Vitamin D and the Thyroid: A Critical Review of the Current Evidence
Abstract
1. Introduction
2. Vitamin D
3. Thyroid Function
4. Vitamin D in Thyroid Disorders
4.1. Vitamin D in Autoimmune Thyroid Diseases
4.2. Vitamin D in Thyroid Cancer
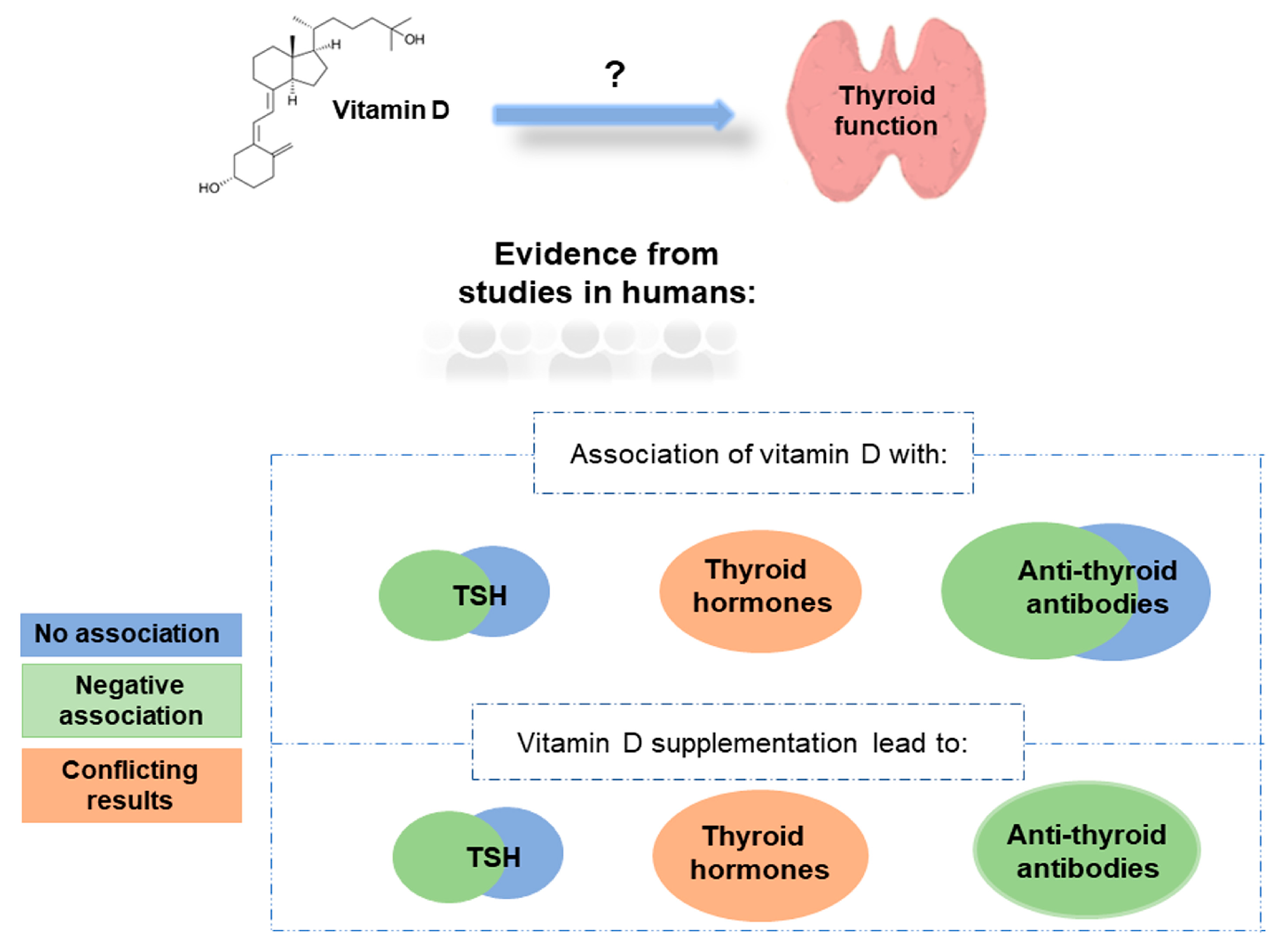
5. The Effect of Vitamin D on Secretion of TSH, Thyroid Hormones and Anti-Thyroid Antibodies
5.1. Evidence from Animal/Cell Models
5.2. Evidence from Human Studies
5.2.1. Observational Studies
5.2.2. Randomised Controlled Trials
5.2.3. Mendelian Randomization
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Grundmann, M.; von Versen-Höynck, F. Vitamin D-roles in women’s reproductive health? Reprod. Biol. Endocrinol. 2011, 9, 146. [Google Scholar] [CrossRef]
- Bikle, D.D. Vitamin D metabolism, mechanism of action, and clinical applications. Chem. Biol. 2014, 21, 319–329. [Google Scholar] [CrossRef]
- Van Driel, M.; van Leeuwen, J.P.T.M. Vitamin D endocrinology of bone mineralization. Mol. Cell. Endocrinol. 2017, 453, 46–51. [Google Scholar] [CrossRef]
- Chakraborti, C.K. Vitamin D as a promising anticancer agent. Indian J. Pharmacol. 2011, 43, 113–120. [Google Scholar] [CrossRef]
- Arnson, Y.; Amital, H.; Shoenfeld, Y. Vitamin D and autoimmunity: New aetiological and therapeutic considerations. Ann. Rheum. Dis. 2007, 66, 1137–1142. [Google Scholar] [CrossRef]
- Pike, J.W.; Meyer, M.B.; Bishop, K.A. Regulation of target gene expression by the vitamin D receptor—An update on mechanisms. Rev. Endocr. Metab. Disord. 2012, 13, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Hossein-Nezhad, A.; Spira, A.; Holick, M.F. Influence of vitamin D status and vitamin D3 supplementation on genome wide expression of white blood cells: A randomized double-blind clinical trial. PLoS ONE 2013, 8, e58725. [Google Scholar] [CrossRef] [PubMed]
- Carlberg, C. Vitamin D: A micronutrient regulating genes. Curr. Pharm. Des. 2019, 25, 1740–1746. [Google Scholar] [CrossRef] [PubMed]
- Stöcklin, E.; Eggersdorfer, M. Vitamin D, an essential nutrient with versatile functions in nearly all organs. Int. J. Vitam. Nutr. Res. 2013, 83, 92–100. [Google Scholar] [CrossRef]
- Fekete, C.; Lechan, R.M. Central regulation of hypothalamic-pituitary-thyroid axis under physiological and pathophysiological conditions. Endocr. Rev. 2014, 35, 159–194. [Google Scholar] [CrossRef]
- Dayan, C.M.; Panicker, V. Novel insights into thyroid hormones from the study of common genetic variation. Nat. Rev. Endocrinol. 2009, 5, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Bianco, A.; Kim, B. Deiodinases: Implications of the local control of thyroid hormone action. J. Clin. Invest. 2006, 116, 2571–2579. [Google Scholar] [CrossRef] [PubMed]
- Hoermann, R.; Midgley, J.E.M.; Larisch, R.; Dietrich, J.W. Relational stability in the expression of normality, variation, and control of thyroid function. Front. Endocrinol. 2016, 7, 142. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, A.; Ferrari, S.M.; Corrado, A.; Di Domenicantonio, A.; Fallahi, P. Autoimmune thyroid disorders. Autoimmun. Rev. 2015, 14, 174–180. [Google Scholar] [CrossRef]
- Misharin, A.; Hewison, M.; Chen, C.R.; Lagishetty, V.; Aliesky, H.A.; Mizutori, Y.; Rapoport, B.; McLachlan, S.M. Vitamin D deficiency modulates Graves’ hyperthyroidism induced in BALB/c mice by thyrotropin receptor immunization. Endocrinology 2009, 150, 1051–1060. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Xiong, F.; Liu, E.; Zhu, M.; Lei, P. Effects of 1,25-dihydroxyvitamin D3 in rats with experimental autoimmune thyroiditis. Nan Fang Yi Ke Da Xue Xue Bao 2010, 30, 1573–1576. [Google Scholar]
- Lopez, E.R.; Zwermann, O.; Segni, M.; Meyer, G.; Reincke, M.; Seissler, J.; Herwig, J.; Usadel, K.H.; Badenhoop, K. A promoter polymorphism of the CYP27B1 gene is associated with Addison’s disease, Hashimoto’s thyroiditis, Graves’ disease and type 1 diabetes mellitus in Germans. Eur. J. Endocrinol. 2004, 151, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Meng, S.; He, S.T.; Jiang, W.J.; Xiao, L.; Li, D.F.; Xu, J.; Shi, X.H.; Zhang, J.A. Genetic susceptibility to autoimmune thyroid diseases in a Chinese Han population: Role of vitamin D receptor gene polymorphisms. Ann. Endocrinol. 2015, 76, 684–689. [Google Scholar] [CrossRef]
- Inoue, N.; Watanabe, M.; Ishido, N.; Katsumata, Y.; Kagawa, T.; Hidaka, Y.; Iwatani, Y. The functional polymorphisms of VDR, GC and CYP2R1 are involved in the pathogenesis of autoimmune thyroid diseases. Clin. Exp. Immunol. 2014, 178, 262–269. [Google Scholar] [CrossRef]
- Štefanić, M.; Tokić, S. Serum 25-hydoxyvitamin D concentrations in relation to Hashimoto’s thyroiditis: A systematic review, meta-analysis and meta-regression of observational studies. Eur. J. Nutr. 2020, 59, 859–872. [Google Scholar] [CrossRef]
- Xu, M.Y.; Cao, B.; Yin, J.; Wang, D.F.; Chen, K.L.; Lu, Q. Bin Vitamin D and Graves’ disease: A meta-analysis update. Nutrients 2015, 7, 3813–3827. [Google Scholar] [CrossRef] [PubMed]
- Taheriniya, S.; Arab, A.; Hadi, A.; Fadel, A.; Askari, G. Vitamin D and thyroid disorders: A systematic review and meta-analysis of observational studies. BMC Endocr. Disord. 2021, 21, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Chen, W.; Li, D.; Yin, X.; Zhang, X.; Olsen, N.; Zheng, S.G. Vitamin D and chronic diseases. Aging Dis. 2017, 8, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Pu, R.; Li, N.; Chen, C.; Li, J.; Dai, W.; Wang, Y.; Hu, J.; Zhu, D.; Yu, Q.; et al. High prevalence of vitamin D deficiency in Asia: A systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. 2021, 16, 1–10. [Google Scholar] [CrossRef]
