Zebrafish as a Potential Model for Neurodegenerative Diseases: A Focus on Toxic Metals Implications
Abstract
1. Introduction
2. Methodology
3. Results
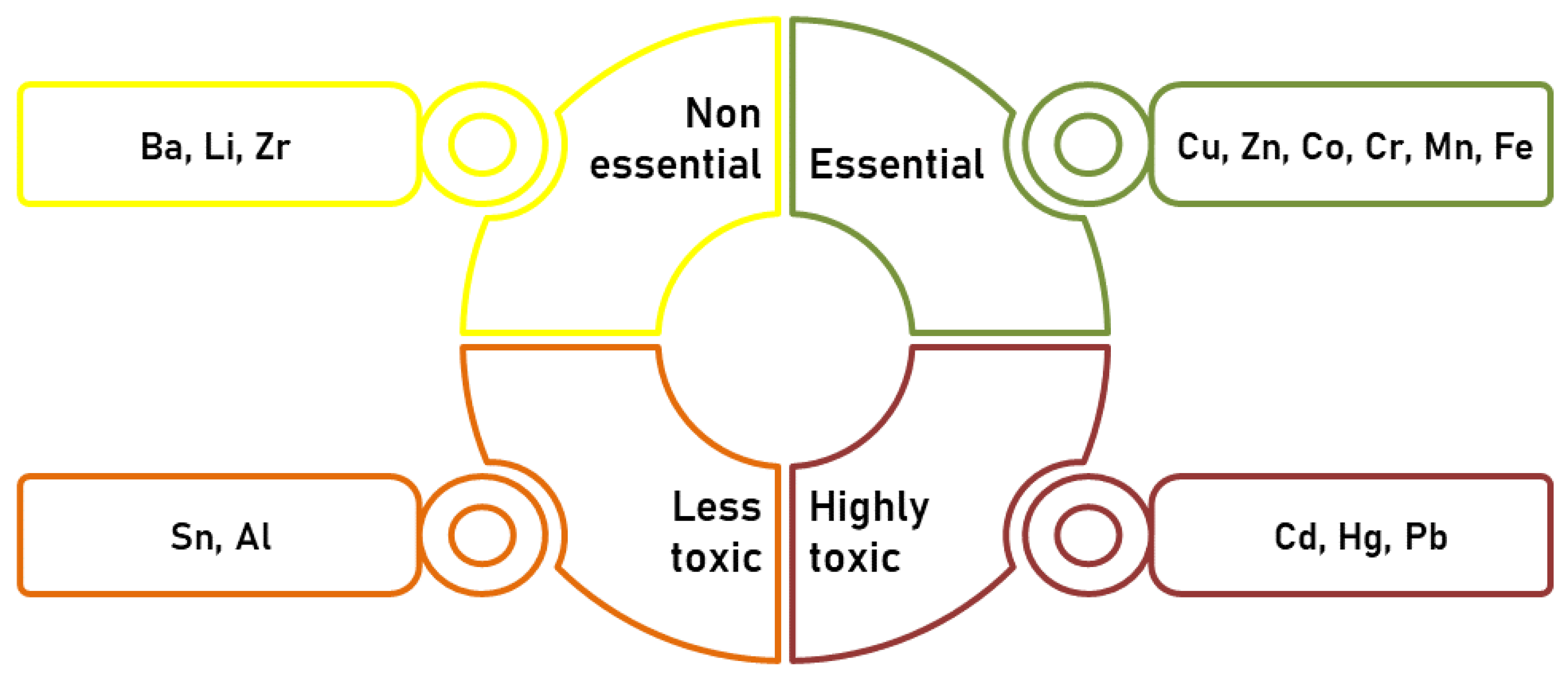
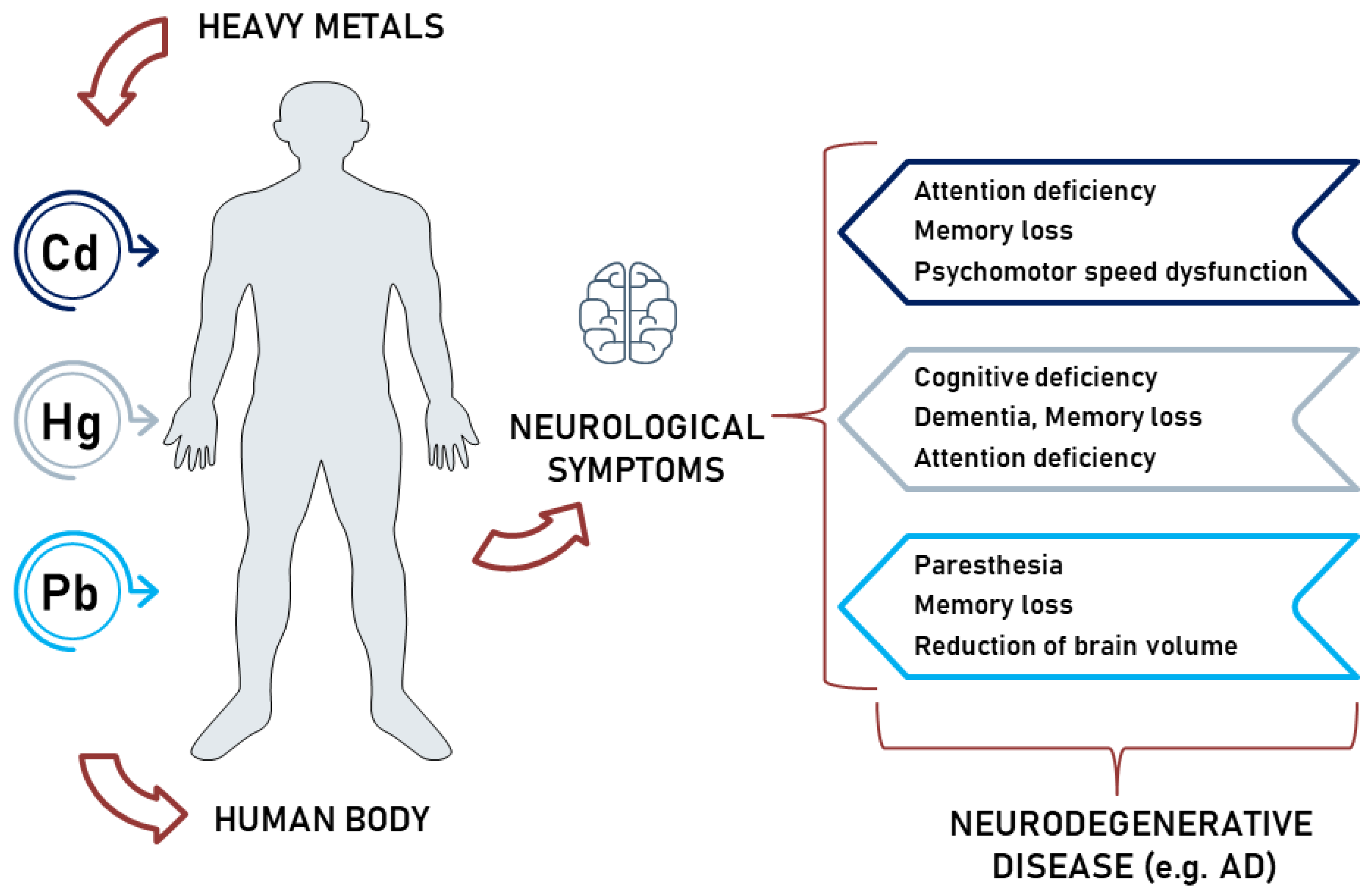
3.1. Neurotoxic Effects of Heavy Metals
3.1.1. Cd-Induced Neurotoxicity
3.1.2. Hg-Induced Neurotoxicity
3.1.3. Pb-Induced Neurotoxicity
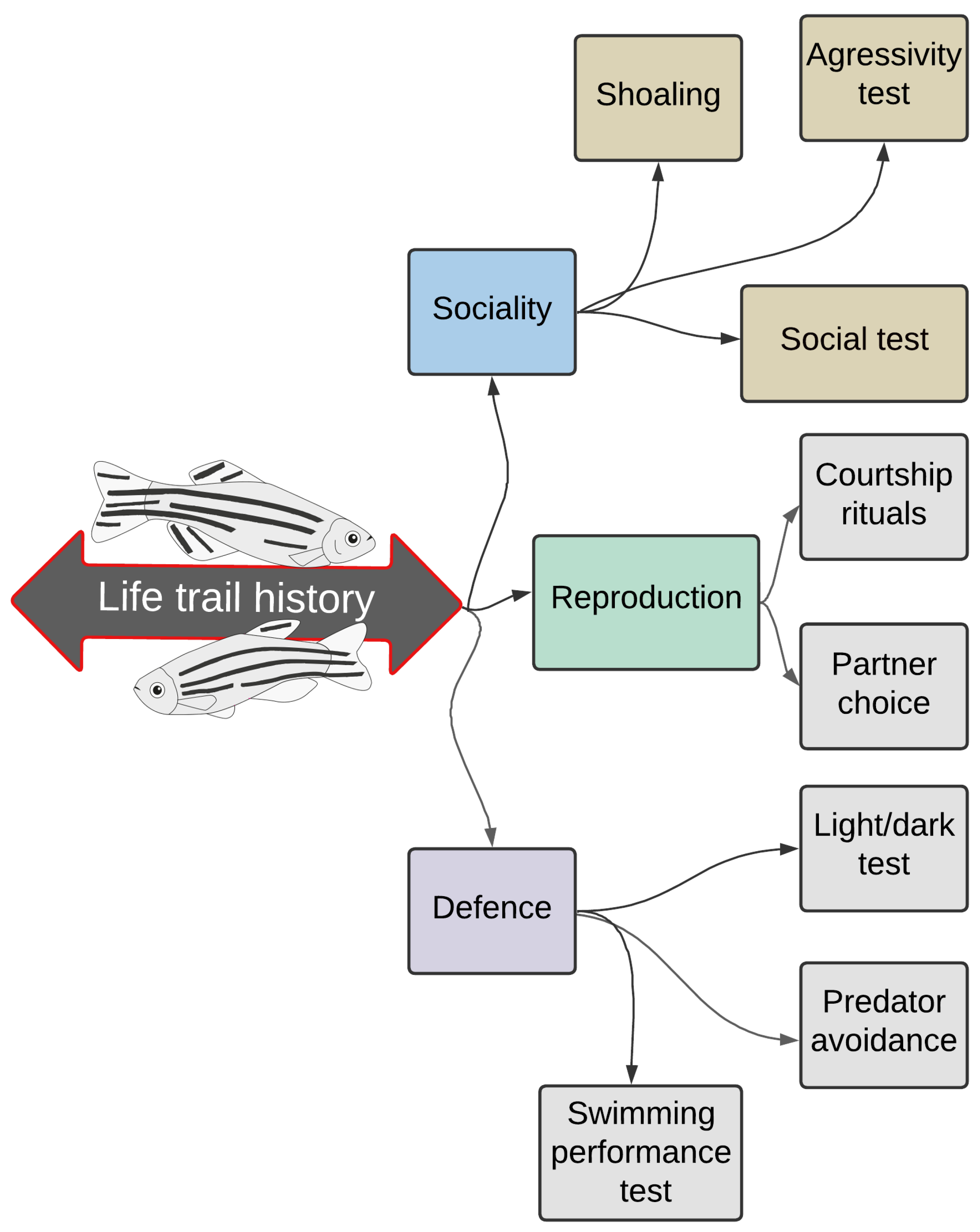
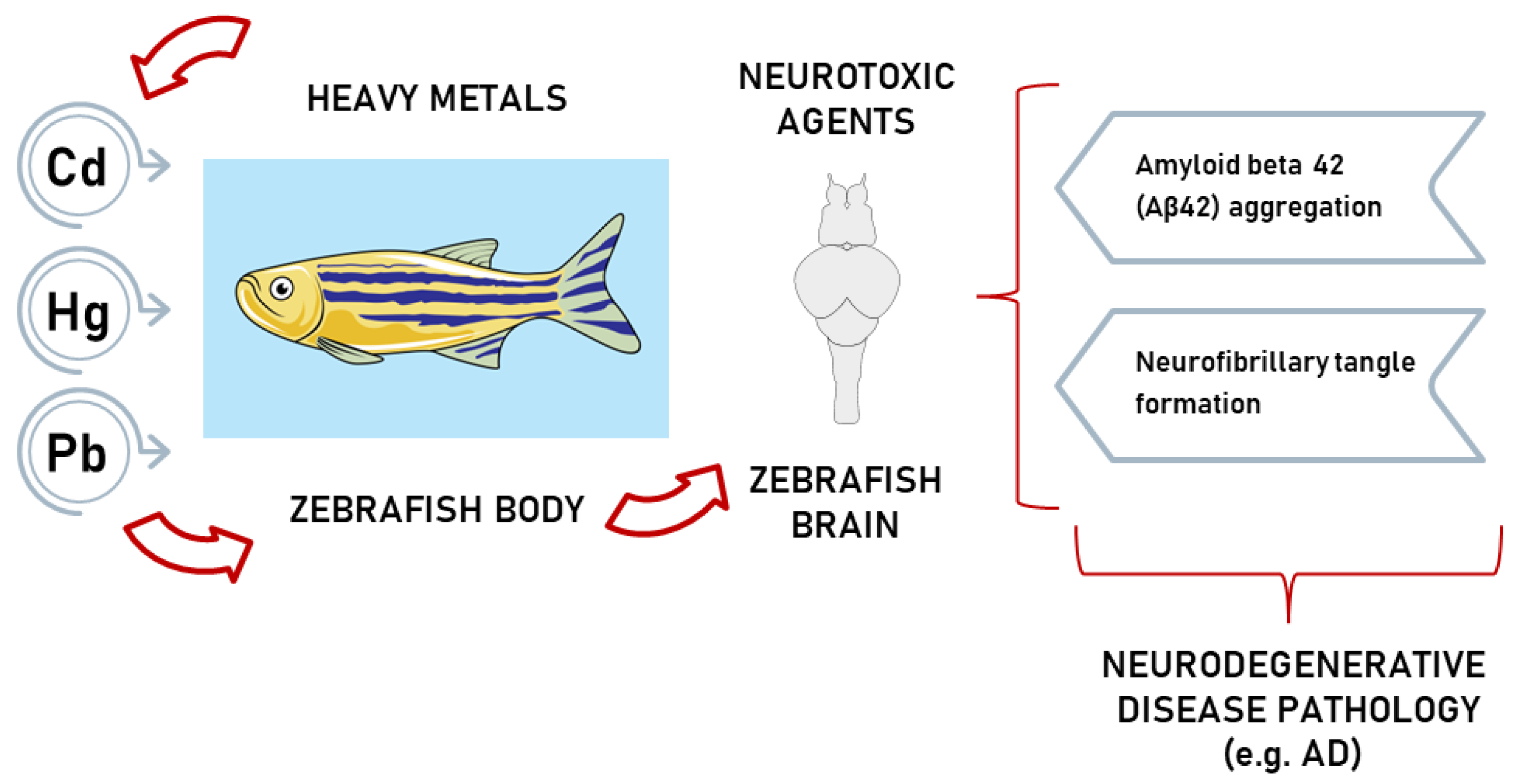
3.2. Zebrafish as a Research Model for Heavy-Metal-Induced Neurological Disorders
3.2.1. Zebrafish as a Model for Heavy-Metal-Induced AD
3.2.2. Zebrafish as a Model for Heavy-Metal-Induced PD
3.3. Experimental Studies Linking Heavy Metal Exposure in Zebrafish and Neurological Disorders
3.3.1. Heavy Metals’ Effects on Zebrafish Swimming Performance Tests
3.3.2. Use of the Social Test on Zebrafish to Assess the Implications of Heavy Metals in Neurological Disorders
3.3.3. Use of the Mirror Test on Zebrafish to Assess the Implications of Heavy Metals in Neurological Disorders
3.3.4. Correlation between Behavioural, Biochemical, Histological, and Bioaccumulation Experimental Studies Linking Heavy Metal Exposure in Zebrafish and Neurological Disorders
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vacca, M.; Fernandes, M.; Spanetta, M.; Placidi, F.; Izzi, F.; Lombardo, C.; Mercuri, N.B.; Liguori, C. Depressive Symptoms in Patients with Epilepsy and Clinically Associated Features in a Single Tertiary Center. Neurol. Sci. 2022, 43, 1965–1974. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.F.; Ding, J.; Li, X.; Mao, L.Y.; Wang, X. Clinical Risk Factors for Depressive Symptoms in Patients with Epilepsy. Acta Neurol. Scand. 2014, 129, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Kalueff, A.V.; Stewart, A.M.; Gerlai, R. Zebrafish as an Emerging Model for Studying Complex Brain Disorders. Trends Pharmacol. Sci. 2014, 35, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Levin, E.D.; Bencan, Z.; Cerutti, D.T. Anxiolytic Effects of Nicotine in Zebrafish. Physiol. Behav. 2007, 90, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Levin, E.D.; Cerutti, D.T. Chapter 15 Behavioral Neuroscience of Zebrafish. In Methods of Behavior Analysis in Neuroscience, 2nd ed.; Buccafusco, J.J., Ed.; CRC Press/Taylor & Francis: Bocca Raton, FL, USA, 2009. [Google Scholar]
- Engeszer, R.E.; Patterson, L.B.; Rao, A.A.; Parichy, D.M. Zebrafish in the Wild: A Review of Natural History and New Notes from the Field. Zebrafish 2007, 4, 21–40. [Google Scholar] [CrossRef]
- Saluja, D.; Jhanji, R.; Kaushal, S.; Verma, B.; Sharma, N.; Singh, R.; Agrawal, S.; Yadav, M.; Kumar, A.; Singh, C.; et al. Importance of Zebrafish as an Efficient Research Model for the Screening of Novel Therapeutics in Neurological Disorders. CNS Neurol. Disord. Drug Targets 2021, 20, 145–157. [Google Scholar] [CrossRef]
- Dohi, E.; Matsui, H. The Utility of Small Fishes for the Genetic Study of Human Age-Related Disorders Finding the Common Shared Genes. Front. Genet. 2022, 13, 928597. [Google Scholar] [CrossRef]
- Dasgupta, S.; Simonich, M.T.; Tanguay, R.L. Zebrafish Behavioral Assays in Toxicology. In High-Throughput Screening Assays in Toxicology; Methods in Molecular Biology; Zhu, H., Xia, M., Eds.; Humana: New York, NY, USA, 2022; Volume 2474, pp. 109–122. [Google Scholar] [CrossRef]
- Spence, R.; Gerlach, G.; Lawrence, C.; Smith, C. The Behaviour and Ecology of the Zebrafish, Danio rerio. Biol. Rev. Camb. Philos. Soc. 2008, 83, 13–34. [Google Scholar] [CrossRef]
- Dutra Costa, B.P.; Moura, L.A.; Gomes Pinto, S.A.; Lima-Maximino, M.; Maximino, C. Zebrafish Models in Neural and Behavioral Toxicology across the Life Stages. Fishes 2020, 5, 23. [Google Scholar] [CrossRef]
- Bailey, J.M.; Oliveri, A.N.; Levin, E.D. Pharmacological Analyses of Learning and Memory in Zebrafish (Danio rerio). Pharmacol. Biochem. Behav. 2015, 139, 103–111. [Google Scholar] [CrossRef]
- Heap, L.A.; Goh, C.C.; Kassahn, K.S.; Scott, E.K. Cerebellar Output in Zebrafish: An Analysis of Spatial Patterns and Topography in Eurydendroid Cell Projections. Front. Neural Circuits 2013, 7, 53. [Google Scholar] [CrossRef] [PubMed]
- Chia, K.; Klingseisen, A.; Sieger, D.; Priller, J. Zebrafish as a Model Organism for Neurodegenerative Disease. Front. Mol. Neurosci. 2022, 15, 940484. [Google Scholar] [CrossRef] [PubMed]
- Ochenkowska, K.; Herold, A.; Samarut, É. Zebrafish Is a Powerful Tool for Precision Medicine Approaches to Neurological Disorders. Front. Mol. Neurosci. 2022, 15, 944693. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, J.-B.; He, K.-J.; Wang, F.; Liu, C.-F. Advances of Zebrafish in Neurodegenerative Disease: From Models to Drug Discovery. Front. Pharmacol. 2021, 12, 713963. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Cao, H. Zebrafish and Medaka: Important Animal Models for Human Neurodegenerative Diseases. Int. J. Mol. Sci. 2021, 22, 10766. [Google Scholar] [CrossRef] [PubMed]
- Caito, S.; Aschner, M. Chapter 11—Neurotoxicity of Metals. In Handbook of Clinical Neurology; Lotti, M., Bleecker, M.L., Eds.; 3rd series; Elsevier: Amsterdam, The Netherlands, 2015; Volume 131, pp. 169–189. [Google Scholar] [CrossRef]
- Jaishankar, M.; Tseten, T.; Anbalagan, N.; Mathew, B.B.; Beeregowda, K.N. Toxicity, Mechanism and Health Effects of Some Heavy Metals. Interdiscip. Toxicol. 2014, 7, 60–72. [Google Scholar] [CrossRef]
- Raikwar, M.K.; Kumar, P.; Singh, M.; Singh, A. Toxic Effect of Heavy Metals in Livestock Health. Vet. World 2008, 1, 28–30. [Google Scholar] [CrossRef]
- Gade, M.; Comfort, N.; Re, D.B. Sex-Specific Neurotoxic Effects of Heavy Metal Pollutants: Epidemiological, Experimental Evidence and Candidate Mechanisms. Environ. Res. 2021, 201, 111558. [Google Scholar] [CrossRef]
