Neutrophil-to-Lymphocyte Ratio Is an Independent Risk Factor for Coronary Artery Disease in Central Obesity
Abstract
1. Introduction
2. Results
2.1. Baseline Characteristics by Dichotomized CACS
2.2. Baseline Characteristics by VAI Tertiles
2.3. Association of Neutrophil-to-Lymphocyte Ratio and Coronary Calcium Score across VAI Tertiles
2.4. Independent Determinants of Increased Coronary Artery Calcium Score
3. Discussion
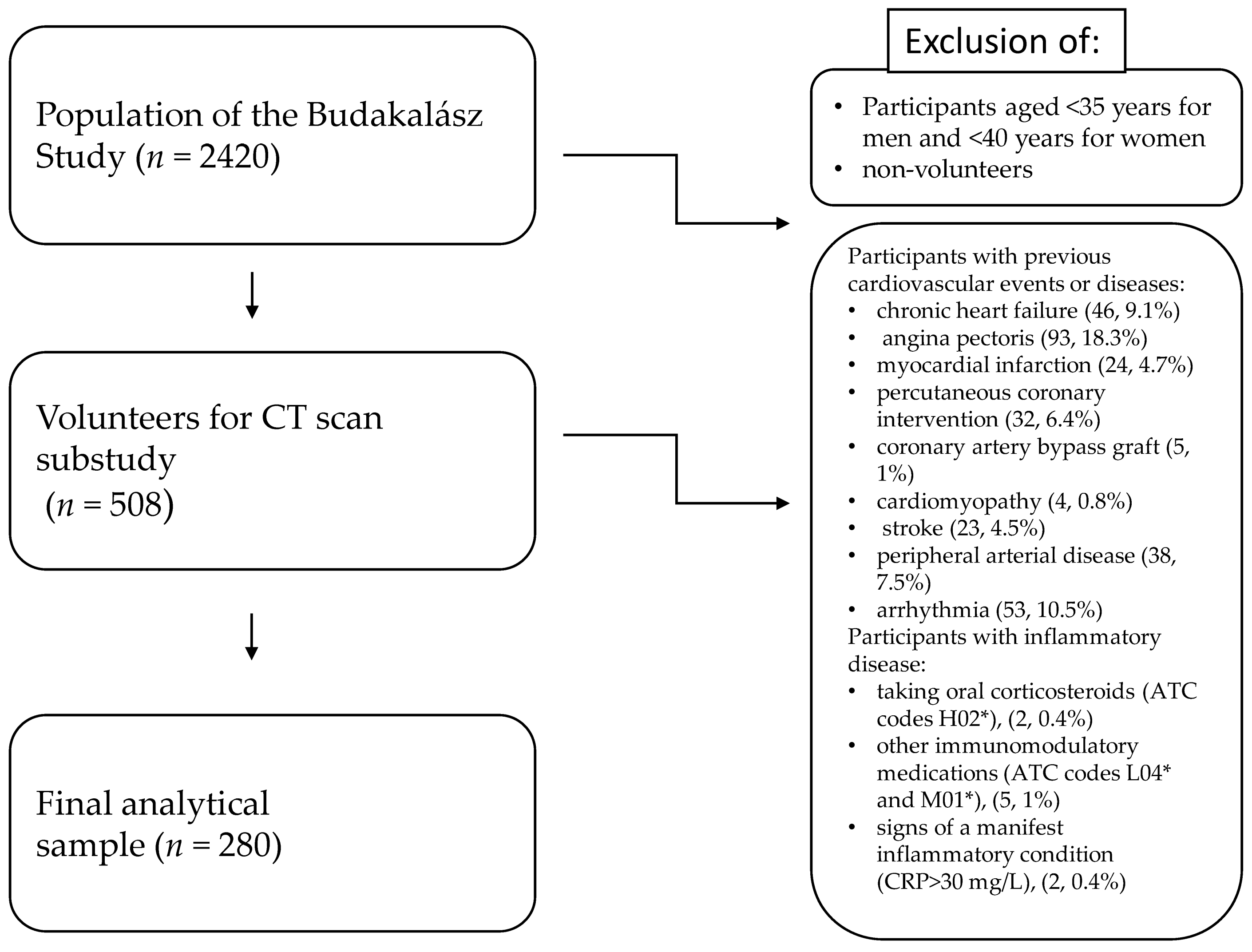
4. Materials and Methods
- Males: VAI = [WC/{39.68 + (1.88 × BMI)}] × (TG/1.03) × (1.31/HDL-C)
- Females: VAI = [WC/{36.58 + (1.89 × BMI)}] × (TG/0.81) × (1.52/HDL-C)
Statistical Methods
5. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Townsend, N.; Nichols, M.; Scarborough, P.; Rayner, M. Cardiovascular disease in Europe—Epidemiological update 2015. Eur. Heart J. 2015, 36, 2696–2705. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.D.; Paisley, R.; Moon, P.; Novak, E.; Villines, T.C. Coronary Artery Calcium and Long-Term Risk of Death, Myocardial Infarction, and Stroke: The Walter Reed Cohort Study. JACC Cardiovasc. Imaging 2018, 11, 1799–1806. [Google Scholar] [CrossRef] [PubMed]
- Rijlaarsdam-Hermsen, D.; Lo-Kioeng-Shioe, M.S.; Kuijpers, D.; van Domburg, R.T.; Deckers, J.W.; van Dijkman, P.R.M. Prognostic value of the coronary artery calcium score in suspected coronary artery disease: Amstudy of 644 symptomatic patients. Neth. Heart J. Mon. J. Neth. Soc. Cardiol. Neth. Heart Found. 2020, 28, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Amato, M.C.; Giordano, C.; Galia, M.; Criscimanna, A.; Vitabile, S.; Midiri, M.; Galluzzo, A. Visceral Adiposity Index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 2010, 33, 920–922. [Google Scholar] [CrossRef]
- Iliodromiti, S.; Celis-Morales, C.A.; Lyall, D.M.; Anderson, J.; Gray, S.R.; Mackay, D.F.; Nelson, S.M.; Welsh, P.; Pell, J.P.; Gill, J.M.R.; et al. The impact of confounding on the associations of different adiposity measures with the incidence of cardiovascular disease: A cohort study of 296 535 adults of white European descent. Eur. Heart J. 2018, 39, 1514–1520. [Google Scholar] [CrossRef]
- Qiao, T.; Luo, T.; Pei, H.; Yimingniyazi, B.; Aili, D.; Aimudula, A.; Zhao, H.; Zhang, H.; Dai, J.; Wang, D. Association between abdominal obesity indices and risk of cardiovascular events in Chinese populations with type 2 diabetes: A prospective cohort study. Cardiovasc. Diabetol. 2022, 21, 225. [Google Scholar] [CrossRef]
