THC and CBD: Villain versus Hero? Insights into Adolescent Exposure
Abstract
1. Introduction
1.1. History and Discovery of Cannabis
1.2. Epidemiology: Use of Cannabis in Adolescence
1.3. THC and CBD Pharmacology
2. Divergent Central Effects of THC and CBD
2.1. Reward and Substance Use Disorders (SUDs)
2.2. Neuropsychiatric Disorders
| Experimental Design | Doses | Results | Safety, Compliance, and Side Effects | References |
|---|---|---|---|---|
| Case report describing 6 patients (5 male; 1 female; ages 33, 24, 16, 19, 16, and 18) who developed persistent depersonalization disorder in adolescence after consuming cannabis. | Patients smoked their own cannabis | All reported cases described onset of depersonalization disorder in adolescence. In 2 of these cases, the illness course was severely disabling. | N/A | [163] |
| Participants divided into case group (cannabis users with a first episode of psychosis; n = 280, 18–65 y) and control group (healthy patients; n = 174, 18–65 y) were assessed for sociodemographic data and use of illicit drugs, including cannabis. | Patients smoked their own cannabis | Patients in the case group were more likely to be current daily users and to have smoked cannabis for more than 5 years. Among those who used cannabis, 78% of the case group used high-potency cannabis (sinsemilla, ‘skunk’) compared with 37% of the control group. | N/A | [170] |
| A randomized, double-blind, between-subjects design trial (n = 48 participants with previous cannabis use, 21–50 y). All participants were assessed at three separate time-points: (1) baseline; (2) post-CBD; and (3) post-THC. All participants were assessed for traits of paranoia, cannabis dependence, psychotic/dysphoric experiences following recreation cannabis use, positive psychotic dimension, mood, and cognitive functioning. | Capsule with CBD 600 mg (n = 22) or placebo (n = 26) 210 min ahead of intravenous THC (1.5 mg) | Clinically significant positive psychotic symptoms were less likely in the CBD group compared with the placebo group. In agreement, post-THC paranoia was less common in the CBD group compared with the placebo group. Episodic memory was poorer relative to baseline in the placebo pre-treated group compared with the CBD group. | N/A | [171] |
| A double-blind, placebo-controlled, within-subjects study (n = 26 healthy occasional cannabis users, 10 males and 16 females, mean age 23.1 y) with 4 treatment conditions separated by a minimum washout period of 7 days to avoid potential carry-over effects. The order of treatment conditions was randomized across participants. All participants were assessed for anxiety, pain, and emotional state. All drugs were self-administered by vaporisation at 200 °C. | THC-dominant cannabis (13.75 mg THC, THC 22%, and CBD < 1%), CBD-dominant cannabis (13.75 mg CBD, THC < 1% and CBD 9%), THC/CBD-equivalent cannabis (13.75 mg THC/13.75 mg CBD), or cannabis placebo (<0.2% total cannabinoid content) | Both THC and THC/CBD significantly increased self-rated state anxiety compared to placebo. State anxiety after THC/CBD was significantly lower than after THC alone. THC-induced anxiety was independent of anxiety at baseline. When baseline anxiety was low, CBD completely counteracted THC-induced anxiety; however, when baseline anxiety was high, CBD did not counteract THC-induced anxiety. There were no effects of any treatment condition on emotional state. | N/A | [173] |
| A double-blind, randomized, four-arm, within-subjects trial in which participants (n = 46 healthy infrequent cannabis users, 21–50 y) inhaled 4 different cannabis vaporized preparations (randomized, counter-balanced order, with minimum one-week wash-out period between each treatment exposure). All participants were assessed for delayed verbal recall, severity of psychotic symptoms, and cognitive, subjective, pleasurable, pharmacological, and physiological effects. | THC 10 mg—CBD 0 mg (0:1 CBD: THC), THC 10 mg—CBD 10 mg (1:1), THC 10 mg—CBD 20 mg (2:1), or THC 10 mg—CBD 30 mg (3:1) | THC (0:1) was associated with impaired delayed verbal recall and induced positive psychotic symptoms. These effects were not significantly modulated by any dose of CBD. Furthermore, there was no evidence of CBD modulating the effects of THC on other cognitive, psychotic, subjective, pleasurable, or physiological measures. | N/A | [174] |
| A double-blind, within-subjects, placebo-controlled study in university students (n = 10, 20–33 y, naive to treatment) with generalized social anxiety syndrome. All participants were assessed for severity of social phobia disorder and phobia. Regional cerebral blood flow at rest and after treatment was measured twice using Technetium-99m-labeled ethyl cysteinate dimer (ECD) single-photon emission computed tomography (SPECT). | Oral dose of CBD, 400 mg or placebo | Relative to placebo, CBD was associated with significantly decreased subjective anxiety, reduced ECD uptake in the left parahippocampal gyrus, hippocampus, and inferior temporal gyrus, and increased ECD uptake in the right posterior cingulate gyrus. | N/A | [176] |
| A double-blind randomized, placebo-controlled trial in never-treated patients (mean age 23 y) with SAD (n = 24) and healthy controls (HC, n = 12). At 6 time points during a simulation public speaking test (SPTS), all participants were assessed for mood, negative state, and physiological measures (blood pressure, heart rate, and skin conductance). | CBD 600 mg (n = 12) or placebo (n = 12) 1 h and half the SPTS test. HC (n = 12) participants did not receive any medication | Pretreatment with CBD significantly reduced anxiety, cognitive impairment, and discomfort in speech performance, and significantly decreased alertness in anticipatory speech. The placebo group presented higher anxiety, cognitive impairment, discomfort, and alert levels when compared with the HC. The increase in negative states during the testing observed in the placebo group was almost abolished in the CBD group. No significant differences were observed between CBD and HC in the cognitive impairment, discomfort, and alert factors. | N/A | [177] |
| A double-blind, placebo-controlled, between-subjects trial in which participants (n = 48, 18–35 y) were randomized to three groups (each n = 16) to receive either (1) CBD prior to extinction (CBD pre-extinction group), (2) CBD following extinction (CBD post-extinction group), or (3) placebo (placebo group). In this study a sub-anxiolytic CBD dose was used. All drugs were vaporized at 210 °C and administered via a Volcano Medic vaporizer. At recall, 48 h later, in the conditioning session, all participants were exposed to conditioned stimuli and conditioning contexts before (recall) and after (reinstatement) exposure to the unconditioned stimulus. Skin conductance and shock expectancy measures of conditioned responding were recorded throughout. All participants were assessed for depressive symptoms, trait anxiety, verbal IQ, and non-emotional explicit memory. | 32 mg of inhaled CBD prior to extinction (CBD pre-extinction group), 32 mg of inhaled CBD following extinction (CBD post-extinction group) or placebo | CBD given post-extinction enhanced consolidation of extinction learning as assessed by shock expectancy. CBD administered at either time produced trend-level reduction in reinstatement of autonomic contextual responding. No acute effects of CBD were found on extinction. | N/A | [178] |
| A double blind, randomized trial in patients diagnosed with PTSD (n = 33 of both sexes, 18–60 y) treated with CBD or placebo. In the first experimental section, all participants were matched by sex, age, body mass index, and PTSD symptoms. On the same day, participants prepared the behavior test, recording accounts of their traumas in digital audio for a minute and a half and then imagining the trauma for 30 s. After 7 days, participants were treated (CBD or placebo) before performing the behavioral test, listening to the trauma account and imagining themselves in that situation. Before and after the behavioral test, all participants were assessed for subjective changes in mood and anxiety, physiological correlates of anxiety (blood pressure, heart rate, and salivary cortisol). Seven days later, participants underwent the same procedures as in the previous session, but without the pharmacological intervention, to assess the effect on reconsolidation of traumatic memories. | CBD 300 mg (n = 17) or placebo (n = 16) | CBD significantly attenuated the cognitive impairment effect that persisted 1 week after drug administration. No significant differences between the effects of CBD and placebo on anxiety, alertness, and discomfort induced by the recall of the traumatic event during the pharmacological intervention and in the subsequent week. There were no significant differences between the CBD and placebo groups regarding physiological data. | N/A | [181] |
| An open-label stage of clinical trial phase 2 (NCT02548559) autoregressive linear modeling assessed efficacy and tolerability of 4-week treatment with high-CBD sublingual solution in 14 outpatients with moderate-to-severe anxiety. Secondary outcomes: at baseline and week 4, patients were assessed for mood, depressive symptoms, sleep disturbance, sexual function, quality of life, and cognitive functions (battery of cognitive tests). | 1 mL t.i.d of high-CBD sublingual solution (CBD 9.97 mg/mL, THC 0.23 mg/mL) | Significant improvement in primary outcomes measuring anxiety and secondary outcomes assessing mood, sleep, quality of life, and cognition (specifically executive function) following treatment. Anxiety was significantly reduced at week 4 relative to baseline. Clinically significant treatment response (≥15% symptom reduction) was achieved and maintained as early as week 1 in most patients; cumulative frequency of treatment responders reached 100% by week 3. | The study drug was well-tolerated, with high adherence/patient retention and no reported intoxication or serious adverse events. Minor side effects, including sleepiness/fatigue, increased energy, and dry mouth, were infrequently endorsed. | [182] |
| A double-blind, randomized, placebo-controlled study in 15 healthy men (18–35 y) who had used cannabis 15 times or fewer in their life. Regional brain activation (blood-oxygenation-level-dependent response), electro-dermal activity (skin conductance response, SCR), and objective and subjective ratings of anxiety were assessed after treatment. All participants were assessed for cannabis and other illicit substance use and underwent urine drug screen analyses prior to each session. Periodic (at baseline and at 1, 2, and 3 h post-administration) psychopathological ratings of mood, anxiety, intoxication, and psychotic symptoms were collected for all participants. | Gelatin capsule with THC 10 mg, CBD 600 mg, or placebo | THC increased anxiety, as well as levels of intoxication, sedation, and psychotic symptoms, whereas there was a trend for a reduction in anxiety following administration of CBD. The number of SCR fluctuations during the processing of intensely fearful faces increased following administration of THC but decreased following administration of CBD. CBD attenuated blood oxygenation-level-dependent signaling in the amygdala and the anterior and posterior cingulate cortex while subjects were processing intensely fearful faces, and its suppression of the amygdalar and anterior cingulate responses was correlated with a concurrent reduction in SCR fluctuations. THC mainly modulated activation in frontal and parietal areas. | No serious adverse events (deaths, hospitalizations, or emergency department visits) occurred during the study. Three subjects from the original samples (n = 18) had a psychotic reaction to THC administration and were excluded since they were unable to perform the tests (final sample, n = 15). These subjects were followed up for 24 h until the psychotic symptoms relieved. They were further monitored monthly and remained well, with no psychiatric or clinical symptoms. | [183] |
| A double-blind, randomized, placebo-controlled crossover study of acute oral challenge of CBD in 24 healthy participants (12 male, 12 female, 18–70 y) on emotional processing, with neuroimaging (viewing emotional faces during functional magnetic resonance imaging) and cognitive (emotional appraisal) measures, as well as subjective response to experimentally induced anxiety. | CBD 600 mg or placebo | CBD did not produce effects on brain responses to emotional faces and cognitive measures of emotional processing or modulate experimentally induced anxiety relative to placebo. | N/A | [184] |
