleton and Membrane Transporters in Cisplatin Resistance of Cancer Cells. Front. Cell Dev. Biol. 2020, 8, 597835. [Google Scholar] [CrossRef]
- Mokady, D.; Meiri, D. RhoGTPases—A novel link between cytoskeleton organization and cisplatin resistance. Drug Resist. Updat. 2015, 19, 22–32. [Google Scholar] [CrossRef]
- Lee, E.L.; Shimizu, T.; Ise, T.; Numata, T.; Kohno, K.; Okada, Y. Impaired activity of volume-sensitive Cl− channel is involved in cisplatin resistance of cancer cells. J. Cell. Physiol. 2006, 211, 513–521. [Google Scholar] [CrossRef]
- Chen, S.-H.; Chang, J.-Y. New Insights into Mechanisms of Cisplatin Resistance: From Tumor Cell to Microenvironment. Int. J. Mol. Sci. 2019, 20, 4136. [Google Scholar] [CrossRef]
- Tannock, I.F.; Lee, C.M.; Tunggal, J.K.; Cowan, D.S.; Egorin, M.J. Limited penetration of anticancer drugs through tumor tissue: A potential cause of resistance of solid tumors to chemotherapy. Clin. Cancer Res. 2002, 8, 878–884. [Google Scholar]
- Senthebane, D.A.; Jonker, T.; Rowe, A.; Thomford, N.E.; Munro, D.; Dandara, C.; Wonkam, A.; Govender, D.; Calder, B.; Soares, N.C.; et al. The Role of Tumor Microenvironment in Chemoresistance: 3D Extracellular Matrices as Accomplices. Int. J. Mol. Sci. 2018, 19, 2861. [Google Scholar] [CrossRef]
- Dasari, S.; Fang, Y.; Mitra, A.K. Cancer Associated Fibroblasts: Naughty Neighbors That Drive Ovarian Cancer Progression. Cancers 2018, 10, 406. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Chen, Z.; Wang, Y.; Zhao, H.; Du, Y. The Role of Cancer-Associated Fibroblasts in Ovarian Cancer. Cancers 2022, 14, 2637. [Google Scholar] [CrossRef] [PubMed]
- Steitz, A.M.; Steffes, A.; Finkernagel, F.; Unger, A.; Sommerfeld, L.; Jansen, J.M.; Wagner, U.; Graumann, J.; Müller, R.; Reinartz, S. Tumor-associated macrophages promote ovarian cancer cell migration by secreting transforming growth factor beta induced (TGFBI) and tenascin C. Cell Death Dis. 2020, 11, 249. [Google Scholar] [CrossRef] [PubMed]
- Lecker, L.S.; Berlato, C.; Maniati, E.; Delaine-Smith, R.; Pearce, O.M.; Heath, O.; Nichols, S.J.; Trevisan, C.; Novak, M.; McDermott, J.; et al. TGFBI Production by Macrophages Contributes to an Immunosuppressive Microenvironment in Ovarian Cancer. Cancer Res 2021, 81, 5706–5719. [Google Scholar] [CrossRef]
- McGuire, W.P.; Hoskins, W.J.; Brady, M.F.; Kucera, P.R.; Partridge, E.E.; Look, K.Y.; Clarke-Pearson, D.L.; Davidson, M. Cyclophosphamide and Cisplatin Compared with Paclitaxel and Cisplatin in Patients with Stage III and Stage IV Ovarian Cancer. N. Engl. J. Med. 1996, 334, 1–6. [Google Scholar] [CrossRef]
- Brown, A.; Kumar, S.; Tchounwou, P.B. Cisplatin-Based Chemotherapy of Human Cancers. J. Cancer Sci. Ther. 2019, 11, 97. [Google Scholar]
- Nugawela, D.; Gorringe, K.L. Targetedtherapy for mucinous ovarian carcinoma: Evidence from clinical trials. Int. J. Gynecol. Cancer 2023, 33, 102–108. [Google Scholar] [CrossRef]
