Contribution of the L-Type Amino Acid Transporter Family in the Diagnosis and Treatment of Prostate Cancer
Abstract
1. Introduction
2. The Structure and Function of LATs
2.1. LAT1
2.2. LAT2
2.3. LAT3
2.4. LAT4
3. LATs and PCa
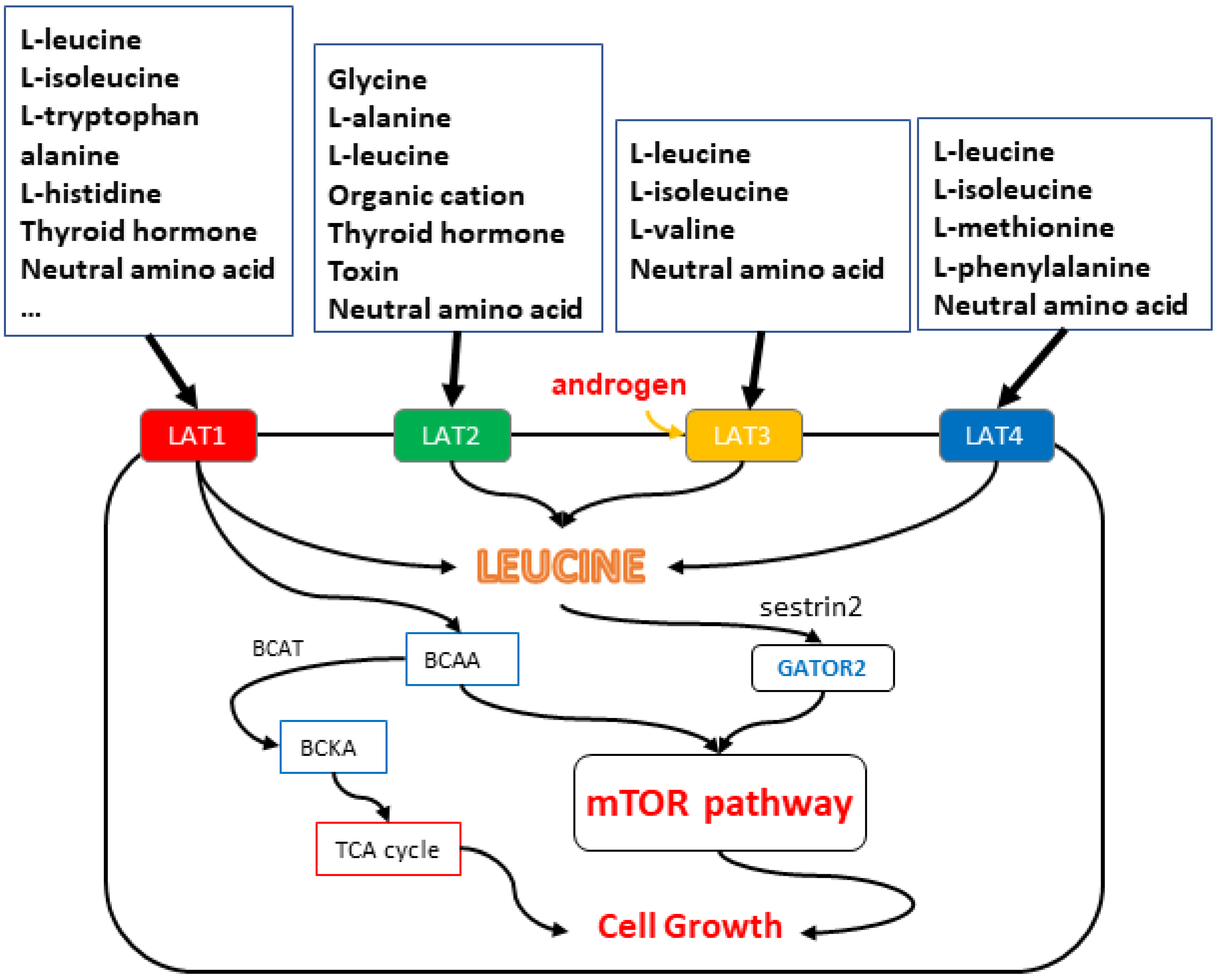
- Amino acid uptake:LATs increase the uptake of essential amino acids into cancer cells, which supports their growth and survival. After being delivered into cells, these amino acids are used to make proteins, nucleic acids, lipids, and ATP. Compared with normal cells, cancer cells have higher upregulation transporters (LATs), which can promote the entry of foreign amino acids into cells, and the stable acquisition of amino acids by cancer cells is important for cancer growth. By increasing the availability of amino acids, LATs can promote PCa cell proliferation and invasion.
- Activation of signaling pathways:LATs have been shown to activate various signaling pathways, including the mTOR pathway, which is involved in the regulation of cell growth, proliferation, metabolism, and survival. LAT1 [23] and LAT3 [41] are highly expressed in prostate cancer, providing branched-chain amino acids (BCAA) to the mammalian target protein of rapamycin complex (mTORC1), which senses amino acid signaling and promotes cell proliferation through multiple downstream effectors related to gene expression and metabolism [15]. Leucine, which enters the cell via LAT1, binds to the leucine sensor sestrin2. The interaction between leucine and sestrin2 can activate GATOR2 and inhibit GATOR1, thus promoting the function of mTORC1 and achieving the purpose of cell proliferation [16,17]. LATs can regulate mTOR activity by influencing the availability of essential amino acids, such as leucine, that activate the pathway.
