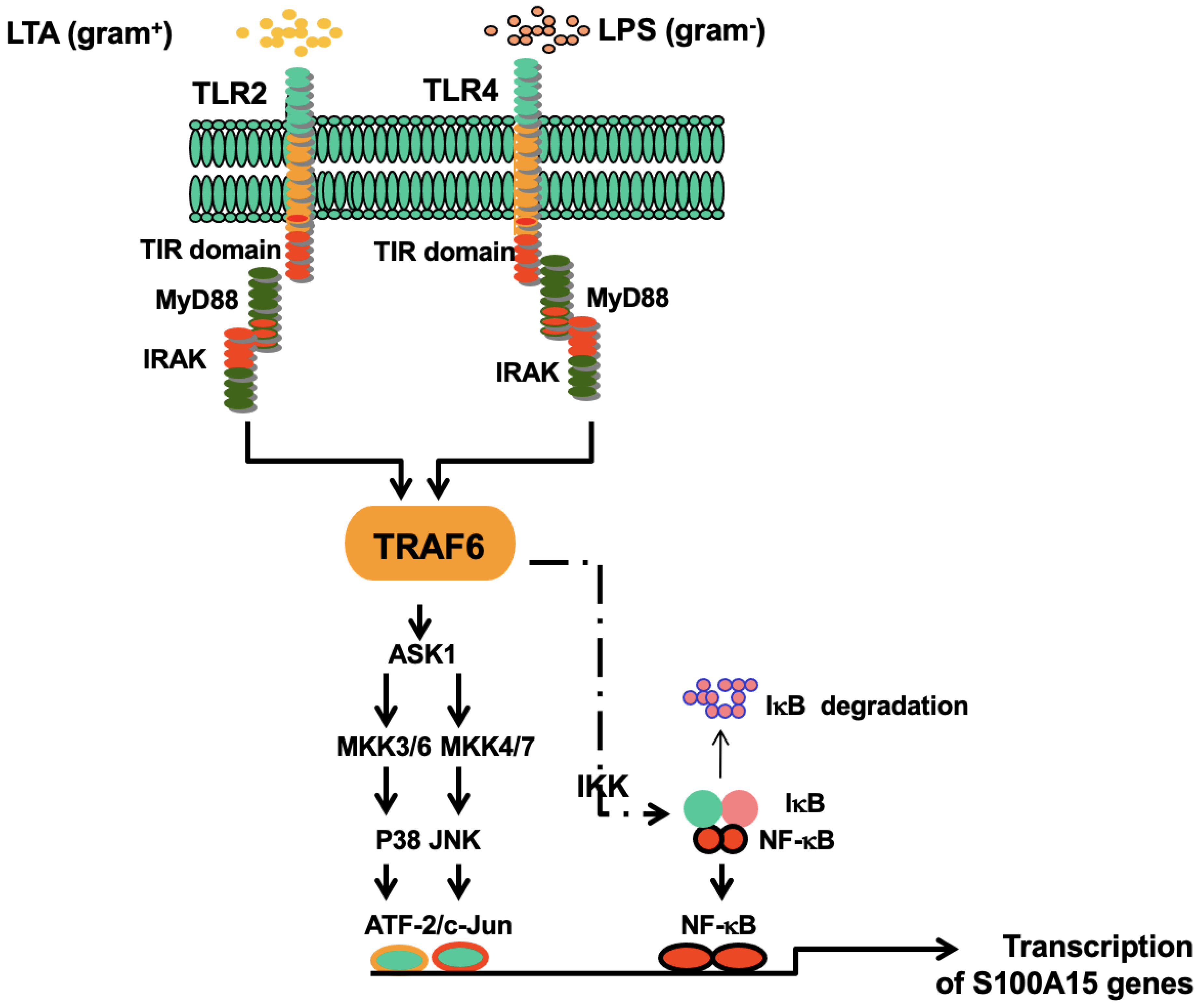
Induction of Antimicrobial Protein S100A15 Expression by Oral Microbial Pathogens Is Toll-like Receptors-Dependent Activation of c-Jun-N-Terminal Kinase (JNK), p38, and NF-κB Pathways
Abstract
1. Introduction
2. Results
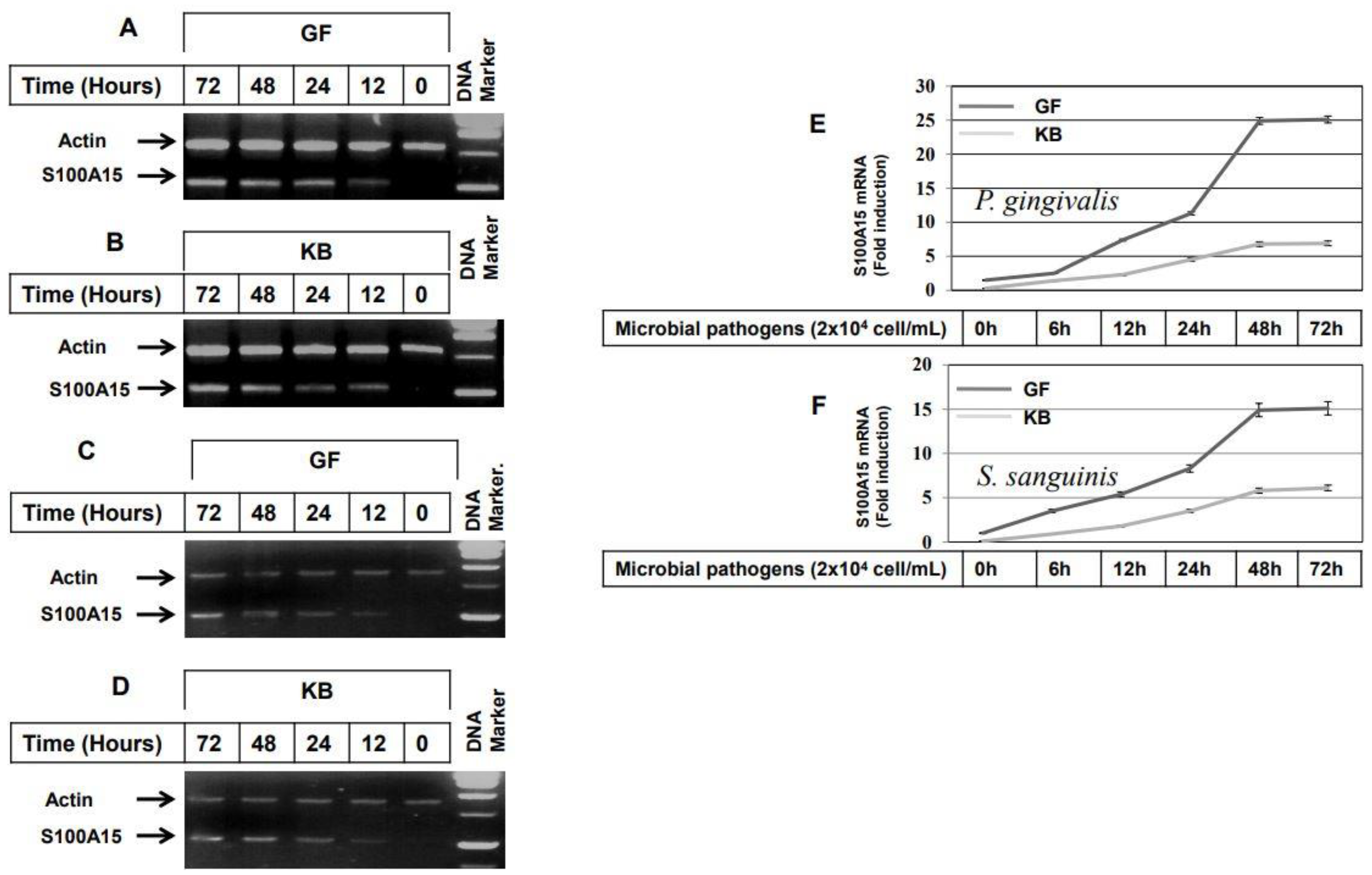
2.1. Induction of the Antimicrobial Protein S100A15 by LPS, LTA, and Bacterial Pathogens in Both GF and KB Cells
2.2. Bacterial Pathogens-Induced Expression of S100A15 in Oral Mucosa via Toll-Like Receptor-Dependent Mechanism
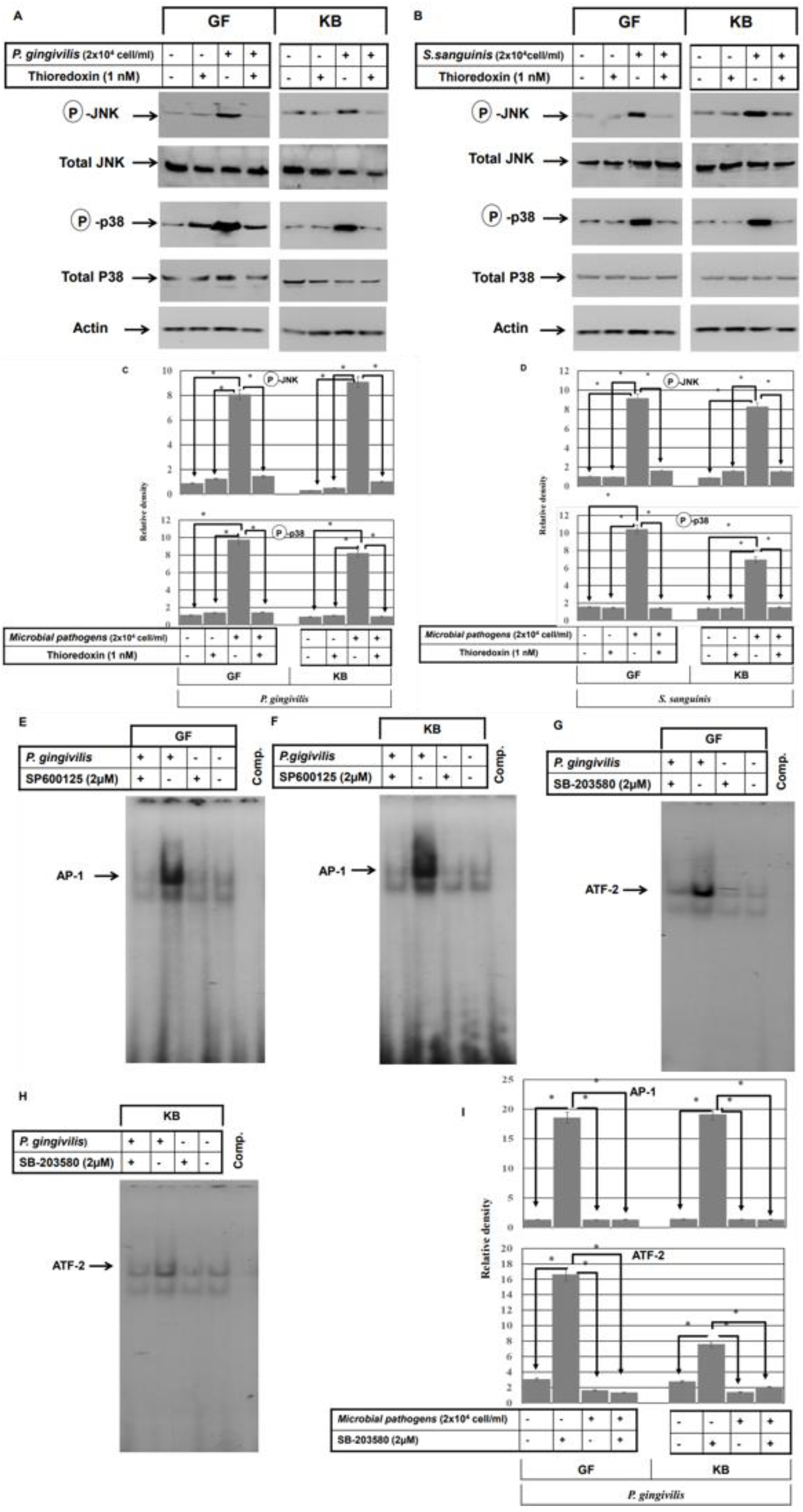
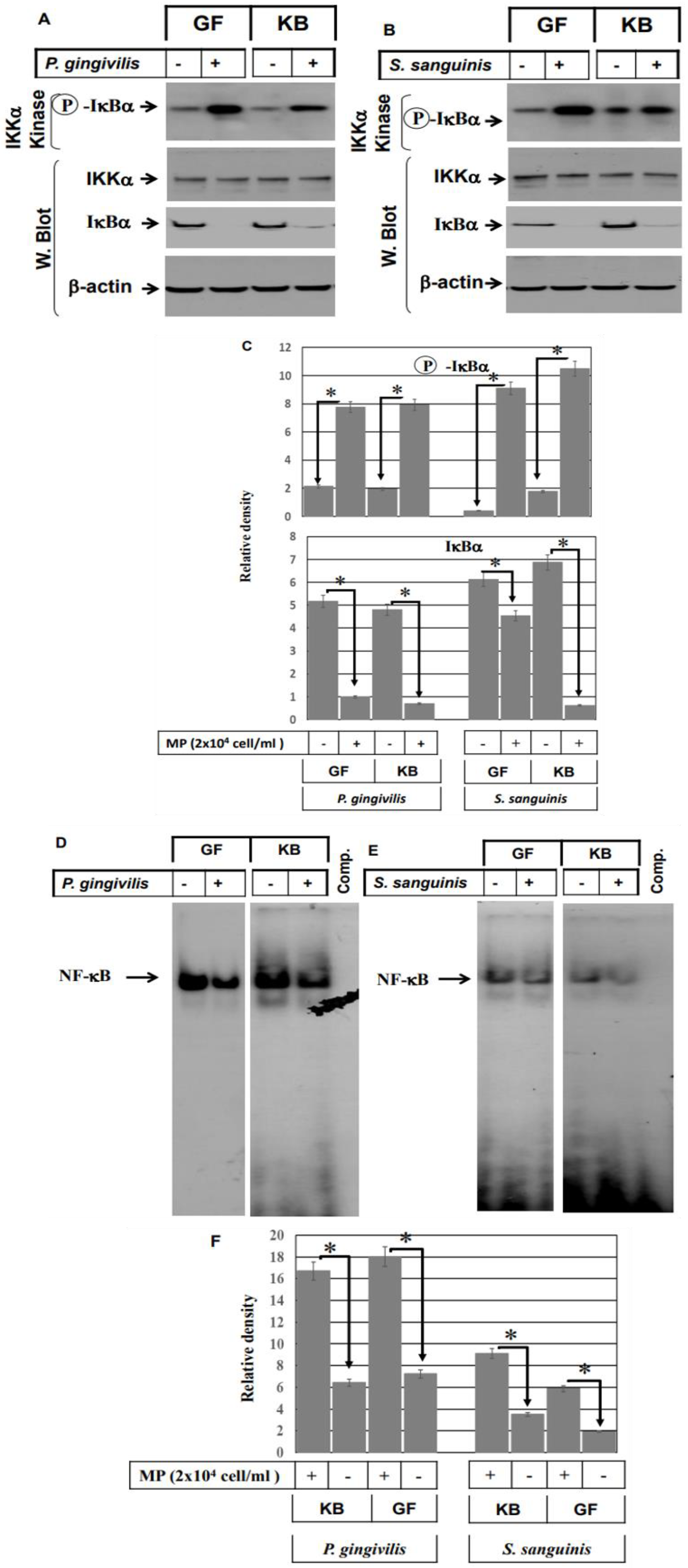
2.3. Activation of ASK1 and NF-kB Pathways in Oral Mucosa-Derived Cells by Both Gram− and Gram+ Bacterial Pathogens
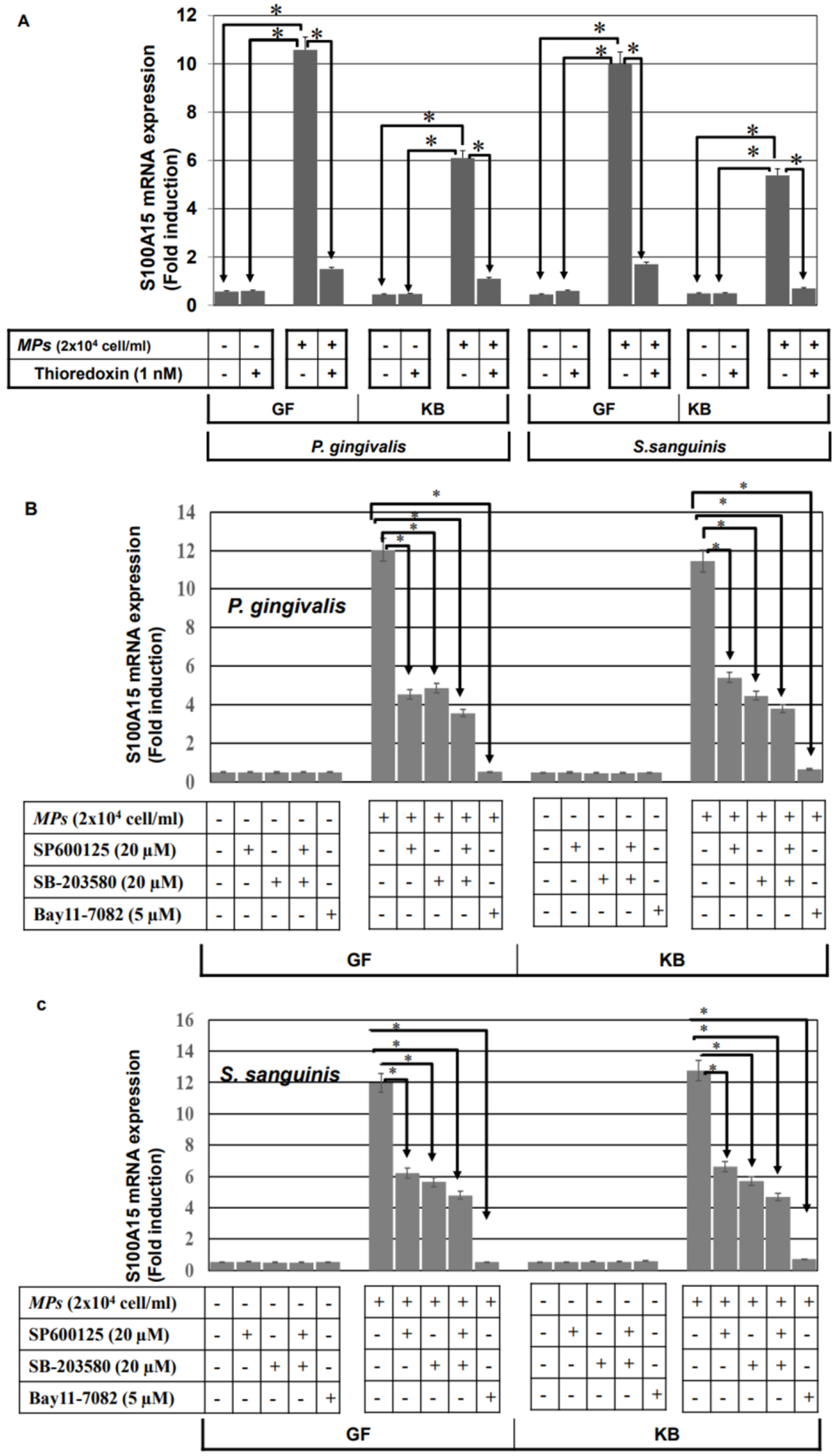
2.4. ASK1-JNK, ASK1-p38, and NF-κB Pathways Are Involved in the Modulation of Bacterial Pathogens-Induced Expression of S100A15 in Oral Mucosa
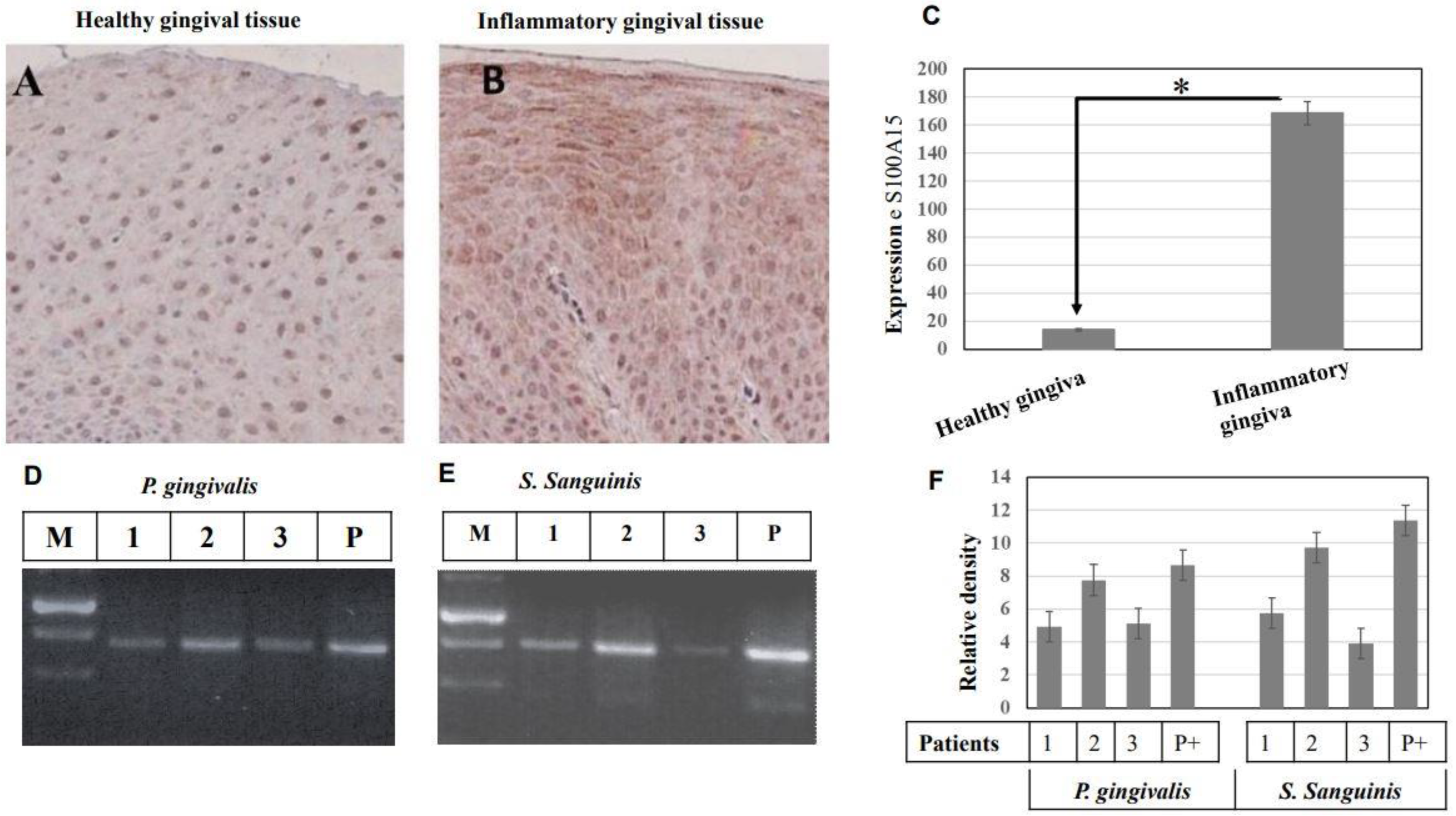
2.5. Verification of the Clinical Validity of Both Gram− and Gram+ Bacterial Pathogens-Induced Expression of S100A15 Protein
3. Discussion
4. Materials and Methods
4.1. Stimulation of Oral Mucosa-Derived Cells Lines by LPS, LTA, and Bacterial Pathogens
4.2. RNA Preparation, Semiquantitative and Real-Time PCR
4.3. Immunoblot
4.4. Preparation of Nuclear Extracts
4.5. Protein Extraction and Enzyme-Linked Immunosorbent Assay (ELISA)
4.6. Electrophoretic Mobility Shift Assay (EMSA)
4.7. In Vitro Kinase Assays
4.8. Collection and Processing of Saliva Samples for PCR