- Kouli, G.M.; Panagiotakos, D.B.; Kyrou, I.; Georgousopoulou, E.N.; Chrysohoou, C.; Tsigos, C.; Tousoulis, D.; Pitsavos, C. Visceral adiposity index and 10-year cardiovascular disease incidence: The ATTICA study. Nutr. Metab. Cardiovasc. Dis. NMCD 2017, 27, 881–889. [Google Scholar] [CrossRef]
- Bagyura, Z.; Kiss, L.; Lux, Á.; Csobay-Novák, C.; Jermendy, Á.L.; Polgár, L.; Szelid, Z.; Soós, P.; Merkely, B. Association between coronary atherosclerosis and visceral adiposity index. Nutr. Metab. Cardiovasc. Dis. NMCD 2020, 30, 796–803. [Google Scholar] [CrossRef]
- Maréchal, P.; Tridetti, J.; Nguyen, M.L.; Wéra, O.; Jiang, Z.; Gustin, M.; Donneau, A.F.; Oury, C.; Lancellotti, P. Neutrophil Phenotypes in Coronary Artery Disease. J. Clin. Med. 2020, 9, 1602. [Google Scholar] [CrossRef]
- Cooper, H.A.; Exner, D.V.; Waclawiw, M.A.; Domanski, M.J. White blood cell count and mortality in patients with ischemic and nonischemic left ventricular systolic dysfunction (an analysis of the Studies Of Left Ventricular Dysfunction [SOLVD]). Am. J. Cardiol. 1999, 84, 252–257. [Google Scholar] [CrossRef]
- Warny, M.; Helby, J.; Nordestgaard, B.G.; Birgens, H.; Bojesen, S.E. Incidental lymphopenia and mortality: A prospective cohort study. CMAJ Can. Med. Assoc. J. = J. De L’association Med. Can. 2020, 192, E25–E33. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rodríguez, E.; López-Sobaler, A.M.; Ortega, R.M.; Delgado-Losada, M.L.; López-Parra, A.M.; Aparicio, A. Association between Neutrophil-to-Lymphocyte Ratio with Abdominal Obesity and Healthy Eating Index in a Representative Older Spanish Population. Nutrients 2020, 12, 855. [Google Scholar] [CrossRef]
- Karakaya, S.; Altay, M.; Kaplan Efe, F.; Karadağ, İ.; Ünsal, O.; Bulur, O.; Eser, M.; Taner Ertuğrul, D. The neutrophil-lymphocyte ratio and its relationship with insulin resistance in obesity. Turk. J. Med. Sci. 2019, 49, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Angkananard, T.; Anothaisintawee, T.; McEvoy, M.; Attia, J.; Thakkinstian, A. Neutrophil Lymphocyte Ratio and Cardiovascular Disease Risk: A Systematic Review and Meta-Analysis. BioMed Res. Int. 2018, 2018, 2703518. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Hou, M.; Ding, Z.; Liu, X.; Shao, Y.; Li, X. Prognostic Value of Neutrophil-to-Lymphocyte Ratio in Stroke: A Systematic Review and Meta-Analysis. Front. Neurol. 2021, 12, 686983. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, J.; Cao, D.; Han, L. Correlation of neutrophil-to-lymphocyte ratio with the prognosis of non-ST-segment elevation in patients with acute coronary syndrome undergoing selective percutaneous coronary intervention. J. Int. Med. Res. 2020, 48, 300060520959510. [Google Scholar] [CrossRef]