| A double-blind, randomized, placebo-controlled trial in patients (n = 80, 18–65 y) with panic disorder with agoraphobia or social anxiety disorder. All participants were exposed to 8 therapist-assisted exposure in vivo sessions (weekly, outpatient) under the treatment condition. The Fear Questionnaire (FQ) was assessed at baseline, mid- and post-treatment, and at 3- and 6-month follow-ups. | Oral CBD 300 mg (n = 39) or placebo (n = 41) | No differences were found in treatment outcomes over time between CBD and placebo groups in terms of FQ scores. | Incidence of adverse effects was equal in the CBD and placebo conditions. | [185] |
| A double-blind parallel, randomized, placebo-controlled study in healthy college students (n = 32) who self-reported moderate-to-severe levels of test anxiety (TA). This study tested single oral-administration doses of CBD, compared to placebo, for reducing test anxiety (TA) in a researcher-derived experimental analog. After treatment, all participants completed a statistics examination, and measures of TA and general anxiety were assessed during examination administration. | CBD (150, 300, or 600 mg) or placebo | No effect of CBD dose on self-reported TA or general anxiety. | N/A | [186] |
| An exploratory double-blind, randomized, parallel group, placebo-controlled trial in patients (n = 88, 18–65 y) with schizophrenia or related psychotic disorders. Patients were randomized to receive CBD or placebo alongside their existing antipsychotic medication. All participants were assessed before and after treatment for mood, psychotic symptoms, cognitive functions, and improvement in clinical state. | CBD 1000 mg/day (n = 43) or placebo (n = 45) for 6 weeks | After 6 weeks of treatment, compared with the placebo group, the CBD group had lower levels of positive psychotic symptoms and were more likely to have been rated as improved and as not severely unwell by the treating clinician. Patients who received CBD also showed greater improvements in cognitive performance and in overall functioning. | CBD was well-tolerated, and rates of adverse events were similar between the CBD and placebo groups. | [187] |
| A parallel group, randomized, placebo-controlled study in stable antipsychotic-treated patients (n = 36, 18–65 y) diagnosed with chronic schizophrenia. Patients were randomized to receive CBD or placebo augmentation. All participants were assessed for cognitive functions (at baseline and at end of 6 weeks of treatment) and psychotic symptoms (at baseline and biweekly). | CBD 600 mg/day or placebo for 6 weeks | CBD treatment was ineffective on psychotic symptoms and on cognitive functioning. | Side effects were similar between CBD and placebo, with the one exception being sedation, which was more prevalent in the CBD group. | [190] |
| A therapeutic exploratory (phase II, NCT00628290), double-blinded, monocenter, randomized, parallel-group, controlled clinical trial of CBD vs. amisulpride efficacy in patients (n = 39, 18–59 y) with diagnosis of schizophrenia or schizophreniform psychosis. All participants were assessed for psychotic symptoms, and measurements of serum prolactin and body weight were taken. Safety measures included repeated electrocardiograms as well as routine blood parameters. | CBD (200–800 mg/day) or amisulpride (200–800 mg/day), 28 days of treatment | Patients undergoing either CBD or amisulpride treatment showed significant clinical improvement (reduction in psychotic and other symptoms of schizophrenia). No significant differences in the clinical effects between treatments were observed. | Both treatments were safe and led to significant clinical improvement, but CBD displayed a markedly superior side-effect profile. Compared with amisulpride, CBD was associated with significantly fewer extrapyramidal symptoms, less weight gain, and lower prolactin increase. Furthermore, CBD was well-tolerated and did not significantly affect hepatic or cardiac functions. | [188] |
| A randomized, placebo-controlled trial to examine the acute effects of THC and CBD alone and in combination in frequent and infrequent cannabis users. Thirty-six participants (31 male, 18–51 y) were subsequently divided into groups of frequent cannabis users (n = 18, 17 male, 21–44 y) and infrequent users/non-naive nonusers (n = 18, 14 male, 18–51 y). All participants were objectively and subjectively assessed for intoxication (primary outcomes). Additional indices of intoxication were assessed (psychiatric symptoms, depression, and anxiety). | THC (8 mg), high CBD (400 mg), THC + low CBD (THC: 8 mg, CBD: 4 mg), THC + high-CBD (THC: 12 mg; CBD: 400 mg) or placebo (ethanol vehicle 400 μL). Five vaporization sessions, with a 1-week washout between | CBD showed some intoxicating properties relative to placebo. Both frequent and infrequent users subjectively reported feeling intoxicated by high-dose CBD administered alone (i.e., not combined with THC), with protracted effects across the 3 h session relative to placebo, but this was not corroborated by the objective intoxication measure. Low doses of CBD when combined with THC enhanced, while high doses of CBD reduced the intoxicating effects of THC. The enhancement of intoxication by low-dose CBD was particularly prominent in infrequent cannabis users and was consistent across objective and subjective measures. | See results | [195] |
| An open-label trial, in young people (n = 31, 12–25 y) with anxiety disorder and no clinical improvement despite treatment with cognitive–behavioral therapy and/or antidepressant medication. All participants received additional CBD treatment. The primary outcome was improvement in anxiety severity at week 12. Secondary outcomes included comorbid depressive symptoms and social and occupational functioning. | CBD treatment on a fixed–flexible schedule (titrated up to 800 mg/d) for 12 weeks | CBD decreased anxiety from baseline to week 12 (−42.6%). Depressive symptoms and functioning improved significantly. | Adverse events were reported in 25 (80.6%) of 31 participants and included fatigue, low mood, and hot flushes or cold chills. There were no serious and/or unexpected adverse events. | [209] |
| A 21 y longitudinal study of a birth cohort (New Zeland). Participants were annually assessed for frequency of cannabis use (from 14 to 21 y), and for psychosocial outcomes including property/violent crime, depression, suicidal ideation, suicide attempt, and other illicit drug use. | Patients smoked their own cannabis | Association between frequency of cannabis use and all outcomes, particularly other illicit drug use. Age-related variation in the strength of association between cannabis use and crime, suicidal behaviors, and other illicit drug use, with younger (14–15 y) users being more affected by regular cannabis use than older (20–21 y) regular users. Association between cannabis use and depression did not vary with age. | N/A | [153] |
| A 6 y cohort study (7 wave) (Australia); 1601 students (14–15 y). Participants were assessed for measure of depression and anxiety at wave 7 (age 21 y). | Patients smoked their own cannabis | 60% of participants had used cannabis by the age of 20; 7% were daily users at that point. Daily use in young women was associated with a more than 5-fold increase in the odds of reporting of depression and anxiety. Weekly or more frequent cannabis use in teenagers predicted approximately 2-fold increase in risk for later depression and anxiety. Depression and anxiety in teenagers predicted neither later weekly nor daily cannabis use. | N/A | [154] |
| A 21 y longitudinal study of a birth cohort (n= 3239) (Australian). All participants were interviewed to assess depression and anxiety using at age 14 y and at age 21 y. | Patients smoked their own cannabis | Those who used cannabis before age 15 y and used it frequently at 21 y were more likely to report symptoms of anxiety and depression in early adulthood. This association was of similar magnitude for those who had only used cannabis and those who reported having used cannabis and other illicit drugs. | N/A | [156] |
| A logistic regression analysis of data from the 1992 NLAES study (n = 42,862 young adults, 18–29 y) (USA). Participants were assessed for drug dependence, depression, and sociodemographic factors. | Patients smoked their own cannabis | The risk of cannabis abuse and dependence was found to increase with the frequency of smoking occasions and slightly decreased with age. More severe comorbidity was associated with dependence compared to abuse, suggesting that cannabis might be used to self-medicate major depression. The strength of the association between cannabis use and abuse was also increased as a function of the number of joints smoked among females, but not males. With respect to cannabis abuse, the odds for abuse were approximately 2 times greater among males than females. The odds of dependence were 2.6 times greater among those respondents with comorbid major depression, 2.2 times greater among respondents with a comorbid drug use disorder, and 2.7 times greater among respondents with comorbid alcohol dependence compared to those not so classified. Sex was found to modify the use ± abuse relationship—the number of joints smoked per smoking occasion increased the risk for abuse, but only among females. The odds of abuse were 2.4 times greater among females who smoked on average two joints per occasion compared to those who smoked 0.50 joints on a typical occasion. For females who smoked on average eight joints per occasion, the odds of cannabis abuse were 5.5 times greater relative to the odds of smoking joints per occasion. | N/A | [161] |
| A web-based cross-sectional study on cannabis use and subclinical psychiatric experiences using the Community Assessment of Psychic Experiences; n = 1877 Dutch young adults and adolescents (18–25 y) consuming the same type of cannabis on the majority of occasions (60% of occasions). | THC and CBD exposure were estimated based on Trimbos Institute annual report on Dutch market | Significant inverse relationship between CBD content and self-reported positive symptoms, but not with negative symptoms of depression. | N/A | [172] |
| A double-blind, placebo-controlled study to assess the efficacy of CBD treatment in Japanese late teenagers (n = 37, 18–19 y) with social anxiety disorder (SAD). Cannabis oil containing CBD or placebo daily for 4 weeks. All participants were assessed for SAD symptoms at the beginning and end of the treatment period. | Cannabis oil containing 300 mg CBD (n = 17) or placebo (n = 20), for 4 weeks | CBD significantly decreased anxiety measured by both scales. | None of the participants had any significant health complaints, although no systematic evaluation of side effects was conducted. | [208] |
2.3. Memory and Attention
| Experimental Design | Doses | Results | Side Effects | References |
|---|---|---|---|---|
| A repeated-measures design compared a sample of cannabis users (n = 94, average age: 21) on 2 days: under the influence of the drug (intoxicated day) and when drug-free (drug-free day) approximately 7 days apart. A sample of cannabis was collected from each user and analyzed for levels of cannabinoids. On the basis of the CBD: THC ratios of the cannabis samples, individuals from the top and bottom tertiles were directly compared on indices of the reinforcing effects of drugs, explicit liking, and implicit attentional bias to drug stimuli. | Patients smoked their own cannabis | When intoxicated, smokers of high-CBD: THC strains showed reduced attentional bias to drug and food stimuli compared with smokers of low-CBD: THC strains. Those smoking higher-CBD: THC strains also showed lower self-rated liking of cannabis stimuli on both test days. | N/A | [227] |
| A repeated-measures design compared a sample of cannabis users (n = 134, average age: 21) assessed on 2 days: under the influence of the drug (intoxicated day) and when drug-free (drug-free day) approximately 7 days apart. A sample of cannabis was collected from each user and analyzed for levels of cannabinoids. On the basis of CBD:THC ratios in the cannabis, individuals from the top and bottom tertiles were directly compared on measures of memory and psychotomimetic symptoms. | Patients smoked their own cannabis | Unlike the marked memory impairment of individuals who smoked cannabis low in cannabidiol, participants smoking cannabis high in cannabidiol showed no memory impairment. Cannabidiol content did not affect psychotomimetic symptoms, which were elevated in both groups when intoxicated. | N/A | [228] |