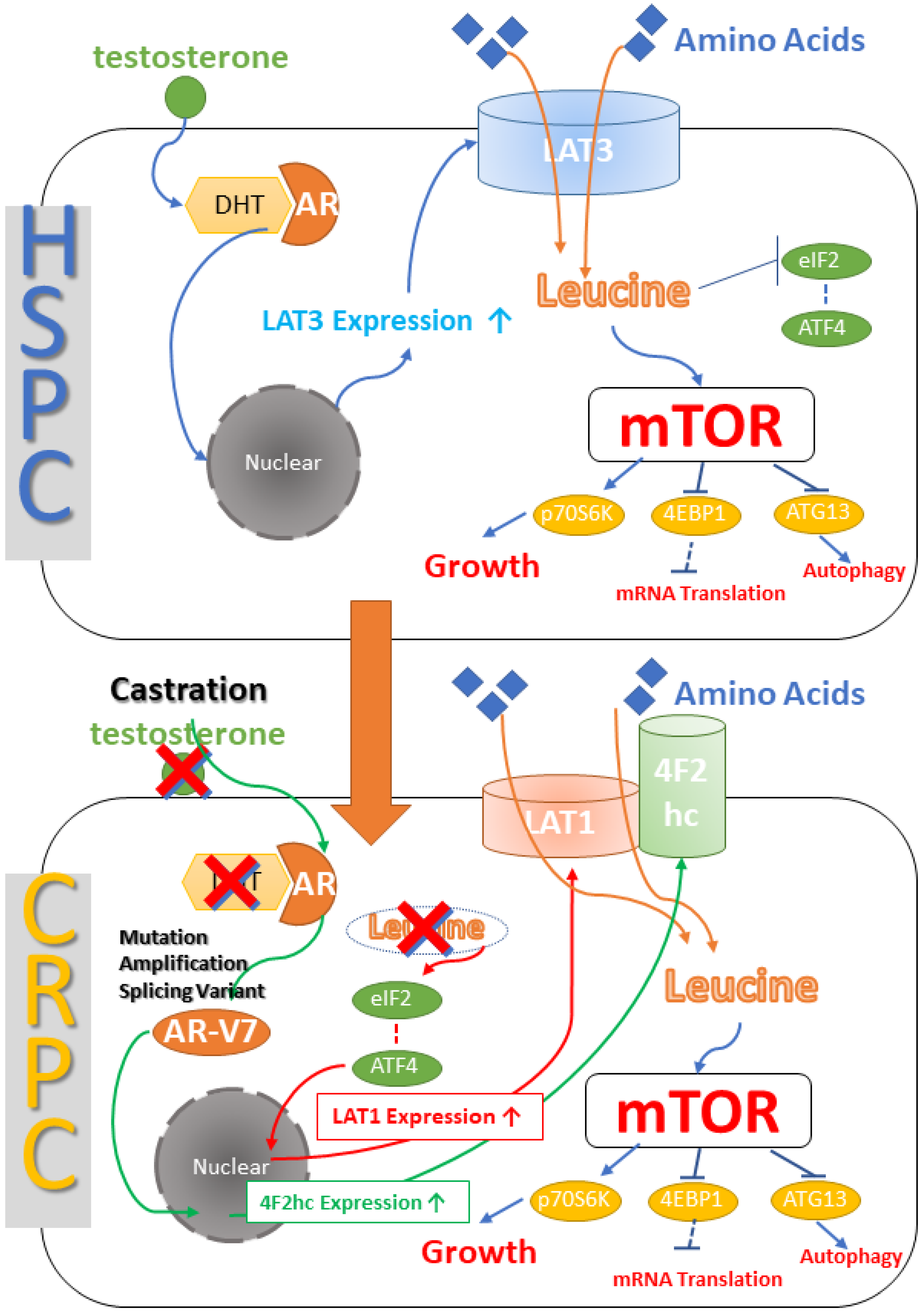
- Drug resistance:In PCa cells resistant to antiandrogen therapy (ADT), the expression of some LATs is up-regulated, which may promote the progression of PCa to castration-resistant prostate cancer (CRPC) through androgen receptor variants [43]. Changes in the microenvironment induced by hormone deprivation therapy can alter the expression of LAT1 and LAT3. Reduced androgen receptor signaling may lead to decreased LAT3 expression and, as another consequence, increased LAT1 expression. Changes in the microenvironment induced by hormone deprivation therapy can alter the expression of LAT1 and LAT3. Decreased androgen receptor signaling may lead to decreased LAT3 expression and, as another consequence, the production of the AR-V7 variant, resulting in increased 4F2hc expression, and decreased leucine, resulting in increased LAT1 expression. The two form a dimer that eventually causes leucine to be re-transported into the cell to promote cancer cell proliferation. PCa is transformed into CRPC, which is resistant to ADT treatment.
- Promotion of angiogenesis:LATs have been implicated in the regulation of blood vessel formation (angiogenesis), which is essential for the growth and spread of PCa cells. Tumors grow and evolve through constant crosstalk with the surrounding microenvironment. New evidence suggests that angiogenesis and immunosuppression often occur together in response to this crosstalk [44]. For example, the expression of LAT1 was significantly correlated with the expression of VEGF, CD34, and microvascular density at the primary and metastatic sites [45,46,47,48]. VEGF and CD34 are factors related to angiogenesis. LAT1 can also mediate the angiogenesis of miR-126 on primary human pulmonary microvascular endothelial cells by regulating mTOR signaling [49].
- Others: Increase the uptake of amino acids by inducing hemoglobin maturation [40]. LAT3 expression is required for the development of red blood cells to produce hemoglobin. LAT3 can be upregulated under the action of androgens [41], which leads to the increase of hemoglobin development and increases the way for tumor cells to obtain nutrients from another side, thus promoting their proliferation.