- Dentali, F.; Nigro, O.; Squizzato, A.; Gianni, M.; Zuretti, F.; Grandi, A.M.; Guasti, L. Impact of neutrophils to lymphocytes ratio on major clinical outcomes in patients with acute coronary syndromes: A systematic review and meta-analysis of the literature. Int. J. Cardiol. 2018, 266, 31–37. [Google Scholar] [CrossRef]
- Del Turco, S.; Bastiani, L.; Minichilli, F.; Landi, P.; Basta, G.; Pingitore, A.; Vassalle, C. Interaction of Uric Acid and Neutrophil-to-Lymphocyte Ratio for Cardiometabolic Risk Stratification and Prognosis in Coronary Artery Disease Patients. Antioxidants 2022, 11, 2163. [Google Scholar] [CrossRef]
- Dziedzic, E.A.; Gąsior, J.S.; Tuzimek, A.; Dąbrowski, M.; Jankowski, P. Neutrophil-to-Lymphocyte Ratio Is Not Associated with Severity of Coronary Artery Disease and Is Not Correlated with Vitamin D Level in Patients with a History of an Acute Coronary Syndrome. Biology 2022, 11, 1001. [Google Scholar] [CrossRef]
- Taurino, M.; Aloisi, F.; Del Porto, F.; Nespola, M.; Dezi, T.; Pranteda, C.; Rizzo, L.; Sirignano, P. Neutrophil-to-Lymphocyte Ratio Could Predict Outcome in Patients Presenting with Acute Limb Ischemia. J. Clin. Med. 2021, 10, 4343. [Google Scholar] [CrossRef]
- Spark, J.I.; Sarveswaran, J.; Blest, N.; Charalabidis, P.; Asthana, S. An elevated neutrophil-lymphocyte ratio independently predicts mortality in chronic critical limb ischemia. J. Vasc. Surg. 2010, 52, 632–636. [Google Scholar] [CrossRef]
- Pasqui, E.; de Donato, G.; Lazzeri, E.; Molino, C.; Galzerano, G.; Giubbolini, M.; Palasciano, G. High Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios Are Associated with a Higher Risk of Hemodialysis Vascular Access Failure. Biomedicines 2022, 10, 2218. [Google Scholar] [CrossRef] [PubMed]
- Suárez-Cuenca, J.A.; Ruíz-Hernández, A.S.; Mendoza-Castañeda, A.A.; Domínguez-Pérez, G.A.; Hernández-Patricio, A.; Vera-Gómez, E.; De la Peña-Sosa, G.; Banderas-Lares, D.Z.; Montoya-Ramírez, J.; Blas-Azotla, R.; et al. Neutrophil-to-lymphocyte ratio and its relation with pro-inflammatory mediators, visceral adiposity and carotid intima-media thickness in population with obesity. Eur. J. Clin. Investig. 2019, 49, e13085. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Lai, X.; Yan, C.; Jia, X.; Li, Y. The associations between neutrophil-to-lymphocyte ratio and the Chinese Visceral Adiposity Index, and carotid atherosclerosis and atherosclerotic cardiovascular disease risk. Exp. Gerontol. 