4.9. Amplification of PCR
4.10. Immune Histochemistry
4.11. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Ma, N.; Zhu, L.; Yang, L.; Cui, Y.; Zhan, Y. Prognostic values of S100 family mRNA expression in ovarian cancer. Cancer Biomark. 2019, 25, 67–78. [Google Scholar] [CrossRef] [PubMed]
- Xiong, T.F.; Pan, F.Q.; Li, D. Expression and clinical significance of S100 family genes in patients with melanoma. Melanoma Res. 2019, 29, 23–29. [Google Scholar] [CrossRef]
- Wang, X.; Sun, Z.; Tian, W.; Piao, C.; Xie, X.; Zang, J.; Peng, S.; Yu, X.; Wang, Y. S100A12 is a promising biomarker in papillary thyroid cancer. Sci. Rep. 2020, 10, 1724. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.Y.; Jin, J.; Huang, J.; Li, P.; Xue, J.W.; Wu, X.J.; He, Z.X. Expression and clinical significance profile analysis of S100 family members in human acute myeloid leukemia. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 7324–7334. [Google Scholar] [PubMed]
- Verma, R.; Verma, P.; Budhwar, S.; Singh, K. S100 proteins: An emerging cynosure in pregnancy & adverse reproductive outcome. Indian J. Med. Res. 2018, 148 (Suppl. S1), S100–S106. [Google Scholar] [PubMed]
- Gonzalez, L.L.; Garrie, K.; Turner, M.D. Role of S100 proteins in health and disease. Biochim. Biophys Acta Mol. Cell Res. 2020, 1867, 118677. [Google Scholar] [CrossRef]
- Donato, R.; Cannon, B.R.; Sorci, G.; Riuzzi, F.; Hsu, K.; Weber, D.J.; Geczy, C.L. Functions of S100 proteins. Curr. Mol. Med. 2013, 13, 24–57. [Google Scholar] [CrossRef]
