Development of New Targeted Nanotherapy Combined with Magneto-Fluorescent Nanoparticles against Colorectal Cancer
Abstract
1. Introduction
2. Results and Discussion
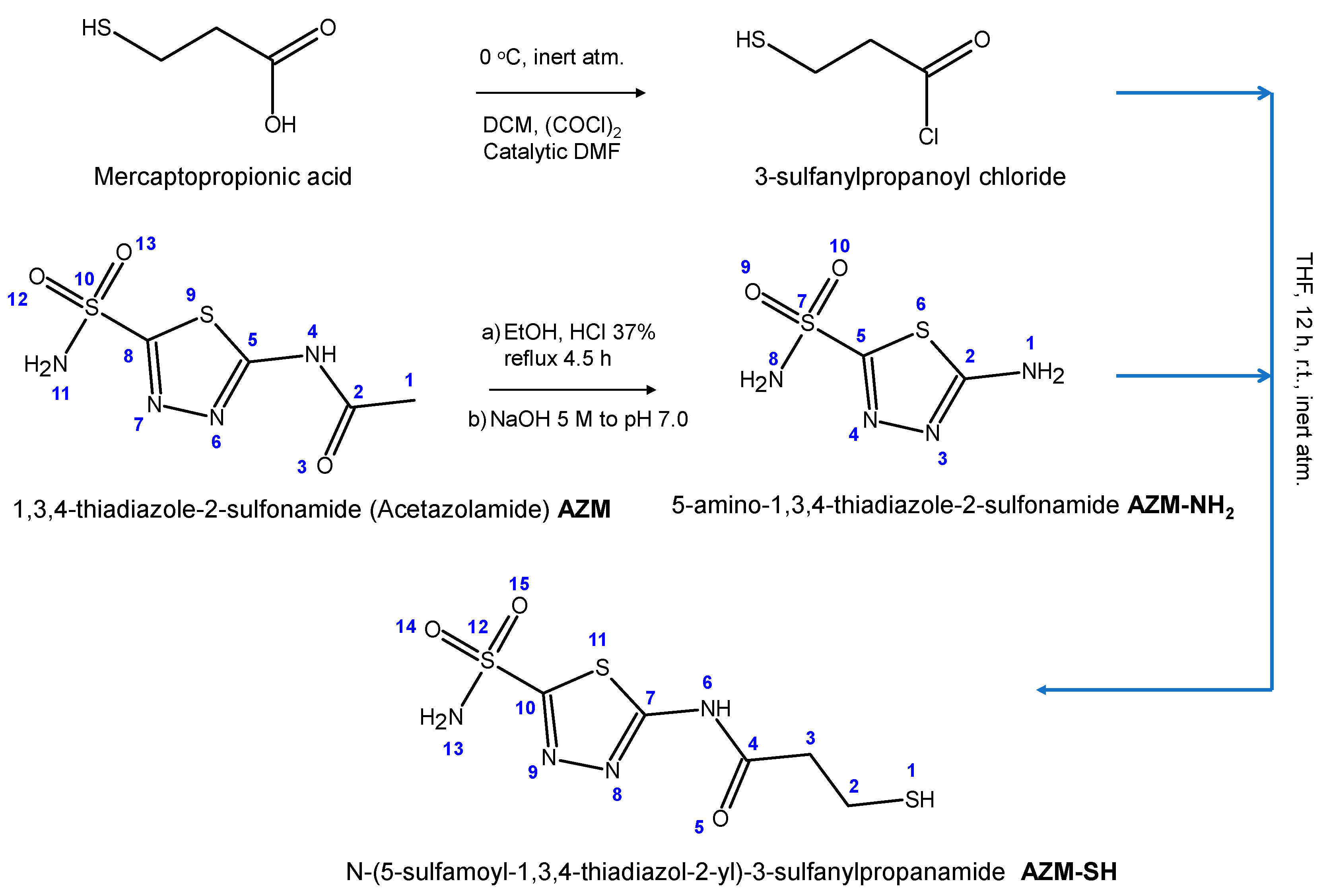
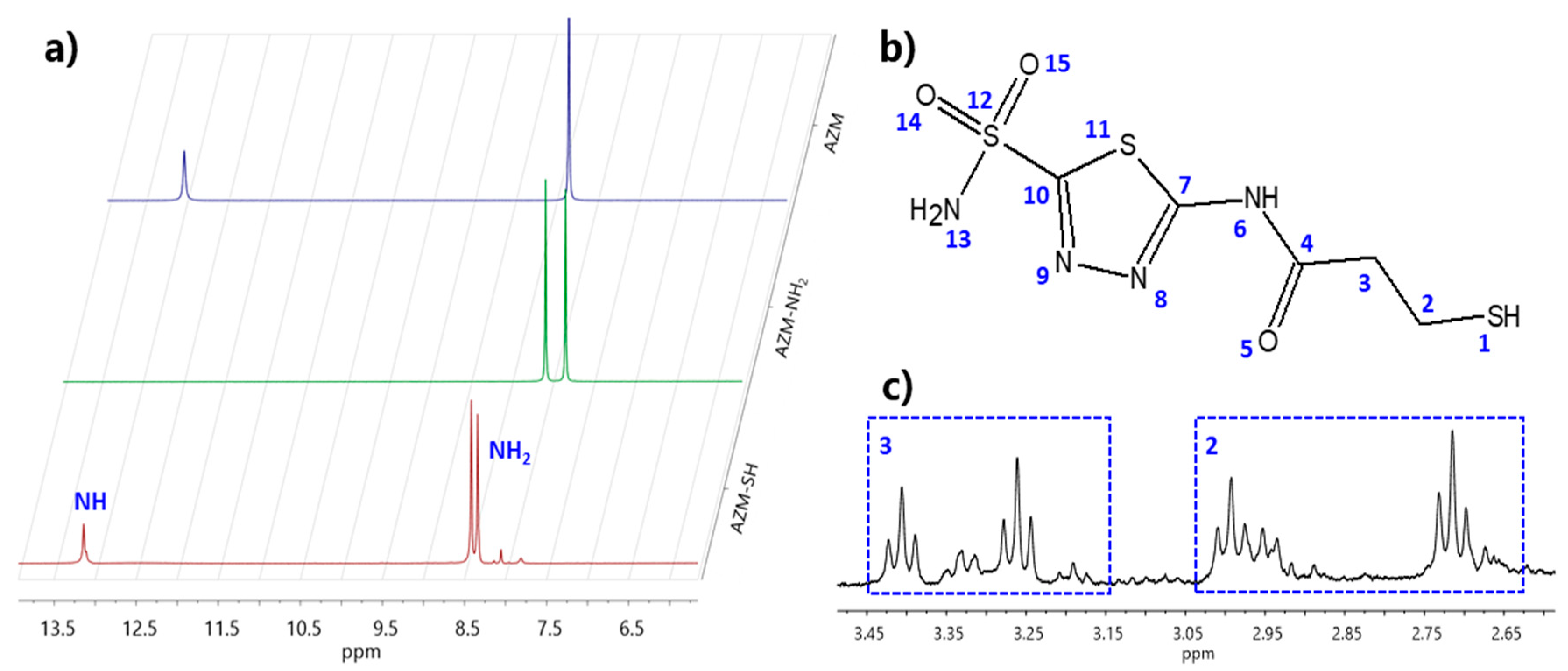
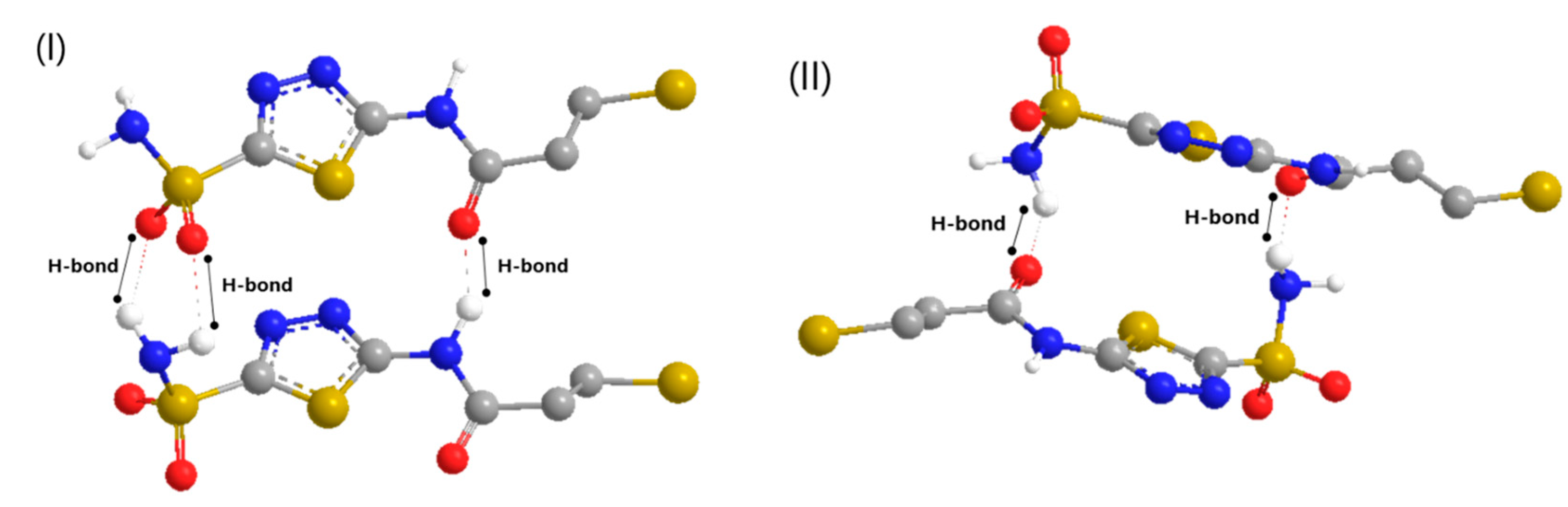
2.1. Synthesis of AZM-SH and Anti-CAIX Action
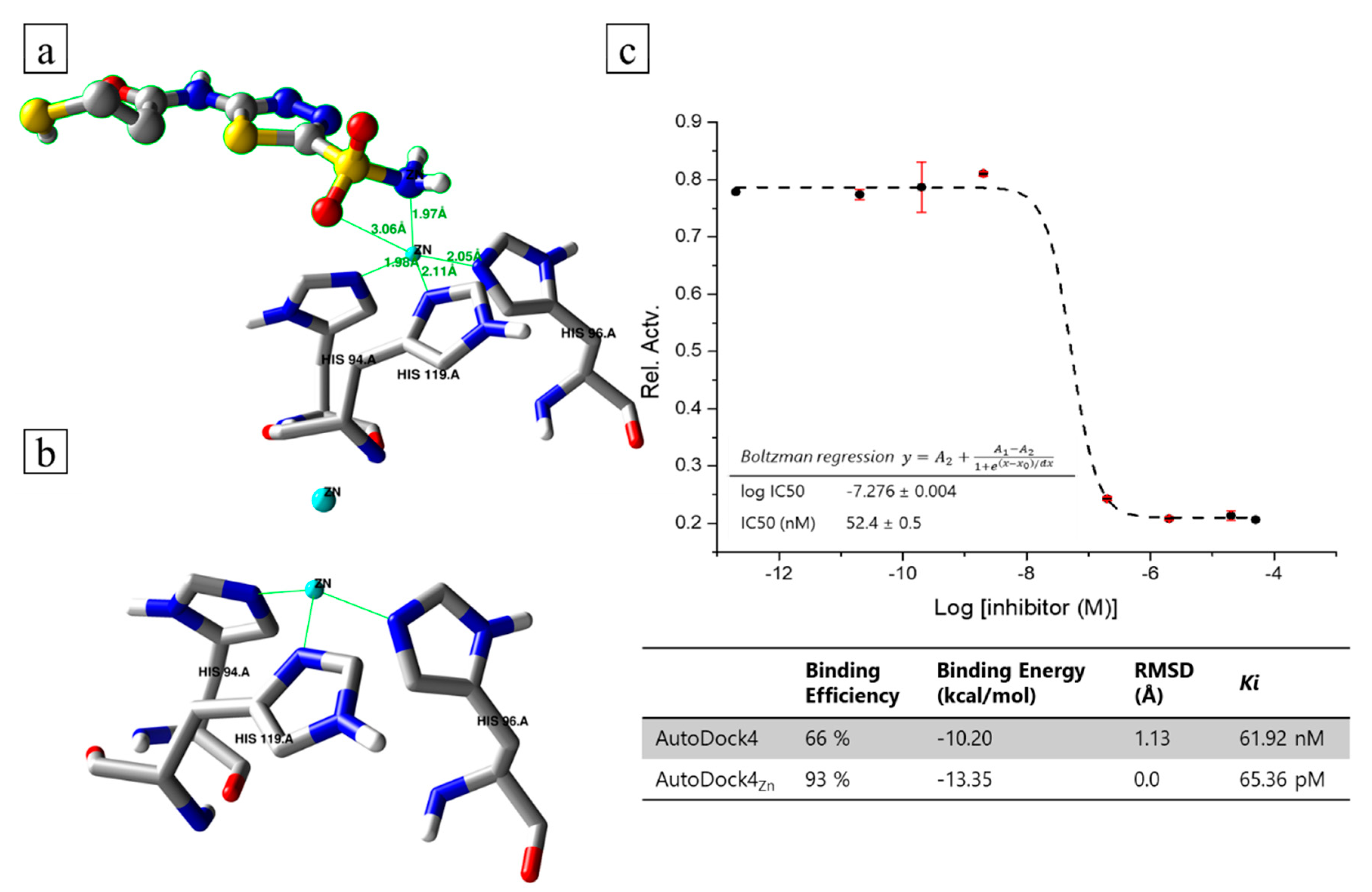
2.2. Docking Modelling and In Vitro Inhibition Studies
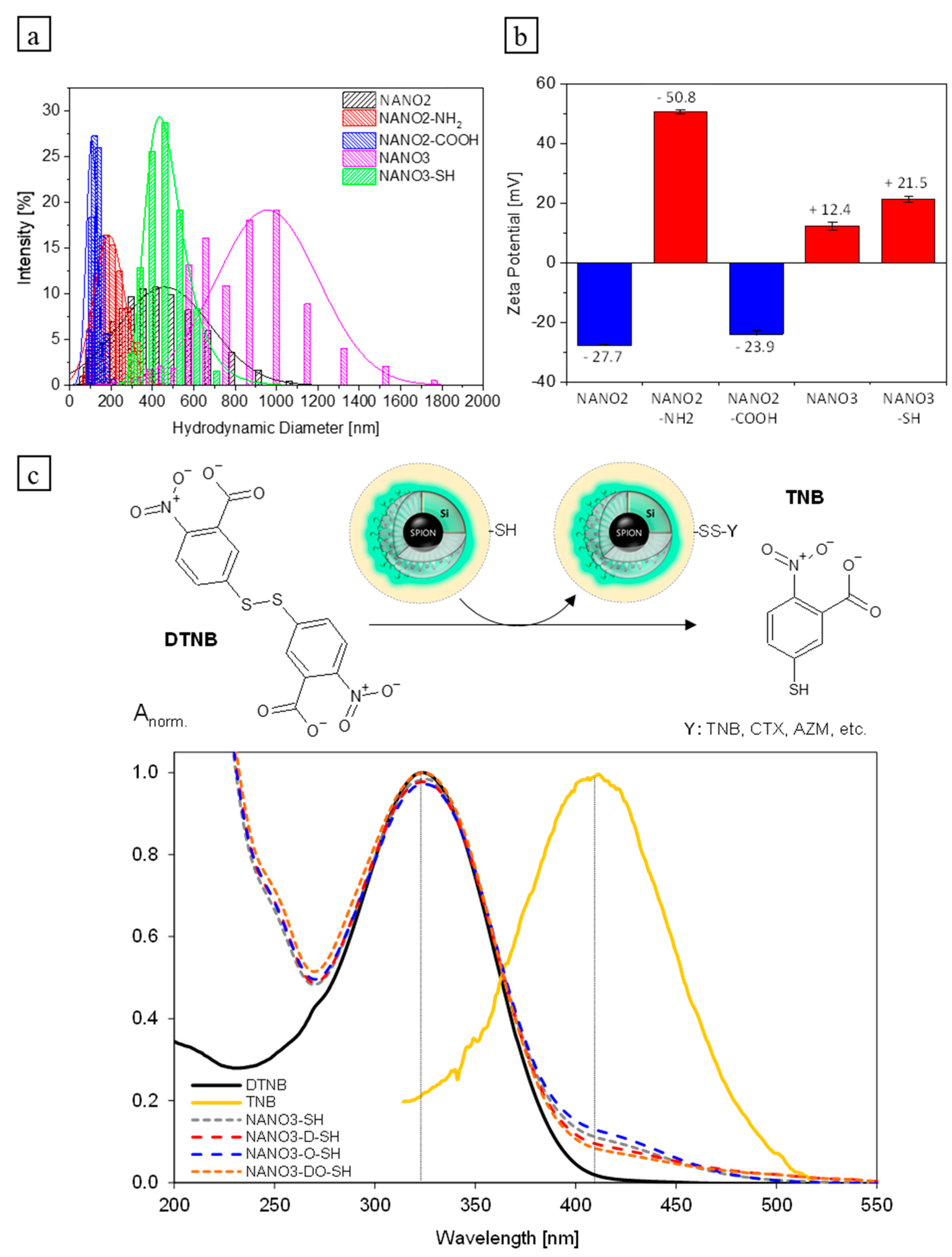
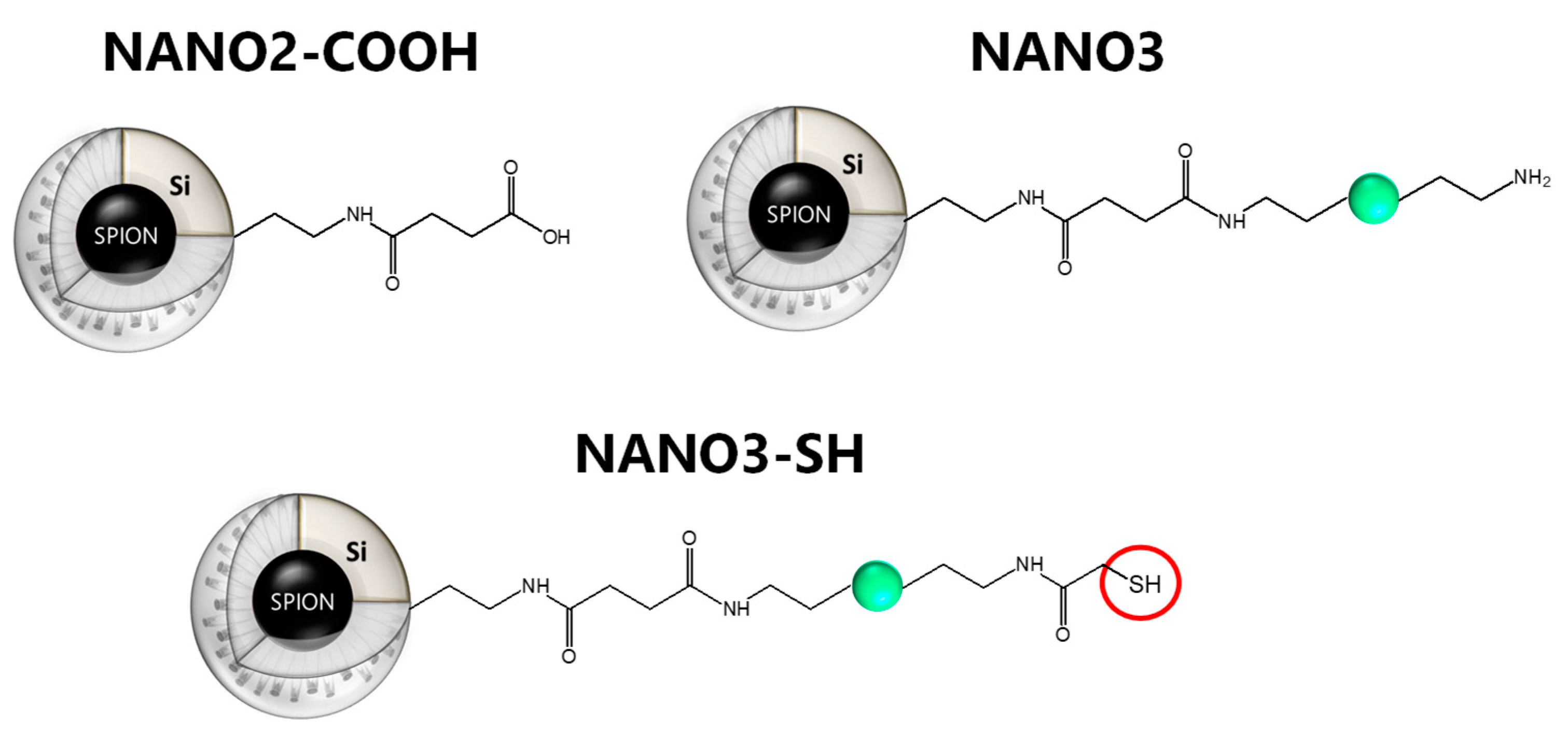
2.3. NANO3-SH Characterization
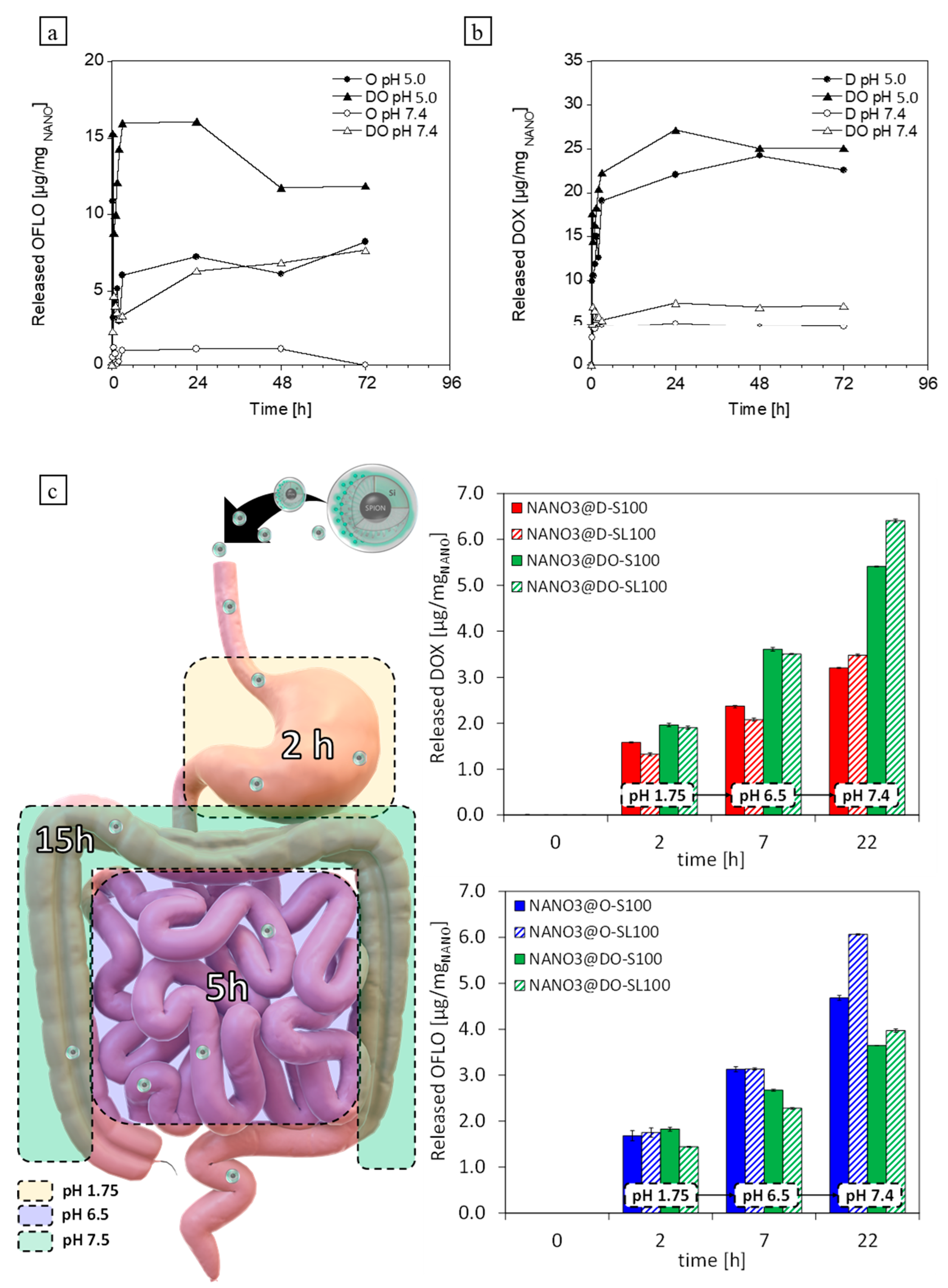
2.4. Loading and Release Assays. Proof of Concept: Enteric Coatings and Gastric Simulated Release
2.5. Biofunctionalization
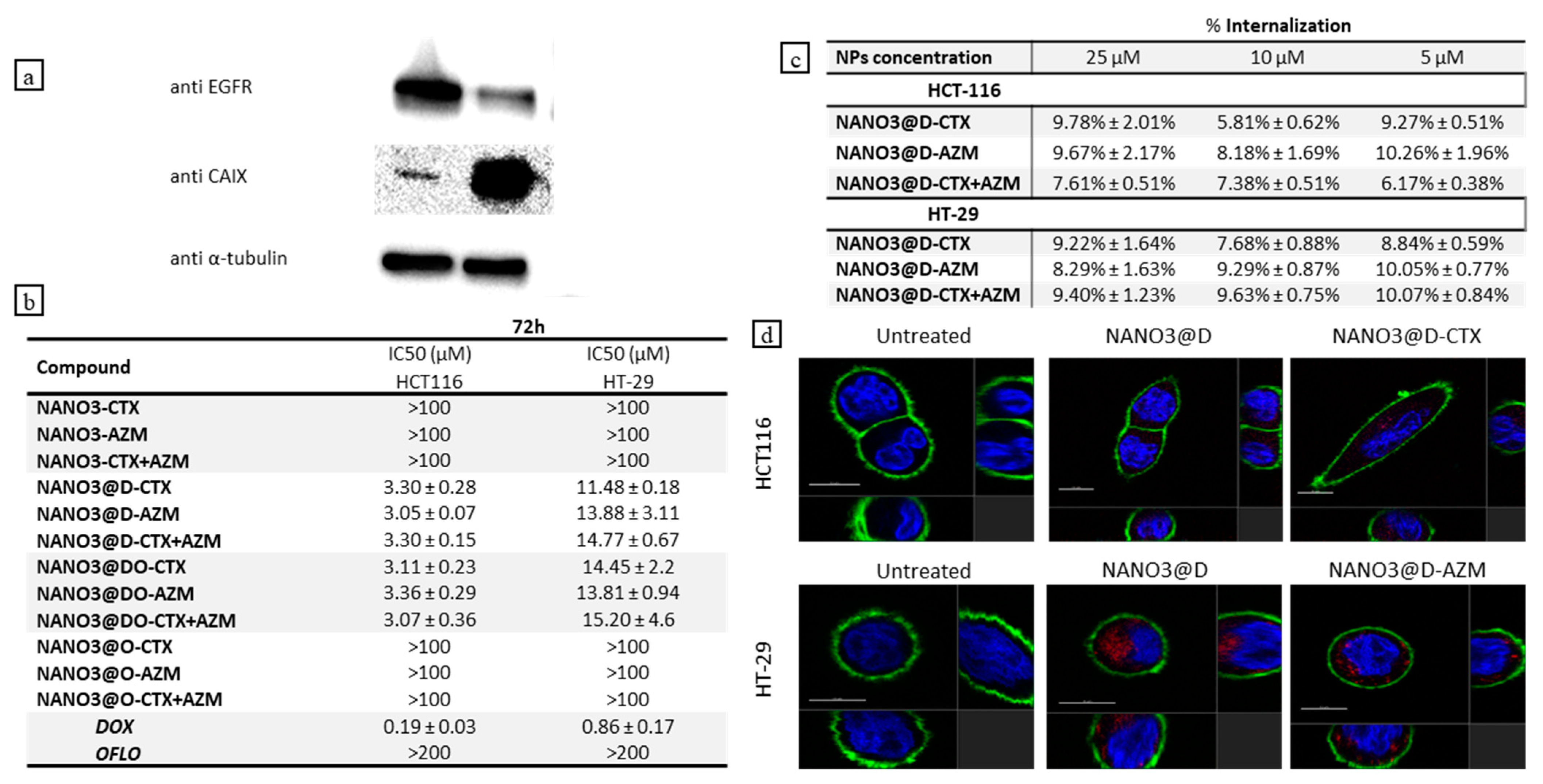
2.6. Cytotoxicity, Antitumor Activity, Cellular Uptake, and Targetability
3. Materials and Methods
3.1. Chemicals
3.2. Instrumentation
3.3. Synthesis and Characterization
3.3.1. N-(5-Sulfamoyl-1,3,4-thiadiazol-2-yl)-3-sulfanylpropanamide (AZM-SH) Synthesis
3.3.2. Synthesis of NANO3-SH
3.4. Modelling Studies and Molecular Docking Simulations
3.5. CA In Vitro Inhibition Assay
3.6. NANO3 Biofunctionalization with CTX-SH and AZM-SH
3.7. Drug Loading and Release Assays
3.8. Enteric Coatings and Simulated Digestive Track Release
3.9. CA-IX and EGFR Expression in CRC Cell Lines
3.10. Cytotoxicity and Cellular Uptake
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xi, Y.; Xu, P. Global Colorectal Cancer Burden in 2020 and Projections to 2040. Transl. Oncol. 2021, 14, 101174. [Google Scholar] [CrossRef] [PubMed]
- Read, B.; Sylla, P. Aggressive Colorectal Cancer in the Young. Clin. Colon Rectal Surg. 2020, 33, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Van der Jeught, K.; Xu, H.C.; Li, Y.J.; Lu, X.B.; Ji, G. Drug Resistance and New Therapies in Colorectal Cancer. World J. Gastroenterol. 2018, 24, 3834–3848. [Google Scholar] [CrossRef] [PubMed]
- Keum, N.N.; Giovannucci, E. Global Burden of Colorectal Cancer: Emerging Trends, Risk Factors and Prevention Strategies. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 713–732. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Goyal, A.K.; Rath, G. Recent Advances in Metal Nanoparticles in Cancer Therapy. J. Drug Target. 2018, 26, 617–632. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.J.; Zhang, W.C.; Guo, Y.W.; Chen, X.Y.; Zhang, Y.N. Metal Nanoparticles as a Promising Technology in Targeted Cancer Treatment. Drug Deliv. 2022, 29, 664–678. [Google Scholar] [CrossRef]
- Gao, L.; Yu, J.; Liu, Y.; Zhou, J.; Sun, L.; Wang, J.; Zhu, J.; Peng, H.; Lu, W.; Yu, L.; et al. Tumor-Penetrating Peptide Conjugated and Doxorubicin Loaded T1-T2 Dual Mode MRI Contrast Agents Nanoparticles for Tumor Theranostics. Theranostics 2018, 8, 92–108. [Google Scholar] [CrossRef]
- Marcelo, G.A.; Montpeyo, D.; Novio, F.; Ruiz-Molina, D.; Lorenzo, J.; Oliveira, E. Luminescent Silicon-Based Nanocarrier for Drug Delivery in Colorectal Cancer Cells. Dye. Pigment. 2020, 181, 108393. [Google Scholar] [CrossRef]
- Păduraru, D.N.; Ion, D.; Niculescu, A.G.; Mușat, F.; Andronic, O.; Grumezescu, A.M.; Bolocan, A. Recent Developments in Metallic Nanomaterials for Cancer Therapy, Diagnosing and Imaging Applications. Pharmaceutics 2022, 14, 435. [Google Scholar] [CrossRef]