2020, 139, 111019. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Gu, C.; Wang, F.; Lv, B.; Zhang, C.; Peng, R.; Cong, X.; Chen, X. Association of Neutrophil-Lymphocyte Ratio and the Presence of Noncalcified or Mixed Coronary Atherosclerotic Plaques. Angiology 2018, 69, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Nam, S.H.; Kang, S.G.; Song, S.W. The Neutrophil-Lymphocyte Ratio Is Associated with Coronary Artery Calcification in Asymptomatic Korean Males: A Cross-Sectional Study. BioMed Res. Int. 2017, 2017, 1989417. [Google Scholar] [CrossRef] [PubMed]
- Serrano, C.V., Jr.; de Mattos, F.R.; Pitta, F.G.; Nomura, C.H.; de Lemos, J.; Ramires, J.A.F.; Kalil-Filho, R. Association between Neutrophil-Lymphocyte and Platelet-Lymphocyte Ratios and Coronary Artery Calcification Score among Asymptomatic Patients: Data from a Cross-Sectional Study. Mediat. Inflamm. 2019, 2019, 6513847. [Google Scholar] [CrossRef]
- Nicoll, R.; Wiklund, U.; Zhao, Y.; Diederichsen, A.; Mickley, H.; Ovrehus, K.; Zamorano, J.; Gueret, P.; Schmermund, A.; Maffei, E.; et al. Gender and age effects on risk factor-based prediction of coronary artery calcium in symptomatic patients: A Euro-CCAD study. Atherosclerosis 2016, 252, 32–39. [Google Scholar] [CrossRef]
- Kiss, L.Z.; Bagyura, Z.; Csobay-Novák, C.; Lux, Á.; Polgár, L.; Jermendy, Á.; Soós, P.; Szelid, Z.; Maurovich-Horvat, P.; Becker, D.; et al. Serum Uric Acid Is Independently Associated with Coronary Calcification in an Asymptomatic Population. J. Cardiovasc. Transl. Res. 2019, 12, 204–210. [Google Scholar] [CrossRef]
- Rohm, T.V.; Meier, D.T.; Olefsky, J.M.; Donath, M.Y. Inflammation in obesity, diabetes, and related disorders. Immunity 2022, 55, 31–55. [Google Scholar] [CrossRef]
- Zhu, Y.; Li, G.; Laukkanen, J.A.; Song, X.; Zhang, J.; Wei, L.; Chen, X.; Li, Y.; Liu, C. Higher neutrophil to lymphocyte ratio is associated with renal dysfunction and cardiac adverse remodeling in elderly with metabolic syndrome. Front. Cardiovasc. Med. 2022, 9, 921204. [Google Scholar] [CrossRef] [PubMed]
- Hashemi Moghanjoughi, P.; Neshat, S.; Rezaei, A.; Heshmat-Ghahdarijani, K. Is the Neutrophil-to-Lymphocyte Ratio an Exceptional Indicator for Metabolic Syndrome Disease and Outcomes? Endocr. Pract. 2022, 28, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, S.; Fujita, T.; Shimabukuro, M.; Iwaki, M.; Yamada, Y.; Nakajima, Y.; Nakayama, O.; Makishima, M.; Matsuda, M.; Shimomura, I. Increased oxidative stress in obesity and its impact on metabolic syndrome. J. Clin. Investig. 2004, 114, 1752–1761. [Google Scholar] [CrossRef] [PubMed]
