Bone Marrow Stem Cells Derived from Nerves Have Neurogenic Properties and Potential Utility for Regenerative Therapy
Abstract
1. Introduction
2. Results
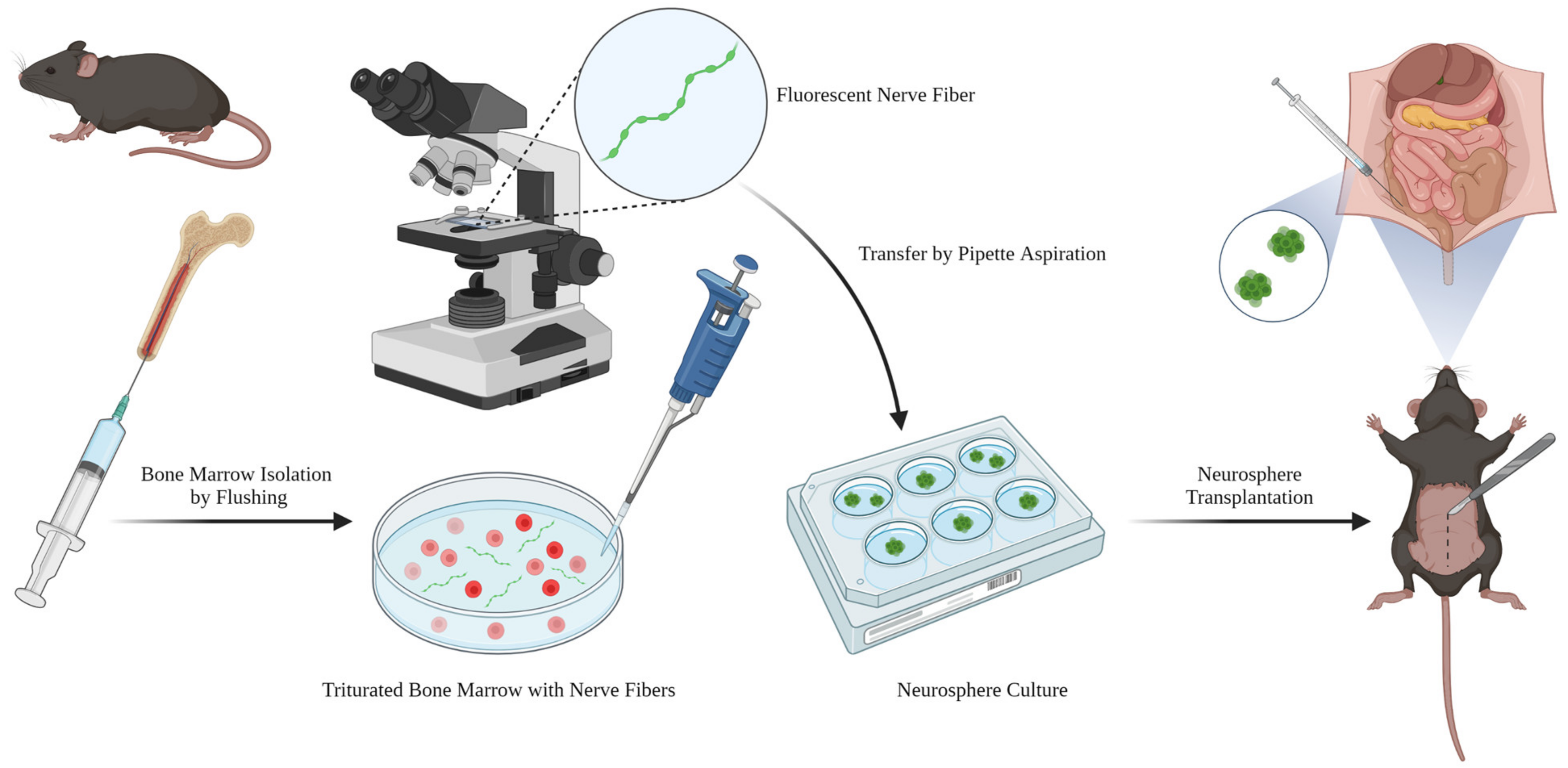
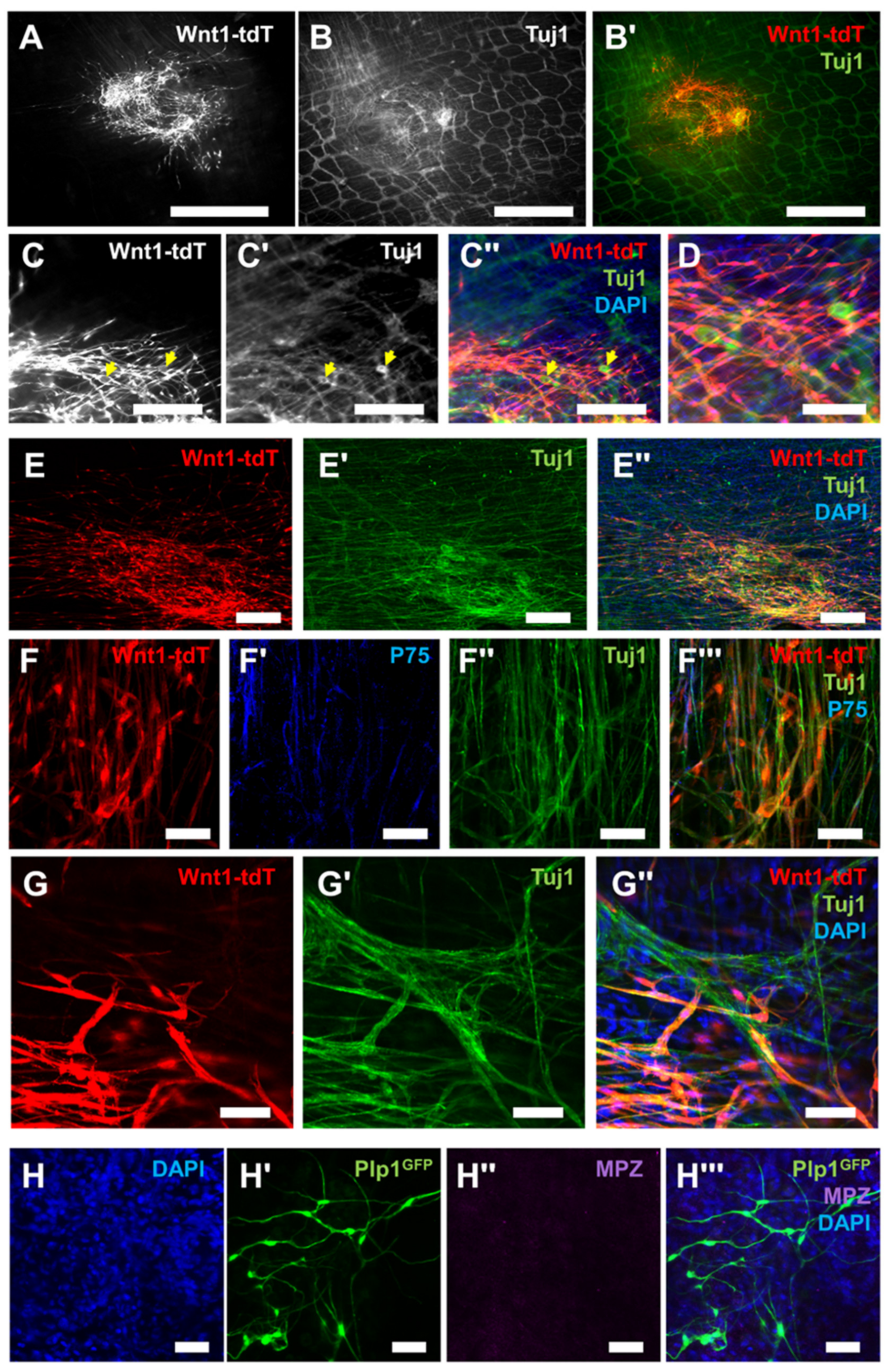
2.1. Schwann Cells Reside along Nerve Fiber Projections in the Bone Marrow in Close Apposition to Blood Vessels
2.2. Schwann Cells Acquire Neural Stem Cell Properties In Vitro
2.3. Bone Marrow Neural Stem Cells Integrate with the Enteric Nervous System in the Gut
3. Discussion
4. Methods
4.1. Study Design
4.2. Mice
4.3. Nerve Fiber Isolation Procedure
4.4. Neurosphere Culture
4.5. Quantitative PCR
4.6. In Vivo Neurosphere Transplantation
4.7. Immunocytochemistry for In Vitro Experiments
4.8. Immunohistochemistry for In Vivo Experiments
4.9. Imaging
4.10. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Adameyko, I.; Lallemend, F.; Aquino, J.B.; Pereira, J.A.; Topilko, P.; Müller, T.; Fritz, N.; Beljajeva, A.; Mochii, M.; Liste, I.; et al. Schwann cell precursors from nerve innervation are a cellular origin of melanocytes in skin. Cell 2009, 139, 366–379. [Google Scholar] [CrossRef]
- Joseph, N.M.; Mukouyama, Y.S.; Mosher, J.T.; Jaegle, M.; Crone, S.A.; Dormand, E.L.; Lee, K.F.; Meijer, D.; Anderson, D.J.; Morrison, S.J. Neural crest stem cells undergo multilineage differentiation in developing peripheral nerves to generate endoneurial fibroblasts in addition to Schwann cells. Development 2004, 131, 5599–5612. [Google Scholar] [CrossRef] [PubMed]
- Dyachuk, V.; Furlan, A.; Shahidi, M.K.; Giovenco, M.; Kaukua, N.; Konstantinidou, C.; Pachnis, V.; Memic, F.; Marklund, U.; Müller, T.; et al. Neurodevelopment. Parasympathetic neurons originate from nerve-associated peripheral glial progenitors. Science 2014, 345, 82–87. [Google Scholar] [CrossRef]
- Espinosa-Medina, I.; Jevans, B.; Boismoreau, F.; Chettouh, Z.; Enomoto, H.; Müller, T.; Birchmeier, C.; Burns, A.J.; Brunet, J.F. Dual origin of enteric neurons in vagal Schwann cell precursors and the sympathetic neural crest. Proc. Natl. Acad. Sci. USA 2017, 114, 11980–11985. [Google Scholar] [CrossRef] [PubMed]
- Uesaka, T.; Nagashimada, M.; Enomoto, H. Neuronal Differentiation in Schwann Cell Lineage Underlies Postnatal Neurogenesis in the Enteric Nervous System. J. Neurosci. 2015, 35, 9879–9888. [Google Scholar] [CrossRef]