- Bjørklund, G.; Dadar, M.; Mutter, J.; Aaseth, J. The Toxicology of Mercury: Current Research and Emerging Trends. Environ. Res. 2017, 159, 545–554. [Google Scholar] [CrossRef] [PubMed]
- López-Berenguer, G.; Peñalver, J.; Martínez-López, E. A Critical Review about Neurotoxic Effects in Marine Mammals of Mercury and Other Trace Elements. Chemosphere 2020, 246, 125688. [Google Scholar] [CrossRef] [PubMed]
- Suvarapu, L.N.; Baek, S.O. Determination of Heavy Metals in the Ambient Atmosphere: A Review. Toxicol. Ind. Health 2017, 33, 79–96. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.F.; Li, Y.W.; Liu, Z.H.; Chen, Q.L. Exposure to Mercuric Chloride Induces Developmental Damage, Oxidative Stress and Immunotoxicity in Zebrafish Embryos-Larvae. Aquat. Toxicol. 2016, 181, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Andrade, V.M.; Aschner, M.; Marreilha dos Santos, A.P. Neurotoxicity of Metal Mixtures. Adv. Neurobiol. 2017, 18, 227–265. [Google Scholar] [CrossRef] [PubMed]
- Chin-Chan, M.; Navarro-Yepes, J.; Quintanilla-Vega, B. Environmental Pollutants as Risk Factors for Neurodegenerative Disorders: Alzheimer and Parkinson Diseases. Front. Cell. Neurosci. 2015, 9, 124. [Google Scholar] [CrossRef]
- Lee, H.J.; Park, M.K.; Seo, Y.R. Pathogenic Mechanisms of Heavy Metal Induced-Alzheimer’s Disease. Toxicol. Environ. Health Sci. 2018, 10, 1–10. [Google Scholar] [CrossRef]
- Rabilloud, T.; Lescuyer, P. Proteomics in Mechanistic Toxicology: History, Concepts, Achievements, Caveats and Potential. Proteomics 2015, 15, 1051–1074. [Google Scholar] [CrossRef] [PubMed]
- Rasinger, J.D.; Lundebye, A.-K.; Penglase, S.J.; Ellingsen, S.; Amlund, H. Methylmercury Induced Neurotoxicity and the Influence of Selenium in the Brains of Adult Zebrafish (Danio rerio). Int. J. Mol. Sci. 2017, 18, 725. [Google Scholar] [CrossRef] [PubMed]
- Cariccio, V.L.; Samà, A.; Bramanti, P.; Mazzon, E. Mercury Involvement in Neuronal Damage and in Neurodegenerative Diseases. Biol. Trace Elem. Res. 2019, 187, 341–356. [Google Scholar] [CrossRef] [PubMed]
- Bakulski, K.M.; Seo, Y.A.; Hickman, R.C.; Brandt, D.; Vadari, H.S.; Hu, H.; Park, S.K. Heavy Metals Exposure and Alzheimer’s Disease and Related Dementias. J. Alzheimer’s Dis. 2020, 76, 1215–1242. [Google Scholar] [CrossRef]
- Islam, F.; Shohag, S.; Akhter, S.; Islam, M.R.; Sultana, S.; Mitra, S.; Chandran, D.; Khandaker, M.U.; Ashraf, G.M.; Idris, A.M.; et al. Exposure of Metal Toxicity in Alzheimer's Disease: An Extensive Review. Front. Pharmacol. 2022, 13, 903099. [Google Scholar] [CrossRef]
- Pamphlett, R.; Bishop, D.P.; Kum Jew, S.; Doble, P.A. Age-related Accumulation of Toxic Metals in the Human Locus Ceruleus. PLoS ONE 2018, 13, e0203627. [Google Scholar] [CrossRef]
- Peters, S.; Visser, A.E.; Weisskopf, M.; Kioumourtzoglou, M.-A.; Vermeulen, R. Chapter 40—Metals and neurodegeneration. In Oxford Textbook of Neurologic and Neuropsychiatric Epidemiology; Brayne, C., Feigin, V.L., Launer, L.J., Logroscino, G., Eds.; Oxford University Press: Oxford, UK, 2020; pp. 417–424. [Google Scholar] [CrossRef]
- Tobwala, S.; Wang, H.-J.; Carey, J.W.; Banks, W.A.; Ercal, N. Effects of Lead and Cadmium on Brain Endothelial Cell Survival, Monolayer Permeability, and Crucial Oxidative Stress Markers in an In Vitro Model of the Blood-Brain Barrier. Toxics 2014, 2, 258–275. [Google Scholar] [CrossRef]
- Li, B.; Xia, M.; Zorec, R.; Parpura, V.; Verkhratsky, A. Astrocytes in Heavy Metal Neurotoxicity and Neurodegeneration. Brain Res. 2021, 1752, 147234. [Google Scholar] [CrossRef] [PubMed]
- Kabir, M.T.; Uddin, M.S.; Zaman, S.; Begum, Y.; Ashraf, G.M.; Bin-Jumah, M.N.; Bungau, S.G.; Mousa, S.A.; Abdel-Daim, M.M. Molecular Mechanisms of Metal Toxicity in the Pathogenesis of Alzheimer's Disease. Mol. Neurobiol. 2021, 58, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Thévenod, F. Catch Me if You Can! Novel Aspects of Cadmium Transport in Mammalian Cells. BioMetals 2010, 23, 857–875. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.R.; DeGheselle, O.; Smeets, K.; Van Kerkhove, E.; Cuypers, A. Cadmium-induced Pathologies: Where is the Oxidative Balance Lost (or Not)? Int. J. Mol. Sci. 2013, 14, 6116–6143. [Google Scholar] [CrossRef]
- Yesildag, K.; Gur, C.; Ileriturk, M.; Kandemir, F.M. Evaluation of Oxidative Stress, Inflammation, Apoptosis, Oxidative DNA Damage and Metalloproteinases in the Lungs of Rats Treated with Cadmium and Carvacrol. Mol. Biol. Rep. 2022, 49, 1201–1211. [Google Scholar] [CrossRef]
- Deng, P.; Ma, Q.; Xi, Y.; Yang, L.; Lin, M.; Yu, Z.; Chen, C.; Zhou, Z. Transcriptomic Insight into Cadmium-induced Neurotoxicity in Embryonic Neural Stem/Progenitor Cells. Toxicol. Vitr. 2020, 62, 104686. [Google Scholar] [CrossRef]
- Chow, E.S.; Hui, M.N.; Lin, C.C.; Cheng, S.H. Cadmium Inhibits Neurogenesis in Zebrafish Embryonic Brain Development. Aquat. Toxicol. 2008, 87, 157–169. [Google Scholar] [CrossRef]
- Wang, B.; Du, Y. Cadmium and Its Neurotoxic Effects. Oxid. Med. Cell. Longev. 2013, 2013, 898034. [Google Scholar] [CrossRef]
- Sankhla, M.S.; Sharma, K.; Kumar, R. Heavy Metal Causing Neurotoxicity in Human Health. Int.J. Innov. Res. Sci. Eng. Technol. 2017, 6, 7721–7726. [Google Scholar] [CrossRef]
- Bjørklund, G.; Tinkov, A.A.; Dadar, M.; Rahman, M.M.; Chirumbolo, S.; Skalny, A.V.; Skalnaya, M.G.; Haley, B.E.; Ajsuvakova, O.P.; Aaseth, J. Insights into the Potential Role of Mercury in Alzheimer’s Disease. J. Mol. Neurosci. 2019, 67, 511–533. [Google Scholar] [CrossRef] [PubMed]
- Paduraru, E.; Iacob, D.; Rarinca, V.; Rusu, A.; Jijie, R.; Ilie, O.D.; Ciobica, A.; Nicoara, M.; Doroftei, B. Comprehensive Review Regarding Mercury Poisoning and Its Complex Involvement in Alzheimer’s Disease. Int. J. Mol. Sci. 2022, 23, 1–25. [Google Scholar] [CrossRef]