- Osaka, M.; Deushi, M.; Aoyama, J.; Funakoshi, T.; Ishigami, A.; Yoshida, M. High-Fat Diet Enhances Neutrophil Adhesion in LDLR-Null Mice Via Hypercitrullination of Histone H3. JACC Basic Transl. Sci. 2021, 6, 507–523. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.S.; Brownlee, M. Molecular and Cellular Mechanisms of Cardiovascular Disorders in Diabetes. Circ. Res. 2016, 118, 1808–1829. [Google Scholar] [CrossRef]
- Flynn, M.C.; Kraakman, M.J.; Tikellis, C.; Lee, M.K.S.; Hanssen, N.M.J.; Kammoun, H.L.; Pickering, R.J.; Dragoljevic, D.; Al-Sharea, A.; Barrett, T.J.; et al. Transient Intermittent Hyperglycemia Accelerates Atherosclerosis by Promoting Myelopoiesis. Circ. Res. 2020, 127, 877–892. [Google Scholar] [CrossRef]
- Vallejo, J.; Cochain, C.; Zernecke, A.; Ley, K. Heterogeneity of immune cells in human atherosclerosis revealed by scRNA-Seq. Cardiovasc. Res. 2021, 117, 2537–2543. [Google Scholar] [CrossRef]
- Mauersberger, C.; Hinterdobler, J.; Schunkert, H.; Kessler, T.; Sager, H.B. Where the Action Is-Leukocyte Recruitment in Atherosclerosis. Front. Cardiovasc. Med. 2021, 8, 813984. [Google Scholar] [CrossRef]
- Silvestre-Roig, C.; Braster, Q.; Ortega-Gomez, A.; Soehnlein, O. Neutrophils as regulators of cardiovascular inflammation. Nat. Rev. Cardiol. 2020, 17, 327–340. [Google Scholar] [CrossRef]
- Akers, E.J.; Nicholls, S.J.; Bartolo, B.A.D. Plaque Calcification. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 1902–1910. [Google Scholar] [CrossRef]
- Jinnouchi, H.; Sato, Y.; Sakamoto, A.; Cornelissen, A.; Mori, M.; Kawakami, R.; Gadhoke, N.V.; Kolodgie, F.D.; Virmani, R.; Finn, A.V. Calcium deposition within coronary atherosclerotic lesion: Implications for plaque stability. Atherosclerosis 2020, 306, 85–95. [Google Scholar] [CrossRef] [PubMed]
- Balmos, I.A.; Horváth, E.; Brinzaniuc, K.; Muresan, A.V.; Olah, P.; Molnár, G.B.; Nagy, E.E. Inflammation, Microcalcification, and Increased Expression of Osteopontin Are Histological Hallmarks of Plaque Vulnerability in Patients with Advanced Carotid Artery Stenosis. Biomedicines 2023, 11, 881. [Google Scholar] [CrossRef] [PubMed]
- Bagyura, Z.; Kiss, L.; Edes, E.; Lux, A.; Polgár, L.; Soós, P.; Szenczi, O.; Szelid, Z.; Vadas, R.; Józan, P.; et al. Cardiovascular screening programme in the Central Hungarian region. The Budakalász Study. Orv. Hetil. 2014, 155, 1344–1352. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, e1082–e1143. [Google Scholar] [CrossRef] [PubMed]