- Tate, S.; Nishikimi, K.; Matsuoka, A.; Otsuka, S.; Shiko, Y.; Ozawa, Y.; Kawasaki, Y.; Shozu, M. Bevacizumab in First-Line Chemotherapy Improves Progression-Free Survival for Advanced OvarianClear Cell Carcinoma. Cancers 2021, 13, 3177. [Google Scholar] [CrossRef]
- Fujimura, M.; Katsumata, N.; Tsuda, H.; Uchi, N.; Miyazaki, S.; Hidaka, T.; Sakai, M.; Saito, S. HER2 Is Frequently Over-expressed in Ovarian Clear Cell Adenocarcinoma: Possible Novel Treatment Modality Using Recombinant Monoclonal Antibody against HER2, Trastuzumab. Jpn. J. Cancer Res. 2002, 93, 1250–1257. [Google Scholar] [CrossRef]
- Matsuo, K.; Nishimura, M.; Bottsford-Miller, J.N.; Huang, J.; Komurov, K.; Armaiz-Pena, G.N.; Shahzad, M.M.; Stone, R.L.; Roh, J.W.; Sanguino, A.M.; et al. Targeting Src in Mucinous Ovarian Carcinoma. Clin. Cancer Res. 2011, 17, 5367–5378. [Google Scholar] [CrossRef]
- Kopacz-Bednarska, A.; Król, T. Selected platinum complexes in standard and modern anti-cancer therapies. Nowotwory. J. Oncol. 2022, 72, 96–105. [Google Scholar] [CrossRef]
- Muggia, F. Overview of carboplatin: Replacing, complementing, and extending the therapeutic horizons of cisplatin. Semin. Oncol. 1989, 16, 7–13. [Google Scholar] [PubMed]
- Ciancetta, A.; Coletti, C.; Marrone, A.; Re, N. Activation of carboplatin by chloride ions: A theoretical investigation. Theor. Chem. Accounts 2011, 129, 757–769. [Google Scholar] [CrossRef]
- Sousa, G.; Wlodarczyk, S.; Monteiro, G. Carboplatin: Molecular mechanisms of action associated with chemo resistance. Braz. J. Pharm. Sci. 2014, 50, 693–701. [Google Scholar] [CrossRef]
- Los, G.; Verdegaal, E.; Noteborn, H.P.; Ruevekamp, M.; de Graeff, A.; Meesters, E.W.; Huinink, D.T.B.; McVie, J. Cellular pharmacokinetics of carboplatin and cisplatin in relation to their cytotoxic action. Biochem. Pharmacol. 1991, 42, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Alcindor, T.; Beauger, N. Oxaliplatin: A Review in the Era of Molecularly Targeted Therapy. Curr. Oncol. 2011, 18, 18–25. [Google Scholar] [CrossRef]
- Bogliolo, S.; Cassani, C.; Gardella, B.; Musacchi, V.; Babilonti, L.; Venturini, P.-L.; Ferrero, S.; Spinillo, A. Oxaliplatin for the treatment of ovarian cancer. Expert Opin. Investig. Drugs 2015, 24, 1062874. [Google Scholar] [CrossRef]
- Takimoto, C.H.; Graham, M.A.; Lockwood, G.; Ng, C.M.; Goetz, A.; Greenslade, D.; Remick, S.C.; Sharma, S.; Mani, S.; Ramanathan, R.K.; et al. Oxaliplatin Pharmacokinetics and Pharmacodynamics in Adult Cancer Patients with Impaired Renal Function. Clin. Cancer Res. 2007, 13, 4832–4839. [Google Scholar] [CrossRef]
- Allain, P.; Heudi, O.; Cailleux, A.; Le Bouil, A.; Larra, F.; Boisdron-Celle, M.; Gamelin, E. Early biotransformations of oxaliplatin after its intravenous administration to cancer patients. Drug Metab. Dispos. 2000, 28, 1379–1384. [Google Scholar]
- Kokabu, T.; Aoyama, K.; Tarumi, Y.; Kataoka, H.; Yoriki, K.; Mori, T. Successful nedaplatin desensitization therapy in a patient with platinum-sensitive recurrent ovarian cancer: A case report and literature review. Gynecol. Oncol. Rep. 2022, 43, 101065. [Google Scholar] [CrossRef]