- El-Nachef, W.N.; Bronner, M.E. De novo enteric neurogenesis in post-embryonic zebrafish from Schwann cell precursors rather than resident cell types. Development 2020, 147, dev186619. [Google Scholar] [CrossRef] [PubMed]
- Stavely, R.; Hotta, R.; Picard, N.; Rahman, A.A.; Pan, W.; Bhave, S.; Omer, M.; Ho, W.L.N.; Guyer, R.A.; Goldstein, A.M. Schwann cells in the subcutaneous adipose tissue have neurogenic potential and can be used for regenerative therapies. Sci. Transl. Med. 2022, 14, eabl8753. [Google Scholar] [CrossRef]
- Guyer, R.A.; Stavely, R.; Robertson, K.; Bhave, S.; Mueller, J.L.; Picard, N.M.; Hotta, R.; Kaltschmidt, J.A.; Goldstein, A.M. Single-cell multiome sequencing clarifies enteric glial diversity and identifies an intraganglionic population poised for neurogenesis. Cell Rep. 2023, 42, 112194. [Google Scholar] [CrossRef]
- Calvo, W.; Forteza-Vila, J. Schwann cells of the bone marrow. Blood 1970, 36, 180–188. [Google Scholar] [CrossRef]
- Yu, V.W.; Scadden, D.T. Heterogeneity of the bone marrow niche. Curr. Opin. Hematol. 2016, 23, 331–338. [Google Scholar] [CrossRef]
- Méndez-Ferrer, S.; Lucas, D.; Battista, M.; Frenette, P.S. Haematopoietic stem cell release is regulated by circadian oscillations. Nature 2008, 452, 442–447. [Google Scholar] [CrossRef]
- Yamazaki, S.; Ema, H.; Karlsson, G.; Yamaguchi, T.; Miyoshi, H.; Shioda, S.; Taketo, M.M.; Karlsson, S.; Iwama, A.; Nakauchi, H. Nonmyelinating Schwann cells maintain hematopoietic stem cell hibernation in the bone marrow niche. Cell 2011, 147, 1146–1158. [Google Scholar] [CrossRef]
- Thai, J.; Green, A.C.; Stamp, L.A.; Spencer, N.J.; Purton, L.E.; Ivanusic, J. A population of nonneuronal GFRα3-expressing cells in the bone marrow resembles nonmyelinating Schwann cells. Cell Tissue Res. 2019, 378, 441–456. [Google Scholar] [CrossRef]
- Kanate, A.S.; Majhail, N.S.; Savani, B.N.; Bredeson, C.; Champlin, R.E.; Crawford, S.; Giralt, S.A.; LeMaistre, C.F.; Marks, D.I.; Omel, J.L.; et al. Indications for Hematopoietic Cell Transplantation and Immune Effector Cell Therapy: Guidelines from the American Society for Transplantation and Cellular Therapy. Biol. Blood Marrow Transpl. 2020, 26, 1247–1256. [Google Scholar] [CrossRef]