- Bizzaro, G.; Shoenfeld, Y. Vitamin D and thyroid autoimmune diseases: The known and the obscure. Immunol. Res. 2015, 61, 107–109. [Google Scholar] [CrossRef]
- Bui, L.; Zhu, Z.; Hawkins, S.; Cortez-Resendiz, A.; Bellon, A. Vitamin D regulation of the immune system and its implications for COVID-19: A mini review. SAGE Open Med. 2021, 9, 1–8. [Google Scholar] [CrossRef]
- Chun, R.F.; Liu, P.T.; Modlin, R.L.; Adams, J.S.; Hewison, M. Impact of vitamin D on immune function: Lessons learned from genome-wide analysis. Front. Physiol. 2014, 5, 151. [Google Scholar] [CrossRef]
- Nettore, I.C.; Albano, L.; Ungaro, P.; Colao, A.; Macchia, P.E. Sunshine vitamin and thyroid. Rev. Endocr. Metab. Disord. 2017, 18, 347–354. [Google Scholar] [CrossRef]
- Deng, Y.J.; Li, H.T.; Wang, M.; Li, N.; Tian, T.; Wu, Y.; Xu, P.; Yang, S.; Zhai, Z.; Zhou, L.H.; et al. Global burden of thyroid cancer from 1990 to 2017. JAMA Netw. Open 2020, 3, e208759. [Google Scholar] [CrossRef]
- Cabanillas, M.E.; McFadden, D.G.; Durante, C. Thyroid cancer. Lancet 2016, 388, 2783–2795. [Google Scholar] [CrossRef]
- Fagin, J.A.; Wells, S.A. Biologic and clinical perspectives on thyroid cancer. N. Engl. J. Med. 2016, 375, 1054–1067. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Wang, K.; Zheng, R.; Derwahl, M. 1,25 dihydroxyvitamin D3 inhibits the proliferation of thyroid cancer stem-like cells via cell cycle arrest. Endocr. Res. 2016, 41, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Chiang, K.C.; Kuo, S.F.; Chen, C.H.; Ng, S.; Lin, S.F.; Yeh, C.N.; Chen, L.W.; Takano, M.; Chen, T.C.; Juang, H.H.; et al. MART-10, the vitamin D analog, is a potent drug to inhibit anaplastic thyroid cancer cell metastatic potential. Cancer Lett. 2015, 369, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Khadzkou, K.; Buchwald, P.; Westin, G.; Dralle, H.; Åkerström, G.; Hellman, P. 25-hydroxyvitamin D3 1alpha-hydroxylase and vitamin D receptor expression in papillary thyroid carcinoma. J. Histochem. Cytochem. 2006, 54, 355–361. [Google Scholar] [CrossRef]
- Clinckspoor, I.; Hauben, E.; Verlinden, L.; van den Bruel, A.; Vanwalleghem, L.; Vander Poorten, V.; Delaere, P.; Mathieu, C.; Verstuyf, A.; Decallonne, B. Altered expression of key players in vitamin D metabolism and signaling in malignant and benign thyroid tumors. J. Histochem. Cytochem. 2012, 60, 502–511. [Google Scholar] [CrossRef] [PubMed]
- Izkhakov, E.; Somjen, D.; Sharon, O.; Knoll, E.; Aizic, A.; Fliss, D.M.; Limor, R.; Stern, N. Vitamin D receptor expression is linked to potential markers of human thyroid papillary carcinoma. J. Steroid Biochem. Mol. Biol. 2016, 159, 26–30. [Google Scholar] [CrossRef]
- Liu, W.; Asa, S.L.; Ezzat, S. 1alpha,25-Dihydroxyvitamin D3 targets PTEN-dependent fibronectin expression to restore thyroid cancer cell adhesiveness. Mol. Endocrinol. 2005, 19, 2349–2357. [Google Scholar] [CrossRef]
- Dackiw, A.P.B.; Ezzat, S.; Huang, P.; Liu, W.; Asa, S.L. Vitamin D3 administration induces nuclear p27 accumulation, restores differentiation, and reduces tumor burden in a mouse model of metastatic follicular thyroid cancer. Endocrinology 2004, 145, 5840–5846. [Google Scholar] [CrossRef]
- Chandler, P.D.; Chen, W.Y.; Ajala, O.N.; Hazra, A.; Cook, N.; Bubes, V.; Lee, I.M.; Giovannucci, E.L.; Willett, W.; Buring, J.E.; et al. Effect of vitamin D3 supplements on development of advanced cancer: A secondary analysis of the VITAL randomized clinical trial. JAMA Netw. Open 2020, 3, e2025850. [Google Scholar] [CrossRef]
- Zhao, J.; Wang, H.; Zhang, Z.; Zhou, X.; Yao, J.; Zhang, R.; Liao, L.; Dong, J. Vitamin D deficiency as a risk factor for thyroid cancer: A meta-analysis of case-control studies. Nutrition 2019, 57, 5–11. [Google Scholar] [CrossRef]
- Danilovic, D.L.S.; Ferraz-de-Souza, B.; Fabri, A.W.; Santana, N.O.; Kulcsar, M.A.; Cernea, C.R.; Marui, S.; Hoff, A.O. 25-Hydroxyvitamin D and TSH as risk factors or prognostic markers in thyroid carcinoma. PLoS ONE 2016, 11, e0164550. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.M.; Kim, W.G.; Kim, T.Y.; Bae, S.J.; Kim, H.K.; Jang, E.K.; Jeon, M.J.; Han, J.M.; Shong, Y.K.; Kim, W.B. Serum vitamin D3 levels are not associated with thyroid cancer prevalence in euthyroid subjects without autoimmune thyroid disease. Korean J. Intern. Med. 2017, 32, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Vassalle, C.; Parlanti, A.; Pingitore, A.; Berti, S.; Iervasi, G.; Sabatino, L. Vitamin D, thyroid hormones and cardiovascular risk: Exploring the components of this novel disease triangle. Front. Physiol. 2021, 12, 722912. [Google Scholar] [CrossRef] [PubMed]
- Alrefaie, Z.; Awad, H. Effect of vitamin D3 on thyroid function and de-iodinase 2 expression in diabetic rats. Arch. Physiol. Biochem. 2015, 121, 206–209. [Google Scholar] [CrossRef]
- Clinckspoor, I.; Verlinden, L.; Mathieu, C.; Bouillon, R.; Verstuyf, A.; Decallonne, B. Vitamin D in thyroid tumorigenesis and development. Prog. Histochem. Cytochem. 2013, 48, 65–98. [Google Scholar] [CrossRef]
- Berg, J.P.; Liane, K.M.; Bjørhovde, S.B.; Bjøro, T.; Torjesen, P.A.; Haug, E. Vitamin D receptor binding and biological effects of cholecalciferol analogues in rat thyroid cells. J. Steroid Biochem. Mol. Biol. 1994, 50, 145–150. [Google Scholar] [CrossRef]
- Lamberg-Allardt, C.; Valtonen, E.; Polojärvi, M.; Stewen, P. Characterization of a 1,25-dihydroxy-vitamin D3 receptor in FRTL-5 cells. Evidence for an inhibitory effect of 1,25-dihydroxy-vitamin D3 on thyrotropin-induced iodide uptake. Mol. Cell. Endocrinol. 1991, 81, 25–31. [Google Scholar] [CrossRef]