- Brar, B.; Ranjan, K.; Palria, A.; Kumar, R.; Ghosh, M.; Sihag, S.; Minakshi, P. Nanotechnology in Colorectal Cancer for Precision Diagnosis and Therapy. Front. Nanotechnol. 2021, 3, 66. [Google Scholar] [CrossRef]
- Viswanath, B.; Kim, S.; Lee, K. Recent Insights into Nanotechnology Development for Detection and Treatment of Colorectal Cancer. Int. J. Nanomed. 2016, 11, 2491–2504. [Google Scholar]
- Mboge, M.Y.; Mahon, B.P.; McKenna, R.; Frost, S.C. Carbonic Anhydrases: Role in PH Control and Cancer. Metabolites 2018, 8, 19. [Google Scholar] [CrossRef] [PubMed]
- Supuran, C.T. Carbonic Anhydrases: Novel Therapeutic Applications for Inhibitors and Activators. Nat. Rev. Drug Discov. 2008, 7, 168–181. [Google Scholar] [CrossRef] [PubMed]
- Supuran, C.T. Carbonic Anhydrase Inhibitors as Emerging Agents for the Treatment and Imaging of Hypoxic Tumors. Expert Opin. Investig. Drugs 2018, 27, 963–970. [Google Scholar] [CrossRef]
- Dubois, L.; Peeters, S.; Lieuwes, N.G.; Geusens, N.; Thiry, A.; Wigfield, S.; Carta, F.; McIntyre, A.; Scozzafava, A.; Dogné, J.M.; et al. Specific Inhibition of Carbonic Anhydrase IX Activity Enhances the in Vivo Therapeutic Effect of Tumor Irradiation. Radiother. Oncol. 2011, 99, 424–431. [Google Scholar] [CrossRef]
- Swietach, P.; Wigfield, S.; Cobden, P.; Supuran, C.T.; Harris, A.L.; Vaughan-Jones, R.D. Tumor-Associated Carbonic Anhydrase 9 Spatially Coordinates Intracellular PH in Three-Dimensional Multicellular Growths. J. Biol. Chem. 2008, 283, 20473–20483. [Google Scholar] [CrossRef]
- Pastorekova, S.; Gillies, R.J. The Role of Carbonic Anhydrase IX in Cancer Development: Links to Hypoxia, Acidosis, and Beyond. Cancer Metastasis Rev. 2019, 38, 65–77. [Google Scholar] [CrossRef]
- Boonstra, M.C.; de Geus, S.W.L.; Prevoo, H.A.J.M.; Hawinkels, L.J.A.C.; van de Velde, C.J.H.; Kuppen, P.J.K.; Vahrmeijer, A.L.; Sier, C.F.M. Selecting Targets for Tumor Imaging: An Overview of Cancer-Associated Membrane Proteins. Biomark. Cancer 2016, 8, 119–133. [Google Scholar] [CrossRef]
- Tupá, V.; Drahošová, S.; Grendár, M.; Adamkov, M. Expression and Association of Carbonic Anhydrase IX and Cyclooxygenase-2 in Colorectal Cancer. Pathol. Res. Pract. 2019, 215, 705–711. [Google Scholar] [CrossRef]
- Korkeila, E.; Talvinen, K.; Jaakkola, P.M.; Minn, H.; Syrjänen, K.; Sundström, J.; Pyrhönen, S. Expression of Carbonic Anhydrase IX Suggests Poor Outcome in Rectal Cancer. Br. J. Cancer 2009, 100, 874. [Google Scholar] [CrossRef]
- Karakuş, F.; Eyol, E.; Yılmaz, K.; Ünüvar, S. In Vitro Effect of Carbonic Anhydrase Inhibitor Acetazolamide on Cell Viability, Migration and Colony Formation of Colorectal Cancer Cells. Biologia 2018, 73, 621–628. [Google Scholar] [CrossRef]
- Kasimoǧullari, R.; Bülbül, M.; Günhan, H.; Güleryüz, H. Effects of New 5-Amino-1,3,4-Thiadiazole-2-Sulfonamide Derivatives on Human Carbonic Anhydrase Isozymes. Bioorg. Med. Chem. 2009, 17, 3295–3301. [Google Scholar] [CrossRef] [PubMed]