- Hoang, D.M.; Pham, P.T.; Bach, T.Q.; Ngo, A.T.L.; Nguyen, Q.T.; Phan, T.T.K.; Nguyen, G.H.; Le, P.T.T.; Hoang, V.T.; Forsyth, N.R.; et al. Stem cell-based therapy for human diseases. Signal Transduct. Target 2022, 7, 272. [Google Scholar] [CrossRef]
- Ramli, K.; Aminath Gasim, I.; Ahmad, A.A.; Hassan, S.; Law, Z.K.; Tan, G.C.; Baharuddin, A.; Naicker, A.S.; Htwe, O.; Mohammed Haflah, N.H.; et al. Human bone marrow-derived MSCs spontaneously express specific Schwann cell markers. Cell Biol. Int. 2019, 43, 233–252. [Google Scholar] [CrossRef] [PubMed]
- Mallon, B.S.; Shick, H.E.; Kidd, G.J.; Macklin, W.B. Proteolipid promoter activity distinguishes two populations of NG2-positive cells throughout neonatal cortical development. J. Neurosci. 2002, 22, 876–885. [Google Scholar] [CrossRef] [PubMed]
- Zhan, X.; Cao, M.; Yoo, A.S.; Zhang, Z.; Chen, L.; Crabtree, G.R.; Wu, J.I. Generation of BAF53b-Cre transgenic mice with pan-neuronal Cre activities. Genesis 2015, 53, 440–448. [Google Scholar] [CrossRef]
- Bhave, S.; Arciero, E.; Baker, C.; Ho, W.L.; Stavely, R.; Goldstein, A.M.; Hotta, R. Enteric neuronal cell therapy reverses architectural changes in a novel diphtheria toxin-mediated model of colonic aganglionosis. Sci. Rep. 2019, 9, 18756. [Google Scholar] [CrossRef] [PubMed]
- Nagy, N.; Barad, C.; Hotta, R.; Bhave, S.; Arciero, E.; Dora, D.; Goldstein, A.M. Collagen 18 and agrin are secreted by neural crest cells to remodel their microenvironment and regulate their migration during enteric nervous system development. Development 2018, 145, dev160317. [Google Scholar] [CrossRef]
- Méndez-Ferrer, S.; Michurina, T.V.; Ferraro, F.; Mazloom, A.R.; Macarthur, B.D.; Lira, S.A.; Scadden, D.T.; Ma’ayan, A.; Enikolopov, G.N.; Frenette, P.S. Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature 2010, 466, 829–834. [Google Scholar] [CrossRef] [PubMed]
- Isern, J.; García-García, A.; Martín, A.M.; Arranz, L.; Martín-Pérez, D.; Torroja, C.; Sánchez-Cabo, F.; Méndez-Ferrer, S. The neural crest is a source of mesenchymal stem cells with specialized hematopoietic stem cell niche function. Elife 2014, 3, e03696. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.; Taylor, G.I.; Newgreen, D.F. The pattern of neurovascular development in the forelimb of the quail embryo. Dev. Biol. 2002, 249, 300–320. [Google Scholar] [CrossRef] [PubMed]