| A total of 120 current cannabis smokers (average age: 20), 66 daily users and 54 recreational users, were classified into groups according to the presence or absence of CBD and high versus low levels of THC. All were assessed on measures of psychosis-like symptoms, memory, and depression/anxiety. | Patients smoked their own cannabis | Recreational users showed increased depression, anxiety, and psychosis-like symptoms that were attenuated in those using cannabis containing CBD. Prose recall and source memory were poorer in high-THC strain daily users, while better recognition memory was measured in those using high-CBD strains. | N/A | [229] |
| A randomized, double-blind crossover design to compare the effects in 48 cannabis users (average age: 21) selected on the basis of (1) schizotypal personality questionnaire scores (low, high) and (2) frequency of cannabis use (light, heavy). The Brief Psychiatric Rating Scale (BPRS), Psychotomimetic States Inventory (PSI), immediate and delayed prose recall (episodic memory), and 1- and 2-back (working memory) were assessed on each day. | Placebo THC 8 mg CBD 16 mg THC 8 mg + CBD 16 mg | THC increased overall scores on the PSI, negative symptoms on the BPRS, and robustly impaired episodic and working memory. Co-administration of CBD did not attenuate these effects. CBD alone reduced PSI scores in light users only. At a ratio of 2:1, CBD does not attenuate the acute psychotic and memory-impairing effects of vaporized THC. | N/A | [231] |
| Placebo-controlled, double-blind, experimental trial with 60 healthy volunteers. Patients were assessed on working memory, cognitive processing speed, attention, and emotional state. | Placebo THC 20 mg CBD 800 mg THC 20 mg + CBD 800 mg | THC affected performance-related activity and extraversion, reduced cognitive processing speed, and impaired attention performance. Administration of CBD alone did not influence emotional state, cognitive performance, or attention. Interestingly, pre-treatment with CBD did not attenuate the effects induced by THC. | N/A | [232] |
| Double-blind, placebo-controlled, randomized crossover trial in 39 healthy young subjects (average age: 22). Participants received once a single dose of vaping after learning 15 unrelated nouns. Short-delay verbal memory performance (number of correctly free-recalled nouns) 20 min after learning was assessed. | Placebo CBD e-liquid (5%) | CBD enhanced verbal episodic memory performance and did not have negative impacts on secondary-outcome measures of attention or working-memory performance. | N/A | [233] |
| Case report describing 3 males (aged 18, 22, and 23) diagnosed with ADHD who integrated cannabis into their treatment regimens. | (Patient1) CBD:THC 20:1, smoking (Patient2) CBD:THC 20:1 oil 1 mL, oral (Patient3) CBD:THC 0:19, smoking | All patients showed substantial improvement in terms of depression, anxiety, and attention. | Short-term memory problems Dry mouth Sleepiness | [242] |
| HIV-infected, antiretroviral-treated individuals (n = 198 sex = male, age = 45–60) were tested to assess the impact of cannabis use on peripheral immune cell frequency, activation, and function using flow cytometry. Amounts of cannabis metabolites were measured in plasma by mass spectrometry to categorize the subjects into three groups: heavy, medium, and non-cannabis users. | Patients smoked their own cannabis | Heavy cannabis users showed a decrease in frequencies of human leukocyte antigen (HLA)-DR + CD38 + CD4+, CD8+ T-cells, intermediate and nonclassical monocyte subsets, as well as decreased frequencies of interleukin 23- and tumor necrosis factor-α-producing antigen-presenting cells compared to non-cannabis-using individuals. | N/A | [243] |
| Comparative Study designed to compare the levels of circulating CD16+ monocytes and interferon-γ-inducible protein 10 (IP-10) between male HIV-infected cannabis users (HIV + MJ+) and non-cannabis users (HIV + MJ−) and determine whether in vitro THC affected CD16 expression as well as IP-10 production by monocytes. Cannabis use was determined by self- reporting and confirmed by serum detection of THC metabolites using a THC ELISA (RTU) Forensic Kit. | Patients smoked their own cannabis | HIV + MJ+ donors had lower levels of circulating serum IP-10 and CD16+ monocytes compared to HIV + MJ − donors, suggesting anti-inflammatory effects due to cannabis consumption. | N/A | [244] |
2.4. Neuroinflammation
3. Materials and Methods
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Crocq, M.A. History of cannabis and the endocannabinoid system. Dialogues Clin. Neurosci. 2020, 22, 223–228. [Google Scholar] [CrossRef]
- Charitos, I.A.; Gagliano-Candela, R.; Santacroce, L.; Bottalico, L. The Cannabis Spread throughout the Continents and its Therapeutic Use in History. Endocr. Metab. Immune Disord. Drug Targets 2021, 21, 407–417. [Google Scholar] [CrossRef]
- Zuardi, A.W. History of cannabis as a medicine: A review. Braz. J. Psychiatry 2006, 28, 153–157. [Google Scholar] [CrossRef]
- Touw, M. The religious and medicinal uses of Cannabis in China, India and Tibet. J. Psychoact. Drugs 1981, 13, 23–34. [Google Scholar] [CrossRef]
- NIDA. Archive Materials for the National Institute on Drug Abuse; NIDA: Washington, DC, USA, 2000.
- Mechoulam, R.; Shvo, Y. Hashish-I. The structure of Cannabidiol. Tetrahedron 1963, 19, 2073–2078. [Google Scholar] [CrossRef]
- Bonini, S.A.; Premoli, M.; Tambaro, S.; Kumar, A.; Maccarinelli, G.; Memo, M.; Mastinu, A. Cannabis sativa: A comprehensive ethnopharmacological review of a medicinal plant with a long history. J. Ethnopharmacol. 2018, 227, 300–315. [Google Scholar] [CrossRef]
- Breijyeh, Z.; Jubeh, B.; Bufo, S.A.; Karaman, R.; Scrano, L. Cannabis: A Toxin-Producing Plant with Potential Therapeutic Uses. Toxins 2021, 13, 117. [Google Scholar] [CrossRef]
- Gaoni, Y.; Mechoulam, R. Isolation, Structure, and Partial Synthesis of an Active Constituent of Hashish. J. Am. Chem. Soc. 1964, 86, 1646–1647. [Google Scholar] [CrossRef]
- Ribeiro, L.I.G.; Ind, P.W. Effect of cannabis smoking on lung function and respiratory symptoms: A structured literature review. npj Prim. Care Respir. Med. 2016, 26, 16071. [Google Scholar] [CrossRef]
- Lee, M.H.S.; Hancox, R.J. Effects of smoking cannabis on lung function. Expert Rev. Respir. Med. 2011, 5, 537–546. [Google Scholar] [CrossRef]
- Piano, M.R. Cannabis Smoking and Cardiovascular Health: It’s Complicated. Clin. Pharmacol. Ther. 2017, 102, 191–193. [Google Scholar] [CrossRef]
- Subramaniam, V.N.; Menezes, A.R.; DeSchutter, A.; Lavie, C.J. The Cardiovascular Effects of Marijuana: Are the Potential Adverse Effects Worth the High? Mol. Med. 2019, 116, 146–153. [Google Scholar]
- Block, R.I.; O’Leary, D.S.; Ehrhardt, J.C.; Augustinack, J.C.; Ghoneim, M.M.; Arndt, S.; Hall, J.A. Effects of frequent marijuana use on brain tissue volume and composition. NeuroReport 2000, 11, 491–496. [Google Scholar] [CrossRef]
- Batalla, A.; Bhattacharyya, S.; Yücel, M.; Fusar-Poli, P.; Crippa, J.A.; Nogué, S.; Torrens, M.; Pujol, J.; Farré, M.; Martin-Santos, R. Structural and Functional Imaging Studies in Chronic Cannabis Users: A Systematic Review of Adolescent and Adult Findings. PLoS ONE 2013, 8, e55821. [Google Scholar] [CrossRef]
- Filbey, F.M.; Aslan, S.; Calhoun, V.D.; Spence, J.S.; Damaraju, E.; Caprihan, A.; Segall, J. Long-term effects of marijuana use on the brain. Proc. Natl. Acad. Sci. USA 2014, 111, 16913–16918. [Google Scholar] [CrossRef]
- Andriot, T.; Ohnmacht, P.; Vuilleumier, P.; Thorens, G.; Khazaal, Y.; Ginovart, N.; Ros, T. Electrophysiological and behavioral correlates of cannabis use disorder. Cogn. Affect. Behav. Neurosci. 2022, 22, 1421–1431. [Google Scholar] [CrossRef]
- Rangel-Pacheco, A.; Lew, B.J.; Schantell, M.D.; Frenzel, M.R.; Eastman, J.A.; Wiesman, A.I.; Wilson, T.W. Altered fronto-occipital connectivity during visual selective attention in regular cannabis users. Psychopharmacology 2021, 238, 1351–1361. [Google Scholar] [CrossRef]
- Medina, K.L.; Nagel, B.J.; Park, A.; McQueeny, T.; Tapert, S.F. Depressive symptoms in adolescents: Associations with white matter volume and marijuana use. J. Child Psychol. Psychiatry 2007, 48, 592–600. [Google Scholar] [CrossRef]
- Gilman, J.M.; Kuster, J.K.; Lee, S.; Lee, M.J.; Kim, B.W.; Makris, N.; van der Kouwe, A.; Blood, A.J.; Breiter, H.C. Cannabis use is quantitatively associated with nucleus accumbens and amygdala abnormalities in young adult recreational users. J. Neurosci. 2014, 34, 5529–5538. [Google Scholar] [CrossRef]
- Bagot, K.S.; Milin, R.; Kaminer, Y. Adolescent Initiation of Cannabis Use and Early-Onset Psychosis. Subst. Abus. 2015, 36, 524–533. [Google Scholar] [CrossRef]
- Fresán, A.; Dionisio-García, D.M.; González-Castro, T.B.; Ramos-Méndez, M.Á.; Castillo-Avila, R.G.; Tovilla-Zárate, C.A.; Juárez-Rojop, I.E.; López-Narváez, M.L.; Genis-Mendoza, A.D.; Nicolini, H. Cannabis smoking increases the risk of suicide ideation and suicide attempt in young individuals of 11–21 years: A systematic review and meta-analysis. J. Psychiatr. Res. 2022, 153, 90–98. [Google Scholar] [CrossRef]
- Meier, M.H.; Caspi, A.; Ambler, A.; Harrington, H.L.; Houts, R.; Keefe, R.S.E.; McDonald, K.; Ward, A.; Poulton, R.; Moffitt, T.E. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc. Natl. Acad. Sci. USA 2012, 109, E2657–E2664. [Google Scholar] [CrossRef]
- United Nations Office On Drugs & Crime. World Drug Report 2021. CrimRxiv 2021. [Google Scholar] [CrossRef]
- Miliano, C.; Margiani, G.; Fattore, L.; De Luca, M.A. Sales and advertising channels of new psychoactive substances (NPS): Internet, social networks, and smartphone apps. Brain Sci. 2018, 8, 123. [Google Scholar] [CrossRef]
- Gicewicz, E.; Gatewood, S.S.; Kaefer, T.N.; Nadpara, P.; Goode, J.V.R. Assessment of hemp oil–based cannabidiol use in a community-based pharmacy setting. J. Am. Pharmacol. Assoc. 2021, 61, S49–S56. [Google Scholar] [CrossRef]
- Sarvet, A.L.; Wall, M.M.; Fink, D.S.; Greene, E.; Le, A.; Boustead, A.E.; Pacula, R.L.; Keyes, K.M.; Cerdá, M.; Galea, S.; et al. Medical marijuana laws and adolescent marijuana use in the United States: A systematic review and meta-analysis. Addiction 2018, 113, 1003–1016. [Google Scholar] [CrossRef]
- Hall, W.; Lynskey, M. Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction 2016, 111, 1764–1773. [Google Scholar] [CrossRef]
- Sarvet, A.L.; Wall, M.M.; Keyes, K.M.; Cerdá, M.; Schulenberg, J.E.; O’Malley, P.M.; Johnston, L.D.; Hasin, D.S. Recent rapid decrease in adolescents’ perception that marijuana is harmful, but no concurrent increase in use. Drug Alcohol Depend. 2018, 186, 68–74. [Google Scholar] [CrossRef]
- Taylor, M.; Cousijn, J.; Filbey, F. Determining Risks for Cannabis Use Disorder in the Face of Changing Legal Policies. Curr. Addict. Rep. 2019, 6, 466–477. [Google Scholar] [CrossRef]
- De Luca, M.A.; Di Chiara, G.; Cadoni, C.; Lecca, D.; Orsolini, L.; Papanti, D.; Corkery, J.; Schifano, F. Cannabis; Epidemiological, Neurobiological and Psychopathological Issues: An Update. CNS Neurol. Disord. Drug Targets 2017, 16, 598–609. [Google Scholar] [CrossRef]
- United Nations Office On Drugs & Crime. World Drug Report; United Nations Office On Drugs & Crime: Washington, DC, USA, 2022. [Google Scholar]
- Chen, C.Y.; Storr, C.L.; Anthony, J.C. Early-onset drug use and risk for drug dependence problems. Addict. Behav. 2009, 34, 319–322. [Google Scholar] [CrossRef]
- Kandel, D.B.; Yamaguchi, K.; Chen, K. Stages of progression in drug involvement from adolescence to adulthood: Further evidence for the gateway theory. J. Stud. Alcohol 1992, 53, 447–457. [Google Scholar] [CrossRef]
- Winters, K.C.; Lee, C.Y.S. Likelihood of developing an alcohol and cannabis use disorder during youth: Association with recent use and age. Drug Alcohol Depend. 2008, 92, 239–247. [Google Scholar] [CrossRef]
- Flory, K.; Lynam, D.; Milich, R.; Leukefeld, C.; Clayton, R. Early adolescent through young adult alcohol and marijuana use trajectories: Early predictors, young adult outcomes, and predictive utility. Dev. Psychopathol. 2004, 16, 193–213. [Google Scholar] [CrossRef]
- Brook, J.S.; Zhang, C.; Brook, D.W. Developmental trajectories of marijuana use from adolescence to adulthood: Personal predictors. Arch. Pediatr. Adolesc. Med. 2011, 165, 55–60. [Google Scholar] [CrossRef]
- Casey, A.M.; Muise, E.D.; Crotty Alexander, L.E. Vaping and e-cigarette use. Mysterious lung manifestations and an epidemic. Curr. Opin. Immunol. 2020, 66, 143–150. [Google Scholar] [CrossRef]
- Corongiu, S.; Dessì, C.; Cadoni, C. Adolescence versus adulthood: Differences in basal mesolimbic and nigrostriatal dopamine transmission and response to drugs of abuse. Addict. Biol. 2020, 25, e12721. [Google Scholar] [CrossRef]