3.1. LAT1
3.2. LAT2
3.3. LAT3
3.4. LAT4
4. Prostate Cancer Diagnosis by LATs
4.1. LAT1
4.2. LAT3
4.3. LAT4
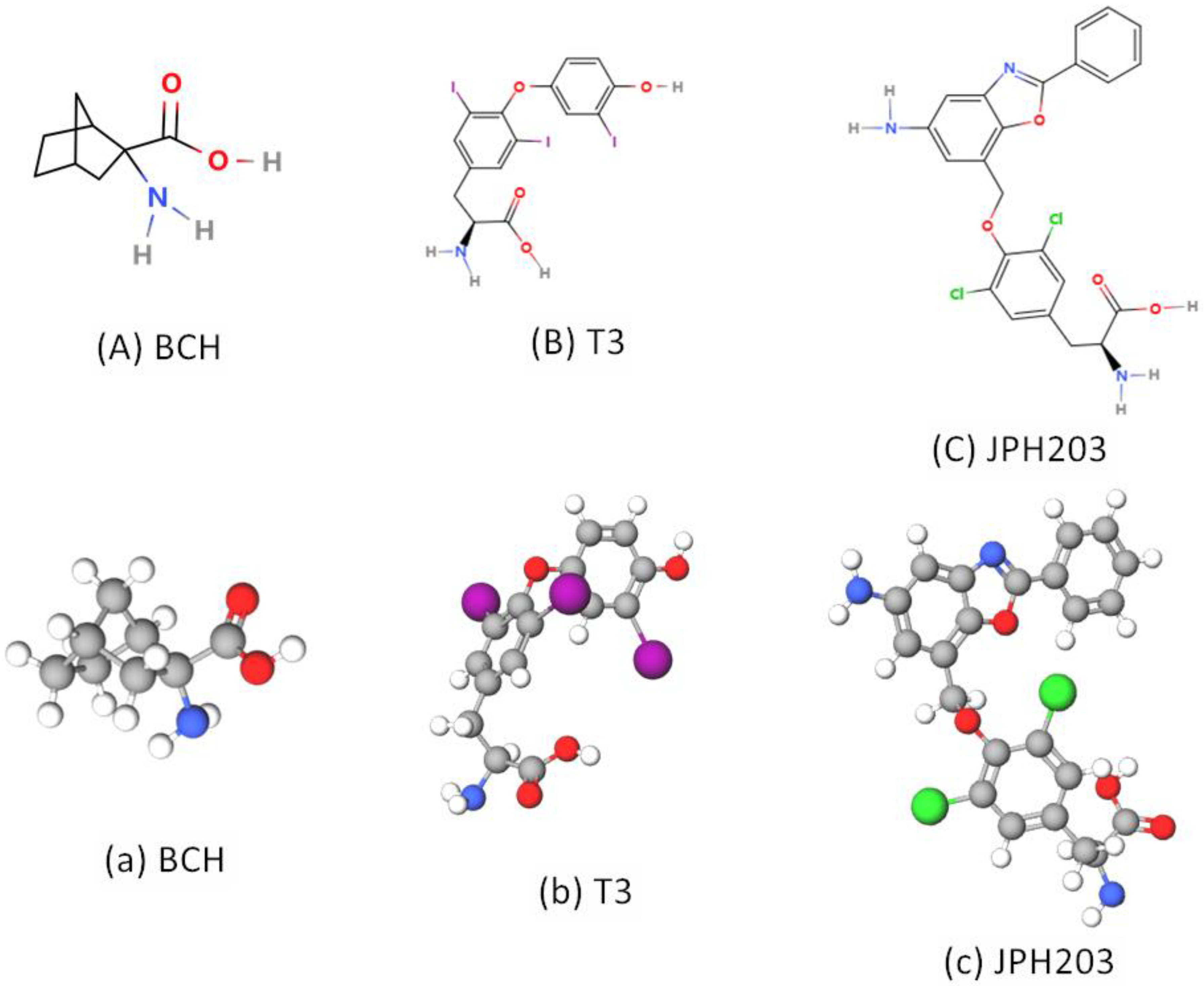
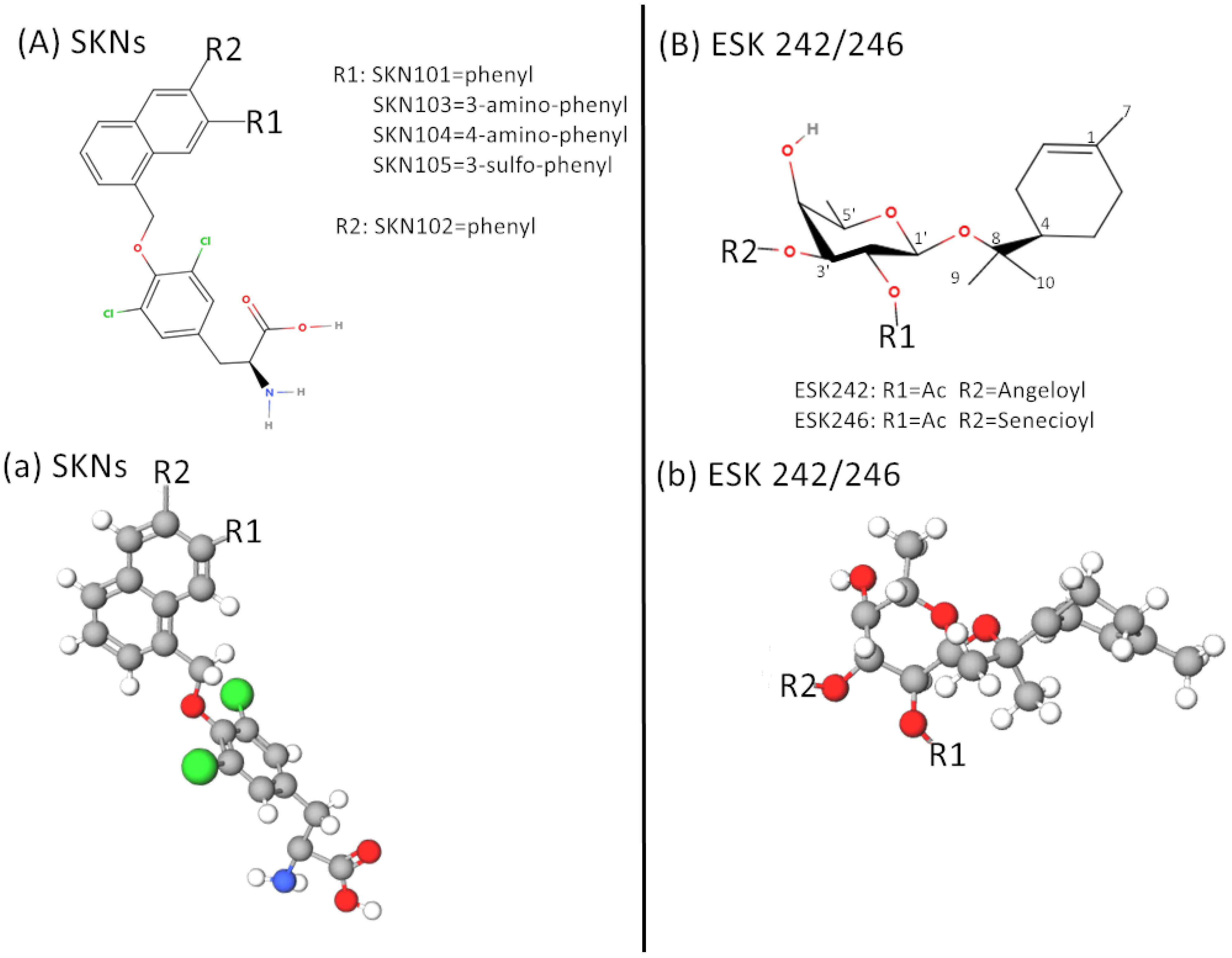
5. Inhibitors of LATs and Targeted Therapy of PCa
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviation
| PCa | prostate cancer |
| LAT | L-type amino acid transporter |
| mTOR | mammalian target of rapamycin |
| EAA | essential amino acid |
| SLC | solute vector family |
| TCR | T cell receptors |
| BCAA | branched-chain amino acid |
| mTORC | mammalian target of rapamycin complex |
| GAP | GTPase-activating protein |
| GATOR | GAP activity toward Rags |
| BCAT | branched-chain amino acid transferase |
| BCKA | branched-chain keto acid |
| Kyn | kynurenine |
| TDO | 2, 3-Deoxygenase |
| IDO | indoleamine 2, 3-Dioxygenase |
| AHR | aryl hydrocarbon receptor |
| ADT | antiandrogen therapy |
| CRPC | castration-resistant prostate cancer |
| AR | androgen receptor |
| HSPC | hormone-sensitive prostate cancer |
| 18F-OMFD | 3-O-methyl-6-18F-fluoro-L-dopa |
| 18F-FDOPA | 18F-fluorodihydroxyphenylalanine |
| BBN | N-butyl- (4-hydroxybutyl) nitrosamine |
| HIFs | hyposia-inducedfactors |
| PET | positron emission computed tomography |
| BCH | 2-aminobicyclo-(2,2,2,1)-heptane-2-caryboxylic acid |
References
- Eagle, H. Nutrition Needs of Mammalian Cells in Tissue Culture. Science 1955, 122, 501–504. [Google Scholar] [CrossRef]
- Qi, W.; Guan, Q.; Sun, T.; Cao, Y.; Zhang, L.; Guo, Y. Improving detection sensitivity of amino acids in thyroid tissues by using phthalic acid as a mobile phase additive in hydrophilic interaction chromatography-electrospray ionization-tandem mass spectrometry. Anal. Chim. Acta 2015, 870, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Kanai, Y.; Segawa, H.; Miyamoto, K.-I.; Uchino, H.; Takeda, E.; Endou, H. Expression Cloning and Characterization of a Transporter for Large Neutral Amino Acids Activated by the Heavy Chain of 4F2 Antigen (CD98). J. Biol. Chem. 1998, 273, 23629–23632. [Google Scholar] [CrossRef] [PubMed]
- Segawa, H.; Fukasawa, Y.; Miyamoto, K.-I.; Takeda, E.; Endou, H.; Kanai, Y. Identification and Functional Characterization of a Na+-independent Neutral Amino Acid Transporter with Broad Substrate Selectivity. J. Biol. Chem. 1999, 274, 19745–19751. [Google Scholar] [CrossRef]
- Babu, E.; Kanai, Y.; Chairoungdua, A.; Kim, D.K.; Iribe, Y.; Tangtrongsup, S.; Jutabha, P.; Li, Y.; Ahmed, N.; Sakamoto, S.; et al. Identification of a Novel System L Amino Acid Transporter Structurally Distinct from Heterodimeric Amino Acid Transporters. J. Biol. Chem. 2003, 278, 43838–43845. [Google Scholar] [CrossRef] [PubMed]
- Bodoy, S.; Martín, L.; Zorzano, A.; Palacín, M.; Estévez, R.; Bertran, J. Identification of LAT4, a Novel Amino Acid Transporter with System L Activity. J. Biol. Chem. 2005, 280, 12002–12011. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Holst, J. L-type amino acid transport and cancer: Targeting the mTORC1 pathway to inhibit neoplasia. Am. J. Cancer Res. 2015, 5, 1281–1294. [Google Scholar]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Mastroberardino, L.; Spindler, B.; Pfeiffer, R.; Skelly, P.J.; Loffing, J.; Shoemaker, C.B.; Verrey, F. Amino-acid transport by heterodimers of 4F2hc/CD98 and members of a permease family. Nature 1998, 395, 288–291. [Google Scholar] [CrossRef]
- Zhao, X.; Sakamoto, S.; Maimaiti, M.; Anzai, N.; Ichikawa, T. Contribution of LAT1-4F2hc in Urological Cancers via Toll-like Receptor and Other Vital Pathways. Cancers 2022, 14, 229. [Google Scholar] [CrossRef]
- Nakada, N.; Mikami, T.; Hana, K.; Ichinoe, M.; Yanagisawa, N.; Yoshida, T.; Endou, H.; Okayasu, I. Unique and selective expression of L-amino acid transporter 1 in human tissue as well as being an aspect of oncofetal protein. Histol. Histopathol. 2014, 29, 217–227. [Google Scholar] [CrossRef]
- Puris, E.; Gynther, M.; Auriola, S.; Huttunen, K.M. L-Type amino acid transporter 1 as a target for drug delivery. Pharm. Res. 2020, 37, 88. [Google Scholar] [CrossRef]