- D’Emden, M.C.; Wark, J.D. 1,25-Dihydroxyvitamin D3 enhances thyrotropin releasing hormone induced thyrotropin secretion in normal pituitary cells. Endocrinology 1987, 121, 1192–1194. [Google Scholar] [CrossRef]
- Barchetta, I.; Baroni, M.G.; Leonetti, F.; De Bernardinis, M.; Bertoccini, L.; Fontana, M.; Mazzei, E.; Fraioli, A.; Cavallo, M.G. TSH levels are associated with vitamin D status and seasonality in an adult population of euthyroid adults. Clin. Exp. Med. 2015, 15, 389–396. [Google Scholar] [CrossRef]
- Chailurkit, L.O.; Aekplakorn, W.; Ongphiphadhanakul, B. High vitamin D status in younger individuals is associated with low circulating thyrotropin. Thyroid 2013, 23, 25–30. [Google Scholar] [CrossRef]
- Muscogiuri, G.; Mari, D.; Prolo, S.; Fatti, L.M.; Cantone, M.C.; Garagnani, P.; Arosio, B.; Di Somma, C.; Vitale, G. 25 hydroxyvitamin D deficiency and its relationship to autoimmune thyroid disease in the elderly. Int. J. Environ. Res. Public Health 2016, 13, 850. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Song, E.; Oh, H.S.; Park, S.; Kwon, H.; Jeon, M.J.; Kim, W.G.; Kim, W.B.; Shong, Y.K.; Kim, T.Y. Vitamin D deficiency affects thyroid autoimmunity and dysfunction in iodine-replete area: Korea national health and nutrition examination survey. Endocrine 2017, 58, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Verrusio, W.; Magro, V.M.; Renzi, A.; Casciaro, B.; Andreozzi, P.; Cacciafesta, M. Thyroid hormones, metabolic syndrome and Vitamin D in middle-aged and older euthyroid subjects: A preliminary study. Aging Clin. Exp. Res. 2019, 31, 1337–1341. [Google Scholar] [CrossRef] [PubMed]
- Mansorian, B.; Attari, M.M.A.; Vahabzadeh, D.; Mohebbi, I. Serum vitamin D level and its relation to thyroid hormone, blood sugar and lipid profiles in iranian sedentary work staff. Nutr. Hosp. 2018, 35, 1107–1114. [Google Scholar] [CrossRef]
- Zhang, Q.; Wang, Z.; Sun, M.; Cao, M.; Zhu, Z.; Fu, Q.; Gao, Y.; Mao, J.; Li, Y.; Shi, Y.; et al. Association of high vitamin D status with low circulating thyroid-stimulating hormone independent of thyroid hormone levels in middle-aged and elderly males. Int. J. Endocrinol. 2014, 2014, 631819. [Google Scholar] [CrossRef] [PubMed]
- Fang, F.; Chai, Y.; Wei, H.; Wang, K.; Tan, L.; Zhang, W.; Fan, Y.; Li, F.; Shan, Z.; Zhu, M. Vitamin D deficiency is associated with thyroid autoimmunity: Results from an epidemiological survey in Tianjin, China. Endocrine 2021, 73, 447–454. [Google Scholar] [CrossRef]
- Goswami, R.; Marwaha, R.K.; Gupta, N.; Tandon, N.; Sreenivas, V.; Tomar, N.; Ray, D.; Kanwar, R.; Agarwal, R. Prevalence of vitamin D deficiency and its relationship with thyroid autoimmunity in Asian Indians: A community-based survey. Br. J. Nutr. 2009, 102, 382–386. [Google Scholar] [CrossRef]
- Sayki Arslan, M.; Topaloglu, O.; Ucan, B.; Karakose, M.; Karbek, B.; Tutal, E.; Caliskan, M.; Ginis, Z.; Cakal, E.; Sahin, M.; et al. Isolated vitamin D deficiency is not associated with nonthyroidal illness syndrome, but with thyroid autoimmunity. Sci. World J. 2015, 2015, 239815. [Google Scholar] [CrossRef]
- Zhou, P.; Cai, J.; Markowitz, M. Absence of a relationship between thyroid hormones and vitamin D levels. J. Pediatr. Endocrinol. Metab. 2016, 29, 703–707. [Google Scholar] [CrossRef]
- Guo, Y.; Wu, C.Y.; Deng, Y.H.; Wu, J.L. Associations between serum 25-hydroxyvitamin D levels and thyroid function parameters in previously healthy children aged 6 to 24 months. Risk Manag. Healthc. Policy 2020, 13, 1647–1653. [Google Scholar] [CrossRef]
- Zaidman, V.; Maceiras, M.; Lazzati, J.; Kutasz, E.; D’Isa, G.; Chilleli, C.; Tau, C.; Viterbo, G.; Rivarola, M.A.; Belgorosky, A.; et al. High prevalence of anti-thyroid antibodies associated with a low vitamin D status in a pediatric cohort. Clin. Chem. Lab. Med. 2014, 52, e119-22. [Google Scholar] [CrossRef] [PubMed]
- De Pergola, G.; Triggiani, V.; Bartolomeo, N.; Giagulli, V.A.; Anelli, M.; Masiello, M.; Candita, V.; De Bellis, D.; Silvestris, F. Low 25 hydroxyvitamin D levels are independently associated with autoimmune thyroiditis in a cohort of apparently healthy overweight and obese subjects. Endocr. Metab. Immune Disord. Drug Targets 2018, 18, 646–652. [Google Scholar] [CrossRef]
- Wang, X.; Liu, H.; Chen, J.; Huang, Y.; Li, L.; Rampersad, S.; Qu, S. Metabolic characteristics in obese patients complicated by mild thyroid hormone deficiency. Horm. Metab. Res. 2016, 48, 331–337. [Google Scholar] [CrossRef]
- Chao, G.; Zhu, Y.; Fang, L. Correlation between Hashimoto’s thyroiditis-related thyroid hormone levels and 25-hydroxyvitamin D. Front. Endocrinol. 2020, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Cvek, M.; Kaličanin, D.; Barić, A.; Vuletić, M.; Gunjača, I.; Torlak Lovrić, V.; Škrabić, V.; Punda, A.; Boraska Perica, V. Vitamin D and Hashimoto’s thyroiditis: Observations from CROHT biobank. Nutrients 2021, 13, 2793. [Google Scholar] [CrossRef] [PubMed]
- Yasmeh, J.; Farpour, F.; Rizzo, V.; Kheradnam, S.; Sachmechi, I. Hashimoto thyroiditis not associated with vitamin D deficiency. Endocr. Pract. 2016, 22, 809–813. [Google Scholar] [CrossRef]
- Krysiak, R.; Szkróbka, W.; Okopień, B. The relationship between statin action on thyroid autoimmunity and vitamin D status: A pilot study. Exp. Clin. Endocrinol. Diabetes 2019, 127, 23–28. [Google Scholar] [CrossRef]
- Camurdan, O.; Doger, E.; Bideci, A.; Celik, N.; Cinaz, P. Vitamin D status in children with Hashimoto thyroiditis. J. Pediatr. Endocrinol. Metab. 2012, 25, 467–470. [Google Scholar] [CrossRef]