- Kasmoullar, R.; Bülbül, M.; Arslan, B.S.; Göke, B. Synthesis, Characterization and Antiglaucoma Activity of Some Novel Pyrazole Derivatives of 5-Amino-1,3,4-Thiadiazole-2-Sulfonamide. Eur. J. Med. Chem. 2010, 45, 4769–4773. [Google Scholar] [CrossRef] [PubMed]
- Bülbül, M.; Kasimoǧullari, R.; Küfrevǐoǧlu, I. Amide Derivatives with Pyrazole Carboxylic Acids of 5-Amino-1,3, 4-Thiadiazole 2-Sulfonamide as New Carbonic Anhydrase Inhibitors: Synthesis and Investigation of Inhibitory Effects. J. Enzyme Inhib. Med. Chem. 2008, 23, 895–900. [Google Scholar] [CrossRef] [PubMed]
- Büyükkidan, N.; Bülbül, M.; Kasimoǧullari, R.; Büyükkidan, B. Synthesis and Characterization of Metal Complexes of Heterocyclic Sulfonamide as Carbonic Anhydrase Inhibitors. J. Enzyme Inhib. Med. Chem. 2012, 28, 311–315. [Google Scholar] [CrossRef] [PubMed]
- De Simone, G.; Vitale, R.M.; di Fiore, A.; Pedone, C.; Scozzafava, A.; Montero, J.L.; Winum, J.Y.; Supuran, C.T. Carbonic Anhydrase Inhibitors: Hypoxia-Activatable Sulfonamides Incorporating Disulfide Bonds That Target the Tumor-Associated Isoform IX. J. Med. Chem. 2006, 49, 5544–5551. [Google Scholar] [CrossRef] [PubMed]
- Chrastina, A.; Závada, J.; Parkkila, S.; Kaluz, Š.; Kaluzová, M.; Rajčáni, J.; Pastorek, J.; Pastoreková, S. Biodistribution and Pharmacokinetics of 125I-Labeled Monoclonal Antibody M75 Specific for Carbonic Anhydrase IX, an Intrinsic Marker of Hypoxia, in Nude Mice Xenografted with Human Colorectal Carcinoma. Int. J. Cancer 2003, 105, 873–881. [Google Scholar] [CrossRef]
- Supuran, C.T.; Winum, J.Y. Carbonic Anhydrase IX Inhibitors in Cancer Therapy: An Update. Future Med. Chem. 2015, 7, 1407–1414. [Google Scholar] [CrossRef]
- Xie, Y.H.; Chen, Y.X.; Fang, J.Y. Comprehensive Review of Targeted Therapy for Colorectal Cancer. Signal Transduct. Target. Ther. 2020, 5, 22. [Google Scholar] [CrossRef]
- García-Foncillas, J.; Sunakawa, Y.; Aderka, D.; Wainberg, Z.; Ronga, P.; Witzler, P.; Stintzing, S. Distinguishing Features of Cetuximab and Panitumumab in Colorectal Cancer and Other Solid Tumors. Front. Oncol. 2019, 9, 849. [Google Scholar] [CrossRef]
- El Hallal, R.; Lyu, N.; Wang, Y. Effect of Cetuximab-Conjugated Gold Nanoparticles on the Cytotoxicity and Phenotypic Evolution of Colorectal Cancer Cells. Molecules 2021, 26, 567. [Google Scholar] [CrossRef]
- Liszbinski, R.B.; Romagnoli, G.G.; Gorgulho, C.M.; Basso, C.R.; Pedrosa, V.A.; Kaneno, R. Anti-EGFR-Coated Gold Nanoparticles in vitro Carry 5-Fluorouracil to Colorectal Cancer Cells. Materials 2020, 13, 375. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Huang, Y.; Wang, L.; Zhou, J.; Tan, Y.; Peng, C.; Yang, P.; Peng, W.; Li, J.; Gu, Q.; et al. Cetuximab Functionalization Strategy for Combining Active Targeting and Antimigration Capacities of a Hybrid Composite Nanoplatform Applied to Deliver 5-Fluorouracil: Toward Colorectal Cancer Treatment. Biomater. Sci. 2021, 9, 2279–2294. [Google Scholar] [CrossRef] [PubMed]
- Marcelo, G.A.; Galhano, J.; Robalo, T.T.; Cruz, M.M.; Marcos, M.D.; Martínez-Máñez, R.; Duarte, M.P.; Capelo-Martínez, J.L.; Lodeiro, C.; Oliveira, E. Magneto-Fluorescent Mesoporous Nanocarriers for the Dual-Delivery of Ofloxacin and Doxorubicin to Tackle Opportunistic Bacterial Infections in Colorectal Cancer. Int. J. Mol. Sci. 2022, 23, 12287. [Google Scholar] [CrossRef] [PubMed]