- Ohgaki, R.; Ohmori, T.; Hara, S.; Nakagomi, S.; Kanai-Azuma, M.; Kaneda-Nakashima, K.; Okuda, S.; Nagamori, S.; Kanai, Y. Essential Roles of L-Type Amino Acid Transporter 1 in Syncytiotrophoblast Development by Presenting Fusogenic 4F2hc. Mol. Cell. Biol. 2017, 37, e00427-16. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, L.V.; Rolf, J.; Emslie, E.; Shi, Y.-B.; Taylor, P.M.; Cantrell, D.A. Control of amino-acid transport by antigen receptors coordinates the metabolic reprogramming essential for T cell differentiation. Nat. Immunol. 2013, 14, 500–508. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, B.C.; Bode, B.P. Amino acid transporters ASCT2 and LAT1 in cancer: Partners in crime? Semin. Cancer Biol. 2005, 15, 254–266. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, R.L.; Chantranupong, L.; Saxton, R.A.; Shen, K.; Scaria, S.M.; Cantor, J.R.; Sabatini, D.M. Sestrin2 is a leucine sensor for the mTORC1 pathway. Science 2016, 351, 43–48. [Google Scholar] [CrossRef]
- Wolfson, R.L.; Sabatini, D.M. The Dawn of the Age of Amino Acid Sensors for the mTORC1 Pathway. Cell Metab. 2017, 26, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Furuya, M.; Horiguchi, J.; Nakajima, H.; Kanai, Y.; Oyama, T. Correlation of L-type amino acid transporter 1 and CD98 ex-pression with triple negative breast cancer prognosis. Cancer Sci. 2012, 103, 382–389. [Google Scholar] [PubMed]
- Kaira, K.; Oriuchi, N.; Imai, H.; Shimizu, K.; Yanagitani, N.; Sunaga, N.; Hisada, T.; Kawashima, O.; Iijima, H.; Ishizuka, T.; et al. Expression of L-type amino acid transporter 1 (LAT1) in neuroendocrine tumors of the lung. Pathol. Res. Pract. 2008, 204, 553–561. [Google Scholar] [CrossRef]
- Ebara, T.; Kaira, K.; Shioya, M.; Asao, T.; Takahashi, T.; Sakurai, H.; Kanai, Y.; Kuwano, H.; Nakano, T. L-type Amino-acid Transporter 1 Expression Predicts the Response to Preoperative Hyperthermo-chemoradiotherapy for Locally Advanced Rectal Cancer. Int. J. Radiat. Oncol. 2010, 78, S330–S331. [Google Scholar] [CrossRef]
- Betsunoh, H.; Fukuda, T.; Anzai, N.; Nishihara, D.; Mizuno, T.; Yuki, H.; Masuda, A.; Yamaguchi, Y.; Abe, H.; Yashi, M.; et al. Increased expression of system large amino acid transporter (LAT)-1 mRNA is associated with invasive potential and unfavorable prognosis of human clear cell renal cell carcinoma. BMC Cancer 2013, 13, 509. [Google Scholar] [CrossRef]
- Maimaiti, M.; Sakamoto, S.; Yamada, Y.; Sugiura, M.; Rii, J.; Takeuchi, N.; Imamura, Y.; Furihata, T.; Ando, K.; Higuchi, K.; et al. Expression of L-type amino acid transporter 1 as a molecular target for prognostic and therapeutic indicators in bladder carcinoma. Sci. Rep. 2020, 10, 1292. [Google Scholar] [CrossRef]
- Xu, M.; Sakamoto, S.; Matsushima, J.; Kimura, T.; Ueda, T.; Mizokami, A.; Kanai, Y.; Ichikawa, T. Up-Regulation of LAT1 during Antiandrogen Therapy Contributes to Progression in Prostate Cancer Cells. J. Urol. 2015, 195, 1588–1597. [Google Scholar] [CrossRef] [PubMed]
- Nawashiro, H.; Otani, N.; Shinomiya, N.; Fukui, S.; Ooigawa, H.; Shima, K.; Matsuo, H.; Kanai, Y.; Endou, H. L-type amino acid transporter 1 as a potential molecular target in human astrocytic tumors. Int. J. Cancer 2006, 119, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Neinast, M.; Murashige, D.; Arany, Z. Branched Chain Amino Acids. Annu. Rev. Physiol. 2019, 81, 139–164. [Google Scholar] [CrossRef] [PubMed]
- Opitz, C.A.; Litzenburger, U.M.; Sahm, F.; Ott, M.; Tritschler, I.; Trump, S.; Schumacher, T.; Jestaedt, L.; Schrenk, D.; Weller, M.; et al. An endogenous tumour-promoting ligand of the human aryl hydrocarbon receptor. Nature 2011, 478, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Pineda, M.; Fernández, E.; Torrents, D.; Estévez, R.; López, C.; Camps, M.; Lloberas, J.; Zorzano, A.; Palacín, M. Identification of a Membrane Protein, LAT-2, That Co-expresses with 4F2 Heavy Chain, an L-type Amino Acid Transport Activity with Broad Specificity for Small and Large Zwitterionic Amino Acids. J. Biol. Chem. 1999, 274, 19738–19744. [Google Scholar] [CrossRef] [PubMed]