- Hanna, H.W.Z.; Rizzo, C.; Abdel Halim, R.M.; El Haddad, H.E.; Salam, R.; El-Sayed Abou-Youssef, H. Vitamin D status in Hashimoto’s thyroiditis and its association with vitamin D receptor genetic variants. J. Steroid Biochem. Mol. Biol. 2021, 212, 105922. [Google Scholar] [CrossRef]
- Stoica, R.A.; Guja, C.; Pantea-Stoian, A.; van Staden, R.I.S.; Popa-Tudor, I.; Ștefan, S.D.; Ancuceanu, R.; Serafinceanu, C.; Tîrgoviște, C.I. No association between 25-hydroxyvitamin D and insulin resistance or thyroid hormone concentrations in a Romanian observational study. Medicina 2020, 57, 25. [Google Scholar] [CrossRef]
- Koehler, V.F.; Filmann, N.; Mann, W.A. Vitamin D status and thyroid autoantibodies in autoimmune thyroiditis. Horm. Metab. Res. 2019, 51, 792–797. [Google Scholar] [CrossRef] [PubMed]
- Krysiak, R.; Szkróbka, W.; Okopień, B. The effect of gluten-free diet on thyroid autoimmunity in drug-naïve women with Hashimoto’s thyroiditis: A pilot study. Exp. Clin. Endocrinol. Diabetes 2019, 127, 417–422. [Google Scholar] [CrossRef]
- Krysiak, R.; Kowalcze, K.; Okopień, B. The impact of combination therapy with metformin and exogenous vitamin D on hypothalamic-pituitary-thyroid axis activity in women with autoimmune thyroiditis and high-normal thyrotropin levels. J. Clin. Pharm. Ther. 2020, 45, 1382–1389. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.Y.; Lee, Y.J.; Choi, J.H.; Lee, S.Y.; Lee, H.Y.; Jeong, D.H.; Choi, Y.J. The association between low vitamin D status and autoimmune thyroid disease in Korean premenopausal women: The 6th Korea national health and nutrition examination survey, 2013–2014. Korean J. Fam. Med. 2019, 40, 323–328. [Google Scholar] [CrossRef]
- Botelho, I.M.B.; Neto, A.M.; Silva, C.A.; Tambascia, M.A.; Alegre, S.M.; Zantut-Wittmann, D.E. Vitamin D in Hashimoto’s thyroiditis and its relationship with thyroid function and inflammatory status. Endocr. J. 2018, 65, 1029–1037. [Google Scholar] [CrossRef]
- Giovinazzo, S.; Vicchio, T.M.; Certo, R.; Alibrandi, A.; Palmieri, O.; Campennì, A.; Cannavò, S.; Trimarchi, F.; Ruggeri, R.M. Vitamin D receptor gene polymorphisms/haplotypes and serum 25(OH)D3 levels in Hashimoto’s thyroiditis. Endocrine 2017, 55, 599–606. [Google Scholar] [CrossRef]
- MacFarlane, I.A.; Mawer, E.B.; Berry, J.; Hann, J. Vitamin D metabolism in hyperthyroidism. Clin. Endocrinol. 1982, 17, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Ke, W.; Sun, T.; Zhang, Y.; He, L.; Wu, Q.; Liu, J.; Zha, B. 25-Hydroxyvitamin D serum level in Hashimoto’s thyroiditis, but not Graves’ disease is relatively deficient. Endocr. J. 2017, 64, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Kim, D. Low vitamin D status is associated with hypothyroid Hashimoto’s thyroiditis. Hormones 2016, 15, 385–393. [Google Scholar] [CrossRef]
- Kmieć, P.; Minkiewicz, I.; Rola, R.; Sworczak, K.; Zmijewski, M.A.; Kowalski, K. Vitamin D status including 3-epi-25(OH)D3 among adult patients with thyroid disorders during summer months. Endokrynol. Pol. 2018, 69, 653–660. [Google Scholar] [CrossRef]
- Mansournia, N.; Mansournia, M.A.; Saeedi, S.; Dehghan, J. The association between serum 25OHD levels and hypothyroid Hashimoto’s thyroiditis. J. Endocrinol. Invest. 2014, 37, 473–476. [Google Scholar] [CrossRef] [PubMed]
- Sönmezgöz, E.; Ozer, S.; Yilmaz, R.; Önder, Y.; Bütün, I.; Bilge, S. Hypovitaminosis D in children with Hashimoto’s thyroiditis. Rev. Med. Chil. 2016, 144, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Zhu, X.Y.; Sun, H.; Xu, X.Q.; Xu, S.A.; Suo, Y.; Cao, L.J.; Zhou, Q.; Yu, H.J.; Cao, W.Z. Low vitamin D levels are associated with cognitive impairment in patients with Hashimoto thyroiditis. BMC Endocr. Disord. 2018, 18, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Evliyaoğlu, O.; Acar, M.; Özcabı, B.; Erginöz, E.; Bucak, F.; Ercan, O.; Kucur, M. Vitamin D deficiency and Hashimoto’s thyroiditis in children and adolescents: A critical vitamin D level for this association? J. Clin. Res. Pediatr. Endocrinol. 2015, 7, 128–133. [Google Scholar] [CrossRef]
- Ma, J.; Wu, D.; Li, C.; Fan, C.; Chao, N.; Liu, J.; Li, Y.; Wang, R.; Miao, W.; Guan, H.; et al. Lower serum 25-hydroxyvitamin D level is associated with 3 types of autoimmune thyroid diseases. Medicine 2015, 94, e1639. [Google Scholar] [CrossRef]
- Shin, D.Y.; Kim, K.J.; Kim, D.; Hwang, S.; Lee, E.J. Low serum vitamin D is associated with anti-thyroid peroxidase antibody in autoimmune thyroiditis. Yonsei Med. J. 2014, 55, 476–481. [Google Scholar] [CrossRef]
- Tau, C.; Garabedian, M.; Farriaux, J.P.; Czemichow, P.; Pomarede, R.; Balsan, S. Hypercalcemia in infants with congenital hypothyroidism and its relation to vitamin D and thyroid hormones. J. Pediatr. 1986, 109, 808–814. [Google Scholar] [CrossRef]
- Zhou, Y.; Wang, X.; Xin, M.; Zhuang, H. Changes in bone mineral density, 25-hydroxyvitamin D3 and inflammatory factors in patients with hyperthyroidism. Exp. Ther. Med. 2021, 21, 617. [Google Scholar] [CrossRef]
- Ahn, H.Y.; Chung, Y.J.; Cho, B.Y. Serum 25-hydroxyvitamin D might be an independent prognostic factor for Graves disease recurrence. Medicine 2017, 96, e7700. [Google Scholar] [CrossRef]
- Li, X.; Wang, G.; Lu, Z.; Chen, M.; Tan, J.; Fang, X. Serum 25-hydroxyvitamin D predict prognosis in radioiodine therapy of Graves’ disease. J. Endocrinol. Invest. 2015, 38, 753–759. [Google Scholar] [CrossRef]