- Huang, C.F.; Hsu, C.J.; Liu, S.H.; Lin-Shiau, S.Y. Neurotoxicological Mechanism of Methylmercury Induced by Low-Dose and Long-Term Exposure in Mice: Oxidative Stress and Down-Regulated Na+/K(+)-ATPase Involved. Toxicol. Lett. 2008, 176, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Ceccatelli, S.; Daré, E.; Moors, M. Methylmercury-Induced Neurotoxicity and Apoptosis. Chem. Biol. Interact. 2010, 188, 301–308. [Google Scholar] [CrossRef]
- Farina, M.; Aschner, M.; Rocha, J.B.T. Oxidative Stress in MeHg-induced Neurotoxicity. Toxicol. Appl. Pharmacol. 2011, 256, 405–417. [Google Scholar] [CrossRef]
- Chung, Y.P.; Yen, C.C.; Tang, F.C.; Lee, K.I.; Liu, S.H.; Wu, C.C.; Hsieh, S.S.; Su, C.C.; Kuo, C.Y.; Chen, Y.W. Methylmercury Exposure Induces ROS/Akt Inactivation-Triggered Endoplasmic Reticulum Stress-Regulated Neuronal Cell Apoptosis. Toxicology 2019, 425, 152245. [Google Scholar] [CrossRef]
- Berg, K.; Puntervoll, P.; Valdersnes, S.; Goksøyr, A. Responses in the Brain Proteome of Atlantic cod (Gadus morhua) exposed to methylmercury. Aquat. Toxicol. 2010, 100, 51–65. [Google Scholar] [CrossRef]
- Pigatto, P.D.; Costa, A.; Guzzi, G. Are Mercury and Alzheimer’s Disease Linked? Sci. Total Environ. 2018, 613–614, 1579–1580. [Google Scholar] [CrossRef]
- Yang, Y.W.; Liou, S.H.; Hsueh, Y.M.; Lyu, W.S.; Liu, C.S.; Liu, H.J.; Chung, M.C.; Hung, P.H.; Chung, C.J. Risk of Alzheimer’s Disease with Metal Concentrations in Whole Blood and Urine: A Case–Control Study Using Propensity Score Matching. Toxicol. Appl. Pharmacol. 2018, 356, 8–14. [Google Scholar] [CrossRef]
- Vasefi, M.; Ghaboolian-Zare, E.; Abedelwahab, H.; Osu, A. Environmental Toxins and Alzheimer’s Disease Progression. Neurochem. Int. 2020, 141, 104852. [Google Scholar] [CrossRef] [PubMed]
- Mutter, J.; Curth, A.; Naumann, J.; Deth, R.; Walach, H. Does Inorganic Mercury Play a Role in Alzheimer’s Disease? A Systematic Review and an Integrated Molecular Mechanism. J. Alzheimer’s Dis. 2010, 22, 357–374. [Google Scholar] [CrossRef]
- Wallin, C.; Friedemann, M.; Sholts, S.B.; Noormägi, A.; Svantesson, T.; Jarvet, J.; Roos, P.M.; Palumaa, P.; Gräslund, A.; Wärmländer, S.K.T.S. Mercury and Alzheimer’s Disease: Hg(II) Ions Display Specific Binding to the Amyloid-β Peptide and Hinder Its Fibrillization. Biomolecules 2020, 10, 44. [Google Scholar] [CrossRef]
- Xu, L.; Zhang, W.; Liu, X.; Zhang, C.; Wang, P.; Zhao, X. Circulatory Levels of Toxic Metals (Aluminum, Cadmium, Mercury, Lead) in Patients with Alzheimer’s Disease: A Quantitative Meta-Analysis and Systematic Review. J. Alzheimer’s Dis. 2018, 62, 361–372. [Google Scholar] [CrossRef]
- Lee, J.W.; Choi, H.; Hwang, U.K.; Kang, J.C.; Kang, Y.J.; Kim, K.I.; Kim, J.H. Toxic Effects of Lead Exposure on Bioaccumulation, Oxidative Stress, Neurotoxicity, and Immune Responses in Fish: A Review. Environ. Toxicol. Pharmacol. 2019, 68, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Virgolini, M.B.; Aschner, M. Chapter 5—Molecular mechanisms of lead neurotoxicity. In Advances in Neurotoxicology; Aschner, M., Costa, L.G., Eds.; Academic Press: Cambridge, MA, USA, 2021; Volume 5, pp. 159–213. [Google Scholar] [CrossRef]
- Sharma, P.; Chambial, S.; Shukla, K.K. Lead and Neurotoxicity. Indian J. Clin. Biochem. 2015, 30, 1–2. [Google Scholar] [CrossRef]
- Meyer, D.N.; Crofts, E.J.; Akemann, C.; Gurdziel, K.; Farr, R.; Baker, B.B.; Weber, D.; Baker, T.R. Developmental Exposure to Pb2+ Induces Transgenerational Changes to Zebrafish Brain Transcriptome. Chemosphere 2020, 244, 125527. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.C.; Gao, Z.Y.; Wang, J.; Wu, M.Q.; Hu, S.; Chen, F.; Liu, J.X.; Pan, H.; Yan, C.H. Lead Exposure Induces Alzheimers’s Disease (AD)-like Pathology and Disturbes Cholesterol Metabolism in the Young Rat Brain. Toxicol. Lett. 2018, 296, 173–183. [Google Scholar] [CrossRef]
- Lee, J.; Freeman, J.L. Embryonic Exposure to 10 µg L−1 Lead Results in Female-Specific Expression Changes in Genes Associated with Nervous System Development and Function and Alzheimer’s Disease in Aged Adult Zebrafish Brain. Metallomics 2016, 8, 586–596. [Google Scholar] [CrossRef]
- Wu, J.; Basha, M.R.; Brock, B.; Cox, D.P.; Cardozo-Pelaez, F.; McPherson, C.A.; Harry, J.; Rice, D.C.; Maloney, B.; Chen, D.; et al. Alzheimer’s Disease (AD)-like Pathology in Aged Monkeys After Infantile Exposure to Environmental Metal Lead (Pb): Evidence for a Developmental Origin and Environmental Link for AD. J. Neurosci. 2008, 28, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Freeman, J.L. Zebrafish as a Model for Investigating Developmental Lead (Pb) Neurotoxicity as a Risk Factor in Adult Neurodegenerative Disease: A Mini-review. NeuroToxicology 2014, 43, 57–64. [Google Scholar] [CrossRef]
- Zhang, J.; Peterson, S.M.; Weber, G.J.; Zhu, X.; Zheng, W.; Freeman, J.L. Decreased Axonal Density and Altered Expression Profiles of Axonal Guidance Genes Underlying Lead (Pb) Neurodevelopmental Toxicity at Early Embryonic Stages in the Zebrafish. Neurotoxicol. Teratol. 2011, 33, 715–720. [Google Scholar] [CrossRef] [PubMed]
- de Abreu, M.S.; Genario, R.; Giacomini, A.C.V.V.; Demin, K.A.; Lakstygal, A.M.; Amstislavskaya, T.G.; Fontana, B.D.; Parker, M.O.; Kalueff, A.V. Zebrafish as a Model of Neurodevelopmental Disorders. Neuroscience 2020, 445, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Green, A.J.; Planchart, A. The Neurological Toxicity of Heavy Metals: A Fish Perspective. Comp. Biochem. Physiol. Part C Toxicol. Pharmacol. 2018, 208, 12–19. [Google Scholar] [CrossRef]
- Ghidersa, M.; Mocanu, D.; Robea, M.A.; Plavan, G.; Luca, I.; Ciobică, A.; Mavroudis, I. Behavioural and Metabolical Changes Associated with the Pathophysiology of Alzheimer’s Disease in Zebrafish. Ann. Acad. Rom. Sci. Ser. Biol. Sci. 2021, 10, 66–78. [Google Scholar] [CrossRef]