- Bautch, V.L.; James, J.M. Neurovascular development: The beginning of a beautiful friendship. Cell Adh. Migr. 2009, 3, 199–204. [Google Scholar] [CrossRef]
- Carmeliet, P. Blood vessels and nerves: Common signals, pathways and diseases. Nat. Rev. Genet. 2003, 4, 710–720. [Google Scholar] [CrossRef]
- Eichmann, A.; Thomas, J.L. Molecular parallels between neural and vascular development. Cold Spring Harb. Perspect. Med. 2013, 3, a006551. [Google Scholar] [CrossRef]
- Gelfand, M.V.; Hong, S.; Gu, C. Guidance from above: Common cues direct distinct signaling outcomes in vascular and neural patterning. Trends Cell Biol. 2009, 19, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Quaegebeur, A.; Lange, C.; Carmeliet, P. The neurovascular link in health and disease: Molecular mechanisms and therapeutic implications. Neuron 2011, 71, 406–424. [Google Scholar] [CrossRef] [PubMed]
- Taylor, G.I.; Gianoutsos, M.P.; Morris, S.F. The neurovascular territories of the skin and muscles: Anatomic study and clinical implications. Plast. Reconstr. Surg. 1994, 94, 1–36. [Google Scholar] [CrossRef]
- Erskine, L.; Reijntjes, S.; Pratt, T.; Denti, L.; Schwarz, Q.; Vieira, J.M.; Alakakone, B.; Shewan, D.; Ruhrberg, C. VEGF signaling through neuropilin 1 guides commissural axon crossing at the optic chiasm. Neuron 2011, 70, 951–965. [Google Scholar] [CrossRef]
- Suchting, S.; Heal, P.; Tahtis, K.; Stewart, L.M.; Bicknell, R. Soluble Robo4 receptor inhibits in vivo angiogenesis and endothelial cell migration. FASEB J. 2005, 19, 121–123. [Google Scholar] [CrossRef] [PubMed]
- Zacchigna, S.; Pattarini, L.; Zentilin, L.; Moimas, S.; Carrer, A.; Sinigaglia, M.; Arsic, N.; Tafuro, S.; Sinagra, G.; Giacca, M. Bone marrow cells recruited through the neuropilin-1 receptor promote arterial formation at the sites of adult neoangiogenesis in mice. J. Clin. Investig. 2008, 118, 2062–2075. [Google Scholar] [CrossRef] [PubMed]
- Burnstock, G.; Ralevic, V. New insights into the local regulation of blood flow by perivascular nerves and endothelium. Br. J. Plast. Surg. 1994, 47, 527–543. [Google Scholar] [CrossRef]