- Miliano, C.; Scott, E.R.; Murdaugh, L.B.; Gnatowski, E.R.; Faunce, C.L.; Anderson, M.S.; Reyes, M.M.; Gregus, A.M.; Buczynski, M.W. Modeling drug exposure in rodents using e-cigarettes and other electronic nicotine delivery systems. J. Neurosci. Methods 2020, 330, 108458. [Google Scholar] [CrossRef]
- Overbeek, D.L.; Kass, A.P.; Chiel, L.E.; Boyer, E.W.; Casey, A.M.H. A review of toxic effects of electronic cigarettes/vaping in adolescents and young adults. Crit. Rev. Toxicol. 2020, 50, 531–538. [Google Scholar] [CrossRef]
- Heinzerling, A.; Armatas, C.; Karmarkar, E.; Attfield, K.; Guo, W.; Wang, Y.; Vrdoljak, G.; Moezzi, B.; Xu, D.; Wagner, J.; et al. Severe Lung Injury Associated with Use of e-Cigarette, or Vaping, Products—California, 2019. JAMA Intern. Med. 2020, 180, 861–869. [Google Scholar] [CrossRef]
- Bhatt, J.M.; Ramphul, M.; Bush, A. An update on controversies in e-cigarettes. Paediatr. Respir. Rev. 2020, 36, 75–86. [Google Scholar] [CrossRef]
- Schäfer, M.; Steindor, M.; Stehling, F.; Dohna-Schwake, C. EVALI (E-cigarette or vaping product use associated lung injury): First case report of an adolescent in Europe. Pediatric Pulmonol. 2021, 56, 1274–1275. [Google Scholar] [CrossRef]
- Marlière, C.; De Greef, J.; Gohy, S.; Hoton, D.; Wallemacq, P.; Jacquet, L.M.; Belkhir, L. Fatal e-cigarette or vaping associated lung injury (EVALI): A first case report in Europe. Eur. Respir. J. 2020, 56, 2000077. [Google Scholar] [CrossRef]
- Ind, P.W. E-cigarette or vaping product use-associated lung injury. Br. J. Hosp. Med. 2020, 81, 1–9. [Google Scholar] [CrossRef]
- Lu, H.C.; MacKie, K. An introduction to the endogenous cannabinoid system. Biol. Psychiatry 2016, 79, 516–525. [Google Scholar] [CrossRef]
- Hohmann, A.G.; Suplita, R.L.; Bolton, N.M.; Neely, M.H.; Fegley, D.; Mangieri, R.; Krey, J.F.; Walker, J.M.; Holmes, P.V.; Crystal, J.D.; et al. An endocannabinoid mechanism for stress-induced analgesia. Nature 2005, 435, 1108–1112. [Google Scholar] [CrossRef]
- Parsons, L.H.; Hurd, Y.L. Endocannabinoid signalling in reward and addiction. Nat. Rev. Neurosci. 2015, 16, 579–594. [Google Scholar] [CrossRef]
- Busquets-Garcia, A.; Desprez, T.; Metna-Laurent, M.; Bellocchio, L.; Marsicano, G.; Soria-Gomez, E. Dissecting the cannabinergic control of behavior: The where matters. BioEssays 2015, 37, 1215–1225. [Google Scholar] [CrossRef]
- Morena, M.; Patel, S.; Bains, J.S.; Hill, M.N. Neurobiological Interactions Between Stress and the Endocannabinoid System. Neuropsychopharmacology 2016, 41, 80–102. [Google Scholar] [CrossRef]
- Gregg, L.C.; Jung, K.M.; Spradley, J.M.; Nyilas, R.; Suplita, R.L.; Zimmer, A.; Watanabe, M.; Mackie, K.; Katona, I.; Piomelli, D.; et al. Activation of type 5 metabotropic glutamate receptors and diacylglycerol lipase-α initiates 2-arachidonoylglycerol formation and endocannabinoid-mediated analgesia. J. Neurosci. 2012, 32, 9457–9468. [Google Scholar] [CrossRef]
- Di Marzo, V.; Fontana, A. Anandamide, an endogenous cannabinomimetic eicosanoid: ‘Killing two birds with one stone’. Prostaglandins Leukot. Essent. Fat. Acids 1995, 53, 1–11. [Google Scholar] [CrossRef]
- Bisogno, T.; Howell, F.; Williams, G.; Minassi, A.; Cascio, M.G.; Ligresti, A.; Matias, I.; Schiano-Moriello, A.; Paul, P.; Williams, E.J.; et al. Cloning of the first sn1-DAG lipases points to the spatial and temporal regulation of endocannabinoid signaling in the brain. J. Cell Biol. 2003, 163, 463–468. [Google Scholar] [CrossRef]
- Dinh, T.P.; Carpenter, D.; Leslie, F.M.; Freund, T.F.; Katona, I.; Sensi, S.L.; Kathuria, S.; Piomelli, D. Brain monoglyceride lipase participating in endocannabinoid inactivation. Proc. Natl. Acad. Sci. USA 2002, 99, 10819–10824. [Google Scholar] [CrossRef]
- Okamoto, Y.; Morishita, J.; Tsuboi, K.; Tonai, T.; Ueda, N. Molecular Characterization of a Phospholipase D Generating Anandamide and Its Congeners. J. Biol. Chem. 2004, 279, 5298–5305. [Google Scholar] [CrossRef]
- Cravatt, B.F.; Giang, D.K.; Mayfield, S.P.; Boger, D.L.; Lerner, R.A.; Gilula, N.B. Molecular characterization of an enzyme that degrades neuromodulatory fatty-acid amides. Nature 1996, 384, 83–87. [Google Scholar] [CrossRef]
- Bénard, G.; Massa, F.; Puente, N.; Lourenço, J.; Bellocchio, L.; Soria-Gómez, E.; Matias, I.; Delamarre, A.; Metna-Laurent, M.; Cannich, A.; et al. Mitochondrial CB 1 receptors regulate neuronal energy metabolism. Nat. Neurosci. 2012, 15, 558–564. [Google Scholar] [CrossRef]
- Serrat, R.; Covelo, A.; Kouskoff, V.; Delcasso, S.; Ruiz-Calvo, A.; Chenouard, N.; Stella, C.; Blancard, C.; Salin, B.; Julio-Kalajzić, F.; et al. Astroglial ER-mitochondria calcium transfer mediates endocannabinoid-dependent synaptic integration. Cell Rep. 2021, 37, 110133. [Google Scholar] [CrossRef]
- Jimenez-Blasco, D.; Busquets-Garcia, A.; Hebert-Chatelain, E.; Serrat, R.; Vicente-Gutierrez, C.; Ioannidou, C.; Gómez-Sotres, P.; Lopez-Fabuel, I.; Resch-Beusher, M.; Resel, E.; et al. Glucose metabolism links astroglial mitochondria to cannabinoid effects. Nature 2020, 583, 603–608. [Google Scholar] [CrossRef]
- Cristino, L.; Bisogno, T.; Di Marzo, V. Cannabinoids and the expanded endocannabinoid system in neurological disorders. Nat. Rev. Neurol. 2020, 16, 9–29. [Google Scholar] [CrossRef]
- Kaczocha, M.; Haj-Dahmane, S. Mechanisms of endocannabinoid transport in the brain. Br. J. Pharmacol. 2022, 179, 4300–4310. [Google Scholar] [CrossRef]
- Metna-Laurent, M.; Marsicano, G. Rising stars: Modulation of brain functions by astroglial type-1 cannabinoid receptors. Glia 2015, 63, 353–364. [Google Scholar] [CrossRef]
- Jacob, W.; Marsch, R.; Marsicano, G.; Lutz, B.; Wotjak, C.T. Cannabinoid CB1 receptor deficiency increases contextual fear memory under highly aversive conditions and long-term potentiation in vivo. Neurobiol. Learn. Mem. 2012, 98, 47–55. [Google Scholar] [CrossRef]
- Vinod, K.Y.; Hungund, B.L. Cannabinoid-1 receptor: A novel target for the treatment of neuropsychiatric disorders. Expert Opin. Ther. Targets 2006, 10, 203–210. [Google Scholar] [CrossRef]
- Lu, H.C.; Mackie, K. Review of the Endocannabinoid System. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2021, 6, 607–615. [Google Scholar] [CrossRef]
- Kimura, T.; Takaya, M.; Usami, N.; Watanabe, K.; Yamamoto, I. ∆(9)-Tetrahydrocannabinol, a major marijuana component, enhances the anesthetic effect of pentobarbital through the CB(1) receptor. Forensic Toxicol. 2019, 37, 207–214. [Google Scholar] [CrossRef]
- Rosenthaler, S.; Pohn, B.; Kolmanz, C.; Huu, C.N.; Krewenka, C.; Huber, A.; Kranner, B.; Rausch, W.D.; Moldzio, R. Differences in receptor binding affinity of several phytocannabinoids do not explain their effects on neural cell cultures. Neurotoxicol. Teratol. 2014, 46, 49–56. [Google Scholar] [CrossRef]
- Pertwee, R.G. The diverse CB 1 and CB 2 receptor pharmacology of three plant cannabinoids: Δ 9-tetrahydrocannabinol, cannabidiol and Δ 9-tetrahydrocannabivarin. Br. J. Pharmacol. 2008, 153, 199–215. [Google Scholar] [CrossRef]
- Ligresti, A.; De Petrocellis, L.; Di Marzo, V. From phytocannabinoids to cannabinoid receptors and endocannabinoids: Pleiotropic physiological and pathological roles through complex pharmacology. Physiol. Rev. 2016, 96, 1593–1659. [Google Scholar] [CrossRef]
- Martínez, V.; Iriondo De-Hond, A.; Borrelli, F.; Capasso, R.; Del Castillo, M.D.; Abalo, R. Cannabidiol and other non-psychoactive cannabinoids for prevention and treatment of gastrointestinal disorders: Useful nutraceuticals? Int. J. Mol. Sci. 2020, 21, 3067. [Google Scholar] [CrossRef]
- Elmes, M.W.; Kaczocha, M.; Berger, W.T.; Leung, K.N.; Ralph, B.P.; Wang, L.; Sweeney, J.M.; Miyauchi, J.T.; Tsirka, S.E.; Ojima, I.; et al. Fatty acid-binding proteins (FABPs) are intracellular carriers for Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD). J. Biol. Chem. 2015, 290, 8711–8721. [Google Scholar] [CrossRef]
- Wu, C.S.; Jew, C.P.; Lu, H.C. Lasting impacts of prenatal cannabis exposure and the role of endogenous cannabinoids in the developing brain. Future Neurol. 2011, 6, 459–480. [Google Scholar] [CrossRef]
- De Petrocellis, L.; Ligresti, A.; Moriello, A.S.; Allarà, M.; Bisogno, T.; Petrosino, S.; Stott, C.G.; Di Marzo, V. Effects of cannabinoids and cannabinoid-enriched Cannabis extracts on TRP channels and endocannabinoid metabolic enzymes. Br. J. Pharmacol. 2011, 163, 1479–1494. [Google Scholar] [CrossRef]
- Di Marzo, V.; Piscitelli, F. The Endocannabinoid System and its Modulation by Phytocannabinoids. Neurotherapeutics 2015, 12, 692–698. [Google Scholar] [CrossRef]
- Anavi-Goffer, S.; Baillie, G.; Irving, A.J.; Gertsch, J.; Greig, I.R.; Pertwee, R.G.; Ross, R.A. Modulation of L-α-lysophosphatidylinositol/GPR55 mitogen-activated protein kinase (MAPK) signaling by cannabinoids. J. Biol. Chem. 2012, 287, 91–104. [Google Scholar] [CrossRef]
- Kohno, M.; Hasegawa, H.; Inoue, A.; Muraoka, M.; Miyazaki, T.; Oka, K.; Yasukawa, M. Identification of N-arachidonylglycine as the endogenous ligand for orphan G-protein-coupled receptor GPR18. Biochem. Biophys. Res. Commun. 2006, 347, 827–832. [Google Scholar] [CrossRef]
- McPartland, J.M.; Glass, M.; Pertwee, R.G. Meta-analysis of cannabinoid ligand binding affinity and receptor distribution: Interspecies differences. Br. J. Pharmacol. 2007, 152, 583–593. [Google Scholar] [CrossRef]
- Burstein, S. Cannabidiol (CBD) and its analogs: A review of their effects on inflammation. Bioorganic Med. Chem. 2015, 23, 1377–1385. [Google Scholar] [CrossRef]
- Kathmann, M.; Flau, K.; Redmer, A.; Trankle, C.; Schlicker, E. Cannabidiol is an allosteric modulator at mu- and delta-opioid receptors. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2006, 372, 354–361. [Google Scholar] [CrossRef]
- Sartim, A.G.; Guimarães, F.S.; Joca, S.R.L. Antidepressant-like effect of cannabidiol injection into the ventral medial prefrontal cortex-Possible involvement of 5-HT1A and CB1 receptors. Behav. Brain Res. 2016, 303, 218–227. [Google Scholar] [CrossRef]
- Fogaça, M.V.; Reis, F.M.C.V.; Campos, A.C.; Guimarães, F.S. Effects of intra-prelimbic prefrontal cortex injection of cannabidiol on anxiety-like behavior: Involvement of 5HT1A receptors and previous stressful experience. Eur. Neuropsychopharmacol. 2014, 24, 410–419. [Google Scholar] [CrossRef]
- Galaj, E.; Bi, G.H.; Yang, H.J.; Xi, Z.X. Cannabidiol attenuates the rewarding effects of cocaine in rats by CB2, 5-HT1A and TRPV1 receptor mechanisms. Neuropharmacology 2020, 167, 107740. [Google Scholar] [CrossRef]
- Ibeas Bih, C.; Chen, T.; Nunn, A.V.W.; Bazelot, M.; Dallas, M.; Whalley, B.J. Molecular Targets of Cannabidiol in Neurological Disorders. Neurotherapeutics 2015, 12, 699–730. [Google Scholar] [CrossRef]
- Aso, E.; Fernández-Dueñas, V.; López-Cano, M.; Taura, J.; Watanabe, M.; Ferrer, I.; Luján, R.; Ciruela, F. Adenosine A2A-Cannabinoid CB1 Receptor Heteromers in the Hippocampus: Cannabidiol Blunts Δ9-Tetrahydrocannabinol-Induced Cognitive Impairment. Mol. Neurobiol. 2019, 56, 5382–5391. [Google Scholar] [CrossRef]
- Viñals, X.; Moreno, E.; Lanfumey, L.; Cordomí, A.; Pastor, A.; De La Torre, R.; Gasperini, P.; Navarro, G.; Howell, L.A.; Pardo, L.; et al. Cognitive impairment induced by delta9-tetrahydrocannabinol occurs through heteromers between cannabinoid CB1 and serotonin 5-HT2A receptors. PLoS Biol. 2015, 13, e1002194. [Google Scholar] [CrossRef]
- Parker, L.A.; Burton, P.; Sorge, R.E.; Yakiwchuk, C.; Mechoulam, R. Effect of low doses of delta9-tetrahydrocannabinol and cannabidiol on the extinction of cocaine-induced and amphetamine-induced conditioned place preference learning in rats. Psychopharmacology 2004, 175, 360–366. [Google Scholar] [CrossRef]
- Vann, R.E.; Gamage, T.F.; Warner, J.A.; Marshall, E.M.; Taylor, N.L.; Martin, B.R.; Wiley, J.L. Divergent effects of cannabidiol on the discriminative stimulus and place conditioning effects of Delta(9)-tetrahydrocannabinol. Drug Alcohol Depend. 2008, 94, 191–198. [Google Scholar] [CrossRef]
- Katsidoni, V.; Anagnostou, I.; Panagis, G. Cannabidiol inhibits the reward-facilitating effect of morphine: Involvement of 5-HT1A receptors in the dorsal raphe nucleus. Addict Biol. 2013, 18, 286–296. [Google Scholar] [CrossRef]
- Grotenhermen, F.; Russo, E.; Zuardi, A.W. Even High Doses of Oral Cannabidol Do Not Cause THC-Like Effects in Humans: Comment on Merrick et al. Cannabis Cannabinoid Res. 2016, 1, 102–112; [Google Scholar] [CrossRef]
- Devinsky, O.; Cilio, M.R.; Cross, H.; Fernandez-Ruiz, J.; French, J.; Hill, C.; Katz, R.; Di Marzo, V.; Jutras-Aswad, D.; Notcutt, W.G.; et al. Cannabidiol: Pharmacology and potential therapeutic role in epilepsy and other neuropsychiatric disorders. Epilepsia 2014, 55, 791–802. [Google Scholar] [CrossRef]
- Zhornitsky, S.; Potvin, S. Cannabidiol in humans-The quest for therapeutic targets. Pharmaceuticals 2012, 5, 529–552. [Google Scholar] [CrossRef]