- Rossier, G.; Meier, C.; Bauch, C.; Summa, V.; Sordat, B.; Verrey, F.; Kühn, L.C. LAT2, a New Basolateral 4F2hc/CD98-associated Amino Acid Transporter of Kidney and Intestine. J. Biol. Chem. 1999, 274, 34948–34954. [Google Scholar] [CrossRef]
- Verrey, F.; Closs, E.I.; Wagner, C.A.; Palacin, M.; Endou, H.; Kanai, Y. CATs and HATs: The SLC7 family of amino acid transporters. Pflug. Arch. 2004, 447, 532–542. [Google Scholar] [CrossRef]
- Braun, D.; Wirth, E.K.; Wohlgemuth, F.; Reix, N.; Klein, M.O.; Grüters, A.; Köhrle, J.; Schweizer, U. Aminoaciduria, but normal thyroid hormone levels and signalling, in mice lacking the amino acid and thyroid hormone transporter Slc7a8. Biochem. J. 2011, 439, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Napolitano, L.; Scalise, M.; Galluccio, M.; Pochini, L.; Albanese, L.M.; Indiveri, C. LAT1 is the transport competent unit of the LAT1/CD98 heterodimeric amino acid transporter. Int. J. Biochem. Cell Biol. 2015, 67, 25–33. [Google Scholar] [CrossRef]
- Nakamura, E.; Sato, M.; Yang, H.; Miyagawa, F.; Harasaki, M.; Tomita, K.; Matsuoka, S.; Noma, A.; Iwai, K.; Minato, N. 4F2 (CD98) Heavy Chain Is Associated Covalently with an Amino Acid Transporter and Controls Intracellular Trafficking and Membrane Topology of 4F2 Heterodimer. J. Biol. Chem. 1999, 274, 3009–3016. [Google Scholar] [CrossRef]
- Maimaiti, M.; Sakamoto, S.; Sugiura, M.; Kanesaka, M.; Fujimoto, A.; Matsusaka, K.; Xu, M.; Ando, K.; Saito, S.; Wakai, K.; et al. The heavy chain of 4F2 antigen promote prostate cancer progression via SKP-2. Sci. Rep. 2021, 11, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Horita, Y.; Kaira, K.; Kawasaki, T.; Mihara, Y.; Sakuramoto, S.; Yamaguchi, S.; Okamoto, K.; Ryozawa, S.; Kanai, Y.; Yasuda, M.; et al. Expression of LAT1 and 4F2hc in Gastroenteropancreatic Neuroendocrine Neoplasms. In Vivo 2021, 35, 2425–2432. [Google Scholar] [CrossRef]
- Chatsirisupachai, K.; Kitdumrongthum, S.; Panvongsa, W.; Janpipatkul, K.; Worakitchanon, W.; Lertjintanakit, S.; Wongtrakoongate, P.; Chairoungdua, A. Expression and roles of system L amino acid transporters in human embryonal car-cinoma cells. Andrology 2020, 8, 1844–1858. [Google Scholar] [CrossRef] [PubMed]
- Kaira, K.; Kawashima, O.; Endoh, H.; Imaizumi, K.; Goto, Y.; Kamiyoshihara, M.; Sugano, M.; Yamamoto, R.; Osaki, T.; Tanaka, S.; et al. Expression of amino acid transporter (LAT1 and 4F2hc) in pulmonary pleomorphic carcinoma. Hum. Pathol. 2018, 84, 142–149. [Google Scholar] [CrossRef]
- Cole, K.A.; Chuaqui, R.F.; Katz, K.; Pack, S.; Zhuang, Z.; Cole, C.E.; Lyne, J.C.; Linehan, W.M.; Liotta, L.A.; Emmert-Buck, M.R. cDNA Sequencing and Analysis of POV1 (PB39): A Novel Gene Up-regulated in Prostate Cancer. Genomics 1998, 51, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Fukuhara, D.; Kanai, Y.; Chairoungdua, A.; Babu, E.; Bessho, F.; Kawano, T.; Akimoto, Y.; Endou, H.; Yan, K. Protein char-acterization of NA+-independent system L amino acid transporter 3 in mice: A potential role in supply of branched-chain amino acids under nutrient starvation. Am. J. Pathol. 2007, 170, 888–898. [Google Scholar] [CrossRef]
- Sekine, Y.; Nishibori, Y.; Akimoto, Y.; Kudo, A.; Ito, N.; Fukuhara, D.; Kurayama, R.; Higashihara, E.; Babu, E.; Kanai, Y.; et al. Amino Acid Transporter LAT3 Is Required for Podocyte Development and Function. J. Am. Soc. Nephrol. 2009, 20, 1586–1596. [Google Scholar] [CrossRef]
- Chung, J.; Bauer, D.E.; Ghamari, A.; Nizzi, C.P.; Deck, K.M.; Kingsley, P.D.; Yien, Y.Y.; Huston, N.C.; Chen, C.; Schultz, I.J. The mTORC1/4E-BP pathway coordinates hemoglobin production with L-leucine availability. Sci. Signal. 2015, 8, ra34. [Google Scholar] [CrossRef]
- Wang, Q.; Bailey, C.G.; Ng, C.; Tiffen, J.; Thoeng, A.; Minhas, V.; Lehman, M.L.; Hendy, S.C.; Buchanan, G.; Nelson, C.C.; et al. Androgen Receptor and Nutrient Signaling Pathways Coordinate the Demand for Increased Amino Acid Transport during Prostate Cancer Progression. Cancer Res. 2011, 71, 7525–7536. [Google Scholar] [CrossRef] [PubMed]
- Guetg, A.; Mariotta, L.; Bock, L.; Herzog, B.; Fingerhut, R.; Camargo, S.M.R.; Verrey, F. Essential amino acid transporter Lat4 (Slc43a2) is required for mouse development. J. Physiol. 2015, 593, 1273–1289. [Google Scholar] [CrossRef] [PubMed]