- Martin, P.; Lewis, J. Origins of the neurovascular bundle: Interactions between developing nerves and blood vessels in embryonic chick skin. Int. J. Dev. Biol. 1989, 33, 379–387. [Google Scholar] [PubMed]
- Mukouyama, Y.S.; Shin, D.; Britsch, S.; Taniguchi, M.; Anderson, D.J. Sensory nerves determine the pattern of arterial differentiation and blood vessel branching in the skin. Cell 2002, 109, 693–705. [Google Scholar] [CrossRef]
- George, L.; Dunkel, H.; Hunnicutt, B.J.; Filla, M.; Little, C.; Lansford, R.; Lefcort, F. In vivo time-lapse imaging reveals extensive neural crest and endothelial cell interactions during neural crest migration and formation of the dorsal root and sympathetic ganglia. Dev. Biol. 2016, 413, 70–85. [Google Scholar] [CrossRef]
- Shen, Q.; Goderie, S.K.; Jin, L.; Karanth, N.; Sun, Y.; Abramova, N.; Vincent, P.; Pumiglia, K.; Temple, S. Endothelial cells stimulate self-renewal and expand neurogenesis of neural stem cells. Science 2004, 304, 1338–1340. [Google Scholar] [CrossRef]
- Zacchigna, S.; Lambrechts, D.; Carmeliet, P. Neurovascular signalling defects in neurodegeneration. Nat. Rev. Neurosci. 2008, 9, 169–181. [Google Scholar] [CrossRef]
- Etchevers, H.C.; Vincent, C.; Le Douarin, N.M.; Couly, G.F. The cephalic neural crest provides pericytes and smooth muscle cells to all blood vessels of the face and forebrain. Development 2001, 128, 1059–1068. [Google Scholar] [CrossRef]
- Korn, J.; Christ, B.; Kurz, H. Neuroectodermal origin of brain pericytes and vascular smooth muscle cells. J. Comp. Neurol. 2002, 442, 78–88. [Google Scholar] [CrossRef]
- Calloni, G.W.; Glavieux-Pardanaud, C.; Le Douarin, N.M.; Dupin, E. Sonic Hedgehog promotes the development of multipotent neural crest progenitors endowed with both mesenchymal and neural potentials. Proc. Natl. Acad. Sci. USA 2007, 104, 19879–19884. [Google Scholar] [CrossRef] [PubMed]
- Calloni, G.W.; Le Douarin, N.M.; Dupin, E. High frequency of cephalic neural crest cells shows coexistence of neurogenic, melanogenic, and osteogenic differentiation capacities. Proc. Natl. Acad. Sci. USA 2009, 106, 8947–8952. [Google Scholar] [CrossRef]
- Kubota, Y.; Takubo, K.; Hirashima, M.; Nagoshi, N.; Kishi, K.; Okuno, Y.; Nakamura-Ishizu, A.; Sano, K.; Murakami, M.; Ema, M.; et al. Isolation and function of mouse tissue resident vascular precursors marked by myelin protein zero. J. Exp. Med. 2011, 208, 949–960. [Google Scholar] [CrossRef] [PubMed]