- Zhang, H.; Liang, L.; Xie, Z. Low vitamin D status is associated with increased thyrotropin-receptor antibody titer in Graves disease. Endocr. Pract. 2015, 21, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Liu, Y.; Zhao, C.; Fang, J.; Wang, X.; Wei, L. Changes of serum 25(OH) D3 and IGF-1 levels in patients with thyroid nodules. BMC Endocr. Disord. 2019, 19, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Abuduwaili, M.; Xing, Z.; Xia, B.; Fei, Y.; Zhu, J.; Su, A. Correlation between pre-operative 25-hydroxyvitamin D levels and poor prognostic factors for papillary thyroid cancer. J. Investig. Surg. 2022, 35, 1076–1082. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.R.; Kim, B.H.; Kim, S.M.; Oh, M.Y.; Kim, W.J.; Jeon, Y.K.; Kim, S.S.; Lee, B.J.; Kim, Y.K.; Kim, I.J. Low serum 25 hydroxyvitamin D is associated with poor clinicopathologic characteristics in female patients with papillary thyroid cancer. Thyroid 2014, 24, 1618–1624. [Google Scholar] [CrossRef] [PubMed]
- Ahn, H.Y.; Chung, Y.J.; Park, K.Y.; Cho, B.Y. Serum 25-hydroxyvitamin D level does not affect the aggressiveness and prognosis of papillary thyroid cancer. Thyroid 2016, 26, 429–433. [Google Scholar] [CrossRef]
- Kuang, J.; Jin, Z.; Chen, L.; Zhao, Q.; Huang, H.; Liu, Z.; Yang, W.; Feng, H.; Yang, Z.; Díez, J.J.; et al. Serum 25-hydroxyvitamin D level is unreliable as a risk factor and prognostic marker in papillary thyroid cancer. Ann. Transl. Med. 2022, 10, 193. [Google Scholar] [CrossRef]
- Zhuo, Y.; Ling, L.; Sun, Z.; Huang, W.; Hong, Z.; Zhang, Y.; Peng, X.; Liu, X.; Yuan, W.; Xu, W.Y.; et al. Vitamin D and iodine status was associated with the risk and complication of type 2 diabetes mellitus in China. Open Life Sci. 2021, 16, 150–159. [Google Scholar] [CrossRef]
- Luciardi, M.C.; Alemán, M.N.; Martinez, D.; Maxzud, M.C.; Soria, A.; Aldonati, M.E.; Luciardi, H.L. Vitamin D levels in a population from Argentina with metabolic disorders. Porto Biomed. J. 2022, 7, e159. [Google Scholar] [CrossRef]
- Krysiak, R.; Kowalska, B.; Okopien, B. Serum 25-hydroxyvitamin D and parathyroid hormone levels in non-lactating women with post-partum thyroiditis: The effect of L-thyroxine treatment. Basic Clin. Pharmacol. Toxicol. 2015, 116, 503–507. [Google Scholar] [CrossRef]
- Bozdag, H.; Akdeniz, E. Does severe vitamin D deficiency impact obstetric outcomes in pregnant women with thyroid autoimmunity? J. Matern. Neonatal Med. 2020, 33, 1359–1369. [Google Scholar] [CrossRef]
- Musa, I.R.; Rayis, D.A.; Ahmed, M.A.; Khamis, A.H.; Nasr, A.M.; Adam, I. Thyroid function and 25 (OH) vitamin D level among Sudanese women in early pregnancy. Open Access Maced. J. Med. Sci. 2018, 6, 488–492. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Miao, W.; Li, C.; Yu, X.; Shan, Z.; Guan, H.; Teng, W. Dynamic changes in serum 25-hydroxyvitamin D during pregnancy and lack of effect on thyroid parameters. PLoS ONE 2014, 9, e90161. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Zhong, S.; Liu, Q.; Wang, C.-B.; Zhu, W.-H.; Shen, X.-A.; Lu, B.; Shen, L.-W.; Zeng, Y. Investigating the relationship between 25-hydroxyvitamin D and thyroid function in second-trimester pregnant women. Gynecol. Endocrinol. 2018, 34, 345–348. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Li, Z.; Li, B.; Guo, S.; Yao, M. Expression and clinical significance of serum 25-OH-D in pregnant women with SCH (Subclinical Hypothyroidism) and GDM (Gestational Diabetes Mellitus). Pakistan J. Med. Sci. 2018, 34, 1278–1282. [Google Scholar] [CrossRef] [PubMed]
- Muscogiuri, G.; Palomba, S.; Caggiano, M.; Tafuri, D.; Colao, A.; Orio, F. Low 25 (OH) vitamin D levels are associated with autoimmune thyroid disease in polycystic ovary syndrome. Endocrine 2016, 53, 538–542. [Google Scholar] [CrossRef]
- Cashman, K.D.; Dowling, K.G.; Škrabáková, Z.; Gonzalez-Gross, M.; Valtueña, J.; De Henauw, S.; Moreno, L.; Damsgaard, C.T.; Michaelsen, K.F.; Mølgaard, C.; et al. Vitamin D deficiency in Europe: Pandemic? Am. J. Clin. Nutr. 2016, 103, 1033–1044. [Google Scholar] [CrossRef]
- Amrein, K.; Scherkl, M.; Hoffmann, M.; Neuwersch-Sommeregger, S.; Köstenberger, M.; Tmava Berisha, A.; Martucci, G.; Pilz, S.; Malle, O. Vitamin D deficiency 2.0: An update on the current status worldwide. Eur. J. Clin. Nutr. 2020, 74, 1498–1513. [Google Scholar] [CrossRef]
- Meltzer, D.O.; Best, T.J.; Zhang, H.; Vokes, T.; Arora, V.M.; Solway, J. Association of vitamin D levels, race/ethnicity, and clinical characteristics with COVID-19 test results. JAMA Netw. Open 2021, 4, e214117. [Google Scholar] [CrossRef]
- Christodoulou, S.; Goula, T.; Ververidis, A.; Drosos, G. Vitamin D and Bone Disease. BioMed Res. Int. 2013, 2013, 396541. [Google Scholar] [CrossRef]
- Munshi, R.; Hussein, M.H.; Toraih, E.A.; Elshazli, R.M.; Jardak, C.; Sultana, N.; Youssef, M.R.; Omar, M.; Attia, A.S.; Fawzy, M.S.; et al. Vitamin D insufficiency as a potential culprit in critical COVID-19 patients. J. Med. Virol. 2021, 93, 733–740. [Google Scholar] [CrossRef]
- Mirhosseini, N.; Brunel, L.; Muscogiuri, G.; Kimball, S. Physiological serum 25-hydroxyvitamin D concentrations are associated with improved thyroid function-observations from a community-based program. Endocrine 2017, 58, 563–573. [Google Scholar] [CrossRef]
- Talaei, A.; Ghorbani, F.; Asemi, Z. The effects of Vitamin D supplementation on thyroid function in hypothyroid patients: A randomized, double-blind, placebo-controlled trial. Indian J. Endocrinol. Metab. 2018, 22, 584–588. [Google Scholar] [CrossRef]