- Sugiura, M.; Sato, H.; Okabe, A.; Fukuyo, M.; Mano, Y.; Shinohara, K.-I.; Rahmutulla, B.; Higuchi, K.; Maimaiti, M.; Kanesaka, M. Identification of AR-V7 downstream genes commonly targeted by AR/AR-V7 and specifically targeted by AR-V7 in cas-tration resistant prostate cancer. Transl. Oncol. 2021, 14, 100915. [Google Scholar] [CrossRef]
- Solimando, A.G.; De Summa, S.; Vacca, A.; Ribatti, D. Cancer-Associated Angiogenesis: The Endothelial Cell as a Checkpoint for Immunological Patrolling. Cancers 2020, 12, 3380. [Google Scholar] [CrossRef]
- Kaira, K.; Sunose, Y.; Ohshima, Y.; Ishioka, N.S.; Arakawa, K.; Ogawa, T.; Sunaga, N.; Shimizu, K.; Tominaga, H.; Oriuchi, N.; et al. Clinical significance of L-type amino acid transporter 1 expression as a prognostic marker and potential of new targeting therapy in biliary tract cancer. BMC Cancer 2013, 13, 482. [Google Scholar] [CrossRef]
- Kaira, K.; Oriuchi, N.; Shimizu, K.; Ishikita, T.; Higuchi, T.; Imai, H.; Yanagitani, N.; Sunaga, N.; Hisada, T.; Ishizuka, T. Correlation of angiogenesis with 18F-FMT and 18F-FDG uptake in non-small cell lung cancer. Cancer Sci. 2009, 100, 753–758. [Google Scholar] [CrossRef]
- Okubo, S.; Zhen, H.-N.; Kawai, N.; Nishiyama, Y.; Haba, R.; Tamiya, T. Correlation of l-methyl-11C-methionine (MET) uptake with l-type amino acid transporter 1 in human gliomas. J. Neuro-Oncol. 2010, 99, 217–225. [Google Scholar] [CrossRef]
- Haining, Z.; Kawai, N.; Miyake, K.; Okada, M.; Okubo, S.; Zhang, X.; Fei, Z.; Tamiya, T. Relation of LAT1/4F2hc expression with pathological grade, proliferation and angiogenesis in human gliomas. BMC Clin. Pathol. 2012, 12, 4. [Google Scholar] [CrossRef]
- Cao, D.; Mikosz, A.M.; Ringsby, A.J.; Anderson, K.C.; Beatman, E.L.; Koike, K.; Petrache, I. MicroRNA-126-3p Inhibits Angiogenic Function of Human Lung Microvascular Endothelial Cells via LAT1 (L-Type Amino Acid Transporter 1)-Mediated mTOR (Mammalian Target of Rapamycin) Signaling. Arter. Thromb. Vasc. Biol. 2020, 40, 1195–1206. [Google Scholar] [CrossRef]
- Otsuki, H.; Kimura, T.; Yamaga, T.; Kosaka, T.; Suehiro, J.-I.; Sakurai, H. Prostate Cancer Cells in Different Androgen Receptor Status Employ Different Leucine Transporters. Prostate 2016, 77, 222–233. [Google Scholar] [CrossRef]
- Rii, J.; Sakamoto, S.; Sugiura, M.; Kanesaka, M.; Fujimoto, A.; Yamada, Y.; Maimaiti, M.; Ando, K.; Wakai, K.; Xu, M.; et al. Functional analysis of LAT3 in prostate cancer: Its downstream target and relationship with androgen receptor. Cancer Sci. 2021, 112, 3871–3883. [Google Scholar] [CrossRef]
- Malviya, G.; Patel, R.; Salji, M.; Martinez, R.S.; Repiscak, P.; Mui, E.; Champion, S.; Mrowinska, A.; Johnson, E.; AlRasheedi, M.; et al. 18F-Fluciclovine PET metabolic imaging reveals prostate cancer tumour heterogeneity associated with disease resistance to androgen deprivation therapy. EJNMMI Res. 2020, 10, 143. [Google Scholar] [CrossRef]
- Wang, Q.; Tiffen, J.; Bailey, C.G.; Lehman, M.L.; Ritchie, W.; Fazli, L.; Metierre, C.; Feng, Y.; Li, E.; Gleave, M.; et al. Targeting Amino Acid Transport in Metastatic Castration-Resistant Prostate Cancer: Effects on Cell Cycle, Cell Growth, and Tumor Development. J. Natl. Cancer Inst. 2013, 105, 1463–1473. [Google Scholar] [CrossRef]
- Kokal, M.; Mirzakhani, K.; Pungsrinont, T.; Baniahmad, A. Mechanisms of Androgen Receptor Agonist- and Antagonist-Mediated Cellular Senescence in Prostate Cancer. Cancers 2020, 12, 1833. [Google Scholar] [CrossRef]
- Barollo, S.; Bertazza, L.; Fernando, S.W.; Censi, S.; Cavedon, E.; Galuppini, F.; Pennelli, G.; Fassina, A.; Citton, M.; Rubin, B.; et al. Overexpression of L-Type Amino Acid Transporter 1 (LAT1) and 2 (LAT2): Novel Markers of Neuroendocrine Tumors. PLoS ONE 2016, 11, e0156044. [Google Scholar] [CrossRef]
- Chu, C.E.; Alshalalfa, M.; Sjöström, M.; Zhao, S.G.; Liu, Y.; Chou, J.; Herlemann, A.; Mahal, B.; Kishan, A.U.; Spratt, D.E.; et al. Prostate-specific Membrane Antigen and Fluciclovine Transporter Genes are Associated with Variable Clinical Features and Molecular Subtypes of Primary Prostate Cancer. Eur. Urol. 2021, 79, 717–721. [Google Scholar] [CrossRef]