- Wen, H.; Park, K. Oral Controlled Release Formulation Design and Drug Delivery: Theory to Practice; John Wiley & Sons: Hoboken, NJ, USA, 2010. [Google Scholar] [CrossRef]
- Hickey, A.J. Emerging Trends in Inhaled Drug Delivery. Adv. Drug Deliv. Rev. 2020, 157, 63–70. [Google Scholar] [CrossRef]
- Urbanska, A.M.; Zhang, X.; Prakash, S. Bioengineered Colorectal Cancer Drugs: Orally Delivered Anti-Inflammatory Agents. Cell Biochem. Biophys. 2015, 72, 757–769. [Google Scholar] [CrossRef]
- Kwakman, J.J.M.; Punt, C.J.A. Oral Drugs in the Treatment of Metastatic Colorectal Cancer. Expert Opin. Pharmacother. 2016, 17, 1351–1361. [Google Scholar] [CrossRef]
- Ying, K.; Bai, B.; Gao, X.; Xu, Y.; Wang, H.; Xie, B. Orally Administrable Therapeutic Nanoparticles for the Treatment of Colorectal Cancer. Front. Bioeng. Biotechnol. 2021, 9, 480. [Google Scholar] [CrossRef]
- Kotla, N.G.; Rana, S.; Sivaraman, G.; Sunnapu, O.; Vemula, P.K.; Pandit, A.; Rochev, Y. Bioresponsive Drug Delivery Systems in Intestinal Inflammation: State-of-the-Art and Future Perspectives. Adv. Drug Deliv. Rev. 2019, 146, 248–266. [Google Scholar] [CrossRef]
- Maderuelo, C.; Lanao, J.M.; Zarzuelo, A. Enteric Coating of Oral Solid Dosage Forms as a Tool to Improve Drug Bioavailability. Eur. J. Pharm. Sci. 2019, 138, 105019. [Google Scholar] [CrossRef]
- Cazzamalli, S.; Dal Corso, A.; Neri, D. Acetazolamide Serves as Selective Delivery Vehicle for Dipeptide-Linked Drugs to Renal Cell Carcinoma. Mol. Cancer Ther. 2016, 15, 2926–2935. [Google Scholar] [CrossRef] [PubMed]
- Kasimoǧullari, R.; Bülbül, M.; Mert, S.; Güleryüz, H. Synthesis of 5-Amino-1,3,4-Thiadiazole-2-Sulphonamide Derivatives and Their Inhibition Effects on Human Carbonic Anhydrase Isozymes. J. Enzyme Inhib. Med. Chem. 2011, 26, 231–237. [Google Scholar] [CrossRef]
- Karcz, D.; Matwijczuk, A.; Kamiński, D.; Creaven, B.; Ciszkowicz, E.; Lecka-Szlachta, K.; Starzak, K. Structural Features of 1,3,4-Thiadiazole-Derived Ligands and Their Zn(II) and Cu(II) Complexes Which Demonstrate Synergistic Antibacterial Effects with Kanamycin. Int. J. Mol. Sci. 2020, 21, 5735. [Google Scholar] [CrossRef]
- Mohammed, S.J.; Salih, A.K.; Rashid, M.A.M.; Omer, K.M.; Abdalkarim, K.A. Synthesis, Spectroscopic Studies and Keto-Enol Tautomerism of Novel 1,3,4-Thiadiazole Derivative Containing 3-Mercaptobutan-2-One and Quinazolin-4-One Moieties. Molecules 2020, 25, 5441. [Google Scholar] [CrossRef] [PubMed]
- Antonaroli, S.; Bianco, A.; Brufani, M.; Baido, L.; Rende, G.; Potier, E. Acetazolamide-Related Compounds, Process for Their Preparation, and Pharmaceutical Composition Containing the Same. U.S. Patent US5010204A, 23 April 1991. [Google Scholar]
- Schuetze, B.; Mayer, C.; Loza, K.; Gocyla, M.; Heggen, M.; Epple, M. Conjugation of Thiol-Terminated Molecules to Ultrasmall 2 Nm-Gold Nanoparticles Leads to Remarkably Complex 1 H-NMR Spectra. J. Mater. Chem. B 2016, 4, 2179–2189. [Google Scholar] [CrossRef] [PubMed]
- Ozel, A.E.; Gunduz, S.K.; Celik, S.; Akyuz, S. Structural and Vibrational Study on Monomer and Dimer Forms and Water Clusters of Acetazolamide. J. Spectrosc. 2013, 2013, 538917. [Google Scholar] [CrossRef]