- d’Amora, M.; Giordani, S. The Utility of Zebrafish as a Model for Screening Developmental Neurotoxicity. Front. Neurosci. 2018, 12, 976. [Google Scholar] [CrossRef]
- Thawkar, B.S.; Kaur, G. Zebrafish as a Promising Tool for Modeling Neurotoxin-Induced Alzheimer’s Disease. Neurotox. Res. 2021, 39, 949–965. [Google Scholar] [CrossRef] [PubMed]
- Newman, M.; Nik, H.M.; Sutherland, G.T.; Hin, N.; Kim, W.S.; Halliday, G.M.; Jayadev, S.; Smith, C.; Laird, A.S.; Lucas, C.W.; et al. Accelerated Loss of Hypoxia Response in Zebrafish with Familial Alzheimer’s Disease-like Mutation of Presenilin 1. Hum. Mol. Genet. 2020, 29, 2379–2394. [Google Scholar] [CrossRef] [PubMed]
- Meleleo, D.; Notarachille, G.; Mangini, V.; Arnesano, F. Concentration-Dependent Effects of Mercury and Lead on Aβ42: Possible Implications for Alzheimer’s Disease. Eur. Biophys. J. 2019, 48, 173–187. [Google Scholar] [CrossRef]
- Klakotskaia, D.; Agca, C.; Richardson, R.A.; Stopa, E.G.; Schachtman, R.; Agca, Y. Memory Deficiency, Cerebral Amyloid Angiopathy, and Amyloid-β Plaques in APP + PS1 Double Transgenic Rat Model of Alzheimer’s Disease. PLoS ONE 2018, 13, 1–16. [Google Scholar] [CrossRef]
- Santana, S.; Rico, E.P.; Burgos, J.S. Can Zebrafish Be Used as Animal Model to Study Alzheimer’s Disease? Am. J. Neurodegener. Dis. 2012, 1, 32–48. [Google Scholar] [PubMed]
- Karran, E.; De Strooper, B. The Amyloid Cascade Hypothesis: Are We Poised for Success or Failure? J. Neurochem. 2016, 139, 237–252. [Google Scholar] [CrossRef] [PubMed]
- Saleem, S.; Kannan, R.R. Zebrafish: An Emerging Real-Time Model System to Study Alzheimer's Disease and Neurospecific Drug Discovery. Cell Death Discov. 2018, 4, 45. [Google Scholar] [CrossRef] [PubMed]
- Richetti, S.K.; Rosemberg, D.B.; Ventura-Lima, J.; Monserrat, J.M.; Bogo, M.R.; Bonan, C.D. Acetylcholinesterase Activity and Antioxidant Capacity of Zebrafish Brain is Altered by Heavy Metal Exposure. Neurotoxicology 2011, 32, 116–122. [Google Scholar] [CrossRef]
- de Lima, D.; Roque, G.M.; de Almeida, E.A. In Vitro and in Vivo Inhibition of Acetylcholinesterase and Carboxylesterase by Metals in Zebrafish (Danio rerio). Mar. Environ. Res. 2013, 91, 45–51. [Google Scholar] [CrossRef]
- Bui Thi, N.H.; Nguyen Thi, N.A.; Audira, G.; Siregar, P.; Liang, S.-T.; Huang, J.-C.; Hsiao, C.-D. Chronic Exposure to Low Concentration Lead Chloride-induced Anxiety and Loss of Aggression and Memory in Zebrafish. Int. J. Mol. Sci. 2020, 21, 1844. [Google Scholar] [CrossRef]
- del Pino, J.; Zeballos, G.; Anadón, M.J.; Moyano, P.; Díaz, M.J.; García, J.M.; Frejo, M.T. Cadmium-induced Cell Death of Basal Forebrain Cholinergic Neurons Mediated by Muscarinic M1 Receptor Blockade, Increase in GSK-3β Enzyme, β-amyloid and Tau Protein Levels. Arch. Toxicol. 2016, 90, 1081–1092. [Google Scholar] [CrossRef]
- Zheng, Q.; Bi, R.; Xu, M.; Zhang, D.-F.; Tan, L.W.; Lu, Y.-P.; Yao, Y.-G. Exploring the Genetic Association of the ABAT Gene with Alzheimer's Disease. Mol. Neurobiol. 2021, 58, 1894–1903. [Google Scholar] [CrossRef]
- Bowery, N.G.; Smart, T.G. GABA and Glycine as Neurotransmitters: A Brief History. Br. J. Pharmacol. 2006, 147, S109–S119. [Google Scholar] [CrossRef]
- Shenoy, A.; Banerjee, M.; Upadhya, A.; Bagwe-Parab, S.; Kaur, G. The Brilliance of the Zebrafish Model: Perception on Behavior and Alzheimer’s Disease. Front. Behav. Neurosci. 2022, 16, 861155. [Google Scholar] [CrossRef]
- Wirbisky, S.E.; Weber, G.J.; Lee, J.W.; Cannon, J.R.; Freeman, J.L. Novel Dose-dependent Alterations in Excitatory GABA During Embryonic Development Associated with Lead (Pb) Neurotoxicity. Toxicol. Lett. 2014, 229, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Cambier, S.; Gonzalez, P.; Mesmer-Dudons, N.; Brèthes, D.; Fujimura, M.; Bourdineaud, J.P. Effects of Dietary Methylmercury on the Zebrafish Brain: Histological, Mitochondrial, and Gene Transcription Analyses. Biometals 2012, 25, 165–180. [Google Scholar] [CrossRef] [PubMed]
- Rizek, P.; Kumar, N.; Jog, M.S. An Update on the Diagnosis and Treatment of Parkinson Disease. CMAJ 2016, 188, 1157–1165. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Yang, B.; Ke, T.; Li, S.; Yang, X.; Aschner, M.; Chen, P. Mechanisms of Metal-induced Mitochondrial Dysfunction in Neurological Disorders. Toxics 2021, 9, 142. [Google Scholar] [CrossRef]
- Singh, A.; Kukreti, R.; Saso, L.; Kukreti, S. Oxidative Stress: A Key Modulator in Neurodegenerative Diseases. Molecules 2019, 24, 1583. [Google Scholar] [CrossRef]
- Doyle, J.M.; Croll, R.P. A Critical Review of Zebrafish Models of Parkinson’s Disease. Front. Pharmacol. 2022, 13, 835827. [Google Scholar] [CrossRef]
- Wang, Z.; Zhao, H.; Xu, Y.; Zhao, J.; Song, Z.; Bi, Y.; Li, Y.; Lan, X.; Pan, C.; Foulkes, N.S.; et al. Early-life Lead Exposure Induces Long-term Toxicity in the Central Nervous System: From Zebrafish Larvae to juveniles and Adults. Sci. Total Environ. 2022, 804, 150185. [Google Scholar] [CrossRef]
- Dantzig, P.I. Parkinson’s Disease, Macular Degeneration and Cutaneous Signs of Mercury Toxicity. J. Occup. Environ. Med. 2006, 48, 656. [Google Scholar] [CrossRef]
- Bera, K.; Das, A.K.; Nag, M.; Basak, S. Development of a Rhodamine-rhodanine-based Fluorescent Mercury Sensor and its Use to Monitor Real-time Uptake and Distribution of Inorganic Mercury in Live Zebrafish Larvae. Anal. Chem. 2014, 86, 2740–2746. [Google Scholar] [CrossRef]
- Amlund, H.; Lundebye, A.K.; Boyle, D.; Ellingsen, S. Dietary Selenomethionine Influences the Accumulation and Depuration of Dietary Methylmercury in Zebrafish (Danio rerio). Aquat. Toxicol. 2015, 158, 211–217. [Google Scholar] [CrossRef]