- Bhattacharyya, S.; Atakan, Z.; Martin-Santos, R.; Crippa, J.A.; McGuire, P.K. Neural mechanisms for the cannabinoid modulation of cognition and affect in man: A critical review of neuroimaging studies. Curr. Pharmacol. Des. 2012, 18, 5045–5054. [Google Scholar] [CrossRef]
- Renard, J.; Norris, C.; Rushlow, W.; Laviolette, S.R. Neuronal and molecular effects of cannabidiol on the mesolimbic dopamine system: Implications for novel schizophrenia treatments. Neurosci. Biobehav. Rev. 2017, 75, 157–165. [Google Scholar] [CrossRef]
- Renard, J.; Rosen, L.G.; Loureiro, M.; De Oliveira, C.; Schmid, S.; Rushlow, W.J.; Laviolette, S.R. Adolescent Cannabinoid Exposure Induces a Persistent Sub-Cortical Hyper-Dopaminergic State and Associated Molecular Adaptations in the Prefrontal Cortex. Cereb. Cortex 2017, 27, 1297–1310. [Google Scholar] [CrossRef]
- Renard, J.; Szkudlarek, H.J.; Kramar, C.P.; Jobson, C.E.L.; Moura, K.; Rushlow, W.J.; Laviolette, S.R. Adolescent THC Exposure Causes Enduring Prefrontal Cortical Disruption of GABAergic Inhibition and Dysregulation of Sub-Cortical Dopamine Function. Sci. Rep. 2017, 7, 11420. [Google Scholar] [CrossRef]
- Laprairie, R.B.; Bagher, A.M.; Kelly, M.E.M.; Denovan-Wright, E.M. Cannabidiol is a negative allosteric modulator of the cannabinoid CB1 receptor. Br. J. Pharmacol. 2015, 172, 4790–4805. [Google Scholar] [CrossRef]
- Mechoulam, R.; Peters, M.; Murillo-Rodriguez, E.; Hanus, L.O. Cannabidiol—Recent advances. Chem. Biodivers. 2007, 4, 1678–1692. [Google Scholar] [CrossRef]
- Petitet, F.; Jeantaud, B.; Reibaud, M.; Imperato, A.; Dubroeucq, M.C. Complex pharmacology of natural cannabinoids: Evidence for partial agonist activity of delta9-tetrahydrocannabinol and antagonist activity of cannabidiol on rat brain cannabinoid receptors. Life Sci. 1998, 63, PL1-6. [Google Scholar] [CrossRef]
- Thomas, A.; Baillie, G.L.; Phillips, A.M.; Razdan, R.K.; Ross, R.A.; Pertwee, R.G. Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro. Br. J. Pharmacol. 2007, 150, 613–623. [Google Scholar] [CrossRef]
- Turkanis, S.A.; Karler, R. Effects of delta-9-tetrahydrocannabinol, 11-hydroxy-delta-9-tetrahydrocannabinol and cannabidiol on neuromuscular transmission in the frog. Neuropharmacology 1986, 25, 1273–1278. [Google Scholar] [CrossRef]
- McPartland, J.M.; Duncan, M.; Di Marzo, V.; Pertwee, R.G. Are cannabidiol and Δ9-tetrahydrocannabivarin negative modulators of the endocannabinoid system? A systematic review. Br. J. Pharmacol. 2015, 172, 737–753. [Google Scholar] [CrossRef]
- Tham, M.; Yilmaz, O.; Alaverdashvili, M.; Kelly, M.E.M.; Denovan-Wright, E.M.; Laprairie, R.B. Allosteric and orthosteric pharmacology of cannabidiol and cannabidiol-dimethylheptyl at the type 1 and type 2 cannabinoid receptors. Br. J. Pharmacol. 2019, 176, 1455–1469. [Google Scholar] [CrossRef]
- Pisanti, S.; Malfitano, A.M.; Ciaglia, E.; Lamberti, A.; Ranieri, R.; Cuomo, G.; Abate, M.; Faggiana, G.; Proto, M.C.; Fiore, D.; et al. Cannabidiol: State of the art and new challenges for therapeutic applications. Pharmacol. Ther. 2017, 175, 133–150. [Google Scholar] [CrossRef]
- Bisogno, T.; Hanuš, L.; De Petrocellis, L.; Tchilibon, S.; Ponde, D.E.; Brandi, I.; Moriello, A.S.; Davis, J.B.; Mechoulam, R.; Di Marzo, V. Molecular targets for cannabidiol and its synthetic analogues: Effect on vanilloid VR1 receptors and on the cellular uptake and enzymatic hydrolysis of anandamide. Br. J. Pharmacol. 2001, 134, 845–852. [Google Scholar] [CrossRef]
- Giuffrida, A.; Parsons, L.H.; Kerr, T.M.; Rodríguez De Fonseca, F.; Navarro, M.; Piomelli, D. Dopamine activation of endogenous cannabinoid signaling in dorsal striatum. Nat. Neurosci. 1999, 2, 358–363. [Google Scholar] [CrossRef]
- Seeman, P. Cannabidiol is a partial agonist at dopamine D2High receptors, predicting its antipsychotic clinical dose. Transl. Psychiatry 2016, 6, e920. [Google Scholar] [CrossRef]
- Hudson, R.; Renard, J.; Norris, C.; Rushlow, W.J.; Laviolette, S.R. Cannabidiol counteracts the psychotropic side-effects of Δ-9-tetrahydrocannabinol in the ventral hippocampus through bidirectional control of erk1-2 phosphorylation. J. Neurosci. 2019, 39, 8762–8777. [Google Scholar] [CrossRef]
- Renard, J.; Loureiro, M.; Rosen, L.G.; Zunder, J.; De Oliveira, C.; Schmid, S.; Rushlow, W.J.; Laviolette, S.R. Cannabidiol counteracts amphetamine-induced neuronal and behavioral sensitization of the mesolimbic dopamine pathway through a novel mTOR/p70S6 kinase signaling pathway. J. Neurosci. 2016, 36, 5160–5169. [Google Scholar] [CrossRef]
- Gunasekera, B.; Diederen, K.; Bhattacharyya, S. Cannabinoids, reward processing, and psychosis. Psychopharmacology 2022, 239, 1157–1177. [Google Scholar] [CrossRef]
- Hindocha, C.; Freeman, T.P.; Grabski, M.; Crudgington, H.; Davies, A.C.; Stroud, J.B.; Das, R.K.; Lawn, W.; Morgan, C.J.A.; Curran, H.V. The effects of cannabidiol on impulsivity and memory during abstinence in cigarette dependent smokers. Sci. Rep. 2018, 8, 7568. [Google Scholar] [CrossRef]
- Hurd, Y.L.; Yoon, M.; Manini, A.F.; Hernandez, S.; Olmedo, R.; Ostman, M.; Jutras-Aswad, D. Early Phase in the Development of Cannabidiol as a Treatment for Addiction: Opioid Relapse Takes Initial Center Stage. Neurotherapeutics 2015, 12, 807–815. [Google Scholar] [CrossRef]
- Allsop, D.J.; Lintzeris, N.; Copeland, J.; Dunlop, A.; McGregor, I.S. Cannabinoid replacement therapy (CRT): Nabiximols (Sativex) as a novel treatment for cannabis withdrawal. Clin. Pharmacol. 2015, 97, 571–574. [Google Scholar] [CrossRef]
- Bhardwaj, A.K.; Allsop, D.J.; Copeland, J.; McGregor, I.S.; Dunlop, A.; Shanahan, M.; Bruno, R.; Phung, N.; Montebello, M.; Sadler, C.; et al. Randomised Controlled Trial (RCT) of cannabinoid replacement therapy (Nabiximols) for the management of treatment-resistant cannabis dependent patients: A study protocol. BMC Psychiatry 2018, 18, 140. [Google Scholar] [CrossRef]
- Crippa, J.A.; Hallak, J.E.; Machado-de-Sousa, J.P.; Queiroz, R.H.; Bergamaschi, M.; Chagas, M.H.; Zuardi, A.W. Cannabidiol for the treatment of cannabis withdrawal syndrome: A case report. J. Clin. Pharmacol. 2013, 38, 162–164. [Google Scholar] [CrossRef]
- Laczkovics, C.; Kothgassner, O.D.; Felnhofer, A.; Klier, C.M. Cannabidiol treatment in an adolescent with multiple substance abuse, social anxiety and depression. Neuropsychiatrie 2021, 35, 31–34. [Google Scholar] [CrossRef]
- Trigo, J.M.; Lagzdins, D.; Rehm, J.; Selby, P.; Gamaleddin, I.; Fischer, B.; Barnes, A.J.; Huestis, M.A.; Le Foll, B. Effects of fixed or self-titrated dosages of Sativex on cannabis withdrawal and cravings. Drug Alcohol Depend. 2016, 161, 298–306. [Google Scholar] [CrossRef]
- Trigo, J.M.; Soliman, A.; Staios, G.; Quilty, L.; Fischer, B.; George, T.P.; Rehm, J.; Selby, P.; Barnes, A.J.; Huestis, M.A.; et al. Sativex Associated With Behavioral-Relapse Prevention Strategy as Treatment for Cannabis Dependence: A Case Series. J. Addict. Med. 2016, 10, 274–279. [Google Scholar] [CrossRef]
- Bonaccorso, S.; Ricciardi, A.; Zangani, C.; Chiappini, S.; Schifano, F. Cannabidiol (CBD) use in psychiatric disorders: A systematic review. Neurotoxicology 2019, 74, 282–298. [Google Scholar] [CrossRef]
- Spiga, S.; Lintas, A.; Diana, M. Altered Mesolimbic Dopamine System in THC Dependence. Curr. Neuropharmacol. 2011, 9, 200–204. [Google Scholar] [CrossRef]
- Gray, K.M.; Carpenter, M.J.; Baker, N.L.; DeSantis, S.M.; Kryway, E.; Hartwell, K.J.; McRae-Clark, A.L.; Brady, K.T. A double-blind randomized controlled trial of N-acetylcysteine in cannabis-dependent adolescents. Am. J. Psychiatry 2012, 169, 805–812. [Google Scholar] [CrossRef]
- Volkow, N.D.; Swanson, J.M.; Evins, A.E.; DeLisi, L.E.; Meier, M.H.; Gonzalez, R.; Bloomfield, M.A.P.; Curran, H.V.; Baler, R. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: A review. JAMA Psychiatry 2016, 73, 292–297. [Google Scholar] [CrossRef]
- Meyer, H.C.; Lee, F.S.; Gee, D.G. The Role of the Endocannabinoid System and Genetic Variation in Adolescent Brain Development. Neuropsychopharmacology 2018, 43, 21–33. [Google Scholar] [CrossRef]
- Fischer, A.S.; Tapert, S.F.; Louie, D.L.; Schatzberg, A.F.; Singh, M.K. Cannabis and the Developing Adolescent Brain. Curr. Treat. Options Psychiatry 2020, 7, 144–161. [Google Scholar] [CrossRef]
- Kandel, D.B.; Davies, M.; Karus, D.; Yamaguchi, K. The consequences in young adulthood of adolescent drug involvement. An overview. Arch. Gen. Psychiatry 1986, 43, 746–754. [Google Scholar] [CrossRef]
- Kandel, D.B. Does marijuana use cause the use of other drugs? JAMA 2003, 289, 482–483. [Google Scholar] [CrossRef]
- Kandel, D.B.; Yamaguchi, K.; Klein, L.C. Testing the Gateway Hypothesis. Addiction 2006, 101, 470–472; discussion 474–476. [Google Scholar] [CrossRef]
- Lynskey, M.T.; Heath, A.C.; Bucholz, K.K.; Slutske, W.S.; Madden, P.A.; Nelson, E.C.; Statham, D.J.; Martin, N.G. Escalation of drug use in early-onset cannabis users vs. co-twin controls. JAMA 2003, 289, 427–433. [Google Scholar] [CrossRef]
- Agrawal, A.; Lynskey, M.T. The genetic epidemiology of cannabis use, abuse and dependence. Addiction 2006, 101, 801–812. [Google Scholar] [CrossRef]
- Fergusson, D.M.; Boden, J.M.; Horwood, L.J. Cannabis use and other illicit drug use: Testing the cannabis gateway hypothesis. Addiction 2006, 101, 556–569. [Google Scholar] [CrossRef]
- Fergusson, D.M.; Horwood, L.J.; Lynskey, M.T.; Madden, P.A. Early reactions to cannabis predict later dependence. Arch. Gen. Psychiatry 2003, 60, 1033–1039. [Google Scholar] [CrossRef]
- Lecca, D.; Scifo, A.; Pisanu, A.; Valentini, V.; Piras, G.; Sil, A.; Cadoni, C.; Di Chiara, G. Adolescent cannabis exposure increases heroin reinforcement in rats genetically vulnerable to addiction. Neuropharmacology 2020, 166, 107974. [Google Scholar] [CrossRef]
- Ellgren, M.; Spano, S.M.; Hurd, Y.L. Adolescent cannabis exposure alters opiate intake and opioid limbic neuronal populations in adult rats. Neuropsychopharmacology 2007, 32, 607–615. [Google Scholar] [CrossRef]
- Tomasiewicz, H.C.; Jacobs, M.M.; Wilkinson, M.B.; Wilson, S.P.; Nestler, E.J.; Hurd, Y.L. Proenkephalin mediates the enduring effects of adolescent cannabis exposure associated with adult opiate vulnerability. Biol. Psychiatry 2012, 72, 803–810. [Google Scholar] [CrossRef]
- Vanyukov, M.M.; Tarter, R.E.; Kirisci, L.; Kirillova, G.P.; Maher, B.S.; Clark, D.B. Liability to substance use disorders: 1. Common mechanisms and manifestations. Neurosci. Biobehav. Rev. 2003, 27, 507–515. [Google Scholar] [CrossRef]
- Zeiger, J.S.; Haberstick, B.C.; Corley, R.P.; Ehringer, M.A.; Crowley, T.J.; Hewitt, J.K.; Hopfer, C.J.; Stallings, M.C.; Young, S.E.; Rhee, S.H. Subjective effects for alcohol, tobacco, and marijuana association with cross-drug outcomes. Drug Alcohol Depend. 2012, 123, S52–S58. [Google Scholar] [CrossRef]
- Solinas, M.; Panlilio, L.V.; Goldberg, S.R. Exposure to delta-9-tetrahydrocannabinol (THC) increases subsequent heroin taking but not heroin’s reinforcing efficacy: A self-administration study in rats. Neuropsychopharmacology 2004, 29, 1301–1311. [Google Scholar] [CrossRef]
- Stopponi, S.; Soverchia, L.; Ubaldi, M.; Cippitelli, A.; Serpelloni, G.; Ciccocioppo, R. Chronic THC during adolescence increases the vulnerability to stress-induced relapse to heroin seeking in adult rats. Eur. Neuropsychopharmacol. 2014, 24, 1037–1045. [Google Scholar] [CrossRef]
- Klein, C.; Karanges, E.; Spiro, A.; Wong, A.; Spencer, J.; Huynh, T.; Gunasekaran, N.; Karl, T.; Long, L.E.; Huang, X.F.; et al. Cannabidiol potentiates Δ 9-tetrahydrocannabinol (THC) behavioural effects and alters THC pharmacokinetics during acute and chronic treatment in adolescent rats. Psychopharmacology 2011, 218, 443–457. [Google Scholar] [CrossRef]
- Surguchov, A.; Bernal, L.; Surguchev, A.A. Phytochemicals as Regulators of Genes Involved in Synucleinopathies. Biomolecules 2021, 11, 624. [Google Scholar] [CrossRef]
- Galve-Roperh, I.; Palazuelos, J.; Aguado, T.; Guzmán, M. The endocannabinoid system and the regulation of neural development: Potential implications in psychiatric disorders. Eur. Arch. Psychiatry Clin. Neurosci. 2009, 259, 371–382. [Google Scholar] [CrossRef]
- Viveros, M.P.; Llorente, R.; Suarez, J.; Llorente-Berzal, A.; López-Gallardo, M.; Rodriguez De Fonseca, F. The endocannabinoid system in critical neurodevelopmental periods: Sex differences and neuropsychiatric implications. J. Psychopharmacol. 2012, 26, 164–176. [Google Scholar] [CrossRef]
- Giedd, J.N.; Blumenthal, J.; Jeffries, N.O.; Castellanos, F.X.; Liu, H.; Zijdenbos, A.; Paus, T.; Evans, A.C.; Rapoport, J.L. Brain development during childhood and adolescence: A longitudinal MRI study [2]. Nat. Neurosci. 1999, 2, 861–863. [Google Scholar] [CrossRef]