- Chaturvedi, D.; Gupta, V.; Tandon, P.; Sharma, A.; Baraldi, C.; Gamberini, M.C. Intermolecular Charge Transfer and Vibrational Analysis of Hydrogen Bonding in Acetazolamide. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2012, 99, 150–159. [Google Scholar] [CrossRef]
- Baraldi, C.; Gamberini, M.C.; Tinti, A.; Palazzoli, F.; Ferioli, V. Vibrational Study of Acetazolamide Polymorphism. J. Mol. Struct. 2009, 918, 88–96. [Google Scholar] [CrossRef]
- Camí, G.E.; Chufán, E.E.; Pedregosa, J.C.; Varetti, E.L. Infrared and Raman Spectra of 5-Amino-1,3,4-Thiadiazole-2-Sulfonamide (Hats). Experimental Data and Quantum Chemistry Calculations. J. Mol. Struct. 2001, 570, 119–127. [Google Scholar] [CrossRef]
- Coates, J. Interpretation of Infrared Spectra, A Practical Approach. In Encyclopedia of Analytical Chemistry; John Wiley & Sons Ltd.: Chichester, UK, 2006. [Google Scholar] [CrossRef]
- Alterio, V.; Hilvo, M.; di Fiore, A.; Supuran, C.T.; Pan, P.; Parkkila, S.; Scaloni, A.; Pastorek, J.; Pastorekova, S.; Pedone, C.; et al. Crystal Structure of the Catalytic Domain of the Tumor-Associated Human Carbonic Anhydrase IX. Proc. Natl. Acad. Sci. USA 2009, 106, 16233–16238. [Google Scholar] [CrossRef]
- Santos-Martins, D.; Forli, S.; Ramos, M.J.; Olson, A.J. AutoDock4Zn: An Improved AutoDock Force Field for Small-Molecule Docking to Zinc Metalloproteins. J. Chem. Inf. Model. 2014, 54, 2371–2379. [Google Scholar] [CrossRef] [PubMed]
- Innocenti, A.; Vullo, D.; Scozzafava, A.; Supuran, C.T. Carbonic Anhydrase Inhibitors: Inhibition of Mammalian Isoforms I-XIV with a Series of Substituted Phenols Including Paracetamol and Salicylic Acid. Bioorg. Med. Chem. 2008, 16, 7424–7428. [Google Scholar] [CrossRef] [PubMed]
- Fisher, S.Z.; Aggarwal, M.; Kovalevsky, A.Y.; Silverman, D.N.; McKenna, R. Neutron Diffraction of Acetazolamide-Bound Human Carbonic Anhydrase II Reveals Atomic Details of Drug Binding. J. Am. Chem. Soc. 2012, 134, 14726–14729. [Google Scholar] [CrossRef] [PubMed]
- Demir-Yazici, K.; Bua, S.; Akgünes, N.M.; Akdemir, A.; Supuran, C.T.; Güzel-Akdemir, Ö. Indole-Based Hydrazones Containing a Sulfonamide Moiety as Selective Inhibitors of Tumor-Associated Human Carbonic Anhydrase Isoforms Ix and Xii. Int. J. Mol. Sci. 2019, 20, 2354. [Google Scholar] [CrossRef]
- Friedl, J.D.; Nele, V.; de Rosa, G.; Bernkop-Schnürch, A. Bioinert, Stealth or Interactive: How Surface Chemistry of Nanocarriers Determines Their Fate In Vivo. Adv. Funct. Mater. 2021, 31, 2103347. [Google Scholar] [CrossRef]
- Hock, N.; Racaniello, G.F.; Aspinall, S.; Denora, N.; Khutoryanskiy, V.V.; Bernkop-Schnürch, A. Thiolated Nanoparticles for Biomedical Applications: Mimicking the Workhorses of Our Body. Adv. Sci. 2022, 9, 2102451. [Google Scholar] [CrossRef]
- Winther, J.R.; Thorpe, C. Quantification of Thiols and Disulfides. Biochim. Biophys. Acta Gen. Subj. 2014, 1840, 838–846. [Google Scholar] [CrossRef]
- Acevedo-León, D.; Monzó-Beltrán, L.; Gómez-Abril, S.Á.; Estañ-Capell, N.; Camarasa-Lillo, N.; Pérez-Ebri, M.L.; Escandón-álvarez, J.; Alonso-Iglesias, E.; Santaolaria-Ayora, M.L.; Carbonell-Moncho, A.; et al. The Effectiveness of Glutathione Redox Status as a Possible Tumor Marker in Colorectal Cancer. Int. J. Mol. Sci. 2021, 22, 6183. [Google Scholar] [CrossRef]