- Broome, A.M.; Ryan, D.; Eckert, R.L. S100 protein subcellular localization during epidermal differentiation and psoriasis. J. Histochem. Cytochem. 2003, 51, 675–685. [Google Scholar] [CrossRef]
- Eckert, R.L.; Broome, A.M.; Ruse, M.; Robinson, N.; Ryan, D.; Lee, K. S100 proteins in the epidermis. J. Investig. Dermatol. 2004, 123, 23–33. [Google Scholar] [CrossRef]
- Emberley, E.D.; Murphy, L.C.; Watson, P.H. S100 proteins and their influence on pro-survival pathways in cancer. Biochem. Cell Biol. 2004, 82, 508–515. [Google Scholar] [CrossRef]
- Marenholz, I.; Heizmann, C.W.; Fritz, G. S100 proteins in mouse and man: From evolution to function and pathology (including an update of the nomenclature). Biochem. Biophys. Res. Commun. 2004, 322, 1111–1122. [Google Scholar] [CrossRef] [PubMed]
- Prantner, D.; Nallar, S.; Vogel, N.S. The role of RAGE in host pathology and crosstalk between RAGE and TLR4 in innate immune signal transduction pathways. FASEB J. 2020, 34, 15659–15674. [Google Scholar] [CrossRef]
- Büchau, A.S.; Hassan, M.; Kukova, G.; Lewerenz, V.; Kellermann, S.; Würthner, J.U.; Wolf, R.; Walz, M.; Gallo, R.L.; Ruzicka, T. S100A15, an antimicrobial protein of the skin: Regulation by E. coli through Toll-like receptor 4. J. Investig. Dermatol. 2007, 127, 2596–2604. [Google Scholar] [CrossRef] [PubMed]
- Dale, B.A.; Fredericks, L.P. Antimicrobial peptides in the oral environment: Expression and function in health and disease. Curr. Issues Mol. Biol. 2005, 7, 119–133. [Google Scholar] [PubMed]