- Zheng, J.L.; Yuan, S.S.; Wu, C.W.; Lv, Z.M. Acute Exposure to Waterborne Cadmium Induced Oxidative Stress and Immunotoxicity in the Brain, Ovary and Liver of Zebrafish (Danio rerio). Aquat. Toxicol. 2016, 180, 36–44. [Google Scholar] [CrossRef]
- Sonnack, L.; Kampe, S.; Muth-Köhne, E.; Erdinger, L.; Henny, N.; Hollert, H.; Schäfers, C.; Fenske, M. Effects of Metal Exposure on Motor Neuron Development, Neuromasts and the Escape Response of Zebrafish Embryos. Neurotoxicol. Teratol. 2015, 50, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Barnhill, L.M.; Murata, H.; Bronstein, J.M. Studying the Pathophysiology of Parkinson’s Disease Using Zebrafish. Biomedicines 2020, 8, 197. [Google Scholar] [CrossRef]
- Monaco, A.; Capriello, T.; Grimaldi, M.C.; Schiano, V.; Ferrandino, I. Neurodegeneration in Zebrafish Embryos and Adults after Cadmium Exposure. Eur. J. Histochem. 2017, 61, 2833. [Google Scholar] [CrossRef] [PubMed]
- Monaco, A.; Grimaldi, M.C.; Ferrandino, I. Neuroglial Alterations in the Zebrafish Brain Exposed to Cadmium Chloride. J. Appl. Toxicol. 2016, 36, 1629–1638. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Zhao, H.; Wang, Z.; Gao, H.; Liu, J.; Li, K.; Song, Z.; Yuan, C.; Lan, X.; Pan, C.; et al. Developmental Exposure to Environmental Levels of Cadmium Induces Neurotoxicity and Activates Microglia in Zebrafish Larvae: From the Perspectives of Neurobehavior and Neuroimaging. Chemosphere 2022, 291, 132802. [Google Scholar] [CrossRef]
- Monnet-Tschudi, F.; Zurich, M.-G.; Boschat, C.; Corbaz, A.; Honegger, P. Involvement of Environmental Mercury and Lead in the Etiology of Neurodegenerative Diseases. Rev. Environ. Health 2006, 21, 105–117. [Google Scholar] [CrossRef] [PubMed]
- Strungaru, S.-A.; Robea, M.A.; Plavan, G.; Todirascu-Ciornea, E.; Ciobica, A.; Nicoara, M. Acute Exposure to Methylmercury Chloride Induces Fast Changes in Swimming Performance, Cognitive Processes and Oxidative Stress of Zebrafish (Danio rerio) as Reference Model for Fish Community. J. Trace Elem. Med. Biol. 2018, 47, 115–123. [Google Scholar] [CrossRef]
- Sperandio, G. Cadmium Affects Boldness, Freezing and Swimming Behavior in Perca fluviatilis—European Perch. Master’s Thesis, University of Siena, Siena, Italy, 2015. [Google Scholar] [CrossRef]
- Grandjean, P.; Weihe, P.; White, R.F.; Debes, F.; Araki, S.; Yokoyama, K.; Murata, K.; Sørensen, N.; Dahl, R.; Jørgensen, P.J. Cognitive Deficit in 7-year-old Children with Prenatal Exposure to Methylmercury. Neurotoxicol. Teratol. 1997, 19, 417–428. [Google Scholar] [CrossRef]
- Ahmad, F.; Liu, P. (Ascorb)ing Pb Neurotoxicity in the Developing Brain. Antioxidants 2020, 9, 1311. [Google Scholar] [CrossRef]
- Little, E.E.; Finger, S.E. Swimming Behavior as an Indicator of Sublethal Toxicity in Fish. Environ. Toxicol. Chem. 1990, 9, 13–19. [Google Scholar] [CrossRef]
- Vezza, P.; Libardoni, F.; Manes, C.; Tsuzaki, T.; Bertoldi, W.; Kemp, P.S. Rethinking Swimming Performance Tests for Bottom-Dwelling Fish: The Case of European Glass Eel (Anguilla anguilla). Sci. Rep. 2020, 10, 16416. [Google Scholar] [CrossRef]
- Plaut, I. Critical Swimming Speed: Its Ecological Relevance. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2001, 131, 41–50. [Google Scholar] [CrossRef]
- Agnisola, C.; Uliano, E.; Simoniello, P.; Motta, C. Effects of Cadmium on Skeletal Muscles and Swimming Performance of Danio rerio. J. Biol. Res. 2011, 84, 11–13. [Google Scholar] [CrossRef]
- Capriello, T.; Grimaldi, M.C.; Cofone, R.; D’Aniello, S.; Ferrandino, I. Effects of Aluminium and Cadmium on Hatching and Swimming Ability in Developing Zebrafish. Chemosphere 2019, 222, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Liao, G.; Wang, P.; Zhu, J.; Weng, X.; Lin, S.; Huang, J.; Xu, Y.; Zhou, F.; Zhang, H.; Tse, L.A.; et al. Joint Toxicity of Lead and Cadmium on the Behavior of Zebrafish Larvae: An Antagonism. Aquat. Toxicol. 2021, 238, 105912. [Google Scholar] [CrossRef]
- Tu, H.; Fan, C.; Chen, X.; Liu, J.; Wang, B.; Huang, Z.; Zhang, Y.; Meng, X.; Zou, F. Effects of Cadmium, Manganese, and Lead on Locomotor Activity and Neurexin 2a Expression in Zebrafish. Environ. Toxicol. Chem. 2017, 36, 2147–2154. [Google Scholar] [CrossRef] [PubMed]
- Dou, C.; Zhang, J. Effects of Lead on Neurogenesis During Zebrafish Embryonic Brain Development. J. Hazard. Mater. 2011, 194, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Ogi, A.; Licitra, R.; Naef, V.; Marchese, M.; Fronte, B.; Gazzano, A.; Santorelli, F.M. Social Preference Tests in Zebrafish: A Systematic Review. Front. Vet. Sci. 2021, 7, 590057. [Google Scholar] [CrossRef]
- Ilie, O.D.; Duta, R.; Jijie, R.; Nita, I.B.; Nicoara, M.; Faggio, C.; Dobrin, R.; Mavroudis, I.; Ciobica, A.; Doroftei, B. Assessing Anti-Social and Aggressive Behavior in a Zebrafish (Danio rerio) Model of Parkinson’s Disease Chronically Exposed to Rotenone. Brain Sci. 2022, 12, 898. [Google Scholar] [CrossRef]
- Zhao, J.; Zhang, Q.; Zhang, B.; Xu, T.; Yin, D.; Gu, W.; Bai, J. Developmental Exposure to Lead at Environmentally Relevant Concentrations Impaired Neurobehavior and NMDAR-dependent BDNF Signaling in Zebrafish Larvae. Environ. Pollut. 2020, 257, 113627. [Google Scholar] [CrossRef]
- Gerlai, R.; Lahav, M.; Guo, S.; Rosenthal, A. Drinks Like a Fish: Zebra Fish (Danio rerio) as a Behavior Genetic Model to Study Alcohol Effects. Pharmacol. Biochem. Behav. 2000, 67, 773–782. [Google Scholar] [CrossRef] [PubMed]
- Strungaru, S.-A.; Plavan, G.; Ciobica, A.; Nicoara, M.; Robea, M.A.; Solcan, C.; Petrovici, A. Toxicity and Chronic Effects of Deltamethrin Exposure on Zebrafish (Danio rerio) as a Reference Model for Freshwater Fish Community. Ecotoxicol. Environ. Saf. 2019, 171, 854–862. [Google Scholar] [CrossRef] [PubMed]