- Aitken, A.; Learmonth, M. Estimation of Disulfide Bonds Using Ellman’s Reagent. In The Protein Protocols Handbook; Humana Press: Totowa, NJ, USA, 2009; pp. 1053–1055. [Google Scholar]
- Fülöp, Z.; Gref, R.; Loftsson, T. A Permeation Method for Detection of Self-Aggregation of Doxorubicin in Aqueous Environment. Int. J. Pharm. 2013, 454, 559–561. [Google Scholar] [CrossRef]
- Van Wieren, E.M.; Seymour, M.D.; Peterson, J.W. Interaction of the Fluoroquinolone Antibiotic, Ofloxacin, with Titanium Oxide Nanoparticles in Water: Adsorption and Breakdown. Sci. Total Environ. 2012, 441, 1–9. [Google Scholar] [CrossRef]
- Shen, J.; He, Q.; Gao, Y.; Shi, J.; Li, Y. Mesoporous Silica Nanoparticles Loading Doxorubicin Reverse Multidrug Resistance: Performance and Mechanism. Nanoscale 2011, 3, 4314. [Google Scholar] [CrossRef] [PubMed]
- Merle, P.; Blanc, J.F.; Phelip, J.M.; Pelletier, G.; Bronowicki, J.P.; Touchefeu, Y.; Pageaux, G.; Gerolami, R.; Habersetzer, F.; Nguyen-Khac, E.; et al. Doxorubicin-Loaded Nanoparticles for Patients with Advanced Hepatocellular Carcinoma after Sorafenib Treatment Failure (RELIVE): A Phase 3 Randomised Controlled Trial. Lancet Gastroenterol. Hepatol. 2019, 4, 454–465. [Google Scholar] [CrossRef] [PubMed]
- Marcelo, G.A.; Duarte, M.P.; Oliveira, E. Gold@mesoporous Silica Nanocarriers for the Effective Delivery of Antibiotics and By-Passing of β-Lactam Resistance. SN Appl. Sci. 2020, 2, 1354. [Google Scholar] [CrossRef]
- Nuti, S.; Fernández-Lodeiro, J.; del Secco, B.; Rampazzo, E.; Rodríguez-González, B.; Capelo, J.L.; Silva, V.; Igrejas, G.; Poeta, P.; Torres, C.; et al. Engineered Nanostructured Materials for Ofloxacin Delivery. Front. Chem. 2018, 6, 554. [Google Scholar] [CrossRef]
- Traverso, N.; Ricciarelli, R.; Nitti, M.; Marengo, B.; Furfaro, A.L.; Pronzato, M.A.; Marinari, U.M.; Domenicotti, C. Role of Glutathione in Cancer Progression and Chemoresistance. Oxid. Med. Cell. Longev. 2013, 2013, 972913. [Google Scholar] [CrossRef] [PubMed]
- Barranco, S.C.; Perry, R.R.; Durm, M.E.; Quraishi, M.; Werner, A.L.; Gregorcyk, S.G.; Kolm, P. Relationship between Colorectal Cancer Glutathione Levels and Patient Survival: Early Results. Dis. Colon Rectum 2000, 43, 1133–1140. [Google Scholar] [CrossRef] [PubMed]
- Wathoni, N.; Nguyen, A.N.; Rusdin, A.; Umar, A.K.; Mohammed, A.F.A.; Motoyama, K.; Joni, I.M.; Muchtaridi, M. Enteric-Coated Strategies in Colorectal Cancer Nanoparticle Drug Delivery System. Drug Des. Dev. Ther. 2020, 14, 4387–4405. [Google Scholar] [CrossRef]
- Barbosa, J.A.C.; Abdelsadig, M.S.E.; Conway, B.R.; Merchant, H.A. Using Zeta Potential to Study the Ionisation Behaviour of Polymers Employed in Modified-Release Dosage Forms and Estimating Their PKa. Int. J. Pharm. X 2019, 1, 100024. [Google Scholar] [CrossRef]
- Hadi, M.A.; Raghavendra Rao, N.G.; Srinivasa Rao, A. Formulation and Evaluation of PH-Responsive Mini-Tablets for Ileo-Colonic Targeted Drug Delivery. Trop. J. Pharm. Res. 2014, 13, 1021–1029. [Google Scholar] [CrossRef]