- Kampan, N.C.; Madondo, M.T.; McNally, O.M.; Quinn, M.; Plebanski, M. Paclitaxel and Its Evolving Role in the Management of Ovarian Cancer. BioMed Res. Int. 2015, 2015, 413076. [Google Scholar] [CrossRef] [PubMed]
- Parness, J.; Horwitz, S.B. Taxol binds to polymerized tubulin in vitro. J. Cell Biol. 1981, 91, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Schiff, P.B.; Fant, J.; Horwitz, S.B. Promotion of microtubule assembly in vitro by taxol. Nature 1979, 277, 665–667. [Google Scholar] [CrossRef]
- Katsumata, N. Docetaxel: An alternative taxane in ovarian cancer. Br. J. Cancer 2003, 89, S9–S15. [Google Scholar] [CrossRef] [PubMed]
- Niu, P.; Shi, D.; Zhang, S.; Zhu, Y.; Zhou, J. Cardamonin enhances the anti-proliferative effect of cisplatin on ovarian cancer. Oncol. Lett. 2018, 15, 3991–3997. [Google Scholar] [CrossRef]
- Chen, Q.; Qin, R.; Fang, Y.; Li, H. Berberine Sensitizes Human Ovarian Cancer Cells to Cisplatin Through miR-93/PTEN/Akt Signaling Pathway. Cell. Physiol. Biochem. 2015, 36, 956–965. [Google Scholar] [CrossRef]
- Ma, J.; Yang, J.; Wang, C.; Zhang, N.; Dong, Y.; Wang, C.; Wang, Y.; Lin, X. Emodin Augments Cisplatin Cytotoxicity in Platinum-Resistant Ovarian Cancer Cells via ROS-Dependent MRP1 Downregulation. BioMed Res. Int. 2014, 2014, 107671. [Google Scholar] [CrossRef]
- Wilson, A.J.; Saskowski, J.; Barham, W.; Yull, F.; Khabele, D. Thymoquinone enhances cisplatin-response through direct tumor effects in a syngeneic mouse model of ovarian cancer. J. Ovarian Res. 2015, 8, 46. [Google Scholar] [CrossRef]
- Solomon, L.A.; Ali, S.; Banerjee, S.; Munkarah, A.R.; Morris, R.T.; Sarkar, F.H. Sensitization of ovarian cancer cells to cisplatin by genistein: The role of NF-kappaB. J. Ovarian Res. 2008, 1, 9. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Luo, Y.; Qiao, T.; Wu, Z.; Huang, Z. Luteolin sensitizes the antitumor effect of cisplatin in drug-resistant ovarian cancer via induction of apoptosis and inhibition of cell migration and invasion. J. Ovarian Res. 2018, 11, 93. [Google Scholar] [CrossRef]
- Tsuyoshi, H.; Wong, V.K.W.; Han, Y.; Orisaka, M.; Yoshida, Y.; Tsang, B.K. Saikosaponin-d, a calcium mobilizing agent, sensitizes chemoresistant ovarian cancer cells to cisplatin-induced apoptosis by facilitating mitochondrial fission and G2/M arrest. Oncotarget 2017, 8, 99825–99840. [Google Scholar] [CrossRef] [PubMed]
- Huh, H.D.; Kim, S. History of Radiation Therapy Technology. Prog. Med. Phys. 2020, 31, 124–134. [Google Scholar] [CrossRef]
- Baskar, R.; Dai, J.; Wenlong, N.; Yeo, R.; Yeoh, K.-W. Biological response of cancer cells to radiation treatment. Front. Mol. Biosci. 2014, 1, 24. [Google Scholar] [CrossRef] [PubMed]
- Hettinga, J.V.E.; Konings, A.W.T.; Kampinga, H.H. Reduction of cellular cisplatin resistance by hyperthermia—A review. Int. J. Hyperth. 1997, 13, 439–457. [Google Scholar] [CrossRef]