- Nagoshi, N.; Shibata, S.; Kubota, Y.; Nakamura, M.; Nagai, Y.; Satoh, E.; Morikawa, S.; Okada, Y.; Mabuchi, Y.; Katoh, H.; et al. Ontogeny and multipotency of neural crest-derived stem cells in mouse bone marrow, dorsal root ganglia, and whisker pad. Cell Stem Cell 2008, 2, 392–403. [Google Scholar] [CrossRef]
- Nagoshi, N.; Shibata, S.; Nakamura, M.; Matsuzaki, Y.; Toyama, Y.; Okano, H. Neural crest-derived stem cells display a wide variety of characteristics. J. Cell Biochem. 2009, 107, 1046–1052. [Google Scholar] [CrossRef] [PubMed]
- Dulauroy, S.; Di Carlo, S.E.; Langa, F.; Eberl, G.; Peduto, L. Lineage tracing and genetic ablation of ADAM12(+) perivascular cells identify a major source of profibrotic cells during acute tissue injury. Nat. Med. 2012, 18, 1262–1270. [Google Scholar] [CrossRef] [PubMed]
- Göritz, C.; Dias, D.O.; Tomilin, N.; Barbacid, M.; Shupliakov, O.; Frisén, J. A pericyte origin of spinal cord scar tissue. Science 2011, 333, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Müller, S.M.; Stolt, C.C.; Terszowski, G.; Blum, C.; Amagai, T.; Kessaris, N.; Iannarelli, P.; Richardson, W.D.; Wegner, M.; Rodewald, H.R. Neural crest origin of perivascular mesenchyme in the adult thymus. J. Immunol. 2008, 180, 5344–5351. [Google Scholar] [CrossRef]
- Doherty, M.J.; Ashton, B.A.; Walsh, S.; Beresford, J.N.; Grant, M.E.; Canfield, A.E. Vascular pericytes express osteogenic potential in vitro and in vivo. J. Bone Min. Res. 1998, 13, 828–838. [Google Scholar] [CrossRef]
- Farrington-Rock, C.; Crofts, N.J.; Doherty, M.J.; Ashton, B.A.; Griffin-Jones, C.; Canfield, A.E. Chondrogenic and adipogenic potential of microvascular pericytes. Circulation 2004, 110, 2226–2232. [Google Scholar] [CrossRef]
- Xu, W.; Sun, Y.; Zhang, J.; Xu, K.; Pan, L.; He, L.; Song, Y.; Njunge, L.; Xu, Z.; Chiang, M.Y.; et al. Perivascular-derived stem cells with neural crest characteristics are involved in tendon repair. Stem Cells Dev. 2015, 24, 857–868. [Google Scholar] [CrossRef]
- Coste, C.; Neirinckx, V.; Sharma, A.; Agirman, G.; Rogister, B.; Foguenne, J.; Lallemend, F.; Gothot, A.; Wislet, S. Human bone marrow harbors cells with neural crest-associated characteristics like human adipose and dermis tissues. PLoS ONE 2017, 12, e0177962. [Google Scholar] [CrossRef] [PubMed]