- Villa, A.; Corsello, A.; Cintoni, M.; Papi, G.; Pontecorvi, A.; Corsello, S.M.; Paragliola, R.M. Effect of vitamin D supplementation on TSH levels in euthyroid subjects with autoimmune thyroiditis. Endocrine 2020, 70, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Chen, X.; Qian, X.; Shao, S. Effects of vitamin D treatment on thyroid function and autoimmunity markers in patients with Hashimoto’s thyroiditis—A meta-analysis of randomized controlled trials. J. Clin. Pharm. Ther. 2022, 47, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, S.; Dutta, D.; Kumar, M.; Saha, S.; Mondal, S.; Kumar, A.; Mukhopadhyay, S. Vitamin D supplementation reduces thyroid peroxidase antibody levels in patients with autoimmune thyroid disease: An open-labeled randomized controlled trial. Indian J. Endocrinol. Metab. 2016, 20, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Nodehi, M.; Ajami, A.; Izad, M.; Asgarian Omran, H.; Chahardoli, R.; Amouzegar, A.; Yekaninejad, S.; Hemmatabadi, M.; Azizi, F.; Esfahanian, F.; et al. Effects of vitamin D supplements on frequency of CD4+ T-cell subsets in women with Hashimoto’s thyroiditis: A double-blind placebo-controlled study. Eur. J. Clin. Nutr. 2019, 73, 1236–1243. [Google Scholar] [CrossRef] [PubMed]
- Krysiak, R.; Kowalcze, K.; Okopień, B. Hyperprolactinaemia attenuates the inhibitory effect of vitamin D/selenomethionine combination therapy on thyroid autoimmunity in euthyroid women with Hashimoto’s thyroiditis: A pilot study. J. Clin. Pharm. Ther. 2020, 45, 1334–1341. [Google Scholar] [CrossRef]
- Krysiak, R.; Szkróbka, W.; Okopień, B. Dehydroepiandrosterone potentiates the effect of vitamin D on thyroid autoimmunity in euthyroid women with autoimmune thyroiditis: A pilot study. Clin. Exp. Pharmacol. Physiol. 2021, 48, 195–202. [Google Scholar] [CrossRef]
- Krysiak, R.; Kowalcze, K.; Okopień, B. Gluten-free diet attenuates the impact of exogenous vitamin D on thyroid autoimmunity in young women with autoimmune thyroiditis: A pilot study. Scand. J. Clin. Lab. Invest. 2022, 82, 518–524. [Google Scholar] [CrossRef]
- Vahabi Anaraki, P.; Aminorroaya, A.; Amini, M.; Momeni, F.; Feizi, A.; Iraj, B.; Tabatabaei, A. Effect of vitamin D deficiency treatment on thyroid function and autoimmunity markers in Hashimoto’s thyroiditis: A double-blind randomized placebo-controlled clinical trial. J. Res. Med. Sci. 2017, 22, 103. [Google Scholar] [CrossRef]
- Barsony, J.; Lakatos, P.; Foldes, J.; Feher, T. Effect of vitamin D3 loading and thyroid hormone replacement therapy on the decreased serum 25-hydroxyvitamin D level in patients with hypothyroidism. Acta Endocrinol 1986, 113, 329–334. [Google Scholar] [CrossRef]
- Krysiak, R.; Kowalcze, K.; Okopien, B. The effect of vitamin D on thyroid autoimmunity in non-lactating women with postpartum thyroiditis. Eur. J. Clin. Nutr. 2016, 70, 637–639. [Google Scholar] [CrossRef]
- Krysiak, R.; Szkróbka, W.; Okopień, B. Moderate-dose simvastatin therapy potentiates the effect of vitamin D on thyroid autoimmunity in levothyroxine-treated women with Hashimoto’s thyroiditis and vitamin D insufficiency. Pharmacol. Rep. 2018, 70, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Krysiak, R.; Szkróbka, W.; Okopień, B. The effect of vitamin D on thyroid autoimmunity in levothyroxine-treated women with Hashimoto’s thyroiditis and normal vitamin D status. Exp. Clin. Endocrinol. Diabetes 2017, 125, 229–233. [Google Scholar] [CrossRef]
- Krysiak, R.; Szkróbka, W.; Okopień, B. The effect of vitamin D and selenomethionine on thyroid antibody titers, hypothalamic-pituitary-thyroid axis activity and thyroid function tests in men with Hashimoto’s thyroiditis: A pilot study. Pharmacol. Rep. 2019, 71, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Krysiak, R.; Kowalcze, K.; Okopień, B. The effect of vitamin D on thyroid autoimmunity in euthyroid men with autoimmune thyroiditis and testosterone deficiency. Pharmacol. Rep. 2019, 71, 798–803. [Google Scholar] [CrossRef]
- Chahardoli, R.; Saboor-Yaraghi, A.A.; Amouzegar, A.; Khalili, D.; Vakili, A.Z.; Azizi, F. Can supplementation with vitamin D modify thyroid autoantibodies (Anti-TPO Ab, Anti-Tg Ab) and thyroid profile (T3, T4, TSH) in Hashimoto’s thyroiditis? A double blind, randomized clinical trial. Horm. Metab. Res. 2019, 51, 296–301. [Google Scholar] [CrossRef]
- Ye, Y.; Yang, H.; Wang, Y.; Zhao, H. A comprehensive genetic and epidemiological association analysis of vitamin D with common diseases/traits in the UK Biobank. Genet. Epidemiol. 2020, 45, 24–35. [Google Scholar] [CrossRef]
- Chen, Y.; Han, B.; Zhu, C.; Li, Q.; Chen, C.; Zhai, H.; Wang, N.; Chen, Y.; Lu, Y. Bidirectional mendelian randomization analysis for vitamin D and thyroid peroxidase antibody. Int. J. Endocrinology. 2022, 2022, 2260388. [Google Scholar] [CrossRef]
- Snellman, G.; Melhus, H.; Gedeborg, R.; Byberg, L.; Berglund, L.; Wernroth, L.; Michaëlsson, K. Determining vitamin D status: A comparison between commercially available assays. PLoS ONE 2010, 5, e11555. [Google Scholar] [CrossRef]
- Wortsman, J.; Matsuoka, L.Y.; Chen, T.C.; Lu, Z.; Holick, M.F. Decreased bioavailability of vitamin D in obesity. Am. J. Clin. Nutr. 2000, 72, 690–693. [Google Scholar] [CrossRef] [PubMed]
- Diffey, B.L. Modelling the seasonal variation of vitamin D due to sun exposure. Br. J. Dermatol. 2010, 162, 1342–1348. [Google Scholar] [CrossRef] [PubMed]
- Datta, S.; Pal, M.; De, A. The dependency of vitamin D status on anthropometric data. Malaysian J. Med. Sci. 2014, 21, 54. [Google Scholar]
| Reference | Correlation of 25(OH)D with TSH, Thyroid Hormones and Thyroglobulin | Correlation of 25(OH)D with Anti-Thyroid Antibodies | Number of Participants | Diagnosis of Participants |
|---|---|---|---|---|