- Farrell, R.; Burling, M. HIPEC: Turning up the heat on ovarian cancer. Aust. N. Z. J. Obstet. Gynaecol. 2021, 61, 11–15. [Google Scholar] [CrossRef]
- Pandey, B.; Shetake, N.G. Hyperthermia therapy of cancer: Need for deeper biological insights for improved therapeutic outcome. J. Radiat. Cancer Res. 2019, 10, 170. [Google Scholar] [CrossRef]
- Miller, E.M.; Samec, T.M.; Alexander-Bryant, A.A. Nanoparticle delivery systems to combat drug resistance in ovarian cancer. Nanomed. Nanotechnol. Biol. Med. 2020, 31, 102309. [Google Scholar] [CrossRef]
- Levy, A.; Leynes, C.; Baig, M.; Chew, S.A. The Application of Biomaterials in the Treatment of Platinum-Resistant Ovarian Cancer. Chemmedchem 2019, 14, 1810–1827. [Google Scholar] [CrossRef]
- ZununiVahed, S.; Salehi, R.; Davaran, S.; Sharifi, S. Liposome-based drug co-delivery systems in cancer cells. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 71, 1327–1341. [Google Scholar] [CrossRef]
- Beloqui, A.; Solinís, M.Á.; Rodríguez-Gascón, A.; Almeida, A.J.; Préat, V. Nanostructured lipid carriers: Promising drug delivery systems for future clinics. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 143–161. [Google Scholar] [CrossRef]
- Dolatabadi, J.E.N.; Valizadeh, H.; Hamishehkar, H. Solid Lipid Nanoparticles as Efficient Drug and Gene Delivery Systems: Recent Breakthroughs. Adv. Pharm. Bull. 2015, 5, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Krieger, M.L.; Eckstein, N.; Schneider, V.; Koch, M.; Royer, H.-D.; Jaehde, U.; Bendas, G. Overcoming cisplatin resistance of ovarian cancer cells by targeted liposomes in vitro. Int. J. Pharm. 2010, 389, 10–17. [Google Scholar] [CrossRef]
- Wang, B.; Wang, S.; Zhang, Q.; Deng, Y.; Li, X.; Peng, L.; Zuo, X.; Piao, M.; Kuang, X.; Sheng, S.; et al. Recent advances in polymer-based drug delivery systems for local anesthetics. Acta Biomater. 2019, 96, 55–67. [Google Scholar] [CrossRef] [PubMed]
- Kamaly, N.; Yameen, B.; Wu, J.; Farokhzad, O.C. Degradable Controlled-Release Polymers and Polymeric Nanoparticles: Mechanisms of Controlling Drug Release. Chem. Rev. 2016, 116, 2602–2663. [Google Scholar] [CrossRef] [PubMed]
- Yellepeddi, V.; Kumar, A.; Maher, D.M.; Chauhan, S.C.; Vangara, K.K.; Palakurthi, S. Biotinylated PAMAM dendrimers for intracellular delivery of cisplatin to ovarian cancer: Role of SMVT. Anticancer. Res. 2011, 31, 897–906. [Google Scholar] [PubMed]
- Gokduman, K. Sensitization of cisplatin-resistant ovarian cancer cells by magnetite iron oxide nanoparticles: An in vitro study. Nanomedicine 2019, 14, 3177–3191. [Google Scholar] [CrossRef]
- Ridwelski, K.; Gebauer, T.; Fahlke, J.; Kröning, H.; Kettner, E.; Meyer, F.; Eichelmann, K.; Lippert, H. Combination chemotherapy with docetaxel and cisplatin for locally advanced and metastatic gastric cancer. Ann. Oncol. 2001, 12, 47–51. [Google Scholar] [CrossRef]
- Lee, Y.J.; Doliny, P.; Gomez-Fernandez, C.; Powell, J.; Reis, I.; Hurley, J. Docetaxel and Cisplatin as Primary Chemotherapy for Treatment of Locally Advanced Breast Cancers. Clin. Breast Cancer 2004, 5, 371–376. [Google Scholar] [CrossRef]