- Way, G.P.; Ruhl, N.; Snekser, J.L.; Kiesel, A.L.; McRobert, S.P. A Comparison of Methodologies to Test Aggression in Zebrafish. Zebrafish 2015, 12, 144–151. [Google Scholar] [CrossRef]
- Fontana, B.D.; Meinerz, D.L.; Rosa, L.V.C.; Mezzomo, N.J.; Silveira, A.; Giuliani, G.S.; Quadros, V.A.; Filho, G.L.B.; Blaser, R.E.; Rosemberg, D.B. Modulatory Action of Taurine on Ethanol-induced Aggressive Behavior in Zebrafish. Pharmacol. Biochem. Behav. 2016, 141, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Kalueff, A.V.; Gebhardt, M.; Stewart, A.M.; Cachat, J.M.; Brimmer, M.; Chawla, J.S.; Craddock, C.; Kyzar, E.J.; Roth, A.; Landsman, S.; et al. Towards a Comprehensive Catalog of Zebrafish Behavior 1.0 and beyond. Zebrafish 2013, 10, 70–86. [Google Scholar] [CrossRef]
- Zheng, X.J.; Wang, T.; Tian, Y.; Hu, Z.Q.; Shang, N. Research on Anxiety-like Neurobehavior of Zebrafish Caused by Lead Exposure and Its Mechanism. Chin. J. Ind. Hyg. Occup. Dis. 2021, 39, 407–411. (In Chinese) [Google Scholar] [CrossRef]
- Spulber, S.; Raciti, M.; Dulko-Smith, B.; Lupu, D.; Rüegg, J.; Nam, K.; Ceccatelli, S. Methylmercury Interferes with Glucocorticoid receptor: Potential Role in the Mediation of Developmental Neurotoxicity. Toxicol. Appl. Pharmacol. 2018, 354, 94–100. [Google Scholar] [CrossRef]
- Maximino, C.; Araujo, J.; Leão, L.K.R.; Grisólia, A.B.A.; Oliveira, K.R.M.; Lima, M.G.; Batista, E.J.O.; Crespo-López, M.E.; Gouveia, A., Jr.; Herculano, A.M. Possible Role of Serotoninergic System in the Neurobehavioral Impairment Induced by Acute Methylmercury Exposure in Zebrafish (Danio rerio). Neurotoxicol. Teratol. 2011, 33, 727–734. [Google Scholar] [CrossRef]
- Abu Bakar, N.; Mohd Sata, N.S.; Ramlan, N.F.; Wan Ibrahim, W.N.; Zulkifli, S.Z.; Abdullah, C.A.C.; Ahmad, S.; Amal, M.N.A. Evaluation of the Neurotoxic Effects of Chronic Embryonic Exposure with Inorganic Mercury on Motor and Anxiety-like Responses in Zebrafish (Danio rerio) Larvae. Neurotoxicol. Teratol. 2017, 59, 53–61. [Google Scholar] [CrossRef]
- Senger, M.R.; Rosemberg, D.B.; Seibt, K.J.; Dias, R.D.; Bogo, M.R.; Bonan, C.D. Influence of Mercury Chloride on Adenosine Deaminase Activity and Gene Expression in Zebrafish (Danio rerio) Brain. Neurotoxicology 2010, 31, 291–296. [Google Scholar] [CrossRef]
- Senger, M.R.; Rico, E.P.; de Bem Arizi, M.; Frazzon, A.P.; Dias, R.D.; Bogo, M.R.; Bonan, C.D. Exposure to Hg2+ and Pb2+ Changes NTPDase and Ecto-5′-nucleotidase Activities in Central Nervous System of Zebrafish (Danio rerio). Toxicology 2006, 226, 229–237. [Google Scholar] [CrossRef]
- Zhu, J.; Wang, C.; Gao, X.; Zhu, J.; Wang, L.; Cao, S.; Wu, Q.; Qiao, S.; Zhang, Z.; Li, L. Comparative Effects of Mercury Chloride and Methylmercury Exposure on Early Neurodevelopment in Zebrafish Larvae. RSC Adv. 2019, 9, 10766–10775. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, P.; Dominique, Y.; Massabuau, J.C.; Boudou, A.; Bourdineaud, J.P. Comparative Effects of Dietary Methylmercury on Gene Expression in Liver, Skeletal Muscle, and Brain of the Zebrafish (Danio rerio). Environ. Sci. Technol. 2005, 39, 3972–3980. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Wang, A.P.; Li, W.F.; Shi, R.; Jin, H.T.; Wei, J.F. Sensitive Biomarkers Identification for Differentiating Cd and Pb Induced Toxicity on Zebrafish embryos. Environ. Toxicol. Pharmacol. 2017, 56, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Han, E.J.; Ahn, G.; Kwak, I.S. Effects of Thermal Stress-induced Lead (Pb) Toxicity on Apoptotic Cell Death, Inflammatory Response, Oxidative Defense, and DNA Methylation in Zebrafish (Danio rerio) Embryos. Aquat. Toxicol. 2020, 224, 105479. [Google Scholar] [CrossRef] [PubMed]
- Komoike, Y.; Matsuoka, M. Developmental Adverse Effects of Trace Amounts of Lead: Evaluation Using Zebrafish model. Front. Pharmacol. 2022, 13, 1014912. [Google Scholar] [CrossRef]
- Chen, J.; Chen, Y.; Liu, W.; Bai, C.; Liu, X.; Liu, K.; Li, R.; Zhu, J.-H.; Huang, C. Developmental Lead Acetate Exposure Induces Embryonic Toxicity and Memory Deficit in Adult Zebrafish. Neurotoxicol. Teratol. 2012, 34, 581–586. [Google Scholar] [CrossRef]
- Kataba, A.; Botha, T.L.; Nakayama, S.M.M.; Yohannes, Y.B.; Ikenaka, Y.; Wepener, V.; Ishizuka, M. Environmentally Relevant Lead (Pb) Water Concentration Induce Toxicity in Zebrafish (Danio rerio) Larvae. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 2022, 252, 109215. [Google Scholar] [CrossRef]
- Kataba, A.; Botha, T.L.; Nakayama, S.M.M.; Yohannes, Y.B.; Ikenaka, Y.; Wepener, V.; Ishizuka, M. Acute Exposure to Environmentally Relevant Lead Levels Induces Oxidative Stress and Neurobehavioral Alterations in Larval Zebrafish (Danio rerio). Aquat. Toxicol. 2020, 227, 105607. [Google Scholar] [CrossRef]
- Zhu, B.; Wang, Q.; Shi, X.; Guo, Y.; Xu, T.; Zhou, B. Effect of Combined Exposure to Lead and Decabromodiphenyl Ether on Neurodevelopment of Zebrafish Larvae. Chemosphere 2016, 144, 1646–1654. [Google Scholar] [CrossRef] [PubMed]
- Green, A.J.; Mattingly, C.J.; Planchart, A. Cadmium Disrupts Vestibular Function by Interfering with Otolith Formation. bioRxiv 2017. preprint. [Google Scholar] [CrossRef]
- Zhang, T.; Zhou, X.Y.; Ma, X.F.; Liu, J.X. Mechanisms of Cadmium-caused Eye Hypoplasia and Hypopigmentation in Zebrafish Embryos. Aquat. Toxicol. 2015, 167, 68–76. [Google Scholar] [CrossRef]
- Ruiter, S.; Sippel, J.; Bouwmeester, M.C.; Lommelaars, T.; Beekhof, P.; Hodemaekers, H.M.; Bakker, F.; van den Brandhof, E.-J.; Pennings, J.L.A.; van der Ven, L.T.M. Programmed Effects in Neurobehavior and Antioxidative Physiology in Zebrafish Embryonically Exposed to Cadmium: Observations and Hypothesized Adverse Outcome Pathway Framework. Int. J. Mol. Sci. 2016, 17, 1830. [Google Scholar] [CrossRef]