| [56] | ↔Thyroid function (levels of TSH, fT4, fT3) | ↓iTgAb, ↓iTPOAb (i-isolated) | 1812 | Healthy controls |
| [57] | ↓TPOAb | 642 | Healthy controls | |
| [52] | ↔TSH, ↔fT4 | ↓TPOAb | 4181 | Healthy controls |
| [54] | ↔TSH, ↓fT3, ↓fT4 | 300 | Healthy controls | |
| [55] | ↓TSH, ↔fT4, ↔fT3 | ↓TPOAb, ↓TgAb | 1424 | Adults (41–78 years) |
| [58] | ↑TSH, ↔fT4, ↔fT3 | ↓TPOAb, ↔TgAb | 155 | Healthy controls |
| [51] | ↔TSH, ↔fT4, ↑fT3 | ↓TPOAb, ↔TgAb | 168 | Elderly participants (65 years and older) |
| [59] | ↔TSH, ↔fT4 | ↔TPOAb, ↔TgAb | 2006 | Healthy controls |
| [49] | ↓TSH (also measured fT4 and fT3, but did not compare with 25(OH)D) | 294 | Healthy controls | |
| [50] | ↓TSH (only in younger participants) | ↔TPOAb, ↔TgAb | 2582 | Healthy controls |
| [53] | ↔TSH, ↑fT4, ↔fT3 | 123 | Healthy controls | |
| [60] | ↔TSH, ↔fT4, ↔fT3 | 2869 | Children (6–24 months of age) | |
| [61] | ↓TSH, ↑T3, ↑T4, ↑fT4 | ↓anti-thyroid antibodies (TPOAb, TgAb) | 153 | Pediatric cohort with balanced bone metabolism |
| [62] | ↓TSH, ↔fT4, ↔fT3 | (also measured TPOAb and TgAb, but did not compare with 25(OH)D) | 261 | Overweight subjects (216 patients with autoimmune thyroiditis) |
| [63] | ↔TSH (also measured fT4 and fT3, but did not compare with 25(OH)D) | 219 | Obese Chinese people (118 with mildly increased TSH) | |
| [64] | ↓TSH, ↑fT4, ↑fT3 | ↔TPOAb, ↔TgAb | 5262 | Healthy controls (4889) and patients with Hashimoto’s thyroiditis (373) |
| [65] | ↓TSH (in patients with Hashimoto’s thyroiditis), ↔fT4, ↔T4, ↔T3 | ↔TPOAb, ↔TgAb | 637 | Healthy controls (176) and patients with Hashimoto’s thyroiditis (461) |
| [66] | ↔TSH | ↑TPOAb (in males), ↔TgAb | 185 | Patients with Hashimoto’s thyroiditis (97) and healthy controls (88) |
| [67] | ↔TSH, ↔fT4, ↔fT3 | ↓TPOAb ↓TgAb | 39 | Euthyroid women with Hashimoto’s thyroiditis |
| [68] | (also measured TSH and fT4, but did not compare with 25(OH)D) | ↓TPOAb (in children with Hashimoto’s thyroiditis) | 152 | Children with Hashimoto’s thyroiditis (78) and healthy controls (74) |
| [69] | (also measured TSH, fT4 and fT3, but did not compare with 25(OH)D) | ↔TPOAb, ↔TgAb | 160 | Hypothyroid patients with and without Hashimoto’s thyroiditis |
| [70] | ↓TSH, ↔fT4 | 353 | Patients with autoimmune thyroiditis (30%), multinodular goiter (21.81%), Basedow disease (1.98%), postoperative myxedema (6.52%) and other pathologies like single thyroid nodule or partial agenesia (the rest of the patients) | |
| [71] | ↔TSH, ↔fT4, ↔fT3 | ↓TPOAb (during winter, but not during summer) | 933 | Autoimmune thyroiditis |
| [72] | ↔TSH, ↔fT4, ↔fT3 | ↓TPOAb, ↓TgAb | 34 | Autoimmune thyroiditis (women) |
| [73] | ↔TSH, ↔fT4, ↔tT4, ↔fT3, ↔tT3 | ↓TPOAb, ↓TgAb | 32 | Prediabetic women with Hashimoto’s thyroiditis |
| [74] | ↓TSH (in men, n = 2193), ↔fT4 | ↓TPOAb (in women, n = 2163) | 4356 | Euthyroid participants, euthyroid participants with TPOAb, participants with hypothyroidism |
| [75] | ↔TSH, ↑fT4 (in patients with Hashimoto’s thyroiditis) | ↔TSHAb, ↔TPOAb ↔TgAb | 159 | Patients with Hashimoto’s thyroiditis (88) and control subjects (71) |
| ↔fT4, ↔TSH in control group | ||||
| [76] | ↔ TSH, ↔ fT4, ↔ fT3 | ↓TPOAb | 200 | Patients with Hashimoto’s Thyroiditis (100) and heathy euthyroid controls (100) |
| [77] | ↔T4, ↔T3 | 21 | Hyperthyroid patients | |
| [78] | ↔TSH, ↔fT4, ↔fT3 | ↔TPOAb, ↔TgAb | 226 | Patients with Graves’ disease (51), euthyroid Hashimoto’s thyroiditis (61), Hashimoto’s thyroiditis receiving hormone therapy (63) and healthy controls (51) |
| [79] | ↓TSH, ↔fT4 | ↔TPOAb, ↔TgAb, ↔TSHRAb | 776 | Patients with Graves’ disease (148), Hashimoto’s thyroiditis (221) and participants with normal thyroid function and negative thyroid autoantibodies (407) |
| [80] | ↔TSH, ↔fT4 | 224 | Patients with diagnosed or suspected thyroid disease (hypo- and hyperthyroidism, thyroid nodule, and/or cancer) | |
| [81] | ↓TSH (in patients with Hashimoto’s thyroiditis) (also measured T4 and T3, but did not compare with 25(OH)D) | ↔TPOAb | 86 | Patients with hypothyroid Hashimoto’s thyroiditis (41) and healthy euthyroid persons (45) |
| [82] | ↔TSH (also measured fT4 and TgAb, but did not compare with 25(OH)D) | ↔TPOAb | 136 | Children with Hashimoto’s thyroiditis (68) and healthy children (68) |
| [83] | ↔TSH, ↔fT4, ↔fT3 | ↓TPOAb, ↔TgAb | 394 | Patients with Hashimoto’s thyroiditis (194) and healthy controls (200) |
| [84] | ↓TSH, ↔fT4, ↑tT4, ↔fT3, ↔tT3 | ↔TPOAb, ↔TgAb | 169 | Patients with hypothyroid Hashimoto’s thyroiditis (90) and healthy controls (79) |
| [85] | ↔TSH (also measured fT4 and fT3, but did not compare with 25(OH)D) | ↔TPOAb, ↔TgAb, ↓TSHRAb | 2 case control studies: (1) 210 (2) 171 | 2 case control studies: (1) Patients with Graves’ disease (70), Hashimoto’s thyroiditis (70) and healthy controls (70) (2) Women with post-partum thyroiditis (57) and euthyroid mothers as controls (114) |
| [86] | (also measured TSH, fT4 and fT3, but did not compare with 25(OH)D) | ↓TPOAb (in patients with autoimmune thyroid disorder), ↔TSHRAb | 304 | Patients with autoimmune thyroid disorder (111) and without autoimmune thyroid disorder (193) |
| [87] | ↔TSH, ↔T4, ↔T3 | 25 | Infants with congenital hypothyroidism | |
| [88] | ↓fT3 (also measured TSH, fT4, tT4 and tT3, but did not compare with 25(OH)D) | 108 | Patients with hyperthyroidisms (55) and healthy controls (53) | |
| [89] | (also measured TSH, fT4 and T3, but did not compare with 25(OH)D) | ↔TBII, ↔TSAb | 143 | Patients with Graves’ disease |
| [90] | ↔ TSH, ↔ fT4, ↔ fT3 | ↑ TSHRAb | 188 | Patients with Graves’ disease who received radioiodine therapy (128) and healthy controls (60) |