- Spear, L.P. The adolescent brain and age-related behavioral manifestations. Neurosci. Biobehav. Rev. 2000, 24, 417–463. [Google Scholar] [CrossRef]
- Bartzokis, G.; Beckson, M.; Lu, P.H.; Nuechterlein, K.H.; Edwards, N.; Mintz, J. Age-related changes in frontal and temporal lobe volumes in men: A magnetic resonance imaging study. Arch. Gen. Psychiatry 2001, 58, 461–465. [Google Scholar] [CrossRef]
- Andersen, S.L. Trajectories of brain development: Point of vulnerability or window of opportunity? Neurosci. Biobehav. Rev. 2003, 27, 3–18. [Google Scholar] [CrossRef]
- Marconi, A.; Di Forti, M.; Lewis, C.M.; Murray, R.M.; Vassos, E. Meta-analysis of the Association Between the Level of Cannabis Use and Risk of Psychosis. Schizophr. Bull. 2016, 42, 1262–1269. [Google Scholar] [CrossRef]
- Gobbi, G.; Atkin, T.; Zytynski, T.; Wang, S.; Askari, S.; Boruff, J.; Ware, M.; Marmorstein, N.; Cipriani, A.; Dendukuri, N.; et al. Association of Cannabis Use in Adolescence and Risk of Depression, Anxiety, and Suicidality in Young Adulthood: A Systematic Review and Meta-analysis. JAMA Psychiatry 2019, 76, 426–434. [Google Scholar] [CrossRef]
- Volkow, N.D.; Compton, W.M.; Weiss, S.R. Adverse health effects of marijuana use. N. Engl. J. Med. 2014, 371, 879. [Google Scholar] [CrossRef]
- Wu, L.T.; Zhu, H.; Swartz, M.S. Trends in cannabis use disorders among racial/ethnic population groups in the United States. Drug Alcohol Depend. 2016, 165, 181–190. [Google Scholar] [CrossRef]
- Chandra, S.; Radwan, M.M.; Majumdar, C.G.; Church, J.C.; Freeman, T.P.; ElSohly, M.A. New trends in cannabis potency in USA and Europe during the last decade (2008–2017). Eur. Arch. Psychiatry Clin. Neurosci. 2019, 269, 5–15. [Google Scholar] [CrossRef]
- Pintori, N.; Loi, B.; Mereu, M. Synthetic cannabinoids: The hidden side of Spice drugs. Behav. Pharmacol. 2017, 28, 409–419. [Google Scholar] [CrossRef]
- Fergusson, D.M.; Horwood, L.J.; Swain-Campbell, N. Cannabis use and psychosocial adjustment in adolescence and young adulthood. Addiction 2002, 97, 1123–1135. [Google Scholar] [CrossRef]
- Patton, G.C.; Coffey, C.; Carlin, J.B.; Degenhardt, L.; Lynskey, M.; Hall, W. Cannabis use and mental health in young people: Cohort study. BMJ 2002, 325, 1195–1198. [Google Scholar] [CrossRef]
- Rey, J.M.; Tennant, C.C. Cannabis and mental health. BMJ 2002, 325, 1183–1184. [Google Scholar] [CrossRef]
- Hayatbakhsh, M.R.; Najman, J.M.; Jamrozik, K.; Mamun, A.A.; Alati, R.; Bor, W. Cannabis and anxiety and depression in young adults: A large prospective study. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 408–417. [Google Scholar] [CrossRef]
- Gage, S.H.; Hickman, M.; Zammit, S. Association Between Cannabis and Psychosis: Epidemiologic Evidence. Biol. Psychiatry 2016, 79, 549–556. [Google Scholar] [CrossRef]
- Murray, R.M.; Englund, A.; Abi-Dargham, A.; Lewis, D.A.; Di Forti, M.; Davies, C.; Sherif, M.; McGuire, P.; D’Souza, D.C. Cannabis-associated psychosis: Neural substrate and clinical impact. Neuropharmacology 2017, 124, 89–104. [Google Scholar] [CrossRef]
- Langlois, C.; Potvin, S.; Khullar, A.; Tourjman, S.V. Down and High: Reflections Regarding Depression and Cannabis. Front. Psychiatry 2021, 12, 625158. [Google Scholar] [CrossRef]
- Renard, J.; Krebs, M.O.; Le Pen, G.; Jay, T.M. Long-term consequences of adolescent cannabinoid exposure in adult psychopathology. Front. Neurosci. 2014, 8, 361. [Google Scholar] [CrossRef]
- Grant, B.F.; Pickering, R. The relationship between cannabis use and DSM-IV cannabis abuse and dependence: Results from the national longitudinal alcohol epidemiologic survey. J. Subst. Abus. 1998, 10, 255–264. [Google Scholar] [CrossRef]
- Green, B.E.; Ritter, C. Marijuana use and depression. J. Health Soc. Behav. 2000, 41, 40–49. [Google Scholar] [CrossRef]
- Hurlimann, F.; Kupferschmid, S.; Simon, A.E. Cannabis-induced depersonalization disorder in adolescence. Neuropsychobiology 2012, 65, 141–146. [Google Scholar] [CrossRef]
- Levine, A.; Clemenza, K.; Rynn, M.; Lieberman, J. Evidence for the Risks and Consequences of Adolescent Cannabis Exposure. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 214–225. [Google Scholar] [CrossRef]
- Hall, W.; Degenhardt, L. Cannabis use and the risk of developing a psychotic disorder. World Psychiatry 2008, 7, 68–71. [Google Scholar] [CrossRef]
- Rubino, T.; Parolaro, D. Long lasting consequences of cannabis exposure in adolescence. Mol. Cell Endocrinol. 2008, 286, S108–S113. [Google Scholar] [CrossRef]
- Stringfield, S.J.; Torregrossa, M.M. Disentangling the lasting effects of adolescent cannabinoid exposure. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 104, 110067. [Google Scholar] [CrossRef]
- Sideli, L.; Trotta, G.; Spinazzola, E.; La Cascia, C.; Di Forti, M. Adverse effects of heavy cannabis use: Even plants can harm the brain. Pain 2021, 162, S97–S104. [Google Scholar] [CrossRef]
- Sideli, L.; Quigley, H.; La Cascia, C.; Murray, R.M. Cannabis Use and the Risk for Psychosis and Affective Disorders. J. Dual. Diagn. 2020, 16, 22–42. [Google Scholar] [CrossRef]
- Di Forti, M.; Morgan, C.; Dazzan, P.; Pariante, C.; Mondelli, V.; Marques, T.R.; Handley, R.; Luzi, S.; Russo, M.; Paparelli, A.; et al. High-potency cannabis and the risk of psychosis. Br. J. Psychiatry 2009, 195, 488–491. [Google Scholar] [CrossRef]
- Englund, A.; Morrison, P.D.; Nottage, J.; Hague, D.; Kane, F.; Bonaccorso, S.; Stone, J.M.; Reichenberg, A.; Brenneisen, R.; Holt, D.; et al. Cannabidiol inhibits THC-elicited paranoid symptoms and hippocampal-dependent memory impairment. J. Psychopharmacol. 2013, 27, 19–27. [Google Scholar] [CrossRef]
- Schubart, C.D.; Sommer, I.E.; van Gastel, W.A.; Goetgebuer, R.L.; Kahn, R.S.; Boks, M.P. Cannabis with high cannabidiol content is associated with fewer psychotic experiences. Schizophr. Res. 2011, 130, 216–221. [Google Scholar] [CrossRef]
- Hutten, N.; Arkell, T.R.; Vinckenbosch, F.; Schepers, J.; Kevin, R.C.; Theunissen, E.L.; Kuypers, K.P.C.; McGregor, I.S.; Ramaekers, J.G. Cannabis containing equivalent concentrations of delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) induces less state anxiety than THC-dominant cannabis. Psychopharmacolology 2022, 239, 3731–3741. [Google Scholar] [CrossRef]
- Englund, A.; Oliver, D.; Chesney, E.; Chester, L.; Wilson, J.; Sovi, S.; De Micheli, A.; Hodsoll, J.; Fusar-Poli, P.; Strang, J.; et al. Does cannabidiol make cannabis safer? A randomised, double-blind, cross-over trial of cannabis with four different CBD:THC ratios. Neuropsychopharmacology 2022. [Google Scholar] [CrossRef]
- Crippa, J.A.; Guimaraes, F.S.; Campos, A.C.; Zuardi, A.W. Translational Investigation of the Therapeutic Potential of Cannabidiol (CBD): Toward a New Age. Front. Immunol. 2018, 9, 2009. [Google Scholar] [CrossRef]
- Crippa, J.A.; Derenusson, G.N.; Ferrari, T.B.; Wichert-Ana, L.; Duran, F.L.; Martin-Santos, R.; Simoes, M.V.; Bhattacharyya, S.; Fusar-Poli, P.; Atakan, Z.; et al. Neural basis of anxiolytic effects of cannabidiol (CBD) in generalized social anxiety disorder: A preliminary report. J. Psychopharmacol. 2011, 25, 121–130. [Google Scholar] [CrossRef]
- Bergamaschi, M.M.; Queiroz, R.H.; Chagas, M.H.; de Oliveira, D.C.; De Martinis, B.S.; Kapczinski, F.; Quevedo, J.; Roesler, R.; Schroder, N.; Nardi, A.E.; et al. Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naive social phobia patients. Neuropsychopharmacology 2011, 36, 1219–1226. [Google Scholar] [CrossRef]
- Das, R.K.; Kamboj, S.K.; Ramadas, M.; Yogan, K.; Gupta, V.; Redman, E.; Curran, H.V.; Morgan, C.J. Cannabidiol enhances consolidation of explicit fear extinction in humans. Psychopharmacology 2013, 226, 781–792. [Google Scholar] [CrossRef]
- Zuardi, A.W.; Shirakawa, I.; Finkelfarb, E.; Karniol, I.G. Action of cannabidiol on the anxiety and other effects produced by delta 9-THC in normal subjects. Psychopharmacology 1982, 76, 245–250. [Google Scholar] [CrossRef]
- Campos, A.C.; Ferreira, F.R.; Guimaraes, F.S. Cannabidiol blocks long-lasting behavioral consequences of predator threat stress: Possible involvement of 5HT1A receptors. J. Psychiatr. Res. 2012, 46, 1501–1510. [Google Scholar] [CrossRef]
- Bolsoni, L.M.; Crippa, J.A.S.; Hallak, J.E.C.; Guimaraes, F.S.; Zuardi, A.W. Effects of cannabidiol on symptoms induced by the recall of traumatic events in patients with posttraumatic stress disorder. Psychopharmacology 2022, 239, 1499–1507. [Google Scholar] [CrossRef]
- Dahlgren, M.K.; Lambros, A.M.; Smith, R.T.; Sagar, K.A.; El-Abboud, C.; Gruber, S.A. Clinical and cognitive improvement following full-spectrum, high-cannabidiol treatment for anxiety: Open-label data from a two-stage, phase 2 clinical trial. Commun. Med. 2022, 2, 139. [Google Scholar] [CrossRef]
- Fusar-Poli, P.; Crippa, J.A.; Bhattacharyya, S.; Borgwardt, S.J.; Allen, P.; Martin-Santos, R.; Seal, M.; Surguladze, S.A.; O’Carrol, C.; Atakan, Z.; et al. Distinct effects of delta9-tetrahydrocannabinol and cannabidiol on neural activation during emotional processing. Arch. Gen. Psychiatry 2009, 66, 95–105. [Google Scholar] [CrossRef]
- Bloomfield, M.A.P.; Yamamori, Y.; Hindocha, C.; Jones, A.P.M.; Yim, J.L.L.; Walker, H.R.; Statton, B.; Wall, M.B.; Lees, R.H.; Howes, O.D.; et al. The acute effects of cannabidiol on emotional processing and anxiety: A neurocognitive imaging study. Psychopharmacology 2022, 239, 1539–1549. [Google Scholar] [CrossRef]
- Kwee, C.M.; Baas, J.M.; van der Flier, F.E.; Groenink, L.; Duits, P.; Eikelenboom, M.; van der Veen, D.C.; Moerbeek, M.; Batelaan, N.M.; van Balkom, A.J.; et al. Cannabidiol enhancement of exposure therapy in treatment refractory patients with social anxiety disorder and panic disorder with agoraphobia: A randomised controlled trial. Eur. Neuropsychopharmacol. 2022, 59, 58–67. [Google Scholar] [CrossRef]
- Stanley, T.B.; Ferretti, M.L.; Bonn-Miller, M.O.; Irons, J.G. A Double-Blind, Randomized, Placebo-Controlled Test of the Effects of Cannabidiol on Experiences of Test Anxiety Among College Students. Cannabis Cannabinoid Res. 2022; ahead of print. [Google Scholar] [CrossRef]
- McGuire, P.; Robson, P.; Cubala, W.J.; Vasile, D.; Morrison, P.D.; Barron, R.; Taylor, A.; Wright, S. Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: A multicenter randomized controlled trial. Am. J. Psychiatry 2018, 175, 225–231. [Google Scholar] [CrossRef]
- Leweke, F.M.; Piomelli, D.; Pahlisch, F.; Muhl, D.; Gerth, C.W.; Hoyer, C.; Klosterkötter, J.; Hellmich, M.; Koethe, D. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl. Psychiatry 2012, 2, e94. [Google Scholar] [CrossRef]
- Boggs, D.L.; Nguyen, J.D.; Morgenson, D.; Taffe, M.A.; Ranganathan, M. Clinical and Preclinical Evidence for Functional Interactions of Cannabidiol and Delta(9)-Tetrahydrocannabinol. Neuropsychopharmacology 2018, 43, 142–154. [Google Scholar] [CrossRef]
- Boggs, D.L.; Surti, T.; Gupta, A.; Gupta, S.; Niciu, M.; Pittman, B.; Schnakenberg Martin, A.M.; Thurnauer, H.; Davies, A.; D’Souza, D.C.; et al. The effects of cannabidiol (CBD) on cognition and symptoms in outpatients with chronic schizophrenia a randomized placebo controlled trial. Psychopharmacology 2018, 235, 1923–1932. [Google Scholar] [CrossRef]
- Souza, J.D.R.; Pacheco, J.C.; Rossi, G.N.; de-Paulo, B.O.; Zuardi, A.W.; Guimaraes, F.S.; Hallak, J.E.C.; Crippa, J.A.; Dos Santos, R.G. Adverse Effects of Oral Cannabidiol: An Updated Systematic Review of Randomized Controlled Trials (2020–2022). Pharmaceutics 2022, 14, 2598. [Google Scholar] [CrossRef]
- van Ours, J.C.; Williams, J.; Fergusson, D.; Horwood, L.J. Cannabis use and suicidal ideation. J. Health Econ. 2013, 32, 524–537. [Google Scholar] [CrossRef]
- Brown, J.D.; Winterstein, A.G. Potential adverse drug events and drug–drug interactions with medical and consumer cannabidiol (CBD) use. J. Clin. Med. 2019, 8, 989. [Google Scholar] [CrossRef]
- Morgan, C.J.A.; Curran, H.V. Effects of cannabidiol on schizophrenia-like symptoms in people who use cannabis. Br. J. Psychiatry 2008, 192, 306–307. [Google Scholar] [CrossRef]
- Solowij, N.; Broyd, S.; Greenwood, L.m.; van Hell, H.; Martelozzo, D.; Rueb, K.; Todd, J.; Liu, Z.; Galettis, P.; Martin, J.; et al. A randomised controlled trial of vaporised Δ 9 -tetrahydrocannabinol and cannabidiol alone and in combination in frequent and infrequent cannabis users: Acute intoxication effects. Eur. Arch. Psychiatry Clin. Neurosci. 2019, 269, 17–35. [Google Scholar] [CrossRef]
- Guimaraes, F.S.; Chiaretti, T.M.; Graeff, F.G.; Zuardi, A.W. Antianxiety effect of cannabidiol in the elevated plus-maze. Psychopharmacology 1990, 100, 558–559. [Google Scholar] [CrossRef]