- Zhang, B.K.; Moran, A.M.; Bailey, C.G.; Rasko, J.E.J.; Holst, J.; Wang, Q. EGF-activated PI3K/Akt signalling coordinates leucine uptake by regulating LAT3 expression in prostate cancer. Cell Commun. Signal. 2019, 17, 83. [Google Scholar] [CrossRef]
- Feral, C.; Tissot, F.; Tosello, L.; Fakhry, N.; Sebag, F.; Pacak, K.; Taïeb, D. 18F-fluorodihydroxyphenylalanine PET/CT in pheochromocytoma and paraganglioma: Relation to genotype and amino acid transport system L. Eur. J. Nucl. Med. 2016, 44, 812–821. [Google Scholar] [CrossRef]
- Haase, C.; Bergmann, R.; Fuechtner, F.; Hoepping, A.; Pietzsch, J. L-Type Amino Acid Transporters LAT1 and LAT4 in Cancer: Uptake of 3-O-Methyl-6- 18F-Fluoro-L-Dopa in Human Adenocarcinoma and Squamous Cell Carcinoma In Vitro and In Vivo. J. Nucl. Med. 2007, 48, 2063–2071. [Google Scholar] [CrossRef]
- Xie, X.-L.; Kakehashi, A.; Wei, M.; Yamano, S.; Takeshita, M.; Yunoki, T.; Wanibuchi, H. l-Leucine and l-isoleucine enhance growth of BBN-induced urothelial tumors in the rat bladder by modulating expression of amino acid transporters and tumorigenesis-associated genes. Food Chem. Toxicol. 2013, 59, 137–144. [Google Scholar] [CrossRef]
- Patel, M.; Dalvi, P.; Gokulgandhi, M.; Kesh, S.; Kohli, T.; Pal, D.; Mitra, A.K. Functional characterization and molecular expression of large neutral amino acid transporter (LAT1) in human prostate cancer cells. Int. J. Pharm. 2013, 443, 245–253. [Google Scholar] [CrossRef]
- Martinez, R.S.; Salji, M.J.; Rushworth, L.; Ntala, C.; Rodriguez Blanco, G.; Hedley, A.; Clark, W.; Peixoto, P.; Hervouet, E.; Renaude, E. SLFN5 Regulates LAT1-Mediated mTOR Activation in Castration-Resistant Prostate CancerSLFN5 Regulates LAT1 in CRPC. Cancer Res. 2021, 81, 3664–3678. [Google Scholar] [CrossRef]
- Wang, Q.; Grkovic, T.; Font, J.; Bonham, S.; Pouwer, R.H.; Bailey, C.G.; Moran, A.M.; Ryan, R.M.; Rasko, J.E.; Jormakka, M.; et al. Monoterpene Glycoside ESK246 from Pittosporum Targets LAT3 Amino Acid Transport and Prostate Cancer Cell Growth. ACS Chem. Biol. 2014, 9, 1369–1376. [Google Scholar] [CrossRef]
- Yue, M.; Jiang, J.; Gao, P.; Liu, H.; Qing, G. Oncogenic MYC Activates a Feedforward Regulatory Loop Promoting Essential Amino Acid Metabolism and Tumorigenesis. Cell Rep. 2017, 21, 3819–3832. [Google Scholar] [CrossRef]
- Zhang, B.; Chen, Y.; Shi, X.; Zhou, M.; Bao, L.; Hatanpaa, K.J.; Patel, T.; DeBerardinis, R.J.; Wang, Y.; Luo, W. Regulation of branched-chain amino acid metabolism by hypoxia-inducible factor in glioblastoma. Cell. Mol. Life Sci. 2020, 78, 195–206. [Google Scholar] [CrossRef]
- Sakata, T.; Ferdous, G.; Tsuruta, T.; Satoh, T.; Baba, S.; Muto, T.; Ueno, A.; Kanai, Y.; Endou, H.; Okayasu, I. L-type amino-acid transporter 1 as a novel biomarker for high-grade malignancy in prostate cancer. Pathol. Int. 2009, 59, 7–18. [Google Scholar] [CrossRef]
- Wang, L.; Qu, W.; Lieberman, B.P.; Plössl, K.; Kung, H.F. Synthesis, uptake mechanism characterization and biological evaluation of 18F labeled fluoroalkyl phenylalanine analogs as potential PET imaging agents. Nucl. Med. Biol. 2011, 38, 53–62. [Google Scholar] [CrossRef]
- Laudicella, R.; Albano, D.; Alongi, P.; Argiroffi, G.; Bauckneht, M.; Baldari, S.; Bertagna, F.; Boero, M.; De Vincentis, G.; Del Sole, A.; et al. 18F-Facbc in Prostate Cancer: A Systematic Review and Meta-Analysis. Cancers 2019, 11, 1348. [Google Scholar] [CrossRef]
- Wiriyasermkul, P.; Moriyama, S.; Kongpracha, P.; Nagamori, S. Drug Discovery Targeting an Amino Acid Transporter for Diagnosis and Therapy. Yakugaku Zasshi 2021, 141, 501–510. [Google Scholar] [CrossRef]
- Baniasadi, S.; Chairoungdua, A.; Iribe, Y.; Kanai, Y.; Endou, H.; Aisaki, K.-I.; Igarashi, K.; Kanno, J. Gene expression profiles in t24 human bladder carcinoma cells by inhibiting an l-type amino acid transporter, lat1. Arch. Pharmacal Res. 2007, 30, 444–452. [Google Scholar] [CrossRef]