- Brboric, A.; Vasylovska, S.; Saarimäki-Vire, J.; Espes, D.; Caballero-Corbalan, J.; Larfors, G.; Otonkoski, T.; Lau, J. Characterization of neural crest-derived stem cells isolated from human bone marrow for improvement of transplanted islet function. Ups. J. Med. Sci. 2019, 124, 228–237. [Google Scholar] [CrossRef]
- Li, W.; Huang, L.; Zeng, J.; Lin, W.; Li, K.; Sun, J.; Huang, W.; Chen, J.; Wang, G.; Ke, Q.; et al. Characterization and transplantation of enteric neural crest cells from human induced pluripotent stem cells. Mol. Psychiatry 2018, 23, 499–508. [Google Scholar] [CrossRef]
- Shea, G.K.; Tsui, A.Y.; Chan, Y.S.; Shum, D.K. Bone marrow-derived Schwann cells achieve fate commitment--a prerequisite for remyelination therapy. Exp. Neurol. 2010, 224, 448–458. [Google Scholar] [CrossRef] [PubMed]
- Mueller, J.L.; Stavely, R.; Hotta, R.; Goldstein, A.M. Peripheral nervous system: A promising source of neuronal progenitors for central nervous system repair. Front. Neurosci. 2022, 16, 970350. [Google Scholar] [CrossRef]
- Fattahi, F.; Steinbeck, J.A.; Kriks, S.; Tchieu, J.; Zimmer, B.; Kishinevsky, S.; Zeltner, N.; Mica, Y.; El-Nachef, W.; Zhao, H.; et al. Deriving human ENS lineages for cell therapy and drug discovery in Hirschsprung disease. Nature 2016, 531, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Hotta, R.; Cheng, L.S.; Graham, H.K.; Pan, W.; Nagy, N.; Belkind-Gerson, J.; Goldstein, A.M. Isogenic enteric neural progenitor cells can replace missing neurons and glia in mice with Hirschsprung disease. Neurogastroenterol. Motil. 2016, 28, 498–512. [Google Scholar] [CrossRef]
- Hotta, R.; Stamp, L.A.; Foong, J.P.; McConnell, S.N.; Bergner, A.J.; Anderson, R.B.; Enomoto, H.; Newgreen, D.F.; Obermayr, F.; Furness, J.B.; et al. Transplanted progenitors generate functional enteric neurons in the postnatal colon. J. Clin. Investig. 2013, 123, 1182–1191. [Google Scholar] [CrossRef]
- Pan, W.; Rahman, A.A.; Stavely, R.; Bhave, S.; Guyer, R.; Omer, M.; Picard, N.; Goldstein, A.M.; Hotta, R. Schwann Cells in the Aganglionic Colon of Hirschsprung Disease Can Generate Neurons for Regenerative Therapy. Stem Cells Transl. Med. 2022, 11, 1232–1244. [Google Scholar] [CrossRef]