- Gao, X.; Wang, J.; Li, M.; Wang, J.; Lv, J.; Zhang, L.; Sun, C.; Ji, J.; Yang, W.; Zhao, Z.; et al. Berberine attenuates XRCC1-mediated base excision repair and sensitizes breast cancer cells to the chemotherapeutic drugs. J. Cell. Mol. Med. 2019, 23, 6797–6804. [Google Scholar] [CrossRef]
- Kou, Y.; Tong, B.; Wu, W.; Liao, X.; Zhao, M. Berberine Improves Chemo-Sensitivity to Cisplatin by Enhancing Cell Apoptosis and Repressing PI3K/AKT/mTOR Signaling Pathway in Gastric Cancer. Front. Pharmacol. 2020, 11, 616251. [Google Scholar] [CrossRef]
- Peng, S.; Wang, J.; Lu, C.; Xu, Z.; Chai, J.-J.; Ke, Q.; Deng, X.-Z. Emodin enhances cisplatin sensitivity in non-small cell lung cancer through Pgp downregulation. Oncol. Lett. 2021, 21, 230. [Google Scholar] [CrossRef]
- Li, X.; Wang, H.; Wang, J.; Chen, Y.; Yin, X.; Shi, G.; Li, H.; Hu, Z.; Liang, X. Emodin enhances cisplatin-induced cytotoxicity in human bladder cancer cells through ROS elevation and MRP1 downregulation. BMC Cancer 2016, 16, 578. [Google Scholar] [CrossRef]
- Huang, L.; Wang, X.-B.; Yu, Q.-M.; Luo, Q.-Y.; Zhang, Z.-Z. Synergistic cancer growth-inhibitory effect of emodin and low-dose cisplatin on gastric cancer cells In vitro. Trop. J. Pharm. Res. 2015, 14, 1427. [Google Scholar] [CrossRef]
- Ding, N.; Zhang, H.; Su, S.; Ding, Y.; Yu, X.; Tang, Y.; Wang, Q.; Liu, P.; Ding, H.Z.N. Emodin Enhances the Chemosensitivity of Endometrial Cancer by Inhibiting ROS-Mediated Cisplatin-resistance. Anti-Cancer Agents Med. Chem. 2018, 18, 1054–1063. [Google Scholar] [CrossRef] [PubMed]
- Jafri, S.H.; Glass, J.; Shi, R.; Zhang, S.; Prince, M.; Kleiner-Hancock, H. Thymoquinone and cisplatin as a therapeutic combination in lung cancer: In vitro and in vivo. J. Exp. Clin. Cancer Res. 2010, 29, 87. [Google Scholar] [CrossRef]
- Liu, H.; Lee, G.; Lee, J.I.; Ahn, T.-G.; Kim, S.A. Effects of genistein on anti-tumor activity of cisplatin in human cervical cancer cell lines. Obstet. Gynecol. Sci. 2019, 62, 322–328. [Google Scholar] [CrossRef]
- Liu, D.; Yan, L.; Wang, L.; Tai, W.; Wang, W.; Yang, C. Genistein enhances the effect of cisplatin on the inhibition of non-small cell lung cancer A549 cell growth in vitro and in vivo. Oncol. Lett. 2014, 8, 2806–2810. [Google Scholar] [CrossRef]
- Özerkan, D. The Determination of Cisplatin and Luteolin Synergistic Effect on Colorectal Cancer Cell Apoptosis and Mitochondrial Dysfunction by Fluorescence Labelling. J. Fluoresc. 2023. [Google Scholar] [CrossRef]
- Hu, J.; Li, P.; Shi, B.; Tie, J. Effects and Mechanisms of Saikosaponin D Improving the Sensitivity of Human Gastric Cancer Cells to Cisplatin. ACS Omega 2021, 6, 18745–18755. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Zheng, X.-L.; Yang, L.; Shi, F.; Gao, L.-B.; Zhong, Y.-J.; Sun, H.; He, F.; Lin, Y.; Wang, X. Reactive oxygen species-mediated apoptosis contributes to chemosensitization effect of saikosaponins on cisplatin-induced cytotoxicity in cancer cells. J. Exp. Clin. Cancer Res. 2010, 29, 159. [Google Scholar] [CrossRef]