- Reddy, K.V.R.; Yedery, R.D.; Aranha, C. Antimicrobial peptides: Premises and promises. Int. J. Antimicrob. Agents 2004, 24, 536–547. [Google Scholar] [CrossRef]
- Kurpe, S.R.; Grishin, S.Y.; Surin, A.K.; Panfilov, A.V.; Slizen, M.V.; Chowdhury, S.D.; Galzitskaya, O.V. Antimicrobial and Amyloidogenic Activity of Peptides. Can Antimicrobial Peptides Be Used against SARS-CoV-2? Int. J. Mol. Sci. 2020, 21, 9552. [Google Scholar] [CrossRef]
- Malanovic, N.; Lohner, K. Antimicrobial Peptides Targeting Gram-Positive Bacteria. Pharmaceuticals 2016, 9, 59. [Google Scholar] [CrossRef]
- Malanovic, N.; Lohner, K. Gram-positive bacterial cell envelopes: The impact on the activity of antimicrobial peptides. Biochim. Biophys Acta 2016, 1858, 936–946. [Google Scholar] [CrossRef]
- Lehrer, R.I.; Ganz, T. Defensins of vertebrate animals. Curr. Opin. Immunol. 2002, 14, 96–102. [Google Scholar] [CrossRef]
- Hancock, R.E. Peptide antibiotics. Lancet 1997, 349, 418–422. [Google Scholar] [CrossRef]
- Schröder, N.W.; Morath, S.; Alexander, C.; Hamann, L.; Hartung, T.; Zähringer, U.; Göbel, U.B.; Weber, J.R.; Schumann, R.R. Lipoteichoic acid (LTA) of Streptococcus pneumoniae and Staphylococcus aureus activates immune cells via Toll-like receptor (TLR)-2, lipopolysaccharide-binding protein (LBP), and CD14, whereas TLR-4 and MD-2 are not involved. J. Biol. Chem. 2003, 278, 15587–15594. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.T.; Huang, K.H.; Chiang, J.Y.; Sung, P.H.; Huang, C.R.; Chu, Y.C.; Chuang, F.C.; Yip, H.K. Extracorporeal Shock Wave Therapy Protected the Functional and Architectural Integrity of Rodent Urinary Bladder against Ketamine-Induced Damage. Biomedicines 2021, 9, 1391. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.; Xiong, Y.; Pattabiraman, G.; Qiu, F.; Medvedev, A.E. Pellino-1 Positively Regulates Toll-like Receptor (TLR) 2 and TLR4 Signaling and Is Suppressed upon Induction of Endotoxin Tolerance. J. Biol. Chem. 2015, 290, 19218–19232. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Huang, J.; Guo-Hua, F. Expression of DUSP12 Reduces Lung Vascular Endothelial Cell Damage in a Murine Model of Lipopolysaccharide-Induced Acute Lung Injury via the Apoptosis Signal-Regulating Kinase 1 (ASK1)-Jun N-Terminal Kinase Activation (JNK) Pathway. Med. Sci. Monit. 2021, 27, e930429. [Google Scholar]
- Zheng, R.; You, Z.; Jia, J.; Lin, S.; Han, S.; Liu, A.; Long, H.; Wang, S. Curcumin enhances the antitumor effect of ABT-737 via activation of the ROS-ASK1-JNK pathway in hepatocellular carcinoma cells. Mol. Med. Rep. 2016, 13, 1570–1576. [Google Scholar] [CrossRef] [PubMed]
- Eversole, L.R.; Miyasaki, K.T.; Christensen, R.E. Keratinocyte expression of calprotectin in oral inflammatory mucosal diseases. J. Oral. Pathol. Med. 1993, 22, 303–307. [Google Scholar] [CrossRef]
- Büchau, A.S.; Gallo, L.R. Innate Immunity and antimicrobial defense systems in psoriasis. Clin. Dermatol. 2007, 25, 616–624. [Google Scholar] [CrossRef]