- Moreira, F.A.; Aguiar, D.C.; Guimaraes, F.S. Anxiolytic-like effect of cannabidiol in the rat Vogel conflict test. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2006, 30, 1466–1471. [Google Scholar] [CrossRef]
- Long, L.E.; Chesworth, R.; Huang, X.F.; McGregor, I.S.; Arnold, J.C.; Karl, T. A behavioural comparison of acute and chronic Delta9-tetrahydrocannabinol and cannabidiol in C57BL/6JArc mice. Int. J. Neuropsychopharmacol. 2010, 13, 861–876. [Google Scholar] [CrossRef]
- Crippa, J.A.; Zuardi, A.W.; Garrido, G.E.; Wichert-Ana, L.; Guarnieri, R.; Ferrari, L.; Azevedo-Marques, P.M.; Hallak, J.E.; McGuire, P.K.; Filho Busatto, G. Effects of cannabidiol (CBD) on regional cerebral blood flow. Neuropsychopharmacology 2004, 29, 417–426. [Google Scholar] [CrossRef]
- Xu, C.; Chang, T.; Du, Y.; Yu, C.; Tan, X.; Li, X. Pharmacokinetics of oral and intravenous cannabidiol and its antidepressant-like effects in chronic mild stress mouse model. Environ. Toxicol. Pharmacol. 2019, 70, 103202. [Google Scholar] [CrossRef]
- Rohleder, C.; Müller, J.K.; Lange, B.; Leweke, F.M. Cannabidiol as a potential new type of an antipsychotic. A critical review of the evidence. Front. Pharmacol. 2016, 7, 422. [Google Scholar] [CrossRef]
- Zuardi, A.W.; Antunes Rodrigues, J.; Cunha, J.M. Effects of cannabidiol in animal models predictive of antipsychotic activity. Psychopharmacology 1991, 104, 260–264. [Google Scholar] [CrossRef]
- Moreira, F.A.; Guimarães, F.S. Cannabidiol inhibits the hyperlocomotion induced by psychotomimetic drugs in mice. Eur. J. Pharmacol. 2005, 512, 199–205. [Google Scholar] [CrossRef]
- Huffstetler, C.M.; Cochran, B.; May, C.A.; Maykut, N.; Silver, C.R.; Cedeno, C.; Franck, E.; Cox, A.; Fadool, D.A. Single cannabidiol administration affects anxiety-, obsessive compulsive-, object memory-, and attention-like behaviors in mice in a sex and concentration dependent manner. Pharmacol. Biochem. Behav. 2023, 222, 173498. [Google Scholar] [CrossRef]
- Fernandes, M.; Schabarek, A.; Coper, H.; Hill, R. Modification of Δ9-THC-actions by cannabinol and cannabidiol in the rat. Psychopharmacologia 1974, 38, 329–338. [Google Scholar] [CrossRef]
- Malone, D.T.; Jongejan, D.; Taylor, D.A. Cannabidiol reverses the reduction in social interaction produced by low dose Δ9-tetrahydrocannabinol in rats. Pharmacol. Biochem. Behav. 2009, 93, 91–96. [Google Scholar] [CrossRef]
- Kasten, C.R.; Zhang, Y.; Boehm, S.L. Acute cannabinoids produce robust anxiety-like and locomotor effects in mice, but long-term consequences are age- And sex-dependent. Front. Behav. Neurosci. 2019, 13, 32. [Google Scholar] [CrossRef]
- Masataka, N. Anxiolytic Effects of Repeated Cannabidiol Treatment in Teenagers With Social Anxiety Disorders. Front. Psychol. 2019, 10, 2466. [Google Scholar] [CrossRef]
- Berger, M.; Li, E.; Rice, S.; Davey, C.G.; Ratheesh, A.; Adams, S.; Jackson, H.; Hetrick, S.; Parker, A.; Spelman, T.; et al. Cannabidiol for Treatment-Resistant Anxiety Disorders in Young People: An Open-Label Trial. J. Clin. Psychiatry 2022, 83, 42111. [Google Scholar] [CrossRef]
- Amminger, G.P.; Lin, A.; Kerr, M.; Weller, A.; Spark, J.; Pugh, C.; O’Callaghan, S.; Berger, M.; Clark, S.R.; Scott, J.G.; et al. Cannabidiol for at risk for psychosis youth: A randomized controlled trial. Early Interv. Psychiatry 2022, 16, 419–432. [Google Scholar] [CrossRef]
- Fletcher, J.M.; Page, J.B.; Francis, D.J.; Copeland, K.; Naus, M.J.; Davis, C.M.; Morris, R.; Krauskopf, D.; Satz, P. Cognitive correlates of long-term cannabis use in Costa Rican men. Arch. Gen. Psychiatry 1996, 53, 1051–1057. [Google Scholar] [CrossRef]
- Broyd, S.J.; Van Hell, H.H.; Beale, C.; Yücel, M.; Solowij, N. Acute and chronic effects of cannabinoids on human cognition—A systematic review. Biol. Psychiatry 2016, 79, 557–567. [Google Scholar] [CrossRef]
- Gruber, S.A.; Sagar, K.A. Marijuana on the Mind? The Impact of Marijuana on Cognition, Brain Structure, and Brain Function, and Related Public Policy Implications. Policy Insights Behav. Brain Sci. 2017, 4, 104–111. [Google Scholar] [CrossRef]
- Blest-Hopley, G.; Giampietro, V.; Bhattacharyya, S. Residual effects of cannabis use in adolescent and adult brains—A meta-analysis of fMRI studies. Neurosci. Biobehav. Rev. 2018, 88, 26–41. [Google Scholar] [CrossRef]
- Bilkei-Gorzo, A.; Albayram, O.; Draffehn, A.; Michel, K.; Piyanova, A.; Oppenheimer, H.; Dvir-Ginzberg, M.; Rácz, I.; Ulas, T.; Imbeault, S.; et al. A chronic low dose of Δ9-tetrahydrocannabinol (THC) restores cognitive function in old mice. Nat. Med. 2017, 23, 782–787. [Google Scholar] [CrossRef]
- Segal-Gavish, H.; Gazit, N.; Barhum, Y.; Ben-Zur, T.; Taler, M.; Hornfeld, S.H.; Gil-Ad, I.; Weizman, A.; Slutsky, I.; Niwa, M.; et al. BDNF overexpression prevents cognitive deficit elicited by adolescent cannabis exposure and host susceptibility interaction. Hum. Mol. Genet. 2017, 26, 2462–2471. [Google Scholar] [CrossRef]
- Murphy, M.; Mills, S.; Winstone, J.; Leishman, E.; Wager-Miller, J.; Bradshaw, H.; Mackie, K. Chronic Adolescent Delta(9)-Tetrahydrocannabinol Treatment of Male Mice Leads to Long-Term Cognitive and Behavioral Dysfunction, Which Are Prevented by Concurrent Cannabidiol Treatment. Cannabis Cannabinoid Res. 2017, 2, 235–246. [Google Scholar] [CrossRef]
- Kevin, R.C.; Wood, K.E.; Stuart, J.; Mitchell, A.J.; Moir, M.; Banister, S.D.; Kassiou, M.; McGregor, I.S. Acute and residual effects in adolescent rats resulting from exposure to the novel synthetic cannabinoids AB-PINACA and AB-FUBINACA. J. Psychopharmacol. 2017, 31, 757–769. [Google Scholar] [CrossRef]
- Cadoni, C.; Simola, N.; Espa, E.; Fenu, S.; Di Chiara, G. Strain dependence of adolescent Cannabis influence on heroin reward and mesolimbic dopamine transmission in adult Lewis and Fischer 344 rats. Addict. Biol. 2015, 20, 132–142. [Google Scholar] [CrossRef]
- Zamberletti, E.; Prini, P.; Speziali, S.; Gabaglio, M.; Solinas, M.; Parolaro, D.; Rubino, T. Gender-dependent behavioral and biochemical effects of adolescent delta-9-tetrahydrocannabinol in adult maternally deprived rats. Neuroscience 2012, 204, 245–257. [Google Scholar] [CrossRef]
- Realini, N.; Vigano, D.; Guidali, C.; Zamberletti, E.; Rubino, T.; Parolaro, D. Chronic URB597 treatment at adulthood reverted most depressive-like symptoms induced by adolescent exposure to THC in female rats. Neuropharmacology 2011, 60, 235–243. [Google Scholar] [CrossRef]
- O’Tuathaigh, C.M.; Hryniewiecka, M.; Behan, A.; Tighe, O.; Coughlan, C.; Desbonnet, L.; Cannon, M.; Karayiorgou, M.; Gogos, J.A.; Cotter, D.R.; et al. Chronic adolescent exposure to Delta-9-tetrahydrocannabinol in COMT mutant mice: Impact on psychosis-related and other phenotypes. Neuropsychopharmacology 2010, 35, 2262–2273. [Google Scholar] [CrossRef]
- Quinn, H.R.; Matsumoto, I.; Callaghan, P.D.; Long, L.E.; Arnold, J.C.; Gunasekaran, N.; Thompson, M.R.; Dawson, B.; Mallet, P.E.; Kashem, M.A.; et al. Adolescent rats find repeated Delta(9)-THC less aversive than adult rats but display greater residual cognitive deficits and changes in hippocampal protein expression following exposure. Neuropsychopharmacology 2008, 33, 1113–1126. [Google Scholar] [CrossRef]
- Rodriguez, G.; Neugebauer, N.M.; Yao, K.L.; Meltzer, H.Y.; Csernansky, J.G.; Dong, H. Delta9-tetrahydrocannabinol (Delta9-THC) administration after neonatal exposure to phencyclidine potentiates schizophrenia-related behavioral phenotypes in mice. Pharmacol. Biochem. Behav. 2017, 159, 6–11. [Google Scholar] [CrossRef]
- Kasten, C.R.; Zhang, Y.; Boehm, S.L., 2nd. Acute and long-term effects of Delta9-tetrahydrocannabinol on object recognition and anxiety-like activity are age- and strain-dependent in mice. Pharmacol. Biochem. Behav. 2017, 163, 9–19. [Google Scholar] [CrossRef]
- Vigano, D.; Guidali, C.; Petrosino, S.; Realini, N.; Rubino, T.; Di Marzo, V.; Parolaro, D. Involvement of the endocannabinoid system in phencyclidine-induced cognitive deficits modelling schizophrenia. Int. J. Neuropsychopharmacol. 2009, 12, 599–614. [Google Scholar] [CrossRef]
- Morgan, C.J.; Freeman, T.P.; Schafer, G.L.; Curran, H.V. Cannabidiol attenuates the appetitive effects of Delta 9-tetrahydrocannabinol in humans smoking their chosen cannabis. Neuropsychopharmacology 2010, 35, 1879–1885. [Google Scholar] [CrossRef]
- Morgan, C.J.; Schafer, G.; Freeman, T.P.; Curran, H.V. Impact of cannabidiol on the acute memory and psychotomimetic effects of smoked cannabis: Naturalistic study: Naturalistic study [corrected]. Br. J. Psychiatry J. Ment. Sci. 2010, 197, 285–290. [Google Scholar] [CrossRef]
- Morgan, C.J.; Gardener, C.; Schafer, G.; Swan, S.; Demarchi, C.; Freeman, T.P.; Warrington, P.; Rupasinghe, I.; Ramoutar, A.; Tan, N.; et al. Sub-chronic impact of cannabinoids in street cannabis on cognition, psychotic-like symptoms and psychological well-being. Psychol. Med. 2012, 42, 391–400. [Google Scholar] [CrossRef]
- Bartschi, J.G.; Greenwood, L.M.; Montgomery, A.; Dortants, L.; Weston-Green, K.; Huang, X.F.; Pai, N.; Potter, J.; Schira, M.M.; Croft, R.; et al. Cannabidiol as a Treatment for Neurobiological, Behavioral, and Psychological Symptoms in Early-Stage Dementia: A Double-Blind, Placebo-Controlled Clinical Trial Protocol. Cannabis Cannabinoid Res. 2022. [Google Scholar] [CrossRef]
- Morgan, C.J.A.; Freeman, T.P.; Hindocha, C.; Schafer, G.; Gardner, C.; Curran, H.V. Individual and combined effects of acute delta-9-tetrahydrocannabinol and cannabidiol on psychotomimetic symptoms and memory function. Transl. Psychiatry 2018, 8, 181. [Google Scholar] [CrossRef]
- Woelfl, T.; Rohleder, C.; Mueller, J.K.; Lange, B.; Reuter, A.; Schmidt, A.M.; Koethe, D.; Hellmich, M.; Leweke, F.M. Effects of Cannabidiol and Delta-9-Tetrahydrocannabinol on Emotion, Cognition, and Attention: A Double-Blind, Placebo-Controlled, Randomized Experimental Trial in Healthy Volunteers. Front. Psychiatry 2020, 11, 576877. [Google Scholar] [CrossRef]
- Hotz, J.; Fehlmann, B.; Papassotiropoulos, A.; de Quervain, D.J.; Schicktanz, N.S. Cannabidiol enhances verbal episodic memory in healthy young participants: A randomized clinical trial. J. Psychiatr. Res. 2021, 143, 327–333. [Google Scholar] [CrossRef]
- Brady, K.T.; Balster, R.L. The effects of delta 9-tetrahydrocannabinol alone and in combination with cannabidiol on fixed-interval performance in rhesus monkeys. Psychopharmacology 1980, 72, 21–26. [Google Scholar] [CrossRef]
- Taffe, M.A.; Creehan, K.M.; Vandewater, S.A. Cannabidiol fails to reverse hypothermia or locomotor suppression induced by Delta(9)-tetrahydrocannabinol in Sprague-Dawley rats. Br. J. Pharmacol. 2015, 172, 1783–1791. [Google Scholar] [CrossRef]
- Wright, M.J., Jr.; Vandewater, S.A.; Taffe, M.A. Cannabidiol attenuates deficits of visuospatial associative memory induced by Delta(9) tetrahydrocannabinol. Br. J. Pharmacol. 2013, 170, 1365–1373. [Google Scholar] [CrossRef]
- Burgdorf, J.R.; Kilmer, B.; Pacula, R.L. Heterogeneity in the composition of marijuana seized in California. Drug Alcohol Depend. 2011, 117, 59–61. [Google Scholar] [CrossRef]
- Jacobs, D.S.; Kohut, S.J.; Jiang, S.; Nikas, S.P.; Makriyannis, A.; Bergman, J. Acute and chronic effects of cannabidiol on Delta(9)-tetrahydrocannabinol (Delta(9)-THC)-induced disruption in stop signal task performance. Exp. Clin. Psychopharmacol. 2016, 24, 320–330. [Google Scholar] [CrossRef]
- Fadda, P.; Robinson, L.; Fratta, W.; Pertwee, R.G.; Riedel, G. Differential effects of THC- or CBD-rich cannabis extracts on working memory in rats. Neuropharmacology 2004, 47, 1170–1179. [Google Scholar] [CrossRef]
- Hayakawa, K.; Mishima, K.; Hazekawa, M.; Sano, K.; Irie, K.; Orito, K.; Egawa, T.; Kitamura, Y.; Uchida, N.; Nishimura, R.; et al. Cannabidiol potentiates pharmacological effects of Δ9-tetrahydrocannabinol via CB1 receptor-dependent mechanism. Brain Res. 2008, 1188, 157–164. [Google Scholar] [CrossRef]
- Rong, C.; Lee, Y.; Carmona, N.E.; Cha, D.S.; Ragguett, R.M.; Rosenblat, J.D.; Mansur, R.B.; Ho, R.C.; McIntyre, R.S. Cannabidiol in medical marijuana: Research vistas and potential opportunities. Pharmacol. Res. 2017, 121, 213–218. [Google Scholar] [CrossRef]
- Mansell, H.; Quinn, D.; Kelly, L.E.; Alcorn, J. Cannabis for the Treatment of Attention Deficit Hyperactivity Disorder: A Report of 3 Cases. Med. Cannabis Cannabinoids 2022, 5, 1–6. [Google Scholar] [CrossRef]
- Manuzak, J.A.; Gott, T.M.; Kirkwood, J.S.; Coronado, E.; Hensley-McBain, T.; Miller, C.; Cheu, R.K.; Collier, A.C.; Funderburg, N.T.; Martin, J.N.; et al. Heavy Cannabis Use Associated With Reduction in Activated and Inflammatory Immune Cell Frequencies in Antiretroviral Therapy-Treated Human Immunodeficiency Virus-Infected Individuals. Clin. Infect. Dis. 2018, 66, 1872–1882. [Google Scholar] [CrossRef]