- Khan, M.Z.I.; Štedul, H.P.; Kurjaković, N. A PH-Dependent Colon-Targeted Oral Drug Delivery System Using Methacrylic Acid Copolymers. II. Manipulation of Drug Release Using Eudragit® L100 and Eudragit S100 Combinations. Drug Dev. Ind. Pharm. 2000, 26, 549–554. [Google Scholar] [CrossRef]
- Qu, Z.; Wong, K.Y.; Moniruzzaman, M.; Begun, J.; Santos, H.A.; Hasnain, S.Z.; Kumeria, T.; McGuckin, M.A.; Popat, A. One-Pot Synthesis of PH-Responsive Eudragit-Mesoporous Silica Nanocomposites Enable Colonic Delivery of Glucocorticoids for the Treatment of Inflammatory Bowel Disease. Adv. Ther. 2021, 4, 2000165. [Google Scholar] [CrossRef]
- Cui, Y.; Zhang, Y.; Tang, X. In Vitro and in Vivo Evaluation of Ofloxacin Sustained Release Pellets. Int. J. Pharm. 2008, 360, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Li, C.F.; Li, Y.C.; Chen, L.B.; Wang, Y.; Sun, L.B. Doxorubicin-Loaded Eudragit-Coated Chitosan Nanoparticles in the Treatment of Colon Cancers. J. Nanosci. Nanotechnol. 2016, 16, 6773–6780. [Google Scholar] [CrossRef]
- He, K.; Du, X.; Sheng, W.; Zhou, X.; Wang, J.; Wang, S. Crystal Structure of the Fab Fragment of an Anti-Ofloxacin Antibody and Exploration of Its Specific Binding. J. Agric. Food Chem. 2016, 64, 6773–6780. [Google Scholar] [CrossRef]
- Marcelo, G.; Ariana-Machado, J.; Enea, M.; Carmo, H.; Rodríguez-González, B.; Luis Capelo, J.; Lodeiro, C.; Oliveira, E. Toxicological Evaluation of Luminescent Silica Nanoparticles as New Drug Nanocarriers in Different Cancer Cell Lines. Materials 2018, 11, 1310. [Google Scholar] [CrossRef]
- Omar, H.; Croissant, J.G.; Alamoudi, K.; Alsaiari, S.; Alradwan, I.; Majrashi, M.A.; Anjum, D.H.; Martins, P.; Laamarti, R.; Eppinger, J.; et al. Biodegradable Magnetic Silica@Iron Oxide Nanovectors with Ultra-Large Mesopores for High Protein Loading, Magnetothermal Release, and Delivery. J. Control. Release 2017, 259, 187–194. [Google Scholar] [CrossRef]
- Bronchud, M.H.; Margison, J.M.; Howell, A.; Lind, M.; Lucas, S.B.; Wilkinson, P.M. Comparative Pharmacokinetics of Escalating Doses of Doxorubicin in Patients with Metastatic Breast Cancer. Cancer Chemother. Pharmacol. 1990, 25, 435–439. [Google Scholar] [CrossRef]
- Lai, C.; Cole, D.; Steinberg, S.M.; Lucas, A.N.; Dombi, E.; Melani, C.; Roschewski, M.J.; Balis, F.M.; Widemann, B.C.; Wilson, W.H. Doxorubicin Pharmacokinetics and Toxicity in Patients with Aggressive Lymphoma and Hepatic Impairment. Blood Adv. 2022, 7, 529–532. [Google Scholar] [CrossRef]
- Wihlm, J.; Jm, L.; Levêque, D.; Duclos, B.; Dufour, P.; Jp, B.; Methlin, G. Pharmacokinetic Profile of High-Dose Doxorubicin Administered during a 6 h Intravenous Infusion in Breast Cancer Patients. Bull. Cancer 1997, 84, 603–608. (In French) [Google Scholar]
- Kandula, M. Compositions and Methods for Suppression of Carbonic Anhydrase Activity. U.S. Patent US9284287B1, 15 March 2016. [Google Scholar]
- Mohapatra, S.; Sahu, S.; Sinha, N.; Bhutia, S.K. Synthesis of a Carbon-Dot-Based Photoluminescent Probe for Selective and Ultrasensitive Detection of Hg2+in Water and Living Cells. Analyst 2015, 140, 1221–1228. [Google Scholar] [CrossRef]