- Płóciennikowska, A.; Hromada-Judycka, A.; Borzęcka, K.; Kwiatkowska, K. Co-operation of TLR4 and raft proteins in LPS-induced pro-inflammatory signaling. Cell Mol. Life Sci. 2015, 72, 557–581. [Google Scholar] [CrossRef]
- Samanta, M.; Swain, B.; Basu, M.; Panda, P.; Mohapatra, G.B.; Sahoo, B.R.; Maiti, N.K. Molecular characterization of toll-like receptor 2 (TLR2), analysis of its inductive expression and associated down-stream signaling molecules following ligands exposure and bacterial infection in the Indian major carp, rohu (Labeo rohita). Fish Shellfish Immunol. 2012, 32, 411–425. [Google Scholar] [CrossRef]
- Sujitha, S.; Dinesh, P.; Rasool, M. Berberine modulates ASK1 signaling mediated through TLR4/TRAF2 via upregulation of miR-23a. Toxicol. Appl. Pharmacol. 2018, 359, 34–46. [Google Scholar] [CrossRef]
- Matsuzawa, A.; Nishitoh, H.; Tobiume, K.; Takeda, K.; Ichijo, H. Physiological roles of ASK1-mediated signal transduction in oxidative stress- and endoplasmic reticulum stress-induced apoptosis: Advanced findings from ASK1 knockout mice. Antioxid. Redox Signal. 2002, 3, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Sayama, K.; Komatsuzawa, H.; Yamasaki, K.; Shirakata, Y.; Hanakawa, Y.; Ouhara, K.; Tokumaru, S.; Dai, X.; Tohyama, M.; Ten Dijke, P.; et al. New mechanisms of skin innate immunity: ASK1-mediated keratinocyte differentiation regulates the expression of beta-defensins, LL37, and TLR2. Eur. J. Immunol. 2005, 35, 1886–1895. [Google Scholar] [CrossRef] [PubMed]