- Buonacera, A.; Stancanelli, B.; Colaci, M.; Malatino, L. Neutrophil to Lymphocyte Ratio: An Emerging Marker of the Relationships between the Immune System and Diseases. Int. J. Mol. Sci. 2022, 23, 3636. [Google Scholar] [CrossRef]
| Demographics and Risk Factors (n (%)/Mean (SD)) | CACS ≤ 100 (201) | CACS > 100 (79) | p |
|---|---|---|---|
| BMI, mean (SD) | 27.6 (4.8) | 29.2 (5.29) | 0.02 |
| hsCRP, mean (SD) | 2.63 (3.05) | 2.89 (3.68) | NS |
| HbA1c, mean (SD) | 5.75 (0.55) | 6.17 (1.1) | 0.01 |
| age, mean (SD) | 57.4 (10.6) | 67 (7.6) | <0.001 |
| NLR, mean (SD) | 1.88 (0.71) | 2.19 (0.88) | 0.008 |
| smoking, n (%) | 24 (11.9) | 10 (12.7) | NS |
| HT, n (%) | 86 (42.8) | 64 (81.0) | <0.001 |
| HLP, n % | 74 (36.8) | 38 (48.1) | NS |
| DM, n % | 11 (5.5) | 22 (27.8) | <0.001 |
| Sex, n % | 77 (38.3) | 45 (57.0) | 0.005 |
| Demographics and Risk Factors (n (%)/Mean (SD) | Total Population | VAI 1st Tertile | VAI 2nd Tertile | VAI 3rd Tertile | p |
|---|---|---|---|---|---|
| n (%) | 280 (100) | 93 | 94 | 93 | NS |
| Male, n (%) | 122 (43.6) | 41 (42.7) | 42 (43.3) | 41 (42.7) | NS |
| VAI mean (SD) | 1.73 (0.32) | 1.72 (0.3) | 1.87 (0.3) | 1.9 (0.35) | <0.001 |
| HLP, n (%) | 112 (40.8) | 33 (35.5) | 39 (41.5) | 40 (43.0) | NS |
| HT, n (%) | 150 (53.6) | 41 (44.1) | 54 (57.4) | 55 (59.1) | NS |
| DM, n (%) | 33 (11.8) | 6 (6.5) | 7 (7.4) | 20 (21.5) | 0.002 |
| Smoking, n (%) | 34 (12.1) | 17 (18.3) | 7 (7.4) | 10 (10.8) | NS |
| Age, years, mean (SD) | 60.3 (10.7) | 56.8 (11.0) | 61.6 (10.5) | 62.1 (10.1) | 0.001 |
| BMI, (kg/m2), mean (SD) | 28.1 (5.0) | 27.5 (5.3) | 29.0 (4.3) | 27.7 (5.2) | NS |
| NLR, mean (SD) | 1.97 (0.77) | 1.88 (0.66) | 1.9 (0.71) | 2.14 (0.91) | 0.042 |
| HbA1c, %, mean (SD) | 5.87 (0.78) | 5.72 (0.58) | 5.84 (0.65) | 6.04 (1.01) | 0.02 |
| hsCRP, mmol/L, mean (SD) | 2.71 (3.24) | 2.43 (3.26) | 2.65 (2.8) | 3.05 (3.6) | NS |
| CACS > 100, n (%) | 79 (28.2) | 17 (18.3) | 26 (27.7) | 36 (38.7) | 0.008 |
| CACS, mean (SD) | 174 (448) | 98.5 (221) | 188.1 (469) | 236 (572) | NS |
| NLR-Mean | Low Risk (CACS ≤ 100) | Moderate to High Risk (CACS > 100) | p |
|---|---|---|---|
| VAI 1st tertile | 1.86 (0.67) | 1.94 (0.59) | NS |
| VAI 2nd tertile | 1.89 (0.73) | 1.94 (0.66) | NS |
| VAI 3rd tertile | 1.89 (0.74) | 2.48 (1.1) | 0.008 |
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Male | 2.70 | 1.48–4.93 | 0.00 | 2.61 | 1.4–4.85 | 0.00 | 2.42 | 1.29–4.53 | 0.01 | 2.08 | 1.06–4.07 | 0.03 | 2.05 | 1.03–4.08 | 0.04 |