- Wang, L.; Al-sawafi, A.G.; Yan, Y. Biochemical Changes in the Tissues of Zebrafish (Danio rerio) Exposed to Organophosphorous Pesticides and Heavy Metal Cadmium. Int. J. Environ. Sci. Dev. 2017, 8, 707–714. [Google Scholar] [CrossRef]
- Al-sawafi, A.G.A.; Wang, L.; Yan, Y. Cadmium Accumulation and Its Histological Effect on Brain and Skeletal Muscle of Zebrafish. J. Heavy Met. Toxic. Dis. 2017, 2, 2–10. [Google Scholar] [CrossRef]
| Heavy Metal | Effects on Human Behaviour and CNS | Effects on Fish Behaviour and CNS | References |
|---|---|---|---|
| Cd | Causes muscle weakness, withdrawal, and impairs cognitive function, may be linked to the development of PD | Impairs swimming ability and causes deficiency in fish functions | [44,104] |
| Hg | Causes memory loss, other cognitive impairments and tremors | Reduces swimming activity and changes in response to stimuli | [103,105] |
| Pb | Causes deficits in cognitive functions and could be related to the development of AD | Impairs memory and learning, decreases locomotion (speed) and changes in response to stimuli | [69,106] |
| Chemical | Developmental Stage | Exposure Duration | Behavioural Alterations | Other Alterations in the Organisms | Reference |
|---|---|---|---|---|---|
| MeHg | larvae | 2 hpf–5 dpf | Increased spontaneity and swimming activity | Interfered with glucocorticoid receptor (GR) signalling | [124] |
| MeHg | adult | 24 h | Presence of anxiety-like behaviour | Intensified increase in the amount of MDA, decreased extracellular serotonin, increased OS, produced mitochondrial dysfunction | [125] |
| HgCl2 | embryos/ larvae | 5–72 hpf | Motor deficit, disruption in the anxiety-like behaviour, and decreased swimming activity | Increased embryo mortality rate, biochemical changes in proteins, lipids, carbohydrates and nucleic acid | [126] |
| HgCl2 | adult | 24–96 h | No changes in swimming behaviour | Inhibited ADA activity | [127] |
| HgCl2 | adult | 24 h, 96 h, 30 days | Behavioural observations not noted | Altered AChE activity and antioxidant capacity | [79] |
| HgCl2 | adult | 24 h, 96 h, 30 days | No changes in the swimming pattern were observed | No observed mortality; during 96 h—inhibited the hydrolysis of adenosine triphosphate (ATP), adenosine diphosphate (ADP) and adenosine monophosphate (AMP); after 30 days—ATP hydrolysis returned to the control levels, ADP hydrolysis was strongly increased and AMP hydrolysis remained inhibited. | [128] |
| HgCl2 | embryos (6 hpf)/ larvae | 24 h | Trajectory disturbance, no significant decrease in the average moving distance | Delayed hatching, decreased body length and eye size, tail bending, increased number of apoptotic cells in the brain, downregulated neural development related genes, reduced levels of neurotransmitters (tyrosine, dopamine, and tryptophan) | [129] |
| CH3HgCl | Significant decrease in the average moving distance and trajectory disturbance | ||||
| CH3HgCl | adult (male) | 7, 21, and 63 days | No decrease in motility | Generated higher levels of bioaccumulation in brain tissue, no increase in mortality | [130] |
| Pb Nitrate—Pb(NO3)2 | embryos/ larvae | 24–96 hpf | Behavioural observations not noted | Decreased survival rate in embryos, reduced hatching rate, increased ROS production and the mRNA expression levels of antioxidant-relevant genes | [131] |
| Pb(NO3)2 | embryos (3–4 hpf) | 1–7 dpf | Behavioural observations not noted | Decreased survival rate, increased apoptosis and transcriptional levels of two genes related to antioxidant defence and two apoptosis-related genes, spinal malformations (curvature) | [132] |
| Pb(C2H3O2)2 | embryos/ larvae | 0–6 dpf | Sluggish action, slow swimming movements, slow escape action | Increased mortality rate and incidence of “S” body malformation, downregulated expression of two genes in the diencephalon and dorsal hindbrain—extensive apoptosis of neuron cells, downregulated expression of two genes related to a decrease in the number of neural cells | [114] |
| Pb(C2H3O2)2 | embryos (6 hpf)/ larvae | 6–72 hpf | Behavioural observations not noted | No difference in viability, shortened hatching period and body length, defects of swim bladder inflation, oedema formation in cerebral area, hatching period and body length, increased ROS levels and the expression levels of OS response-related genes | [133] |
| Pb(C2H3O2)2 | embryos (2 hpf) | 12–36 hpf | Behavioural observations not noted | Alterations in neuronal growth, decreased axonal density, interfered with the expression of 3 genes involved in axonogenesis (downregulated sonic hedgehog signalling molecule a (shha) and ephrin type-A receptor A4b (epha4b) genes, and overexpression of netrin (netrin2) gene) | [67] |
| Pb(C2H3O2)2 | embryos (2 hpf)/ larvae/ adults (exposure only during embryogenesis) | 2–120 hpf | Decreased larval moving distance and acceleration, elevated acceleration in juvenile zebrafish, increased travelling distance and velocity in adults | Decreased survival rate, slightly increased hatching rate, decreased body length, severe malformations (scoliosis, tail and head deformities), tendency to neuron loss, extensive apoptosis, induced varicosities formation in adult zebrafish brain | [92] |
| Pb(C2H3O2)2 | adult (exposure only during embryogenesis) | 1–72 hpf | Behavioural observations not noted | Alterations in genes associated with nervous system’s development and function, more pronounced in a set of 89 genes associated with AD (including human homologous APP and APOE) | [64] |
| Pb(C2H3O2)2 | adult | 24 h, 96 h, 30 days | Behavioural observations not noted | Altered AChE activity but not antioxidant capacity | [79] |