- Sobke, A.C.; Selimovic, D.; Orlova, V.; Hassan, M.; Chavakis, T.; Athanasopoulos, A.N.; Schubert, U.; Hussain, M.; Thiel, G.; Preissner, K.T.; et al. The extracellular adherence protein from Staphylococcus aureus abrogates angiogenic responses of endothelial cells by blocking Ras activation. FASEB J. 2006, 20, 2621–2623. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.; Ghozlan, H.; Abdel-Kader, O. Activation of c-Jun NH2-terminal kinase (JNK) signaling pathway is essential for the stimulation of hepatitis C virus (HCV) non-structural protein 3 (NS3)-mediated cell growth. Virology 2005, 333, 324–336. [Google Scholar] [CrossRef]
- Hassan, M.; Alaoui, A.; Feyen, O.; Mirmohammadsadegh, A.; Essmann, F.; Tannapfel, A.; Gulbins, E.; Schulze-Osthoff, K.; Hengge, U.R. The BH3-only member Noxa causes apoptosis in melanoma cells by multiple pathways. Oncogene 2008, 27, 4557–4568. [Google Scholar] [CrossRef]
- El Jamal, S.M.; Grada, Z.; El Dinali, M.H.; Zhou, H.; Hassan, S.Y.; Saad, A.G.; Gibson, B.; Zhou, X.; Abulsayen, H.A.; Khadra, H.S.; et al. MEF2B is a member of the BCL6 gene transcriptional complex and induces its expression in diffuse large B-cell lymphoma of the germinal center B-cell-like type. Lab. Investig. 2019, 99, 539–550. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Selimovic, D.; Kharouf, N.; Carrouel, F.; Hassan, S.-Y.; Flanagan, T.W.; Hassan, S.-L.; Megahed, M.; Haikel, Y.; Santourlidis, S.; Hassan, M. Induction of Antimicrobial Protein S100A15 Expression by Oral Microbial Pathogens Is Toll-like Receptors-Dependent Activation of c-Jun-N-Terminal Kinase (JNK), p38, and NF-κB Pathways. Int. J. Mol. Sci. 2023, 24, 5348. https://doi.org/10.3390/ijms24065348