- Morimoto, E.; Kanai, Y.; Kim, D.K.; Chairoungdua, A.; Choi, H.W.; Wempe, M.F.; Anzai, N.; Endou, H. Establishment and Characterization of Mammalian Cell Lines Stably Expressing Human L-Type Amino Acid Transporters. J. Pharmacol. Sci. 2008, 108, 505–516. [Google Scholar] [CrossRef]
- Oda, K.; Hosoda, N.; Endo, H.; Saito, K.; Tsujihara, K.; Yamamura, M.; Sakata, T.; Anzai, N.; Wempe, M.F.; Kanai, Y.; et al. l-Type amino acid transporter 1 inhibitors inhibit tumor cell growth. Cancer Sci. 2009, 101, 173–179. [Google Scholar] [CrossRef]
- Rosilio, C.; Nebout, M.; Imbert, V.; Griessinger, E.; Neffati, Z.; Benadiba, J.; Hagenbeek, T.; Spits, H.; Reverso, J.; Ambrosetti, D. L-type amino-acid transporter 1 (LAT1): A therapeutic target supporting growth and survival of T-cell lymphoblastic lym-phoma/T-cell acute lymphoblastic leukemia. Leukemia 2015, 29, 1253–1266. [Google Scholar] [CrossRef]
- Okano, N.; Naruge, D.; Kawai, K.; Kobayashi, T.; Nagashima, F.; Endou, H.; Furuse, J. First-in-human phase I study of JPH203, an L-type amino acid transporter 1 inhibitor, in patients with advanced solid tumors. Investig. New Drugs 2020, 38, 1495–1506. [Google Scholar] [CrossRef]
- Kongpracha, P.; Nagamori, S.; Wiriyasermkul, P.; Tanaka, Y.; Kaneda, K.; Okuda, S.; Ohgaki, R.; Kanai, Y. Structure-activity relationship of a novel series of inhibitors for cancer type transporter L-type amino acid transporter 1 (LAT1). J. Pharmacol. Sci. 2017, 133, 96–102. [Google Scholar] [CrossRef]
- Nagamori, S.; Wiriyasermkul, P.; Okuda, S.; Kojima, N.; Hari, Y.; Kiyonaka, S.; Mori, Y.; Tominaga, H.; Ohgaki, R.; Kanai, Y. Structure–activity relations of leucine derivatives reveal critical moieties for cellular uptake and activation of mTORC1-mediated signaling. Amino Acids 2016, 48, 1045–1058. [Google Scholar] [CrossRef]

| LATs | PCa Cell Lines | Up-Regulation of Expression | Inhibitors | Be Inhibited Effects | Diagnosis/Treatment |
|---|---|---|---|---|---|
| LAT1 [23,33,41,43,50,53,61] | LNCAP | ↑/— | T3, BCH, JPH 203, ESK242, SKN, OKY-034 | Lower proliferation, Higher apoptosis, Lower leucine absorption, Lower mTORC1 activity, Amino acid stress, Reduced tumor metastasis ability. | Used as a PET tracer transporter in the diagnosis of malignant tumors. As a target for targeted therapy. |
| C4-2 | ↑ | ||||
| PC3 | ↑ | ||||
| DU145 | ↑ | ||||
| VCAP | ↑ | ||||
| 22Rv1 | ↑ | ||||
| LAT2 [55,56] | prostate specimen | ↑ | BCH | N/A | Associated with a better prognosis. |
| LAT3 [5,41,51,53,54,62,63] | LNCAP | ↑ | ESK242, ESK246 | Lower proliferation, higher apoptosis, Reduced tumor metastasis ability. | As a tumor marker for HSPC to CRPC transformation, As a targeted therapeutic target. |
| C4-2 | ↑ | ||||
| PC3 | — | ||||
| DU145 | — | ||||
| LAT4 [42,52,58,59] | 22Rv1 (Simulate the CRPC situation) | ↑ | N/A | Growth retardation in mouse models. | Possible as a PET tracer target for 18F-labeled amino acids in CRPC. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, X.; Sakamoto, S.; Wei, J.; Pae, S.; Saito, S.; Sazuka, T.; Imamura, Y.; Anzai, N.; Ichikawa, T. Contribution of the L-Type Amino Acid Transporter Family in the Diagnosis and Treatment of Prostate Cancer. Int. J. Mol. Sci. 2023, 24, 6178. https://doi.org/10.3390/ijms24076178
Zhao X, Sakamoto S, Wei J, Pae S, Saito S, Sazuka T, Imamura Y, Anzai N, Ichikawa T. Contribution of the L-Type Amino Acid Transporter Family in the Diagnosis and Treatment of Prostate Cancer. International Journal of Molecular Sciences. 2023; 24(7):6178. https://doi.org/10.3390/ijms24076178
Chicago/Turabian StyleZhao, Xue, Shinichi Sakamoto, Jiaxing Wei, Sangjon Pae, Shinpei Saito, Tomokazu Sazuka, Yusuke Imamura, Naohiko Anzai, and Tomohiko Ichikawa. 2023. "Contribution of the L-Type Amino Acid Transporter Family in the Diagnosis and Treatment of Prostate Cancer" International Journal of Molecular Sciences 24, no. 7: 6178. https://doi.org/10.3390/ijms24076178
APA StyleZhao, X., Sakamoto, S., Wei, J., Pae, S., Saito, S., Sazuka, T., Imamura, Y., Anzai, N., & Ichikawa, T. (2023). Contribution of the L-Type Amino Acid Transporter Family in the Diagnosis and Treatment of Prostate Cancer. International Journal of Molecular Sciences, 24(7), 6178. https://doi.org/10.3390/ijms24076178