| Pb(C2H3O2)2 | adult | 24 h, 96 h, 30 days | No changes in the swimming pattern were observed | No observed mortality; during 96 h—caused a significant decrease only on ATP hydrolysis; after 30 days— promoted the inhibition of ATP, ADP and AMP hydrolysis | [128] |
| Pb acetate trihydrate— Pb(C2H3O2)2*3(H2O) | embryos/ larvae | 6–120 hpf | Altered spontaneous movement (decreased tail bend frequency in embryos), hyperactivity in larvae (increased swimming activity and speed), impaired learning/memory performance (reduction in the accuracy rate and an increase of time to reach the food end) | Induced malformations (bent spine) | [134] |
| Pb(C2H3O2)2*3(H2O) | embryos (2.5 hpf)/ larvae | 96 hpf | Induced muscular twitching | Attenuated burst activity in embryos, induced changes in the mRNA expression levels of antioxidant and OS response enzymes | [135] |
| Pb(C2H3O2)2*3(H2O) | larvae (120 hpf) | 30 min | Enhanced hyperactivity (significant increases in distance covered, swimming speed and mobile frequency as well as increased distance covered and speed under light illumination) | Upregulated the mRNA expression of genes related to increased ROS | [136] |
| Pb(C2H3O2)2*3(H2O) and deca-brominated diphenyl ether (BDE-209) | embryos (2 hpf)/ larvae | 2–144 hpf | Reduced average swimming speed | No observed interference with hatching percentage, growth rate, or survival percentage, increased malformation (axial spinal curvature), decreased dorsal axon length, Downregulated the expression of three CNS genes (mbp, α1-tubulin, and gfap), increase in ROS, lipid peroxidation (increased MDA levels), DNA damage, perturbation of the antioxidant system, (decrease in GSH, reduction of SOD activity) | [137] |
| CdCl2 | embryos/ larvae | 4 hpf–7 dpf | Hyperactivity and increased rotational movement | Induced reduction in saccule otolith diameter, pronounced changes in the otolith’s ultrastructure, altered expression level of a gene important for vestibular Ca sensing and transport | [138] |
| CdCl2 | embryos/ larvae | 2.5–96 hpf | Behavioural observations not noted | Induced malformations (reduced body size, trunk abnormalities including hyphosis typified by dorsal convex curvature of the vertebral column and lordosis typified by dorsal concave curvature of the vertebral column, hypopigmentation, head hypoplasia, microphthalmia, reduced interorbital distance), increased mortality, reduced expression of genes labelling the neural crest and its derivative pigment cells, blockage of neural crest formation, inhibition of specification of pigment cells | [139] |
| CdCl2 | embryos (≤1 hpf) | 24–72 hpf | Affected the escape response | Increased mortality rate, no observed effects on hatching rate, lowered number of normally developing primary and secondary motor neurons, neuromast damage | [97] |
| CdCl2 | embryos/ adult (exposure only during embryogenesis) | 0–72 hpf | Hyperactivity, impaired stress handling (increased duration in the stress response) | Reduced embryo survival, altered DNA methylation, altered body antioxidant physiology (decreased glutathione peroxidase GPx, decreased GSH, increase oxidized glutathione GSSG, no effects observed on activity of glutathione reductase GR and SOD) | [140] |
| CdCl2 | adult | 0–96 h | Decreased activity, loss of equilibrium, restlessness, abnormal swimming behaviour, rapid gill movement | Increased AChE activity in the brain, increased SOD and CAT activity in the brain, decreased protein content in brain tissue, increased total lipid content, bioaccumulation factor in the body was 30 mg·L−1 | [141] |
| Cd acetate—C4H6CdO4 | embryos/ larvae | 24–96 hpf | Behavioural observations not noted | Decreased survival rate in embryos, reduced hatching rate, increased ROS production and the mRNA expression levels of antioxidant-relevant genes | [131] |
| C4H6CdO4 | adult | 24 h, 96 h, 30 days | Behavioural observations not noted | Generated no alterations in AChE activity or antioxidant capacity | [79] |
| Cd | adult (female) | 24 h, 96 h | Behavioural observations not noted | Increased ROS, nitric oxide and MDA levels in the brain, no significant alteration of Cu/Zn-SOD and CAT levels, up-regulated the mRNA, protein and activity levels of iNOS and COX-2 in the brain (associated with inflammatory response) | [96] |
| Cd | adult | 0–25 days | Induced erratic swimming and aggressiveness, hyperventilation | Increased mortality rate, increased bioaccumulation factor values in body, histopathological changes in the brain (degeneration of Purkinje cells, different extents of granule cell loss, neutrophil loss, aggregation area of gliosis, various degrees of necrosis) | [142] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paduraru, E.; Iacob, D.; Rarinca, V.; Plavan, G.; Ureche, D.; Jijie, R.; Nicoara, M. Zebrafish as a Potential Model for Neurodegenerative Diseases: A Focus on Toxic Metals Implications. Int. J. Mol. Sci. 2023, 24, 3428. https://doi.org/10.3390/ijms24043428
Paduraru E, Iacob D, Rarinca V, Plavan G, Ureche D, Jijie R, Nicoara M. Zebrafish as a Potential Model for Neurodegenerative Diseases: A Focus on Toxic Metals Implications. International Journal of Molecular Sciences. 2023; 24(4):3428. https://doi.org/10.3390/ijms24043428
Chicago/Turabian StylePaduraru, Emanuela, Diana Iacob, Viorica Rarinca, Gabriel Plavan, Dorel Ureche, Roxana Jijie, and Mircea Nicoara. 2023. "Zebrafish as a Potential Model for Neurodegenerative Diseases: A Focus on Toxic Metals Implications" International Journal of Molecular Sciences 24, no. 4: 3428. https://doi.org/10.3390/ijms24043428
APA StylePaduraru, E., Iacob, D., Rarinca, V., Plavan, G., Ureche, D., Jijie, R., & Nicoara, M. (2023). Zebrafish as a Potential Model for Neurodegenerative Diseases: A Focus on Toxic Metals Implications. International Journal of Molecular Sciences, 24(4), 3428. https://doi.org/10.3390/ijms24043428