Selimovic D, Kharouf N, Carrouel F, Hassan S-Y, Flanagan TW, Hassan S-L, Megahed M, Haikel Y, Santourlidis S, Hassan M. Induction of Antimicrobial Protein S100A15 Expression by Oral Microbial Pathogens Is Toll-like Receptors-Dependent Activation of c-Jun-N-Terminal Kinase (JNK), p38, and NF-κB Pathways. International Journal of Molecular Sciences. 2023; 24(6):5348. https://doi.org/10.3390/ijms24065348
Chicago/Turabian StyleSelimovic, Denis, Naji Kharouf, Florence Carrouel, Sofie-Yasmin Hassan, Thomas W. Flanagan, Sarah-Lilly Hassan, Mosaad Megahed, Youssef Haikel, Simeon Santourlidis, and Mohamed Hassan. 2023. "Induction of Antimicrobial Protein S100A15 Expression by Oral Microbial Pathogens Is Toll-like Receptors-Dependent Activation of c-Jun-N-Terminal Kinase (JNK), p38, and NF-κB Pathways" International Journal of Molecular Sciences 24, no. 6: 5348. https://doi.org/10.3390/ijms24065348
APA StyleSelimovic, D., Kharouf, N., Carrouel, F., Hassan, S.-Y., Flanagan, T. W., Hassan, S.-L., Megahed, M., Haikel, Y., Santourlidis, S., & Hassan, M. (2023). Induction of Antimicrobial Protein S100A15 Expression by Oral Microbial Pathogens Is Toll-like Receptors-Dependent Activation of c-Jun-N-Terminal Kinase (JNK), p38, and NF-κB Pathways. International Journal of Molecular Sciences, 24(6), 5348. https://doi.org/10.3390/ijms24065348