- Bolla, G.; Nangia, A. Binary and Ternary Cocrystals of Sulfa Drug Acetazolamide with Pyridine Carboxamides and Cyclic Amides. IUCrJ 2016, 3, 152–160. [Google Scholar] [CrossRef] [PubMed]
- O’Boyle, N.M.; Banck, M.; James, C.A.; Morley, C.; Vandermeersch, T.; Hutchison, G.R. Open Babel: An Open Chemical Toolbox. J. Cheminform. 2011, 3, 33. [Google Scholar] [CrossRef] [PubMed]
- Morris, G.M.; Ruth, H.; Lindstrom, W.; Sanner, M.F.; Belew, R.K.; Goodsell, D.S.; Olson, A.J. AutoDock4 and AutoDockTools4: Automated Docking with Selective Receptor Flexibility. J. Comput. Chem. 2009, 30, 2785–2791. [Google Scholar] [CrossRef] [PubMed]
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C.; Couch, G.S.; Greenblatt, D.M.; Meng, E.C.; Ferrin, T.E. UCSF Chimera—A Visualization System for Exploratory Research and Analysis. J. Comput. Chem. 2004, 25, 1605–1612. [Google Scholar] [CrossRef] [PubMed]
| Drug Loading | Biofunctionalization | ||||||
|---|---|---|---|---|---|---|---|
| Sample | NANO3 (mg) | DOX (mg/gNANO) | OFLOX (mg/gNANO) | CTX (mg/gNANO) | AZM-SH (mg/gNANO) | CTX (#/NANO) | AZM-SH (#/NANO) |
| NANO3-CTX | 5.0 | - | - | 13.65 | - | 5.54 | - |
| NANO3-AZM | 5.0 | - | - | - | 0.27 | - | 58.91 |
| NANO3-CTX+AZM | 5.0 | - | - | 5.62 | 0.33 | 2.28 | 72.39 |
| NANO3@D-CTX | 5.0 | 278.5 | - | 14.12 | - | 5.73 | - |
| NANO3@D-AZM | 5.0 | 278.5 | - | - | 0.32 | - | 69.85 |
| NANO3@D-CTX+AZM | 5.0 | 278.5 | - | 7.05 | 0.22 | 2.86 | 47.64 |
| NANO3@DO-CTX | 5.0 | 274.0 | 140.0 | 8.38 | - | 3.40 | - |
| NANO3@DO-AZM | 5.0 | 274.0 | 140.0 | - | 0.48 | - | 106.87 |
| NANO3@DO-CTX+AZM | 5.0 | 274.0 | 140.0 | 11.18 | 0.61 | 4.54 | 133.80 |
| NANO3@O-CTX | 5.0 | - | 182.8 | 9.76 | - | 3.96 | - |
| NANO3@O-AZM | 5.0 | - | 182.8 | - | 0.42 | - | 93.41 |
| NANO3@O-CTX+AZM | 5.0 | - | 182.8 | 6.13 | 0.35 | 2.49 | 77.97 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcelo, G.A.; Montpeyó, D.; Galhano, J.; Martínez-Máñez, R.; Capelo-Martínez, J.L.; Lorenzo, J.; Lodeiro, C.; Oliveira, E. Development of New Targeted Nanotherapy Combined with Magneto-Fluorescent Nanoparticles against Colorectal Cancer. Int. J. Mol. Sci. 2023, 24, 6612. https://doi.org/10.3390/ijms24076612
Marcelo GA, Montpeyó D, Galhano J, Martínez-Máñez R, Capelo-Martínez JL, Lorenzo J, Lodeiro C, Oliveira E. Development of New Targeted Nanotherapy Combined with Magneto-Fluorescent Nanoparticles against Colorectal Cancer. International Journal of Molecular Sciences. 2023; 24(7):6612. https://doi.org/10.3390/ijms24076612
Chicago/Turabian StyleMarcelo, Gonçalo A., David Montpeyó, Joana Galhano, Ramón Martínez-Máñez, José Luis Capelo-Martínez, Julia Lorenzo, Carlos Lodeiro, and Elisabete Oliveira. 2023. "Development of New Targeted Nanotherapy Combined with Magneto-Fluorescent Nanoparticles against Colorectal Cancer" International Journal of Molecular Sciences 24, no. 7: 6612. https://doi.org/10.3390/ijms24076612
APA StyleMarcelo, G. A., Montpeyó, D., Galhano, J., Martínez-Máñez, R., Capelo-Martínez, J. L., Lorenzo, J., Lodeiro, C., & Oliveira, E. (2023). Development of New Targeted Nanotherapy Combined with Magneto-Fluorescent Nanoparticles against Colorectal Cancer. International Journal of Molecular Sciences, 24(7), 6612. https://doi.org/10.3390/ijms24076612