- Rizzo, M.D.; Crawford, R.B.; Henriquez, J.E.; Aldhamen, Y.A.; Gulick, P.; Amalfitano, A.; Kaminski, N.E. HIV-infected cannabis users have lower circulating CD16+ monocytes and IFN-gamma-inducible protein 10 levels compared with nonusing HIV patients. AIDS 2018, 32, 419–429. [Google Scholar] [CrossRef]
- Irani, D.N. How much control does the brain exert over the immune system? Curr. Opin. Neurol. 2002, 15, 323–326. [Google Scholar] [CrossRef]
- Lacagnina, M.J.; Rivera, P.D.; Bilbo, S.D. Glial and Neuroimmune Mechanisms as Critical Modulators of Drug Use and Abuse. Neuropsychopharmacology 2017, 42, 156–177. [Google Scholar] [CrossRef]
- Adler, M.W.; Geller, E.B.; Chen, X.; Rogers, T.J. Viewing chemokines as a third major system of communication in the brain. AAPS J. 2006, 7, E865–E870. [Google Scholar] [CrossRef]
- Najjar, S.; Pearlman, D.M.; Alper, K.; Najjar, A.; Devinsky, O. Neuroinflammation and psychiatric illness. J. Neuroinflamm. 2013, 10, 43. [Google Scholar] [CrossRef]
- Rossi, S.; Motta, C.; Musella, A.; Centonze, D. The interplay between inflammatory cytokines and the endocannabinoid system in the regulation of synaptic transmission. Neuropharmacology 2015, 96, 105–112. [Google Scholar] [CrossRef]
- Stella, N. Cannabinoid and cannabinoid-like receptors in microglia, astrocytes, and astrocytomas. Glia 2010, 58, 1017–1030. [Google Scholar] [CrossRef]
- Al-Ghezi, Z.Z.; Busbee, P.B.; Alghetaa, H.; Nagarkatti, P.S.; Nagarkatti, M. Combination of cannabinoids, delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD), mitigates experimental autoimmune encephalomyelitis (EAE) by altering the gut microbiome. Brain Behav. Immun. 2019, 82, 25–35. [Google Scholar] [CrossRef]
- Watt, G.; Karl, T. In vivo Evidence for Therapeutic Properties of Cannabidiol (CBD) for Alzheimer’s Disease. Front. Pharmacol. 2017, 8, 20. [Google Scholar] [CrossRef]
- Sarne, Y.; Asaf, F.; Fishbein, M.; Gafni, M.; Keren, O. The dual neuroprotective-neurotoxic profile of cannabinoid drugs. Br. J. Pharmacol. 2011, 163, 1391–1401. [Google Scholar] [CrossRef]
- Lawston, J.; Borella, A.; Robinson, J.K.; Whitaker-Azmitia, P.M. Changes in hippocampal morphology following chronic treatment with the synthetic cannabinoid WIN 55,212-2. Brain Res. 2000, 877, 407–410. [Google Scholar] [CrossRef]
- Cutando, L.; Busquets-Garcia, A.; Puighermanal, E.; Gomis-Gonzalez, M.; Delgado-Garcia, J.M.; Gruart, A.; Maldonado, R.; Ozaita, A. Microglial activation underlies cerebellar deficits produced by repeated cannabis exposure. J. Clin. Investig. 2013, 123, 2816–2831. [Google Scholar] [CrossRef]
- Pintori, N.; Castelli, M.P.; Miliano, C.; Simola, N.; Fadda, P.; Fattore, L.; Scherma, M.; Ennas, M.G.; Mostallino, R.; Flore, G.; et al. Repeated exposure to JWH-018 induces adaptive changes in the mesolimbic and mesocortical dopaminergic pathways, glial cells alterations, and behavioural correlates. Br. J. Pharmacol. 2021, 178, 3476–3497. [Google Scholar] [CrossRef]
- Stiglick, A.; Llewellyn, M.E.; Kalant, H. Residual effects of prolonged cannabis treatment on shuttle-box avoidance in the rat. Psychopharmacology 1984, 84, 476–479. [Google Scholar] [CrossRef]
- Landfield, P.W.; Cadwallader, L.B.; Vinsant, S. Quantitative changes in hippocampal structure following long-term exposure to delta 9-tetrahydrocannabinol: Possible mediation by glucocorticoid systems. Brain Res. 1988, 443, 47–62. [Google Scholar] [CrossRef]
- Scallet, A.C. Neurotoxicology of cannabis and THC: A review of chronic exposure studies in animals. Pharmacol. Biochem. Behav. 1991, 40, 671–676. [Google Scholar] [CrossRef]
- Zamberletti, E.; Gabaglio, M.; Prini, P.; Rubino, T.; Parolaro, D. Cortical neuroinflammation contributes to long-term cognitive dysfunctions following adolescent delta-9-tetrahydrocannabinol treatment in female rats. Eur. Neuropsychopharmacol. 2015, 25, 2404–2415. [Google Scholar] [CrossRef]
- Zamberletti, E.; Gabaglio, M.; Grilli, M.; Prini, P.; Catanese, A.; Pittaluga, A.; Marchi, M.; Rubino, T.; Parolaro, D. Long-term hippocampal glutamate synapse and astrocyte dysfunctions underlying the altered phenotype induced by adolescent THC treatment in male rats. Pharmacol. Res. 2016, 111, 459–470. [Google Scholar] [CrossRef]
- Moretti, S.; Castelli, M.; Franchi, S.; Raggi, M.A.; Mercolini, L.; Protti, M.; Somaini, L.; Panerai, A.E.; Sacerdote, P. Delta(9)-Tetrahydrocannabinol-induced anti-inflammatory responses in adolescent mice switch to proinflammatory in adulthood. J. Leukoc. Biol. 2014, 96, 523–534. [Google Scholar] [CrossRef]
- Moretti, S.; Franchi, S.; Castelli, M.; Amodeo, G.; Somaini, L.; Panerai, A.; Sacerdote, P. Exposure of Adolescent Mice to Delta-9-Tetrahydrocannabinol Induces Long-Lasting Modulation of Pro- and Anti-Inflammatory Cytokines in Hypothalamus and Hippocampus Similar to that Observed for Peripheral Macrophages. J. Neuroimmune Pharmacol. 2015, 10, 371–379. [Google Scholar] [CrossRef]
- Vallee, A.; Lecarpentier, Y.; Guillevin, R.; Vallee, J.N. Effects of cannabidiol interactions with Wnt/beta-catenin pathway and PPARgamma on oxidative stress and neuroinflammation in Alzheimer’s disease. Acta Biochim. Biophys. Sin. 2017, 49, 853–866. [Google Scholar] [CrossRef]
- Watt, G.; Shang, K.; Zieba, J.; Olaya, J.; Li, H.; Garner, B.; Karl, T. Chronic Treatment with 50 mg/kg Cannabidiol Improves Cognition and Moderately Reduces Abeta40 Levels in 12-Month-Old Male AbetaPPswe/PS1DeltaE9 Transgenic Mice. J. Alzheimer’s Dis. 2020, 74, 937–950. [Google Scholar] [CrossRef]
- Yang, S.; Du, Y.; Zhao, X.; Tang, Q.; Su, W.; Hu, Y.; Yu, P. Cannabidiol Enhances Microglial Beta-Amyloid Peptide Phagocytosis and Clearance via Vanilloid Family Type 2 Channel Activation. Int. J. Mol. Sci. 2022, 23, 5367. [Google Scholar] [CrossRef]
- Giuliano, C.; Francavilla, M.; Ongari, G.; Petese, A.; Ghezzi, C.; Rossini, N.; Blandini, F.; Cerri, S. Neuroprotective and Symptomatic Effects of Cannabidiol in an Animal Model of Parkinson’s Disease. Int. J. Mol. Sci. 2021, 22, 8920. [Google Scholar] [CrossRef]
- Hosseinzadeh, M.; Nikseresht, S.; Khodagholi, F.; Naderi, N.; Maghsoudi, N. Cannabidiol Post-Treatment Alleviates Rat Epileptic-Related Behaviors and Activates Hippocampal Cell Autophagy Pathway Along with Antioxidant Defense in Chronic Phase of Pilocarpine-Induced Seizure. J. Mol. Neurosci. 2016, 58, 432–440. [Google Scholar] [CrossRef]
- Leo, A.; Russo, E.; Elia, M. Cannabidiol and epilepsy: Rationale and therapeutic potential. Pharmacol. Res. 2016, 107, 85–92. [Google Scholar] [CrossRef]
- Elliott, D.M.; Singh, N.; Nagarkatti, M.; Nagarkatti, P.S. Cannabidiol Attenuates Experimental Autoimmune Encephalomyelitis Model of Multiple Sclerosis Through Induction of Myeloid-Derived Suppressor Cells. Front. Immunol. 2018, 9, 1782. [Google Scholar] [CrossRef]
- Dopkins, N.; Miranda, K.; Wilson, K.; Holloman, B.L.; Nagarkatti, P.; Nagarkatti, M. Effects of Orally Administered Cannabidiol on Neuroinflammation and Intestinal Inflammation in the Attenuation of Experimental Autoimmune Encephalomyelitis. J. Neuroimmune Pharmacol. 2022, 17, 15–32. [Google Scholar] [CrossRef]
- Nichols, J.M.; Kummari, E.; Sherman, J.; Yang, E.J.; Dhital, S.; Gilfeather, C.; Yray, G.; Morgan, T.; Kaplan, B.L.F. CBD Suppression of EAE Is Correlated with Early Inhibition of Splenic IFN-gamma + CD8+ T Cells and Modest Inhibition of Neuroinflammation. J. Neuroimmune Pharmacol. 2021, 16, 346–362. [Google Scholar] [CrossRef]
- Ceprian, M.; Jimenez-Sanchez, L.; Vargas, C.; Barata, L.; Hind, W.; Martinez-Orgado, J. Cannabidiol reduces brain damage and improves functional recovery in a neonatal rat model of arterial ischemic stroke. Neuropharmacology 2017, 116, 151–159. [Google Scholar] [CrossRef]
- Meyer, E.; Rieder, P.; Gobbo, D.; Candido, G.; Scheller, A.; de Oliveira, R.M.W.; Kirchhoff, F. Cannabidiol Exerts a Neuroprotective and Glia-Balancing Effect in the Subacute Phase of Stroke. Int. J. Mol. Sci. 2022, 23, 12886. [Google Scholar] [CrossRef]
- Mori, M.A.; Meyer, E.; Soares, L.M.; Milani, H.; Guimaraes, F.S.; de Oliveira, R.M.W. Cannabidiol reduces neuroinflammation and promotes neuroplasticity and functional recovery after brain ischemia. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2017, 75, 94–105. [Google Scholar] [CrossRef]
- Garcia-Arencibia, M.; Gonzalez, S.; de Lago, E.; Ramos, J.A.; Mechoulam, R.; Fernandez-Ruiz, J. Evaluation of the neuroprotective effect of cannabinoids in a rat model of Parkinson’s disease: Importance of antioxidant and cannabinoid receptor-independent properties. Brain Res. 2007, 1134, 162–170. [Google Scholar] [CrossRef]
- Marinelli, L.; Balestrino, M.; Mori, L.; Puce, L.; Rosa, G.M.; Giorello, L.; Curra, A.; Fattapposta, F.; Serrati, C.; Gandolfo, C.; et al. A randomised controlled cross-over double-blind pilot study protocol on THC:CBD oromucosal spray efficacy as an add-on therapy for post-stroke spasticity. BMJ Open 2017, 7, e016843. [Google Scholar] [CrossRef]
- Martin-Moreno, A.M.; Reigada, D.; Ramirez, B.G.; Mechoulam, R.; Innamorato, N.; Cuadrado, A.; de Ceballos, M.L. Cannabidiol and other cannabinoids reduce microglial activation in vitro and in vivo: Relevance to Alzheimer’s disease. Mol. Pharmacol. 2011, 79, 964–973. [Google Scholar] [CrossRef]
- Pazos, M.R.; Cinquina, V.; Gomez, A.; Layunta, R.; Santos, M.; Fernandez-Ruiz, J.; Martinez-Orgado, J. Cannabidiol administration after hypoxia-ischemia to newborn rats reduces long-term brain injury and restores neurobehavioral function. Neuropharmacology 2012, 63, 776–783. [Google Scholar] [CrossRef]
- Pazos, M.R.; Mohammed, N.; Lafuente, H.; Santos, M.; Martinez-Pinilla, E.; Moreno, E.; Valdizan, E.; Romero, J.; Pazos, A.; Franco, R.; et al. Mechanisms of cannabidiol neuroprotection in hypoxic-ischemic newborn pigs: Role of 5HT(1A) and CB2 receptors. Neuropharmacology 2013, 71, 282–291. [Google Scholar] [CrossRef]
- Jones, E.; Vlachou, S. A Critical Review of the Role of the Cannabinoid Compounds Delta(9)-Tetrahydrocannabinol (Delta(9)-THC) and Cannabidiol (CBD) and their Combination in Multiple Sclerosis Treatment. Molecules 2020, 25, 4930. [Google Scholar] [CrossRef]
- Velayudhan, L.; McGoohan, K.; Bhattacharyya, S. Safety and tolerability of natural and synthetic cannabinoids in adults aged over 50 years: A systematic review and meta-analysis. PLoS Med. 2021, 18, e1003524. [Google Scholar] [CrossRef]
- Pagano, C.; Navarra, G.; Coppola, L.; Avilia, G.; Bifulco, M.; Laezza, C. Cannabinoids: Therapeutic Use in Clinical Practice. Int. J. Mol. Sci. 2022, 23, 3344. [Google Scholar] [CrossRef]
- Kmietowicz, Z. Cannabis based drug is licensed for spasticity in patients with MS. BMJ 2010, 340, c3363. [Google Scholar] [CrossRef]
- Fernandez-Ruiz, J.; Sagredo, O.; Pazos, M.R.; Garcia, C.; Pertwee, R.; Mechoulam, R.; Martinez-Orgado, J. Cannabidiol for neurodegenerative disorders: Important new clinical applications for this phytocannabinoid? Br. J. Clin. Pharmacol. 2013, 75, 323–333. [Google Scholar] [CrossRef]
- Majdi, F.; Taheri, F.; Salehi, P.; Motaghinejad, M.; Safari, S. Cannabinoids Delta(9)-tetrahydrocannabinol and cannabidiol may be effective against methamphetamine induced mitochondrial dysfunction and inflammation by modulation of Toll-like type-4(Toll-like 4) receptors and NF-kappaB signaling. Med. Hypotheses 2019, 133, 109371. [Google Scholar] [CrossRef]
- Garcia-Baos, A.; Puig-Reyne, X.; Garcia-Algar, O.; Valverde, O. Cannabidiol attenuates cognitive deficits and neuroinflammation induced by early alcohol exposure in a mice model. Biomed. Pharmacol. 2021, 141, 111813. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
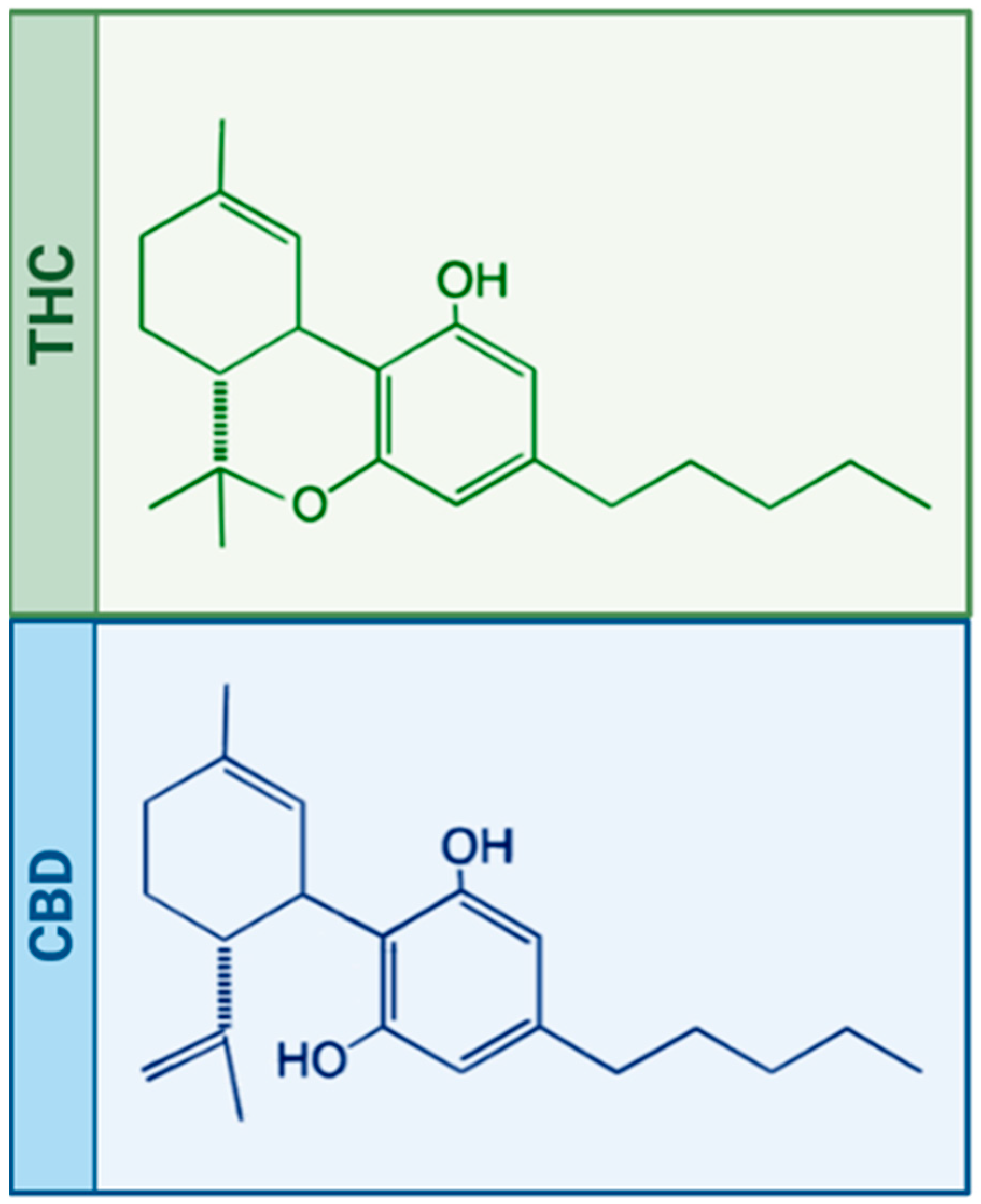
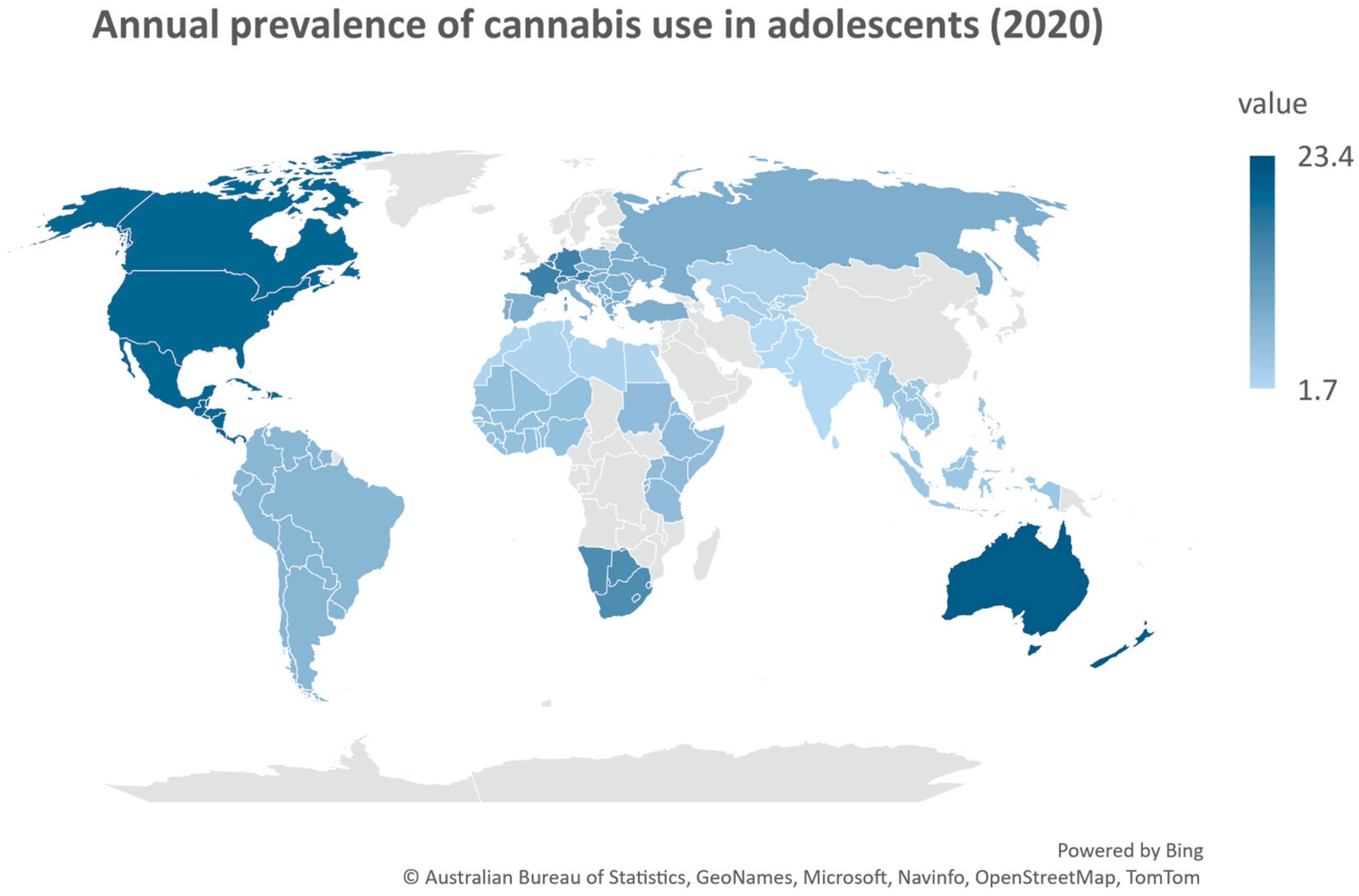
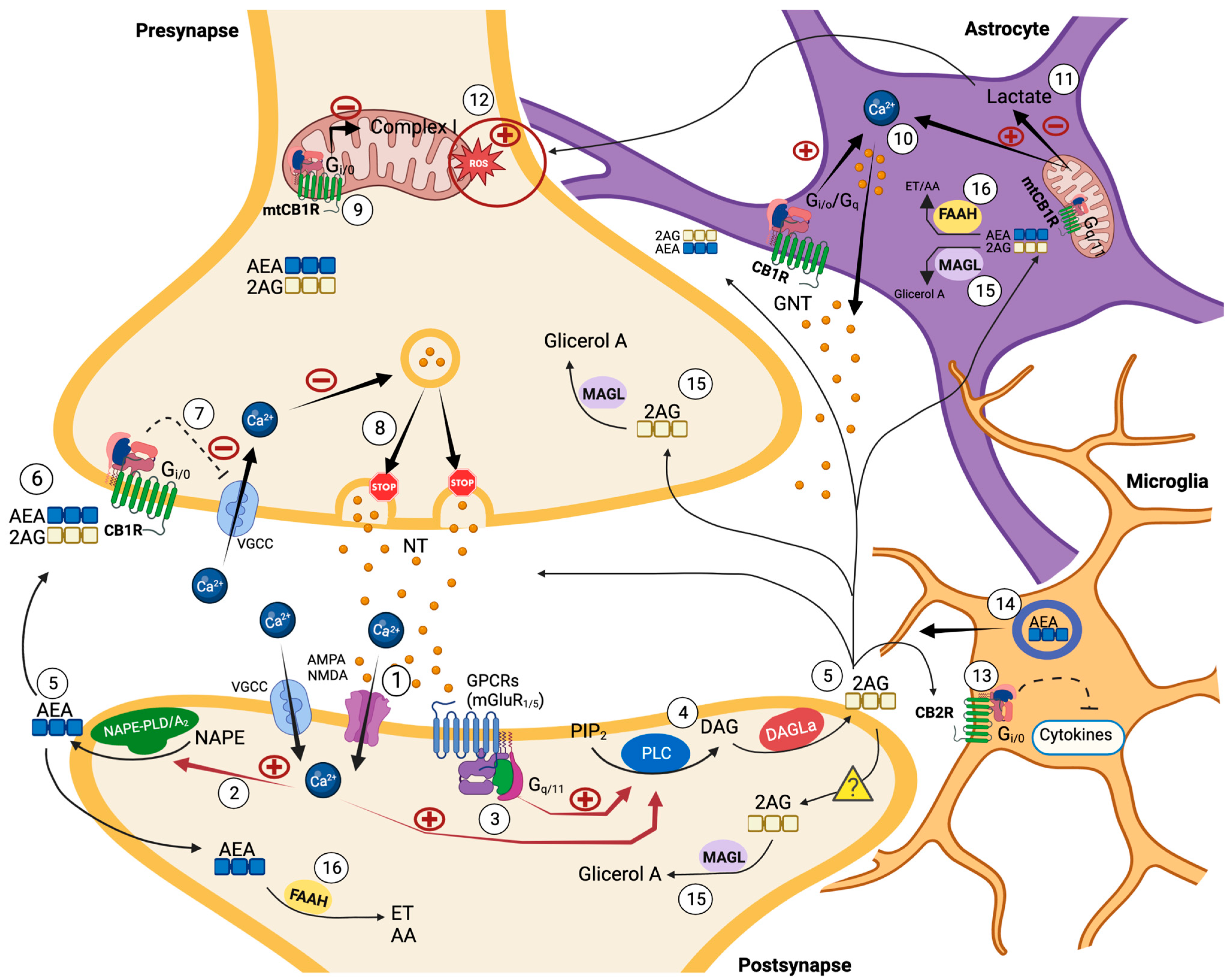
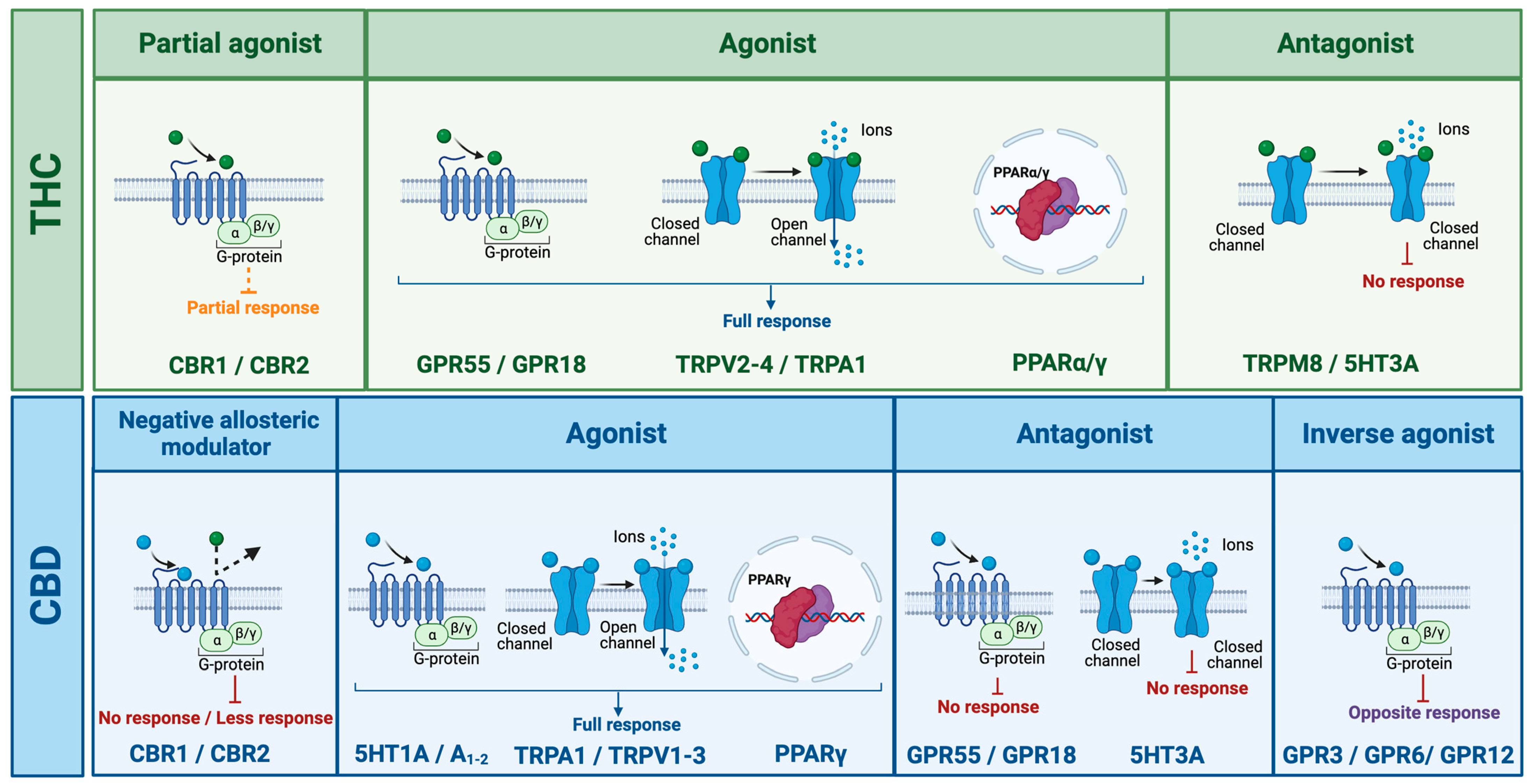
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pintori, N.; Caria, F.; De Luca, M.A.; Miliano, C. THC and CBD: Villain versus Hero? Insights into Adolescent Exposure. Int. J. Mol. Sci. 2023, 24, 5251. https://doi.org/10.3390/ijms24065251
Pintori N, Caria F, De Luca MA, Miliano C. THC and CBD: Villain versus Hero? Insights into Adolescent Exposure. International Journal of Molecular Sciences. 2023; 24(6):5251. https://doi.org/10.3390/ijms24065251
Chicago/Turabian StylePintori, Nicholas, Francesca Caria, Maria Antonietta De Luca, and Cristina Miliano. 2023. "THC and CBD: Villain versus Hero? Insights into Adolescent Exposure" International Journal of Molecular Sciences 24, no. 6: 5251. https://doi.org/10.3390/ijms24065251
APA StylePintori, N., Caria, F., De Luca, M. A., & Miliano, C. (2023). THC and CBD: Villain versus Hero? Insights into Adolescent Exposure. International Journal of Molecular Sciences, 24(6), 5251. https://doi.org/10.3390/ijms24065251