| [91] | ↔TSH, ↔fT4, ↔fT3 | ↓TSHRAb, ↔TPOAb, ↔TgAb | 140 | Patients with Graves’ disease (70) and healthy controls (70) |
| [92] | ↔ Thyroid function (described by the levels of TSH, tT4, tT3 and TPOAb) | 398 | Healthy controls (109) and patients with thyroid nodules (289) | |
| [93] | ↓TSH, ↔Tg | ↔TgAb | 1161 | Patients with papillary thyroid cancer |
| [94] | ↔TSH | 548 | Female patients with papillary thyroid cancer | |
| [95] | ↓TSH | ↓TPOAb | 820 | Patients with papillary thyroid cancer |
| [41] | ↔TSH | 433 | Patients with benign thyroid nodules and thyroid carcinomas | |
| [96] | ↓TSH, ↔fT4, ↑fT3 | 1706 | Patients with papillary thyroid carcinoma (1578) and benign thyroid diseases (128) | |
| [97] | ↓TSH, ↔fT4, ↔fT3 | (also measured TPOAb, TSHRAb and TgAb, but did not compare with 25(OH)D) | 567 | Patients with type 2 diabetes mellitus (389) and healthy controls (178) |
| [98] | ↔TSH, ↔fT4 | 151 | Patients with metabolic disorders | |
| [99] | ↓TSH, ↑fT4, ↑fT3 | ↓TPOAb, ↓TgAb | 59 | Women with post-partum thyroiditis; hypothyroid (14), euthyroid with post-partum thyroiditis (14), with non-autoimmune hypothyroidism (16) and healthy controls (15) |
| [100] | ↔TSH, ↓fT3, ↔fT4 | ↔TPOAb, ↔TgAb | 283 | Pregnant women with vitamin D deficiency |
| [101] | ↔TSH, ↔fT4, ↔fT3 | 132 | Women in early pregnancy (1st trimester) | |
| [102] | ↔TSH, ↔fT4, ↔fT3 | ↔TPOAb, ↔TgAb | 50 | Pregnant women |
| [103] | ↑TSH, ↓fT4, ↔tT4, ↓fT3, ↔tT3 | 277 | Women in 2nd trimester of pregnancy | |
| [104] | ↓TSH, ↔fT4 | ↓TPOAb, ↓TgAb | 200 | Pregnant woman with subclinical hypothyroidism and gestational diabetes mellitus (100) and healthy pregnant woman (100) |
| [105] | ↔TSH, ↔fT4, ↔fT3 | ↔TPOAb, ↔TgAb | 50 | Women with polycystic ovary syndrome (autoimmune thyroid disease detected in 12 patients) |
| Reference | Vitamin D Therapy/Supplementation Caused the Following Changes in the Levels of TSH, Thyroid Hormones and Thyroglobulin: | Vitamin D Therapy/Supplementation Caused the Following Changes in the Levels of Anti-Thyroid Antibodies: | Number of Participants | Diagnosis of Participants |
|---|---|---|---|---|
| [114] (meta-analysis) | ↔ TSH, ↔ fT4, ↔ fT3 | ↓TPOAb, ↔TgAb | 258 | Hashimoto’s thyroiditis |
| [111] | ↓TSH, ↓fT3, ↓fT4, ↓Tg | ↓TPOAb, ↓TgAb | 11,017 | Participants in wellness program receiving vitamin D supplementation (2% hypothyroid and 22% subclinical hypothyroid) |
| [113] | ↓TSH (in autoimmune thyroiditis positive group) | 198 | Autoimmune thyroiditis negative (103) and autoimmune thyroiditis positive (95) | |
| [115] | ↔TSH, ↔fT4 | ↓TPOAb | 100 | Patients with autoimmune thyroid disorder |
| [116] | ↔TSH | ↔TPOAb, ↔TgAb | 34 | Female patients with Hashimoto’s thyroiditis |
| [112] | ↓TSH, ↔T4, ↔T3 | 201 | Hypothyroid patients | |
| [117] | Vitamin D/selenomethionine combination therapy caused: ↔TSH, ↔fT4, ↔fT3, ↓fT4/fT3 | Vitamin D/selenomethionine combination therapy caused: ↓TPOAb, ↓TgAb | 38 | Euthyroid women with Hashimoto’s thyroiditis |
| [118] | Vitamin D/dehydroepiandrosterone(DHEA) combination therapy caused: ↓TSH, ↔fT4, ↔fT3 | Vitamin D therapy or vitamin D/dehydroepiandrosterone (DHEA) combination therapy caused: ↓TPOAb, ↓TgAb | 35 | Women with Hashimoto’s thyroiditis |
| [119] | ↔TSH, ↔fT4, ↔fT3, ↔fT4/fT3 | ↓TPOAb, ↓TgAb | 62 | Women with Hashimoto’s thyroiditis |
| [120] | ↔TSH | ↔TPOAb | 56 | Hashimoto’s thyroiditis |
| [121] | ↓TSH, ↑T4 | 12 | Hypothyroid patients | |
| [122] | ↔TSH, ↔fT4, ↔fT3 | ↓TPOAb, ↓TgAb | 59 | Non-lactating L-thyroxine-treated women with postpartum thyroiditis (38) and matched healthy postpartum women (21) |
| [123] | ↔TSH, ↔fT4, ↔fT3 | ↓TPOAb, ↓TgAb | 57 | Levothyroxine-treated euthyroid women with Hashimoto’s thyroiditis and vitamin D insufficiency |
| [124] | ↔TSH, ↔fT4, ↔fT3 | ↓TPOAb, ↓TgAb | 34 | Women with Hashimoto’s thyroiditis |
| [125] | ↔TSH, ↔fT4, ↔fT3 | ↓TPOAb, ↓TgAb | 37 | Euthyroid men with autoimmune thyroiditis |
| [126] | ↔TSH, ↔fT4, ↔fT3 | ↓TPOAb, ↓TgAb | 36 | Men with euthyroid Hashimoto’s thyroiditis and testosterone deficiency |
| [73] | Vitamin D/metformin combination therapy caused: ↓TSH, ↔fT4, ↔fT3 | Vitamin D/ metformin combination therapy caused: ↓TPOAb, ↓TgAb | 32 | Women with Hashimoto’s thyroiditis |
| [127] | ↓TSH (in patients receiving vitamin D supplementation), ↔T4, ↔T3 | ↔TPOAb, ↓TgAb (in patients receiving vitamin D supplementation) | 40 | Female patients with Hashimoto’s thyroiditis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Babić Leko, M.; Jureško, I.; Rozić, I.; Pleić, N.; Gunjača, I.; Zemunik, T. Vitamin D and the Thyroid: A Critical Review of the Current Evidence. Int. J. Mol. Sci. 2023, 24, 3586. https://doi.org/10.3390/ijms24043586
Babić Leko M, Jureško I, Rozić I, Pleić N, Gunjača I, Zemunik T. Vitamin D and the Thyroid: A Critical Review of the Current Evidence. International Journal of Molecular Sciences. 2023; 24(4):3586. https://doi.org/10.3390/ijms24043586
Chicago/Turabian StyleBabić Leko, Mirjana, Iva Jureško, Iva Rozić, Nikolina Pleić, Ivana Gunjača, and Tatijana Zemunik. 2023. "Vitamin D and the Thyroid: A Critical Review of the Current Evidence" International Journal of Molecular Sciences 24, no. 4: 3586. https://doi.org/10.3390/ijms24043586
APA StyleBabić Leko, M., Jureško, I., Rozić, I., Pleić, N., Gunjača, I., & Zemunik, T. (2023). Vitamin D and the Thyroid: A Critical Review of the Current Evidence. International Journal of Molecular Sciences, 24(4), 3586. https://doi.org/10.3390/ijms24043586