| Age | 1.13 | 1.08–5.03 | <0.001 | 1.12 | 1.08–1.16 | <0.001 | 1.13 | 1.08–1.17 | <0.001 | 1.11 | 1.06–1.17 | <0.001 | 1.11 | 1.06–1.16 | <0.001 |
| VAI tertile 1 by NLR | 0.99 | 0.60–1.59 | NS | 1.06 | 0.65–1.72 | 0.03 | 1.09 | 0.67–1.72 | NS | 1.16 | 0.7–1.92 | NS | |||
| VAI tertile 2 by NLR | 1.09 | 0.687–1.75 | NS | 1.13 | 0.71–1.82 | NS | 1.13 | 0.69–1.86 | NS | 1.21 | 0.73–1.99 | NS | |||
| VAI tertile 3 by NLR | 1.45 | 0.97–2.18 | 0.07 | 1.56 | 1.02–2.4 | 0.04 | 1.52 | 1–2.34 | 0.05 | 1.67 | 1.06–2.62 | 0.03 | |||
| Current smoking | 2.18 | 0.82–5.7 | NS | 3.20 | 1.2–10.45 | 0.02 | 3.97 | 1.34–11.7 | 0.02 | ||||||
| BMI (kg/m2) | 1.08 | 1–1.15 | 0.02 | 1.04 | 0.97–1.1 | NS | 1.05 | 0.97–1.14 | NS | ||||||
| HLP | 1.62 | 0.83–3.15 | NS | 1.50 | 0.79–3.3 | NS | |||||||||
| HT | 3.14 | 1.4–6.87 | 0.01 | 3.14 | 1.43–6.91 | <0.01 | |||||||||
| DM | 2.25 | 0.85–5.95 | NS | 1.69 | 1.73–4.93 | NS | |||||||||
| HbA1c (%) | 1.28 | 0.81–2.04 | NS | ||||||||||||
| hsCRP (mg/L) | 0.93 | 0.82–1.05 | NS | ||||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bagyura, Z.; Kiss, L.; Lux, Á.; Csobay-Novák, C.; Jermendy, Á.L.; Polgár, L.; Tabák, Á.G.; Soós, P.; Szelid, Z.; Merkely, B.; et al. Neutrophil-to-Lymphocyte Ratio Is an Independent Risk Factor for Coronary Artery Disease in Central Obesity. Int. J. Mol. Sci. 2023, 24, 7397. https://doi.org/10.3390/ijms24087397
Bagyura Z, Kiss L, Lux Á, Csobay-Novák C, Jermendy ÁL, Polgár L, Tabák ÁG, Soós P, Szelid Z, Merkely B, et al. Neutrophil-to-Lymphocyte Ratio Is an Independent Risk Factor for Coronary Artery Disease in Central Obesity. International Journal of Molecular Sciences. 2023; 24(8):7397. https://doi.org/10.3390/ijms24087397
Chicago/Turabian StyleBagyura, Zsolt, Loretta Kiss, Árpád Lux, Csaba Csobay-Novák, Ádám L. Jermendy, Lívia Polgár, Ádám G. Tabák, Pál Soós, Zsolt Szelid, Béla Merkely, and et al. 2023. "Neutrophil-to-Lymphocyte Ratio Is an Independent Risk Factor for Coronary Artery Disease in Central Obesity" International Journal of Molecular Sciences 24, no. 8: 7397. https://doi.org/10.3390/ijms24087397
APA StyleBagyura, Z., Kiss, L., Lux, Á., Csobay-Novák, C., Jermendy, Á. L., Polgár, L., Tabák, Á. G., Soós, P., Szelid, Z., Merkely, B., Kőhidai, L., & Pállinger, É. (2023). Neutrophil-to-Lymphocyte Ratio Is an Independent Risk Factor for Coronary Artery Disease in Central Obesity. International Journal of Molecular Sciences, 24(8), 7397. https://doi.org/10.3390/ijms24087397