- Itoh, Y.; Yamada, Y.; Kazaoka, Y.; Ishiguchi, T.; Honda, N. Combination of chemotherapy and mild hyperthermia enhances the anti-tumor effects of cisplatin and adriamycin in human bladder cancer T24 cells in vitro. Exp. Ther. Med. 2010, 1, 319–323. [Google Scholar] [CrossRef]
- Sato, I.; Umemura, M.; Mitsudo, K.; Kioi, M.; Nakashima, H.; Iwai, T.; Feng, X.; Oda, K.; Miyajima, A.; Makino, A.; et al. Hyperthermia generated with ferucarbotran (Resovist®) in an alternating magnetic field enhances cisplatin-induced apoptosis of cultured human oral cancer cells. J. Physiol. Sci. 2014, 64, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-Y.; Cheng, M.; Lee, N.-R.; Huang, H.-Y.; Lee, W.-L.; Chang, W.-H.; Wang, P.-H. Comparing Paclitaxel–Carboplatin with Paclitaxel–Cisplatin as the Front-Line Chemotherapy for Patients with FIGO IIIC Serous-Type Tubo-Ovarian Cancer. Int. J. Environ. Res. Public Health 2020, 17, 2213. [Google Scholar] [CrossRef] [PubMed]
- Yu, K.D.; Ye, F.G.; He, M.; Fan, L.; Ma, D.; Mo, M.; Wu, J.; Liu, G.-Y.; Di, G.; Zeng, X.-H.; et al. Effect of Adjuvant Paclitaxel and Carboplatin on Survival in Women With Triple-Negative Breast Cancer: A Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020, 6, 1390–1396. [Google Scholar] [CrossRef]
- Shimada, M.; Kigawa, J.; Itamochi, H. Nedaplatin: A cisplatin derivative in cancer chemotherapy. Cancer Manag. Res. 2013, 5, 67–76. [Google Scholar] [CrossRef]
- Hua, S.; Kong, X.; Chen, B.; Zhuang, W.; Sun, Q.; Yang, W.; Liu, W.; Zhang, S.H.A.Y. Anticancer Mechanism of Lobaplatin as Monotherapy and in Combination with Paclitaxel in Human Gastric Cancer. Curr. Mol. Pharmacol. 2018, 11, 316–325. [Google Scholar] [CrossRef]
- Zhou, N.-N.; Zhao, Y.-Y.; Zhai, L.-Z.; Ruan, C.-M.; Yang, Y.-P.; Huang, Y.; Hou, X.; Chen, L.-K.; Zhou, T.; Zhang, L. The Efficacy and Toxicity of Lobaplatin-contained Chemotherapy in Extensive-stage Small-cell Lung Cancer. J. Cancer 2018, 9, 2232–2236. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zoń, A.; Bednarek, I. Cisplatin in Ovarian Cancer Treatment—Known Limitations in Therapy Force New Solutions. Int. J. Mol. Sci. 2023, 24, 7585. https://doi.org/10.3390/ijms24087585
Zoń A, Bednarek I. Cisplatin in Ovarian Cancer Treatment—Known Limitations in Therapy Force New Solutions. International Journal of Molecular Sciences. 2023; 24(8):7585. https://doi.org/10.3390/ijms24087585
Chicago/Turabian StyleZoń, Aleksandra, and Ilona Bednarek. 2023. "Cisplatin in Ovarian Cancer Treatment—Known Limitations in Therapy Force New Solutions" International Journal of Molecular Sciences 24, no. 8: 7585. https://doi.org/10.3390/ijms24087585
APA StyleZoń, A., & Bednarek, I. (2023). Cisplatin in Ovarian Cancer Treatment—Known Limitations in Therapy Force New Solutions. International Journal of Molecular Sciences, 24(8), 7585. https://doi.org/10.3390/ijms24087585