- Hotta, R.; Cheng, L.; Graham, H.K.; Nagy, N.; Belkind-Gerson, J.; Mattheolabakis, G.; Amiji, M.M.; Goldstein, A.M. Delivery of enteric neural progenitors with 5-HT4 agonist-loaded nanoparticles and thermosensitive hydrogel enhances cell proliferation and differentiation following transplantation in vivo. Biomaterials 2016, 88, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Stavely, R.; Bhave, S.; Ho, W.L.N.; Ahmed, M.; Pan, W.; Rahman, A.A.; Ulloa, J.; Bousquet, N.; Omer, M.; Guyer, R.; et al. Enteric mesenchymal cells support the growth of postnatal enteric neural stem cells. Stem Cells 2021, 39, 1236–1252. [Google Scholar] [CrossRef] [PubMed]
- Stavely, R.; Robinson, A.M.; Miller, S.; Boyd, R.; Sakkal, S.; Nurgali, K. Human adult stem cells derived from adipose tissue and bone marrow attenuate enteric neuropathy in the guinea-pig model of acute colitis. Stem Cell Res. 2015, 6, 244. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ott, L.C.; Han, C.Y.; Mueller, J.L.; Rahman, A.A.; Hotta, R.; Goldstein, A.M.; Stavely, R. Bone Marrow Stem Cells Derived from Nerves Have Neurogenic Properties and Potential Utility for Regenerative Therapy. Int. J. Mol. Sci. 2023, 24, 5211. https://doi.org/10.3390/ijms24065211
Ott LC, Han CY, Mueller JL, Rahman AA, Hotta R, Goldstein AM, Stavely R. Bone Marrow Stem Cells Derived from Nerves Have Neurogenic Properties and Potential Utility for Regenerative Therapy. International Journal of Molecular Sciences. 2023; 24(6):5211. https://doi.org/10.3390/ijms24065211
Chicago/Turabian StyleOtt, Leah C., Christopher Y. Han, Jessica L. Mueller, Ahmed A. Rahman, Ryo Hotta, Allan M. Goldstein, and Rhian Stavely. 2023. "Bone Marrow Stem Cells Derived from Nerves Have Neurogenic Properties and Potential Utility for Regenerative Therapy" International Journal of Molecular Sciences 24, no. 6: 5211. https://doi.org/10.3390/ijms24065211
APA StyleOtt, L. C., Han, C. Y., Mueller, J. L., Rahman, A. A., Hotta, R., Goldstein, A. M., & Stavely, R. (2023). Bone Marrow Stem Cells Derived from Nerves Have Neurogenic Properties and Potential Utility for Regenerative Therapy. International Journal of Molecular Sciences, 24(6), 5211. https://doi.org/10.3390/ijms24065211




